An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.11(12); 2021


Original research
Impact of public-funded health insurances in india on health care utilisation and financial risk protection: a systematic review, bhageerathy reshmi.
1 Department of Health Information Management, Manipal College of Health Professions, Manipal Academy of Higher Education (MAHE), Manipal, Karnataka, India
Bhaskaran Unnikrishnan
2 Department of Community Medicine, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, Karnataka, India
3 Department of Health Information, Public Health Evidence South Asia, Prasanna School of Public Health, Manipal Academy of Higher Education (MAHE), Manipal, Karnataka, India
Shradha S Parsekar
Ratheebhai vijayamma.
4 Manipal Institute of Communication, MAHE, Manipal, Karnataka, India
Bhumika Tumkur Venkatesh
Associated data.
bmjopen-2021-050077supp001.pdf
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information. The datasets used and/or analysed during the current study are available from the corresponding author on request.
Universal Health Coverage aims to address the challenges posed by healthcare inequalities and inequities by increasing the accessibility and affordability of healthcare for the entire population. This review provides information related to impact of public-funded health insurance (PFHI) on financial risk protection and utilisation of healthcare.
Systematic review.
Data sources
Medline (via PubMed, Web of Science), Scopus, Social Science Research Network and 3ie impact evaluation repository were searched from their inception until 15 July 2020, for English-language publications.
Eligibility criteria
Studies giving information about the different PFHI in India, irrespective of population groups (above 18 years), were included. Cross-sectional studies with comparison, impact evaluations, difference-in-difference design based on before and after implementation of the scheme, pre–post, experimental trials and quasi-randomised trials were eligible for inclusion.
Data extraction and synthesis
Data extraction was performed by three reviewers independently. Due to heterogeneity in population and study design, statistical pooling was not possible; therefore, narrative synthesis was performed.
Utilisation of healthcare, willingness-to-pay (WTP), out-of-pocket expenditure (including outpatient and inpatient), catastrophic health expenditure and impoverishment.
The impact of PFHI on financial risk protection reports no conclusive evidence to suggest that the schemes had any impact on financial protection. The impact of PFHIs such as Rashtriya Swasthy Bima Yojana, Vajpayee Arogyashree and Pradhan Mantri Jan Arogya Yojana showed increased access and utilisation of healthcare services. There is a lack of evidence to conclude on WTP an additional amount to the existing monthly financial contribution.
Different central and state PFHIs increased the utilisation of healthcare services by the beneficiaries, but there was no conclusive evidence for reduction in financial risk protection of the beneficiaries.
Registration
Not registered.
Strengths and limitations of this study
- Inclusion of all kinds of empirical evidence to answer the research question about impact of public-funded health insurance (PFHI) schemes in India.
- This is one of the very few reviews that has used a systematic methodology to provide latest evidence on the impact of the newly launched Pradhan Mantri Jan Arogya Yojana scheme in India.
- Choice of quality appraisal tool, due to unavailability of other tools for this kind of study, was a limitation.
- Multiple PFHI (state-specific and central) schemes in India (with different benefit packages) and modifications in the schemes due to changes in central/state governments led to high data heterogeneity.
- Due to heterogeneity in data, we could not provide the pooled estimate via meta-analysis. However, results were explained via a narrative synthesis.
Introduction
India has a complex and mixed healthcare framework with presence of parallel public and private healthcare systems. 1 2 There is a stark difference in government spending on both public and private healthcare. 3 Health policies in India have been guided by the principle of equity with prioritising the needs of the poor and underprivileged. 4 Out-of-pocket expenditure (OOPE) for health is one of the important factors while addressing the inequities in healthcare, and in India, it is an important source of healthcare financing. It is estimated that, in India, around 71% of the healthcare spending is met by OOPE. This not only is an immediate financial burden to the poor households but also pushes the households into a never-ending poverty trap. 5 Health-related OOPE poses a threat to the principle of financial risk protection and adds to the unaffordability and inaccessibility of healthcare for the poor. High OOPE also leads to catastrophic health expenditure (CHE), which is the increase in healthcare payment by a household, beyond the threshold, where the threshold is defined as the household’s income or capacity to pay. This is further divided into catastrophe 1, where healthcare OOPE exceeds by 10% of the household’s consumption expenditure, and catastrophe 2, if OOPE exceeds to more than 40% of the household’s non-food expenditure. The increase in OOPE affects the rural population marginally more than the urban population and the effect of OOPE is more pronounced among the people living below the poverty line (BPL) than those above the poverty line (APL), as BPL people are pushed more into poverty than APL, due to the high OOPE, when measured via the increase in poverty head counts. 5
Over the years, government of India has rolled out different initiatives to address the healthcare-related inequities in India. The public healthcare system was revised and reframed as the National Rural Health Mission in 2005, later restructured as National Health Mission in 2014. 5 6 Other initiatives like Janani Suraksha Yojana and the public funded health insurance (PFHI) schemes such as Rashtriya Swasthya Bima Yojana (RSBY) were also introduced to address the health inequalities, improve health outcomes and provide financial risk protection. 6 Many states sponsored health insurance (HI) schemes, viz., the Vajpayee Arogyashree Scheme (VAS) by Karnataka, Comprehensive Health Insurance Scheme (CHIS) by Kerala and Chief Minister Health Insurance Scheme (CMHIS) by Tamil Nadu, which have been introduced for ensuring financial protection of the vulnerable population.
Challenges posed by healthcare inequalities and inequities like OOPE can also be addressed via the Universal Health Coverage (UHC). The UHC, as defined by the WHO, means that all people and communities can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship. The UHC aims towards increasing the accessibility and affordability of healthcare for the entire population. The definition of UHC is embodied in its three objectives, that is, equity, quality and financial protection. 7
The twelfth 5-year plan of the government of India acknowledges the importance of UHC as it introduces a work plan for achieving UHC for the 1.3 billion population of the country. The agenda for this plan is based on the principle of providing affordable, accessible and good quality healthcare with financial protection to the people of the country. 8 The provision of UHC has been included in the National Health Policy of India (2017). To achieve the UHC, government of India announced the ‘Ayushman Bharat’ programme in 2018 with two initiatives, that is, (a) Health and Wellness center and (b) National health protection scheme —Pradhan Mantri Jan Arogya Yojana (PMJAY), that is intended to cover around 500 million beneficiaries (from vulnerable families) and is intended to cover up to Indian National Rupees (INR) 500 000 per family, per year, for secondary and tertiary hospitalisation. 9
The addition of PMJAY scheme to the various existing PFHI (central and state) schemes aims to increase the UHC, by increasing the affordability and accessibility of good quality healthcare. It is important to assess whether these schemes (including PMJAY) have been proven to be effective in improving health outcomes and providing financial protection to the vulnerable population. Following the principles of UHC, willingness to pay (WTP) for a particular HI scheme can also be used as an indicator to assess the affordability and effectiveness of a scheme in providing good quality healthcare. Additionally, data on beneficiaries willing to pay more or contribute more for a HI scheme (viz., CGHS) indirectly provide information on their satisfaction with the services provided by the scheme, therefore, making it an indicator to assess effectiveness of the scheme. The previous systematic review 10 on assessing the effectiveness of PFHI schemes in India was conducted before complete rolling out of the PMJAY and, therefore, did not include findings on the effectiveness of the scheme (PMJAY). Also, this review 10 did not provide information on the WTP component of assessing impact of the HI schemes. The present review was, therefore, conducted with an aim to provide information related to effectiveness of the central and state-funded HI schemes (including the PMJAY scheme) via healthcare utilisation, WTP and financial risk protection of the beneficiaries. This review was planned to answer the following research question: (a) What is the impact of PFHI schemes on access and utilisation of healthcare, willingness-to-pay and financial risk protection in India?
This systematic review follows the methodology by Cochrane handbook for systematic review of interventions 11 and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist was used to report the review. 12
Criteria for including studies in the review
- Population: population group above 18 years of age enrolled in a PFHI scheme in India.
- Intervention: HI schemes funded by either central or state government, and that covers, range of services such as hospitalisation, out-patient charges, medicine costs, treatment procedures, etc. Different PFHI schemes in India, for example, RSBY, VAS, CMHIS and PMJAY were eligible to be included. Private or community-based HIs were not eligible to be included. Mixture of HIs was excluded provided a study carried out subgroup analysis for PFHIs.
- Comparison: comparison group comprises of people who did not receive any PFHI services.
- Outcomes: this review includes the following outcomes: (a) utilisation of healthcare, (b) WTP, (c) financial risk protection measured in terms of OOPE, CHE and impoverishment.
- Study design: cross-sectional studies with comparison, impact evaluations, difference-in-differences design based on before and after implementation of the scheme, pre–post design, experimental trials and quasi-randomised trials were eligible to be included.
Search methods for identification of studies
Electronic databases such as Medline (via PubMed, Web of Science), SCOPUS, Social Science Research Network and International Initiative for impact evaluation (3ie) repository were searched from their inception until 15 July 2020; however, only English publications, published in the last 10 years were considered. References and forward citations of the included studies were scanned through for any additional eligible studies. Keywords were identified before the initiation of the search. The initial search was carried out in PubMed ( online supplemental file 1 ) and was replicated in other databases. Search was conducted by a designated information scientist.
Supplementary data
Data collection.
Result of search strategy was imported to Endnote V.X7 reference manager software. Duplicates were removed and the unique citations were exported to Microsoft Excel spreadsheet for screening.
Selection of studies
Unique citations were subjected to title and abstract screening independently by two reviewers. Eligible abstracts of all the relevant studies as per the inclusion criteria were included for full-text screening (by BTV, ER and SSP) and relevant ones from these were included for analysis. Before initiating full-text screening, we tried to retrieve the full-text articles by contacting authors of the respective articles and the full texts that were not retrieved were excluded. Disagreements were resolved by discussion or by a third reviewer.
Data extraction
Data extraction was done (by ER, BTV, SSP) using a predesigned data extraction form. Information on variables such as bibliographic details (author names, publication year, journal name); study details (information about the objectives of the study and research question addressed); study setting (name of the state, rural/urban); participant characteristics (age, gender, socioeconomic status, occupation); intervention details (name and type of HI, mode of delivery of the HI, incentives given, healthcare services covered, time duration of seeking HI, any additional HIs); comparison details; outcome details (information about changes in accessibility of healthcare, utilisation of healthcare services, OOPE, WTP, health outcomes like morbidity and mortality, measurement of the outcomes, method used for measurement, time at which the outcome was measured) and study design details (type of study design and analysis) were extracted.
After pilot testing of the data extraction form, it was revised according to the modifications suggested by the team. Disagreements among the reviewers, during data extraction, were resolved by consensus, if still not resolved, third reviewer was approached for resolving the disagreements. Extracted data from all the included studies were cross-checked and independent extraction was done for one-third randomly selected studies.
Methodological quality
The methodological quality of the included studies was assessed using Effective Public Health Practice Project Quality Assessment Tool (EPHPP). 13 This tool assesses methodological quality of the quantitative studies based on questions under the following seven domains, that is, (a) selection bias, (b) study design, (c) confounders, (d) blinding, (e) data collection method, (f) withdrawals and dropouts, (g) intervention integrity and (h) analysis. Quality assessment using this scale was performed independently by reviewers in groups of two. After discussion, global rating for the scale was followed and studies were marked as (1) methodologically strong, if none of the domains had any weak rating, (2) moderate, if at least one domain was marked as weak and (3) weak, if two or more domains were marked as weak. Quality assessment was performed using Microsoft excel spreadsheet.
Data analysis
Due to heterogeneity in data, narrative synthesis was performed to answer the research question. The results are summarised based on outcomes and types of PFHIs. The effect measures of included studies such as mean difference or correlation coefficients with appropriate CI and/or p values are reported.
Public and patient involvement
We did not involve public or patient during the process of this review.
The literature search on electronic databases generated 555 citation yield, out of which 179 were duplicates. Additionally, 17 records were identified from forward and backward reference checking. After title and abstract screening of 393 citations, 157 were included for full-text screening, of which finally 25 articles were included for data synthesis. Schematic representation of the selection process is shown in figure 1 .

