The 8 Principles of Primary Health Care: A Comprehensive Guide
- by Laura Rodriguez
- October 4, 2024
Primary Health Care (PHC) is the foundation of a well-functioning healthcare system . It is a holistic approach that focuses on providing essential healthcare services to individuals and communities, with the aim of promoting health and well-being for all. But what exactly are the principles of primary health care?
In this blog post, we will explore the 8 key principles that form the bedrock of primary health care. From understanding why these principles are crucial to discovering their practical applications, we will delve into the core concepts that shape the provision of primary health care in the modern world. So, whether you are a healthcare professional, a student, or simply curious about healthcare systems, get ready to dive into the fundamental principles that govern primary health care in 2023.
But first, let’s start with a brief introduction to primary health care and why it holds such significance in today’s healthcare landscape.


Primary Health Care: Understanding the 8 Principles
Primary health care is the backbone of healthcare systems worldwide, aiming to provide accessible, comprehensive, and patient-centered care. To achieve this goal, primary health care is guided by eight fundamental principles. Let’s take a closer look at these principles and uncover their significance in shaping the delivery of primary care services.
Principle 1: Accessibility – Unlocking the Doors to Health
The first principle of primary health care is Accessibility . This principle emphasizes the importance of ensuring that essential health services are available to all individuals, regardless of their socioeconomic status or geographical location. In essence, it aims to unlock the doors to health and remove any barriers that might prevent people from receiving the care they need.
Principle 2: Empowerment – Putting Health in Your Hands
Empowerment forms the second principle, highlighting the need to empower individuals and communities in managing and making decisions about their own health. It recognizes the importance of active participation and collaboration between health professionals and patients, fostering a sense of ownership and self-determination in achieving optimal health outcomes.
Principle 3: Health Promotion – Prevention is Better than Remedying
Health Promotion underlies the third principle, emphasizing the significance of prevention in healthcare. By focusing on disease prevention and health promotion, primary health care aims to reduce the incidence of illnesses before they occur. Encouraging healthy lifestyles, immunizations, and regular screenings are essential aspects of this principle.
Principle 4: Coordinated Care – Building Bridges for Better Health
Primary health care places great importance on Coordinated Care , ensuring that all aspects of an individual’s health are addressed comprehensively. It advocates for the seamless integration of services across different healthcare providers , facilitating smooth transitions and effective communication between healthcare professionals, ultimately leading to better health outcomes.
Principle 5: Quality – The Assurance of Excellent Care
The fifth principle revolves around Quality – a crucial element necessary for delivering excellent healthcare services. Primary health care aims to provide care that is safe, effective, and patient-centered. Through continuous quality improvement initiatives and adherence to evidence-based practices, primary health care strives to meet the highest standards of medical care.
Principle 6: Cultural Sensitivity – Embracing Diversity
Cultural Sensitivity represents the sixth principle, emphasizing the need to respect and embrace the diversity of patients’ cultural backgrounds. By being aware of cultural norms, beliefs, and values, healthcare professionals can build trust and enhance communication with patients. This principle recognizes that cultural competence is integral in delivering healthcare that meets the unique needs of individuals and communities.
Principle 7: Equity – Leveling the Playing Field
Equity forms the seventh principle and focuses on promoting fairness in healthcare. It acknowledges that certain groups may face disadvantages or experience barriers to healthcare access due to various factors, such as socioeconomic status or discrimination. Primary health care seeks to address these disparities and ensure that everyone has an equal opportunity to achieve the highest level of health.
Principle 8: Sustainability – Paving the Way for Future Generations
The final principle, Sustainability , highlights the importance of maintaining primary health care services for future generations. By adopting sustainable practices and policies, primary health care aims to ensure that the necessary resources and infrastructure are available to meet the evolving healthcare needs of communities in the years to come.
Understanding these eight principles is essential in appreciating the comprehensive and patient-centered approach primary health care aims to provide. By embracing accessibility, empowerment, health promotion, coordinated care, quality, cultural sensitivity, equity, and sustainability, primary health care strives to be the cornerstone of a healthy society. So, let’s continue championing primary health care and unlock the doors to a healthier future for all!

FAQ: What are the 8 principles of primary health care?
What are the 8 elements of primary health care.
Primary health care encompasses eight key elements that form the foundation of comprehensive and effective healthcare delivery:
Accessible healthcare : Primary health care should be universally accessible to all individuals, regardless of their socioeconomic background or geographic location. Everyone should have the right to receive essential healthcare services.
Public participation : Community involvement and active participation are essential in primary health care. It is crucial for individuals and communities to have a say in the decision-making processes that affect their health and wellbeing.
Health promotion : Primary health care emphasizes proactive measures to prevent diseases and promote overall well-being. It focuses on educating individuals about healthy lifestyles, disease prevention, and the importance of early intervention.
Preventive care : Primary health care places a strong emphasis on prevention rather than solely treating illnesses. Regular check-ups, immunizations, and screenings help identify potential health risks early on and allow for timely interventions.
Integrated care : Primary health care aims to provide holistic and comprehensive care that addresses not only physical health but also mental, emotional, and social well-being. It reinforces the importance of coordinating care across different healthcare providers and specialties.
Multi-sectoral collaboration : Primary health care recognizes that health is influenced by various social, economic, and environmental factors. Collaboration with sectors such as education, housing, and transportation helps address these determinants of health and promotes a more inclusive approach to care.
Equity : Primary health care serves as a means to achieve health equity by ensuring that everyone has fair and equal access to healthcare services, regardless of their income, race, gender, or other social determinants of health.
Appropriate use of technology : Primary health care leverages technology to enhance healthcare delivery, improve access to information, and support decision-making processes. It recognizes the potential of technology in bridging gaps and reaching underserved populations.
Why are the principles of care important
The principles of primary health care play a critical role in shaping healthcare systems and promoting better health outcomes for individuals and communities. These principles ensure that healthcare is accessible, comprehensive, and focused on prevention and wellness. By emphasizing public participation and multi-sectoral collaboration, primary health care creates a more patient-centered and community-driven approach to healthcare. Furthermore, the principles of care help address health inequities and strive for equal opportunities for all individuals to achieve optimal health and well-being.
What are the 12 care domains
Primary health care encompasses twelve essential care domains that cover various aspects of healthcare:
- Health promotion
- Disease prevention
- Diagnosis and treatment
- Rehabilitation and palliative care
- Maternal and child health
- Mental health
- Chronic disease management
- Emergency care
- Infectious disease control
- Nutrition and food safety
- Environmental health
- Social determinants of health
These care domains ensure that primary health care addresses the diverse needs of individuals and communities, providing comprehensive care across the lifespan and addressing the various determinants that impact health.
What are the 14 components of primary health care
Primary health care consists of fourteen key components that contribute to its effectiveness and comprehensiveness:
- Accessible and equitable healthcare services
- Health workforce development and training
- Adequate health infrastructure and resources
- Essential medicines and technologies
- Health information system
- Financing and affordability of healthcare
- Health legislation and policies
- Governance and leadership in healthcare
- Health research and innovation
- Community engagement and participation
- Health promotion and education
- Quality and safety in healthcare delivery
- Monitoring and evaluation of health services
- Collaboration and coordination with other sectors
These components work together to ensure that primary health care addresses the varying healthcare needs of individuals and communities, regardless of their location or socioeconomic status.
How many essential elements does PHC have
Primary health care has eight essential elements that form its foundation. These elements include accessible healthcare, public participation, health promotion, preventive care, integrated care, multi-sectoral collaboration, equity, and the appropriate use of technology. These elements collectively contribute to the effectiveness and success of primary health care in providing comprehensive and patient-centered healthcare services.
What are the 5 elements of primary health care
Primary health care encompasses eight key elements:
- Accessible healthcare
- Public participation
- Preventive care
- Integrated care
- Multi-sectoral collaboration
- Appropriate use of technology
These elements serve as guiding principles for primary health care and aim to ensure comprehensive and inclusive healthcare delivery.
Who is the father of PHC
The father of primary health care is Dr. Halfdan Mahler. As the director-general of the World Health Organization (WHO) from 1973 to 1988, Dr. Mahler played a pivotal role in shaping the concept of primary health care and advocating for its implementation worldwide. His leadership and vision laid the foundation for the principles and values that primary health care embodies today.
What are the three principles of primary health care
Primary health care adheres to three core principles:
Universality: Primary health care should be accessible and available to all individuals, regardless of their background or circumstances.
Equity: Primary health care aims to reduce health disparities and promote equal opportunities for health for all individuals.
Participation: Individuals and communities should actively participate in decision-making processes and have a voice in matters that affect their health and well-being.
These principles ensure that primary health care is patient-centered, comprehensive, and focused on achieving health equity.
What is primary health care (PHC)
Primary health care (PHC) refers to the essential healthcare services that are universally accessible and provided as the first point of contact with the healthcare system. It encompasses a wide range of health promotion, disease prevention, diagnosis, treatment, and rehabilitation services. Primary health care serves as the foundation of healthcare systems, focusing on comprehensive and continuous care to address individuals’ physical, mental, and social well-being.
What are the principles of health
The principles of health encompass various factors that contribute to overall well-being and optimal functioning. These principles can include:
Physical well-being: Maintaining a healthy body through proper nutrition, regular physical activity, and preventive healthcare measures.
Mental and emotional well-being: Nurturing positive mental health, managing stress, seeking support when needed, and promoting emotional resilience.
Social well-being: Building and maintaining healthy relationships, fostering a sense of belonging and connectedness, and participating in community activities.
Spiritual well-being: Connecting with one’s beliefs, values, and understanding of purpose, and finding meaning in life.
The principles of health highlight the interconnectedness of these various dimensions and emphasize the importance of addressing each aspect to achieve overall well-being.
What are the 6 principles of primary health
Primary health care operates based on six core principles:
Accessibility: Primary health care should be easily accessible to all individuals, regardless of their location or socioeconomic status.
Public participation: Individuals and communities have the right to actively participate in decisions affecting their health and well-being.
Health promotion and disease prevention: Proactive measures are essential to prevent diseases, promote healthy behaviors, and enhance overall well-being.
Integrated care: Primary health care aims to provide comprehensive care that addresses not only physical health but also mental, emotional, and social well-being.
Multi-sectoral collaboration: Collaborating with various sectors like education, housing, and transportation helps address social determinants of health and promote a holistic approach to care.
Equity and social justice: Primary health care strives to reduce health disparities and ensure access to quality healthcare for all individuals, regardless of their background or circumstances.
What are the functions of primary health care
Primary health care serves several important functions in healthcare systems:
Disease prevention and health promotion: Primary health care focuses on preventing diseases and promoting healthy habits through education, screenings, immunizations, and lifestyle interventions.
Diagnosis and treatment: Primary health care providers serve as the first point of contact for individuals seeking healthcare services, conducting initial evaluations, providing diagnosis, and initiating treatment plans.
Comprehensive care: Primary health care offers holistic and continuous care that addresses physical, mental, and social well-being. It involves coordinating care across different healthcare providers and specialties.
Referrals and coordination: Primary health care professionals help individuals navigate the healthcare system, referring them to appropriate specialists when necessary and ensuring seamless care coordination.
Health education: Primary health care providers play a vital role in educating individuals about disease prevention, self-care management, and healthy lifestyle choices.
Monitoring and surveillance: Primary health care contributes to monitoring population health trends, identifying emerging health issues, and implementing surveillance systems for timely interventions.
What are the 4 A’s in primary health care
The 4 A’s in primary health care refer to four key elements that characterize effective primary care:
Accessible care : Primary health care should be easily accessible to individuals, ensuring that they can seek healthcare services when needed without barriers such as distance, cost, or discrimination.
Available care : Adequate healthcare resources and services should be in place to meet the population’s needs, ensuring that timely care is available to all individuals.
Affordable care : Primary health care should be affordable, taking into consideration individuals’ financial circumstances and ensuring that cost is not a barrier to accessing essential healthcare services.
Appropriate care : Primary health care should provide appropriate and evidence-based care that meets individuals’ health needs, ensuring that the care delivered aligns with established guidelines and best practices.
These four elements collectively contribute to the effectiveness and success of primary health care in delivering comprehensive and patient-centered healthcare services.
What are the four pillars of primary health care
Primary health care rests upon four essential pillars:
Preemptive care: Emphasizes proactive measures to prevent diseases and promote healthy lifestyles, focusing on health promotion and disease prevention.
Comprehensive care: Encompasses a broad range of healthcare services that address individuals’ physical, mental, and social well-being, providing holistic care that considers all aspects of health.
Coordinated care: Primary health care strives to ensure continuity of care by coordinating services across different healthcare providers and specialties, ensuring that individuals receive integrated and seamless care.
Community engagement: Individuals and communities are actively involved in decision-making processes, with their input shaping healthcare policies, programs, and services. Community engagement facilitates a patient-centered approach and ensures that healthcare meets specific community needs.
Together, these pillars create a strong foundation for primary health care, promoting inclusivity, accessibility, and quality healthcare services.
What are the 9 elements of primary health care
Primary health care encompasses nine key elements that contribute to its effectiveness:
Accessibility: Ensuring that healthcare services are easily accessible to all individuals, regardless of their location or socioeconomic status.
Public participation: Encouraging community engagement in healthcare decision-making processes, giving individuals a voice in shaping healthcare policies and services.
Health promotion: Focusing on proactive measures to promote health and prevent diseases, emphasizing the importance of education, lifestyle modification, and early intervention.
Prevention: Implementing strategies to prevent diseases and injuries through immunizations, screenings, and risk factor assessment.
Treatment and care: Providing timely diagnosis, treatment, and ongoing care to individuals, ensuring that their healthcare needs are met.
Coordination: Coordinating care across different healthcare providers and specialties to ensure comprehensive and integrated healthcare delivery.
Equity: Addressing health inequities by providing fair and equal access to healthcare services for all individuals, regardless of their background or circumstances.
Efficient use of resources: Optimizing the use of available healthcare resources to ensure cost-effective and sustainable healthcare delivery.
Appropriate technology: Utilizing technology to enhance healthcare delivery, improve access to information, and support decision-making processes.
These elements collectively contribute to the success and effectiveness of primary health care in meeting the healthcare needs of individuals and communities.
What are the six elements of primary health care
Primary health care encompasses six core elements:
Accessibility: Ensuring that healthcare services are geographically, financially, and culturally accessible to all individuals, promoting equal opportunities for healthcare.
Health promotion and disease prevention: Focusing on proactive measures to promote healthy behaviors, prevent diseases, and improve overall well-being.
Comprehensive care: Providing a wide range of healthcare services that address physical, mental, and social well-being, ensuring holistic care for individuals and communities.
Coordination: Coordinating care across different healthcare providers and specialties to ensure seamless and integrated healthcare delivery.
Community participation: Encouraging active involvement from individuals and communities in healthcare decision-making processes, recognizing the importance of community engagement in shaping healthcare services.
Equity: Addressing health disparities and promoting equal access to healthcare services for all individuals, regardless of their socioeconomic background or other determinants of health.
These elements collectively contribute to the effectiveness and success of primary health care in providing comprehensive and inclusive healthcare services.
What is the meaning of Alma Ata
Alma Ata refers to the Declaration of Alma Ata, a significant milestone in the history of primary health care. It was adopted at the International Conference on Primary Health Care held in Alma Ata, Kazakhstan, in 1978. The declaration emphasized the importance of primary health care in achieving better health outcomes for all individuals and reaffirmed health as a fundamental human right. The Alma Ata Declaration called for universal access to healthcare, community participation, intersectoral collaboration, and a strong focus on prevention and promotion. This declaration laid the foundation for the principles and values that primary health care embodies today.
What are the 10 principles of primary health care
The ten principles of primary health care, as outlined in the Alma Ata Declaration, are as follows:
Universality: Primary health care should be accessible to all individuals, regardless of their geographic location or socioeconomic background.
Equity: Primary health care should strive for equity in healthcare, aiming to reduce health disparities and ensure equal opportunities for health for all individuals.
Community engagement: Individuals and communities should participate in decision-making processes that affect their health, ensuring that healthcare services are tailored to their specific needs.
Intersectoral collaboration: Collaboration with other sectors such as education and housing is crucial to address the social determinants of health and promote a holistic approach to care.
Empowerment: Primary health care should empower individuals to take charge of their own health and make informed decisions about their
- active participation
- collaboration
- communities
- comprehensive
- disease prevention
- essential healthcare services
- health promotion
- overall well-being
- primary health care
- well-functioning healthcare system
Laura Rodriguez
You may also like, mystery solved: unraveling the enigma of ash’s family in pokémon, how tall is jim halpert unveiling the height of the office’s beloved prankster.
- by Thomas Harrison
How to Fully Power Your Beacon: A Comprehensive Guide
- by Donna Gonzalez
Welcome to the World of YouTube: How Much Does a YouTuber with 10 Million Subscribers Make?
- by Mr. Gilbert Preston
Will Killer Frost Get Out of Jail? Exploring the Fate of Caitlin Snow in The Flash
- by Daniel Taylor
Real Estate Blog: Understanding RBA in the Property Market
Public Health Notes
Your partner for better health, primary health care (phc): history, principles, pillars, elements & challenges.
December 10, 2020 Kusum Wagle Global Health 0

Table of Contents

Table of Contents:
What is primary health care (phc).
- History of Primary Health Care
- Objectives of Primary Health Care (PHC)?
- Principles of Primary Health Care (PHC):
- What are the Pillars of PHC?
- Elements/components of PHC
Why is Primary Health Care (PHC) Important?
What are the challenges for implementation of phc, what are the mitigation measures for ensuring effective phc.
- References and For More Information
- Primary Health Care (PHC) is the health care that is available to all the people at the first level of health care.
- According to World Health Organization (WHO), ‘Primary Health Care is a basic health care and is a whole of society approach to healthy well-being, focused on needs and priorities of individuals, families and communities.’
- Primary Health Care (PHC) is a new approach to health care which integrates at the community level all the factors required for improving the health status of the population.
- Primary health care is both a philosophy of health care and an approach to providing health services.
- It addresses the expansive determining factor of health and ensures whole person care for health demands during the course of the natural life.
- It is developed with the concept that the people of the country receive at least the basic minimum health services that are essential for their good health and care.
History of Primary Health Care:
- Before 1978, globally, existing health services were failing to provide quality health care to the people.
- Different alternatives and ideas failed to establish a well-functioning health care system.
- Considering these issues, a joint WHO-UNICEF international conference was held in 1978 in Alma Ata (USSR), commonly known as Alma-Ata conference.
- The conference included participation from government from 134 countries and other different agencies.
- The conference jointly called for a revolutionary approach to the health care.
- The conference declared ‘The existing gross inequality in the health status of people particularly between developed and developing countries as well as within countries is politically, socially and economically unacceptable’.
- Thus, the Alma-Ata conference called for acceptance of WHO goal of ‘Health for All’ by 2000 AD.
- Furthermore, it proclaimed Primary Health Care (PHC) as a way to achieve ‘Health for All’.
- In this way, the concept of Primary Health Care (PHC) came into existence globally in 1978 from the Alma-Ata Conference .
Objectives of Primary Health Care (PHC):
- To increase the programs and services that affect the healthy growth and development of children and youth.
- To boost participation of the community with government and community sectors to improve the health of their community.
- To develop community satisfaction with the primary health care system.
- To support and advocate for healthy public policy within all sectors and levels of government.
- To support and encourage the implementation of provincial public health policies and direction.
- To provide reasonable and timely access to primary health care services.
- To apply the standards of accountability in professional practice.
- To establish, within available resources, primary health care teams and networks.
- To support the provision of comprehensive, integrated, and evidence-based primary health care services.
Five (5) Principles of Primary Health Care (PHC):
- Social equity
- Nation-wide coverage/wider coverage
- Self- reliance
- Intersectoral coordination
- People’s involvement (in planning and implementation of programs)
What are the Pillars of Primary Health Care (PHC)?
