Appointments at Mayo Clinic
Alzheimer's treatments: what's on the horizon.
Despite many promising leads, new treatments for Alzheimer's are slow to emerge.
Current Alzheimer's treatments temporarily improve symptoms of memory loss and problems with thinking and reasoning.
These Alzheimer's treatments boost the performance of chemicals in the brain that carry information from one brain cell to another. They include cholinesterase inhibitors and the medicine memantine (Namenda). However, these treatments don't stop the underlying decline and death of brain cells. As more cells die, Alzheimer's disease continues to progress.
Experts are cautious but hopeful about developing treatments that can stop or delay the progression of Alzheimer's. Experts continue to better understand how the disease changes the brain. This has led to the research of potential Alzheimer's treatments that may affect the disease process.
Future Alzheimer's treatments may include a combination of medicines. This is similar to treatments for many cancers or HIV / AIDS that include more than one medicine.
These are some of the strategies currently being studied.

Taking aim at plaques
Some of the new Alzheimer's treatments target clumps of the protein beta-amyloid, known as plaques, in the brain. Plaques are a characteristic sign of Alzheimer's disease.
Strategies aimed at beta-amyloid include:
Recruiting the immune system. Medicines known as monoclonal antibodies may prevent beta-amyloid from clumping into plaques. They also may remove beta-amyloid plaques that have formed. They do this by helping the body clear them from the brain. These medicines mimic the antibodies your body naturally produces as part of your immune system's response to foreign invaders or vaccines.
In 2023, the U.S. Food and Drug Administration (FDA) approved lecanemab (Leqembi) for people with mild Alzheimer's disease and mild cognitive impairment due to Alzheimer's disease.
A phase 3 clinical trial found that the medicine slowed cognitive decline in people with early Alzheimer's disease. The medicine prevents amyloid plaques in the brain from clumping. The phase 3 trial was the largest so far to study whether clearing clumps of amyloid plaques from the brain can slow the disease.
Lecanemab is given as an IV infusion every two weeks. Your care team likely will watch for side effects and ask you or your caregiver how your body reacts to the drug. Side effects of lecanemab include infusion-related reactions such as fever, flu-like symptoms, nausea, vomiting, dizziness, changes in heart rate and shortness of breath.
Also, people taking lecanemab may have swelling in the brain or may get small bleeds in the brain. Rarely, brain swelling can be serious enough to cause seizures and other symptoms. Also in rare instances, bleeding in the brain can cause death. The FDA recommends getting a brain MRI before starting treatment. It also recommends being monitored with brain MRI s during treatment for symptoms of brain swelling or bleeding.
People who carry a certain form of a gene known as APOE e4 appear to have a higher risk of these serious complications. The FDA recommends being tested for this gene before starting treatment with lecanemab.
If you take a blood thinner or have other risk factors for brain bleeding, talk to your health care professional before taking lecanemab. Blood-thinning medicines may increase the risk of bleeds in the brain.
More research is being done on the potential risks of taking lecanemab. Other research is looking at how effective lecanemab may be for people at risk of Alzheimer's disease, including people who have a first-degree relative, such as a parent or sibling, with the disease.
Another medicine being studied is donanemab. It targets and reduces amyloid plaques and tau proteins. It was found to slow declines in thinking and functioning in people with early Alzheimer's disease.
The monoclonal antibody solanezumab did not show benefits for individuals with preclinical, mild or moderate Alzheimer's disease. Solanezumab did not lower beta-amyloid in the brain, which may be why it wasn't effective.
Preventing destruction. A medicine initially developed as a possible cancer treatment — saracatinib — is now being tested in Alzheimer's disease.
In mice, saracatinib turned off a protein that allowed synapses to start working again. Synapses are the tiny spaces between brain cells through which the cells communicate. The animals in the study experienced a reversal of some memory loss. Human trials for saracatinib as a possible Alzheimer's treatment are now underway.
Production blockers. These therapies may reduce the amount of beta-amyloid formed in the brain. Research has shown that beta-amyloid is produced from a "parent protein" in two steps performed by different enzymes.
Several experimental medicines aim to block the activity of these enzymes. They're known as beta- and gamma-secretase inhibitors. Recent studies showed that the beta-secretase inhibitors did not slow cognitive decline. They also were associated with significant side effects in those with mild or moderate Alzheimer's. This has decreased enthusiasm for the medicines.
Keeping tau from tangling
A vital brain cell transport system collapses when a protein called tau twists into tiny fibers. These fibers are called tangles. They are another common change in the brains of people with Alzheimer's. Researchers are looking at a way to prevent tau from forming tangles.
Tau aggregation inhibitors and tau vaccines are currently being studied in clinical trials.
Reducing inflammation
Alzheimer's causes chronic, low-level brain cell inflammation. Researchers are studying ways to treat the processes that lead to inflammation in Alzheimer's disease. The medicine sargramostim (Leukine) is currently in research. The medicine may stimulate the immune system to protect the brain from harmful proteins.
Researching insulin resistance
Studies are looking into how insulin may affect the brain and brain cell function. Researchers are studying how insulin changes in the brain may be related to Alzheimer's. However, a trial testing of an insulin nasal spray determined that the medicine wasn't effective in slowing the progression of Alzheimer's.
Studying the heart-head connection
Growing evidence suggests that brain health is closely linked to heart and blood vessel health. The risk of developing dementia appears to increase as a result of many conditions that damage the heart or arteries. These include high blood pressure, heart disease, stroke, diabetes and high cholesterol.
A number of studies are exploring how best to build on this connection. Strategies being researched include:
- Current medicines for heart disease risk factors. Researchers are looking into whether blood pressure medicines may benefit people with Alzheimer's. They're also studying whether the medicines may reduce the risk of dementia.
- Medicines aimed at new targets. Other studies are looking more closely at how the connection between heart disease and Alzheimer's works at the molecular level. The goal is to find new potential medicines for Alzheimer's.
- Lifestyle choices. Research suggests that lifestyle choices with known heart benefits may help prevent Alzheimer's disease or delay its onset. Those lifestyle choices include exercising on most days and eating a heart-healthy diet.
Studies during the 1990s suggested that taking hormone replacement therapy during perimenopause and menopause lowered the risk of Alzheimer's disease. But further research has been mixed. Some studies found no cognitive benefit of taking hormone replacement therapy. More research and a better understanding of the relationship between estrogen and cognitive function are needed.
Speeding treatment development
Developing new medicines is a slow process. The pace can be frustrating for people with Alzheimer's and their families who are waiting for new treatment options.
To help speed discovery, the Critical Path for Alzheimer's Disease (CPAD) consortium created a first-of-its-kind partnership to share data from Alzheimer's clinical trials. CPAD 's partners include pharmaceutical companies, nonprofit foundations and government advisers. CPAD was formerly called the Coalition Against Major Diseases.
CPAD also has collaborated with the Clinical Data Interchange Standards Consortium to create data standards. Researchers think that data standards and sharing data from thousands of study participants will speed development of more-effective therapies.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Treatments and research. Alzheimer's Association. https://www.alz.org/alzheimers-dementia/research_progress/treatment-horizon. Accessed March 23, 2023.
- Cummings J, et al. Alzheimer's disease drug development pipeline: 2022. Alzheimer's and Dementia. 2022; doi:10.1002/trc2.12295.
- Burns S, et al. Therapeutics of Alzheimer's disease: Recent developments. Antioxidants. 2022; doi:10.3390/antiox11122402.
- Plascencia-Villa G, et al. Lessons from antiamyloid-beta immunotherapies in Alzheimer's disease. Handbook of Clinical Neurology. 2023; doi:10.1016/B978-0-323-85555-6.00019-9.
- Brockmann R, et al. Impacts of FDA approval and Medicare restriction on antiamyloid therapies for Alzheimer's disease: Patient outcomes, healthcare costs and drug development. The Lancet Regional Health. 2023; doi:10.1016/j.lana. 2023.100467 .
- Wojtunik-Kulesza K, et al. Aducanumab — Hope or disappointment for Alzheimer's disease. International Journal of Molecular Sciences. 2023; doi:10.3390/ijms24054367.
- Can Alzheimer's disease be prevented? Alzheimer's Association. http://www.alz.org/research/science/alzheimers_prevention_and_risk.asp. Accessed March 23, 2023.
- Piscopo P, et al. A systematic review on drugs for synaptic plasticity in the treatment of dementia. Ageing Research Reviews. 2022; doi:10.1016/j.arr. 2022.101726 .
- Facile R, et al. Use of Clinical Data Interchange Standards Consortium (CDISC) standards for real-world data: Expert perspectives from a qualitative Delphi survey. JMIR Medical Informatics. 2022; doi:10.2196/30363.
- Imbimbo BP, et al. Role of monomeric amyloid-beta in cognitive performance in Alzheimer's disease: Insights from clinical trials with secretase inhibitors and monoclonal antibodies. Pharmacological Research. 2023; doi:10.1016/j.phrs. 2022.106631 .
- Conti Filho CE, et al. Advances in Alzheimer's disease's pharmacological treatment. Frontiers in Pharmacology. 2023; doi:10.3389/fphar. 2023.1101452 .
- Potter H, et al. Safety and efficacy of sargramostim (GM-CSF) in the treatment of Alzheimer's disease. Alzheimer's and Dementia. 2021; doi:10.1002/trc2.12158.
- Zhong H, et al. Effect of peroxisome proliferator-activated receptor-gamma agonists on cognitive function: A systematic review and meta-analysis. Biomedicines. 2023; doi:10.3390/biomedicines11020246.
- Grodstein F. Estrogen and cognitive function. https://www.uptodate.com/contents/search. Accessed March 23, 2023.
- Mills ZB, et al. Is hormone replacement therapy a risk factor or a therapeutic option for Alzheimer's disease? International Journal of Molecular Sciences. 2023; doi:10.3390/ijms24043205.
- Custodia A, et al. Biomarkers assessing endothelial dysfunction in Alzheimer's disease. Cells. 2023; doi:10.3390/cells12060962.
- Overview. Critical Path for Alzheimer's Disease. https://c-path.org/programs/cpad/. Accessed March 29, 2023.
- Shi M, et al. Impact of anti-amyloid-β monoclonal antibodies on the pathology and clinical profile of Alzheimer's disease: A focus on aducanumab and lecanemab. Frontiers in Aging and Neuroscience. 2022; doi:10.3389/fnagi. 2022.870517 .
- Leqembi (approval letter). Biologic License Application 761269. U.S. Food and Drug Administration. https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=761269. Accessed July 7, 2023.
- Van Dyck CH, et al. Lecanemab in early Alzheimer's disease. New England Journal of Medicine. 2023; doi:10.1056/NEJMoa2212948.
- Leqembi (prescribing information). Eisai; 2023. https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&varApplNo=761269. Accessed July 10, 2023.
Products and Services
- A Book: Mayo Clinic on Alzheimer's Disease
- Assortment of Products for Independent Living from Mayo Clinic Store
- A Book: Day to Day: Living With Dementia
- A Book: Mayo Clinic on Healthy Aging
- Give today to find Alzheimer's cures for tomorrow
- Alzheimer's sleep problems
- Alzheimer's 101
- Understanding the difference between dementia types
- Alzheimer's disease
- Alzheimer's drugs
- Alzheimer's genes
- Alzheimer's prevention: Does it exist?
- Alzheimer's stages
- Antidepressant withdrawal: Is there such a thing?
- Antidepressants and alcohol: What's the concern?
- Antidepressants and weight gain: What causes it?
- Antidepressants: Can they stop working?
- Antidepressants: Side effects
- Antidepressants: Selecting one that's right for you
- Antidepressants: Which cause the fewest sexual side effects?
- Anxiety disorders
- Atypical antidepressants
- Caregiver stress
- Clinical depression: What does that mean?
- Corticobasal degeneration (corticobasal syndrome)
- Depression and anxiety: Can I have both?
- Depression, anxiety and exercise
- What is depression? A Mayo Clinic expert explains.
- Depression in women: Understanding the gender gap
- Depression (major depressive disorder)
- Depression: Supporting a family member or friend
- Diagnosing Alzheimer's
- Did the definition of Alzheimer's disease change?
- How your brain works
- Intermittent fasting
- Lecanemab for Alzheimer's disease
- Male depression: Understanding the issues
- MAOIs and diet: Is it necessary to restrict tyramine?
- Marijuana and depression
- Mayo Clinic Minute: 3 tips to reduce your risk of Alzheimer's disease
- Mayo Clinic Minute: Alzheimer's disease risk and lifestyle
- Mayo Clinic Minute: New definition of Alzheimer's changes
- Mayo Clinic Minute: Women and Alzheimer's Disease
- Memory loss: When to seek help
- Monoamine oxidase inhibitors (MAOIs)
- Natural remedies for depression: Are they effective?
- Nervous breakdown: What does it mean?
- New Alzheimers Research
- Pain and depression: Is there a link?
- Phantosmia: What causes olfactory hallucinations?
- Positron emission tomography scan
- Posterior cortical atrophy
- Seeing inside the heart with MRI
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Sundowning: Late-day confusion
- Treatment-resistant depression
- Tricyclic antidepressants and tetracyclic antidepressants
- Video: Alzheimer's drug shows early promise
- Vitamin B-12 and depression
- Young-onset Alzheimer's
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Alzheimer s treatments What s on the horizon
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
- International edition
- Australia edition
- Europe edition

New Alzheimer’s drug slows cognitive decline by 35%, trial results show
Donanemab is second drug in a year to succeed in trials in what could be ‘beginning of the end’ of disease
A new Alzheimer’s drug slowed cognitive decline by 35%, according to late-stage trial results, raising the prospect of a second effective treatment for the disease.
Donanemab met all goals of the trial and slowed progression of the condition by 35% to 36% compared with a placebo in 1,182 people with early-stage Alzheimer’s, the drugmaker Lilly said.
It comes after trial results published last year showed that lecanemab , made by Eisai and Biogen, reduced the rate of cognitive decline by 27% in patients with early Alzheimer’s.
“This could be the beginning of the end of Alzheimer’s disease,” said Dr Richard Oakley, the associate director of research at the Alzheimer’s Society in the UK. “After 20 years with no new Alzheimer’s drugs, we now have two potential new drugs in just 12 months – and for the first time, drugs that seem to slow the progression of disease.”
Maria Carrillo, the chief science officer of the Alzheimer’s Association in the US, also hailed donanemab’s trial results. “These are the strongest phase 3 data for an Alzheimer’s treatment to date,” she said.
Alzheimer’s is the most common cause of dementia, one of the world’s biggest health threats. The number of people living with dementia globally is forecast to nearly triple to 153 million by 2050, and experts have said it presents a rapidly growing threat to future health and social care systems in every community, country and continent.
In patients on donanemab, 47% showed no signs of the disease progressing after a year, according to a statement issued by Lilly . That compared to 29% on a placebo.
The drug resulted in 40% less decline in the ability to perform activities of daily living, the company said. Patients on donanemab also experienced a 39% lower risk of progressing to the next stage of disease compared to those on a placebo.
However, the company also reported side-effects.
Brain swelling occurred in 24% of those on donanemab, with 6.1% experiencing symptoms, Lilly said. Brain bleeding occurred in 31.4% of the donanemab group and 13.6% of the placebo group.
Lilly also said the incidence of serious brain swelling in the donanemab study was 1.6%, including two deaths attributed to the condition and a third death after an incident of serious brain swelling.
“The treatment effect is modest, as is the case for many first-generation drugs, and there are risks of serious side-effects that need to be fully scrutinised before donenemab can be marketed and used,” said Dr Susan Kohlhaas, the executive director of research and partnerships at Alzheimer’s Research UK.
But she said the results were still “incredibly encouraging” and represented “another hugely significant moment for dementia research”.
“We’re now on the cusp of a first generation of treatments for Alzheimer’s disease, something that many thought impossible only a decade ago,” she added. “People should be really encouraged by this news, which is yet more proof that research can take us ever closer towards a cure.”
Lilly said it planned to apply for approval from the US Food and Drug Administration next month, and with regulators in other countries shortly thereafter.
“At face value, these data look positive, but we need to see the full dataset,” said Dr Liz Coulthard, an associate professor in dementia neurology at the University of Bristol.
“Donanemab seems to help people with early Alzheimer’s retain cognitive function for longer – and this effect looks to be clinically meaningful. Donanemab might help people live well with Alzheimer’s for longer. If approved alongside lecanemab, this potentially brings a choice of treatments for patients.”
- Alzheimer's
- Pharmaceuticals industry

Air pollution could be significant cause of dementia – even for those not predisposed

Early blood test to predict dementia is step closer as biological markers identified

Blood test could revolutionise diagnosis of Alzheimer’s, experts say

Alcohol misuse and loneliness ‘increase risk of early-onset dementia’

Inequality leaving 115,000 dementia cases ‘undiagnosed’ in England

Gabriel García Márquez’s last novel stands in tribute to his defiance of dementia

Dementia risk factors pose more danger for ethnic minorities, finds study

Walks, tech and protein: how to parent your own parents

One of the hardest parts of getting older? Pondering the ‘me’ in dementia

‘Hard to know’ if Bruce Willis is aware of dementia condition, wife says
Most viewed.
Suggestions or feedback?
MIT News | Massachusetts Institute of Technology
- Machine learning
- Social justice
- Black holes
- Classes and programs
Departments
- Aeronautics and Astronautics
- Brain and Cognitive Sciences
- Architecture
- Political Science
- Mechanical Engineering
Centers, Labs, & Programs
- Abdul Latif Jameel Poverty Action Lab (J-PAL)
- Picower Institute for Learning and Memory
- Lincoln Laboratory
- School of Architecture + Planning
- School of Engineering
- School of Humanities, Arts, and Social Sciences
- Sloan School of Management
- School of Science
- MIT Schwarzman College of Computing
A new peptide may hold potential as an Alzheimer’s treatment
Press contact :, media download.
*Terms of Use:
Images for download on the MIT News office website are made available to non-commercial entities, press and the general public under a Creative Commons Attribution Non-Commercial No Derivatives license . You may not alter the images provided, other than to crop them to size. A credit line must be used when reproducing images; if one is not provided below, credit the images to "MIT."
Previous image Next image
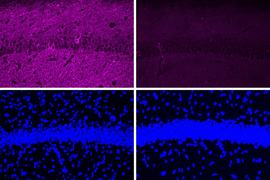
MIT neuroscientists have found a way to reverse neurodegeneration and other symptoms of Alzheimer’s disease by interfering with an enzyme that is typically overactive in the brains of Alzheimer’s patients.
When the researchers treated mice with a peptide that blocks the hyperactive version of an enzyme called CDK5, they found dramatic reductions in neurodegeneration and DNA damage in the brain. These mice also showed improvements in their ability to perform tasks such as learning to navigate a water maze.
“We found that the effect of this peptide is just remarkable,” says Li-Huei Tsai, director of MIT’s Picower Institute for Learning and Memory and the senior author of the study. “We saw wonderful effects in terms of reducing neurodegeneration and neuroinflammatory responses, and even rescuing behavior deficits.”
With further testing, the researchers hope that the peptide could eventually be used as a treatment for patients with Alzheimer’s disease and other forms of dementia that have CDK5 overactivation. The peptide does not interfere with CDK1, an essential enzyme that is structurally similar to CDK5, and it is similar in size to other peptide drugs that are used in clinical applications.
Picower Institute Research Scientist Ping-Chieh Pao is the lead author of the paper , which appears this week in the Proceedings of the National Academy of Sciences .
Targeting CDK5
Tsai has been studying CDK5’s role in Alzheimer’s disease and other neurodegenerative diseases since early in her career. As a postdoc, she identified and cloned the CDK5 gene, which encodes a type of enzyme known as a cyclin-dependent kinase. Most of the other cyclin-dependent kinases are involved in controlling cell division, but CDK5 is not. Instead, it plays important roles in the development of the central nervous system, and also helps to regulate synaptic function.
CDK5 is activated by a smaller protein that it interacts with, known as P35. When P35 binds to CDK5, the enzyme’s structure changes, allowing it to phosphorylate — add a phosphate molecule to — its targets. However, in Alzheimer’s and other neurodegenerative diseases, P35 is cleaved into a smaller protein called P25, which can also bind to CDK5 but has a longer half-life than P35.
When bound to P25, CDK5 becomes more active in cells. P25 also allows CDK5 to phosphorylate molecules other than its usual targets, including the Tau protein. Hyperphosphorylated Tau proteins form the neurofibrillary tangles that are one of the characteristic features of Alzheimer’s disease.
In previous work, Tsai’s lab has shown that transgenic mice engineered to express P25 develop severe neurodegeneration. In humans, P25 has been linked to several diseases, including not only Alzheimer’s but also Parkinson’s disease and frontotemporal dementia.
Pharmaceutical companies have tried to target P25 with small-molecule drugs, but these drugs tend to cause side effects because they also interfere with other cyclin-dependent kinases, so none of them have been tested in patients.
The MIT team decided to take a different approach to targeting P25, by using a peptide instead of a small molecule. They designed their peptide with a sequence identical to that of a segment of CDK5 known as the T loop, which is a structure critical to the binding of CDK5 to P25. The entire peptide is only 12 amino acids long — slightly longer than most existing peptide drugs, which are five to 10 amino acids long.
“From a peptide drug point of view, usually smaller is better,” Tsai says. “Our peptide is almost within that ideal molecular size.”
Dramatic effects
In tests in neurons grown in a lab dish, the researchers found that treatment with the peptide led to a moderate reduction in CDK5 activity. Those tests also showed that the peptide does not inhibit the normal CDK5-P35 complex, nor does it affect other cyclin-dependent kinases.
When the researchers tested the peptide in a mouse model of Alzheimer’s disease that has hyperactive CDK5, they saw a myriad of beneficial effects, including reductions in DNA damage, neural inflammation, and neuron loss. These effects were much more pronounced in the mouse studies than in tests in cultured cells.
The peptide treatment also produced dramatic improvements in a different mouse model of Alzheimer’s, which has a mutant form of the Tau protein that leads to neurofibrillary tangles. After treatment, those mice showed reductions in both Tau pathologies and neuron loss. Along with those effects in the brain, the researchers also observed behavioral improvements. Mice treated with the peptide performed much better in a task that required learning to navigate a water maze, which relies on spatial memory, than mice that were treated with a control peptide (a scrambled version of the peptide used to inhibit CDK5-P25).
In those mouse studies, the researchers injected the peptide and found that it was able to cross the blood-brain barrier and reach neurons of the hippocampus and other parts of the brain.
The researchers also analyzed the changes in gene expression that occur in mouse neurons following treatment with the peptide. Among the changes they observed was an increase in expression of about 20 genes that are typically activated by a family of gene regulators called MEF2. Tsai’s lab has previously shown that MEF2 activation of these genes can confer resilience to cognitive impairment in the brains of people with Tau tangles, and she hypothesizes that the peptide treatment may have similar effects.
“Further development of such peptide inhibitors toward a lead therapeutic candidate, if proven to be selective for the target and relatively free of clinical side effects, may eventually lead to novel treatments for neurodegenerative disorders ranging from Alzheimer’s disease to Frontotemporal dementia to Parkinson’s disease,” says Stuart Lipton, a professor of neuroscience at Scripps Research, who was not involved in the study.
Tsai now plans to do further studies in other mouse models of diseases that involve P25-associated neurodegeneration, such as frontotemporal dementia, HIV-induced dementia, and diabetes-linked cognitive impairment.
“It’s very hard to say precisely which disease will most benefit, so I think a lot more work is needed,” she says.
The research was funded by the National Institutes of Health.
Share this news article on:
Press mentions, new york post.
In a new study, researchers at MIT showed that they “were able to interfere with an enzyme typically found to be overactive in the brains of Alzheimer’s patients,” reports Alex Mitchell for The New York Post . After using a peptide to treat the overactive enzyme, they found that “the peptide shows protective effects against loss of neurons and also appears to be able to rescue some of the behavior deficits,” says Prof. Li-Huei Tsai.
Previous item Next item
Related Links
- Li-Huei Tsai
- Department of Brain and Cognitive Sciences
Related Topics
- Neuroscience
- Alzheimer's
- Brain and cognitive sciences
- Picower Institute
- National Institutes of Health (NIH)
Related Articles