PRISMA flow diagram. PFHI, public-funded health insurance; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Characteristics of included studies
The summary of study characteristics is given in table 1 and the detailed characteristics of included studies are given in online supplemental file 1 .
Summary characteristics of included studies
| Serial number | Study characteristic | Summary |
| 1. | Geographical location | Out of the 25 included studies, 10 studies were conducted nationally, and one was conducted in 12 cities—Bhubaneshwar, Thiruvananthapuram, Ahmedabad, Chandigarh, Meerut, Patna, Jabalpur, Lucknow, Hyderabad, Kolkata, Mumbai and Delhi. Other studies were conducted in different states. Studies covering northern region of India were conducted in Uttar Pradesh, Haryana and Punjab. Studies covering southern region of India were undertaken in Karnataka, Andhra Pradesh, Kerala and Tamil Nadu. Remaining studies were carried out in eastern region, ., Jharkhand, Bihar, Chhattisgarh and western region, ., Maharashtra. |
| 2. | Population | Population among the included studies differed in characteristics. General population was included in nine studies. Around seven studies comprised of below poverty line (BPL) households. A mixed population from rural and urban households was considered in three studies. One study comprised of patients selected from Rashtriya Swasthya Bima Yojana (RSBY) empaneled hospitals and key stakeholders. One study included Self-help group members or head of the households. One study comprised of socially excluded households focusing on Scheduled Castes, Muslims and upper caste poor. Two studies comprised of a mix population of BPL and above poverty line households. One study comprised of Central Government Health Scheme (CGHS) and Ex-servicemen Contributory Health Scheme (ECHS) principal beneficiaries, empaneled private healthcare providers and officials of the schemes across 12 Indian cities. |
| 3. | Type of Insurance | Central government-funded health insurance (HI): about 14 studies were conducted on central government-funded HI schemes, that is, RSBY. One study was conducted on Pradhan Mantri Jan Arogya Yojana (PMJAY). Three studies were conducted on CGHS. Two studies were conducted on Employee State Insurance Scheme. State government funded HI: three studies each were conducted on Vajpayee Arogyashree Scheme (VAS) in Karnataka and Rajiv Arogya Shree (RAS) in Andhra Pradesh. One study each reported on CHIS (Philip ) and ECHS. Any government-funded HI: remaining other studies were generally all PFHI. |
| 4. | Study design | Impact evaluation including quasi-randomised designs was used in eight studies. Observational study design was used in five studies. Secondary data analysis was performed in 11 studies. Mixed method approach was used in one study. |
| 5. | Outcomes | The impact of different PFHI schemes (including state insurance schemes) on financial risk protection were reported by 13 studies. Impact of RAS was assessed by single study. Five studies assessed the impact of CHIS on utilisation of healthcare. One study evaluated the impact of PMJAY on healthcare utilisation. Hospitalisation rate was reported in two studies with the implementation of RAS. Two studies reported hospital utilisation rate with implementation of VAS. |
| 6. | Methodological quality | Out of 25 studies, 3 were of moderate quality, 2 weak methodological quality and remaining others were of high quality. |
Impact of PFHI on financial risk protection, utilisation of healthcare and WTP
This systematic review provides evidence on the impact of different PFHI schemes that have been operational in India. These schemes are funded by the central government, viz., RSBY, CGHS, Employee State Insurance Scheme, Swavlamban, Nirmaya-Disability Health Insurance Scheme and PMJAY and by the state governments like VAS (Karnataka), Rajiv Arogya Shree (Andhra Pradesh) and CHIS (Tamil Nadu). The eligibility criteria and benefits offered under each scheme vary according to different state governments. More information on these PFHI schemes is given in box 1 .
Central and state-sponsored PFHI schemes in India
Central-funded health insurance schemes
- Rashtriya Swasthya Bima Yojana—RSBY (2008) is a central-funded health insurance scheme in which 75% of the annual premium is provided by the central government and rest 25% by the state governments. In-patient expenditure of upto Indian National Rupees (INR) 30 000 per family per annum is insured for below poverty line families. Unorganised sector is also covered under this scheme.
- Prime Minister’s Jan Arogya Yojana—PMJAY (2018) is a fully government sponsored scheme, which provides a cover of INR 500 000 per family per year in government empanelled public and private hospitals of India, for secondary and tertiary-level hospitalisation. Vulnerable and below the poverty line (BPL) families are eligible to avail the services under this scheme.
- Central Government Health Scheme (1954) is eligible for central government employees and pensioners enrolled under the scheme. According to this scheme, inpatient services at the government empanelled hospitals, outpatient services including medicines, consultation by experts, maternity and child health services (family welfare) and medical consultation for alternative system of medicines are covered.
- Swavlamban (2015), this is a central-funded health insurance scheme for people with disabilities. Eligible population includes BPL and differently abled people with blindness, hearing impairment, leprosy-cured, locomotor disability, mental illness, etc. A sum of INR 200 000 per annum is covered and treatment of pre-existing illness is covered under the scheme.
- Nirmaya-Disability Health Insurance Scheme (2008), this central-funded health insurance scheme is specifically for people with Cerebral Palsy, autism, multiple disabilities and mental retardation. Services of upto INR 100 000 are covered under this scheme.
- Employee State insurance Scheme—Employee State Insurance Scheme(1952), this scheme is funded by the employers and staff contributions and is applicable to employees of factories and establishments drawing wages upto INR 15 000 a month. Under this scheme, a number of benefits to protect the employees or workers from illness, disability and death are paid to the beneficiaries. Benefits such as sickness benefit (70% of wages), temporary disablement benefit (90% of last wage), permanent disability benefit (90% of wage), maternity benefit (100% of wage), dependent benefit (90% of wage), INR 10000 to dependents for funeral expenses in case of death of the employees and other benefits like vocational and physical rehabilitation are given to the beneficiaries.
State government-funded health insurance schemes
- Aarogyasri Scheme (2007), this scheme is by the Telangana state and BPL families belonging to the state are eligible. Benefits include cashless transactions for treatment of extreme illness, for up to INR 200 000 per year, covered under the scheme.
- Ayushman Bharat—Mahatma Gandhi Rajasthan Swasthya Bima Yojana (2019), this scheme is by the government of Rajasthan and is formed by merging PMJAY scheme and Bhamashah Swasthya Bima Yojana. All the Rajasthani families belonging to BPL category are covered under this scheme. Under this scheme, an insured amount of INR 50 000and INR 450 000 are provided for secondary and tertiary illness, respectively.
- Chief Minister’s Comprehensive Health Insurance Scheme (2012), this is a state-funded HI scheme by government of Tamil Nadu. People belonging to families of less than INR 72 000 are annual earning or less and members of unorganised labour welfare boards, including their families are eligible. Services and benefits of up to INR 500 000 per family per year are covered under the scheme.
- Deen Dayal Swasthaya Seva Yojana (2016), by Goa government, for residents of Goa (residing for at least 5 years), central and state government employees already covered under other government health insurance benefits are eligible. Benefits include cashless inpatient services under government empanelled services. Annual coverage of upto INR 250 000 for a family of three and INR 400 000 for a family of four or more is given. Beneficiaries have to provide an annual premium of INR 200–300 to avail the benefits of the scheme.
- Dr YSR Aarogyasri Scheme (Formerly called Rajiv Arogyasri Community Health Insurance Scheme)−2007, by the Andhra Pradesh government, this scheme covers BPL families from Andhra Pradesh. Under this scheme, free end-to-end cashless services are provided for patients undergoing treatment for therapies listed by the network hospitals. Free outpatient assessments are done for patients not undergoing treatment under the sited therapies.
- Vajpayee Arogaya Shree (2009), this scheme is funded by the government of Karnataka and is applicable for BPL families from rural and urban areas of Karnataka. A total of INR 150 000 is reimbursed for services provided to five members of the beneficiary family, an extra sum of INR 50 000 per annum is provided in case-to-case basis.
- West Bengal Health for All Employees and Pensioners Cashless Medical Treatment Scheme (2014), previously known as ‘West Bengal Health Scheme’, by the government of West Bengal, this scheme is for West Bengal government employees, pensioners and their family members. Benefits include reimbursement for in-patient services in the state empaneled hospitals and outpatient services for 15 diseases mentioned in the scheme. Cashless medical treatment for up to INR 100 000 is provided for inpatient treatment.
- Yeshasvini co-operative farmer’s healthcare scheme (2003), by government of Karnataka, this scheme is for farmers who are members of the cooperative societies. According to this scheme, beneficiaries from the rural areas have to contribute INR 250 (for general category) and INR 50 (for SC/ST families) per annum. Beneficiaries from the urban areas have to contribute INR 710 (for general category) and INR 110 (for SC/ST) per annum. Benefits include inpatient services, discount rates for lab investigations, tests, outpatient services and medical emergency services due to mishaps during farming or any other agriculture related work.
Summary of the impact findings of RSBY and other PFHIs is given in tables 2 and 3 , respectively, and the detailed synthesis is provided in online supplemental file 1 .
Impact of RSBY on financial risk protection and healthcare utilisation
| Outcome | Findings |
| ) | The per-capita inpatient expenditure for RSBY-treated households, decreased in both rural and urban areas. The impact of RSBY on inpatient expenditure was reduced for unmatched and matched samples, when RSBY was implemented for a minimum of 2 months duration. After removing Uttar Pradesh (UP) and Haryana from the analysis, the triple difference findings (ie, with a second control of non-BPL households) showed a reduction in inpatient expenditure, but the double difference analysis showed an increase in inpatient expenditure due to RSBY. However, none of these findings was statistically significant. Both the studies included NSSO data from Andhra Pradesh, Karnataka and Tamil Nadu and used matching and DID methodology for analysis. Sabharwal , used PSM impact analysis to report that average annual household expenditure on inpatient care was significantly less for RSBY beneficiary households when compared with non-beneficiary households. This study also reported that average annual household expenditure spent on inpatient was higher for RSBY beneficiaries who used the smart card for inpatient expenses than the RSBY beneficiaries who did not use the RSBY smart card. However, a low methodological study reported a significant increase in inpatient expenditure for both public and private healthcare, in the state of Maharashtra. This difference was calculated using DID method for the years 2004 and 2012 (after implementation of RSBY in the state). The scheme did not have a significant effect on the OOPE expenditure for inpatient visits. A good methodological study applied the coarsened exact matching and linear and logit regression to report the impact of RSBY on OOPE for inpatient visits, among insured households. No statistically significant difference was reported between RSBY-insured and uninsured households. Another good methodological study, applied PSM and DID approach, to find the impact of RSBY on inpatient OOPE in total household expenditure, by dividing treatment districts into Treatment 1 (TT1), ie, March 2010 and Treatment 2 (TT2) group, ie, April 2010 to March 2012. No impact of RSBY on the inpatient OOPE as share of total household expenditure was observed. The probability of incurring 0 OOPE inpatient expenditure was not significantly different for RSBY and non-RSBY families. RSBY increased the probability of incurring inpatient OOPE by 22% (TT1) and 28% (TT2), respectively. However, these findings were not significant. provided inconclusive information on the effect of RSBY on outpatient OOPE. RSBY had a negative impact on the outpatient expenditure. According to Azam, implementation of RSBY reduced the per capita outpatient expenditure for both rural and urban areas. The outpatient expenditure reduced for RSBY households for the overall matched sample and for the matched sample minus UP and Haryana. There was no statistically significant difference between RSBY-insured and uninsured households in terms of OOPE on outpatient visits. RSBY increased the probability of incurring outpatient OOPE for households participating in RSBY before March 2010, by 23%; however, there was no significant effect on the scheme on outpatient OOPE for the RSBY households between April 2010 and March 2012. RSBY resulted in reduction of total OOPE of the households. The findings of these studies were mostly not significant. Two studies used matching and DID for analysis and two used matching and regression. |
| ) | Four studies provided information on the effect of RSBY on CHE, the RSBY households were less likely to incur CHE for outpatient care, inpatient care and overall CHE. It was observed that beneficiaries of the scheme reported a reduction in CHE; however, one study reported that there was no effect of RSBY on CHE. According to Azam, the effect was same for both rural and urban households. RSBY increased the likelihood of CHE 25. All these findings about the impact of RSBY on CHE were not significant. However, incidence of CHE was significantly reduced for RSBY households with childbirth in last 1 year of data collection. Two studies performed matching and analysed using DID analysis, and other studies performed matching and linear and logistic regression. The cost of medicines was significantly reduced by 22 INR for RSBY households in the rural areas; however, it increased for the urban households by 28 INR, but this result was not significant. |
| The effect of RSBY on impoverishment was not clear. One study reported that RSBY had no effect on impoverishment due to OOP on inpatient care and on the total overall probability of impoverishment. However, in another study among RSBY enrolled APL households, the incidence of health expenditure induced poverty was significantly increased, that is, APL households were pushed to BPL because of healthcare expenditure. Both the studies performed matching and used regression analysis, linear and logistic regression. | |