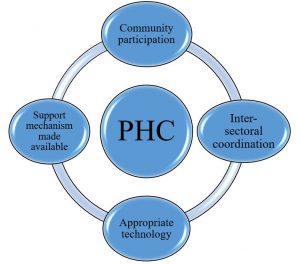
FIG: PILLARS OF PRIMARY HEALTH CARE
- Primary health care consists of an integrative group of health care professionals coordinating to provide basic health care services to a particular group of people or population.
- The Primary Health care outline is built on four key pillars.
- These pillars are reinforcement for the delivery of safe health care.
The four major pillars of primary health care are as follows:
- Community Participation
- Inter-sectoral Coordination
- Appropriate Technology
- Support Mechanism Made Available
1. Community Participation
- Community participation is a process in which community people are engaged and participated in making decisions about their own health.
- It is a social approach to point out the health care needs of the community people.
- Community participation involves participation of the community people from identifying the health needs of the community, planning, organizing, decision making and implementation of health programs.
- It also ensures effective and strategic planning and evaluation of health care services.
- In lack of community participation, the health programs cannot run smoothly and universal achievement by primary health care cannot be achieved.
2. Inter-sectoral Coordination
- Inter-sectoral coordination plays a vital role in performing different functions in attaining health services.
- The involvement of specialized agency, private sectors, and public sectors is important to achieve improved health facilities.
- Intersectoral coordination will ensure different sectors to collaborate and function interdependently to meet the health care needs of the people.
- It also refers to delivering health care services in an integrated way.
- Therefore, the departments like agriculture, animal husbandry, food, industry, education, housing, public works, communication, and other sectors need to be involved in achieving health for all.
3. Appropriate Technology
- Appropriate healthcare technologies are an important strategy for improving the availability and accessibility of healthcare services.
- It has been defined as ‘’technology that is scientifically sound, adaptable to local needs and acceptable to those who apply it and to whom it is applied and that can be maintained by people themselves in keeping with the principle of self-reliance with the resources the community and country can afford.’’
- Appropriate technology refers to using cheaper, scientifically valid and acceptable equipment and techniques.
- Scientifically reliable and valid
- Adapted to local needs
- Acceptable to the community people
- Accessible and affordable by the local resources
4. Support Mechanism Made Available
- Support Mechanism is vital to health and quality of life. Support mechanism in primary health care is a well-known process focused to develop the quality of life.
- Support mechanism includes that the people are getting personal, physical, mental, spiritual and instrumental support to meet goals of primary health care.
- Primary health care depends on adequate number and distribution of trained physicians, nurses, community health workers, allied health professions and others working as a health team and supported at the local and referral levels.
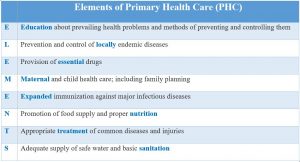
Elements/Components of PHC:
- There are eight (8) elements of Primary Health Care.
- These 8 elements are also known as ‘essential health care’. They are:
- Primary Health Care focuses more on quality health service and cost-effectiveness.
- Primary Health Care focuses on “Health for all”
- Primary Health Care integrates preventive, promotive, curative, rehabilitative and palliative health care services.
- Primary Health Care encourages new connection and community participation.
- It includes services that are readily accessible and available to the community.
- Primary Health Care can be easily accessible by all as it includes services that are simple and efficient with respect to cost, techniques and organization.
- Primary Health Care promotes equity and equality.
- Primary Health Care improves safety, performance, and accountability.
- Primary Health Care advocates on health promotion and focuses on prevention, screening and early intervention of health disparities.
- Primary Health Care is also perceived as an integral part of country’s socio-economic development.
- Poor staffing and shortage of health personnel
- Inadequate technology and equipment
- Poor condition of infrastructure/infrastructure gap, especially in the rural areas
- Concentrated focus on curative health services rather than preventive and promotive health care services.
- Challenging geographic distribution
- Poor quality of health care services
- Lack of financial support in health care programs
- Lack of community participation
- Poor distribution of health workers/health workers concentrated on the urban areas.
- Lack of intersectoral collaboration
- Encouraging community participation through rapport building, effective communication and sharing objectives and benefits of PHC.
- Developing quality assurance mechanisms through the development of various indicators and standards.
- Development of clinical guidelines including the implementation of Essential drugs list
- Allocating resources as per the need of the central, provincial/state and local level.
- Develop a planning process to define objectives and set targets by giving priority on those families and communities most at risk.
- Promoting problem-orientated research in health management system.
- Creating pathways to give health higher priority on the agenda of district development and collaboration of health departments to perform its role in health activities.
- Develop guidelines and framework that specify the roles and responsibilities of the provincial states.
References and For More Information:
https://www.who.int/news-room/fact-sheets/detail/primary-health-care
https://www.health.gov.nl.ca/health/publications/moving_forward_together_apple.pdf
https://www.open.edu/openlearncreate/mod/oucontent/view.php?id=219§ion=1.5.2
http://nursingexercise.com/primary-health-care-pillars/
http://www.atmph.org/article.asp?issn=1755-6783;year=2015;volume=8;issue=1;spage=5;epage=9;aulast=Chinawa
https://www.devex.com/news/5-challenges-in-implementing-primary-care-innovations-and-how-to-overcome-them-85579
https://apps.who.int/medicinedocs/documents/s22232en/s22232en.pdf
https://www.health.gov.au/internet/publications/publishing.nsf/Content/NPHC-Strategic-Framework~priorities-and-objectives
https://ccchclinic.com/low-income-clinics/importance-benefits-primary-health-care/
https://www.who.int/management/district/WhatReallyImprovesQualityPHC.pdf
- 4 pillars of PHC
- 4 pillars of primary health care
- alma ata conference
- Challenges for Implementation of PHC
- Components/elements of PHC
- Components/elements of Primary health care
- elements of primary health care
- five principles of primary health care
- health for all
- History of PHC
- history of primary health care
- hy is Primary Health Care (PHC) Important
- importance of primary health care
- Mitigation Measures for Ensuring Effective PHC
- Mitigation Measures for Ensuring Effective Primary health care
- what are the pillars of PHC
- what are the pillars of primary health care
- what are the principles of PHC
- what are the principles of Primary health care
- what is PHC
- what is Primary health care
Copyright © 2024 | WordPress Theme by MH Themes
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Implementing High-Quality Primary Care; Robinson SK, Meisnere M, Phillips RL Jr., et al., editors. Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care. Washington (DC): National Academies Press (US); 2021 May 4.

Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care.
- Hardcopy Version at National Academies Press
4 Person-Centered, Family-Centered, and Community-Oriented Primary Care
Primary care does not exist within a vacuum. Rather, it is a reflection of societal norms and values. Many primary care settings today are structured in a way that prevents the team from understanding and addressing the context in which a patient lives. An approach to care limited in this way perpetuates disadvantage and health inequity. Institutional inequalities, including structural racism, sexism, and classism, that are present throughout American society also exist within primary care today ( Feagin and Bennefield, 2014 ; NASEM, 2017 ). Over time, these influences have led to a dominant paradigm in primary care that is clinician centric and paternalistic, mirroring the broader U.S. health care system. The need to shift that paradigm has become even more clear given the unequal impact that the COVID-19 pandemic has had on disadvantaged communities and the current acceleration and amplification of long-standing calls for social justice and the dismantling of structural inequities, including racism, that are woven deeply within the fabric of society ( Morse et al., 2020 ).
Fortunately, primary care has seized on opportunities to shift toward an approach that is more grounded in tenets of care that are crucial to high-quality primary care: relationships with the people, their families, and the communities being served; and equity , which acknowledges and empowers those people, families, and communities. These two tenets represent an important transition in how primary care needs to move forward in the twenty-first century. While it will require a shift in the dominant paradigm to accelerate this forward progress, it is important to acknowledge the long history and many successful models (current and historical) based on this approach ( Geiger, 2002 ; IOM, 1983 ; Kark and Kark, 1999 ; National Commission on Community Health Services, 1967 ; Rosen, 1971 ; The Folsom Group, 2012 ). Box 4-1 summarizes the history and outcomes of one of these models, the patient-centered medical home. (See Chapter 9 for more on this model's financing and outcomes.)
The Patient-Centered Medical Home.
Crossing the Quality Chasm: A New Health System for the 21st Century ( IOM, 2001 ) helped highlight the need to shift the paradigm, proposing the concept of patient-centered care and describing it as “respectful of and responsive to individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions” (p. 40). Since then, momentum has been growing to realize the ideal vision for primary care—moving further toward care that is person centered, family centered, and community oriented (a model developed in the 1940s [ Kark and Kark, 1999 ; Kark and Riche, 1944 ]) rather than clinic oriented ( Health centres of tomorrow, 1947 ; Susser et al., 1955 ). This conceptualization focuses on the entire individual over the course of their lifetime and in the context of their family and community, not solely on a specific health issue and a specific clinical visit. It also emphasizes prevention and well-being, or well care rather than sick care. In addition, this conceptualization recognizes that knowledge accumulated over time—about the person, the family, and the community in which they live—creates a better foundation for recognizing health problems and the delivery of care that is appropriate in the context of other needs individuals might have ( Starfield, 2011 ).
This chapter describes what the committee heard about what individuals seeking care, families, and communities want from primary care and then presents the evidence for why a person-centered, family-centered, and community-oriented approach can deliver on those wants, and in doing so, will benefit all parties involved. The chapter also discusses how primary care can overcome the historical barriers to fully operationalize these concepts, as well as two tenets of person-centered, family-centered, and community-oriented primary care: the primacy of relationships and health equity.
- LISTENING TO INDIVIDUAL, FAMILY, AND COMMUNITY VOICES
In a survey that asked people about their personal definitions of health, answers included “not being sick” but also being happy, calm and relaxed, and able to live independently ( AAFP, 2018 ). Separately, community health workers (CHWs) in Philadelphia asked approximately 10,000 people “what do you need to improve your health?” Their answers were not limited to care focused on disease but also included psychosocial support, health behavior coaching, health-promoting resources, health system navigation, and clinical care ( NASEM, 2019b ). They expressed a desire to eliminate the racism and systematic injustice that permeates their daily lives and influences their experiences with health care, their health outcomes, and their life expectancy ( Kangovi et al., 2014a ; Williams et al., 2019a , b ). These drivers of health mirror epidemiologic studies suggesting that socioeconomic and behavioral factors influence health outcomes more than health care or genetics do ( Artiga and Hinton, 2018 ; Braveman and Gottlieb, 2014 ; McGinnis et al., 2002 ). While primary care teams have known this for a long time, primary care has encountered significant barriers—most notably incompatible payment models—that prevent it from moving away from a biomedical, disease-focused model to one that addresses people's expressed needs and preferences, includes individuals and families more in their care, and responds to the multitude of factors that impact health, including the context of the community ( Puffer et al., 2015 ).
Early in its deliberations, the committee sought input from individuals and families on their experiences with primary care. On June 2, 2020, the committee hosted a webinar titled Patient Perspectives on Primary Care. 1 Representatives from AARP, Family Voices, the Migrant Clinicians Network, the National Patient Advocate Foundation, the National Health Council, the University of North Carolina Family Support Program, and the U.S. Department of Veterans Affairs (VA) participated in the webinar and presented on the following topics:
- What does primary care mean to the people, families, and communities your organization represents?
- What can primary care do to better serve them?
Separately, the committee also sought to hear from people directly about their experiences with primary care. Through an online form posted on the project website, people shared their stories, ideas, and experiences with primary care. Anonymous submissions from this exercise and excerpts from conversations in the webinar appear below to illustrate the importance of relationships and equity in primary care and reinforce the importance of organizing primary care in a way that honors and responds to individual and family preferences, needs, values, and goals ( Greene et al., 2012 ).
Continuity of Relationships
A defining aspect of the committee's vision of primary care is the trusting relationship between the interprofessional care team and the person seeking care. Patients and advocacy groups provided multiple descriptions of the importance of relationship building. One woman from New York views her primary care clinician as a whole-person health expert and not just someone that completes an annual exam. Others reported that if it were not for primary care, no one would know—or care about—their overall health. The primacy of this relationship was described by a 33-year-old woman from rural Iowa:
I live in a rural community, and my primary physician is truly a “one-stop shop” for all of my health care questions. Not that all services and supports are provided by my physician, but there is always a way to ask a question and be referred to what I need.
Part of this trusting relationship involves an element of partnership and inclusivity. People felt positive about feeling heard and negative when their care remained unaligned with their personal preferences and priorities. The following two submissions are, respectively, from a 52-year-old in Ohio who illustrates the importance of being heard and a 77-year-old woman in Massachusetts who remarks on a breach of trust that compelled her to seek care elsewhere:
I like that my doctor and I have a long history together. He listens to my suggestions if I have a medical issue and tries to address them based on my symptoms or issues. I have been living in a nursing home for 18 1/2 years. A medical director was my primary care physician here for many years. Then, one year, I read my medical record and saw that I was on nine unnecessary medications—either for medical conditions I did not have or for which treatment wasn't needed. This physician did not have the expertise I needed, so I now go outpatient for primary care. He never apologized either.
Gwen Darien with the National Patient Advocate Foundation spoke to the primacy of relationships and said, “it's very fair to say … that health care relationships used to just be doctors and patients, but we have certainly gone well beyond doctors and patients in our health care.” She went on to describe the importance of the relationship with the person who coordinates a patient's care and of a trusting relationship that patients can depend on, particularly those with multiple health conditions. She also questioned why, when people get into the U.S. specialist system, there is no transition back into primary care, which should be about follow-up and continued relationships.
Marc Boutin, chief executive officer of the National Health Council, stressed that taking time to understand people's circumstances and personal goals is the basis of relationship building. With this knowledge, the care team should design care that can help the person and their family achieve the goal that was most important to them. Integrating these two processes would dramatically change how health is viewed and help us get the outcomes that matter for the person and family.
Jennifer Purdy from the VA illustrated important components of the clinician–patient relationship and how the VA health system solicits feedback to better understand that relationship. The VA asks for the patient's perspective on what it was like before the visit and how the patient felt they needed to prepare for it. They also listen to the patient's perspective of the experience of arriving at a facility or clinic to receive care or even clicking the telehealth button to start an appointment. They ask questions about what it was like to have care in the exam itself. Veterans have reported that they want to feel heard and to be able to trust their clinician without explaining themselves over and over again. They want to know what comes next and understand their role in their whole health care. The VA also inquires about what happens after the visit and when the person returned home, including how fast they would see test results that mattered to them and their role in receiving the next parts of their care.
Amy Liebman from the Migrant Clinician Network also talked about building relationships when a person's residence is not fixed. She stated that health systems need to be redesigned to ensure that the relationship can be maintained even with challenges of migrant populations. The ultimate goal, she said, is not to interrupt the health care relationship. The COVID-19 pandemic has provided an illustration of how telehealth has enabled primary care relationships to be maintained and even flourish when office visits are not possible.
Family Focus
While “family” in the 21st century can mean different things to different people (and many people may not have anyone in their lives that they consider to be part of their family), the patient advocacy webinar panelists and individuals from the community presented many illustrations of the importance of the family in the delivery of primary care. That same 33-year-old woman from Iowa with the “one-stop shop” physician followed up to write that:
My other experience with primary care that I would like to share, is the immense value when my doctor has knowledge of my family health. I was pregnant at 19 years old, and one great gift was that my daughter and I received care from the same doctor. We could attend appointments together (and did for many years) which reduced my burden of travel and time. The doctors could respond to our combined needs—the [e]ffect the health of another family member has on your health could be addressed, etc. In my dream for the future, primary care could be provided knowing the full context of the families experience and therefore be able to connect and respond to the needs and supports beyond just the individual in the office chair.
But others see the role of primary care through different lenses. Another individual from California submitted this:
Since I'm a fairly healthy adult, I only use primary care episodically for minor acute issues. My perspective about primary care has more to do with helping my mother manage her care. There's much to be desired in terms of how involved the provider really wants to be in her overall care. It's not clear that the provider wants to go above the basics.
Allysa Ware from Family Voices spoke about her organization being a network of families with diverse experiences that share on-the-ground information on what is happening in primary care visits. In focus groups, Family Voices listened to families who felt doctors were just going through a checklist without a meaningful relationship. One family member said the doctor was checking off things on a paper but not personalizing it to their child and did not take environmental factors into account. The doctor did not offer suggestions for helping, seem to take her concerns seriously, or say anything to lessen those concerns. Family Voices often heard that visits are fast and families do not feel like partners. One theme was that the primary care team took a wait-and-see approach, instead of really listening to the parents. The fragile relationship was illustrated by families reporting fear that if they raised concerns or disagreed with their clinician, it would impact the care their child received.
Barbara Leach, a special projects coordinator in the University of North Carolina School of Social Work, reinforced the importance of primary care and family support with children and youth with special needs. Parents start out looking to their primary care physician, their family doctor, to make sure their child gets what they need and serve as the gatekeepers of information about their child. She also pointed out the important role of primary care in coordinating care with different specialists. Parents expect primary care clinicians to provide education and information about their child's challenging conditions and referrals to specialists and connect the family to community resources and supports. She described the role of primary care clinicians as comprehensive and conducted in partnership with the family, understanding the problems families face and helping them to learn and support their child's well-being.
Community Resources
The panel discussed at length the important role that primary care plays in connecting people with community resources and addressing issues related to the community. These resources (e.g., social services, nutrition assistance programs) are fundamental to whole-person health but are generally considered to be separate from traditional, disease-focused medical care. Ware described that families often do not know which way to go and that social determinants of health (SDOH) play a major role in the ability to navigate the community. The panelists gave examples of clinicians not always being sufficiently knowledgeable about the community to connect someone to resources that could help them, and people submitting their primary care experiences online also expressed the need for strong connections between primary care and additional health and community resources. One individual, a 31-year-old, non-binary woman from Massachusetts, experienced a rotating door of clinicians—six since 2017—and found that the majority avoided care related to mental health and eating disorders and were usually unable to create a safe care environment.
Seeking primary care is difficult because I do not trust that doctors want me to have a healthier body, just a smaller one. I am queer and transgender, so safety comes to mind as well as [whether] the office will be respectful of my pronouns, my body, or my family. I have mental health needs, and many doctors do not want to touch or talk about that beyond the small survey at the end of visits. And it is clear despite the many and serious effects that eating disorders can have on the body, that PCPs are not trained in how to work with patients in ED recovery.
- ACHIEVING PERSON-CENTERED CARE
The terms “patient-centered” and “person-centered” are often used interchangeably but are conceptually different. Moving from patient-centered to person-centered care represents an evolution of primary care to focus on individual people in the context of their lived experiences, family, social worlds, and community ( Starfield, 2011 ; van Weel, 2011 ) (see Table 4-1 ).
The World Health Organization (WHO) defines people-centered care 2 as
focused and organized around the health needs and expectations of people and communities rather than on diseases. People-centered care extends the concept of patient-centered care to individuals, families, communities and society. Whereas patient-centered care is commonly understood as focusing on the individual seeking care—the patient—people-centered care encompasses these clinical encounters and also includes attention to the health of people in their communities and their crucial role in shaping health policy and health services. (2020b, p. 12)
According to WHO's Framework on Integrated People-Centered Health Services ( WHO, 2016 ), a people-centered approach is needed to ensure the following:
TABLE 4-1 The Differences Between Patient-Centered Care and Person-Centered Care
View in own window
Starfield (2011) uses “person-focused” rather than the committee's preferred term, “person-centered.”
SOURCE: Starfield, 2011 .
- Equity: For everyone, everywhere to access the quality health services they need, when and where they need them. (See section below for more on this subject.)
- Quality: Safe, effective, and timely care that responds to people's comprehensive needs and is of the highest possible standards.
- Responsiveness and participation: Care that is coordinated around people's needs, respects their preferences, and allows for their participation in health affairs.
- Efficiency: The assurance that services are provided in the most cost-effective setting with the right balance between health promotion, prevention, and in-and-out care, avoiding duplication and waste of resources.
