- Department of Health and Human Services
- National Institutes of Health


COVID-19 Research Studies
More information, about clinical center, clinical trials and you, participate in a study, referring a patient, about clinical research.
Research participants are partners in discovery at the NIH Clinical Center, the largest research hospital in America. Clinical research is medical research involving people The Clinical Center provides hope through pioneering clinical research to improve human health. We rapidly translate scientific observations and laboratory discoveries into new ways to diagnose, treat and prevent disease. More than 500,000 people from around the world have participated in clinical research since the hospital opened in 1953. We do not charge patients for participation and treatment in clinical studies at NIH. In certain emergency circumstances, you may qualify for help with travel and other expenses Read more , to see if clinical studies are for you.
Medical Information Disclaimer
Emailed inquires/requests.
Email sent to the National Institutes of Health Clinical Center may be forwarded to appropriate NIH or outside experts for response. We do not collect your name and e-mail address for any purpose other than to respond to your query. Nevertheless, email is not necessarily secure against interception. This statement applies to NIH Clinical Center Studies website. For additional inquiries regarding studies at the National Institutes of Health, please call the Office of Patient Recruitment at 1-800-411-1222

Find NIH Clinical Center Trials
The National Institutes of Health (NIH) Clinical Center Search the Studies site is a registry of publicly supported clinical studies conducted mostly in Bethesda, MD.

Browse by collection
- Anaesthesia
- Clinical pharmacology
- Critical care
- Dentistry and oral medicine
- Dermatology
- Ear, nose and throat
- Emergency medicine
- Endocrinology
- Gastroenterology
- General practice and family medicine
- Geriatric medicine
- Global health
- Haematology
- Images in...
- Infectious diseases
- Nutrition and metabolism
- Obstetrics and gynaecology
- Open access
- Ophthalmology
- Orthopaedics
- Paediatrics
- Palliative care
- Rehabilitation medicine
- Renal medicine
- Respiratory medicine
- Rheumatology
- Sexual health
- Sports and exercise medicine
- Search Menu
- Sign in through your institution
- Volume 2024, Issue 10, October 2024
- Volume 2024, Issue 9, September 2024 (In Progress)
- Case of the Year
- MSF Case Reports
- Audiovestibular medicine
- Cardiology and cardiovascular systems
- Critical care medicine
- Dermatology
- Emergency medicine
- Endocrinology and metabolism
- Gastroenterology and hepatology
- Geriatrics and gerontology
- Haematology
- Infectious diseases and tropical medicine
- Medical ophthalmology
- Medical disorders in pregnancy
- Paediatrics
- Palliative medicine
- Pharmacology and pharmacy
- Radiology, nuclear medicine, and medical imaging
- Respiratory disorders
- Rheumatology
- Sexual and reproductive health
- Sports medicine
- Substance abuse
- Author Guidelines
- Submission Site
- Open Access
- Reasons to publish with us
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Editor-in-Chief
Richard Watts
Executive Editors
Tamim Alsuliman
Aloysious Aravinthan
Amanda Goodwin
Abraham Gracia-Ramos
Nitin Gupta
Eleana Ntatsaki
Vassilis Vassiliou
Publish with Oxford Medical Case Reports
Oxford Medical Case Reports is an open access, peer-reviewed journal publishing original and educationally valuable case reports that expand the field of medicine. To understand more about why OMCR is a great fit for your research, head to our 'Why Publish With Us?' page here .

Browse by specialty
Oxford Medical Case Reports publish insightful cases across all medical specialties.
Browse collections including nephrology , palliative care , and geriatric medicine .
Explore more

- Submit your case
Oxford Medical Case Reports publishes original and educationally valuable case reports across all medical specialties.
- Author guidelines
Case Reports From Humanitarian And Resource Limited Settings

Médecins Sans Frontières (MSF) is working with OMCR to encourage clinicians in low-income and/or emergency contexts to submit interesting case reports and series from the field.
Browse the case reports from humanitarian and low resource settings

Enhanced discoverability
Oxford Medical Case Reports deposits all cases in PubMed Central . Physicians and researchers can find your work through PubMed , helping you reach the widest possible audience.
The journal is also indexed in the Web of Science Core Collection .
Latest articles

OMCR : Case Report of the Year
Get a taste of recent and enlightening reports from OMCR by reading our Case Report of the Year, selected by Editor-in-Chief Richard Watts, and some of our most popular cases from 2023.
Join us on Facebook and Twitter
Be the first to read the latest news and cases by joining the Oxford Medical Case Reports community on Facebook , or by following us on Twitter .
Publish with OMCR
Editor-in-Chief Dr Richard Watts explains the benefits of publishing with Oxford Medical Case Reports.

Test your knowledge
A 57 year-old man has chest pain, but what is the diagnosis? Answer multiple choice questions to find out.
Take the test
Related Titles
- X (formerly Twitter)
Affiliations
- Online ISSN 2053-8855
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Clinical Cases
Litfl clinical cases database.
The LITFL Clinical Case Collection includes over 250 Q&A style clinical cases to assist ‘ Just-in-Time Learning ‘ and ‘ Life-Long Learning ‘. Cases are categorized by specialty and can be interrogated by keyword from the Clinical Case searchable database.
Search by keywords; disease process; condition; eponym or clinical features…
Compendium of Clinical Cases
LITFL Top 100 Self Assessment Quizzes
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Cases Database
Elizabeth (beth) ketterman , mls.
- Author information
- Copyright and License information
Cases in clinical medicine can be defined as reports on patients where symptoms, diagnosis, treatment, and outcome are described, and some new side effect, disease association, symptom, or unusual presentation is observed. Usually in case reports, the patient is also described in detail: age, weight, gender, ethnicity, or some other clinically relevant attribute. Cases Database, launched by BioMed Central (BMC) on December 10, 2012, aims to pull together similar cases from published journals to assist researchers in finding trends in this subset of the medical literature. According to the Cases Database website, the purpose of this resource is to provide clinicians, researchers, regulators, and patients a starting place to explore content and identify emerging trends in medicine. Matt Cockerill, BMC's managing director explains, “Our vision, when we launched Journal of Medical Case Reports , was that case reports would have much more value if they could be assembled together in large numbers and made easy to find and compare” [1].
Content in Cases Database is pulled from BMC's Journal of Medical Case Reports, cases published in other BMC journals, and cases from other published medical journals using a text-mining method designed and built just for the database. New content is added on an ongoing basis as new articles are published. All cases indexed in Cases Database are peer reviewed, and because the resource is open access, everyone can use it at no cost. This makes the database highly accessible. Because all the cases are pulled from previously published material, there is also no charge to publish in Cases Database; however, authors cannot submit directly to Cases Database. They must publish in either the Journal of Medical Case Reports or in a journal already indexed by Cases Database. The inclusion of papers is completely at the discretion of the editors.
One of the most noticeable features of the database is the Google-like search box on the home page. It stands out on the page because it is quite large and really invites a user to start a keyword search right away. There is an option to do an advanced search right below the main box. The advanced options include limits by patient information (sex, age, ethnicity); clinical characteristics (condition, symptom, medication, etc.); and a particular publication. Author country is, interestingly enough, the first limitation offered in that section.
The home page also has some other interesting features like a tag cloud of sorts of popular searches, the current number of reports in the database, and the number of journals indexed (as of November 22, 2013, those numbers are 30,081 and 257, respectively). That is about as complicated as a search gets in this resource. Once a search is performed, more limits can be applied. The author of this review did a keyword search for “diabetic ketoacidosis” and noticed that for the 112 cases returned, the same limits mentioned previously all appeared in a left-hand navigation pane. The clinical characteristics were also pre-scoped to those associated with diabetic ketoacidosis.
Another option is to create an account with Cases Database in order to save cases and/or searches, download results to the computer, and receive alerts when new cases match a saved search. Overall, the usability of this database is good, the interface is clean and simple to navigate, and the usual functions and limits are all present. Librarians who are interested in usage statistics do not have such luck, however. This reviewer asked the vendor if there is an administrative utility that could capture use data based on Internet protocol (IP), but no statistics are available.
The most difficult part of this review is determining whether Cases Databases is worth recommending to clinical providers as a worthwhile source for information. All the cases in the database can be found elsewhere, either by searching BioMed Central's site or searching MEDLINE and limiting to cases. In fact, pretty much any instance of MEDLINE would assuredly provide a more comprehensive amount of cases on a particular topic. With all the medical and health databases out there vying for a researcher's time, is Cases Database worth recommending and using? Yes, but only in particular situations and with some explanation.
Academic health sciences librarians may frequently be asked by students for assistance in locating particular kinds of studies, usually by assignment from their instructors. Cases Database would be a really good source for students to find case reports. Because the resource is limited to cases and everything in it is peer reviewed, this database could be very helpful in this scenario. Cases Database would also be a suitable recommendation for a clinician who is looking to compare information about a patient to other similar patients mentioned in quality case reports. The caveat is that the clinician would need to know that the database does not have the depth of coverage that a source like MEDLINE would provide. The benefit for this kind of user would be Cases Database's quick and easy-to-use interface.
Cases Database is limited by the fact that only 252 titles are currently indexed, but the developers have a standing call for other publishers to allow indexing of more journals. Until then, it would be difficult to recommend this database to other user groups, as a limit to case studies in MEDLINE sources would provide a more authoritative search. Cases Database would not be recommended, therefore, to librarians or researchers conducting intensive literature reviews.
- 1. Unlocking the value of medical case reports: BioMed Central launches Cases Database [Internet] BioMed Central; 10 Dec 2012 [cited 30 Sep 2013]. < http://www.biomedcentral.com/presscenter/pressreleases/20121210 >. [ Google Scholar ]
- View on publisher site
- PDF (49.1 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