| Around eight studies looked at the impact of RSBY on healthcare utilisation. The outcomes assessed by these studies include reporting of illness, hospitalisation rate, outpatient care and inpatient care utilisation and utilisation of hospital services. The impact of RSBY on hospitalisation was assessed by six studies ; all the studies showed increase in the hospitalisation, of which three studies showed significant increase in hospitalisation among female heads, scheduled tribes and for poorest. For women seeking treatment in obstetrics department. The studies suggested increase in both, inpatient and outpatient services. However, the results were significant for inpatient care for one of the studies. A study assessed the impact of health insurance on reporting morbidity and seeking treatment for illness in both rural and urban areas. The ATT analysis suggested increase in reporting of morbidity, seeking treatment for short-term and long-term illnesses and long-term morbidity in rural India compared with urban India. The increased value ranges from 0.7% to 3.2%. In urban India, the increase in reporting illness by RSBY holders varied from 2.3% to 2.4%, which was not statistically significant. |
APL, Above poverty line; ATT, Average Treatment Effect on Treated; DID, Difference in Differences; NSSO, National Sample Survey Office; OOPE, out-of-pocket expenditure; PSM, Propensity Score Matching; RSBY, Rashtriya Swasthya Bima Yojana.
Impact of other public-funded health insurance (PFHI) schemes on financial risk protection and healthcare utilisation
| Outcome | Findings |
| ) | The PFHI households were less likely to entail OOPE and there was a significant reduction in OOP for these households. All the studies used regression analysis, linear and logit model for analysis. However, using Tobit regression, it was found that there was no effect of PFHI schemes on OOPE of the households. For Vajpayee Arogyashree Scheme (VAS), the OOPE was less for the insured households, when compared with uninsured households; however, the two-stage least squares (2sls) regression model reported no association between VAS enrolment and size of OOPE. According to Barnes , reduction in OOPE increased with increase in quantiles of spending. At the 75th quantile, the significant reduction in OOPE for VAS households was Indian National Rupees (INR) 4485, and at 95th quantile, it was INR 23548.19. There was no association between RAS (Andhra Pradesh- AP) enrolment and size of OOPE, by using 2sls regression model. By using difference-in-differences (DID), among phase 1 (2007), for Arogyashree enrolled households (AP), significant reduction in per-capital monthly OOP inpatient expenditure and inpatient drug expenditure was observed ; and an increase in inpatient expenditure for RAS households. For Rajiv Arogya Shree (RAS) (AP), Katyal reported a significant increase in both public and private inpatient expenditure, when calculated for the year 2004 and 2012 via DID analysis. Enrolment in CHIS of Tamil Nadu was not significantly associated with size of OOPE. For the CHIS operational in Kerala, the mean OOP expenses for inpatient services among insured participants (INR 448.95) was significantly higher than that of the uninsured households (INR 159.93), using Mann-Whitney U test. There was one study that reported findings on the effect of Pradhan Mantri Jan Arogya Yojana (PMJAY) on OOPE and CHE. It was reported that enrolment in PMJAY did not decrease the OOPE or CHE. There was statistically insignificant more reduction in OOPE for PMJAY enrolled households than other PFHI enrolled households. Statistical significant reduction in log of OOPE was marginally more for PMJAY-enrolled households than other PFHIs. OLS model was used for calculation of the abovementioned continuous outcome variable. As per the Probit model, there was a significant increase in CHE25 and CHE40 of PMJAY-enrolled households. But not for Propensity Score Matching (PSM) model, wherein reduction in OOPE for PMJAY and other PFHI was significant and CHE10 was not associated with PMJAY and PFHI enrolment according to any of the models. The naïve OLS model showed no association between the size of OOPE and enrolment under PMJAY or any PFHI schemes, these findings did not change under propensity score matching and Instrumental Variable (IV) models. |
| ) | Six studies reported the effect of PFHI schemes on CHE. The PFHIs led to reduction in CHE; however, the effect was very small. With PSM, the PFHI-enrolled households were 13% less likely to experience CHE10% and 6% less likely to experience CHE25. For the lowest three quintiles, this effect was even less pronounced as only 0.4% of PFHI households and 1% of PFHI households were likely to experience CHE10 and CHE25. There was a consistent increase in the catastrophic headcount threshold 40% of non-food expenditure for treatment, outpatient, inpatient and drugs. This increase was even reported in a long-term sample, that is, households that have been enrolled in the PFHI schemes for a year. Two studies used DID for analysis, whereas another used logistic regression for analysis. The VAS scheme had a limited effect on CHE; there was no association between enrolment in VAS and CHE25, CHE40 and CHE10, using two-step IV Probit model. In another study, the percentage of VAS households borrowing money for health reasons in the past 1 year was significantly lower than non-VAS households. According to Barnes , there was a marginal reduction in % of CHE (both as % of non-food expenditure and total expenditure) for VAS households than non-VAS households. This finding consists of both non-significant and significant results; however, reduction for 40% and 80% of CHE of the total non-food expenditure and 40% of CHE of the total expenditure was a significant finding. Additionally, money spent by VAS households on CHE was significantly lesser than non-VAS households. For RAS in Andhra Pradesh, there was no association between RAS enrolment and CHE25, CHE40, CHE10, by using two-step IV Probit model. There was no clear effect of Arogyashree enrolment on CHE. Enrolment in CHIS of Tamil Nadu was not significantly associated with CHE25, CHE40 and CHE10. |
| The PFHIs had a marginal effect on the reduction of impoverishment of households. For the overall sample, the PFHIs led to marginal reduction in overall impoverishment and OOP impoverishment, for both short-term and long-term samples (more than a year). However, in the state fixed effect model for overall impoverishment, it was reported that the PFHI schemes had no effect on impoverishment. The state-fixed effect model was used because of the assumption that presence of different state health insurance (HI) schemes alter the findings, and this was analysed using regression analysis. There was no significant difference seen among Arogyashree-enrolled households in AP, compared with south India and all India sample on impoverishment and impoverishment due to OOPE. | |
| Two studies exclusively assessed impact of VAS on hospital utilisation rate. There was significant increase in utilisation of healthcare for all tertiary care facilities. The quasi-randomised study suggested significant increase in healthcare utilisation with respect to accessing healthcare for any symptoms with adjusted difference of 4.96%. The increase in rate of hospitalisation in primary and tertiary care varied from 4.3% to 12.3%, showing the significant change in healthcare utilisation after the implementation of VAS. The quasi-randomised study found significant increase in treatment-seeking behaviour for symptoms associated with cardiac conditions than for non-cardiac symptoms. Eligible households for VAS were 4.4% more likely to seek treatment than non-eligible households. The RAS was assessed by Katyal . The DID analysis suggested increase in healthcare utilisation in Andhra Pradesh and hospitalisation. The five studies assessed the impact of CHIS and other PFHIs and suggested an increase in inpatient and outpatient services. The matched cross-sectional study suggests significant increase in overall utilisation of inpatient services and non-significant results with respect to outpatient services among CHIS insured compared with uninsured. The multivariate analysis showed increased hospitalisation, hospitalisation for chronic conditions, hospitalisation among all age groups for PFHI households. It was also observed via Tobit regression model, being enrolled in PFHI was not significantly associated with length of stay during hospitalisation, contradictory to people with chronic illness. Though the association of HI with healthcare utilisation was high, inequality in accessing healthcare was higher among the higher economic people. The naive profit model analysis that assessed VAS, RAS and CHIS suggested significant increase in hospitalisation in Karnataka after the implementation of VAS. The only study that evaluated PMJAY; the data analysis from NSS data based on PSM and naive models on the hospitalisation did not show any significant difference in hospital care utilisation among both enrolled and non-enrolled population for insurance. |
OLS, Ordinary Least Squares.
Financial risk protection
Twenty-one studies measured financial risk protection, of which 17 were of strong methodological quality, 14–30 3 of moderate methodological quality 31–33 and 1 weak methodological quality. 34 Nine studies 14 16 18 19 23 25 30 32 34 reported the impact of RSBY alone on financial protection. Thirteen studies 15 17 20–22 24 26–29 31–33 provided information on the effect of different PFHI schemes (including state insurance schemes) on financial risk protection.
Three high methodological quality studies reported a reduction in in-patient OOPE for RSBY households; 14 18 30 however, the findings were not significant. One low methodological study stated that after implementation of RSBY in Maharashtra state, there was a significant increase in in-patient expenditure for both public and private healthcare. 32 RSBY did not have a significant effect on in-patient OOPE as a share of total health expenditure, this was reported by two good methodological studies. 16 19 The findings for the impact of RSBY on outpatient OOPE were mixed as out of five good methodological quality studies, two studies mentioned that RSBY led to a reduction in outpatient OOPE, 14 18 two studies reported that RSBY did not have any impact on the outpatient OOPE 16 30 and one study reported that the probability of incurring increased after implementation of RSBY. 19 It was reported that the RSBY households were less likely to incur CHE for outpatient care, in-patient care and overall CHE; 14 16 19 however, one high methodological quality study reported that there was no impact of RSBY on CHE. 25 All these findings were non-significant. The effect of RSBY on impoverishment was not clear as one study reported that RSBY had no effect on impoversihment, 16 whereas another study reported an increase in impoverishment among the Above Poverty Line (APL) housholds. 25
For other PFHI schemes, the findings for effect of HI schemes on financial risk protection were mixed. Three studies reported a reduction in OOPE for insured households, 20 21 26 whereas another study reported no effect on OOPE. 24 For households insured under VAS and RAS, no effect of these schemes was seen on OOPE. 17 One study reported a reduction in in-patient drug expenditure for RAS households; 15 however, other studies reported an increase in-patient household expenditure. 27 32 For CHIS in Tamil Nadu, one study reported no association of CHIS with size of OOPE 17 and another study reported an increase in OOPE in-patient expenditure. 33 It was reported that CHE was reduced for households enrolled under different PFHI schemes, 21 28 however, specifically for VAS, one study reported reduction in CHE, 31 and another study reported no association between CHE and insurance. 17 For CHIS and RAS, no association was reported for CHE and insurance schemes. 15 17 Enrolment in PMJAY did not decrease the OOPE or CHE of the enrolled households. 29
Due to mixed evidence reported for the impact of PFHI schemes on different financial risk protection parameters, it is not possible to conclude whether these schemes have proven to be beneficial in reducing financial risk of the beneficiaries. A summary of these findings is given in tables 2 and 3 .
Access and utilisation of health services
Overall, 16 studies assessed the impact of PFHI on access and utilisation of health services ( tables 2 and 3 ). The HI programmes were RSBY, 14 16 23 26 27 30 32 35 VAS 36 37 RAS, 17 27 32 CHIS 20 21 24 26 33 and PMJAY. 29 Of the 16 studies, 13 studies 14 16 17 20 21 23 24 26 27 29 30 36 37 were assessed to be of strong methodological quality, 32 33 2 were assessed as of moderate quality and 35 1 was rated as weak quality. The analysis that was carried out majorly to look at the impact was logistic regression, profit models and other types. The outcomes that were reported include reporting of illness or morbidity, hospitalisation rate, outpatient care and in-patient care utilisation, duration of hospitalisation and utilisation of hospital services. Findings demonstrated increased access, utilisation of healthcare (both in rural and urban areas) and hospitalisation for RSBY. 14 16 23 26 27 30 32 35 For other PFHI schemes like VAS, RAS and CHIS, an increase in utilisation of healthcare and in-patient outpatient services was reported. 20 21 24 26 32 33 36 37 No significant difference in healthcare utilisation was reported for PMJAY beneficiaries. 29
Willingness-to-pay
A high methodological study 38 reported WTP for the insurance scheme. A majority (71 per cent) of CGHS beneficiaries considered that their current contribution was low and were willing to contribute more. Only 28 per cent Ex-servicemen Contributory Health Scheme beneficiaries were willing to pay an additional monthly financial contribution for better quality healthcare under the schemes. In comparison to higher employment grade beneficiaries, the CGHS beneficiaries from low employment grade were more willing to pay an additional amount to the existing monthly financial contribution.
This review identified and provided information on the impact of different PFHI schemes (operational in India) on healthcare utilisation, WTP and financial risk protection of the beneficiaries. It was observed that although the utilisation of healthcare services via in-patient and outpatient visits increased for insured beneficiaries, there was inconclusive evidence on the impact of different PFHII schemes on financial risk protection.
Our findings report that there is no conclusive evidence to suggest that RSBY reduced the OOPE and CHE or had an impact on financial risk protection. For other PFHIs including the state-sponsored PFHIs, viz., RAS, VAS and CHIS, the findings suggest a mixed impact of these schemes on OOPE, CHE and impoverishment, leading to inconclusive evidence for financial risk protection. Our findings are similar to another systematic review, 10 which reported lack of substantial evidence for reduction in OOPE or improvement in financial risk protection by PFHI schemes in India.