Study links gene to cognitive resilience in the elderly

Study offers an explanation for why the APOE4 gene enhances Alzheimer’s risk

Neuroscientists discover roles of gene linked to Alzheimer’s
![new research dementia alzheimer's “…[I]f humans behave similarly to mice in response to this treatment, I would say the potential is just enormous, because it’s so noninvasive, and it’s so accessible,” says Li-Huei Tsai, the Picower Professor of Neuroscience, when describing a new treatment for Alzheimer’s disease.](https://news.mit.edu/sites/default/files/styles/news_article__archive/public/images/201612/MIT-li-huei-tsai.jpg?itok=jrC2K2AI)
Unique visual stimulation may be new treatment for Alzheimer’s
More mit news.
Does technology help or hurt employment?
Read full story →

Most work is new work, long-term study of U.S. census data shows
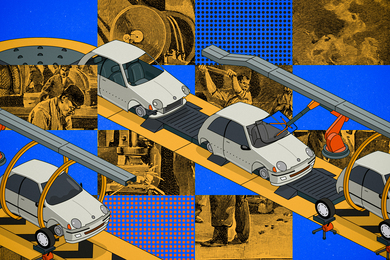
A first-ever complete map for elastic strain engineering

“Life is short, so aim high”

Shining a light on oil fields to make them more sustainable

MIT launches Working Group on Generative AI and the Work of the Future
- More news on MIT News homepage →
Massachusetts Institute of Technology 77 Massachusetts Avenue, Cambridge, MA, USA
- Map (opens in new window)
- Events (opens in new window)
- People (opens in new window)
- Careers (opens in new window)
- Accessibility
- Social Media Hub
- MIT on Facebook
- MIT on YouTube
- MIT on Instagram
- Open access
- Published: 02 October 2023
Clinical trials of new drugs for Alzheimer disease: a 2020–2023 update
- Li-Kai Huang 1 , 2 , 3 na1 ,
- Yi-Chun Kuan 2 , 3 , 4 , 5 na1 ,
- Ho-Wei Lin 6 &
- Chaur-Jong Hu ORCID: orcid.org/0000-0002-4900-5967 1 , 2 , 3 , 4
Journal of Biomedical Science volume 30 , Article number: 83 ( 2023 ) Cite this article
19k Accesses
17 Citations
24 Altmetric
Metrics details
Alzheimer's disease (AD) is the leading cause of dementia, presenting a significant unmet medical need worldwide. The pathogenesis of AD involves various pathophysiological events, including the accumulation of amyloid and tau, neuro-inflammation, and neuronal injury. Clinical trials focusing on new drugs for AD were documented in 2020, but subsequent developments have emerged since then. Notably, the US-FDA has approved Aducanumab and Lecanemab, both antibodies targeting amyloid, marking the end of a nearly two-decade period without new AD drugs. In this comprehensive report, we review all trials listed in clinicaltrials.gov, elucidating their underlying mechanisms and study designs. Ongoing clinical trials are investigating numerous promising new drugs for AD. The main trends in these trials involve pathophysiology-based, disease-modifying therapies and the recruitment of participants in earlier stages of the disease. These trends underscore the significance of conducting fundamental research on pathophysiology, prevention, and intervention prior to the occurrence of brain damage caused by AD.
Alzheimer disease (AD) represents a major global medical, social, and economic burden. The World Alzheimer Report 2022 revealed that more than 55 million people have AD or related conditions worldwide, and this number is projected to reach 82 million by 2030 and 138 million by 2050 [ 1 ]. Typically, AD first manifests as progressive memory decline accompanied or followed by other cognitive dysfunctions, such as visuospatial abnormalities, navigation difficulties, executive problems, and language disturbances. These cognitive impairments affect the performance of activities of daily living. During the course of AD, many behavioral and psychological symptoms of dementia (BPSD) occur [ 2 , 3 , 4 ].
Although the exact causes of AD remain unclear, the disease has two pathological hallmarks: plaques composed of amyloid-beta (Aβ) fibrils and neurofibrillary tangles (NFTs) consisting of hyperphosphorylated tau protein [ 5 , 6 , 7 ]. The key event in AD pathogenesis is believed to be Aβ accumulation. Cerebral Aβ fibril deposition may occur decades before the onset of clinical symptoms [ 8 ]. Brain atrophy, particularly in the hippocampus, is major indicator of early Aβ accumulation, particularly in the presubiculum [ 9 , 10 ]. Aβ accumulation was discovered to be crucial by three independent research groups in 1991 [ 11 , 12 , 13 ]. In familial AD, mutant autosomal-dominant genes, including the genes for amyloid precursor protein ( APP ), presenilin-1 ( PSEN1 ), and presenilin-2 ( PSEN2 ), encode the major proteins involved in amyloid metabolism [ 13 , 14 , 15 ]. Individuals with trisomy 21 (Down syndrome) have an extra copy of the APP gene, which may result in increased amyloid production and AD risk in middle age [ 16 ]. At present, the predominant theory regarding the cause of AD is the amyloid hypothesis; crucial advancements in AD therapy have been made on the basis of the proposed role of amyloid accumulation in the AD development. The United States Food and Drug Administration (US FDA) granted traditional approval for Leqembi (lecanemab-irmb) on July 6, 2023, for the treatment of AD [ 17 ]. The approval of this treatment not only affirms the pathophysiological significance of amyloid in AD but also marks a notable advance in clinical approaches to AD treatment, remedying the scarcity of new drugs in the market for nearly two decades.
Tau is a microtubule-associated protein that aids in microtubule assembly and stabilization. In AD, tau becomes hyperphosphorylated and aggregates to form paired helical filaments, a major component of NFTs within the neuronal cytoplasm. As the disease progresses, the gradual spread of tau pathology throughout brain regions has been suggested to be caused by the transfer of abnormal types of tau protein from one neuron to another [ 18 ]. The accumulation of NFTs might be initiated between the accumulation of Aβ and the development of clinical symptoms of AD [ 19 ]. NFTs and quantitative neuronal loss may be more closely correlated with disease severity and dementia progression than the amyloid plaque burden [ 20 , 21 , 22 ]. Positron emission tomography (PET) investigations have revealed a strong correlation between the binding characteristics of tau tracers and the severity of clinical manifestations in individuals with AD [ 23 ]. Molecular imaging modalities (PET) and cerebrospinal fluid (CSF) and blood–based biomarkers have extended the diagnostic scope of AD pathology to both clinical and even preclinical settings. The analysis of a combination of biomarkers such as amyloid, tau, and neurodegeneration (collectively, ATN classification) has been proposed by research on AD [ 24 , 25 ]. Furthermore, the exceptional diagnostic accuracy of plasma-based biomarkers has facilitated the clinical transition of fluid biomarkers from research settings to clinical practice. A recent presentation at the Alzheimer’s Association International Conference in 2023 highlighted the clinical and research applications of two fundamental AD biomarker categories, labeled as A and T. The A category pertains to biomarkers associated with the Aβ proteinopathy pathway, and the T category pertains to biomarkers linked to tau proteinopathy [ 26 ].
Aβ serves as a proinflammatory agent and triggers the nuclear factor κB (NF-κB) pathway in astrocytes, increasing complement C3 release. Subsequently, by binding to C3a receptors, C3 causes neuronal dysfunction and microglial activation [ 27 ]. In the early stage of AD, activated microglia may play a protective, anti-neuroinflammatory role by clearing amyloids and releasing nerve growth factors. However, activated microglia induce neurotoxic A1 astrocyte reactivity through the release of IL-1α, C1q, and TNF-α, resulting in a feedback loop of dysregulated inflammation in AD [ 28 ]. The excessive accumulation of Aβ or other toxic compounds activates proinflammatory phenotypes, resulting in neuronal damage [ 29 ]. Sustained inflammation has been observed in the brains of patients with AD [ 30 , 31 ]. The inadequate clearance of Aβ along with the aggregation of tau disrupts microglial defense mechanisms, resulting in sustained and harmful microglial activation [ 32 ]. The sequential occurrence of amyloid plaque formation, microglial activation, and the pathological phosphorylation and aggregation of tau proteins to form NFTs is the fundamental notion of the amyloid cascade–inflammation hypothesis. In the Multi-Ethnic Study of Atherosclerosis (multiple covariates were controlled for), vascular risk factor profiles and Aβ deposition significantly predicted cognitive decline [ 33 ]. Vascular risk factors can also lead to inflammation in the brain, which damages neuronal cells and further increases the likelihood of AD dementia [ 34 ].
The role of autophagy impairment is proposed in a novel hypothesis concerning plaque formation in AD. Among neurons that are compromised but still maintain some integrity, autophagic vacuoles (AVs) containing abundant Aβ are notably present. These AVs cluster within expansive membrane blebs, exhibiting a distinctive flower-like arrangement termed PANTHOS. These formations constitute the primary source of the majority of amyloid plaques found in mouse models of AD [ 35 ]. Neuroprotective therapies, including free radical scavengers, regeneration enhancers, and the suppression of excitable amino acid signaling pathways, have been proposed for preventing neuronal death or brain atrophy caused by amyloid, tau, and neuroinflammation [ 36 ]. Pathological evidence indicates that AD is also associated with degeneration in cholinergic neuron-rich regions, such as the nucleus basalis of Meynert, frontal cortex, and anterior and posterior cingulate cortex, which can lead to the symptoms of memory impairment and agitation. Acetylcholine (ACh) plays a vital role in memory function, including memory encoding, consolidation, and retrieval processes, and increasing Ach levels by using cholinesterase inhibitors (AChEIs) has become a standard therapy for the symptoms of AD [ 37 ].
Clinical trials of early or preventive interventions based on amyloid/tau theory and those targeting other pathophysiologies are ongoing or have been initiated. Many ongoing clinical trials on AD are focused on disease-modifying therapies (DMTs) that target the causes and can change the course of AD. The other trials involve symptomatic treatments—for example, enhancing cognitive function and relieving BPSD (Fig. 1 ). In this review, we summarize the new drugs being examined in ongoing trials (listed on ClinicalTrials.gov) and discuss the trends in and obstacles in AD clinical trials.