My Case History
Save and email your answers for case & comprehensive questions. Track what cases you open and complete.
New on Case Files Collection

Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 21, Issue 1
- What is a case study?
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Roberta Heale 1 ,
- Alison Twycross 2
- 1 School of Nursing , Laurentian University , Sudbury , Ontario , Canada
- 2 School of Health and Social Care , London South Bank University , London , UK
- Correspondence to Dr Roberta Heale, School of Nursing, Laurentian University, Sudbury, ON P3E2C6, Canada; rheale{at}laurentian.ca
https://doi.org/10.1136/eb-2017-102845
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
What is it?
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research. 1 However, very simply… ‘a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units’. 1 A case study has also been described as an intensive, systematic investigation of a single individual, group, community or some other unit in which the researcher examines in-depth data relating to several variables. 2
Often there are several similar cases to consider such as educational or social service programmes that are delivered from a number of locations. Although similar, they are complex and have unique features. In these circumstances, the evaluation of several, similar cases will provide a better answer to a research question than if only one case is examined, hence the multiple-case study. Stake asserts that the cases are grouped and viewed as one entity, called the quintain . 6 ‘We study what is similar and different about the cases to understand the quintain better’. 6
The steps when using case study methodology are the same as for other types of research. 6 The first step is defining the single case or identifying a group of similar cases that can then be incorporated into a multiple-case study. A search to determine what is known about the case(s) is typically conducted. This may include a review of the literature, grey literature, media, reports and more, which serves to establish a basic understanding of the cases and informs the development of research questions. Data in case studies are often, but not exclusively, qualitative in nature. In multiple-case studies, analysis within cases and across cases is conducted. Themes arise from the analyses and assertions about the cases as a whole, or the quintain, emerge. 6
Benefits and limitations of case studies
If a researcher wants to study a specific phenomenon arising from a particular entity, then a single-case study is warranted and will allow for a in-depth understanding of the single phenomenon and, as discussed above, would involve collecting several different types of data. This is illustrated in example 1 below.
Using a multiple-case research study allows for a more in-depth understanding of the cases as a unit, through comparison of similarities and differences of the individual cases embedded within the quintain. Evidence arising from multiple-case studies is often stronger and more reliable than from single-case research. Multiple-case studies allow for more comprehensive exploration of research questions and theory development. 6
Despite the advantages of case studies, there are limitations. The sheer volume of data is difficult to organise and data analysis and integration strategies need to be carefully thought through. There is also sometimes a temptation to veer away from the research focus. 2 Reporting of findings from multiple-case research studies is also challenging at times, 1 particularly in relation to the word limits for some journal papers.
Examples of case studies
Example 1: nurses’ paediatric pain management practices.
One of the authors of this paper (AT) has used a case study approach to explore nurses’ paediatric pain management practices. This involved collecting several datasets:
Observational data to gain a picture about actual pain management practices.
Questionnaire data about nurses’ knowledge about paediatric pain management practices and how well they felt they managed pain in children.
Questionnaire data about how critical nurses perceived pain management tasks to be.
These datasets were analysed separately and then compared 7–9 and demonstrated that nurses’ level of theoretical did not impact on the quality of their pain management practices. 7 Nor did individual nurse’s perceptions of how critical a task was effect the likelihood of them carrying out this task in practice. 8 There was also a difference in self-reported and observed practices 9 ; actual (observed) practices did not confirm to best practice guidelines, whereas self-reported practices tended to.
Example 2: quality of care for complex patients at Nurse Practitioner-Led Clinics (NPLCs)
The other author of this paper (RH) has conducted a multiple-case study to determine the quality of care for patients with complex clinical presentations in NPLCs in Ontario, Canada. 10 Five NPLCs served as individual cases that, together, represented the quatrain. Three types of data were collected including:
Review of documentation related to the NPLC model (media, annual reports, research articles, grey literature and regulatory legislation).
Interviews with nurse practitioners (NPs) practising at the five NPLCs to determine their perceptions of the impact of the NPLC model on the quality of care provided to patients with multimorbidity.
Chart audits conducted at the five NPLCs to determine the extent to which evidence-based guidelines were followed for patients with diabetes and at least one other chronic condition.
The three sources of data collected from the five NPLCs were analysed and themes arose related to the quality of care for complex patients at NPLCs. The multiple-case study confirmed that nurse practitioners are the primary care providers at the NPLCs, and this positively impacts the quality of care for patients with multimorbidity. Healthcare policy, such as lack of an increase in salary for NPs for 10 years, has resulted in issues in recruitment and retention of NPs at NPLCs. This, along with insufficient resources in the communities where NPLCs are located and high patient vulnerability at NPLCs, have a negative impact on the quality of care. 10
These examples illustrate how collecting data about a single case or multiple cases helps us to better understand the phenomenon in question. Case study methodology serves to provide a framework for evaluation and analysis of complex issues. It shines a light on the holistic nature of nursing practice and offers a perspective that informs improved patient care.
- Gustafsson J
- Calanzaro M
- Sandelowski M
Competing interests None declared.
Provenance and peer review Commissioned; internally peer reviewed.
Read the full text or download the PDF:
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Insomnia and exacerbation of anxiety associated with high-EPA fish oil supplements after successful treatment of depression
Lauren b blanchard, gordon c mccarter.
- Author information
- Article notes
- Copyright and License information
Correspondence address. 1310 Club Drive, Vallejo, CA 94592, USA. Tel: +1-707-638-5919; Fax: +1-707-638-5266; E-mail: [email protected]
Received 2015 Feb 20; Accepted 2015 Feb 26; Collection date 2015 Mar.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License ( http://creativecommons.org/licenses/by-nc/4.0/ ), which permits non-commercial re-use, distribution, and reproduction in any medium, provided the original work is properly cited. For commercial re-use, please contact [email protected]
A 54-year-old male consulted his general practitioner for increasing general anxiety and mild panic attacks despite effective treatment for recurrent major depressive disorder, which included a fish oil supplement enriched in eicosapentaenoic acid (EPA). The patient would awaken suddenly at night with shortness of breath and overwhelming worry. During the daytime, he felt a general, nonspecific anxiety and frequently experienced sympathetic activation upon confronting routine challenges. He also experienced dyspnea-induced feelings of panic. He reported that he stopped taking the fish oil supplements after several more months of symptoms, and his anxiety and insomnia then largely disappeared. Several weeks later, he resumed consumption of high-EPA fish oil at the prior dosage for 2 days. On both nights, the patient reported nighttime awakening similar to the previous episodes, followed by daytime agitation. Since halting the fish oil supplements, the anxiety and insomnia have not returned and his depression remains in remission.
INTRODUCTION
Long-chain omega-3 polyunsaturated fatty acids (ω-3 PUFAs) are the key ingredient in fish oil nutritional supplements and evidence exists for their benefit to both cardiovascular and psychiatric health [ 1 , 2 ]. Eicosapentaenoic acid (EPA), in particular, has been implicated in improving mood disorders [ 3 ] and EPA-enriched fish oil preparations are available. Sales in fish oil supplements are in the billions of dollars (US) annually and clinicians are increasingly likely to encounter patients who are regularly taking these supplements. Adverse events related to fish oil supplements are rarely reported and are described as mild to moderate [ 2 , 4 ].
CASE REPORT
The patient is a 55-year-old male employed as a professor in the USA. At Age 42, he consulted his general practitioner for major depressive disorder and was prescribed fluoxetine, eventually titrated to 40 mg. Pharmacotherapy combined with psychotherapy generally relieved the worst episodes of depressive disorder, but occasional relapses occurred for the next 10 years or more. On at least three occasions, the patient discontinued the fluoxetine when the depression was in remission, but symptoms returned within a few months each time and he resumed taking the medication. When he was 46, his general practitioner suggested adding fish oil supplements to his regimen, particularly those that are enriched in EPA, at a dose of 2–3 g/day total lipids. He began taking with morning meals two 1-g softgels per day of fish oil that contained 6 : 1 EPA : DHA (docosahexaenoic acid, 500 mg EPA per softgel). The patient reported that the supplements seemed to noticeably relieve his depressive symptoms. He continued taking the same brand of high-EPA fish oil daily for 8 years (Metagenics ‘EPA 500 Concentrate’, formerly named ‘EPA : DHA 6 : 1’) and while the depressive episodes did not completely abate for several more years, they became shorter in duration and more manageable. At Age 54, he had not experienced a significant relapse for over a year so he once again tapered off the fluoxetine. Of note, until this time he had not reported any significant anxiety symptoms. The patient exercises regularly and is in excellent health. Other significant history includes asthma that is well controlled and a cerebral aneurysm successfully treated with endovascular coiling at Age 52. He uses an albuterol inhaler for rare exacerbations of asthma, usually during upper respiratory tract infections, and takes a daily multivitamin. He is medically literate and was cared for by two successive clinicians (including L.B.B.) in the same medical office for more than 20 years.
Six months after stopping the fluoxetine, the patient reported that he had recently begun experiencing gradually worsening insomnia and general anxiety. He often awakened after 2 or 3 h of sound sleep, sometimes with shortness of breath, and was then unable to stop ruminating about possible catastrophic scenarios. On some occasions, he felt so uncomfortable that he was forced to arise to take up reading for an hour or more until he could resume sleep. During the day, he sometimes felt overwhelmed and would experience a flush of alarm, during which his heart rate increased and he began to perspire. On several occasions, exercise-induced dyspnea triggered strong feelings of panic, most acutely when bicycling at high elevations.
The patient mentioned that he had recently run out of his fish oil supplements and seemed to feel better for the few days before he was able to purchase a new bottle. However, he felt that his remission from depression was due in part to these supplements so he continued to take them daily at the same dose. He was prescribed lorazepam for his anxiety. After 6 more months of the anxiety symptoms and insomnia, he stopped taking the fish oil supplements altogether. Within days he felt noticeable relief. He was much more at ease during the day and he could sleep through the night without significant awakenings. He stated that after he had been largely anxiety-free for several weeks, he experimented by resuming the supplements at the same dose as previously for two mornings. On both subsequent nights, and for one additional night, around 2 a.m. he suddenly became fully awake and could not resume sleep for at least an hour. While he did not experience feelings of doom on these awakenings, his thoughts were racing and he was again forced to arise and read for an hour or more. On the following days, he felt agitated and uneasy, which he said was typical when he did not get enough sleep. Two days after the trial ended, he was sleeping well again. At the time of this writing, the patient reports that he remains largely free of anxiety and insomnia. He also reports that he has not experienced significant depressive symptoms either.
There is mounting but somewhat conflicting evidence that fish consumption and a diet rich in long-chain omega-3 fatty acids may decrease the risk of depression and anxiety [ 2 , 3 , 5 – 8 ]. Interestingly, a large prospective cohort study found a U-shaped relationship between ω-3 PUFA consumption and mental disorders, with only the intermediate, but not the lowest and highest, levels of ω-3 PUFA intake reducing the risk of depression and anxiety [ 5 ]. In another study, a high-EPA regimen reduced depressive symptoms only in patients without comorbid anxiety [ 8 ]. The consumption of fish oil supplements (up to 2 g total EPA + DHA per day) has been recognized as safe and potentially beneficial by the American Heart Association and few adverse events have heretofore been associated with their consumption [ 9 ]. However, individual responses to any substance can vary from person to person. We provide here the first report known to us where omega-3 fatty acids are associated with an increase in insomnia and anxiety symptoms. Questions that arise from this case include why the apparent earlier benefits of the fish oil changed to deleterious effects after resolution of the depression and whether the latter effects were specific to high-EPA fish oil. Perhaps the patient's increasing age played a role in the change. Consumers and clinicians should be aware of potential idiosyncratic adverse events to any substance as widely consumed as ω-3 PUFAs.
CONFLICT OF INTEREST STATEMENT
None declared.
- 1. Delgado-Lista J, Perez-Martinez P, Lopez-Miranda J, Perez-Jimenez F. Long chain omega-3 fatty acids and cardiovascular disease: a systematic review. Br J Nutr 2012;107(Suppl 2):S201–13. [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. Mischoulon D, Freeman MP. Omega-3 fatty acids in psychiatry. Psychiatr Clin North Am 2013;36:15–23. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Sublette ME, Ellis SP, Geant ML, Mann JJ. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry 2011;72:1577–84. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Villani AM, Crotty M, Cleland LG, James MJ, Fraser RJ, Cobiac L, et al. Fish oil administration in older adults: is there potential for adverse events? A systematic review of the literature. BMC Geriatr 2013;13:41. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Sanchez-Villegas A, Henriquez P, Figueiras A, Ortuno F, Lahortiga F, Martinez-Gonzalez MA. Long chain omega-3 fatty acids intake, fish consumption and mental disorders in the SUN cohort study. Eur J Nutr 2007;46:337–46. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Kiecolt-Glaser JK, Belury MA, Andridge R, Malarkey WB, Glaser R. Omega-3 supplementation lowers inflammation and anxiety in medical students: a randomized controlled trial. Brain Behav Immun 2011;25:1725–34. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. van de Rest O, Geleijnse JM, Kok FJ, van Staveren WA, Hoefnagels WH, Beekman AT, et al. Effect of fish-oil supplementation on mental well-being in older subjects: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr 2008;88:706–13. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Lesperance F, Frasure-Smith N, St-Andre E, Turecki G, Lesperance P, Wisniewski SR. The efficacy of omega-3 supplementation for major depression: a randomized controlled trial. J Clin Psychiatry 2011;72:1054–62. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Smith SC, Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and Other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation 2011;124:2458–73. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (179.0 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Case report
- Open access
- Published: 09 October 2024