For financial risk protection, varying results, from different studies for the same PFHI scheme, resulted in mixed findings for this outcome. Therefore, it was a challenge to pool evidence together and conclude on the impact of PFHI schemes on financial risk protection. One of the plausible reasons for this can be the different study designs and analysis methods used by different studies to assess the impact of financial risk protection. Also, difference in benefits packages and implementation of the scheme by various successive governments might have resulted in these mixed findings for this outcome.
One of the reasons for studies reporting no substantial impact of RSBY on financial risk protection can be the limited insurance cover, for example, INR 30 000 annually under RSBY. As the utilisation of healthcare and hospitalisation under RSBY has increased over the years, 10 it is possible that beneficiaries would have been hospitalised for hospital services of more than INR 30 000, leading to additional OOP payment. Hospitalisation for services not offered by the RSBY package and denial of hospitalisation by the empaneled hospitals has also led to an increase in OOPE. 39 Another reason for the negligible impact of RSBY in reducing OOPE, as reported in some of the studies, can be the operational or functional error of the scheme. An important component of the scheme is the insurance companies, which are responsible for enrolling beneficiaries, empaneling hospitals, processing claims and reimbursing money. Delayed reimbursement from the insurance companies leads to hospitals asking beneficiaries to buy medicines and other consumables from outside, which results in high OOPE. Additionally, as there is no incentive for the insurance companies to keep a check on the OOPE payments, hospitals might charge patients or deny reimbursement of money on trivial grounds, leading to high OOPE. 39 Another reason could be (which is based on personal experience of authors) to get an appointment for the surgery in empenelled hospitals, beneficiaries of the PFHIs usually wait for a longer period of time. Therefore, to avoid the delay in treatment, beneficiaries have to resort to OOP.
The impact of PFHIs (other than RSBY) including the state-sponsored schemes was reported to be mixed and inconclusive, similar to another systematic review that reported lack of substantial evidence of impact on OOPE for PFHI operational in low and middle-income countries (LMICs). 40 Additionally, as the functioning of any PFHI scheme depends on the governance, different governance structures and demographic profiles of the states would have led to heterogeneity in results. Poor impact of different PFHIs on financial risk protection (reported in some of the studies) can be attributed to similar factors that affect RSBY, that is, low coverage or benefits offered by the schemes leading to OOPE and CHE even for insured beneficiaries and interference or reimbursement issues due to functioning of insurance companies or ‘trusts’.
This systematic review is the first one that has focused on the impact of PMJAY. Our findings suggest that there is a lack of evidence related to the impact of PMJAY, as only one study reported the poor impact of PMJAY on reduction in OOPE and financial risk protection. The reasons for poor impact can be similar as experienced by the earlier PFHIs schemes that is, problem of ‘double billing’, private providers monopoly and administrative problems. As PMJAY is a relatively new scheme, more evidence is needed to conclude on its impact. Additionally, as the only study included in the review was specifically for the state of Chhattisgarh, availability of evidence from other states is needed to summarise the impact of this scheme.
According to our review, there was an increase in incidence of outpatient and in-patient visits and the utilisation of medical services, however, the healthcare utilisation rate differed between states. The utilisation rate increased both among rural and urban areas for the RSBY and VAS. However, there was one study that assessed healthcare utilisation for PMJAY, and the results reported no significant increase in utilisation of healthcare by the PMJAY enrolees. One plausible reason for these results could be the lack of awareness regarding PMJAY, as it is a relatively new scheme. It is not justified to conclude based on a single study, and at the same time, it is important to look into various other aspects, due to which the results of the PMJAY are insignificant in increasing healthcare utilisation. The healthcare utilisation rate was assessed in terms of reporting morbidity, hospitalisation, utilisation of inpatient and outpatient services.
Overall, majority of the evidence suggests that implementation of PFHI has increased hospitalisation and the utilisation of outpatient care. Our findings are consistent with other systematic reviews, 10 40 that is, PFHIs had a positive influence on utilisation of healthcare and hospitalisation in India and other LMICs. Although there is substantial evidence on the impact of PFHI on healthcare utilisation, more rigorous evaluation studies are required to evaluate the impact of health insurance schemes and especially the newly launched PMJAY.
It was reported that although the participants were willing to pay more, the findings for WTP are inconclusive, because the evidence is generated from a single study and the focus of the insurance was limited.
Strengths and limitations
Our review is the first comprehensive review, which has summarised the impact of PFHI schemes in India (including the new scheme of PMJAY under the Ayushman Bharat) on utilisation of healthcare and financial risk protection. One of the limitations of the review is the choice of quality assessment tool used for critical appraisal of included studies due to absence of any other valid tool for secondary data analysis. Responses to some of the questions and individual domain ratings for the EPHPP tool were subjective, although, before finalising the rating, we had a substantial discussion on every domain rating score. Additionally, the tool is used to assess quality of all the quantitative studies, which makes it very vague. Also, due to heterogeneity in methods, population and types of insurances, we could not perform meta-analysis.
Implications of practice and research
Our systematic review has vast policy and practice implications. Since UHC is one of the important components to achieve the sustainable development goals, the role of PFHI becomes even more important in providing equitable and affordable healthcare access to everyone. Financial risk protection is one of the key components of any PFHI scheme that ensures affordable healthcare for everyone. Poor impact of PFHIs on financial risk protection also indicates failure of the PFHI schemes. More research on PFHIs, especially PMJAY and its effect on financial risk protection and healthcare utilisation, are needed as this scheme is an important component of the Ayushman Bharat scheme under the UHC. Similarly, future studies can consider studying the effect of some of the state-funded insurances such as by the government of Goa and West Bengal, which also includes APL households, for which, currently, there is no evidence.
State and central governments could consider including APL households, especially middle-income group under the purview of PMJAY. There should be mechanisms to check corruption in the process of PFHI enrolment and focus could be provided to ease out the administrative difficulties faced by people at the time of claiming insurance. Future research in form of rigorous qualitative research, formative evaluations and process evaluations should be directed towards the reasons for the failure of different PFHIs in improving financial risk protection of the beneficiaries and demand-side and supply-side barriers to implementation and uptake of PFHI. Research reporting reasons for failure of the PFHIs, in improving financial protection, will help in revising and modifying the functioning and implementation of the PFHI schemes for benefit of the consumers.
PFHI schemes, viz, RSBY, VAS, RAS and CHIS have been operational in India since 2008. These schemes have been impactful in increasing healthcare utilisation in terms of outpatient and in-patient care in both rural and urban areas. However, evidence related to financial risk protection was mixed and inconclusive. The new scheme of Pradhan Mantri Jan Arogya Yojana or PMJAY has incorporated administrative and strategic changes, which were based on the shortcomings of earlier PFHIs, viz., provision of a 24-hour inquiry helpline and increased coverage of healthcare services and benefit package. However, limited evidence available on the impact of PMJAY suggests no improvement in healthcare utilisation and financial risk protection of the beneficiaries. Future research on the impact of PMJAY and reasons for failure of other PFHIs on financial risk protection need to be explored.
Supplementary Material
Acknowledgments.
We acknowledge PHRI-RESEARCH grant by Public Health Foundation of India, with the financial support of Department of Science and Technology to partially support authors to carry out this research. We would like to acknowledge the technical support provided by Public Health Evidence South Asia (PHESA), Prasanna School of Public Health (PSPH), Manipal Academy of Higher Education (MAHE), Manipal. We would like to thank Dr. Jisha B Krishnan, Research Assistant, PHESA, PSPH, MAHE, Manipal for supporting us in the title/abstract screening and quality assessment of the included studies and Dr. Vijay Shree Dhyani, Research Assistant, PHESA, PSPH, MAHE, Manipal, for supporting us in title abstract screening.
Twitter: @ParsekarShrads
Contributors: RB is the guarantor of the review. BTV, ER, RB and SSP conceptualised the topic. RV developed search strategy and conducted the search. SSP carried out title/abstract screening and BTV, ER, SSP carried out full text screening. BTV, ER and SSP extracted first round of data extraction, analysed and synthesised the data for the review. Extracted data from all the included studies was cross-checked and independent extraction was done for one third randomly selected studies by BTV, ER, SSP. Quality assessment was performed by BTV, ER, SSP. BTV, ER, SSP drafted the first version of report, which was further edited by RB, BTV, ER, RV, BU and SSP. All the authors read, provided feedback and approved the final report.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Ethics statements, patient consent for publication.
Not applicable.
Ethics approval
This study does not involve human participants.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals
You are here
- Volume 11, Issue 4
- Health insurance awareness and its uptake in India: a systematic review protocol
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Bhageerathy Reshmi 1 ,
- Bhaskaran Unnikrishnan 2 ,
- http://orcid.org/0000-0002-8824-9198 Shradha S Parsekar 3 ,
- Eti Rajwar 3 ,
- Ratheebhai Vijayamma 4 ,
- http://orcid.org/0000-0002-3338-6478 Bhumika Tumkur Venkatesh 3
- 1 Health Information Management, Manipal College of Health Professionals , Manipal Academy of Higher Education , Manipal , India
- 2 Kasturba Medical College, Mangalore , Manipal Academy of Higher Education , Manipal , India
- 3 Public Health Evidence South Asia, Department of Health Information, Prasanna School of Public Health, Manipal Academy of Higher Education , Manipal Academy of Higher Education , Manipal , India
- 4 Manipal Institute of Communication , Manipal Academy of Higher Education , Manipal , India
- Correspondence to Dr Bhumika Tumkur Venkatesh; bhumika.tv{at}manipal.edu
Introduction Health insurance is one of the important approaches that can help in boosting universal healthcare coverage through improved healthcare utilisation and financial protection. This objectives of this review are to identify various interventions implemented in India to promote awareness of health insurance, and to provide evidence for the effectiveness of such interventions on the awareness and uptake of health insurance by the resident Indian population.
Methods and analysis A systematic review will be carried out based on the Cochrane handbook for systematic reviews of interventions. The review will include experimental and analytical observational studies that have included adult population (>18 years) in India. We will include any intervention, policy or programme that directly or indirectly affects awareness or uptake of health insurance. The following outcomes will be eligible to be included: awareness or health insurance literacy, attitude such as readiness to buy health insurance or decision making, uptake of health insurance, demand-side and supply-side factors for awareness of health insurance, and awareness as a factor for uptake and re-enrolment in health insurance. Databases such as MEDLINE (PubMed), Web of Science, Scopus, 3ie impact evaluation repository and Social Science Research Network will be searched from January 2010 to 15 July 2020. Additionally, important government websites and references of the included studies will be scanned to identify potential records. Three authors, independently, will carry out screening and data extraction. Studies will be categorised into quantitative and qualitative, and mixed-methods synthesis will be employed to analyse the findings.
Ethics and dissemination This review will be based on published studies and will not recruit human participants directly, therefore, ethical clearance is not applicable. We will disseminate the final review findings in a national or international conference and publish in a peer-reviewed journal.
- health economics
- health policy
- public health
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-043122
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
This systematic review will use mixed-methods analysis involving findings from quantitative and qualitative studies conducted in India.
We will comprehensively search the evidence in various databases, grey literature and reference and forward citations of included studies, however, the publications will be restricted to English.
We anticipate heterogeneity owing to study designs of potentially included studies, however, to mitigate this challenge we have planned to conduct subgroup analysis based on PROGRESS-Plus framework.
Introduction
Low-income and middle-income countries (LMICs) contribute to around 84% of the world population and 90% of the global burden of disease. 1 People living in the LMICs rely majorly on out-of-pocket payments as the prime source for managing healthcare expenses, that results in a massive demand for services and financial burden of households (usually catastrophic), which in turn leads to impoverishment. 1–5 It is projected that every year approximately 150 million people experience financial catastrophe, by spending more than 40% on health expenses other than food. 6 Families generally spend more than 10% of the household income on illness-related expenses, due to which other household expenses are affected. 2 5 To make it worse, evidence suggests that per capita spending on healthcare in many LMICs is expected to increase in coming years. 4 Additionally, the increased costs of seeking and receiving care can hinder the access to healthcare. 7
