Internet Explorer is no longer supported by Microsoft. To browse the NIHR site please use a modern, secure browser like Google Chrome, Mozilla Firefox, or Microsoft Edge.


How to disseminate your research

Published: 01 January 2019
Version: Version 1.0 - January 2019
This guide is for researchers who are applying for funding or have research in progress. It is designed to help you to plan your dissemination and give your research every chance of being utilised.
What does NIHR mean by dissemination?
Effective dissemination is simply about getting the findings of your research to the people who can make use of them, to maximise the benefit of the research without delay.
Research is of no use unless it gets to the people who need to use it
Professor Chris Whitty, Chief Scientific Adviser for the Department of Health
Principles of good dissemination
Stakeholder engagement: Work out who your primary audience is; engage with them early and keep in touch throughout the project, ideally involving them from the planning of the study to the dissemination of findings. This should create ‘pull’ for your research i.e. a waiting audience for your outputs. You may also have secondary audiences and others who emerge during the study, to consider and engage.
Format: Produce targeted outputs that are in an appropriate format for the user. Consider a range of tailored outputs for decision makers, patients, researchers, clinicians, and the public at national, regional, and/or local levels as appropriate. Use plain English which is accessible to all audiences.
Utilise opportunities: Build partnerships with established networks; use existing conferences and events to exchange knowledge and raise awareness of your work.
Context: Understand the service context of your research, and get influential opinion leaders on board to act as champions. Timing: Dissemination should not be limited to the end of a study. Consider whether any findings can be shared earlier
Remember to contact your funding programme for guidance on reporting outputs .
Your dissemination plan: things to consider
What do you want to achieve, for example, raise awareness and understanding, or change practice? How will you know if you are successful and made an impact? Be realistic and pragmatic.
Identify your audience(s) so that you know who you will need to influence to maximise the uptake of your research e.g. commissioners, patients, clinicians and charities. Think who might benefit from using your findings. Understand how and where your audience looks for/receives information. Gain an insight into what motivates your audience and the barriers they may face.
Remember to feedback study findings to participants, such as patients and clinicians; they may wish to also participate in the dissemination of the research and can provide a powerful voice.
When will dissemination activity occur? Identify and plan critical time points, consider external influences, and utilise existing opportunities, such as upcoming conferences. Build momentum throughout the entire project life-cycle; for example, consider timings for sharing findings.
Think about the expertise you have in your team and whether you need additional help with dissemination. Consider whether your dissemination plan would benefit from liaising with others, for example, NIHR Communications team, your institution’s press office, PPI members. What funds will you need to deliver your planned dissemination activity? Include this in your application (or talk to your funding programme).
Partners / Influencers: think about who you will engage with to amplify your message. Involve stakeholders in research planning from an early stage to ensure that the evidence produced is grounded, relevant, accessible and useful.
Messaging: consider the main message of your research findings. How can you frame this so it will resonate with your target audience? Use the right language and focus on the possible impact of your research on their practice or daily life.
Channels: use the most effective ways to communicate your message to your target audience(s) e.g. social media, websites, conferences, traditional media, journals. Identify and connect with influencers in your audience who can champion your findings.
Coverage and frequency: how many people are you trying to reach? How often do you want to communicate with them to achieve the required impact?
Potential risks and sensitivities: be aware of the relevant current cultural and political climate. Consider how your dissemination might be perceived by different groups.
Think about what the risks are to your dissemination plan e.g. intellectual property issues. Contact your funding programme for advice.
More advice on dissemination
We want to ensure that the research we fund has the maximum benefit for patients, the public and the NHS. Generating meaningful research impact requires engaging with the right people from the very beginning of planning your research idea.
More advice from the NIHR on knowledge mobilisation and dissemination .
What you need to know about research dissemination
Last updated
5 March 2024
Reviewed by
In this article, we'll tell you what you need to know about research dissemination.
- Understanding research dissemination
Research that never gets shared has limited benefits. Research dissemination involves sharing research findings with the relevant audiences so the research’s impact and utility can reach its full potential.
When done effectively, dissemination gets the research into the hands of those it can most positively impact. This may include:
Politicians
Industry professionals
The general public
What it takes to effectively disseminate research will depend greatly on the audience the research is intended for. When planning for research dissemination, it pays to understand some guiding principles and best practices so the right audience can be targeted in the most effective way.
- Core principles of effective dissemination
Effective dissemination of research findings requires careful planning. Before planning can begin, researchers must think about the core principles of research dissemination and how their research and its goals fit into those constructs.
Research dissemination principles can best be described using the 3 Ps of research dissemination.
This pillar of research dissemination is about clarifying the objective. What is the goal of disseminating the information? Is the research meant to:
Persuade policymakers?
Influence public opinion?
Support strategic business decisions?
Contribute to academic discourse?
Knowing the purpose of sharing the information makes it easy to accurately target it and align the language used with the target audience.
The process includes the methods that will be used and the steps taken when it comes time to disseminate the findings. This includes the channels by which the information will be shared, the format it will be shared in, and the timing of the dissemination.
By planning out the process and taking the time to understand the process, researchers will be better prepared and more flexible should changes arise.
The target audience is whom the research is aimed at. Because different audiences require different approaches and language styles, identifying the correct audience is a huge factor in the successful dissemination of findings.
By tailoring the research dissemination to the needs and preferences of a specific audience, researchers increase the chances of the information being received, understood, and used.
- Types of research dissemination
There are many options for researchers to get their findings out to the world. The type of desired dissemination plays a big role in choosing the medium and the tone to take when sharing the information.
Some common types include:
Academic dissemination: Sharing research findings in academic journals, which typically involves a peer-review process.
Policy-oriented dissemination: Creating documents that summarize research findings in a way that's understandable to policymakers.
Public dissemination: Using television and other media outlets to communicate research findings to the public.
Educational dissemination: Developing curricula for education settings that incorporate research findings.
Digital and online dissemination: Using digital platforms to present research findings to a global audience.
Strategic business presentation: Creating a presentation for a business group to use research insights to shape business strategy
- Major components of information dissemination
While the three Ps provide a convenient overview of what needs to be considered when planning research dissemination, they are not a complete picture.
Here’s a more comprehensive list of what goes into the dissemination of research results:
Audience analysis : Identifying the target audience and researching their needs, preferences, and knowledge level so content can be tailored to them.
Content development: Creating the content in a way that accurately reflects the findings and presents them in a way that is relevant to the target audience.
Channel selection: Choosing the channel or channels through which the research will be disseminated and ensuring they align with the preferences and needs of the target audience.
Timing and scheduling: Evaluating factors such as current events, publication schedules, and project milestones to develop a timeline for the dissemination of the findings.
Resource allocation: With the basics mapped out, financial, human, and technological resources can be set aside for the project to facilitate the dissemination process.
Impact assessment and feedback: During the dissemination, methods should be in place to measure how successful the strategy has been in disseminating the information.
Ethical considerations and compliance: Research findings often include sensitive or confidential information. Any legal and ethical guidelines should be followed.
- Crafting a dissemination blueprint
With the three Ps providing a foundation and the components outlined above giving structure to the dissemination, researchers can then dive deeper into the important steps in crafting an impactful and informative presentation.
Let’s take a look at the core steps.
1. Identify your audience
To identify the right audience for research dissemination, researchers must gather as much detail as possible about the different target audience segments.
By gathering detailed information about the preferences, personalities, and information-consumption habits of the target audience, researchers can craft messages that resonate effectively.
As a simple example, academic findings might be highly detailed for scholarly journals and simplified for the general public. Further refinements can be made based on the cultural, educational, and professional background of the target audience.
2. Create the content
Creating compelling content is at the heart of effective research dissemination. Researchers must distill complex findings into a format that's engaging and easy to understand. In addition to the format of the presentation and the language used, content includes the visual or interactive elements that will make up the supporting materials.
Depending on the target audience, this may include complex technical jargon and charts or a more narrative approach with approachable infographics. For non-specialist audiences, the challenge is to provide the required information in a way that's engaging for the layperson.
3. Take a strategic approach to dissemination
There's no single best solution for all research dissemination needs. What’s more, technology and how target audiences interact with it is constantly changing. Developing a strategic approach to sharing research findings requires exploring the various methods and channels that align with the audience's preferences.
Each channel has a unique reach and impact, and a particular set of best practices to get the most out of it. Researchers looking to have the biggest impact should carefully weigh up the strengths and weaknesses of the channels they've decided upon and craft a strategy that best uses that knowledge.
4. Manage the timeline and resources
Time constraints are an inevitable part of research dissemination. Deadlines for publications can be months apart, conferences may only happen once a year, etc. Any avenue used to disseminate the research must be carefully planned around to avoid missed opportunities.
In addition to properly planning and allocating time, there are other resources to consider. The appropriate number of people must be assigned to work on the project, and they must be given adequate financial and technological resources. To best manage these resources, regular reviews and adjustments should be made.
- Tailoring communication of research findings
We’ve already mentioned the importance of tailoring a message to a specific audience. Here are some examples of how to reach some of the most common target audiences of research dissemination.
Making formal presentations
Content should always be professional, well-structured, and supported by data and visuals when making formal presentations. The depth of information provided should match the expertise of the audience, explaining key findings and implications in a way they'll understand. To be persuasive, a clear narrative and confident delivery are required.
Communication with stakeholders
Stakeholders often don't have the same level of expertise that more direct peers do. The content should strike a balance between providing technical accuracy and being accessible enough for everyone. Time should be taken to understand the interests and concerns of the stakeholders and align the message accordingly.
Engaging with the public
Members of the public will have the lowest level of expertise. Not everyone in the public will have a technical enough background to understand the finer points of your message. Try to minimize confusion by using relatable examples and avoiding any jargon. Visual aids are important, as they can help the audience to better understand a topic.
- 10 commandments for impactful research dissemination
In addition to the details above, there are a few tips that researchers can keep in mind to boost the effectiveness of dissemination:
Master the three Ps to ensure clarity, focus, and coherence in your presentation.
Establish and maintain a public profile for all the researchers involved.
When possible, encourage active participation and feedback from the audience.
Use real-time platforms to enable communication and feedback from viewers.
Leverage open-access platforms to reach as many people as possible.
Make use of visual aids and infographics to share information effectively.
Take into account the cultural diversity of your audience.
Rather than considering only one dissemination medium, consider the best tool for a particular job, given the audience and research to be delivered.
Continually assess and refine your dissemination strategies as you gain more experience.
Should you be using a customer insights hub?
Do you want to discover previous research faster?
Do you share your research findings with others?
Do you analyze research data?
Start for free today, add your research, and get to key insights faster
Editor’s picks
Last updated: 18 April 2023
Last updated: 27 February 2023
Last updated: 6 February 2023
Last updated: 5 February 2023
Last updated: 16 April 2023
Last updated: 9 March 2023
Last updated: 30 April 2024
Last updated: 12 December 2023
Last updated: 11 March 2024
Last updated: 4 July 2024
Last updated: 6 March 2024
Last updated: 5 March 2024
Last updated: 13 May 2024
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next, log in or sign up.
Get started for free
- Reserve a study room
- Library Account
- Undergraduate Students
- Graduate Students
- Faculty & Staff
Create a Research Dissemination Plan
- Research Dissemination
Dissemination and exploitation of research results
Strategy, documents, tools and opportunities related to disseminating and exploiting research project results.
What is dissemination and exploitation?
Every year researchers funded by the European Union produce a substantial number of research results. For these results to benefit society, they must be made available to the relevant people and used to generate further impact.
Dissemination and exploitation are 2 key activities to
- diffuse knowledge
- increase the uptake of research and innovation project results in the EU
- demonstrate the generated impact of the projects funded
Dissemination
The public disclosure of the results not only by scientific publications but via any pertinent medium. Dissemination means making results available to the people that can best make use of them e.g. scientific community, industry, other commercial players, policymakers, and more.
Dissemination helps to explain the wider relevance of science to society, build support for future research and innovation funding, ensure the uptake of results within the scientific community, and open up potential business opportunities for novel products or services.
Exploitation
The use of results in developing, creating and marketing or improving a product or process, or in creating and providing a service in standardisation activities or shaping a policy.
Exploitation can be commercial, societal, political, or aimed at improving public knowledge and action. It also includes recommendations for policy making through feedback to policy project partners or facilitating uptake by others e.g. through making results available under open licences.
Exploitation focuses on the actual use of the results, translating research concepts into concrete solutions that have a positive impact on the public's quality of life.
Focus on project results
The focus of the dissemination and exploitation policy is on the results, i.e. all output generated by the project during its implementation.
These may include know-how, innovative solutions, algorithms, proof of feasibility, new business models, policy recommendations, guidelines, prototypes, demonstrators, databases and datasets, trained researchers, new infrastructures, networks, etc.
The results have the potential to be either commercially exploited, e.g. products or services, or lay the foundation for further research, work for policy making or innovation, e.g. novel knowledge, insights, technologies, methods, data, and more.
The European Commission designed and is implementing a dissemination and exploitation strategy to support funding beneficiaries taking their results a step further e.g. market uptake, wider scientific use, advice for policymaking, etc.
The Commission supports this by
- offering free tailor-made dissemination and exploitation support services
- providing the tools aimed at increasing visibility and recognition of successful results
- putting forward a Commission-wide scheme to collect and utilise results relevant to policy making i.e. Feedback to Policy framework
Objectives of the strategy
- guide and train applicants and beneficiaries, by offering dissemination and exploitation capacity building activities
- motivate beneficiaries, with incentives to scale up their results
- support beneficiaries by offering targeted services, including on Intellectual Property Management
- synergise with other EU programmes and initiatives
In line with the new European Research Area , the dissemination and exploitation strategy sets the vision of making Horizon Europe a global reference for transforming research and innovation results into scientific, economic and societal value.
The dissemination and exploitation strategy aims to accompany beneficiaries along their dissemination and exploitation journey support them through an integrated ecosystem of services, and bring them closer to relevant stakeholders.
Further activities are foreseen to meet the aforementioned objectives while delivering on the unique aspects of Horizon Europe, such as the EU Missions , as well as on cross-cutting priorities, like the Widening participation and Spreading excellence .
Legal obligations
Beneficiaries of the EU's research and innovation framework programmes are legally obliged to disseminate and exploit results.
Horizon Europe
Horizon Europe is the successor to Horizon 2020. It runs from 2021 to 2027.
Exploitation and Dissemination remains an obligation under article 39 of the regulation establishing Horizon Europe.
Article 39: Exploitation and dissemination
Horizon 2020
Horizon 2020 was the research and innovation funding programme until 2020.
As stated in the rules for participation and articles 28 and 29 it is an obligation for the beneficiaries to plan and implement the dissemination and exploitation of the project results.
Article 28: exploitation of results / Article 29: dissemination of results
Online events
Dissemination & Exploitation
This session introduces you to the Dissemination & Exploitation Strategy, highlighting the role of the Horizon Results Platform, Horizon Dashboard, CORDIS, and the Horizon Results Booster, as well as testimonials from EU-funded projects.
Watch video
Horizon Results Booster
This info session covers information about the services and includes testimonials from those who have already benefited from Horizon Results Booster support.
Horizon Results Platform:
Discover how the European Commission's Horizon Results Platform (HRP) promotes EU R&I innovative solution(s) to third parties: the investor community, partners, policy makers and other actors that can help promote project results to the right audience.
Guidance documents
- Online Manual
- Programme Guide
- AGA – Annotated Grant Agreement, art 16 and Annex
- Your guide to Intellectual Property in Horizon 2020
- How to make full use of the results of your Horizon 2020 project
- AGA- Annotated Grant Agreement, art 28 and art 29
Data and statistics
An interactive and user-friendly knowledge platform offering data and statistics on research programmes. It can be used to produce statistics and analysis on topics, countries, organisations and sectors, individual projects and beneficiaries.
Online repository of all EU-funded research projects and their results. It provides project factsheets, Horizon 2020 reports and deliverables and highlights results in multilingual articles and thematic publications for specialised audiences.
Other tools and opportunities
A package of free-of-charge specialised consultancy services for framework programme beneficiaries to support them in their dissemination and exploitation activities. The services include portfolio dissemination and exploitation strategy, business plan development and go-to-market guidance.
An online platform that hosts and promotes research results and bridges the gap between the research results and generating value for economy and society. Beneficiaries are able to address their targeted audiences and express their specific exploitation needs. External visitors are able to use the various search criteria in order to identify the results of relevance to their activities.
Access to the aggregated information on the Horizon 2020 and Interreg programmes, specifically taking into account potential synergies by analysing thematic priorities and regional participation.
A policy tool that helps to identify high potential innovations and innovators in EU-funded research and innovation projects.
Intellectual property (IP) service providing free-of-charge support to help European SMEs and beneficiaries of EU-funded research projects manage their IP in the context of transnational business or EU research and innovation programmes.
A tailored, free-of-charge, first-line Intellectual Property (IP) support service provided by the European Commission. It is specifically designed to help European start-ups and other SMEs involved in EU-funded collaborative research projects to efficiently manage and valorise IP in collaborative R&I efforts.
Recognition
Horizon Impact Award (HIA)
An initiative to recognise and celebrate outstanding projects that have used their results to provide value for society. The award aims to show the wider socio-economic benefits of EU investment in research and innovation. It also enables individuals or teams to showcase their best practices and achievements and aspires to encourage other beneficiaries to use and manage their results in the best way possible.
Other EU awards

Includes the actions HRP is undertaking to reflect our aim (e.g. increase the number of collaborations, mention existing collaborations and projects helped).
Related links
Horizon Europe The EU's research and innovation funding programme 2021-2027
Share this page
Designing A Dissemination Strategy: Turning Evidence Into Action

Introduction
At Evidence for Action (E4A), our mission is to support research that contributes to real-world advances in health and racial equity. The essence of action-oriented research is disseminating the findings in meaningful ways to decision-makers, communities, and others who can drive action to advance health and racial equity.
At E4A, we define dissemination as the targeted sharing of relevant information with specific audiences for a specific purpose, with an opportunity for bi-directional knowledge exchange . Dissemination is most effective when there is a clear strategy that lays out the who, what, when, why, and how of sharing the findings.
Building a Dissemination Strategy
To aid E4A applicants and other researchers in developing a plan for disseminating their findings, we’ve put together a dissemination strategy template ( access the Google doc version ). The template is structured in such a way to guide folks through a step-by-step process from identifying objectives to selecting communications tactics and materials. Each component should flow into the next. The different components of the template and key considerations for completing each one are outlined below.
Dissemination Objectives
Establishing your objectives for disseminating your work sets the stage for the rest of your strategy. Essentially this boils down to, why are you doing the research? What changes are you hoping to see in the world because you did this research? These objectives can be to inform development or implementation of policies or practices or to build the evidence base, for example. The objectives should be realistic, timely, and aligned with stakeholder priorities and needs. There should be concrete ways to determine whether you’re making progress toward achieving them.
Who needs to know about your findings in order to achieve your objectives? These individuals or groups will be your primary audiences, the individuals who will use the evidence to make decisions and work to advance health and racial equity. In addition to the people who have direct decision-making power, you should also consider who influences their decision-making. For example, if you’re trying to affect local or state policymaking, audiences that have sway with the policymakers might include advocacy organizations, local media outlets that can broadly share the findings and increase public awareness, community based organizations, and specific segments of the general public. People most likely to be impacted by the topic or intervention of interest should always be a priority audience.
It’s also important to keep in mind that audience groups are not monolithic; they are composed of individuals who may have different priorities, values, perspectives, interests, and other attributes. This may mean that the methods you use to engage with them or the messages you convey to them should be tailored to different segments of the broader audience.
Desired Actions
What are you asking audience members to do? These actions can range from retweeting a social media post to using the evidence in their policy- or decision-making. Questions to consider when determining the desired actions for members of each audience include, does the action align with their values? Do they have the authority and ability to do what you’re asking? Is what you’re asking them to do reasonable? If you’re not sure about the answers to these questions, you should work to learn more about the audiences you’ve identified. The best way to learn about your audiences is to engage with members of those audiences early and often. In addition to enhancing your dissemination strategy and activity, engaging with the end users of your findings may inform aspects of the research itself, from developing research questions to interpreting the data and disseminating the findings.
Relationship Building Tactics
Building relationships allows you to learn more about your audiences, and the more you know about them, the more effective your outreach and engagement will be. You’ll have a better sense of where they get their information, who they trust, what their values are, and what messages and which messengers are most likely to resonate with them. Additionally, the more your audiences know about you, the more likely they will be to engage with you, trust you, and undertake what you’re asking them to do.
Communications Tactics
How will you engage with each audience? Some of the questions you’ll need to answer to figure out the best tactics are: where do members of this audience acquire information? What sources do they trust? Example communications tactics include, but are in no way limited to, posts to social media channels, emails, phone calls, text messages, websites, podcasts, and op-eds (these last three can be considered both Communications Tactics and Supplemental Materials, because they can be sent to audiences as part of other communications). This shouldn’t be a one-size-fits all approach for different audiences or even individuals within an audience. For example, if we are trying to reach federal policymakers we might conduct a targeted email campaign that includes key staffers, make appointments for in person meetings, or place a piece in a publication such as The Hill. If we’re trying to reach high school students, a video to YouTube or a story on Instagram might be more effective.
