An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Am J Lifestyle Med
- v.12(6); Nov-Dec 2018

Lifestyle Medicine: The Health Promoting Power of Daily Habits and Practices
There is no longer any serious doubt that daily habits and actions profoundly affect both short-term and long-term health and quality of life. This concept is supported by literally thousands of research articles and incorporated in multiple evidence-based guidelines for the prevention and/or treatment of chronic metabolic diseases. The study of how habits and actions affect both prevention and treatment of diseases has coalesced around the concept of “lifestyle medicine.” The purpose of this review is to provide an up-to-date summary of many of the modalities fundamental to lifestyle medicine, including physical activity, proper nutrition, weight management, and cigarette smoking cessation. This review will also focus specifically on how these modalities are employed both in the prevention and treatment of chronic diseases including coronary heart disease, diabetes, obesity, and cancer. The review concludes with a Call to Action challenging the medical community to embrace the modalities of lifestyle medicine in the daily practice of medicine.
‘The strength of the scientific literature supporting the health impact of daily habits and actions is underscored by their incorporation into virtually every evidence-based clinical guideline . . .’
An overwhelming body of scientific and medical literature supports the concept that daily habits and actions exert an enormous impact on short-term and long-term health and quality of life. 1 This influence may be either positive or negative. Thousands of studies provide evidence that regular physical activity, maintenance of a healthy body weight, not smoking cigarettes, and following sound nutritional and other health promoting practices all profoundly influence health. The strength of the scientific literature supporting the health impact of daily habits and actions is underscored by their incorporation into virtually every evidence-based clinical guideline stressing the prevention and treatment of metabolically related diseases. 2 - 18 A sampling of the guidelines and consensus statements from various prestigious medical organizations is found in Table 1 . All of these statements emphasize lifestyle habits and practices as key components in the prevention and treatment of disease.
Sampling of Guidelines That Incorporate Lifestyle Recommendations for the Threat or Prevention of Chronic Disease.
Despite the widespread recognition of the important role of lifestyle measures and practices as a key component of the treatment of metabolic diseases, scant progress has been made in improving the habits and actions of the American population. For example, in the Strategic Plan for 2020 released by the American Heart Association, it was stated that only 5% of the adult population of the United States practice all of the positive lifestyle measures known to significantly reduce the risk of developing cardiovascular disease (CVD). 14
The power of positive lifestyle decisions and actions is underscored by multiple randomized controlled trials and a variety of cohort studies. For example, the Nurses’ Health Study demonstrated that 80% of all heart disease and over 91% of all diabetes in women could be eliminated if they would adopt a cluster of positive lifestyle practices including maintenance of a healthy body weight (body mass index [BMI] of 19-25 kg/m 2 ); regular physical activity (30 minutes or more on most days); not smoking cigarettes; and following a few, simple nutritional practices such as increasing whole grains and consuming more fruits and vegetables. 19 The US Health Professionals Study showed similar, dramatic reductions in risk of chronic disease in men from these same positive behaviors. 20 In fact, if individuals adopted only one of these positive behaviors, their risk of developing coronary artery disease (CAD) could be cut in half.
For decades physicians have emphasized the importance of practicing “evidence-based medicine.” Yet when it comes to incorporating the vast amount of evidence supporting positive health outcomes from lifestyle practices and habits, the medical community has been relatively slow to respond. This, despite the fact that virtually every physician would agree with the premise that regular physical activity, weight management, sound nutrition, and not smoking all result in significant health benefits.
The purpose of the current review is to provide a summary of the literature underscoring the benefits of positive health promoting habits and to present some strategies and guidelines for implementing these actions within the practice of medicine and issue a call for increased emphasis on lifestyle medicine among physicians.
What Is Lifestyle Medicine?
I had the privilege of editing the first, multi-author, academic textbook in lifestyle medicine. 21 In fact, this textbook, published in 1999, coined the term lifestyle medicine , which we defined as “the discipline of studying how daily habits and practices impact both on the prevention and treatment of disease, often in conjunction with pharmaceutical or surgical therapy, to provide an important adjunct to overall health.”
While there have been a number of different constructs concerning these disciplines and many investigators have made important contributions to components of lifestyle medicine such as nutrition, physical activity, weight management, smoking cessation, and so on, it is clear that the field is now going to coalesce around the term lifestyle medicine . For example, the American Heart Association changed the name of one its Councils from the “Council on Nutrition, Physical Activity and Metabolism” to the “Council on Lifestyle and Cardiometabolic Health” in 2013. 22 In addition, both the American College of Preventive Medicine and the American Academy of Family Practice have established working groups and educational tracks in the area of lifestyle medicine. Circulation , a major academic journal from the American Heart Association, published a series of multiple articles titled “Recent Advances in Preventive Cardiology and Lifestyle Medicine.” Representatives from a variety of organizations including the American Academy of Pediatrics, the American College of Sports Medicine, the Academy of Nutrition and Dietetics, the American Academy of Family Practice, and the American College of Preventive Medicine sent representatives to a working group that established the first summary of competencies physicians should possess to practice lifestyle medicine, which was published in the Journal of the American Medical Association . 23
Importantly, a new health care organization has been formed called the “American College of Lifestyle Medicine” (ACLM), which is devoted to providing a professional home for individuals who wish to emphasize lifestyle medicine in their practices. 24 This organization has doubled its membership each year for the past 5 years. ACLM has also spawned initiatives to develop curricula and encourage education of medical students in the area of lifestyle medicine. ACLM has also supported the development of Lifestyle Medicine Student Interest Groups at medical schools and has developed criteria for lifestyle medicine certification. 25 The goal of this organization is ultimately to establish certification boards in lifestyle medicine. Lifestyle medicine has also become an international movement with the development of the Lifestyle Medicine Global Alliance. 26
In addition, a peer-reviewed academic journal has been established, the American Journal of Lifestyle Medicine , 27 to provide a forum for individuals interested in exchanging academic information in this growing field.
There are multiple reasons why the term lifestyle medicine seems particularly appropriate for this discipline. First, the field is focused on lifestyle and its relationship to health. Second, it is clearly medicine based on the wide range and large volume of evidence supporting the health benefits of daily habits and actions.
The Power of Lifestyle Habits and Practices to Promote Good Health
Multiple daily practices have a profound impact on both long-term and short-term health and quality of life. This review will focus on 5 key aspects of lifestyle habits and practices: regular physical activity, proper nutrition, weight management, avoiding tobacco products, and stress reduction/mental health. This initial section will focus on general considerations related to each of these lifestyle habits and practices. In the subsequent section, this information will be applied to specific diseases or conditions.
Physical Activity
Physical activity is a vitally important component to overall health and both prevention and treatment of various diseases. Regular physical activity has been specifically demonstrated to reduce risk of CVD, type 2 diabetes, the metabolic syndrome, obesity, and certain types of cancer. 18 The important role of physical activity in these conditions has been underscored by its prominent role in evidence-based guidelines and consensus statements from virtually every organization that deals with chronic disease. In addition, there is strong evidence that regular physical activity is important for brain health and cognition as well as reduction in anxiety and depression and amelioration of stress. 16
The recently released 2018 Physical Activity Guidelines Advisory Committee Scientific Report emphasizes that increased physical activity carries multiple individual and public health benefits. 18 This report also catalogs that physical activity contributes powerfully to improved quality of life by improving sleep, general feelings of well-being, and daily functioning. The report emphasizes that some of the benefits of physical activity occur immediately and most of the benefits become even more significant with ongoing and regular performance of moderate to vigorous physical activity.
In addition, physical activity has been shown to prevent or minimize excessive weight gain in adults as well as reducing the risk of both excess body weight and adiposity in children. 28 Physical activity decreases the likelihood that women will gain excessive weight during pregnancy, making them less likely to develop gestational diabetes. 29 Physical activity may also decrease the likelihood of postpartum depression.
Physical activity has also been demonstrated to lower the risk of dementia and improve other aspects of cognitive functioning. Importantly, as the population in the United States continues to grow older regular physical activity has been shown to decrease the likelihood of falls 30 and fall-related injuries and assist in the preservation of lean body mass. 31
Other conditions that regular physical activity improves are osteoarthritis and hypertension. 18 All in all, the multiple benefits of regular physical activity make it one of the key considerations that should be recommended to all children and adults as part of a comprehensive lifestyle medicine approach to health and well-being.
Numerous studies have shown that physicians’ own physical activity behavior predicts the likelihood that they will recommend physical activity to their patients. Unfortunately, it has been estimated that less than 40% of physicians regularly counsel their patients on the importance of increasing physical activity. The low level of prescription among physicians, as well as the recognized benefits of regular physical activity in health, stimulated the American College of Sports Medicine to launch the “Exercise is Medicine®” (EIM) initiative. This initiative is designed to encourage primary care providers and health providers to design treatment plans that include physical activity or to refer patients to evidence-based exercise programs with qualified exercise professionals. EIM also encourages health care providers to assess and record physical activity as a vital sign during patients’ visits. The initiative further recommends concluding each visit with an exercise “prescription.” 32
Nutrition plays a key role in lifestyle habits and practices that affect virtually every chronic disease. There is strong evidence for a role of nutrition in CVD, diabetes, obesity, and cancer, among many other conditions. 33 Dietary guidelines and consensus statements from a variety of organizations have recognized the key role for nutrition, both in the prevention and treatment of chronic disease. 4 , 6 , 8 These consensus statements are very similar to each other in nature and consistently recommend a dietary pattern higher in fruits and vegetables, whole grains (particularly, high fiber), nonfat dairy, seafood, legumes and nuts. 34 Guidelines further recommend that those who consume alcohol (among adults), do so in moderation. The guidelines are also consistent in recommending diets that are lower in red and processed meats, refined grains, sugar sweetened foods, and saturated and trans fats. All the guidelines also emphasize the importance of balancing calories and also regular physical activity as strategies for maintaining a healthy weight and, thereby, further reducing the risk of chronic diseases.