The Universal Health Coverage (UHC) is embedded within the Sustainable Development Goals (SDGs) and aims ‘to ensure healthy lives and promote well-being for all at all ages by 2030’. 8 It includes financial risk protection and equal access to quality essential healthcare services. 8 9 In other terms, UHC encourages equitable healthcare 2 and nations across the world are committed to achieving SDGs through UHC. 10
Health insurance is one of the important approaches that can help in boosting UHC through improved healthcare utilisation and financial protection. 7–9 11 There are multiple types of insurance in LMICs that differ with providers (government vs private sector), scales and types of beneficiaries. 8 However, in many LMICs, due lack of acceptability and unwillingness to pay (WTP) premiums, health insurance coverage is limited. 2 4 This increases the risk of excluding vulnerable and at-risk population, who cannot afford to pay health insurance premium. 8 Additionally, the older adults, and the individuals with disability and chronic diseases, have less probability of enrolling in health insurance schemes or their specific needs may not be covered under the scheme. 8
The coverage of health insurance policies or programmes in India is improving, however, the publicly funded health insurance schemes are mostly restricted to socioeconomically backward people or government employees. 12 India’s first health insurance programme, launched in the 1950s, was limited to central government employees and certain low-income population. 11 Over the years, the private healthcare providers’ dominance in quality healthcare service provision can be seen. 11 Nevertheless, many economically backward families are either deprived of healthcare or are pushed into poverty in the absence of financial protection. 11 In 2002, targeted health insurance programmes for low-income households were introduced by central and state governments in partnership with private sector and non-governmental organisations (NGO). Since 2002 (recommendations of National Health Policy 2002), more than 17 health insurance schemes have been launched by various governments in India. 11 The most recent one is ‘Ayushman Bharat’ or Pradhan Mantri Jan Arogya Yojana (PMJAY) (Prime minister’s health assurance scheme) launched in 2018 to achieve UHC. PMJAY is fully financed by the government and seeks to cover 500 million citizens with an annual cover of approximately US$7000 per household. The main aim of the PMJAY is to lessen the economic burden experienced by poor and vulnerable groups for access to healthcare facility. 13
Despite the availability of multiple health insurance schemes, evidence suggests that the uptake of health insurance in India is poor. As per the recently concluded National Sample Survey Office data, there were as low as 14% rural and 18% urban residents of India having some form of health insurance. 14 The low coverage of health insurance was evident in other literature, wherein it was reported to be less than 20%. 5 12 Similarly, other LMICs have reported poor registrations in the national health insurance schemes. 8 9 12 15
There are multiple factors that are responsible for awareness and enrolment in health insurance schemes. 2 4 These factors can be broadly divided into individual (age, gender, education, employment status, marital status), 2 9 16 and household characteristics (wealth, size of family). 1 9 17 Other factors are programme-related (premium amount, rules, regulation and procedures), social capital (trust, networks and group participation, social norms and solidarity and togetherness features of the social organisation of the community), institutional factors (regulatory mechanisms, complaint handling systems and insurance education) and supply-side factors (quality of care and distance of house from the nearest health facility). 2 The aforementioned factors may also determine the consumer preference in selecting the health insurance. 17 Inadequate claim returns, poor accountability and non-transparent operations hinders the uptake of health insurance. 18
In Indian studies, a scant that is, 34% of the participants who did not have health insurance were willing to pay for any health insuance. 5 Previous research in LMICs suggests that financial status of household is positively associated with WTP. 2 4 9 18 Whereas level of education received contradictory findings, that is, a study conducted in Nigeria reported that education was negatively associated with WTP 4 contrary to study conducted in Uganda, 1 Ghana 16 and India. 5 Family who had good perceived health had less probability of getting insurance as compared with those individuals who perceived their health as poor. Similarly, those individuals who had chronic diseases were more inclined to have health insurance than those who did not have chronic diseases. 2 Corruption and mistrust in the health insurance scheme 1 5 18 and expensive plans 5 18 were some of the reasons for non-WTP. Lack of information or health insurance illiteracy is another important reason for non-WTP. 1 5 18
Health insurance literacy is defined as ‘the degree to which individuals have the knowledge, ability and confidence to find and evaluate information about health plans, select the best plan for their own (or their families) financial and health circumstances, and use the plan once enrolled.’ 1 Lack of health insurance literacy or education hinders the uptake of health insurance and in many LMICs health insurance literacy is poor. A study conducted in Uganda reported that about 34% of the studied population were not aware of health insurance. 1 Whereas, proportion of people having inadequate knowledge about health insurance was found to be high in countries such as India (46%), 5 Myanmar (66%) 3 and Hispanic American in the USA (70%). 19
Familiarity or awareness of the insurance schemes increases the utilisation of health insurance and subsequently help in healthcare uptake. 1 2 19 Individuals usually enrol into health insurance because of their personal experiences, awareness or word-of-mouth advertisements. 17 Mass media such as newspaper, radio and television play an important role in making people aware of health insurance schemes. 1 Friends, community meetings, school gatherings and health workers have an influence on increasing the health insurance awareness of the people. 1 Although, aforesaid factors help in increasing the awareness and enrolment in health insurance scheme, some enrollees may not pay premium on regular basis and might not get to know even after health insurance is lapsed. 9 Women farmers, as compared with other occupations, had more odds of unawareness that their insurance was lapsed. 9
It is evident from the above description that there is inadequate awareness of health insurance among general population in LMICs. Knowledge about health insurance can boost individuals’ confidence and self-efficacy; thus, it is an important a priori factor that is required to get enrolled in health insurance scheme. 19 Outreach programmes to increase general knowledge of health insurance and integrating health insurance education within health delivery systems may help to improve the uptake of health insurance. 19 Globally, there are different methods available to promote and raise awareness about different health insurance schemes. However, India is a diverse country with a complex health system and numerous contextual factors. A ‘one size fits all’ approach for any policy or intervention is not suitable for the country. Therefore, it is imperative to understand the different approaches implemented to raise awareness about health insurance in the country. Additionally, due to increased population and a meagre public health spending on healthcare, it is important to understand if the resources are being used appropriately. To ensure this, understanding the effectiveness of such policies is essential, so that focus is directed towards the suitable interventions. ‘Ayushman Bharat Scheme-PMJAY’ is implemented to ensure increased utilisation of the healthcare facilities with financial protection of the beneficiaries. The evidence available on the effectiveness of the PMJAY scheme states no effect of the scheme on utilisation of healthcare and financial protection of enrolled beneficiaries, 13 however, this evidence is limited. Therefore, in the Indian context, it is important to understand if awareness is a factor that has led to decreased utilisation of PMJAY or failure of the other schemes (viz. Rashtriya Swasthya Bima Yojana-RSBY) in securing financial protection of the beneficiaries. 20 Also, it is vital to understand the importance of awareness programmes for success of the health insurance schemes, which will be the focus of this review.
A systematic review will help in synthesising high-quality evidence in a systematic manner, for this important topic of interest. The proposed systematic review will, therefore, identify the different approaches and interventions for increasing health insurance awareness in India and will give information about the impact of these interventions. This review is planned to address the following research questions:
What are the various interventions implemented in India to promote awareness of health insurance?
What is the effectiveness of the above interventions on the awareness and uptake of health insurance by people of India?
Methods and analysis
Methodology for this systematic review will be based on the Cochrane handbook for systematic reviews of interventions 21 and we have adhered to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-Protocols guidelines for reporting this protocol. 22
Criteria for including studies in the review
Population: The review will include studies conducted in India that involve adult population (>18 years). We will consider the studies having household as a unit of analysis, if the head of the family (or the family member who was interviewed) is an adult.
Intervention/exposure: We will include any intervention, policy or programme that directly or indirectly affects awareness of health insurance. The health insurance scheme could be of any type, including but not limited to, public, private, for profit and not-for-profit. Contribution for premiums could be made by individual, NGO, employer or government. There is no restriction on focus of health insurance for example, hospital stay, surgery or critical illness.
Intervention/exposure could be educational, informative, training, technology and m-health or e-health related. The interventions could be focused on raising income threshold to be eligible for health insurance, such as, conditional or unconditional cash transfers that indirectly influences awareness of health insurance. Similarly, training and performance-based financing for healthcare staff or other groups will be eligible for inclusion. The intervention could be a modification of the enrolment procedure, changes in the premium or organisational changes in handling health insurance. Intervention could be directed on general population or targeted groups such as vulnerable population, indigenous groups, community leaders, employees, formal or informal groups and healthcare staff.
Comparison: This review will not restrict the studies based on comparison, as having a comparison group may not always be feasible.
Awareness/health insurance literacy (refers to knowledge of the household head or household member on the presence of insurance schemes, its principles and significance. The outcome measure can be objective or subjective).
Attitude: Readiness to buy health insurance, decision making.
Uptake of health insurance.
Demand-side and supply-side factors for awareness of health insurance.
Awareness of health insurance as a factor for uptake or re-enrolment of health insurance.
Types of study designs: This review will include experimental studies that assessed the effect of intervention to promote awareness and uptake of health insurance. It is sometimes not practical to conduct randomised controlled trials (RCTs) to measure the effect of public health interventions, therefore, the review will also include other study designs. Studies with following designs will be included: RCTs, interrupted time-series studies, difference-in-difference, regression discontinuity designs, statistical matching, quasi-randomised and non-randomised trials. Additionally, this review will include prospective, retrospective, analytical cross-sectional and studies related to process evaluation and policy analysis, if the studies have provided description of intervention or exposure of our interest. Qualitative studies are important source of information about barriers and enabling factors that can complement the findings, therefore, we will also include these types of studies. This review will exclude descriptive cross-sectional (prevalence) studies, commentaries, perspectives, editorials, reviews and conference abstracts. Policy papers that do not provide details of implementation of intervention will not be considered.
Searching and locating the studies
The electronic databases such as MEDLINE (PubMed), Web of Science and Scopus will be searched to identify potential records. Additionally, 3ie impact evaluation repository and Social Science Research Network will be searched. Databases will be searched from January 2010 to 15 July 2020 and publications will be restricted to English language. Ministry of Health and Family Welfare, RSBY, Ayushman Bharat and other state health insurance websites will be searched for reports on the health insurance schemes. We will also scan through references of the included studies for any additional eligible records. After identifying the keywords, initial search will be carried out in PubMed, which will then be replicated in other databases. A designated information scientist will be responsible for conducting search. The preliminary search concepts and key terms are given in table 1 .
- View inline
Search concepts and key words
Applying eligibility and screening the studies
The results of search will be imported to Endnote X7 reference manager software and duplicates will be removed. MS Excel spreadsheet will be used to screen the records. Based on inclusion and exclusion criteria, all the records will be subjected to two stage—title/abstracand full text (FT)—screening process, independently by three (SSP, ER and BTV) reviewers (in pairs). Any disagreements between the reviewers will be resolved by discussion, and senior reviewer will be involved in decision making in case of disagreements between the reviewers. The reasons for excluding FTs will be documented and the PRISMA flow diagram will be provided. A detailed screening protocol will be used as a back-up document to aid the screening process. Table 2 gives detailed screening protocol.
Screening protocol

