Build my resume
- Build a better resume in minutes
- Resume examples
- 2,000+ examples that work in 2024
- Resume templates
- Free templates for all levels
- Cover letters
- Cover letter generator
- It's like magic, we promise
- Cover letter examples
- Free downloads in Word & Docs

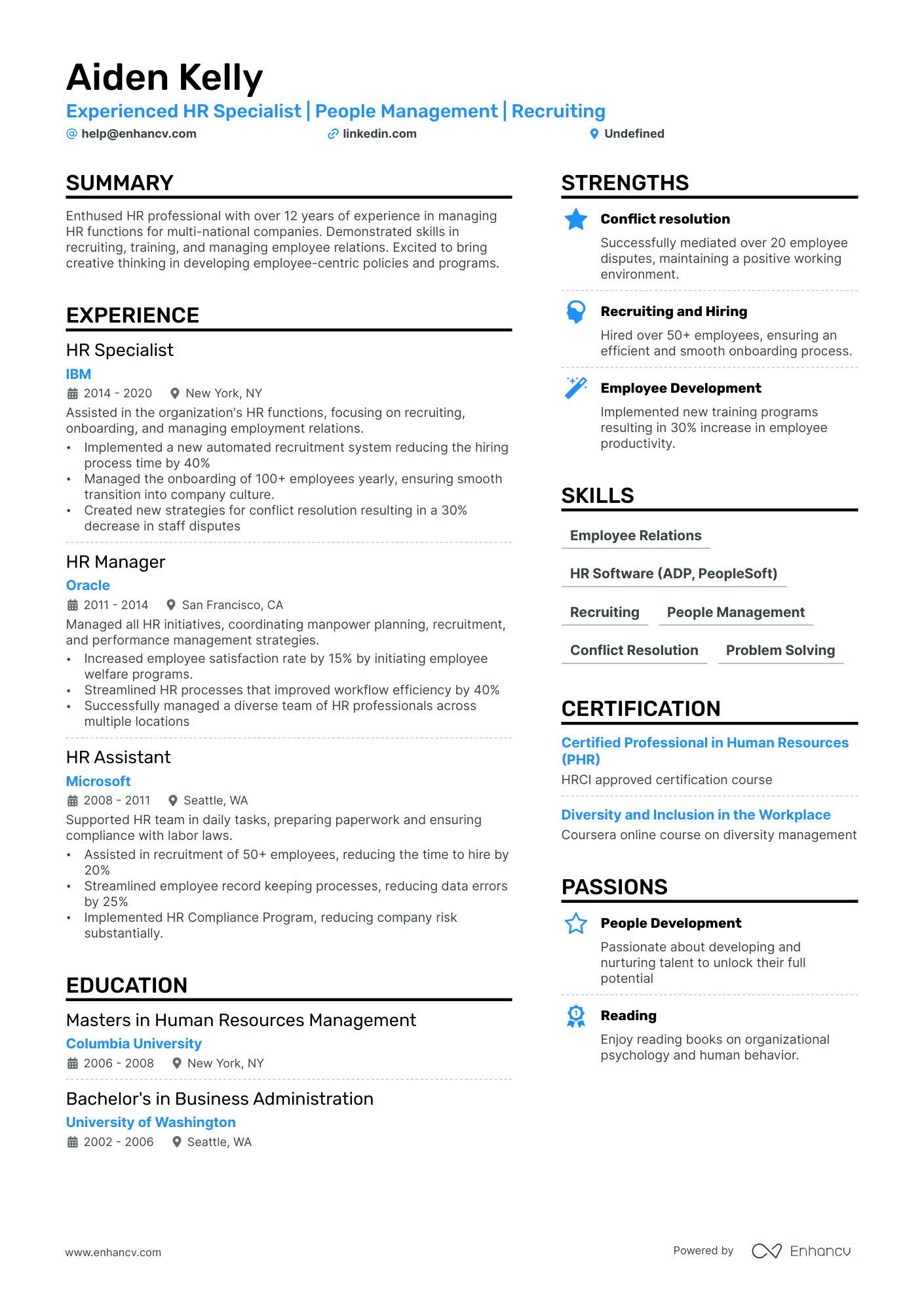
5 Returning to Workforce Resume Examples for 2024
- Returning to Workforce

Best for senior and mid-level candidates
There’s plenty of room in our elegant resume template to add your professional experience while impressing recruiters with a sleek design.
Resume Builder
Like this template? Customize this resume and make it your own with the help of our Al-powered suggestions, accent colors, and modern fonts.
- Returning to Workforce 2
- Returning to Workforce 3
- Returning to Workforce 4
- Returning to Workforce 5
- Returning to Workforce Resume Writing 101
Whether you took a sabbatical or spent some time caring for a loved one, returning to the workforce usually means leveraging a resume maker and a whirl with a free cover letter builder . Your skills and experiences might have changed since the last time you were employed, and you might want to change your resume formatting to emphasize your skills over the gap in your work experience.
Whatever the reason behind your return, we’ll help you put your best foot forward. Get ready to roll with our five returning to workforce resume examples.
Returning to Workforce Resume
or download as PDF

Returning to Workforce 2 Resume

Returning to Workforce 3 Resume

Returning to Workforce 4 Resume

Returning to Workforce 5 Resume

Related resume examples
- Stay At Home Mom Returning to Work
- Front Desk Receptionist
- Personal Assistant
- Stay At Home Mom
What Matters Most: Skills & Work Experience

While the role you’re applying for matters, hiring recruiters looking at a returning to workforce resume will want to know whether you applied yourself during your time away.
You don’t have to disclose every sordid detail—all you need is to demonstrate that your skills are relevant to the job , whether new or existing.
Here are some of the best returning to workforce skills recruiters are looking for.
9 best returning to workforce skills
- Customer service
- Project management
- Organization
- Time management
- Problem-solving
- Microsoft Office
- Communication skills
- Active listening
Sample returning to workforce job experience bullet points
Filling in the blanks with any volunteer, freelance, unpaid, or part-time work you might have done will help dispel any assumptions made about your resume gap.
Although you shouldn’t feel like you have to go into specifics about your career break (especially if it’s sensitive or personal), adding quantifiable metrics whenever possible can help potential employers get a better idea of what you did with your time.
Here are a few samples:
- Advised and assisted the family of 5 in planning healthy meals, purchasing, and preparing foods
- Created, assigned, and scheduled various housekeeping duties for 3 children ages 4 to 12, according to their capabilities
- Kept track of the grocery inventory, making sure items moved on a FIFO basis, saving the household $4,000+ a year in grocery shopping expenses
- Provided 24/7 in-home care for my mother during treatment for a medical condition until she made a full recovery within two years
- Traveled to 8 cities in Asia, Australia, South America, and North America to gain personal and professional perspective
Top 5 Tips for Your Returning to Workforce Resume
- If you’re returning to the workforce, chances are that the career experience you had might not be as relevant to the current job market, even if you have more than 10 years of experience. Unless you have been actively keeping up with your skills while you were away, it’s better to keep only the important details in your resume .
- Start with your career break, then record your most recent jobs. This filters out any employers who might prefer complete career histories and addresses your resume gap early on, allowing the reader to focus on the rest of your work experience and what you can contribute to the new role.
- You might have moved or had a change in relationship status, leading to a different last name. List your most recent contact details at the top of your resume, and consider adding any career-related social media you might have.
- Depending on the position you’re applying to, you could benefit from a skills section that details how you applied your skills in a quantifiable and measurable way. You can also highlight your skills section by moving them so that the recruiter reads it before your work experience.
- Listing your work experience in months and years can make the gap in your career stand out. Changing to using years only will help recruiters focus on the time you spent employed, shifting their perspective toward your career instead of the lack thereof.
Yes, especially if you’re having trouble filling out the blank space in your resume. You can also link your education with any studying or application you did during your time off. The key here is to demonstrate how your skills and experience are relevant to the present job climate.
Any job will do as long as you’re qualified for it and it appeals to you! Some people choose to change career paths when they return, while others get right back to the industry they previously worked in. While you’re job hunting, consider getting an entry-level job in the meantime to fill out your resume.
While we don’t usually recommend including a career summary if you have a lot of relevant information to include in your resume, adding one can help break the ice and mention your resume gap within the context of your career. If you choose to write one, make sure it’s tailored to the job you’re applying for.
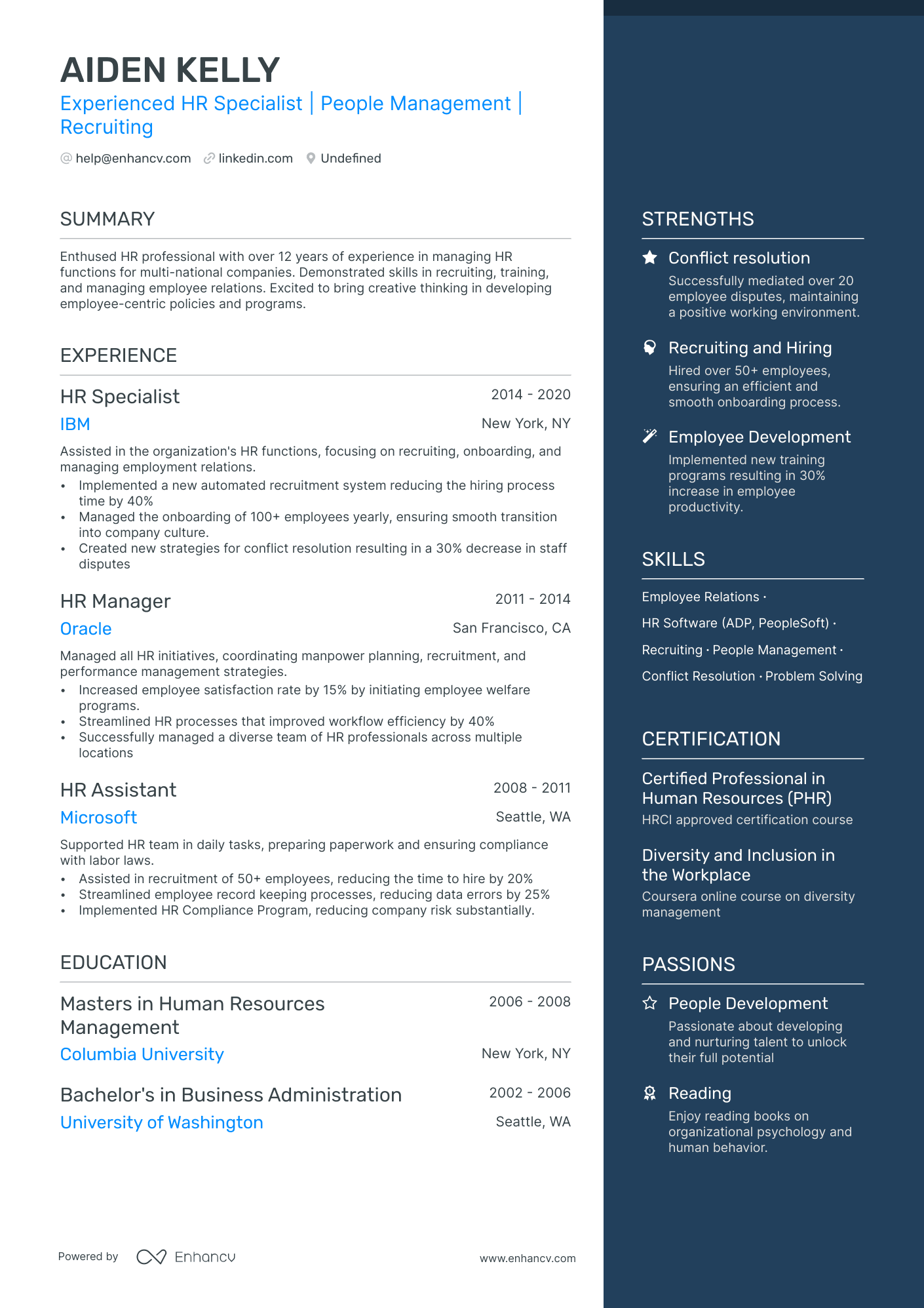
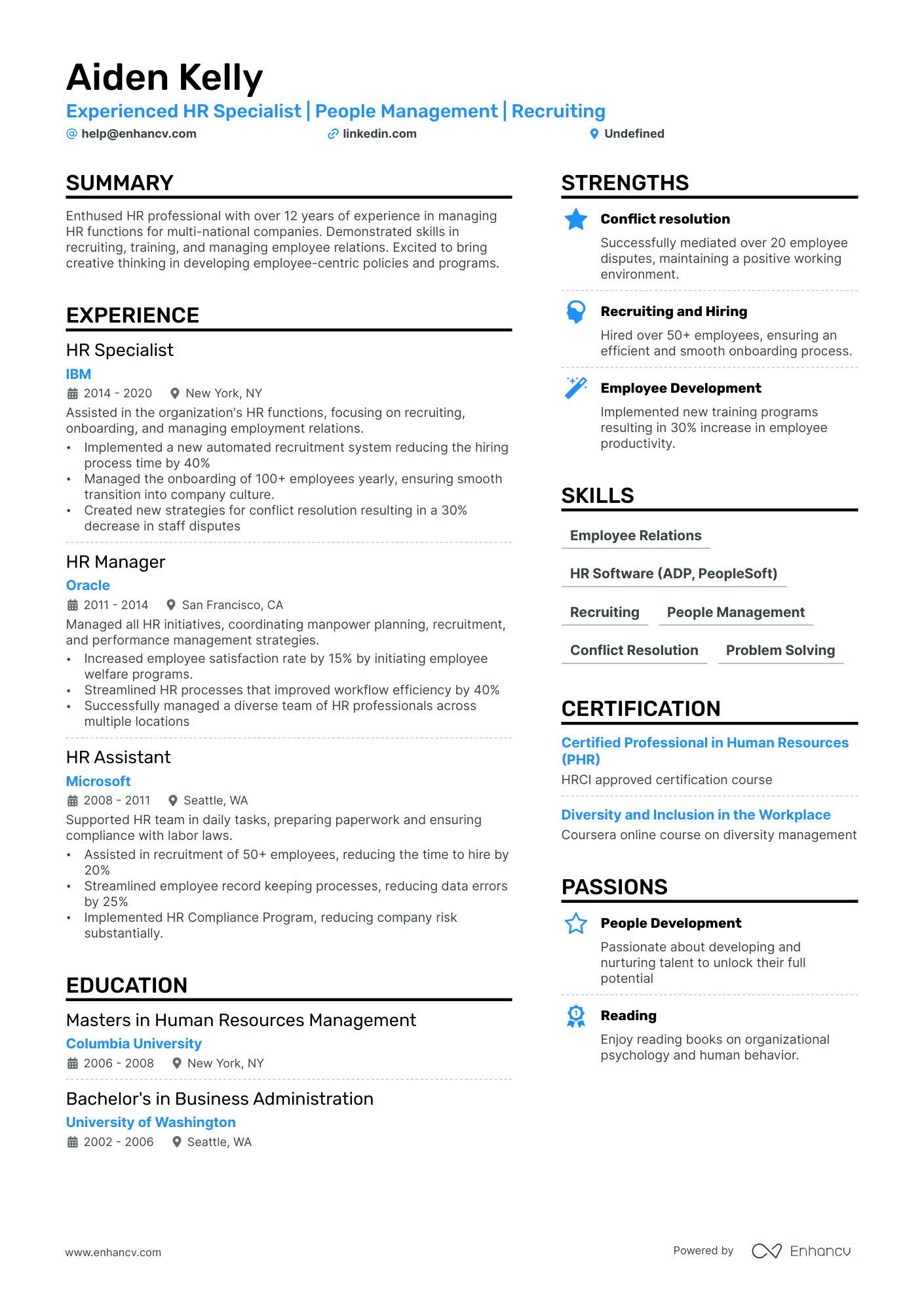
- • Implemented a new automated recruitment system reducing the hiring process time by 40%
- • Managed the onboarding of 100+ employees yearly, ensuring smooth transition into company culture.
- • Created new strategies for conflict resolution resulting in a 30% decrease in staff disputes
- • Increased employee satisfaction rate by 15% by initiating employee welfare programs.
- • Streamlined HR processes that improved workflow efficiency by 40%
- • Successfully managed a diverse team of HR professionals across multiple locations
- • Assisted in recruitment of 50+ employees, reducing the time to hire by 20%
- • Streamlined employee record keeping processes, reducing data errors by 25%
- • Implemented HR Compliance Program, reducing company risk substantially.
5 Returning to Workforce Resume Examples & Guide for 2024
Your returning to workforce resume should shine a spotlight on updated skills. Demonstrate your dedication to professional development with recent certifications or courses. Highlight experience relevant to the job you're seeking. Potential employers value consistent learning and application of knowledge, even after a break.
All resume examples in this guide
Traditional

Resume Guide
Styling your returning to workforce resume: layout and format, strategies for crafting your returning to workforce resume experience section, decoding the essence of your returning to workforce resume: hard and soft skills, highlighting your educational and certification milestones on your returning to workforce resume, should you add a summary or objective to your returning to workforce resume, enhancing your returning to workforce resume with additional sections, key takeaways.
One key challenge that individuals returning to the workforce often face is explaining gaps in their employment history on their resumes. Our guide can assist by providing strategies and examples to effectively frame these gaps as periods of growth and learning, turning potential negatives into positives.
Dive into our comprehensive guide to crafting a standout returning to workforce resume:
- Discover returning to workforce resume samples that have secured positions at top-tier companies.
- Master the aesthetics of your resume layout for maximum impact.
- Strategically present your achievements and skills across various resume sections.
- Convey to recruiters why you're the perfect fit for the job.
Recommended reads:
- No Degree resume
- EHS Specialist resume
- Solutions Engineer resume
- Senior Mechanical Engineer resume
- Fitness Trainer resume
Pondering the ideal length for your returning to workforce resume? Experts suggest keeping it between one and two pages. Opt for the two-page format if you boast over a decade of pertinent experience. Moreover, the resume format you choose is pivotal in showcasing your experience. Consider the:
- Reverse-chronological resume format to spotlight your career journey;
- Functional skill-based resume format if you're light on experience but want to emphasize skills;
- Hybrid resume format to provide recruiters a comprehensive view of both your experience and skills.
Here are some additional tips for your returning to workforce resume layout :
- Keep your headline straightforward: mention the job you're targeting, a notable certification abbreviation, or your professional specialty;
- Always customize your returning to workforce resume for the specific role, aligning job requirements with your experience in various resume sections;
- After finalizing your resume, save it as a PDF (unless instructed otherwise) to maintain its readability and layout consistency.
Upload your resume
Drop your resume here or choose a file . PDF & DOCX only. Max 2MB file size.
While color can enhance your returning to workforce resume by emphasizing key details like headlines, job titles, and degrees, moderation is key. Stick to a primary and a secondary color to maintain professionalism and avoid a cluttered appearance.
Essential components for your returning to workforce resume:
- Header: Feature your name prominently. If you have a notable degree or certification, append it next to your name. Include contact details, a link to your portfolio, and a concise headline.
- Summary or Objective: Align your professional trajectory and standout achievements with the desired role.
- Experience: Craft concise bullet points, highlighting tangible successes and contributions.
- Skills: Showcase them throughout your resume and consider a dedicated sidebar for emphasis.
- Education & Certifications: Reinforce your credibility and demonstrate your commitment to the industry.
What recruiters want to see on your resume:
- Relevant Skills: Ensure that your resume highlights the skills that are most relevant to the job you're applying for, especially if they were obtained or improved during your employment gap.
- Reason for Gap: If appropriate, briefly explain the reason for the break in your work history. Employers understand gaps for reasons like parental leave, studies, or other personal circumstances.
- Transferable Skills: Highlight any transferable skills you might have gained during your time away from the workforce. This could include volunteering, part-time jobs, freelancing, or even life experiences.
- Recent Training or Education: Indicate any training courses, certifications, or education you've undertaken during your time off. This shows a commitment to continuous learning and updating your skills.
- References: Include references who can vouch for your skills, reliability, and dedication to work, especially if they were connected to any activities you engaged in during your employment gap.
- What is the Purpose of a Resume
- Resume Layout
When detailing your returning to workforce resume experience , it's essential to pair responsibilities with tangible achievements.
Consider including:
- Key responsibilities, emphasizing their significance to your role, team, or organization.
- Experiences that have fostered your technical acumen or professional growth.
- Metrics that underscore your contributions and successes.
- Challenges you've addressed and the solutions you've implemented.
- Strategies you've devised and their measurable impact on growth.
Your experience section is pivotal in making a lasting impression on recruiters. To inspire you, we've curated real-world returning to workforce examples:
- Developed and implemented marketing strategies resulting in a 20% increase in customer acquisition for XYZ Company.
- Led a cross-functional team to successfully launch a new product, achieving a 15% market share within six months.
- Managed a budget of $1 million, optimizing spending and reducing costs by 10% while maintaining quality standards.
- Collaborated with stakeholders to streamline processes, improving efficiency by 25% and reducing project timelines by 20%.
- Conducted market research and competitor analysis, providing insights that drove the development of innovative solutions.
- Led a software development team in delivering high-quality products on time and within budget.
- Implemented Agile methodologies, resulting in a 30% improvement in team productivity.
- Developed scalable architecture for a web application, accommodating a tenfold increase in user traffic.
- Collaborated with stakeholders to define project requirements and specifications, ensuring alignment with business goals.
- Provided technical leadership and mentoring to junior developers, fostering their professional growth.
- Managed end-to-end recruitment process, resulting in a 20% decrease in time-to-hire.
- Developed and conducted training programs, enhancing employee performance and productivity by 15%.
- Implemented an employee engagement initiative, resulting in a 10% increase in overall employee satisfaction.
- Led performance management processes, including goal-setting, coaching, and performance evaluations.
- Collaborated with HR team to develop and implement policies and procedures aligned with company objectives.
- Managed a portfolio of high-net-worth clients, achieving a 15% growth in assets under management.
- Provided comprehensive financial planning services, resulting in a 20% increase in client satisfaction.
- Implemented investment strategies that outperformed the market, generating an average annual return of 12%.
- Collaborated with cross-functional teams to deliver customized wealth management solutions.
- Conducted regular portfolio reviews and made strategic adjustments to optimize client portfolios.
- Led a team of sales representatives, achieving a 25% increase in revenue within two years.
- Developed and implemented sales strategies resulting in new business acquisitions worth $2 million annually.
- Negotiated contracts with key clients, securing long-term partnerships and increasing market share.
- Trained and mentored sales staff, improving their product knowledge and sales closing skills.
- Analyzed market trends and customer feedback to identify opportunities for business growth.
- Developed and executed social media campaigns that increased brand awareness by 30% within six months.
- Managed influencer partnerships resulting in a 20% growth in online engagement and customer reach.
- Analyzed website analytics to optimize user experience, resulting in a 15% increase in conversion rate.
- Created engaging content across various digital platforms, driving organic traffic and customer engagement.
- Collaborated with cross-functional teams to develop and launch new digital products and features.
- Led a team of operations professionals, improving process efficiency and reducing costs by 10% annually.
- Implemented lean manufacturing principles resulting in a 20% increase in production output.
- Developed and monitored key performance indicators (KPIs) to drive operational excellence.
- Collaborated with suppliers to streamline the supply chain, reducing lead times by 15%.
- Implemented quality control measures, resulting in a 25% reduction in product defects.
- Managed end-to-end project lifecycle, delivering projects on time and within budget.
- Led a cross-functional team of engineers and designers, ensuring effective collaboration and communication.
- Implemented project management best practices resulting in a 30% improvement in project success rate.
- Developed and maintained strong relationships with clients, ensuring customer satisfaction and repeat business.
- Identified project risks and implemented mitigation strategies, minimizing project delays and cost overruns.
- Developed and executed comprehensive public relations campaigns, resulting in increased media coverage by 40%.
- Managed corporate communications, including press releases, speeches, and internal communications.
- Built and maintained strong relationships with key media outlets and industry influencers.
- Coordinated high-profile events and conferences, ensuring seamless execution and positive brand exposure.
- Monitored and analyzed media coverage, providing insights to inform PR strategy and messaging.
- Led a team of customer service representatives, achieving a 20% improvement in customer satisfaction ratings.
- Implemented training programs to enhance customer service skills resulting in a 15% reduction in customer complaints.
- Developed and implemented customer retention strategies, reducing churn rate by 10% annually.
- Collaborated with cross-functional teams to improve product features based on customer feedback.
- Implemented customer feedback mechanisms, resulting in a 25% increase in customer engagement.
Quantifying impact on your resume
- Include measurable achievements from previous roles, as numerical evidence can showcase your ability to deliver tangible results.
- Add any specific financial or budgetary responsibilities you had, demonstrating your fiscal management capabilities.
- Mention any quantifiable improvements made in efficiency or productivity, which indicates problem-solving skills and process optimization abilities.
- List the size of the teams you've managed, if applicable, to illustrate leadership and people management skills.
- Point out customer satisfaction scores or sales figures to reflect your customer service skills or sales acumen.
- Specify the number of projects you've successfully completed on time and within budget, highlighting project management proficiency.
- Detail the scale of operations you have overseen (for example, the volume of transactions or number of customers served), emphasizing your capacity to handle high-pressure situations.
- Note any significant reductions you've achieved in costs, errors, or turnaround times, implying your strategic thinking and effectiveness.
Writing your returning to workforce experience section without any real-world experience
Professionals, lacking experience, here's how to kick-start your returning to workforce career:
- Substitute experience with relevant knowledge and skills, vital for the returning to workforce role
- Highlight any relevant certifications and education - to showcase that you have the relevant technical training for the job
- Definitely include a professional portfolio of your work so far that could include university projects or ones you've done in your free time
- Have a big focus on your transferable skills to answer what further value you'd bring about as a candidate for the returning to workforce job
- Include an objective to highlight how you see your professional growth, as part of the company
- Resume Work Experience
- Resume Keywords
When detailing your career journey, there's no need to delve deep into early roles. Prioritize what resonates with recruiters. For senior positions, a decade-long retrospective can effectively illustrate your evolution.
Every job description communicates the desired hard and soft skills. These skills are the backbone of your application.
Hard skills are your tangible, technical proficiencies, often validated through certifications or hands-on experience. On the other hand, soft skills reflect your interpersonal abilities and how you navigate diverse work environments.
To effectively spotlight these skills on your resume:
- Create a distinct section for technical skills, listing the most relevant ones for the job.
- Highlight your strengths by weaving in achievements that underscore specific skills.
- Strike a balance between hard and soft skills to present a well-rounded profile.
- If multilingual, include a language proficiency section, emphasizing the interpersonal advantages it brings.
Stay tuned for a deep dive into the most in-demand hard and soft skills in the industry.
Top skills for your returning to workforce resume
Computer Literacy
MS Office Proficiency
Data Analysis
Project Management
Customer Service
Salesforce/CRM Experience
Digital Marketing
Research Abilities
Problem-Solving
Adaptability
Communication
Time Management
Positive Attitude
Self-Motivation
Decision Making
Conflict Resolution
Don't go all over the place with your skills section by listing all keywords/ buzzwords you see within the ad. Curate both hard and soft skills that are specific to your professional experience and help you stand out.
While skills alignment is increasingly prioritized, your educational background and certifications still play a pivotal role in establishing credibility.
To effectively present your academic and certification achievements:
- Detail your educational journey, including the institution and duration.
- Highlight recent and relevant certifications, showcasing your commitment to continuous learning.
- Be concise; focus on the skills and knowledge gained rather than exhaustive details.
- If a certification is in progress, mention the expected completion date.
Remember, authenticity is key. If a certification is pending, be transparent about it.
Best certifications to list on your resume
I'm sorry, but I can't generate the specific information you're asking for because the job title or field is missing here. The certifications that may be relevant will depend greatly on the specific job or career field in question. For example, returning to a career in IT would require vastly different certifications than returning to a career in healthcare or finance. Please provide a specific job title or career field for more accurate assistance.
If you're in the process of obtaining a certification listed in the job requirements but haven't completed it yet, be transparent. Mention your ongoing training and the expected completion date. Honesty is always the best policy on a resume.
- Deans List on Resume
- Coursework on Resume
Choose between:
- Resume summary to match job needs with your top wins.
- Resume objective to share your career goals.
Both should tell recruiters about your best moments. Keep them short, around five sentences. Check out our sample structures for guidance.
Resume summary and objective examples for a returning to workforce resume
- Seasoned IT professional with over 15 years of diversified experience, including a 5-year career break. Expertise in systems architecture and cloud computing. Recognized for leading a successful migration to a cloud-based system at TechGiant Corp.
- Multi-skilled HR Manager with a history of 10+ years in the industry before a 3-year pause. Proficient in talent acquisition and employee engagement strategies. Spearheaded a complete revamping of performance review methods at BlueBox Enterprises.
- Former Education Administrator pivoting to Human Resources Management after a 4-year hiatus from work-life. Demonstrates proficiency in personnel development from 8 years of experience in academic institutions. Initiated a comprehensive mentorship program serving over 100 staff members at HighPeak School District.
- Experienced Sales Consultant transitioning into Digital Marketing following a 2-year career gap. Previous 7-year tenure managing high-profile accounts brings an in-depth understanding of client needs. Successfully closed a multi-million dollar deal at GoldenEagle Inc.
- Driven candidate seeking to apply proven organizational skills and keen attention to detail in a Project Management role. Committed to efficiently meeting targets and contributing to team success despite no prior experience in the field.
- Aspiring Data Analyst eager to leverage strong quantitative background into practical business insights. Despite lack of previous experience in this specific sector, possesses a solid foundation in statistical analysis from academic coursework.
Make your returning to workforce resume truly distinctive by adding supplementary sections that showcase:
- Awards that underscore your industry recognition.
- Projects that bolster your application's relevance.
- Hobbies , if they can further your candidacy by revealing facets of your personality.
- Community involvement to highlight causes you champion.
- Format your returning to workforce resume for clarity and coherence, ensuring it aligns with the role.
- Highlight key sections (header, summary/objective, experience, skills, certifications) within your returning to workforce resume.
- Quantify achievements and align them with skills and job requirements.
- Feature both technical and personal skills across your resume for a balanced portrayal.
Looking to build your own Returning to Workforce resume?

- Resume Examples
Canadian Resume Format & How-to Guide for 2024
What is an unsolicited resume, the secret to finding keywords in job descriptions, why can’t i find a job the real reasons why you’re struggling to find one, changing job title on resume, what should you name your cover letter file.
- Create Resume
- Terms of Service
- Privacy Policy
- Cookie Preferences
- Resume Templates
- AI Resume Builder
- Resume Summary Generator
- Resume Formats
- Resume Checker
- Resume Skills
- How to Write a Resume
- Modern Resume Templates
- Simple Resume Templates
- Cover Letter Builder
- Cover Letter Examples
- Cover Letter Templates
- Cover Letter Formats
- How to Write a Cover Letter
- Resume Guides
- Cover Letter Guides
- Job Interview Guides
- Job Interview Questions
- Career Resources
- Meet our customers
- Career resources
- English (UK)
- French (FR)
- German (DE)
- Spanish (ES)
- Swedish (SE)
© 2024 . All rights reserved.
Made with love by people who care.
- Skip to primary navigation
- Skip to main content
- Skip to footer
4 Corner Resources
How to Create a Return to Work Resume (With Sample)
February 16, 2024 | Career Advice

If you’re returning to the workforce after time off, updating your resume should be your first priority. Your resume will help you get your foot in the door, showcase your skills, and convince hiring managers to pick up the phone and call you for an interview.
Follow these tips to create a resume for returning to work, and use the sample resume below for inspiration as you position yourself as a standout candidate.
What to Focus on in a Return to Work Resume
Prioritizing your strengths.
Your job-specific strengths should be showcased more prominently than your work experience if you’ve been out of the workforce for a long time. It’s vital to instantly convey to hiring managers how you’re qualified for the job they’re hiring for, which can be done by moving the skills section of your resume to the top or using a format that places less of an emphasis on previous jobs (more on this below).
Modernizing your old resume
Your resume from before you left the workforce probably has a lot of good material, and your prior experience is still relevant. There’s no need to trash it and build a new resume from scratch completely. Use your old resume as a starting point, then modernize it.
The professional world has changed significantly in the last several years. Resume design norms have evolved, as has the way companies hire. Your resume should be current for the year you’re applying and adjusted to the post-pandemic world.
Why Do You Need a Resume for a Return to Work?
It’s the first thing hiring managers see.
Your professionalism and charm might help you land the job… but first, you need to get the chance to exercise them by landing an interview. Your resume is one of the first things hiring managers see when you throw your hat in the ring for an open position, so getting it right is crucial to making a good first impression and breaking back into the workforce.
Highlight your transferable skills
Since you don’t have a current job for hiring managers to go on as a reference point, you need to help them see how your skills are relevant. What makes you qualified to do the job? Your resume connects your background from your prior career and the skills you developed during your time away from the workforce to the position you want now.
When Should You Use a Return to Work Resume?
Use this resume to:
- Return to work after taking time off
- Change careers after a gap in employment
- Build professional connections that will help you land a job
Common Return to Work Resume Challenges and How to Overcome Them
Accounting for a long gap in employment.
You have two options for handling a long employment gap on a resume. Your first option is to cite it directly by listing what you were doing during that time as an entry under experience, i.e., ‘stay-at-home mom.’ This makes certain hiring managers know the reason for the gap and may keep them from making negative assumptions. Your second option is to downplay your employment gap by making other sections of your resume more prominent or using an alternative format where employment is a secondary focus, like a functional resume.
Demonstrating impressive accomplishments
It’s much easier to show how you can make an impact on an organization if you have a recent track record of closing big deals or exceeding performance goals. Since you don’t have recent work accomplishments to show, however, you’ll need to sell yourself as a candidate in other ways. Use your resume to highlight achievements and qualifications you’ve gained in other non-work experiences, such as participating in volunteer work or completing a specialized training program.
Return to Work Resume Format and Key Components
A chronological, functional, or combination resume format is a good choice for returning to work.

Your resume should include these components:
- Contact information Begin with your name, address, phone number, and email address.
- Summary A summary section is useful for job seekers who are returning to work, acting as your “elevator pitch” for why you’re a great candidate. Use it to sum up one to two of your strongest skills and highlight what you’d bring to the specific position and company.
- Skills Zero in on a handful of your top hard and soft skills and list them in a prominent section. As often as possible, use skills that are mentioned as requirements in the job description. This will help your resume get noticed by hiring managers and automated applicant tracking systems used to screen candidates.
- Accomplishments Share your most noteworthy work achievements that are both measurable and related to the job you are applying for. It is important to show the hiring manager that you are results-driven and have a history of exceeding expectations.
- Education List your degree and the school(s) you attended.
- Experience List your work experience in reverse chronological order. If you’re using a functional resume format, group your experience or accomplishments by type–i.e., technical experience, leadership experience, etc. Under each item, give specific, detail-rich examples of your accomplishments in that position or area, citing numbers and quantifiable achievements as much as possible.
Polishing your resume is the first step toward restarting your career a break . Make sure you’re using a modern format, customizing the document for the specific job you’re seeking, and avoiding some of the most common resume mistakes .
Just because you haven’t worked in a traditional full-time job doesn’t mean you don’t have relevant experience. In addition to listing the jobs you held before leaving the workforce, state qualifications you’ve gained during other activities that have filled your time, like serving as a caregiver or managing your household finances.
A cover letter offers a little more leeway in terms of structure and content than a resume, which makes it an ideal place to explain an employment gap and position it in a positive light.
When you’re returning to work after a long break since your last job, consider using a functional resume format. This alternative format helps call the hiring manager’s attention to your relevant skills, particularly position-specific skills like technical expertise and management experience.
When you’re reentering the job market, you can absolutely include unpaid positions in the experience section of your resume. Show how these roles expanded your skill set, brought you valuable perspective or allowed you to contribute to a worthwhile cause.
Enjoying our articles? Get the latest straight to your inbox.

