An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Management of pelvic organ prolapse during pregnancy: Case report
Brandon alejandro muñoz vargas, aura esperanza velasco garcía, rafael leonardo aragón mendoza, camilo alberto garzón sarmiento, elman hackson leal vargas.
- Author information
- Article notes
- Copyright and License information
Corresponding author at: Carrera 8 No 0-29 sur, Postcode 110411003, Colombia. [email protected]
Received 2022 Apr 28; Revised 2022 May 9; Accepted 2022 May 11; Collection date 2022 Jul.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
During pregnancy, pelvic organ prolapse is uncommon and is associated with adverse outcomes such as vaginal infection, cervical ulceration, and preterm delivery. Treatment includes conservative and surgical management during pregnancy. A 32-year-old woman presented with a history of vaginal delivery eight months earlier reported the sensation of a vaginal mass lasting seven months. On physical examination, we noted pelvic organ prolapse and 19-week pregnancy. We treated her conservatively with a Gellhorn pessary and antenatal corticosteroid for fetal lung maturation at 32 weeks due to a high risk of preterm delivery. The pregnancy proceeded with no obstetric complications and vaginal delivery at term of a healthy neonate. Conservative management for patients with pelvic organ prolapse during pregnancy using a pessary is the best option to improve maternal symptomatology and minimize gestational risk; there is no contraindication for vaginal delivery, and cesarean section is reserved for obstetric indications.
Keywords: High-risk pregnancy, Pelvic organ prolapse, Pregnancy, Uterine prolapse, Vaginal ring pessary
During pregnancy, pelvic organ prolapse is uncommon.
Treatment includes conservative and surgical management during pregnancy.
A pessary is the best option to improve maternal symptomatology and minimize gestational risk.
1. Introduction
Pelvic organ prolapse is defined as the partial or total descent of pelvic organs through the vagina due to abnormalities of the supporting tissues ( 1 ). The condition occurs in 25% to 65% of gynecologic clinic populations ( 2 , 3 ). Pelvic organ prolapse is one of the main indications for gynecological surgery, with an incidence of 1.5 to 1.8 surgeries for every 1000 women per year ( 1 , 4 ).
There are multiple risk factors, including multiparity, vaginal deliveries, instrumental delivery, connective tissue disorders, obesity and age ( 4 , 5 ). The most frequent clinical symptom is a sensation of heaviness or mass in the vaginal region ( 6 ), leading to secondary sexual dysfunction in some cases and a significant effect on quality of life, particularly in young patients ( 7 ). The Pelvic Organ Prolapse Quantification (POP-Q) is the tool used to objectively assess the extent of the genital prolapse ( 4 ) to determine the best treatment option (whether surgical or conservative) to restore the anatomy, recover function, and improve patient symptoms.
Pelvic organ prolapse during pregnancy is uncommon, with only a few reported cases ( 8 ); treatment aims to minimize obstetric risks such as vaginal infection, cervical ulceration, and preterm delivery. Conservative and surgical management have been described, although there are no unified management guidelines for these patients ( 9 ). Consequently, several critical factors must be considered in this population, such as prenatal steroid administration, the type of recommended management, gestational age for delivery, and delivery route ( 9 ). This report describes a patient with pelvic organ prolapse in the second trimester of pregnancy treated with conservative management with an adequate perinatal outcome.