Data extraction
Data will be extracted independently by three reviewers (SSP, ER and BTV). A predesigned data extraction form will be used for extraction of the data. The data extraction form will be subjected to pilot testing and will be revised as per the suggestions by the reviewers and the experts at this stage. Any disagreements during data extraction will be resolved by consensus supported by the senior reviewer. Data will be extracted based on the characteristics mentioned in the table 3 .
Data extraction format
Critical appraisal of included studies
Effective Public Health Practice Project (EPHPP) tool 23 will be used to assess the methodological quality of quantitative studies (except observational studies) and Newcastle-Ottawa scale (NOS) 24 will be used for the observational studies. The EPHPP rates the study as ‘strong’, ‘moderate’ or ‘weak’ based on eight domains. These domains are selection bias, study design, confounders, blinding, data collection methods, withdrawals and drop-outs, intervention integrity and analysis. 23 NOS rates the study based on three domains viz. selection, comparability and outcome, and the final score ranges between 0 and 10. 24 Reviewers (BTV, ER and SSP), independently in pairs, will appraise the included studies. Any discrepancies between the decisions of reviewers will be resolved by discussion until consensus is achieved. If required, a senior reviewer will be involved as arbitrator and final decision maker to rate the study quality.
Data analysis
Study characteristics consisting of population, intervention/exposure, comparator, outcome, study design components across studies will be tabulated, which will help us to compare and analyse. Subsequently, studies will be categorised into quantitative and qualitative and will be analysed separately. This step will be followed by mixed methods synthesis as suggested by Panda et al . 25
Quantitative studies
Studies will be grouped based on study design, and type of data available (continuous or categorical). If possible, similar studies will be pooled to perform meta-analysis using random effect model. If data are continuous, standardised mean difference will be calculated with 95% CI. For categorical data, OR or risk ratio will be calculated and reported with 95% CI. Meta-analysis will be visually represented with a forest plot. We assume possibility of heterogeneity owing to differences in study design or analysis, intervention, type of insurance and other contextual factors. If heterogeneity exists due to aforementioned components, we will not perform meta-analysis. After ruling out clinical or methodological heterogeneity, we will statistically measure heterogeneity by using I 2 test. If significant heterogeneity (>50%) persists for a particular outcome, meta-analysis will not be conducted. In this case, our focus would be on conducting narrative synthesis and undertaking a subgroup analysis. Key findings of the studies will be summarised in tables/figures or vote counting will be considered. Subgroups could be based on study design, intervention type, insurance type (such as private and public), region and other contextual factors (eg, urban/rural).
Qualitative synthesis
We will carry out thematic analysis as suggested by Thomas and Harden. 26 An iterative process of line-by-line coding will be undertaken as a first step, which will be followed by categorising the codes into code families. Subsequently, a code tree will be created, and themes and subthemes will be generated. Three reviewers (SSP, ER and BTV) will code the data independently and resolve the discrepancies by discussion until consensus is achieved.
Mixed-methods synthesis
The result from both, qualitative and quantitative synthesis will be merged for each outcome. Parallel synthesis will be carried out, and the findings will be summarised narratively. 25 To understand the influence of inequality in uptake of health insurance based on type of insurance, we will explore the possibility of conducting subgroup analysis based on some of the components of PROGRESS ( P lace of residence, R ace/ethnicty/culture/language, O ccupation, G ender, R eligion, E ducation, S ocio-economic status, S ocial capital)-Plus framework. 27
Grading the evidence
We will use the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to evaluate the certainty of evidence for each outcome. 21 Using GRADE profiler software, we will present the main findings of the systematic review in a summary of findings table.
Patient and public involvement
We did not involve patients or public while designing and writing this protocol.
Ethics and dissemination
This review will be based on published studies, therefore, an ethical clearance is not applicable. We have planned following activities to communicate and disseminate the findings of this review. We plan to make at least one national or international conference presentation. We will prepare policy brief to be shared with funder and to get a wider reader, we plan to submit the manuscript to a peer-reviewed journal. On journal publication, we intend to circulate the findings through our social media platform and website.
Acknowledgments
We are grateful to Dr Prachi Pundir, Research Officer, public Health Evidence South Asia, Prasanna School of Public Health, Manipal Academy of Higher Education, Manipal, for proof reading the final document.
- Kyasiimire EP ,
- Namyalo PK , et al
- Mirach TH ,
- Demissie GD ,
- Myint C-Y ,
- Pavlova M ,
- Ogundeji YK ,
- Akomolafe B ,
- Ohiri K , et al
- Surendar RAM ,
- Madhumadhi S ,
- Saravanan R
- Seddoh A , et al
- Kuwawenaruwa A ,
- Binyaruka P , et al
- van Hees SGM ,
- O'Fallon T ,
- Hofker M , et al
- Kanmiki EW ,
- Akazili J , et al
- Fadlallah R ,
- El-Jardali F ,
- Hemadi N , et al
- Lagomarsino G ,
- Garabrant A ,
- Adyas A , et al
- Bebarta KK ,
- ↵ NSS 75th Round . Key indicators of social consumption in India health . New Delhi The government of India, MInistry of Statistics and Programme Implementation, National Statistical Office ; 2019 . http://mospi.nic.in/sites/default/files/publication_reports/KI_Health_75th_Final.pdf
- Abiola AO ,
- Ladi-Akinyemi TW ,
- Oyeleye OA , et al
- Michael GC ,
- Grema BA , et al
- Ayanore MA ,
- Kugbey N , et al
- Ghaddar S ,
- Krishnaswami J
- Chauhan AS ,
- Karan A , et al
- Higgins JPT ,
- Chandler J , et al.
- Liberati A ,
- Tetzlaff J , et al
- Effective Public Health Practice Project
- O'Connell D
- Perez Koehlmoos T , et al
- Kavanagh J ,
Twitter @ParsekarShrads
Contributors RB is the guarantor of the review. RB, SSP, ER and BTV conceptualised the manuscript. SSP drafted the first manuscript, which was further edited by ER. RV developed the search strategy. All the authors (RB, BU, SSP, ER, RV and BTV) read, edited, provided feedback and approved the final manuscript.
Funding This work was supported by PHRI-RESEARCH grants awarded by PHFI with the financial support of Department of Science and Technology (DST). We appreciate the technical support provided by public Health Evidence South Asia, Prasanna School of Public Health, Manipal Academy of Higher Education, Manipal.
Disclaimer Funder did not have any role in writing this protocol and decision to submit it for publication.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
An Analysis of the Evolution of Insurance in India
Cite this chapter.