Triphallia: the first cadaveric description of internal penile triplication: a case report
- John Buchanan 1 ,
- Madeleine Gadd 1 ,
- Rose How ORCID: orcid.org/0000-0002-6620-4925 1 ,
- Edward Mathews 1 ,
- Andre Coetzee 1 &
- Karuna Katti 1
Journal of Medical Case Reports volume 18 , Article number: 490 ( 2024 ) Cite this article
149k Accesses
739 Altmetric
Metrics details
Introduction
Triphallia, a rare congenital anomaly describing the presence of three distinct penile shafts, has been reported only once in the literature. This case report, based on an extensive literature review, describes the serendipitous discovery during cadaveric dissection of the second reported human case of triphallia, distinctly morphologically different from the previous case.
Case presentation
Despite the normal appearance of external genitalia on examination, the dissection of a 78-year-old white male revealed a remarkable anatomical variation: two small supernumerary penises stacked in a sagittal orientation posteroinferiorly to the primary penis. Each penile shaft displayed its own corpora cavernosa and glans penis. The primary penis and largest and most superficial of the supernumerary penises shared a single urethra, which coursed through the secondary penis prior to its passage through the primary penis. A urethra-like structure was absent from the smallest supernumerary penis.
This case report provides a comprehensive description of the anatomical features of triphallia in a cadaver, shedding light on the morphology, embryology, and clinical implications of this anomaly. Without dissection, this anatomical variation would have remained undiscovered, suggesting the prevalence of polyphallia may be greater than expected. The single tortuous urethra present in this case, as well as the supernumerary and blind ending urethras present in many cases of penile duplication, may pose significant risk of infection, sexual dysfunction, subfertility, and traumatic catheterization.
Significance
These findings underscore the importance of meticulous anatomical dissections and may act as a resource for anatomists and those studying genitourinary anomalies. Although we can only speculate as to which functional implications this patient may have experienced, understanding such anatomical variations contributes to both knowledge of human anatomy and clinical management should the condition be encountered in living individuals.
Peer Review reports
Congenital supernumerary penile formation is an extremely rare abnormality affecting approximately 1 in 5–6 million live births ( 1 ). In total, 168 papers, dated from 1606 to 2023, were found to report polyphallia ( 2 , 3 ). According to the classification system by Vilanova ( 4 ), 112 showed complete diphallia, 50 demonstrated pseudodiphallia, and 1 reported triphallia; 5 did not contain sufficient information to classify. The phenotypic differences displayed across these papers varied dramatically, potentially due to the wide range of pathophysiological causes, however, this made little difference clinically. Almost all surgeons decided to remove an additional external penis, often the non-functional or smaller of the two. However, typically no action was taken with regard to internal penis formation, as they are usually asymptomatic.
Six diphallia cases have been reported with internal accessory penises, meaning that the accessory penis is concealed within the skin ( 5 , 6 , 7 , 8 , 9 , 10 ). Despite the majority of external penile duplication being associated with other congenital abnormalities, including midline structure duplication and vertebrae, anus, heart, trachea, esophagus, kidney, and limbs (VACTERYL) association, internal penile duplication often presents later in life as an incidental finding.
As the second known case of triphallia, this case is noteworthy, not only due to its rarity, but also because of the phenotypic differences between this case and the prior triphallia case reported by Jabali and Mohammed ( 1 ). As the inferior two penises were concealed within the scrotal sac, external genitalia appeared normal. This may explain why the abnormality was not observed until post mortem exploration.
Without any symptoms and additional medical needs, concealed internal penises may not present themselves, preventing diagnosis. Hence, polyphallia may be more prevalent than currently understood. It is of clinical importance for healthcare providers to be aware of polyphallia for the diagnosis of patients presenting with urological symptoms and for healthcare interventions, such as simple catheter insertion, urological imaging, and surgery.
This case report will provide a description of the triphallia, found incidentally, discussing its pathophysiology and potential impacts on health.
Normal male genital embryology
From week 4 of embryonic development, there is proliferation of mesenchymal cells surrounding the cloacal membrane. At the caudal end, these form the genital tubercle, and at the cranial end, they form the urogenital folds (inner genital swellings) and the more lateral genital swellings ( 11 , 12 ).
In fetuses with the Y chromosome, the sex-determining region Y (SRY) gene is expressed, triggering testicular development. This begins with the development of Sertoli cells, which induce development of Leydig cells. The Leydig cells produce testosterone from 8–9 weeks, which induces the development of male external genitalia ( 11 , 13 ). Testosterone is converted to dihydrotestosterone (DHT) by 5α-reductase, which is expressed in the urogenital sinus and genital tubercle, and the DHT acts on androgen receptors in these areas to promote development of male external genitalia ( 13 ).
The genital tubercle elongates and becomes the corpora cavernosa and spongiosum, as well as the glans penis. The urethral plate (derived from endoderm) extends from the pelvic urethra into the glans penis. The urethral plate is canalized from proximal to distal, often referred to as the “opening zipper.” This canalization stops at the coronal sulcus, and hence does not extend into the glans penis. Urethral formation is different in the penile shaft as opposed to the glans penis. In the penile shaft, the edges of the canalized urethral plate fuse, forming the penile urethra (“closing zipper”), leaving the median penile raphe. In the glans there is direct canalization of the urethral plate to form the remainder of the urethra, with no urethral groove ( 13 ). The skin of the penis and the prepuce are formed from the ectoderm ( 11 , 13 ).
According to local policy, the identity of donors, and their medical history, must not be disclosed to researchers. As such, knowledge of this patient’s medical history is limited, and restricted to findings made during anatomical dissection and inspection.
Patient description
This white male, in his late 70s, was around 6 feet tall and of a medium–large build. The most notable finding, as previously discussed, was the presence of internal penile triplication. These penile morphological abnormalities may not have been identified during his life. However, he may have lived with functional deficits due to the abnormal anatomy of the region, which may include urinary tract infections, erectile dysfunction, or fertility issues, as later described.
Cadaveric findings
With the skin of the pelvis largely intact, the pelvis was divided in a midsagittal plane; we incised through the pubic symphysis, the penis, and the scrotum, and extended the dissection of the pelvic floor to just anterior to the anus. This midline dissection allowed us to appreciate a sagittal cross section of the penis as well as visualize both undissected testes, one on either side of the incision. Upon further exploration, three penis-like structures were found adjacent to each other, aligned in the mid-sagittal plane from dorsal to ventral. This is known as sagittal stacking ( 3 ). After further meticulous dissection, discussions and review of literature, we came to the conclusion that this was a case of triphallia.
The largest and most dorsal of the structures was the only structure seen externally and hence will be referred to as the primary penis. The other two structures (termed the secondary and tertiary penises) appeared to be located within the skin of the scrotal sac, hence why they were not visible in the undissected specimen. The secondary penis was located immediately deep to the primary penis and had macroscopically discernible and distinct regions comparable to the normal penile anatomy (the corpus spongiosum and urethra, corpora cavernosa, and the glans penis). The tertiary penis lay deep to the secondary penis, however, did not have the same obvious anatomical features seen in the primary or secondary penises; corpora cavernosa and glans penis were identified, however, there was an absence of corpus spongiosum and a urethra (Figs. 1 , 2 ).