- Resilience: Strengthened capacity of health actors, institutions, and populations to prepare for, and effectively respond to, public health crises.
The essence of person-centered care is that it extends beyond any one clinical encounter and involves continuous and holistic knowledge of patients as people, their families, their social world, and the communities in which they live and work. This knowledge accrues over time and is not specific to disease-oriented episodes. Furthermore, this knowledge, and the time spent attaining it, strengthens the relationships between the primary care team and the people seeking care. Compared to patient-centered care, person-centered care has been shown to lead to agreement on care plans, better health outcomes, and higher patient satisfaction ( Ekman et al., 2011 ). The WHO Astana Declaration in 2018 reiterated and refreshed commitments made by the world's governments to primary health care ( WHO and UNICEF, 2018 ), which is the integration of primary care and public health, with the collective goal of caring for populations. This puts the goals of this report squarely in line with the Astana Declaration and the commitments of the U.S. government as one of its cosigners.
The Role of the Individual
Activating and empowering individuals to be a part of their own care team should function cyclically and iteratively—as people become more knowledgeable and confident in their own health care and continue to experience success, they may take on increasingly sustained and eventually proactive roles. While empowerment has become a highly visible initiative in public health and policy reforms in the past decade (e.g., some provisions of the Patient Protection and Affordable Care Act [ACA] 3 encourage engaging care-seekers in this way), the methods of reaching person-centered care can and should look different depending on context ( Chen et al., 2016 ). One foundational tenet, though, is respecting people as experts in their own lives ( Kennedy, 2003 ). The Chronic Care Model explicitly recognizes that “informed, activated patients” are needed to improve health outcomes for individuals with chronic diseases. One of the six components of that model is self-management support ( Bodenheimer et al., 2002 ). Apart from engaging individuals in their own care, understanding the individual's goals for their care, particularly as they age, can be especially important. Naik and colleagues (2018) noted that “eliciting and documenting the personal values of older, multimorbid adults is uncommon in routine care, despite playing a central role in person-centered care.” Models for capturing the goals, values, and preferences of older adults in the primary care setting have been shown to be feasible ( Blaum et al., 2018 ; Naik et al., 2018 ).
The Role of Family and Informal Caregivers
Family members and other informal caregivers may not be licensed to provide care, but their voice and presence is an important component of person-centered primary care and can improve health outcomes, health care quality, and the overall care experience for people and their families. Primary care that includes family members or companions is associated with improved self-management, satisfaction, communication, and understanding ( Cen é et al., 2015 ; Rosland et al., 2011 ). In fact, an individual's most important health care resource may be their family or informal supports (if they have them) ( Cole-Kelly and Seaburn, 1999 ). Research shows that most individuals prefer clinicians to involve their families and other informal caregivers in their health care ( Andrades et al., 2013 ; Botelho et al., 1996 ). Family members play a supportive role in most consultations with clinicians ( Andrades et al., 2013 ; Sayers et al., 2006 ), as well as helping their loved one to navigate the increasing complexity of health care systems, including making and keeping appointments and following up on referrals ( Andrades et al., 2013 ; Botelho et al., 1996 ; Igel and Lerner, 2016 ; IOM, 2008 ). In addition, a family member or other informal caregiver can be a valuable source of health information and insights about the home and community environments that clinicians may not get from the person seeking care.
Family members can take many roles aside from providing companionship and comfort when they accompany a loved one to an office visit ( Brown et al., 1998 ; Clayman et al., 2005 ; Cornelius et al., 2018 ; Schilling et al., 2002 ). As an advocate, they can communicate the person's needs and concerns and may translate or interpret in situations with a language gap, especially in emergencies ( Rimmer, 2020 ). They can also act as an additional set of ears to ensure the person understands their disease, medications, procedures, and treatments, which may result in better outcomes ( Whitehead et al., 2018 ). Family members can help someone make decisions that are aligned with their personal and cultural beliefs. For chronic illnesses, family members may come to see themselves as the primary care team's partner in providing care. It is important in such cases for communication to continue to include the individual, particularly when they are capable of making decisions about their care.
Research has identified core facilitators of family-centered care models that benefit the individual while protecting the health and well-being of family members ( Kokorelias et al., 2019 ): (1) development and implementation of care plans that include the family; (2) collaboration between family members and health care clinicians in the delivery of care; (3) education for patients, families, and clinicians; and (4) dedicated policies and procedures that address inclusion of family members ( Kokorelias et al., 2019 ). When implemented, family-centered primary care can reduce admissions, readmissions, and length of hospital stay; increase patient, family, and clinician satisfaction; and improve relationships ( Kuhlthau et al., 2011 ; Park et al., 2018 ). However, despite the benefits of such inclusive care, family and informal caregivers often need additional support, including more consistent and explicit inclusion in the care team, training, respite, and financial security ( IOM, 2008 ).
Examples from Medical Disciplines
Centering care around the family was a major driver in creating the medical specialty of family medicine in 1969 ( Green and Puffer, 2010 ; Stephens, 2010 ). In the early years of this emerging new medical and academic discipline, family medicine adapted care based on the biopsychosocial model of care and incorporated unique training elements to strengthen the expertise of primary care teams to think of individuals within the context of their families and their communities ( Borrell-Carrió et al., 2004 ; Engel, 2012 ; Martin et al., 2004 ). Today, family medicine teams often care for several members of the same family and have developed advanced skills to incorporate families into care plans and seamlessly care for multiple family members of various ages at one clinic visit or during one hospitalization ( Beasley et al., 2004 ; Flocke et al., 1998 ). Other primary care medical disciplines not focused on all ages, such as pediatrics ( Clay and Parsh, 2016 ; Jolley and Shields, 2009 ; Pettoello-Mantovani et al., 2009 ) and geriatrics, have also embraced family-centered care concepts and practices. Pediatric clinicians who adopt family-centered practices recognize the importance of including family members in evaluating, planning, and delivering treatment and incorporate that ideology into policies, programs, facility design, and day-to-day interactions ( Committee on Hospital Care, 2003 ; Committee on Hospital Care and IPFCC, 2012 ).
Similarly, geriatricians understand that families can provide information that plays an important role in clinical decision making. Geriatrics care tends to focus on assessing function and cognition and emphasizes the goals of care. Involving the family in assessing and caring for older adults is both important and challenging, particularly for the many who have multiple chronic disorders ( American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity, 2012 ; Boyd et al., 2005 ; Tinetti et al., 2012 ). The changes in sensory, cognitive, and physical functions that come with aging may prompt some older adults to need or want to involve family members or close friends in managing their health ( IOM, 2008 ; Wolff and Roter, 2011 ). A 2015 survey of older adults and their preferences for care found that while nearly 70 percent of older adults manage their own care, they prefer family members, in addition to their clinicians, to be involved in making health care decisions ( Wolff and Boyd, 2015 ).
The Role of Community and Community-Oriented Care
The importance of recognizing community needs in primary care has been described for decades. Community-Oriented Primary Care: New Directions for Health Services Delivery ( IOM, 1983 , p. 70) defined community-oriented primary care as
an approach to medical practice that undertakes responsibility for the health of a defined population, by combining epidemiologic study and social intervention with the clinical care of individuals, so that the primary care practice itself becomes a community medicine program. Both the individual and the community or population are the focus of diagnosis, treatment, and ongoing surveillance.
People-centered and community-oriented care overlap considerably and link strongly to the goals of WHO and the World Health Assembly in the 2018 Declaration of Astana and subsequent commitments.
Adding community-oriented care to the new conceptualization of primary care addresses the individual's and family's cultural and social context as they are embedded within a medical and social neighborhood, rather than from a solely delivery-centric model ( Braddock et al., 2013 ; Buchmueller and Carpenter, 2010 ; Chokshi and Cohen, 2018 ; Davis et al., 2005 ; DeVoe et al., 2009 ; Driscoll et al., 2013 ; Edgoose and Edgoose, 2017 ; Enard and Ganelin, 2013 ; Etz, 2016 ; Finkelstein et al., 2020 ; Kramer et al., 2018 ; Landon et al., 2012 ; Possemato et al., 2018 ; Starfield, 2011 ; Yoon et al., 2018 ). In addition, community-oriented care facilitates coordination between public health approaches and primary care delivery, opening the door for primary care to play a central role in improving community health ( Eng et al., 1992 ), particularly for communities with disadvantaged populations ( Cyril et al., 2015 ; Derose et al., 2019 ; Shukor et al., 2018 ).
Benefits of Community-Oriented Care
Community-oriented care improves outcomes in many areas and for different populations, including well-child care ( Jones et al., 2018 ); maternal, neonatal, and child health ( Black et al., 2017 ); and for people with depression ( Izquierdo et al., 2018 ; Ong et al., 2017 ), obesity ( Derose et al., 2019 ), hypertension ( Epstein et al., 2002 ), and opioid use disorder ( Wells et al., 2018 ). It can also play an important role in reducing health disparities ( Derose et al., 2019 ), decreasing unnecessary use of the emergency department, and increasing the ability for older adults to live independently ( Institute for Clinical Systems Improvement, 2014 ).
Despite the strong evidence that partnering with the community will benefit person- and family-centered care, studies have found that models involving shared decision making, such as integrating the community into primary care, can be challenging to the health care enterprise on practical, structural, and systematic levels. For example, some clinicians have difficulty recognizing the power dynamics between them and other care team members or people seeking care: specifically, the power that inherently comes with the position of health care clinician ( Nimmon and Stenfors-Hayes, 2016 ; Singer, 1989 ).
Clinicians and systems may see community-oriented approaches as a means to bolster medical care but not necessarily whole-person health ( Garfield and Kangovi, 2019 ). In addition, most challenges are exacerbated by fee-for-service (FFS) payment that incentivizes diagnosing and treating diseases, performing procedures, prescribing medications, and providing care based on traditional biomedical models. For example, a 2018 study found that primary care clinicians felt pressure to focus on diagnosis and treatment and had a hard time imagining how evidence-based, community-partnered programs for disease self-management and prevention could contribute to either of those primary functions ( Leppin et al., 2018 ). The study authors concluded that “primary care and community-based programs exist in disconnected worlds. Without urgent and intentional efforts to bridge well-care and sick-care, interventions that support people's efforts to be and stay well in their communities will remain outside of—if not at odds with—health care” (p. 1). These words echo those of primary care clinicians nearly a century ago ( Burnham, 1920 ; Susser et al., 1955 ; Wald, 1911 ). Such long-standing challenges can be overcome when payment is reformed to better align incentives to support community-oriented care ( Gofin et al., 2015 ; IOM, 1983 ; Lloyd et al., 2020 ). See Chapter 9 for more about primary care payment.
The Role of the Interprofessional Care Team
Ideally, person-centered care is delivered via interprofessional teams who establish long-term relationships with care-seeking individuals and their families. Achieving this aim requires a team structure that places individuals in the driver's seat of care that aligns with their needs and preferences. Well-designed teams can support nurturing, longitudinal, person-centered care ( Mitchell et al., 2012 ; Sullivan and Ellner, 2015 ). A commonly used definition of team-based care is “the provision of health services to individuals, families, [and] their communities by at least two health providers who work collaboratively with patients and their caregivers—to the extent preferred by each patient—to accomplish shared goals within and across settings to achieve coordinated, high-quality care” ( Mitchell et al., 2012 , p. 5; Okun et al., 2014 , p. 46) (see Chapter 6 for more on primary care teams).
The Role of Relationships in Primary Care
Primary care settings continue to expand beyond traditional health care settings and move beyond the walls of clinics and hospitals to community-based settings, such as schools, employment sites, and housing complexes. In addition, primary care is increasingly using technology-enabled care delivery modalities, including telehealth and smartphone apps. As a result, the personal relationship between the person seeking care and the care team providing that care as a foundation for consistency is more important than ever. The person–care team relationship is the “bedrock of value in primary care” and symbiotically related to other components of high-quality care, including whole-person care and coordination ( Ellner and Phillips, 2017 ), and continuity of care ( Andres et al., 2016 ; Rhodes et al., 2014 ). Evidence of the benefits of a strong relationship to both the individual and care team is well documented; a relationship built on respect and acceptance can lead to patient satisfaction and empowerment, improved outcomes and safety, increased adherence, prolonged engagement, and decreased burnout for care team members ( Bogart et al., 2016 ; Brown et al., 2015 ; Chaudhri et al., 2019 ; Pollack, 2019 ).
Relationships can be healing in their own right, outside of any health services, and personal connections with care staff other than the immediate primary care team, such as front office staff, subspecialists, consultants, and care extenders, also contribute a vital dimension to the patient experience ( Kravitz and Feldman, 2017 ). Over time, relationships encourage the care-seeker to feel understood, hopeful about the future, and comfortable with the care team or in a health environment ( Scott et al., 2008 ). Comfort and trust are crucial for beginning to reduce health inequities and improve access for marginalized care-seekers, including formerly incarcerated individuals, those who are not U.S. citizens, people with disabilities, veterans, people who are homeless, and communities of color. Trauma-informed care and anti-racism curricula in training, in addition to diversified hiring practices for these teams, improve team members' abilities to connect with patients, foster a relationship of understanding and trust, and ultimately begin to improve disparities in health access and outcomes ( Alsan et al., 2019 , 2020 ; Chaudhri et al., 2019 ; Garcia et al., 2019 ; Saha et al., 1999 ; Shen et al., 2018 ). Relationships are a function of time, trust, and respect, measures of continuity and longitudinality, and patient-reported outcomes, described in Chapter 8 , are an effort to assess relationships systematically as high-value measures of primary care.
Few primary care team members would likely disagree with the importance of relationships, and some evidence suggests that medical school graduates who go into primary care may choose it at least in part for its relationship aspect ( Osborn et al., 2017 ). The reality, however, is less than the ideal, and care teams struggle with time constraints, reimbursement barriers, and administrative hurdles that get in the way of relationship building. While some suggest simply reprioritizing and freeing up time to work on relationships, other more novel options have been conceived including changes to the electronic medical record system, building communication skills, reconfiguring the primary care team, and overhauling payment models so they are compatible with the time and effort needed to build and sustain relationships with people seeking care ( AHRQ, 2018 ; Montague and Asan, 2014 ; Pollack, 2019 ).
The patient–care team relationship is all the more important in times of crisis and uncertainty, such as during the COVID-19 pandemic. A survey found that even in the midst of the pandemic, the majority of primary care patients continue to value a relationship with their care clinician, citing desires for being known as individuals, help understanding current events, and a safe environment for asking questions; 83 percent expressed distress at the thought of losing that relationship ( The Larry A. Green Center and PCC, 2020 ). In another wave of that survey, two-thirds of patients most preferred speaking with a member of their primary care team about potential exposure to COVID-19, as opposed to public health officials, hospital workers, or trained community members. 4 Additional research found dozens of ways to improve relationships, even during telehealth visits, casting the pandemic as an opportunity to reinvent primary care's investment in relationships ( Bergman et al., 2020 ).
Even though primary care's emphasis on relationships is not consistently realized, isolated exemplars do exist. For example, Southcentral Foundation's (SCF's) Nuka 5 System of Care built relationships into the core of its operational principles and responsibilities. The Alaska Native–owned, nonprofit health care organization also focuses on responding to the wide range of opportunities for feedback from patients, whom SCF refers to as “customer-owners.” SCF succeeds in part as a result of the bespoke tailoring of its system for the people, families, and communities it serves. From the beginning, the entire health system was based on Alaska Native values and needs. This was possible thanks to federal legislation 6 that allows for self-governance and the foundation's reliance on customer-owner surveys and feedback ( Gottlieb, 2013 ) (see Chapter 5 for a more detailed discussion of SCF's integrated system of care).
The Individualized Management for Patient-Centered Targets (IMPaCT) program is a community-based model founded on the notion that CHWs can improve outcomes by building relationships and providing person-centered support. CHWs provide personalized and holistic social support, advocacy, coaching, and health system navigation ( Seervai, 2020 ), and the CHWs start by getting to know the person outside of their medical history and health complaints, initially addressing the social or behavioral needs that are obstacles to health care, such as loneliness or distrust of clinicians. The relationship, built on trust and understanding, is essential for this to happen, for it allows the CHWs to understand those in their care so that later in the relationship, they can guide them toward the health resources needed for whole-person care. IMPaCT has seen positive results across a wide variety of measures, including body mass index, hemoglobin and blood pressure levels, self-rated mental health, quality of care, total hospital days, and likelihood to complete a primary care follow-up appointment within 14 days of discharge from the hospital. The program yields a return on investment of $2.47 for every dollar invested by Medicaid and has been replicated across 20 states. Its success indicates that addressing socioeconomic and behavioral needs in a whole-person approach to care can improve access to and quality of primary care ( Kangovi et al., 2014b , 2017 ).
- HEALTH EQUITY AND THE ROLE OF PRIMARY CARE
Health equity is a guiding principle for many primary care teams. Primary care improves equity ( Starfield, 2009 , 2012 ; Starfield et al., 2005 ), and an ultimate goal for improving primary care is to reduce inequities as much as possible. Health disparities are the metrics used to measure progress toward achieving health equity (see Box 4-2 ). The United States has health disparities in terms of education, race, ethnicity, sex, sexual orientation, and place of residence ( Adler et al., 2016 ). Greater equity is achieved by improving the health specifically of those who are economically or socially disadvantaged, and reductions in health disparities (both absolute and relative) are evidence of a move toward greater health equity. Achieving health equity means achieving social justice in health—no one is denied the possibility of a healthy life as a result of belonging to a population that has historically been disadvantaged ( Braveman, 2014 ; Martinez-Bianchi et al., 2019 ). Health disparities and health care disparities are separate concepts and should not be confused. Ensuring equitable access to high-quality health care for all is not a guaranteed way to reduce health disparities and ensure health equity, given the many factors that have a much greater impact on health than health care does.
Definition of Health Disparities.
Improving Primary Care Models to Address Inequities
A 2016 review comparing the standard medical model of primary care to community-oriented primary care found that the latter did a much better job of addressing sociocultural issues that act as barriers to care and SDOH that lead to health inequities among immigrant populations ( Batista et al., 2018 ). The study's authors suggested that community-oriented primary care is better suited to address health equity in general.
A community-oriented approach to primary care is not the silver bullet to address inequities in health care—workforce solutions ( Jackson and Gracia, 2014 ), digital health ( Zhang et al., 2019 ), and policy measures ( Holden et al., 2019 ) are also needed. However, it is an essential part of the solution. Over the past 40 years, practice-based research networks (PBRNs), each comprising at least 15 primary care clinicians or ambulatory practices that are linked closely with their communities, have been conducting research on how to improve primary care delivery, often with an explicit focus on health equity ( Westfall et al., 2019 ). For example, the Southeast Regional Clinicians' Network PBRN, based out of the Morehouse School of Medicine and comprising 203 federally qualified health centers (FQHCs) across eight southeastern states ( MSM, 2021 ), has studied equity-addressing interventions for improving cancer screening ( Hunt and Hurlbert, 2016 ) and treatment of asthma ( Rust et al., 1999 ), heart disease ( Daniels et al., 2012 ), and mental health issues ( Rust et al., 2005 ) for high-disparity, underserved populations.
Consistent with the concept of whole-person, equitable health care and the person-centered, family-centered, and community-oriented approaches described in this chapter, the need to address SDOH is a key feature of the committee's definition of high-quality primary care (see Chapter 2 ). In the past decade, consistent and compelling evidence concerning SDOH and their influence in shaping individual health have led the health care sector to reconsider its role in care. As discussed earlier in this chapter, a person's health is a culmination of factors and is not limited to the absence of disease. SDOH represent some of these factors and are defined as the “conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life” ( WHO, 2020a ). What these determinants mean for each individual can be different, though; they can enhance wellness for some yet embody barriers and social risk patterns that contribute to increased morbidity and mortality for others ( NASEM, 2019a ). Addressing SDOH is an essential component of whole-person health and can eliminate some of the factors that contribute to health inequities.