Dietary guidance over the past 2 decades has moved from specific foods and nutrients to a greater emphasis on dietary patterns. The emphasis has also shifted to the critical aspect of providing practical advice for implementing recommendations. 9 This latter emphasis recognizes that despite consistent guidelines and nutrition recommendations for many decades, a distinct minority of Americans are following these guidelines. For example, in the area of hypertension <20% of individuals with high blood pressure follow the DASH Diet. 35 It is also estimated that <30% of adults in the United States consume the recommended daily number of fruits and vegetables. 34
The 2015-2020 Dietary Guidelines for Americans focused on integrating available science and systematic reviews, scientific research, and food pattern modeling on current intake of the US population to develop the “Healthy U.S. Style Eating Pattern.” 8 This approach allowed blending recommendations for an overall diet including constituent foods, beverages, nutrients, and health outcomes, while allowing for flexibility in amounts of food from all food groups to establish healthy eating patterns that meet nutrient needs and accommodated limitations for saturated fats, added sugars, and sodium. This approach also allowed for the potential nutritional areas of public health concern. Utilizing this approach to Dietary Guidelines for Americans 2015-2020 indicated the following:
Within the body of evidence higher intakes of vegetables and fruits consistently have been identified as characteristic of healthy eating patterns: whole grains have been identified as well, although slightly less consistently. Other characteristics of healthy eating patterns have been identified with less consistency including fat free or low fat dairy, seafood, legumes and nuts. Lower intakes of meats including processed meats, poultry, sugar sweetened foods (particularly beverages), and refined grains have also been identified as characteristics of healthy eating patterns.
Despite the multiple known benefits of proper nutrition, most physicians feel they have inadequate education in this area. In one survey, 22% of polled physicians received no nutrition education in medical school, and 35% polled said that nutrition education came in a single lecture or a section of a single lecture. 36 The situation does not improve during medical residency. More than 70% of residents surveyed felt they received minimal or no education on nutrition during medical residency. In the United States, 67% of physicians indicate they have nutritional counseling sessions for patients. However, this education was largely focused on the ill effects of high sodium, sugars, and fried foods. It is noteworthy that only 21% of patients feel they received effective communication in the area of nutrition from their physician. 36
Issues related to healthy nutrition permeate virtually every condition where lifestyle medicine plays a role and will be treated in detail under each specific condition.
Weight Management
In many ways overweight and obesity represent quintessential lifestyle diseases. These conditions serve as significant public health problems in the United States and other countries throughout the world. 37 In the United States, the prevalence of overweight (BMI ≥ 19-25 kg/m 2 ) has been estimated at approximately 70%, while obesity (BMI ≥ 30 kg/m 2 ) is estimated at 36%, and severe obesity (BMI ≥ 35 kg/m 2 ) at 16%. 38 These rates are significant since even small amounts of excess body weight have been associated with many chronic diseases including CVD, diabetes, some forms of cancer, 39 muscular skeletal disorders, arthritis, 40 and many others. The cornerstone of obesity treatment relies on lifestyle measures that contribute to balancing energy to prevent weight gain or creating an energy deficit to achieve weight loss. These lifestyle factors including both physical activity and nutrition are cornerstone modalities to achieve these results.
Tobacco Products
Overwhelming evidence exists from multiple sources that cigarette smoking significantly increases the risk of multiple chronic diseases including heart disease and stroke, diabetes, and cancer. Early in the 20th century in the United States, cigarette smoking was more prevalent in men than women. 41 However, women have rapidly caught up with men. The health risks of smoking in women are the equivalent of men. Substantial benefits in the reduction of risk of both CVD and cancer accrue in individuals who stop smoking cigarettes. These benefits occur over a very brief period of time. 42
After years of significant decreases in cigarette smoking, the prevalence of cigarette smoking has appeared to level off in recent years with approximately 15% of individuals currently smoking cigarettes. 43
It should be noted that secondhand smoke also increases the risk of multiple chronic diseases, since secondhand smoke contains numerous carcinogens and may linger, particularly in indoor air environments, for a number of hours after cigarettes have been smoked. 44
Stress, Anxiety, and Depression
Stress is endemic in the modern, fast-paced world. It has been estimated that up to one third of the adult population in the United States experiences enough stress in their daily lives to have an adverse impact on their home or work performance. Anxiety and depression are also very common. Lifestyle measures, such a regular physical activity, have been demonstrated to provide effective amelioration of many aspects of all three of these conditions. 45 , 46
Interestingly, in the past decade positive psychology has also emerged as a significant component of lifestyle medicine. 47 This field has demonstrated that positive approaches to psychological issues such as gratitude, forgiveness, and other strategies can play a very important role in stress reduction and amelioration of both anxiety and depression.
Obtaining adequate amounts of sleep has also been demonstrated to be an effective strategy in all these conditions, which proved so troublesome to many individuals. 48
Lifestyle Medicine Approaches in the Treatment and Prevention of Chronic Diseases
Lifestyle medicine modalities have been demonstrated in multiple studies to play an important role in both the treatment and prevention of many chronic diseases and conditions. This section will explore some of the most common diseases or conditions where lifestyle modalities have been studied.
Cardiovascular Disease
Daily lifestyle practices and habits profoundly affect the likelihood of developing CVD. Many of these same practices and habits also play a role in treating CVD. 1 - 4 , 9 , 14 - 16
Numerous studies have demonstrated that regular physical activity, not smoking cigarettes, weight management, and positive nutritional practices all profoundly affect both CVD itself and also risk factors for CVD. 49 , 50 Numerous epidemiologic studies have shown that positive lifestyle decisions such as engaging in at least 30 minutes of physical activity on most days; not smoking cigarettes; consuming a diet of more fish, whole grains, fruits, and vegetables; and maintaining a healthy body weight can reduce the incidence of CHD by over 80% and diabetes by over 90% in both men and women. 19 , 20
Between 1980 and 2000, mortality rates from CHD fell by over 40%. 51 CVD, nonetheless, remains the leading cause of worldwide mortality, and in the United States, it results in over 37% of annual mortality. 51 Approximately half of the reduction in CVD deaths since 1980 can be attributed to reduction in major lifestyle risk factors such as increasing physical activity, smoking cessation, and better control of blood pressure and cholesterol. Unfortunately, increases in obesity and diabetes have moved in the opposite direction and could jeopardize the gains achieved in other lifestyle risk factors, unless these negative trends can be reversed. 51
In the past decade a number of important initiatives have been undertaken and comprehensive summaries published linking overall life strategies to reductions in cardiovascular risks. In 2012, the American Heart Association (AHA) released its National Goals for Cardiovascular Health Promotion and Disease Reductions for 2020 and beyond. 14 This important document also introduced the concept of “primordial prevention” (preventing risk factors from occurring in the first place) into the cardiology lexicon as well as introducing the concept of “ideal cardiovascular health.” Daily lifestyle measures were central to both these new concepts. In 2013, the American Heart Association and American College of Cardiology (ACC) jointly issued Guidelines for Lifestyle Management to Reduce Cardiovascular Risk, 52 which also emphasized lifestyle measures to reduce the risk of CVD or assist in its treatment if already present.
Unfortunately, a distinct minority of Americans are following the recommendations from the AHA to achieve “ideal” cardiovascular health. Ideal cardiovascular health was defined as achieving appropriate levels of physical activity, consuming a healthy diet score, maintaining a total blood cholesterol of <200 mg/dL, maintaining a blood pressure of <120/<80 mm Hg, and a fasting blood glucose of <100 mg/dL (the cholesterol, blood pressure, and glucose parameters were all defined as “untreated” values). In the AHA document, it was noted that less than 5% of adults in the United States fulfill all 7 criteria for achieving ideal cardiovascular health. 14
Metrics for Cardiovascular Health
Overweight and obesity represent significant risk factors for cardiovascular disease. Guidelines developed by a joint effort from The Obesity Society (TOS), AHA, and ACC 53 were designed to help physicians manage obesity more effectively. Key recommendations include enrolling overweight or obese patients in comprehensive lifestyle interventions for weight loss delivery and programs for 6 months or longer.
Increased levels of moderate or vigorous intensity physical activity have been repeatedly shown to lower the risk for cardiovascular disease. Compared with those who are physically active, the risk of coronary heart disease (CHD) in sedentary individuals is 150% to 240% higher. 54 Unfortunately, only about 25% of Americans engage in enough regular physical activity to meet minimum standards of the Centers for Disease Control and Prevention of at least 150 minutes/week of moderate intensity aerobic exercise or at least 75 minutes of vigorous exercise and muscle strengthening activities at least 2 days/week. 18
The greatest reduction in risk for CHD appears to result from those engaging in even modest amounts of physical activity compared with the most physically inactive. Even relatively small amounts of increase in physical activity could potentially result in a significant decrease in CHD for a large portion of the American population. Both the 2008 Physical Activity Guidelines for Americans and the 2018 55 Physical Activity Guidelines Advisory Committee Scientific Report 18 recommend similar levels of physical activity as an important component of the reduction of risk for CHD.
There is no question that diet plays a significant role in overall strategies for cardiovascular risk reduction. 56 , 57 This fact is recognized by numerous scientific statements and documents from the American Heart Association including the AHA 2020 Strategic Plan 14 as well as the AHA/ACC Guidelines for Lifestyle Management 52 and the 2006 AHA Nutrition Guidelines. 56 All these recommendations are similar and include consumption of increased fruits and vegetables, consuming at least 2 fish meals/week (preferably oily fish), consuming fiber-rich grains, and restricting sodium to <1500 mg/day and sugar sweetened beverages ≤450 kcal (36 ounces) per week. The AHA Dietary Guidelines recommend plant-based diets such as the DASH Diet 35 (Dietary Approach to Stop Hypertension), as well as the Mediterranean-style diets. 58 Definitive evidence-based guidelines for overall dietary health are summarized in the Dietary Guidelines for Americans 2015-2020 Report. 8
Smoking and Use of Tobacco Products
Overwhelming evidence from multiple sources demonstrates that cigarette smoking significantly increases the risk of both heart disease and stroke. This evidence has been ably summarized elsewhere 59 and is incorporated as a recommendation for every AHA document including the 2020 Strategic Plan. The good news is that risk of CHD and stroke diminish rapidly once smoking cessation occurs. It should also be noted that secondhand smoke also increases the risk of CHD. It has been estimated that 1 nonsmoker dies from secondhand smoke exposure to every 8 smokers who die from smoking. 60
Hypertension
Hypertension represents a significant risk factor for CHD and is the leading risk factor for stroke. The recently released 2017 Guidelines for the Prevention and Detection, Evaluation and Management for High Blood Pressure in Adults from the AHA and the ACC defines normal blood pressure as <120 mm Hg/<80 mm Hg, and hypertension as systolic >120 mm Hg and diastolic high blood pressure as >80 mm Hg. 3 The new criteria are found on Table 2 . Using these criteria, more than 40% of the adult population in the United States has high blood pressure. Recommendations for treating high blood pressure, particularly in the lowest categories, involve a number of lifestyle medicine modalities such as increased physical activity, weight loss (if necessary), and improved nutrition including a salt reduction to <1500 mg/day. 3
2017 Blood Pressure Guidelines From the American Heart Association and American College of Cardiology.
Dyslipidemias
In 2013, the ACC and AHA issued “Guidelines for the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Disease in Adults.” 6 These guidelines recommend an increased use of statin medications to reduce atherosclerotic cardiovascular disease (ASCVD) both in primary and secondary prevention and recommended the discontinuation of the use of specific low-density lipoprotein and high-density lipoprotein treatment targets. Within these guidelines for treating blood lipids, it was acknowledged that lifestyle is the foundation of ASCVD risk reduction efforts. This includes adhering to a heart healthy diet, regular exercise, avoidance of tobacco, and maintenance of a healthy body weight.