Sagittal, cross-sectional dissection of the male pelvis. This is a photograph taken of the male pelvis in situ, following a sagittal, cross-sectional, cadaveric dissection. The structures have been labelled as follows: 1. primary penis, 2. secondary penis, 3. tertiary penis, 4. pubic symphysis, and 5. testes. Following dissection in situ, the three penises along with the urinary bladder and prostate were excised together for further exploration

Ex situ triphallia dissection. This figure shows a midline section of the penile triplication. The following structures have been identified: 1. corpora spongiosum of glans penis (with urethra), 2. corpora spongiosa of primary and secondary penises, 3. corpora cavernosa of primary and secondary penises, 4. external urethral meatus of primary penis, 5. tertiary penis, 6. secondary penis, 7. primary penis, and 8. corpora cavernosa of tertiary penis
With the aim of tracing the urethra of the primary penis, a probe was inserted into the external urethral orifice and advanced into the urethra. When it became apparent that the probe could not be advanced further, the primary penis was dissected more posteriorly in a sagittal plane. At this point, it became evident that the urethra of the primary penis extended into the secondary penis, and then could be traced superiorly to the internal urethral orifice. This revealed the meandering course of a single urethra, devoid of any branches, through the secondary and then primary penis up to the external urethral orifice. No urethra-like structure was identified in the tertiary penis.
Some important negative cadaveric findings in this case are accessory kidney, ureter, or bladder; duplication of the lower gastrointestinal tract; bifid or solitary scrotum; imperforate anus; and anterior abdominal wall defects.
The schematic diagram below (Fig. 3 ) shows the primary penis and two supernumerary penises, the penile and scrotal skin, and the testis.