According to Healthy People 2020, these determinants come in five key areas that span spheres of influence on an individual: economic stability or socioeconomic status (SES), education, social and community context, health and health care, and neighborhood and built environment ( ODPHP, 2020 ). Those with lower SES, and the resulting stress, shoulder a heavier burden of poor health than those with higher SES ( Adler and Rehkopf, 2008 ; Bor et al., 2017 ). If SDOH inform social care and its integration into health care, clinicians can treat the upstream factors that so often become barriers to future health equity.
Integrating Social Care into the Delivery of Health Care to Improve the Nation's Health ( NASEM, 2019a ) looked at the current state of U.S. social care and recommended changes to health care and policy infrastructure that promote alignment across sectors in order to better inform care delivery for all people. This report details five areas where health care systems can work with people and communities to encourage better social care for all ( NASEM, 2019a ): promoting awareness, adjustment, assistance, alignment, and advocacy. All of these actions will ultimately benefit individuals seeking care. Adjustment and assistance focus on improving care delivery specifically for individuals based on information about their social needs, while alignment and advocacy focus more delivery activities that the health care sector can carry out through coordinated care.
Advocacy activities promote health equity for people who may not have a voice in the current value-based care system and can range from light-touch (e.g., referring people to social workers to obtain rental assistance) to high-touch (e.g., longer, more intensive interventions that seek to address social needs) assistance. One example of a successful advocacy program is the Boston Medical Center Medical-Legal Partnership, which involved a coordinated team of lawyers and clinicians who worked together to change utility shutdown regulation with the Massachusetts Department of Public Utilities, to ensure that high-risk people did not have their heat shut off during the winter ( National Center for Medical-Legal Partnership, 2017 ). Activities such as these ensure that social needs and determinants are taken into account and those with more barriers are not necessarily relegated to worse health outcomes.
The Role of Empanelment
Empanelment, sometimes known internationally as “rostering,” is the process of assigning all individuals in a given population to an interprofessional care team or team member that is then responsible for providing primary care. It is an approach that can help achieve equitable access to care for all and improved population health outcomes. Empanelment usually has delivery systems or care teams making the assignments, whereas attribution, covered further in Chapter 9 , typically involves payers doing so ( AIR, 2013 ). Approaches vary and can be based on geography, insurance, or patient preference ( Joint Learning Network for Universal Health Coverage et al., 2019 ). Panel size is frequently predetermined to ensure sufficient resources for the target population. More sophisticated processes may also acknowledge population health profiles to more evenly distribute health needs among primary care teams and help team members better understand the needs of their panels ( PHCPI, 2019 ).
Empanelment ensures that each individual in a given population has a consistent and reliable source of primary care. It can be a strong foundation for trusting, continuous team member–patient relationships and provides community members with the access to appointments when they need them ( Bodenheimer et al., 2014 ; Wagner et al., 2012 ). For these reasons, empanelment is an important component of community-oriented and PCMH primary care models, which emphasize ease of access to care and sustained clinician–patient relationships ( Brownlee and Van Borkulo, 2013 ). Ideally, empanelment can help primary care meet access and convenience needs that frequently drive people to retail clinics and emergency departments ( Coster et al., 2017 ). However, empanelment is not a one-time fix; it requires proactive maintenance to ensure consistent, timely access and resource capacity for all panel members ( Joint Learning Network for Universal Health Coverage et al., 2019 ). See Chapter 6 for more on empanelment, panel size, and building primary care teams to meet the needs of a population.
- SHIFTING PRIMARY CARE TO BE MORE COMMUNITY-ORIENTED
If one goal of person- and family-centered primary care is to move from a reactive to proactive approach, it is essential for teams to understand the health trends and demographic characteristics of the populations they serve ( Hollander-Rodriguez and DeVoe, 2018 ). Multiple levers can help shift primary care toward community-oriented models, including data systems, workforce, care delivery settings, and partnerships between primary care, public health, and community-based organizations. All of these levers can be influenced by policy changes and innovative payment models ( Bailey and Goodman-Bacon, 2015 ; Bitton et al., 2019 ; Cometto et al., 2018 ; Enard and Ganelin, 2013 ; Fertig et al., 2012 ; Gold et al., 2019 ; Hone et al., 2018 ; Krist et al., 2013 ; Ockene et al., 2007 ; SNOCAP-USA et al., 2014 ; Wiggins et al., 2013 ). The following sections discuss each lever in more detail.
Data Systems
Without data systems to understand the population being served, community-oriented primary care is not possible. Whereas the door-to-door data collection performed by the primary care leaders of the past century posed issues of representativeness and accuracy, today's data are often quite complete ( Mullan and Epstein, 2002 ). Instead, care teams and their partners struggle with collecting and aggregating multiple data sources into a comprehensive, usable community-oriented system. Doing this will optimize tools such as patient registries, “community vital signs,” and geographic information systems to take the pulse of a community, orienting local care teams to health and social needs, issues of access, and the intervention strategies and collaborations needed to address them ( AMA, 2016 ; Hughes et al., 2016 ; Phillips et al., 2019 ; Rock et al., 2019 ). See Chapter 7 for more information regarding data tools in primary care's continued shift toward community-oriented care.
In most settings, the primary care physician workforce does not reflect the people it serves and is disproportionately male and white compared to the U.S. population ( Xierali and Nivet, 2018 ). Physicians also increasingly come from privileged backgrounds. One study showed that more than half of all first-year medical students came from households in the top income quintile, whereas fewer than 5 percent were from the bottom income quintile ( Youngclaus and Roskovensky, 2018 ). Individuals and families may perceive this discordance as a barrier to care ( Malat et al., 2009 ; Saha et al., 1999 ) and prefer to see racial-concordant physicians ( Alsan et al., 2019 ; Cooper et al., 2003 ; Saha and Beach, 2020 ; Saha et al., 2000 ). Increasing workforce diversity is believed to be essential in “(1) advancing cultural competency, (2) increasing access to high-quality health care services, (3) strengthening the medical research agenda, and (4) ensuring optimal management of the health care system” ( Cohen et al., 2002 , p. 91) and can contribute to a more equitable system for all. Chapter 6 explores the factors influencing the composition of the primary care workforce and strategies to increase its number and diversity.
One critical strategy for aligning the primary care workforce with its community is to expand opportunities to integrate CHWs and promotores de salud into primary care teams. CHWs are trusted community members who share a common background with the people they serve and have often experienced obstacles to health care or other forms of injustice themselves. They reflect the diversity of disadvantaged Americans: 65 percent are Black or Hispanic, 23 percent are white, 10 percent are American Indian or Alaska Native, and 2 percent are Asian or Pacific Islander ( Arizona Prevention Research Center, 2015 ).
A large body of evidence suggests that CHWs can engage people with underlying socioeconomic issues into primary care ( Wang et al., 2012 ), improve preventive screening rates ( O'Brien et al., 2010 ), and reduce costly hospitalizations ( Campbell et al., 2015 ). The use of CHWs, however, should not deter the necessary efforts to diversify the overall primary care workforce across professions to create a local workforce that reflects the diversity of the community in which it is practicing. See Chapter 6 for more on the primary care workforce.
Delivery Setting
Primary care is often delivered in settings outside of the clinician's office and more integrated into community settings. Innovative models of community-oriented primary care further integrate care delivery in non-clinical settings, including the workplace, college campuses and schools, recreation centers, places of worship, retail shops (e.g., barbershops), homeless shelters, housing for older adults, and institutions (e.g., prisons and jails). This shift to primary care in non-clinical settings increases access to care, allows for greater community participation, and relies on settings that are contextualized in other aspects of a person's daily life.
The COVID-19 pandemic quickly illustrated that primary care can be delivered outside the traditional office visit. As the pandemic swept the nation and prompted a need to socially distance—for the safety of both clinicians and individuals—telehealth adoption in primary care increased by nearly 50 percent, with clinicians in both rural and urban settings seeing increases ( Bosworth et al., 2020 ; Mann et al., 2020 ; Mehrotra et al., 2020 ). Even before, interest in use of telehealth services was increasing for both clinicians and individuals ( AMA, 2020 ; Martinez et al., 2018 ; Orlando et al., 2019 ). Pandemic-related policy changes reduced barriers to telehealth access and promoted its use for primary and specialty care ( Bashshur et al., 2020 ; CMS, 2020b ). In addition, many professional medical societies endorse telehealth services and provide guidance for medical practice in this evolving landscape ( AANP, 2019 ; CDC, 2020 ; Committee on Pediatric Workforce, 2015 ; Joint Task Force for the Development of Telepsychology Guidelines for Psychologists, 2013 ). See Chapter 7 for more about telehealth services.
A report from the U.S. Department of Health and Human Services (HHS) notes that even after Medicare in-person primary care visits resumed in May 2020, demand was steady for telehealth visits ( Bosworth et al., 2020 ). A 2020 survey by McKinsey found that 48 percent of individuals who used telehealth during the pandemic were satisfied with the care they received, and 37 percent were likely to use telehealth in the future ( Cordina et al., 2020 ). While in-person, patient–clinician interactions will remain necessary, and likely preferred by many people, the pandemic accelerated openness to telehealth in ways previously unseen from policy makers, clinicians, and individuals alike.
Where telehealth has been unable to meet people's needs, including testing for and treating COVID-19 itself, primary care teams have partnered with health departments, academic institutions, local governments, and others to create opportunities for care. This includes developing drive-through testing sites and respiratory diagnostic centers that preserve personal protective equipment, especially important in federally designated shortage areas, and protecting both team members and individuals from potential spread ( Barzin et al., 2020 ; Ton et al., 2020 ). The disruption and forced innovation brought about by COVID-19 could lead to purposeful changes in primary care delivery and enable better person-centered care if policy makers and payers make it a priority.
Partnerships Among Primary Care, Public Health, and Community-Based Organizations
Having primary care teams embedded within communities and partnering with public health and community-based organizations is not a new idea in the United States. In the late nineteenth century, dispensaries were established to provide medical care to the poor in neighborhood settings ( Rosenberg, 1974 ). Although dispensaries were short-lived due to concerns about direct competition with private physicians ( Burrow, 1977 ), their creation was prompted by a recognition that social conditions were influencing health and that health care services, informed by social medicine ideals, should be moved out of the hospital into the community ( Janes, 1876 ; Rosen, 1947 , 1949 ).
In the early twentieth century, many U.S. cities were proposing to organize and coordinate networks of health centers in each district that would serve defined geographic communities, adhere to the notion that a neighborhood should be identified and assessed, and recognize that unique health services should be targeted toward the special needs of each individual community ( Davis, 1927 ; Hiscock, 1935 ; Pomeroy, 1929 ; Schmacke, 1998 ; Wilinsky, 1933 ). This period also featured a growing realization that community members should be involved in care delivery.
While district centers were created and called for services in the community, for the community, and by the community, most were limited to only offering public health and preventive services that complemented care already offered by private physicians, thus creating the chasm between modern day primary care and public health ( Burrow, 1977 ; Winslow, 1919 , 1929 ). One exception was the Indian Health Service (IHS), which implemented a more comprehensive model that combined primary care and public health in the late 1950s; it proved effective in promoting healthy behaviors, preventing disease ( Nutting et al., 1979 ), and improving quality of care ( Shorr and Nutting, 1977 ).
In 1966, the U.S. government produced Health Is a Community Affair ( National Commission on Community Health Services, 1967 ). This 3-year study of healthy communities reviewed the evidence supporting the effectiveness of partnerships between primary care, public health, and communities and described the notion of “communities of solution” as an approach to health care defined by problems to be solved rather than geographic locales, specific delivery systems, or governmental agencies. A community of solution comprises people who come together to address an important problem or seize an opportunity to improve health, and it envisions primary care teams collaborating with many diverse partners, depending on the nature of the problems and the community. In addition to community members and public health professionals, each unique community of solution would include many other public and private partners and community-based organizations ( Gotler et al., 2020 ; Griswold et al., 2013 ; The Folsom Group, 2012 ; Westfall, 2013 ).
Community participation in primary care was formalized as an important concept in the Alma-Ata Declaration of 1978. 7 Community-oriented care was recognized by the Institute of Medicine in 1983 as an important aspect of high-quality primary care and further emphasized in Primary Care: America's Health in a New Era ( IOM, 1996 ). More recently, the ACA created new incentives for primary care to pursue community-based population health care. The October 2018 Global Conference on Primary Health Care in Astana, Kazakhstan, and resulting Astana Declaration reasserted this commitment to people-centered care and the role of community as well as both primary care and primary health care to achieving it ( WHO and Ministry of Healthcare Republic of Kazakhstan, 2018 ; WHO and UNICEF, 2018 ).
Health Centers
Health centers provide high-quality, locally tailored, comprehensive primary care services and gynecologic, behavioral health, preventive health (including dental, cancer screening, family planning, and immunizations), vision and eye care, and diagnostic laboratory and radiologic services. They also offer case management services, 8 referrals to specialty care and social services, and transportation and translation services. The care delivered by health centers, which include FQHCs, health care for people who are homeless, health centers for residents of public housing, school-based health clinics, and migrant health centers, is based on tenets of community-oriented primary care and represents the largest segment of the primary care system.
Health centers are descendants of the original neighborhood health centers, which started in 1965 as two demonstration projects of the Office of Economic Opportunity Community Action Program to provide health and social services access points in poor and medically underserved communities and promote community empowerment ( CHroniCles, 2020 ; Levitan, 1974 ). Congress passed an amendment to the original Economic Opportunity Act in 1966 to provide further funding for the planning of operation of more “comprehensive health service programs” ( Anderson et al., 1976 , p. 13). By 1972, more than 100 neighborhood health centers and other comprehensive health service projects had been initiated with grant assistance from the Office of Economic Opportunity ( Zwick, 1972 ).
FQHCs are health centers that receive Health Resources and Services Administration (HRSA) Health Center Program federal grant funding to improve the health of underserved populations ( HRSA, 2020a ). Today, more than 1,400 FQHCs operate nearly 13,000 delivery sites. They serve nearly 30 million people, including more than 398,000 veterans, one-third of all people living in poverty, 20 percent of those living in rural locations, and more than 10 percent of all children ( HRSA, 2020b ). Delivery sites include tribal or urban American Indian and Alaska Native areas, remote sites connected to a community health center, and sites deemed “lookalikes” that meet the requirements of FQHCs but do not receive federal grant funding ( Rural Health Information Hub, 2019 ).
Rural health clinics (RHCs) are Centers for Medicare & Medicaid Services (CMS)-certified clinics in rural Medically Underserved Areas or Health Professional Shortage Areas and provide primary care services. RHCs, like FQHCs, must meet Medicare and Medicaid health and safety standards in 42 CFR Part 491; however, RHCs are not subject to many of the other FQHC requirements and may be privately owned ( CMS, 2019 ).
One key community-oriented feature of health centers is that all are required to have at least 51 percent of their governing boards of directors composed of people in the community who are served by the health center and reflect the demographic characteristic of its population ( HRSA, 2020a ; Taylor, 2004 ). This requirement ensures that the people served—who are often from under-represented communities that rarely are included in organization-level decision making—have a voice in how services are delivered. In practice, some evidence indicates that the demographics of patients on health center governing boards are not always representative of the patient population overall and that they seldom hold executive positions on the board ( Wright, 2013 , 2015 ). Nevertheless, including patients in the system-wide decision-making process is a practical way to engage the community and ensure that its needs are addressed in the health centers' daily operations.
Health centers are also required to complete a community needs assessment every 3 years, which includes a review of barriers (including transportation) and unmet health needs of the medically underserved (including the ratio of primary care physicians relative to the population, health indexes for the population served, the poverty level, and other demographic factors in demand for services, such as the percent of the population over age 65). In addition, they must make and maintain a reasonable effort to build and sustain relationships with other clinicians and services, such as hospitals and specialists, within their catchment areas to help facilitate seamless coordination with services that are not offered within the health centers themselves. They must also annually assess the geographic boundaries of their patient population ( HRSA, 2018 ). In some communities, the community needs assessment is coordinated with those mandated for nonprofit hospitals and accredited public health departments with the goal of also coordinating their collective response to identified needs—an approach recommended by Primary Care and Public Health: Exploring Integration to Improve Population Health ( IOM, 2012 ).
Health centers are financially accessible to the communities they serve. They are required to provide services to everyone, regardless of insurance status or ability to pay out of pocket. Uninsured individuals pay on a board-approved sliding scale based on income and family size. Revenue streams for health centers include Medicaid, Medicare, private insurance, and out-of-pocket payments. Medicare and Medicaid largely use a bundled, prospective payments system (PPS) that pays health centers per visit, not per service rendered. This allows for more flexibility and efficiency because health centers are not ordinarily covered by Medicaid FFS payments. However, the PPS rates have not kept up with inflation or the recent expansion of health center services in recent years and now only cover about 82 percent of the cost to care for Medicaid recipients ( NACHC, 2020b ). Similarly, while FQHCs provide services for 16 percent of Medicaid recipients, less than 2 percent of Medicaid payments go to them. Still, there is evidence that Medicaid beneficiary costs at FQHCs are lower than in other settings. A study of Medicaid beneficiaries comparing those who primarily receive primary care at FQHCs to those who seek care elsewhere found that costs were 24 percent lower for FQHC users. They also had fewer hospital admissions, fewer visits overall, and spent less on inpatient and specialty care ( Nocon et al., 2016 ).
Evidence indicates that health centers have reduced access and outcome disparities across racial and ethnic groups, income, and insurance status ( NACHC, 2020a ; Politzer et al., 2001 ). Their enabling services, such as transportation, nutrition assistance, health education, and housing, play a particularly important role in improving access. One recent nationally representative study found that among HRSA-funded health center clients, those who used enabling services had nearly twice as many visits and were more likely to get routine check-ups, receive preventive care and flu shots, and report higher patient satisfaction than those who did not ( Yue et al., 2019 ). Health centers also outperform other delivery settings across a wide array of measures spanning quality and outcomes, patient satisfaction, and cost-effectiveness ( NACHC, 2020a ).
While the number of health centers has increased since the passage of the ACA, the expansion was largely in urban areas and less likely in areas that were rural or had more than 20 percent of the population below the federal poverty level ( Chang et al., 2019 ). This suggests that improving access to health care for financially disadvantaged populations will require increasing the number of health centers to reach them; however, this is proving more difficult to achieve, as workforce shortages in primary care have contributed to a greater percentage of health centers reporting budgeted but unfilled positions for primary care physicians, registered nurses or licensed practical nurses, and licensed mental health clinicians ( Lewis et al., 2019 ). One strategy health centers have employed to counter this is the Teaching Health Center Graduate Medical Education program, which places physician and dental trainees in health centers, mostly in primary care settings and rural or underserved areas ( HRSA, 2021 ).
Health centers partner with the communities in which they operate in a variety of ways—from designing communication materials that community members want to working with local health departments to optimize and widen services offered and populations served ( Mader et al., 2019 ; NACHC and NACCHO, 2010 ). Initiatives such as the Migrant Clinicians Network also work with health centers to help improve access and reduce disparities among vulnerable migrant populations ( MCN, 2021 ). These models of partnership have improved health outcomes for millions of Americans and been shown to reduce access to care disparities for disadvantaged populations ( HRSA, 2020b ; Jones et al., 2013 ).
Indian Health Service
An agency within HHS, the IHS provides health care to approximately 2.6 million American Indian and Alaska Native people from more than 574 federally recognized tribes in 37 states ( IHS, 2020a ). Its primary care clinics include federal, tribal, and Urban Indian Health organizations that provide comprehensive care across the lifespan in rural areas, on reservations, and, increasingly, in urban population centers ( IHS, 2020b ). Many IHS-affiliated clinics serve as safety net clinics to both IHS beneficiaries and non-beneficiaries within their communities, and some are also designated FQHCs ( IHS, 2005 , 2020c ). The vast majority of IHS primary care is administered by tribes through self-determination contracts rather than by the federal government, with more than 60 percent of IHS appropriations administered by tribes ( IHS, 2020b ). Self-determination is at the heart of person-centered, family-centered, and community-oriented primary care. It enhances the mission of the IHS, which is to raise the physical, mental, social, and spiritual health of American Indian and Alaska Native people to the highest level. As recognized in the 2019 IHS strategic plan, ensuring the availability and accessibility of high-quality, culturally appropriate, primary, and preventive care services to all beneficiaries best supports accomplishing the IHS mission ( IHS, 2019 ).