2. Case Presentation
A 33-year-old patient, G2P1V1, reported a sensation of vaginal mass lasting seven months with no incontinence and a history of 12 months between pregnancies, with prior uncomplicated vaginal delivery at term. On physical examination, we noted genital prolapse of the cervix with evidence of a 1.5-cm area of ulceration in the posterior labium; enlarged uterus POP-Q Aa −2, Ba −2, C + 4, D -3, Bp-2, Ap −2, total vaginal length 9, perineal body 1.5, Hg 3.5 (POP-Q IIIC; Fig. 1 A). We conducted additional tests before selecting a treatment option, with an obstetric ultrasound scan showing a 19-week pregnancy of adequate weight for the gestational age. A gynecology meeting with the maternal-fetal medicine and pelvic floor teams decided to pursue conservative management during gestation using a Gellhorn vaginal pessary 2–3/4 (70 mm; Fig. 1 B), with antenatal corticosteroid for fetal lung maturation at 32 weeks, clinical monitoring every two weeks, and monthly ultrasound follow-up. The cervical ulceration was resolved during pregnancy, two weeks after the placement of the vaginal pessary. The clinical specialist removed, washed, and replaced the vaginal pessary at each clinical visit. The patient developed a recurrent fungal vaginal infection, w which was managed with vaginal clotrimazole, and resolved after administration of a single 150 mg dose of fluconazole. The pessary was removed at 39 weeks of gestation, at the time of hospital admission, without evidence of prolapse, so only conduction was performed and the patient had an uncomplicated vaginal delivery ( Fig. 2 ) with a healthy neonate who weighed 2670 g. After 24 h of in-hospital monitoring, the mother and neonate were discharged. Evidence of POP-Q was found at the postpartum follow-up visit, with no changes in relation to the initial assessment, so it was decided to arrange pelvic floor rehabilitation therapy.
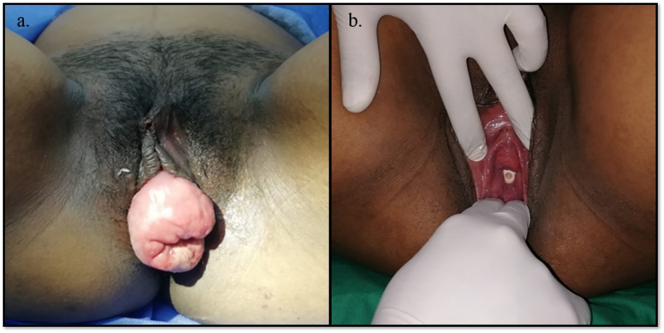
a. Prolapse seen on the first visit, at 19 weeks of gestation. b. Prolapse reduction with the use of the Gellhorn type pessary.
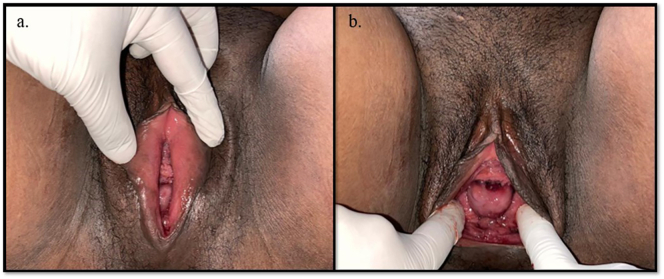
Prolapse during the postpartum period.
3. Discussion
Pelvic organ prolapse is uncommon among pregnant women, with an incidence of one case for every 10,000 to 15,000 pregnancies ( 8 ); for this reason, there are no management guidelines or protocols, and only case reports are available, with literature reviews and recommendations extrapolated from non-pregnant patients ( 9 ).
The treatment of pelvic organ prolapse during pregnancy is individualized and depends on patient preference ( 10 ). It must be performed by a multidisciplinary team, considering the obstetric future, follow-up and recommendations during pregnancy, and the risks of premature delivery, halted dilatation, shoulder dystocia, uterine rupture, and localized infections in these patients ( 1 , 11 ).
The management of choice is conservative, with the use of vaginal pessaries, the most commonly used being the Gellhorn type, followed by the membrane ring type ( 9 ). This treatment provides vaginal support, reducing prolapse and improving symptoms of vaginal mass sensation, vaginal pressure and voiding difficulty, among others ( 12 ). The absence of active vaginal infections and the possibility of patient follow-up are prerequisites for its use ( 9 ). It may have adverse effects that need to be explained to the patient, including abundant or fetid vaginal discharge, urinary or vaginal infections, vaginal or cervical erosions, difficulty voiding or defecating, and impact on sexual life ( [12] , [13] , [14] ). It is worth noting that prolapse symptoms improve during the second and third trimesters of gestation when the uterus becomes an abdominal organ [9], hence the removal, in our case, of the vaginal pessary at 39 weeks with no self-reported prolapse-related symptoms during the last week of gestation, allowing for vaginal delivery at term.