Supplemental Materials
Supplemental materials are the resources we put together for audiences to convey the key findings of the research in ways that are engaging, easy to understand, and relevant to them. These resources are vital to help individuals understand the findings and implications and to give credence to them. Examples of supplemental materials include data visualizations (e.g., maps, graphs, etc.), policy or research briefs, one-pagers, toolkits or implementation guides, short- or long-form videos, case studies, GIFs, press releases, and academic journal articles. Similar to the tactics, the materials and information you provide each audience or segments of each audience are not likely to be the same. For instance, while emailing an academic journal article to your colleague in a similar discipline may be sufficient, that would not be advisable for almost any other audience. Journal articles are often long and include jargon and too much detail, making it challenging to read and understand the implications for real world decision-making. If you’re reaching out to policymakers and advocacy organizations, a policy brief may be much more effective than if you’re reaching out to practitioners, student groups, or members of the “general public.” The materials used will also depend on the communication tactic you are using. For example, videos and GIFs may be very effective via social media, but may not be very effective for in-person meetings or town hall events.
What’s Next?
Completing the dissemination strategy template is a great starting point, but the real work starts when it comes to implementation. While specific communication tactics and materials may need to wait for research findings or until academic journal publication, there are other things you can get started on in the meantime. It’s never too soon to start learning more about your audiences and building relationships. You can also build the foundations for some of your tactics, such as developing distribution lists, establishing yourself or your organization on the social media channels you plan to use, and building your team’s capacity to implement some aspects of your plan.
One last piece of advice, dissemination strategies are not meant to be set in stone. Try to be flexible. Things may change with your projects, you may identify new or different audiences, things may happen in the world that impact your research or the application of your findings. It’s a good idea to revisit your plan regularly and update it as needed.
If you would like to learn more about developing and implementing a dissemination plan, check out the video guide I put together. Still have questions? Reach out to E4A on Twitter or LinkedIn.
Tools & Resources
- The E4A Dissemination Strategy Template
- Developing A Dissemination Strategy: A Video Guide by Steph Chernitskiy ( Access the Full Transcript )
- Request a Workshop
About the author(s)
Steph Chernitskiy (she/her) is the E4A Communications Manager. She manages the external communications for Evidence for Action, and works closely with grantees on findings dissemination. She is a frequent contributor to the E4A Methods Blog.
Additional Resources
Access a Video Tutorial ( Full Transcript ) Access the E4A Dissemination Strategy Template
- Systematic Review
- Open access
- Published: 22 November 2010
Disseminating research findings: what should researchers do? A systematic scoping review of conceptual frameworks
- Paul M Wilson 1 ,
- Mark Petticrew 2 ,
- Mike W Calnan 3 &
- Irwin Nazareth 4
Implementation Science volume 5 , Article number: 91 ( 2010 ) Cite this article
87k Accesses
137 Citations
20 Altmetric
Metrics details
Addressing deficiencies in the dissemination and transfer of research-based knowledge into routine clinical practice is high on the policy agenda both in the UK and internationally.
However, there is lack of clarity between funding agencies as to what represents dissemination. Moreover, the expectations and guidance provided to researchers vary from one agency to another. Against this background, we performed a systematic scoping to identify and describe any conceptual/organising frameworks that could be used by researchers to guide their dissemination activity.
We searched twelve electronic databases (including MEDLINE, EMBASE, CINAHL, and PsycINFO), the reference lists of included studies and of individual funding agency websites to identify potential studies for inclusion. To be included, papers had to present an explicit framework or plan either designed for use by researchers or that could be used to guide dissemination activity. Papers which mentioned dissemination (but did not provide any detail) in the context of a wider knowledge translation framework, were excluded. References were screened independently by at least two reviewers; disagreements were resolved by discussion. For each included paper, the source, the date of publication, a description of the main elements of the framework, and whether there was any implicit/explicit reference to theory were extracted. A narrative synthesis was undertaken.
Thirty-three frameworks met our inclusion criteria, 20 of which were designed to be used by researchers to guide their dissemination activities. Twenty-eight included frameworks were underpinned at least in part by one or more of three different theoretical approaches, namely persuasive communication, diffusion of innovations theory, and social marketing.
Conclusions
There are currently a number of theoretically-informed frameworks available to researchers that can be used to help guide their dissemination planning and activity. Given the current emphasis on enhancing the uptake of knowledge about the effects of interventions into routine practice, funders could consider encouraging researchers to adopt a theoretically-informed approach to their research dissemination.
Peer Review reports
Healthcare resources are finite, so it is imperative that the delivery of high-quality healthcare is ensured through the successful implementation of cost-effective health technologies. However, there is growing recognition that the full potential for research evidence to improve practice in healthcare settings, either in relation to clinical practice or to managerial practice and decision making, is not yet realised. Addressing deficiencies in the dissemination and transfer of research-based knowledge to routine clinical practice is high on the policy agenda both in the UK [ 1 – 5 ] and internationally [ 6 ].
As interest in the research to practice gap has increased, so too has the terminology used to describe the approaches employed [ 7 , 8 ]. Diffusion, dissemination, implementation, knowledge transfer, knowledge mobilisation, linkage and exchange, and research into practice are all being used to describe overlapping and interrelated concepts and practices. In this review, we have used the term dissemination, which we view as a key element in the research to practice (knowledge translation) continuum. We define dissemination as a planned process that involves consideration of target audiences and the settings in which research findings are to be received and, where appropriate, communicating and interacting with wider policy and health service audiences in ways that will facilitate research uptake in decision-making processes and practice.
Most applied health research funding agencies expect and demand some commitment or effort on the part of grant holders to disseminate the findings of their research. However, there does appear to be a lack of clarity between funding agencies as to what represents dissemination [ 9 ]. Moreover, although most consider dissemination to be a shared responsibility between those funding and those conducting the research, the expectations on and guidance provided to researchers vary from one agency to another [ 9 ].
We have previously highlighted the need for researchers to consider carefully the costs and benefits of dissemination and have raised concerns about the nature and variation in type of guidance issued by funding bodies to their grant holders and applicants [ 10 ]. Against this background, we have performed a systematic scoping review with the following two aims: to identify and describe any conceptual/organising frameworks designed to be used by researchers to guide their dissemination activities; and to identify and describe any conceptual/organising frameworks relating to knowledge translation continuum that provide enough detail on the dissemination elements that researchers could use it to guide their dissemination activities.
The following databases were searched to identify potential studies for inclusion: MEDLINE and MEDLINE In-Process and Other Non-Indexed Citations (1950 to June 2010); EMBASE (1980 to June 2010); CINAHL (1981 to June 2010); PsycINFO (1806 to June 2010); EconLit (1969 to June 2010); Social Services Abstracts (1979 to June 2010); Social Policy and Practice (1890 to June 2010); Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Cochrane Methodology Register, Database of Abstracts of Reviews of Effects, Health Technology Assessment Database, NHS Economic Evaluation Database (Cochrane Library 2010: Issue 1).
The search terms were identified through discussion by the research team, by scanning background literature, and by browsing database thesauri. There were no methodological, language, or date restrictions. Details of the database specific search strategies are presented Additional File 1 , Appendix 1.
Citation searches of five articles [ 11 – 15 ] identified prior to the database searches were performed in Science Citation Index (Web of Science), MEDLINE (OvidSP), and Google Scholar (February 2009).
As this review was undertaken as part of a wider project aiming to assess the dissemination activity of UK applied and public health researchers [ 16 ], we searched the websites of 10 major UK funders of health services and public health research. These were the British Heart Foundation, Cancer Research UK, the Chief Scientist Office, the Department of Health Policy Research Programme, the Economic and Social Research Council (ESRC), the Joseph Rowntree Foundation, the Medical Research Council (MRC), the NIHR Health Technology Assessment Programme, the NIHR Service Delivery and Organisation Programme and the Wellcome Trust. We aimed to identify any dissemination/communication frameworks, guides, or plans that were available to grant applicants or holders.
We also interrogated the websites of four key agencies with an established record in the field of dissemination and knowledge transfer. These were the Agency for Healthcare Research and Quality ( AHRQ ) , the Canadian Institutes of Health Research (CIHR), the Canadian Health Services Research Foundation (CHSRF), and the Centre for Reviews and Dissemination (CRD).
As a number of databases and websites were searched, some degree of duplication resulted. In order to manage this issue, the titles and abstracts of records were downloaded and imported into EndNote bibliographic software, and duplicate records removed.
References were screened independently by two reviewers; those studies that did not meet the inclusion criteria were excluded. Where it was not possible to exclude articles based on title and abstract alone, full text versions were obtained and their eligibility was assessed independently by two reviewers. Where disagreements occurred, the opinion of a third reviewer was sought and resolved by discussion and arbitration by a third reviewer.
To be eligible for inclusion, papers needed to either present an explicit framework or plan designed to be used by a researcher to guide their dissemination activity, or an explicit framework or plan that referred to dissemination in the context of a wider knowledge translation framework but that provided enough detail on the dissemination elements that a researcher could then use it. Papers that referred to dissemination in the context of a wider knowledge translation framework, but that did not describe in any detail those process elements relating to dissemination were excluded from the review. A list of excluded papers is included in Additional File 2 , Appendix 2.
For each included paper we recorded the publication date, a description of the main elements of the framework, whether there was any reference to other included studies, and whether there was an explicit theoretical basis to the framework. Included papers that did not make an explicit reference to an underlying theory were re-examined to determine whether any implicit use of theory could be identified. This entailed scrutinising the references and assessing whether any elements from theories identified in other papers were represented in the text. Data from each paper meeting the inclusion criteria were extracted by one researcher and independently checked for accuracy by a second.
A narrative synthesis [ 17 ] of included frameworks was undertaken to present the implicit and explicit theoretical basis of included frameworks and to explore any relationships between them.
Our searches identified 6,813 potentially relevant references (see Figure 1 ). Following review of the titles and abstracts, we retrieved 122 full papers for a more detailed screening. From these, we included 33 frameworks (reported in 44 papers) Publications that did not meet our inclusion criteria are listed in Additional File 2 , Appendix 2.
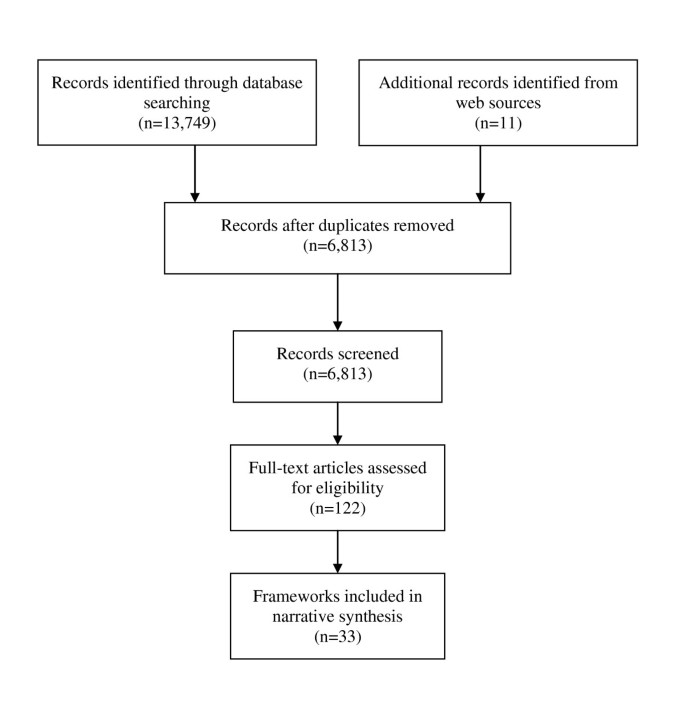
Identification of conceptual frameworks .
Characteristics of conceptual frameworks designed to be used by researchers
Table 1 summarises in chronological order, twenty conceptual frameworks designed for use by researchers [ 11 , 14 , 15 , 18 – 34 ]. Where we have described elements of frameworks that have been reported across multiple publications, these are referenced in the Table.
Theoretical underpinnings of dissemination frameworks
Thirteen of the twenty included dissemination frameworks were either explicitly or implicitly judged to be based on the Persuasive Communication Matrix [ 35 , 36 ]. Originally derived from a review of the literature of persuasion which sought to operationalise Lasswell's seminal description of persuasive communications as being about 'Who says what in which channel to whom with what effect' [ 37 ]. McGuire argued that there are five variables that influence the impact of persuasive communications. These are the source of communication, the message to be communicated, the channels of communication, the characteristics of the audience (receiver), and the setting (destination) in which the communication is received.
Included frameworks were judged to encompass either three [ 21 , 27 , 29 ], four [ 15 , 20 , 23 , 26 , 28 , 31 , 38 ], or all five [ 11 , 18 , 25 ] of McGuire's five input variables, namely, the source, channel, message, audience, and setting. The earliest conceptual model included in the review explicitly applied McGuire's five input variables to the dissemination of medical technology assessments [ 11 ]. Only one other framework (in its most recent version) explicitly acknowledges McGuire [ 17 ]; the original version acknowledged the influence of Winkler et al . on its approach to conceptualising systematic review dissemination [ 18 ]. The original version of the CRD approach [ 18 , 39 ] is itself referred to by two of the other eight frameworks [ 20 , 23 ]
Diffusion of Innovations theory [ 40 , 41 ] is explicitly cited by eight of the dissemination frameworks [ 11 , 17 , 19 , 22 , 24 , 28 , 29 , 34 ]. Diffusion of Innovations offers a theory of how, why, and at what rate practices or innovations spread through defined populations and social systems. The theory proposes that there are intrinsic characteristics of new ideas or innovations that determine their rate of adoption, and that actual uptake occurs over time via a five-phase innovation-decision process (knowledge, persuasion, decision, implementation, and confirmation). The included frameworks are focussed on the knowledge and persuasion stages of the innovation-decision process.
Two of the included dissemination frameworks make reference to Social Marketing [ 42 ]. One briefly discusses the potential application of social and commercial marketing and advertising principles and strategies in the promotion of non-commercial services, ideas, or research-based knowledge [ 22 ]. The other briefly argues that a social marketing approach could take into account a planning process involving 'consumer' oriented research, objective setting, identification of barriers, strategies, and new formats [ 30 ]. However, this framework itself does not represent a comprehensive application of social marketing theory and principles, and instead highlights five factors that are focussed around formatting evidence-based information so that it is clear and appealing by defined target audiences.
Three other distinct dissemination frameworks were included, two of which are based on literature reviews and researcher experience [ 14 , 32 ]. The first framework takes a novel question-based approach and aims to increase researchers' awareness of the type of context information that might prove useful when disseminating knowledge to target audiences [ 14 ]. The second framework presents a model that can be used to identify barriers and facilitators and to design interventions to aid the transfer and utilization of research knowledge [ 32 ]. The final framework is derived from Two Communities Theory [ 43 ] and proposes pragmatic strategies for communicating across conflicting cultures research and policy; it suggests a shift away from simple one-way communication of research to researchers developing collaborative relationships with policy makers [ 33 ].
Characteristics of conceptual frameworks relating to knowledge translation that could be used by researchers to guide their dissemination activities
Table 2 summarises in chronological order the dissemination elements of 13 conceptual frameworks relating to knowledge translation that could be used by researchers to guide their dissemination activities [ 13 , 44 – 55 ].
Only two of the included knowledge translation frameworks were judged to encompass four of McGuire's five variables for persuasive communications [ 45 , 47 ]. One framework [ 45 ] explicitly attributes these variables as being derived from Winkler et al [ 11 ]. The other [ 47 ] refers to strong direct evidence but does not refer to McGuire or any of the other included frameworks.
Diffusion of Innovations theory [ 40 , 41 ] is explicitly cited in eight of the included knowledge translation frameworks [ 13 , 45 – 49 , 52 , 56 ]. Of these, two represent attempts to operationalise and apply the theory, one in the context of evidence-based decision making and practice [ 13 ], and the other to examine how innovations in organisation and delivery of health services spread and are sustained in health service organisations [ 47 , 57 ]. The other frameworks are exclusively based on the theory and are focussed instead on strategies to accelerate the uptake of evidence-based knowledge and or interventions
Two of the included knowledge translation frameworks [ 50 , 53 ] are explicitly based on resource or knowledge-based Theory of the Firm [ 58 , 59 ]. Both frameworks propose that successful knowledge transfer (or competitive advantage) is determined by the type of knowledge to be transferred as well as by the development and deployment of appropriate skills and infrastructure at an organisational level.
Two of the included knowledge translation frameworks purport to be based upon a range of theoretical perspectives. The Coordinated Implementation model is derived from a range of sources, including theories of social influence on attitude change, the Diffusion of Innovations, adult learning, and social marketing [ 45 ]. The Practical, Robust Implementation and Sustainability Model was developed using concepts from Diffusion of Innovations, social ecology, as well as the health promotion, quality improvement, and implementation literature [ 52 ].
Three other distinct knowledge translation frameworks were included, all of which are based on a combination of literature reviews and researcher experience [ 44 , 51 , 54 ].
Conceptual frameworks provided by UK funders
Of the websites of the 10 UK funders of health services and public health research, only the ESRC made a dissemination framework available to grant applicants or holders (see Table 1 ) [ 26 ]. A summary version of another included framework is available via the publications section of the Joseph Rowntree Foundation [ 60 ]. However, no reference is made to it in the submission guidance they make available to research applicants.
All of the UK funding bodies made brief references to dissemination in their research grant application guides. These would simply ask applicants to briefly indicate how findings arising from the research will be disseminated (often stating that this should be other than via publication in peer-reviewed journals) so as to promote or facilitate take up by users in the health services.
This systematic scoping review presents to our knowledge the most comprehensive overview of conceptual/organising frameworks relating to research dissemination. Thirty-three frameworks met our inclusion criteria, 20 of which were designed to be used by researchers to guide their dissemination activities. Twenty-eight included frameworks that were underpinned at least in part by one or more of three different theoretical approaches, namely persuasive communication, diffusion of innovations theory, and social marketing.
Our search strategy was deliberately broad, and we searched a number of relevant databases and other sources with no language or publication status restrictions, reducing the chance that some relevant studies were excluded from the review and of publication or language bias. However, we restricted our searches to health and social science databases, and it is possible that searches targeting for example the management or marketing literature may have revealed additional frameworks. In addition, this review was undertaken as part of a project assessing UK research dissemination, so our search for frameworks provided by funding agencies was limited to the UK. It is possible that searches of funders operating in other geographical jurisdictions may have identified other studies. We are also aware that the way in which we have defined the process of dissemination and our judgements as to what constitutes sufficient detail may have resulted in some frameworks being excluded that others may have included or vice versa. Given this, and as an aid to transparency, we have included the list of excluded papers as Additional File 2 , Appendix 2 so as to allow readers to assess our, and make their own, judgements on the literature identified.
Despite these potential limitations, in this review we have identified 33 frameworks that are available and could be used to help guide dissemination planning and activity. By way of contrast, a recent systematic review of the knowledge transfer and exchange literature (with broader aims and scope) [ 61 ] identified five organising frameworks developed to guide knowledge transfer and exchange initiatives (defined as involving more than one way communications and involving genuine interaction between researchers and target audiences) [ 13 – 15 , 62 , 63 ]. All were identified by our searches, but only three met our specific inclusion criteria of providing sufficient dissemination process detail [ 13 – 15 ]. One reviewed methods for assessment of research utilisation in policy making [ 62 ], whilst the other reviewed knowledge mapping as a tool for understanding the many knowledge creation and translation resources and processes in a health system [ 63 ].
There is a large amount of theoretical convergence among the identified frameworks. This all the more striking given the wide range of theoretical approaches that could be applied in the context of research dissemination [ 64 ], and the relative lack of cross-referencing between the included frameworks. Three distinct but interlinked theories appear to underpin (at least in part) 28 of the included frameworks. There has been some criticism of health communications that are overly reliant on linear messenger-receiver models and do not draw upon other aspects of communication theory [ 65 ]. Although researcher focused, the included frameworks appear more participatory than simple messenger-receiver models, and there is recognition of the importance of context and emphasis on the key to successful dissemination being dependent on the need for interaction with the end user.
As we highlight in the introduction, there is recognition among international funders both of the importance of and their role in the dissemination of research [ 9 ]. Given the current political emphasis on reducing deficiencies in the uptake of knowledge about the effects of interventions into routine practice, funders could be making and advocating more systematic use of conceptual frameworks in the planning of research dissemination.
Rather than asking applicants to briefly indicate how findings arising from their proposed research will be disseminated (as seems to be the case in the UK), funding agencies could consider encouraging grant applicants to adopt a theoretically-informed approach to their research dissemination. Such an approach could be made a conditional part of any grant application process; an organising framework such as those described in this review could be used to demonstrate the rationale and understanding underpinning their proposed plans for dissemination. More systematic use of conceptual frameworks would then provide opportunities to evaluate across a range of study designs whether utilising any of the identified frameworks to guide research dissemination does in fact enhance the uptake of research findings in policy and practice.
There are currently a number of theoretically-informed frameworks available to researchers that could be used to help guide their dissemination planning and activity. Given the current emphasis on enhancing the uptake of knowledge about the effects of interventions into routine practice, funders could consider encouraging researchers to adopt a theoretically informed approach to their research dissemination.
Cooksey D: A review of UK health research funding. London: Stationery Office. 2006
Google Scholar
Darzi A: High quality care for all: NHS next stage review final report. 2008, London: Department of Health
Department of Health: Best Research for Best Health: A new national health research strategy. 2006, London: Department of Health
National Institute for Health Research: Delivering Health Research. National Institute for Health Research Progress Report 2008/09. London: Department of Health. 2009
Tooke JC: Report of the High Level Group on Clinical Effectiveness A report to Sir Liam Donaldson Chief Medical Officer. London: Department of Health. 2007
World Health Organization: World report on knowledge for better health: strengthening health systems. Geneva: World Health Organization. 2004
Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, Robinson N: Lost in knowledge translation: time for a map?. J Contin Educ Health Prof. 2006, 26: 13-24.
Article PubMed Google Scholar
World Health Organization: Bridging the 'know-do' gap: meeting on knowledge translation in global health 10-12 October 2005. 2005, Geneva: World Health Organization
Tetroe JM, Graham ID, Foy R, Robinson N, Eccles MP, Wensing M, Durieux P, Légaré F, Nielson CP, Adily A, Ward JE, Porter C, Shea B, Grimshaw JM: Health research funding agencies' support and promotion of knowledge translation: an international study. Milbank Q. 2008, 86: 125-55.