Despite many Tribal and Urban Indian Health Programs serving as “the glue that holds their communities together,” the IHS is chronically underfunded and provides health care services to less than half the eligible population ( UCLA American Indian Studies Center, 2016 ; Urban Indian Health Commission, 2007 , p. 7). This underfunding contributes to the persistent health disparities among the American Indian and Alaska Native population ( Warne and Frizzell, 2014 ). A 2018 U.S. Government Accountability Office (GAO) report found that IHS, as an agency, spends approximately $4,000 per beneficiary, which represents less than 50 and 30 percent of the amount spent by the VA ($10,692) and Medicare ($13,185), respectively ( GAO, 2018b ). A separate GAO report found that in part as a result of its inability to match market-rate salaries, IHS struggles to fill vacancies for clinicians, which negatively affects patient access and quality of care ( GAO, 2018a ). Evidence also suggests IHS could be more systematic in assessing community needs ( GAO, 2020 ). Despite these significant limitations and challenges, many Tribal and Urban Indian Health Programs have found ways to thrive and deliver comprehensive and holistic community-oriented health care to their communities to achieve the IHS mission. SCF's Nuka System of Care represents the gold standard for tribal health organizations seeking to transform care for their own people and communities, as evidenced by its outcomes achievements and multiple quality awards ( Gottlieb, 2013 ).
School-Based Health Center Partnerships
The nearly 2,600 school-based health centers (SBHCs) represent another example of effective partnerships between community organizations and primary care that have increased access ( Love et al., 2019b ). Some 6.3 million students nationwide have access to care at an SBHC from an interprofessional team of clinicians, including primary care and mental health clinicians, in collaboration with the school community. SBHCs often function as a partnership between the school and the community's health organization, such as a health center, hospital, or local health department. Specific SBHC services vary based on community needs and resources as determined through collaborations among the community, the school district, and local health care clinicians. Sixty-two percent of SBHCs have provided services to individuals other than the students in their schools, including faculty and school personnel, family members of student users, out-of-school youth, and others in the broader community. This enhanced access to care, including primary care, has reduced health care disparities for disadvantaged populations and improved oral health outcomes ( Love et al., 2019b ).
In recent years, SBHCs have begun using telehealth to further expand their reach into communities and enhance the effectiveness of their services. More than half the SBHCs offering telehealth serve rural communities, where access to care is often limited by clinician shortages and transportation issues, and approximately three-quarters are staffed by primary care clinicians only, with the remainder staffed by primary care and mental health care clinicians ( Love et al., 2019a ).
Nurse-Managed Health Centers
Nurse-managed health centers (NMHCs) deliver whole-person primary care and are led and primarily staffed by advanced practice registered nurses (APRNs). The estimated 250 NMHCs in the United States serve more than 1.5 million medically underserved people, typically in low-income urban and rural areas ( Esperat et al., 2012 ; IOM, 2011 ). Most NMHCs are affiliated with university-based nursing schools or independent nonprofits, but some are affiliated with FQHCs, SBHCs, or other health centers.
Though NMHCs resemble community health centers in the populations and areas they serve, they are generally ineligible for FQHC status and federal funding due to a governance structure that includes the boards of their founding institutions, rather than the center's patients ( Hansen-Turton et al., 2010 ). To enable federal support, section 5208 of the ACA established a federal program to fund NMHCs, earmarking $50 million to be distributed that year via one-time grants and noting that “such sums as may be necessary for each of the fiscal years 2011 through 2014.” 9 Through HRSA, nearly $15 million in grants was awarded to 10 NMHCs, which provided care to more than 94,000 patients and trained more than 900 APRNs ( Cooper, n.d. ; Hansen-Turton, 2012 ). However, in an effort to decrease overall spending, federal funding stopped there and the program was not renewed ( Carthon et al., 2015 ).
Settings of Care for Older Adults
Older adults may need to receive primary care in a variety of settings outside of a traditional primary care practice. Residents of nursing homes often have complex care needs and include individuals who need post-acute care (after a hospital stay) and those who are long-term stay residents. Care of the nursing home resident includes assessment and management of both acute and chronic physical and psychosocial health care needs, coordination of needed health care services, the management of transitions between different health care settings, and advance care planning, among other services ( Unwin et al., 2010 ). Increasingly, medical care in nursing homes is provided by nurse practitioners (NPs) and physician assistants ( Teno et al., 2017 ).
Some older adults are home bound and thus rely on home-based care. The Independence at Home model provides comprehensive primary care services to Medicare beneficiaries with severe chronic illness and disability within their own homes ( CMS, 2020a ). The VA also has a home-based primary care program that serves veterans in their homes ( VA, 2020 ).
Across settings, the Geriatric Resources for Assessment and Care of Elders (GRACE) model focuses on primary care for low-income older adults ( Counsell et al., 2006 ). An NP paired with a social worker—the support team—leads the GRACE model, and the two professionals work together with an interdisciplinary team (including a geriatrician, pharmacist, physical therapist, mental health social worker, and community services liaison) to develop a care plan. The support team then works directly with the primary care physician to implement the plan. The model includes in-home visits by the support team, and plays a particularly important role in continuity of care during care transitions ( Bielaszka-DuVernay, 2011 ). The GRACE model has been associated with satisfaction among primary care physicians ( Counsell et al., 2009 ) and improved quality of care and quality of life ( Counsell et al., 2006 ). For high-risk patients, the model has been associated with reduced hospitalization rates ( Counsell et al., 2007 ).
Each of the previous levers requires supportive policies and payment arrangements. FFS payment covers the vast majority of primary care payment in the United States today and is a major challenge for primary care practices when partnering with communities, including the use of community members like CHWs and promotores de salud. Currently, CHWs are paid through a patchwork of funding options, such as Medicaid demonstration waivers, health homes, Medicaid managed care plans, and grants ( Lloyd et al., 2020 ). This gap would be addressed by a comprehensive payment model that supports the organization and delivery of primary care services that fits community needs, as outlined in Chapter 9 . For example, if certain communities want to expand their CHW workforce and integrate CHWs into their primary care teams, this comprehensive payment would allow for flexible allocation of resources and not depend on billing for each individual service provided by only certain members of the care team (e.g., physician, NP) under certain conditions (e.g., billable in-person visit code). In addition, incremental financing options could more adequately fund CHWs and other primary care–community partnerships. One example is a policy initiative currently under consideration that would support creating an optional Medicaid benefit to fund CHWs and be linked to evidence-informed standards for hiring, training, and deploying them ( Biden, 2020 ).
- FINDINGS AND CONCLUSIONS
Moving from patient-centered care to a person-centered, family-centered, and community-oriented approach represents an evolution of primary care to focus on individual people in the context of their lived experiences, their family, their social worlds, and their community. The relationship between the person seeking care (and their family) and the interprofessional team is an essential component of this shift. Building and maintaining this relationship in what is currently a disease-focused system, and achieving personalized, prioritized, and coordinated care for all people and families in communities, will require a system that supports developing and sustaining strong individual and community relationships in primary care to build a foundation for dismantling the pervasive systemic inequities in health care. Supporting and expanding delivery models, particularly those for the underserved (such as health centers), and empaneling populations will help ensure that all Americans have a usual source of primary care. Creating opportunities for individuals, families, and communities to participate in the organizational decision making at health care organizations and that related to the care itself will help the nation to reduce health disparities, particularly in underserved populations, and support achieving health equity for all populations.
Instead of responding to whole-health needs using a community-oriented approach, clinicians and health care organizations are rewarded for preventing, diagnosing, and treating diseases and performing procedures, prescribing medications, and providing care based on traditional biomedical models. Multiple levers can help shift primary care toward community-oriented models, including data systems, interprofessional care teams, care delivery settings, and partnerships between primary care, public health, and community-based organizations. All of these levers can be influenced by policy changes and innovative payment models.
As the United States grapples with the effects of the COVID-19 pandemic, levels of unemployment not seen since the Great Depression, and a reckoning of its long-standing history of racism and injustice, primary care will have to transform to meet current demands. This is an opportunity to radically reimagine it so that it is built around the people it serves, their families, and their communities, paid in ways that support this approach, and grounded in relationship-centered care, equity, and social justice. Until the barriers to innovation and sustainability are removed, it will be challenging to achieve high-quality, high-value primary care for all communities. Without success in expanding and supporting primary care's ability to address the needs of not only individuals but families and communities, the nation will be challenged to meet the health care needs of all communities, particularly underserved populations.
- AAFP (American Academy of Family Physicians). Survey takes hard look at physician-patient conversations. 2018. [August 24, 2020]. https://www .aafp.org /news/practice-professional-issues /20181107doc-patientcomms .html .
- AANP (American Association of Nuse Practitioners). Position statement: Telehealth. Austin, TX: American Association of Nurse Practitioners; 2019.
- Adamson M. The patient-centered medical home: An essential destination on the road to reform. American Health & Drug Benefits. 2011; 4 (2):122–124. [ PMC free article : PMC4106584 ] [ PubMed : 25126345 ]
- Adler NE, Rehkopf DH. U.S. disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health. 2008; 29 (1):235–252. [ PubMed : 18031225 ]
- Adler NE, Glymour MM, Fielding J. Addressing social determinants of health and health inequalities. JAMA. 2016; 316 (16):1641–1642. [ PubMed : 27669456 ]
- AHRQ (Agency for Healthcare Research and Quality). Physician burnout. Rockville, MD: Agency for Healthcare Research and Quality; 2017.
- AHRQ. Guide to improving patient safety in primary care settings by engaging patients and families. Rockville, MD: Agency for Healthcare Research and Quality; 2018.
- AIR (American Institute for Research). Empanelment implementation guide. Washington, DC: American Institute for Research; 2013.
- Alexander JA, Cohen GR, Wise CG, Green LA. The policy context of patient centered medical homes: Perspectives of primary care providers. Journal of General Internal Medicine. 2013; 28 (1):147–153. [ PMC free article : PMC3539022 ] [ PubMed : 22790613 ]
- Alsan M, Garrick O, Graziani G. Does diversity matter for health? Experimental evidence from Oakland. American Economic Review. 2019; 109 (12):4071–4111.
- Alsan M, Wanamaker M, Hardeman RR. The Tuskegee study of untreated syphilis: A case study in peripheral trauma with implications for health professionals. Journal of General Internal Medicine. 2020; 35 (1):322–325. [ PMC free article : PMC6957600 ] [ PubMed : 31646456 ]
- AMA (American Medical Association). Point-of care registries: Proactively manage chronic care conditions. 2016. [May 6, 2020]. https://edhub .ama-assn .org/steps-forward/module/2702745 .
- AMA. AMA digital health research: Physicians' motivations and requirements for adopting digital health and attitudinal shifts from 2016–2019. Chicago, IL: American Medical Association; 2020.
- American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. Patient-centered care for older adults with multiple chronic conditions: A stepwise approach from the American Geriatrics Society: American Geriatrics Society expert panel on the care of older adults with multimorbidity. Journal of the American Geriatrics Society. 2012; 60 (10):1957–1968. [ PMC free article : PMC4459791 ] [ PubMed : 22994844 ]
- Anderson EJ, Judd LR, May JT, New PK. The neighborhood health center program: Its growth and problems: An introduction. Washington, DC: National Association of Community Health Centers; 1976.
- Andrades M, Kausar S, Ambreen A. Role and influence of the patient's companion in family medicine consultations: “The patient's perspective.” Journal of Family Medicine and Primary Care. 2013; 2 (3):283–287. [ PMC free article : PMC3902688 ] [ PubMed : 24479099 ]
- Andres C, Spenceley S, Cook LL, Wedel R, Gelber T. Improving primary care: Continuity is about relationships. Canadian Family Physician. 2016; 62 (2):116–119. [ PMC free article : PMC4755624 ] [ PubMed : 26884518 ]
- Arizona Prevention Research Center. National community health worker advocacy survey. Tucson, AZ: University of Arizona; 2015.
- Artiga S, Hinton E. Beyond health care: The role of social determinants in promoting health and health equity. 2018. [January 21, 2021]. https://www .kff.org/racial-equity-and-health-policy /issue-brief /beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity .
- Bailey MJ, Goodman-Bacon A. The war on poverty's experiment in public medicine: Community health centers and the mortality of older Americans. American Economic Review. 2015; 105 (3):1067–1104. [ PMC free article : PMC4436657 ] [ PubMed : 25999599 ]
- Barzin A, Wohl DA, Daaleman TP. Development and implementation of a COVID-19 respiratory diagnostic center. Annals of Family Medicine COVID-19 Collection. 2020; 18 (5):464. [ PMC free article : PMC7489981 ] [ PubMed : 32928767 ]
- Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemedicine and e-Health. 2020; 26 (5):571–573. [ PubMed : 32275485 ]
- Batista R, Pottie K, Bouchard L, Ng E, Tanuseputro P, Tugwell P. Primary health care models addressing health equity for immigrants: A systematic scoping review. Journal of Immigrant and Minority Health. 2018; 20 (1):214–230. [ PubMed : 27858278 ]
- Beasley JW, Hankey TH, Erickson R, Stange KC, Mundt M, Elliott M, Wiesen P, Bobula J. How many problems do family physicians manage at each encounter? A WREN study. Annals of Family Medicine. 2004; 2 (5):405–410. [ PMC free article : PMC1466713 ] [ PubMed : 15506571 ]
- Bergman D, Bethell C, Gombojav N, Hassink S, Stange KC. Physical distancing with social connectedness. Annals of Family Medicine. 2020; 18 (3):272–277. [ PMC free article : PMC7213990 ] [ PubMed : 32393566 ]
- Biden J. The Biden plan for mobilizing American talent and heart to create a 21st century caregiving and education workforce. 2020. [August 17, 2020]. https://medium .com/@JoeBiden /the-biden-plan-for-mobilizing-american-talent-and-heart-to-create-a-21st-century-caregiving-and-af5ba2a2dfeb .
- Bielaszka-DuVernay C. The GRACE model: In-home assessments lead to better care for dual eligibles. Health Affairs. 2011; 30 (3):431–434. [ PubMed : 21383359 ]
- Bitton A, Fifield J, Ratcliffe H, Karlage A, Wang H, Veillard JH, Schwarz D, Hirschhorn LR. Primary healthcare system performance in low-income and middle-income countries: A scoping review of the evidence from 2010 to 2017. BMJ Global Health. 2019; 4 :e001551. [ PMC free article : PMC6703296 ] [ PubMed : 31478028 ]
- Black RE, Taylor CE, Arole S, Bang A, Bhutta ZA, Chowdhury AMR, Kirk-wood BR, Kureshy N, Lanata CF, Phillips JF, Taylor M, Victora CG, Zhu Z, Perry HB. Comprehensive review of the evidence regarding the effectiveness of community-based primary health care in improving maternal, neonatal and child health: 8. Summary and recommendations of the expert panel. Journal of Global Health. 2017; 7 (1):010908. [ PMC free article : PMC5475312 ] [ PubMed : 28685046 ]
- Blaum CS, Rosen J, Naik AD, Smith CD, Dindo L, Vo L, Hernandez-Bigos K, Esterson J, Geda M, Ferris R, Costello D, Acampora D, Meehan T, Tinetti ME. Feasibility of implementing patient priorities care for older adults with multiple chronic conditions. Journal of the American Geriatrics Society. 2018; 66 (10):2009–2016. [ PMC free article : PMC7015118 ] [ PubMed : 30281777 ]
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002; 288 (14):1775–1779. [ PubMed : 12365965 ]
- Bodenheimer T, Ghorob A, Willard-Grace R, Grumbach K. The 10 building blocks of high-performing primary care. Annals of Family Medicine. 2014; 12 (2):166–171. [ PMC free article : PMC3948764 ] [ PubMed : 24615313 ]
- Bogart LM, Wagner GJ, Green HD Jr., Mutchler MG, Klein DJ, McDavitt B, Lawrence SJ, Hilliard CL. Medical mistrust among social network members may contribute to antiretroviral treatment nonadherence in African Americans living with HIV. Social Science & Medicine. 2016; 164 :133–140. [ PMC free article : PMC4981525 ] [ PubMed : 27046475 ]
- Bor J, Cohen GH, Galea S. Population health in an era of rising income inequality: USA, 1980-2015. The Lancet. 2017; 389 (10077):1475–1490. [ PubMed : 28402829 ]
- Borrell-Carrió F, Suchman AL, Epstein RM. The biopsychosocial model 25 years later: Principles, practice, and scientific inquiry. Annals of Family Medicine. 2004; 2 (6):576–582. [ PMC free article : PMC1466742 ] [ PubMed : 15576544 ]
- Bosworth A, Ruhter J, Samson LW, Sheingold S, Taplin C, Tarazi W, Zuckerman R. Medicare beneficiary use of telehealth visits: Early data from the start of the COVID-19 pandemic. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; 2020.
- Botelho RJ, Lue BH, Fiscella K. Family involvement in routine health care: A survey of patients' behaviors and preferences. Journal of Family Practice. 1996; 42 (6):572–576. [ PubMed : 8656167 ]
- Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: Implications for pay for performance. JAMA. 2005; 294 (6):716–724. [ PubMed : 16091574 ]
- Braddock CH 3rd, Snyder L, Neubauer RL, Fischer GS. American College of Physicians Ethics, Professionalism and Human Rights Committee, and the Society of General Internal Medicine Ethics Committee. The patient-centered medical home: An ethical analysis of principles and practice. Journal of General Internal Medicine. 2013; 28 (1):141–146. [ PMC free article : PMC3539020 ] [ PubMed : 22829295 ]
- Braveman P. What are health disparities and health equity? We need to be clear. Public Health Reports. 2014; 129 (Suppl 2):5–8. [ PMC free article : PMC3863701 ] [ PubMed : 24385658 ]
- Braveman P, Gottlieb L. The social determinants of health: It's time to consider the causes of the causes. Public Health Reports. 2014; 129 (Suppl 2):19–31. [ PMC free article : PMC3863696 ] [ PubMed : 24385661 ]
- Braveman PA, Kumanyika S, Fielding J, Laveist T, Borrell LN, Manderscheid R, Troutman A. Health disparities and health equity: The issue is justice. American Journal of Public Health. 2011; 101 (Suppl 1):S149–S155. [ PMC free article : PMC3222512 ] [ PubMed : 21551385 ]
- Brown EJ, Kangovi S, Sha C, Johnson S, Chanton C, Carter T, Grande DT. Exploring the patient and staff experience with the process of primary care. Annals of Family Medicine. 2015; 13 (4):347–353. [ PMC free article : PMC4508176 ] [ PubMed : 26195680 ]
- Brown JB, Brett P, Stewart M, Marshall JN. Roles and influence of people who accompany patients on visits to the doctor. Canadian Family Physician. 1998; 44 :1644–1650. [ PMC free article : PMC2277722 ] [ PubMed : 9721420 ]
- Brownlee B, Van Borkulo N. Empanelment: Establishing patient–provider relationships. Seattle, WA: Qualis Health, The MacColl Center for Health Care Innovation at the Group Health Research Institute; 2013.
- Buchmueller T, Carpenter CS. Disparities in health insurance coverage, access, and outcomes for individuals in same-sex versus different-sex relationships, 2000–2007. American Journal of Public Health. 2010; 100 (3):489–495. [ PMC free article : PMC2820046 ] [ PubMed : 20075319 ]
- Burnham AC. The community health problem. New York: The Macmillan Company; 1920.
- Burrow JG. Organized medicine in the progressive era: The move toward monopoly. Baltimore, MD: The Johns Hopkins University Press; 1977.