Schematic diagram of internal triphallia. This figure is a schematic diagram of the sagittal cross section of the male pelvis in this case. The arrangement of triphallia can be seen above. The diagram can be labeled as follows: 1. pubic symphysis, 2. vas deferens, 3. epididymis, 4. testicle, 5. skin, 6. tertiary penis, 7. corpus cavernosum of tertiary penis, 8. glans of tertiary penis, 9. corpus spongiosum of secondary penis, 10. secondary penis, 11. corpus cavernosum of secondary penis, 12. glans of secondary penis, 13. urethral pathway, 14. corpus spongiosum of primary penis (continuous with glans), 15. corpus cavernosum of primary penis, 16. glans of primary penis, 17. urethral opening, 18. primary penis, and 19. connective tissue
The dimensions of the three penile structures are presented in Table 1 .
This table lists the dimensions of each penis. All measurements of length were taken from the base of the body of the penis to the furthest point at the tip of the glans penis. All measurements of width were taken at the widest point of the glans penis from dorsal to ventral.
The penis develops from the genital tubercle and is controlled by DHT. Genetic abnormalities affecting the expression of androgen receptors may cause morphological genital abnormalities ( 1 ). In this case, there may have been triplication of the genital tubercle. The urethra originally developed in the secondary penis, however, when this penis failed to develop, the urethra diverted its course and developed in the primary penis instead. The tertiary penis is a remnant of the triplicated genital tubercle.
There is an increased risk of urinary tract infections in diphallia or triphallia cases with multiple or blind-ending urethras due to urine stagnation ( 14 ). In this case, the risk of urinary tract infections (UTIs) is not likely to be increased as there is no blind-ending urethra. This person may have experienced dyspareunia due to the potential erection of the secondary and tertiary penises.
Most cases of supernumerary penises either presented in the neonatal period with evident external polyphallia or with sexual dysfunction, obstructive urinary symptoms, and urinary incontinence in adulthood ( 2 , 8 , 15 , 16 , 17 ). The majority of these cases are associated with various other congenital defects, including “defects in number” of kidneys, ureters, and bladders; ectopic and extrophic bladder and other abdominal viscera; supernumerary or imperforate anuses; and hypo/epispadias; among many others ( 6 , 18 , 19 , 20 , 21 , 22 ).
We cannot be certain that in this case the defect remained unnoticed in life, as there is a history of inguinal hernia repair. Due to the tortuous nature of the urethra, a urinary catheter would have proved challenging to pass. If the defect had been noticed during his life it may have simply been left untouched due to the apparent lack of symptoms and its benign nature. In other similar cases of supernumerary penises, but with prevalent undesirable symptoms or cosmetic appearance, surgical resection was frequently utilized ( 23 , 24 , 25 , 26 ).
There are currently no all-encompassing or clinically useful classification systems for supernumerary penises. The majority of studies use the classification system proposed by Schneider et al . ( 27 ); however, their categories fail to involve all cases of supernumerary penises and have little clinical relevance. Other systems have been created, such as that produced by Kendrick and Kimble ( 3 ), which builds on the Schneider classification. This newer system, despite capturing a greater number of the phenotypes and describing them more clearly, adds in a degree of complexity that once again reduces the clinical usefulness of the system. Moreover, due to the uncertainty surrounding nomenclature in the literature, classification of this case is difficult.
Through lack of consensus and the poor clinical usefulness of the current systems, a new classification system that retains simplicity and uniformity would be invaluable in the clinical setting and should be the focus of further reports.
Availability of data and materials
Not applicable.
Abbreviations
Sex-determining region Y
Dihydrotestosterone
Urinary tract infection
Jabali SS, Mohammed AA. Triphallia (triple penis), the first reported case in human. Int J Surg Case Rep. 2020;4(77):198–200.
Article Google Scholar
Samadi Y, Werner Z, Crigger C, Elbakry A, Ozolek J, Al-Omar O. Surgical correction of true diphallia in a newborn male. Urology. 2021;156:e117–20.
Article PubMed Google Scholar
Kendrick DJ, Kimble RM. Diphallia: literature review and proposed surgical classification system. ANZ J Surg. 2022;92(9):2053–65.
Article PubMed PubMed Central Google Scholar
Vilanova X, Raventos A. Pseudodiphallia, a rare anomaly. J Urol. 1954;71(3):338–46.
Article CAS PubMed Google Scholar
Torres Peris V, Jorda Cuevas E, Ramon QL. Pseudodiphallia. Int J Dermatol. 1992;31(2):119–21.
Arunachalam P, Pillai SB, Citla SD. Classical cloacal exstrophy with intravesical phallus. J Pediatr Surg. 2012;47(7):E5-8.
Gammie WP, Davies JH. Diphallus in an adult. Br J Urol. 1988;62(2):185–6.
Fowler MF. Double penis: report of a case with surgical management. Am Surg. 1963;29:555–6.
CAS PubMed Google Scholar
Zischka-Konorsa W, Bibus B. On a partially into the urinary bladder protruding diphallus bifidus. Zentralbl Allg Pathol. 1965;107(2):166–9.
Soccorso G, Ninan GK. A case of perineal lipoma with accessory scrotum and pseudo- diphallia. Eur J Pediatr Surg. 2009;19(1):55–6.
Yiee JH, Baskin LS. Penile embryology and anatomy. ScientificWorldJournal. 2010;29(10):1174–9.
Sajjad Y. Development of the genital ducts and external genitalia in the early human embryo. J Obstet Gynaecol Res. 2010;36(5):929–37.
Baskin L, Shen J, Sinclair A, Cao M, Liu X, Liu G, et al . Development of the human penis and clitoris. Differentiation. 2018;103:74–85.
Article CAS PubMed PubMed Central Google Scholar
Heyns CF. Urinary tract infection associated with conditions causing urinary tract obstruction and stasis, excluding urolithiasis and neuropathic bladder. World J Urol. 2012;30(1):77–83.
Gavali JS, Deshpande AV, Sanghani HH, Hirugade ST, Talpallikar MC, Borwankar SS. Glanular diphallus with urethral stricture. Pediatr Surg Int. 2002;18(1):70–1.
Kardasevic M, Begic F, Sivic M. Penile duplication in newborn with multiple anomalies. Med Arch. 2012;66(3):206–8.
Skott M, Korsgaard U, Rawashdeh YF. A case of penile duplication with neonatal teratoma and bladder neck incompetence. Scand J Urol. 2021;55(5):422–6.
Westenfelder M. Diphallus and bladder exstrophy: a case report. Monogr Paediatr. 1981;12:50–4.
Cernach MC, Hayashi H, Soares D. Diphallia associated with malformation of hindgut derivatives. Urology. 1989;33(3):209–10.
Marti-Bonmati L, Menor F, Gomez J, Cortina H, Garcia IF. Value of sonography in true complete diphallia. J Urol. 1989;142(2 Pt 1):356–7.
Mutlu N, Baykal M, Merder E, Culha M, Canbazoglu N. Diphallus with urethral duplication: a rare case. Int J Clin Pract. 1997;51(8):525–6.
Varghese VC, Sukumaran TU. Penile duplication. Indian Pediatr. 2004;41(11):1166.
PubMed Google Scholar
Dewan PA, Lawrence MJ, Pip A, Kasa S. Diphallus associated with partial caudal duplication. Pediatr Surg Int. 1998;14(1–2):131–3.
Karagözlü Akgül A, Uçar M, Çelik F, Kırıştıoğlu İ, Kılıç N. Complete penile duplication with structurally normal penises: a case report. Balkan Med J. 2018;35(4):340–3.
Macedo A, Ottoni SL, Camilato PCB, Ganchozo HSC, Garrone G, de Marcondes RM, et al . Complete diphallia: how to proceed? J Pediatr Urol. 2022;18(3):399–400.
Zhang W, Yu N, Liu Z, Wang X. Pseudodiphallia: a rare kind of diphallia: a case report and literature review. Medicine. 2020;99(33): e21638.
Schneider P, Lamitter JK, Uson AC, Melicow AC, et al . The male genital tract. In: Mustard WT, Ravitch MM, Snyder WH, et al ., editors. Pediatric surgery. 2nd ed. Chicago: Year Book Medical Publishers; 1969. p. 1263.
Google Scholar
Download references
Acknowledgements
We would first like to express our gratitude to the donor who gave the most selfless gift of all. Thanks must also go to Vicky Cottrell and Natasha Russell for their advice and assistance. Finally, thanks to our friends and family for the unwavering encouragements.
No funding was required for completion of the research. The University of Birmingham publisher agreements will be fulfilled providing acceptance of publication.
Author information
Authors and affiliations.
University of Birmingham Medical School, Edgbaston, Birmingham, West Midlands, B15 2TT, UK
John Buchanan, Madeleine Gadd, Rose How, Edward Mathews, Andre Coetzee & Karuna Katti
You can also search for this author in PubMed Google Scholar
Contributions
RH, JB, MG, and EM contributed equally as main researchers, performing dissection and completing this report. KK and AC supervised this project. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Rose How .
Ethics declarations
Ethics approval and consent to participate.
The authors state that every effort was made to follow all local and international ethical guidelines and laws that pertain to the use of human cadaveric donors in anatomical research. Written informed consent was obtained from the patient for participation in this case report and any accompanying images. A copy of written consent is available for review by the Editor-in-Chief of this journal.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
All authors declare there are no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Buchanan, J., Gadd, M., How, R. et al. Triphallia: the first cadaveric description of internal penile triplication: a case report. J Med Case Reports 18 , 490 (2024). https://doi.org/10.1186/s13256-024-04751-5
Download citation
Received : 08 November 2023
Accepted : 05 July 2024
Published : 09 October 2024
DOI : https://doi.org/10.1186/s13256-024-04751-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cadaveric dissection
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
News releases.
News Release
Thursday, October 10, 2024
First wave of COVID-19 increased risk of heart attack, stroke up to three years later
NIH-funded study focused on original virus strain, unvaccinated participants during pandemic.