Diabetes and Pre-Diabetes
Dramatic increases in diabetes have occurred around the world in the past 2 decades. Lifestyle medicine modalities to prevent or treat diabetes focus on nutrition therapy, physical activity, education, counseling, and support given the great importance given to the metabolic basis of the vast majority of individuals who have either pre-diabetes or diabetes. 61 The International Diabetes Federation estimates that 387 million adults in the world live with type 1 or type 2 diabetes. Tragically, almost half of these individuals do not know they have these diseases. It is estimated that the number of individuals living with diabetes will increase to 392 million people by 2035.
In the United States in 2011-2012, the estimated prevalence of diabetes was 12% to 14%. 62 There is a higher prevalence in adults who are non-Hispanic-Black, non-Hispanic-Asian, or Hispanic. The proportion of people who have undiagnosed diabetes has decreased between 3.1% and 5.2% during this period of time. The prevalence of pre-diabetes has been reported to be between 37% and 38% of the overall US population. Consequently, 49% to 52% of the US population has either diabetes or pre-diabetes. 63
Pre-Diabetes
Multiple lifestyle interventions play critically important roles in preventing pre-diabetes from turning into diabetes. The strongest evidence comes from the Diabetes Prevention Program (DPP), which demonstrated that an intensive lifestyle intervention in individuals with pre-diabetes could reduce the incidence of type 2 diabetes by 58% over 3 years. 64 Other studies that have supported the importance of lifestyle intervention for diabetes prevention include the Da Qing Study, where 43% reduction in conversion from pre-diabetes to diabetes occurred at 20 years, 65 and the Finnish Diabetes Prevention Study, which showed also a 43% reduction in conversion of pre-diabetes to diabetes at 7 years and a 34% reduction at 10 years. 66
The 2 major goals of the DPP in the lifestyle intervention arm were to achieve a minimum of 7% weight loss and 150 minutes of physical activity/week at a moderate intensity such as brisk walking. These goals were selected based on previous literature suggesting that these were both feasible and could influence the development of diabetes. Both these goals were largely met in the DPP.
The nutrition plan in DPP focused on reducing calorie intake in order to achieve weight loss if needed. The recommended diet was consistent with both Mediterranean and DASH eating patterns. Conversely, sugar sweetened beverages and red meats were minimized since they are associated with the increased risk of type 2 diabetes. 63 The 150 minutes/week of moderate intensity physical activity was achieved largely through brisk walking, which also contributed to beneficial effects in individuals with pre-diabetes.
Education and support in the DPP was provided with an individual model of treatment rather than a group-based approach including a 16-session core curriculum completed in the first 24 weeks including sections on lowering calories, increasing physical activity, self-monitoring, maintaining healthy lifestyle behaviors, and psychological, social, and motivational challenges. 63
Recent evidence has also suggested that breaking up sedentary time (such as screen time) further decreases the risk of pre-diabetes being converted to diabetes.
Lifestyle modalities are a cornerstone for diabetes care. These modalities include medical nutrition therapy (MNT), physical activity, smoking cessation, counseling, psychosocial care, and diabetes self-management education support. 66
There are many different ways of achieving the nutritional goals. Individuals with diabetes should be referred for individualized MNT. MNT promotes healthful eating patterns emphasizing a variety of nutrient-dense foods at appropriate levels with the goal of achieving and maintaining healthy body weight; maintaining individual glycemic, blood pressure, and lipid goals; and delaying or preventing complications of diabetes. There is not one ideal percentage of calories from carbohydrate, protein, and fat for all people with diabetes. A variety of eating patterns are acceptable for the management of diabetes including the Mediterranean, DASH, and other plant-based diets. All of these have been shown to achieve benefits for people with diabetes. 67
Weight management, if necessary, and reduction of weight are important particularly for overweight and obese people with diabetes. Weight loss can be attained in lifestyle programs that achieve 500 to 750 kcal daily reduction for both men and women adjusted to the individual based on body weight. For many obese individuals with type 2 diabetes, weight loss >5% is necessary in order to achieve beneficial outcomes for glycemic control, lipids, and blood pressure, while sustained weight loss of >7% is optimal.
Regular physical activity is also vitally important for the management of diabetes. People with diabetes should be encouraged to perform both aerobic and resistance exercise regularly. 68 Aerobic activity bouts should ideally be at least 10 minutes, with a goal of 30 minutes/day or more on most days of the week. Recent evidence supports the concept that individuals with diabetes should be encouraged to reduce time spent being sedentary in activities such as working at a computer, watching TV, and so on, or breaking up sedentary activities by briefly standing, walking, or performing light physical activity. Research trials have demonstrated strong evidence for A1C lowering value of exercise in individuals with type 2 diabetes. The ADA Consensus Report indicates that prior to starting an exercise program medical providers should perform a careful history to assess cardiovascular risk factors and be aware of atypical presentation of CAD in patients with diabetes. Health care providers should customize exercise regiments to individuals’ needs. 67
In many ways obesity represents the quintessential lifestyle disease. 34 Obesity is the result of energy imbalance, since energy expenditure and energy intake are key factors in the energy balance equation. 61 Thus, both nutritional and physical activity components of lifestyle intervention are critically important to both short-term weight loss and also long-term maintenance of healthy body weight.
It is currently estimated that 78 million individuals in the United States are obese. This represents 36% of the population. 37 More than 70% of individuals in the United States are overweight (BMI ≥ 25 kg/m 2 ), including obese (BMI ≥ 30 kg/m 2 ) and severely obese (BMI ≥ 35 kg/m 2 ). While it may seem simple that either decreased caloric intake or increased physical activity may contribute to weight loss, in fact the process is complicated. As emphasized in the Consensus Statement on Obesity from the American Society of Nutrition, metabolism consists of multiple factors including percent body fat, other issues related to metabolism, and a host of environmental factors. 69
At any time, approximately 50% to 70% of obese Americans are actively trying to lose weight. Sustained weight loss of as little as 5% to 10% is considered clinically significant, since it reduces risk factors for a variety of chronic diseases such as diabetes and heart disease. Both the Diabetes Prevention Program and the Look AHEAD Trial 70 showed that weight loss of 7% in obese individuals resulted in significant improvement in risk factors for both heart disease and diabetes. Nutrition represents a cornerstone of treatment for overweight and obesity. 71 Dietary treatments for disease have been called MNT. This therapeutic approach has been used in a variety of medical conditions, but there is particularly strong proof that MNT improves waist circumference, waist-to-hip ratio, fasting blood sugar, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, and blood pressure.
Typical nutritional interventions for weight loss in obese individuals involve sustaining an average daily caloric deficit of 500 kcal. Energy recommendations also include that intake should not be <1200 calories/day for male or female adults in order to maintain adequate nutrient intake.
A variety of evidence-based diets have been demonstrated to assist in healthy weight loss. These include the Mediterranean diet, the DASH diet, and the Healthy U.S. Eating Style Pattern. It has also been demonstrated that macronutrient composition of a weight loss plan (eg, low fat vs low carb, etc) do not achieve different results in studies lasting longer than one year.
The Weight Loss Guidelines jointly issued by the US Preventive Services Task Force, the American Heart Association, the American College of Cardiology, the Obesity Society, and the Academy of Nutrition and Dietetics all recommend a multidisciplinary team approach to managing obesity. 53 These approaches include physical activity counseling, MNT, as well as a structured approach to behavioral change utilizing problem solving and goal setting as well as self-monitoring. Most evidence suggests that effective weight loss programs should last at least 6 months and have a minimum of 24 counseling sessions.
There is a prevalent misconception that maintenance of weight loss is virtually impossible. In both the Diabetes Prevention Program and the Look AHEAD Trial, however, individuals who completed the initial 16-week program and then were followed on a monthly basis for the next 3 to 4 years were able to maintain 90% of the weight that they initially lost. The National Weight Control Registry, which is a registry of over 10 000 individuals who have lost at least 50 pounds and kept it off for at least 1 year, also demonstrated that key components of lifestyle measures such as regular attention to monitoring nutritional intake as well as regular physical activity (on average 60 minutes/day) were key components of how these individuals were able to maintain initial weight loss. 72
It has been argued that physical activity alone is not a powerful tool for initial weight loss. However, abundant evidence supports the concept that regular physical activity is a key component of long-term maintenance of weight loss. Regular physical activity also plays an important role in preservation of lean body mass, which is a key component of maintaining adequate metabolism to support maintenance of weight loss. 28 As already indicated, regular physical activity also conveys a host of health enhancing benefits in addition to its role in weight loss and weight management.