- Campbell JD, Brooks M, Hosokawa P, Robinson J, Song L, Krieger J. Community health worker home visits for Medicaid-enrolled children with asthma: Effects on asthma outcomes and costs. American Journal of Public Health. 2015; 105 (11):2366–2372. [ PMC free article : PMC4605150 ] [ PubMed : 26270287 ]
- Carthon JMB, Barnes H, Sarik DA. Federal polices influence access to primary care and nurse practitioner workforce. The Journal for Nurse Practitioners. 2015; 11 (5):526–530. [ PMC free article : PMC4596547 ] [ PubMed : 26457073 ]
- CDC (Centers for Disease Control and Prevention). Using telehealth to expand access to essential health services during the COVID-19 pandemic. 2020. [December 21, 2020]. https://www .cdc.gov/coronavirus /2019-ncov/hcp/telehealth .html#edn6 .
- Cené CW, Haymore LB, Lin FC, Laux J, Jones CD, Wu JR, DeWalt D, Pignone M, Corbie-Smith G. Family member accompaniment to routine medical visits is associated with better self-care in heart failure patients. Chronic Illness. 2015; 11 (1):21–32. [ PMC free article : PMC8099456 ] [ PubMed : 24740555 ]
- Chang CH, Bynum JPW, Lurie JD. Geographic expansion of federally qualified health centers 2007–2014. Journal of Rural Health. 2019; 35 (3):385–394. [ PMC free article : PMC6478577 ] [ PubMed : 30352132 ]
- Chaudhri S, Zweig KC, Hebbar P, Angell S, Vasan A. Trauma-informed care: A strategy to improve primary healthcare engagement for persons with criminal justice system involvement. Journal of General Internal Medicine. 2019; 34 (6):1048–1052. [ PMC free article : PMC6544694 ] [ PubMed : 30912031 ]
- Chen J, Mullins CD, Novak P, Thomas SB. Personalized strategies to activate and empower patients in health care and reduce health disparities. Health Education & Behavior. 2016; 43 (1):25–34. [ PMC free article : PMC4681678 ] [ PubMed : 25845376 ]
- Chokshi DA, Cohen L. Progress in primary care—from Alma-Ata to Astana. JAMA. 2018; 320 (19):1965–1966. [ PubMed : 30458480 ]
- CHroniCles. Community health centers: Chronicling their history and broader meaning. 2020. [July 17, 2020]. https://www .chcchronicles .org/stories/community-health-centers-chronicling-their-history-and-broader-meaning .
- Clay AM, Parsh B. Patient- and family-centered care: It's not just for pediatrics anymore. AMA Journal of Ethics. 2016; 18 (1):40–44. [ PubMed : 26854635 ]
- Clayman ML, Roter D, Wissow LS, Bandeen-Roche K. Autonomy-related behaviors of patient companions and their effect on decision-making activity in geriatric primary care visits. Social Science & Medicine. 2005; 60 (7):1583–1591. [ PubMed : 15652689 ]
- CMS (Centers for Medicare & Medicaid Services). Medicare benefit policy manual. Baltimore, MD: Centers for Medicare & Medicaid Services; 2019. [January 12, 2021]. Chapter 13—rural health clinic (RHC) and federally qualified health center (FQHC) services. https://www .cms.gov/Regulations-and-Guidance /Guidance/Manuals /Internet-Only-Manuals-IOMs-Items /CMS012673 .
- CMS. Independence at home demonstration. 2020a. [February 26, 2021]. https://innovation .cms .gov/innovation-models /independence-at-home .
- CMS. Interim final rule with comment period: Medicare and Medicaid programs; policy and regulatory revisions in response to the COVID-19 public health emergency as published on April 6, 2020. Federal Register. 2020b; 85 (66):19230–19292. [December 18, 2020]; https://www .federalregister .gov/documents /2020/04/06/2020-06990 /medicare-and-medicaid-programs-policy-and-regulatory-revisions-in-response-to-the-covid-19-public .
- Cohen JJ, Gabriel BA, Terrell C. The case for diversity in the health care workforce. Health Affairs. 2002; 21 (5):90–102. [ PubMed : 12224912 ]
- Cole-Kelly K, Seaburn D. Five areas of questioning to promote a family-oriented approach in primary care. Families, Systems, & Health. 1999; 17 (3):341–348.
- Cometto G, Ford N, Pfaffman-Zambruni J, Akl EA, Lehmann U, McPake B, Ballard M, Kok M, Najafizada M, Olaniran A, Ajuebor O, Perry HB, Scott K, Albers B, Shlonsky A, Taylor D. Health policy and system support to optimise community health worker programmes: An abridged WHO guideline. The Lancet Global Health. 2018; 6 (12):e1397–e1404. [ PubMed : 30430994 ]
- Committee on Hospital Care. Family-centered care and the pediatrician's role. Pediatrics. 2003; 112 (3):691–696. [ PubMed : 12949306 ]
- Committee on Hospital Care and IPFCC (Institute for Patient- and Family-Centered Care). Patient- and family-centered care and the pediatrician's role. Pediatrics. 2012; 129 (2):394–404. [ PubMed : 22291118 ]
- Committee on Pediatric Workforce. The use of telemedicine to address access and physician workforce shortages. Pediatrics. 2015; 136 (1):202. [ PubMed : 26122802 ]
- Cooper K. Affordable Care Act nurse managed health clinics (NMHC): Frequently asked questions. n.d. [March 9, 2021]. https://www .hrsa.gov /sites/default/files /grants/healthprofessions/acafaq.pdf .
- Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Annals of Internal Medicine. 2003; 139 (11):907–915. [ PubMed : 14644893 ]
- Cordina J, Stein G, Levin E. McKinsey consumer healthcare insights. 2020. [December 18, 2020]. https://www .mckinsey .com/industries/healthcare-systems-and-services /our-insights /helping-us-healthcare-stakeholders-understand-the-human-side-of-the-covid-19-crisis .
- Cornelius T, Moise N, Birk JL, Edmondson D, Chang BP. The presence of companions during emergency department evaluation and its impact on perceptions of clinician-patient communication. Emergency Medicine Journal. 2018; 35 (11):701–703. [ PMC free article : PMC6335085 ] [ PubMed : 30131354 ]
- Coster JE, Turner JK, Bradbury D, Cantrell A. Why do people choose emergency and urgent care services? A rapid review utilizing a systematic literature search and narrative synthesis. Academic Emergency Medicine. 2017; 24 (9):1137–1149. [ PMC free article : PMC5599959 ] [ PubMed : 28493626 ]
- Counsell SR, Callahan CM, Buttar AB, Clark DO, Frank KI. Geriatric Resources for Assessment and Care of Elders (GRACE): A new model of primary care for low-income seniors. Journal of the American Geriatrics Society. 2006; 54 (7):1136–1141. [ PubMed : 16866688 ]
- Counsell SR, Callahan CM, Clark DO, Tu W, Buttar AB, Stump TE, Ricketts GD. Geriatric care management for low-income seniors: A randomized controlled trial. JAMA. 2007; 298 (22):2623–2633. [ PubMed : 18073358 ]
- Counsell SR, Callahan CM, Tu W, Stump TE, Arling GW. Cost analysis of the Geriatric Resources for Assessment and Care of Elders care management intervention. Journal of the American Geriatrics Society. 2009; 57 (8):1420–1426. [ PMC free article : PMC3874584 ] [ PubMed : 19691149 ]
- Cyril S, Smith BJ, Possamai-Inesedy A, Renzaho AM. Exploring the role of community engagement in improving the health of disadvantaged populations: A systematic review. Global Health Action. 2015; 8 :29842. [ PMC free article : PMC4685976 ] [ PubMed : 26689460 ]
- Daniels EC, Powe BD, Metoyer T, McCray G, Baltrus P, Rust GS. Increasing knowledge of cardiovascular risk factors among African Americans by use of community health workers: The ABCD community intervention pilot project. Journal of the National Medical Association. 2012; 104 (3–4):179–185. [ PMC free article : PMC4017345 ] [ PubMed : 22774385 ]
- Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. Journal of General Internal Medicine. 2005; 20 (10):953–957. [ PMC free article : PMC1490238 ] [ PubMed : 16191145 ]
- Davis MM. Goal-posts and yardsticks in health center work. American Journal of Public Health. 1927; 17 (5):433–440. [ PMC free article : PMC1321776 ] [ PubMed : 18012149 ]
- Derose KP, Williams MV, Branch CA, Flórez KR, Hawes-Dawson J, Mata MA, Oden CW, Wong EC. A community-partnered approach to developing church-based interventions to reduce health disparities among African-Americans and Latinos. Journal of Racial and Ethnic Health Disparities. 2019; 6 (2):254–264. [ PMC free article : PMC6378139 ] [ PubMed : 30120736 ]
- DeVoe JE, Saultz JW, Krois L, Tillotson CJ. A medical home versus temporary housing: The importance of a stable usual source of care. Pediatrics. 2009; 124 (5):1363–1371. [ PMC free article : PMC3116519 ] [ PubMed : 19841117 ]
- Driscoll DL, Hiratsuka V, Johnston JM, Norman S, Reilly KM, Shaw J, Smith J, Szafran QN, Dillard D. Process and outcomes of patient-centered medical care with Alaska Native people at Southcentral Foundation. Annals of Family Medicine. 2013; 11 (Suppl 1):S41–S49. [ PMC free article : PMC3707246 ] [ PubMed : 23690385 ]
- Edgoose JYC, Edgoose JM. Finding hope in the face-to-face. Annals of Family Medicine. 2017; 15 (3):272–274. [ PMC free article : PMC5422090 ] [ PubMed : 28483894 ]
- Ekman I, Swedberg K, Taft C, Lindseth A, Norberg A, Brink E, Carlsson J, Dahlin-Ivanoff S, Johansson IL, Kjellgren K, Lidén E, Öhlén J, Olsson L-E, Rosén H, Rydmark M, Sunnerhagen KS. Person-centered care—ready for prime time. European Journal of Cardiovascular Nursing. 2011; 10 (4):248–251. [ PubMed : 21764386 ]
- Ellner AL, Phillips RS. The coming primary care revolution. Journal of General Internal Medicine. 2017; 32 (4):380–386. [ PMC free article : PMC5377886 ] [ PubMed : 28243869 ]
- Enard KR, Ganelin DM. Reducing preventable emergency department utilization and costs by using community health workers as patient navigators. Journal of Healthcare Management. 2013; 58 (6):412–427. discussion 428. [ PMC free article : PMC4142498 ] [ PubMed : 24400457 ]
- Eng E, Salmon ME, Mullan F. Community empowerment: The critical base for primary health care. Family & Community Health: The Journal of Health Promotion & Maintenance. 1992; 15 (1):1–12.
- Engel GL. The need for a new medical model: A challenge for biomedicine. Psycho-dynamic Psychiatry. 2012; 40 (3):377–396. [ PubMed : 23002701 ]
- Epstein L, Gofin J, Gofin R, Neumark Y. The Jerusalem experience: Three decades of service, research, and training in community-oriented primary care. American Journal of Public Health. 2002; 92 (11):1717–1721. [ PMC free article : PMC1447316 ] [ PubMed : 12406791 ]
- Esperat MCR, Hanson-Turton T, Richardson M, Tyree Debisette A, Rupinta C. Nurse-managed health centers: Safety-net care through advanced nursing practice. Journal of the American Academy of Nurse Practitioners. 2012; 24 (1):24–31. [ PubMed : 22243678 ]
- Etz RS. People are primary: A perspective from the Keystone IV conference. Journal of the American Board of Family Practice. 2016; 29 (Suppl 1):S40–S44. [ PubMed : 27387163 ]
- Feagin J, Bennefield Z. Systemic racism and U.S. health care. Social Science & Medicine. 2014; 103 :7–14. [ PubMed : 24507906 ]
- Fertig AR, Corso PS, Balasubramaniam D. Benefits and costs of a free community-based primary care clinic. Journal of Health and Human Services Administration. 2012; 34 (4):456–470. [ PubMed : 22530286 ]
- Finkelstein A, Zhou A, Taubman S, Doyle J. Health care hotspotting—a randomized, controlled trial. New England Journal of Medicine. 2020; 382 (2):152–162. [ PMC free article : PMC7046127 ] [ PubMed : 31914242 ]
- Flocke SA, Goodwin MA, Stange KC. The effect of a secondary patient on the family practice visit. Journal of Family Practice. 1998; 46 (5):429–434. [ PubMed : 9598002 ]
- Fortuna RJ, Johnson W, Clark JS, Messing S, Flynn S, Judge SR. Population Health Management. 2020. Impact of patient-centered medical home transformation on providers, staff, and quality. Epub ahead of print. [ PubMed : 32208969 ]
- Friedberg MW, Schneider EC, Rosenthal MB, Volpp KG, Werner RM. Association between participation in a multipayer medical home intervention and changes in quality, utilization, and costs of care. JAMA. 2014; 311 (8):815–825. [ PMC free article : PMC6348473 ] [ PubMed : 24570245 ]
- GAO (U.S. Government Accountability Office). Indian Health Service: Agency faces ongoing challenges filling provider vacancies. Washington, DC: U.S. Government Accountability Office; 2018a.
- GAO. Indian Health Service: Spending levels and characteristics of IHS and three other federal health care programs. Washington, DC: U.S. Government Accountability Office; 2018b.
- GAO. Indian Health Service: Actions needed to improve oversight of federal facilities' decision-making about the use of funds. Washington, DC: U.S. Government Accountability Office; 2020.
- Garcia ME, Bindman AB, Coffman J. Language-concordant primary care physicians for a diverse population: The view from California. Health Equity. 2019; 3 (1):343–349. [ PMC free article : PMC6626968 ] [ PubMed : 31312781 ]
- Garfield C, Kangovi S. Health Affairs Blog. May 10, 2019. [January 21, 2021]. Integrating community health workers into health care teams without coopting them. https://www .healthaffairs .org/do/10.1377/hblog20190507 .746358/full .
- Geiger HJ. Community-oriented primary care: A path to community development. American Journal of Public Health. 2002; 92 (11):1713–1716. [ PMC free article : PMC3221474 ] [ PubMed : 12406790 ]
- Gofin J, Gofin R, Stimpson JP. Community-oriented primary care (COPC) and the Affordable Care Act: An opportunity to meet the demands of an evolving health care system. Journal of Primary Care & Community Health. 2015; 6 (2):128–133. [ PubMed : 25351764 ]
- Gold R, Bunce A, Cowburn S, Davis JV, Nelson JC, Nelson CA, Hicks E, Cohen DJ, Horberg MA, Melgar G, Dearing JW, Seabrook J, Mossman N, Bulkley J. Does increased implementation support improve community clinics' guideline-concordant care? Results of a mixed methods, pragmatic comparative effectiveness trial. Implementation Science. 2019; 14 (1):100. [ PMC free article : PMC6894475 ] [ PubMed : 31805968 ]
- Gotler RS, Green LA, Etz RS. Milbank Quarterly Opinion. 2020. [June 10, 2020]. What 1966 can teach us about the future of primary care: The case for communities of solution. https://www .milbank.org /quarterly/opinions /what-1966-can-teach-us-about-the-future-of-primary-care-the-case-for-communities-of-solution .
- Gottlieb K. The Nuka system of care: Improving health through ownership and relationships. International Journal of Circumpolar Health. 2013; 72 [ PMC free article : PMC3752290 ] [ PubMed : 23984269 ]
- Green LA, Puffer JC. Family medicine at 40 years of age: The journey to transformation continues. Journal of the American Board of Family Medicine. 2010; 23 :S1–S4. [ PubMed : 20207908 ]
- Greene SM, Tuzzio L, Cherkin D. A framework for making patient-centered care front and center. The Permanente Journal. 2012; 16 (3):49–53. [ PMC free article : PMC3442762 ] [ PubMed : 23012599 ]
- Griswold KS, Lesko SE, Westfall JM, Folsom G. Communities of solution: Partnerships for population health. Journal of the American Board of Family Medicine. 2013; 26 (3):232–238. [ PubMed : 23657688 ]
- Hansen-Turton T. Nurse-managed health clinics provided badly needed primary care—but without funding, they and their patients are at risk. 2012. [March 9, 2021]. https://www .rwjf.org /en/blog/2012/01/nurse-managed-health-clinics-provided-badly-needed-primary-carebut-without-funding-they-and-their-patients-are-at-risk.html .
- Hansen-Turton T, Bailey DN, Torres N, Ritter A. Nurse-managed health centers. American Journal of Nursing. 2010; 110 (9):23–26. [ PubMed : 20736703 ]
- Health centres of tomorrow. The Lancet. 1947; 249 (6436):32–33. [ PubMed : 20278701 ]
- Helfrich CD, Dolan ED, Simonetti J, Reid RJ, Joos S, Wakefield BJ, Schectman G, Stark R, Fihn SD, Harvey HB, Nelson K. Elements of team-based care in a patient-centered medical home are associated with lower burnout among VA primary care employees. Journal of General Internal Medicine. 2014; 29 (Suppl 2):S659–S666. [ PMC free article : PMC4070238 ] [ PubMed : 24715396 ]
- Hiscock IV. The development of neighborhood health services in the United States. Milbank Quarterly. 1935; 13 (1):30–51.
- Holden KB, Hopkins J, Belton A, Butty K, Tabor DC, Satcher D. Leveraging science to advance health equity: A regional health policy research center's approach. Ethnicity & Disease. 2019; 29 (Suppl 2):323–328. [ PMC free article : PMC6604777 ] [ PubMed : 31308600 ]
- Hollander-Rodriguez J, DeVoe JE. Family medicine's task in population health: Defining it and owning it. Family Medicine. 2018; 50 (9):659–661. [ PubMed : 30307582 ]
- Hone T, Macinko J, Millett C. Revisiting Alma-Ata: What is the role of primary health care in achieving the sustainable development goals? The Lancet. 2018; 392 (10156):1461–1472. [ PubMed : 30343860 ]
- HRSA (Health Resources and Services Administration). Health center program compliance manual. 2018. [August 27, 2020]. https://bphc .hrsa.gov /programrequirements /compliancemanual/introduction.html .
- HRSA. Health center program. 2020a. [July 30, 2020]. https://bphc .hrsa.gov /programrequirements .
- HRSA. Health center program: Impact and growth. 2020b. [February 17, 2021]. https://bphc .hrsa.gov /about/healthcenterprogram .
- HRSA. Teaching Health Center Graduate Medical Education (THCGME) program. 2021. [March 30, 2021]. https://bhw .hrsa.gov /grants/medicine/thcgme .
- Hughes LS, Phillips RL Jr., DeVoe JE, Bazemore AW. Community vital signs: Taking the pulse of the community while caring for patients. Journal of the American Board of Family Practice. 2016; 29 (3):419–422. [ PubMed : 27170802 ]
- Hunt BR, Hurlbert MS. Black:white disparities in breast cancer mortality in the 50 largest cities in the United States, 2005–2014. Cancer Epidemiology. 2016; 45 :169–173. [ PubMed : 27720130 ]
- Igel LH, Lerner BH. Moving past individual and “pure” autonomy: The rise of family-centered care. AMA Journal of Ethics. 2016; 18 (1):56–62. [ PubMed : 26854637 ]
- IHS (Indian Health Service). Indian health manual. Rockville, MD: Indian Health Service; 2005. Part 2—services to Indians and others (Chapter 4 Other beneficiaries).
- IHS. Notice: Indian Health Service strategic plan fiscal year 2019–2023 as published on February 28, 2019. Federal Register. 2019; 84 (40):6796–6807. [December 18, 2020]; https://www .federalregister .gov/documents /2019/02/28/2019-03486 /indian-health-service-strategic-plan-fiscal-year-2019-2023 .
- IHS. About IHS. 2020a. [December 14, 2020]. https://www .ihs.gov/aboutihs .
- IHS. IHS profile. 2020b. [December 14, 2020]. https://www .ihs.gov/newsroom /factsheets/ihsprofile .