Infection from COVID-19 appeared to significantly increase the risk of heart attack, stroke, and death for up to three years among unvaccinated people early in the pandemic when the original SARS-CoV-2 virus strain emerged, according to a National Institutes of Health (NIH)-supported study. The findings, among people with or without heart disease, confirm previous research showing an associated higher risk of cardiovascular events after a COVID-19 infection but are the first to suggest the heightened risk might last up to three years following initial infection, at least among people infected in the first wave of the pandemic.
Compared to people with no COVID-19 history, the study found those who developed COVID-19 early in the pandemic had double the risk for cardiovascular events, while those with severe cases had nearly four times the risk. The findings were published in the journal Arteriosclerosis, Thrombosis, and Vascular Biology .
“This study sheds new light on the potential long-term cardiovascular effects of COVID-19, a still-looming public health threat,” said David Goff, M.D., Ph.D., director for the Division of Cardiovascular Sciences at NIH’s National Heart, Lung, and Blood Institute (NHLBI), which largely funded the study. “These results, especially if confirmed by longer term follow-up, support efforts to identify effective heart disease prevention strategies for patients who’ve had severe COVID-19. But more studies are needed to demonstrate effectiveness.”
The study is also the first to show that increased risk of heart attack and stroke in patients with severe COVID-19 may have a genetic component involving blood type. Researchers found that hospitalization for COVID-19 more than doubled the risk of heart attack or stroke among patients with A, B, or AB blood types, but not in patients with O types, which seemed to be associated with a lower risk of severe COVID-19.
Scientists studied data from 10,000 people enrolled in the UK Biobank, a large biomedical database of European patients. Patients were ages 40 to 69 at the time of enrollment and included 8,000 who had tested positive for the COVID-19 virus and 2,000 who were hospitalized with severe COVID-19 between Feb. 1, 2020, and Dec. 31, 2020. None of the patients had been vaccinated, as vaccines were not available during that period.
The researchers compared the two COVID-19 subgroups to a group of nearly 218,000 people who did not have the condition. They then tracked the patients from the time of their COVID-19 diagnosis until the development of either heart attack, stroke, or death, up to nearly three years.
Accounting for patients who had pre-existing heart disease – about 11% in both groups – the researchers found that the risk of heart attack, stroke, and death was twice as high among all the COVID-19 patients and four times as high among those who had severe cases that required hospitalization, compared to those who had never been infected. The data further show that, within each of the three follow-up years, the risk of having a major cardiovascular event was still significantly elevated compared to the controls – in some cases, the researchers said, almost as high or even higher than having a known cardiovascular risk factor, such as Type 2 diabetes.
“Given that more than 1 billion people worldwide have already experienced COVID-19 infection, the implications for global heart health are significant,” said study leader Hooman Allayee, Ph.D., a professor of population and public health sciences at the University of Southern California Keck School of Medicine in Los Angeles. “The question now is whether or not severe COVID-19 should be considered another risk factor for cardiovascular disease, much like type 2 diabetes or peripheral artery disease, where treatment focused on cardiovascular disease prevention may be valuable.”
Allayee notes that the findings apply mainly to people who were infected early in the pandemic. It is unclear whether the risk of cardiovascular disease is persistent or may be persistent for people who have had severe COVID-19 more recently (from 2021 to the present).
Scientists state that the study was limited due to inclusion of patients from only the UK Biobank, a group that is mostly white. Whether the results will differ in a population with more racial and ethnic diversity is unclear and awaits further study. As the study participants were unvaccinated, future studies will be needed to determine whether vaccines influence cardiovascular risk. Studies on the connection between blood type and COVID-19 infection are also needed as the mechanism for the gene-virus interaction remains unclear.
This study was supported by NIH grants R01HL148110, R01HL168493, U54HL170326, R01DK132735, P01HL147823, R01HL147883, and P30ES007048.
About the National Heart, Lung, and Blood Institute (NHLBI): NHLBI is the global leader in conducting and supporting research in heart, lung, and blood diseases and sleep disorders that advances scientific knowledge, improves public health, and saves lives. For more information, visit www.nhlbi.nih.gov .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
NIH…Turning Discovery Into Health ®
Allayee, H, et al. COVID-19 Is a Coronary Artery Disease Risk Equivalent and Exhibits a Genetic Interaction With ABO Blood Type . [2024] Arteriosclerosis, Thrombosis, and Vascular Biology . DOI: 10.1161/ATVBAHA.124.321001
Connect with Us
- More Social Media from NIH
Cutting-edge test uses DNA sequencing to yield diagnoses for some medical mysteries
The Summary
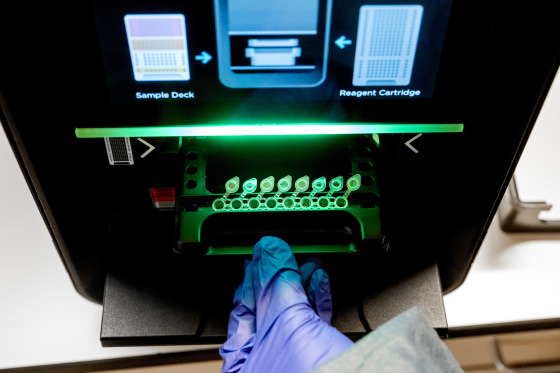
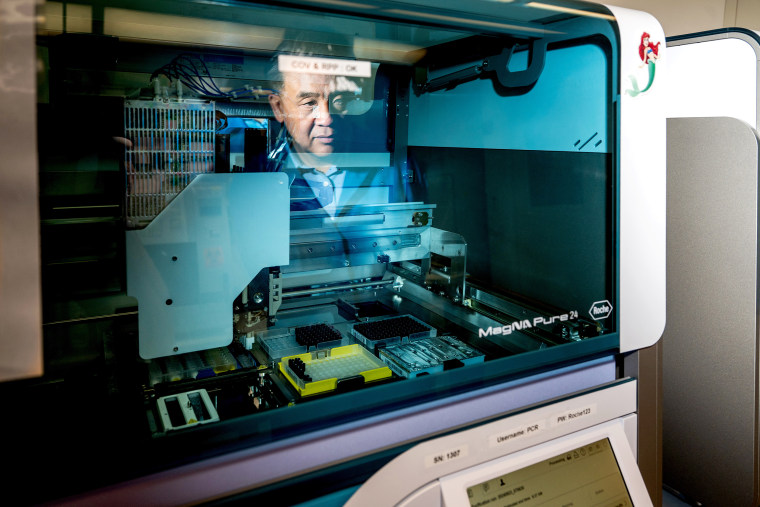
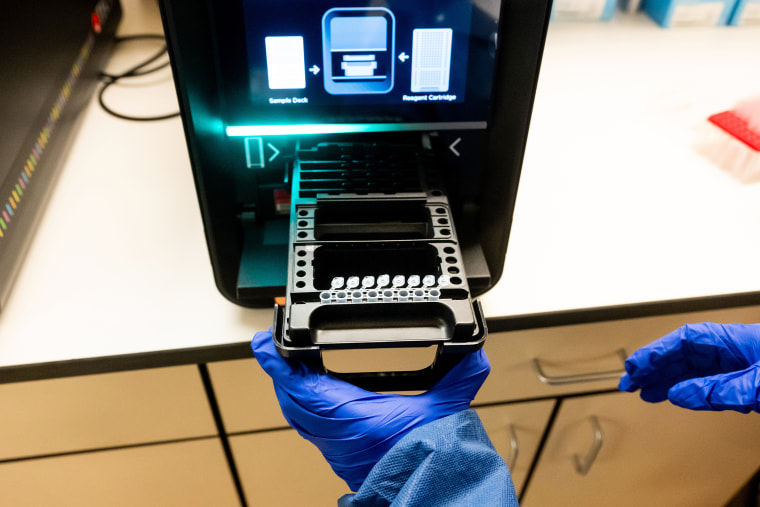
- An advanced diagnostic test uses genetic sequencing to detect a variety of pathogens — viruses, bacteria, fungi and parasites — that might be causing an illness.
- A new study found that it has been effective at identifying the cause of neurological infections like meningitis.
- The test is not yet FDA-approved, and it is expensive to run, but its creators hope it is used more broadly in the future.
A cutting-edge diagnostic test is helping some doctors find diagnoses for medical mysteries by analyzing DNA and RNA to detect a broad swath of viruses, bacteria, fungi and parasites, according to a pair of studies published Tuesday.
Traditional diagnostic tests are generally designed to measure specific substances such as proteins, hormones or trace amounts of genetic material. But the genomic test, developed at the University of California, San Francisco, instead extracts all the DNA and RNA present in a sample of blood, tissue or body fluid, then sequences that genetic material. It compares the sequences to a vast database of pathogens to see what matches up.
The technology is not a replacement for existing tests used to diagnose common illnesses — like those for Covid or strep throat — since it’s slower to deliver results and more expensive. But it shows promise in a particular scenario: when a patient is in the hospital with severe symptoms, but initial tests come back negative and doctors can’t figure out what’s wrong.
Already, the test has been effective at identifying the cause of neurological infections such as meningitis and encephalitis (swelling of the brain or its surrounding membranes), according to one of the new studies, published Tuesday in the journal Nature Medicine. Using samples of spinal fluid, it was able to diagnose 86% of the neurological infections it encountered out of more than 4,800 samples gathered at UCSF over a roughly seven-year period.
In 2021 and 2022, the test was able to link cases of encephalitis among transplant recipients to yellow fever in their organ donor . And last year, it helped pinpoint the cause of a meningitis outbreak among patients who had undergone surgical procedures in Mexico.
“Our test was used to identify the cause of it as a specific fungus, Fusarium solani, from one of the early patients who had become symptomatic,” said Dr. Charles Chiu, a professor of laboratory medicine and infectious diseases at UCSF and the senior author of the new study.
The second study on the test, published Tuesday in the journal Nature Communications, suggests it could also be used to detect novel viruses, including those with the potential to start pandemics. The researchers ran a simulation to see whether the test could pick up on human viruses like the coronavirus that causes Covid, even if the researchers removed those viruses’ genetic sequences from the database on which the test relies.
The test still identified the viruses based on related strains in animals, Chiu said.
The Food and Drug Administration has granted the test a “breakthrough device” designation, which allows labs to use it based on its potential to help patients, even though the agency hasn’t yet approved it. But the test is expensive: Running it costs $3,000 per sample and fewer than 10 labs use it routinely, Chiu said.
“Traditionally, it’s been used as a test of last resort, but that’s primarily because of issues involving, for instance, the cost of the test, the fact that it’s only available in specialized reference laboratories, and it also is quite laborious to run,” he said.
Chiu added that the new research “raises the possibility that we perhaps should be considering running this test earlier” in the course of a person’s infection.
Chiu and his fellow UCSF researchers developed the test 10 years ago. Shortly after, it detected a case of leptospirosis , a bacterial infection, in a 14-year-old boy who was in a medically induced coma. The diagnosis led doctors to prescribe penicillin, after which the boy recovered quickly.
But the test comes with limitations, according to Susan Butler-Wu, an associate professor of clinical pathology at the University of Southern California.
The technology is likely too complicated for the average community hospital to adopt in the foreseeable future, she said. And doctors could have a hard time interpreting the results, so they would need to consult with a laboratory director who has the appropriate expertise.
“This just is not something that a clinical lab will be doing until somebody commercially puts it in a box with an easy button,” Butler-Wu said.
The test also misses some cases, she added, so it should be used alongside other diagnostic tests in hospitals.
“It’s not a one-stop shop,” Butler-Wu said. “It just can be helpful as an additional tool.”
Nonetheless, Chiu said, he could envision the test being used widely in hospitals someday to diagnose all sorts of illnesses, such as the root causes of pneumonia or sepsis.
“We need to get the cost down and we need to get the turnaround times down as well,” he said.
Aria Bendix is the breaking health reporter for NBC News Digital.
- help center