According to the amyloid hypothesis, the pathophysiology and clinical course of Alzheimer's disease progress as follows: amyloid accumulation, neuroinflammation, tau accumulation, brain metabolism dysfunction, brain atrophy, cognitive decline (from mild cognitive impairment to dementia), and the development of dementia symptoms. Novel drugs should target at least one of these events. AD Alzheimer's disease, aMCI amnestic mild cognitive impairment, BPSD behavioral psychological symptoms of dementia
Anti-amyloid therapy
Table 1 summarizes the US FDA approval status of anti-amyloid agents. Tables 2 and 3 summarize the ongoing phase 3 and phase 2 trials of anti-amyloid therapy respectively.
Aducanumab (brand name: Aduhelm) is a high-affinity, fully human immunoglobulin gamma 1 (IgG1) monoclonal antibody that binds to the N-terminus of Aβ fibrils and blocks amyloid aggregation [ 38 ]. In August 2015, two phase 3 clinical trials, namely ENGAGE and EMERGE studies, were initiated. These trials compared monthly intravenous infusions of aducanumab at one of three doses with infusions of placebo over 18 months, and the primary outcomes were cognitive and functional decline, which were assessed using the Clinical Dementia Rating (CDR) scale Sum of Boxes (CDR-SB). The secondary outcomes were other cognitive and functional measures. The trials were conducted in 150 centers across North America, Europe, Australia, and Asia. However, the findings of the EMERGE trial reached statistical significance, whereas the primary endpoint was not reached in the ENGAGE trial. An exploratory analysis revealed that a subgroup of the participants in the ENGAGE trial who received a high dose of aducanumab exhibited slow decline, which was similar to that observed among the participants in the EMERGE trial. The US FDA approved aducanumab in June 2021 on the basis of the data of the EMERGE and ENGAGE trials. Both trials presented evidence of an intermediate effect of the drug on biomarkers, indicating amyloid removal, which is likely linked to the clinical benefit of aducanumab. Further trials must be conducted to confirm the potential benefit of aducanumab [ 39 ]. The phase 3b/4 ENVISION trial (NCT05310071), which began in 2022, will enroll 1,512 patients with early AD who will receive either monthly doses of aducanumab of up to 10 mg/kg or placebo for 18 months. The aim of the trial is to determine the efficacy of aducanumab in delaying cognitive and functional decline in comparison with placebo, which would be determined on the basis of CDR-SB scores. The secondary endpoints of the trial include scores on the Alzheimer’s Disease Assessment Scale–Cognitive Subscale (ADAS-Cog) 13, Alzheimer’s Disease Cooperative Study–Activities of Daily Living Inventory (ADCS-ADL)–Mild Cognitive Impairment Version, Integrated Alzheimer’s Disease Rating Scale (iADRS), Mini-Mental State Examination, and Neuropsychiatric Inventory. The trial intends to recruit 18% of its participants from Black and Latinx populations in the United States and will have a long-term follow-up of up to 4 years, with results expected by 2026. The EMBARK trial (NCT04241068) is a phase 3b open-label study including 1,696 participants from previous aducanumab trials (from trials 221AD103, 221AD301, 221AD302, and 221AD205) that will assess aducanumab safety and tolerability over 100 weeks after a wash-out period. Participants will receive an intravenous infusion of aducanumab at 10 mg/kg monthly for 2 years, and eligible participants will continue to receive the infusion for another 52 weeks during the long-term extended treatment period. The primary outcomes are safety and tolerability, and the efficacy endpoints are the same as those in the EMERGE and ENGAGE trials, and Caregiver Global Impression of Change evaluations will be conducted every 6 months. All participants will undergo volumetric magnetic resonance imaging (MRI) scans, and a subset of the study population will undergo biomarker testing, including amyloid PET, tau PET, and CSF testing.
Lecanemab (brand name: Leqembi), a humanized IgG1 antibody derived from mAb158, selectively binds to soluble Aβ protofibrils [ 40 ]. The US FDA approved it on January 6, 2023, through an accelerated approval pathway on the basis of evidence of amyloid removal in a phase 2 trial (NCT01767311) and because it had a likelihood of having clinical benefits [ 41 ] A double-blind, placebo-controlled phase 2 trial recruited 856 patients with AD with mild cognitive impairment (MCI) or mild dementia and verified amyloid pathology through amyloid PET or CSF Aβ1-42 [ 42 ]. The results revealed a significant and dose-dependent reduction of amyloid plaques in the lecanemab group (10 mg/kg, intravenous infusion every 2 weeks) from baseline to week 79 compared with the placebo group. At the time of writing this paper, three phase 3 clinical trials on lecanemab are underway. The first trial, Clarity AD (NCT03887455), was initiated in March 2019 and was conducted at 250 sites around the world. It reported favorable outcomes for all primary and secondary measures, including ADAS-Cog14, AD Composite Score (ADCOMS), and ADCS-MCI-ADL scores [ 43 ]. The second trial is AHEAD 3–45 (NCT04468659), which was initiated in July 2020 as a 4-year trial comprising two substudies, one of which is A3, and the other one is A45. A3 is enrolling 400 people whose amyloid levels are below the brain-wide threshold for positivity; participants will receive 5 mg/kg lecanemab titrated to 10 mg/kg or placebo every month for 216 weeks. A45 is enrolling 1,000 cognitively healthy participants with positive amyloid PET scans, and they will receive lecanemab titrated to 10 mg/kg every 2 weeks for 96 weeks, followed by 10 mg/kg every month through week 216. The trial is expected to run until October 2027. The third phase 3 clinical trial is the Dominantly Inherited Alzheimer Network Trials Unit (DIAN-TU) Next Generation trial (DIAN-TU-001 (E2814), NCT05269394), in which a combination of lecanemab and the anti-tau antibody E2814 (phase 2) will be administered to 168 people with familial AD mutations. On July 6, 2023, Leqembi (lecanemab-irmb) received traditional approval from the US FDA for the treatment of AD based on Phase 3 data from the Clarity AD clinical trial [ 17 ].
The appropriate use recommendations (AURs) for lecanemab and aducanumab highlight the importance of patient selection, surveillance for adverse events, and clinician preparedness [ 44 , 45 ]. The AURs for both drugs have several similarities with respect to age criteria, biomarker requirements (positive amyloid PET or CSF findings indicative of AD), diagnosis (MCI due to AD or mild AD dementia), and MRI exclusion criteria (e.g., microhemorrhages and cortical infarction). The AURs also emphasize the importance of monitoring for amyloid-related imaging abnormalities (ARIAs), which can occur in patients receiving these drugs. APOE genotyping is recommended for informing risk discussions with candidate participants because APOE4 allele carriers, especially APOE4 homozygotes, are at a high risk of ARIAs. Patients receiving treatment must have care partners or family members who can provide necessary support and who clearly understand the nature and requirements of the therapy. Discontinuation of treatment is recommended in the following situations: when a patient is taking drugs with associated risks, such as anticoagulation agents for conditions like atrial fibrillation, deep vein thrombosis, or pulmonary embolism; or when any of the following conditions occur: a hypercoagulable state, or the development of any of the following: cerebral macrohemorrhage, multiple areas of superficial siderosis, more than 10 instances of microhemorrhages since treatment initiation, severe symptoms of ARIAs, or two or more episodes of ARIAs.
Donanemab is a humanized monoclonal antibody developed from mouse mE8-IgG2a. It recognizes Aβ (3–42), an aggregated form of Aβ found in amyloid plaques [ 46 ]. It was discovered to be bound to approximately one-third of amyloid plaques in postmortem brain samples of patients with AD or Down syndrome, and it strongly reacted with the plaque core [ 47 ]. In the phase 2 TRAILBLAZER-ALZ study, the safety, tolerability, and efficacy of donanemab alone and in combination with the Beta-Secretase 1 (BACE1) inhibitor LY3202626 (developed by Eli Lilly and Company) were evaluated over 18 months. The trial met its primary endpoint of delaying decline—which was determined on the basis of iADRS scores—by 32% compared with placebo. Amyloid burden reduction was correlated with improvement in iADRS scores only in ApoE4 carriers [ 48 ]. Donanemab reduced the tau burden in the temporal, parietal, and frontal lobes and significantly decreased plasma pTau217 by 24% in the treatment group, whereas the placebo group exhibited a 6% increase in plasma pTau217 at the end of the trial [ 49 ]. At the time of writing this paper, five phase 3 trials of donanemab are underway: TRAILBLAZER-ALZ 2, TRAILBLAZER-ALZ 3, TRAILBLAZER-ALZ 4, TRAILBLAZER-ALZ 5 and TRAILBLAZER-ALZ 6. The TRAILBLAZER-ALZ 2 (NCT04437511) trial was initially started in June 2020 as a phase 2 safety and efficacy trial, and 500 patients with early AD were recruited. Inclusion criteria of TRAILBLAZER-ALZ 2 are similar to those of TRAILBLAZER-ALZ: a ≥ 6-month history of worsening memory and positive amyloid (flortaucipir) PET. The trial was subsequently extended to a phase 3 trial with 1,800 participants. The primary outcome is iADRS, and the effectiveness of treatment is being measured using a disease-progression model rather than solely on the basis of changes at the final time point. Trial results for 1,736 participants were published to report donanemab’s impact on early symptomatic AD. Using PET imaging to categorize individuals into groups with low/medium or high tau pathology load, the study spanned 18 months and assessed cognitive and functional scales. Donanemab achieved significant cognitive improvement in the low/medium tau group (iADRS change: − 6.02 vs. − 9.27 placebo) and combined population (change: − 10.2 vs. − 13.1 placebo). The drug notably reduced decline by 60% in patients with early-stage AD, supporting the efficacy of short-term dosing. Twenty-four outcomes were evaluated, with significant findings for 23 outcomes. Adverse effects included amyloid-related imaging problems (24% donanemab vs. 2.1% placebo) and infusion-related reactions (8.7% donanemab vs. 0.5% placebo). The study findings indicated the potential of donanemab to slow AD progression, particularly in the early stage [ 50 ]. In the TRAILBLAZER-ALZ study, donanemab slowed disease progression by 32% at 18 months ( p = 0.04 vs. placebo), thus demonstrating clinical efficacy [ 51 ]. TRAILBLAZER-ALZ 3 (NCT05026866) is a placebo-controlled phase 3 prevention trial that was started in August 2021. The trial plans to enroll 3,300 cognitively healthy people aged 50–55 years who are at high risk of AD, as determined by elevated plasma pTau217 levels and Telephone Interview for Cognitive Status-modified scores. The primary outcome is the time to clinical progression, which is measured using global CDR scores. Participants are to be monitored every 6 months until cognitive impairment is noted (i.e., a score above 0 on the CDR for two consecutive evaluations) in 434 participants. The trial has a decentralized design and is being conducted at more than 200 sites in the United States, Japan, and Puerto Rico until November 2027. TRAILBLAZER-ALZ 4 (NCT05108922) is a phase 3, open-label, head-to-head comparison of amyloid clearance by either donanemab or aducanumab that began in November 2021 after the US FDA approval of aducanumab. The trial enrolled 200 people with early symptomatic AD, as indicated by a global CDR score of 0.5 or 1, at 31 sites in the United States. The primary outcome is the percentage of participants who achieve complete amyloid plaque clearance after 6 months for each treatment group, with clearance determined using amyloid (florbetapir) PET. The trial has 17 secondary outcomes, which are all related to amyloid PET measurements at up to 18 months. The preliminary results were presented at the 2022 Clinical Trial of AD (CTAD) conference: 38% of the patients on donanemab exhibited amyloid levels below the amyloid positivity threshold after 6 months, whereas only 2% of the patients on aducanumab has such findings. Plasma pTau217 levels decreased by 25% for the participants receiving donanemab, but not at all for those receiving aducanumab. The side effect of ARIA-edema occurred in 22% of the participants in both groups. TRAILBLAZER-ALZ 5 (NCT05508789) is being conducted to assess the safety and efficacy of donanemab in individuals with early symptomatic AD. The trial started in October 2022; 1,500 participants will be recruited by using the same criteria as those of TRAILBLAZER-ALZ 2 from 148 sites across China, Korea, Taiwan, and Europe; and the trial is expected to run until mid-2025. Participants will be administered monthly infusions of either donanemab or placebo, and the primary outcome will be measured on the basis of iADRS score changes after 18 months. TRAILBLAZER-ALZ 6 (NCT05738486) is a phase 3b study that will assess the impact of various dosing regimens of donanemab on the occurrence and severity of ARIA-E (ARIA with edema or effusion) in 800 adults with early symptomatic AD. The study also seeks to identify participant characteristics that predict the risk of ARIA-E. The trial is divided into four arms, each with a distinct donanemab dose.
Remternetug is a monoclonal antibody that recognizes a pyroglutamated form of Aβ that aggregates into amyloid plaques. In August 2022, Eli Lilly and Company initiated a phase 3 trial called TRAILRUNNER-ALZ1 (NCT05463731) that will randomize 600 patients with early symptomatic AD across 75 sites in the United States and 2 sites in Japan into groups receiving the antibody or placebo through intravenous infusion or subcutaneous injection for 1 year. The primary outcome is the percentage of patients whose amyloid plaques are cleared by the end of the treatment period. The secondary outcomes include the measurement of amyloid clearance, pharmacokinetics, and treatment-emergent anti-drug antibodies. The study also plans to conduct a year-long, blinded crossover extension. An additional safety cohort of 640 patients will receive open-label remternetug for 1 year.
Solanezumab is a humanized monoclonal antibody that targets the mid-domain of the Aβ peptide for increasing Aβ clearance [ 52 ]. Phase 3 trials of solanezumab, including EXPEDITION-1 and EXPEDITION-2, which enrolled 2,052 patients with mild-to-moderate AD, did not reveal improvements in ADAS-Cog11 and ADCS-ADL scores, which were the primary outcome measures. Similarly, the phase 3 trial EXPEDITION-3 demonstrated that 400 mg solanezumab administered every 4 weeks did not have significant effects on cognitive decline in patients with mild AD [ 52 ]. A4 (NCT02008357) is a phase 3 prevention trial focused on slowing memory and cognitive decline in elderly individuals without cognitive impairment or dementia. A4 is using a sensitive cognitive battery—the Alzheimer Disease Cooperative Study Preclinical Alzheimer Cognitive Composite—and was initiated in February 28, 2014. On March 8, 2023, Eli Lilly and Company reported that solanezumab did not slow cognitive decline or clear amyloid plaques in individuals with preclinical AD in the A4 study. DIAN-TU-001 (NCT01760005) is another ongoing phase 3 clinical trial that is testing the combination of solanezumab and gantenerumab in 210 asymptomatic and mildly symptomatic carriers of autosomal-dominant mutations in AD genes. However, on February 10, 2020, the study investigators announced that the primary endpoint was not achieved in the trial, namely treatment-related changes on the DIAN-Multivariate Cognitive Endpoint. The results indicated that the solanezumab-treated group had greater cognitive decline on some measures relative to placebo, and that solanezumab treatment did not exert any beneficial effects on downstream biomarkers, whereas gantenerumab significantly reduced amyloid plaques, CSF total tau, and phospho-tau181 and attenuated increases in neurofilament light chain [ 53 ]. The participants were offered an open-label extension with high-dose gantenerumab because of its positive effects on imaging and other biomarkers, such as normalized CSF Aβ42, and because it reduced CSF total tau and pTau181 levels.
ALZ-801 is a prodrug of tramiprosate, a small molecule of anti-Aβ oligomers and an aggregation inhibitor [ 54 ]. The phase 3 trial APOLLOE4 (NCT04770220) is evaluating the safety and efficacy of ALZ-801 for patients with early AD and carrying the homozygous ε4 allele on the apolipoprotein E gene ( APOE4/4 ). The recruited patients are receiving 265 mg ALZ-801 or placebo twice daily for 18 months. The trial started in May 2021. The primary endpoint is ADAS-Cog scores, and the secondary endpoints are scores of the Disability Assessment for Dementia, CDR-SB, and Amsterdam-iADL. The biomarkers of interest include the hippocampal volume, as determined through MRI and based on CSF and plasma pTau181 levels. Another phase 2 trial (NCT04693520) is investigating the effects of oral ALZ-801 administered to participants with early AD who have the APOE4/4 or APOE3/4 genotype with biomarkers of core AD pathology. The study is also assessing the efficacy, safety, and tolerability of ALZ-801.
Simufilam (PTI-125) is a drug that binds to filamin, a scaffolding protein that stabilizes the interaction between soluble Aβ42 and the α7 nicotinic acetylcholine receptor [ 55 ]. Two phase 3 trials, namely RETHINK-ALZ (NCT04994483) and REFOCUS-ALZ (NCT05026177), were commenced in November 2021. Both are safety and efficacy studies of simufilam and have enrolled participants with mild-to-moderate AD. RETHINK-ALZ will randomize 750 participants with AD and CDR scores of 0.5, 1, or 2 into groups receiving either placebo or 100 mg of simufilam twice a day for 1 year (52 weeks). The coprimary outcomes of this trial are ADAS-Cog12 and ADCS-ADL scores, and the trial is set to run through October 2023. REFOCUS-ALZ will randomize 1,083 participants into groups receiving placebo or 50 or 100 mg of simufilam (1:1:1) for 76 weeks. The primary outcome measures are similar to those of the RETHINK-ALZ trial. A phase 3 trial of simufilam (NCT05575076) was started in November 2022 to assess the long-term safety and tolerability of simufilam in participants with mild-to-moderate AD. That open-label extension study is intended to assess the long-term safety and tolerability of simufilam 100 mg twice daily in patients who have completed the RETHINK-ALZ or REFOCUS-ALZ Phase 3 clinical trials. The primary outcome measure is adverse event monitoring from baseline to week 52.
Varoglutamstat (PQ912) is a glutaminyl cyclase inhibitor that reduces pGlu-Aβ generation [ 56 ]. Glutaminyl cyclase catalyzes the cyclization of an exposed glutamate at the N-terminus of Aβ, resulting in the formation of toxic pGlu-Aβ, a major component of amyloid plaques. Two ongoing phase 2 clinical trials, namely VIVA-MIND and VIVIAD, are evaluating the safety, tolerability, and efficacy of varoglutamstat in participants with MCI and mild dementia due to AD. VIVA-MIND (NCT03919162) is a phase 2A multicenter, randomized, double-blind, placebo-controlled, parallel-group study of varoglutamstat, with a stage gate to phase 2B. Phase 2A involves an adaptive dosing evaluation of three doses of varoglutamstat or placebo for ≥ 24 weeks. VIVIAD (NCT04498650) is a phase 2B, multicenter, randomized, double-blind, placebo-controlled, parallel-group, dose-finding study being conducted to evaluate the safety, tolerability, and efficacy of varoglutamstat in 259 participants with MCI and mild dementia due to AD.
ABBV-916 is a monoclonal antibody to Aβ. It recognizes N-terminal truncated Aβ modified with pyroglutamate at position 3 (N3), a form of Aβ that is aggregated into amyloid plaques. A two-stage phase 2 trial of ABBV-916 is ongoing (NCT05291234). Stage A is a multiple ascending dose study, and participants have a 25% chance of receiving placebo. Stage B is a proof-of-concept study, and participants have a 20% chance of receiving placebo. The first 6 months of the study are a double-blinded period, which is to be followed by a 2-year extension period in which all participants receive ABBV-916. Approximately 195 participants aged 50–90 years are to be enrolled at approximately 90 sites across the world. The participants are to receive intravenous doses of ABBV-916 or placebo once every 4 weeks for 24 weeks and are to be followed up for an additional 16 weeks.
CT1812 is a ligand that targets the component 1 subunit of the sigma2/progesterone membrane receptor. It functions as a negative allosteric regulator, reducing the affinity of oligomeric Aβ and interfering with Aβ-induced synaptic toxicity [ 57 ]. START(COG0203) study (NCT05531656) is a phase 2, multicenter, randomized, double-blind, placebo-controlled trial that was initiated in September 2022 for evaluating the efficacy and safety of CT1812. START is comparing the effects of CT1812 (100 or 300 mg) with those of placebo over 18 months in 540 people with MCI or mild dementia due to AD. The SHINE (COG0201) study (NCT03507790) is a multicenter, randomized, double-blind, placebo-controlled, parallel-group, 36-week phase 2 study of two doses of CT1812 in adults with mild-to-moderate AD. The study is evaluating the safety, tolerability, pharmacokinetics, and efficacy of CT1812.
Anti-tau therapy
Table 4 summarizes the ongoing phase 2 trials of anti-tau therapy.
Bepranemab (UCB0107) is a monoclonal IgG4 antibody that targets a central tau epitope. An ongoing phase 2 trial (NCT04867616) enrolling 421 participants with prodromal or mild AD is investigating the safety, tolerability, and efficacy of bepranemab. After an 80-week double-blinded treatment period, the participants are eligible to enter a 48-week open-label extension period, in which they are to receive bepranemab treatment for 44 weeks. Subsequently, they are to participate in a safety evaluation visit 20 weeks after the last infusion. The primary outcome measure is the CDR-SB score.
JNJ-63733657 is a humanized IgG1 monoclonal antibody that targets the microtubule-binding region of tau and prevents the cell-to-cell propagation of pathogenic tau aggregates. The AUTONOMY trial (NCT04619420) is an ongoing phase 2, randomized, double-blind, placebo-controlled, parallel-group multicenter study. Participants with early AD symptoms and a positive tau PET scan are randomized to groups receiving JNJ-63733657 or placebo. This trial is enrolling 420 participants and is expected to be completed by November 2025. The primary outcome measure is clinical decline, as determined using the iADRS.
ACI-35 is a liposome-based vaccine that targets pathological conformations of phosphorylated tau. A phase 1b/2a multicenter, double-blind, randomized, placebo-controlled trial (NCT04445831) was conducted to evaluate the safety, tolerability, and immunogenicity of various doses, regimens, and combinations of tau-targeting vaccines in individuals with early AD. The vaccines tested were JACI-35.054 and ACI-35.030 at various dose levels. The findings were presented at the 2022 CTAD conference. The results indicated that participants who received ACI-35.030 exhibited a strong and sustained immune response against pathological tau proteins (pTau) and nonphosphorylated tau (ePHF), particularly in the mid- and low-dose groups. Recipients of JACI-35.054 also displayed a robust immune response against ePHF and pTau, but without a clear dose–effect relationship. The trial has been conducted across nine centers in Finland, Sweden, the Netherlands, and the United Kingdom and is expected to be completed by October 2023.
E2814 is a monoclonal IgG1 antibody that targets an HVPGG epitope in the microtubule-binding domain of tau, prevents cell-to-cell propagation, and mediates the clearance of pathogenic tau proteins. The DIAN-TU-001 (E2814) trial (NCT05269394) is a phase 2/3 multicenter, randomized, double-blind, placebo-controlled platform trial of potential disease-modifying therapies with biomarker, cognitive, and clinical endpoints. The trial is enrolling patients with dominantly inherited AD. The study design involves the use of the anti-amyloid antibody lecanemab. Some participants are receiving a matching placebo plus lecanemab, whereas others are receiving concurrent therapy with E2814 plus lecanemab.
LY3372689 is a small-molecule inhibitor of O-GlcNAcase, which promotes tau glycosylation and prevents tau aggregation [ 58 ]. A phase 2 trial (NCT05063539) was initiated in September 2021 for assessing the safety, tolerability, and efficacy of LY3372689 in 330 patients with early symptomatic AD with progressive memory changes for ≥ 6 months and who met the criterion of having a positive flortaucipir-PET scan.
BIIB080 is a tau DNA/RNA-based antisense oligonucleotide that inhibits the translation of tau mRNA into protein, thus suppressing tau expression. CELIA (NCT05399888) is an ongoing phase 2 trial that is aiming to determine whether BIIB080 can delay AD progression in comparison with placebo and to identify the most effective dose of BIIB080. In March 2019, Biogen/Ionis performed a 4-year open-label extension trial of quarterly injections for individuals who completed the randomized portion of the trial. The initial data of this trial were reported at the Alzheimer’s Association International Conference (2021), revealing no serious adverse events from the intrathecal injection of BIIB080 at either of three doses every month for 3 months or two high-dose injections 3 months apart. BIIB080 led to a dose-dependent reductions of 30%–50% in total tau and pTau181 levels in CSF.
Neuroprotectors and cognitive enhancers
Table 5 summarizes the ongoing phase 3 trials for therapies other than anti-amyloid/tau treatment.
The active metabolite of fosgonimeton (ATH-1017) is a positive modulator of hepatocyte growth factor (HGF)/MET signaling [ 59 ]. A phase 3 trial of fosgonimeton (NCT04488419) was initiated in September 2020 and is expected to be completed in February 2024. This study is evaluating the safety and efficacy of fosgonimeton in participants with mild-to-moderate AD, with double-blind, parallel-arm treatment implemented for 26 weeks. The primary outcome measure is the overall treatment effect of fosgonimeton, as measured using the Global Statistical Test, which combines cognition (ADAS-Cog) and function (ADCS-ADL) scores.
AR-1001 selectively inhibits phosphodiesterase 5 and suppresses cGMP hydrolysis, resulting in the activation of protein kinase G and the increased phosphorylation of the cAMP-responsive element-binding protein at Ser133. It can rescue long-term potentiation impairment and cognitive dysfunction in animal models of AD [ 60 ]. A phase 3 trial of AR-1001 (NCT05531526) was started in December 2022 and is estimated to be completed in December 2027. The study aims to evaluate the efficacy and safety of AR1001 in participants with early AD. The primary outcome measure is the change in the CDR-SB from baseline to week 52.
BPDO-1603 is a potential cognitive-enhancing drug for AD, but its mechanism of action remains unknown [ 61 ]. A phase 3 trial of BPDO-1603 (NCT04229927) was started in February 2020 and is estimated to be completed in March 2023. The study has been undertaken to evaluate the efficacy and safety of BPDO-1603 in patients with moderate-to-severe AD. The primary outcome measures are the change in Severe Impairment Battery total scores from baseline to week 24, and CIBIC-plus total scores at week 24.
Buntanetap is a novel translational inhibitor of multiple neurotoxic proteins, including APP, tau, and α-synuclein, by enhancing the binding of the atypical iron response element in the 5′UTR regions of the mRNA of the neurotoxic proteins to iron regulatory protein 1 [ 62 ]. In February 2023, phase 2 and 3 trials (NCT05686044) were initiated to measure the efficacy and safety of three doses of buntanetap in comparison with placebo in participants with mild-to-moderate AD. The primary outcome measures are ADAS-Cog and ADCS Clinical Global Impression of Change (ADCS-CGIC) scores.
Caffeine is an adenosine receptor antagonist that has been reported to be associated with slower cognitive decline and lower cerebral amyloid accumulation [ 63 ]. A phase 3 trial of caffeine (NCT04570085) was started in March 2021 to evaluate the efficacy of 30 weeks of caffeine intake in comparison with placebo on cognitive decline in patients with mild-to-moderate AD dementia (Mini-Mental State Examination scores: 16–24). The primary outcome measure is changes in neuropsychological test battery scores between the randomized value and the value after 30 weeks of treatment.
Hydralazine may have anti-neurodegenerative effects because it activates the Nrf2 pathway, which involves more than 200 antioxidant proteins; improves mitochondrial function; and increases respiration capacity and the production of adenosine triphosphate; hydralazine also activates autophagy, which aids in the clearance of intracellular aggregates [ 64 , 65 , 66 ]. A phase 3 trial of hydralazine (NCT04842552) was started in August 2021 and is anticipated to be completed in December 2023. The study is comparing the effects of 75 mg hydralazine versus placebo in patients with mild-to-moderate AD. Various cognitive and function tests, including olfactory tests, biochemical analyses, and adverse effect monitoring, are being conducted regularly during follow-up.
KarXT (xanomeline-trospium), comprised of muscarinic agonist xanomeline and muscarinic antagonist trospium, is designed to preferentially activate muscarinic receptor in the CNS and ameliorate the peripheral muscarinic side effects. It is reported that KarXT improves cognition in patients with AD and schizophrenia [ 67 ]. A 38-week phase 3 trial comparing the effects of KarXT (NCT05511363) and placebo in participants with psychosis associated with AD dementia was started in August 2022. The trial is analyzing the time from randomization to relapse (primary outcome) as well as the time from randomization to discontinuation for any reason and the safety and tolerability of KarXT (secondary outcomes).
Metformin, a commonly prescribed antidiabetic medication, has been reported to improve cognition or mood in many neurological disorders [ 68 , 69 ]. A phase 3 trial of metformin (NCT04098666) was started in March 2021 and is anticipated to be completed in April 2026. The primary outcome measure is the total recall of the Free and Cued Selective Reminding Test at 24 months.
Nilotinib is a tyrosine kinase inhibitor that preferentially targets discoidin domain receptors and can effectively reduce the occurrence of misfolded proteins in animal models of neurodegeneration by crossing the blood–brain barrier and promoting Aβ and tau degradation [ 70 ]. A phase 3 trial (NCT05143528) was initiated in February 2022 to investigate the safety and efficacy of nilotinib BE (bioequivalent) in individuals with early AD. The primary outcome measure is changes in CDR-SB scores between baseline and week 72.
Piromelatine is a melatonin MT1/2/3 and serotonin 5-HT-1A/1D receptor agonist and was developed as a treatment for mild AD [ 71 ]. In May 2022, a randomized trial (NCT05267535) was initiated in 225 noncarriers of a specific polymorphism, and these participants with mild dementia due to AD are allocated at a ratio of 1:1 to receive piromelatine or placebo for 26 weeks. A 12-month extension involves treating the placebo group with piromelatine to assess the drug’s disease-modifying effects. The primary analysis will be conducted after the initial 26 weeks. If efficacy is not confirmed, the study is to end without the extension phase.
Semaglutide is a peptidic GLP-1 receptor agonist that may regulate the aggregation of Aβ in AD. GLP-1 receptors are involved in cognition, synaptic transmission in hippocampal neurons, and cell apoptosis; thus, they may serve as targets for exploring candidate drugs with neuroprotective and cognition-enhancing effects [ 72 ]. A phase 3 trial of semaglutide (NCT04777396) was started in May 2021 to investigate the efficacy of semaglutide in individuals with early AD. The primary outcome measure is changes in the CDR-SB score from baseline to week 104.
Tricaprilin, a semisynthetic medium-chain triglyceride, is hydrolyzed to octanoic acid after administration and is further metabolized to ketones, which serve as an alternative energy substrate for the brain [ 73 ]. Therefore, tricaprilin can be used as a ketogenic source for the management of mild-to-moderate AD. A phase 3 trial (NCT04187547) was started in June 2022 to evaluate the efficacy and safety of tricaprilin in participants with mild-to-moderate AD. The primary outcome measure is changes in ADAS-Cog scores from baseline to week 20.
Anti-neuroinflammation therapy
Masitinib, an oral tyrosine kinase inhibitor, exerts effects by inhibiting mast cell and microglia/macrophage activity, with significant CNS penetration [ 74 ]. It is currently undergoing a phase 3 trial (NCT05564169) with 600 participants, employing a randomized, double-blind, placebo-controlled, parallel-group design over 24 weeks, followed by a 24-week extension phase. Quadruple masking ensures blinding. The study aims to evaluate Masitinib as an adjunct therapy for mild to moderate AD. Estimated to conclude on December 15, 2025, the trial assesses primary outcomes through changes from baseline in ADAS-Cog-11 and ADCS-ADL scores, measuring cognitive and functional abilities, respectively.
NE3107 is an anti-inflammatory insulin sensitizer that can cross the blood–brain barrier and bind to ERK. NE3107 can selectively inhibit inflammation-driven ERK- and NF-κB-stimulated inflammatory mediators, including TNF-α, without disturbing their homeostatic functions [ 75 ]. A multicenter phase 3 trial (NCT04669028) was started in August 2021 to investigate the safety and efficacy of NE3107 at 20 mg that was orally administered twice daily versus placebo in adult participants with mild-to-moderate AD. The primary outcome measures are changes in ADAS-Cog12 and ADCS-CGIC scores from baseline to week 30 [ 76 ].
BPSD-relieving therapy
Masupirdine, a selective 5‐HT6 receptor antagonist with favorable physicochemical properties and absorption, distribution, metabolism, and excretion properties, may have beneficial effects on agitation, aggression, and psychosis in patients with moderate AD [ 77 ]. A phase 3 trial (NCT05397639) was started in November 2022 to evaluate the efficacy, safety, tolerability, and pharmacokinetics of masupirdine in comparison with placebo for treating agitation in participants with AD dementia. The primary outcome measure is the change in the score of the Cohen–Mansfield Agitation Inventory from baseline to week 12.
Nabilone is a partial agonist of cannabinoid receptor 1 (CB1) and CB2 in the brain and in peripheral tissues, and it has been reported to provide effective treatment for agitation in patients with AD [ 78 ]. A phase 3 trial (NCT04516057) was started in February 2021 to investigate whether nabilone is an effective treatment for agitation in AD patients. The primary outcome measure is agitation (Cohen–Mansfield Agitation Inventory) between baseline and week 8.
Phase 4 and repurposing trials
Table 6 summarizes ongoing phase 4 trials.
Escitalopram, a selective-serotonin reuptake inhibitor, is a commonly used antidepressant. It ameliorates cognitive impairment and could selectively attenuate phosphorylated tau accumulation in stressed rats by regulating hypothalamic–pituitary–adrenal axis activity and the insulin receptor substrate/glycogen synthase kinase-3β signaling pathway [ 79 ]. A phase 4 trial (NCT05004987) was started in February 2022 to investigate whether a reduction in depressive symptoms owing to the administration of escitalopram oxalate is associated with the normalization of AD biomarkers in CSF and inflammatory markers in the peripheral blood. The primary outcome measures are changes in CSF Aβ40 and Aβ42 levels, vascular dysfunction biomarker levels, and scores of the Montgomery–Asberg Depression Ratio Scale at week 8.
Sodium oligomannate (GV-971), a marine-derived oligosaccharide, can reconstitute the gut microbiota, reduce bacterial metabolite–driven peripheral infiltration of immune cells into the brain, inhibit amyloid-β fibril formation, and inhibit neuroinflammation in the brain, as demonstrated in animal studies [ 80 , 81 ]. A phase 4 trial (NCT05181475) was initiated in December 2021 to examine the long-term efficacy and safety of GV-971 as well as changes in blood and gut microbiota biomarkers and thereby validate its mechanism of action and establish guidance for the more rational use of drugs in clinical practice. The primary outcome measure is changes in ADAS-Cog11 scores from baseline to week 48. Another phase 4 trial was started in July 2022 and is comparing the efficacy and safety of memantine and GV-971 monotherapy and combination therapy in patients with moderate-to-severe AD. The primary outcome measure is changes in cognitive function at weeks 12, 24, 36, and 48.
Spironolactone, an aldosterone mineralocorticoid receptor antagonist, has been commonly used to treat cardiovascular diseases, including hypertension. It has anti-inflammatory effects on the peripheral tissues and central nervous system and therefore may have beneficial effects on neurological disorders [ 82 ]. A phase 4 trial (NCT04522739) was started in September 2022 to investigate whether spironolactone can be tolerated by older Black American adults with MCI and to determine its effect on memory and thinking abilities, as measured by participant performance on cognitive tests. The primary outcome measures are the number of adverse events and the attrition rate.
Published results
Among the clinical trials newly registered in the last 4 years, four articles pertaining to two trials have been published in peer-reviewed scientific journals. The characteristics of the published randomized controlled trials are summarized in Table 7 [ 43 , 53 , 83 , 84 ]. Two articles reported the results of NCT03887455 [ 43 , 84 ], and the other two reported the results of NCT01760005 [ 53 , 83 ]. The articles were published between 2018 and 2023. The results of both NCT03887455 (Clarity AD) and NCT01760005 have been discussed in the anti-amyloid section. The methodological quality of these studies is summarized in Table 8 . Both trials (NCT03887455 and NCT01760005) had a overall low risk of bias [ 43 , 53 , 83 , 84 ].
Our understanding of AD originated from clinical research, and how pathological findings are associated with clinical presentation of AD has continued to intrigue the neuroscience research community over the past century. DMTs have become the core of new drug development, and the accumulation of knowledge is leading to the evolution of diagnostic criteria and clinical outcome measurements. The view of clinical outcomes has shifted from considering them as solely determinative to considering them to be just one of the determinants. In accordance with the 2018 NIA-AA Research Framework criteria [ 25 ] or the new 2023 NIA-AA revised criteria for AD [ 26 ], the incorporation of biomarkers is necessary in clinical practice.
This review documented that in terms of the number of AD drug trials and the number of recruited participants, the majority of trials continue to focus on mechanisms involving amyloid and tau. Our 2020 report highlighted that due to the failure of early anti-amyloid trials to achieve their intended outcomes, particularly studies involving BACE inhibitors and monoclonal antibodies, some have questioned whether amyloid remains clinically relevant in AD. This shift in perspective has led to a change in the focus of research toward populations in the prodromal or preclinical stage with positive results for diagnostic biomarkers. Additionally, the validity of the amyloid hypothesis has been contested, resulting in a significant reduction in the number of anti-amyloid phase 3 trials since 2019. However, the targets of both phase 1 and phase 2 trials are diverse, with a noticeable increase in the number of phase 1 trials focusing on neuroprotection and phase 2 trials focusing on anti-neuroinflammation [ 85 ]. Since the positive outcomes in terms of slow decline in cognitive abilities in the lecanemab Clarity AD trial [ 43 ] and the donanemab trial TRAILBLAZER-ALZ [ 86 ], the impact of amyloid and consequent pathological alterations is likely to become the main focus of clinical trials. The incorporation of amyloid-related therapy either as an add-on or as a link to specific aspects of AD pathophysiology might become an important trend in clinical trials of new drugs in the future. However, despite this expansion of research areas, the scope of indications for novel anti-amyloid monoclonal antibody therapy remains limited. The mode of treatment administration and the high monitoring costs along with the need for specialized facilities and imaging scans remain challenges. Other unmet needs, such as addressing BPSD and enhancing cognitive function, necessitate pharmaceutical research. Examining drugs with diverse mechanisms necessitates thorough evaluation that extends beyond mere clinical measurements to encompass their intermediate impact on biomarkers. It is essential to investigate the potential synergy between a new drug and existing medications approved by the US FDA. This approach could even be extended to situations where adjuvant treatment, such as tau-related treatments, is provided after amyloid clearance has been achieved. Clinical trials related to AD have also exhibited a shift in focus toward the earlier stages of AD, such as MCI, or even cognitively healthy participants for developing prevention interventions.
Successful phase 3 trials such as Clarity AD (lecanemab) and EMERGE (aducanumab) have evaluated anti-amyloid treatment in mild AD (Fig. 2 ). Trials that do not target specific pathophysiologies are becoming fewer in all phases (Figs. 2 and 3 ). However, an increasing number of early-phase trials of therapies for symptoms, including cognitive enhancers and agents for relieving BPSD, are being conducted. This reflects the unmet clinical need for such therapies (Figs. 2 and 3 ). Similarly, an increasing number of phase 1 trials involving DMTs, particularly those targeting both anti-amyloid and anti-tau mechanisms, has been noted, indicating the importance of basic research (Fig. 3 ). Outcome measurement tools have also become more diverse, which has enabled meaningful improvements in AD and the efficacy of treatments to be clearly determined in clinical trials. Overall, the field of AD clinical trials is evolving, and additional promising treatments for AD are likely to be developed in the near future.
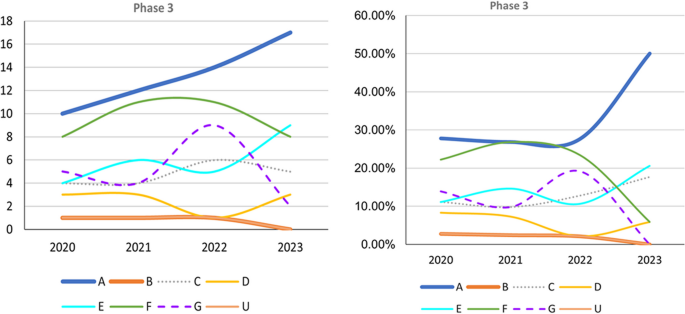
Trends in Phase 3 trials, 2020–2023, categorized according to event-related themes in ClinicalTrials.gov. Left: Number of Phase 3 trials. Right: Percentage of Phase 3 trials. A anti-amyloid therapy, B anti-tau therapy, C neuroprotection, D anti-neuroinflammation, E cognitive enhancer, F relief of behavioral psychological symptoms of dementia, G others, U undisclosed
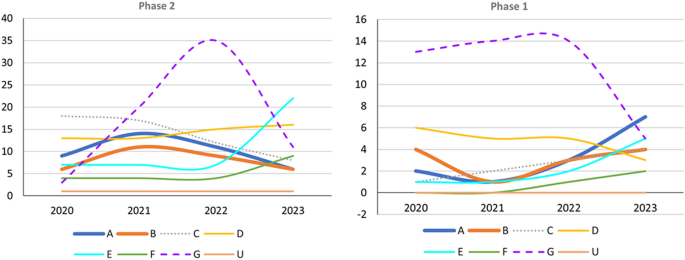
Trends in Phase 1 and 2 trials, 2020–2023, categorized according to event-related themes in ClinicalTrials.gov. Left: Number of Phase 2 trials. Right: Number of Phase 1 trials; A anti-amyloid therapy, B anti-tau therapy, C neuroprotection, D anti-neuroinflammation, E cognitive enhancer, F relief of behavioral psychological symptoms of dementia, G others, U undisclosed
Availability of data and materials
Not applicable.
Abbreviations
Amyloid-beta
Acetylcholine
Cholinesterase inhibitors
- Alzheimer disease
Alzheimer’s Disease Assessment Scale–Cognitive Subscale
Alzheimer’s Disease Cooperative Study–Activities of Daily Living Inventory–Mild Cognitive Impairment Version
Apolipoprotein gene
Amyloid precursor protein
Amyloid-related imaging abnormalities
Amyloid, tau, and neurodegeneration biomarkers
Appropriate use recommendations
Autophagic vacuoles
Beta-secretase 1
Behavioral psychological symptoms of dementia
Clinical Dementia Rating scale
Clinical Dementia Rating scale Sum of Box
Caregiver Global Impression of Change
Cerebrospinal fluid
Clinical Trial of AD
Disease-modifyung therapies
Integrated Alzheimer’s Disease Rating Scale
Immunoglobulin gamma 1
Mild cognitive impairment
Magnetic resonance imaging
Nuclear factor κB
Neurofibrillary tangles
Neuropsychiatric Inventory
Positron emission tomography
Presenilin-1
Presenilin-2
Gauthier S WC, Servaes S, Morais JA, Rosa-Neto P. World Alzheimer Report 2022: Life after diagnosis: Navigating treatment, care and support; 2022.
Apostolova LG. Alzheimer disease. Continuum (Minneap Minn). 2016;22(2 Dementia):419–34.
Mega MS, Cummings JL, Fiorello T, Gornbein J. The spectrum of behavioral changes in Alzheimer’s disease. Neurology. 1996;46(1):130–5.
Article CAS PubMed Google Scholar
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–9.
Article PubMed PubMed Central Google Scholar
Glenner GG, Wong CW. Alzheimer’s disease: initial report of the purification and characterization of a novel cerebrovascular amyloid protein. Biochem Biophys Res Commun. 1984;120(3):885–90.
Masters CL, Simms G, Weinman NA, Multhaup G, McDonald BL, Beyreuther K. Amyloid plaque core protein in Alzheimer disease and Down syndrome. Proc Natl Acad Sci U S A. 1985;82(12):4245–9.
Article CAS PubMed PubMed Central Google Scholar
Goedert M, Spillantini M, Crowther R. Tau proteins and neurofibrillary degeneration. Brain Pathol. 1991;1(4):279–86.
Sperling R, Mormino E, Johnson K. The evolution of preclinical Alzheimer’s disease: implications for prevention trials. Neuron. 2014;84(3):608–22.
De Leon MJ, George AE, Golomb J, Tarshish C, Convit A, Kluger A, et al. Frequency of hippocampal formation atrophy in normal aging and Alzheimer’s disease. Neurobiol Aging. 1997;18(1):1–11.
Article PubMed Google Scholar
Parker TD, Cash DM, Lane CAS, Lu K, Malone IB, Nicholas JM, et al. Hippocampal subfield volumes and pre-clinical Alzheimer’s disease in 408 cognitively normal adults born in 1946. PLoS ONE. 2019;14(10): e0224030.
Beyreuther K, Masters CL. Amyloid precursor protein (APP) and beta A4 amyloid in the etiology of Alzheimer’s disease: precursor-product relationships in the derangement of neuronal function. Brain Pathol. 1991;1(4):241–51.
Hardy J, Allsop D. Amyloid deposition as the central event in the aetiology of Alzheimer’s disease. Trends Pharmacol Sci. 1991;12(10):383–8.
Selkoe DJ. The molecular pathology of Alzheimer’s disease. Neuron. 1991;6(4):487–98.
Kang J, Lemaire H-G, Unterbeck A, Salbaum JM, Masters CL, Grzeschik K-H, et al. The precursor of Alzheimer’s disease amyloid A4 protein resembles a cell-surface receptor. Nature. 1987;325(6106):733–6.
Gunawardena S, Yang G, Goldstein LS. Presenilin controls kinesin-1 and dynein function during APP-vesicle transport in vivo. Hum Mol Genet. 2013;22(19):3828–43.
Kolata G. Down Syndrome—Alzheimer’s Linked: Down syndrome adults get Alzheimer-like changes in their brains and many become demented, leading researchers to ask about the connection. Science. 1985;230(4730):1152–3.
FDA Converts Novel Alzheimer’s Disease Treatment to Traditional Approval-Action Follows Confirmatory Trial to Verify Clinical Benefit. 2023.
Medina M, Avila J. The role of extracellular Tau in the spreading of neurofibrillary pathology. Front Cell Neurosci. 2014;8:113.
Jack CR, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, et al. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol. 2010;9(1):119–28.
Gómez-Isla T, Hollister R, West H, Mui S, Growdon JH, Petersen RC, et al. Neuronal loss correlates with but exceeds neurofibrillary tangles in Alzheimer’s disease. Ann Neurol. 1997;41(1):17–24.
Arriagada PV, Growdon JH, Hedley-Whyte ET, Hyman BT. Neurofibrillary tangles but not senile plaques parallel duration and severity of Alzheimer’s disease. Neurology. 1992;42(3 Pt 1):631–9.
Bierer LM, Hof PR, Purohit DP, Carlin L, Schmeidler J, Davis KL, et al. Neocortical neurofibrillary tangles correlate with dementia severity in Alzheimer’s disease. Arch Neurol. 1995;52(1):81–8.
Okamura N, Yanai K. Applications of tau PET imaging. Nat Rev Neurol. 2017;13(4):197–8.
Jack CR Jr, Bennett DA, Blennow K, Carrillo MC, Feldman HH, Frisoni GB, et al. A/T/N: an unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology. 2016;87:539–47.
Jack CR Jr, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14(4):535–62.
NIA-AA Revised Clinical Criteria for Alzheimer's Disease. 2023.
Lian H, Yang L, Cole A, Sun L, Chiang AC, Fowler SW, et al. NFκB-activated astroglial release of complement C3 compromises neuronal morphology and function associated with Alzheimer’s disease. Neuron. 2015;85(1):101–15.
Liddelow SA, Guttenplan KA, Clarke LE, Bennett FC, Bohlen CJ, Schirmer L, et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature. 2017;541(7638):481–7.
Hamelin L, Lagarde J, Dorothée G, Leroy C, Labit M, Comley RA, et al. Early and protective microglial activation in Alzheimer’s disease: a prospective study using 18 F-DPA-714 PET imaging. Brain. 2016;139(4):1252–64.
Gomez-Nicola D, Boche D. Post-mortem analysis of neuroinflammatory changes in human Alzheimer’s disease. Alzheimers Res Ther. 2015;7(1):42.
Zimmer ER, Leuzy A, Benedet AL, Breitner J, Gauthier S, Rosa-Neto P. Tracking neuroinflammation in Alzheimer’s disease: the role of positron emission tomography imaging. J Neuroinflammation. 2014;11(1):1–12.
Article Google Scholar
McGeer PL, McGeer EG. The amyloid cascade-inflammatory hypothesis of Alzheimer disease: implications for therapy. Acta Neuropathol. 2013;126(4):479–97.
Lockhart SN, Schaich CL, Craft S, Sachs BC, Rapp SR, Jung Y, et al. Associations among vascular risk factors, neuroimaging biomarkers, and cognition: Preliminary analyses from the Multi-Ethnic Study of Atherosclerosis (MESA). Alzheimers Dement. 2022;18(4):551–60.
Wanleenuwat P, Iwanowski P, Kozubski W. Alzheimer’s dementia: pathogenesis and impact of cardiovascular risk factors on cognitive decline. Postgrad Med. 2019;131(7):415–22.
Lee J-H, Yang D-S, Goulbourne CN, Im E, Stavrides P, Pensalfini A, et al. Faulty autolysosome acidification in Alzheimer’s disease mouse models induces autophagic build-up of Aβ in neurons, yielding senile plaques. Nat Neurosci. 2022;25(6):688–701.
Chi H, Chang H-Y, Sang T-K. Neuronal cell death mechanisms in major neurodegenerative diseases. Int J Mol Sci. 2018;19(10):3082.
Raina P, Santaguida P, Ismaila A, Patterson C, Cowan D, Levine M, et al. Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline. Ann Intern Med. 2008;148(5):379–97.
Arndt JW, Qian F, Smith BA, Quan C, Kilambi KP, Bush MW, et al. Structural and kinetic basis for the selectivity of aducanumab for aggregated forms of amyloid-β. Sci Rep. 2018;8(1):6412.
Dunn B, Stein P, Cavazzoni P. Approval of aducanumab for Alzheimer disease—the FDA’s perspective. JAMA Intern Med. 2021;181(10):1276–8.
Tucker S, Möller C, Tegerstedt K, Lord A, Laudon H, Sjödahl J, et al. The murine version of BAN2401 (mAb158) selectively reduces amyloid-β protofibrils in brain and cerebrospinal fluid of tg-ArcSwe mice. J Alzheimers Dis. 2015;43(2):575–88.
Canady VA. FDA approves new treatment for Alzheimer’s disease. Ment Heal Wkly. 2023;33(3):6–7.
Swanson CJ, Zhang Y, Dhadda S, Wang J, Kaplow J, Lai RY, et al. A randomized, double-blind, phase 2b proof-of-concept clinical trial in early Alzheimer’s disease with lecanemab, an anti-Aβ protofibril antibody. Alzheimers Res Ther. 2021;13(1):80.
Van Dyck CH, Swanson CJ, Aisen P, Bateman RJ, Chen C, Gee M, et al. Lecanemab in early Alzheimer’s disease. N Engl J Med. 2023;388(1):9–21.
Cummings J, Rabinovici G, Atri A, Aisen P, Apostolova L, Hendrix S, et al. Aducanumab: appropriate use recommendations update. J Prev Alzheimers Di s. 2022;9(2):221–30.
CAS Google Scholar
Cummings J, Apostolova L, Rabinovici G, Atri A, Aisen P, Greenberg S, et al. Lecanemab: appropriate use recommendations. J Prev Alzheimers Dis. 2023;10(3):362–77.
CAS PubMed Google Scholar
Irizarry MC, Sims JR, Lowe SL, Nakano M, Hawdon A, Willis BA, et al. O4–08-06: Safety, pharmacokinetics (PK), and florbetapir F-18 positron emission tomography (PET) after multiple dose administration of LY3002813, a β-amyloid plaque-specific antibody, in Alzheimer’s disease. Alzheimers Dement. 2016;12:P352–3.
Bouter Y, Liekefeld H, Pichlo S, Westhoff AC, Fenn L, Bakrania P, et al. Donanemab detects a minor fraction of amyloid-β plaques in post-mortem brain tissue of patients with Alzheimer’s disease and Down syndrome. Acta Neuropathol. 2022;143(5):601–3.
Shcherbinin S, Evans CD, Lu M, Andersen SW, Pontecorvo MJ, Willis BA, et al. Association of amyloid reduction after donanemab treatment with tau pathology and clinical outcomes: the TRAILBLAZER-ALZ randomized clinical trial. JAMA Neurol. 2022;79(10):1015–24.
Pontecorvo MJ, Lu M, Burnham SC, Schade AE, Dage JL, Shcherbinin S, et al. Association of donanemab treatment with exploratory plasma biomarkers in early symptomatic Alzheimer disease: a secondary analysis of the TRAILBLAZER-ALZ randomized clinical trial. JAMA Neurol. 2022;79(12):1250–9.
Sims JR, Zimmer JA, Evans CD, Lu M, Ardayfio P, Sparks J, et al. Donanemab in early symptomatic Alzheimer disease: the TRAILBLAZER-ALZ 2 randomized clinical trial. JAMA. 2023;330(6):512–27.
Wessels AM, Dennehy EB, Dowsett SA, Dickson SP, Hendrix SB. Meaningful clinical changes in Alzheimer disease measured with the iADRS and illustrated using the donanemab TRAILBLAZER-ALZ study findings. Neurol Clin Pract. 2023;13(2): e200127.
Honig LS, Vellas B, Woodward M, Boada M, Bullock R, Borrie M, et al. Trial of solanezumab for mild dementia due to Alzheimer’s disease. N Engl J Med. 2018;378(4):321–30.
Salloway S, Farlow M, McDade E, Clifford DB, Wang G, Llibre-Guerra JJ, et al. A trial of gantenerumab or solanezumab in dominantly inherited Alzheimer’s disease. Nat Med. 2021;27(7):1187–96.
Hey JA, Yu JY, Versavel M, Abushakra S, Kocis P, Power A, et al. Clinical pharmacokinetics and safety of ALZ-801, a novel prodrug of tramiprosate in development for the treatment of Alzheimer’s disease. Clin Pharmacokinet. 2018;57(3):315–33.
Wang HY, Bakshi K, Frankfurt M, Stucky A, Goberdhan M, Shah SM, et al. Reducing amyloid-related Alzheimer’s disease pathogenesis by a small molecule targeting filamin A. J Neurosci. 2012;32(29):9773–84.
Lues I, Weber F, Meyer A, Bühring U, Hoffmann T, Kühn-Wache K, et al. A phase 1 study to evaluate the safety and pharmacokinetics of PQ912, a glutaminyl cyclase inhibitor, in healthy subjects. Alzheimers Dement (N Y). 2015;1(3):182–95.
Grundman M, Morgan R, Lickliter JD, Schneider LS, DeKosky S, Izzo NJ, et al. A phase 1 clinical trial of the sigma-2 receptor complex allosteric antagonist CT1812, a novel therapeutic candidate for Alzheimer’s disease. Alzheimers Dement (N Y). 2019;5:20–6.
Paul S, Haskali MB, Liow JS, Zoghbi SS, Barth VN, Kolodrubetz MC, et al. Evaluation of a PET radioligand to image O-GlcNAcase in brain and periphery of rhesus monkey and knock-out mouse. J Nucl Med. 2019;60(1):129–34.
Johnston JL, Reda SM, Setti SE, Taylor RW, Berthiaume A-A, Walker WE, et al. Fosgonimeton, a novel positive modulator of the HGF/MET system, promotes neurotrophic and procognitive effects in models of dementia. Neurotherapeutics. 2023;20(2):431–51.
Kang BW, Kim F, Cho J-Y, Kim S, Rhee J, Choung JJ. Phosphodiesterase 5 inhibitor mirodenafil ameliorates Alzheimer-like pathology and symptoms by multimodal actions. Alzheimers Res Ther. 2022;14(1):92.
Cummings J, Lee G, Nahed P, Kambar MEZN, Zhong K, Fonseca J, et al. Alzheimer’s disease drug development pipeline: 2022. Alzheimers Dement (N Y). 2022;8(1): e12295.
Fang C, Hernandez P, Liow K, Damiano E, Zetterberg H, Blennow K, et al. Buntanetap, a novel translational inhibitor of multiple neurotoxic proteins, proves to be safe and promising in both Alzheimer’s and Parkinson’s patients. J Prev Alzheimers Dis. 2023;10(1):25–33.
Gardener SL, Rainey-Smith SR, Villemagne VL, Fripp J, Doré V, Bourgeat P, et al. Higher coffee consumption is associated with slower cognitive decline and less cerebral Aβ-Amyloid accumulation over 126 months: data from the Australian imaging, biomarkers, and lifestyle study. Front Aging Neurosci. 2021;13: 744872.
Chhunchha B, Kubo E, Krueger RR, Singh D. Hydralazine revives cellular and ocular lens health-span by ameliorating the aging and oxidative-dependent loss of the Nrf2-activated cellular stress response. Antioxidants (Basel). 2023;12(1):140.
Chang T-T, Chen J-W. Potential Impacts of Hydralazine as a Novel Antioxidant on Cardiovascular and Renal Disease—Beyond Vasodilation and Blood Pressure Lowering. Antioxidants (Basel). 2022;11(11):2224.
Dehghan E, Goodarzi M, Saremi B, Lin R, Mirzaei H. Hydralazine targets cAMP-dependent protein kinase leading to sirtuin1/5 activation and lifespan extension in C. elegans . Nat Commun. 2019;10(1):4905.
Sauder C, Allen LA, Baker E, Miller AC, Paul SM, Brannan SK. Effectiveness of KarXT (xanomeline-trospium) for cognitive impairment in schizophrenia: post hoc analyses from a randomised, double-blind, placebo-controlled phase 2 study. Transl Psychiatry. 2022;12(1):491.
Li N, Zhou T, Fei E. Actions of metformin in the brain: a new perspective of metformin treatments in related neurological disorders. Int J Mol Sci. 2022;23(15):8281.
Khaleghi-Mehr M, Delshad A-A, Shafie-Damavandi S, Roghani M. Metformin mitigates amyloid β1-40-induced cognitive decline via attenuation of oxidative/nitrosative stress and neuroinflammation. Metab Brain Dis. 2023;38(4):1127–42.
Turner RS, Hebron ML, Lawler A, Mundel EE, Yusuf N, Starr JN, et al. Nilotinib effects on safety, tolerability, and biomarkers in Alzheimer’s disease. Ann Neurol. 2020;88(1):183–94.
Schneider L, Laudon M, Nir T, Caceres J, Ianniciello G, Capulli M, et al. A polymorphism cluster at the 2q12 locus may predict response to piromelatine in patients with mild Alzheimer’s disease. J Prev Alzheimers Dis. 2022;9(2):247–54.
Mahapatra MK, Karuppasamy M, Sahoo BM. Therapeutic potential of semaglutide, a newer GLP-1 receptor agonist, in abating obesity, non-alcoholic steatohepatitis and neurodegenerative diseases: a narrative review. Pharm Res. 2022;39(6):1233–48.
Li Z, et al. Modeling digestion, absorption, and ketogenesis after administration of tricaprilin formulations to humans. Eur J Pharm Biopharm. 2023;182:41–52.
Li T, Martin E, Abada YS, et al. Effects of chronic masitinib treatment in APPswe/PSEN1dE9 transgenic mice modeling Alzheimer’s disease. J Alzheimers Dis. 2020;76(4):1339–45.
Reading CL, Ahlem CN, Murphy MF. NM101 Phase III study of NE3107 in Alzheimer’s disease: rationale, design and therapeutic modulation of neuroinflammation and insulin resistance. Neurodegener Dis Manag. 2021;11(4):289–98.
Nirogi R, Jayarajan P, Benade V, Shinde A, Goyal VK, Jetta S, et al. Potential beneficial effects of masupirdine (SUVN-502) on agitation/aggression and psychosis in patients with moderate Alzheimer’s disease: exploratory post hoc analyses. Int J Geriatr Psychiatry. 2022. https://doi.org/10.1002/gps.5813 .
Herrmann N, Ruthirakuhan M, Gallagher D, Verhoeff N, Kiss A, Black SE, et al. Randomized Placebo-Controlled Trial of Nabilone for Agitation in Alzheimer’s Disease. Am J Geriatr Psychiatry. 2019;27(11):1161–73.
Wu C, Gong W-G, Wang Y-J, Sun J-J, Zhou H, Zhang Z-J, et al. Escitalopram alleviates stress-induced Alzheimer’s disease-like tau pathologies and cognitive deficits by reducing hypothalamic-pituitary-adrenal axis reactivity and insulin/GSK-3β signal pathway activity. Neurobiol Aging. 2018;67:137–47.
Xiao S, Chan P, Wang T, Hong Z, Wang S, Kuang W, et al. A 36-week multicenter, randomized, double-blind, placebo-controlled, parallel-group, phase 3 clinical trial of sodium oligomannate for mild-to-moderate Alzheimer’s dementia. Alzheimers Res Ther. 2021;13(1):62.
Lu J, Pan Q, Zhou J, Weng Y, Chen K, Shi L, et al. Pharmacokinetics, distribution, and excretion of sodium oligomannate, a recently approved anti-Alzheimer’s disease drug in China. J Pharm Anal. 2022;12(1):145–55.
Mehdipour M, Emamghoreishi M, Farrokhi MR, Amirinezhadfard E, Keshavarz M. The effect of spironolactone on β-amyloid-induced memory impairment in male rats: the role of microglial inhibition. Adv Pharm Bull. 2022;12(3):623–31.
Bateman RJ, Benzinger TL, Berry S, Clifford DB, Duggan C, Fagan AM, et al. The DIAN-TU Next Generation Alzheimer’s prevention trial: Adaptive design and disease progression model. Alzheimers Dement. 2017;13(1):8–19.
Tahami Monfared AA, Ye W, Sardesai A, Folse H, Chavan A, Aruffo E, et al. A path to improved Alzheimer’s care: simulating long-term health outcomes of lecanemab in early Alzheimer’s disease from the CLARITY AD trial. Neurol Ther. 2023;12(3):863–81.
Huang L-K, Chao S-P, Hu C-J. Clinical trials of new drugs for Alzheimer disease. J Biomed Sci. 2020;27(1):18.
Mintun MA, Lo AC, Duggan Evans C, Wessels AM, Ardayfio PA, Andersen SW, et al. Donanemab in early Alzheimer’s disease. N Engl J Med. 2021;384(18):1691–704.
Download references
Acknowledgements
This manuscript was edited by Wallace Academic Editing.
The authors have not received any funding.
Author information
Li-Kai Huang and Yi-Chun Kuan contributed equally to this work.
Authors and Affiliations
PhD Program in Medical Neuroscience, College of Medical Science and Technology, Taipei Medical University, No. 291, Zhong Zheng Road, Zhonghe District, New Taipei City, Taiwan
Li-Kai Huang & Chaur-Jong Hu
Taipei Neuroscience Institute, Taipei Medical University, New Taipei City, Taiwan
Li-Kai Huang, Yi-Chun Kuan & Chaur-Jong Hu
Dementia Center and Department of Neurology, Shuang-Ho Hospital, Taipei Medical University, New Taipei City, Taiwan
Department of Neurology, School of Medicine, College of Medicine, Taipei Medical University, Taipei, Taiwan
Yi-Chun Kuan & Chaur-Jong Hu
Department of Biomedical Engineering, National Taiwan University, Taipei, Taiwan
Yi-Chun Kuan
School of Medicine, College of Medicine, Taipei Medical University, Taipei, Taiwan
You can also search for this author in PubMed Google Scholar
Contributions
LKH and YCK: Conducted literature search, developed the study concept and design, extracted information from trials and studies, and contributed to manuscript drafting and revision. HWL: Extracted information from trials and studies and contributed to manuscript drafting and revision. CJH: Contributed to the study concept and design, interpreted the data and information, finalized and revised the manuscript, and provided overall supervision of the entire project.
Corresponding author
Correspondence to Chaur-Jong Hu .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Huang, LK., Kuan, YC., Lin, HW. et al. Clinical trials of new drugs for Alzheimer disease: a 2020–2023 update. J Biomed Sci 30 , 83 (2023). https://doi.org/10.1186/s12929-023-00976-6
Download citation
Received : 31 May 2023
Accepted : 26 September 2023
Published : 02 October 2023
DOI : https://doi.org/10.1186/s12929-023-00976-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical trials
- Anti-amyloid
- Neuroprotection
- Cognitive enhancement
- Neuroinflammation
Journal of Biomedical Science
ISSN: 1423-0127
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
MIT Technology Review
- Newsletters
New breakthroughs on Alzheimer’s
MIT scientists have pinpointed the first brain cells to show signs of neurodegeneration in the disorder and identified a peptide that holds potential as a treatment.
- Anne Trafton archive page
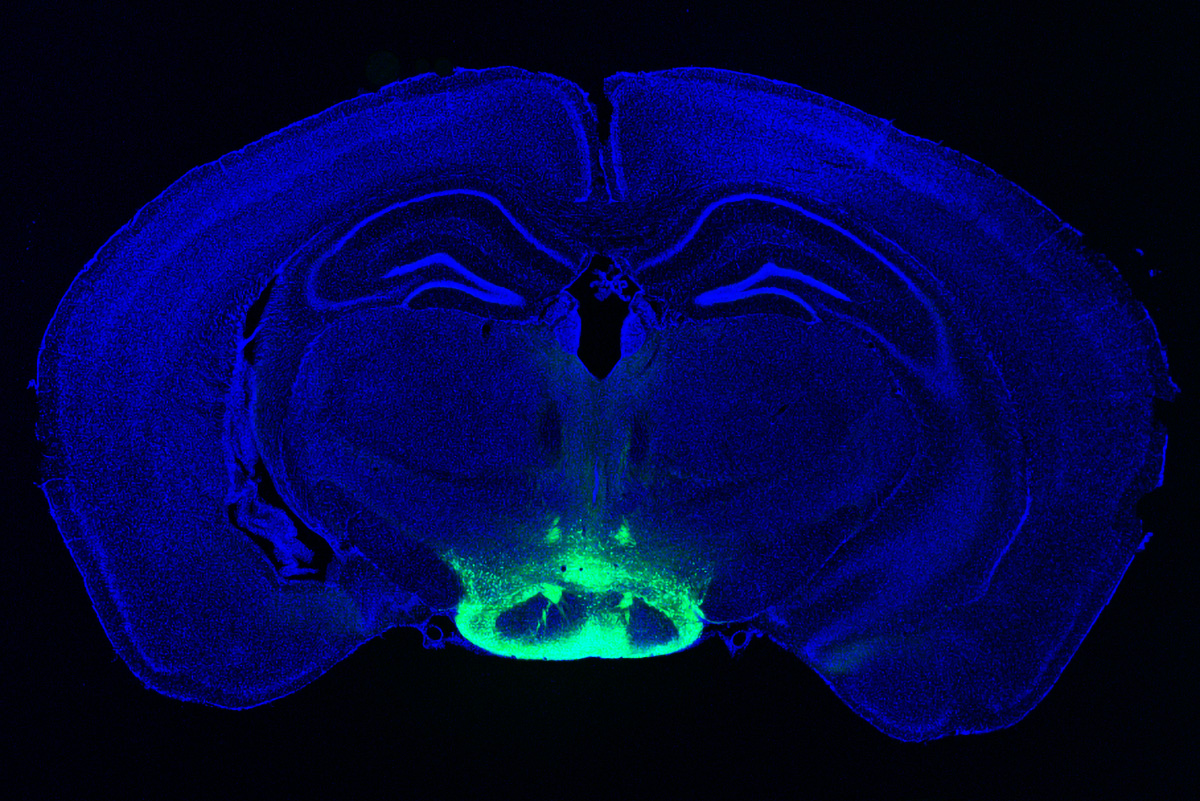
Neuronal hyperactivity and the gradual loss of neuron function are key features of Alzheimer’s disease. Now researchers led by Li-Huei Tsai, director of MIT’s Picower Institute for Learning and Memory, have identified the cells most susceptible to this damage, suggesting a good target for treatment. Even more exciting, Tsai and her colleagues have found a way to reverse neurodegeneration and other symptoms by interfering with an enzyme that is typically overactive in the brains of Alzheimer’s patients.
In one study , the researchers used single-cell RNA sequencing to distinguish two populations of neurons in the mammillary bodies, a pair of structures in the hypothalamus that play a role in memory and are affected early in the disease. Previous work by Tsai’s lab found that they had the highest density of amyloid beta plaques, abnormal clumps of protein that are thought to cause many Alzheimer’s symptoms.
The researchers found that neurons in the lateral mammillary body showed much more hyperactivity and degeneration than those in the larger medial mamillary body. They also found that this damage led to memory impairments in mice and that they could reverse those impairments with a drug used to treat epilepsy.
In the other study , the researchers treated mice with a peptide that blocks a hyperactive version of an enzyme called CDK5, which plays an important role in development of the central nervous system. They found dramatic reductions in neurodegeneration and DNA damage in the brain, and the mice got better at tasks such as learning to navigate a water maze.
CDK5 is activated by a smaller protein known as P35, allowing it to add a phosphate molecule to its targets. However, in Alzheimer’s and other neurodegenerative diseases, P35 breaks down into a smaller protein called P25, which allows CDK5 to phosphorylate other molecules—including the Tau protein, leading to the Tau tangles that are another characteristic of Alzheimer’s.
Pharmaceutical companies have tried to target P25 with small-molecule drugs, but these drugs also interfere with other essential enzymes. The MIT team instead used a peptide—a string of amino acids, in this case a sequence matching that of a CDK5 segment that is critical to binding P25.
In tests on neurons in a lab dish, the researchers found that treatment with the peptide moderately reduced CDK5 activity. But in a mouse model that has hyperactive CDK5, they saw myriad beneficial effects, including reductions in DNA damage, neural inflammation, and neuron loss.
The treatment also produced dramatic improvements in a different mouse model of Alzheimer’s, which has a mutant form of the Tau protein. Tsai hypothesizes that the peptide might confer resilience to cognitive impairment in the brains of people with Tau tangles.
“We found that the effect of this peptide is just remarkable,” she says. “We saw wonderful effects in terms of reducing neurodegeneration and neuroinflammatory responses, and even rescuing behavior deficits.”
The researchers hope the peptide could eventually be used as a treatment not only for Alzheimer’s but for frontotemporal dementia, HIV-induced dementia, diabetes-linked cognitive impairment, and other conditions.
Keep Reading
Most popular, large language models can do jaw-dropping things. but nobody knows exactly why..
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
- Will Douglas Heaven archive page
OpenAI teases an amazing new generative video model called Sora
The firm is sharing Sora with a small group of safety testers but the rest of us will have to wait to learn more.
Google’s Gemini is now in everything. Here’s how you can try it out.
Gmail, Docs, and more will now come with Gemini baked in. But Europeans will have to wait before they can download the app.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
- Casey Crownhart archive page
Stay connected
Get the latest updates from mit technology review.
Discover special offers, top stories, upcoming events, and more.
Thank you for submitting your email!
It looks like something went wrong.
We’re having trouble saving your preferences. Try refreshing this page and updating them one more time. If you continue to get this message, reach out to us at [email protected] with a list of newsletters you’d like to receive.
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Shots - Health News
Alzheimer's researchers are looking beyond plaques and tangles for new treatments.