Lifestyle measures play a critically important role both in the prevention of cancer and treatment of individuals who have already established cancer. Moreover, lifestyle measures play a very important role in the ongoing health of cancer survivors. These facts are underscored by the joint statement issued by the American Cancer Society, the American Diabetes Association, and the American Heart Association on preventing cancer, CVD, and diabetes. 15
Cancer is a generic term that represents more than 100 diseases, each of which has a different etiology. Nonetheless, lifestyle measures can play a critically important role in virtually every form of cancer. In 2016, an estimated 1 685 210 new cases of cancer were diagnosed in the United States and 595 690 people died from the disease. 73 Worldwide it has been estimated that the number of new cancers could rise by as much as 70% over the next 2 decades. Approximately 70% of deaths from cancer will occur in low- and middle-income countries. 74
Cancer is no longer viewed as an inevitable consequence of aging. In fact, only 5% to 10% of cancers can be classified as familial. Thus, most cancers are associated with multiple environmental factors including lifestyle issues. For example, the importance of nutrition was emphasized more than 35 years ago by Dahl and Petro. They estimated that approximately 35% (10% to 70%) of all cancers in the United States could be attributable to dietary factors. 75 In 2007, the World Cancer Research Fund and American Institute for Cancer Research (WCRF/AICR) evaluated 7000 studies and concluded that diet and physical activity were major determents of cancer risk. 76 Thus, on a global scale, 3 to 4 million cancer cases could be prevented each year from more positive lifestyle habits and actions. 76
The relationship of obesity to cancer is also very strong. 77 This relationship is based not only on hormonal changes associated with obesity but also a variety of other physiologic mechanisms. Adipocytes, which compose the predominant cell in body fat, have been historically thought to be simply passive storage vessels. It is now clear, however, that adipocytes secrete a variety of metabolically active substances that promote inflammation, insulin resistance, and a variety of other factors, all of which may promote cancer cell growth. The AICR and IARC (International Agency for Research on Cancer) have concluded that there is sufficient evidence to link 13 human malignancies to excess body fatness. 78 Excess body fatness is now the second leading preventable cause of cancer, behind only cigarette smoking. 79 The AICR also reported in 2017, that, unfortunately, only 50% of Americans are aware that obesity promotes cancer growth, so there is an important educational issue to combat, as well. 80
Individuals who are overweight or obese should follow standard cancer screening guidelines. Intentional weight loss lowers cancer risk and improves survival. Individuals with cancer should avoid excess weight gain or, if already overweight or obese, should attempt to lose weight to improve prognosis. The typical program for safe and effective weight loss involves both regular physical activity and caloric restriction. These programs may need to be modified given the unique aspects of each cancer.
General nutrition guidelines for cancer prevention and treatment are very similar to those for healthy eating, in general. However, some modifications may be necessary to protect against certain cancers or treat various side effects of cancer therapy, such as excessive weight loss. In general, lifestyle nutrition measures for cancer prevention involve increasing the consumption of foods that have been shown to decrease the cancer risk, which include whole grains, vegetables, fruits, and legumes. In addition, individuals should decrease consumption of foods associated with increased cancer risk such as processed meat (including ham and bacon), red meat such as beef, pork and lamb, and decrease alcoholic beverages and salt preserved foods. Individuals should eat a healthy diet rather than relying on supplements to protect against cancer.
Physical activity also plays a key role in the association of lifestyle risk to cancer. 81 , 82 Although specific biologic mechanisms linking physical activity to cancer reduction remain unknown, there is growing evidence supporting the role of physical inactivity in various cancer diagnoses. According to the World Cancer Research Fund International, 20% of cancer cases in the United States could be prevented through physical activity, weight control, and consumption of a healthy diet. 83 In addition, a pooled analysis of 12 prospective cohort studies involving 1.4 million participants in the United States and Europe demonstrated an association between higher levels of leisure time physical activity and risk reduction of 13 different cancer types. 84
Among those cancers linked to inactivity, colon, breast, and endometrial cancers are the most studied. 85 The link between physical activity and breast cancer may be through reducing levels of sex hormones and increasing concentrations of sex hormone binding globulin proteins. 86 The relationship between exercise and decreased endometrial cancer risks may have similar mechanisms. 87 The relationship between physical activity and decreased colon cancer risk may be due to immune function modulation reduction in intestinal transit time, hyperinsulinemia, and inflammation. 88 Despite these postulated underlying factors, the biological link between physical activity and reduced colon cancer risk is not well understood.
There are multiple physical activity guidelines that not only have been demonstrated to reduce the risk of cancer, but may also be employed as a treatment tool for cancer populations. Safety is the key consideration in physical activity for cancer survivors. Guidelines for physical activity and cancer have been issued both by the American Cancer Society 89 and the AICR. 90 While a detailed explanation of these guidelines is beyond the scope of this review, the interested reader is referred to these guidelines for more specific detail.
Dementia/Cognition
Maintaining cognitive function is vital to maintaining quality of life, functional independence, and is an important component of the aging process. As life expectancy continues to increase in developed countries, the number of individuals over the age of 65 will undoubtedly increase dramatically over the next 15 to 20 years. 16 It has been estimated that there are currently 47 million people with dementia worldwide and this is projected to increase to 75 million individuals in 2030 and 131 million individuals by 2050. 16
There is a strong linkage between brain health and cardiovascular health. This central fact is underscored by the Presidential Advisory from the AHA and American Stroke Association (ASA) on “Defining Optimal Brain Health in Adults.” 16
Lifestyle measures play a central role in the recommendations from the AHA/ASA for maintaining healthy cognition throughout a lifetime. Modifiable risk factors that may compromise brain health are also associated with poor cardiovascular health such as uncontrolled hypertension, diabetes mellitus, obesity, physical inactivity, smoking, and depression. Each of these conditions has been shown to be potentially ameliorated, at least to some degree, by positive lifestyle measures. For this reason, the AHA and ASA have identified 7 metrics to define optimal brain health including nonsmoking, physical activity at goal levels, a healthy diet consistent with current guideline levels, and a body mass index of <25 kg/m 2 . 16 In addition, the AHA and ASA recommend 3 ideal health factors including an untreated blood pressure of <120/<80 mm Hg, untreated cholesterol <200 mg/dL, and fasting blood glucose of <100 mg/dL.
Virtually all of these factors are affected by positive lifestyle decisions, making cognition and reducing the risk of dementia strongly linked to lifestyle factors. Furthermore, it is important to stress that while many of the manifestations of the spectrum ranging from diminished cognition to dementia occur in individuals in their 50s, 60s, and beyond, paying attention to these risk factors should occur throughout a lifetime, thus enhancing the importance of lifestyle measures in maintaining positive brain health.
A variety of dietary habits have also been shown to decrease the risk of cognitive decline and risk of dementia. These include Mediterranean style diets (MST) and the Dietary Approach to Stop Hypertension (DASH) diet. 91 A combination of MST and DASH (the so-called MIND diet) has also been observed to be associated with decreased risk of dementia with aging. All of these diets are plant based as their principle sources of energy and involve a high intake of grains and cereals, fruits, vegetables, legumes, nuts, olive oil, and fish as fat sources. In addition, a recent study demonstrated that consumption of cocoa, both in individuals over the age of 60 with maintained cognition and also mild cognitive impairment, may improve levels of cognition. 92 , 93 A number of studies have shown that regular physical activity is associated with improved cognition. 16
Anxiety, Depression, and Stress Reduction
Anxiety, depression, and stress are all endemic in the modern, fast-paced world. Lifestyle interventions have been demonstrated to play an effective role in ameliorating all three of these conditions.
Within all of the mental health disorders, anxiety is the most common. 94 The overall prevalence of anxiety disorders has been reported at more than 30%. Regular physical activity has been demonstrated in multiple studies to lower anxiety levels. While the state of anxiety has been shown to be reduced immediately after performing a single bout of exercise, the anxiolytic effect of treating the trait of anxiety appears to require a training period of at least 10 weeks. The exact level of physical activity has not been determined. However, most studies employ the general guidelines of 30 minutes of moderate intensity physical activity/session.
Depression is also quite common with a lifetime prevalence of significant depression of approximately 10% in the US population. 95 Even in the absence of significant depressive disorder, symptoms of depression can negatively influence health and quality of life. Physical activity has been repeatedly shown to decrease symptoms of depression. Typical levels of physical activity employed once again have involved at least 30 minutes of moderate intensity physical activity performed on a regular basis.
Stress is endemic in our modern world. 96 While exact prevalence figures for stress are difficult or impossible to determine, most people experience at least moderate stress in their daily lives. It has been estimated that up to one third of individuals experience enough stress in their daily life to decrease their performance at either work or home. While a certain level of stress may be protective, excessive stress may be harmful through a variety of physiologic and psychological effects.
A variety of approaches to ameliorate stress have been studied and found effective. These include the relaxation response and other mind-body therapies. Certainly, these mind-body therapies play an important role in the delivery of lifestyle medicine. One other aspect of modern psychological therapy that has gained increased prominence in the past decade is positive psychology involving modalities and concepts such as gratitude and forgiveness, which may help reduce stress.
Lifestyle Medicine and Pediatrics
A detailed discussion of lifestyle medicine in the pediatric population is beyond the scope of this review. However, it should be noted that many of the conditions that manifest themselves in adulthood have their roots in childhood. In particular, there has been a dramatic increase in the prevalence of overweight and obesity in children 97 and a corresponding increase in the prevalence of type 2 diabetes. Dyslipidemia 98 and hypertension 99 have also increased in prevalence in the pediatric population.
There is emerging evidence that many of the conditions now increasing in prevalence in children may actually begin in utero. 100 The same types of lifestyle measures that are applicable both for the prevention and treatment of chronic disease in adults are also very relevant to children. Good information on physical activity in children can be found in the recently revised Physical Activity Guidelines for Americans. 18 Nutritional guidance may also be found in the 2015-2020 Dietary Guidelines for Americans. 8 Since many of the lifestyle medicine modalities employed in adults are highly relevant to families, issues related to physical activity, nutrition, and weight management should be addressed in the family setting.
Conclusions
There is no longer any serious doubt that daily habits and practices profoundly affect the short-term and long-term health and quality of life. Increased physical activity, proper nutrition, weight management, avoidance of tobacco, and stress reduction are all key modalities that can lower the risk of chronic disease and improve quality of life. Despite the overwhelming evidence that these practices have a profound impact on health, the medical community has been slow to respond in addressing these modalities and in encouraging patients to make positive lifestyle changes. This represents a significant missed opportunity since more 75% of Americans see a primary care doctor every year. Employing the principles of lifestyle medicine in the daily practice of medicine represents a substantial opportunity to increase the value of proposition in medicine by improving outcomes for patients, while controlling costs. 101 The time has come to employ the vast body of evidence in lifestyle medicine and encourage positive lifestyle medicine not only for our patients but also in our own lives.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Rippe is the editor in chief, American Journal of Lifestyle Medicine , and editor of Lifestyle Medicine (CRC Press). He is also founder and director, Rippe Lifestyle Institute, a research organization that has conducted multiple studies in physical activity, nutrition, and weight management.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
You are using an outdated browser. Please upgrade your browser to improve your experience.