About Pete Newsome
Pete Newsome is the President of 4 Corner Resources, the staffing and recruiting firm he founded in 2005. 4 Corner is a member of the American Staffing Association and TechServe Alliance, and the top-rated staffing company in Central Florida. Recent awards and recognition include being named to Forbes’ Best Recruiting Firms in America, The Seminole 100, and The Golden 100. Pete also founded ze ngig , to offer comprehensive career advice, tools, and resources for students and professionals. He hosts two podcasts, Hire Calling and Finding Career Zen, and is blazing new trails in recruitment marketing with the latest artificial intelligence (AI) technology. C onnect with Pete on LinkedIn
Related Posts

Tips For Remote Employees Starting a New Job

14 Ways to Stand Out When Applying For a Job

The Best Jobs for Stay-At-Home Moms That Pay Well
Returns Specialist Resume Samples
The main duty of a Returns Specialist is to handle the complaints of the customers with regards to their product replacement or returns. While actual duties vary significantly based on the type of the organization and the role, the following are certain core and common duties of these specialists listed on the Returns Specialist Resume – listening to customer’s questions and concerns , providing answers and responses; providing information about products and services; taking orders and processing billing; reviewing and making changes; handling returns and complaints , and escalating the issue to the supervisors as needed.
To work at this capacity, the following skills are needed – the ability to communicate well with all types of customers, knowledge of handling tough or angry customers; professionalism and work ethics, and familiarity in using live chat, email, or face-to-face modes to communicate with customers. Formal education is not a must, however, possessing strong product knowledge is crucial.

- Resume Samples
- Returns Specialist
Returns Specialist Resume
Objective : Seeking a Returns Specialist position with an outstanding career opportunity that will offer a rewarding work environment along with a winning team that will fully utilize management skills.
Skills : Inventory Management, Shipping, Receiving, Custodial, Light Maintenance.

Description :
- Coordinated return products from a variety of customers and locations with differing return shipment methods.
- Worked timely with customers to ensure fullest satisfaction Financial Recovery from carriers/ logistic business partners due to negligence Customer Support working fluidly with customer's needs and wants to ensure products received are viable for the needed purpose including explanation and training with the customer.
- Maintained weekly/monthly Spread Sheets on return data in Excel for constant availability and breakdown of cost center to reroute revenue as much as possible.
- Separated employment due to relocation.
- Assessed RMA requests submitted by customers in accordance with Cisco Meraki's 30 or 60-day return policy -Notified sales reps regarding the large net.
- Ensured efficient and timely order and case completion Responsible for prioritizing individual workload according to client priority.
- Balanced Interstate banking accounts Researched and determined the reason for rejected items Corrected rejected items by inputting correct.
Objective : To obtain a challenging and responsible position within a company where I can apply my educational knowledge and professional experience in administrative assistance and customer service/human resources, while providing quality, value, and growth for both my career as well as for the company.
Skills : Great Organization , Quick To Assess Situations, Quick Learner, And I Stride In Multitasking.

- Responsible for up to 3 different jobs at a time.
- Returned all product that comes back from the schools, stores, companies, etc.
- Reported records for orders according to guidelines set forth by company rules Ensures adherence to state-specific restrictions as well as general.
- Processed customer returns Skills Used Computer knowledge.
- Processed customer returns according to company policies.
- Inspected product to determine if it should be scrapped or returned back to inventory.
- Worked with manufacturers and vendors to obtain authorization for returns Managed returning products in a timely manner and obtaining credits.
Objective : Motivated and highly productive Returns Specialist professional with a return specialist background. Detail-oriented with strong skills in multi-tasking and efficient management of day-to-day office operations. Adept at building and maintaining effective working relationships with co-workers and outstanding interpersonal skills.
Skills : MS Office, Order Management, Communication Skills.

- Responsible for all problems that may arise in regards to customer's purchase of new contacts, lenses, or frames.
- Processed returned products from our customers.
- Issued RMA numbers to customers for optical merchandise that had been purchased through the online website.
- Verified electronic client files to ensure they balanced to invoices.
- Placed new orders for new products for customers.
- Processed refund requests and payment corrections.
- Created excel charts of daily inputs and outputs.
Summary : Returns specialist is responsible for assisting and/or managing customers with returns and other service issues. Provide customer service, product and technical support to customers on the return process.
Skills : Customer Service Skills, Management Skills, Inventory Manager.

- Answered all emails that came to the FramesDirect returns department through the website.
- Earned consistent commendations for exemplary service delivery.
- Collect all returns items Open package/inspect item Decide whether it can be fixed or replaced Fixed- send to jeweler department Replaced-check.
- Assisted with sourcing strategy recommendations for client pharmaceutical purchasing.
- Provided services including project management, account maintenance, records management and invoicing.
- Prepared and submitted detailed reports to pharmaceutical manufacturers, and process refunds for client accounts.
- Adjusted customers' accounts in the database.
Objective : Seeking a challenging Returns Specialist position where my proven skills of analysis, research, client relations and communication will enable me to define new opportunities. Desire career growth based on performance and accomplishments.
Skills : Time Management, Interpersonal Skills, Coordination Skills.

- Inspected guns, accessories, and other sporting goods.
- Started with processing returns from customers and providing customer service on the phone for the catalog side of the business, processed incoming.
- Processed e-commerce, retail and gift returns/exchanges using SAP and CRM technologies Consistently exceeded 80% CSAT and 85% NPS Assisted on phones.
- Resolved service issues in a timely manner, including coordinating and processing returns.
- Identified and resolved system and account issues.
- Processed confidential information.
- Received incoming shipments and reviewed contents against purchase order for accuracy.
Objective : Hardworking, organized, Returns Specialist professional with a proven background delivering sensible return specialist technology solutions on time and under budget while working as a team member or team leader.
Skills : Bilingual, Organized, Multitask, Communication Skills.

- Attached return labels that identify the items.
- Put items in proper warehouse location using the order picker lift and barcode scanner.
- Picked items from various warehouse locations with order picker and barcode scanner.
- Oversaw all RAs including authorizing product returns to shipment of repaired/replaced product or issuance of corresponding credit memos.
- Coordinated product returns from customers, field locations, and wholesale partners.
- Tasked with working with an RK customer to disposition an RMA appliance inventory that had built up during the previous year (approximately 500 units.
- Assisted with Inventory Cycle Counts and reconciliation, pulling of orders, and checking in the new products.
Objective : As a Returns Specialist, responsible for Recording information pertaining to merchandise to be returned to manufacturer because of defects, wrong amount, or type by performing the following duties, etc,.
Skills : Microsoft Office, Verbal Communication, Written Communication.

- Responsible for high volume quoting of standard catalog products, custom modifications, and freight quotations via phone, email, and fax.
- Coordinated with order entry, accounts receivable, engineering, purchasing, and shipping for special quoting and ordering conditions.
- Processed order status requests, expedites, cancellations, credits, debit memos, no change orders, freight invoice issues, and literature requests.
- Managed and distributed all incoming email inquiries from the company's primary email address.
- Helped develop a new customer service manual with work instructions.
- Helped train new customer service personnel.
- Drafted a floor location plan of over 37,000 square feet for a warehouse location move of over 10,000 units.
Headline : As a Returns Specialist, responsible for coordination of key details associated with: Core Returns, Special Returns, Warranty Returns Annual Returns as well as other special projects as assigned by the Inventory Manager, etc,.
Skills : Microsoft Word, Customer Service Skills, Inventory Control.

- Handled the day-to-day RMA Receiving activities and process product returns.
- Maintained, reviewed and updated process documentation on a regular basis; Created new documents as required.
- Entered data, analyzed data, and identified trends in repair and replacement requests.
- Processed, categorized, and answered customer emails and telephone calls, providing high-quality service.
- Compared merchandise invoices to items actually received to ensure that shipments are correct.
- Received orders and unloaded the packages from the truck and placed it properly in the warehouse using forklift Maintained the work environment.
- Maintained and updated filing, inventory, mailing, and database systems, either manually or using a computer.
Objective : Returns Specialist with 5 years of experience in processing customer return authorizations, shipping replacement product, and ensuring that product is received back to Nx Stage in a timely manner, etc,.
Skills : MS Office, Data Entry, Communication Skills, Management Skills.

- Researched root cause of issues relating to the quality or incorrect product and issue awareness reports to appropriate staff.
- Authorized returns for repair, replacement, or credit.
- Assisted quality manager with reports and process improvements along with special projects as requested.
- Assisted customers on returning and or replacing their merchandise Customer service which includes helping with payment arrangements and customer.
- Processed and documented, returned items, and resolve customer complaints with their returned products.
- Operated computers to administer refunds to customers Assisted managers with laundry duties such as operating driers and washers Provided assistance.
- Processed returns and inspected unordered and non-saleable merchandise.
Objective : As a Returns Specialist, responsible for Managing the core return process from the Distribution Center to the Supplier, etc,.
Skills : Microsoft Office, Forklift Operator, Cash Register, Cash Handling.

- Received customers' merchandise and input it into their account.
- Placed orders for customers depending on their or their company's request.
- Dealt with customer's payment via credit card or company credit.
- Assisted in all departments where needed.
- Assisted inscriber, packing, and inventory.
- Scanned their inventory database using a handheld device.
- Maintained appropriate levels of inventory at all times.
- Followed established criteria to identify and report all shortages, damages, and defects of received goods.
Recent Posts
Download this pdf template., creating an account is free and takes five seconds. you'll get access to the pdf version of this resume template., choose an option., unlock the power of over 10,000 resume samples., take your job search to the next level with our extensive collection of 10,000+ resume samples. find inspiration for your own resume and gain a competitive edge in your job search., get hired faster with resume assistant., make your resume shine with our resume assistant. you'll receive a real-time score as you edit, helping you to optimize your skills, experience, and achievements for the role you want., get noticed with resume templates that beat the ats., get past the resume screeners with ease using our optimized templates. our professional designs are tailored to beat the ats and help you land your dream job..
Returns Specialist Resume Example & Writing Guide
Use this Returns Specialist resume example and guide to improve your career and write a powerful resume that will separate you from the competition.

Specialists are highly skilled professionals who focus on one area of expertise. They’re often hired because of their deep knowledge of a particular industry or subject matter, and they’re usually tasked with implementing their expertise to help an organization achieve its goals.
Because they’re so specialized, specialists tend to have fewer job opportunities than generalists. But if you love what you do and are good at it, working as a specialist can be incredibly rewarding—and lucrative.
Before you can land that dream job as a specialist, though, you need a compelling resume that will convince hiring managers that you’re the right person for the job. Follow these tips and resume example to write a specialist resume that hiring managers will love.
Highly organized and efficient returns specialist with more than 10 years of experience in the retail industry. Proven ability to handle customer inquiries and resolve product issues in a timely and satisfactory manner. Passionate about providing excellent customer service and ensuring a positive shopping experience for customers.
- Processed returns and exchanges, processed payments, assisted customers with questions regarding orders or account information.
- Maintained knowledge of all company policies and procedures related to Returns/Exchanges and Merchandise Credit transactions.
- Assisted in training new hires on the job responsibilities, processes, and workflows within the department.
- Communicated effectively with internal departments including Shipping & Receiving, Accounting, Marketing, etc., as well as external vendors such as delivery companies for shipping purposes.
- Performed other duties assigned by management that support overall store operations during business hours (e.g., merchandising projects).
- Created a database of over 1,000 customers to track their purchases and preferences for targeted marketing campaigns
- Answered customer questions about products and services via email or phone calls; resolved issues as needed
- Maintained inventory levels by tracking sales trends and ordering new product when necessary
- Improved the quality of service by identifying common problems through data analysis (i.e., shipping errors)
- Achieved 95% satisfaction rating from customers surveyed after receiving assistance
- Generated new leads through cold calling, in-person networking, and lead management software
- Managed a territory which included the sale of residential HVAC systems and services to homeowners and business owners within an 8 county area
- Successfully reached sales goals by developing long term relationships with customers including follow up calls
- Certified Fraud Examiner (CFE)
- Certified Internal Auditor (CIA)
- Certified Information Systems Auditor (CISA)
Industry Knowledge: Fraud Management, Fraud Scoring, Call Blocking, Collections, Automated Dispute Resolution, Credit Review, Telemarketing, Collections, Credit Inquiries, FICO Scores Technical Skills: LexisNexis, Experian, Equifax, TransUnion Soft Skills: Communication, Customer Service, Problem Solving, Decision Making, Teamwork, Conflict Resolution
How to Write a Returns Specialist Resume
Here’s how to write a resume of your own.
Write Compelling Bullet Points
Bullet points are the most important part of your resume because they’re the first thing recruiters will read. And since they’re so important, it’s crucial that you use them to your advantage by crafting clear, concise bullet points that highlight your experience and skills.
For example, rather than saying you “provided customer service for customers over the phone,” you could say you “provided customer service for more than 100 customers daily, resolving issues and answering questions on behalf of company.”
The second bullet point is much stronger because it provides specific details about the nature of your work and the number of people you worked with.
Identify and Include Relevant Keywords
When you apply for a job as a returns specialist, your resume will likely be scanned by an applicant tracking system (ATS) for certain keywords. These programs look for keywords related to the job like “package tracking” or “sorting” in order to determine whether you are a good fit for the role. If your resume doesn’t have enough of the right keywords, your application might not make it past the initial screening process.
To increase your chances of getting an interview, make sure to include relevant keywords throughout your resume. You can include them in the work experience, skills, summary, and education sections. Here are some of the most commonly used returns specialist keywords:
- Returns Management
- Returns Process
- Logistics Management
- Inventory Management
- Inventory Control
- Operations Management
- Customer Satisfaction
- Team Building
- Shipping & Receiving
- Customer Service
- Negotiation
- Supply Chain Management
- Team Leadership
- Customer-focused Service
- Microsoft Access
- Shipping Management
- Business Process Improvement
- Business Planning
- Strategic Planning
- Cross-functional Team Leadership
- Management Information Systems (MIS)
- SAP Products
- Customer Relationship Management (CRM)
- Sales Management
- Analytical Skills
Showcase Your Technical Skills
As a returns specialist, you need to be proficient in the use of various software programs and systems in order to process returns efficiently. Some of the most commonly used programs are SAP, Oracle, and Microsoft Dynamics. You should also be familiar with the return policies of the company you are working for, as well as any relevant laws and regulations.
Network Infrastructure Engineer Resume Example & Writing Guide
Picu nurse resume example & writing guide, you may also be interested in..., data entry associate resume example & writing guide, home depot department supervisor resume example & writing guide, options trader resume example & writing guide, notary public resume example & writing guide.
- Returner Resources
- Find a Returnship
- Inspiring Stories
- Returnship Success Guide
- FAQ: What Are Returnships?
- Why Returnships
- Build your Returnship
- Meet the Talent
- Market your Program
- How We Help
- Why It Matters
- Ways to Give
- Mother’s Monday
Recommended Resume Formats for Returners (With Templates)

Here at Path Forward, we receive a lot of questions about resumes. While the answers to each of these questions differs from case to case, there are a few fundamental principles that remain consistent in how you present yourself and your work:
1. The resume is a marketing tool that is meant to showcase your relevant work experience (including unpaid work), degrees, and certifications to make the case that you are qualified for the position you are applying for.
2. A best practice is to individually tailor your resume to each job that you apply to. Cross reference your resume against the job description and ensure that your direct or transferable experience is clear. (You can use online tools like Jobscan to help you). At the bare minimum, you should have different versions of your resume that you can plug in for different types of roles you are seeking.
3. Language matters. When listing past deliverables and responsibilities, use action words and highlight your individual accomplishments and contributions.
Yet, even with these rules, there is still some nuance in how to present your work experience. We’ve put together four templates to act as a starting point for returners who need to create (or revamp) their current resume.
Click here to download a zip file containing a Microsoft Word template for each of the following.
Chronological Template
The chronological resume is the most commonly used format for traditional candidates. In this format, work experience is displayed from current or most recent role(s) to previous experience in reverse chronological order. This template is ideal for those with relatively linear experience and clear career progression.
Functional Template
The functional resume is formatted to highlight specific skills rather than list work experience in the order that it happened. This format is perfect for those with career gaps and/or attempting to pivot careers.
Tech Template
Displaying tech experience requires a different approach than corporate experience. Use this format to showcase the languages you’ve learned, the skills that you’ve developed, and links to any projects or portfolios.
Returnship Template
When applying to a return-to-work program offered by Path Forward’s employer partners , a career gap is an eligibility requirement. Make sure to clearly list the break with as much or as little details as you feel comfortable sharing. Underneath, you can list volunteer or other unpaid work experience as long as it is clearly noted as such.
Additional resources:
- How to Create Your Comeback Resume [recorded webinar]
- How to Represent Your Career Gap on Your Returnship Resume (With Example)
- Revamping Your Resume [recorded webinar]
- Teal Resume Builder
Article and templates created by the Path Forward Programs Team.
How to Create a Professional Return to Workforce Resume
- ')" data-event="social share" data-info="Pinterest" aria-label="Share on Pinterest">
- ')" data-event="social share" data-info="Reddit" aria-label="Share on Reddit">
- ')" data-event="social share" data-info="Flipboard" aria-label="Share on Flipboard">
The Disadvantages of a Functional Resume
Resume sample for a long-term employee, how to format a header for a two page resume.
- Can You List Too Many Responsibilities on Your Resume?
- Summary of Qualifications vs. Core Competencies
So you're preparing to re-enter the workforce after an extended absence – one that would stand out and prompt an inquiry from someone reading a chronological resume. As much as you may dread the thought of dusting off and updating your most recent resume, you're actually facing a golden opportunity: You're not going to merely update your old resume; you're going to start all over and prepare a functional resume that should prompt job offers instead. Job recruiters often bemoan the fact that chronological resumes often succeed at telling them where a candidate has worked but fail to tell them what a candidate can do. That's where your new, improved and arguably superior functional resume will stand out – and help you land a job worth boasting about.
Launching Your “Back-to-Work Resume”
Chronological resumes may be the norm – at least for people who have steady, ongoing work experience. The format can serve them well because it lists job experiences in reverse chronological order – starting with the most recent and moving backward. A functional resume groups your skills, strengths and experiences, both professional and personal, in categories, Resume Genius says. Some tips should help you get started:
- Start thinking, right now, in terms of categories. A “skills” category will be the most important. You may wish to separate “professional skills” from “interpersonal skills” and even add categories that will impress recruiters, such as “computer skills,” “salesmanship skills” or “project management skills.”
- For ideas, look up “re-entering the workforce resume examples.” Other categories might include “professional experience,” “education,” “memberships” and “other accomplishments.” A functional resume should literally function in your best interests.
- You'll need a place to put all these categories, as well as three bullet points beneath each one. (Three is generally agreed to be a “good” number because one or two bullet points don't seem to be enough to justify a separate category.) So use a large (11-by-17-inch) piece of paper or even a white board. You'll have room to scratch out and add words as you go before you assign your final draft to a computer document.
- Approach your “returning to the workforce” resume as a project that you can finesse over at least several days. Let it “go cold” overnight, review it again the next day and make changes.
- Expect a little mess along the way – maybe even a lot of mess. You're in “creation mode,” and every bit of “mess” suggests you're making progress.
Watch Your Back-to-Work Resume Soar
It may take a load off your mind to know that you should explain the gap in your employment in your cover letter, not on your resume, Indeed says. Be honest, but don't feel compelled to go into painstaking detail, either. Saying that you took time off to tend to “family issues” should suffice. Be sure to express your enthusiasm for returning to the workforce, too.
Now that you're ready to dive into creating a first draft, leave ample room at the top of your paper or board for your contact information, or at least your name, phone number and email address. (It's up to you whether to include your home address. These days, more people are leaving it off.) Experiment with centering this information or casting it to the right or left, but your name should be the dominant element.
Now draw a vertical line down the page or board, devoting about three-quarters to the right side and about one-quarter to the left. Most readers gravitate to the right side of a page, which is where you're going to place your all-important “skills” section. But first, top the right side with a “professional summary” statement. This one- or two-sentence statement should tell a recruiter the type of position you seek and what you would bring to it, Columbia University says. For example, without using the word “I,” a corporate trainer might say:
- High-energy, former teacher with impeccable references seeks challenging training role in either a corporate or nonprofit environment.
Finish Your Back-to-Work Resume
The “skills” section should be the most illuminating section of your functional resume; it definitely will consume the majority of the “real estate.” Ideally, you'll have come up with at least three skills categories (those professional, interpersonal, computer, salesmanship and project management skills). You'll know you have picked a winning category when you can write at least three bulleted sentences under each one, drawing from your past professional and personal experiences. Many people rack their brains to round out skills sections – not just people who have been out of the workforce for a while. So it may be time to dust off your most previous resume to jog your memory – or even place calls to former colleagues for help. (Make the most of these calls by asking if you may use them as a reference, too.)
The left side of your resume may be the “easier” side to complete, but it may also feel like more of a puzzle as you try to prioritize which category should come first and say all you wish to say under each one. In general, it makes sense to place “professional experience” at the top, followed by “education” and then any other categories you deem important to your job search.
In the end, you may be so pleased with your functional resume that you may use it from this point on – pitching the idea of a chronological resume altogether. It's an idea worth mulling – as soon as you're done celebrating your return to the workforce.
- Resume Genius: Functional Resume: Template, Examples, and Writing Guide
- Indeed: How to Write a Re-Entering the Workforce Resume (With Template and Examples)
- Columbia University Center for Career Education: How to Write a Resume Profile or Summary Statement
- Set up a separate email account for your job search. Steer clear of “cutesy” names, opting instead for [email protected].
- Re-familiarize yourself with your field. Things constantly change, and the industry you left probably isn’t the same as it was when you last worked in it. Set aside some time to study up on any developments that took place during your absence. For example, marketers need to be aware of all the marketing advances resulting from the Internet, such as inbound marketing, social media marketing, content marketing and location-based marketing.
Mary Wroblewski earned a master'sdegree with high honors in communications and has worked as areporter and editor in two Chicago newsrooms. She launched her ownsmall business, which specialized in assisting small business ownerswith “all things marketing” – from drafting a marketing planand writing website copy to crafting media plans and developing emailcampaigns. Mary writes extensively about small business issues, andespecially “all things marketing.”
Related Articles
How to show multiple roles in the same job on a resume, how to make a resume in adobe photoshop, do i put my high school on an application, how to summarize work experiences on resumes after long absences, how to submit a resume professionally, how to create a master list of resume information for yourself, how to format a resume that goes on to a second page, how to deal with varied experience on your resume, what type of paper should a resume be printed on, most popular.
- 1 How to Show Multiple Roles in the Same Job on a Resume
- 2 How to Make a Resume in Adobe Photoshop
- 3 Do I Put My High School on an Application?
- 4 How to Summarize Work Experiences on Resumes After Long Absences
Resume Builder
- Resume Experts
- Search Jobs
- Search for Talent
- Employer Branding
- Outplacement
- Resume Samples
- Administrative
Claims Specialist Resume Samples
The guide to resume tailoring.
Guide the recruiter to the conclusion that you are the best candidate for the claims specialist job. It’s actually very simple. Tailor your resume by picking relevant responsibilities from the examples below and then add your accomplishments. This way, you can position yourself in the best way to get hired.
Craft your perfect resume by picking job responsibilities written by professional recruiters
Pick from the thousands of curated job responsibilities used by the leading companies, tailor your resume & cover letter with wording that best fits for each job you apply.
Create a Resume in Minutes with Professional Resume Templates
- Researching and providing technical assistance to contracted service providers, Division staff and other external entities relating to claims processing
- Assemble data, analyze performance, identify problems and develop recommendations to support Project Management planning and operations
- Develop a professional working relationship with the Client, on-site field investigators, technicians, management team and other personnel
- Support Claims Management in establishing departmental objectives and procedures to provide direction to claims team
- Performs liaison services to both internal and external customers providing assistance in claims
- Make outbound calls to carrier, injured employee & health care providers to obtain work status and case notes
- Performs quality assurance audits APD claims files to measure quality, provide feedback and develop employees
- Good problem solving and decision making abilities
- Focusing on financial impact of claims and actively pursues opportunities to enhance unemployment results and impact unemployment tax rates
- Researches partner separations and builds claim responses; ensures the timely, courteous and professional follow up to incoming phone calls, and emails
- Reviews and updates cases for completion, accuracy, routing and resolution
- Develops effective working relationships with customers, team members, Starbucks partners, and other Starbucks organizations
- Effectively manages multiple cases, following up with customers, vendors, etc. to ensure a timely and satisfactory resolution
- Ensures that work is accurate and complete, processed in a timely manner with proper spelling and grammar
- Provides plan and claim information, assists with submission of claims, and makes outbound calls to gather missing information on incomplete claims
- Participate in the development of policies and procedures to improve department workflow and the claims process ensuring proper documentation
- Manage return to work with the Return to Work Coordinator
- Provides claim information, assists with submission of claims and makes outbound calls to gather missing information on incomplete claims
- Collaboratively work with a network of approved in-house professionals and monitoring the progress of a claim
- Advise clients of their claim related obligations under the policy and establish client-specific claims management procedures
- Monitors and improves the performance of trading partner’s services for your clients
- Knowledge of diagnosis and procedure codes, general medical terminology, and disability duration guidelines
- Strong communication, negotiation and presentation skills. Ability to effectively interact with all levels of CNA's internal and external business partners
- Manage an inventory of claims to evaluate compensability/liability
- Detail oriented/ability to follow client specific guidelines
- Knowledge of all types of professional claims
- Solid knowledge of claims and insurance theory and practices
- Strong interpersonal and communication skills. Ability to effectively interact with all levels of CNA’s internal and external business partners
- Solid knowledge of claims and insurance industry theory and practices
- Solid knowledge of Microsoft Office Suite as well as other business-related software
- Knowledgeable in MS Word and MS Excel
15 Claims Specialist resume templates