Jon Hamilton
Scientists say research into Alzheimer's needs to take a broader view of how the disease affects the brain — whether that's changes in the cortex or the role of inflammation. Matt York/AP hide caption
Scientists say research into Alzheimer's needs to take a broader view of how the disease affects the brain — whether that's changes in the cortex or the role of inflammation.
The field of Alzheimer's research is branching out.
After decades of focusing on the sticky amyloid plaques and tangled tau fibers associated with the disease, brain researchers are searching for other potential causes of impaired memory and thinking.
That search is on full display this week at the Alzheimer's Association International Conference in San Diego, where sessions are exploring factors including genes, brain injury, clogged arteries and inflammation.
A group of researchers from Seattle even unveiled a highly detailed atlas showing how different types of brain cells change in Alzheimer's. The goal is to help scientists identify new approaches to treatment.
"Certainly, plaques and tangles are a hallmark," says Maria Carrillo , chief science officer of the Alzheimer's Association. "It doesn't mean plaques are the cause of cell death."
Plaques are clumps of a protein called beta-amyloid that appear in the spaces between neurons. Tangles are made up of a protein called tau that appears inside a neuron.
Both proteins tend to accumulate in the brains of people with Alzheimer's. But their role in killing brain cells is still unclear.
Carrillo says the Alzheimer's field needs to look to cancer research where a deeper understanding of the disease has led to better treatments.
The shift comes after a series of experimental drugs have succeeded in removing amyloid plaques and tau tangles from the brain, but failed to halt the disease.
The Food and Drug Administration has approved one amyloid drug, Aduhelm, but is still evaluating whether it actually helps patients.
An Alzheimer's Atlas
The study that produced the atlas is emblematic of how researchers are recalibrating.
"What we're trying to do with this study is to look at cell vulnerability early on in disease, before [people] have plaques and tangles, before they have cognitive impairment," says Dr. C. Dirk Keene , a neuropathologist at the University of Washington.
To create the atlas, Keene and a team of researches analyzed more than a million cells from 84 brains donated by people who'd signed up for Alzheimer's research projects run by the University of Washington and Kaiser Permanente Washington Research Institute.
The brains came from donors "at all different stages of disease" Keene says, "so we can pinpoint what's happening from the earliest levels all the way through to people with advanced disease."
The effort is funded by the National Institute on Aging and grew out of the federal BRAIN initiative launched by President Obama in 2013.
The atlas came from the realization that "If we want to treat diseases of an extremely complex cellular organ, you need to understand that organ much better than we do," says Ed Lein , a senior investigator at the Allen Institute for Brain Science, which played a key role in analyzing the brain tissue.
So the team spent years studying cells in healthy brains before looking at brains affected by Alzheimer's.
"We've defined what a normal adult brain looks like," Lein says, "and now we can use that knowledge and look for changes that are happening in specific kinds of cells."