Skip to Site Navigation Skip to Page Content
- Physician Referrals
- Patient Resources
- Why UT Southwestern
Refine your search: Find a Doctor Search Conditions & Treatments Find a Location

Appointment New Patient Appointment or Call 214-645-8300
Diet and Nutrition; Prevention
Lifestyle Medicine: How it could save your life
December 30, 2021
It’s 2 p.m. and you’re tired. You drink a caffeinated soda for a boost of energy, but it fades quickly. By dinnertime, you’re too exhausted or busy to cook, so you hit the drive-thru. And the restful evening you desperately need is cut short because you are driving your kids to their activities and worrying about everything else you didn’t get done.
We all have days like this. But if chaos becomes routine, our health pays the price – often without us even realizing it.
Studies continuously show that the way we live is linked to our risk of chronic disease. For example, data show that behavior changes could prevent 80% of heart disease , stroke , and Type 2 diabetes , and 40% of cancer diagnoses .
What’s especially troubling is how early chronic conditions are developing. An in-depth review of mortality in the United States found that unhealthy behaviors, such as substance abuse and lack of exercise, are decreasing life expectancy in adults ages 25-44.
I’m not sharing these statistics to scare you. Quite the opposite: Research shows that committing to healthy lifestyle changes can reduce – and often reverse – the burden of chronic illness. A physician who helps you focus on the six pillars of a healthy lifestyle can help you set reasonable goals to make incremental, impactful, and lasting changes.
Lifestyle Medicine shifts the focus of treatment from symptoms to causes. Doctors certified and trained in the tenets of Lifestyle Medicine can help you adopt healthier behaviors that lower the risk of developing chronic conditions such as:
- Alzheimer’s disease and dementia
- Coronary heart disease
- Heart failure
- High cholesterol
- Hypertension
- Kidney disease
- Obstructive pulmonary disease
UT Southwestern is eager to be your source for accurate, manageable advice that can help you take control of your future health. Beginning today, my colleagues and I will provide regular articles on UTSW’s MedBlog devoted to Lifestyle Medicine, which addresses the root causes of chronic diseases and can prevent, treat, and even reverse them.
6 pillars of Lifestyle Medicine
The American College of Lifestyle Medicine has established six key areas that impact everyone’s overall health and goals:
1. Nutrition: We’ve all heard it: “You are what you eat.” And eating mostly plant-based foods, such as fruits, vegetables, beans, nuts, seeds, and whole grains, is the foundation of a healthy diet.
2. Exercise: Regularly engaging in physical activity, which can include walking, gardening, sports, running, and strength training, is also a vital part of your overall health.
3. Stress management: Stress is unavoidable, especially these days, and it can affect every aspect of your health. But you can learn healthy techniques to manage it.
4. Substance abuse: Reducing or eliminating the use of addictive substances, such as tobacco, alcohol, and drugs, is particularly important in lowering your risk of cancer and heart disease.
5. Sleep: The amount and quality of sleep you get affects your immune system, but your need for restful sleep is often overlooked. Diet changes and other behaviors can improve sleep health.
6. Relationships: Positive social connections are beneficial for mental and physical health. The pandemic has taken a significant toll on our mental health and contributed to an overall sense of isolation.
A team-based approach is the key to success. At UT Southwestern, primary care providers collaborate with specialists and other health professionals who work within each of these six pillars to ensure patients receive personalized, comprehensive care.
Related reading: The art and science of tackling obesity
Focus on controllable factors
While Lifestyle Medicine emphasizes individual decision-making, practitioners understand that many patients’ choices are influenced by factors outside of their control, from health policies to socioeconomic status.
Focusing on what you can control, regardless of circumstances, can be empowering. And small changes can make a big difference . For example, I’ve helped patients learn how to fit healthy food choices into a tight budget, plan healthy meals that can be made quickly, and practice mindfulness techniques to lower anxiety levels caused by a stressful job they can’t afford to lose.
If your health is suffering for reasons beyond your control, talk with your doctor. They can connect you with resources to address these issues and provide evidence-based guidance that will help you optimize your health in practical, sustainable ways.
Related reading: 4 studies that defy conventional thinking about race, weight loss, and heart health
It can be easy to get used to living a certain way and hard to acknowledge that some of our favorite habits – such as drinking three or four sodas a day – may be doing more harm than good. But to realize the impact, you must make the change.
When I talk with patients about their lifestyle, we also discuss their personal goals and priorities. If multiple behaviors need to be modified, I don’t recommend changing everything at once. Instead, we decide together which ones are easiest to start with and work from there.
Evidence-based expertise
As a primary care provider focused on internal medicine , I’m also one of several UT Southwestern physicians certified in Lifestyle Medicine by the American College of Lifestyle Medicine . The certification means I have a solid understanding of the evidence that shows lifestyle directly affects your health.
My colleagues and I wanted to start this regular Lifestyle Medicine blog to help patients understand some of the everyday factors that affect their health. We look forward to exploring topics such as:
- Diet trends: the benefits and drawbacks of different fad diets
- The power of plant-based diets to lower cholesterol
- Lifestyle Medicine’s impact on mental health – particularly in pediatric populations
- The long-term effects of eating too many processed foods
- How interrupted sleep patterns affect your physical and mental health
We also know that even the healthiest person can develop a chronic condition. Lifestyle changes do not guarantee a disease-free life, and any person or product claiming otherwise is not to be trusted. The strategies we recommend when helping patients reach their goals are helpful, impactful – and truthful.
UT Southwestern providers work together to create customized care plans that can help patients reach their goals. This allows patients to get all the support they need within one system, from specialists who have quick access to their medical history. No matter which habits you want to make – or break – we’re here to help make your progress easier and more successful.
To discuss healthy lifestyle habits with a Lifestyle Medicine doctor, call 214-645-8300 or request an appointment online .
More in: Diet and Nutrition , Prevention

Next Article Food Is Medicine research hits home, help patients improve long-term health
More from Diet and Nutrition
Diet and Nutrition
Food Is Medicine research hits home, help patients improve long-term health
- Jaclyn Albin, M.D.
April 9, 2024

5 tips for a healthy Ramadan fast
- Zaiba Jetpuri, D.O.
March 15, 2024

Cancer; Diet and Nutrition
Ask the dietitian: How can good nutrition help cancer patients?
February 22, 2024

Dry January: The health benefits of going 31 days without alcohol
- Bethany Agusala, M.D.
December 27, 2023

6 tips for healthy, happy eating during the holidays
December 21, 2023

Traveling with diabetes: Tips for packing, snacking, monitoring, and more
November 20, 2023

6 health benefits of pumpkin and its spices – beyond the latte
October 23, 2023

Weight-loss medications: The 5 most-asked questions
- Tonia Vinton, M.D.
October 6, 2023

Anti-obesity drugs are closing the gap between dieting and bariatric surgery
- Jaime Almandoz, M.D.
September 7, 2023
More Articles
Appointment New Patient Appointment or 214-645-8300 or 817-882-2400
- Share via Facebook facebook
- Share via Twitter twitter
- Share via LinkedIn linkedin
- Share via Email email
- Print this page print
Advertisement
The Dynamic Interplay of Healthy Lifestyle Behaviors for Cardiovascular Health
- Nutrition (K. Petersen, Section Editor)
- Open access
- Published: 24 November 2022
- Volume 24 , pages 969–980, ( 2022 )
Cite this article
You have full access to this open access article
- Penny M. Kris-Etherton ORCID: orcid.org/0000-0001-6012-4900 1 na1 ,
- Philip A. Sapp ORCID: orcid.org/0000-0003-1431-0619 1 na1 ,
- Terrance M. Riley 1 ,
- Kristin M. Davis 1 , 2 ,
- Tricia Hart 1 &
- Olivia Lawler 1
3626 Accesses
9 Citations
Explore all metrics
Purpose of Review
The recent rise in cardiovascular disease (CVD) deaths in the USA has sparked interest in identifying and implementing effective strategies to reverse this trend. Healthy lifestyle behaviors (i.e., healthy diet, regular physical activity, achieve and maintain a healthy weight, avoid tobacco exposure, good quality sleep, avoiding and managing stress) are the cornerstone for CVD prevention.
Recent Findings
Achieving all of these behaviors significantly benefits heart health; however, even small changes lower CVD risk. Moreover, there is interplay among healthy lifestyle behaviors where changing one may result in concomitant changes in another behavior. In contrast, the presence of one or more unhealthy lifestyle behaviors may attenuate changing another lifestyle behavior(s) (poor diet, inadequate physical activity, overweight/obesity, poor sleep quality, tobacco exposure, and poor stress management).
It is important to assess all of these lifestyle behaviors with patients to plan an intervention program that is best positioned for adherence.
Similar content being viewed by others

Lifestyle Medicine and the Management of Cardiovascular Disease
Kimberly N. Doughty, Nelson X. Del Pilar, … David L. Katz

Changing Lifestyle Behaviors to Improve the Prevention and Management of Cardiovascular Disease

Avoid common mistakes on your manuscript.
A Healthy Dietary Pattern
Evidence from epidemiologic studies and clinical trials has shown that a healthy dietary pattern significantly reduces risk of CVD and also major risk factors for CVD. Strong and consistent evidence from epidemiologic studies has shown that higher diet quality is associated with lower relative and absolute risk of CVD and also longer CVD-free survival time [ 10 ]. In the Nurses’ Health Study I and II and the Health Professionals Follow-up Study, participants in the highest diet quality quintile compared with the lowest diet quality quintile had a 14–21% lower risk of CVD [ 11 ]. Likewise, in the Women’s Health Initiative Observational Study, a higher diet quality was associated with an 18–26% lower risk of all-cause and CVD mortality [ 12 ]. There is convincing clinical trial evidence demonstrating that a healthy dietary pattern decreases multiple major CVD risk factors, including elevated LDL-C and blood pressure [ 13 ] in addition to other cardiometabolic risk factors (i.e., increased blood glucose, triglycerides, waist circumference, and body weight) [ 14 ]. Based on these collective findings, the 2020 DGAC Committee concluded that there was strong and consistent evidence that a healthy dietary pattern is associated with a decreased risk of CVD [ 13 ], a conclusion that aligns with the 2021 AHA Scientific Statement, Dietary Guidance to Improve Cardiovascular Health [ 15 •].