Article PubMed PubMed Central Google Scholar
Wilson PM, Petticrew M, Calnan MW, Nazareth I: Why promote the findings of single research studies?. BMJ. 2008, 336: 722-
Winkler JD, Lohr KN, Brook RH: Persuasive communication and medical technology assessment. Arch Intern Med. 1985, 145: 314-17.
Article CAS PubMed Google Scholar
Lomas J: Diffusion, Dissemination, and Implementation: Who Should Do What. Ann N Y Acad Sci. 1993, 703: 226-37.
Dobbins M, Ciliska D, Cockerill R, Barnsley J, DiCenso A: A framework for the dissemination and utilization of research for health-care policy and practice. Online J Knowl Synth Nurs. 2002, 9: 7-
PubMed Google Scholar
Jacobson N, Butterill D, Goering P: Development of a framework for knowledge translation: understanding user context. J Health Serv Res Policy. 2003, 8: 94-9.
Lavis JN, Robertson D, Woodside JM, McLeod CB, Abelson J, Knowledge Transfer Study G: How can research organizations more effectively transfer research knowledge to decision makers?. Milbank Q. 2003, 81: 221-48.
Wilson PM, Petticrew M, Calnan MW, Nazareth I: Does dissemination extend beyond publication: a survey of a cross section of public funded research in the UK. Implement Sci. 2010, 5: 61-
Centre for Reviews and Dissemination: Undertaking systematic reviews of research on effectiveness: CRD's guidance for carrying out or commissioning reviews. 2009, York: University of York, 3
NHS Centre for Reviews and Dissemination: Undertaking systematic reviews of research on effectiveness: CRD's guidance for carrying out or commissioning reviews. York: University of York. 1994
National Center for the Dissemination of Disability Research: A Review of the Literature on Dissemination and Knowledge Utilization. Austin, TX: National Center for the Dissemination of Disability Research, Southwest Educational Development Laboratory. 1996
Hughes M, McNeish D, Newman T, Roberts H, Sachdev D: What works? Making connections: linking research and practice. A review by Barnardo's Research and Development Team. Ilford: Barnardo's. 2000
Harmsworth S, Turpin S, TQEF National Co-ordination Team, Rees A, Pell G, Bridging the Gap Innovations Project: Creating an Effective Dissemination Strategy. An Expanded Interactive Workbook for Educational Development Projects. Centre for Higher Education Practice: Open University. 2001
Herie M, Martin GW: Knowledge diffusion in social work: a new approach to bridging the gap. Soc Work. 2002, 47: 85-95.
Scullion PA: Effective dissemination strategies. Nurse Res. 2002, 10: 65-77.
Farkas M, Jette AM, Tennstedt S, Haley SM, Quinn V: Knowledge dissemination and utilization in gerontology: an organizing framework. Gerontologist. 2003, 43 (Spec 1): 47-56.
Canadian Health Services Research Foundation: Communication Notes. Developing a dissemination plan Ottawa: Canadian Health Services Research Foundation. 2004
Economic and Social Research Council: Communications strategy: a step-by-step guide. Swindon: Economic and Social Research Council. 2004
European Commission. European Research: A guide to successful communication. 2004, Luxembourg: Office for Official Publications of the European Communities
Carpenter D, Nieva V, Albaghal T, Sorra J: Development of a Planning Tool to Guide Dissemination of Research Results. Advances in Patient Safety: From Research to Implementation, Programs, Tools and Practices. 2005, Rockville, MD: Agency for Healthcare Research and Quality, 4:
Bauman AE, Nelson DE, Pratt M, Matsudo V, Schoeppe S: Dissemination of physical activity evidence, programs, policies, and surveillance in the international public health arena. Am J Prev Med. 2006, 31 (1 Suppl): S57-S65.
Formoso G, Marata AM, Magrini N: Social marketing: should it be used to promote evidence-based health information?. Soc Sci Med. 2007, 64: 949-53.
Zarinpoush F, Sychowski SV, Sperling J: Effective Knowledge Transfer and Exchange: A Framework. Toronto: Imagine Canada. 2007
Majdzadeh R, Sadighi J, Nejat S, Mahani AS, Gholami J: Knowledge translation for research utilization: design of a knowledge translation model at Tehran University of Medical Sciences. J Contin Educ Health Prof. 2008, 28: 270-7.
Friese B, Bogenschneider K: The voice of experience: How social scientists communicate family research to policymakers. Fam Relat. 2009, 58: 229-43.
Yuan CT, Nembhard IM, Stern AF, Brush JE, Krumholz HM, Bradley EH: Blueprint for the dissemination of evidence-based practices in health care. Issue Brief (Commonw Fund). 2010, 86: 1-16.
McGuire WJ: The nature of attitudes and attitude change. Handbook of social psychology. Edited by: Lindzey G, Aronsen E. 1969, Reading, Mass: Addison-Wesley Publishing, 136-314.
McGuire WJ: Input and output variables currently promising for constructing persuasive communications. Public communication campaigns. Edited by: Rice R, Atkin C. 2001, Thousand Oaks, CA: Sage, 22-48. 3
Chapter Google Scholar
Lasswell HD: The structure and function of communication in society. The communication of ideas. Edited by: Bryson L. 1948, New York: Harper and Row, 37-51.
National Center for the Dissemination of Disability Research: Developing an Effective Dissemination Plan. 2001, Austin, Tx: Southwest Educational Development Laboratory (SEDL)
Freemantle N, Watt I: Dissemination: implementing the findings of research. Health Libr Rev. 1994, 11: 133-7.
Rogers EM: The diffusion of innovations. 1962, New York: Free Press
Rogers EM: Diffusion of innovations. 2003, New York, London: Free Press, 5
Kotler P, Zaltman G: Social Marketing: An Approach to Planned Social Change. J Market. 1971, 35: 3-12.
Article CAS Google Scholar
Caplan N: The two-communities theory and knowledge utilization. Am Behav Sci. 1979, 22: 459-70.
Article Google Scholar
Funk SG, Tornquist EM, Champagne MT: A model for improving the dissemination of nursing research. West J Nurs Res. 1989, 11: 361-72.
Lomas J: Teaching old (and not so old) docs new tricks: effective ways to implement research findings. 1993, CHEPA working paper series No 93-4. Hamiltion, Ont: McMaster University
Elliott SJ, O'Loughlin J, Robinson K, Eyles J, Cameron R, Harvey D, Raine K, Gelskey D, Canadian Heart Health Dissemination Project Strategic and Research Advisory Groups: Conceptualizing dissemination research and activity: the case of the Canadian Heart Health Initiative. Health Educ Behav. 2003, 30: 267-82.
Greenhalgh T, Robert G, Bate P, Macfarlane , Kyriakidou O, Peacock R: How to spread good ideas. A systematic review of the literature on diffusion, dissemination and sustainability of innovations in health service delivery and organisation. London: National Co-ordinating Centre for NHS Service Delivery and Organisation (NCCSDO). 2004
Green LW, Orleans C, Ottoson JM, Cameron R, Pierce JP, Bettinghaus EP: Inferring strategies for disseminating physical activity policies, programs, and practices from the successes of tobacco control. Am J Prev Med. 2006, 31 (1 Suppl): S66-S81.
Owen N, Glanz K, Sallis JF, Kelder SH: Evidence-based approaches to dissemination and diffusion of physical activity interventions. Am J Prev Med. 2006, 31 (1 Suppl): S35-S44.
Landry R, Amara N, Ouimet M: Determinants of Knowledge Transfer: Evidence from Canadian University Researchers in Natural Sciences and Engineering. J Technol Transfer. 2007, 32: 561-92.
Baumbusch JL, Kirkham SR, Khan KB, McDonald H, Semeniuk P, Tan E, Anderson JM: Pursuing common agendas: a collaborative model for knowledge translation between research and practice in clinical settings. Res Nurs Health. 2008, 31: 130-40.
Feldstein AC, Glasgow RE: A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf. 2008, 34: 228-43.
Clinton M, Merritt KL, Murray SR: Using corporate universities to facilitate knowledge transfer and achieve competitive advantage: An exploratory model based on media richness and type of knowledge to be transferred. International Journal of Knowledge Management. 2009, 5: 43-59.
Mitchell P, Pirkis J, Hall J, Haas M: Partnerships for knowledge exchange in health services research, policy and practice. J Health Serv Res Policy. 2009, 14: 104-11.
Ward V, House A, Hamer S: Developing a framework for transferring knowledge into action: a thematic analysis of the literature. J Health Serv Res Policy. 2009, 14: 156-64.
Ward V, Smith S, Carruthers S, House A, Hamer S: Knowledge Brokering. Exploring the process of transferring knowledge into action Leeds: University of Leeds. 2010
Greenhalgh T, Robert G, Macfarlane , Bate P, Kyriakidou O: Diffusion of innovations in service organizations: systematic review and recommendations. Millbank Q. 2004, 82: 581-629.
Wernerfelt B: A resource-based view of the firm. Strategic Manage J. 1984, 5: 171-80.
Grant R: Toward a knowledge-based theory of the firm. Strategic Manage J. 1996, 17: 109-22.
Joseph Rowntree Foundation: Findings: Linking research and practice. York: Joseph Rowntree Foundation. 2000
Mitton C, Adair CE, McKenzie E, Patten SB, Waye Perry B: Knowledge transfer and exchange: review and synthesis of the literature. Milbank Q. 2007, 85: 729-68.
Hanney S, Gonzalez-Block M, Buxton M, Kogan M: The utilisation of health research in policy-making: concepts, examples and methods of assessment. Health Res Policy Syst. 2003, 1: 2-
Ebener S, Khan A, Shademani R, Compernolle L, Beltran M, Lansang M, Lippman M: Knowledge mapping as a technique to support knowledge translation. Bull World Health Organ. 2006, 84: 636-42.
Article CAS PubMed PubMed Central Google Scholar
Grol R, Bosch M, Hulscher M, Eccles M, Wensing M: Planning and studying improvement in patient care: the use of theoretical perspectives. Milbank Q. 2007, 85: 93-138.
Kuruvilla S, Mays N: Reorienting health-research communication. Lancet. 2005, 366: 1416-18.
Download references
Acknowledgements
This review was undertaken as part of a wider project funded by the MRC Population Health Sciences Research Network (Ref: PHSRN 11). The views expressed in this paper are those of the authors alone.
Author information
Authors and affiliations.
Centre for Reviews and Dissemination, University of York, YO10 5DD, UK
Paul M Wilson
Social and Environmental Health Department, London School of Hygiene and Tropical Medicine, WC1E 7HT, UK
Mark Petticrew
School of Social Policy, Sociology and Social Research, University of Kent, CT2 7NF, UK
Mike W Calnan
MRC General Practice Research Framework, University College London, NW1 2ND, UK
Irwin Nazareth
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Paul M Wilson .
Additional information
Competing interests.
Paul Wilson is an Associate Editor of Implementation Science. All decisions on this manuscript were made by another senior editor. Paul Wilson works for, and has contributed to the development of the CRD framework which is included in this review. The author(s) declare that they have no other competing interests.
Authors' contributions
All authors contributed to the conception, design, and analysis of the review. All authors were involved in the writing of the first and all subsequent versions of the paper. All authors read and approved the final manuscript. Paul Wilson is the guarantor.
Electronic supplementary material
13012_2010_305_moesm1_esm.doc.
Additional file 1: Appendix 1: Database search strategies. This file includes details of the database specific search strategies used in the review. (DOC 39 KB)
13012_2010_305_MOESM2_ESM.DOC
Additional file 2: Appendix 2: Full-text papers assessed for eligibility but excluded from the review. This file includes details of full-text papers assessed for eligibility but excluded from the review. (DOC 52 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Wilson, P.M., Petticrew, M., Calnan, M.W. et al. Disseminating research findings: what should researchers do? A systematic scoping review of conceptual frameworks. Implementation Sci 5 , 91 (2010). https://doi.org/10.1186/1748-5908-5-91
Download citation
Received : 04 January 2010
Accepted : 22 November 2010
Published : 22 November 2010
DOI : https://doi.org/10.1186/1748-5908-5-91
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Knowledge Translation
- Social Marketing
- Dissemination Activity
- Research Dissemination
- Persuasive Communication
View archived comments (1)
Implementation Science
ISSN: 1748-5908
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search

The Role of Dissemination as a Fundamental Part of a Research Project
Affiliations.
- 1 1 Agència de Salut Pùblica de Barcelona.
- 2 2 CIBER Epidemiología y Salud Pública (CIBERESP), Madrid, Spain.
- 3 3 Institut d'Investigació Biomèdica (IIB Sant Pau), Barcelona, Spain.
- 4 4 Universitat Pompeu Fabra, Barcelona, Spain.
- PMID: 27799595
- DOI: 10.1177/0020731416676227
Dissemination and communication of research should be considered as an integral part of any research project. Both help in increasing the visibility of research outputs, public engagement in science and innovation, and confidence of society in research. Effective dissemination and communication are vital to ensure that the conducted research has a social, political, or economical impact. They draw attention of governments and stakeholders to research results and conclusions, enhancing their visibility, comprehension, and implementation. In the European project SOPHIE (Evaluating the Impact of Structural Policies on Health Inequalities and Their Social Determinants and Fostering Change), dissemination was an essential component of the project in order to achieve the purpose of fostering policy change based on research findings. Here we provide our experience and make some recommendations based on our learning. A strong use of online communication (website, Twitter, and Slideshare accounts), the production of informative videos, the research partnership with civil society organizations, and the organization of final concluding scientific events, among other instruments, helped to reach a large public within the scientific community, civil society, and the policy making arena and to influence the public view on the impact on health and equity of certain policies.
Keywords: communication; health inequalities; knowledge transfer; public policies; research dissemination; social media.
PubMed Disclaimer
Similar articles
- Introduction to the "Evaluating the Impact of Structural Policies on Health Inequalities and Their Social Determinants and Fostering Change" (SOPHIE) Project. Borrell C, Malmusi D, Muntaner C. Borrell C, et al. Int J Health Serv. 2017 Jan;47(1):10-17. doi: 10.1177/0020731416681891. Int J Health Serv. 2017. PMID: 27956577
- Structural Transformation to Attain Responsible BIOSciences (STARBIOS2): Protocol for a Horizon 2020 Funded European Multicenter Project to Promote Responsible Research and Innovation. Colizzi V, Mezzana D, Ovseiko PV, Caiati G, Colonnello C, Declich A, Buchan AM, Edmunds L, Buzan E, Zerbini L, Djilianov D, Kalpazidou Schmidt E, Bielawski KP, Elster D, Salvato M, Alcantara LCJ, Minutolo A, Potestà M, Bachiddu E, Milano MJ, Henderson LR, Kiparoglou V, Friesen P, Sheehan M, Moyankova D, Rusanov K, Wium M, Raszczyk I, Konieczny I, Gwizdala JP, Śledzik K, Barendziak T, Birkholz J, Müller N, Warrelmann J, Meyer U, Filser J, Khouri Barreto F, Montesano C. Colizzi V, et al. JMIR Res Protoc. 2019 Mar 7;8(3):e11745. doi: 10.2196/11745. JMIR Res Protoc. 2019. PMID: 30843870 Free PMC article.
- Communication in a Human biomonitoring study: Focus group work, public engagement and lessons learnt in 17 European countries. Exley K, Cano N, Aerts D, Biot P, Casteleyn L, Kolossa-Gehring M, Schwedler G, Castaño A, Angerer J, Koch HM, Esteban M, Schoeters G, Den Hond E, Horvat M, Bloemen L, Knudsen LE, Joas R, Joas A, Dewolf MC, Van de Mieroop E, Katsonouri A, Hadjipanayis A, Cerna M, Krskova A, Becker K, Fiddicke U, Seiwert M, Mørck TA, Rudnai P, Kozepesy S, Cullen E, Kellegher A, Gutleb AC, Fischer ME, Ligocka D, Kamińska J, Namorado S, Reis MF, Lupsa IR, Gurzau AE, Halzlova K, Jajcaj M, Mazej D, Tratnik JS, Huetos O, López A, Berglund M, Larsson K, Sepai O. Exley K, et al. Environ Res. 2015 Aug;141:31-41. doi: 10.1016/j.envres.2014.12.003. Epub 2014 Dec 12. Environ Res. 2015. PMID: 25499539
- Community health outreach program of the Chad-Cameroon petroleum development and pipeline project. Utzinger J, Wyss K, Moto DD, Tanner M, Singer BH. Utzinger J, et al. Clin Occup Environ Med. 2004 Feb;4(1):9-26. doi: 10.1016/j.coem.2003.09.004. Clin Occup Environ Med. 2004. PMID: 15043361 Review.
- [DECIDE: developing and evaluating communication strategies to support informed decisions and practice based on evidence]. Parmelli E, Amato L, Saitto C, Davoli M; Gruppo di Lavoro "DECIDE Italia. Parmelli E, et al. Recenti Prog Med. 2013 Oct;104(10):522-31. doi: 10.1701/1349.14997. Recenti Prog Med. 2013. PMID: 24326703 Review. Italian.
- Harnessing real-life experiences: the development of guidelines to communicate research findings on Developmental Coordination Disorder/dyspraxia. Purcell C, Dahl A, Gentle J, Hill E, Kirby A, Mason A, McQuillan V, Meek A, Payne S, Scott-Roberts S, Shaw K, Wilmut K. Purcell C, et al. Res Involv Engagem. 2024 Aug 8;10(1):84. doi: 10.1186/s40900-024-00611-0. Res Involv Engagem. 2024. PMID: 39118133 Free PMC article.
- The cultural safety of research reports on primary healthcare use by Indigenous Peoples: a systematic review. Hiyare-Hewage A, Sinka V, Grande ED, Kerr M, Kim S, Mallitt KA, Dickson M, Jaure A, Wilson R, Craig JC, Stephens JH. Hiyare-Hewage A, et al. BMC Health Serv Res. 2024 Jul 31;24(1):873. doi: 10.1186/s12913-024-11314-3. BMC Health Serv Res. 2024. PMID: 39085815 Free PMC article.
- Comparison of recruitment methodologies for clinical trials: Results from the time for living and caring (TLC) intervention study. Sparks C, Hsu A, Neller SA, Eaton J, Thompson A, Wong B, Iacob E, Terrill AL, Caserta M, Stark L, Utz RL. Sparks C, et al. Contemp Clin Trials. 2024 May;140:107518. doi: 10.1016/j.cct.2024.107518. Epub 2024 Mar 29. Contemp Clin Trials. 2024. PMID: 38554816
- Supporting early-career dementia researchers: Identifying support needs and ways forward via a European study. Dupont C, Gilissen J, Dassen FCM, Branco RM, Heins P, Heffernan E, Bartels SL. Dupont C, et al. Alzheimers Dement. 2024 Feb;20(2):1321-1333. doi: 10.1002/alz.13530. Epub 2023 Nov 20. Alzheimers Dement. 2024. PMID: 37983858 Free PMC article.
- Cutting Through the Noise: Predictors of Successful Online Message Retransmission in the First 8 Months of the COVID-19 Pandemic. Renshaw SL, Mai S, Dubois E, Sutton J, Butts CT. Renshaw SL, et al. Health Secur. 2021 Jan-Feb;19(1):31-43. doi: 10.1089/hs.2020.0200. Health Secur. 2021. PMID: 33606574 Free PMC article.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources, other literature sources.
- scite Smart Citations
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Dissemination of Results
It is expected that results from of research conducted at an academic institution will be made available to the scientific community and otherwise generally benefit society. Sponsors may also have certain dissemination requirements, such as registering and posting clinical trial results to NIH ClinicalTrials.gov .
Most often, activities such as submitting manuscripts for publication in scientific journals (and ultimately providing open access), presenting research results at scientific conferences, posting research data to a publicly-available web site, providing data to scientists upon request, and participating in media interviews fulfill expectations and requirements for dissemination of results. Data and publications may also be deposited to open access repositories. UW Libraries Scholarly Publishing and Open Access page provides general information on a range of open access topics, plus a link on the proposed UW faculty open access policy now under discussion in the Faculty Senate.
- The Principal Investigator (PI) is responsible for validation of results to be disseminated and for determining when and how they will be disseminated. Collaborators should be consulted with respect to all of these activities, as appropriate.
- Research staff may assist with the preparation of reports, manuscripts, archived data, and web site postings, as appropriate, under the direction of the PI.
- Prepare a detailed report of the research, including the results, for submission to a scientific journal.
- Present research results at one or more scientific conferences.
- Post detailed methodology, including statistical approach, and raw data to a publicly-available web site or make this information available upon requests.
- Consider responding to media requests for interviews or lay summaries of the research.
Clinical trials: Post results at ClinicalTrials.gov
Studies that are registered at ClinicalTrials.gov must post the results to this website. The deadline for reporting is usually no later than one year after the final subject was examined or received an intervention for final collection of data for the primary outcome. This requirement must be fulfilled even if the trial never enrolled any subjects or was terminated prematurely for any reason. Review this clinical trials registration and reporting guidance for information about exceptions, alternate timelines, and penalties for non-compliance.
Forms, Tools, and Resources
- ClinicalTrials.gov
- Open access resources at UW
- Data Management Resources at UW
- NIH: PubMed
- NIH: Article Publication
- CoC Decision Tree: Is my research subject to CoC?
Policy, Regulation, and Guidance
- NIH: Certificate of Confidentiality
Announcements
University of washington office of research, or support offices.