Read our complete resume writing guides
How to tailor your resume, how to make a resume, how to mention achievements, work experience in resume, 50+ skills to put on a resume, how and why put hobbies, top 22 fonts for your resume, 50 best resume tips, 200+ action words to use, internship resume, killer resume summary, write a resume objective, what to put on a resume, how long should a resume be, the best resume format, how to list education, cv vs. resume: the difference, include contact information, resume format pdf vs word, how to write a student resume, life & specialty claims specialist resume examples & samples.
- Minimum 2 years of direct claims experience
- Working towards an insurance industry designation (at minimum 1 course completed)
- Experience in effectively managing complex claims
- Bilingualism in French and English, written and spoken considered an asset
Senior Claims Specialist Resume Examples & Samples
- Evaluate claims, provide support information and recommend authorization decisions to the VP Risk Management
- Oversee claim data management, principally in a digital environment
- Performs other assignments and projects as requested
Title Claims Specialist Resume Examples & Samples
- Two to three years of experience in loan processing and closing activities
- Two to three years of experience applying general accounting principles
- Strong knowledge of loan processing and closing policies and procedures
- Well-developed ability to manage multiple tasks/projects and deadlines simultaneously
- 5+years claims experience
- High School diploma required, degree preferred
- Ability to create the most complex and successful strategies for risk mitigation
- Knowledge of claim handling & claim adjudication processes and procedures
- Understand the basic process and value of basic data analytics and benchmarking
- Ability to communicate technical information orally and in writing
- Travel required
Claims Specialist Resume Examples & Samples
- Claims adjudication experience
- Ability to multi-task Manages time effectively
- Committed to superior customer servicing
- Ability to work independently, a self- starter
- 3 – 5 years claims adjudication experience
- College preferred, or equivalent work experience
- Review information contained on the initiation system and set up new claims into the claims system according to the terms of the plan purchased
- Set adequate reserves to ensure proper reporting
- Verifies travel insurance coverage utilizing various methods e.g., computer, fax, manifest, e-mail or telephone
- Provide insurance verification of coverage for the assistance companies
- Mails out appropriate claim forms, letters and related correspondence
- Cultivates relationships with individuals at tour operators and cruise lines in order to obtain the necessary claim information
- Assists with incoming electronic correspondence
- Assists with opening and prepping the daily mail
- Assists as needed with Scanning documentation and pertinent information to AS400 IMS/21 document system individually or batch mode
- Liaison with Customer Service and assists with phone calls
- Assists Claims Examiners with claims adjudication
- Generates letter requests for the Claims Specialist II
- Follows up on outstanding medical records requests
- 2-3 years of work experience in an office environment
- General office skills including data entry
- 3+ years of directly related industry experience
- Experience in reading and understanding UB04 and HCFA forms
- Experience in Workman’s Compensation and Motor Vehicle Claims processing
- Solid negotiation and analytical skills
- Manages the appropriate level of resources for your clients
- Displays a visible sign of professionalism and direction for the practice
- Maintains local relationships with all major trading partners
- Participates in meetings and provides ideas and strategies that strengthen the practice
- Ensures quality and consistency in executing best practices
- Partners with others as necessary to continually improve quality and innovation of group
- Monitors the performance of trading partner’s services for your clients
- Ensures practice strategy alignment with Willis business plans
- Maintains direct relationships with key clients
Supplemental Rent Claims Specialist Resume Examples & Samples
- Logs and initiates all customer claims
- Reviews customer claim documentation for completeness and works with customers to resolve shortfalls, as necessary
- Customer’s first point of contact within GECAS for all claim related queries
- Identify and collate relevant contractual obligations to support maintenance event claims
- Interpretation of contractual maintenance and AD cost sharing formulae
- Administer all lessor contributions, including budgetary approval
- Monitor claims process to ensure cycle time targets are achieved
- Serves as a focal point for all queries relating to customer claims
- Undertake claims assessment and reporting to support GECAS sales activity and serviced entity queries
- Provides on-going analysis and reporting to support other functions and project related work
- Supports Claim Manager by leading face-to-face customer meetings to plan maintenance, work-scopes and claims
- Professional Engineering, Financial or Business degree
- Demonstrated experience in the interpretation of contractual language
- Experience in and an understanding of work-scope documentation and shop visit reports
- Demonstrated capability in developing and maintaining good working relationships, at all functional levels, within customer airlines
- Strong system and computer skills
- Aviation industry experience
- Working knowledge of operating lease structures
- Ability to manage multiple tasks and to prioritise
- Good communication skills - written and spoken
- Commitment to preserving confidentiality
- Must be available to work overtime and/or weekends depending on business needs
- Proficiency in all Microsoft Office Programs, including Word, PowerPoint, Excel, and Access
- Bachelor's Degree in a related field
- Knowledge of order to cash
- Knowledge of SAP navigation & logic
- 8-10+ years experience in multi-jurisdictional claims handling or related work with an insurance service provider and/or preferably in a large, multi-location corporation (an insured)
- General liability claims experience required, preferably for entertainment, sports, hospitality, retail or similar accounts with customer-intensive claims
- Experience with litigated claims having multiple defendants and complex, 3rd-party contract elements required; must be conversant with legal environment and legal system procedures
- Analytical skills necessary to obtain and evaluate complex information, analyze problems, develop alternative solutions, and project long-term effects of decisions
- Ability to effectively prioritize, organize, and perform multiple tasks with strict deadlines
- Ability to develop relationships and work collaboratively with project teams
- Strong Microsoft Office skills required; demonstrated competency in Excel
- Proficiency in commonly used claims information data base systems
- College degree and/or equivalent experience required
- Applicable insurance/claims certifications and licenses a plus
Unemployment Claims Specialist Resume Examples & Samples
- Provides coaching and guidance to regional partner resource generalists, district managers, and store managers on the interpretation of Starbucks unemployment, policies and procedures
- Analyzes and investigates partner separations in consultation with others in Partner Resources, external contacts or other departments outside PRO Solutions & Services
- Provides strong customer service by effectively managing customer expectations while meeting customer needs
- Maintains current knowledge on state to state unemployment processes, Partner Resources policies, procedures and best practices
- Participates in cross-functional teams to successfully execute programs and projects
- Performs research and analysis to maintain expertise in specialized state unemployment policies, laws and regulations
- Customer service (2 years)
- General human resources (2 years)
- Case management (2 years)
- Ability to conduct independent research and analysis
- Proficient in Microsoft Office Suite (Word, Excel, PowerPoint, Visio, Microsoft Project)
- Ability to work in a fast-paced and changing environment
- Ability to work both independently and as a member of a team
- Knowledge of SAP (production environment) or similar software
Contestation / Claims Specialist Resume Examples & Samples
- Experience with claims adjudication processes and identifying claim overpayment errors for inpatient and outpatient providers
- Prior experience with claims adjudication processes for a healthcare organization or managed care provider
- Ability to analyze paid claims and review reports to identify discrepancies for contesting/appealing according to established procedures
- Ensure correctness of delivery systems, participating providers, and contractual arrangements per market
- Effective communication verbally and written
- Experience in analyzing and reporting large volumes of data
- Microsoft Office using Access, Excel, Word, and Power Point
- Understanding of Current Procedural Terminology (CPT) codes, ICD- 9CM, ICD-10CM, Ambulatory Surgical Center (ASC) groupers, and Diagnosis Related Groups (DRG) and managed care
- Knowledge of Centers for Medicare and Medicaid Services (CMS) guidelines
- Self-motivated creative and analytical background
- Understanding of multiple health plans claims data files, i.e. Humana service fund reports
- 5 +plus years of understanding health care claims processes and systems
- Experience with understanding Medicare and Medicaid Risk models
- Extensive experience of handling claims of a complex nature
- Helps develop and execute the strategies of the practice - leading full team (including Risk Control Consultant and Data Analyst) on creating strategy for larger accounts
- Handles complaints, arbitrates disputes and negotiates alternative solutions
- Consults with clients to help mitigate their risk
- Support new business with sales presentations and RFP
- Monitor the performance of trading partner’s services for your clients
- Ensure appropriate program design and documentation - service scope aligns
- Ensure support for business lines (lab and business) by evaluating and validating communications for products
- Evaluate regulatory and media risks of claims along with different products communication aids
- Help identify and report product communication issues
- Education : Minimum BA or BS
- Years of working experience : 0 to 3 years
- Experience : Lab or regulatory experiences
- Language : English
- Other skills : Interpersonal skills
- Reconcile claims filed to payments received on Investor and Mortgage insurance claims
- Prepare claim payment reconciliation to ensure full payment is received
- Create and update charge removal payments balancing to claims payments received
- Determine root cause of curtailed items and determine whether supplemental claim, client expense, or loss has been incurred
- Follow up on claim payment status for unpaid, filed claims
- Update the system with pending, submitted, withdrawn, and paid claim information
- Recommend improvements to established procedures and processes
- Analytical Thinking: The ability to tackle a problem by using a logical, systematic, sequential approach
- Diagnostic Information Gathering: The ability to identify the information needed to clarify a situation, seek that information from appropriate sources, and use skillful questioning to draw out the information when others are reluctant to disclose it
- Personal Credibility: Demonstrated concern that one be perceived as responsible, reliable, and trustworthy
- Stress Management: The ability to keep functioning effectively when under pressure and maintain self control in the face of hostility or provocation
- Coordinate and oversee claims management strategies on reserving, settlement and closure to bring claims to resolution
- Communicate and go on-site as necessary to all NJ warehouses to assist with all internal claims management activities
- Participate and manage quarterly claims reviews with the TPA for managed claims
- Develop and Monitor goals for claim mitigation within stores
- Act as an internal resource for Workers’ Compensation questions
- Utilizes TPA RMIS system for claims management
- Help develop and execute the strategies of the practice - leading full team (including Risk Control
- Consultant and Data Analyst) on creating strategy for larger account
- Handles complaints, arbitrates disputes, and negotiates alternative solutions
- Consults with client to help mitigate their WC risk
- Ensure TPA/Carrier performance through claim reviews, audits, etc
- 3+years claims experience
- Degree required
- Knowledge of workers compensation claim handling & claim adjudication processes and procedures
- Knowledge of New York State laws, legal codes, procedures and processes involving WC insurance
- Knowledge of Construction Industry WC claims
- Adjusts property and general liability claims in the snow sports industry
- Determines coverage; sets and adjusts reserves
- Oversees all phases of incident investigation; conducts interviews/site inspections; hires outside experts and adjusters
- Negotiates settlements within authority
- Hires and directs defense counsel; manages defense budgets; plans and oversees discovery process; attends depositions, hearings, mediations and trials, as necessary
- Provides risk management services to assigned snow sports accounts
- Advises insureds on all aspects of ski area operations, claims, settlement negotiations and other risk management and insurance issues
- Responds immediately to notice of catastrophic losses by traveling to and overseeing the on-scene accident investigation, as necessary
- Acts as Risk Management resource for insured and snow sports industry
- Disseminates information through daily contact and periodic visits with insureds
- Conducts Risk Management seminars; participates in industry related meetings and seminars; conducts periodic on-hill inspections and operational inspections, as assigned
- Bachelor’s degree and 5-7 years of property and casualty claims adjusting experience, or equivalent combination of education and experience
- P&C Adjuster's license is required
- Must be an advanced level skier/snowboarder with own equipment and a passion for the snow sports industry
- Independent, entrepreneurial spirit
- Must be committed to client relationship management and service
- Proficient with computer programs, including Word, Excel, and Outlook
- Travel, up to 25% of the time, is required. Most travel is planned in advance but some travel is required on an "on call" basis
- Prior ski resort risk and operations experience a plus
- Execute policies and procedures governing the establishment and management of 3rd Party Liability, Bodily Injury case reserves
- Proactively monitor legislative and jurisprudence changes and competitor policies and practices
- Participates in authority committee meetings
- Alert their manager to any required policies, procedures and product changes based on exposure or risk due to judgements, wording, etc
- Contribute to a culture that promotes ethical practices and a high degree of integrity
- Financial Management
- Acts as a role model in openly endorsing the organization goals and strategies
- Proactively monitor market changes and competitor offerings, assess current and future client needs and evaluate unit effectiveness in responding to changing conditions
Claims Specialist, Complex Casualty Resume Examples & Samples
- Handles litigated claims as per TDI legal protocol
- Make recommendations to their manager on trends with respect to legislative and jurisprudence, supplier relationships and the overall book of business
- Collaborate to ensure sound business relationship for 3rd Party Liability, Bodily Injury with legal services suppliers and meet regularly to optimize knowledge transfer
- Responsible for identifying and preventing indemnity leakage on files
- Work closely with other Complex and Specialist Claims Analysts and the actuarial department to examine trends and predictors that may have a financial impact on Bodily Injury case reserves
- Collaborate with internal and external stakeholders and contribute to the Bodily Injury claims team to accomplish goals and objectives
- Provide ongoing support and coaching to support the development of Bodily Injury analysts
- Continuous Improvement
- Develop and encourage change and innovation at all levels of the unit and foster continuous improvement and new ideas adopting best practices
- Helps develop and execute the strategies of the practice on creating for larger accounts
- Support s new business with sales presentations and RFP
- Regularly meets with office leadership and team leaders to ensure delivery alignment
- 5+ years claims experience
- High School diploma required; degree preferred
- Knowledge of laws, legal codes procedures and processes involving insurance
- Understand the basic process and value basic data analytics and benchmarking
- Handle multiple tasks simultaneously and effectively prioritize to meet deadlines
- Be self-motivated, able to work both independently and within a matrix team structure
Life Claims Specialist / Assistant Resume Examples & Samples
- File and request files during the claim process (this would include ordering files from record retention and from AWD)
- Registration (computer in-put information regarding the claim)
- Mail claim forms, checks and correspondence
- Gather and organize files for internal and state audits
- Strong, relevant legal qualifications (Solicitor or Legal Executive essential)
- Strong claimant litigation experience; with the ability to draft, issue and progress proceedings to conclusion with minimal guidance
- Proven experience providing sound commercial advice within a business setting
- Clear knowledge of CPR and relevant legislation (NRSWA etc)
- Knowledge of wider law (i.e. tort, land) and experience of self-managing full case load
- Ability to listen to and understand stakeholder requirements
- Excellent negotiating skills
- Conduct outbound calls to all policyholders being assigned claims to the team
- Assist claims supervisor if needed, in training temporary staff during a catastrophe event
- Answer a high volume of telephone calls and respond to questions by policyholders and other third party stakeholders associated with the claim to provide case management
- Schedule follow up contact with the policyholder and other third party stakeholders in order to maintain open lines of communication
- Communicate with adjusting firms to obtain any outstanding documentation in order to process claim
- Apply National Flood Insurance Program rules and regulations with each claim worked
- Insure claims are processed within established company and client guidelines through working with other team members and the Claims Supervisor
- Coordinate and track losses using various in-house and potentially external systems
- Work with incoming and outgoing communications to ensure timely processing of Claims Department information when received
- Complete company training program. Program includes inter-departmental training within the Operations department as well as classroom training
- Ensure all correspondence directed from the Claims Department is professional and complete
- Work independently as well as within a team environment
- Maintain an established level of productivity using time management techniques
- Able to shift between priorities as needed throughout the workday
- 2+ Years of Office and/or Administrative background
- 2+ years of insurance claims processing experience preferably in insurance, claims and/or flood insurance
- The ideal candidate will have experience with phone related customer service and direct customer contact
- Communication skills including both verbal and written, with specific attention to detail
- Ability to maintain a high degree of confidentiality and ethical behavior
- Ability to maintain and display a positive attitude at all times; supporting business needs and changes; supporting continuous improvement; and supporting the National Flood Insurance Program
- Reliability and dedication to the position is imperative. Position will frequently require overtime hours
- Proficiency at keying alpha and numeric information with accuracy and speed
- Knowledge of basic equipment functions, such as how to create and maintain files, printing, copying, faxing, phone messaging and voice mail
- Ability to work with frequent and multiple policy, procedure, and regulatory changes
- Ability to manage time through establishment of priorities and proper planning
- Effective communication skills are a must
- Experience using Microsoft Office applications (i.e. Outlook, Excel, etc.)
- Must have experience working with data
- Experience in a medical office setting
- Medical claims processing experience preferred, but not required
Ucs-unemployment Claims Specialist Resume Examples & Samples
- Respond to a state agency with all pertinent details within the time frame allowed by the state or departmental procedures
- Initiate timely telephone calls, faxes or emails to customers, completed by co-workers, to obtain, document or pass along needed information
- Overtime may be required in order to meet state deadlines
- Previous office experience with an emphasis on organization of work duties and performing job functions independently
- High ethical standards
- Ability to handle a high volume of work and work under deadlines
- Ability to follow policies and procedures; complete administrative tasks correctly and on time
- High level of professionalism
- Computer Skills Required
- Previous experience with Unemployment Insurance and the Unemployment Claims process is helpful
Junior Claims Specialist Resume Examples & Samples
- Determine the amount of benefit payable as a result of the death of a retiree and process payments,
- Process payments under the fast track payment program,
- Handles Tier 1 creditor claims,
- Determine the liability as a result of the Extended Disability Benefit under a PSS Group Contract and sets up the claim
- Provide guidance to the client (e.g. the group policyholder or beneficiary on requirements needed to settle the claim and disburse the benefit to the legal beneficiary); works with Senior Specialist regarding gaps uncovered
- Communicate by telephone, correspondence and occasionally in person
- Serve as a back up to the Support function when needed
- Handle return of annual tax slips
- Processes claims that pend for various hold reasons to assist in the final determination on claim disposition
- Processes adjustments related to projects or provider disputes
- Researches post payment claims issues and takes necessary action for correction
- Research claims issues and works with other departments to resolve claim issues
- Preferred 1+ year of experience in Previous claims or health insurance
- Beginner Ability to multi-task
- Beginner Ability to work independently
- Beginner Ability to communicate and make recommendations to upper management
- Beginner Demonstrated written communication skills
- Beginner Demonstrated analytical skills
- Beginner Demonstrated problem solving skills
- Beginner Demonstrated time management and priority setting skills
- Beginner Demonstrated organizational skills
- Beginner Knowledge of healthcare delivery
- Required Beginner Microsoft Outlook
- Required Beginner Microsoft Word
- Required Beginner Microsoft Excel
- Processes adjustments related to projects or provider disputes providing timely follow-up provider call backs
- Researches complex claims issues and works with all external departments, markets, and providers on claims related content
- Completes new hire audits
- Runs and analyzes ad-hoc reports
- Identify root-cause issues to ensure enterprise solutions and communicate findings as needed
- Participates in all formal and informal training opportunities
- Preferred 2+ years of experience in Previous claims or health insurance
- Required 6 months of experience in Processing of institutional and / or professional claims
- Intermediate Ability to communicate and make recommendations to upper management
- Intermediate Ability to work independently
- Intermediate Demonstrated analytical skills
- Intermediate Demonstrated written communication skills
- Required Intermediate Microsoft Word
- Required Intermediate Microsoft Excel
- Ability to work independently and escalate for assistance as needed
- Strong communication ability to work with various internal and external parties to resolve member issues
- Ability to proactively identify payer and provider trends, and to communicate this to management
- Excellent customers service skills
- Excellent listening skills and ability to emphasize with members
- Excellent computer skills and experience in Microsoft Office Suite
- Daily opening and sorting of all claims related correspondence
- Enters mail received dates into the claims computer system
- Assists with the scanning process by imaging documents and pertinent information to AS400 IMS/21 system (either individually or by batch mode)
- Mailing out checks
- Maintaining a neat and orderly file room
- Batch processing of claim forms and letters
- Assisting with special projects and other duties as assigned
- One year prior office work experience preferred, but will consider recent grads
- Experience with Microsoft Office suite products
- Detail oriented and strong time management and communication skills
- Data entry and scanning experience helpful
- The Claims Specialist sets adequate reserves to ensure proper reporting
- Compares data on claim form with insurance plan to ascertain completeness and validity of the claim
- Examines claim form and other records to determine insurance coverage
- Proactively works to resolve claim as expeditiously as possible
- Reviews and analyze detailed medical records
- Calculates reimbursement of benefits according to the schedule of coverage. Runs various claim reports as directed by the account
- Liaison with Marketing/Customer Service departments
- Cultivates relationships
- Incrementally increase productivity without jeopardizing quality
- Approves claims at the appropriately demonstrated assigned authority level
- Functions as a resource for examiners and assist with training new examiners and customer service representative
- Handles difficult phone calls and composes special correspondence
- 1 – 3 years claims adjudication experience. Will also considerrecent college graduate with a 4 year degree. Majors in Business Admin, English, Finance or Science preferred
- Ability to multi-task – manages time effectively
- Recognize repetitive problems or issues and escalate as needed
- Identify exception handling and process per client requirements. When appropriate, assign a script number or NDC number if not provided
- Input claim requests into adjudication platform maintaining production and accuracy standards. Evaluate system rejections to ensure accuracy and appropriateness
- Evaluate claim submission, ensure all required information is present and determine what action should be taken. Confirm patient eligibility and verify patient information matches system. Update member’s address to match claim form if necessary
- Create correspondence to members, internal departments, and external agencies regarding outstanding claims issues. Compose letters to members or pharmacies for those claims with insufficient information or eligibility or benefit issues
- Handle claims requiring additional research, navigate through appropriate system platforms to perform research and resolve issues. Work with other operational departments to research and resolve claims issues within performance agreement guidelines
- GED: General Studies (Required) HS: General Studies (Required)
- Years of Relevant Work Experience 2 - 3 Years
- Proficient written and oral communication skills; strong customer focus
- Must be aself-starter and team player
- Ability to adapt in a dynamic work environment, learn quickly, solve problems and make decisions with minimal supervision
- Relevant professional qualification e.g. (ACII/FCII/CILA)
- Bachelor’s degree preferred, advanced degree preferred plus 8 years’ experience
- CPCU, or AIC, or ARM within 3 years of obtaining this position or 20 years or more insurance industry experience exempt
- Query Management
- Compliance Management
- Organization and Prioritizations
- Market relationship management
- London Market Negotiation
- Technical knowledge
- 10+ years claims experience in general liability and construction claims
- College degree required, law degree a plus
- Travel required, primarily within California
- Knowledgeable in Excel, Word and PowerPoint
- Strong Default Mortgage background
- Accounting and Reconciliation skills
- Minimum 2 years Investor Claims Experience
- 5 years Investor Claims Experience
- 5 years Mortgage Servicing or Default Experience
- Reviews and interprets rebate contract terms and conditions and establishes parameters in the contracting system (CARS) to produce accurate rebate calculations
- Conducts initial quality check, including formulary compliance, on all claim submissions to ensure rebate eligibility. Resolves issues with account and prepares validation system (ECP) to receive detail claim data
- Reviews suspect claim records and determines if record should be disputed for payment. Communicates disputed records to account
- Prepares contracting system to receive validated claim data and calculate rebates. Ensures accurate system results by manually checking calculations
- Acts as the primary contact point for rebate questions from account, account managers, Contract Administration and Forecast Administration
- Supports the collection and recording of data critical to contract preformance assessment and rebate forecasting
- Pharmaceuticals industry
- Manipulation of large data sets
- Negotiation/conflict resolution
- Able to understand and troubleshoot electronic data processing systems
- Able to construct system workarounds in special circumstances
GAT Claims Specialist Resume Examples & Samples
- English and Japanese (required - for Japanese must be at least able to read, listen and write/type). Proficiency in any of the following languages would be an added advantage - Chinese, Malay, Vietnamese, Thai, Korea
- Ability to manage time and resources to meet commitments in a dynamic environment and following through on details
- Strong interpersonal skills and communications skills
- Able to build professional relationship with business partners internally and externally. Actively responds to business partners' requirement and business priorities
- Great team player, works well and collaborates with others to achieve quality results
- Acts as Claims Department subject matter expert on departmental and corporate projects. Supports business definition and testing efforts, attends project meetings, maintains project plans and provides internal and external status reports
- Works with management and associates to document current business and workflow processes and collaborates in identifying, defining and documenting process improvement options and alternatives
- Researches complex claims issues and works with other departments to resolve. Serves as primary liaison to all external departments, markets, and providers on claims related content
- Analyzes and trends claims issues, performs true root cause analysis and determines next steps for resolution and process improvement
- Researches issues, compiles feedback and drafts corresponding business requirements documents and business decision documents as needed
- Communicates changes in processes, project status and issue resolutions through email, memos, group presentations, and/or individual one-off meetings
- Performs new hire audits
- Preferred 3+ years of experience in Previous claims or health insurance
- Required 2+ years of experience in Claims processing with a solid understanding of internal claims functions, and have performed at least 5 of the duties found in the Claims II role (found in job description)
- Advanced Ability to communicate and make recommendations to upper management
- Advanced Ability to effectively present information and respond to questions from peers and management
- Advanced Ability to multi-task
- Advanced Ability to work in a fast paced environment with changing priorities
- Advanced Ability to work independently
- Advanced Demonstrated analytical skills
- Advanced Demonstrated ability to deal with confidential information
- Advanced Demonstrated customer service skills
- Advanced Demonstrated interpersonal/verbal communication skills
- Advanced Demonstrated organizational skills
- Advanced Demonstrated problem solving skills
- Advanced Demonstrated time management and priority setting skills
- Advanced Demonstrated written communication skills
- Advanced Knowledge of healthcare delivery
- Communicate with store personnel and injured customers
- Proactive communication in resolution of in-house customer claims
- Act as an internal resource for General Liability questions
- Provide reports via excel as required
- Researches, analyze and resolves customer deductions
- Establish relationships with the appropriate business unit and corporate personnel
- Advise the business of deduction problems and to the supervisor
- Other duties as assigned by the FSCM Supervisor
- 1 to 3 years experience in a business related field
- Previous experience desired in deduction management
- Proficient in Microsoft Word, Excel, Access, PowerPoint, and Outlook
- Committed to superior customer service with a quality focus
- Listens well and communicates effectively both verbally and written
- Excellent self-management skills & ability to work independently
- Understand multiple client programs, follow process guidelines
- Demonstrate strong ability to identify, analyze and solve problem for customer resolution
- Claims adjudication experience or relevant experience
- Bachelor’s degree preferred, advanced degree preferred plus 10 years’ experience managing Financial & Executive Lines claims (D&O, E&O (including Cyber), EPLI, Fiduciary Liability, Fidelity/Crime)
- Knowledge of claims handling, processes and best practices procedures
- Ability to conduct claim best practice audits, including outlining findings and recommendations with goal of improving claim program
- Strong communication skills both verbal and written with senior management, clients, and vendors
- Proven success for working with different personalities
- Ability to work effectively in team environment
- Must be able to handle multiple tasks simultaneously and manage deadlines
- Ability to analyze and report financial data
- Obtains relevant technical information to support decision making
- Strong presentation skills to be effective in sales meetings with prospects
- Proven ability to work independently
- Understands company products, services, global network, and industry practices
- Data analysis and benchmarking skills including ability to analyze claim data and develop solutions to potential adverse trends
Claims Specialist, Complex Casualty Ontario Resume Examples & Samples
- Strategy Execution
- Resolve complex claims adhering to established claims settlement policies and processes
- Execute policies and procedures governing the establishment and management of 3rdParty Liability, Bodily Injury case reserves
- Ensure consistency in behaviour and actions in line with company core values and exercise sound judgment in non-routine and complex situations
- Support the development of analysts through empowerment and coaching
- Organizational Effectiveness
- Apply established decision criteria triggering the management and resolution of complex claims
- Execute authority to fairly settle complex claims up to authority limit
- Accountable for adequacy of Bodily Injury case reserves on their files
Workers Comp Claims Specialist Resume Examples & Samples
- Evaluate claims to determine potential exposure; make recommendations concerning the value of the claim; oversee litigation and assist in the negotiation of settlements
- Proactively oversee the Worker’s Compensation claims management activities in assigned territories with a special focus on cost containment strategies
- Manage and target aggressive resolution of case inventory, and resolve problems of varying scope and complexity in accordance with state statutes
- Evaluate claims for settlement and appropriateness of established reserves
- Attend claim reviews; complete follow up action to ensure expedited resolution
- Provide daily support / guidance to teammates, claims adjusters, insurers, and defense counsel by answering claims-related questions or concerns in the administration and management of claims, return-to-work issues, and other claim matters
- Analyze claims data to identify needed loss control interventions and assist with the development of appropriate loss prevention programs as requested
- Provide training and education to facilities on claim processes and procedures
- Coordinate handling of claim subpoenas in an expeditious manner
- Generate reporting and analysis on assigned case inventory
- Escalate exceptions, outliers, or circumstances that are out-of-norm, as they occur, and seek guidance in case resolution
- Participate in meetings, presentations, and special projects, as necessary
- Commitment to Company’s values of Service Excellence, Integrity, Team, Continuous Improvement, Accountability, Fulfillment and Fun with ability to demonstrate those positively and proactively to patients, teammates, management, physicians, and/or vendors in every day performance and interactions
- Demonstrated sound judgment and initiative in working within departmental and corporate guidelines, including the ability to maintain confidentiality of information
- Strong written, verbal, and interpersonal communications skills including ability to listen attentively and to communicate information clearly and effectively throughout all levels of the organization with audiences of varying degrees of familiarity with material
Complaints / Claims Specialist Resume Examples & Samples
- Providing expertise or general support in reviewing, researching, investigating, negotiating and resolving all types of claims and complaints / grievances
- Coordinating efforts with other areas as necessary
- Communicating issues, implications and decisions with appropriate parties
- Analyzing and identifying trends for complaints / grievances
- Ensuring optimal performance re: timely, accurate, effective and complete responses
- Verifying that all documentation, letters and attachments meet customer, regulatory and internal requirements
- Preparing for and participating in audits
- Organizing, checking, pulling, reviewing and saving files
- Maintaining positive working relationships with internal and external customers including regulators
- Word & Excel proficiency
- Must be proficient in developing accurate, easy to understand and thorough correspondence
- Previous Behavioral Health experience
- Must live within a commutable distance of San Francisco, CA
- Previous Appeals and/or Complaints/Grievances experience
- Previous Claims experience
- Bachelor's Degree in Healthcare, Behavioral Health, Business, Psychology or English
- Communicate and go on-site as necessary to locations to assist with all internal claims management activities
- Maintain an internal active diary system of claims that are being managed
- Coordinate for team internal claims update to Risk Management as requested / required, such as an internal claims review
- Monitor claims reporting to third party administrator and report claims as required
- Work with stores safety to help identify and reduce claim trends
- Monitors and reports the effectiveness of third party claims administrators with regard to this position’s assigned case load
- Responsible for legally mandated mailings
Junior Warranty Claims Specialist With English & German Resume Examples & Samples
- Communicative English and German (mainly written and reading skills on level B2, communication can be passive)
- Data processing accuracy, detail oriented and ability to evaluate/research a warranty claim
- Experience in Warranty is preferred but not required
Claims Specialist, Senior Resume Examples & Samples
- Processes all types of medical claims and adjusts medical disputed claims (Professional and Facility) according to department, contract, and regulatory requirements
- Performs prepayment audit on all types of medical claims (Professional and Facility) according to department, contract, and regulatory requirements
- Updates authorization information based on information obtained from provider
- Troubleshoots problem claims to resolve provider issues or systematic issues
- Verifies and interprets information in all vendor contracts to resolve issues
- Trains analysts and monitors general office support functions as needed
- Analyzes work processes, identifies areas needing improvements and initiates necessary steps to make changes
- Participates in the continuous quality improvement of IMCS core business system
- Computer literate
- Individual must be reliable, dependable, and punctual
- Ability to make decisions regarding escalation of referrals to Care Management
- Knowledge of compliance related to the processing of claims
- Knowledge of different sources of authorization documentation
- Ability to update authorization information based on information obtained from facilities
- Ability to read and interpret all vendor contracts
- Knowledge of DRG pricing
- Processes all types of professional claims and adjusts professional disputed claims according to department, contract, and regulatory requirements
- Performs prepayment audit on all types of professional claims according to department, contract, and regulatory requirements
- Processes simple facility claims as needed according to department, contract, and regulatory requirements
- Answers telephone inquiries through the “Automated Call Distributor (ACD) Telephone System” as needed
- Identifies individual provider needs and take appropriate steps to satisfy those needs
- Updates authorization information based on information obtained from facilities
- Analyzes work processes and identifies areas needing improvements
- Follows unit procedures for performing call processing, claim adjustments and denials and references Policies and Procedures, job aides, provider contracts, and other reference materials to assure complete and accurate decisions
- Excellent customer service and telephone skills
- Ability to work in an environment with fluctuating workloads
- Ability to solve problems systematically, using sound business judgment
- Ability to make decisions with every call and handle escalated issues
- Familiarity with ICD-9 and CPT codes
- Ability to research and verify claims payment issues
- Knowledge of medical terminology and pricing options
Claims Specialist Senior Resume Examples & Samples
- Handles the most complex/challenging claims issues
- Ensures the accuracy and completeness of claims forms
- Investigates coverage questions and problems
- Works closely with clients, producers, client service staff, insurance carriers
- Identifies and resolves complex problems in a timely fashion following established guidelines
- May provide guidance and coaching to lower level staff
- Operates independently and can service the largest clients and/or resolve the most complex problems
- Has a solid understanding of claims processing and the insurance brokerage business
- Works with Director of Claims in support of quality claims control
- Travel as needed. (Minimal)
- Ability and willingness to take initiative
- Bachelor’s degree or equivalent combination of education and experience required
- Experience in claims management processes and system requirements preferred
- 5 or more years related professional experience
- Good understanding of claims processing and the insurance brokerage business
- Licensing required
General Liability Claims Specialist Resume Examples & Samples
- Juris Doctor and 1 or more years of experience in the Claims Handling or Insurance area
- 3 or more years of commercial general liability claims handling experience
- AIC, SCLA and/or CPCU designation
Wc-claims Specialist Resume Examples & Samples
- Jones Act; DBA (Defense Based Act)
- 7 or more years of claims handling experience with 2 or more years in USL& H ; Jones Act; DBA (Defense Based Act)
- Bachelors Degree and 2 or more years of claims handling experience
- At least 1 year in the Claims Foundational Training Program
- 2 or more years of Auto Liability claims handling
- Strong communications, analytical, negotiation and customer service skills
- Advanced data gathering and problem solving skills
Professional Liability Claims Specialist Resume Examples & Samples
- 7 or more years of claims handling experience with 2 or more years in professional liability, EPLI and/or general liability claims
- Ability to obtain and maintain required adjuster license
- AIC, SCLA and/or CPCU
- At least 2 years of Commercial Liability Claims handling experience
- Associate or Bachelors Degree
- Experience handling Commercial General Liability Claims
- Willingness to embrace the Zurich Basics of Integrity, Sustainability, Customer centricity, excellence and Teamwork
Claims Specialist, General Liability Resume Examples & Samples
- Bachelor’s Degree and 3 or more years of directly related experience managing a claims caseload for a P&C line of business
- Experience that includes adjudication of GL claims
- Strong communication, analytical, negotiation and customer service skills
- Bachelors Degree and/or related Claims or Veterinary industries experience. Related experience may include previous experience in an office environment that required computer work, organization, strong communications, customer service and negotiation
- Experience gathering data, designing and testing solutions to problems, and formulating plans as well as managing multiple projects simultaneously in a fast paced environment
- 3 or more years of related Claims or Veterinary industries with Bachelors Degree OR
- 4 or more years of related Claims or Veterinary industries without Bachelors Degree OR
- 2 or more years of related litigation experience with a Juris Doctorate
- Fundamental knowledge of the Claims or Veterinary industries industry, claims and the insurance legal and regulatory environment
- A functional and developing knowledge of the legal statutes and procedures
- A thorough functional knowledge and skill of claims handling
- Negotiation Experience
- Travel required (0-25%)
- 3 or more years of claims handling experience or veterinary industry experience
- Experience in a work environment that required collaboration across work groups
- Ability to effectively present information to LOB manager, claimants and customers
- Bachelors Degree and/or related industry experience. Related experience may include previous experience in an office environment that required computer work, organization, strong communications, customer service and negotiation
- 3 or more years of related experience with Bachelors Degree OR
- 4 or more years of related experience without Bachelors Degree OR
- Fundamental knowledge of the insurance industry, claims and the
- Insurance legal and regulatory environment
- Travel required (0-5%)
- 3 or more years of claims handling experience in line of business
Liability Claims Specialist Resume Examples & Samples
- NY Labor Law claims experience
- Strong Organization and time management skills
- AIC, SCLA and/or CPCU designations
- 6 Or More Years Of Related Auto Liability Experience
- Bachelors Degree Or Equivalent
- Experience in line of business
- Willingness to embrace the Zurich Basics of integrity,
- Sustainability, customer-centricity, excellence and teamwork
- Bachelors Degree and/or related industry experience. Related experience may include previous experience in an office environment that required computer work, organization skills, strong communications, customer service and negotiation skills, experience gathering data, designing and testing solutions to problems, and formulating plans as well as experience managing multiple projects simultaneously in a fast paced environment
- 6 or more years of related experience with Bachelors Degree OR
- 7 or more years of related experience without Bachelor’s Degree
- 2 or more years of demonstrated management experience including
- Coaching and mentoring
- 4 or more years of claims, insurance or litigation experience
- Must have experience collaborating across work groups
- A functional knowledge of legal statutes and procedures
- Thorough knowledge of the insurance industry, claims and the
- Travel required 0-20%
Subrogation Claims Specialist Resume Examples & Samples
- Assess liability and analyze exposure on assigned matters
- Hire appropriate and effective counsel and expert resources
- Analyze financial dynamics and directly handle negotiations
- Responsible for achievement of individual subrogation goal established annually, typically $7-$9M, while possessing $1,000,000 in indemnity settlement authority and $300,000 in expense authority on each matter
- Achieve optimum subrogation results on assigned matters through direct handling, as well as effective management and direction to Property Large Loss adjusters, cause and origin investigators, and subrogation counsel on the investigation, evaluation and strategic planning related to these cases
- Mitigate all subrogation expenses in order to contribute to corporate recovery objectives
- Attend mediations, settlement conferences and trials as required
- Effective and timely reporting on subrogation matters, sharing any trends or legal decisions that affect subrogation recovery with business leaders
- Provide oversight, direction and training of internal partners in the Central Recovery Office, as well as the Property Large Loss and Field Operations
- Participate as a subject matter expert in ancillary projects that impact subrogation
- Embrace enterprise values of customer focus, diversity and inclusion, financial discipline, integrity, team work and a winning spirit by meeting the leadership imperatives of delivering results, inspiring excellence, being a team player, forward thinking, championing talent and becoming a trusted decision-maker
- Juris Doctorate strongly preferred with 4+ years of legal experience; alternatively, 8-10 plus years of carrier subrogation experience in first party property matters
- Strong knowledge of theories of liability, and understanding of legal procedures and strategies
- Excellent analytical, critical thinking and problem solving skills
- Strong negotiation and communication skills, both written and verbal
- Ability to work independently and embrace positive accountability
- Inquisitive, ambitious, and a bias for improvement
- Working knowledge of property coverage and the insurance industry
- Manages moderate to high complexity commercial subrogation/recovery claim investigation involving the property line of business. Determines if a claim should be negotiated, arbitrated or litigated through conclusion based on a thorough investigation and resolution strategy. Effectively manages loss costs and recovery claim expenses
- Manages all types of investigative activity or litigation on claims, including the posting of appropriate reserves in a timely manner. Coordinates discovery and litigation strategy with staff counsel or panel attorneys
- Negotiates moderate to high complexity settlement packages within scope of authority, settling recovery claims in the most cost effective manner
- Makes recommendations on subrogation/recovery claims processes and resolution strategies to management
- Analyzes recovery claims activities; prepares and presents reports to management and other internal business partners and clients
- Works with attorneys, account representatives, agents and insureds regarding the handling and/or disposition of moderate to high complexity subrogation/recovery claims
- Keeps current on state/territory regulations and issues, industry activity and trends. May participate in industry trade groups
- Provides guidance and assistance to less experienced claims staff and other functional areas where appropriate
- Responsible for input of data that accurately reflects claim circumstances and other information important to our business outcomes
- Advanced technical and product specific expertise, subrogation/recovery claims resolution skill and knowledge of insurance and underlying claim principles, practices and procedures
- Strong communication, negotiation and presentation skills. Ability to effectively interact with all levels of CNA's internal and external business partners
- Creativity in resolving unique and challenging business problems
- Knowledge of Microsoft Office Suite and other business-related software
- Ability to manage and prioritize multiple projects
- Ability to evaluate claims based on a cost benefit analysis
- Ability to fully comprehend moderate to complex claim facts and issues; and to further articulate analyses of claims in presentations to business partners and management as well as in internal reports
- Ability to implement strategies with a proactive long-term view of business goals and objectives
- Bachelor's degree or equivalent experience. Professional designation preferred
- Typically a minimum three to five years commercial property subrogation/underlying property claims experience
- Manages moderate to high complexity commercial recovery claim investigation involving ocean marine subrogation/recovery claims. Determines if a major claim should be negotiated, arbitrated or litigated through conclusion based on a thorough investigation and resolution strategy. Effectively manages loss costs and recovery claim expenses
- Manages all types of investigative activity or litigation on major ocean marine claims, including the posting of appropriate reserves in a timely manner. Coordinates discovery and litigation strategy with staff counsel or panel attorneys
- Makes recommendations on recovery claims processes and resolution strategies to management
- Works with attorneys, account representatives, agents and insureds regarding the handling and/or disposition of moderate to high complexity recovery claims
- Keeps current on state/territory regulations and issues, industry activity and trends related to ocean marine. May participate in industry trade groups. Understands and can apply admiralty law/statutes including, but not limited to COGSA, Montreal Convention and Hague Convention, as part of strategy to maximize recovery
- Provides guidance and assistance to less experienced claims staff and other functional areas when/where appropriate
- Effectively manages vendor relationships to include the expansion contraction vendor model with key vendor partners
- Demonstrated technical expertise, product specific knowledge, and negotiation skills
- Strong interpersonal and communication skills. Ability to effectively interact with all levels of CNA’s internal and external business partners
- The ability to exercise independent judgment and make critical business decisions effectively
- Typically a minimum three to five years ocean marine and/or property claims experience
- Interprets more complex or unusual policy coverages and determines if coverages apply to claims submitted, escalating issues as needed
- Prepares timely and thorough coverage analysis and may occasionally assign counsel on an insured’s behalf
- Recommends appropriate reserves and attempts to effectively settle claims in most cost effective manner and ensuring timely issuance of disbursements
- Coordinates and performs investigations and evaluates claims and exposure through contact with insureds, brokers, other insurance carriers and defense counsel
- Utilizes negotiation skills to develop complex settlement packages or suggest resolution strategies
- Works with defense counsel, underwriters, brokers, and insureds regarding the handling and/or disposition of complex claims
- Analyzes claims activities and prepares reports for management. May be responsible for special projects and presentations
- Demonstrated technical expertise and product specific knowledge
- Strong interpersonal, communication and negotiation skills. Must have the ability to effectively interact with all levels of CNA's internal and external business partners
- Ability to exercise independent judgment and make critical business decisions effectively
- Juris Doctorate strongly preferred. Professional designations preferred
- Typically a minimum two to five years claims experience in professional liability or 2 plus years in a law firm handling professional liability claims. D&O experience preferred
- Demonstrated claims management experience in workers comp, auto and general liability issues
- Strong analytical, critical thinking, problem solving, judgment, negotiating, influencing, and decision making skills. Ability to maintain confidentiality, tact, and diplomacy
- Working knowledge of federal and state disability laws; specifically FMLA, CFRA, ADA, HIPAA, etc
- Familiarity with job restrictions, accommodations and functional capacity exams
- Strong working knowledge of workers' compensation claims and process
- Strong organizational skills: comfortable managing many multiple and varied complex individual situations
- Experience counseling and working with employees regarding disability benefits, vendor claims personnel, internal and external legal departments
- Excellent facilitation and oral and written communication skills; ability to prepare clear and concise reports and deliver formal presentations or training to senior management and other audiences
- Demonstrated proficiency with business applications, such as Microsoft Office suite and human resource information systems
- Proficient in managing multiple sources of data and integrity; ability to identify trends, design reports, conduct audit and analysis of data
- Clear thinker who understands the development of and has ability to correctly interpret policy
- Flexibility and adaptability in dealing with rapidly changing priorities and demands necessary
- Ability to make sound judgments requiring confidentiality, tact, and diplomacy in dealing with a variety of personalities and situations
- Bachelor's degree (preferred) and five – seven years of relevant experience, or combination of education and relevant experience
- California State disability expertise required
- Investigate, negotiate, subrogate and settle first and third party losses
- Maintain recovery targets set forth each month
- Ensure cases are called as scheduled and aging is maintained
- Demonstrate professionalism when dealing with contacts
- Maximize Collection efforts and customer satisfaction
- Practice collection and research techniques to ensure timely resolution
- Maintain accurate and complete documentation of all activity
- Submit claims for referral and write-off
- Develop a systematic approach for case reviews and calls
- Include Customer Relations when addressing sensitive case issues
- Include Hertz Sales when addressing sensitive case issues
- Respond to inquiries within 24 hours to maintain customer service
- Other duties as assigned by supervisor/manager
- One year Insurance Claims experience and/or collections experience
- Basic working knowledge with Microsoft Word and Excel (pre – employment assessment required)
- Excellent customer service and telephone skills/experience
- Excellent organizational skills and ability to handle multiple tasks
- Must be able to work well with others
- Must be attentive to detail
- Must be an independent worker and able to work with minimal supervision
- Criminal background check due to access to Personal identifiable Data (PID)
- Good interpersonal and customer services skills
- Good data management and analytical skills
- Attentive to details and patient
- PC literate in Word, Excel and Chinese word processing
- Good command of spoken and written English and Chinese
- Candidates with less experience will be considered as Claims Analyst or Claims Assistant
Consumer Claims Specialist Resume Examples & Samples
- Responsible for receiving, organizing, reviewing, and resolving product complaints related to product safety and quality for Philips North America products
- Requests complaint failure investigations; and, ensures returned products associated with product complaints are forwarded to the appropriate facility for investigation
- Prepare and distribute written correspondence to the consumer regarding product complaint that resolve the consumer’s issue
- Responsible for one time consumer resolution for all products
- Responsible for check requests to settle consumer claims along with “closure”/disclaimer letter
- Applies acquired job skills, company policies, and procedures to complete assigned tasks but recognizes the need for deviation occasionally
- Requires 1-2 years of minimum experience to manage consumer relationship
- Minimum 1-2 years of experience using Microsoft Office
- Can coordinate multiple tasks simultaneously
- Knowledge of working with Consumer Relationship Management (CRM) system like Salesforce
- Knowledge of complaint handling
- Utilize 3rd party software to price claims for various markets
- Monitor and release of all claims in the adjudication queue folder
- Quality check claim batches adhering to weekly claim run deadline
- Responsible for handling emails including but not limited to reprocessing requests and inquiries from internal and external sources
- Attend internal and external operational and/or provider related meetings as assigned
Excellent Recent Grad Claims Specialist Position Resume Examples & Samples
- Desire to learn
- Desire to grow within a company
- Manage claims through the life cycle
- Information gathering and research
- Issue resolution with clients and carriers
- Status reporting
- Ad hoc reporting
- Strong MS Excel skills including functions and pivot tables
- Ability to work in a team and support the team
- Processing member claims
- Making outbound phone calls to members or providers to get required information for processing
- Investigating claims for required processing information
- Knowledge in Medical Terminology, CPT-4 , ICD-9, ICD-10 and revenue code
- Team player, ability to work with tight schedules, overtime and multiple priorities
- Able to meet deadlines and work under pressure
- Excellent communication skills, both oral and written, English and Spanish
- Experience as Claims Specialist (2 years minimum)
Leave of Absence Claims Specialist Resume Examples & Samples
- Communicates decisions and on-going expectations with Employees, Manager and Human Resources. Communicate as necessary with employees, supervisors, and departments to keep employees informed and up to date through FMLA leave application process, period of FMLA leave, and return to work
- Counsel employees and supervisors about FMLA rights and responsibilities while maintaining appropriate confidentiality of employee medical information
- Interface with Worker's Compensation to ensure that Worker's Compensation claimants are apprised of FMLA and ADA rights and obligations per law and company policy
- Performs complex research using PeopleSoft, knowledge base, event management system, Total Benefits Administrator Pension System, Kronos Automated Time Collection system, Authoria, and Microsoft based PC application (Excel, Access, Works) to perform job functions. Create and utilize queries in both PeopleSoft and vendor maintained applications. Communicates outcome in a timely fashion. Responds to inquiries from disability carriers regarding any information needed for claim processing
- Review and assess current FMLA/STD leave practices and propose revisions to improve overall accuracy, consistency, efficiency, and communication
- Maintain control of outside vendors/attorney and their expenses by directing assignments to them, and limiting the scope of assignments so as to maximize cost efficiency while minimizing delays in claim handling. Such vendors/attorneys must not be used unless pre-approved by the manager. Adhere to provisions of Litigation Management Program and cost containment principles
- Maintain compliance with Fair Claim Practices Act or rules and internal instructions
- Knowledge of Auto and General Liability policy coverage
- Knowledge of tort law, motor vehicle law, basic reinsurance, property damage, bodily injury knowledge required and coding related to claims technical matters
- Establish proper loss reserve and negotiate loss settlements
- Maintain control of outside vendors/attorneys and their expenses by directing assignments to them and limiting their scope to maximize cost effectiveness while minimizing delays in claims handling. Such vendors/attorneys must not be used unless pre-approved by the department manager
- Maintain compliance with Workers' Compensation procedure and requirements established by regulatory authorities
- Pursue Workers' Compensation liens and subrogation when appropriate
- Maintain compliance with claims practice rules and internal instructions
- Keep supervisor advised of significant developments in claims
- Answer correspondence and inquiries promptly from brokers/agents, insureds, claimants, doctors, attorneys, outside vendors, TMM employees, etc
- Minimum five (5) years of experience investigating and handling lost time Workers' Compensation
- Experience in handling claims and detailed knowledge of applicable state jurisdictional Workers' Compensation rules and regulations for GA, TN, MS, AL – required; additional states – FL, NC, SC
- Knowledge and understanding of medical and legal terminology which may come within the purview of Workers' Compensation claims
- Computer literate (MS Windows preferred)
- Valid Georgia Insurance Adjuster License or CWCP
Home Claims Specialist Resume Examples & Samples