It is well known that social and behavioral risk markers (e.g., physical activity, diet, smoking, and socioeconomic position) cluster and have a corresponding impact on risk of CVD [ 16 , 17 ]. With respect to social determinants, the AHA Healthy Diet Score is related to race and ethnicity, and to the family income to poverty ratio, such that diet quality decreases with lower economic status [ 2 ]. In addition, in the Women’s Health Initiative, women reporting a higher diet quality at baseline were non-Hispanic white, educated, physically active, past or never smokers, hormone therapy users, had lower BMI and waist circumference, and were less likely to have chronic conditions [ 18 ]. Evidence of a healthy diet clustering with other healthy lifestyle behaviors comes from a cross-sectional analysis of the Prevención con Dieta Mediterránea (PREDIMED)-Plus Trial designed to evaluate the effects of a Mediterranean Diet plus body mass reduction achieved by physical activity promotion and dietary energy reduction in 6646 participants living in Spain [ 19 ]. Lifestyle factors including nonsmoking and avoidance of sedentary lifestyles were associated with better diet quality. Moreover, in a cross-sectional analysis conducted with participants in the PREDIMED Trial, better sleep quality was related to higher adherence to a Mediterranean Diet, a lower BMI and waist circumference compared to poor sleep quality [ 20 ].
Given that a healthy diet clusters with other lifestyle behaviors, questions persist about whether a diet intervention specifically can “spillover” and benefit other lifestyle behaviors and, in fact, be a gateway for a change in other lifestyle behaviors not targeted. In a short literature review on this topic, Sarma et al. concluded that the evidence is inconsistent, which prompted their study to evaluate the effect of a diet intervention on other lifestyle modifications in participants in the Women’s Health Initiative (WHI) [ 21 ]. After 1 year, there was no change in physical activity, alcohol consumption, and smoking behavior in women in the diet intervention group leading the authors to conclude that diet modification does not have a spillover effect on untargeted behaviors and that changing multiple health behaviors may require targeting additional behaviors. However, there were benefits of the dietary intervention on several health factors and behaviors in WHI. For example, the dietary intervention benefited body fat percentage (− 0.8% [95% CI − 1.0%, − 0.6%]) despite this not being targeted for change [ 22 ]. Moreover, a 10% increase in diet quality was associated with a smaller increase in waist circumference (0.07 to 0.43 cm) after 3 years (all P < 0.05) [ 23 ]. In addition, at 1-year follow-up, the diet intervention was associated with significant improvements in three health-related quality of life (HRQoL) subscales: general health, physical functioning, and vitality [ 24 ]. Finally, there is evidence that improvements in diet quality scores are related to optimism and good mental health in postmenopausal women [ 18 , 25 ].
Physical Activity
Current recommendations for physical activity are 150 min per week of moderate physical activity or 75 min per week of vigorous physical activity, which is equivalent to 11.25 metabolic equivalent hours per week (MET h/week) [ 26 , 27 ]. Based on an extensive literature review of physical activity and health issued by the 2018 Physical Activity Guidelines Advisory Committee, there is a strong evidence for an inverse dose–response relation between moderate-to-vigorous physical activity and CVD incidence [ 26 , 28 ]. Adults increasing physical activity from baseline inactivity to low (0–11.5 MET h/week), medium (11.5–29.5 MET h/week), and high (> 29.5 MET h/week) physical activity had a reduced risk of CVD incidence (0.89 [95% CI 0.82, 0.98]; 0.79 [95% CI 0.69, 0.89]; and 0.75 [95% CI 0.64, 0.87]) [ 26 ]. In addition, there is strong evidence demonstrating a significant relationship between greater amounts of physical activity and decreased incidence of CVD, stroke, and heart failure. Physical activity also decreases CVD risk factors, including overweight or obesity, hypertension, high blood cholesterol, and blood glucose [ 29 , 30 ].
A meta-analysis of 33 studies evaluating the relationship between CVD and physical activity with an average follow-up of 12.8 years found that sedentary adults (ages 25–93 years) that increased physical activity to the current recommendation (11.25 MET h/week) had a 23% (95% CI, 0.71–0.84) reduction in risk of CVD mortality and a 17% (95% CI, 0.77–0.89) reduction in CVD incidence [ 26 ]. Additionally, individuals who were inactive (0 MET h/week) and incorporated even small amounts (6 MET h/week) of physical activity into their routine had a reduction in CVD risk [ 26 ]. This increase in sedentary to light activity over a ~ 13-year period resulted in a risk reduction of 4.3% per MET h/week for CVD mortality and 1.7% for CVD incidence [ 26 ]. Potential mechanisms for the dose-dependent response of exercise to decreased CVD risk include improved glycemic control [ 31 ], improved vascular health [ 29 , 32 , 33 ], and improved leptin sensitivity [ 34 ].
While the focus of physical activity attenuating CVD risk is often associated with concurrent weight loss, physical activity benefits CVD risk independent of body weight changes [ 26 ]. An AHA meta-analysis highlighted several trials showing physical activity, independent of weight loss, benefits CVD mortality with only moderate changes in risk ratios when adjusting for weight loss [ 26 , 35 ]. Moreover, a NHANES study (2007–2016) with 22,476 adults revealed a lower 10-year CVD risk when comparing obese inactive (1–149 min/week moderate to vigorous activities) (OR: 0.66 [95% CI: 0.49, 0.89]) and obese active (≥ 150 min/week moderate to vigorous activities) (OR: 0.50 [95% CI: 0.37, 0.69]) to obese and sedentary individuals (0 min/week moderate to vigorous activities) [ 36 ]. Across all BMI categories, active individuals had a lower 10-year CVD risk than inactive adults (< 150 min/week) [ 36 ]. Although physical activity independently improves CVD risk, the addition of other healthy lifestyle factors provides cumulative benefits [ 16 ]. When nutrition education alone is compared with education plus physical activity, the combined intervention resulted in greater weight loss (10.9 kg [95% CI 9.1–12.7]) than nutrition education over 6 months (8.2 kg [95% CI 6.4–9.9]) [ 37 ].
Meeting physical activity recommendations may influence other lifestyle behaviors. The US Department of Health and Human Services Advisory Committee reported that regular physical activity could improve sleep, reduce anxiety, slow or reduce weight gain, prevent weight regain after initial loss, and contribute to weight loss [ 30 ]. The 2018 Physical Activity Guidelines Advisory Committee Scientific Report rated the evidence as strong for the effect of moderate-to-vigorous exercise on improvements in sleep quality, reducing both acute and chronic anxiety and preventing obesity [ 38 ]. Thus, increasing physical activity can benefit other lifestyle behaviors to lower CVD risk.
Healthy Weight
Clinical and observational studies support a consistent relationship between body weight, CVD risk, and CVD-related risk factors. Weight status is often classified by a BMI score calculated by kg/m 2 (underweight, ≤ 18.5; normal weight, 18.5–24.9; overweight, 25–29.9; obesity, 30–34.9; and morbid obesity, ≥ 35). A recent review of meta-analyses of observational studies reported a consistent positive association between BMI and CVD risk [ 39 ]. Khan et al. assessed the relationship between CVD and BMI with data from 10 US cohorts (3.2 million person-years) and reported that, compared to men and women with a normal BMI, those with an overweight, obese, and morbidly obese BMI had a 21–32%, 67–85%, and 253–314% increased risk of having a CVD event [ 40 ]. The long-term effects of weight loss on CVD outcomes are limited, but there is substantial clinical trial evidence demonstrating that weight loss improves dyslipidemia [ 41 ], blood pressure [ 42 ], and glucose [ 43 ]. Based on epidemiological and clinical trial evidence, a recent AHA Scientific Statement on Obesity and CVD concluded that obesity contributes to increased CVD risk factors and the development of CVD. Further long-term clinical trials assessing lifestyle interventions for weight loss are necessary [ 44 ].
Body weight (BMI) and healthy lifestyle behaviors (e.g., diet, physical activity, stress, and sleep) are interconnected. In an analysis of the National Health and Nutrition Examination Survey (NHANES) III data, women and men, respectively, had 8.3 and 14.5% lower odds of abdominal obesity for each 10-point increase in Healthy Eating Index (range: 0–100) [ 45 ]. Ford et al. analyzed data from the Geisinger Rural Aging Study and reported that health and activity limitation index (perceived health and activity limitation) scores were significantly higher for adults with a normal BMI compared to those with an underweight, overweight, or obese BMI [ 46 ]. Similarly, in a cross-sectional analysis of UK adults, greater weekly physical activity was inversely associated with BMI and body fat percentage [ 47 ]. Lastly, cross-sectional studies consistently show an inverse association between BMI and sleep quality, but further research is necessary to understand this association and determine causation [ 48 ]. There is a consistent relationship between BMI and other lifestyle behaviors, but it is important to understand how these behaviors change when body weight, or BMI, improves.
There is consistent clinical evidence supporting dietary modification and increased physical activity for weight loss [ 49 ], but few trials have evaluated the effects of weight loss on other lifestyle behaviors. Das et al. conducted a 12-month parallel randomized controlled trial in free-living adults comparing two weight-loss interventions with the common goal of reducing calories (500–1000 kcal/day) and achieving physical activity goals (150 min/week), but one emphasized weight loss through tracking food and physical activity (modified Diabetes Prevention Program [m-DPP]) and the other emphasized behavior change (stress management, mindful eating, etc.) (Healthy Weight for Living [HWL]) [ 50 ]. Both interventions (m-DPP and HWL) significantly improved weight (− 7.32 and 7.46 kg) and cardiometabolic risk factors (LDL-C [− 10 and − 15 mg/dL], triglycerides [18 and − 21 mg/dL], and glucose [− 3 and − 6 mg/dL]) from baseline with similar non-significant improvements in sleep, emotional, and general health. Additionally, a systematic review of studies on behavioral and dietary weight loss interventions found simultaneous improvements in depressive symptoms, body image, and health-related quality of life (perceived physical and mental health) with weight loss [ 51 ].