Future Alzheimer's Treatments Aim To Do More Than Clear Plaques From The Brain
Finding vulnerable brain cells.
At the Alzheimer's meeting, the team described changes they saw in more than 100 types of cells taken from the cortex — an area of the brain which is important to memory and thinking.
One finding was that neurons that make connections within the cortex itself were much more likely to die than those that connect to distant areas of the brain.
"What we're seeing is a profound effect on cortical circuitry that very plausibly is the reason we have cognitive decline," Lein says.
If so, a treatment designed to protect those vulnerable neurons might prevent declines in memory and thinking linked to Alzheimer's.
The team also found a proliferation of brain cells that contribute to inflammation. These included certain immune cells and a type of cell that responds to injury.
"So while the neurons are lost, the non-neuronal cells are actually increasing and changing" Lein says.
The finding supports the idea that inflammation plays an important role in Alzheimer's, and that anti-inflammatory drugs might help protect the brain.
The Seattle team hopes other scientists will use the brain cell atlas to come up with new treatments for Alzheimer's.
"We've created an open-access resource where the whole community can come and look at this data," Lein says. "They can mine it to speed up progress in the field as a whole."
Speeding up progress is one reason Kyle Travaglini , a researcher at the Allen Institute, jumped at the chance to work on the Alzheimer's project.
"My grandmother started developing Alzheimer's disease when I was just going off to college," says Travaglini, who received his PhD in 2021.
Travaglini says the atlas project is appealing because it isn't based on a preconceived idea about what causes Alzheimer's.
"It's like looking at the same disease that everyone has been looking at but in an entirely different way," he says.