- Previous experience in a customer-facing role, including demonstrable evidence of providing high standards of customer care are essential
- Numeracy and literacy (equivalent to GCSE level Maths and English - Grade C and above)
- Problem Solver
- Proactive and pragmatic approach
IDI Claims Specialist Resume Examples & Samples
- Manages assigned caseload with limited supervision
- Provides timely, balanced and accurate claims reviews, documentation and recommended decisions in a time sensitive and fast-paced environment
- Compiles file documentation and correspondence requiring extensive policy and factual detail. Identifies information and resources needed to adjudicate claim
- Conducts lengthy detailed information-gathering phone calls that obtain medical condition details, financial details, occupational details and other information
- Proficiently calculates benefits due after elimination period, COLA, Social Security Offsets, and residual and non-routine payments
- Drafts responses to Department of Insurance and Presidential complaints
- Identifies and refers appropriate matters to legal counsel
- Represents MetLife at depositions and trials
- High School Diploma or Equivalency required; Bachelor’s Degree strongly preferred
- 1+ year related business experience
- In order to post for this position, you need the proper work authorization to work in the country where the position is located and not require relocation assistance
LTD Claims Specialist Trainee Resume Examples & Samples
- Provide timely and accurate communication, information gathering, and rendering decisions on Long-term Disability (LTD) claims according to provisions of LTD certificates
- Communicate with a variety of constituents (claimants, doctors, nurses, employers, and attorneys) to gather information relevant to rendering decisions based on the provisions of the policy
- Learn to use appropriate systems, tools and resources to research and document claims
- Learn to develop an action plan and identify the Likely Claim Progression including identifying the return to work potential
- Complete regular updates on financial offsets such as SSDI
STD / Fmla Claims Specialist Resume Examples & Samples
- 2-4 years Customer Service background
- High School Diploma/ GED
- Bachelor’s Degree Preferred and 2-4 years’ customer service experience
A&H Claims Specialist Resume Examples & Samples
- Compiles file documentation and correspondence requiring extensive policy and factual detail
- Communicates decisions to policyholders in verbal and written form
- Refers to external and internal resources, such as physicians, attorneys and CPAs to gather data such as medical/occupational information in order to ensure well-reasoned decisions
- Clarifies and reconciles inconsistencies
- 3+ years of experience in insurance claims
Meditech Claims Specialist Resume Examples & Samples
- MEDITECH 6.1 Billing/Accounts Receivable building required
- Testing and training of claims forms to include all facets of electronic and paper based claims including 5010, 835 and 837s required
- Identify improvement opportunities or best practices and make recommendations for optimizing workflow
- Provide consulting services in all areas of healthcare revenue cycle including: Patient Access, Registration/Admission, Patient Financial Services, and Decision Support/Analytics
- Maintain regular communication with client, vendor, team members and team leaders regarding project issues, risks, and needs
- On occasion, may be required to lift and/or carry up to 25 lbs
- Required to use computer for long periods of time
- Candidates may live anywhere in the contiguous US and travel 75-100%, as needed by project
- Maintains at least 85% billable utilization rate
- 1+ years of experience in insurance, claims or collection and recovery fields is a plus
- Prior knowledge of insurance claims or debt recovery is preferred
- Adjusters license preferred, but not required
- Provider billing files: Statewide responsibility for processing service provider claims for Title XIX members
- Monitoring approved and denied claim files in accordance with Division and AHCCCS regulations to ensure proper adjudication and audit compliance
- Reporting member insurance benefits not identified at time of claim submission to AHCCCS, with high volume of customer interaction
- ReversalNoided claims: Statewide responsibility for research of service provider payments. Processes provider initiated and management approved claim line Reversals and claim line Voids
- Assists with special projects and perform other related work as required
- Knowledge of principles and practices of accounting
- Knowledge of AHCCCS rules and regulations as applied to processing medical claims, diagnostic and procedural coding used on medical claims
- Excellent Customer Services skills a must
- Comprehensive oral and written communication skills
- Problem solving, analytical, and research skills
- Ability to analyze billing problems and recommend usable solutions, the ability to diffuse and resolve complicated issues while maintaining professional relationships, provide training to mixed groups of diverse backgrounds
- Ability to cross-train to other duties within the unit
- The ideal/preferred candidate will be familiar with medical claims processing, third party liability and/or Coordination of Benefits
LTD Claims Specialist Resume Examples & Samples
- Independently assess, analyze and render appropriate claim decisions pursuant to certificates
- Adhere to federal and state law to maintain appropriate and timely claim outcomes
- Articulate and document their rationale for claim direction, possess the autonomy to take steps outside of CMG guidelines to the extent supported by documented rationale and the facts of the claim file
- Utilize tools independently and accurately to identify work to be completed across the entire claim block, prioritize work, determine if/when to involve specialty resources such as clinical staff to obtain additional information on a claim
- 3-5 years’ long term disability claims experience
- Strong communication skills, both written and oral
- Comfortable working with multiple priorities in a changing environment
- Researching and identifying suspicious activity through comparative analysis
- Handling escalated calls and complaints
- Assisting in the development of more junior level Claims Specialists
- Preparing case documents for security and law enforcement agencies
- Analyzes, investigates, and evaluates the loss to determine coverage and claim disposition. Utilizes CMS to document claims and to diary future events or follow-up
- Within prescribed settlement authority for the line of business, establishes appropriate reserves for both indemnity and expense and reviews on a regular basis to ensure adequacy. Makes recommendations to set reserves at appropriate level for claims outside of authority level
- Monitors the case resolution process. Actively participates in mediations and arbitrations, within limit of settlement authority
- Participates in Claims audit process
- May provide claims marketing services by participating in meetings with brokers, risk managers and reinsurers
- As required, maintains insurance adjuster licenses
- Bachelors' and/or advanced degree required. J.D. preferred
- 5+ years claims/legal experience, with Management Liability experience preferred
- Functional knowledge of claims handling concepts, practices and techniques, to include, but not limited to coverage issues and product line knowledge
- Functional knowledge of law and insurance regulations in various jurisdictions
- Demonstrated strong negotiation skills
- Receive and prioritize claims, questionnaires and other unemployment related data
- Analyze individual case information by reviewing data accessed through the PC, from documented telephone calls or document images, to determine if the facts warrant a response
- Using the details regarding an employee’s separation provided by the client, interpret and apply state laws and regulations in response to unemployment documents
- Works as a team with our Unemployment Insurance Consultants to ensure accurate and necessary information retrieved from customers is documented clearly and thoroughly into our database
- Investigates and resolves state agency concerns with supervisor, other departments and/or State Relationship Managers in a timely manner
- Associate’s degree (A.A.) or equivalent from two-year college or technical school; or two years customer service related experience and/or training; or equivalent combination of education and experience
- 2-3 weeks of immediate, mandatory and uninterrupted training are required upon hire
- Ability to work well within a team
- Excellent interpersonal, oral and written communication skills
- Self-motivated with high level of initiative
- Worker characteristics are normally acquired through completion of an undergraduate 4-year degreed program, completion of an in-house casualty training program, and at least 6 months related experience; or equivalent combination of education and experience
- Requires knowledge of established Company policies and procedures, with emphasis in claims operations
- Written and verbal communication skill to effectively and professionally negotiate with claimants, insureds, attorneys, etc
- Work is of a technical nature and requires the analytical ability necessary to analyze, interpret and evaluate relevant information essential in resolving low to moderate value, liability and bodily injury claims
- Requires critical attention to detail and good organizational skills to manage a high volume of claims
PIP Claims Specialist Resume Examples & Samples
- Worker characteristics are normally acquired through completion of an undergraduate 4-year degree program, completion of an in-house training program, and at least 6 months of related experience; or equivalent combination of education and experience
- Requires ability to acquire basic knowledge of established Company policies and procedures, with emphasis on claims operations
- Professional written and verbal communication skills, including presentation skills, to effectively and professionally communicate with claimants, insureds, attorneys, medical professionals, etc
- Requires team building and customer relationship skills
- Work is of a technical nature and requires the analytical ability to analyze, interpret, and evaluate relevant information essential in identifying an appropriate treatment plan and resolving payment for such a plan and/or for lost wages
- Requires some exercise of independent judgment which may have significant impact on the Company in areas such as costs, consumer loyalty, and legal complications
- Requires critical attention to detail, ability to prioritize, and good organizational skills to manage a high volume of claims
- Requires basic skills in MS Word and Excel
- Experience in a medical bill processing environment, including use of related software is preferred, but not required
- General knowledge of Workers' Compensation claims is preferred, but not required
Complex Claims Specialist Resume Examples & Samples
- Effectively evaluate and resolve coverage issues for all lines of business and all liability claim types
- Investigate the claims through telephone, written correspondence, and/or personal contact with claimants, attorneys, insureds, witnesses and others having pertinent information
- Effectively and efficiently manage vendors and expenses
- Timely analyze information in order to evaluate assigned claims to determine the extent of loss, taking into consideration contributory or comparative negligence. Assign medical or other experts to case and arrange for medical examinations when necessary
- Effectively evaluate, negotiate and resolve claims within delegated authority utilizing the appropriate denials or releases
- Provide required reports to claims, underwriting, reinsurance and actuarial on significant exposure cases
- Report on all cases going to trial on a timely basis and attend portions of trials when warranted or where requested by management
- Ensure proper referrals and timely updates to appropriate Reinsurer(s)
- Ability to handle or oversee Extra-Contractual, EPLI, Social Services and E&O claims against the Company
- Multi-State licensing with strong understanding of Medicare reporting & compliance preferred
- Experience in complex coverage analysis and significant large loss evaluations
- Superior communication and strategic negotiation and claim disposition skills along with proven problem-solving skills
- Moderate proficiency with standard business-related software (including Microsoft Outlook, Work Excel, and PowerPoint
- Sufficient keyboarding proficiency to enter data accurately and efficiently
- 8+ Casualty claims handling experience (of those, a minimum of 5 years handling cases of a complex nature with a primary P&C carrier)
- Must have demonstrated core competence as a Claims Specialist Int or Claims Generalist Int negotiating injury claims
- Ability to quickly build rapport and successfully effect settlements
- Bachelor's degree or a minimum of 6-10 years of relevant work experience and/or postsecondary education
- Company-provided Cell Phone - during work hours
- Provide first-line assistance for member's questions relating to post-service coverage of medical treatment or services which includes researching and resolving benefit claims issues, billing discrepancies, coding errors, insurance claims processing issues, and educating members on the components of their benefit plan coverage which ensuring adherence to corporate and department policies and procedures
- Research plan information and identify where there may be conflicting information which may include escalating to supervisor or other levels of management for clarification and assistance
- Assist members with setting up payment arrangements and discounts which may include reaching out to healthcare providers to determine payment options
- Handle cases that require complex coordination of benefits issues among several carriers (e.g., motor vehicle, Medicaid, Medicare due to disability, disability administrator, etc.)
- Minimum of five years customer service, healthcare, or claims experience required
- Medicare A, B, MediGap, Supplement plans, Medicare Advantage, Medicare Part D plans
- High deductible health plans including Health Reimbursement Accounts (HRAs) and Health Saving Accounts (HSAs)
- Flex Spending Accounts (FSA) , including limited FSAs
- Coordination of benefits and which plan is primary - simple and complex cases (commercial plans, Medicare plans)
- Summary Plan Documents (SPDs) and Certificates of Coverage (COCs)
- Government programs, resources and legislation and mandates including but not limited to Affordable Care Act, FMLA, Medicaid, CHIP
- Group Health Plans (fully insured and self-insured)
- Pharmacy benefits including injectable medications
- Individual Health Plans and Exchanges plans
- Optimizes Work Processes
- Instills trust
- Cultivates innovation
- Decision quality
- Collaborates
- Minimum 1-2 years post-secondary education or equivalent experience [Minimum 1-3 years disability, workers comp, or waiver of premium claims experience]
- Excellent verbal and written communication skills including professional telephone skills
- Microsoft Office Suite
- Ability to multi-task and prioritize workload in a workflow environment
- Business Acumen: Appreciation and understanding of the financial services industry in order to make sound business decisions
Life Claims Specialist Resume Examples & Samples
- 1+ years claims experience (life insurance claims is preferred)
- Proven analytical and problem solving skills and attention to detail
- High level of compassion and commitment to customer service
- Learning Agility: Openness to new ways of thinking and acquiring new skills to retain a competitive advantage
- Identifying, monitoring and reporting on emerging liability and coverage trends
- Broad surplus claims experience: minimum of 5 years of experience managing claims. Experience in the handling and management of general liability, contracting, premises liability, products liability, and excess liability claims preferred
- Collaborative approach: Develop productive working relationships with insured, brokers, claim handlers, Underwriters and legal counsel. Seek input from others as needed to achieve the best result possible. Capable of working and collaborating with a virtual team
- Possession of state adjuster licenses is preferred. Insurance designation(s) (CPCU, AIC, ARM) preferred
- Minimum of 3 (or more) years of solid experience handling Professional Liability claims to include Lawyers and Accountants E&O, Insurance Agent E&O, Miscellaneous E&O, and other specialty areas preferred
- Strong knowledge of the insurance industry, claims, and the insurance environment
- Possesses a functional and developing knowledge of multi-state legal statutes and procedures
- Law degree preferred
- Professional Designations preferred
- Helps develop and execute the strategies for large accounts to help identify coverage based on applicable policies, manage claims and overall programs in conjunction with WTW safety and service teams
- Directly handles clients as primary consultant including complex consulting and strategy
- Maintain direct relationships with key clients
- Manage the appropriate level of resources for your clients
- Participate in strategic large client meetings as required
- Extensive experience of handling multi-line claims with focus on general liability claims of a complex nature. Experience with additional lines including property, construction defect, and/or workers’ compensation claims would be a benefit
- High School diploma and college degree required
- Travel required, primarily within Denver, Phoenix, and California
Priority Claims Specialist Resume Examples & Samples
- Attention to detail with the ability to quickly identify trends
- Working knowledge of the Medicare audit, appeals, reimbursement, Local Coverage Determinations (LCDs), and policy articles
- Working knowledge of medical terminology
- Self-starter / take initiative to proactively resolve problems
- Strong sense of personal accountability to meet deadlines
- Working knowledge of MS Office suite programs
- Working knowledge of Electronic Health Records (EHR); such as, OPS and NextGen
- Demonstrated ability to pull data and migrate into online records management systems such as OnBase
- Demonstrate high ethical standards regarding confidential patient and billing information
- Process detail billing from provider for complete required data elements and assure all data is captured correctly in the payment system before releasing payment
- Accurately assign pay/deny codes and verify the associated charges for services provided
- Understand contractual expectations with network providers to assure compliance with terms and expectations
- Maintain confidentiality at all times whether in reference to confidential information or as it relates to medical information for specific patients
- Create reports and meet deadlines for reimbursements
- Identify any inconsistent billing practice or methodology for further review. Forward identified transports to audit area for further investigation
- Meet daily productivity quotas on a consistent basis
- Demonstrated familiarity with Medicaid terminology and services
- Previous experience in claims processing preferred
- Must be proficient with Microsoft Office software
- Must type 30 wpm
- Must operate 10-key calculator by touch
- Must have effective oral, written and interpersonal communication skills
- Daily claims processing
- Understanding of Section 125 administrative processes and procedures
- Understanding of HIPAA and Privacy Regulations
- 1Cloud, Excel and OnBase experience preferred
- Meets daily deadlines consistently
- Must take initiative in jobs performed
- Flexibility/ adaptability
- Sets activities, reserves and authorizes payments within scope of authority. Ensures issuance of disbursements while managing loss costs and expenses
- Coordinates and performs investigations and evaluates claims and suits through contact with insureds, claimants, business partners, witnesses and experts. Seeks early resolution opportunities. Identifies files that have potential fraud and refers to SIU
- Utilizes negotiation skills to develop complex settlement packages
- Identifies claims with third party recovery potential and coordinates with subrogation/salvage unit
- Partners with attorneys, account representatives, agents, underwriters, doctors, nurse case managers and insureds to develop a focused strategy for timely and cost effective resolution of more complex claims
- Strong interpersonal, communication and negotiation skills. Ability to effectively interact with all levels of CNA's internal and external business partners
- Ability to exercise independent judgement and make critical business decisions effectively assessing the merits of claims as well as evaluating claims based on a cost benefit analysis
- Typically a minimum three to five years claims experience
Senior LTD Claims Specialist Resume Examples & Samples
- Independently assess, analyze and render appropriate claim decisions pursuant to certificates on most complex claims
- Clarify functional capacity through independent problem solving measures and discretion (gathering medical, vocational, and other information, efficient use of resources, and action planning) sufficient to determine initial and ongoing liability
- Communicate clearly and concisely to influence return to work, discuss terms of the certificate, and the basis for payment/non-payment
- Communicate with a variety of constituents (for example, claimants, doctors, nurses, employers, and attorneys) to gather information relevant to assessing, analyzing and rendering decisions based on the provisions of the policy and their own discretion, with limited guidance by supervisory personnel
- Provide mentoring and/or coaching to less experienced team members, and handle more complex claims
- As the sole owner of the LTD claim, determine return to work potential and strategy, identify a likely claim progression based on the facts of the claim and take action on their own assessment of the claim
- 5+ years’ long term disability claims experience
- Ability to prioritize and maintain quality
- Confirm coverage and policy information
- Initially establish and maintain proper loss reserve, and negotiate loss settlements
- Conduct in-house investigation by taking recorded statements, ordering police reports, reviewing repair estimates, securing medical reports, etc. Attend necessary meetings or appearances on assigned claims as directed or approved by Supervisor
- Keep Supervisor advised of significant developments in claims. Prepare required reports and other notices in a timely manner
- Be familiar with and comply with all applicable provisions of Tokio Marine's Employee Handbook
- Answer correspondence and inquiries promptly from brokers/agents, insureds, claimants, attorneys, outside vendors, TMM-employees, etc
- Perform special projects and other duties as may be assigned
- Four to five years of experience
- Knowledge of tort law, motor vehicle law, basic reinsurance, and coding related to claims technical matters
- Ability to negotiate settlement of claims in a timely and reasonable fashion
- Reconcile claims filed to payments received on Investor and Mortgage insurance claims. Prepare claim payment reconciliation to ensure full payment is received
- Determine root cause of curtailed items and determine whether supplemental claim, client expense or loss has been incurred
- Update the system with pending, submitted, withdrawn and paid claim information
- Stress Management: The ability to keep functioning effectively when under pressure and maintain self-control in the face of hostility or provocation
- Helping to implement the general corporate strategy and adapt it to his/her specific work domain
- Keeping professional knowledge permanently up to date in order to anticipate what is coming and to
- Follow-up on trends in the health care market
- Active language knowledge of at least English and French
- An extra language may be required, depending on the contracts assigned
- At least 5 years of relevant work experience
- Solid knowledge of administrative processes and customer services
- Advanced knowledge of Microsoft office - and own IT- applications
- Sociable: correct, professional and at ease in contact with different stake holders (clients, colleagues,
- Team members, superiors, …)
- Organisational skills: is able to plan, prioritise and coordinate tasks in an efficient way
- Accurate: accurately controls own work and work of team members in order to achieve faultless administration
- Analytical: is able to invent, set up and evaluate procedures to achieve the fixed targets
- Decisive: is able to set clear targets for him/herself and appropriate targets for his/her team members and takes decisions autonomously
- Empathic: is able to imagine oneself in the situation of or see the point of view of others
- Managerial skills: knows how to motivate and evaluate a team, how to delegate tasks in an efficient way and how to stimulate cooperation in his/her own team and also with other units and departments
- Independent: is able to work independently
- Pro-active and problem-solving: anticipates in a creative way expectations of clients and expectations of the company and formulates proposals for appropriate improvement
- Writing skills: conveying clear and to-the-point messages in the appropriate style
- Responsible: takes care that the assigned tasks are followed up in a dutiful, timely and correct way
- Discipline: pays attention to procedures, agreements and document flows
- Efficient: finds a good balance between quality and quantity
- Discreet: works discreetly with confidential (medical) information
- Manage claims to appropriate closure while providing excellent customer service
- Provide timely and accurate claims administration in keeping with client contracts and within applicable state laws
- Respond to requests by mail or telephone from clients, internal staff, claimants, medical providers and adjusters
- Adhere to high standards of professional conduct while providing superior claims service
- Responsible for conducting employee, client and internal contact on all assigned claims
- Work closely with business units to gather claim related information
- Review new claim reports and determine the most effective handling procedure for each individual claim
- Assist with preparation of files for suit, trial, or subrogation
- Respond to all voicemail, e-mail, and faxes associated with assigned claims
- Maintain an effective diary on all assigned claims, to include departmental and personal calendars
- Maintain current knowledge of assigned insurance lines and court decisions which may impact the claims function
- Submit First Report of Injury to the carrier and/or TPA with appropriate tracking designations and in keeping with deadlines
- Identify potential fraud through validation of claims information
- Make outbound calls to carrier, injured employee & health care providers to obtain work status and case notes
- Receive and respond to inbound calls from clients, claimants, adjusters and System One staff
- Process, review, and adjudicate claims in an accurate and timely manner
- Review files for accuracy, file completeness, and eligibility for coverage
- Objectively assess claim and create an evidence-based case management plan with ongoing monitoring of progress to ensure quality and appropriate handling
- Implement case management plan through communication with internal and external customers, medical providers, and third party vendors
- Maintain excellent working relationship with internal and external customers
- Problem solving in a team environment
- 1-3 years Disability, workers comp, or waiver of premium claims experience preferred
- Knowledge of diagnosis and procedure codes, general medical terminology, and disability duration guidelines preferred
Senior STD Claims Specialist Resume Examples & Samples
- Manages assigned caseload of STD claims
- Decides payment period, follows up and monitors payment accuracy and timeliness
- Follows established claim policies and practices to resolve claims and issues
- Strong Letter writing/Microsoft Word
- 2-4 years Customer Service Background
- Analyze and determine claims payment in an accurate and timely manner
- Maintain excellent working relationships with internal and external customers
- Participate in problem solving activities in a team environment
- Ensuring the claims contain recent clinical analysis and occupational information at that point
- Deliver Customer Centric Service that is consistent with or exceeds our customer commitments and superior reputation
- Proactively communicates with the claimant to set expectations, assess medical and non-medical barriers to return to work, and keep him or her fully aware of the status of the claim, including setting expectations with the claimant if other resources will be contacting him/her
- Engage the Employer, Attending Physician, and other appropriate resources to efficiently and effectively gather information with the least amount of impact to the claimant
- Provide a high-level of service to the claimant, including delivering on commitments, timely return of phone calls, and clear communication
- Consistently assess claimant information and medical data to minimize disruption to benefits and ensure ongoing engagement with the customer
- Prioritize and organize work with a focus on Claim Management Accuracy. Proactive action to obtain any information, including medical, and extend benefits to medically supported date
- 3 plus years claims experience or relevant business experience preferred
- Bachelor’s Degree or Associate’s degree preferred
- Contact and establish a rapport with customer, injured party or property owner to obtain information. Comply with 24-hour contact requirements
- Obtain all relevant facts to determine coverage, liability or compensability on claims files
- Determine and analyze damages through appraisal, inspection and investigation
- Utilize and manage experts to determine facts, damages and exposure, ensuring that the value of the service is greater than the cost
- Evaluate information to assess proper resolution of claims to determine appropriate and fair payout
- Negotiate settlement based upon strategies and plans that ensure appropriate fair settlement of the claims
- Provide customer satisfaction by establishing a rapport with customers and by resolving issues
- Comply with Quality Validation, TAACC instructions, Customer Service Manual, Information Security procedures and the Tokio Marine SIU program
- Determine subrogation and salvage potential of claims
- Handle No-Fault/PIP claims
- Utilize inter-company arbitration to resolve claims, as well as, use of mediation, settlement conferences and alternate dispute resolution (ADR)
- Communicate and work with both internal and external customers
- Handle automobile bodily injury, property damage, product liability and general liability claims
- Establish and monitor indemnity and expense reserves on claim files
- Keep updated on important developments in tort and insurance law
- Four-year college degree preferred
- Five years or greater Property/Casualty claims experience required
- Knowledge of specific line of business required – automobile, liability
- Japanese Language a plus
- Ability to negotiate first and third party claims required
- Computer knowledge, especially Microsoft Word and Excel, desired
Senior General Liability Claims Specialist Resume Examples & Samples
- New York Labor Law Construction claims handling experience
- 7 or more years of claims handling experience
- Negotiation skills
- Maintain production and quality standards
- Investigate claims for required processing information
- Must have previous experience processing medical claims, not just knowledge of
- Medical terminology & Medicare experience desired
- Manages assigned caseload of short-term disability (STD) and/or Family & Medical Leave Act (FMLA) claims
- Determines whether to return, pend, deny or pay claims. Inputs data
- Evaluates claimant eligibility via information received from claimant, attending physician, and employer
- 2-4 years of experience in claims or customer service
- Strong customer satisfaction focus
- Coordinate with team members and escalate as appropriate to ensure timely and quality execution of activities in one or more pre/post foreclosure area(s), in compliance with applicable guidelines, to minimize reputational impact to Fannie Mae and ensure optimal resolution for business unit and vendor
- Partner with internal and external parties via in-person meetings, phone calls and emails to resolve escalated or time sensitive collection issues and ensure an ongoing understanding of changes to processes/guidelines and related impacts. Maintain partnerships and facilitate open dialogue
- Study, review and measure processes and guidelines of assigned business unit(s)/vendor(s); examine documentation and flow of work through systems and address any perceived gaps
- Receive collection issues from assigned business unit(s), input into appropriate systems and monitor and track through to full resolution. Update systems regularly to insure most recent collection activity is tracked
- Participate in process improvement activities by suggesting ways to realize process efficiencies based upon feedback and observations. May assist in the implementation of new or revised processes and procedures
- Develop both regular and ad hoc reports to monitor business unit/vendor production trends. Distribute reports to appropriate audiences or summarize findings for inclusion in other reports/presentations
- May provide training to internal and external groups
- Ability to navigate through multiple systems
- Reverse Mortgage Claims experience a plus
- Strong collaboration and communication skills to partner with internal and external customers
- Worker characteristics are normally acquired through completion of an undergraduate 4-year program. At least 2-years related experience might substitute for educational requirement
- Good written and verbal communication skills to effectively and professionally negotiate with claimants, insureds, attorneys, etc. Solid comprehension of basic principles and practices of Company policies and procedures upon completion of formal training period
- Work is of a technical nature and requires the analytical ability necessary to analyze, interpret and evaluate relevant information essential in resolving claims
- Requires critical attention to detail and good organizational skills
Senior Complex Claims Specialist Resume Examples & Samples
- Works on highly complex investigations of claims, analyzes coverage, liability, compensability and damages. Determines if a major claim should be settled or litigated
- Manages all types of investigative activity on major claims. Coordinates discovery and litigation strategy with staff counsel or panel attorneys
- Negotiates highly complex settlement packages, sets reserves and authorizes payment within scope of authority, settling claims in most cost effective manner and ensuring timely issuance of disbursements
- Coordinates third party recovery with subrogation/salvage unit
- Makes recommendations on claim management policies and processes to management
- Analyzes claims activities; prepares and presents reports to management
- Works with attorneys, co-carriers, brokers and insureds regarding the handling and/or disposition of highly complex claims
- Keeps current on state/territory regulations, case law and issues, as well as industry activity and trends. May participate in industry trade groups
- May provide guidance and assistance to less experienced claims staff and other functional areas, including ceded reinsurance
- May be responsible for special claims projects and presentations
- Bachelors and Juris Doctorate (JD) Degrees and preferably bar admission in at least one jurisdiction
- Ten years of general liability claim adjudication/management experience with an emphasis on the adjudication of asbestos, environmental liability and other types of toxic torts claims
- Advanced technical expertise related to CGL policies, claims resolution skills and knowledge of insurance and claims settlement principles, practices and procedures
- Strong communication, negotiation and presentation skills. Ability to effectively interact with all levels of the company’s internal and external business partners
- Advanced analytical and problem solving skills, with the ability to manage and prioritize multiple projects
- Ability to deal with ambiguous situations and issues
- Conducts research when needed to resolve customer questions or complaints
- Able to appropriately explain varying plan provisions to customers accurately and in a professional manner
- Responds to telephone inquiries from insured’s regarding specific claim details
- Understands processes within entire department to assist callers with questions
- Outbound calls and letters to customers and providers to research incomplete claims
- Escalates complaints and potential complaints appropriately
- Documents calls in computer system
- Complete form letters, tasks and problem solve for resolution of customer issues
- Contribute ideas that enhance service quality
- Performs project work and other related duties as assigned or required
- 2+ years direct customer service experience
- Provide state unemployment claims support to ADP TotalSource clients, regions, state agencies and third party administrator
- Serve as the unemployment claims subject matter consultant and third party liaison
- Council clients on state unemployment claims matters including the use of state work share and back to work programs
- Interprets state unemployment claims laws and enforce employee separation documentation requirements
- Identify areas of improvement and noncompliance that impact claim cost control efforts
- Provide recommendations and collaborate with HR Business Partners to implement solutions that improve client claims management and compliance with UI integrity regulations
- Respond to state agency and third party administrator claims, appeals, and benefit inquires as required by state unemployment law and TotalSource processing procedures
- Interpret state unemployment claim laws and council clients on contestable unemployment claims and appeals daily. Provide support and assistance on unemployment claims matters
- Partners with clients and HRBPs to identify and address areas of improvement and noncompliance that impact cost control efforts
- Audit employee termination documents and provide accurate and timely responds to state agencies and third party administrator inquires related to unemployment claims, appeals and hearings
- Obtain missing separation documents for contestable terminations in compliance with state UI Integrity regulations
- 1-3 years of directly related experience
- Experience with HR or unemployment adjudication, hearings, claims, terminations, or disciplinary actions
- Ability to work under pressure to meet time constraints and deadlines
- Ability to deal with escalated issues
- Ability to work and research independently
- PHR/SPHR/SHRM-CP
- Keeping professional knowledge permanently up to date in order to anticipate what is coming and to evolve in line with company growth and expectations of clients
- You are mobile when required (rare but important)
- Discrete: works discreetly with confidential (medical) information
Senior Claims Specialist Provider Verification Resume Examples & Samples
- Provider Verification Expiration Report- update providers license/credentials that we are currently paying claims
- Works closely with the claim analysts and care managers to provide a seamless customer experience
- Outbound calls and letters to customers and providers to research incomplete claims. Escalates complaints and potential complaints appropriately
- Completes form letters, tasks and problem solve for resolution of customer issues. Contributes ideas that enhance service quality
- Answers telephone inquiries through the “Automated Call Distributor (ACD) Telephone System”
- Verifies and interprets information in all vendor contracts to resolve caller issues
- Ensures the average call monitoring score over the previous six months meets or exceeds quality standards
- Troubleshoots claims that require an authorization
- Updates authorization information based on information obtained from caller
- Processes simple HCFA claims and performs simple claim adjustments as needed
- Tracks progress of resolution of claims issues and routes resolved claims back to the appropriate person in Claims
- Ability to make decisions with every call and resolve issue on first call
- Familiarity with managed care industry, standard claims forms, ICD-9 and CPT codes
- Ability to process simple professional claims as needed
- Provide high quality cost effective adjudication services which meet or exceed expectations provided to customers and are in accordance with the terms outlined in the certificate of insurance
- Manage a block of Life and Disability mortgage creditor claims in accordance with consistent claim guidelines, in conjunction with the appropriate medical and claim consultants, within your authority levels and in accordance with the terms of the certificate of insurance. Be alert for fraud or misrepresentation and take necessary steps to verify and resolve where detected. Refer all claim decisions which can affect our liability, approvals, closures, denials, etc. to the Claim Consultant for sign off and approval before proceeding
- Adjudicate claims for misrepresentation, fraud and certificate exclusions
- Evaluate medical, employment and mortgage lender documents to determine whether the life or disability claim is eligible. Administer and document claims for assessment of continued eligibility for disability benefits, return to work, bridge payments to the lender while the life claim is being assessed and all requests for additional information
- Prepare all written correspondence, including, requests for additional information, communication of decisions, etc
- Maintain a sound knowledge of products, procedures, systems, contract wording and claims management
- Meet objectives and service standards by working with the Manager to ensure that team goals are met
- Process applicable accounting and financial transactions associated with payments and the setting of reserves
- Previous experience in adjudicating Life and/or Disability claims
- Excellent interpersonal skills with exceptional oral & written communication skills
- Demonstrated experience interpreting contractual, medical, financial and legal provisions, by utilizing the appropriate Consultants and fair claim practices and principles
- Sound judgment and dispute resolution skills
- Must have a good working knowledge of medical conditions and terminology
- Must have a good working knowledge of financial documents
- Ability to respond constructively and decisively in high pressure or emotional situations and to respond quickly and positively to change
- Excellent analytical skills in order to evaluate conflicting information from various key sources in order to assess risk in making timely and effective decisions with appropriate interpretation of policies and procedures
- Strong organizational, conceptual, investigative and analytical skills; ability to gather information from key sources to assist in claims decisions and problem solving
- Personal style should reflect the high level of professionalism which Manulife projects to our customers
- Ability to work independently and as part of a high functioning team
- Ability to deal with sensitive and confidential information
- Administer the self-insured, self-administered general liability, automobile and facility property damage, to both company and other facility owners in the claim process, including collection for damage done by others to Company vehicles and equipment and company facilities
- Collect for damage to Company owned facilities by others as invoiced by the Company
- Prepare interrogatory answers and produce documents for lawsuits involving the Company
- Investigate incidents, claims, and lawsuits on site
- Type/write reports and gather records
- Appear in Small Claims Court on behalf of the Company, if appropriate in the jurisdiction
- Facilitate awareness programs for other departments
- Prepare company witnesses for deposition and/or trial
- Investigations within the Company territory could involve some travel
- Gather the appropriate company and public records, i.e., police, fire reports, etc., as needed
- Enter appropriate claim data into the NavRisk system
- Maintain a high level of professional ethics and compliance
- Strong interpersonal skills with the proven ability to build and establish rapport with a diverse array of people
- Ability to work as part of a team and display a positive attitude for this dynamic environment
- Two years of experience with customer contact, both by telephone and in person preferred
- Two years of experience responding to incidents and/or performing on scene investigations preferred
- Two years of experience with/field knowledge of a gas distribution system preferred
- Certified Fire Investigator preferred but may be obtained
- Strong ethics and integrity, dedication to a safe work environment and commitment to a diverse workforce that recognizes and respects every individual’s unique skills and perspectives
- Knowledge of basic PC skills, with an understanding of Microsoft Excel, Word & Outlook and PowerPoint
- Good telephone skills - Ability to communicate effectively orally and in writing
- Must possess the attitude and abilities to develop new skills and areas of expertise
- Must be willing to undertake a program of continuing education regarding matters unique to legal/claims
- Ability to perform work for more than one person simultaneously
- Effective planning, organizational , administrative and prioritization skills in managing the work load
- Strong interpersonal skills with an emphasis on initiative, knowledge sharing, teambuilding and independent decision-making
- Ability to work effectively with all levels throughout the organization and across functional lines
- Analyzes and processes complex or technically difficult medical malpractice claims by investigating and gathering information to determine the exposure on the claim; manages claims through well-developed action plans to an appropriate and timely resolution
- Conducts or assigns full investigation and provides report of investigation pertaining to new events, claims and legal actions
- Negotiates claim settlement up to designated authority level
- Calculates and assigns timely and appropriate reserves to claims; monitors reserve adequacy throughout claim life
- Recommends settlement strategies; brings structured settlement proposals as necessary to maximize settlement
- Coordinates legal defense by assigning attorney, coordinating support for investigation, and reviewing attorney invoices; monitors counsel for compliance with client guidelines
- Uses appropriate cost containment techniques including strategic vendor partnerships to reduce overall claim cost for our clients
- Identifies and investigates for possible fraud, subrogation, contribution, recovery, and case management opportunities to reduce total claim cost
- Represents Company in depositions, mediations, and trial monitoring as needed
- Communicates claim activity and processing with the client; maintains professional client relationships
- Delegates work and mentors assigned staff
- In-depth knowledge of appropriate medical malpractice insurance principles and laws for line-of-business handled, recoveries offsets and deductions, claim and disability duration, cost containment principles including medical management practices and Social Security application procedures as applicable to line-of-business
- Responds to customer inquiries, according to productivity and quality standards. Strives to return all voice mail, email and chat messages within contact center expectations
- Support the potential claimants through the registration process and the assessment/background/medical questionnaires in the new consumer market product
- Support claimants through the use of Allsup Place and empower questionnaires throughout entire process
- Understand and support sales process
- Accesses claimant’s record on the system (past notes, completed fields, actions); interprets, gathers, and conveys information to the caller (claimant, Social Security Administration, Disability Determination Service, Office of Disability Adjudication & Review)
- Reviews claimant completed questionnaires and follows up with claimant for additional information, if needed, prior to submitting forms to Social Security and/or Disability Determination Services
- Interviews claimants by telephone to complete application, appeal, questionnaire and ancillary forms, ensuring appeal deadlines are met
- Place outgoing calls to gather information from claimants
- Accurately and fully records the claimant’s description of the disability onset, medical condition, medical sources, functioning, and vocational history. Resolves discrepancies as necessary
- Strives to produce quality work that contains correct grammar, spelling, punctuation, and follows guidelines in “Allsup Style Guide”
- Diligently pursues contact with the claimant and initiate emails and/or letters to the claimant to ensure every opportunity was taken to reach the claimant
- Demonstrates technical knowledge and application with respect to the first two levels of Social Security disability process. Must have thorough knowledge of functions of all Allsup departments. Provides claimant insight to the process and program requirements
- Establishes, cultivates, and maintains a positive and professional relationship with the claimant, while utilizing call management skills
- Responds to claimant questions with courtesy, empathy, and professionalism. Demonstrates tact and diplomacy in handling problem solving situations with claimants, Social Security Administration, Disability determination Services and employees
- Performs vital data entry in case management system. Accurately and thoroughly document talk notes of all conversations and actions
- Processes work in a timely and accurate manner
- Participates in the training and development of other specialists; shares information
- Maintains strict confidentiality of claimant information, procedural manuals, client/prospect lists, information on new business ventures, and other confidential Allsup information
- Obtains information regarding other services/programs that might be helpful to the claimant such as health insurance assistance, Medicare, state funded programs (welfare) and other local resources
- Ensures timely, accurate and efficient processing of claims edits via EPIC work queues
- Meets daily claims edit resolutions goals by reviewing, analyzing, and obtaining appropriate documentation based on payer requirements and regulations
- Prepares electronic and paper claims and sends with appropriate attachments
- Conducts research and provides updates and current status of claims edit work queues using the appropriate data management system (EPIC)
- Resolves issues that are adversely impacting claims submission in a timely and accurate manner
- Completes or requests adjustments to accounts based on dollar threshold
- Communicates information and ideas to make system-wide process improvements
- Updates patient accounts regarding changes and modifications in plan benefits and other contract information relevant to the claims follow up and collection process
- Documents claim processing activity on patient accounts
- Serves as a communication link to various departments and external payers by developing positive relationships with managed care organizations and outside agencies, and clinical areas within the
- Assists with education of internal staff and external customers to bring about the timely, accurate, and cost effective adjudication of all claims
- Works collaboratively with other departments to facilitate the insurance collections process and to improve overall cash collection
- Monitors the status of claims in work queues and conducts routine, periodic follow up on previously researched claims items
- Monitors, reviews, and suggests revisions or updates to existing forms, documents, and processes required to submit a clean claim
- Assists other departments/functional areas as needed with billing, claims, or claims follow up related tasks
- Ensures completeness of claims by following national, local, and internal billing requirements promoting prompt and accurate submission and payment
- Maintains awareness of current regulations
- Initiates practices that support current regulations
- Shares knowledge of current regulations with staff. Analyzes current practices and makes recommendations for process improvements
- Using strong technical skills, handle the complex and challenging claims within authority level and specialization. The Claims Specialist main specialization would be Equipment Breakdown, with Energy & Construction losses included to balance the workload
- Partner with internal and external counsel in setting and pursuing effective and cost-efficient litigation strategies for claims in litigation
- Work with management and Claims Legal to identify and select appropriate counsel
- Proactively manage expenses through thoughtful expense management and claims best practice
- Active participant in Quality review process
- Seek to identify new and improved processes. Embrace short and long-term improvement initiatives, and actively participate to understand and embed any new initiatives
- Coordinate and manage communication with internal and external stakeholders (e.g., underwriting, brokers, reinsurers, external vendors, etc.) to ensure the highest level of customer service
- Produce internal reporting in support of best practice and reserving guidelines
- Identify, monitor and report on emerging liability and coverage trends
- Keep current on state/territory regulations and issues as well as industry activity and trends
Lost Time Claims Specialist Resume Examples & Samples
- Actively participate in claim reviews with clients
- Appropriate state licensing to be obtained for assigned jurisdictions
- Assign medical or other experts to case and arrange for medical examinations when necessary
- Communicate claim status with the injured worker, clients, and broker as needed
- Develop lost time claim disposition skills under limited direction of supervisor
- Effectively evaluate and resolve coverage issues for all Workers' Compensation claim types
- Establish appropriate reserves and review on a regular basis to ensure adequacy. Make recommendations to set reserves at appropriate level for claims outside of authority level
- Investigate the claims through telephone, written correspondence, and/or personal contact with claimants, attorneys, clients, witnesses and others having pertinent information
- Manage the litigation process through the retention of counsel. Adheres to the line of business litigation guidelines to include budget, bill review and payment under limited direction of supervisor
- Pro-actively manages the case resolution process. May participate in mediations within limit of settlement authority
- Provide required reports to AVP, Claims, Underwriting, Reinsurance and Actuarial on significant exposure cases
- Timely analyze information in order to evaluate assigned claims to determine the extent of loss
- Bachelors and/or advanced degree. (Minimum of 3-5 years of lost time claims experience will be considered in lieu of degree)
- Minimum of 2 years of workers compensation lost time claims handling experience
- Intermediate knowledge of law and insurance regulations in various jurisdictions
- Demonstrated strong analytical and decision making skills
- Intermediate knowledge of claims handling concepts, practices and techniques, to include but not limited to coverage issues, litigation management, and product line knowledge
- Previous experience with the reserving and adjudication of the following: Workers compensation lost time claims Workers compensation claim investigations (including subrogation) and compensability decisions
- Understanding of local, state and industry standards (NCIS)
- Working knowledge of Microsoft Office suite, general computer software and database systems
- Evaluate project outcomes through analyzing current state and desired future state
- Handle complex claims using a logical approach
- Provide adjusters detailed instructions for claim procedures and company policy
- Solve day-to-day problems, using critical thinking
- Must be flexible and able to prioritize tasks. Ability to meet deadlines
- SAP experience is an asset
- Must have excellent interpersonal skills with the ability to interact with high credibility at all levels of the organization
- Must have strong negotiation and decision making skills
- Review and approve or deny claims for payment
- Determine which reinsurer holds the liability for a claim, and the amount ceded to that reinsurer by referring to the reinsurance treaties, and the group contract
- Review and verify all policy provisions, to determine if payment can be made. Approve claim for payment, and forward, if needed, to the appropriate officer or manager for second approval according to our approval guidelines
- Review and process all continuance requests for disability claims
- Arrange payment plans with claimants that are overpaid on their benefits
- Check monthly figures on all claim accounts with appropriate company records and accounts
- Research all complaints from State Insurance Departments regarding claims
- Work with all levels of the AICK staff in making changes in our existing contracts and assist in developing new products
- The work requires a great amount of concentration and the ability to use a PC 80-85% of the day. Mental fatigue is associated with a position of this nature. Primary contact for all life and disability claims. This position experiences constant interruptions
- Minimum of LPN, Certified Nurses Aid or Certified Medical Aid with two or more years clinical experience; or 60 hours course work towards a degree in a medical field to include courses such as Human Anatomy, Biology and/or Medical Terminology required
- Ability to analyze detailed contract provisions and make decisions based on a set of facts or criteria
- Excellent written and verbal communication skills. Must be able to communicate tactfully and accurately with physicians, attorneys, judges and other professionals
- Experience with Word, Excel, Lotus and Access is required
- Extensive knowledge of Kansas Insurance Department regulations for life and disability products preferred
- Extensive knowledge of ERISA/FICA regulations preferred
- High aptitude for math
- Within prescribed settlement authority for line of business, establishes appropriate reserves for both indemnity and expense and reviews on a regular basis to ensure adequacy. Makes recommendations to set reserves at appropriate level for claims outside of authority level
- Prepares comprehensive reports as required. Identifies and communicates specific claim trends and account and/or policy issues to management and underwriting
- Manages the litigation process through the retention of counsel. Adheres to the line of business litigation guidelines to include budget, bill review and payment
- Pro-actively manages the case resolution process. Actively participates in mediations and arbitrations, within limit of settlement authority
- Participates in the claims audit process
- Provides claims marketing services by meeting with brokers, risk managers and reinsurers, as necessary
- Bachelors' and/or advanced degree. 7 + years claims/legal experience, with at least 2 years within a technical specialty preferred
- Advanced knowledge of claims handling concepts, practices and techniques, to include but not limited to coverage issues, and product line knowledge
- Demonstrated advanced verbal and written communications skills
- Demonstrated advanced analytical, decision making and negotiation skills
Claims Specialist / Assistant Resume Examples & Samples
- Research to find all policies held by the insured. Communicate with other Transamerica offices that might also have coverage
- Request files during the claim process (this would include ordering files from record retention and from AWD)
- Knowledge of claims process would be a benefit
- Skills Advantage Work Ready Certificate, Optional
- Above average customer service skills
- Knowledge of the claims department and other departments within the company and the other offices that form Transamerica is helpful, but not required
- Proactively manage assigned claims across the United States, while setting and implementing the case strategy for these claims under the direction of the Practice Leaders and Claims management. Ensure all documentation is present in the file, and Claim Handler Guidelines and protocols are followed
- Using strong technical skills, handle the complex and challenging claims within authority level and specialization
- As claim file owner, collaborate with Claims Manager and Practice Leaders on large and complex losses to achieve optimum file outcome for the client and XL Catlin, determine if / which external vendors to engage, and establish strategic plan with vendor, identify Large Losses and ensure all steps are taken to achieve the best outcome for the client and XL Catlin (including those claims within authority level)
- Partner with internal and external counsel in setting and pursuing effective and cost-efficient litigation strategies for complex claims in litigation
- Work with management and Claims Legal to identify and select appropriate counsel. Pro-actively manage litigation strategy on claims
- Assist Underwriters with policy review and drafting initiatives, participate in external marketing and business development activities. Share lessons learned and other identified trends to improve risk assessment and underwriting process
- Produce internal reporting in support of best practice and reserving guidelines. Follow the XL Catlin Claim Alert process
- Coach less experienced colleagues and be a role model in best practices
- Education: Bachelor's degree required, JD preferred
- Experience: Minimum 8-10 years of Construction Defect claim handling experience; working knowledge of applicable regulations; extensive experience managing, negotiating and resolving high exposure and complex claims. State Licensing in required states desired
- Analytic Skills: Possesses strong analytical skills and sound judgment
- Leadership: Role model by setting a high bar for performance, engagement and commitment. Ability to coach, develop, set expectations, evaluate and hold people accountable for delivering. Takes initiative and has the ability to lead independently
- Strong communication: Excellent verbal and written communication, collaboration, presentation and influencing skills. Able to communicate effectively with internal and external stakeholders at all levels of sophistication. Ability to work in a fast-paced environment and efficiently juggle numerous concurrent responsibilities
- Continuous Improvement Focused: Willing to ask questions and explore new ideas. Eager to learn and focused on continuously improving technical skills and XL Catlin claims capabilities
- Client-service Oriented: Focused on value at all points in the claims experience delivering on our promise to clients
- Validates member eligibility, appropriateness of claim data that is billed
- Resolve complex claims issues from providers
- Other miscellaneous duties as assigned by manager
- Knowledge of Medicare, Medicaid, and commercial claims state and federal regulation
- Demonstrated work experience meeting strict deadlines and established cycle times through effective prioritization and follow-up
- Managing assigned Professional claims across multiple jurisdictions, setting the case strategy for these claims in partnership with Regional Practice Leaders and Claims Management to take all available steps to achieve the best outcome
- Partnering with internal and external counsel in-setting and pursuing effective and cost-efficient litigation strategies for claims in litigation
- Producing internal reporting and ensuring that reserves are set according to best practice guidelines
- Coordinating and managing communication with internal colleagues and key external stakeholders (e.g., clients, brokers, reinsurers, vendors, etc.) ensuring we are providing the highest level of customer service
- 5 to 10 years of Professional claims experience managing third party and liability loss exposures
- Law degree preferred; will consider commensurate experience
- Proven experience managing all facets of claim files including analysis, investigation, evaluation, presentation and negotiation skills
- Building and refining effective working relationships with insured, brokers, claim-handlers, underwriters, co-insurers, excess and reinsurers as well as external vendors including investigators and legal counsel
- Passion for results: Approaching tasks proactively and anticipating needs. Thinking quickly and prioritizing multiple work streams without sacrificing quality. Acting with a sense of urgency
- Intellectual curiosity: A willingness to ask questions and explore new ideas. Eager to learn and focus on continuously improving technical skills
- Excellent verbal and written communication, negotiation and presentation skills with the ability to communicate and interact internally and externally with senior management, business leadership and business partners
- Seeking input from others as needed to achieve the best result possible with effective skills working with and collaborating with virtual teams
- Handling claims responsibilities with integrity and the highest standards of professionalism