Avoid Tobacco Exposure
Tobacco use is a well-established, major risk factor for CVD. Components in tobacco products are causally linked to diseases of every major organ system mediated in part by dysfunction of the heart and vasculature [ 52 , 53 , 54 ]. Although smoking prevalence has declined in the USA over the last several decades, tobacco smoking is the second leading risk factor of overall disease burden [ 55 ] and second leading population attributable fraction (PAF: 13.7% [95% CI 4.8–22.3%]) for CVD mortality [ 56 ]. A retrospective analysis of 5 cohorts ( n = 2.2 million) from 2000 to 2010 showed a 3 times greater risk of death from ischemic heart disease (IHD) in smokers aged 55–74 compared to never smokers [ 57 ]. The risk of IHD increases in a dose-dependent manner with the number of cigarettes smoked per day. The Pooling Project on Diet and Coronary Heart Disease (CHD) comprising 12 prospective cohorts ( n = 266,787) showed that the probability of CHD in smokers, relative to never smokers, is the highest in women aged 40 to 49 years (HR: 8.5 [95% CI 5.0–14.0]) and that the majority of CHD cases were attributable to smoking among all age groups (40 to 49 years, 88% (95% CI = 82%, 94%); 50 to 59 years 81% (95% CI = 77%, 85%); 60 to 69 years, 71% (95% CI = 65%, 76%), + 70 years, 68 (95% CI = 53%, 82%)) [ 58 ].
Tobacco use in the form of electronic nicotine delivery systems (i.e., electronic(e)-cigarettes, vaping, etc.) is also of significant concern. E-cigarette use has increased over the last decade primarily in adolescents (12–19 years of age) [ 59 ]. In 2019, the National Youth and Tobacco Survey found that about 8 million (53.3%) high school students and 2.9 million (24.3%) middle school students reported ever using tobacco products of which e-cigarettes were the most common (35.0%) [ 9 •]. Although the long-term effects are not yet confirmed, the metabolic damage seen in e-cigarette users aligns with those seen in smokers. Current evidence suggests e-cigarettes and vaping results in systemic inflammation, endothelial dysfunction, vascular stiffening, and increased blood pressure [ 59 ]. Due to the similarities in metabolic effects, use of electronic nicotine delivery systems is likely to cause adverse CVD outcomes.
Cessation of tobacco use independently and in combination with CVD-related health behaviors (e.g. diet, exercise, weight management) improves CVD risk. A meta-analysis of 25 cohorts ( n = 503,905) of men and women 60 years and older showed lower cardiovascular mortality risk for former smokers (HR: 1.37 [95% CI 1.25–1.49]) than current smokers (2.07 [95% CI 1.82–2.36]) when compared with non-smokers over an 8 to 13 year follow up [ 60 ]. Early cessation improves health outcomes such that quitting smoking between 25 and 35 years of age is associated with up to a 10 year longer life expectancy [ 57 ]. The benefits may be augmented when accompanied by healthy behaviors. In a cohort ( n = 32,887) of Chinese adults with prehypertension (SBP, 120–139 mm Hg; DBP, 80–89 mm Hg), there was a stepwise risk reduction (~ 14%) of progression to hypertension for each increase in the number of health behaviors (0 to > 5), including quitting smoking, over 6 years [ 61 ]. The Organization to Assess Strategies in Acute Ischemic Syndromes (OASIS) Registry of five trials including 18,809 patients from 41 countries with unstable angina or myocardial infarction demonstrated that smoking cessation coupled with diet and exercise improved the odds of a repeat CVD event (OR: 1.62 [95% CI 0.96–2.75]) compared to persistent smoking without modification of diet or exercise (OR: 3.77 [95% CI 2.40–5.91]) over 6 months [ 62 ]. Comparatively, persistent smokers without diet and lifestyle changes had 3.77 higher odds (95% CI: 2.40–5.91) of a repeat event. These findings support the incorporation of treatments that target healthy behaviors in addition to smoking cessation to improve CVD-related outcomes.
Tobacco cessation interventions have been shown to adversely affect healthy lifestyle behaviors and CVD risk factors. Increases in caloric intake, appetite, and weight following smoking cessation have been commonly reported and may reduce abstinence [ 63 ]. A recent Cochrane systematic review and meta-analysis of 83 trials examining intervention designed to aid smoking cessation (e.g., diet, exercise, nicotine replacement therapies) found that exercise reduced weight gain (mean difference − 2.07 kg [95% CI − 3.78 to − 0.36]) at 12 months but not immediately following the interventions [ 64 ]. Mean difference in personalized weight management support (i.e., very low-calorie diet, diet education) showed no differences in weight reduction. However, many results were of low certainty of evidence suggesting that more research combining cessation interventions with other healthy behaviors is needed. Nonetheless, since 68% of smokers desire to quit [ 65 ], integrating cessation interventions with other healthy lifestyle behaviors will be most beneficial to CVD risk.
Addressing negative impacts to healthy behaviors with smoking cessation may require an environmental and social approach. A recent rapid-realist review ( n = 138 trials) using a behavior change framework (motivation, capability, opportunity) suggests that the best approaches for successful smoking cessation in public health promotion interventions should shift from “individualistic epidemiology” to targeting of external factors [ 66 •]. Studies that improve resource access (i.e. healthy foods, exercise), changed the physical environment (smoke-free policies), and improved support networks (including family members into care, social events) were more likely to help with cessation. Moreover, interventions that modified external factors intended to prompt or facilitate multiple healthy behaviors were associated with greater success, whereas successful interventions with an individualistic focus (i.e., enhancing knowledge/skills) tended to be context dependent. Overall, innovative clinical and public health approaches combining smoking cessation and environmental factors as parts of multicomponent behavioral interventions are needed to determine effective strategies in health promotion.
Sleep Quality
Sleep is considered to be an emerging risk factor for CVD [ 67 ]. There is growing evidence that both sleep duration and sleep quality affect CVD risk development [ 68 ]. In the Multi-Ethnic Study of Atherosclerosis (MESA) with 1992 participants free of CVD, those with most irregular sleep duration or timing versus those with the most regular sleep patterns had more than a twofold greater risk of developing CVD after 4.9 years of follow-up [ 69 ]. A large prospective cohort study of 60,586 adults in Taiwan examined the impact of sleep quality and duration on the risk of CHD and reported that short sleep duration (< 6 h/day) and poor sleep quality (measured by sleep index score—comparing the lowest versus the highest quintiles) increased risk of CHD by about 30% [ 70 ]. Similarly, in an analysis of 407,500 participants in the UK Biobank Study, excess sleep (over 9 h) or short sleep (under 5 h), compared to the reference group (7 h), was associated with a higher risk of CVD mortality (HR: 1.27 [95% CI 1.09–1.49] and HR: 1.32 [95% CI 1.16–1.50], respectively) and CVD incidence (HR: 1.23 [95% CI 1.16–1.31] and HR: 1.08 [95% CI 1.02–1.15], respectively) [ 71 ]. Sleep irregularity also has been shown to increase cardiometabolic disease risk. In a review of cross-sectional and prospective studies published between 2015 and 2020, Zuraikat et al. reported that greater variability in sleep duration and sleep onset was associated with increased risk for metabolic syndrome, type-2 diabetes, and obesity [ 72 ].
Studies of coronary patients also have shown an association between sleep duration and increased risk of CVD. Using data from the Emory Cardiovascular Biobank of 2846 patients with coronary artery disease, both short sleep duration (< 6.5 h) and long sleep duration (≥ 7.5 h) compared to normal sleep (≥ 6.5 and < 7.5 h) were associated with higher all-cause mortality (HR: 1.44 [95% CI 1.10–1.89] and 1.41 [95% CI 1.08–1.85], respectively) [ 73 ]. For cardiovascular mortality, only short sleep duration increased risk (HR: 1.48 [95% CI 1.05–2.09]) [ 73 ]. In the Progression of Early Subclinical Atherosclerosis Study of 3974 patients, those who slept less than 6 h had a greater preclinical atherosclerotic burden versus the reference group (who slept 7–8 h) [ 74 ].
Poor quality sleep adversely affects diet quality and physical activity, which could, in part, explain the cardiometabolic health consequences related to unhealthy sleep. In the AHA Go Red for Women prospective cohort study of 495 participants, poor sleep quality was associated with greater food intake and lower-quality diet (i.e., lower unsaturated fat intake; higher food weight, energy, and added sugars consumed; and a lower intake of whole grains) [ 75 ]. Similarly, a review on sleep, diet, and cardiovascular health by St-Onge and Zuraikat suggests sleep restriction increases unhealthy food choices and energy intake [ 76 ]. Short sleepers (< 7 h) reported lower intakes of fruits and vegetables and fiber, and higher intakes of saturated fat and snacks relative to adequate sleepers (at least 7 h). In a meta-analysis of 11 randomized controlled sleep restriction studies, the average increase in energy intake was 385 cal per day after partial sleep deprivation (3.75 to 5.5 h for several days) compared to adequate sleep (7–9 h) [ 77 ]. Interestingly, there also is a relationship between poor diet quality and poor sleep quality. In a systematic review of nine studies that assessed the relationship between diet quality and sleep quality, consumption of a healthy dietary pattern (which included high intake of plant derived foods, whole grains, legumes, seafood, and olive oil) was associated with better sleep quality, whereas higher intake of processed foods and added sugars was associated with lower sleep quality [ 78 ].
Poor sleep quality affects other lifestyle behaviors, including physical activity and stress-related disorders. A systematic review and meta-analysis including observational and intervention studies examined daily associations between sleep and physical activity and reported that three sleep parameters (sleep quality, sleep efficiency, and wake after sleep onset) were associated with physical activity the following day [ 79 ]. The authors noted, however, that the associations were small and variable relative to the sleep parameter assessed (sleep quality, sleep efficiency, and wake after sleep onset) that could have been related to the different methods used to evaluate both sleep measures and physical activity. In addition, sleep and physical activity associations were evaluated in ten studies, four of which associated high sleep quality with higher total physical activity, whereas six studies reported no association. In the UK Biobank cohort of 82,995 participants, an inverse “U-shaped” relationship between objective sleep duration and physical activity level identified the most physical activity reported for those who slept between 6 and 7 h [ 80 ]. Another recent meta-analysis reported that sleep disturbances increase risk of anxiety-related disorders [ 81 ] with some evidence indicating that sleep deprivation adversely affects stress.