A substance found in young spinal fluid helps old mice remember


Scientists look to people with Down syndrome to test Alzheimer's drugs
Call our 24 hours, seven days a week helpline at 800.272.3900

- Professionals

- Younger/Early-Onset Alzheimer's
- Is Alzheimer's Genetic?
- Women and Alzheimer's
- Creutzfeldt-Jakob Disease
- Dementia with Lewy Bodies
- Down Syndrome & Alzheimer's
- Frontotemporal Dementia
- Huntington's Disease
- Mixed Dementia
- Normal Pressure Hydrocephalus
- Posterior Cortical Atrophy
- Parkinson's Disease Dementia
- Vascular Dementia
- Korsakoff Syndrome
- Traumatic Brain Injury (TBI)
- Know the 10 Signs
- Difference Between Alzheimer's & Dementia
- 10 Steps to Approach Memory Concerns in Others
- Medical Tests for Diagnosing Alzheimer's
- Why Get Checked?
- Visiting Your Doctor
- Life After Diagnosis
- Stages of Alzheimer's
- Earlier Diagnosis
- Part the Cloud
- Research Momentum
- Our Commitment to Research
- TrialMatch: Find a Clinical Trial
- What Are Clinical Trials?
- How Clinical Trials Work
- When Clinical Trials End
- Why Participate?
- Talk to Your Doctor
- Clinical Trials: Myths vs. Facts
- Can Alzheimer's Disease Be Prevented?
- Brain Donation
- Navigating Treatment Options
- Lecanemab Approved for Treatment of Early Alzheimer's Disease
- Aducanumab Discontinued as Alzheimer's Treatment
- Medicare Treatment Coverage
- Donanemab for Treatment of Early Alzheimer's Disease — News Pending FDA Review
- Questions for Your Doctor
- Medications for Memory, Cognition and Dementia-Related Behaviors
- Treatments for Behavior
- Treatments for Sleep Changes
- Alternative Treatments
- Facts and Figures
- Assessing Symptoms and Seeking Help
- Now is the Best Time to Talk about Alzheimer's Together

- Daily Care Plan
- Communication and Alzheimer's
- Food and Eating
- Art and Music
- Incontinence
- Dressing and Grooming
- Dental Care
- Working With the Doctor
- Medication Safety
- Accepting the Diagnosis
- Early-Stage Caregiving
- Middle-Stage Caregiving
- Late-Stage Caregiving
- Aggression and Anger
- Anxiety and Agitation
- Hallucinations
- Memory Loss and Confusion
- Sleep Issues and Sundowning
- Suspicions and Delusions
- In-Home Care
- Adult Day Centers
- Long-Term Care
- Respite Care
- Hospice Care
- Choosing Care Providers
- Finding a Memory Care-Certified Nursing Home or Assisted Living Community
- Changing Care Providers
- Working with Care Providers
- Creating Your Care Team
- Long-Distance Caregiving
- Community Resource Finder
- Be a Healthy Caregiver
- Caregiver Stress
- Caregiver Stress Check
- Caregiver Depression
- Changes to Your Relationship
- Grief and Loss as Alzheimer's Progresses
- Home Safety
- Dementia and Driving
- Technology 101
- Preparing for Emergencies
- Managing Money Online Program
- Planning for Care Costs
- Paying for Care
- Health Care Appeals for People with Alzheimer's and Other Dementias
- Social Security Disability
- Medicare Part D Benefits
- Tax Deductions and Credits
- Planning Ahead for Legal Matters
- Legal Documents
- Get Educated
- Just Diagnosed
- Sharing Your Diagnosis
- Changes in Relationships
- If You Live Alone
- Treatments and Research
- Legal Planning
- Financial Planning
- Building a Care Team
- End-of-Life Planning
- Programs and Support
- Overcoming Stigma
- Younger-Onset Alzheimer's
- Taking Care of Yourself
- Reducing Stress
- Tips for Daily Life
- Helping Family and Friends
- Leaving Your Legacy
- Live Well Online Resources
- Make a Difference
- ALZ Talks Virtual Events
- ALZNavigator™
- Veterans and Dementia
- The Knight Family Dementia Care Coordination Initiative
- Online Tools
- Asian Americans and Pacific Islanders and Alzheimer's
- Native Americans and Alzheimer's
- Black Americans and Alzheimer's
- Hispanic Americans and Alzheimer's
- LGBTQ+ Community Resources for Dementia
- Educational Programs and Dementia Care Resources
- Brain Facts
- 50 Activities
- For Parents and Teachers
- Resolving Family Conflicts
- Holiday Gift Guide for Caregivers and People Living with Dementia
- Trajectory Report
- Resource Lists
- Search Databases
- Publications
- Favorite Links
- 10 Healthy Habits for Your Brain
- Stay Physically Active
- Adopt a Healthy Diet
- Stay Mentally and Socially Active
- Online Community
- Support Groups
- Find Your Local Chapter
- Any Given Moment
- New IDEAS Study
- RFI Amyloid PET Depletion Following Treatment
- Bruce T. Lamb, Ph.D., Chair
- Christopher van Dyck, M.D.
- Cynthia Lemere, Ph.D.
- David Knopman, M.D.
- Lee A. Jennings, M.D. MSHS
- Karen Bell, M.D.
- Lea Grinberg, M.D., Ph.D.
- Malú Tansey, Ph.D.
- Mary Sano, Ph.D.
- Oscar Lopez, M.D.
- Suzanne Craft, Ph.D.
- About Our Grants
- Andrew Kiselica, Ph.D., ABPP-CN
- Arjun Masurkar, M.D., Ph.D.
- Benjamin Combs, Ph.D.
- Charles DeCarli, M.D.
- Damian Holsinger, Ph.D.
- David Soleimani-Meigooni, Ph.D.
- Donna M. Wilcock, Ph.D.
- Elizabeth Head, M.A, Ph.D.
- Fan Fan, M.D.
- Fayron Epps, Ph.D., R.N.
- Ganesh Babulal, Ph.D., OTD
- Hui Zheng, Ph.D.
- Jason D. Flatt, Ph.D., MPH
- Jennifer Manly, Ph.D.
- Joanna Jankowsky, Ph.D.
- Luis Medina, Ph.D.
- Marcello D’Amelio, Ph.D.
- Marcia N. Gordon, Ph.D.
- Margaret Pericak-Vance, Ph.D.
- María Llorens-Martín, Ph.D.
- Nancy Hodgson, Ph.D.
- Shana D. Stites, Psy.D., M.A., M.S.
- Walter Swardfager, Ph.D.
- ALZ WW-FNFP Grant
- Capacity Building in International Dementia Research Program
- ISTAART IGPCC
- Alzheimer’s Disease Strategic Fund: Endolysosomal Activity in Alzheimer’s (E2A) Grant Program
- Imaging Research in Alzheimer’s and Other Neurodegenerative Diseases
- Zenith Fellow Awards
- National Academy of Neuropsychology & Alzheimer’s Association Funding Opportunity
- Part the Cloud-Gates Partnership Grant Program: Bioenergetics and Inflammation
- Pilot Awards for Global Brain Health Leaders (Invitation Only)
- Robert W. Katzman, M.D., Clinical Research Training Scholarship
- Funded Studies
- How to Apply
- Portfolio Summaries
- Supporting Research in Health Disparities, Policy and Ethics in Alzheimer’s Disease and Dementia Research (HPE-ADRD)
- Diagnostic Criteria & Guidelines
- Annual Conference: AAIC
- Professional Society: ISTAART
- Alzheimer's & Dementia
- Alzheimer's & Dementia: DADM
- Alzheimer's & Dementia: TRCI
- International Network to Study SARS-CoV-2 Impact on Behavior and Cognition
- Alzheimer’s Association Business Consortium (AABC)
- Global Biomarker Standardization Consortium (GBSC)
- Global Alzheimer’s Association Interactive Network
- International Alzheimer's Disease Research Portfolio
- Alzheimer’s Disease Neuroimaging Initiative Private Partner Scientific Board (ADNI-PPSB)
- Research Roundtable
- About WW-ADNI
- North American ADNI
- European ADNI
- Australia ADNI
- Taiwan ADNI
- Argentina ADNI
- WW-ADNI Meetings
- Submit Study
- RFI Inclusive Language Guide
- Scientific Conferences
- AUC for Amyloid and Tau PET Imaging
- Make a Donation
- Walk to End Alzheimer's
- The Longest Day
- RivALZ to End ALZ
- Ride to End ALZ
- Tribute Pages
- Gift Options to Meet Your Goals
- Founders Society
- Fred Bernhardt
- Anjanette Kichline
- Lori A. Jacobson
- Pam and Bill Russell
- Gina Adelman
- Franz and Christa Boetsch
- Adrienne Edelstein
- For Professional Advisors
- Free Planning Guides
- Contact the Planned Giving Staff
- Workplace Giving
- Do Good to End ALZ
- Donate a Vehicle
- Donate Stock
- Donate Cryptocurrency
- Donate Gold & Sterling Silver
- Donor-Advised Funds
- Use of Funds
- Giving Societies
- Why We Advocate
- Ambassador Program
- About the Alzheimer’s Impact Movement
- Research Funding
- Improving Care
- Support for People Living With Dementia
- Public Policy Victories
- Planned Giving
- Community Educator
- Community Representative
- Support Group Facilitator or Mentor
- Faith Outreach Representative
- Early Stage Social Engagement Leaders
- Data Entry Volunteer
- Tech Support Volunteer
- Other Local Opportunities
- Visit the Program Volunteer Community to Learn More
- Become a Corporate Partner
- A Family Affair
- A Message from Elizabeth
- The Belin Family
- The Eliashar Family
- The Fremont Family
- The Freund Family
- Jeff and Randi Gillman
- Harold Matzner
- The Mendelson Family
- Patty and Arthur Newman
- The Ozer Family
- Salon Series
- No Shave November
- Other Philanthropic Activities
- Still Alice
- The Judy Fund E-blast Archive
- The Judy Fund in the News
- The Judy Fund Newsletter Archives
- Sigma Kappa Foundation
- Alpha Delta Kappa
- Parrot Heads in Paradise
- Tau Kappa Epsilon (TKE)
- Sigma Alpha Mu
- Alois Society Member Levels and Benefits
- Alois Society Member Resources
- Zenith Society
- Founder's Society
- Joel Berman
- JR and Emily Paterakis
- Legal Industry Leadership Council
- Accounting Industry Leadership Council
Find Local Resources
Let us connect you to professionals and support options near you. Please select an option below:
Use Current Location Use Map Selector
Search Alzheimer’s Association
As the largest nonprofit funder of Alzheimer's research, the Association is committed to accelerating the global progress of new treatments, preventions and, ultimately, a cure.
Information for Researchers
Research we fund, apply for a grant, find a clinical trial, efforts we lead, the first survivor of alzheimer's is out there, but we won't get there without you., learn how alzheimer’s disease affects the brain..
Take the Brain Tour
Don't just hope for a cure. Help us find one. Volunteer for a clinical trial.
Keep up with alzheimer’s news and events.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

Asking the internet about birth control

‘Harvard Thinking’: Facing death with dignity

Novel teamwork, promising results for glioblastoma treatment
The brain that defied alzheimer’s.
Genetic mutation found that could shed light on mechanism for disease resistance, lead to new therapies
Neil Osterweil
MGH News and Public Affairs
Illustration by Roy Scott
Aliria Rosa Piedrahita de Villegas should have developed Alzheimer’s disease in her 40s and died from the disease in her 60s because of a rare genetic mutation.
Instead, she lived dementia-free into her 70s, and now her brain is yielding important clues about the pathology of dementia and possible treatments for Alzheimer’s disease.
As researchers at Massachusetts General Hospital and other centers first described in 2019, the woman, from Medellin, Colombia, was a member of an extended family with a mutation in a gene labeled PSEN1. The PSEN1 E280A mutation is autosomal dominant, meaning that only a single copy of the gene is required to cause disease. Carriers of the mutation typically exhibit symptoms of Alzheimer’s in their 40s or 50s, and die from the disease soon after, but this woman did not begin to show signs of Alzheimer’s until her early 70s. She died in 2020 from metastatic melanoma at the age of 77.
The key difference in the Colombian woman’s ability to fend off the disease for three decades appeared to be that in addition to having the PSEN1 E280A mutation, she was also a carrier of both copies of a mutation known as APOE3 Christchurch.
“This exceptional case is an experiment designed by nature that teaches us a way to prevent Alzheimer’s: let’s observe, learn, and imitate nature.” Francisco Lopera, director of the Neuroscience Group of Antioquia in Medellín, Colombia.
The APOE family of genes control production of apolipoproteins, which transport lipids (fats) in blood and other bodily fluids. The APOE2 variant is known to be protective against Alzheimer’s dementia, while the APOE4 variant is linked to an increased risk for the disease.
APOE3, the most common variant, is not typically associated with either reduced or increased risk for Alzheimer’s.
“This is a ground-breaking case for Alzheimer’s disease and has already opened new paths for treatment and prevention, which we’re currently pursuing with some collaborators. This work is now bringing light into some of the mechanisms of resistance to Alzheimer’s disease” says investigator Yakeel T. Quiroz
Quiroz is director of the Multicultural Alzheimer Prevention Program (MAPP ) at Mass General, an associate professor of psychology at Harvard Medical School, and Paul B. and Sandra M. Edgerley MGH Research Scholar 2020-2025 .
As Quiroz and colleagues now report in the neuropathology journal Acta Neuropathologica , the woman did, in fact, have pathologic features of Alzheimer’s disease in her brain, but not in regions of the brain where the hallmarks of Alzheimer’s are typically found.
“This patient gave us a window into many competing forces — abnormal protein accumulation, inflammation, lipid metabolism, homeostatic mechanisms — that either promote or protect against disease progression, and begin to explain why some brain regions were spared while others were not,” says Justin Sanchez, co-first author, and an investigator at MGH Neurology.
Researchers identified in Aliria’s brain a distinct pattern of abnormal aggregation or “clumping” of tau, a protein known to be altered in Alzheimer’s disease and other neurologic disorders.
In this case, the tau pathology largely spared the frontal cortex, which is important for judgment and other “executive” functions, and the hippocampus, which is important for memory and learning. Instead, the tau pathology involved the occipital cortex, the area of the brain at the back of the head that controls visual perception.
The occipital cortex was the only major brain region to exhibit typical Alzheimer’s features, such as chronic inflammation of protective brain cells called microglia, and reduced levels of APOE expression.
“Thus, the Christchurch variant may impact the distribution of tau pathology, modulates age at onset, severity, progression, and clinical presentation of [autosomal dominant Alzheimer’s disease], suggesting possible therapeutic strategies,” the researchers write.
“It is seldom that we have nice surprises while studying familial Alzheimer’s disease brains. This case showed an amazingly clear protected phenotype. I am sure our molecular and pathologic findings will at least suggest some avenues of research and elicit hope for a successful treatment against this disorder.” says co-first author Diego Sepulveda-Falla, research lead at University Medical Center Hamburg-Eppendorf in Hamburg, Germany.
“This exceptional case is an experiment designed by nature that teaches us a way to prevent Alzheimer’s: let’s observe, learn, and imitate nature,” concludes Francisco Lopera, director of the Neuroscience Group of Antioquia in Medellín, Colombia. Lopera is a co-senior author and the neurologist who discovered this family and has been following them for the last 30 years.
Quiroz is a co-senior author of the report, along with Kenneth S. Kosik, University of California, Santa Barbara; Lopera, and Sepulveda-Falla. Sanchez contributed equally to the study.
The study was supported by grants from the National Institutes of Health, MGH Executive Committee on Research (MGH Research Scholar Award), Alzheimer’s Association, the Deutsche Forschungsgemeinschaft, Universidad de Antioquia, the Werner Otto Stiftung, and the Gernam Federal Ministiry of Education and Research.
Share this article
You might like.
Only a fraction of it will come from an expert, researchers say

In podcast episode, a chaplain, a bioethicist, and a doctor talk about end-of-life care

Researchers cite ‘academic medicine’ as key factor in success
College accepts 1,937 to Class of 2028
Students represent 94 countries, all 50 states
Pushing back on DEI ‘orthodoxy’
Panelists support diversity efforts but worry that current model is too narrow, denying institutions the benefit of other voices, ideas
So what exactly makes Taylor Swift so great?
Experts weigh in on pop superstar's cultural and financial impact as her tours and albums continue to break records.

- April 1, 2024 | New Alzheimer’s Disease Treatment Target Discovered
- April 1, 2024 | Unlocking the Secrets of Life With RNA’s Ancient Code
- April 1, 2024 | Decoding Earth’s Cosmic Shields in Groundbreaking Study
- March 31, 2024 | Revolutionary Study Reveals High-Intensity Exercise May Reverse Parkinson’s Disease Neurodegeneration
- March 31, 2024 | Quantum Computing Recharged With Electromagnetic Ion Trap Innovation
New Alzheimer’s Disease Treatment Target Discovered
By Lancaster University April 1, 2024
Researchers have identified PDE4B as a potential new target for treating Alzheimer’s disease. By reducing PDE4B activity in a mouse model, they observed significant improvements in memory and brain glucose metabolism, providing hope for new therapeutic strategies for Alzheimer’s and possibly other dementias. Further research on PDE4B inhibiting drugs is needed to explore their efficacy in Alzheimer’s treatment.
Scientists at the University of Leeds and Lancaster University in the UK have discovered a potential new target for Alzheimer’s disease treatment – PDE4B.
Alzheimer’s disease is the leading cause of dementia and disability in old age. As the number of people diagnosed with Alzheimer’s disease is on the increase, new treatments are urgently needed to improve the quality of life for people living with the disease.
PDE4B is an enzyme inside cells that breaks down a molecule known as cyclic AMP, which regulates a range of cellular processes. Based on an Australian study that identified the PDE4B gene as a risk factor for developing Alzheimer’s disease, the UK team investigated whether reducing PDE4B activity might protect against Alzheimer’s disease pathology and be a useful treatment approach. To this end, they introduced a gene for reduced PDE4B activity into an Alzheimer’s disease (AD) mouse model that develops amyloid plaques in the brain, a key pathological feature of the disease.
Research Findings and Implications
The researchers observed that AD mice showed memory deficits in maze tests, but memory was unimpaired in AD mice with genetically reduced PDE4B activity. Using functional brain imaging, the team found the metabolism of glucose, the main source of energy in the brain, was impaired in AD mice, like that seen in patients with the disease. However, AD mice with genetically reduced PDE4B activity showed healthy levels of glucose metabolism in the brain.
To understand the mechanisms involved, the researchers next looked at gene and protein expression levels in the brain. This identified increased inflammation in the brains of AD mice, like that seen in Alzheimer’s disease patients, but inflammation was lower in AD mice with genetically reduced PDE4B activity. Similar effects were seen for a range of other proteins involved in Alzheimer’s disease pathology. Overall, these data suggest that reducing PDE4B activity might be a useful approach for the treatment of Alzheimer’s disease, although more research is needed to validate the use of drugs that target the enzyme.
Dr Steven Clapcote, the lead researcher, from the University of Leeds, said, “Reducing the activity of the PDE4B enzyme had a profound protective effect on memory and glucose metabolism in the AD mouse model, despite these mice showing no decrease in the number of amyloid plaques in the brain. This raises the prospect that reducing PDE4B activity may protect against cognitive impairment not only in Alzheimer’s disease but also in other forms of dementia, such as Huntington’s disease.”
Dr Neil Dawson, a co-author of the paper, from Lancaster University, echoed these sentiments: “These results offer real hope for the development of new treatments that will benefit patients with Alzheimer’s disease in the future. It was intriguing to find that reducing PDE4B activity by just 27% could dramatically rescue memory, brain function, and inflammation in the AD mice. The next stage is to test whether PDE4B inhibiting drugs have similar beneficial effects in the AD mouse model, to test their potential efficacy in Alzheimer’s disease.”
Reference: “Protective effect of PDE4B subtype-specific inhibition in an App knock-in mouse model for Alzheimer’s disease” by Paul Armstrong, Hüseyin Güngör, Pariya Anongjanya, Clare Tweedy, Edward Parkin, Jamie Johnston, Ian M. Carr, Neil Dawson and Steven J. Clapcote, 23 March 2024, Neuropsychopharmacology . DOI: 10.1038/s41386-024-01852-z
The research was supported by the Dunhill Medical Trust, BBSRC, Alzheimer’s Research UK, and the Scientific and Technological Research Council of Turkey.
More on SciTechDaily