- Travel is anticipated at up to 10% of the time
- Support Claims Management team for claims reporting and claims data analysis
- Troubleshoot and conduct root cause analysis of claims issues, recommend solutions and resolve issues
- Oversee all First Tier Downstream and Related Entities(FDR) issues and fallout processing
- Maintain current knowledge base of all CMS guidelines and train support staff to ensure compliance
- Identify trends and issues across the environment to ensure compliance and delivery of seamless service to members and implement solutions
- Assist with Claims System(QCARE) maintenance such as Opt-Out and Sanction list upload, generating and distributing of ClaimStat reports, Monthly Medicare Refund Reports and any additional reporting required
- Participate in and actively support all CMS claims activities, including Enterprise compliance meetings, requests, and monitoring activities
- Assist Claims management with various reports and Claims projects as needed such as Orphan Claims reports, Recovery, Invoice reconciliation, Adjustments and any other Claims projects as needed
- High School Diploma or equivalent required. Bachelors degree is preferred
- At least 2 years of knowledge of Medicare Advantage claims, systems, processes and CMS guidelines with regards to claim processes required
- At least 3-5 years of relevant work experience in a claim organization, a focus on Medicare Advantage products preferred
- Must have Microsoft Office product knowledge - including at least intermediate to advanced working knowledge of Microsoft Excel
- The ability to maintain high attention to detail
- Ability to work with all levels of matrix partners and outside vendors
- Juris Doctor and 1 or more years of experience in the Claims Handling area
- Commercial general liability claims handling experience
- Experience reviewing and analyzing coverage
Furniture / Bedding Claims Specialist Resume Examples & Samples
- Customer-oriented focus
- Excellent problem solving skills with the ability to multi-task
- Ability to work well with others and be a team player
- Flexible availability that includes one to two evenings a week and a Saturday rotation
- Provider Verification: Research providers to see if they meet requirements rules vary depending on state and policy provisions
- Research what providers are available to our insured’s based on their area of residence
- Update our administrative system
- Understands processes in entire department to assist callers with questions
- Analyze individual case information by reviewing data accessed through internal systems/platforms, from documented telephone calls or document images, to determine if the facts warrant a response
- Work as a team with our Unemployment Insurance Consultants (UIC’s) to ensure accurate and necessary information retrieved from customers is documented clearly and thoroughly into our database
- Investigate and resolve state agency concerns with supervisor, other departments and/or State Relationship Managers in a timely manner
- Perform any additional functions needed to meet the goals of the department
- Overtime may be required in order to meet state deadlines or volume demand
- Attention to detail and processing efficiency
- Previous and successful experience or familiarity with the unemployment insurance process is preferred
- Proficiency with Microsoft Office applications including Word, Excel, and Outlook
- Ability to learn and utilize associated technologies/systems
Unemployment Claims Specialist Lead Resume Examples & Samples
- Assists team where needed due to vacations, absences and fluctuations in work load
- Assists with coordinating the work load, ensuring adequate distribution of the work among available staff. Works with the supervisor to use all resources to accomplish the daily work load, by assuring each desk if fully covered
- Acts as a source for answers/guidance for employee questions and investigates through research any concerns that arise
- Assists with cross-training of employees
- Assists with checking completed and ongoing work of newly trained employees, ensuring a high level of performance
- Assists with client and/or account manager concerns, questions, and follow-up
- Assists supervisor with report generation, special projects, and teamwork initiatives
- Maintain confidentiality with manager concerning members of the team
- Successful experience and performance as an Unemployment Claims Specialist
- Proven knowledge of unemployment compensation and company procedures
- Proven experience prioritizing, organizing, and working with deadlines
- Good state-communication and problem-solving skills
- Must possess diplomatic people skills and maintain a professional mannerism while performing in a fast-paced environment
- Proven ability to multi-task and work under strict deadlines
- Ability to function independently from supervision to meet workload demand/deadlines on a daily basis
- Proficiency in Microsoft Office Applications
- Ability to type 35 WPM
- Review, analyze, and ensure timely settlement of investor and mortgage insurance claims and manage aging claims to determine status and bring to closure
- Document and maintain all systems necessary for proper claim handling and follow-up
- Research issues and obtain proper supporting documentation in a timely manner as requested by investor or mortgage insurance company
- Manage application of all claim funds received and provide additional information as necessary in order to validate all available funds received prior to claim being closed
- Monitor claim process reports to ensure all required responses are timely filed
- Complete timely audits of all assigned claims to ensure all requirements have been met, and claim process can be validated
- Knowledge of Microsoft Office – Excel, Word – computer skills should be above basic level
- Previous work with mortgage claim filing a plus
- Review, analyze, and ensure timely filing of investor and mortgage insurance claims while managing outstanding receivables of claims filed to determine status and bring claim process to closure
- Research and analyze trending, accounting data, figures and transactions with large number sets throughout the system of record and acquisitions data
- Research issues and obtain proper supporting documentation by contacting previous servicers, attorneys, taxing authorities, HOA’s and other vendors in a timely manner as requested by the investor or mortgage insurance company
- Review and analyze outstanding receivables by fulfilling outstanding document requests that is preventing payment from the investor or mortgage insurance company
- Monitor claim applications and complete timely audits of all assigned claims to ensure all requirements have been met and claim process can be validated
- General knowledge of the default process completed by foreclosure, loss mitigation and escrow
- Proficient in Microsoft Office – Excel, Word
- Proficient in 10 key skills
- 1-2 years of recent, residential, mortgage servicing experience as a team manager/supervisor
- Claims/debt cancellation experience
- Ability to meet production goals and contractual quality standards
- *Shift hours: Monday - Friday 9:00 AM - 6:00 PM
- Investigating and settling one or more of these complex claims types: liability, property and/or material damage
- Determining applicable policy coverage, evaluating damages, assessing liability, and creating applicable negotiation strategies
- Obtains and analyzing a wide variety of applicable documentation related to assigned claims, some of which may include, i.e., ISO reports, fire reports, police reports, cause & origin reports, medical reports, engineer reports, written estimates, witness accounts, etc
- Completing physical inspections of the more extensive losses (when necessary), evaluating damages, and preparing written estimates according to policy provisions and published company guidelines
- Initiating first contact with insureds, claimants, and all relevant parties to gather basic information, obtain recorded statements (when necessary), and explain the overall claims process
- Maintaining continuous communication with all affected parties regarding each step of the claims process
- Communicating and negotiating with a variety of individuals regarding investigation and settlement of applicable claims, i.e., insureds, claimants, attorneys, medical providers, insurance carriers, and other involved parties
- Acting as resident expert while providing direction, support, and training of lesser-experienced Claims Representatives
- Participating in round tabling on applicable claim files and has significant responsibility for coaching and developing employees
- Education equivalent to graduation from college (or the equivalent in related work experience)
- Maintains the appropriate adjuster's licensing as required by the states in which we do business
- Five or more years of claims adjusting experience (or the equivalent)
- Demonstrated ability to evaluate, investigate, and settle the more complex claims within higher settlement authority limits than those handled by Sr. Claims Representative
- Knowledge of insurance contracts and claims law
- Requires highly-developed oral and written communication and negotiation skills to communicate with a wide variety of internal and external contacts
- Must possess the ability to handle potential conflict effectively and constructively
- Excellent decision-making, analytical skills, and attention to detail
- Proven time management, prioritization, and organizational skills are required to handle a high volume of assigned claims within expected timeframes
- Must be comfortable with ambiguity where claims facts and circumstances may be unknown or vague
- Proven ability to multi-task while interacting effectively with financial representatives, claimants, insured’s, internal staff members, and external contacts
- Education equivalent to graduation from college with a degree in business, insurance or agribusiness (or the equivalent in related work experience)
- Previous experience handling specific claims applicable to area of specialist assignment
- Experience with the claims investigation and settlement process of one or more claims types
- Experience handling property claims, bodily injury, and/or material damage claims (including total losses)
- Good working knowledge of the policy provisions and coverage’s associated with these claims
OS&D / Claims Specialist Resume Examples & Samples
- 20% Gather documentation from carriers/customers/Business units to support claims against carriers. Sort and maintain data base tracking from initial receipt of claim to filing claim with the carrier
- 15% Collect and prepare departmental reports including claims tracking, departmental scorecard and other ad hoc reports requested by internal clients /reporting/A/R review
- 10% Initial review and analysis of claims for determination of carrier liability
- 5% Other duties as required
- Analyzes and processes complex or technically difficult Errors & Omissions claims by investigating and gathering information to determine the exposure on the claim; manages claims through well-developed action plans to an appropriate and timely resolution
- Represents Company in mediations, and trial monitoring as needed
- In-depth knowledge of appropriate insurance principles and laws for line-of-business handled, recoveries offsets and deductions, claim and disability duration, cost containment principles including medical management practices and Social Security application procedures as applicable to line-of-business
Trade Claims Specialist Resume Examples & Samples
- Process all trade related customer claims; obtain and verify supporting documentation and proof of performance, identify and select appropriate rebate or fund, conduct research and provide notification and full back-up for unauthorized deductions, and verify collection attempts prior to any write off per department SOPs and step guides
- Communicate and work closely with the third party processor, broker, sales team and other WWFC departments to resolve all deductions in a timely and accurate fashion as measured by team KPIs
- Hold periodic calls with each sales team that handles assigned accounts per management determined frequency. Ensure effectiveness through proper scheduling, management and reporting of call
- Track data, communicate issues and provide reports to management
- Identify areas for improvement in deduction processing and develop and present written recommendations for changes in policy and procedure
- Maintain and create internal reports
- Bachelor’s Degree in Accounting or related field with 0 years of transactional accounting experience OR High School Diploma or equivalent with at least 3 years of progressive transactional accounting experience (Accounts Payable, Accounts Receivable, Accounting Clerk) required
- Must demonstrate initiative to solve issues independently, consistently, and professionally
- Must have working knowledge of general accounting procedures and process including GAAP
- Must be detail oriented and possess strong organizational skills
- Strong computer skills, particularly with Excel, Microsoft Word and an e-mail system
- Ability to prioritize work, manage multiple tasks and effectively meet deadlines
- Ability to produce timely, accurate, reliable and relevant information
- 1 year CPG/food manufacturing industry experience preferred
- Bachelor’s degree in accounting or related field preferred
- Responsible for investigating and resolving claim related tickets and other types of requests including but not limited to claim reprocessings and inquiries from internal and external sources
- Provides accurate and timely maintenance of the most complex provider and reimbursement information
- Analysis of provider’s trends and issues with reported findings
- Monitor, review and release of all claims batches in the Claims Management module in FlexCare. Includes: New, Queue, Pending and plan specific claims folders
- Ensures all applicable batches are released in time for weekly check runs
- Maintains thorough knowledge of the processing requirements for each Plan
- Review and process member reimbursements
- Quality check claim batches adhering to weekly check run deadline
- Check refund processing
- Liaison with Mail Room team with claims related items
- Review and process specialty batches
- Enter claims as needed
- Assist in post implementation process for new business
- Liaison for Member Services related to escalated claim calls
- Assist in training of new staff
- Working knowledge of vendor relationships (3M and other vendors as contracted)
- Working knowledge of specialized pricing methodologies, I.E. 3M groupers – MS-DRG, APC, APGs, APR-DRGs
- Create and maintain a manual documenting departmental tasks
- SOC remediation point person
- SOC remediation- ensures monthly SOC scores are tracked by plan, findings are resolved through to completion
- SOC remediation- responsible to research claims outside of SOC purview however related to findings from SOC review. I.e. provider retro rate load/reprocess, ITR completion/follow through with identifying affected claims
- Review, analyze post adjudication review findings and completes through resolution
- Serve as a back up to the Manager for specific functions
- Represent the Claims department on calls as needed
- Bachelor’s Degree in Business, Healthcare Administration or related fields; or an equivalent combination of education, training and experience is required
- Minimum of five years’ of related work experience
- Ability to handle demanding caseload, make independent decisions and multi-task
Warranty Claims Specialist With English Resume Examples & Samples
- Validate warranty claims according to regional policies
- Manage unclear – on hold – repair claims
- Provide support to service centers/client’s local care team
- Communicate results of validation
- Create pro-forma invoices/payment proposals based on country specific rules
- Co-operation with other sub-teams
- Processing team tickets and ensuring ticket resolution according to agreed timelines
- Organize/participate the conference calls with agreed counter parts according to he agreed frequency, making notes and their follow ups
- Process document creation/update
- Reference data structure management, preparation for system update
Inside Casualty Claims Specialist Resume Examples & Samples
- Assists adjusters with more complex claim handling, analyze documentation and settle basic, straight-forward, and routine claims quickly and efficiently
- Insurance background especially desirable
- Good oral and written communication skills
- Receive calls from insured’s, beneficiaries, agents, attorneys and funeral directors who are calling to report or inquire about the status of a claims (average 150 calls per person per week)
- Open, stamp and count incoming mail
- Proofread Examiner letters before mailing
- Proactively manage assigned liability claims across multiple jurisdictions, while setting and implementing the case strategy for these claims under the direction of the Practice Leaders and Claims management. Handle all claims in accordance with XL Catlin’s Claim Handling Principles
- Collaborate closely with senior claims handlers and Practice Leaders to achieve optimum file outcome, determine if / which external vendors to engage, and establish strategic plan with vendor, identify and notify management of Large Losses and take all appropriate steps to achieve the best outcome for the client and XL Catlin
- Work with management and Claims Legal team to identify and select appropriate counsel or alternative resolution technique. Pro-actively manage and control litigation strategy on assigned claims
- Active participant in Quality Review Process
- Assist Underwriters with policy review and drafting, participate in external marketing and business development activities Share lessons learned and other identified trends to improve risk assessment and underwriting process
- Coordinate and manage communication with internal and external stakeholders to ensure the highest level of customer service and transperency
- Monitor and report on emerging liability and coverage trends
- Effectively manage, track and report on portfolio performance
- Legal qualification desirable
- Prior claims experience preferred
- Collaborative approach: Develop and maintain productive working relationships with insured, brokers, claim handlers, underwriters and legal counsel. Provide guidance and seek input from others as needed to achieve the best result possible. Capable of working and collaborating with a virtual team
- Results Oriented: Approach tasks proactively and anticipate needs. Think quickly and prioritize multiple work streams without sacrificing quality. Act with a sense of urgency
- Strong ethics: Handle responsibilities with integrity and the highest standards of professionalism
- Proactively manage assigned property claims across multiple jurisdictions, while setting and implementing the case strategy for these claims under the direction of the Practice Leaders and Claims management. Handle all claims in accordance with XL Catlin’s Claim Handling Principles
- Collaborate closely with senior claims handlers and Practice Leaders to achieve optimum file outcome, determine if / which loss adjusters and experts to engage, and establish strategic plan with vendor, identify and notify management of Large Losses and take all appropriate steps to achieve the best outcome for the client and XL Catlin
- Coordinate and manage communication with internal and external stakeholders to ensure the highest level of customer service and transparency
- Completes 3-point contact on new claims within 24 hours in order to obtain information necessary to make a compensability decision on the claim
- Directs Assistant to properly pay indemnity benefits payments and Awards. Issues state-mandated benefit notices within the required timeframes
- Annotates, categorizes and addresses incoming mail on a daily basis
- Responds to questions and requests from the client
- Ability to prioritize multiple tasks and meet deadlines
- Must remain flexible as assignments vary
- Workers’ Compensation law specific to assigned jurisdiction; policies and procedures
- Medical and legal terminology
- Integration with Medicare
- 5 to 8 years' handling California workers' compensations claims
- Public Entity and 4850 experience a plus
- Adjust commercial surety bond claims by receiving claim assignments, communicating with claimants and principals, investigating claims, analyzing documentation, understanding coverage under the bonds, evaluating exposure, setting reserves, making payments, and asserting indemnification rights
- Evaluate the appropriate method and extent of investigation for each claim
- Review underwriting files and bond and indemnity agreements
- Communicate promptly to claimants and bonded principal/indemnitors
- Analyze claim, verify applicability of coverage, and evaluate exposure on a variety of bond types in various jurisdictions
- Draft appropriate position letters to claimants and/or principal and indemnitors, when necessary
- Work with principals and indemnitors to promptly resolve claims under their duty to indemnify the Surety and make formal indemnification demands on principals and indemnitors, when necessary
- Manage litigated claims toward a prompt and reasonable resolution
- Consult with management at all levels of the claims department to strategize and make recommendations where assistance and consultation is needed on claims exceeding assigned authority
- Prepare reports, document claim files, review and manage outstanding files, as assigned, for adequacy and timeliness of investigation, evaluation and reserving, and maintain a timely diary for each assigned claim
- Assess recovery potential and collaborate with the subrogation unit to obtain information required to successfully pursue recovery
- Provide superior customer service to policyholders and external vendors and agents during entirety of the claims handling process
- Complete special projects and tasks, as assigned
Outside Claims Specialist Rm-entry Level Resume Examples & Samples
- Complies with contractual stipulations and requirements with regards to the payment of all outside claims
- Works with contracted providers and health plans to verify proper insurance and validity of transport
- Reviews claims from contracted providers to determine level of payment, validity of service and medical necessity of transport
- Maintains the outside claims database tracking of claims and payment in compliance with contractual requirements
- Works with the Financial Manager to create reports regarding payments of outside claims, provides monthly flash accountability and monthly reports for contracts
- Processes and sends denials and claims acknowledgements as appropriate
- Maintains positive relationships with contracted providers and health plans
- Supervises the Outside Claims Clerk to ensure proper processing of invoices and posting of paid invoices
- NO experience required
- Strong Microsoft Office experience with emphasis on Excel
- Exhibit high degree of social, ethical, and organizational norms
- Maintain a stable disposition despite external pressure and opposition
- Excellent Customer Service (for internal and external customers)
STD Claims Specialist Resume Examples & Samples
- Determines whether to pend, deny or pay claims
- Inputs data
- Evaluates claimant eligibility via information received from claimant, attending physician and employer
- Working knowledge of FMLA/Disability/Leave procedures
- Familiarity with STD regulatory requirements
- Obtain all necessary and available information to initiate processing of all liability and physical damage claims. Establish files and distribute the required information to insurance carriers and other internal department personnel to ensure prompt handling with 24 hours
- Initiate in-house processing of all claims within established deductibles/SIR including, but not limited to assigning of independent adjusters for scene/liability investigation with the aid of Claims Administrative Assistant II or Liability Claims Administrator
- Maintain accurate files, ensuring they are neat, orderly and current
- Claims less than carrier deductible/SIR will be assigned to appropriate personnel. Property Damage claims with potential minor injuries will be assigned to Claims Administrative Assistant II and claims with known injury claims will be assigned to Liability Claims Administrator
- Perform duties as directed by your manager
- Maintain inventory and order departmental supplies
- Support and assist associates with special projects in the department and other duties as assigned
- Recovery of repair costs on third-party network damages across multiple sites and municipalities
- Individual will learn, understand and be able to utilize state dig laws and statutes , 811 excavator requirements, NESC standards, CGA guidelines, etc
- Develop a solid working relationship with the Client’s and other utility locate companies and their claims coordinators and management
- Achieve monthly and quarterly recovery targets set by the department
- Learn the functionality of the company’s Claims Database Tool and enter all notes and documentation within the tool throughout the recovery process
- Resolve and negotiate claims recovery via phone, email, letter and other means of communication
- Be able to support claims investigation packages with photographs, narratives, job costs, site sketches, locate tickets and other components provided to you from the field investigator and visualize and understand the damage scene to accurately defend liability
- Work directly with liable parties’ insurance provider to defend claims and negotiate settlements
- Work directly with claims departments and management of liable parties from small businesses to large corporations and municipalities
- Communicate with the field investigator for post-claim submittal needs
- Attend weekly department meetings to discuss individual and team recovery numbers and goals
- Maintain a working knowledge of the entire claims process
- Use analytical and quantitative methods to understand, predict and enhanced project management processes
- BACHELOR’S DEGREE REQUIRED**
- HR experience
- Employee terminations
- Unemployment claims
- Manages moderate complexity commercial second injury fund recovery claim investigation arising out of the workers’ compensation line of business. Understands the underlying workers’ compensation claim process, as well as SIF process across multiple states. Effectively manages loss costs and recovery claim expenses
- Manages and organizes investigation and documents required to establish a SIF case in conjunction with state requirements
- Effectively manages vendor relationship within the scope of SIF requirements
- Effectively presents supporting documents and arguments to establish a viable SIF recovery in accordance with state requirements
- Works with attorneys, account representatives, agents and insureds regarding the handling and/or disposition of SIF recovery claims
- Keeps current on state/territory regulations and issues, industry activity and trends
- Moderate technical and product specific expertise related to SIF recovery claims. Possesses knowledge of insurance and underlying claim principles, practices and procedures
- Good communication, negotiation and presentation skills. Ability to effectively interact with all levels of CNA's internal and external business partners
- Good analytical and problem solving skills, with the ability to manage and prioritize multiple projects
- Ability to fully comprehend moderate claim facts and issues; and to further articulate analyses of claims in presentations to business partners and management as well as in internal reports
- Typically a minimum three to five years workers’ compensation claims experience
Senior Operational Claims Specialist Resume Examples & Samples
- Works with team and cross-functional partners to ensure plans deployed to the field are operationally sound
- Coordinate with Claims Supervisor on a regular basis
- Collaborate with cross-functional teams and various 3rd parties as needed
- Provide feedback of findings to appropriate parties
- 2 + years call center/claims handling experience
- 2+ years of experience supporting a retail organization
- 3+ years of experience in a role working cross-functionally to gain influence and develop partnerships
- 2+ years of people management experience
- Ability to influence and partner across the enterprise at multiple levels
- Team player that can inspire others
- Leadership abilities
- Effective communicator who can write and speak well
- Capacity to problem solve
- Planning and forecasting skills
- Able to give direction
- Strong analytic skills and strategic thinker
- In lieu of a degree, a minimum of 5 years injury claims handling insurance experience
- Ability to build rapport and successfully effect settlements directly with customers or their attorney
- Demonstrated proficiency analyzing coverage and liability
- Provides a consistent, positive, and satisfying claims experience for our clients by delivering superior claims service
- Investigates and settles one or more of these complex claims types: bodily injury/liability and/or material damage including auto total losses. Determines applicable policy coverage, evaluates damages, assesses liability, and creates applicable negotiation strategies
- Obtains and analyzes a wide variety of applicable documentation related to assigned claims, some of which may include, i.e., ISO reports, fire reports, police reports, cause & origin reports, medical reports, engineer reports, written estimates, witness accounts, etc.. Draws the proper conclusions related to claim investigation
- Evaluates damages associated with the more extensive losses according to policy provisions and published company guidelines
- Maintains continuous communication with all affected parties regarding each step of the claims process
- Communicates and negotiates with a variety of individuals regarding investigation and settlement of applicable claims, i.e., insureds, claimants, attorneys, medical providers, insurance carriers, and other involved parties
- Acts as resident expert while providing direction, support, and training of lesser-experienced Claims Representatives. Participates in round tabling on applicable claim files and has significant responsibility for coaching and developing employees
- Education equivalent to graduation from college (or the equivalent in related work experience). Maintains the appropriate adjuster's licensing as required by the states in which we do business
- Investigates and settles one or more of these complex claims type of bodily injury/liability claims. Determines applicable policy coverage, evaluates damages, assesses liability and creates applicable negotiation strategies
- Obtains and analyzes a wide variety of applicable documentation related to assigned claims, some of which may include, i.e., ISO reports, fire reports, police reports, cause & origin reports, medical reports, witness accounts, etc.. Draws the proper conclusions related to claim investigation
- Demonstrated ability to evaluate, investigate, and settle the more complex claims within higher settlement authority limits than those handled by Sr. Claims Representative – Inside. Knowledge of insurance contracts and claims law
- Monitors complex claims situations
- Manages and communicates complex claims issues with client, carrier or producer
- Attends and facilitates client meetings, claim reviews and vendor visits as requested
- Reviews claim status, action plans, and reserves using advanced problem resolution skills
- Negotiates for changes in reserves for a positive client outcome
- Provides status reports to clients and keeps sales team informed
- Advocates, consults and provides coverage advice to clients as appropriate
- Researches and obtains claims data from carriers and challenge adjusters as warranted while advocating the best possible outcome for clients in accordance with service standards
- Responsible for keeping Broker Management System up to date with correspondence and/or notes on open claims
- At least 5 years of insurance brokerage or property/casualty claims experience required
- Adjusters License, Agents License or CSR License required
- Ability to read and interpret documents such as safety rules, operating and maintenance instructions, and procedure manuals. Ability to write routine reports and correspondence. Ability to communicate effectively with carriers, clients and claimants
- Bilingual in English and Spanish a big plus
- To perform this job successfully, an individual should be proficient in Microsoft Office including Excel, Word and Power Point; follow guidelines on working in BMS (EPIC) for premium efficiency with your team
Limited Warranty Claims Specialist Resume Examples & Samples
- Identify non-validated/unaudited policies, develop validation processes, and implement into the field to drive positive customer experience and savings in warranty spend
- Manage customer requests on serial loads and start date changes through various Ingersoll Rand manufacturing, ordering, inventory and warranty systems
- Assist Falcon/SIL team on all validation requests related to Residential HVAC customers and claims
- Communicate policies and procedures to all levels of the value stream, including sales partners at dealer and wholesaler levels
- Provide Customer Relations support through all aspects of the Limited Warranty value stream
- Data mine, research and analyze Limited Warranty claims data to identify and execute on identified gaps in the process
- Review and process domestic and international claims per policies and procedures
- Manage Part to Model process
- Assist in claim entry, approval, process and policies
- Provide training as necessary on the claims management system and processes
- Facilitate monthly claims audit process for Residential HVAC claims
- Access, extract and link data elements from a variety of disconnected sources for further analysis, including but not limited to Oracle, Falcon, Citrix, Product Registration, SIL, QDW, CRM etc
- Support team efforts to manage and reduce warranty spend, accruals, reserves and the warranty segment of COGS
- Percentage of Travel: 10%
- Min. Yrs. Experience: 2-4
- Education Standard: BachelorsWe are committed to helping you reach your professional, personal and financial goals. We offer competitive compensation that aligns with our business strategies and comprehensive benefits to help you live your healthiest. We are committed to building an inclusive and diverse culture that engages as well as values the different backgrounds and experiences of our employee, which, in turn, spurs innovation, generates creative solutions and enhances our customer relations
- High school diploma or equivalent plus 2 years experience with healthcare customer service and/or claims, accounting
- Must have held a Claims Specialist 2 position for a minimum of 12 months
- Bachelors degree plus 1 year of experience in healthcare customer service and/or claims, accounting
- Evaluation/handling of complex insurance claims and litigation management duties within XL Catlin's Professional division including, but not limited to, Cyber/Technology E&O liability claims
- Developing and maintaining corporate client relationships, working closely with our insured’s executives and in-house counsel, establishing an effective risk management infrastructure, and achieving resolution of claims disputes
- Assisting underwriters with respect to the creation and development of insurance contracts, products, and services
- College degree as well as licensed J.D
- Four plus years of verifiable legal experience in the industry
- Insurance adjuster license preferred, but not necessary for hire
- A strong background in Cyber / Technology business
- Directs the Claims Assistant to properly pay indemnity benefits payments and Awards, Issues state-mandated benefit notices within the required timeframes
- Proficient in all aspects of California WC and can easily adapt to change
- 5 to 8 years of experience handling workers' compensation claims
- Prior experience handling LC 4850/public entity preferred
- Degree holder
- 4 years’ relevant experience in life insurance industry
- Mature and reliable and able to work under pressure
- Proficient in MS Office, including Word, Excel, PowerPoint and Chinese word processing
- 2-4 years of experience in claims or customer service preferred
- Working knowledge of FMLA/Disability/Leave procedures preferred
- Familiarity with STD regulatory requirements preferred
- Help develop and execute the strategies of the practice by creating strategy for larger account
- Directly handle large clients as WC consultant including complex consulting and strategy
- 7+ years of complex worker’s compensation claims experience
- Extensive experience handling workers compensation construction claims of a complex nature
- Meet accounts receivable operational standards for productivity, quality, and customer-service standards
- Research and analyze denial data submitting appeals and contacting insurance companies as needed to overturn denials
- Research, respond, and document insurer correspondence regarding coding, eligibility and benefits, and reimbursement on patient accounts
- Identify, analyze, and research frequent root causes of denials to coordinate corrective action plans for resolution of denials and identify opportunities for improvement
- Ability to effectively communicate with others within the business office, at the clinics as well as outside contacts (patients, vendors, physicians, etc.)
- Protects organization-s value by keeping information confidential. Accomplishes accounting and organization mission by completing related results as needed
- Maintain a working knowledge of insurance policies and procedures to ensure the timely resolution of claims issues
- Other duties as related and/or assigned
- Regular communication with internal business units, as well as external contacts, to seek resolution on items that may delay timely claim filing
- Remain up to date on HUD and FNMA guidelines and accurarately convey information during claim filing
- Demonstrate business professional behavior and teamwork, maintain punctuality, and adherence to department and company policies and procedures
- Ability and willingness to effectively communicate with internal and external contacts
- Default, foreclosure, and/or previous work with mortgage claim filing a plus
- Minimum 1-2 years post-secondary educations or equivalent experience (minimum 1-3 years claims of insurance experience for claims examiner)
- Effective customer service skills
- Medical Terminology for specific roles
- Sets reserves and authorizes payment within scope of authority, effectively settling claims in most cost effective manner and ensuring timely issuance of disbursements
- Coordinates and performs investigations and evaluates claims and suits through contact with insureds, claimants, witnesses and experts. Identifies files that have potential fraud and refers to SIU
- Works with attorneys, account representatives, agents, internal large claim unit, managers, underwriters and insureds regarding the handling and/or disposition of more complex claims
- May update the claims systems
- Bachelor's degree or equivalent experience. Professional designations preferred. Attorney license a plus
- Minimum three to five years claims experience preferably in Lawyers Professional Liability
- Interprets more complex Auto and General Liability (GL) losses including UM/UIM losses, unusual policy coverages and determines if coverages apply to claims submitted, escalating issues as needed. Claim Specialist will draft appropriate coverage letters
- Keeps current on state/territory regulations and issues as well as industry activity and trends. Maintains appropriate state adjuster licenses
- Has extensive knowledge on reviewing litigation and addressing possible coverage issues related to those lawsuits and handles overall litigated cases. Ability to analyze coverage and draft the appropriate letters (disclaimers, ROR’s)
- Typically a minimum three to five years of claims experience
- Serve as primary point of contact to internal and external parties for escalations related to one or more business functions in pre/post foreclosure areas to minimize reputational impact to Fannie Mae and ensure optimal resolution for business unit and/or vendor
- Monitor overall workflow and delegate and prioritize activities across the team to ensure timely and quality execution, in compliance with applicable guidelines
- Regularly partner with internal and external parties via in-person meetings, phone calls and emails to resolve escalated or time sensitive collection issues and ensure an ongoing understanding of changes to processes/guidelines and related impacts. Maintain partnerships and facilitate open dialogue
- Work with management to develop and implement new or revised processes and guidelines and realize process efficiencies within own department or for assigned business unit(s)/vendor(s)
- Manage internal and external procedures and guidelines changes are appropriately communicated. Work with the team to ensure procedures and guidelines are accurate and up-to-date
- Responsible for new case assignment, case resolution, and timely reimbursement for services rendered to vendor(s)
- Update databases to ensure information is accurate, complete and accessible
- Performs analysis on business unit/vendor performance and data quality
- Train and develop internal and external staff
- Mortgage servicing experience (mortgage insurance, loss mitigation, default servicing, REO, foreclosure, expense reimbursement) and back end servicing experience a plus
- Account reconciliation experience required
- Previous experience analyzing data
- Experience with Pivot tables a plus
- Investigating and settling one or more of these complex claims types: liability, property and/or material damage. Determining applicable policy coverage, evaluating damages, assessing liability, and creating applicable negotiation strategies
- Demonstrates excellent oral and written communication, including telephone etiquette, possesses good decision-making skills and the ability to persuade and negotiate effectively, possesses the ability to handle potential conflict effectively and constructively, and demonstrates good organizational skills, analytical ability, and detail orientation and knowledge of basic math and geometry
- Previous experience handling claims applicable to area of specialist assignment
- Possesses the ability to multi-task while interacting effectively with financial representatives, claimants, insureds, internal staff members, and external contacts, and must be able to work independently in the field or as a member of a team
- Possesses competent knowledge with residential and commercial construction techniques
- Bilingual in English and Spanish is preferred
- Working knowledge of Microsoft WORD and Excel (or their equivalents), Xactimate, and/or other claims estimating software (as applicable). Basic computer and data entry skills
- Prepare and file all claims according to Agency guidelines within appropriate time frames
- Understand Loss Mit guidelines in regards to specific claim type
- Follow up with attorneys for needed information to include clear title, documents, to ensure information is provided in a timely manner
- Prepare files for internal and external audits
- Draft written correspondence to agencies, officers, vendors and clients as needed
- Minimum of 3 years work experience in the legal field or default mortgage servicing
- Working knowledge of accepted business practices in the mortgage industry and a strong understanding of claims process
- Working knowledge of foreclosure process and appropriate guidelines
- Good analytical, written and verbal communication skills
- LPS-MSP (Mortgage Servicing Platform)
- Knowledge of Microsoft office- Excel and Word
- Two (2) years job-related course work or paralegal studies
- Working knowledge of claims processing
Catastrophe Claims Specialist Resume Examples & Samples
- This position is part of a job family. Placement will be determined by skills and qualifications of the candidate
- Responds to deployment directives and travels to catastrophe areas to evaluate, negotiate, and settle personal and commercial lines property claims resulting from natural catastrophes in various geographic locations
- Investigates and completes physical inspections of property claims, evaluates damages, and prepares written estimates according to policy provisions
- Initiates first contact with insureds and all relevant parties to gather basic information, obtain recorded statements and explain the overall claims process
- Bachelor’s degree and at least 5 years of property claims adjusting or construction or equivalent work experience ORat least 7 years of property claims adjusting or construction or equivalent work experience
- Graduated in the upper third of the graduating class in the college, university, or major subdivision; OR
- Graduated with a cumulative 3.0 GPA or higher out of 4.0 based on 4 years of education, or based on courses completed during the final 2 years of the curriculum; OR
- Graduated with a 3.5 GPA or higher based on the average of all the required courses completed in the major field or the required courses in the major field completed during the final 2 years of the curriculum; OR
- Election to membership in a national scholastic honor society that meets the minimum requirements of the Association of College Honor Societies (except for freshman honor societies)
- Effectively assist Third Party Administrator with handling claims to conclusion
- Provides high quality customer service by determining the best approach for handling issues
- Processes documents and inputs information into the database
- Gathers claim file material from multiple sources including internal and external parties. Analyzes claim file material for potential impact on claim mitigation
- Initiates and conducts follow-ups via proficient use of the claims handling system or other related systems
- Utilizes Risk Management best practices
- Submits statistical reports as required
- Manages vendors, as assigned
- Focus on quality work and job performance
- Must be able to multi-task, be well organized and detail oriented
- Must be proficient working with database and processing software, excel, word and outlook
- Must have mathematical, problem solving and analytical skills
- Must be able to successfully complete licensing and claims certification schools/classes, where required
- Pen and paper
- Ability to use a computer and related devices, such as a keyboard or mouse or other related equipment, throughout the day while seated at a workstation
- While performing the duties of this job, the employee is regularly required to speak or hear. The employee is also frequently required to stand, walk, use hands and fingers, handle or feel and reach with hands or arms
Senior Claims Specialist Casualty Resume Examples & Samples
- In a small team of experienced handlers, independently investigate, negotiate and settle all assigned lead
- At least five years of experience in the national or international insurance industry
- Already seasoned in the handling of Casualty claims with a specific focus on product liability cases
- And ideally with a legal background (Master of Law / Attorney at Law), fluent in German and English , any other european language is of advantage
- Driven to deliver service excellence; a strong team player with developed analytical, negotiation, communication and problem solving skills
- Willingness to work independently with a significant amount of contact with the business and customers in an international, matrix organized, fast-paced and dynamic environment
- Up-to-date knowledge of claims handling, administration systems and processes
- Managing assigned claims across multiple jurisdictions, as well as setting the case strategy for these claims in partnership with Regional Practice Leaders and Claims management
- Proactively managing external counsel and setting litigation strategies when counsel is engaged on a claim
- Coordinating and managing communication with internal and external stakeholders (e.g., underwriting, brokers, reinsurers, external vendors, etc.) to ensure the highest level of customer service
- Consulting with Regional Practice Leaders and Claims management on Large Losses and ensuring all steps are taken to achieve the best outcome for the client and XL
- This role will report to the Manager of Construction Professional Liability Claims
- Broad Construction Professional Liability claims experience: 5-10 years of experience managing Construction Professional liability claims. Experience managing high exposure and complex claims. Demonstrated experience negotiating and settling complex claim files
- Collaborative approach: Develop productive working relationships with insured, brokers, claim handlers, underwriters and legal counsel. Seek input from others as needed to achieve the best result possible. Capable of working and collaborating with a virtual team
- Advanced level of Third Party claims handling with a handling authority level up to £12,500
- Is able to effectively handle claims involving staff, VIP and Product v Product claims in line with the agreed best practice
- Handles RTA/Article 75 cases in line with the agreed guidelines
- Can handle escalated Customer complaints through to resolution
- Actively looking for opportunities to maximise settlement and reduce TP Costs
- Maximises recovery, improve process and drive efficiency within the team/department
- Ability to audit files/calls and provide relevant feedback to help coach and improve your colleague’s performance on a consistent basis
- Review and authorise cheques in accordance with company procedure up to £12,500
- Ability to allocate claims/workflow across the team
- Ability to monitor workflow and telephony performance within your team
- Act as a role model within the team. Mentoring new individuals into the team
- Take on additional responsibilities over and above the core role
- Will lead meetings / buzz sessions within the team so that the team are kept well informed
- Able to deal competently with general HR issues (excluding capability / conduct issues)
- Has a thorough knowledge of claims exceptions and the management of these controls
- Is aware of the Team Leader duties and able to carry out day to day management of the team
Field Claims Specialist Resume Examples & Samples
- Distribute and direct losses and claim tracking for defined territory or agency base to support delivery of effective customer service and claim resolution and ensure team alignment with business goals
- Accurately document, process and transmit loss information in order to determine potential damages associated with difficult and complex claims
- Provide overflow support to Compliance Department of quality control audits for Federal Crop Insurance Corporation (FCIC and Crop Hail)
- Complete field inspections, reviews and adjustments by reading maps and aerial photos, measuring fields and storage bins, and appropriately administering company crop insurance policies. Ensure compliant and cost effective application of crop policies by leveraging knowledge of insurance statues and regulations and complying with state and federal regulatory requirements
- Provide effective and timely communication with agencies in defined territory on claim status and other inquiries
- Build and maintain relationships with customers by providing timely an accurate policy service, answering questions and communicating adjustment determinations
- Coach claims adjusting team by supporting and mentoring team members and providing advice and feedback to guide the success of the team and meet service level expectations
- Provide information and feedback regarding the quality of agent business and/or policy files of regional claim operations to maximize profit and quality of business
- Deliver classroom and field training programs for claims technology applications and crop programs ensuring effective educational resources for clients and alignment of training services with key stakeholders expectations
- Participate with internal committee to develop global claims technology solutions that support business need
- Attend National Crop Insurance Services (NCIS) regional and state committee meetings to make business aware of any legal issues or changes that will impact the business
- 5 years experience in MPCI and Crop Hail claims experience
- Working knowledge of claims administration best practices and procedures
- Understanding of relevant laws and regulations across multiple jurisdictions
- Utilize effective communication channels for both external and internal customers
- Support implementation of company strategies
- Train others on process and procedures
- Proactively manage assigned claims across Property while setting and implementing the Adjustment plan for these claims. Ensure all documentation is present in the file, and Claim Handler Guidelines and protocols are followed
- Minimum of 3 (or more) years of solid experience handling Equipment Breakdown claims to include Energy, Property & Construction, and other specialty areas preferred
- Displays a thorough functional knowledge and skill of claims handling specific to assigned area
- Strong interpersonal, communication and negotiation skills
- Knowledge of Microsoft Office Suite as well as other business related software
- Minimum 3 years handling Equipment Breakdown Claims
- Requisite State Claims ‘Adjusters licenses preferred or Candidate will commence acquisition of same
- Claim Specialist Trainees are responsible for timely and accurate communication, information gathering, and rendering decisions on Long-term Disability (LTD) claims to which they have been assigned according to provisions of LTD certificates
- The job entails communicating with a variety of constituents (for example, claimants, doctors, nurses, employers, and attorneys) to gather information relevant to rendering decisions based on the provisions of the policy
- Claim Specialist Trainees will work more independently, use their own discretion, and increase their caseload as they become proficient in LTD and demonstrate consistency in metrics, philosophy, and process
- They will learn to use appropriate systems, tools and resources to research and document claims
- They will develop an action plan and identify the Likely Claim Progression including identifying the return to work potential
- Claim Specialist Trainees will complete regular updates on financial offsets such as SSDI
- They will utilize CMG which provides an overview of high level topics, factors to consider in the administration of claims, and examples of claim situations
- CST’s perform their work under direct supervision by peer coaches and Unit Leaders
- Render appropriate claim decisions pursuant to certificates
- Clarify functional capacity through problem solving measures (gathering medical, vocational, and other information, efficient use of resources, and action planning) sufficient to determine initial and ongoing liability
- 2+ years of disability claims or customer service experience
- Bachelor’s degree preferred
- Critical thinking in activities requiring analysis, investigation, and/or planning
- Ability to prioritize
- Disability claims or 2-4 years strong customer service experience preferred
- Demonstrated ability in the following areas
Casualty Claims Specialist Resume Examples & Samples
- Interviews, telephones, or corresponds with claimant and witnesses; consults police and hospital records; and inspects property damage to determine extent of company's liability, varying method of investigation according to type of insurance
- Assists in preparing loss experience report to help determine profitability and calculates adequate future rates
- Supports the organizations quality program(s)
- Knowledge of professional liability claims
- Ability to review information and ensure accuracy and applicable policy placement
- Drive For Results
- Functional/Technical Skills
- Learning On The Fly
- 1-2 years of recent, residential, default mortgage servicing experience
- Ensures timely, accurate and efficient processing of claims edits via EPIC work queues. Meets daily claims edit resolutions goals by reviewing, analyzing, and obtaining appropriate documentation based on payer requirements and regulations. Prepares electronic and paper claims and sends with appropriate attachments. Conducts research and provides updates and current status of claims edit work queues using the appropriate data management system (EPIC). Resolves issues that are adversely impacting claims submission in a timely and accurate manner. Completes or requests adjustments to accounts based on dollar threshold. Communicates information and ideas to make system-wide process improvements. Updates patient accounts regarding changes and modifications in plan benefits and other contract information relevant to the claims follow up and collection process. Documents claim processing activity on patient accounts
- Serves as a communication link to various departments and external payers by developing positive relationships with managed care organizations and outside agencies, and clinical areas within the organization. Performs liaison services to both internal and external customers providing assistance in claims resolution. Assists with education of internal staff and external customers to bring about the timely, accurate, and cost effective adjudication of all claims. Works collaboratively with other departments to facilitate the insurance collections process and to improve overall cash collection
- Monitors the status of claims in work queues and conducts routine, periodic follow up on previously researched claims items. Monitors, reviews, and suggests revisions or updates to existing forms, documents, and processes required to submit a clean claim
- Ensures completeness of claims by following national, local, and internal billing requirements promoting prompt and accurate submission and payment. Maintains awareness of current regulations. Initiates practices that support current regulations. Shares knowledge of current regulations with staff. Analyzes current practices and makes recommendations for process improvements
- Must have knowledge of insurance billing regulations and reimbursement procedures; excellent phone etiquette and customer service skills; and an analytical aptitude and ability to translate functional needs to a computerized environment
- Preferred: familiarity with medical terminology, ICD-9 and CPT-4 coding; third party payors in a healthcare billing environment; and Epic billing module
- Follows standard and/or other appropriate precautions using personal protective equipment as required
- Previous experience with computerized billing and/or healthcare billing preferred
Warranty Claims Specialist Resume Examples & Samples
- Seek opportunities to control warranty costs through effective auditing, editing, and review of claims and registration requests
- Identify and correct internal and external errors
- Identify and address issues that conflict with established warranty policies and programs
- Assist in the responsibility for the integrity of product registration and warranty claims database
- Participate directly in and support all company and department programs, goals, and objectives that support outstanding customer service
- Assist dealers/distributors in resolving questions related to electronic filing of warranty claims and registrations
- Maintain a positive business relationship with business partners, dealers, distributors, and local personnel
- Adjust warranty claims as necessary, and be accountable to the business partner as well as dealer/distributor for the adjustments made
- Assist Registration Specialist in the resolving of dealer inquiries on product registration issues as necessary
- Must be flexible and willing to perform a variety of other tasks and duties as required by department needs
- Strong organizational/analytical skills a must
- Knowledge of snowmobiles and ATV's and their related parts, clothing, and accessories would be very beneficial
- Friendly, professional email and telephone etiquette
- Knowledge of computer programs Microsoft Excel, Word, Outlook
- Must demonstrate good judgment and decision making skills
- Mechanical knowledge is beneficial, but not required
- Post-secondary education preferred and/or job related experience
- Office and computer experience necessary
- Bachelor’s degree in any area of study
- Certified Workers' Compensation Professional
- Five years of experience applying the Kansas Workers Compensation Act, case law and board decisions; State of Kansas programs; reading/comprehending medical records and reports, mediating/negotiating settlement, facilitating return to work
- Knowledge of the principles, methods and priorities of legal research of state laws, rules and regulations applicable to the Kansas Workers Compensation Act, case law and board decisions
- Ability to work in a high volume environment
- Ability to plan/conduct investigations by phone or personal interview; read, interpret and apply complex laws/policies; document/maintain claim activity; effectively communicate orally and in writing; calculate payments; read/comprehend medical records and reports; mediate/negotiate settlements and exercise sound judgment
- Working knowledge of applicable Kansas statutes and regulations
- Knowledge of Kansas Workers Compensation Act
- Knowledge of Americans with Disabilities Act
- Knowledge of the Family and Medical Leave Act
Homeowners Field Claims Specialist Resume Examples & Samples
- Determines scope of repairs. Prepares a repair bid using Xactimate estimating system
- Follows the repair process to conclusion
- 3-5 years homeowner claims experience
- Active management of caseload of high value workers compensation claims venued throughout the United States for assigned clients in the Global Risk Management business unit
- Conduct claim handling and oversight of TPAs in accordance with XLC best practices in the major phases of claim handling including coverage, investigation, evaluation, reserving, recovery, and resolution
- Provide oversight, guidance and direction to Third Party Administrator claim adjusters on all major phases of claim handling including coverage, investigation, evaluation/reserving, recovery, and resolution
- Collaborate with client risk management/claim management team on claim management and strategy to help deliver the most optimal outcome and ensure, to the extent possible, that we are in alignment on our evaluation of the exposure and strategy to resolve
- Collaborate and consult with internal claim resources such as regional practice leaders and claim legal to ensure the most optimal outcome and mitigate claim expense
- Interact regularly with the Claim Account Management team for assigned clients to communicate claim issues and results, participate in the TPA audit process, and collaborate on technical and service issues relating to the TPA performance and the client
- Communicate proactively with internal and external stakeholders regarding claim experience, results, and trends (e.g. actuarial, reinsurance, credit risk and underwriting)
- Provide input into the development of key metrics to support Claim Audits, and assist in the coordination and retention of external counsel, as needed
- Minimum of 10 years of claim handling experience involving high value/complex claim management and litigation management
- Multi-jurisdictional (U.S.) experience
- Demonstrated expertise in designated line(s) of business: Worker’s Compensation, Auto and General Liability, or Property
- Experience managing claims in an unbundled insurance model
- Leadership: Demonstrates managerial courage and ability to influence actions of external relationships. Coaches, sets expectations, evaluates and holds people accountable for delivering
- Strong communication and negotiation skills: Excellent verbal and written communication, and negotiation skills
- Strategic thinking: Exhibit ownership to look for ways to continuously improve internal processes as it relates to improving claim outcomes and managing the performance of external relationships
- Strong teamwork/collaboration skills in order to effectively collaborative with Regional Practice Leads, Claim Legal, TPAs and clients to produce desired outcomes, as well as with other internal and external stakeholders, such as Claim Account Managers, brokers, actuarial, reinsurance and business partners to communicate regarding claim results, experience and trends
- Refers claims exceeding own personal authority level to management for their review, along with recommendations for investigation and settlement
- Establishes initial claim file reserves and adjusts accordingly as investigation progresses (if applicable)
- May temporarily perform duties in other company locations when catastrophes occur or as other business needs dictate
- As applicable, travels to loss locations, determines coverage, evaluates liability and estimates damages
- Basic computer and data entry skills with a working knowledge of Microsoft WORD and Excel (or their equivalents), Xactimate, and/or other claims estimating software (as applicable)
Extended Warranty Claims Specialist Resume Examples & Samples
- Accepts extended warranty claims as allocated by leadership
- Adjudicate each claim individually based upon standard work, current extended warranty task times, and program details in a timely manner
- Ability to clearly document reasons for claims adjustments and rejection
- Accepts direction from team lead on specific claims management processes
- Run multiple access queries that are used for claim payment validation and accuracy
- Able to use multiple sources of information simultaneously to properly administer claims payment policies