- Human Subjects Division (HSD)
- Office of Animal Welfare (OAW)
- Office of Research (OR)
- Office of Research Information Services (ORIS)
- Office of Sponsored Programs (OSP)
OR Research Units
- Applied Physics Laboratory (APL-UW)
- WA National Primate Research Center (WaNPRC)
Research Partner Offices
- Corporate and Foundation Relations (CFR)
- Enivronmental Health and Safety (EH&S)
- Grant and Contract Accounting (GCA)
- Institute of Translational Health Sciences (ITHS)
- Management Accounting and Analysis (MAA)
- Post Award Fiscal Compliance (PAFC)
Collaboration
- Centers and Institutes
- Collaborative Proposal Development Resources
- Research Fact Sheet
- Research Annual Report
- Stats and Rankings
- Honors and Awards
- Office of Research
© 2024 University of Washington | Seattle, WA
Pardon Our Interruption
As you were browsing something about your browser made us think you were a bot. There are a few reasons this might happen:
- You've disabled JavaScript in your web browser.
- You're a power user moving through this website with super-human speed.
- You've disabled cookies in your web browser.
- A third-party browser plugin, such as Ghostery or NoScript, is preventing JavaScript from running. Additional information is available in this support article .
To regain access, please make sure that cookies and JavaScript are enabled before reloading the page.
Loading metrics
Open Access
Ten simple rules for innovative dissemination of research
* E-mail: [email protected]
Affiliation Open and Reproducible Research Group, Institute of Interactive Systems and Data Science, Graz University of Technology and Know-Center GmbH, Graz, Austria
Affiliation Center for Research and Interdisciplinarity, University of Paris, Paris, France
Affiliation Freelance Researcher, Vilnius, Lithuania
Affiliation University and National Library, University of Debrecen, Debrecen, Hungary
Affiliation Institute for Research on Population and Social Policies, National Research Council, Rome, Italy
Affiliation Open Knowledge Maps, Vienna, Austria
Affiliation National and Kapodistrian University of Athens, Athens, Greece
Affiliation Center for Digital Safety and Security, AIT Austrian Institute of Technology, Vienna, Austria
- Tony Ross-Hellauer,
- Jonathan P. Tennant,
- Viltė Banelytė,
- Edit Gorogh,
- Daniela Luzi,
- Peter Kraker,
- Lucio Pisacane,
- Roberta Ruggieri,
- Electra Sifacaki,
- Michela Vignoli

Published: April 16, 2020
- https://doi.org/10.1371/journal.pcbi.1007704
- Reader Comments
Author summary
How we communicate research is changing because of new (especially digital) possibilities. This article sets out 10 easy steps researchers can take to disseminate their work in novel and engaging ways, and hence increase the impact of their research on science and society.
Citation: Ross-Hellauer T, Tennant JP, Banelytė V, Gorogh E, Luzi D, Kraker P, et al. (2020) Ten simple rules for innovative dissemination of research. PLoS Comput Biol 16(4): e1007704. https://doi.org/10.1371/journal.pcbi.1007704
Editor: Russell Schwartz, Carnegie Mellon University, UNITED STATES
Copyright: © 2020 Ross-Hellauer et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: This work was partly funded by the OpenUP project, which received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No. 710722. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: We have read the journal's policy and have the following conflicts: TR-H is Editor-in-Chief of the open access journal Publications . JT is the founder of the Open Science MOOC, and a former employee of ScienceOpen.
Introduction
As with virtually all areas of life, research dissemination has been disrupted by the internet and digitally networked technologies. The last two decades have seen the majority of scholarly journals move online, and scholarly books are increasingly found online as well as in print. However, these traditional communication vehicles have largely retained similar functions and formats during this transition. But digital dissemination can happen in a variety of ways beyond the traditional modes: social media have become more widely used among researchers [ 1 , 2 , 3 ], and the use of blogs and wikis as a specific form of ‘open notebook science’ has been popular for more than a decade [ 4 ].
Professional academic social networks such as ResearchGate and Academia.edu boast millions of users. New online formats for interaction with the wider public, such as TED talks broadcast via YouTube, often receive millions of views. Some researchers have even decided to make all of their research findings public in real time by keeping open notebooks [ 5 , 6 ]. In particular, digital technologies invoke new ways of reaching and involving audiences beyond their usual primary dissemination targets (i.e., other scholars) to actively involve peers or citizens who would otherwise remain out of reach for traditional methods of communication [ 7 ]. Adoption of these outlets and methods can also lead to new cross-disciplinary collaborations, helping to create new research, publication, and funding opportunities [ 8 ].
Beyond the increase in the use of web-based and computational technologies, other trends in research cultures have had a profound effect on dissemination. The push towards greater public understanding of science and research since the 1980s, and an emphasis on engagement and participation of non-research audiences have brought about new forms of dissemination [ 9 ]. These approaches include popular science magazines and science shows on television and the radio. In recent years, new types of events have emerged that aim at involving the general public within the research process itself, including science slams and open lab days. With science cafés and hackerspaces, novel, participatory spaces for research production and dissemination are emerging—both online and offline. Powerful trends towards responsible research and innovation, the increasing globalisation of research, and the emergence and inclusion of new or previously excluded stakeholders or communities are also reshaping the purposes of dissemination as well as the scope and nature of its audiences.
Many now view wider dissemination and public engagement with science to be a fundamental element of open science [ 10 ]. However, there is a paradox at play here, for while there have never been more avenues for the widespread dissemination of research, researchers tend nonetheless to value and focus upon just a few traditional outputs: journal articles, books, and conference presentations [ 11 ].
Following Wilson and colleagues [ 12 ], we here define research dissemination as a planned process that involves consideration of target audiences, consideration of the settings in which research findings are to be received, and communicating and interacting with wider audiences in ways that will facilitate research uptake and understanding. Innovative dissemination, then, means dissemination that goes beyond traditional academic publishing (e.g., academic journals, books, or monographs) and meetings (conferences and workshops) to achieve more widespread research uptake and understanding. Hence, a citizen science project, which involves citizens in data collection but does not otherwise educate them about the research, is not here considered innovative dissemination.
We here present 10 steps researchers can take to embrace innovative dissemination practices in their research, either as individuals or groups ( Fig 1 ). They represent the synthesis of multidimensional research activities undertaken within the OpenUP project ( https://www.openuphub.eu/ ). This European Coordination and Support Action grant award addressed key aspects and challenges of the currently transforming science landscape and proposed recommendations and solutions addressing the needs of researchers, innovators, the public, and funding bodies. The goal is to provide stakeholders (primarily researchers but also intermediaries) with an entry point to innovative dissemination, so that they can choose methods and tools based on their audience, their skills, and their requirements. The advice is directed towards both individual researchers and research teams or projects. It is similar to other entries in the Ten Simple Rules series (e.g., [ 13 , 14 ]). Ultimately, the benefit here for researchers is increased recognition and social impact of their work.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pcbi.1007704.g001
Rule 1: Get the basics right
Despite changes in communication technologies and models, there are some basic organisational aspects of dissemination that remain important: to define objectives, map potential target audience(s), target messages, define mode of communication/engagement, and create a dissemination plan. These might seem a bit obvious or laborious but are critical first steps towards strategically planning a project.
Define objectives
The motivation to disseminate research can come in many forms. You might want to share your findings with wider nonacademic audiences to raise awareness of particular issues or invite audience engagement, participation, and feedback. Start by asking yourself what you want to achieve with your dissemination. This first strategic step will make all other subsequent steps much simpler, as well as guide how you define the success of your activities.
Map your audience
Specify who exactly you want your research results to reach, for which purposes, and what their general characteristics might be (e.g., policy makers, patient groups, non-governmental organisations). Individuals are not just ‘empty vessels’ to be filled with new knowledge, and having a deeper contextual understanding of your audience can make a real difference to the success of your engagement practices. Who is most affected by your research? Who might find it most valuable? What is it that you want them to take away? Get to know your target audiences, their needs and expectations of the research outcomes, as well as their preferred communication channels to develop a detailed understanding of their interests and align your messages and media with their needs and priorities. Keep in mind, too, that intermediaries such as journalists or science communication organisations can support or mediate the dissemination process.
Target/frame your messages
Target and frame the key messages that you want to communicate to specific groups. Think first from the perspective of what they might want or need to hear from you, rather than what you want to tell them. Choosing media and format of your communication strongly depends on your communication objectives, i.e., what you want to achieve. There are many ways to communicate your research; for example, direct messages, blog/vlog posts, tweeting about it, or putting your research on Instagram. Form and content go hand in hand. Engage intermediaries and leverage any relevant existing networks to help amplify messages.
Create a dissemination plan
Many funded research projects require a dissemination plan. However, even if not, the formal exercise of creating a plan at the outset that organises dissemination around distinct milestones in the research life cycle will help you to assign roles, structure activities, as well as plan funds to be allocated in your dissemination. This will ultimately save you time and make future work easier. If working in groups, distribute tasks and effort to ensure regular updates of content targeted to different communities. Engage those with special specific skills in the use and/or development of appropriate communication tools, to help you in using the right language and support you in finding the suitable occasions to reach your identified audience. Research is not linear, however, and so you might find it best to treat the plan as a living document to be flexibly adapted as the direction of research changes.
Rule 2: Keep the right profile
Whether communicating as an individual researcher, a research project, or a research organisation, establishing a prominent and unique identity online and offline is essential for communicating. Use personal websites, social media accounts, researcher identifiers, and academic social networks to help make you and your research visible. When doing this, try to avoid any explicit self-promotion—your personal profile naturally will develop based on your ability to be an effective and impactful communicator.
Academia is a prestige economy, where individual researchers are often evaluated based on their perceived esteem or standing within their communities [ 15 ]. Remaining visible is an essential part of accumulating esteem. An online presence maintained via personal websites, social media accounts (e.g., Facebook, Twitter, LinkedIn), researcher identifiers (e.g., ORCID), and academic social networks (e.g., ResearchGate, institutional researcher profiles) can be a personal calling card, where you can highlight experience and demonstrate your expertise in certain topics. Being active on important mailing lists, forums, and social media is not only a good chance to disseminate your findings to those communities but also offers you the chance to engage with your community and potentially spark new ideas and collaborations.
Using researcher identifiers like ORCID when disseminating outputs will ensure that those outputs will be unambiguously linked back to the individual researcher (and even automatically updated to their ORCID profile). The OpenUP survey showed that nearly half of the respondents (41%) use academic social networks as a medium to disseminate their research, and a quarter of respondents (26%) said that these networks informed their professional work [ 16 ].
Create a brand by giving your project a unique name, ideally with some intuitive relation to the issue you are investigating. Create a striking visual identity, with a compelling logo, core colours, and a project slogan. Create a website that leverages this visual identity and is as simple and intuitive as possible, both in its layout and in the way content is formulated (limit insider jargon). Create associated appropriate social media accounts (e.g., Twitter, Facebook, LinkedIn, SlideShare, YouTube) and link to this from the project website. Aim for a sustained presence with new and engaging content to reinforce project messaging, and this can help to establish a core following group or user base within different platforms. Include links to other project online presences such as social media accounts, or a rolling feed of updates if possible. Consider including a blog to disseminate core findings or give important project updates. A periodical newsletter could be released in order to provide project updates and other news, to keep the community informed and activated regarding project issues. Depending on the size of your project and budget, you might want to produce hard copy material such as leaflets or fact sheets, as well as branded giveaways to increase awareness of your project. Finally, and perhaps most importantly, try not to come across as a ‘scientific robot’, and make sure to communicate the more human personality side of research.
Rule 3: Encourage participation
In the age of open research, don’t just broadcast. Invite and engage others to foster participation and collaboration with research audiences. Scholarship is a collective endeavour, and so we should not expect its dissemination to be unidirectional, especially not in the digital age. Dissemination is increasingly done at earlier stages of the research life cycle, and such wider and more interactive engagement is becoming an integral part of the whole research workflow.
Such participative activities can be as creative as you wish; for example, through games, such as Foldit for protein folding ( https://fold.it/portal/ ). You might even find it useful to actively engage ‘citizen scientists’ in research projects; for example, to collect data or analyse findings. Initiatives such as Zooniverse ( https://www.zooniverse.org/ ) serve as great examples of allowing anyone to freely participate in cutting-edge ‘people-powered research’.
Disseminating early and often showcases the progress of your work and demonstrates productivity and engagement as part of an agile development workflow. People like to see progress and react positively to narrative, so give regular updates to followers on social media, for example, blogging or tweeting early research findings for early feedback. Alternatively, involving businesses early on can align research to industry requirements and expectations, thus potentially increasing commercial impact. In any case, active involvement of citizens and other target audiences beyond academia can help increase the societal impact of your research [ 17 ].
Rule 4: Open science for impact
Open science is ‘transparent and accessible knowledge that is shared and developed through collaborative networks’, as defined by one systematic review [ 18 ]. It encompasses a variety of practices covering a range of research processes and outputs, including areas like open access (OA) to publications, open research data, open source software/tools, open workflows, citizen science, open educational resources, and alternative methods for research evaluation including open peer review [ 19 ]. Open science is rooted in principles of equitable participation and transparency, enabling others to collaborate in, contribute to, scrutinise and reuse research, and spread knowledge as widely as possible [ 20 ]. As such, innovative dissemination is a core element of open science.
Embracing open science principles can boost the impact of research. Firstly, OA publications seem to accrue more citations than their closed counterparts, as well as having a variety of possible wider economic and societal benefits [ 21 ]. There are a number of ways to make research papers OA, including at the journal site itself, or self-archiving an accepted manuscript in a repository or personal website.
Disseminating publications as preprints in advance of or parallel to journal submission can increase impact, as measured by relative citation counts [ 22 ]. Very often, traditional publishing takes a long time, with the waiting time between submission and acceptance of a paper being in excess of 100 days [ 23 ]. Preprinting speeds up dissemination, meaning that findings are available sooner for sharing and reuse. Potential platforms for disseminating preprints include the Open Science Framework, biorXiv, or arXiv.
Dissemination of other open science outputs that would usually remain hidden also not only helps to ensure the transparency and increased reproducibility of research [ 24 ], but also means that more research elements are released that can potentially impact upon others by creating network effects through reuse. Making FAIR (Findable, Accessible, Interoperable, Reusable) research data and code available enables reuse and remixing of core research outputs, which can also lead to further citations for projects [ 25 , 26 , 27 ]. Published research proposals, protocols, and open notebooks act as advertisements for ongoing research and enable others to reuse methods, exposing the continuous and collaborative nature of scholarship.
To enable reuse, embrace open licenses. When it comes to innovative dissemination, the goal is usually that the materials are accessible to as large an audience as possible. If appropriate open licenses are not used, while materials may be free to access, they cannot be widely used, modified, or shared. The best in this case is the widely adopted Creative Commons licenses, CC BY or CC 0. Variations of these licenses are less permissive and can constrain reuse for commercial or derivative purposes. This limitation, however, prevents the use of materials in many forms of (open) educational resources and other open projects, including Wikipedia. Careful consideration should be given to licensing of materials, depending on what your intended outcomes from the project are (see Rule 1). Research institutes and funding bodies typically have a variety of policies and guidance about the use and licensing of such materials, and should be consulted prior to releasing any materials.
Rule 5: Remix traditional outputs
Traditional research outputs like research articles and books can be complemented with innovative dissemination to boost impact; for example, by preparing accompanying nonspecialist summaries, press releases, blog posts, and visual/video abstracts to better reach your target audiences. Free media coverage can be an easy way to get results out to as many people as possible. There are countless media outlets interested in science-related stories. Most universities and large research organisations have an office for public affairs or communication: liaise with these experts to disseminate research findings widely through public media. Consider writing a press release for manuscripts that have been accepted for publication in journals or books and use sample forms and tools available online to assist you in the process. Some journals also have dedicated press teams that might be able to help you with this.
Another useful tool to disseminate traditional research outputs is to release a research summary document. This one- or two-page document clearly and concisely summarises the key conclusions from a research initiative. It can combine several studies by the same investigator or by a research group and should integrate two main components: key findings and fact sheets (preferably with graphical images to illustrate your point). This can be published on your institutional website as well as on research blogs, thematic hubs, or simply posted on your social media profiles. Other platforms such as ScienceOpen and Kudos allow authors to attach nonspecialist summaries to each of their research papers.
To maximise the impact of your conference presentations or posters, there are several steps that can be taken. For instance, you can upload your slides to a general-purpose repository such as Figshare or Zenodo and add a digital object identifier (DOI) to your presentation. This also makes it easier to integrate such outputs with other services like ORCID. You can also schedule tweets before and during any conferences, and use the conference hashtag to publicise your talk or poster. Finally, you can also add information about your contributions to email signatures or out-of-office messages [ 28 ].
Rule 6: Go live
In-person dissemination does not just have to be at stuffy conferences. With research moving beyond the walls of universities, there are several types of places for more participatory events. Next to classic scientific conferences, different types of events addressing wider audiences have emerged. It is possible to hit the road and take part in science festivals, science slams, TEDx talks, or road shows.
Science slams are short talks in which researchers explain a scientific topic to a typically nonexpert audience. Similar to other short talk formats like TED talks, they lend themselves to being spread over YouTube and other video channels. A prominent example from the German-speaking area is Giulia Enders, who won the first prize in a science slam that took place in 2012 in Berlin. The YouTube video of her fascinating talk about the gut has received over 1 million views. After this success, she got an offer to write a book about the gut and the digestive system, which has since been published and translated into many languages. You never know how these small steps might end up having a wider impact on your research and career.
Another example is Science Shops, small entities which provide independent, participatory research support to civil society. While they are usually linked to universities, hacker and maker spaces tend to be community-run locations, where people with an interest in science, engineering, and art meet and collaborate on projects. Science festivals are community-based showcases of science and technology that take place over large areas for several days or weeks and directly involve researchers and practitioners in public outreach. Less formally, Science Cafés or similar events like Pint of Science are public engagement events in casual settings like pubs and coffeehouses.
Alternatively, for a more personal approach, consider reaching out to key stakeholders who might be affected by your research and requesting a meeting, or participating in relevant calls for policy consultations. Such an approach can be especially powerful in getting the message across to decision-makers and thought-leaders, although the resources required to schedule and potentially travel to such meetings means you should target such activities very carefully. And don’t forget the value of serendipity—who knows who you’ll meet in the course of your everyday meetings and travels. Always be prepared with a 30 second ‘elevator pitch’ that sums up your project in a confident and concise manner—such encounters may be the gateways to greater engagement or opportunities.
Rule 7: Think visual
Dissemination of research is still largely ruled by the written or spoken word. However, there are many ways to introduce visual elements that can act as attractive means to help your audience understand and interpret your research. Disseminate findings through art or multimedia interpretations. Let your artistic side loose or use new visualisation techniques to produce intuitive, attractive data displays. Of course, not everyone is a trained artist, and this will be dependent on your personal skills.
Most obviously, this could take the form of data visualisation. Graphic representation of quantitative information reaches back to ‘earliest map-making and visual depiction’ [ 29 ]. As technologies have advanced, so have our means of visually representing data.
If your data visualisations could be considered too technical and not easily understandable by a nonexpert reader, consider creating an ad hoc image for this document; sometimes this can also take the form of a graphical abstract or infographic. Use online tools to upload a sample of your data and develop smart graphs and infographics (e.g., Infogr.am, Datawrapper, Easel.ly, or Venngage).
Science comics can be used, in the words of McDermott, Partridge, and Bromberg [ 30 ], to ‘communicate difficult ideas efficiently, illuminate obscure concepts, and create a metaphor that can be much more memorable than a straightforward description of the concept itself’. McDermott and colleagues continue that comics can be used to punctuate or introduce papers or presentations and to capture and share the content of conference talks, and that some journals even have a ‘cartoon’ publication category. They advise that such content has a high chance of being ‘virally’ spread via social media.
As previously discussed, you may also consider creating a video abstract for a paper or project. However, as with all possible methods, it is worth considering the relative costs versus benefits of such an approach. Creating a high-quality video might have more impact than, say, a blog post but could be more costly to produce.
Projects have even successfully disseminated scientific findings through art. For example, The Civilians—a New York–based investigative theatre company—received a three-year grant to develop The Great Immensity , a play addressing the complexity of climate change. AstroDance tells the story of the search for gravitational waves through a combination of dance, multimedia, sound, and computer simulations. The annual Dance Your PhD contest, which began in 2007 and is sponsored by Science magazine, even asks scientists to interpret their PhD research as dance. This initiative receives approximately 50 submissions a year, demonstrating the popularity of novel forms of research dissemination.
Rule 8: Respect diversity
The academic discourse on diversity has always included discussions on gender, ethnic and cultural backgrounds, digital literacy, and epistemic, ideological, or economic diversity. An approach that is often taken is to include as many diverse groups into research teams as possible; for example, more women, underrepresented minorities, or persons from developing countries. In terms of scientific communication, however, not only raising awareness about diversity issues but also increasing visibility of underrepresented minorities in research or including more women in science communication teams should be considered, and embedded in projects from the outset. Another important aspect is assessing how the communication messages are framed, and if the chosen format and content is appropriate to address and respect all audiences. Research should reach all who might be affected by it. Respect inclusion in scientific dissemination by creating messages that reflect and respect diversity regarding factors like gender, demography, and ability. Overcoming geographic barriers is also important, as well as the consideration of differences in time zones and the other commitments that participants might have. As part of this, it is a key responsibility to create a healthy and welcoming environment for participation. Having things such as a code of conduct, diversity statement, and contributing guidelines can really help provide this for projects.
The 2017 Progression Framework benchmarking report of the Scientific Council made several recommendations on how to make progress on diversity and inclusion in science: (1) A strategy and action plan for diversity should developed that requires action from all members included and (2) diversity should be included in a wide range of scientific activities, such as building diversity into prizes, awards, or creating guidance on building diversity and inclusion across a range of demographics groups into communications, and building diversity and inclusion into education and training.