Certified Clinical Medical Assistant (CCMA) - Practice Tests + Study Guide
Ideal for exam preparation, our dynamic Certified Clinical Medical Assistant (CCMA) study guide and practice tests package is designed to help candidates enrolled in a medical assisting training program to succeed on the NHA CCMA exam and enter the healthcare workforce. These resources offer a comprehensive and structured approach directly aligned to NHA's CCMA test plan and exam domains.
Study Guide is available in printed and online formats; practice tests are available online only.
*Online materials can only be accessed on your computer or tablet.
The CCMA Practice Tests Include:
Four unique 150-item practice tests, up to 6 total attempts
Focused Review® online remediation
Performance Analytics to assess learner performance, progress, and usage
Available online from any computer or tablet with an internet connection to access practice tests whenever and wherever you want.
Practice Test Details
There are four unique versions of the practice test to evaluate knowledge of CCMA principles.
The Baseline (1 attempt) and Final Practice Test (1 attempt) are timed (3 hours), without rationales, to mimic the experience of sitting for the National Exam, with 150 questions, plus 30 pretest items.
The Practice Tests (4 total attempts) contains 150 questions, are not timed, contain rationales, and Focused Review (Remediation).
Practice Tests are aligned to the NHA test plan and work in conjunction with the CCMA study guide.
Online Practice Tests can be accessed from any Internet connection, offering candidates the flexibility to test anytime.
CCMA Study Guide Options
The ccma study guide includes 13 modules covering the core medical assistant knowledge, skills and principles needed for job-readiness:.
Foundational Knowledge and Basic Science
Anatomy & Physiology
Patient Intake and Vitals
General Patient Care Part 1
General Patient Care Part 2
Infection Control and Safety
Point of Care Testing and Laboratory Procedures
EKG and Cardiovascular Testing
Patient Care Coordination and Education
Administrative Assisting
Communication and Customer Service
Medical Law and Ethics
Disclaimer: The purchase of NHA exam preparation materials is not required to sit for any NHA certification exam and use does not guarantee a passing score on an exam. All NHA certification programs and the corresponding exams are NCCA-accredited.
Related Products

Certified Medical Assistant (CCMA) Exam Application

Certified Clinical Medical Assistant (CCMA) Study Guide

Certified Clinical Medical Assistant (CCMA) Practice Tests


- Denna sida på svenska
- Nyheter startsida
- ki.se startsida
Very early medical abortion is effective and safe

Clinics and hospitals currently defer medication abortion until ultrasound confirms a pregnancy inside the uterus. However, a large international study led by researchers from Karolinska Institutet now indicates that treatment can be equally effective and safe even before the sixth week of pregnancy. The study is published in The New England Journal of Medicine.
35,550 abortions took place in Sweden in 2023, over 60 per cent of them before the end of the seventh week of pregnancy. Often, the procedure is held off until intrauterine pregnancy is confirmed by vaginal ultrasound to rule out the possibility of an ectopic pregnancy, in which the embryo attaches outside the uterus, usually in the fallopian tubes. An ectopic pregnancy is not terminated by a medication abortion and can be life-threatening for the woman. Ultrasound reveals a pregnancy in week five to six.

“Women often find out very early if they’re pregnant, and a majority also know if they want a termination and if so, want it to take place as quickly as possible,” says the study’s first author Karin Brandell , gynaecologist at Karolinska University Hospital and doctoral student at the Department of Women’s and Children’s Health , Karolinska Institutet. “Observational studies have produced contradictory results as regards effectiveness, so we wanted to study if very early abortion is just as effective and safe as waiting.”
Women from nine countries
The VEMA (Very early medical abortion) study included over 1,500 women at 26 clinics in nine countries who requested an abortion before ultrasound was able to confirm intrauterine pregnancy. They were randomly assigned to either a delayed abortion once pregnancy could be confirmed in the uterus (in week 5 to 6) or to early abortion (in week 4 to 6). Both groups received two drugs – mifepristone and misoprostol.
At the start of the study, all participants were up to six weeks pregnant and presented no symptoms of ectopic pregnancy (e.g. abdominal pain or bleeding) or risk factors for such a pregnancy (e.g. pregnancy despite a coil or previous ectopic pregnancies). The outcome measure was terminated pregnancy (complete abortion).

“Very early medical abortion was just as effective and safe to perform, even in case of an undiagnosed ectopic pregnancy,” says Kristina Gemzell-Danielsson , professor of obstetrics and gynaecology at the same department at Karolinska Institutet, senior physician at Karolinska University Hospital and project leader of the VEMA study.
A political issue
In both groups, over 95 per cent of the women had a complete abortion, but the few procedures that failed differed between the groups. On delayed treatment, the treatment was incomplete in 4.5 per cent of cases and required additional vacuum aspiration (surgery). In 0.1 per cent of cases, the pregnancy continued. In the early group, the pregnancy continued in 3 per cent of cases and 1.8 per cent required surgery for incomplete abortion. A total of 1 per cent of all participants had an ectopic pregnancy.
The women in the early group reported less pain and bleeding. In both groups, the women also expressed a desire to have the abortion performed as quickly as possible.
“Abortion is a political as well as a medical issue,” says Dr Brandell. “In Sweden, a woman can repeat the procedure a week after a failed early abortion. But a woman in Texas, where abortion is banned after the sixth week, can’t. It was therefore important to show that early abortion is equivalent to current standard procedure at a later stage of pregnancy.”
Better abortions and contraceptives
The researchers now want to test if a new combination of drugs for early abortion is also effective for ectopic pregnancies. They are also developing new contraceptives based on one of the components of current medical abortions, mifepristone.
“It can be taken in a lower dose than for abortion to prevent unwanted pregnancies in the form of one tablet a week, or when needed,” says Professor Gemzell-Danielsson.
The study was supported by grants from the Swedish Research Council, research funds of the Hospital System of Helsinki and Uusimaa, the European Society of Contraception and Reproductive Health, the Nordic Federation of Societies of Obstetrics and Gynecology, the Gothenburg Society of Medicine, and an ALF grant (Karolinska Institutet/Region Stockholm). The researchers’ conflicts of interests are reported in full in the study.
Publication
”Randomized Trial of Very Early Medication Abortion” , Karin Brandell, Tagrid Jar-Allah, John Reynolds-Wright, Helena Kopp Kallner, Helena Hognert, Frida Gyllenberg, Janina Kaislasuo, Anand Tamang, Heera Tuladhar, Clare Boerma, Karen Schimanski, Gillian Gibson, Mette Løkeland, Pia Teleman, Marie Bixo, Mette Mandrup Kjaer, Ervin Kallfa, Johan Bring, Oskari Heikinheimo, Sharon Cameron, and Kristina Gemzell-Danielsson, New England Journal of Medicine , online 6 November 2024, doi: 10.1056/NEJMoa2401646.