- Tapen Sinha 4 , 5
Part of the book series: Huebner International Series on Risk, Insurance and Economic Security ((HSRI,volume 26))
2681 Accesses
4 Citations
India had the nineteenth largest insurance market in the world in 2003. Strong economic growth in the last decade combined with a population of over one billion makes it one of the potentially largest markets in the future. Insurance in India has gone through two radical transformations. Before 1956, insurance was private with minimal government intervention. In 1956, life insurance was nationalized and a monopoly was created. In 1972, general insurance was nationalized as well. 255 But, unlike life insurance, a different structure was created for the industry. One holding company was formed with four subsidiaries. As a part of the general opening up of the economy after 1992, a government-appointed committee recommended that private companies should be allowed to operate. It took six years to implement the recommendation. The private sector was allowed into the insurance business in 2000. However, foreign ownership was restricted. No more than 26 percent of any company can be foreign-owned.
The term general insurance is used in Britain and other Commonwealth countries. Elsewhere, the equivalent term is property-casualty insurance or non-life insurance .
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Unable to display preview. Download preview PDF.
Similar content being viewed by others

Insurance Directives and the Single Market: Towards a Trivialisation of Private Health Insurance?

Changing Insurance Contract Law: An Age-Old, Slow and Unfinished Story

Few and Small: The Reinsurance Industry in Italy in the Twentieth Century
13.6 references.
Annual Report of the Ministry of Finance (Section 3, Insurance Division, finmin.nic.in/the_ministry/dept_eco_affairs/budget/annual_report/9596ea3.pdf).
Google Scholar
Bhattacharya, Saugata and Urjit R. Patel (2003). “Reform strategies in the Indian financial sector,” paper presented to the Conference on India’s and China’s Experience with Reform and Growth, November.
Central Statistical Organization database.
Cummins, David, Mary Weiss, and Hongmin Zi (1997). “Organizational form and efficiency,” Financial Institutions Center, Working Paper No. 97–2, Wharton School, University of Pennsylvania.
Farrell, M. (1957). “The measurement of productive efficiency,” Journal of the Royal Statistical Society , Series A, 120,253–281.
Gazette of India Extraordinary Part III Section 4 (2000). Insurance Regulatory and Development Authority (Investment) Regulations.
General Insurance Corporation (various years). Annual reports.
Guerrero, Victor and Tapen Sinha (2004). “Statistical analysis of market penetration in a mandatory privatized pension market using generalized logistic curves,” Journal of Data Science , 2, 196–211.
Indian Insurance Commissioner’s Report (1929). Her Majesty’s Stationery Office, London.
Insurance Regulatory and Development Authority Annual Report (IRDA) (2002–2003). Appendix III.
IRDA Journal (2004). “Market share for premiums: Life market (March 2003–February 2004),” April, 38–39.
IRDA Journal (2004). “Gross premium underwritten by general insurance companies (April 2003–February 2004),” April, 40.
Life Insurance Corporation (various years). Annual reports.
Malaviya, H. D. (n.d.). “Insurance in India.”
Malhotra Committee Report on Reforms in the Insurance Sector (1994). Government of India, Ministry of Finance, New Delhi.
Office of Economic and Cultural Development (2003). OECD Handbook on Insurance , Paris.
Press Trust of India (2004). “India leads the world in road accident deaths,” wire report, January 3.
Rajagopalan, R. (2004). “Valuing the term insurance products in the Indian market,” paper presented to the Fifth Global Conference of the Actuaries, January 25, New Delhi.
Rao, G. V. (2003). “Playing it safe,” IRDA Journal , November, 14–16.
Rodrik, Dani and Arvind Subramanian (2004). “Why India can grow at seven percent,” Economic and Political Weekly , April 17.
Sigma (2003). “World insurance in 2002.” Swiss Re.
Srinivasan, K. K. (2003). “Transition from tariff model of pricing non-life insurance in emerging markets: Issues & prospects,” paper presented to the Seventh Conference of the Asia Pacific Risk an Insurance Association Conference, Bangkok, July 23.
Swain, Shitanshu (2004). “LIC refusing to see the writing on the wall,” Financial Express , April 19.
Swiss Reinsurance Company database.
Tripathi, Dwijendra (2004). The Oxford History of Indian Business (Oxford University Press, Oxford).
Vaidyanathan, L. S. (1934). “Mortality experience of assured lives in India, 1905-1925,” Journal of the Institute of Actuaries , 60, 5–66.
Vaidyanathan, L. S. (1939). “Mortality experience of assured lives in India, 1925–1935,” Journal of the Institute of Actuaries , 70, 42–71.
Wilson, Dominic and Rupa Purushothaman (2003). “Dreaming with BRICs: The Path to 2050,” Goldman and Sachs, Global Economics Paper No. 99, October.
Download references
Author information
Authors and affiliations.
Institute Tecnologico Autonomo de Mexico, Mexico
Tapen Sinha
University of Nottingham, Nottingham
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Fox School of Business and Management, Temple University, USA
J. David Cummins
AUDENCIA Nantes School of Management, France
Bertrand Venard
Rights and permissions
Reprints and permissions
Copyright information
© 2007 Springer Science+Business Media, LLC
About this chapter
Sinha, T. (2007). An Analysis of the Evolution of Insurance in India. In: Cummins, J.D., Venard, B. (eds) Handbook of International Insurance. Huebner International Series on Risk, Insurance and Economic Security, vol 26. Springer, Boston, MA. https://doi.org/10.1007/978-0-387-34163-7_13
Download citation
DOI : https://doi.org/10.1007/978-0-387-34163-7_13
Publisher Name : Springer, Boston, MA
Print ISBN : 978-0-387-34162-0
Online ISBN : 978-0-387-34163-7
eBook Packages : Mathematics and Statistics Mathematics and Statistics (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
A Study on the Growth of Indian Insurance Sector
International Journal of Management, Volume 1, Issue 1, May 2010, pp. 17-32
16 Pages Posted: 22 Dec 2012
Independent
Date Written: 2010
The Insurance sector in India governed by Insurance Act, 1938, the Life Insurance Corporation Act, 1956 and General Insurance Business (Nationalisation) Act, 1972, Insurance Regulatory and Development Authority (IRDA) Act, 1999 and other related Acts. With such a large population and the untapped market area of this population Insurance happens to be a very big opportunity in India. Today it stands as a business growing at the rate of 15-20 per cent annually. Together with banking services, it adds about 7 per cent to the country’s GDP .In spite of all this growth the statistics of the penetration of the insurance in the country is very poor. Nearly 80% of Indian populations are without Life insurance cover and the Health insurance. This is an indicator that growth potential for the insurance sector is immense in India. It was due to this immense growth that the regulations were introduced in the insurance sector and in continuation “Malhotra Committee” was constituted by the government in 1993 to examine the various aspects of the industry. The key element of the reform process was Participation of overseas insurance companies with 26% capital. Creating a more efficient and competitive financialsystem suitable for the requirements of the economy was the main idea behind this reform. Since then the insurance industry has gone through many sea changes .The competition LIC started facing from these companies were threatening to the existence of LIC .since the liberalization of the industry the insurance industry has never looked back and today stand as the one of the most competitive and exploring industry in India. The entry of the private players and the increased use of the new distribution are in the limelight today. The use of new distribution techniques and the IT tools has increased the scope of the industry in the longer run.
Suggested Citation: Suggested Citation
N. Kannan (Contact Author)
Do you have a job opening that you would like to promote on ssrn, paper statistics, related ejournals, io: empirical studies of firms & markets ejournal.
Subscribe to this fee journal for more curated articles on this topic
Microeconomics: Decision-Making under Risk & Uncertainty eJournal
Insurance law, legislation, & policy ejournal.
Subscribe to this free journal for more curated articles on this topic
Development Economics: Regional & Country Studies eJournal
India law ejournal.
Crop Insurance in India: Key Issues and Way Forward
Author(s): Dr. Ashok Gulati , Ms. Prerna Terway, Mr. Siraj Hussain
Working Paper 352

The research leading to this paper was undertaken at ICRIER as a part of the project “Supporting Indian Farms the Smart Way: Rationalising Subsidies and Investments for Faster, Inclusive and Sustainable Growth”. The project is supported by Syngenta Foundation to which we are grateful. We would like to thank Dr. Marco Ferroni, Dr. Yuan Zhou, and Baskar Reddy, of Syngenta Foundation for Sustainable Agriculture for their detailed and very useful comments. The authors would like to acknowledge the invaluable comments from officers of various insurance companies, Dr. Ashish Kumar Bhutani, Joint Secretary (Credit and Cooperation), Government of India, Dr. Shibendu S. Ray, Director of Mahalanobis National Crop Forecast Centre, Scott Sindelar, former Minister Counselor, U.S. Department of Agriculture, U.S. Embassy in India, Rajeev Chawla, Additional Chief Secretary, Karnataka and Vinod Kumar Singh, Directorate of Economics and Statistics, Uttar Pradesh. Our special thanks are due to Prof. Anwarul Hoda, Chair Professor of ICRIER’s Trade Policy and WTO Research Programme and Mr Umesh Mongia, Associate Vice President at ICICI Lombard General Insurance Company Limited for their helpful comments and suggestions to improve the paper.
Team Members

Recent Publications

Optimising Reverse Supply Chains for Resource Recovery: Insights from ICRIER Sampada WSUT- Linear Programming Model

Unravelling India’s E-Waste Supply Chain: A Comprehensive Analysis and Mapping of the Key Actors Involved