Rule 9: Find the right tools
Innovative dissemination practices often require different resources and skills than traditional dissemination methods. As a result of different skills and tools needed, there may be higher costs associated with some aspects of innovative dissemination. You can find tools via a more-complete range of sources, including the OpenUP Hub. The Hub lists a catalogue of innovative dissemination services, organised according to the following categories, with some suggested tools:
- Visualising data: tools to help create innovative visual representations of data (e.g., Nodegoat, DataHero, Plot.ly)
- Sharing notebooks, protocols, and workflows: ways to share outputs that document and share research processes, including notebooks, protocols, and workflows (e.g., HiveBench, Protocols.io, Open Notebook Science Network)
- Crowdsourcing and collaboration: platforms that help researchers and those outside academia to come together to perform research and share ideas (e.g., Thinklab, Linknovate, Just One Giant Lab)
- Profiles and networking: platforms to raise academic profile and find collaboration and funding opportunities with new partners (e.g., Humanities Commons, ORCID, ImpactStory)
- Organiding events: tools to help plan, facilitate, and publicise academic events (e.g., Open Conference Systems, Sched, ConfTool)
- Outreach to wider public: channels to help broadcast your research to audiences beyond academia, including policy makers, young people, industry, and broader society (e.g., Famelab, Kudos, Pint of Science)
- Publishing: platforms, tools, and services to help you publish your research (e.g., Open Science Framework, dokieli, ScienceMatters)
- Archive and share: preprint servers and repositories to help you archive and share your texts, data, software, posters, and more (e.g., BitBucket, GitHub, RunMyCode)
The Hub here represents just one attempt to create a registry of resources related to scholarly communication. A similar project is the 101 Innovations in Scholarly Communication project, which contains different tools and services for all parts of a generalised research workflow, including dissemination and outreach. This can be broadly broken down into services for communication through social media (e.g., Twitter), as well as those designed for sharing of scholarly outputs, including posters and presentations (e.g., Zenodo or Figshare). The Open Science MOOC has also curated a list of resources for its module on Public Engagement with Science, and includes key research articles, organisations, and services to help with wider scientific engagement.
Rule 10: Evaluate, evaluate, evaluate
Assess your dissemination activities. Are they having the right impact? If not, why not? Evaluation of dissemination efforts is an essential part of the process. In order to know what worked and which strategies did not generate the desired outcomes, all the research activities should be rigorously assessed. Such evaluation should be measured via the use of a combination of quantitative and qualitative indicators (which should be already foreseen in the planning stage of dissemination; see Rule 1). Questionnaires, interviews, observations, and assessments could also be used to measure the impact. Assessing and identifying the most successful practices will give you the evidence for the most effective strategies to reach your audience. In addition, the evaluation can help you plan your further budget and minimise the spending and dedicating efforts on ineffective dissemination methods.
Some examples of quantitative indicators include the following:
- Citations of publications;
- alternative metrics related to websites and social media platforms (updates, visits, interactions, likes, and reposts);
- numbers of events held for specific audiences;
- numbers of participants in those events;
- production and circulation of printed materials;
- media coverage (articles in specialised press newsletters, press releases, interviews, etc.); and
- how much time and effort were spent on activities.
Some examples of qualitative indicators include the following:
- Visibility in the social media and attractiveness of website;
- newly established contacts with networks and partners and the outcomes of these contacts;
- feedback from the target groups; and
- share feedback within your group on what dissemination strategies seemed to be the most effective in conveying your messages and reaching your target audiences.
We recognise that researchers are usually already very busy, and we do not seek to pressurise them further by increasing their burdens. Our recommendations, however, come at a time when there are shifting norms in how researchers are expected to engage with society through new technologies. Researchers are now often partially evaluated based on such, or expected to include dissemination plans in grant applications. We also do not want to encourage the further fragmentation of scholarship across different platforms and ‘silos’, and therefore we strongly encourage researchers to be highly strategic in how they engage with different methods of innovative dissemination. We hope that these simple rules provide guidance for researchers and their future projects, especially as the tools and services available evolve through time. Some of these suggestions or platforms might not work across all project types, and it is important for researchers to find which methods work best for them.
Acknowledgments
Many thanks to everyone who engaged with the workshops we conducted as part of this grant award.
- View Article
- Google Scholar
- PubMed/NCBI
- 19. Pontika N, Knoth P, Cancellieri M, Pearce S. Fostering Open Science to Research Using a Taxonomy and an ELearning Portal. In: iKnow: 15th International Conference on Knowledge Technologies and Data Driven Business, 21–22 Oct 2015, Graz, Austria [cited 2020 Mar 23]. Available from: http://oro.open.ac.uk/44719/
- 29. Friendly M. A Brief History of Data Visualization. In: Handbook of Data Visualization . Chen C, Härdle W, Unwin A, editors. Springer Handbooks Comp.Statistics. Berlin, Heidelberg: Springer Berlin Heidelberg. https://doi.org/10.1007/978-3-540-33037-0_2 . 2008. Pp.15–56.
This paper is in the following e-collection/theme issue:
Published on 16.8.2024 in Vol 26 (2024)
Factors Influencing the Implementation of Digital Advance Care Planning: Qualitative Interview Study
Authors of this article:

Original Paper
- Andy Bradshaw 1 , BSc, PhD ;
- Jacqueline Birtwistle 2 , BSc, MSc ;
- Catherine J Evans 1, 3 , BSc, MSc, RGN, SPQDN, PhD ;
- Katherine E Sleeman 1 , BSc, MBBS, MRCP, PhD ;
- Suzanne Richards 2 , BSc, PhD ;
- Robbie Foy 2 , MBChB, MRCGP, MSc, MFPHM, PhD ;
- Pablo Millares Martin 4 , LMS, DCS, MSc ;
- Paul Carder 5 , BSc ;
- Matthew J Allsop 2 , BSc, PhD, CPsychol ;
- Maureen Twiddy 6 , BSc, MSc, PhD
1 Cicely Saunders Institute, Kings College London, London, United Kingdom
2 Leeds Institute of Health Sciences, University of Leeds, Leeds, United Kingdom
3 Sussex Community NHS Foundation Trust, Brighton, United Kingdom
4 Whitehall Surgery, Leeds, United Kingdom
5 NHS West Yorkshire Integrated Care Board, White Rose House, Wakefield, United Kingdom
6 Hull York Medical School, Institute of Clinical and Applied Health Research, Allam Medical Building, University of Hull, Hull, United Kingdom
Corresponding Author:
Matthew J Allsop, BSc, PhD, CPsychol
Leeds Institute of Health Sciences
University of Leeds
Worsley Building
Leeds, LS2 9LU
United Kingdom
Phone: 44 1133434185
Email: [email protected]
Background: Palliative care aims to improve the quality of life for people with life-limiting illnesses. Advance care planning conversations that establish a patient’s wishes and preferences for care are part of a person-centered approach. Internationally, electronic health record systems are digital interventions used to record and share patients’ advance care plans across health care services and settings. They aim to provide tools that support electronic information sharing and care coordination. Within the United Kingdom, Electronic Palliative Care Coordination Systems (EPaCCS) are an example of this. Despite over a decade of policy promoting EPaCCS nationally, there has been limited implementation and consistently low levels of use by health professionals.
Objective: The aim of this study is to explore the factors that influence the implementation of EPaCCS into routine clinical practice across different care services and settings in 2 major regions of England.
Methods: A qualitative interview study design was used, guided by Normalization Process Theory (NPT). NPT explores factors affecting the implementation of complex interventions and consists of 4 primary components (coherence, cognitive participation, collective action, and reflexive monitoring). Health care and social care practitioners were purposively sampled based on their professional role and work setting. Individual web-based semistructured interviews were conducted. Data were analyzed using thematic framework analysis to explore issues which affected the implementation of EPaCCS across different settings at individual, team, organizational, and technical levels.
Results: Participants (N=52) representing a range of professional roles were recruited across 6 care settings (hospice, primary care, care home, hospital, ambulatory, and community). In total, 6 themes were developed which mapped onto the 4 primary components of NPT and represented the multilevel influences affecting implementation. At an individual level, these included (1) EPaCCS providing a clear and distinct way of working and (2) collective contributions and buy-in. At a team and organizational level, these included (3) embedding EPaCCS into everyday practice and (4) championing driving implementation. At a technical level, these included (5) electronic functionality, interoperability, and access. Breakdowns in implementation at different levels led to variations in (6) confidence and trust in EPaCCS in terms of record accuracy and availability of access.
Conclusions: EPaCCS implementation is influenced by individual, organizational, and technical factors. Key challenges include problems with access alongside inconsistent use and engagement across care settings. EPaCCS, in their current format as digital advance care planning systems are not consistently facilitating electronic information sharing and care coordination. A redesign of EPaCCS is likely to be necessary to determine configurations for their optimal implementation across different settings and locations. This includes supporting health care practitioners to document, access, use, and share information across multiple care settings. Lessons learned are relevant to other forms of digital advance care planning approaches being developed internationally.
Introduction
Palliative care aims to improve the quality of life for people with life-limiting illnesses through a person-centered, multidisciplinary, and holistic approach [ 1 ]. The focus on person-centeredness is reflected in health policy both within the United Kingdom and internationally [ 2 - 5 ]. Key to facilitating person-centered care in palliative services is the concept of advance care planning. This involves having planned conversations with a patient around their individual goals, wishes, and preferences for their current and future care [ 6 ]. If a person’s preferences are documented and shared, there is evidence of beneficial outcomes. Advance care planning has been associated with better quality of care, helping people to be cared for and die in their usual place of residence, and preventing unplanned hospital admissions [ 7 - 9 ]. However, other studies indicate that it has no impact on patient outcomes or quality of life [ 10 - 12 ]. Despite this uncertainty, advance care planning has been adopted by health care systems internationally as a key feature of person-centered care.
While there are benefits associated with advance care planning, delivery of palliative care requires the involvement of, and communication between, multiprofessional services across different settings of care (ie, hospice, general practice, community-based care, out-of-hours services, hospitals, emergency services, care homes, and social care) [ 13 , 14 ]. To overcome the need for information sharing across multiple health care providers and settings, electronic health record systems are increasingly being used to document and share advance care planning information. This approach has been reported across countries that include the United States [ 15 , 16 ], Australia [ 17 ], and the United Kingdom. In the United Kingdom, the use of electronic health record systems for documenting and sharing advance care plans are called Electronic Palliative Care Coordination Systems, often referred to using the acronym EPaCCS.
EPaCCS emerged in response to the Department of Health’s 2008 End of Life Care Strategy, which advocated for improved coordination of care at the end of life for people with life-limiting conditions (ie, cancer and noncancer conditions, including dementia) [ 18 ]. Policy drivers for the widespread use of electronic systems (such as EPaCCS) across health and social care providers have continued to the present day [ 19 , 20 ]. This includes, for example, an expectation that care records for all people living with a long-term condition should include a person’s care needs and preferences, and should be shared with all those involved in their care [ 19 ]. The development of EPaCCS sought to overcome challenges arising through the fragmentation of health systems that can lead to patients not receiving person-centered care at the right time and in the right place [ 21 , 22 ]. This can result in patient needs not being met, unplanned and avoidable hospital admissions, and patients not being cared for, or dying in a place of their choice [ 23 - 25 ].
EPaCCS have been developed across the United Kingdom since 2008 and multiple variants have arisen. These include standalone web-based electronic registers such as Coordinate my Care which was implemented in London [ 26 ], and template forms integrated into already-existing electronic patient records, such as in Leeds [ 27 ] and the Key Information Summary in Scotland [ 28 ]. Regardless of the mode used for implementing EPaCCS locally across regions, the Palliative and End of Life Care Information Standard specifies the core content that should be recorded and shared (eg, demographic information, diagnosis, medication, advance care planning information, Do Not Attempt Cardiopulmonary Resuscitation decisions, and preferred places of care and death) [ 29 ]. The expectation is that once this information is stored, it should be possible to share across all settings involved in the delivery of palliative and end-of-life care, as well as sharing any updates on the care plan.
However, there is widespread variation with regard to how EPaCCS are implemented within local health care systems (eg, who initiates the creation of a record, which settings of care can access and edit information in EPaCCS records) [ 14 ] which has resulted in variable levels of interoperability and access [ 14 , 30 - 33 ]. In part, this may be a factor influencing the low use rates reported for EPaCCS, with 9%-43% of people with palliative care needs having an EPaCCS record created before death [ 14 , 27 , 34 , 35 ]. Alongside low use, there is uncertainty about how EPaCCS are being used in routine practice and limited evidence of their impact, inhibiting the development of an evidence base to guide how their implementation might be optimized [ 13 , 14 , 30 , 36 , 37 ]. The aim of this study was to explore health care professionals’ perspectives on factors that influence the implementation of EPaCCS in routine clinical practice across different care settings in England.
We undertook a qualitative interview study. This approach was selected as we sought to develop new insights and knowledge on a relatively understudied topic area [ 38 ]. Our study was informed by an interpretative paradigm [ 39 ]. That is, we explored the study aim from the standpoint of ontological relativism (the acceptance of multiple, mind-dependent realities) and epistemological constructionism (an appreciation that knowledge generated during data analysis and write-up reflected interpretations made collectively by the research team) [ 40 ]. We reported the research in line with the consolidated criteria for reporting qualitative research (COREQ [consolidated criteria for reporting qualitative research], see Multimedia Appendix 1 ) [ 41 ].
Theoretical Perspective
EPaCCS can be conceptualized as a complex intervention. This is because they comprise multiple interacting components and operate at the interface of different health care professionals, organizations, settings of care, and patients and their families [ 42 ]. Normalization Process Theory (NPT) is an implementation theory that is used to explain how complex interventions are normalized (ie, deeply embedded into, and used as part of, routine practice) [ 43 - 45 ].
In explaining the different types of “work” that people do in normalizing complex interventions, NPT consists of 4 interlinked primary constructs ( Table 1 ) [ 46 , 47 ]. We used these primary constructs of NPT as a guiding theoretical framework to guide data collection, analysis, and interpretation in understanding the factors affecting the implementation of EPaCCS into routine clinical practice.
| NPT construct | Definition | Framework applied in this study |
| Coherence (“sense-making work”) | “How do people work together in everyday settings to understand and plan the activities that need to be accomplished to put an intervention and its components into practice?” | The ways in which participants think about distinguishing use of digital systems from other formats for advance care planning, collectively agreeing on the purpose of EPaCCS individually understanding what EPaCCS requires of them, and constructing potential value of EPaCCS for their work. |
| Cognitive participation (“relational work”) | “How do people work together to create networks of participation and communities of practice around interventions and their components?” | The ways in which participants become engaged in understanding what they need to do and support for EPaCCS to be sustained, influencing how EPaCCS use can be sustained, adapting to EPaCCS to support use by themselves and others, and supporting others’ engagement with EPaCCS. |
| Collective action (“operational work”) | “How do people work together to enact interventions and their components?” | The ways in which participants perform the tasks required for EPaCCS to support advance care planning, build accountability and maintain confidence in the use of EPaCCS, understand the appropriateness of existing roles and responsibilities relating to EPaCCS use, and view the resources and organizational support for EPaCCS use. |
| Reflexive monitoring (“appraisal work”) | “How do people work together to appraise interventions and their components?” | The ways in which participants appraise the effects of EPaCCS, themselves and with colleagues understand whether EPaCCS are operating well, individually understand and respond to the impact of EPaCCS, and modify their work in response to their appraisal of EPaCCS. |
a Definitions derived from May et al (2022) [ 46 ].
b How definitions of NPT constructs were “in the simplest possible terms” [ 48 ] and applied to data collection, analysis, and interpretation.
c EPaCCS: Electronic Palliative Care Coordination Systems.
Recruitment and Settings
Recruitment took place in 2 UK regions in London (population circa 9 million) and West Yorkshire (population circa 2.3 million). Participants comprised a subsample of respondents to an earlier survey who had agreed to be contacted for follow-up interviews. In West Yorkshire, EPaCCS comprise a template that is embedded within a patient’s electronic record, generally in the electronic record system used by primary care providers that can share information across different care settings within a defined geographical area. Within London, at the time of this study, the most used EPaCCS system was “Coordinate My Care” (CMC). This was a standalone system (eg, it operated outside routinely used patient records), and enabled patients to access their own records [ 14 ]. Since the conception of this study, it has been superseded by an EPaCCS system called “Universal Care Plan.”
Participants were initially selected using purposive maximum variation sampling to gather the widest range of perspectives [ 49 ]. This entailed sampling participants based on specific criteria (geographical location, professional role, setting of care, and levels of understanding of or engagement with EPaCCS based on previous survey responses). The logic underpinning this approach was to explore our research aim from diverse perspectives [ 49 ]. We worked across primary, secondary, and tertiary care settings in purposefully recruiting doctors, nurses, care home staff, paramedics, and general practitioners. Difficulties in recruitment, however, meant that we supplemented our recruitment approach with convenience sampling using the same criteria.
Participants were approached via email and provided with a participant information sheet. A combination of verbal and written informed consent was obtained, either by AB or JB, prior to interviews being conducted. Recruitment ran concurrently with data collection between November 2021 and June 2022. The concept of “information power” [ 50 ] was used to guide decisions on when to halt recruitment and data collection. This entailed several meetings during which research team members (AB, JB, MT, MA, CE, and KS) considered whether and when data collected from our sample held enough relevant and detailed information to comprehensively understand our research aim.
Data Collection
Single, web-based interviews were conducted by 1 of 2 researchers, both of whom had prior experience in qualitative interviewing [AB (male, research fellow) and JB (female, research fellow)]. The topic guide (provided in Multimedia Appendix 2 ) comprised questions about how participants used EPaCCS, alongside the factors that they perceived affected their implementation. During development, these questions were mapped onto the 4 primary constructs of NPT. Interviews were audio recorded, anonymized, and transcribed verbatim. All participant personal data were stored in a secure cloud storage platform within password-protected files. These data were only accessible to, shared between, and used by members of the research team, using data-sharing agreements.
Interview data were managed using NVivo (version 12; Lumivero) [ 51 ] and analyzed using thematic Framework analysis [ 52 ]. The 4 primary constructs of NPT were used as the theoretical framework to guide the coding and interpretation of data. Data analysis included moving between induction and deduction. We first used NPT to deductively build our initial analytic framework and then supplemented this through inductive coding in which we explored how patterns grounded in the data related to and enriched our analytic framework. Analysis consisted of seven iterative steps: (1) familiarization (through rereading transcripts), (2) coding (by labeling relevant segments of transcripts that aligned with our research aims), (3) creation of an initial analytic framework (by grouping similar codes into categories and categories into themes), (4) indexing (by applying our analytic framework back to raw data and refining it where appropriate), (5) charting (by creating a matrix that explored differences in data across region, role, and setting of care), (6) description (through defining and describing themes), and (7) interpretation (using our theoretical framework to further interpret our findings through the write-up of data). This approach allowed us to conduct within- and between-case pattern matching to explore where participant accounts on the use and implementation of EPaCCS converged or diverged, and how this was influenced by contextual factors (ie, setting, region, and role). Data analysis was led by AB, with fortnightly meetings between authors (AB, JB, MT, and MJA) to review the ongoing coding and analysis.
Multiple approaches were used to ensure rigor during data analysis. Throughout data collection and analysis, the researchers engaged in different forms of reflexivity. This included reflecting introspectively (inward reflections on how they impacted the research process and vice versa) and intersubjectively (reflections on relationships between them and participants) [ 53 ]. These were used as a “springboard for interpretations and more general insight” into the ways through which understandings of the research aim were being co-constructed through the research process, including analysis [ 53 ]. This included regular discussions with JB, who shared data collection and who was familiar with the data corpus. Moreover, throughout the analytical process, members of the wider interdisciplinary research team (consisting of academics and clinicians with experience in palliative care research and practice from across care settings including hospital, community, and primary care) acted as “critical friends” [ 54 ]. This entailed working collaboratively through regular meetings and written feedback in which findings were constructively challenged, reflexivity encouraged, and alternative interpretations of the data proposed. This process took place until the research team agreed that the final analytic framework accurately reflected participant accounts.
Ethical Considerations
The North of Scotland Research Ethics Committee approved the research (reference 21/PR/0428). In this study, we also recognized ethics as a reflexive process through engaging in “ethics in practice” [ 55 ]. This approach was used to remain responsive to and navigate ongoing and potentially unexpected ethical issues that may have arisen throughout data collection, analysis, and write-up (eg, by reflecting on how the research might affect professionals’ clinical practice and potential impact on patients and carers). All participants provided written consent prior to participating in the study. Before analysis, all interview transcripts were deidentified and stored on a secure cloud storage platform only accessible to the study team. Organizations in which participants were based were offered reimbursement of £75 (US $95.91) for allowing a professional to participate in the study. The level of the incentive payment was based on the cost of 1 hour of a locum doctor in the United Kingdom and was agreed upon by the research ethics committee and study funder.
A total of 52 people (characterized in Table 2 ) participated out of the 99 people approached for interview participated (characterized in Table 2 ), from London (n=29) and West Yorkshire (n=23). These participants represented a range of different professionals who work across hospice, primary care, care home, hospital, and community settings.