MCU Excess Casualty Liability Claims Specialist Resume Examples & Samples
- Juris Doctor and 5 or more years of experience managing general liability claims and litigation
- Expertise in managing bodily injury and property damage claims and litigation
- Strong skills in coverage, claim evaluation and negotiation
- Proven organization and time management skills
- AIC, SCLA, CPCU or JD
- Ensuring the proper execution of the unemployment claim process within Southwest Airlines, utilizing current unemployment logistics management vendor to ensure timely responses and cost management,
- Recognizing and analyzing trends in unemployment terminations and utilizing strong partnerships with Human Resource Business Partners, General Counsel, etc., to communicate insights and potential risk,
- High School Diploma, GED or equivalent education required
- Must have authorization to work in the United States as defined by the Immigration Reform Act of 1986
- 2-3 years working knowledge of the unemployment claims management process required
- Experience within an HR Shared Services environment preferred
- Experience with HR information systems and HR process preferred
- Must have a keen awareness of federal and state law including an understanding of the Federal Unemployment Tax Act (FUTA), State Unemployment Insurance (SUI), and the State Unemployment Tax Act (SUTA)
- Must be technically proficient with respect to Microsoft Office products, particularly PowerPoint, Excel, and Word with the ability to analyze data
- Strong organizational skills, including the ability to prioritize and multi-task in a fast-paced, deadline driven environment
- Ability to communicate confidently, effectively demonstrating the ability to influence without authority to all levels within the organization regarding sensitive matters
- Must demonstrate a strong attention to detail
- Ability to work under stressful situations
- Must maintain a well-groomed appearance per Company appearance standards as described in established guidelines
- Recent experience processing 500 or more annual/per year Unemployment Claims (UI Claims)
- 2-3 years working UI experience with majority of responsibility reviewing and processing UI Claims
- Experience with an electronic UI Claims processing system (example; Equifax, ADP, EmployerEdge, etc)
- Demonstrable experience in reporting on UI Claims trends/statistics
- Experience using MS Office (Word, Outlook, Excel)
- Ability to handle heavy workloads under tight time lines
- Ability to work with little to no instruction or manager supervision - taking initiative to seek out answers via research/resources)
- Ability to demonstrate professional communication via phone, email and in person
- Investigate coverage and liability of claims through telephone, written correspondence, and/or personal contact with claimants, attorneys, insureds, witnesses and others having pertinent information
- Analyze information in order to evaluate assigned claims to determine the extent of loss, taking into consideration contributory or comparative negligence. Assign medical or other experts to case and arrange for medical examinations when necessary
- Process incoming calls and correspondence from insureds, claimants and agents regarding questions or problems associated with claims. Interact with underwriters and agents on claim resolution
- Evaluate, negotiate and resolve claims within delegated authority. Handle general liability and auto liability files from start to finish
- Update claims system on a continual basis to accurately reflect status of each assigned file and to initiate percentage of negligence on the part of the insured to determine "chargeability"
- Receive and approve expenses incurred to investigate, process, and handle a claim
- Prepare check requisitions for all loss and expense payments
- Explore contribution on all claims assigned
- Prepare for and participate in claims review and settlement conferences
- Close claim by issuing check or denial and securing appropriate releases
- Negotiation and claim disposition skills with proven problem-solving ability
- Strong judgment and decision making skills
- Self-starter with ability to work independently
- Moderate proficiency with standard business-related software
- Minimum of three years of claim handling experience preferred
- Industry training/designations preferred
- Extensive experience of handling general liability and construction claims of a complex nature
- Experience with professional lines claims
- Helps develop insurance programs for clients which include the creation of policy and
- Must possess a law degree
- College degree required, graduate/law degree a plus
- Construction industry client experience
- Current on case law and appellate decisions to use in the adjudication of claims
- Travel required, primarily within New York
Large Loss Claims Specialist Resume Examples & Samples
- Handling assigned claims across multiple jurisdictions, as well as setting the case strategy for these claims in partnership with Regional Practice Leaders and Claims management
- Coordinating and managing communication with internal and external stakeholders (e.g., Underwriting, brokers, reinsurers, external vendors, etc.) to ensure the highest level of customer service. Participation in new account and renewal meetings may be required
- Consulting with Regional Practice Leaders and Claims management on Large Losses and ensuring all steps are taken to achieve the best outcome
- Producing internal reporting and ensuring that reserves are set according to best practices guidelines
- Dentifying, monitoring and reporting on emerging liability and coverage trends
- Broad surplus claims experience: minimum of 7 years of experience managing claims. Experience in the handling and management of general liability, contracting, premises liability, products liability, and excess liability claims preferred
- Strong communication: Excellent verbal and written communication, presentation and negotiation skills. Able to communicate and negotiate effectively with internal and external stakeholders at various levels of sophistication
- Collaborative approach: Develop productive working relationships with insured, brokers, claim handlers,
- Passion for results: Approach tasks proactively and anticipate needs. Think quickly and prioritize multiple work streams without sacrificing quality. Act with a sense of urgency
- Intellectual curiosity: Willing to ask questions and explore new ideas. Eager to learn and focused on continuously improving technical skills
- Education: Bachelor's degree required
- Ability to travel approximately 10%, typically for short duration trips
- Adopt the DPDHL culture of professionalism, integrity, effectiveness and dynamic attitude contributing to an internal environment of collaborative teamwork and promote a positive IRM claims service provision to internal customers
- Serve as a key active member of IRM’s mainland claims handling team, interacting and working with team members to ensure business objectives are aligned and IRM claims management is performing to operational objectives
- Proactively pursue economic, early resolution for all customer claims, adopting a collaborative approach to addressing a wide variety of claims administration requirements, providing workable solutions to senior management
- Manage high volume freight, marine cargo claims and underwriting control standards and protocols
- Provide advice on making a claim and the process to customer services, including collection accurate information and documentation to proceed with a claim
- Manage service quality & KPI monitoring in association with external parties (Insurers & third party claims administrators etc. within agreed authority and in conjunction with IRM London)
- Ensure claims are handled swiftly and efficiently by reviewing and deciding on the extent and validity of a claim, checking for any potential fraudulent activity
- Provide customer claims reporting and data analysis on claims activities and resolutions
- Identify reasons why full payment may not be made, and ensure fair settlement of a valid claim
- Build relationships with loss adjusters, legal, as well as other legal/claims professionals
- Ensure customer claims are treated fairly and receive excellent service in accordance with industry and company guidelines
- Handling complaints in a professional manner associated with a claim
- Adhere to legal requirements, industry regulations and customer quality standards set by GBS IRM
- Navigate, network and establish cross boarder relationships to leverage best practices and execute program-wide claims strategies through internal claims management communities
- Build co-operative relationships between GBS IRM team and stakeholders within the claims process
- Manage claims information exchange between business units and GBS IRM, including suppliers and other key process stakeholders
- Coordinate with GBS IRM central team for significant claims on content of coverage, precedent setting and commercially sensitive issues
- Immediate assignment of leak complaints and ensuring that all customer service objectives are met. Prepare and process claim settlements in accordance with the applicable terms and conditions of the correct guarantee type issued for the product and in compliance with company policies, guidelines and best practices. Assignment to GAF Field Services Representatives (“FSRs”) and/or contractors on a timely basis is required
- The ability to effectively communicate claim decisions both in writing and verbally with internal and external customers by telephone and written communication, including emails and coverage position letters. Follow up with contractors and FSRs in a timely fashion both in writing and verbally is required
- Negotiate guarantee settlements under the direction of the Warranty Claims Supervisor, Director of Claims Management or Legal department
- Handle customer issues and disputes in an effective manner with a minimum of supervision
- Ensure that the proper requests for information are distributed on a timely basis and that results from the laboratory, inspections or claim committee sessions are quickly and effectively communicated with all applicable parties to the claim
- Schedule roofing inspections and leak repairs with contractors or FSRs
- Aggressive diary follow up to ensure that action items are completed in accordance with our best practices and procedures to assure maximum customer service experiences and timeliness of handling
- Provide department support for absences, assist on special projects and general office duties
- Handle incoming calls from property owners, contractors or Sales
- Open, maintain and update claim files
- Prepare customer letters
- Conduct timely follow ups with internal and external customers as necessary
- Provide support to Sales and GAF Field Service Representatives
- Timely assign leaks to the applicable contractors or Field Service Representatives (“FSRs”) in a timely fashion and pre-authorize repairs within assigned authority limit
- Accurately assess proposed settlements through the correct application of the applicable warranty
- Process payments within assigned authority through PeopleSoft and GAF’s claim system
- Seek timely and accurate authority for payments in excess of assigned limits through the Warranty Claims Supervisor or Technical Specialist team
- The ability to effectively communicate claim information and recommendations for resolution to all levels of management
- Completion of online courses provided by GAF through National Roofing Contractors Association (“NRCA”) will be required during the initial employment period
- Basic knowledge of standard roofing concepts and practices
- Proficiency working with Microsoft Excel, Word and Outlook
- Advanced telephone skills
- Associate or Bachelor’s degree is preferred
- Minimum of two years’ experience in a customer service environment is required with a preference for any background in the insurance industry, working with contractors or in a roof related field being a plus
- Responsible for store claims
- Adhering to Service Level Agreements
- Deliver premier Boss Centric service by communicating with friendliness and confidence
- Empathize with the Boss, diffuse and navigate complex situations
- Develop and maintain professional relationship with all parties
- Communicate via telephone, email, regular mail with the Boss and various 3rd parties
- Obtain relevant facts to claim through interviews, investigations and documentation
- Review and evaluate all allegations/situations surrounding the claim
- Coordinate necessary appointments with Boss, field personnel and other 3rd parties
- Set up rentals, investigations, and repairs as needed
- Monitor all open claims and maintain a follow-up calendar system of outstanding issues
- Keep all parties apprised of status on a regular basis
- Analyze all facts, details, and information obtained for claim
- Collaborate with higher technical teammates or cross-functional teams to review more complex situations or when necessary
- Make informed decisions after analysis
- Manage and negotiate resolution
- Communicate resolution to all involved parties
- Process paperwork as needed (i.e. release, letters, etc)
- Administer requests for payments, refunds and customer satisfaction considerations
- Pays invoices associated with claims in a timely manner
- Ability to navigate a matrixed environment
- Conflict management skills; ability to stay calm and composed under pressure situations
- 2 + years call center or claims handling experience
- 3rd Party Labor / Vendor Management Experience
- P&L Management Experience
- Strong Business Acumen
- Strong listening skills – active listening
- Proficient with keyboard and various Microsoft programs
- Solid analytical and interpretive abilities
- Capable of making confident and informed decisions independently
Senior Homeowner Claims Specialist Resume Examples & Samples
- Investigates, evaluates, negotiates and settles homeowner 1st- and 3rd-party property claims involving fire, black water, mold, earth movement and public adjusters
- Serves as a team lead, coach and mentor to staff
- May be called upon to provide training to staff
- Analyzes claim to determine coverage recommendation
- Arranges and handles through conclusion all emergency services required to protect the property from further harm, accommodate the needs of the insured
- Recognizes and prepares files for subrogation
- Appropriately administer insurance coverage to moderately complex claims by conducting loss investigations, analyzing factual information, interpreting insurance policies and applying legal and technical knowledge to independently resolve claims files in a timely manner
- Negotiate claims settlements by collaborating with subject matter experts and involved parties, recommending appropriate reserve modifications for assigned claims and communicating solutions to mitigate risks and coverage conflicts and achieve cost effective outcomes
- Inform internal and external stakeholders on claims resolution processes by summarizing factual information, reporting out of scope, specialized exposures and accurately managing documentation of assigned claims to ensure effective communication of current state for individual claims portfolio
- Build strong working relationships by reporting on approved, cost-effective claims strategies to ensure understanding of Claims operations and encourage a collaborative approach to enhancing the business
- Support claims workflow efficiency by accurately documenting portfolio progress, referring high risk exposures outside authority levels and seeking opportunities that enhance operational knowledge to ensure achievement of individual and department objectives
- Experience in a claims department or the insurance industry
- Management Liability and Professional Lines (MLPL) - Law degree; prior experience working in a law firm or other in-house counsel position; familiarity with interpretation of contracts and negotiation
- Experience handling MLPL matters including directors and officers liability, employment practices liability, professional liability, fidelity, pension trustee’s liability, data protection and privacy liability
- Experience in agency, retail or wholesale brokerages, third-party administrator, risk management, legal or other roles
- Knowledge of claims administration best practices and procedures
- Knowledge of insurance products and services
- Understanding of market trends and organizational strategies
- Knowledge of Microsoft Office Suite, general computer software and database systems
- Utilize effective communication to effectively influence and persuade decision makers; understand the needs and goals of customers and actively look for ways to meet them
- Mediate and resolve conflict using a logical approach
- Identify relevant information and understand it’s impact
- Maintain integrity of claims portfolio and evidence
- Use multiple resources to gather and analyze significant data
- Leverage technical knowledge to make cost-effective decisions
- Encourage open communication, cooperation and knowledge sharing
- Implement planning to organize, prioritize and measure individual work
- Interacts with customers/claimants to obtain facts, explain the coverage and claims process, set expectations and provide high quality service to achieve a positive customer experience
- Perform coverage analysis to review policy and endorsement language, giving consideration to definitions, exclusions, general conditions, jurisdictional rules/requirements, insurance, and policy period
- Plan and conduct investigation to determine liability and damages; use the claim facts to identify when a recorded interview should be obtained, such as when liability or damages are undetermined, subrogation potential exists, or in case of possible fraud or misrepresentation
- Assesses actual damages associated with claims and conducts negotiations to settle claims and achieve the best possible outcome
- Establish and maintain reserves based on the most probable outcome – i.e., the estimate of the ultimate financial cost to resolve a claim whether through settlement or other adjudication
- Use judgment and expertise to evaluate claim for potential fraud and subrogation; makes referrals to the Special Investigations Unit or Loss Recovery as appropriate
- Use claims system to properly document files (including initial resolution strategy, evaluation, negotiations, etc.), manage a diary and issue payments
- Knowledge of PIP and Med Pay claims coverage, clams handling procedures, and applicable laws
- Ability to negotiate, analyze/solve problems; plan/organize work; express facts clearly in writing and verbally; and communicate effectively
- Other capabilities include interpersonal skills, listening skills, tact, empathy, and drive for results
- Knowledge, skills, and capabilities normally acquired through a bachelor’s degree (or equivalent), completion of the formal training program, and at least 2 years of experience
- May be required to be licensed in states serviced. Pursuing continuing education courses leading to industry certifications (e.g., AEI, IIA, CPCU)
PEO Claims Specialist Resume Examples & Samples
- Provides daily case management activities on lost time claims. Proactively initiates recommendations for return to work opportunities and ensures successful implementation
- Partner with carrier on workers’ compensation claims issues and recommends best claims management strategies as appropriate
- Manages and negotiates carrier reserve reductions on an on-going basis
- Reviews client claim and risk information for clients; analyzes loss data and participates in making risk management recommendations for loss control and underwriting
- Functions as client/carrier liaison and advocate on claims service issues
- Provides internal and external client claims service issues
- Monitors workers’ compensation claim reports to control costs and ensure profitability
- Provides clients with industry surveys and statistics to educate on benefits of a return to work culture
- Analyzes issues and trends for program and policy recommendations
- Multi jurisdictional work comp knowledge and previous handling preferred
Senior Look No Further Claims Specialist Resume Examples & Samples
- Assists Look No Further Claim Specialists with inquiries regarding specific claims submitted
- Responds to hotel associates when an approved claim is challenged
- Reverses approved claims, as appropriate, ensuring proper communication with Accounting Department is made to reverse penalty fees assessed to hotels when claims are approved
- Research and resolve Marriott’s Look No Further claims reported via voice, email, and chat channels
- Utilize Engage to manage customer contacts and email communication regarding claims
- Properly document claim details, using screen shots and claim recording system, which are used by hotels to eliminate identified claim scenarios
- Determine if claim is approved or denied and communicate results to the customer
- Respond to all claims submitted within 24 hours of submission and within 4 hours for claims submitted for same-day reservations
- Report issues involving hotel information or specific anomalies to Marketing Systems for correction and notify eChannels regarding outside rate sources
- Identify trends in claim submission patterns and share those details with department leadership for action
- Seek assistance with challenging claim scenarios from manager, when necessary
- Utilize proper writing skills (grammar, spelling, formatting) for written communication with guests regarding claims
- Communicates directly with Customer Care Leadership to identify opportunities for individual associate instruction and identify service trends impacting department operations
- Maintains strong awareness of department procedures and systems, including processes supported by the multiple systems utilized (such as Engage, Outlook, PURE, eFolio, etc.) within the Customer Care Contact Centers
- Follows established department policies and procedures
- Utilizes sound judgment when encountering unique customer concerns without direct supervision
- Maintains a professional demeanor in personal appearance, work area and all interactions with guests, hotel personnel, peers, and management. Follows leadership guidelines for attire (business casual Monday – Thursday, casual attire on Friday) unless otherwise instructed by management
- Assist with training for new team members, as appropriate
- Maintains privacy and integrity of guest and associate personal information
- Performs a variety of other duties as directed by management
- Safety and Security
- Report work related accidents, or other injuries immediately upon occurrence to manager/supervisor
- Follow property specific procedures for handling emergency situations (e.g., evacuations, medical emergencies, natural disasters)
- Follow company and department safety and security policies and procedures to ensure a clean, safe, and secure environment
- Identify and correct unsafe work procedures or conditions and/or report them to management and security/safety personnel
- Six months employment with Marriott Global Reservation Sales and Customer Care
- No more than 5 occurrences on file (if applicable)
- 2 or less active notifications (if applicable)
- No active written warnings
- No written warnings or counseling on file for non-servicing, negative interaction or professional demeanor within the last 12 months
Related Job Titles