Galactic Surprise: James Webb Space Telescope Unveils Hidden Companion Galaxy
Cracking the Code: The Math Behind Nature’s Cellular Puzzles

Magnet Mayhem: How Meteorite Hunters Accidentally Destroy Scientific Goldmines

NASA to Practice Artemis Moonwalking, Roving Operations in Arizona Desert

50% of Parents Regularly Give Kids Dietary Supplements

Soft, Stretchy and Strong Electronic Skin Mimics Natural Functions of Human Skin

First Complete Cellular Map of a Mammalian Brain Reveals Over 5,300 Cell Types

Cutting-Edge Science Advances on Space Station as Crew Prepares for Departure
Be the first to comment on "new alzheimer’s disease treatment target discovered", leave a comment cancel reply.
Email address is optional. If provided, your email will not be published or shared.
Save my name, email, and website in this browser for the next time I comment.
New treatment target identified for Alzheimer's disease
Researchers at the University of Leeds and Lancaster University in the UK have identified a new potential target for the treatment of Alzheimer's disease -- PDE4B.
Alzheimer's disease is the leading cause of dementia and disability in old age. As the number of people diagnosed with Alzheimer's disease is on the increase, new treatments are urgently needed to improve the quality of life for people living with the disease.
PDE4B is an enzyme inside cells that breaks down a molecule known as cyclic AMP, which regulates a range of cellular processes. Based on an Australian study that identified the PDE4B gene as a risk factor for developing Alzheimer's disease, the UK team investigated whether reducing PDE4B activity might protect against Alzheimer's disease pathology and be a useful treatment approach. To this end, they introduced a gene for reduced PDE4B activity into an Alzheimer's disease (AD) mouse model that develops amyloid plaques in the brain, a key pathological feature of the disease.
The researchers observed that AD mice showed memory deficits in maze tests, but memory was unimpaired in AD mice with genetically reduced PDE4B activity. Using functional brain imaging, the team found the metabolism of glucose, the main source of energy in the brain, was impaired in AD mice, like that seen in patients with the disease. However, AD mice with genetically reduced PDE4B activity showed healthy levels of glucose metabolism in the brain.
To understand the mechanisms involved, the researchers next looked at gene and protein expression levels in the brain. This identified increased inflammation in the brains of AD mice, like that seen in Alzheimer's disease patients, but inflammation was lower in AD mice with genetically reduced PDE4B activity. Similar effects were seen for a range of other proteins involved in Alzheimer's disease pathology. Overall, these data suggest that reducing PDE4B activity might be a useful approach for the treatment of Alzheimer's disease, although more research is needed to validate the use of drugs that target the enzyme.
Dr Steven Clapcote, the lead researcher, from the University of Leeds, said, "Reducing the activity of the PDE4B enzyme had a profound protective effect on memory and glucose metabolism in the AD mouse model, despite these mice showing no decrease in the number of amyloid plaques in the brain. This raises the prospect that reducing PDE4B activity may protect against cognitive impairment not only in Alzheimer's disease but also in other forms of dementia, such as Huntington's disease."
Dr Neil Dawson, a co-author of the paper, from Lancaster University, echoed these sentiments: "These results offer real hope for the development of new treatments that will benefit patients with Alzheimer's disease in the future. It was intriguing to find that reducing PDE4B activity by just 27% could dramatically rescue memory, brain function and inflammation in the AD mice. The next stage is to test whether PDE4B inhibiting drugs have similar beneficial effects in the AD mouse model, to test their potential efficacy in Alzheimer's disease."
The research was published in the Nature Portfolio journal Neuropsychopharmacology and was supported by the Dunhill Medical Trust, BBSRC, Alzheimer's Research UK, and the Scientific and Technological Research Council of Turkey.
- Alzheimer's Research
- Healthy Aging
- Diseases and Conditions
- Alzheimer's
- Disorders and Syndromes
- Alzheimer's disease
- House mouse
- Stem cell treatments
- Memory-prediction framework
- Memory bias
- Dementia with Lewy bodies
Story Source:
Materials provided by Lancaster University . Note: Content may be edited for style and length.
Journal Reference :
- Paul Armstrong, Hüseyin Güngör, Pariya Anongjanya, Clare Tweedy, Edward Parkin, Jamie Johnston, Ian M. Carr, Neil Dawson, Steven J. Clapcote. Protective effect of PDE4B subtype-specific inhibition in an App knock-in mouse model for Alzheimer’s disease . Neuropsychopharmacology , 2024; DOI: 10.1038/s41386-024-01852-z
Cite This Page :
Explore More
- Simple Brain-Computer Link: Gaming With Thoughts
- Clinical Reasoning: Chatbot Vs Physicians
- Understanding People Who Can't Visualize
- Illuminating Oxygen's Journey in the Brain
- DNA Study IDs Descendants of George Washington
- Heart Disease Risk: More Than One Drink a Day
- Unlocking Supernova Stardust Secrets
- Why Do Some Memories Become Longterm?
- Cell Division Quality Control 'Stopwatch'
- What Controls Sun's Differential Rotation?
Trending Topics
Strange & offbeat.
Alzheimer's Research & Therapy
Announcing the launch of mini reviews.

Concise overview articles of key topics in neurodegeneration, which can be read wherever you are, whenever suits you.
Find out more here .
New Thematic Series - AI in Dementia

Alzheimer's Research & Therapy presents a thematic series focusing on the use of artificial intelligence, machine learning and related techniques in dementia research.
Find out more about the series here .
- Most accessed
White matter hyperintensity patterns: associations with comorbidities, amyloid, and cognition
Authors: Dario Bachmann, Bettina von Rickenbach, Andreas Buchmann, Martin Hüllner, Isabelle Zuber, Sandro Studer, Antje Saake, Katrin Rauen, Esmeralda Gruber, Roger M. Nitsch, Christoph Hock, Valerie Treyer and Anton Gietl
A systematic review of progranulin concentrations in biofluids in over 7,000 people—assessing the pathogenicity of GRN mutations and other influencing factors
Authors: Imogen J. Swift, Rosa Rademakers, NiCole Finch, Matt Baker, Roberta Ghidoni, Luisa Benussi, Giuliano Binetti, Giacomina Rossi, Matthis Synofzik, Carlo Wilke, David Mengel, Caroline Graff, Leonel T. Takada, Raquel Sánchez-Valle, Anna Antonell, Daniela Galimberti…
ANU-ADRI scores, tau pathology, and cognition in non-demented adults: the CABLE study
Authors: Shan Yin, Pei-Yang Gao, Ya-Nan Ou, Yan Fu, Ying Liu, Zuo-Teng Wang, Bao-Lin Han and Lan Tan
Potential ocular indicators to distinguish posterior cortical atrophy and typical Alzheimer’s disease: a cross-section study using optical coherence tomography angiography
Authors: Yan Sun, Lumi Zhang, Hui Ye, Lumin Leng, Yi Chen, Yujie Su, Peifang Ren, Hong Lu and Guoping Peng
Navigating the metabolic maze: anomalies in fatty acid and cholesterol processes in Alzheimer’s astrocytes
Authors: Xiaoyu Zhang, Chuanying Chen and Yi Liu
Most recent articles RSS
View all articles
Stem cell factor and granulocyte colony-stimulating factor reduce β-amyloid deposits in the brains of APP/PS1 transgenic mice
Authors: Bin Li, Maria E Gonzalez-Toledo, Chun-Shu Piao, Allen Gu, Roger E Kelley and Li-Ru Zhao
Cerebral microbleeds: overview and implications in cognitive impairment
Authors: Sergi Martinez-Ramirez, Steven M Greenberg and Anand Viswanathan
BACE1 inhibitor drugs in clinical trials for Alzheimer’s disease
Authors: Robert Vassar
A randomized, double-blind, phase 2b proof-of-concept clinical trial in early Alzheimer’s disease with lecanemab, an anti-Aβ protofibril antibody
Authors: Chad J. Swanson, Yong Zhang, Shobha Dhadda, Jinping Wang, June Kaplow, Robert Y. K. Lai, Lars Lannfelt, Heather Bradley, Martin Rabe, Akihiko Koyama, Larisa Reyderman, Donald A. Berry, Scott Berry, Robert Gordon, Lynn D. Kramer and Jeffrey L. Cummings
The Correction to this article has been published in Alzheimer's Research & Therapy 2022 14 :70
Alzheimer’s disease drug-development pipeline: few candidates, frequent failures
Authors: Jeffrey L Cummings, Travis Morstorf and Kate Zhong
Most accessed articles RSS
Early Career Researcher Reviewer Panel
Interested in an introduction to peer reviewing articles for Alzheimer's Research & Therapy?
Find out more about our ECR Peer Reviewer Panel!
Aims and scope
Alzheimer's Research & Therapy is the major forum for translational research into Alzheimer's disease. An international peer-reviewed journal, it publishes open access basic research with a translational focus, as well as clinical trials, research into drug discovery and development, and epidemiologic studies. The journal also provides reviews, viewpoints, commentaries, debates and reports.
Although the primary focus is Alzheimer's disease, the scope encompasses translational research into other neurodegenerative diseases.
Published Thematic Series

10 Years of Alzheimer's Research & Therapy

Subject Cognitive Decline
Latest Tweets
Your browser needs to have JavaScript enabled to view this timeline
Alzheimer's blogs from BMC
Failed to load RSS feed.
- Editorial Board
- Instructions for Editors
- Sign up for article alerts and news from this journal
Affiliated with

Annual Journal Metrics
2022 Citation Impact 9.0 - 2-year Impact Factor 9.2 - 5-year Impact Factor 1.849 - SNIP (Source Normalized Impact per Paper) 2.650 - SJR (SCImago Journal Rank)
2023 Speed 15 days submission to first editorial decision for all manuscripts (Median) 152 days submission to accept (Median)
2023 Usage 1,914,774 downloads 2,982 Altmetric mentions
- More about our metrics
ISSN: 1758-9193
- General enquiries: [email protected]
6.9 million Americans have Alzheimer's disease: How to reduce your risk

A new report estimates 6.9 million older Americans are living with Alzheimer’s disease in 2024, an increase of about 200,000 cases of the mind-robbing disease from 2023 and "a significant public health crisis," according to an expert.
Another 5 million to 7 million adults have mild cognitive impairment, a set of early changes to memory and thinking linked to Alzheimer's, according to an Alzheimer's Association's annual facts and figures report released Wednesday.
The report also highlights good news. Other studies indicate that dementia rates have declined over the past 25 years as more adults are achieving higher levels of education, staying active and exercising, reducing their blood pressure, avoiding cigarettes and staying socially engaged.
Adults face a higher risk of Alzheimer's and other types of dementia as they age, and the number of Americans 65 and older is projected to swell from 58 million in 2022 to 82 million in 2050. In just six years, the youngest baby boomers will be 65.
The nation's aging population will create profound economic and social challenges. The annual cost of caring for people with Alzheimer’s or other types of dementia will be $360 billion in 2024, up $15 billion from a year ago, the report said.
Medicare and Medicaid will cover the bulk of that, spending $231 billion this year to care for people with Alzheimer’s and dementia. Public and private spending to take care of Alzheimer's and dementia patients will skyrocket to nearly $1 trillion in 2050, the report projects.
"Our population is aging, so we really need to address these issues," said Sam Fazio, the Alzheimer Association's senior director of quality care and psychosocial research. "Alzheimer's disease remains a significant public health crisis."
Lifestyle changes reduce risk
Other Alzheimer's experts not involved with the report said more Americans are taking steps to reduce their risk for Alzheimer's or dementia.
Research suggests up to 40% of dementia cases can be prevented through lifestyle changes, said Dr. Keith Vossel, a neurologist and director of the Mary S. Easton Center for Alzheimer’s Research and Care at the University of California, Los Angeles.
Vossel said people who exercise regularly, do not smoke and achieve higher levels of education tend to have lower risk. Reducing blood pressure in midlife, in particular, is linked to lower risk, he said.
Paying close attention to elevated blood pressure is especially important, Vossel said. "We know that lowering blood pressure among people with elevated blood pressure in middle life can lower risk of dementia or (mild cognitive impairment) later on."
Caregivers spend 31 hours a week on Alzheimer's, dementia patients
Families and other caregivers take on an array of tasks, scheduling appointments and feeding and caring for people with Alzheimer's or dementia. The report said 11.5 million relatives and caregivers provided more than 18 million hours of unpaid care last year.
That amounted to a full-time job for caregivers who spent an average of nearly 31 hours a week caring for a person with Alzheimer's or dementia.
In July, the Centers for Medicare & Medicaid Services will launch an initiative to improve the quality of life for people with dementia, allowing them to remain at home and reduce the strain on unpaid caregivers. The model, called Guiding an Improved Dementia Experience , will coordinate care and provide a 24/7 support line. Families also can access care navigators who can connect patients and caregivers to services and support. Doctors and clinics who participate will receive a monthly per-patient fee from Medicare.
Fazio said access to navigators is crucial because the report showed that families live through a great deal of stress and that workers in the field believe the health care system is not equipped to help people living with dementia. President Joe Biden recently expanded a similar navigator plan for cancer patients in which private health insurers will cover such services.
Families "really want help and need help to navigate the system," Fazio said.
New drugs, old target
Of the eight drugs approved for Alzheimer's patients, only two attempt to attack the disease and slow memory and cognitive decline. Biogen has discontinued one of those drugs, aducanumab, sold under the brand Aduhelm. The Food and Drug Administration approved the drug despite mixed clinical trial results . Biogen also faced withering criticism when it launched Aduhelm, initially priced at $56,000 a year.
In January 2023, Eisai won FDA approval for its amyloid beta-busting drug , lecanemab. Sold under the brand name Leqembi, the drug is intended for patients in the early stages of the disease, the population studied in clinical trials.
The Alzheimer's Association report notes that the benefits of lecanemab "in the short term may be imperceptible" because it's designed to slow the disease, not reverse cognitive decline. The report said the long-term results of the drug are not clear.
Earlier this month, the FDA delayed action for Eli Lilly's drug donanemab , the drug manufacturer said. The FDA expects to convene an advisory committee to discuss the treatment.
Clinical trials of all three amyloid-removing drugs have side effects visible on brain scans, such as brain swelling and bleeding. Some patients don't notice symptoms. Others have experienced headaches, dizziness, nausea, confusion and vision changes.
Though drugmakers largely have focused on drugs to target and clear amyloid from the brains of Alzheimer's patients, the report says, other studies are examining different methods of attacking the disease. Other potential drugs are being studied to limit the accumulation of tau protein, inflammation, altered cell metabolism and damage from toxic oxygen molecules, the report said.
Ken Alltucker is on Twitter at @kalltucker, or can be emailed at [email protected].
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Alzheimer's disease articles from across Nature Portfolio
Alzheimer's disease is a progressive neurodegenerative disease that impairs memory and cognitive judgment and is often accompanied by mood swings, disorientation and eventually delirium. It is the most common cause of dementia.
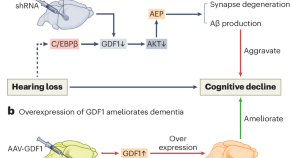
Hearing loss promotes Alzheimer’s disease
Epidemiological studies reveal a correlation between hearing loss and the development and progression of Alzheimer’s disease (AD), but the underlying causal mechanisms remain unclear. A study now provides experimental evidence that hearing loss can promote AD via the growth differentiation factor 1 (GDF1) pathway, which may aid in developing potential AD therapeutic strategies.
- Hong-Bo Zhao
Latest Research and Reviews
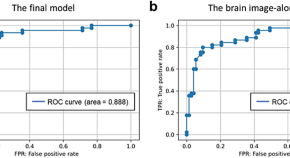
Amyloid-β prediction machine learning model using source-based morphometry across neurocognitive disorders
- Yuki Momota
- Shogyoku Bun
- Masaru Mimura
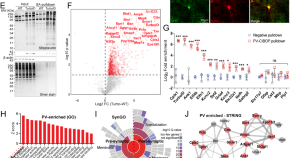
Native-state proteomics of Parvalbumin interneurons identifies unique molecular signatures and vulnerabilities to early Alzheimer’s pathology
Native state proteomics of PV interneurons revealed unique molecular features of high translational and metabolic activity, and enrichment of Alzheimer’s risk genes. Early amyloid pathology exerted unique effects on mitochondria, mTOR signaling and neurotransmission in PV neurons.
- Prateek Kumar
- Annie M. Goettemoeller
- Srikant Rangaraju
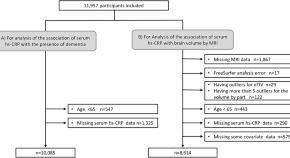
Serum high-sensitivity C-reactive protein and dementia in a community-dwelling Japanese older population (JPSC-AD)
- Ayumi Tachibana
- Jun-ichi Iga
- Yutaka Kiyohara

Xenografted human microglia display diverse transcriptomic states in response to Alzheimer’s disease-related amyloid-β pathology
Human microglia transplanted in the mouse brain mount a multipronged response to amyloid-β pathology, displaying unique transcriptional states. Alzheimer’s disease risk genes are differentially regulated across cell states and profoundly alter microglial function.
- Renzo Mancuso
- Nicola Fattorelli
- Bart De Strooper

Single-nucleus RNA velocity reveals critical synaptic and cell-cycle dysregulations in neuropathologically confirmed Alzheimer’s disease
- Quadri Adewale
- Ahmed F. Khan
- Yasser Iturria-Medina

TREM1 disrupts myeloid bioenergetics and cognitive function in aging and Alzheimer disease mouse models
The role of TREM1 in neurodegenerative diseases is unclear. Here the authors show that TREM1 promotes cognitive decline in aging and in the context of amyloid pathology in a mouse model of Alzheimer disease.
- Edward N. Wilson
- Congcong Wang
- Katrin I. Andreasson
News and Comment
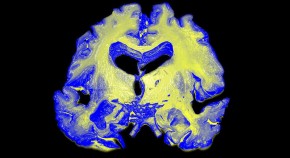
A test for Alzheimer’s-disease stage predicts dementia risk
Levels of a host of molecules in the cerebrospinal fluid reliably assess development of the disease.

A timeline of biomarker changes before Alzheimer’s disease
Longitudinal data from the China Cognition and Aging Study map the sequential biomarker changes that begin almost two decades before clinical onset of Alzheimer’s disease.
- Karen O’Leary
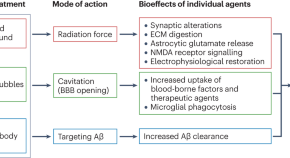
Ultrasound and antibodies — a potentially powerful combination for Alzheimer disease therapy
Success in a trial of low-intensity ultrasound combined with an amyloid-β antibody represents a major stride towards integrating pharmacological and nonpharmacological approaches to reduce the amyloid-β load in patients with mild Alzheimer disease. This trial also highlights the potential of therapeutic ultrasound modalities to combat neurodegenerative diseases.
- Jürgen Götz
- Pranesh Padmanabhan
Early dementia diagnosis: blood proteins reveal at-risk people
The results of a large-scale screening study could be used to develop blood tests to diagnose diseases such as Alzheimer’s before symptoms take hold.
- Miryam Naddaf
Regional vulnerability to Aβ and tau pathology
Quick links.
- Explore articles by subject
- Guide to authors
- Editorial policies

New wonder jab to prevent dementia available on NHS in FIVE years - 'Massive breakthrough'

WATCH HERE: New wonder jab to prevent dementia could be available within five years in 'massive breakthrough'

By Oliver Trapnell
Published: 31/03/2024
Updated: 31/03/2024
Scientists have branded the vaccine a ‘game-changer’
Don't miss, urgent intervention to stop 'health and safety killjoys' silencing historic gun salute from edinburgh castle, paul o’grady fans left ‘in tears’ as he makes stark health admission in last series: ‘something for my heart’, david attenborough fans complain minutes into ‘brutal’ hunting scenes as mammal series begins, king charles sitting separately during the easter service 'brings back memories of the queen', driving law changes in april will see britons impacted - new car tax costs, dvla updates & more, easter bank holiday opening times: what stores will open tesco, next, aldi, ikea and more, zara tindall tipped to 'pick up the slack' during prince william's reign, james middleton breaks silence after vowing to 'climb mountain' with kate, harry and meghan attacks have brought kate, william, charles and camilla together - lady c, trending on gb news, pippa middleton's friends lift lid on her relationship with kate.
A revolutionary wonder jab to help prevent dementia could be available on the NHS in as little as five years in what is being hailed as a “massive breakthrough” by health experts.
The vaccine is currently in the early stages of patient trials and is tipped to become widely available on the NHS within five years.
Targeting toxic proteins in the brain, the jab aims to remove the harmful chemicals before they can cause damage and lead to the most common form of dementia, Alzheimer’s.
Alzheimer’s affects roughly 540,000 people in the UK but this number is expected to rise to almost 1 million people by 2040.
New wonder jab to prevent dementia available on NHS in FIVE years - 'Massive breakthrough'
Getty Images
The disease affects several aspects of the brain including memory, thinking and ability to function.
Scientists believe it is caused when naturally occurring proteins, known as amyloids become “misfolded” and clump together which causes irreparable damage over time and leads to a gradual decline in cognitive function.
Ruthie Henshall, 57, told the Sunday Express the jab could be a “miracle” for sufferers.
The West End star, whose late mother Gloria had dementia, said: “A drug would be a miracle because there are enormous numbers of people with dementia and it's on the rise because we're living longer.
“This drug could be the hope people have been dreaming of - up there with finding the cure for cancer.”
- England fans warned of new terror threat for Euro 2024 with 'dangers raised to new level' ahead of tournament
- Paul receives chilling challenge ahead of controversial Tyson boxing fight - 'I'll hurt him'
- Angela Levin issues warning King to 'be careful' ahead of Easter service
The drug is known as ACI-24
Five centres in the UK are believed to be carrying out studies on the vaccine including Oxford and Cambridge Universities with trials being backed by the Government’s National Institute for Health and Care Research.
Preliminary results of the trials will be presented at a conference in the US in July.
The drug, known as ACI-24, helps the body develop a natural immune defence against dementia by targetting toxic amyloid proteins and clearing them from the brain.
Administered in up to five jabs over the course of a year, the jab prompts the body’s immune cells to latch onto the amyloids and remove them.
Dr Shahid Zaman said he was 'very excited' about what the drug could acheive
Trials are set to involve two sets of people who have shown early signs of dementia, one group aged 50-58 and the other aged 35-50 who have Down syndrome and are therefore at greater risk of developing the disease.
Dr Shahid Zaman, an Alzheimer’s expert at Cambridge University, said: “This is so important and exciting especially for the Down syndrome population who have a gene which overproduces this toxic amyloid protein putting them at very high risk of this disease.
“We finally have something that targets the amyloid protein and clears it.
“We can be very optimistic this vaccine will prevent or delay the onset of Alzheimer’s.”
He added: “Alzheimer’s can take decades of time before symptoms appear due to a build up of damage.
“For over a decade drug companies have put millions of pounds into drugs to target the amyloid plaques in the brain, but previous drugs have been shown to have awful side effects including brain bleeds.
“While this vaccine still has some side effects they are far less. I am very excited.”
You may like
Listen live
Study finds 3 big risk factors for dementia