Six themes were developed and are represented under the corresponding constructs of NPT (coherence, cognitive participation, collective action, and reflexive monitoring). Figure 1 provides an overview of these main themes.
| London | West Yorkshire | Total | ||
| 29 | 23 | 52 | ||
| Hospice | 8 | 4 | 12 | |
| Primary care | 7 | 5 | 12 | |
| Care home | 5 | 4 | 9 | |
| Hospital | 5 | 3 | 8 | |
| Ambulance | 3 | 3 | 6 | |
| Community nurse | 1 | 4 | 5 | |
| Registered nurse | 6 | 7 | 13 | |
| Care home | 4 | 3 | 6 | |
| Community | 1 | 4 | 5 | |
| Hospital | 1 | 1 | 2 | |
| General practitioner | 7 | 5 | 12 | |
| Palliative care consultant | 6 | 4 | 13 | |
| Paramedic | 3 | 3 | 6 | |
| Clinical Nurse Specialist | 4 | 1 | 5 | |
| Care home manager | 1 | 2 | 3 | |

Coherence: How Participants Understood EPaCCS—Theme 1: A Clear and Distinct Way of Working
For a complex intervention to be normalized, it needs to be understood as a clear and distinct way of working that enhances patient care. In the case of EPaCCS, this required health care professionals to appreciate how adding all relevant advance care planning information onto a single digital platform allowed for easier sharing among organizations. Across all settings of care, however, participants did not always see how EPaCCS enhanced patient care and outcomes compared to traditional channels of communication. These included using paper-based discharge summaries, cover letters, face-to-face conversations, emails, and telephone for direct communication of advance care plans across settings:
I don’t think it [EPaCCS] changes much in terms of our GP engagement with patients … our primary channel of communication is telephone, face to face, perhaps email and EPaCCS doesn’t sort of sit with any of those. Our primary function really is to provide the clinical care and record that clinical care and those are traditional methods of doing that. EPaCCS is an add-on, and I think because it’s an add-on, it’s not the primary form of communication. [Lon18, GP, London]
Participants working in care homes across London and West Yorkshire reported using a range of different electronic patient record systems for documenting their residents’ care plans. These systems facilitated the documentation of patient wishes and preferences that could be easily accessed, reviewed, and updated internally by care home staff. Some electronic record systems used in care homes were also capable of integrating and sharing data with other systems across different settings, but this was often limited to those in general practice and not on the scale envisaged by EPaCCS:
The electronic care plan system that we are using, it’s something called PCS, so Person Centred Software. You can do your usual stuff like you said, day-to-day care notes and things like that. There also with PCS, the party piece it has is something called GP connect … with PCS if you do kind of speak with them, they are able to kind of merge certain systems together with their [other healthcare settings’] system … as far as I know PCS works with all of them [WY12&WY13, care home managers, West Yorkshire]
Cognitive Participation: How Participants Built Networks of Practice Around and Bought Into EPaCCS
Theme 2: embedding epaccs into everyday practice.
The service-wide embedding of EPaCCS into everyday practice varied and was partly influenced by the extent to which they were an integral part of everyday care processes, structures, and settings. In some contexts, entire services had no access to EPaCCS. Where EPaCCS were present and accessible across multiple settings, implementation was still thwarted because they were not used consistently by some health care professionals:
it can be like an easy thing to do and I think it gets ingrained in your normal kind of process of doing a patient’s notes … but I think when people just don’t know about it or don’t know how to access it, it then becomes, it seems more of a challenge to actually set one up whereas once you’ve got used to it, it just becomes part of your normal routine first assessment, set up CMC and then it’s done. [Lon5, hospice community doctor, London]
Some participants reported that EPaCCS were integrated into everyday clinical routines. In these instances, EPaCCS were referred to as being “part of what we do” [WY2, community/hospice, West Yorkshire]. This included ensuring that EPaCCS management was integrated into key care processes such as initial assessments, caseload reviews, admission and discharge planning, multidisciplinary team meetings, handover sheets, and standard operating procedures:
Whenever we take on a new patient onto the caseload, we will do our level best to have a conversation about the current EPaCCS system we use, which is Coordinate My Care, to get consent to put people on that system … it’s very much part of our mantra, it’s something that we do … We talk about Coordinate My Care at our weekly multidisciplinary team meetings, so we ask people to check that people are on there and if they’re not, we try and think of a plan to get somebody on there. [Lon26, hospice consultant nurse, London]
Theme 3: Championing Driving Implementation
Participants across all professional groups in both regions reflected on the role of colleagues who championed the use of EPaCCS. Champions were typically individuals who had been given dedicated time within their role to promote implementation and who encouraged staff engagement with EPaCCS. Champions used a range of approaches including offering peer support, taking active roles in teaching and education, presenting the potential benefits of EPaCCS, and keeping them present or “in view” in everyday clinical practice:
Having local champions who are just, [I] don’t want to say checking, but just ensuring that locally they’re being completed, that they’re demonstrating a difference. You know, there’s no point doing it if it’s not demonstrating any benefit really is there? [WY2, community/hospice consultant, West Yorkshire]
There were examples where engaging staff in the use of EPaCCS and learning how different systems work was described as a “constant recurring battle” [Lon06, hospital Clinical Nurse Specialist, London] that required time, dedication, and energy. This view was particularly present in hospital settings and the challenge was mainly attributed to high staff turnover. Different staff meant that the same messages and training had to be repeated continuously for EPaCCS to remain a priority for teams. However, such training did not always translate into increases in health professional use:
The reality is, I think that EPaCCS is underused, but generally across the hospital. That's why I have to be out there doing education and encouragement… it's continually education, trial, training, nudging, pushing to get them to use it because, a level of busyness, a churn of staff, you know they’re churning staff all the time, they’re coming from different Trusts who are not used to SystmOne, never mind EPaCCS, so it's a continual, continual, continual thing and training [WY7, hospital nurse, West Yorkshire]
Collective Action: How People Enact EPaCCS
Theme 4: collective contributions and buy-in.
Collective contributions referred to the extent to which health care professionals across settings of care contributed to the creation, sharing, updating, and use of EPaCCS records to inform care. Underpinning collective contributions was the degree to which health care professionals “bought into” EPaCCS by seeing them as a legitimate part of their role or as supporting the work of others. There was a general agreement that EPaCCS needed “buy-in from everyone - not just palliative care teams – for it to work ” [WY2, consultant, community/hospice consultant, West Yorkshire]. Despite this, health care professionals working in specialist palliative care were often the ones creating and updating EPaCCS records.
Participants had different perceptions in terms of the skills and capacity of professionals across different care settings to support advance care planning. Some felt that staff working in specialist palliative care were best placed to initiate sensitive conversations about advance care planning and end-of-life choices. Others reflected that although they believed health care professionals working outside of palliative care settings could broach advance care planning conversations, they did not always have the confidence to do so. Indeed, participant accounts suggested that when palliative care services were not involved in a patient’s care, this led to a general lack of clarity over who should do what, when, and how, which often resulted in the ad hoc creation of records.
If they’re working in specialist palliative care, most of those people will have those skills [for advance care planning]. If we then look at people who don’t deal exclusively with palliative care but see a lot of it, so district nurses, elderly medicine doctors, general practitioners, I think there is a lot of skill there. There’s not always the skill and there’s often a gap in confidence to apply the skills that people have … when people don’t have the skills and confidence, that first conversation where we seek, where we explain to the patient where they are in their illness and the fact that they’re in a palliative phase of their illness and seeking consent to use an EPaCCS doesn’t happen [WY6, hospice, West Yorkshire]
…in [our] Community Trust we’ve also got a respiratory service who are involved with people that are end stage of respiratory failure and we also have heart failure nurses and diabetic nurse specialists, and you know, those sorts of questions are talked about with patients often. But what we’re trying to do as a service in palliative care [non-specialist palliative care in Community Nurse Team] is encourage that to be done because it isn’t done as much as it should be really. You know when people are actually reaching sort of end-stage heart failure but yet nobody’s actually spoken to them about their wishes at the end of life. They feel it’s not their responsibility. [WY9, community nurse, West Yorkshire]
A concern among participants working in general practice was that it was difficult to contribute to EPaCCS because they did not always fit with their existing ways of working. Given the time constraints and competing priorities in general practice, accessing an EPaCCS record and then conducting and documenting advance care planning conversations was often seen as unmanageable and unrealistic:
we’ve only got a 10- or 15-minute window to see that patient for their current problem, so we don’t bother to update the CMC after just because of sheer time. So, unless you’re having a special CMC kind of session and you’ve dedicated a bit of time to go and do a home visit on someone or you’ve planned it in that you’re going to update the CMC and those wishes and concerns etc, that’s only when it really gets touched by the GP practice. [Lon16, GP, London]
Conversely, paramedics with access in London were likely to use EPaCCS records, typically because it helped decision-making around the urgent management of patients that they were hitherto unfamiliar with:
…we use it just as part of our decision making … I would say it’s a big part of my role… in the main bulk of my role which is in an ambulance setting I use it all the time, it’s second nature and it’s very valuable. [Lon29, paramedic, London]
Theme 5: Electronic Functionality, Interoperability, and Access
At a technical level, the integration of EPaCCS within existing electronic systems was important to their implementation. However, according to participants, this process of integration had not always occurred. Across most care settings in London, participants were frustrated that CMC was not seamlessly interoperable with existing electronic patient record systems. This lack of technical interoperability (ie, basic data exchange capabilities between systems) created a restrictive process that resulted in additional work because health care professionals had to remember (and frequently update) log-in details and enter duplicate information across different systems:
Coordinate My Care for us is a completely separate system … it doesn’t pull data from the current electronic system, you still have to kind of manually enter the patient’s name, address, NHS number … it is extra work … that kind of influence[s] how detailed a care record might be. Sometimes we will just put on the basic information that you think’s important … if it was integrated into a current kind of electronic system then I guess it would just make it easier. [Lon5, hospice community doctor, London]
In services across West Yorkshire, problems were caused by the fact that EPaCCS were embedded within several different electronic health record systems. However, because no mechanism in place allowed for the sharing of information between these systems, health care professionals could not always access relevant information from EPaCCS records when they needed it:
In this area a lot of folks were using SystmOne and we use EMIS … So, they [hospice services] can’t see what we’ve done on our system and it’s a bit messy … I know EPaCCS is supposed to be a document that everyone can access and fill in, but you can’t, ours is just on our system and ‘cos no one else can fill it in or see what’s been changed that’s where it falls down…. it is stupid that you can’t share an EPaCCS with anyone, it seems like a bit pointless [WY17, GP, West Yorkshire]
Reflexive Monitoring (“Appraisal Work”): Appraising the Value of EPaCCS—Theme 6: Confidence and Trust in EPaCCS
Participants across different regions and settings reflected on the potential value of EPaCCS as a tool that could facilitate the coordination of care. Others reflected on first-hand experiences of how EPaCCS were valuable in the context of crisis and out-of-hours care. In particular, paramedics who had access felt that EPaCCS provided vital information needed to effectively support person-centered decision-making with people whom they did not know:
If I saw a CMC for example where it was recorded that the patient had a preference for treatment care in the home, that would make it much more likely that I would dispatch one of my colleagues because we already know that that is the patient’s preferences and so as far as possible, we’re going to work to make that happen … End of life care pushes against the normal direction of paramedic care, [the] normal direction of paramedic care is rescue, save … end of life care obviously isn’t about life-saving, it’s about dignified death, symptom control management. It’s a change of thinking and so a lot of paramedics struggle with that, and I think they will look for anything that will help them guide them in that process and I think CMC is one that people are very familiar with using and generally find quite helpful. [Lon29, paramedic, London]
I’ve worked with the ambulance service in the time before it [EPaCCS] was standard practice and I would say it’s such a necessity now that we’ve got it, if we lost it I think it would literally be like losing my hand … it cuts out awkward conversations and it also cuts out us doing something that may be an issue would be against their wishes … it takes that anxiety or the uncertainty out of the what are we going to do and see what’s best for this patient. [Lon28, paramedic, London]
However, other professionals reported that EPaCCS records were sometimes of poor quality and that there were frequent problems with accessing the system. Consequently, this reduced their confidence that EPaCCS records contained sufficiently up-to-date information to support decision-making. Concerns were not about the potential of EPaCCS to improve care but regarding implementation issues such as restricted access, shareability, and inconsistent use of these records by staff. There was a fear that such problems could lead to patients receiving interventions and treatments that were against their stated and recorded wishes and preferences. This was particularly the case for paramedics who, without access to records, were more likely to make risk-averse decisions to hospitalize patients in the absence of knowing their wishes:
I can tell you categorically that we have not acted in the patient’s best interest … I’ll have taken somebody into hospital without my knowledge that [they have] an end-of-life care plan somewhere [WY21, paramedic, West Yorkshire]
Principal Results
This study explored factors that influenced the implementation of EPaCCS in routine clinical practice across different care settings in 2 major regions of England. It identifies and elaborates on challenges around the implementation of EPaCCS, including problems with access, and inconsistent use and engagement across settings. A key issue was technological limitations, with separate electronic health records often operating in parallel systems or failing to provide sufficient documentation or access. Such problems have led to the potential value of EPaCCS being unrealized.
Guided by sociotechnical systems theory [ 56 ], Figure 2 summarizes these issues by highlighting how interactions between the individual, team, organizational, and technical dimensions of EPaCCS affected implementation. The content of this figure is grounded in the data. It was generated inductively through highlighting relationships between each of our themes alongside how they related to different levels of practice. This allowed us to move beyond description by explaining linkages between themes and bringing them together in a way that tells an overarching story of health care professionals’ perspectives on the processes that influenced the implementation of EPaCCS.

Comparison With Prior Work
A key theme in this study was that limited buy-in and collective contributions to the creation, initiation, and use of EPaCCS across care settings affected implementation. Previous research has primarily used quantitative approaches to explore EPaCCS implementation, such as determining the proportion of EPaCCS records created across a specified population, and the average number of days that EPaCCS records are created before death [ 27 , 34 ]. However, our findings add novel and unique contributions by describing who initiates EPaCCS records, the factors that influence this, and the differences across regions. While some general practitioners and community nurses reported recording advance care planning discussions electronically, our study also highlights contributions made by health care professionals working across specialist palliative care settings. For some participants, providers of specialist palliative care were perceived as being better placed to initiate advance care planning conversations. A referral of a patient to specialist palliative care was perceived as affording greater time to interact with patients and other staff groups, alongside their experience in facilitating advance care planning discussions with patients and their families.
Participant experiences resonate with previously documented challenges related to advance care planning such as perceived lack of time, hesitancy in initiating conversations, and lack of care continuity [ 57 - 59 ]. Lack of clarity over who contributed to records and the timing of these contributions often resulted in poor-quality data. Such issues led to fears that EPaCCS records were incomplete or out of date, with some records being overly detailed or conversely, insufficiently informative to effectively support decision-making in out-of-hours or emergency care. The successful implementation of interventions that work across organizations (such as EPaCCS) relies on “whole systems” thinking [ 35 ]. Such implementation entails those involved in the use and implementation of EPaCCS (including commissioners and those responsible for service [re]design) accounting for the needs and influence of people working across different care settings and specialties.
In this study, care home staff reported having detailed discussions regarding residents’ wishes and preferences for care and documenting these within their own electronic systems. This aligns with previous research that the close relationships between care home staff and residents mean that staff are also well placed to have the sensitive and in-depth conversations required for advance care planning [ 60 ]. In this study, while electronic systems were reported to be used and engaged across care homes, the information contained within them was mostly inaccessible to external services. Care homes were also largely unable to access or provide helpful and detailed information from EPaCCS that could be used by other services. This highlights a key gap in the “whole systems” approach to EPaCCS. Addressing this gap is especially important given that care homes are projected to be the most common place of death in England by 2040 [ 61 ].
The implementation of EPaCCS at the individual, team, and organizational levels was affected by wider technological challenges. Issues related to the technical dimensions of EPaCCS have been well documented in the literature [ 13 , 30 , 33 , 36 ]. However, this study provides novel findings relating to health professional experiences of EPaCCS, further strengthened by its collection of data across 2 large geographical regions. This study builds on previous work and contributes details of how and why issues with access, functionality, and technical interoperability (ie, data integration, presentation, and exchange) [ 62 ] affected the implementation of EPaCCS across the United Kingdom. In London, challenges were experienced around the ability to move data between EPaCCS and existing electronic patient record systems (and vice versa) without duplication. Across West Yorkshire, a major interoperability issue was the failure of different electronic patient record systems to exchange advance care planning information. Moreover, while paramedics were most likely to use information within EPaCCS records in London to support decision-making in crisis contexts, they did not have this access across West Yorkshire. While these interoperability limitations affected health care professionals in different ways, they ultimately hindered the harnessing of the electronic information sharing and care coordination that EPaCCS is intended for.
Implications for Policy and Practice
Our findings highlight implications for practice relating to the use and implementation of electronic systems for palliative and end-of-life care. For complex interventions like EPaCCS to become normalized into everyday practice, they must fit within and enhance established systems of care [ 63 ]. It is also crucial that users can see their benefits to patient care and clinical practice compared to traditional ways of working [ 64 , 65 ]. However, these findings suggest that, in their current format, EPaCCS are not working as intended for facilitating person-centered care. Implementation challenges which resulted in missed opportunities to deliver care in line with recorded patient wishes, sometimes led to a loss of trust and confidence in EPaCCS, instead staff opted for more traditional means of communication and a return to traditional communication methods. Consequently, a redesign of EPaCCS is likely to be necessary to achieve the optimal configuration for successful implementation across different settings of care and geographical locations. To this end, we have generated a set of questions focusing on factors that were found to be influencing the uptake and use of EPaCCS across different settings of care (see Table 3 ).
| Level of action | Relevant to | Questions to consider |
| Individual or user | Professionals across settings of care involved in the creation, updating, reviewing, and use of electronic information sharing systems to inform decision-making | |
| Team or organizational | Team leaders and service management | |
| Technical or structural | Commissioners and policy makers |
While this study was conducted within England and discussed within the policy context of the United Kingdom, the policy implications have international relevance. The global strategy on digital health from the World Health Organization calls for the implementation of functional and interoperable electronic health records that can contribute to informed decision-making and high-quality, person-centered care [ 66 ]. Our findings highlight factors to consider when developing electronic systems for use in the delivery of palliative and end-of-life care. The questions presented in Table 3 , therefore, are likely to have relevance to policy makers and practitioners seeking to use and implement similar complex digital interventions (including electronic information-sharing systems) across multiple country and health care contexts. With increasing governmental policies on the development and implementation of health information technologies within the United Kingdom [ 62 ], these questions can guide efforts in the context of palliative and end-of-life care.
Strengths and Limitations
A strength and novelty of this work lies in the adoption of NPT to explain the processes across different levels of the health care system which affected whether and how EPaCCS were normalized into everyday practice. Through recruiting a wide range of health care professionals, across 5 settings of care, and 2 major regions within the United Kingdom, naturalistic generalizations [ 67 ] may be made from this work. That is, the findings of this study are likely to resonate with the personal experiences of healthcare professionals who use EPaCCS and similar health information technologies across end-of-life settings. We highlight 4 study limitations. First, we struggled to recruit community nurses across London, meaning that the application of study findings to this professional group is likely to be limited. Second, this study only sought the perspectives of health care professionals. Future research should explore patients' preferences on the content, sharing, and accessibility of their electronic records, alongside the impact of such digital interventions on the patient experience and clinical outcomes. Third, in line with other studies [ 68 ] throughout analysis, we found that the technical language of NPT and the overlapping of its components made deductively coding and interpreting data using this theoretical framework challenging. Fourth, we also appreciate that constructs comprising NPT focus on specific factors that influenced the implementation of EPaCCS in routine practice. Other implementation theories, models, and frameworks (eg, the Consolidated Framework for Implementation Research [ 69 ], Promoting Action on Research Implementation in Health Services [ 70 ], Capability, Opportunity, Motivation and Behaviour Theory [ 71 ]) may have provided different, yet equally valuable insights into answering the research question.
Conclusions
The successful implementation of digital interventions into routine care depends on the extent to which they enhance established ways of working with minimal disruption. EPaCCS represents just 1 approach to the electronic sharing of advance care plans, and other forms of digital advance care planning exist internationally. Integral to the implementation of digital advance care planning systems for palliative care is ensuring they can allow health care practitioners to document, access, use, and share information across multiple care settings. There also needs to be an effort at individual, team, and organizational levels to make sure that these tools are embedded into everyday care practices. It is paramount that they are championed within and between services, and that people know when, how, and why to use them. Commissioners, health care services, and practitioners should consider these multilevel factors when planning and rolling out digital advance care planning approaches.
Acknowledgments
This study is funded by the NIHR Health and Social Care Delivery Research Programme (NIHR129171). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. MA is a University Academic Fellow, funded through a research fellowship from Yorkshire Cancer Research. We wish to acknowledge Dr Samantha Coster, our colleague at King's College London, for her support and guidance in editing this article. This manuscript is published on behalf of the wider Optimal Care project team. Members of the team who are not included as authors on this manuscript but who were coapplicants and made significant contributions to the conceptualization and design of the project include Prof Michael Bennett (University of Leeds) and Dr Samuel Relton (University of Leeds, United Kingdom). We would also like to extend specific acknowledgment and recognition of our patient and public involvement lead for the Optimal Care project, Mrs Barbara Hibbert, who supported the development of project plans, formed our patient involvement group and facilitated inclusive and insightful patient and public involvement group meetings.
Data Availability
Deidentified transcripts generated and analyzed during this study are available from the corresponding author on reasonable request.
Authors' Contributions
MJA is the grant holder and Chief Investigator and was responsible for study conceptualization and development of the study protocol, with critical input from grant coapplicants, SR, RF, MT, KES, CJE, PC, and PMM. AB and JB conducted interviews with study participants. Analysis was led by AB and conducted with critical input and supervision from JB, MT, and MA. All authors had access to all study data, discussed the interpretation of findings, take responsibility for data integrity and analysis, contributed to the analysis plan, and provided critical comments and contributed to the writing and development of the manuscript. All authors reviewed the final manuscript. Artificial Intelligence was not used to generate any portions of the submitted manuscript.