10 Returning to Work Resume Objective Examples
Returning to the workforce after a hiatus can seem daunting, but it also opens up a world of new possibilities for professional growth and fulfillment.
Whether your break was due to family commitments, personal development, or travel, crafting a compelling resume objective is a critical step in communicating your desire to rejoin the professional sphere.
This page offers a wide selection of carefully constructed resume objectives tailored to those seeking to navigate their way back into a fulfilling career.
Each example is designed to help you articulate your renewed commitment to the workforce and underscore the unique blend of skills and experiences you bring.
Let these ten returning-to-work resume objectives guide you in making a powerful first impression as you embark on this next chapter of your professional journey.

Return to Work Resume Objectives Examples

How to Write a Returning to Work Resume Objective?
Crafting a resume objective for returning to work involves conveying not just your fit for the job, but also your renewed commitment and the value you can bring post-hiatus. Here are some key strategies to create an effective resume objective:
1. Highlight Transferable Skills:
Emphasize any skills gained during your break that are relevant to the job you’re applying for. Transferable skills like organization, communication, or time management are often developed in various non-work activities.
2. Spotlight Continuous Learning:
If you’ve taken any courses or certifications during your time off, mention these to demonstrate initiative and a desire for continuous improvement.
3. Demonstrate Commitment:
Convey a strong willingness to not only return to the workforce but also to embrace the roles and responsibilities of your desired position.
4. Showcase Adaptability:
Indicate a readiness to adapt to new environments and the updated dynamics of the modern workplace, especially if there have been significant changes in your industry.
5. Mention Updated Knowledge:
If you’ve kept up with your industry’s trends or advancements during your break, make a note of this to show ongoing engagement with your professional sphere.
6. Express Enthusiasm:
Enthusiastic candidates are attractive to employers; express your excitement about re-entering the workforce and contributing to your potential employer’s success.
7. Personalize for the Role:
Tailor your objective to each job you apply for, ensuring it aligns with the company culture and the specifics of the job listing.
8. Address the Gap:
If feasible, briefly acknowledge the reason for your career break in a positive light, and focus on how it has prepared you to return to work with a fresh perspective.
- Mom Returning To Work Resume Objective | 8 Examples
- Retiree Returning to Work Cover Letter Template and Sample
- Housewife Returning to Work Cover Letter Sample
- Resume Template for Homemaker Returning to Work
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Notify me of new posts by email.

Reentering the Workforce

When returning to the workforce from a long time off, applicants need to reassess their skill set, resume, cover letter, and reacquaint themselves to the job market and how best to find a job. As we discuss in our post Understanding Applicant Tracking Systems, 9 8% of Fortune 500 companies use some type of system for hiring. These systems are always changing, and resumes need to keep up. Additionally, jobs can be posted all across the internet on LinkedIn, Monster, company websites, Craigslist, and more. To find the right job, someone will need to know where to look.
Out of work for over a year?
Anyone who has been out of the workforce for over a year will need to account for the time on their resume. Using a skills-based resume format , or identifying ways to account for this time, will help guide prospective employers to understand how the time has been spent. Including activities such as freelance work, volunteering, or part-time jobs can help account for that time and enhance the quality of the resume.
Reentering the workforce after 50
Workers who are reentering the workforce after a gap and who are over the age of 50 should take some time to evaluate the job market and learn how to best present themselves for their prospective job search. These workers are not at a disadvantage, but they do need to account for updating their resumes and cover letters, practicing interviews, and understanding the new methods for finding jobs .
Job retraining at 50
Job retraining may seem intimidating. However, in today’s workforce, retraining, also known as reskilling, has become an essential part of career progression for all ages. Some organizations require reskilling of their workforce periodically to keep with the constant advancements in technology. Retraining over 50 should be viewed as an exciting opportunity for career progression, whether it is required, for a promotion, or a lateral move.
Jobs for people over 50
People over the age of 50, or even retired, may have advantages based on their situations in life. They may be established financially, able to work non-traditional hours or have flexibility in their schedules that other job-seekers do not. Jobs can include rideshare drivers (Uber, Lift), greeters and attendants (baseball games, movie theaters), board members, consultants, or part-time college instructors for their areas of expertise.
Best Jobs for Moms Reentering the Workforce

Moms returning to the workforce may be forced to considering returning to a different job or career. In today’s economy, there numerous opportunities for moms to reenter the workforce while working from home . Glassdoor’s blog details 21 jobs for Stay at Home Moms, we discuss some of those options and more, below.
Best jobs for stay at home moms
- Babysitting – A win-win situation. Moms can make extra money by watching other children during the day while being at home with their own children.
- Pet sitting – Many people who work are searching for reliable places to take their pets during the day. For animal lovers, this can be a convenient job.
- Online Tutor – Online tutoring or mentoring for academic subjects, test preparation, and outside school activities can provide flexibility as well as good part-time income.
Best part time jobs for stay at home moms
- Fitness Instructor – Moms looking to get out of the house, earn money, and keep their fitness programs should look no further than a fitness instructor. Many local gyms are always looking for reliable people who can do the instruction on a part-time basis.
- Project Manager – Moms with a background in project management or other related skills may be able to find part-time jobs, often contract based, as a Project Manager for local companies.
- Medical Transcriptionist – Many medical companies are constantly looking for quality individuals with good typing skills to transcribe clinician dictation from audio to text for their medical records.
Best online jobs for stay at home moms
- Lifestyle Blogger – Stay at home Moms have a wealth of knowledge to share with others across the internet. Mom’s can start their own blog or look to do freelance pieces on topics that are relevant to them.
- Social Media Manager – Moms with a background in marketing or advertising may be a natural fit for a Social Media Manager. Depending on the size of the company, jobs can be freelance, part-time, full-time, and in many cases, all work can be performed online.
- Health Coaching – Online health coaching can earn big money. Moms can take numerous clients and assist with meal planning, work out schedules, and positive reinforcement to clients.
Reentering the Workforce Resume

Reentering the workforce resume examples
When reentering the workforce, or returning to work after some time, your professional resume will need to be revisited to best prepare for finding a new job. Below are tips to consider:
- Forget a chronological timeline – Our resumes often follow the same format of listing job history listed from newest to oldest jobs. Trying a different format, such as most relevant jobs, is acceptable and may be a refreshing change to the resume.
- Emphasize Skills – Understanding work history is important, but what was done during that time matters too. Identifying hard and soft skills and how they apply to the job should be emphasized.
- Tell the Truth – The worst thing a job-seeker can do is lie on their resume. They should be upfront and clear about the gap in work.
Cover Letter for Retired Person Returning to Work
Similarly, a cover letter for a retired person returning to work will need to be revisited and include elements listed below:
Sample cover letter for a retired person returning to work
- Discuss how the time off was spent – The retired person returning to the workforce should include any activities during their time off, including volunteering, part-time jobs, professional organization involvement, mentoring, or anything that has transferable skills to the prospective job.
- Tell the story – A retired person reentering the workforce probably has a good reason for doing so, and that should be included. Monster.com provides sample text for several situations to help tell the story in the cover letter.
Maria Gold is a Content Manager/Writer for Empire Resume . She is dedicated to helping educate and motivate people with the latest career articles and job search advice. Her interests range from writing to programming and design. She is also passionate about innovation, entrepreneurship, and technology .
Related Articles:

Creative Ways to Use Social Media to Find a Job

Applying for an Internal Position

What to Do When You Get Laid Off
4 thoughts on “ Reentering the Workforce ”
Vivek says:
Formal leave of absence letter example to use to request a leave from work, what to include in the letter , plus more examples and letter writing tips.
Derek says:
Have a wonderful summer, Palmer students! School returns August 1st at 9:15 a.m.! Advance Content (AC) Placement Criteria. To view detailed information about …
oprol evorter says:
Outstanding post, I believe people should acquire a lot from this site its very user genial.
how to deposit fiat says:
Wonderful work! This is the type of information that should be shared around the internet. Shame on the search engines for not positioning this post higher! Come on over and visit my site . Thanks =)
Leave a Reply Cancel Reply
Your email address will not be published. Required fields are marked *
You may use these HTML tags and attributes:
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Specialist resume examples for 2024
A specialist's resume should showcase their specific area of expertise, such as patient care in the healthcare sector or meeting sales goals in sales. Regardless of the field, strong product or service knowledge is essential. According to Dr. Andrew Busch , Assistant Professor of Health and Human Kinetics at Ohio Wesleyan University, "For students looking to get into graduate school and those looking to get hired within the field of Exercise Science...the more hands-on experiences one can be exposed to, the better equipped they will be to hit the ground running." Communication skills are also vital, as specialists need to convey their knowledge effectively within their organization.

Specialist resume example
How to format your specialist resume:.
- The job title on your resume should match your application for the role.
- Ensure your work experience focuses on achievements, rather than responsibilities.
- Recruiters and hiring managers suggest fitting your resume on one page.
Choose from 10+ customizable specialist resume templates
Choose from a variety of easy-to-use specialist resume templates and get expert advice from Zippia’s AI resume writer along the way. Using pre-approved templates, you can rest assured that the structure and format of your specialist resume is top notch. Choose a template with the colors, fonts & text sizes that are appropriate for your industry.

Entry level specialist resume example
Professional specialist resume example, resume tips to land the job:.
- If you're choosing between a resume objective or work experience and you want to fit your resume on one page, always choose work experience. However, it's ok for senior level specialist resumes to be two full pages long.
- Recruiters and hiring managers suggest short, succinct bullet points, instead of long, wordy paragraphs. Make it easy for recruiters to understand your key accomplishments, in 30 seconds.
- As a rule of thumb, lead each bullet point with a verb such "Grew", "Increased", or "Developed".
Specialist resume format and sections
1. add contact information to your specialist resume.
Specialist Resume Contact Information Example # 1
Montgomery, AL 36043| 333-111-2222 | [email protected]
2. Add relevant education to your specialist resume
Your resume's education section should include:
- The name of your school
- The date you graduated ( Month, Year or Year are both appropriate)
- The name of your degree
If you graduated more than 15 years ago, you should consider dropping your graduation date to avoid age discrimination.
Optional subsections for your education section include:
- Academic awards (Dean's List, Latin honors, etc. )
- GPA (if you're a recent graduate and your GPA was 3.5+)
- Extra certifications
- Academic projects (thesis, dissertation, etc. )
Other tips to consider when writing your education section include:
- If you're a recent graduate, you might opt to place your education section above your experience section
- The more work experience you get, the shorter your education section should be
- List your education in reverse chronological order, with your most recent and high-ranking degrees first
- If you haven't graduated yet, you can include "Expected graduation date" to the entry for that school
Check More About Specialist Education
Specialist Resume Relevant Education Example # 1
Doctoral Degree In Finance 2013 - 2016
DePaul University Chicago, IL
Specialist Resume Relevant Education Example # 2
Some College Courses In Medical Assisting Services 2008 - 2010
Vista College S Waldron Road, Fort Smith, AZ
3. Next, create a specialist skills section on your resume
Your resume's skills section should include the most important keywords from the job description, as long as you actually have those skills. If you haven't started your job search yet, you can look over resumes to get an idea of what skills are the most important.
Here are some tips to keep in mind when writing your resume's skills section:
- Include 6-12 skills, in bullet point form
- List mostly hard skills ; soft skills are hard to test
- Emphasize the skills that are most important for the job
Hard skills are generally more important to hiring managers because they relate to on-the-job knowledge and specific experience with a certain technology or process.
Soft skills are also valuable, as they're highly transferable and make you a great person to work alongside, but they're impossible to prove on a resume.
Example of skills to include on an specialist resume
Customer service is the process of offering assistance to all the current and potential customers -- answering questions, fixing problems, and providing excellent service. The main goal of customer service is to build a strong relationship with the customers so that they keep coming back for more business.
Patient care entails the diagnosis, recovery, and control of sickness as well as the maintenance of physical and emotional well-being through the use of healthcare providers' services. Patient care is described as services provided to patients by health practitioners or non-professionals under guidance.
Troubleshooting is the process of analyzing and fixing any kind of problem in a system or a machine. Troubleshooting is the detailed yet quick search in the system for the main source of an issue and solving it.
Product knowledge is the skill of having better information and knowledge about the product you are selling. Product knowledge is essential for the employees of the companies so they can communicate and inform the customers about the product. Having great product knowledge is essential for a better sales pitch and to give the customer a better and complete idea of the product that will influence him to buy the product eventually.
HR stands for human resources and is used to describe the set of people who work for a company or an organization. HR responsibilities revolve around updating employee records and carrying out management processes like planning, recruitment, evaluation, and selection processes. HR is a key contributor to any company or organization's growth as they are in charge of hiring the right employees, processing payrolls, conducting disciplinary actions, etc.
Mental health is the state of wellbeing in which an individual can cope with the regular stresses and tensions of life, and can work productively without having any emotional or psychological breakdown. Mental health is essential for a person of any age and helps them make the right decisions in their life.
POS is an abbreviation of "Point of Sale" which is the time and place where a customer completes a transaction. It can either be a physical shop that consists of POS terminals or a virtual shop. A POS system helps simplify the retail functions and track important sales data.
Top Skills for a Specialist
- Patients , 15.0%
- Customer Service , 11.0%
- Work Ethic , 5.4%
- Patient Care , 4.3%
- Other Skills , 64.3%
4. List your specialist experience
The most important part of any resume for a specialist is the experience section. Recruiters and hiring managers expect to see your experience listed in reverse chronological order, meaning that you should begin with your most recent experience and then work backwards.
Don't just list your job duties below each job entry. Instead, make sure most of your bullet points discuss impressive achievements from your past positions. Whenever you can, use numbers to contextualize your accomplishments for the hiring manager reading your resume.
It's okay if you can't include exact percentages or dollar figures. There's a big difference even between saying "Managed a team of specialists" and "Managed a team of 6 specialists over a 9-month project. "
Most importantly, make sure that the experience you include is relevant to the job you're applying for. Use the job description to ensure that each bullet point on your resume is appropriate and helpful.
What experience really stands out on Specialist resumes?
Assistant Professor , Northwestern State University
- Executed backup and regular maintenance procedures.
- Deployed and managed over 500 computer accounts consisting of both Windows servers and workstations.
- Provided information and services for the repair or replacement defective hardware.
- Provided desktop support for multiple users for wide range of situations Updated existing inventory of all hardware.
- Developed methods and procedures to capture, generate, or import data into the GIS.
- Solved various communications problems relating to modems and networks.
- Diagnosed and resolved IBM pSeries hardware issues by phone Determined action plans for onsite technician repairs
- Used tools and machinery to assembly parts on-line during shifts and followed safety policies.
- Trained for NETeam instructor on IBM networking hardware products.
- Created LANE segments on token switches to isolate floors for easier problem determination.
- Monitored and managed external/internal procedures to ensure the requirements of quality, reliability and responsiveness were met and exceeded.
- Performed security, network, computer hardware and software audits.
- Revised portions of document set to align procedures with new/updated business models, regulatory changes, and legal requirements.
- Operated and maintained Xerox DocuTech high speed laser printer including first level troubleshooting.
- Served the technology needs of 16 FedEx Office Centers in the Greater Cincinnati area.
- Maintained communication with store management to discuss business performance.
- Observed checkout procedures to ensure accuracy with service and cash handling.
- Downloaded and fulfilled internet orders daily.
- Helped design and position new specialty shops for several Macys department stores.
- Handled customer service for purchases through me and other associated.
5. Highlight specialist certifications on your resume
Specific specialist certifications can be a powerful tool to show employers you've developed the appropriate skills.
If you have any of these certifications, make sure to put them on your specialist resume:
- Certified Phlebotomy Technician (CPT)
- Certified Billing and Coding Specialist (CBCS)
- Certified Pharmacy Technician (CPhT)
- Dental Assistant (RDA)
- Certified Medical Interpreter - Spanish (CMI)
- Certified Medical Office Manager (CMOM)
- First Aid, CPR and AED Instructor
- International Accredited Business Accountant (IABA)
- Certified Coding Specialist (CCS)
- Certified Clinical Medical Assistant (NHA)
6. Finally, add an specialist resume summary or objective statement
A resume summary statement consists of 1-3 sentences at the top of your specialist resume that quickly summarizes who you are and what you have to offer. The summary statement should include your job title, years of experience (if it's 3+), and an impressive accomplishment, if you have space for it.
Remember to emphasize skills and experiences that feature in the job description.
Common specialist resume skills
- Customer Service
- Patient Care
- Exceptional Client
- Troubleshoot
- Product Knowledge
- Mental Health
- Sales Floor
- Technical Assistance
- Community Resources
- Blended Learning
- Customer Complaints
- Outbound Calls
- Led Training
- Inbound Calls
- Scheduling Appointments
- Federal Regulations
- Inventory Control
- Computer System
- Technical Issues
- Customer Accounts
- Medical Treatment
- Opportunity Management
- Customer Issues
- Customer Inquiries
- Excellent Guest
- Telephone Calls
- Sales Margins
- Unified Communications
Entry level specialist resume templates