- IHS. Office of Urban Indian Health programs. 2020c. [December 14, 2020]. https://www .ihs.gov/urban .
- Institute for Clinical Systems Improvement. Building community relations: Real-life examples. Princeton, NJ: Robert Wood Johnson Foundation; 2014.
- International Conference on Primary Health Care. Declaration of Alma-Ata. Alma-Ata, USSR: World Health Organization; 1978.
- IOM (Institute of Medicine). Community oriented primary care: New directions for health services delivery. Washington, DC: National Academy Press; 1983. [ PubMed : 25121320 ]
- IOM. Primary care: America's health in a new era. Washington, DC: National Academy Press; 1996. [ PubMed : 25121221 ]
- IOM. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press; 2001. [ PubMed : 25057539 ]
- IOM. Retooling for an aging America: Building the health care workforce. Washington, DC: The National Academies Press; 2008. [ PubMed : 25009893 ]
- IOM. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press; 2011. [ PubMed : 24983041 ]
- IOM. Primary care and public health: Exploring integration to improve population health. Washington, DC: The National Academies Press; 2012. [ PubMed : 24851288 ]
- Izquierdo A, Ong M, Pulido E, Wells KB, Berkman M, Linski B, Sauer V, Miranda J. Community partners in care: 6- and 12-month outcomes of community engagement versus technical assistance to implement depression collaborative care among depressed older adults. Ethnicity & Disease. 2018; 28 (Suppl 2):339–348. [ PMC free article : PMC6128340 ] [ PubMed : 30202186 ]
- Jackson CS, Gracia JN. Addressing health and health-care disparities: The role of a diverse workforce and the social determinants of health. Public Health Reports. 2014; 129 (Suppl 2):57–61. [ PMC free article : PMC3863703 ] [ PubMed : 24385666 ]
- Janes EH. Health of tenement populations and the sanitary requirements of their dwelling. Reports and Papers of the American Public Health Association in the Years 1874–1875. 1876; 2 :115–124.
- Joint Learning Network for Universal Health Coverage, Ariadne Labs, and Comagine Health. Empanelment: A foundational component of primary health care. Ariadne Labs, Comagine Health; 2019.
- Joint Task Force for the Development of Telepsychology Guidelines for Psychologists. Guidelines for the practice of telepsychology. Washington, DC: American Psychological Association; 2013. [ PubMed : 24341643 ]
- Jolley J, Shields L. The evolution of family-centered care. Journal of Pediatric Nursing. 2009; 24 (2):164–170. [ PubMed : 19268238 ]
- Jones E, Shi L, Hayashi AS, Sharma R, Daly C, Ngo-Metzger Q. Access to oral health care: The role of federally qualified health centers in addressing disparities and expanding access. American Journal of Public Health. 2013; 103 (3):488–493. [ PMC free article : PMC3673494 ] [ PubMed : 23327254 ]
- Jones KA, Do S, Porras-Javier L, Contreras S, Chung PJ, Coker TR. Feasibility and acceptability in a community-partnered implementation of “CenteringParenting” for group well-child care. Academic Pediatrics. 2018; 18 (6):642–649. [ PubMed : 29890229 ]
- Kangovi S, Barg FK, Carter T, Levy K, Sellman J, Long JA, Grande D. Challenges faced by patients with low socioeconomic status during the post-hospital transition. Journal of General Internal Medicine. 2014a; 29 (2):283–289. [ PMC free article : PMC3912302 ] [ PubMed : 23918162 ]
- Kangovi S, Mitra N, Grande D, White ML, McCollum S, Sellman J, Shannon RP, Long JA. Patient-centered community health worker intervention to improve posthospital outcomes: A randomized clinical trial. JAMA Internal Medicine. 2014b; 174 (4):535–543. [ PubMed : 24515422 ]
- Kangovi S, Mitra N, Grande D, Huo H, Smith RA, Long JA. Community health worker support for disadvantaged patients with multiple chronic diseases: A randomized clinical trial. American Journal of Public Health. 2017; 107 (10):1660–1667. [ PMC free article : PMC5607679 ] [ PubMed : 28817334 ]
- Kark SL, Kark E. Promoting community health: From Pholela to jerusalem. Johannesburg, ZA: Witwatersrand University Press; 1999.
- Kark SL, Riche HL. A health study of South African Bantu school children. South African Medical Journal. 1944; 18 :100–103.
- Kennedy I. Patients are experts in their own field. BMJ. 2003; 326 (7402):1276–1277. [ PMC free article : PMC1126161 ] [ PubMed : 12805126 ]
- Kokorelias KM, Gignac MAM, Naglie G, Cameron JI. Towards a universal model of family centered care: A scoping review. BMC Health Services Research. 2019; 19 (1):564. [ PMC free article : PMC6693264 ] [ PubMed : 31409347 ]
- Kramer BJ, Creekmur B, Mitchell MN, Saliba D. Expanding home-based primary care to American Indian reservations and other rural communities: An observational study. Journal of the American Geriatrics Society. 2018; 66 (4):818–824. [ PubMed : 29529341 ]
- Kravitz RL, Feldman MD. Reinventing primary care: Embracing change, preserving relationships. Journal of General Internal Medicine. 2017; 32 (4):369–370. [ PMC free article : PMC5377901 ] [ PubMed : 28243872 ]
- Krist AH, Shenson D, Woolf SH, Bradley C, Liaw WR, Rothemich SF, Slonim A, Benson W, Anderson LA. Clinical and community delivery systems for preventive care: An integration framework. American Journal of Preventive Medicine. 2013; 45 (4):508–516. [ PMC free article : PMC4544711 ] [ PubMed : 24050428 ]
- Kuhlthau KA, Bloom S, Van Cleave J, Knapp AA, Romm D, Klatka K, Homer CJ, Newacheck PW, Perrin JM. Evidence for family-centered care for children with special health care needs: A systematic review. Academic Pediatrics. 2011; 11 (2):136–143. [ PubMed : 21396616 ]
- Landon BE, Grumbach K, Wallace PJ. Integrating public health and primary care systems: Potential strategies from an IOM report. JAMA. 2012; 308 (5):461–462. [ PubMed : 22851111 ]
- Leppin AL, Schaepe K, Egginton J, Dick S, Branda M, Christiansen L, Burow NM, Gaw C, Montori VM. Integrating community-based health promotion programs and primary care: A mixed methods analysis of feasibility. BMC Health Services Research. 2018; 18 (1):72. [ PMC free article : PMC5793407 ] [ PubMed : 29386034 ]
- Levitan S. Healing the poor in their backyard. In: Hollister R, Kramer B, Bellin S, editors. Neighborhood health centers. Lexington, MA: Lexington Books; 1974. p. 54.
- Lewis C, Getachew Y, Abrams MK, Doty MM. Changes at community health centers, and how patients are benefiting: Results from the Commonwealth Fund national survey of federally qualified health centers, 2013–2018. 2019. [November 24, 2020]. https://www .commonwealth-fund .org/publications /issue-briefs/2019 /aug/changes-at-community-health-centers-how-patients-are-benefiting .
- Liss DT, Fishman PA, Rutter CM, Grembowski D, Ross TR, Johnson EA, Reid RJ. Outcomes among chronically ill adults in a medical home prototype. American Journal of Managed Care. 2013; 19 (10):e348–e358. [ PMC free article : PMC4074014 ] [ PubMed : 24304182 ]
- Lloyd J, Moses K, Davis R. Recognizing and sustaining the value of community health workers and promotores. Hamilton, NJ: Center For Health Care Strategies; 2020.
- Love H, Panchal N, Schlitt J, Behr C, Soleimanpour S. The use of telehealth in school-based health centers. Global Pediatric Health. 2019a; 6 :2333794X19884194. 2333794X19884194. [ PMC free article : PMC6811756 ] [ PubMed : 31692723 ]
- Love HE, Schlitt J, Soleimanpour S, Panchal N, Behr C. Twenty years of school-based health care growth and expansion. Health Affairs. 2019b; 38 (5):755–764. [ PubMed : 31059359 ]
- Mader K, Sammen JM, Klene C, Nguyen J, Simpson M, Ruland SL, Westfall JM. Community-designed messaging interventions to improve cost-of-care conversations in settings serving low-income, Latino populations. Annals of Internal Medicine. 2019; 170 (Suppl 9):S79–S86. [ PubMed : 31060058 ]
- Malat J, van Ryn M, Purcell D. Blacks' and whites' attitudes toward race and nativity concordance with doctors. Journal of the National Medical Association. 2009; 101 (8):800–807. [ PubMed : 19715044 ]
- Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: Evidence from the field. Journal of the American Medical Informatics Association. 2020; 27 (7):1132–1135. [ PMC free article : PMC7188161 ] [ PubMed : 32324855 ]
- Martin JC, Avant RF, Bowman MA, Bucholtz JR, Dickinson JR, Evans KL, Green LA, Henley DE, Jones WA, Matheny SC, Nevin JE, Panther SL, Puffer JC, Roberts RG, Rodgers DV, Sherwood RA, Stange KC, Weber CW. The future of family medicine: A collaborative project of the family medicine community. Annals of Family Medicine. 2004; 2 (Suppl 1):S3–S32. [ PMC free article : PMC1466763 ] [ PubMed : 15080220 ]
- Martinez KA, Rood M, Jhangiani N, Kou L, Rose S, Boissy A, Rothberg MB. Patterns of use and correlates of patient satisfaction with a large nationwide direct to consumer telemedicine service. Journal of General Internal Medicine. 2018; 33 (10):1768–1773. [ PMC free article : PMC6153236 ] [ PubMed : 30112737 ]
- Martinez-Bianchi V, Frank B, Edgoose J, Michener L, Rodriguez M, Gottlieb L, Reddick B, Kelly C, Yu K, Davis S, Carr J, Lee JW, Smith KL, New RD, Weida J. Addressing family medicine's capacity to improve health equity through collaboration, accountability and coalition-building. Family Medicine. 2019; 51 (2):198–203. [ PubMed : 30736047 ]
- MCN (Migrant Clinicians Network). Our story. 2021. [March 10, 2021]. https://www .migrantclinician .org/about/our-story .
- McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Affairs. 2002; 21 (2):78–93. [ PubMed : 11900188 ]
- Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. What impact has COVID-19 had on outpatient visits? New York: The Commonwealth Fund; 2020.
- Mitchell P, Wynia M, Golden R, McNellis B, Okun S, Webb CE, Rohrbach V, Von Kohorn I. Core principles & values of effective team-based health care. NAM Perspectives. National Academy of Medicine; Washington, DC: 2012. Discussion Paper.
- Montague E, Asan O. Dynamic modeling of patient and physician eye gaze to understand the effects of electronic health records on doctor-patient communication and attention. International Journal of Medical Informatics. 2014; 83 (3):225–234. [ PMC free article : PMC4046907 ] [ PubMed : 24380671 ]
- Morse M, Finnegan A, Wispelwey B, Ford C. Health Affairs Blog. Jul 2, 2020. [August 17, 2020]. Will COVID-19 pave the way for progressive social policies? Insights from critical race theory? https://www .healthaffairs .org/do/10.1377/hblog20200630 .184036/full .
- MSM (Morehouse School of Medicine). Southeast regional clinicians network membership. 2021. [March 2, 2021]. https://www .msm.edu/Research /research_centersandinstitutes /NCPC /divisions/research/sercn-membership .php .
- Mullan F, Epstein L. Community-oriented primary care: New relevance in a changing world. American Journal of Public Health. 2002; 92 (11):1748–1755. [ PMC free article : PMC3221479 ] [ PubMed : 12406800 ]
- NACHC (National Association of Community Health Centers). Community health center chartbook. Bethesda, MD: National Association of Community Health Centers; 2020a.
- NACHC. The facts about Medicaid's FQHC prospective payment system (PPS). National Association of Community Health Centers; 2020b.
- NACHC and NACCHO (National Association of County and City Health Officials). Partnerships between federally qualified health centers and local health departments for engaging in the development of a community-based system of care. Bethesda, MA: National Association of Community Health Centers; 2010.
- Naik AD, Dindo LN, Van Liew JR, Hundt NE, Vo L, Hernandez-Bigos K, Esterson J, Geda M, Rosen J, Blaum CS, Tinetti ME. Development of a clinically feasible process for identifying individual health priorities. Journal of the American Geriatrics Society. 2018; 66 (10):1872–1879. [ PMC free article : PMC10185433 ] [ PubMed : 30281794 ]
- NASEM (National Academies of Sciences, Engineering, and Medicine). Communities in action: Pathways to health equity. Washington, DC: The National Academies Press; 2017. [ PubMed : 28418632 ]
- NASEM. Integrating social care into the delivery of health care: Moving upstream to improve the nation's health. Washington, DC: The National Academies Press; 2019a. [ PubMed : 31940159 ]
- NASEM. Investing in interventions that address non-medical, health-related social needs: Proceedings of a workshop. Washington, DC: The National Academies Press; 2019b. [ PubMed : 31693330 ]
- National Center for Medical-Legal Partnership. Helping families keep their heat and lights on. 2017. [November 2, 2020]. https: //medical-legalpartnership .org/utility-story .
- National Commission on Community Health Services. Health is a community affair: Report of the National Commission on Community Health Services. Cambridge, MA: Harvard University Press; 1967.
- NCQA (National Committee for Quality Assurance). Patient-centered medical home (PCMH). 2020. [June 2, 2020]. https://www .ncqa.org /programs/health-care-providers-practices /patient-centered-medical-home-pcmh .
- Nimmon L, Stenfors-Hayes T. The “handling” of power in the physician-patient encounter: Perceptions from experienced physicians. BMC Medical Education. 2016; 16 [ PMC free article : PMC4835893 ] [ PubMed : 27091146 ]
- Nocon RS, Lee SM, Sharma R, Ngo-Metzger Q, Mukamel DB, Gao Y, White LM, Shi L, Chin MH, Laiteerapong N, Huang ES. Health care use and spending for Medicaid enrollees in federally qualified health centers versus other primary care settings. American Journal of Public Health. 2016; 106 (11):1981–1989. [ PMC free article : PMC5055764 ] [ PubMed : 27631748 ]
- Nutting PA, Barrick JE, Logue SC. The impact of a maternal and child health care program on the quality of prenatal care: An analysis by risk group. Journal of Community Health. 1979; 4 (4):267–279. [ PubMed : 469037 ]
- O'Brien MJ, Halbert CH, Bixby R, Pimentel S, Shea JA. Community health worker intervention to decrease cervical cancer disparities in Hispanic women. Journal of General Internal Medicine. 2010; 25 (11):1186–1192. [ PMC free article : PMC2947642 ] [ PubMed : 20607434 ]
- Ockene JK, Edgerton EA, Teutsch SM, Marion LN, Miller T, Genevro JL, Loveland-Cherry CJ, Fielding JE, Briss PA. Integrating evidence-based clinical and community strategies to improve health. American Journal of Preventive Medicine. 2007; 32 (3):244–252. [ PubMed : 17296474 ]
- ODPHP (Office of Disease Prevention and Health Promotion). Access to primary care. 2020. [November 2, 2020]. https://www .healthypeople .gov/2020/topics-objectives /topic/social-determinants-health /interventions-resources /access-to-primary .
- Okun S, Schoenbaum S, Andrews D, Chidambaran P, Chollette V, Gruman J, Leal S, Bown BA, Mitchel PH, Parry C, Prins W, Ricciardi R, Simon MA, Stock R, Strasser DC, Webb CE, Wynia MK, Henderson D. Patients and health care teams forging effective partnerships. NAM Perspectives. National Academy of Medicine; 2014. Discussion Paper.
- Ong MK, Jones L, Aoki W, Belin TR, Bromley E, Chung B, Dixon E, Johnson MD, Jones F, Koegel P, Khodyakov D, Landry CM, Lizaola E, Mtume N, Ngo VK, Perlman J, Pulido E, Sauer V, Sherbourne CD, Tang L, Vidaurri E, Whittington Y, Williams P, Lucas-Wright A, Zhang L, Southard M, Miranda J, Wells K. A community-partnered, participatory, cluster-randomized study of depression care quality improvement: Three-year outcomes. Psychiatric Services. 2017; 68 (12):1262–1270. [ PMC free article : PMC5711579 ] [ PubMed : 28712349 ]
- Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers' satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients' health. PLOS ONE. 2019; 14 (8):e0221848. [ PMC free article : PMC6716655 ] [ PubMed : 31469865 ]
- Osborn HA, Glicksman JT, Brandt MG, Doyle PC, Fung K. Primary care specialty career choice among Canadian medical students: Understanding the factors that influence their decisions. Canadian Family Physician. 2017; 63 (2):e107–e113. [ PMC free article : PMC5395408 ] [ PubMed : 28209702 ]
- Park M, Giap TT, Lee M, Jeong H, Jeong M, Go Y. Patient- and family-centered care interventions for improving the quality of health care: A review of systematic reviews. International Journal of Nursing Studies. 2018; 87 :69–83. [ PubMed : 30056169 ]
- Peikes D, Zutshi A, Genevro J, Smith K, Parchman M, Meyers D. Early evidence on the patient-centered medical home. Rockville, MD: Agency for Healthcare Quality and Research; 2015.
- Pettoello-Mantovani M, Campanozzi A, Maiuri L, Giardino I. Family-oriented and family-centered care in pediatrics. Italian Journal of Pediatrics. 2009; 35 (1):12. [ PMC free article : PMC2691736 ] [ PubMed : 19490603 ]
- PHCPI (Primary Health Care Performance Initiative). Population health management: Empanelment. Primary Health Care Performance Initiative; 2019.
- Philip S, Govier D, Pantely S. Patient-centered medical home: Developing the business case from a practice perspective. Seattle, WA: Milliman, National Committee for Quality Assurance; 2019.
- Phillips RL, Cohen DJ, Kaufman A, Dickinson WP, Cykert S. Facilitating practice transformation in frontline health care. Annals of Family Medicine. 2019; 17 (Suppl 1):S2–S5. [ PMC free article : PMC6827672 ] [ PubMed : 31405869 ]
- Politzer RM, Yoon J, Shi L, Hughes RG, Regan J, Gaston MH. Inequality in America: The contribution of health centers in reducing and eliminating disparities in access to care. Medical Care Research and Review. 2001; 58 (2):234–248. [ PubMed : 11398647 ]
- Pollack SM. NEJM Catalyst. 2019. Pay for relationship: A novel solution to the primary care crisis.
- Pomeroy JL. Health center development in Los Angeles County. JAMA. 1929; 93 (20):1546–1550.