Conflicts of Interest
This study is funded by the NIHR Health and Social Care Delivery Research Programme (NIHR129171). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. KES is the Laing Galazka chair at King’s College London, funded through an endowment from Cicely Saunders International and the Kirby Laing Foundation. MJA is a University Academic Fellow, funded through a research fellowship from Yorkshire Cancer Research. RF receives funding from the UK National Institute for Health and Care Research and is chair of the National Institute for Health and Care Excellence Implementation Strategy Group. We wish to acknowledge Dr Samantha Coster, our colleague at King's College London, for her support and guidance in editing this article. This manuscript is published on behalf of the wider Optimal Care project team. Members of the team who are not included as authors on this manuscript but who were coapplicants and made significant contributions to the conceptualization and design of the project include Prof Michael Bennett (University of Leeds) and Dr Samuel Relton (University of Leeds, United Kingdom). We would also like to extend specific acknowledgment and recognition of our patient and public involvement lead for the Optimal Care project, Mrs Barbara Hibbert, who supported the development of project plans, formed our patient involvement group and facilitated inclusive and insightful patient and public involvement group meetings.
COREQ (consolidated criteria for reporting qualitative research) checklist.
Interview topic guide.
- Twycross R. Introducing Palliative Care. United Kingdom. Radcliffe Publishing; 2003.
- Paparella G. Person-Centred Care in Europe: A Cross-Country Comparison of Health System Performance, Strategies and Structures. England. Picker Institute; 2016.
- WHO global strategy on integrated people-centred health services 2016-2026: Executive Summary. Geneva, Switzerland. World Health Organisation; 2015.
- Sleeman KE, Timms A, Gillam J, Anderson JE, Harding R, Sampson EL, et al. Priorities and opportunities for palliative and end of life care in United Kingdom health policies: a national documentary analysis. BMC Palliat Care. 2021;20(1):108. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Alderwick H, Dixon J. The NHS long term plan. BMJ. 2019;364:l84. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sudore RL, Lum HD, You JJ, Hanson LC, Meier DE, Pantilat SZ, et al. Defining advance care planning for adults: a consensus definition from a multidisciplinary delphi panel. J Pain Symptom Manage. 2017;53(5):821-832. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. 2014;28(8):1000-1025. [ CrossRef ] [ Medline ]
- Klingler C, in der Schmitten J, Marckmann G. Does facilitated advance care planning reduce the costs of care near the end of life? Systematic review and ethical considerations. Palliat Med. 2016;30(5):423-433. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Abel J, Pring A, Rich A, Malik T, Verne J. The impact of advance care planning of place of death, a hospice retrospective cohort study. BMJ Support Palliat Care. 2013;3(2):168-173. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Korfage IJ, Carreras G, Arnfeldt Christensen CM, Billekens P, Bramley L, Briggs L, et al. Advance care planning in patients with advanced cancer: a 6-country, cluster-randomised clinical trial. PLoS Med. 2020;17(11):e1003422. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Malhotra C, Shafiq M, Batcagan-Abueg APM. What is the evidence for efficacy of advance care planning in improving patient outcomes? A systematic review of randomised controlled trials. BMJ Open. 2022;12(7):e060201. [ CrossRef ]
- Rietjens J, Korfage I, van der Heide A. Advance care planning: not a panacea. Palliat Med. 2016;30(5):421-422. [ CrossRef ] [ Medline ]
- Allsop MJ, Chumbley K, Birtwistle J, Bennett MI, Pocock L. Building on sand: digital technologies for care coordination and advance care planning. BMJ Support Palliat Care. 2022;12(2):194-197. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Birtwistle J, Millares-Martin P, Evans CJ, Foy R, Relton S, Richards S, et al. Mapping and characterising electronic palliative care coordination systems and their intended impact: a national survey of end-of-life care commissioners. PLoS One. 2022;17(10):e0275991. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Huber MT, Highland JD, Krishnamoorthi VR, Tang JW. Utilizing the electronic health record to improve advance care planning: a systematic review. Am J Hosp Palliat Care. 2018;35(3):532-541. [ CrossRef ] [ Medline ]
- Lamas D, Panariello N, Henrich N, Hammes B, Hanson LC, Meier DE, et al. Advance care planning documentation in electronic health records: current challenges and recommendations for change. J Palliat Med. 2018;21(4):522-528. [ CrossRef ] [ Medline ]
- McCarthy S, Meredith J, Bryant L, Hemsley B. Legal and Ethical Issues Surrounding Advance Care Directives in Australia: Implications for the Advance Care Planning Document in the Australian My Health Record. J Law Med. 2017;25(1):136-149. [ Medline ]
- End of Life Care Strategy promoting high quality care for all adults at the end of life. UK. Department of Health; 2008.
- National Palliative and End of Life Care Partnership, Ambitions for Palliative and End of Life Care: A National Framework for Local Action 2021-2026. 2021. URL: https://www.england.nhs.uk/wp-content/uploads/2022/02/ambitions-for-palliative-and-end-of-life-care-2nd-edition.pdf [accessed 2024-06-18]
- Our Commitment to you for end of life care: the Government Response to the Review of Choice in End of Life Care. London. Department of Health; 2016.
- den Herder-van der Eerden M, van Wijngaarden J, Payne S, Preston N, Linge-Dahl L, Radbruch L, et al. Integrated palliative care is about professional networking rather than standardisation of care: a qualitative study with healthcare professionals in 19 integrated palliative care initiatives in five European countries. Palliat Med. 2018;32(6):1091-1102. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hsiao CJ, King J, Hing E, Simon AE. The role of health information technology in care coordination in the United States. Med Care. 2015;53(2):184-190. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Beernaert K, Cohen J, Deliens L, Devroey D, Vanthomme K, Pardon K, et al. Referral to palliative care in COPD and other chronic diseases: a population-based study. Respir Med. 2013;107(11):1731-1739. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Billingham MJ, Billingham S. Congruence between preferred and actual place of death according to the presence of malignant or non-malignant disease: a systematic review and meta-analysis. BMJ Support Palliat Care. 2013;3(2):144-154. [ CrossRef ] [ Medline ]
- Ko W, Deliens L, Miccinesi G, Giusti F, Moreels S, Donker GA, et al. EURO IMPACT. Care provided and care setting transitions in the last three months of life of cancer patients: a nationwide monitoring study in four European countries. BMC Cancer. 2014;14:960. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Smith C, Hough L, Cheung C, Millington-Sanders C, Sutton E, Ross JR, et al. Coordinate my care: a clinical service that coordinates care, giving patients choice and improving quality of life. BMJ Support Palliat Care. 2012;2(4):301-307. [ CrossRef ] [ Medline ]
- Allsop MJ, Kite S, McDermott S, Penn N, Millares-Martin P, Bennett MI. Electronic palliative care coordination systems: devising and testing a methodology for evaluating documentation. Palliat Med. 2017;31(5):475-482. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Finucane AM, Davydaitis D, Horseman Z, Carduff E, Baughan P, Tapsfield J, et al. Electronic care coordination systems for people with advanced progressive illness: a mixed-methods evaluation in Scottish primary care. Br J Gen Pract. 2020;70(690):e20-e28. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Palliative and end of life care information standard. Professional Record Standards Body. 2022. URL: https://prsb2.vercel.app/page/palliative-and-end-of-life-care-information-standard?hsCtaTracking=f03fff77-1ecb-44e3-955b- a56f038c83dd%7C52d83f23-deb4-48a6-99ef-5bd893ec26b6 [accessed 2024-06-18]
- Standing H, Patterson R, Lee M, Dalkin SM, Lhussier M, Bate A, et al. Information sharing challenges in end-of-life care: a qualitative study of patient, family and professional perspectives on the potential of an electronic palliative care Co-ordination system. BMJ Open. 2020;10(10):e037483. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Patterson R, Standing H, Lee M, Dalkin S, Lhussier M, Exley C, et al. Paramedic information needs in end-of-life care: a qualitative interview study exploring access to a shared electronic record as a potential solution. BMC Palliat Care. 2019;18(1):108. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Electronic palliative care co-ordination systems (EPaCCS). Public Health England. 2013. URL: https://www.gov.uk/government/publications/electronic-palliative-care-co-ordination-systems-epaccs [accessed 2024-06-18]
- Millares Martin P. Electronic palliative care coordination system (EPaCCS): interoperability is a problem. BMJ Support Palliat Care. 2018;8(3):358-359. [ CrossRef ] [ Medline ]
- Pocock L, Morris R, French L, Purdy S. Underutilisation of EPaCCS (electronic palliative care coordination systems) in end-of life-care: a cross-sectional study. BMJ Support Palliat Care. 2021:bmjspcare-2020-002798. [ CrossRef ] [ Medline ]
- Wye L, Lasseter G, Simmonds B, Duncan L, Percival J, Purdy S. Electronic palliative care coordinating systems (EPaCCS) may not facilitate home deaths: A mixed methods evaluation of end of life care in two English counties. Journal of Research in Nursing. 2016;21(2):96-107. [ CrossRef ]
- Petrova M, Riley J, Abel J, Barclay S. Crash course in EPaCCS (electronic palliative care coordination systems): 8 years of successes and failures in patient data sharing to learn from. BMJ Support Palliat Care. 2018;8(4):447-455. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Leniz J, Weil A, Higginson IJ, Sleeman KE. Electronic palliative care coordination systems (EPaCCS): a systematic review. BMJ Support Palliat Care. 2020;10(1):68-78. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stebbins RA. Exploratory research in the social sciences. London. Sage Publications; 2001.
- Bryman A. Social research methods. England. Oxford: Oxford University Press; 2004.
- Burke S. Rethinking 'validity' and 'trustworthiness' in qualitative inquiry: How might we judge the quality of qualitative research in sport and exercise sciences?, in Routledge Handbook of Qualitative Research in Sport and Exercise. London. Routledge; 2016:330-339.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-357. [ CrossRef ] [ Medline ]
- Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of medical research council guidance. BMJ. 2021;374:n2061. [ FREE Full text ] [ CrossRef ] [ Medline ]
- May CR, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci. 2009;4:29. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med. 2010;8:63. [ FREE Full text ] [ CrossRef ] [ Medline ]
- May C. Towards a general theory of implementation. Implement Sci. 2013;8:18. [ FREE Full text ] [ CrossRef ] [ Medline ]
- May CR, Albers B, Bracher M, Finch TL, Gilbert A, Girling M, et al. Translational framework for implementation evaluation and research: a normalisation process theory coding manual for qualitative research and instrument development. Implement Sci. 2022;17(1):19. [ FREE Full text ] [ CrossRef ] [ Medline ]
- McEvoy R, Ballini L, Maltoni S, O'Donnell CA, Mair FS, Macfarlane A. A qualitative systematic review of studies using the normalization process theory to research implementation processes. Implement Sci. 2014;9:2. [ FREE Full text ] [ CrossRef ] [ Medline ]
- May CR, Finch T, Ballini L, MacFarlane A, Mair F, Murray E, et al. Evaluating complex interventions and health technologies using normalization process theory: development of a simplified approach and web-enabled toolkit. BMC Health Serv Res. 2011;11:245. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Etikan I, Musa SA, Alkassim RS. Comparison of convenience sampling and purposive sampling. AJTAS. 2016;5(1):1. [ CrossRef ]
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753-1760. [ CrossRef ] [ Medline ]
- NVIVO. 2020. URL: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/support-services/nvivo-downloads/older-versions [accessed 2024-06-18]
- Ritchie L, Lewis J, Nicholls CM, Ormston R. Qualitative research practice: a guide for social science students and researchers. California. Los Angeles, CA: Sage; 2003.
- Finlay L. Negotiating the swamp: the opportunity and challenge of reflexivity in research practice. Qualitative Research. 2016;2(2):209-230. [ CrossRef ]
- Smith B, McGannon KR. Developing rigor in qualitative research: problems and opportunities within sport and exercise psychology. International Review of Sport and Exercise Psychology. 2017;11(1):101-121. [ CrossRef ]
- Sparkes A, Smith B. Qualitative Research Methods in Sport, Exercise & Health From Process to Product. London. Routledge; 2014.
- Papagiannidis S. TheoryHub book: A theory resource for students and researchers alike. UK. Theory for Explaining; 2022.
- Bernacki RE, Block SD, American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014;174(12):1994-2003. [ CrossRef ] [ Medline ]
- De Vleminck A, Houttekier D, Pardon K, Deschepper R, Van Audenhove C, Vander Stichele R, et al. Barriers and facilitators for general practitioners to engage in advance care planning: a systematic review. Scand J Prim Health Care. 2013;31(4):215-226. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jabbarian LJ, Zwakman M, van der Heide A, Kars MC, Janssen DJA, van Delden JJ, et al. Advance care planning for patients with chronic respiratory diseases: a systematic review of preferences and practices. Thorax. 2018;73(3):222-230. [ CrossRef ] [ Medline ]
- Bradshaw A, Ostler S, Goodman C, Batkovskyte I, Ellis-Smith C, Tunnard I, et al. Provision of palliative and end-of-life care in UK care homes during the Covid-19 pandemic: a mixed methods observational study with implications for policy. Front Public Health. 2023;11:1058736. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bone AE, Gomes B, Etkind SN, Verne J, Murtagh FE, Evans CJ, et al. What is the impact of population ageing on the future provision of end-of-life care? Population-based projections of place of death. Palliat Med. 2018;32(2):329-336. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sheikh A, Anderson M, Albala S, Casadei B, Franklin BD, Richards M, et al. Health information technology and digital innovation for national learning health and care systems. Lancet Digit Health. 2021;3(6):e383-e396. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dorr D, Bonner LM, Cohen AN, Shoai RS, Perrin R, Chaney E, et al. Informatics systems to promote improved care for chronic illness: a literature review. J Am Med Inform Assoc. 2007;14(2):156-163. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hall S, Murchie P, Campbell C, Murray SA. Introducing an electronic palliative care summary (ePCS) in Scotland: patient, carer and professional perspectives. Fam Pract. 2012;29(5):576-585. [ CrossRef ] [ Medline ]
- Carlfjord S, Lindberg M, Bendtsen P, Nilsen P, Andersson A. Key factors influencing adoption of an innovation in primary health care: a qualitative study based on implementation theory. BMC Fam Pract. 2010;11:60. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Global strategy on digital health 2020-2025. California. World Health Organisation; 2020.
- Smith B. Generalizability in qualitative research: misunderstandings, opportunities and recommendations for the sport and exercise sciences. Qualitative Research in Sport, Exercise and Health. 2017;10(1):137-149. [ CrossRef ]
- May CR, Cummings A, Girling M, Bracher M, Mair FS, May CM, et al. Using normalization process theory in feasibility studies and process evaluations of complex healthcare interventions: a systematic review. Implement Sci. 2018;13(1):80. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rycroft-Malone J. The PARIHS framework--a framework for guiding the implementation of evidence-based practice. J Nurs Care Qual. 2004;19(4):297-304. [ CrossRef ] [ Medline ]
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
| Coordinate My Care |
| consolidated criteria for reporting qualitative research |
| Electronic Palliative Care Coordination Systems |
| Normalization process theory |
Edited by A Mavragani; submitted 23.06.23; peer-reviewed by C Laranjeira, T Phenwan; comments to author 14.09.23; revised version received 18.10.23; accepted 30.05.24; published 16.08.24.
©Andy Bradshaw, Jacqueline Birtwistle, Catherine J Evans, Katherine E Sleeman, Suzanne Richards, Robbie Foy, Pablo Millares Martin, Paul Carder, Matthew J Allsop, Maureen Twiddy. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 16.08.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research (ISSN 1438-8871), is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
Embracing Gen AI at Work
- H. James Wilson
- Paul R. Daugherty

The skills you need to succeed in the era of large language models
Today artificial intelligence can be harnessed by nearly anyone, using commands in everyday language instead of code. Soon it will transform more than 40% of all work activity, according to the authors’ research. In this new era of collaboration between humans and machines, the ability to leverage AI effectively will be critical to your professional success.
This article describes the three kinds of “fusion skills” you need to get the best results from gen AI. Intelligent interrogation involves instructing large language models to perform in ways that generate better outcomes—by, say, breaking processes down into steps or visualizing multiple potential paths to a solution. Judgment integration is about incorporating expert and ethical human discernment to make AI’s output more trustworthy, reliable, and accurate. It entails augmenting a model’s training sources with authoritative knowledge bases when necessary, keeping biases out of prompts, ensuring the privacy of any data used by the models, and scrutinizing suspect output. With reciprocal apprenticing, you tailor gen AI to your company’s specific business context by including rich organizational data and know-how into the commands you give it. As you become better at doing that, you yourself learn how to train the AI to tackle more-sophisticated challenges.
The AI revolution is already here. Learning these three skills will prepare you to thrive in it.
Generative artificial intelligence is expected to radically transform all kinds of jobs over the next few years. No longer the exclusive purview of technologists, AI can now be put to work by nearly anyone, using commands in everyday language instead of code. According to our research, most business functions and more than 40% of all U.S. work activity can be augmented, automated, or reinvented with gen AI. The changes are expected to have the largest impact on the legal, banking, insurance, and capital-market sectors—followed by retail, travel, health, and energy.
- H. James Wilson is the global managing director of technology research and thought leadership at Accenture Research. He is the coauthor, with Paul R. Daugherty, of Human + Machine: Reimagining Work in the Age of AI, New and Expanded Edition (HBR Press, 2024). hjameswilson
- Paul R. Daugherty is Accenture’s chief technology and innovation officer. He is the coauthor, with H. James Wilson, of Human + Machine: Reimagining Work in the Age of AI, New and Expanded Edition (HBR Press, 2024). pauldaugh
Partner Center

Unbowed by Jan. 6 Charges, Republicans Pursue Plans to Contest a Trump Defeat
Mr. Trump’s allies are preparing to try to short-circuit the election system, if he does not win.
Nearly four years ago, Mr. Trump’s attempt to challenge the election results was chaotic and improvised. This year, his allies are systematically searching for any vulnerability in the nation’s election system. Credit... Scott McIntyre for The New York Times
Supported by
- Share full article

By Jim Rutenberg and Nick Corasaniti
- July 13, 2024
The Republican Party and its conservative allies are engaged in an unprecedented legal campaign targeting the American voting system. Their wide-ranging and methodical effort is laying the groundwork to contest an election that they argue, falsely, is already being rigged against former President Donald J. Trump.
The campaign involves a powerful network of Republican lawyers and activist groups, working loosely in concert with the Republican National Committee. Many of the key players were active in Mr. Trump’s attempt to overturn the results of the 2020 election.
But unlike the chaotic and improvised challenge four years ago, the new drive includes a systematic search for any vulnerability in the nation’s patchwork election system.
Mr. Trump’s allies have followed a two-pronged approach: restricting voting for partisan advantage ahead of Election Day and short-circuiting the process of ratifying the winner afterward, if Mr. Trump loses. The latter strategy involves an ambitious — and legally dubious — attempt to reimagine decades of settled law dictating how results are officially certified in the weeks before the transfer of power.
At the heart of the strategy is a drive to convince voters that the election is about to be stolen, even without evidence. Democrats use mail voting, drop boxes and voter registration drives to swing elections, they have argued. And Mr. Trump’s indictments and criminal conviction are a Biden administration gambit to interfere with the election, they claim.
“As things stand right now, there’s zero chance of a free and fair election,” Mike Howell, a project director at the Heritage Foundation, a conservative think tank, said at an event this week. “I’m formally accusing the Biden administration of creating the conditions that most reasonable policymakers and officials cannot in good conscience certify an election.”
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
Advertisement
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Henriksen K, Battles JB, Marks ES, et al., editors. Advances in Patient Safety: From Research to Implementation (Volume 4: Programs, Tools, and Products). Rockville (MD): Agency for Healthcare Research and Quality (US); 2005 Feb.

Advances in Patient Safety: From Research to Implementation (Volume 4: Programs, Tools, and Products).
Development of a planning tool to guide research dissemination.
Deborah Carpenter , Veronica Nieva , Tarek Albaghal , and Joann Sorra .
Affiliations
Investigation in patient safety improvement is constantly yielding new research results, yet efforts to put the results into practice are inconsistent. Therefore, a pragmatic tool is needed. The Dissemination Planning Tool was developed to assist the Agency for Healthcare Research and Quality (AHRQ) Patient Safety grantees with disseminating their research results. It was designed to help researchers consider major areas in dissemination: packaging research results, identifying target users, engaging connector organizations, identifying barriers, developing success measures, and allocating resources to implement the plan. Developing the tool included several stages, beginning with adapting Rogers' seminal diffusion theory. Literature was reviewed from health care, sociology, organizational development, psychology, and social sciences, thus providing a breath of dissemination theory and practices. Tools currently used in field-specific instances were reviewed. All of these sources were synthesized through a process of refinement, expert review, and testing.
- Introduction
New research results regularly provide an abundance of information to improve health care. Unfortunately, putting these results into practice often falls short of their envisioned potential. Even when research results are successfully disseminated, diffusion of the innovation occurs slowly, if at all. 1 In many cases, it sometimes takes decades to put research into practice. 2
Most grant-funding entities typically support basic research rather than intervention or implementation studies. An exception is the Agency for Healthcare Research Quality (AHRQ)—a division of the Department of Health and Human Services—which is committed to helping bridge the time gap between discovering scientific evidence and improving patient care. For example, through their Translating Research into Practice (TRIP) initiative, AHRQ aims to accelerate the impact of research on patient care to improve clinical outcomes and enhance cost effectiveness and efficiency using partnerships between researchers and health care organizations. 3 Beginning in 2001, AHRQ awarded a series of grants and contracts to stimulate research and demonstrations in patient safety and medical error reduction. These grants and contracts were collectively named the AHRQ Patient Safety Portfolio. AHRQ's Patient Safety Research Coordinating Center (AHRQ-PSRCC) provides assistance and support for the Patient Safety Portfolio in collaboration with the coordinating center's steering committee, whose members represent patient safety grantees across the portfolio. As with its TRIP initiative, AHRQ is committed to disseminating the research results from this portfolio to improve patient care practices, thus ultimately helping to make the health care system safer.