Making State Circular Economy Parks Work for Indian States (Part 2): An Economic Analysis Using the ICRIER’s Sampada WSUT Model

Making State Circular Economy Parks Work for the Indian States (Part 1): An Emerging Story of Rajasthan

Estimating loss and damage from climate-induced disasters: An Evaluation using ICRIER ‘Prakriti’ Model
@ 2024 ICRIER. All rights reserved.
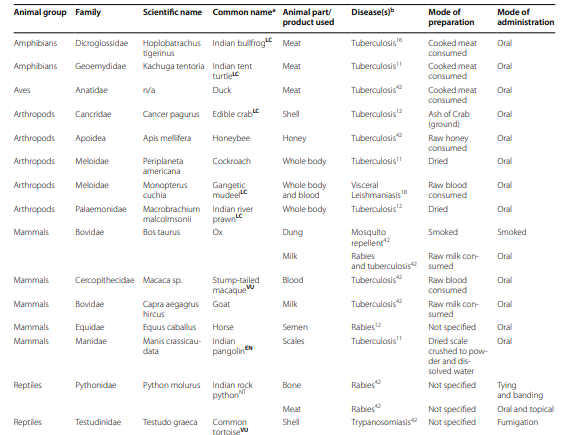
Research Paper: What is the state of the art on traditional medicine interventions for zoonotic diseases in the Indian subcontinent? A scoping review of the peer-reviewed evidence base
What is the state of the art on traditional medicine interventions for zoonotic diseases in the indian subcontinent a scoping review of the peer-reviewed evidence base.
Festus A. Asaaga, Emmanuel S. Tomude, Mujeeb Rahman, Irfan Shakeer, Nitya S. Ghotge, Sarah J. Burthe, Stefanie M. Schäfer, Abi T. Vanak, Bethan V. Purse, Subhash L.Hoti
29 June 2024
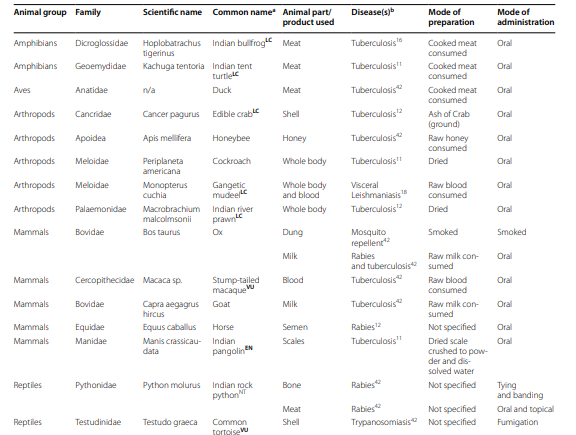
Traditional medicine (TM) interventions are plausible therapeutic alternatives to conventional medical interventions against emerging and endemic zoonotic diseases, particularly in low-and middle-income countries that may lack resources and infrastructure. Despite the growing popularity in the usage of TM interventions, their clinical safety and effectiveness are still contested within conventional healthcare in many countries.
We conducted a scoping review of the peer-reviewed literature that synthesises and maps the evidence on TM interventions for the treatment and prevention of zoonoses on the Indian subcontinent. The region, a global hotspot of biodiversity and emerging infections, is characterised by high prevalence of TM use. Based on the scientific literature, our review (1) maps the scope of the literature, (2) synthesises the evidence on the application of TM interventions for zoonoses, and (3) critically reflects on the state of TM and identifies areas for future research focus.
The evidence synthesis confirmed widespread usage of TM interventions for zoonoses on the subcontinent, with the majority of research reported from India, followed by Pakistan, Bangladesh, and Sri Lanka. Most of the reviewed studies reported on ethno-medicinal uses of plant species, primarily for treating dengue, tuberculosis, Escherichia coli infection, lymphatic filariasis and cholera. However, the evidence on the safety and effectiveness of these reported TM interventions is limited, indicating that these data are rarely collected and/or shared within the peer-reviewed literature.
This review thus highlights that, whilst TMs are already being used and could offer more widely accessible interventions against emerging and endemic zoonoses and ectoparasites, there is an urgent need for rigorous clinical testing and validation of the safety and effectiveness of these interventions.
Asaaga, F.A., Tomude, E.S., Rahman, M. et al.What is the state of the art on traditional medicine interventions for zoonotic diseases in the Indian subcontinent? A scoping review of the peer-reviewed evidence base. BMC Complement Med Ther 24, 249 (2024).
https://doi.org/10.1186/s12906-024-04553-8
Published: 29 June 2024

COMMENTS
India's insurance penetration is lower in both life and non-life insurance sectors compared to advanced countries. In 2017, insurance penetration was 11.6 per cent in South Korea, 9.6 per
India has run multiple Government-Funded Health Insurance schemes (GFHIS) over the past decades to ensure affordable healthcare. We assessed GFHIS evolution with a special focus on two national schemes - Rashtriya Swasthya Bima Yojana (RSBY) and Pradhan Mantri Jan Arogya Yojana (PMJAY). RSBY suffered from a static financial coverage cap, low enrollment, inequitable service supply, utilization ...
Table 2 provides insight into the performance of health insurance sector in India. The growth of health insurance in India has been from Rs.1909 crores for the financial year 2006-2007 to Rs. 33011crores for the financial year 2018-2019. The growth percentage is 1629% i.e. growing at an average rate of 135% per annum.
The public-sector non-life insurance, standalone health insurance, and private non-life insurance companies had shares of 52%, 24%, and 24%, respectively, in health insurance premium collected. Out of the three broad lines of business, that is, group, individual, and government, from 2014-2015 to 2018-2019, there was a decrease in the share ...
Introduction. India has a complex and mixed healthcare framework with presence of parallel public and private healthcare systems. 1 2 There is a stark difference in government spending on both public and private healthcare. 3 Health policies in India have been guided by the principle of equity with prioritising the needs of the poor and underprivileged. 4 Out-of-pocket expenditure (OOPE) for ...
The Insurance Regulatory and Development Authority of India (IRDAI) is committed to enabling 'Insurance for all' by 2047.1 As one of the many steps taken to translate this vision into a reality, the IRDAI, in a recent amendment, increased the maximum number of insurer tie-ups by three times for corporate agents and international monetary funds.
Introduction Health insurance is one of the important approaches that can help in boosting universal healthcare coverage through improved healthcare utilisation and financial protection. This objectives of this review are to identify various interventions implemented in India to promote awareness of health insurance, and to provide evidence for the effectiveness of such interventions on the ...
This type of health insurance plan is for older people in the family. It provides covers and protection from health issues during old age. 1.5.5 Maternity Health insurance. Maternity health insurance ensures coverage for maternity and other additional expenses. 1.5.6 Hospital daily cash bene t plans.
In India, Ayushman Bharat Pradhan Mantri Jan Aarogya Yojana (PMJAY), a cashless publicly financed health insurance scheme, was launched in 2018, to provide secondary and tertiary hospitalisation care for surgical and medical care to 40% of India's population. Under the PMJAY, the empanelled public and private hospitals are reimbursed, who are paid a uniform case-based bundled payment.
This paper examines challenges to implementing health insurance in India and makes a case for anthropological studies of the social life of insurance schemes (Dao and Nichter Citation 2015) as a means of providing fresh insights to the emerging interdisciplinary field of health policy and service research (Gilson et al. Citation 2011; Mills ...
Insurance in India has gone through two radical transformations. Before 1956, insurance was private with minimal government intervention. In 1956, life insurance was nationalized and a monopoly was created. In 1972, general insurance was nationalized as well. 255 But, unlike life insurance, a different structure was created for the industry.
Binny, Dr. Meenu Gupta (2017), Health insurance in India- Oppor tunities and challenges. The. paper is about present trends of health insurance sector in India. Growth oppo rtunities and ...
6 Protection landscape in India - Past, Present & Future 7 Ibid. 8 Swiss Re Institute, Jan 2023 publication - India's insurance market: poised for rapid growth Figure 3: Insurance claims settlement ratios in India across life, general and health insurance sectors 95% 97% 97% 99% 2009-10 2014-15 2019-20 2021-22 LI claims settlement (Individual ...
The Insurance sector in India governed by Insurance Act, 1938, the Life Insurance Corporation Act, 1956 and General Insurance Business (Nationalisation) Act, 19. ... Research Paper Series; Conference Papers; Partners in Publishing; Jobs & Announcements; Special Topic Hubs; SSRN Rankings . Top Papers; Top Authors; Top Organizations;
FCs are broadening the reach of the sector (IBEF, 2019). Among the 24 life insurers currently operating in the Indian market, the Life Insur. nce Corporation (LIC) is the sole public sector company. Motor, health, and crop insurance segme. ts are driving growth in the non-life insurance segment. Among the 35.
GDP originating from the service sector recorded a growth rate of 9.30 per cent in 2010-. 201 1. The contours of insurance business have been changing across the globe and rippling effect. of the ...
This research examines the evolution of the insurance industry in India, highlighting key milestones and regulatory changes. Furthermore, the study delves into the economic impact of insurance on various facets of the Indian economy. It investigates the role of insurance in risk mitigation, financial stability, and long-term capital formation.
3)J.Anita studied the health insurance products in India and implications of privatization of Health insurance in India. Meaning: Health insurance is an insurance product which covers medical and surgical expenses of an insured individual.It reimburses the expenses incurred due to illness or injury or pays the care provider of the insured
The. role of technology has increased a lot IoT, Big data, Artificial Intelligence play a big role in insur ance sector. The present paper focuses on impact of COVID 19 pandemic on health ...
15. Table 3.8- Premium Underwritten by General Insurance Companies in India (2000-2019). 16. Table 3.9- Market Share of Life Insurance Companies in India (2000-2019). 17. Table 3.10- Expenses of Life Insurance Companies in India (2000-2019). 18. Table 3.11- Expenses of General Insurance Companies in India (2000-2019). 19.
The research leading to this paper was undertaken at ICRIER as a part of the project "Supporting Indian Farms the Smart Way: Rationalising Subsidies and Investments for Faster, Inclusive and Sustainable Growth". The project is supported by Syngenta Foundation to which we are grateful. We would like to thank Dr. Marco Ferroni, Dr. Yuan Zhou,
The present paper is an attempt to outline the current picture of health insurance sector in India which is a part and parcel of general insurance. Health insurance sector in India has gained huge ...
This article examines the determinants of India's information and communications technology (ICT) access. We use the second wave of the India Human Development Survey (IHDS) of 2011-2012, a nationally representative survey at the individual level, and find that ICT ownership and usage are abysmally low for women compared to men.
Research Paper: What is the state of the art on traditional medicine interventions for zoonotic diseases in the Indian subcontinent? A scoping review of the peer-reviewed evidence base. ... with the majority of research reported from India, followed by Pakistan, Bangladesh, and Sri Lanka. Most of the reviewed studies reported on ethno-medicinal ...
new companies into the market and has b ecome quite co mpetitive with. rising awareness among the insured. This research paper aims to. analytical study of Ind i. an general insurance companies of ...