COMMENTS
For additional inquiries regarding studies at the National Institutes of Health, please call the Office of Patient Recruitment at 1-800-411-1222. Find NIH Clinical Center Trials. The National Institutes of Health (NIH) Clinical Center Search the Studies site is a registry of publicly supported clinical studies conducted mostly in Bethesda, MD.
Case 31-2024: A 37-Year-Old Man with Fever, Myalgia, Jaundice, and Respiratory Failure W.C. Hillmann and Others N Engl J Med 2024;391:1343-1354 A 37-year-old man was transferred to the hospital ...
A journal publishing case reports in all medical disciplines, including general medicine, drug interaction and adverse reactions. The largest online collection of medical case reports. Validation period: 11/12/2024, 12:52:32 AM - 11/12/2024, 6:52:32 AM
A 44-year-old woman presented with cough, dyspnea, and chest pain. On examination, she had tachycardia and hypotension. Evaluation revealed SARS-CoV-2 RNA in a nasopharyngeal swab, as well as eleva...
Aims and scope. Journal of Medical Case Reports will consider any original case report that expands the field of general medical knowledge, and original research relating to case reports. Case reports should show one of the following: Unreported or unusual side effects or adverse interactions involving medications.
Renal medicine. Respiratory medicine. Rheumatology. Sexual health. Sports and exercise medicine. Surgery. Urology. A journal publishing case reports in all medical disciplines, including general medicine, drug interaction and adverse reactions. The largest online collection of medical case reports.
Navbar Search Filter Mobile Enter search term Search. Issues Volume 2024, Issue 10, October 2024 (In Progress) Volume 2024, Issue 9, September 2024 (In Progress) Volume 2024, Issue 8, August 2024 ... Oxford Medical Case Reports is an open access, ...
R. Olson and Others N Engl J Med 2024;390:e51. Interactive Medical Case; VOL. 389 NO. 25; Dec 21, 2023; Uncovering a Hidden Threat
SAGE Open Medical Case Reports is a peer-reviewed, open access journal, which focusses on providing a publication home for short case reports and case series, which often do not find a place in traditional primary research journals, but provide key insights into real medical cases that are essential for physicians, and may ultimately help to improve patient outcomes.
About the Journal. Medicine: Case Reports and Study Protocols ® is a fully open access journal, providing authors with a distinctive new service offering continuous publication of case reports and study protocols across a broad spectrum of medical scientific disciplines and sub-specialties.. The APC for Medicine: Case Reports and Study Protocols ® is $600 (USD) for the Creative Commons CCBY ...
The LITFL Clinical Case Collection includes over 250 Q&A style clinical cases to assist ' Just-in-Time Learning ' and ' Life-Long Learning '. Cases are categorized by specialty and can be interrogated by keyword from the Clinical Case searchable database. Search by keywords; disease process; condition; eponym or clinical features….
Cases Database. 236 Gray's Inn Road, London, WC1X 8HB, United Kingdom; [email protected]; www.casesdatabase.com; continuously updated; open access; no cost. BioMed Central. Cases in clinical medicine can be defined as reports on patients where symptoms, diagnosis, treatment, and outcome are described, and some new side effect, disease ...
Clinical Case Reports is an open access journal aiming to improve global health outcomes by conveying important best practice messages and sharing clinical knowledge with medical case reports, clinical images, and procedural videos. As part of Wiley's Forward Series, this journal offers a streamlined, faster publication experience with a ...
Track what cases you open and complete. Sign In Create a Free Profile. Subscribe: Institutional or Individual. New on Case Files Collection. Case Files Collection. About. Basic Science Cases. Clinical Rotation Cases. Post-Graduate Cases.
Abstract. Case reports are a time-honored, important, integral, and accepted part of the medical literature. Both the Journal of Medical Case Reports and the Case Report section of BioMed Central Research Notes are committed to case report publication, and each have different criteria.Journal of Medical Case Reports was the world's first international, PubMed-listed medical journal devoted ...
CASE RECORDS OF THE MASSACHUSETTS GENERAL HOSPITAL 5 Case 10-2017 — A 6-Month-Old Boy with Gastrointestinal Bleeding and Abdominal Pain L.M. Allister and Others Mar 30, 2017 14 Case 2-2017 — An 18-Year-Old Woman with Acute Liver Failure K.R. Olson and Others Jan 19, 2017 CLINICAL PROBLEM-SOLVING 26 Making the Connection
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research.1 However, very simply… 'a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units'.1 A case study has also been described as an intensive, systematic investigation of a ...
Referring to the scenario in Unfolding Case Study 3, as soon as the patient arrived at the emergency room, the nurse began the process of critically thinking about what needed to be done. The nurse assessed the patient's situation and then recognized, analyzed, and prioritized the patient's needs.
Dr. Bardia: The Covid-19 pandemic poses a major challenge to the health care system, and several organizations have released consensus recommendations for management of breast cancer during this ...
case report The patient is a 55-year-old male employed as a professor in the USA. At Age 42, he consulted his general practitioner for major depressive disorder and was prescribed fluoxetine, eventually titrated to 40 mg. Pharmacotherapy combined with psychotherapy generally relieved the worst episodes of depressive disorder, but occasional ...
Background Hyperthyroidism, caused by metastatic differentiated thyroid cancer, is a rare condition that can be difficult to diagnose. Thyrotoxicosis and metastatic disease regarding functional metastasis increase morbidity and mortality in patients with functional metastasis and need to be treated. This study aims to present a case of hyper-functional metastasis of thyroid cancer to analyze ...
Introduction Triphallia, a rare congenital anomaly describing the presence of three distinct penile shafts, has been reported only once in the literature. This case report, based on an extensive literature review, describes the serendipitous discovery during cadaveric dissection of the second reported human case of triphallia, distinctly morphologically different from the previous case. Case ...
The study is also the first to show that increased risk of heart attack and stroke in patients with severe COVID-19 may have a genetic component involving blood type. Researchers found that hospitalization for COVID-19 more than doubled the risk of heart attack or stroke among patients with A, B, or AB blood types, but not in patients with O ...
A case report on a woman who fell sick after eating a zucchini has highlighted the importance of getting an accurate medical history and the role of nurses in making a diagnosis. A 54-year-old ...
A Woman with Depression, Recurrent Falls, and Inability to Care for Herself. A 65-year-old woman with depression presented with worsening neuropsychiatric symptoms, weight loss, unsteady gait ...
Online Study Guide. Printed Study Guide. Included Features: Recommended : Instructional lesson content aligned with the CCMA exam Case studies End of module quizzes Professionalism tips videos with self-reflection activities Interactive and engaging gaming-style activities to assess knowledge EHR simulation activities
A cutting-edge diagnostic test is helping some doctors find diagnoses for medical mysteries by analyzing DNA and RNA to detect a broad swath of viruses, bacteria, fungi and parasites, according to ...
Online Study Guide. Printed Study Guide. Included Features: Recommended : Instructional lesson content aligned with the CCMA exam Case studies End of module quizzes Professionalism tips videos with self-reflection activities Interactive and engaging gaming-style activities to assess knowledge EHR simulation activities
"Very early medical abortion was just as effective and safe to perform, even in case of an undiagnosed ectopic pregnancy," says Kristina Gemzell-Danielsson, professor of obstetrics and gynaecology at the same department at Karolinska Institutet, senior physician at Karolinska University Hospital and project leader of the VEMA study.. A political issue
Alfandre D. Clinical recommendations in medical practice: a proposed framework to reduce bias and improve the quality of medical decisions. J Clin Ethics 2016;27:21-27. Crossref