Dissemination and implementation are complex processes, involving many disciplines and players within an organization. No one approach or strategy universally applies in every situation. Researchers, therefore, need to use multiple methods and tools to navigate their dissemination course ( Figure 1 ). Members of the AHRQ-PSRCC and the steering committee developed a conceptual framework that gives context for the patient safety researchers' dissemination plans. The Framework for Knowledge Transfer of Patient Safety Research (Framework) includes three major processes: knowledge creation and distillation, mass diffusion and targeted dissemination, and organizational adaptation and use. 4 As an outgrowth of this conceptual framework, the AHRQ-PSRCC, in response to the steering committee's recommendation, developed a practical planning tool to help researchers spread actionable knowledge to potential users.
Components of a dissemination plan*. *A complete model of the Dissemination Planning Tool is available from the corresponding author
The process of implementing any research outcome begins with awareness—when potential users learn about the products, tools, or findings and gain some understanding about how they work. 5 This planning tool helps increase awareness in a systematic way by wedding the constructs of diffusion and dissemination. Diffusion is defined as a passive process by which an innovation is communicated through channels over time in a social system. 5 Dissemination involves a more active, tailored process of communication, with a goal of persuading users to adopt the innovation. 6 Alone, neither construct offers sufficient guidance for successful dissemination of research results; together, the ideas complement and support each other. Both constructs are embodied in the development of this planning tool to guide dissemination of research results.
- Purpose of the tool
The Dissemination Planning Tool was designed to help researchers create a dissemination plan that reaches beyond the traditional ways of getting the message out (e.g., peer-reviewed publications and conference presentations). Research shows that employing only traditional methods is ineffective. In a systematic review of 102 controlled trials examining the effectiveness of strategies for changing behavior, Oxman 7 found that passive approaches to sharing information, such as conference presentations, were less effective than social influencing interventions, such as having respected opinion leaders promote the innovation.
The planning tool encourages researchers to think through the dissemination process and to assemble the building blocks needed to construct a formal dissemination plan specific to their particular research and their intended users' needs and interests. Dissemination plans created by using this tool highlight ways that researchers can attain their unique project goals and reach target user audiences. The tool also helps researchers evaluate the best ways to distribute patient safety information by emphasizing the benefits of working with intermediaries and dissemination partners to amplify the reach to, and receptivity of, user communities.
The planning tool is useful at various points in the research process. One obvious time to complete it is toward the end of a research project, when findings are known or the research efforts have produced a product, tool, or program. Having the research results with associated evidence and pilot information on implementation can provide a compelling case for dissemination partners and end-users. The tool also is applicable at the early stage of the research proposal process—it can help determine user needs and dissemination partner interests. This information will refine research questions to address the users' practical questions. Using this tool will also plant the seeds of interest of both users and partners, enlisting their support throughout the project. 8, 9 Furthermore, this tool is appropriate for funding organizations that, through their grant solicitation structures, increasingly influence and guide researchers to consider and plan for dissemination as a key component of their initial research designs.
- Development and early testing
Developing the tool involved several stages, beginning with adapting Rogers' work on the theory of diffusion. 5 In particular, Rogers describes the innovation decision process in progressive stages: knowledge, persuasion, decision, implementation, and confirmation. The key processes in his first two stages involve understanding the innovation, including its importance and cost benefit; and identifying key adopters, their values and culture, and how to reach them. The aim of these processes is to convince the user of the merit of the innovation. Additional research that was applied in designing the tool was Lavis' 10 organizing approach for transferring knowledge, which includes specifying the message, the target audience, the messenger, how the message should be transferred, and how to evaluate the effect. We further reviewed relevant literature from health care, sociology, organizational development, change management, psychology, and social sciences, all of which provided a wide breadth of knowledge in dissemination theory and practices.
We also searched for existing dissemination self-assessment tools for researchers in the public domain. Although much literature has been produced on the implementation of research results, a pragmatic assessment tool that prepares patient safety researchers to effectively put their results into practice has yet to be developed. In fact, with one notable exception, The Dissemination Self Assessment Inventory from The National Center for the Dissemination of Disability Research (NCDDR), there appears to be an absence of practical dissemination planning tools for researchers. The NCDDR inventory is specifically aimed at disability researchers' dissemination efforts in the assessment of four areas: organizational structure and policies, research design, dissemination, and evaluation plans. 11
We synthesized all sources to identify key aspects of dissemination planning, and narrowed down to the current sections described later in this paper. We then developed draft questions to assess each of these key areas and invited expert reviews of the draft tool from a variety of disciplines. Reviewers included experienced health services researchers involved in patient safety research, national and international experts in dissemination research, professors involved in dissemination theory, knowledge management professionals, leaders in research dissemination organizations, and professionals who are responsible for developing and maintaining dissemination partnerships.
Based on their feedback, the tool transitioned through a series of iterations. For example, experts recommended that the questions be open-ended in order to help educate and stimulate researchers' thoughts about dissemination. This format was suggested over one featuring descriptive sentences with an agree/disagree scale of responses (a style that is frequently used in other instruments). Experts also wanted to include additional content to account for the human and financial resources needed for dissemination and to specify tactical activities and individuals responsible for achieving the activities. They also noted the importance of considering informal user networks, where, as evidence suggests, vital opportunities for dissemination exist. 12 They further encouraged highlighting the importance of linking research results to the agenda of connector organizations and recognizing the importance of timing—identifying events and issues in the partner's environment that may help or hinder their interest in the research results.
Patient safety researchers within the Patient Safety Portfolio also were recruited to complete the draft tool with their own research in mind. In line with the expert feedback, researchers also recommended adding an action planning section to help the respondent consider practical next steps to help make the plan operational.
- Description of the tool
The tool is intended to produce a working document that requires several iterations to fully complete. Changes are made as additional information emerges. While an individual such as the principal investigator may coordinate completing the tool, he or she should expect to consult with other members of the research team to fully capitalize on their knowledge and, importantly, to gain their support of the plan. The planning tool serves as a discussion structure for the team, with every member providing his or her unique perspective. Optimally, the dissemination planning team should include end users and partners to better understand their needs and, thus, the best possible methods for and approaches to “selling” the innovation.
The tool is structured into six sections: defining the research, identifying target users, working with dissemination partners, communicating the research, evaluating the success of the dissemination process, and developing an action plan. Each section builds on another to help researchers create their comprehensive plan. A construct rationale and overview for each section is briefly discussed below.
Research findings and products—what is going to be disseminated? Patient safety research efforts may yield several findings and/or tools that warrant distribution to other researchers or target users. This section helps researchers specifically identify what they want to disseminate and how to craft the value statement for the user. In traditional marketing terms, this section helps define the “product,” which is a fundamental step in the dissemination process. To define the product, the tool helps researchers consider ways to bundle or package their research. For example, if the research results include an event reporting system, the researcher could choose to disseminate it as a package, or separately disseminate the taxonomy or data analytic methods that were developed as a component of the reporting system. For each product that the researcher develops, an evaluation of its readiness for dissemination is vital. The planning tool helps researchers consider if the finding or product is ready for immediate use by assessing its track record of success in practice, the strength of scientific evidence that supports the results, and whether it conforms to established procedures. This evaluation of product-implementation readiness helps the researcher create a compelling value proposition to influence user interest.
End-users—who will apply it in practice? End-users are individuals or organizations that could benefit by applying the research results. Specifying end- users focuses the dissemination plan and targets the message. Change programs often do not work because they fail to involve formal structures and systems. 13 Understanding the behaviors of the end-users and the systems they work within is important in planning for dissemination, 14 because these user networks are a powerful milieu for sharing innovation. The Dissemination Planning Tool prompts the researcher to think about the users' (consumers') needs and values, and why the research is important to them (e.g., saves time, improves their work). User needs are often driven by external forces in the environment, such as regulatory pressures. The tool invites the researcher to think about related events that may help or hinder users' interest in their research. For example, a standard issued from the Joint Commission on Accreditation in Healthcare Organizations (JCAHO) on assessing organizational leadership responsibility in creating a nonpunitive culture may prompt a hospital administrator to seek a patient safety culture-assessment instrument. The Dissemination Planning Tool also prompts the researcher to think about barriers of user implementation and how to mitigate them. Considering the end-users' needs transforms the research message from a research-centric to a user-centric one, aimed at creating a pull from the users who will want to “buy the product.” Attracting users to the product, rather than pushing it on them, will enhance the dissemination effort. 15
Dissemination partners—how can you reach the users? End-users share information in both formal and informal social networks. 5 Because who introduces an innovation can influence how rapidly an innovation is disseminated, 16 social system norms can dictate how members communicate, and ultimately affect the rate of adoption. Dissemination is not a linear effort, but is often a fluid storytelling process. Informal spread of innovation—through networking, between users, or tapping into existing networks—is a powerful means of dissemination. The tool prompts researchers to list organizations with existing networks that can influence target users through their credibility, expertise, and power of their distribution capacity. By partnering with key intermediaries or connector organizations, researchers can capitalize on the organization's reach to tailor and amplify their message to users. A key strategy in implementing innovations in organizations involves aligning the innovation with organizational goals and values. 17 As in the end-user section, this section of the tool helps researchers think about the advantages for partners to take part in disseminating the research to help answer their inevitable “What's in it for me?” question.
Communication—how do you convey the research outcomes? Effective dissemination relies on using varied channels. Bero 18 found that multifaceted interventions were consistently effective in promoting change. While many communication strategies can influence provider practice, (e.g., published and unpublished material, education, academic detailing, etc.), Borenstein 19 suggests that it also is the frequency of exposure to different strategies that most influences behavior. Furthermore, it is important to match the complexity of the research with the right medium. This section of the tool helps researchers to identify ways that users get their information and, importantly, to recognize those channels that are available through identified connector organizations, such as Web sites and newsletters. User feedback about their information-seeking behavior also can provide insight into the best ways to promote the research.
Evaluation—how do you determine what worked? While the ultimate measure of success is improved patient care, this section of the tool helps the researcher think about interim process measures of success, such as the number of physicians who request additional information following a product demonstration. Evaluating the success of the dissemination plan is an iterative process. Dissemination is not a one-time activity, but a process that involves a long-term relationship with users and partners. Continuous feedback helps researchers appraise the effectiveness of their messages, such as what method or approach worked best or which method was most cost-effective. Researchers can use the feedback to improve their dissemination plan. Moreover, a working dialogue among the researchers, partners, and users can improve how the research is applied and mitigate potential barriers, such as those categorized by TRIP grantees (behavioral, structural, process, human subjects, partner, study site, and costs). 20
Dissemination workplan—where do you start? In addition to helping develop the dissemination plan, the tool further provides a final section to begin accounting for resources, both human and financial, that will realistically make it happen. Dissemination plans often fall short in two places. First, they become an unrealistic “shopping list” of every possible or desired use for the product that can be identified, but without realistic time and resource commitments. Second, no lead person is identified who would be responsible for ensuring that the tasks planned are actually performed. 21 The dissemination work plan section helps the researcher outline both immediate and long-term next-action steps with associated timeframes and people responsible. The work plan also prompts the researcher to consider what resources are needed to implement the dissemination plan.
- Conclusion and future developments
In their review, experts confirmed the need for a planning tool. Comments included “What a good idea!” and “This tool is an important contribution; there generally appears to be an absence of practical dissemination planning tools for researchers, and it is nice to see this need addressed.” Feedback from researchers who completed the tool also was positive: “I learned a great deal completing it”; “It provides explicit and detailed thinking”; “I plan to assemble the research team to gather additional input”; and “I found myself iterating my thinking as I went through each question—a very effective developmental tool.”
Receptivity to this planning tool and the noted dearth of similar tools reinforce the need to convert dissemination theory into practical tools and techniques. This is especially true as researchers strive to bring patient safety innovations into practice. In consideration of these dynamics, we recognize the need to further develop a dissemination toolkit that would provide additional self-help aids—such as detailed workbooks, project management templates, and resource tracking grids—to further advance the adoption and practice of worthy patient safety innovations.
Researchers traditionally have not been expected to think about dissemination of research results for use in practice. With the recent and ongoing importance given by funding agencies to translating research into practice, researchers will benefit by understanding the dissemination process and its practical application. This does not suggest that researchers will become experts in dissemination, but rather that they will develop a sensitivity to the value and opportunities inherent in this process. The Dissemination Planning Tool is designed to promote awareness among researchers about where their research might and should be applied in practice. It provides a structure to think about what can appear to be a nebulous charge to which researchers are increasingly expected to respond. More importantly, it helps them recognize the importance of the research's use and practical application.
- Acknowledgments
The authors gratefully acknowledge the contributions of the AHRQ-PSRCC Steering Committee members in developing the tool, including Nancy Donaldson, R.N., D.N.S., John Combes, M.D., and Christine Kovner, Ph.D., R.N.
- Cite this Page Carpenter D, Nieva V, Albaghal T, et al. Development of a Planning Tool to Guide Research Dissemination. In: Henriksen K, Battles JB, Marks ES, et al., editors. Advances in Patient Safety: From Research to Implementation (Volume 4: Programs, Tools, and Products). Rockville (MD): Agency for Healthcare Research and Quality (US); 2005 Feb.
- PDF version of this page (158K)
In this Page
Other titles in this collection.
- Advances in Patient Safety
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review From Science to Service: A Framework for the Transfer of Patient Safety Research into Practice. [Advances in Patient Safety: Fr...] Review From Science to Service: A Framework for the Transfer of Patient Safety Research into Practice. Nieva VF, Murphy R, Ridley N, Donaldson N, Combes J, Mitchell P, Kovner C, Hoy E, Carpenter D. Advances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology). 2005 Feb
- Review Updating Systematic Reviews [ 2007] Review Updating Systematic Reviews Shojania KG, Sampson M, Ansari MT, Ji J, Garritty C, Rader T, Moher D. 2007 Sep
- Review Beyond the Dusty Shelf: Shifting Paradigms and Effecting Change. [Advances in Patient Safety: Fr...] Review Beyond the Dusty Shelf: Shifting Paradigms and Effecting Change. McNeill D, Holland H, Henriksen K. Advances in Patient Safety: From Research to Implementation (Volume 3: Implementation Issues). 2005 Feb
- Making inpatient medication reconciliation patient centered, clinically relevant and implementable: a consensus statement on key principles and necessary first steps. [J Hosp Med. 2010] Making inpatient medication reconciliation patient centered, clinically relevant and implementable: a consensus statement on key principles and necessary first steps. Greenwald JL, Halasyamani L, Greene J, LaCivita C, Stucky E, Benjamin B, Reid W, Griffin FA, Vaida AJ, Williams MV. J Hosp Med. 2010 Oct; 5(8):477-85.
- Review Outcomes of adoption: measuring evidence uptake by individuals and organizations. [Worldviews Evid Based Nurs. 2004] Review Outcomes of adoption: measuring evidence uptake by individuals and organizations. Donaldson NE, Rutledge DN, Ashley J. Worldviews Evid Based Nurs. 2004; 1 Suppl 1:S41-51.
Recent Activity
- Development of a Planning Tool to Guide Research Dissemination - Advances in Pat... Development of a Planning Tool to Guide Research Dissemination - Advances in Patient Safety: From Research to Implementation (Volume 4: Programs, Tools, and Products)
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
COMMENTS
Innovative dissemination, then, means dissemination that goes beyond traditional academic publishing (e.g., academic journals, books, or monographs) and meetings (conferences and workshops) to achieve more widespread research uptake and understanding.
This guide is for researchers who are applying for funding or have research in progress. It is designed to help you to plan your dissemination and give your research every chance of being used.
Learn the necessary steps and best practices for getting your research results out into the world. Explore tips on how to plan effectively, use different tactics for dissemination, and maximize your…
ng or have research in progress. It is designed to help you to plan your dissemination and give your researc What does NIHR mean by dissemination? Effective dissemination is simply about getting the findings of your research to the people who can make use of them, to maximise the benefit of the research without delay.
How will you execute this plan? What actions and strategies will you take to disseminate your research? When and how frequently will you share your data and findings, including preliminary findings, your research process and methodology, and any lessons learned? When is it most valuable for each of your audiences to receive your research findings?
Dissemination Planning To ensure that the project results will be used, research projects must develop a dissemination plan that explains how the outcomes of the project will be shared with stakeholders, relevant institutions, organizations, and individuals. Specifically, a dissemination plan explains:
These toolkits contain guidelines, strategies, checklists, worksheets, templates, examples, and case studies for developing dissemination plans and products. This section contains toolkits that assist with planning for research dissemination and developing a dissemination plan. Developing a dissemination plan will help to facilitate the uptake ...
The push towards greater public understanding of science and research since the 1980s, and an emphasis on engagement and participation of non-research audiences have brought about new forms of dissemination [9]. These approaches include popular science magazines and science shows on television and the radio.
The latter may take the form of either oral (platform) or poster presentations. Presenting clinical or practice research at a professional meeting offers the opportunity to disseminate research findings quickly, since the lag time between completing the research and presenting at a conference may be short.
Conclusions Effective dissemination of research to US policymakers exists; yet, rigorous quantitative evaluation is rare. A number of cross-cutting strategies appear to enhance the translation of research evidence into policy.
Dissemination Plan Examples The Community Voice: A Photovoice Project Identifying Barriers and Facilitators to Health and Health Care
Dissemination Planning Tool. Purpose. AHRQ is increasingly interested in research that has "real world" impact in the practice of health care. This tool will help you, the Patient Safety Researcher, develop a plan for disseminating your research findings and products to potential users in the health care system.
The European Commission designed and is implementing a dissemination and exploitation strategy to support funding beneficiaries taking their results a step further e.g. market uptake, wider scientific use, advice for policymaking, etc. The Commission supports this by. offering free tailor-made dissemination and exploitation support services.
What is dissemination? Dissemination is "the intentional, active process of identifying target audiences and tailoring communication strategies to increase awareness and understanding of evidence and motivate its use in policy, practice, and individual choice" (PCORI ). 1 Simply put, dissemination is about getting research results to the people who can benefit from those findings.
Building a Dissemination Strategy To aid E4A applicants and other researchers in developing a plan for disseminating their findings, we've put together a dissemination strategy template ( access the Google doc version ). The template is structured in such a way to guide folks through a step-by-step process from identifying objectives to selecting communications tactics and materials. Each ...
Background Addressing deficiencies in the dissemination and transfer of research-based knowledge into routine clinical practice is high on the policy agenda both in the UK and internationally. However, there is lack of clarity between funding agencies as to what represents dissemination. Moreover, the expectations and guidance provided to researchers vary from one agency to another. Against ...
We define dissemination as a planned process that involves consideration of target audiences and the settings in which research findings are to be received and, where appropriate, communicating and interacting with wider policy and health service audiences in ways that will facilitate research uptake in decision-making processes and practice.
Effective dissemination and communication are vital to ensure that the conducted research has a social, political, or economical impact. They draw attention of governments and stakeholders to research results and conclusions, enhancing their visibility, comprehension, and implementation.
Plan/Act Prepare a detailed report of the research, including the results, for submission to a scientific journal. Present research results at one or more scientific conferences. Post detailed methodology, including statistical approach, and raw data to a publicly-available web site or make this information available upon requests.
2 Dissemination Plan for Research on Hospital Readmission Introduction Poot et al. (2021) indicated that in the rapidly changing health care environment, dissemination of research information is the most important factor for achieving better treatment and improving the health of patients. For prospective nurses, it is crucial to understand the value of communicating evidence-based practices ...
Many funded research projects require a dissemination plan. However, even if not, the formal exercise of creating a plan at the outset that organises dissemination around distinct milestones in the research life cycle will help you to assign roles, structure activities, as well as plan funds to be allocated in your dissemination.
Background: Palliative care aims to improve the quality of life for people with life-limiting illnesses. Advance care planning conversations that establish a patient's wishes and preferences for care are part of a person-centered approach. Internationally, electronic health record systems are digital interventions used to record and share patients' advance care plans across health care ...
Most top-down, target-driven transformation programs fail to produce lasting results. Bain's research on over 350 companies worldwide found that only one in 12 target-driven transformations ...
Introduction: Translating research findings into practice requires understanding how to meet communication and dissemination needs and preferences of intended audiences including past research participants (PSPs) who want, but seldom receive, information on research findings during or after participating in research studies.
Research is shedding light on different chromosomal make-ups and what advantages they may bring to sport.
As a federal supreme court shut down Johnson & Johnson's third attempt at bankruptcy to settle thousands of talc ovarian cancer lawsuits in federal and state courts, sources say the health care giant may have received enough plaintiff votes in favor of its $6.5 billion settlement offer.. The baby powder maker faces about 61,000 lawsuits that claim the company's talc products led people to ...
Effective dissemination of evidence is important in bridging the gap between research and policy. In this paper, we list 10 approaches for improving the visibility of research findings, which in turn will hopefully contribute towards changes in policy. ...
This article describes the three kinds of "fusion skills" you need to get the best results from gen AI. ... According to our research, most business functions and more than 40% of all U.S ...
The effort involves a sprawling network of groups and includes some people that worked to overturn the results in 2020 — a campaign that led to federal and state criminal charges against Mr ...
Investigation in patient safety improvement is constantly yielding new research results, yet efforts to put the results into practice are inconsistent. Therefore, a pragmatic tool is needed. The Dissemination Planning Tool was developed to assist the Agency for Healthcare Research and Quality (AHRQ) Patient Safety grantees with disseminating their research results. It was designed to help ...