- Possemato K, Wray LO, Johnson E, Webster B, Beehler GP. Facilitators and barriers to seeking mental health care among primary care veterans with posttraumatic stress disorder. Journal of Traumatic Stress. 2018; 31 (5):742–752. [ PubMed : 30338576 ]
- Puffer JC, Borkan J, DeVoe JE, Davis A, Phillips RL Jr., Green LA, Saultz JW. Envisioning a new health care system for America. Family Medicine. 2015; 47 (8):598–603. [ PubMed : 26382117 ]
- Reid RJ, Coleman K, Johnson EA, Fishman PA, Hsu C, Soman MP, Trescott CE, Erikson M, Larson EB. The group health medical home at year two: Cost savings, higher patient satisfaction, and less burnout for providers. Health Affairs (Project Hope). 2010; 29 (5):835–843. [ PubMed : 20439869 ]
- Rhodes P, Sanders C, Campbell S. Relationship continuity: When and why do primary care patients think it is safer? British Journal of General Practice. 2014; 64 (629):e758–e764. [ PMC free article : PMC4240148 ] [ PubMed : 25452540 ]
- Rimmer A. Can patients use family members as non-professional interpreters in consultations? BMJ. 2020; 368 :m447. [ PubMed : 32047051 ]
- Rock RM, Liaw WR, Krist AH, Tong S, Grolling D, Rankin J, Bazemore AW. Clinicians' overestimation of their geographic service area. Annals of Family Medicine. 2019; 17 (Suppl 1):S63–S66. [ PMC free article : PMC6827668 ] [ PubMed : 31405878 ]
- Rosen G. What is social medicine? A genetic analysis of the concept. Bulletin of the History of Medicine. 1947; 21 (5):674–733. [ PubMed : 18901361 ]
- Rosen G. The idea of social medicine in America. Canadian Medical Association Journal. 1949; 61 (3):316–323. [ PMC free article : PMC1591620 ] [ PubMed : 18139488 ]
- Rosen G. Public health: Then and now. The first neighborhood health center movement—its rise and fall. American Journal of Public Health. 1971; 61 (8):1620–1637. [ PMC free article : PMC1530197 ] [ PubMed : 4935169 ]
- Rosenberg CE. Social class and medical care in nineteenth-century America: The rise and fall of the dispensary. Journal of the History of Medicine and Allied Science. 1974; 29 (1):32–54. [ PubMed : 4589725 ]
- Rosland AM, Piette JD, Choi H, Heisler M. Family and friend participation in primary care visits of patients with diabetes or heart failure: Patient and physician determinants and experiences. Medical Care. 2011; 49 (1):37–45. [ PMC free article : PMC3712763 ] [ PubMed : 21102357 ]
- Rural Health Information Hub. Federally qualified health centers (FQHCs) and the health center program. 2019. [November 2, 2020]. https://www .ruralhealthinfo .org/topics/federally-qualified-health-centers .
- Rust GS, Murray V, Octaviani H, Schmidt ED, Howard JP, Anderson-Grant V, Willard-Jelks K. Asthma care in community health centers: A study by the Southeast Regional Clinicians' Network. JAMA. 1999; 91 (7):398–403. [ PMC free article : PMC2608475 ] [ PubMed : 10643212 ]
- Rust G, Daniels E, Satcher D, Bacon J, Strothers H, Bornemann T. Ability of community health centers to obtain mental health services for uninsured patients. JAMA. 2005; 293 (5):554–556. [February 2, 2020]; https://jamanetwork .com /journals/jama/fullarticle/200284 . [ PubMed : 15687308 ]
- Saha S, Beach MC. Impact of physician race on patient decision making and ratings of physicians: A randomized experiment using video vignettes. Journal of General Internal Medicine. 2020; 35 (4):1084–1091. [ PMC free article : PMC7174451 ] [ PubMed : 31965527 ]
- Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Archives of Internal Medicine. 1999; 159 (9):997–1004. [ PubMed : 10326942 ]
- Saha S, Taggart SH, Komaromy M, Bindman AB. Do patients choose physicians of their own race? Health Affairs. 2000; 19 (4):76–83. [ PubMed : 10916962 ]
- Sarinopoulos I, Bechel-Marriott DL, Malouin JM, Zhai S, Forney JC, Tanner CL. Patient experience with the patient-centered medical home in Michigan's statewide multi-payer demonstration: A cross-sectional study. Journal of General Internal Medicine. 2017; 32 (11):1202–1209. [ PMC free article : PMC5653555 ] [ PubMed : 28808852 ]
- Sayers SL, White T, Zubritsky C, Oslin DW. Family involvement in the care of healthy medical outpatients. Family Practice. 2006; 23 (3):317–324. [ PubMed : 16461451 ]
- Schilling LM, Scatena L, Steiner JF, Albertson GA, Lin CT, Cyran L, Ware L, Anderson RJ. The third person in the room: Frequency, role, and influence of companions during primary care medical encounters. Journal of Family Practice. 2002; 51 (8):685–690. [ PubMed : 12184964 ]
- Schmacke N. Health promotion through neighborhood health centers: A tribute to George Rosen on the 20th anniversary of his death. Health Promotion International. 1998; 13 (2):151–154.
- Schwenk TL. The patient-centered medical home: One size does not fit all. JAMA. 2014; 311 (8):802–803. [ PubMed : 24570242 ]
- Scott JG, Cohen D, Dicicco-Bloom B, Miller WL, Stange KC, Crabtree BF. Understanding healing relationships in primary care. Annals of Family Medicine. 2008; 6 (4):315–322. [ PMC free article : PMC2478496 ] [ PubMed : 18626031 ]
- Seervai S. How community health workers put patients in charge of their health. 2020. [June 12, 2020]. https://www .commonwealthfund .org/publications /podcast/2020/may /how-community-health-workers-put-patients-charge-their-health .
- Shen MJ, Peterson EB, Costas-Muñiz R, Hernandez MH, Jewell ST, Matsoukas K, Bylund CL. The effects of race and racial concordance on patient-physician communication: A systematic review of the literature. Journal of Racial and Ethnic Health Disparities. 2018; 5 (1):117–140. [ PMC free article : PMC5591056 ] [ PubMed : 28275996 ]
- Shorr GI, Nutting PA. A population-based assessment of the continuity of ambulatory care. Medical Care. 1977; 15 (6):455–464. [ PubMed : 875491 ]
- Shukor AR, Edelman S, Brown D, Rivard C. Developing community-based primary health care for complex and vulnerable populations in the Vancouver coastal health region: Healthconnection clinic. The Permanente Journal. 2018; 22 :18–010. [ PMC free article : PMC6141648 ] [ PubMed : 30227907 ]
- Singer M. The coming of age of critical medical anthropology. Social Science & Medicine. 1989; 28 (11):1193–1203. [ PubMed : 2660276 ]
- Stewart EE, Taylor-Post N, Nichols L, Staton EW, Schleunin A. SNOCAP-USA (State Networks of Colorado Ambulatory Practices and Partners). Community connections: Linking primary care patients to local resources for better management of obesity. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [November 24, 2020]. https://www .ahrq.gov /ncepcr/tools/obesity-kit/index.html .
- Starfield B. Primary care and equity in health: The importance to effectiveness and equity of responsiveness to peoples' needs. Humanity & Society. 2009; 33 (1–2):56–73.
- Starfield B. Is patient-centered care the same as person-focused care? The Permanente Journal. 2011; 15 :63–69. [ PMC free article : PMC3140752 ] [ PubMed : 21841928 ]
- Starfield B. Primary care: An increasingly important contributor to effectiveness, equity, and efficiency of health services. SESPAS report 2012. Gaceta Sanitaria. 2012; 26 (Suppl 1):20–26. [ PubMed : 22265645 ]
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Quarterly. 2005; 83 (3):457–502. [ PMC free article : PMC2690145 ] [ PubMed : 16202000 ]
- Stephens GG. Remembering 40 years, plus or minus. Journal of the American Board of Family Practice. 2010; 23 (Suppl 1):S5–S10. [ PubMed : 20207919 ]
- Sullivan EE, Ellner A. Harvard Business Review. 2015. [January 12, 2021]. Strong patient-provider relationships drive healthier outcomes. https://hbr .org/2015 /10/strong-patient-provider-relationships-drive-healthier-outcomes .
- Susser M, Stein Z, Cormack M, Hathorn M. Medical care in a South African township. The Lancet. 1955; 268 (6870):912–915. [ PubMed : 14368909 ]
- Taylor J. The fundamentals of communith health centers. Washington, DC: The George Washington University; 2004.
- Teno JM, Gozalo PL, Trivedi AN, Mitchell SL, Bunker JN, Mor V. Temporal trends in the numbers of skilled nursing facility specialists from 2007 through 2014. JAMA Internal Medicine. 2017; 177 (9):1376–1378. [ PMC free article : PMC5629965 ] [ PubMed : 28692731 ]
- The Folsom Group. Communities of solution: The Folsom Report revisited. Annals of Family Medicine. 2012; 10 (3):250–260. [ PMC free article : PMC3354975 ] [ PubMed : 22585890 ]
- The Larry A. Green Center and PCC (Primary Care Collaborative). Quick COVID-19 primary care survey: Patient series 1 fielded May 4–11, 2020. 2020. [January 21, 2021]. https://www .green-center .org/covid-survey .
- Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition—multimorbidity. JAMA. 2012; 307 (23):2493–2494. [ PMC free article : PMC4083627 ] [ PubMed : 22797447 ]
- Ton AN, Jethwa T, Waters K, Speicher LL, Francis D. COVID-19 drive through testing: An effective strategy for conserving personal protective equipment. American Journal of Infection Control. 2020; 48 (6):731–732. [ PMC free article : PMC7162738 ] [ PubMed : 32305432 ]
- UCLA (University of California, Los Angeles) American Indian Studies Center. Access to care among American Indians and Alaska Natives in Los Angeles. 2016. [December 14, 2020]. https://www .aisc.ucla .edu/research/pb4.aspx .
- Unwin BK, Porvaznik M, Spoelhof GD. Nursing home care: Part I. Principles and pitfalls of practice. American Family Physician. 2010; 81 (10):1219–1227. [ PubMed : 20507046 ]
- Urban Indian Health Commission. Invisible tribes: Urban Indians and their health in a changing world. Seattle, WA: Urban Indian Health Commission; 2007.
- VA (U.S. Department of Veterans Affairs). What is home based primary care? 2020. [February 26, 2021]. https://www .va.gov/GERIATRICS /pages/Home_Based_Primary_Care .asp .
- van den Berk-Clark C, Doucette E, Rottnek F, Manard W, Prada MA, Hughes R, Lawrence T, Schneider FD. Do patient-centered medical homes improve health behaviors, outcomes, and experiences of low-income patients? A systematic review and meta-analysis. Health Services Research. 2018; 53 (3):1777–1798. [ PMC free article : PMC5980195 ] [ PubMed : 28670708 ]
- van Weel C. Person-centred medicine in the context of primary care: A view from the world organization of family doctors (WONCA). Journal of Evaluation in Clinical Practice. 2011; 17 (2):337–338. [ PubMed : 21269379 ]
- Wagner EH, Coleman K, Reid RJ, Phillips K, Abrams MK, Sugarman JR. The changes involved in patient-centered medical home transformation. Primary Care: Clinics in Office Practice. 2012; 39 (2):241–259. [ PubMed : 22608865 ]
- Wald LD. The house on Henry Street. New York: Henry Holt & Co; 1911.
- Wang EA, Hong CS, Shavit S, Sanders R, Kessell E, Kushel MB. Engaging individuals recently released from prison into primary care: A randomized trial. American Journal of Public Health. 2012; 102 (9):e22–e29. [ PMC free article : PMC3482056 ] [ PubMed : 22813476 ]
- Warne D, Frizzell LB. American Indian health policy: Historical trends and contemporary issues. American Journal of Public Health. 2014; 104 (Suppl 3):S263–S267. [ PMC free article : PMC4035886 ] [ PubMed : 24754649 ]
- Wells KB, Watkins KE, Hurley B, Tang L, Jones F, Gilmore J. Commentary: Applying the community partners in care approach to the opioid crisis. Ethnicity & Disease. 2018; 28 (Suppl 2):381–388. [ PMC free article : PMC6128328 ] [ PubMed : 30202191 ]
- Westfall JM. Cold-spotting: Linking primary care and public health to create communities of solution. Journal of the American Board of Family Medicine. 2013; 26 (3):239–240. [ PubMed : 23657689 ]
- Westfall JM, Roper R, Gaglioti A, Nease DE Jr. Practice-based research networks: Strategic opportunities to advance implementation research for health equity. Ethnicity & Disease. 2019; 29 (Suppl 1):113–118. [ PMC free article : PMC6428170 ] [ PubMed : 30906158 ]
- Whitehead L, Jacob E, Towell A, Abu-Qamar M, Cole-Heath A. The role of the family in supporting the self-management of chronic conditions: A qualitative systematic review. Journal of Clinical Nursing. 2018; 27 (1–2):22–30. [ PubMed : 28231630 ]
- WHO (World Health Organization). Framework on integrated, people-centered health services. Geneva, Switzerland: World Health Organization; 2016.
- WHO. Social determinants of health. 2020a. [November 2, 2020]. https://www .who.int/health-topics /social-determinants-of-health .
- WHO. World Health Organization health systems strengthening glossary. Geneva, Switzerland: World Health Organization; 2020b.
- WHO and Ministry of Healthcare Republic of Kazakhstan. Global Conference on Primary Health Care. 25–26 October 2018—Astana, Kazakhstan. 2018. [March 24, 2019]. https://www .who.int/news-room /events/detail /2018/10/25/default-calendar /global-conference-on-primary-health-care .
- WHO and UNICEF (United Nations Children's Fund). Declaration of Astana. Astana, Kazakhstan: World Health Organization and United Nations Children's Fund; 2018.
- Wiggins N, Kaan S, Rios-Campos T, Gaonkar R, Morgan E, Robinson J. Preparing community health workers for their role as agents of social change: Experience of the community capacitation center. Journal of Community Practice. 2013; 21 :186–202.
- Wilinsky C. Health units of Boston, 1924–1933. Boston, MA: City of Boston Printing Department; 1933.
- Williams DR, Lawrence JA, Davis BA. Racism and health: Evidence and needed research. Annual Review of Public Health. 2019a; 40 :105–125. [ PMC free article : PMC6532402 ] [ PubMed : 30601726 ]
- Williams DR, Lawrence JA, Davis BA, Vu C. Understanding how discrimination can affect health. Health Services Research. 2019b; 54 (Suppl 2):1374–1388. [ PMC free article : PMC6864381 ] [ PubMed : 31663121 ]
- Winslow C-EA. The health center movement. Modern Medicine. 1919; 1 (4)
- Winslow C-EA. The life of Hermann M. Biggs: M.D., D. Sc., LL. D., physician and statesman of the public health. Philadelphia, PA: Lea & Febiger; 1929.
- Wolff JL, Boyd CM. A look at person- and family-centered care among older adults: Results from a national survey [corrected] Journal of General Internal Medicine. 2015; 30 (10):1497–1504. [ PMC free article : PMC4579212 ] [ PubMed : 25933625 ]
- Wolff JL, Roter DL. Family presence in routine medical visits: A meta-analytical review. Social Science & Medicine. 2011; 72 (6):823–831. [ PMC free article : PMC3070824 ] [ PubMed : 21353358 ]
- Wright B. Who governs federally qualified health centers? Journal of Health Politics, Policy and Law. 2013; 38 (1):27–55. [ PMC free article : PMC5602556 ] [ PubMed : 23052684 ]
- Wright B. Do patients have a voice? The social stratification of health center governing boards. Health Expectations. 2015; 18 (3):430–437. [ PMC free article : PMC5060786 ] [ PubMed : 23432950 ]
- Xierali IM, Nivet MA. The racial and ethnic composition and distribution of primary care physicians. Journal of Health Care for the Poor and Underserved. 2018; 29 (1):556–570. [ PMC free article : PMC5871929 ] [ PubMed : 29503317 ]
- Yoon J, Chang E, Rubenstein LV, Park A, Zulman DM, Stockdale S, Ong MK, Atkins D, Schectman G, Asch SM. Impact of primary care intensive management on high-risk veterans' costs and utilization: A randomized quality improvement trial. Annals of Internal Medicine. 2018; 168 (12):846–854. [ PubMed : 29868706 ]
- Youngclaus J, Roskovensky L. An updated look at the economic diversity of U.S. Medical students. AAMC in Brief. 2018; 18 (5)
- Yue D, Pourat N, Chen X, Lu C, Zhou W, Daniel M, Hoang H, Sripipatana A, Ponce NA. Enabling services improve access to care, preventive services, and satisfaction among health center patients. Health Affairs. 2019; 38 (9):1468–1474. [ PubMed : 31479374 ]
- Zhang X, Hailu B, Tabor DC, Gold R, Sayre MH, Sim I, Jean-Francois B, Casnoff CA, Cullen T, Thomas VA Jr., Artiles L, Williams K, Le PT, Aklin CF, James R. Role of health information technology in addressing health disparities: Patient, clinician, and system perspectives. Medical Care. 2019; 57 [ PMC free article : PMC6589829 ] [ PubMed : 31095049 ]
- Zwick DI. Some accomplishments and findings of neighborhood health centers. The Milbank Memorial Fund Quarterly. 1972; 50 (4):387–420. [ PubMed : 4565573 ]
The webinar agenda, speaker bios, and archived presentations can be found at https://www .nationalacademies .org/event/06-02-2020 /patient-perspectives-on-primary-care-a-webinar (accessed February 14, 2021).
WHO uses “people-centered care” instead of “person-centered care,” but both terms represent the same concept.
Patient Protection and Affordable Care Act, Public Law 111-148 (March 23, 2010).
These data come from the third wave of the Green Center's COVID-19 survey, but were not published in the executive summary. The national aggregate data are available upon request from the project public access file. To request, follow the link on the project webpage ( www .nationalacademies.org/primarycare [accessed February 14, 2021]) for contacting the Public Access Records Office.
Nuka is an Alaska Native word used for strong, giant structures and living things.
The Indian Self-Determination and Education Assistance Act, Public Law 93-638 (January 4, 1975).
The Declaration of Alma-Ata was adopted at the International Conference on Primary Health Care in what was then known as Alma-Ata in the Soviet Socialist Republic (today, it is known as Almaty, Kazakhstan). The conference and declaration called for national and international action to strengthen primary health care throughout the world ( International Conference on Primary Health Care, 1978 ). The Declaration is available at https://www .who.int/publications /almaata_declaration_en.pdf (accessed October 5, 2020).
In 42 CFR § 440.169 (2009), the Centers for Medicare & Medicaid Services (CMS) defines case management services as “services furnished to assist individuals … in gaining access to needed medical, social, educational, and other services” (which does not include “the direct delivery of underlying medical, educational, social, or other services”).
Patient Protection and Affordable Care Act, Public Law 111-148, § 5208 (March 23, 2010).
- Cite this Page National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Implementing High-Quality Primary Care; Robinson SK, Meisnere M, Phillips RL Jr., et al., editors. Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care. Washington (DC): National Academies Press (US); 2021 May 4. 4, Person-Centered, Family-Centered, and Community-Oriented Primary Care.
- PDF version of this title (4.1M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Person-Centered, Family-Centered, and Community-Oriented Primary Care - Implemen... Person-Centered, Family-Centered, and Community-Oriented Primary Care - Implementing High-Quality Primary Care
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Primary health care (PHC) refers to the essential healthcare services that are universally accessible and provided as the first point of contact with the healthcare system. It encompasses a wide range of health promotion, disease prevention, diagnosis, treatment, and rehabilitation services.
This document discusses primary health care (PHC), including its definition, principles, and the role of nurses. It provides the following key points: 1. PHC is defined as universally accessible and affordable health care that involves community participation.
What distinguishes primary health care from primary care? (a) A focus on primary, secondary and tertiary intervention (b) Provision of interventions specific to the health need (c) Works within a multidisciplinary framework (d) Planning and operation of services is centralised
Primary health care consists of an integrative group of health care professionals coordinating to provide basic health care services to a particular group of people or population. The Primary Health care outline is built on four key pillars.
This course explores why primary health care is central for achieving Health for All. It provides examples of how primary health care has been instrumental in approaching this goal in selected populations and how the principles of primary health care can guide future policies and actions.
Explore the principles and implementation of primary health care for achieving global Health for All, featuring real-world examples and innovative community-based approaches.
This Primer is about the 'how' of primary health care (PHC) and brings together best practices and knowledge that countries have generated through 'natural experiments' in strengthening PHC with the best available research evidence.
HEALTH EQUITY AND THE ROLE OF PRIMARY CARE. Health equity is a guiding principle for many primary care teams. Primary care improves equity (Starfield, 2009, 2012; Starfield et al., 2005), and an ultimate goal for improving primary care is to reduce inequities as much as possible.
Primary health care is widely regarded as the most inclusive, equitable and cost-effective way to achieve universal health coverage. It is also key to strengthening the resilience of health systems to prepare for, respond to and recover from shocks and crises.
The primary healthcare model promotes empowerment and involvement of the client in their own care to take care of themselves with regard to their disease, illness, or injury. The primary care model is government funded in order to provide its services to consumers. It also aims to diminish the burden of minor incidents such as a small wound of ...