Surgical treatment has also been described, indicated when conservative treatment fails or the pelvic floor cannot be restored to its normal condition. However, it is not indicated as a first-line treatment because of the surgical and anesthetic risk as well as potential deleterious effects on pregnancy ( 15 , 16 ). Laparoscopic surgical treatment has been described in the first trimester ( [15] , [16] , [17] ) or at the time of cesarean section ( 18 , 19 ).
Prenatal steroid administration must be considered given the high risk of preterm labor and delivery in patients with pelvic organ prolapse. It was used in our case in week 32 of gestation.
There are no contraindications for vaginal delivery and no recommendations regarding the delivery route in patients with exteriorized uterus; however, in cases of significant prolapse with severe cervical edema or non-reducible prolapse, dystocia may occur, potentially precluding vaginal delivery ( 19 , 20 ).
4. Conclusions
As this case illustrates, the treatment of pelvic organ prolapse during pregnancy must be individualized and requires a multidisciplinary approach with close follow-up during prenatal visits due to increased obstetric morbidity, including preterm delivery. The first option is conservative management with a vaginal pessary, which provides adequate support for the pelvic floor and is well tolerated, with surgical management being the second option in case of conservative treatment failure.

Contributors
Brandon Alejandro Muñoz Vargas contributed to manuscript editing, acquisition, analysis and interpretation of data, patient care.
Aura Esperanza Velasco García contributed to manuscript editing, acquisition, analysis and interpretation of data.
Rafael Leonardo Aragón Mendoza contributed to manuscript editing, patient care, acquisition, analysis and interpretation of data, final approval of manuscript.
Camilo Alberto Garzón Sarmiento contributed to manuscript editing, patient care, final approval of manuscript.
Elman Hackson Leal Vargas contributed to manuscript editing, acquisition,analysis and interpretation of data.
This work received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Patient consent
Provenance and peer review.
This article was not commissioned and was peer reviewed.
Conflict of interest statement
The authors declare that they have no conflict of interest regarding the publication of this case report.
- 1. Tsikouras P., Dafopoulos A., Vrachnis N., Iliodromiti Z., Bouchlariotou S., Pinidis P., et al. Uterine prolapse in pregnancy: risk factors, complications and management. J. Matern. Fetal Neonatal Med. 2014;27 doi: 10.3109/14767058.2013.807235. [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Swift S., Woodman P., O’Boyle A., Kahn M., Valley M., Bland D., et al. Pelvic Organ Support Study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am. J. Obstet. Gynecol. 2005;192:795–806. doi: 10.1016/j.ajog.2004.10.602. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Arango-Buitrago V., Restrepo-Moreno M., Echavarría-Restrepo L.G., Gómez-Londoño M. Prolapso de órganos pélvicos durante el embarazo tratado con pesario. Reporte de dos casos. Ginecol. Obstet. Mex. 2016;84(9) [ PubMed ] [ Google Scholar ]
- 4. Pelvic Organ Prolapse: ACOG Practice Bulletin, Number 214. Vol. 134. Obstet. Gynecol. 2019;134:e126–e142. doi: 10.1097/AOG.0000000000003519. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Trutnovsky G., Kamisan Atan I., Martin A., Dietz H.P. Delivery mode and pelvic organ prolapse: a retrospective observational study. BJOG: Int. J. Obstetrics Gynaecol. 2016;123(9) doi: 10.1111/1471-0528.13692. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Reimers C., Stær-Jensen J.E., Siafarikas F., Bø K., Engh M.E. Association between vaginal bulge and anatomical pelvic organ prolapse during pregnancy and postpartum: an observational study. Int. Urogynecol. J. 2018;29(3) doi: 10.1007/s00192-017-3407-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Umachanger J.K., Marcussen M.L., Bøggild H., Kjærgaard N., Glavind K. First-line treatment of pelvic organ prolapse and discontinuation of pessary treatment. Int. Urogynecol. J. 2020;31(9) doi: 10.1007/s00192-020-04338-w. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Zeng C., Yang F., Wu C., Zhu J., Guan X., Liu J. Uterine prolapse in pregnancy: two cases report and literature review. Case Rep. Obstet. Gynecol. 2018;2018 doi: 10.1155/2018/1805153. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Gómez Londoño M., Echavarría Restrepo L.G., Henao López C.P., Campo Campo M.N., Sanín Ramírez D. Uso de pesario para prolapso de órganos pélvicos durante el embarazo: serie de casos y revisión de la literatura. Revista chilena de obstetricia y ginecología. 2020;85(3) [ Google Scholar ]
- 10. Wang K., Zhang J., Xu T., Yu H., Wang X. Successful deliveries of uterine prolapse in two primigravid women after obstetric management and perinatal care: case reports and literature review. Ann. Palliative Med. 2021;10(6) doi: 10.21037/apm-20-1322. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Mohamed-Suphan N.B., Ng R.K.W. Uterine prolapse complicating pregnancy and labor: a case report and literature review. Int. Urogynecol. J. 2012;23 doi: 10.1007/s00192-011-1573-2. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Cundiff G.W., Amundsen C.L., Bent A.E., Coates K.W., Schaffer J.I., Strohbehn K., et al. The PESSRI study: symptom relief outcomes of a randomized crossover trial of the ring and Gellhorn pessaries. Am. J. Obstet. Gynecol. 2007;196(4) doi: 10.1016/j.ajog.2007.02.018. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Wu V., Farrell S.A., Baskett T.F., Flowerdew G. A simplified protocol for pessary management. Obstet. Gynecol. 1997;90(6) doi: 10.1016/s0029-7844(97)00481-x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Clemons J.L., Aguilar V.C., Tillinghast T.A., Jackson N.D., Myers D.L. Risk factors associated with an unsuccessful pessary fitting trial in women with pelvic organ prolapse. Am. J. Obstet. Gynecol. 2004;190(2) doi: 10.1016/j.ajog.2003.08.034. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Haliloglu Peker B., Ilter E., Peker H., Celik A., Gursoy A., Gunaldi O. Laparoscopic sacrohysteropexy in a woman at 12 Weeks’ gestation. J. Minim. Invasive Gynecol. 2018;25(7) doi: 10.1016/j.jmig.2018.01.035. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Pirtea L., Balint O., Secosan C., Ilina R., Grigoras D. Laparoscopic promontohysteropexy during pregnancy. J. Minim. Invasive Gynecol. 2017;24(7) doi: 10.1016/j.jmig.2017.03.007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Matsumoto T., Nishi M., Yokota M., Ito M. Laparoscopic treatment of uterine prolapse during pregnancy. Obstet. Gynecol. 1999;93(5 SUPPL) doi: 10.1016/s0029-7844(98)00494-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Karatayli R., Gezginç K., Kantarci A.H., Acar A. Successful treatment of uterine prolapse by abdominal hysteropexy performed during cesarean section. Arch. Gynecol. Obstet. 2013;287(2) doi: 10.1007/s00404-012-2563-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Meydanli M.M., Üstün Y., Yalcin O.T. Pelvic organ prolapse complicating third trimester pregnancy: a case report. Gynecol. Obstet. Investig. 2006;61(3) doi: 10.1159/000090034. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Pizzoferrato A.C., Bui C., Fauconnier A., Bader G. Advanced uterine prolapse during pregnancy: pre- and postnatal management. Gynecol. Obstetrique Fertilite. 2013;41(7–8) doi: 10.1016/j.gyobfe.2013.06.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (791.6 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