Diabetes, air pollution and alcohol consumption could be the biggest risk factors for dementia, a study has found.
Researchers compared modifiable risk factors for dementia — which is characterized by the impairment of memory, thinking and reasoning — and studied how these factors appear to affect certain brain regions that are already particularly vulnerable to Alzheimer’s disease and schizophrenia.
The research, based on brain scans of nearly 40,000 adults, between ages 44 and 82, in Britain was published Wednesday in Nature Communications.
These vulnerable regions of the brain develop during adolescence and help the brain process and integrate “bits of information across different modalities, across different senses,” said Gwenaëlle Douaud , an associate professor at the University of Oxford and co-author of the study. But “they’re the first ones to go when we start aging.”
“What we’re trying to do is say: What are the common risk factors for dementia that are affecting these regions?” Douaud said. “These are the three most harmful but then, obviously, the others, they have an effect.”
- Researchers investigated the genetic and modifiable risk factors that contribute to the vulnerability of the “most fragile parts of the brain” by studying the brain scans of nearly 40,000 relatively healthy participants from the U.K. Biobank.
- The study examined 161 modifiable risk factors, including blood pressure, cholesterol, diabetes, weight, alcohol consumption, smoking, mood, inflammation, pollution, hearing, sleep, socialization, diet, physical activity and education.
- A diagnosis of diabetes, the amount of nitrogen dioxide in the air and how often someone drinks alcohol — from never to daily, or nearly every day — were found to be the three most detrimental risk factors to these regions of the brain, Douaud said.
- Diabetes, air pollution and alcohol consumption each has an effect that is about twice as much as the other leading risk factors, Douaud said. The next major risk factors are sleep, weight, smoking and blood pressure.
- Researchers identified seven genetic clusters that affect these vulnerable parts of the brain, some of which are also associated with Parkinson’s and Alzheimer’s diseases. Douaud said the genetic and modifiable risk factors are not comparable.
More than 55 million people live with dementia around the world, and that figure is expected to increase to 153 million by 2050, according to the World Health Organization.
Get Well+Being tips straight to your inbox

Dementia is the loss of cognitive function, and symptoms result from brain neurons losing their connection to other brain cells and eventually dying, according to the National Institute on Aging . Everyone loses neurons over time, but the loss is more significant in dementia patients.
Diabetes and alcohol consumption “have been consistently shown to be associated with both cerebral and cognitive decline,” the researchers wrote in the Nature Communications study. And there is growing evidence that exposure to air pollution is a risk factor for cognitive decline and dementia.
A 2020 Lancet report on dementia found that a dozen modifiable risk factors such as hypertension, hearing impairment, smoking and obesity together account for up to 40 percent of dementia cases worldwide.
A person’s age, genes, family history, a traumatic brain injury or a stroke also are potential risk factors .
What other experts say
Gill Livingston , a professor of psychiatry of older people at University College London and the lead author of the 2020 Lancet report, said that the new study was “very interesting” but that the participants in the U.K. Biobank are a “much healthier” and highly motivated group. The findings may not be applicable to a broader population.
Still, they show that people can make decisions to reduce their risk of cognitive decline as they age, Livingston said.
“There’s quite a lot people can do in their everyday life to maintain cognitive health ,” she said. “This just reinforces it.”
What you can do about it
Try to eat a healthy, varied diet to help lower your blood sugar, take measures to protect against “traffic-related pollution” and drink alcohol in moderation, Douaud said in an email.
“Of course, some of these should not only be down to individuals, and the burden should also be shared with (local) governments devising helpful policies,” she said.
Livingston said social and physical activity — talking with friends and exercising — “make a huge difference.” And stimulating experiences, walking outside , “seeing different things” can be beneficial, she said.
Hearing loss , which is more likely as a person ages, can take away opportunities for conversations that lead to “rapid brain stimulation,” Livingston said.
“And if you smoke, stop,” she said.
Marlene Cimons contributed to this report.
Read more from Well+Being
Well+Being shares news and advice for living well every day. Sign up for our newsletter to get tips directly in your inbox.
Vitamin B12 for fatigue has no proven benefit unless you have a deficiency that causes anemia.
Flashes, shimmers and blind spots: Here’s what migraine aura looks like.
Sparkling water is a better choice for your teeth than most popular beverages.
You can help your brain form healthy habits and break the bad ones.
Our 7 best tips to build an exercise habit .

More From Forbes
Kerrin laz inspires napa valley with her fight against alzheimer’s.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Kerrin Laz - Founder of Inspire Napa Valley
Ten years ago Kerrin Laz learned her mother had early-onset Alzheimer’s disease. Alzheimer’s disease affects almost 7 million people in the U.S. and nearly 60 million worldwide. While we all deal with adversity in our own ways Kerrin and her mother refused to be defined by the disease. In 2017 Kerrin channeled her anguish into action with the founding of Inspire Napa Valley . Through her visionary initiative, Laz has transcended the boundaries of conventional charity. With meticulous care and determination, she has harnessed the power of wine to bring light and hope to those impacted by Alzheimer's. At the event each sip becomes a gesture of support, each bottle bid on becomes a beacon of unity in the fight against this relentless illness. Since 2017, the fundraising event in partnership with the Alzheimer’s Association , has raised more than $6 million for the Alzheimer’s Association’s care, support, and research programs.
“The incredible generosity of my family, friends, and fellow winemakers is a testament to our shared commitment to one day live in a world without Alzheimer's disease," said Inspire Napa Valley founder Kerrin Laz. “Because of their kindness, we are helping move the needle – in honor of my mother and millions of others – in Alzheimer’s and dementia research while supporting people and their families who are struggling with the disease.”
2024 marks the fifth year for Inspire Napa Valley, which will take place from May 3rd through 5th at various locations around Napa Valley Wine Country. Alongside Honorary Committee members, including executive wine editor of Food & Wine Ray Isle, Vinous Founder Antonio Galloni, and Bryant Wines proprietor Bettina Bryant, Laz and Inspire Napa Valley will offer guests a unique opportunity to mingle with Napa Valley’s top vintners and winemakers. The weekend’s list of events includes:
● Friday, May 3: The weekend will kick off with an intimate, one-of-a-kind evening featuring a VIP Welcome Dinner paired with wines from some of the most revered wineries in Napa Valley.
● Saturday, May 4 (morning): The weekend will continue with a VIP Alzheimer’s Research Update & Wine Seminar at Round Pond Estate . Following the Alzheimer’s research update by Alzheimer’s Association Chief Science Officer Dr. Maria Carrillo, a group of distinguished panelists will discuss a hand-picked lineup of compelling wines chosen for the sit-down wine tasting seminar.
● Saturday, May 4 (evening): The Main Event will commence with a walk-around wine tasting at Beaulieu Garden featuring 30 of the most exclusive wineries in California with culinary stations prepared by top Napa chefs. The evening will continue with a seated dinner and conclude with Inspire Napa Valley’s signature live auction and paddle raise.
Total Solar Eclipse Emoji Map Meme Tells You All You Need To Know
The walking dead the ones who live season finale review super easy barely an inconvenience, the russians sent a platoon of grenade hurling robotic mini tanks into battle the ukrainians blew up the bots in the usual way with drones.
● Sunday, May 5: The weekend tops off with a VIP Farewell Brunch at Thomas Keller’s Ad Hoc + Addendum , featuring fried chicken and waffles supplemented by offerings from the restaurant’s signature Bloody Mary and Mimosa bar.
I had the pleasure of catching up with Kerrin Laz to discuss her wine label, what’s new this year with Inspire Napa Valley, and misconceptions about Alzheimer’s and what the public can do to help fight it.
Napa Valley's top Vintners are at INV
1. What was your first experience with wine? Did your parents drink wine?
I drank wine in college from time to time. It was with college friends and the wines were what we like to say, ‘easy drinkers.’ My mom drank wine on occasion and pretty much stuck to dry white wines.
2. When did you decide wine was more than a hobby?
I went from drinking wine casually, to becoming more curious when I started working at a restaurant. It became a defining part of my life when I literally chose wine over food as my specialty when beginning my career with a company called DEAN & DELUCA. I randomly walked into the Georgetown/DC store and the manager asked me what I was interested in doing and I answered, ‘maybe food or wine’ and she asked, ‘well, which one?’ And I said ‘wine…?’
3. What formal education or certifications do you possess? What educational opportunities are you currently pursuing? Any obstacles?
I never received a formal education in the wine industry, but people have told me I got the million-dollar education from having the privilege to learn from the best vintners, winemakers, and viticulturists in California. I went from occasionally drinking $15 bottles in college to regularly tasting and drinking wines that were $100+ per bottle within a year of getting into wine. When I moved out to California, I really started soaking it all in and listening and learning from the best in the business. From meeting vintners to the managers, production, sales, viticulturists, and winemakers - you name it. They all shared their stories with me and were so generous with their knowledge. I just continued to listen and learn, weaving all their stories and knowledge together in my mind.
4. Tell me more about your role. What does it entail? What do you like or love about? Challenges?
My mentor once told me that I am not a great manager. I looked at him in disbelief at the time and now 10 years later I see what he meant. I am better at envisioning ideas, formulating plans, and executing them. I love having the ability to steer the business into the best possible growth potential, in a nimble way. The downside is there always work to be done. It never ends. I just try to get to a good stopping point.
5. When your mother was diagnosed with Alzheimer’s how did you turn that struggle into positive action with the creation of Inspire Napa Valley?
It only took me a few weeks to decide that I wanted to start Inspire Napa Valley . I was in the perfect position with all the contacts and relationships I had developed being in the wine industry for over a decade. It was like having both sides of the coin – the clientele that would hopefully become potential guests and the wineries that would hopefully become partners in my vision. The rest of the community also began getting involved after Inspire launched.
6 . What misconceptions do people have over the disease?
I think that people might think that everyone’s path with Alzheimer’s and dementia is the same after diagnosis. I’ve learned through the years that is not the case. Those who are diagnosed don’t all have the same rate of progression, and it will affect everyone differently. I also think that someone who has a relative with Alzheimer's and dementia will automatically worry that they have it, which is only natural. But that is not the case for everyone.
7. In addition to donating to Inspire Napa Valley what can we do to support those with Alzheimer’s?
I think volunteering locally at memory care centers is helpful. Music and art are an incredible connection for those with Alzheimer’s and dementia so if you’re musically or artistically inclined, that’s even better. Just visiting and playing music from a playlist is great too.
8. What should consumers expect in 2024 at Inspire Napa Valley? Anything new?
The VIP Friday dinner will be at a new winery with a new theme and Saturday’s main event will also be at a new location, with a hybrid of the last two years when it comes to the food. The VIP Saturday Wine Seminar will also have a different theme with a new set of panelists and of course, a focus on new wines. We loved the food stations we did at last year’s tasting so we will continue that but also when guests get into the tent, we will have a sit-down coursed dinner. We’re continuously learning from the previous year so each year will have adaptations.
9. I heard you have your own wine label. What went into your decision to start it?
Yes, K. LAZ WINE COLLECTION . In regard to starting my own label, it was a hypothetical question I asked myself. I thought – ‘what if?’ What if I could start my own wine label? Who would I ask to be my winemaker? Where would we source the grapes? Napa Valley was the obvious answer because K. LAZ was only a year old in Yountville, so I needed to be in Napa Valley. I love the wines that Celia Welch makes, and we met, and I think the project was small enough that she didn’t feel like it would take time away from existing clients.
10. In regards to diversity, what has the wine industry gotten right and/or improved upon in the last 5 years?
The wine industry, overall, is trying to improve. There seems to be a conscious effort to be more inclusive, whether it's driven by a sense of moral responsibility or as a strategic marketing approach. Either way though, it is happening. I recently noticed that companies now highlight in their marketing materials that they are women-owned or minority-owned. I believe this prompts people to reflect, and that's a positive development.
11. Spirits does a better job of advertising to young, diverse 21+ consumers in the U.S. As an insider, what are tangible actions to promote to a broader demographic of wine consumers?
That’s the billion-dollar question and I’m not sure what the answer is. I admit, we are lucky because our demographic is all over the place. We have a broad spectrum, in truth, because we are a company led by younger professionals, and we have many longtime clients on our mailing list who have kids now who are drinking so we’re now working with them, too. And they have friends who they’ve connected with us with and so on. Word of mouth has been so important to us and when we have the 20-somethings visiting us, they are telling all their friends and posting on social media. In essence, they are marketing for us.
12. What’s next for you in your career? I want to focus on growing Inspire Napa Valley. I am also considering expanding K. LAZ in a few select locations.
13. If you could only drink one varietal for the rest of this year, what would it be? Chardonnay because the styles are endless! And I can always drink a great Blanc de Blancs because that counts, right?!
14 . If you weren’t working in wine what would be your profession?
I think I would have been a therapist, social worker, or psychologist.
15. Favorite wine region outside of California? Burgundy.
16. Who do you look up to and/or admire in the wine industry? Why?
Leslie Rudd because he was a great thinker and listener and completely original. He shared his knowledge with me and was a great mentor to me.
Francoise Peschon because she has a great work/life balance, and she has never let her success change her demeanor or outlook.
David Abreu has built a vineyard management company that is one of the best in California with little turnover on his team which says a lot. He has planted what has become some of the best estates today in California all while building his own winery that is also one of the best.

- Editorial Standards
- Reprints & Permissions

IMAGES
COMMENTS
Other studies are looking more closely at how the connection between heart disease and Alzheimer's works at the molecular level. The goal is to find new potential medicines for Alzheimer's. Lifestyle choices. Research suggests that lifestyle choices with known heart benefits may help prevent Alzheimer's disease or delay its onset.
Susan, who is 70, began showing signs of Alzheimer's about four years ago. So she enrolled in a clinical trial of Leqembi at Washington University in St. Louis and has been receiving the drug ever ...
Researchers say we appear to be at the start of a new era for Alzheimer's treatment. Trial results published in January showed that for the first time a drug has been able to slow the cognitive decline characteristic of the disease. The drug, lecanemab, is a monoclonal antibody that works by binding to a key protein linked to the malady ...
November 08, 2022. Alzheimer's Disease. NIH has released Advancing Alzheimer's Disease and Related Dementias Research for All Populations: Prevent. Diagnose. Treat. Care. (PDF, 17M), a 2022 scientific progress report. The report features science advances and related efforts made between March 2021 and early 2022 in areas including drug ...
A new Alzheimer's drug slowed cognitive decline by 35%, according to late-stage trial results, raising the prospect of a second effective treatment for the disease. Donanemab met all goals of ...
In a new study, researchers at MIT showed that they "were able to interfere with an enzyme typically found to be overactive in the brains of Alzheimer's patients," reports Alex Mitchell for The New York Post.After using a peptide to treat the overactive enzyme, they found that "the peptide shows protective effects against loss of neurons and also appears to be able to rescue some of ...
Alzheimer's disease (AD) is the leading cause of dementia, presenting a significant unmet medical need worldwide. The pathogenesis of AD involves various pathophysiological events, including the accumulation of amyloid and tau, neuro-inflammation, and neuronal injury. Clinical trials focusing on new drugs for AD were documented in 2020, but subsequent developments have emerged since then.
Anne Trafton. June 27, 2023. A pair of structures in the hypothalamus called the mammillary bodies (highlighted in green) are among the first brain regions to show neurodegeneration in Alzheimer ...
What thrilled Sperling, who won the award for her work on clinical trials of Alzheimer's treatments, was a sense of hope, which has been conspicuously missing from research into the disease for ...
Credit: Science Photo Library. Some researchers are celebrating this week's announcement that a drug candidate for Alzheimer's disease slowed the rate of cognitive decline for people in a ...
The research team — located at Emory University School of Medicine, part of the Accelerating Medicines Partnership® Program for Alzheimer's Disease (AMP®-AD) Consortium — used advanced automated techniques to compare the levels of both proteins and RNA molecules in more than 1,000 brain tissue samples. The samples came from the ...
NIH has released Advancing Alzheimer's Disease and Related Dementias Research for All Populations: Prevent.Diagnose. Treat. Care. (PDF, 17M), a 2022 scientific progress report. The report features science advances and related efforts made between March 2021 and early 2022 in areas including drug development, lifestyle interventions, biomarker research, and more.
A new NIH intramural dementia research center designed to further accelerate a broad range of scientific discovery; FY 24 bypass budget. This year's progress report was preceded by the Fiscal Year 2024 Professional Judgment Budget for Alzheimer's Disease and Related Dementias announced in late July.
In 2022, multiple research milestones have occurred in the field of dementia. Therapeutics went through a fundamental transition, with amyloid-β (Aβ) targeted drugs gradually moving from clinical trials into real-world application. Encouraging findings on biomarkers and risk factors also marked the ongoing shift towards precise diagnosis and early prevention. We believe that this progress ...
Abstract. Alzheimer disease (AD) is the most common contributor to dementia in the world, but strategies that slow or prevent its clinical progression have largely remained elusive, until recently ...
Research and Progress This is a time of unprecedented promise in the quest to end Alzheimer's. Today, we are growing philanthropic support for Alzheimer's research, fostering a dynamic community of Alzheimer's scientists and securing increased federal funding for research - all of which are instrumental to finding new treatments to stop, slow and prevent Alzheimer's disease.
Alzheimer's researchers are looking beyond plaques and tangles for new treatments. Scientists say research into Alzheimer's needs to take a broader view of how the disease affects the brain ...
Of the many compounds in NIH-supported drug development programs for Alzheimer's and related dementias, 18 new dementia drug candidates have now matured through the pipeline, from discovery in the lab all the way through preclinical development, to reach the stage of human testing. ... Challenges for the Alzheimer's Research Community Even ...
Alzheimer's and dementia research - find the latest information on research funding, grants, clinical trials and global research news. Get information and resources for Alzheimer's and other dementias from the Alzheimer's Association. Call our 24 hours, seven days a week helpline at 800.272.3900.
Instead, she lived dementia-free into her 70s, and now her brain is yielding important clues about the pathology of dementia and possible treatments for Alzheimer's disease. As researchers at Massachusetts General Hospital and other centers first described in 2019, the woman, from Medellin, Colombia, was a member of an extended family with a ...
Scientists at the University of Leeds and Lancaster University in the UK have discovered a potential new target for Alzheimer's disease treatment - PDE4B.. Alzheimer's disease is the leading cause of dementia and disability in old age. As the number of people diagnosed with Alzheimer's disease is on the increase, new treatments are urgently needed to improve the quality of life for ...
Alzheimer's disease is the leading cause of dementia and disability in old age. ... can restore memory and cognitive function in mice that display symptoms of Alzheimer's disease, new research has ...
New Thematic Series - AI in Dementia. ... Alzheimer's Research & Therapy is the major forum for translational research into Alzheimer's disease. An international peer-reviewed journal, it publishes open access basic research with a translational focus, as well as clinical trials, research into drug discovery and development, and epidemiologic ...
Total payments in 2022 for health care, long-term care and hospice services for people age 65 and older with dementia are estimated to be $321 billion. A recent survey commissioned by the Alzheimer's Association revealed several barriers to consumers' understanding of MCI. The survey showed low awareness of MCI among Americans, a reluctance ...
A new report estimates 6.9 million older Americans are living with Alzheimer's disease in 2024, an increase of about 200,000 cases of the mind-robbing disease from 2023 and "a significant public ...
A test for Alzheimer's-disease stage predicts dementia risk Levels of a host of molecules in the cerebrospinal fluid reliably assess development of the disease. Research Highlights 26 Mar 2024 ...
Targeting toxic proteins in the brain, the jab aims to remove the harmful chemicals before they can cause damage and lead to the most common form of dementia, Alzheimer's. Alzheimer's affects roughly 540,000 people in the UK but this number is expected to rise to almost 1 million people by 2040.
In a new study published in Alzheimer's & Dementia: The Journal of the Alzheimer's Association, ... Research reported in this news release was supported by the Marcus Family Foundation and National Institutes of Health under award numbers NIH-NIA R01AG080093, R01AG062588, R01AG057234, P30AG062422, P01AG019724, U19AG079774, NIH-NINDS U54NS123985 ...
A 2020 Lancet report on dementia found that a dozen modifiable risk factors such as hypertension, hearing impairment, smoking and obesity together account for up to 40 percent of dementia cases ...
Ten years ago Kerrin Laz learned her mother had early-onset Alzheimer's disease. Alzheimer's disease affects almost 7 million people in the U.S. and nearly 60 million worldwide. While we all ...