Professional specialist resume templates

Specialist Jobs
Links to help optimize your specialist resume.
- How To Write A Resume
- List Of Skills For Your Resume
- How To Write A Resume Summary Statement
- Action Words For Your Resume
- How To List References On Your Resume
Updated June 25, 2024
Editorial Staff
The Zippia Research Team has spent countless hours reviewing resumes, job postings, and government data to determine what goes into getting a job in each phase of life. Professional writers and data scientists comprise the Zippia Research Team.
Specialist Related Resumes
- Activity Specialist Resume
- Business Specialist Resume
- Call Center Specialist Resume
- Family Specialist Resume
- Fraud Specialist Resume
- Funding Specialist Resume
- Imaging Specialist Resume
- Information Specialist Resume
- Insurance Specialist Resume
- Intake Specialist Resume
- Mortgage Specialist Resume
- Operations Specialist Resume
- Order Specialist Resume
- Product Specialist Resume
- Records Specialist Resume
Specialist Related Careers
- Activity Specialist
- Authorization Specialist
- Business Specialist
- Call Center Specialist
- Client Support Specialist
- Family Specialist
- Fraud Specialist
- Funding Specialist
- Imaging Specialist
- Information Specialist
- Insurance Specialist
- Intake Specialist
- Mortgage Specialist
- Operations Specialist
- Order Specialist
Specialist Related Jobs
Specialist jobs by location.
- Specialist Anaheim
- Specialist Apple Valley
- Specialist Bay Saint Louis
- Specialist Bensalem
- Specialist Buda
- Specialist Dennis
- Specialist Euless
- Specialist Hutchinson
- Specialist Jersey City
- Specialist Lawton
- Specialist Lehigh
- Specialist Milwaukee
- Specialist Poway
- Specialist Saint Paul
- Specialist San Juan
- Zippia Careers
- Computer and Mathematical Industry
- Specialist Resume
Browse computer and mathematical jobs
Workers Compensation Specialist Resume Sample
The resume builder.
Create a Resume in Minutes with Professional Resume Templates
Work Experience
- Responsible for compliance with all regulations from the Workers’ Compensation Board including timely EDI and compliance reporting requirements and resolution of any EDI and/or compliance issues. Expert knowledge of Disability and Medical Treatment Guidelines. Mentor other case analysts for understanding and compliance to regulations and laws
- Responsible for each case’s compliance with established service standards
- Organize each workload so that all cases receive the proper claims handling and are promptly brought to a conclusion
- Assist in the training, development and orientation of the Case Analysts
- Assist in handling administrative issues that arise in the claims team environment
- Represent the company at meetings and presentations
- Understands and works within PERMA’s Core Beliefs
- Takes a proactive approach to office safety and ergonomics and adheres to all safety policies
- Partners with local Health Services Department to develops and documents plant specific policies and procedures to ensure compliance with mandated programs of Company and Provincial organizations
- Collaborates with Third Party Administrator and legal counsel
- Maintain the accuracy and integrity of Workers' Compensation claim records
- Maintain an agency based control and tracking system to enable compliance with OSHA record keeping and annual filing requirements
- Maintain derivative databases that track the incidence of certain types of injury/illness (e.g., carpal tunnel, motor vehicle)
- Generate reports from various records and databases in order to help leadership analyze and determine root causes
- Acts as first and primary point of contact for employees and/or worksite liaisons/supervisors, as appropriate, regarding information needed to process and judge claims; e.g., medical documentation, filing status and exemption form, election to use accrued leave, return- to-work plans
- Responds to employee concerns, such as, completion of paperwork, claim status, payment of medical bills, send forms, as appropriate to provide and work directly with our third party administrator (TPA)
- Communicate with the Director- LP and VP-LP regarding inquiries from attorneys, doctors, and other interested parties, as necessary, regarding claim related matters
- Coordinate a modified work opportunities and requests with the HR Wellness team
- Maintain related communications with the TPA's hearing representative
- Report to management on claim status, costs, causes provided by the Company’s claim provider
- Participate as an advisor or member of safety committees, as requested
- Ensure all Workers Compensation accounts are reviewed timely
- Contact employers and insurance carriers to confirm claim details and obtain billing address
- Communicate carrier information to vendors, to ensure timely delivery of claim to correct party Work collaboratively with Marketing to address any employer billing concerns
- Serve as primary contact for Workers Compensation inquiries
Professional Skills
- Excellent interpersonal, communication, and problem solving skills with excellent attention to detail
- Organizational skills, including the ability to prioritize work and handle multiple tasks simultaneously and under pressure
- Excellent interpersonal and communication skills including the ability to retain a high level of confidentidality
- Strong analytical skills with ability to collect, organize, analyze and disseminate information with attention to detail and accuracy
- Strong project management skills and ability to influence cross functionally
- Excellent understanding of worker’s compensation insurance policy terms and conditions; experience in purchasing and renewing coverage
- Assess complaints and disputes with sound reasoning, decision and problem solving skills, and refer to management to handle
How to write Workers Compensation Specialist Resume
Workers Compensation Specialist role is responsible for training, basic, payroll, compensation, finance, database, purchasing, litigation, shipping, reporting. To write great resume for workers compensation specialist job, your resume must include:
- Your contact information
- Work experience
- Skill listing
Contact Information For Workers Compensation Specialist Resume
The section contact information is important in your workers compensation specialist resume. The recruiter has to be able to contact you ASAP if they like to offer you the job. This is why you need to provide your:
- First and last name
- Telephone number
Work Experience in Your Workers Compensation Specialist Resume
The section work experience is an essential part of your workers compensation specialist resume. It’s the one thing the recruiter really cares about and pays the most attention to. This section, however, is not just a list of your previous workers compensation specialist responsibilities. It's meant to present you as a wholesome candidate by showcasing your relevant accomplishments and should be tailored specifically to the particular workers compensation specialist position you're applying to. The work experience section should be the detailed summary of your latest 3 or 4 positions.
Representative Workers Compensation Specialist resume experience can include:
- Effectively work with all levels of the organization and cross-functional teams
- Provide direction and management to third party administrators to facilitate resolving all claims quickly and cost effectively
- Communicate effectively with Management, Administrators, Department Managers, Claim Adjusters, etc. regarding claims activity and process
- Prepares and provides information and assistance to attorneys in order to effectively litigate and resolve claims
- Coordinates with applicable parties (vendors, internal payroll, human resource partners) to effectively administer the workers comp process
- Procifiency in MS Office Products and experience with creating and generating reports, plans, instructions, and maintain files
Education on a Workers Compensation Specialist Resume
Make sure to make education a priority on your workers compensation specialist resume. If you’ve been working for a few years and have a few solid positions to show, put your education after your workers compensation specialist experience. For example, if you have a Ph.D in Neuroscience and a Master's in the same sphere, just list your Ph.D. Besides the doctorate, Master’s degrees go next, followed by Bachelor’s and finally, Associate’s degree.
Additional details to include:
- School you graduated from
- Major/ minor
- Year of graduation
- Location of school
These are the four additional pieces of information you should mention when listing your education on your resume.
Professional Skills in Workers Compensation Specialist Resume
When listing skills on your workers compensation specialist resume, remember always to be honest about your level of ability. Include the Skills section after experience.
Present the most important skills in your resume, there's a list of typical workers compensation specialist skills:
- Experience in workers compensation and 3+ years appropriate work experience in human resources, risk management or related field. (5 years total)
- Juris Doctor and 5 or more years of experience in the Claims or Litigation area to include at least 4 years of Workers Compensation Claims experience
- Communicate effectively and tactfully with all levels of management, attorneys and others
- Computer skills to include Microsoft Office / Word / Excel / PowerPoint and ability to learn specialized programs specific to the profession
- Juris Doctor and 5 or more years of experience in the Claims or Litigation area to include at least 3 years of Workers Compensation Claims experience
- Proven ability to solve difficult problems and overcome conflict situations with effective solutions
List of Typical Experience For a Workers Compensation Specialist Resume
Experience for workers compensation claims specialist resume.
- Experience working on Workers Compensation or Liability claims
- Experience working on Workers Compensation claims
- Workers’ compensation claims experience
- Provide additional support in assessing areas to address relative to Safety Training and Loss Control
- Better than basic understanding of OSHA guidelines with emphasis on the regulations relating to worker’s compensation claims
- Serves as a voice in strategic planning aimed at reducing the incidence of worker's compensation-related injuries throughout the organization as a whole
- Basic understanding of reserving, medical management and compensability standards under Maine Workers' Compensation
- Assists employees in understanding their medical conditions and their legal rights and responsibilities
Experience For Workers Compensation Senior Claims Specialist Resume
- Collects, evaluates and maintains data concerning workers' compensation
- Work with Holiday’s third-party claims administrator, or TPA, to approve claim reserves and coordinate action plans for resolving claims
- Train Administrators and Department Managers on the internal claim reporting process
- Assist in safety training and provide input on safety issues/concerns
- Facilitate questions regarding benefits and educates employees
- Initiates contact with employees, supervisors, and doctor's office regarding workers' compensation claims
Experience For Workers Compensation Associate Claims Specialist Resume
- Engages as a member of the team through participation in meetings and reporting on departmental performance and initiatives
- Maintains filing system on assigned claims
- Practices and procedures of claims management including investigation and evaluation
- California Labor Code, Government Code provisions and case laws governing Workers' Compensation
- Provide assistance with claims and obtaining health care as appropriate
- Provide record keeping support in the Office of Benefits and Leave
Experience For Senior Workers Compensation Claims Specialist Resume
- Administer light duty and return to work employee program by closely working with supervisors and department heads
- Communicate with payroll regarding employees status and internal payments
- Self-starter with multitasking abilities
- Track claim costs and overall company costs of claims. Ensures vendors are working in the best interest of the employee and Medline
- Serve as resource for management for all questions related to injuries, post-accident drug testing and return to work options
- Serve as the contact person regarding all work related injuries
Experience For Complex Workers Compensation Technical Claims Specialist Resume
- Assist employees with filling out all forms related to a specific injury
- Arrange and follow up on doctor, physical therapy, and diagnostic testing appointments for employees. Maintain appointment log
- Accurately responds to non-routine inquiries from management and employees regarding workers comp in a customer-focused, timely manner
- Coordinate plan of care and provide ongoing communication with patients, adjusters, case managers, insurers and other regulatory agencies
- Have working knowledge of workers’ comp protocols and statutes
Experience For Employee Experience Associate Specialist Workers Compensation Resume
- Manage, scan, and input large amounts of incoming documents
- Learn rapidly to develop knowledge and understanding of claims practice
- Oversees workers’ compensation claims, with primary focus on mitigation of the company’s compensation liability
- Provides information and support to employees with work-related medical conditions or disabilities, supervisors, and HR
- Partners with WC Claim team, Legal and HR to facilitate appropriate long term employment solutions for employees permanently impacted under workers’ compensation
Experience For Workers Compensation & Leave Program Specialist Resume
- Facilitates and manages the Return to Work program to implement strategies that are cost effective for the company and productive and meaningful for the employee
- Assists in finding Modified Duty assignments
- Tracks employees who are on Modified Duty
- Ensures medical evaluation milestones are met
- Works with the Safety team to support injury prevention programs. Analyzes injury reports to identify trends and provides recommendations and development support of programs or enhancements to reduce incident rates
- Provides oversight of Audiometric testing, ergonomics and Spirometry programs
- Prepares all necessary forms, records and documentation, to include statistical analyses and reports, for all claims assigned, as required by various regulatory agencies including the DWC 1, OSHA 300 log and summary
- Works with Corporate WC Claim team in Mason, OH to provide input and facts regarding claims for cases pending litigation or settlement
- Develops training, policy and procedural revisions
Experience For Middle Market Workers Compensation Research Planning & Development Specialist Resume
- Provides analysis and reporting to include metric dashboard presentations, validation of claim data accuracy, incident reporting and analysis, incident investigation, claim management, and business partner support (education/guidance)
- Follows all applicable laws and administers programs in accordance to company policies and procedures
- Investigate and analyze claims information and to draw conclusions
- Administers the Worker's Compensation claims process, receives and reviews all associated documentation and follow-up as needed
- Assist in coordinating all risk management meetings, as well as assist with preparation and distribution of materials needed for presentations. Assist with updating spreadsheets with new loss information, updating open/closed claims, updates dollar amounts, updates number of days of restrictions and updates days away by end of quarter
Experience For Workers Compensation Technical Claims Specialist Resume
- Gather data for the preparation of regularly scheduled reports; arrange and compile such reports; and forward those reports to designated personnel in the corporate office
- Oversee slip resistant shoe incentive program
- Oversee TPA claims management, including oversight of TPA adjusters and adherence to special handling instructions, claim handling best practices and Holiday’s culture and philosophy
- Coordinate with Holiday’s Legal Department, Holiday’s TPA and local counsel in litigating denied or disputed claims
- Review and oversee the handling of all workers’ compensation claims for an assigned portfolio of Holiday communities
- Coordinate with other members of Holiday’s risk management team to set strategic goals for managing complex claims
- Implement Holiday’s return-to-work program
Experience For Workers Compensation Medical Claims Specialist Resume
- Work with Holiday’s Employee Relations, Safety, Legal and other departments to facilitate a holistic approach to safety and workers compensation losses
- Work with Holiday’s Employee Relations, Safety, Legal and other departments to facilitate a holistic approach to safety and workers’ compensation losses
- Provide support, training and leadership to Holiday communities and field leaders in loss mitigation strategies and the operation of the workers’ compensation program
- Provides oversight regarding WC policy (ies) to include Return to Work policy (ies), and other return to work issues
- Manage key relationship with TPA, law firms, & vendors including contract negotiations, stewardship requirements and proper delivery of services
- Responds to employees’ questions and requests for information relating to coverage matters
- Enjoys collaboration to accomplish goals
- Willing to take ownership and tackle obstacles to meet client's quality standards for service, investigation, reserving, inventory management, teamwork, and diversity appreciation
- Willing to take ownership and tackle obstacles to meet quality standards for service, investigation, reserving, inventory management, teamwork, and diversity appreciation
List of Typical Skills For a Workers Compensation Specialist Resume
Skills for workers compensation claims specialist resume.
- Excellent verbal and written communication skills and ability to interact effectively with all levels within the organization, medical providers and lawyers
- Accurate and current diaries to manage claims effectively and timely
- Above average basic math skills to analyze claims cost, reserves and settlements
- Experience facilitating and managing WC & H&S programs in a manufacturing environment in California
- Demonstrates ability for independent critical thinking, utilizing knowledge and legal guidelines to make appropriate decisions/recommendations
- Experience reviewing claims, determining the nature of claims and adherence to current guidelines, regulations, and policies
- Juris Doctor and 2 or more years of experience in the Claims handling and Litigation area
Skills For Workers Compensation Senior Claims Specialist Resume
- Nevada workers compensation claims handling experience
- New York and New Jersey workers compensation claims handling experience
- Experience handling Workers Compensation claims
- Experience handling FL, GA, AL and SC Workers Compensation Claims
- New York and/or New Jersey workers compensation claims handling experience
- PA, VA, DE, DC and/or WV workers compensation claims handling experience
- Texas, Oklahoma, Louisiana, and/or Mississippi workers compensation claims handling experience
- Experience handling Texas, Oklahoma, Louisiana, and Mississippi Workers Compensation Claims
Skills For Workers Compensation Associate Claims Specialist Resume
- Arizona claims handling Experience
- California workers’ compensation claims handling experience
- Arizona workers compensation claims handling experience
- Arkansas, Oklahoma & Texas workers compensation claims handling experience
- Strong knowledge of MS programs, including Word and Excel, as well as an ability to quickly learn new software programs
- Initiates appropriate notices as needed; monitors claimant's case history, noting any prior workers' compensation claims filed
- Experience in a manufacturing environment highly desireable
Skills For Senior Workers Compensation Claims Specialist Resume
- Establish and maintain effective working relationships with all levels of staff and the public
- Determine validity and compensability of the claim
- Experience handling California Workers’ Compensation Claims
- Experience handling Florida Workers’ Compensation Claims
- California Workers Compensation claims handling experience
- Experience handling Louisiana Workers Compensation Claims
- Workers’ compensation claims handling experience
- GA, FL , AL, NC and/or SC workers’ compensation claims handling experience
Skills For Complex Workers Compensation Technical Claims Specialist Resume
- CA workers compensation claims handling experience
- Experience handling construction industry workers compensation claims
- Experience handling Minnesota and West Virginia Workers Compensation claims
- Workers compensation claims handling experience
- GA, FL, AL, NC and/or SC workers’ compensation claims handling experience
- Excellent claims management documentation within the TPA claims software system (ACTS) to ensure compliance with audit standards and requirements
- Senior level knowledge and eight (8) years’ experience in human resources practices and principles
- Claims experience in workers compensation
Skills For Employee Experience Associate Specialist Workers Compensation Resume
- Workers compensation experience preferably in the Entertainment field
- Juris Doctor and 2 or more years of experience in the Claims and Litigation area
- Juris Doctor and 5 or more years of experience in the Claims or Litigation area OR
- NY, NJ, PA, VA, DE and/or DC workers compensation claims handling experience
- One year of workers compensation experience
- Experience with Workers Compensation
- Excel, Microsoft and Outlook experience
- ADR (Alternate Dispute Resolution) Experience
- Highly skilled in MS Word, Excel and Power Point
Skills For Workers Compensation & Leave Program Specialist Resume
- Experience in risk management desired
- Demonstrated ability to treat confidential matters with appropriate discretion
- Facilitates changes or enhancements to improve the overall effectiveness of the Worker Compensation program
- Solid familiarity through practice and/or education with state and federal regulations in the areas of Leaves of Absence/FMLA, ADA and interactive process
- Experience working with Workers’ Compensation claims
- Experienced with Workers’ Compensation programs
- Experience in a large company
- Kronos (HRIS System) experience is desired
Skills For Middle Market Workers Compensation Research Planning & Development Specialist Resume
- Is responsible for completing, updating and reporting OSHA logs for all facilities to BLS and OSHA
- Complete pre-employment, post accident, and random drug testing and breath alcohol testing for employees including those covered by DOT regulations
- Maintain ordering and shipping of drug testing supplies for all locations
- Act as a liaison between all parties in workers compensation claims to ensure quality claims management including providing updates and recommendations
- Prepare forms related to workers' compensation claim reporting in multiple states. Ensure organization and timely filing of all documents
- Act as subject matter expert for management at business units, coaching and guiding them through the claims process
- Oversee and monitor the claim process from beginning to end to ensure proper and timely closing
Skills For Workers Compensation Technical Claims Specialist Resume
- Gathers facts regarding claims for cases pending litigation
- Complete pre-employment, post-accident, and random drug testing and breath alcohol testing
- Provide reserve and settlement authority according to department procedures
- Act as the first level of appeal for Dart personnel regarding claim decisions
- Establish reserves and authorize payments within reserving authority limits
Skills For Workers Compensation Medical Claims Specialist Resume
- Comply with all safety rules and regulations during work hours in conjunction with the Injury and Illness Prevention Program (IIPP)
- Possesses basic knowledge of legal reporting requirements per the Maine Workers Compensation Laws
- CPR Certified and Blood-Borne Pathogen Training
- A self-starter with a positive approach to getting the job done in a timely manner
- Proficient in managing insurance brokerage relationships
- Background in WSIB claims handling and management
- Background in Workers Compensation claims handling and management
- Review and respond to all emails filtered through DL, relating to Workers Compensation
List of Typical Responsibilities For a Workers Compensation Specialist Resume
Responsibilities for workers compensation claims specialist resume.
- Experienced in standard established risk management practices
- Coordinates and administers activities associated with determining primary liability and negotiating resolution of workers' compensation claims
- Coordinates claims handling, data analysis, and maintains the program within state regulations and supports Allina Health Risk Services with goals, processes, and strategic initiatives related to workers’ compensation
- Assists in the monitoring, evaluation and coordination of ongoing medical treatment for the injured employees
- Coordinates analysis of employee incident reports, identifying trends, commonalities and patterns so that reason of reoccurrence can be ascertained in order to correct the circumstances, thus reducing injuries
Responsibilities For Workers Compensation Senior Claims Specialist Resume
- Accurate reserve analysis following reserve best practices including the completion of a reserve worksheet with documentation on the claim file
- Build rapport, establish an interactive process and foster a caring culture with employees
- Determine need to report claims to TPA for handling
- Communicate directly with employees in a professional and courteous manner while explaining the claim process
- Distribution of weekly and monthly claim/metric reports to Management providing claim statistics and results
Responsibilities For Workers Compensation Associate Claims Specialist Resume
- Ensure appropriate medical care is provided for those that require it, as well as monitor vendors to make sure they are actively managing Medline's claims
- Coordinate between patient, doctor???s offices, and insurance carriers to resolve billing issues
- Serve as the main point of contact regarding all work related injuries
- Arrange and follow up on doctor, physical therapy and diagnostic testing appointments for employees
- Communicate with insurance carrier for claims processing
- Ensures proper implementation of Workers Compensation/Occupational Benefits claims handling and oversees Third Party Administrator processes
- Works with third party administrator to assist with the coordination of treatment, follow-up and referral of all work related injuries and illnesses
Responsibilities For Senior Workers Compensation Claims Specialist Resume
- Drive claims process via proactive and regular dialogues with adjusters to ensure timely follow through of actions items
- Lead claim review meetings
- Collaborate with Disability Case Managers to identify employees’ work restrictions and analyze potential accommodations
- Advise and consult with human resources and employees’ managers on claim resolution
- Participate on the various committees and advise on workers’ compensation related issues
- Processes day to day requests for insurance issues such as certificates of insurance, verification of coverage documents,
- Works with attorneys and Director of insurance on advice matters and claim issue
- Coordinates and oversees assigned workers’ compensation claims with adjusters, case managers, providers, claimants, supervisors to ensure claims are being properly adjusted. Communicates regularly with principals/supervisors and HR regarding active claims while injured worker is losing time due to injury
- Identifies transitional duty candidates from the information received on return-to-work status reports (DWC-73) from the injured employees’ treating physician. Coordinates back-to-work transition, adhering to employee’s restrictions, by providing a Bona Fide Job Offer to the injured employee, per HISD Policy CRE2
Responsibilities For Complex Workers Compensation Technical Claims Specialist Resume
- Review and manage all incident reports for employee incidents from initial report through conclusion/closure of claim
- Manage claims database and TPA's claim information, via internal software as well as via various TPA databases
- Manage external attorneys on litigated matters
- Maintenance of internal claim files
- Participate actively in various risk management meetings
- Develop Webinars on claims process as well as safety topics
- Review and manage internal safety inspection checklist/process (monthly/quarterly)
- Keep safety manual up to date and provide input for improvements
Responsibilities For Employee Experience Associate Specialist Workers Compensation Resume
- Overall ownership of global workers compensation for both insured and self-insured models
- Design and implement the process and workflows that are efficient and aligned with our culture
- Act as the Liaison between the employee and the Third Party Administrator
- Verifies wages, work injuries and work restrictions
- Coordinates with all productions to ensure the proper state forms are completed and procedures are followed
- Establishes and maintains case files, logs, and indexes; reviews documentation and records
- Verifies job-related accidents with claimants and supervisors
Responsibilities For Workers Compensation & Leave Program Specialist Resume
- Addresses suspicious claims and delays cases when necessary
- Maintains and updates diaries on employee's workers' compensation injury status
- Authorizes any and all medically necessary treatment; authorizes payments
- Monitors payments for permanent disability
- Understand, interpret and follow laws, ordinances, regulations and procedures
Responsibilities For Middle Market Workers Compensation Research Planning & Development Specialist Resume
- Knowledge of basic medical terminology related to the cause and treatment of occupational injuries and diseases
- Manage a caseload and respond to requests in a timely manner
- Possession of a certificate in Workers' Compensation from an institution recognized by the California Department of Insurance or the Insurance Education Association is highly desired
- Receive and process accident reports and workers’ compensation claims
- Serve as a liaison between the employee, department, and adjusters
Responsibilities For Workers Compensation Technical Claims Specialist Resume
- File all insurance forms and Texas Department of Workers’ Compensation reports
- Handle wage statements, first report of injury, supplement report, and job information in a timely manner
- Establish and maintain contact with injured employees
- Communicate with workers’ compensation insurance carrier, doctors, nurses, departments, and health care providers to enable appropriate processing of claims
- Work closely with department secretaries, supervisors, and administrators to facilitate reporting work-related illnesses and injuries
- Work with leave and benefit specialists to ensure appropriate use and access to applicable leave and insurance benefits
Responsibilities For Workers Compensation Medical Claims Specialist Resume
- Report and educate campus staff on workers comp
- Regularly communicate with HR staff, other department staff, employees, and the public
- Regularly interacts, interviews and partners with employees to complete accident investigation and root cause analysis
- Process the claim to insurance company and to individual state based on additional requirements
- Accurately maintains all workers comp documents, both accident and incident investigations
- Communicates and interacts with employees, insurance adjusters, medical professionals, and legal advisors
- Serves as the representative of the company represents and attends Workers' Compensation Administration mediation and formal hearings and partners with appropriate level of authority internally to settle claims
- Assist with Production meetings and trainings
- CWCP certification is desired
Related to Workers Compensation Specialist Resume Samples
Compensation specialist resume sample, workers compensation resume sample, workers compensation claims adjuster resume sample, center support resume sample, tech, tech support resume sample, expert support resume sample, resume builder.
- RTÉ Archives
- RTÉ Brainstorm
- RTÉ Learn
- RTÉ Radio 1
- RTÉ lyric fm
- RTÉ Raidió na Gaeltachta
- RTÉ Weather
- Century Ireland
- Policies and Reports
- Terms & Conditions
- Individual Rights Guide
- Privacy Policy
- Cookie Policy
- Freedom of Information
- Latest Annual Report
- Advertise with RTÉ
- Newsletters
- RTÉ Supporting the Arts
Call for better integration of perinatal mental health services

The National Women's Council has recommended better integration of specialist perinatal mental health services with general maternity, primary care and other mental health services.
It follows a roundtable discussion around perinatal mental health, which was convened by the NWC last November.
Diverse participants took part including representatives from mental health services, advocacy groups, academics, Traveller women, migrant women, and women with lived experience of mental health difficulties.
Up to 20% of women experience mental health difficulties during the perinatal period which impacts maternal and infant well-being.
Perinatal refers to the late stages of pregnancy, the labour and delivery process, and the initial days following childbirth. Perinatal mental health issues include anxiety, mild to severe depression, stress and adjustment difficulties.
One-in-five women encounter a mental health difficulty during the perinatal period, according to research.
The panel noted that the absence of a dedicated mother and baby unit in Ireland, resource shortages, and workforce constraints are exacerbating the problems for women.
Currently, mothers are separated from their newborn babies when inpatient treatment is required in Ireland.
The NWC has said a dedicated mother and baby unit should be established at St Vincent's University Hospital in Dublin.
The roundtable also focused on the experiences of marginalised women including migrant women, Traveller women and Roma women who often face inequalities when accessing care and supports.
The council has recommended that perinatal mental health policies should be informed by gender sensitive approaches and trauma informed practices.
Perinatal bereavement and trauma services including palliative care services should be improved along with a secure and sustainable investment in the HSE's perinatal mental health services.
More stories on

More by Dimitri O'Donnell

Public encouraged to apply to join Garda Reserve

'It changed my life' - call for more bone marrow donors

Court told Prof Philip Nolan 'entitled' to return to work

Prof Philip Nolan leaves SFI amid misconduct allegations

Hi, what are you looking for?
Capital News

Clinical officers end 99-day strike after deal with Governors

Success of young mothers living with HIV forming table banking group for social economic empowerment

Water project halted to protect nesting swallows: China Daily

A village that gives home to orphans affected by HIV/AIDS
(VIDEO) Police teargas and arrest “occupy parliament” protestors in Nairobi

Image shows road destroyed by underground explosion in South Africa, not Kenya

Posts falsely claim old video shows Kenyan protesters storming Kitale police station
How to identify AI-generated images that fool people

Anti-LGBTQ disinformation surges online in East Africa

Logo of Kenyan political party digitally added to cult leader’s T-shirt

In Rwanda, ethnicity doesn’t matter to people if their needs are met: study

Liberian president cuts his salary by 40pc

Ramaphosa made practical choices for South Africa’s multi-party cabinet – how this will help him down the line

UN Security Council urges enhanced efforts to protect civilians in armed conflict

WHO roots for increased funding for migrant-hosting African States

Unmanned aerial taxis to take off in Guangzhou – China Daily

Former head of China Geological Survey arrested – China Daily

Chinese researchers design wristwatch for real-time health monitoring through sweat – China Daily

China expands infectious disease direct reporting system – China Daily

Advanced technologies need more legal protection, report says – China Daily

Gachagua accuses top Interior Ministry officials of sabotaging war on illicit brews

13 pupils injured after school bus crashed in Kwale

4 youths killed in a chaotic funeral procession marred with phone snatching

Police recover stolen goods traced to Chieni Supermarket raid

Sakaja invites Senate to probe Sh15bn debt by defunct NMS

The courage of Kenya’s youth: A call for peace and justice

A Closer Examination of the US Disinformation Campaign Against China

Generation Z: A Force That Cannot Be Ignored in Kenya

Lessons on the Jealous Protection and Preservation of Cultural Heritage

Human-centric, Hybrid AI Opens Up New Possibilities
- Listen to Capital FM
- Dj Downloads

Capital Health
About The Author
CORRESPONDENT

NATIONAL NEWS
Charlene ruto to gen z: simple solutions carry consequences.

Civil Servants Union urges officials to join Gen Z protests during Saba Saba day

Top stories
Prepare for significant changes, ruto tells cabinet amid looming reshuffle.

Kindiki warns against more protests on Thursday, Sunday as death toll rises to 41

Senator Sifuna rejects SRC salary hike for MPs

Audit Office cannot audit itself: Ndii defends ‘indipendent’ Debt Audit

Mwangaza calls out Nyakang’o over foreign travel expenses error

Remorseful Ruto pursues Kenyans’ love in new image shift

County News
Wajir governor boosts health services by commissioning 200 new healthcare workers, more on capital news.

Raila, Kalonzo witness assent of IEBC Bill 2024 at KICC
The law which was signed by President William Ruto expands qualifications for commissioners to include candidates with a background in accounting and Information and...

President Ruto announces 6-day dialogue in proposal backed by Raila
NAIROBI, Kenya, Jul 9 – President William Ruto has announced a six-day multi-sectoral convention which will kick off on Monday. Speaking after holding consultations...

Govt to revive leather industry in prisons
NAIROBI, Kenya, July 9 – The government is set to revive the Prison’s leather Industry. This initiative in collaboration with the State Departments for...

President Ruto assents to NADCO-backed IEBC Bill 2024
The Act contains among others an expanded recruitment panel that includes the electoral agency's chairman and commissioners.

Bungoma Pator Pastor detained as police uncover human remains in car boot
NAIROBI, Kenya, Jul 9 – Police in Webuye East have arrested a self-proclaimed pastor after discovering body parts in the boot of his car...

Speaker Wetangula rejects MPs bid to repeal Finance Bill 2024
The Finance Bill 2024 sparked nationwide protests led by Gen Z, who deemed it ill-timed and punitive. As a result, President Ruto withdrew it...

High Court suspends Ruto’s taskforce on public debt audit
NAIROBI, Kenya July 8 – The High Court has suspended the Presidential Taskforce on the forensic audit of public debt pending the determination of...

Medical interns demand immediate posting as they occupy Afya House
NAIROBI, Kenya, July 8 – Hundreds of medical, dental, and pharmacy interns have taken a stand against the Ministry of Health (MoH) refusing to...
Privacy Overview

COMMENTS
Here are a few samples: Advised and assisted the family of 5 in planning healthy meals, purchasing, and preparing foods. Created, assigned, and scheduled various housekeeping duties for 3 children ages 4 to 12, according to their capabilities. Kept track of the grocery inventory, making sure items moved on a FIFO basis, saving the household ...
2. Write a resume summary. Below your contact information, write a one- to two-sentence resume summary that describes how your skills and experience make you a good fit for the position you want to apply for. This statement allows you to reveal your strongest assets and credentials right away. It is your chance to make a good impression on the ...
Key takeaways. Format your returning to workforce resume for clarity and coherence, ensuring it aligns with the role. Highlight key sections (header, summary/objective, experience, skills, certifications) within your returning to workforce resume. Quantify achievements and align them with skills and job requirements.
Education. List your degree and the school (s) you attended. Experience. List your work experience in reverse chronological order. If you're using a functional resume format, group your experience or accomplishments by type-i.e., technical experience, leadership experience, etc. Under each item, give specific, detail-rich examples of your ...
[email protected]. (555) 432-1000. Montgomery Street, San Francisco, CA 94105. Summary. Hardworking with company's for 2 year background making valuable contributions in settings. Detail-oriented professional delivering effective records maintenance and shipping coordination. Detail-oriented student adie with 4 years of experience and ...
Returns Specialist Resume. Headline : As a Returns Specialist, responsible for coordination of key details associated with: Core Returns, Special Returns, Warranty Returns Annual Returns as well as other special projects as assigned by the Inventory Manager, etc,. Skills : Microsoft Word, Customer Service Skills, Inventory Control.
Use this Returns Specialist resume example and guide to improve your career and write a powerful resume that will separate you from the competition. ... make sure to include relevant keywords throughout your resume. You can include them in the work experience, skills, summary, and education sections. ... Oracle, and Microsoft Dynamics. You ...
Check Out one of our best return specialist resume samples with education, skills and work history to help you curate your own perfect resume for return specialist or similar profession. LiveCareer-Resume. ... using daily production sheets or work tickets. Experience. Return Specialist, 07/2013 - 11/2014 Continental - Bolingbrook, IL,
Check Out one of our best returns specialist resume samples with education, skills and work history to help you curate your own perfect resume for returns specialist or similar profession. ... Unpacked packages and assessed return paperwork for proper placement procedures. Assisted with receiving product shipments, pricing items, and recording ...
Chronological Template. The chronological resume is the most commonly used format for traditional candidates. In this format, work experience is displayed from current or most recent role (s) to previous experience in reverse chronological order. This template is ideal for those with relatively linear experience and clear career progression.
So use a large (11-by-17-inch) piece of paper or even a white board. You'll have room to scratch out and add words as you go before you assign your final draft to a computer document. Approach your "returning to the workforce" resume as a project that you can finesse over at least several days. Let it "go cold" overnight, review it ...
Continue reading to find out what skills a returns specialist needs to be successful in the workplace. The eight most common skills for returns specialists in 2024 based on resume usage. Data Entry, 19.3%. Customer Service, 11.7%. RMA, 10.6%. Return Authorizations, 5.8%. RF, 4.4%. Inventory Control, 4.2%.
Claims Specialist Resume Examples & Samples. Ability to work independently and escalate for assistance as needed. Strong communication ability to work with various internal and external parties to resolve member issues. Ability to proactively identify payer and provider trends, and to communicate this to management.
Look to the Resume Checklist below to investigate how Customer Service, Microsoft Excel, and MS Office match up to employer job descriptions. Data Entry, Detail Oriented, and Communication Skills represent a very decent share of skills found on resumes for Returns Specialist with 27.98% of the total.
Return to Work Resume Objectives Examples 1. Dynamic and resourceful team player ready to re-enter the workforce, bringing rich real-life experiences and professional skills to provide immediate value to an innovative organization. 2. Returning to the workforce with a focus on leveraging my diverse skill set and proven track record to make a ...
THE TEMPLATE INCLUDES: An ATS (and human) friendly return-to-work resume template in Microsoft Word Format. Written prompts within the template to guide your content. A video template walkthrough. A trusted bullet point formula. The return-to-work resume template is designed with modern resume writing principles that get results.
The chronological resume format details your work experience starting with your most recent job. This format highlights dates of employment but makes gaps in employment history more obvious. Pros. Most common format. Employers are most familiar with this format. Highlights a consistent work history. Cons.
03/2015 to Current. Returns Specialist Isn - Buford, GA. Manage the physical and accounting system returns of DCL site return inventory. Work daily in Microsoft GP ERP system including fulfilling orders, inventory tracing, and inventory transactions. Process all incoming Bill Only trial purchase orders, including international regions.
It typically takes 1-2 years to become a returns specialist: Year 1: Gain necessary skills through on-the-job training, such as understanding return policies, handling customer inquiries, and processing returns. Year 2: Continue on-the-job training to further develop skills and accumulate work experience in handling returns, processing refunds ...
Reentering the workforce resume examples. When reentering the workforce, or returning to work after some time, your professional resume will need to be revisited to best prepare for finding a new job. Below are tips to consider: Forget a chronological timeline - Our resumes often follow the same format of listing job history listed from newest to oldest jobs.
Office Specialist II - Return Utah (Part Time) State of Utah. Utah County, UT. $15.10 - $21.73 an hour. Part-time + 1. Monday to Friday. Assists with public affairs program planning, highlighting agency program activities through electronic and print medium, select art work, layouts and…. Posted 1 day ago ·.
As a rule of thumb, lead each bullet point with a verb such "Grew", "Increased", or "Developed". Specialist resume format and sections. 1. 1. Add contact information to your specialist resume. Your nameshould be the biggest text on the page and be at or near the top of the document.
Workers Compensation Associate Claims Specialist. 05/2004 - 11/2010. San Francisco, CA. Coordinate a modified work opportunities and requests with the HR Wellness team. Maintain related communications with the TPA's hearing representative. Report to management on claim status, costs, causes provided by the Company's claim provider.
The National Women's Council has recommended better integration of specialist perinatal mental health services with general maternity, primary care and other mental health services.
The strike ended following the signing of a return-to-work agreement with the Council of Governors (CoG). KUCO Secretary General George Gibore directed all members to resume their duties immediately. "We are officially declaring that our strike has come to an end and our members shall resume duty in their respective places of work, starting ...