Collectively, the evidence shows many associations between sleep quality and risk of cardiovascular/cardiometabolic diseases. The associations of sleep with other lifestyle behaviors including diet quality, physical activity, and stress management reinforce the importance of getting quality sleep for heart health. However, evidence suggests that poor adherence to other lifestyle behaviors (e.g., poor quality diet) can adversely affect sleep quality, which underscores the importance of understanding of how all lifestyle behaviors interact to affect cardiovascular health.
Stress Management
The association between psychosocial stress and CVD risk has substantial empirical support [ 82 , 83 , 84 , 85 ]. Prospective observational studies have found that chronic stress is associated with a 40–50% increase in CHD risk [ 82 ]. Results from the INTERHEART study suggest that general stress increases risk of myocardial infarction by 38% (several periods of stress) to 114% (permanent stress) [ 86 ]. Stress has also been associated with increased risk of other forms of CVD, including stroke and atrial fibrillation [ 87 ], hypertension, blood pressure fluctuation, and carotid artery plaque [ 88 ], and stress (Takotsubo) cardiomyopathy [ 89 ]. Briefly, acute psychosocial stress activates two key stress response systems, the sympathetic nervous system (SNS) and the hypothalamic–pituitary–adrenal (HPA) axis. Activation of the SNS results in increased inflammation, potentially accelerating the atherosclerotic process [ 90 ]. The end product of the HPA axis, cortisol, has anti-inflammatory properties; however, under conditions of chronic stress, glucocorticoid resistance can result in upregulated inflammation [ 91 , 92 ]. Between-person differences in the degree of SNS and HPA axis activation may moderate the association between perceived stress and CVD risk [ 83 ]. Similarly, augmented activity of the amygdala has been implicated in the association between stress and CVD risk; because the amygdala is a brain region that regulates physiological stress responses, increased activity here implies greater stress reactivity [ 83 ]. Chronic or traumatic stress in childhood compared to adulthood appears to have a stronger effect on CVD risk [ 87 ]. However, stress in adulthood can accelerate the development of atherosclerosis, act as a disease trigger in individuals with advanced atherosclerotic plaques, and adversely affect CVD prognosis and outcomes [ 87 , 93 ]. Cultivating healthy stress management practices has shown promise for both the primary and secondary prevention of CVD [ 94 ] leading to the inclusion of stress management in some clinical guidelines for CVD risk reduction [ 95 ].
Stress is often tied to the development of maladaptive coping mechanisms, with a negative impact on CVD outcomes [ 82 , 83 ]. High stress levels are associated with poor health behaviors, including worse diet quality [ 96 , 97 , 98 , 99 , 100 , 101 ]; less physical activity [ 85 , 101 , 102 ]; increased use of tobacco, alcohol, and other drugs [ 85 , 103 , 104 , 105 , 106 ]; and reduced sleep quantity and quality [ 107 , 108 , 109 , 110 ]. Stress also negatively impacts body weight and body composition [ 96 , 111 ]. Those experiencing ≥ 3 chronic stressors have a 50% increase in odds of obesity and are more likely to have an elevated waist circumference and body fat percentage compared to those without chronic stress [ 96 ]. Poor health behaviors mediate the association between stress and CVD risk, accounting for 65% of the observed variance [ 85 ]. Evidence suggests that the relationship between health behaviors and stress is often bi-directional. For example, those with high stress levels are less likely to engage in regular physical activity [ 101 , 102 ], and regular exercise has been shown to improve stress reactivity [ 112 , 113 ] and reduce perceived stress [ 114 ]. Similarly, while high stress levels are often associated with sleep impairments, sufficient sleep quantity and quality can reduce stress levels [ 107 , 108 , 115 ]. This bi-directionality has potentially wide-reaching benefits for prevention and intervention research: targeting stress may help improve other health behaviors, and targeting other health behaviors may be an effective way to improve stress management.
Stress management- and stress reduction-based intervention techniques are widely used, especially in the context of improving health behaviors [ 116 , 117 , 118 ]. Mindfulness-based interventions appear to be a particularly valuable tool for improving stress management abilities, with positive impacts on CVD risk [ 119 ]. To date, few interventions using stress reduction to improve diet quality have been tested, but initial results are promising. For example, mindfulness-based stress reduction interventions have successfully reduced sweets consumption in obese adults [ 120 ] and improved diet quality in healthy adults [ 121 ]. Research is needed to investigate the impact of stress reduction on physical activity. Results thus far have been conflicting: some studies have found that stress reduction improves physical activity outcomes, others have reported no association, and still others have observed adverse outcomes [ 102 ]. Evidence suggests that weight loss interventions are less effective for highly stressed individuals; very few intervention studies have targeted stress management as a weight loss intervention [ 111 ]. Of two known studies, both are small ( n = 34 and 44), and only one reported that including stress management significantly improved weight loss [ 122 ]. The other reported a non-significant trend toward improved weight loss with the addition of stress management [ 123 ]. Use of stress management as a tobacco cessation tool is well-supported. Evidence suggests that tobacco is often used to cope with stress, and that smoking cessation requires the development of healthier coping strategies [ 124 ]. Stress management interventions reduce tobacco use [ 125 ] and improve cessation outcomes, including reducing the risk of relapse [ 126 , 127 ]. Meta-analyses suggest that mindfulness-based stress reduction techniques may help improve sleep in individuals with insomnia [ 128 ] and in individuals without sleep disorders [ 118 ], but mixed results have been reported [ 129 ]. One interesting longitudinal study found that employees given more control over their work schedules reported less stress and getting an extra 30 min of sleep on weeknights [ 130 ]. Thus, stress management is a promising avenue for improving other health behaviors, including diet, physical activity, tobacco use, and sleep.
It is important for clinicians to be aware of the interplay of lifestyle behaviors. Modifying just one lifestyle behavior may be hindered by the presence of other unhealthy lifestyle behaviors. Therefore, identifying underlying lifestyle behavior-related problems (such as poor sleep, high stress) that could prevent the modification of a selected behavior will help guide a successful lifestyle behavior intervention program to improve heart health. Identifying a lifestyle behavior to target initially requires shared decision-making between the clinician and patient with the goal being to help the patient modify the selected lifestyle behavior(s). For some patients, targeting multiple lifestyle behaviors simultaneously may work. Regardless, it is important to be mindful of the status of all of the patient’s lifestyle behaviors in order to implement interventions that achieve optimal cardiovascular health.
Further research is needed to better understand the dynamic interplay of healthy lifestyle behaviors for cardiovascular health. Current lifestyle behavior research often focuses on just one specific lifestyle behavior. Future clinical trials need to evaluate the interplay of the multiple lifestyle behaviors discussed herein with the objective being to identify the best intervention strategies for successful lifestyle behavior change for improved cardiovascular health.
Papers of particular interest, published recently, have been highlighted as: • Of importance
Oblast T. Decline in deaths from heart disease and stroke—United States, 1900–1999. Hear Dis Stroke. 1900;63:593–7.
Google Scholar
Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation. 2022;145:e153-639.
Article Google Scholar
Sacco RL. The new American Heart Association 2020 goal: achieving ideal cardiovascular health. J Cardiovasc Med. 2011;12:255–7.
Lloyd-Jones DM, Allen NB, Anderson CAM, Black T, Brewer LC, Foraker RE, et al. Life’s essential 8: updating and enhancing the American Heart Association’s Construct of Cardiovascular Health: a presidential advisory from the American Heart Association. Circulation. 2022;146:e1–26.
Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD, et al. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–6.
Tsai M-C, Lee C-C, Liu S-C, Tseng P-J, Chien K-L. Combined healthy lifestyle factors are more beneficial in reducing cardiovascular disease in younger adults: a meta-analysis of prospective cohort studies. Sci Rep. 2020;10:1–10.
Article CAS Google Scholar
Li Y, Pan A, Wang DD, Liu X, Dhana K, Franco OH, et al. Impact of healthy lifestyle factors on life expectancies in the US population. Circulation. 2018;138:345–55.
• Kris-Etherton PM, Petersen KS, Després J-P, Braun L, de Ferranti SD, Furie KL, et al. Special considerations for healthy lifestyle promotion across the life span in clinical settings: a science advisory from the American Heart Association. Circulation. 2021;144:e515–32. This American Heart Association Science Advisory summarizes the 5A Model (assess, advise, agree, assist, and arrange) for counseling lifestyle behavior change (consuming a healthy diet, participating in regular physical activity, avoiding tobacco, achieving adequate sleep, and managing stress) across the lifespan.
• Kris-Etherton PM, Petersen KS, Després J-P, Anderson CAM, Deedwania P, Furie KL, et al. Strategies for promotion of a healthy lifestyle in clinical settings: pillars of ideal cardiovascular health: a science advisory from the American Heart Association. Circulation. 2021;144:e495-514. This American Heart Association Science Advisory presents strategies for clinicians and health care professionals to implement for efficient counseling of patients about healthy lifestyle behavior changes.
Petersen KS, Kris-Etherton PM. Diet quality assessment and the relationship between diet quality and cardiovascular disease risk. Nutrients. 2021;13:4305.
Shan Z, Li Y, Baden MY, Bhupathiraju SN, Wang DD, Sun Q, et al. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med. 2020;180:1090–100.
George SM, Ballard-Barbash R, Manson JE, Reedy J, Shikany JM, Subar AF, et al. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the women’s health initiative observational study: evidence to inform National Dietary Guidance. Am J Epidemiol. 2014;180:616–25.
Dietary Guidelines Advisory Committee. Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report of the Secretary of Agriculture and the Secretary of Health and Human Services. Washington, DC; 2020.
Kahleova H, Salas-Salvadó J, Rahelić D, Kendall CWC, Rembert E, Sievenpiper JL. Dietary patterns and cardiometabolic outcomes in diabetes: a summary of systematic reviews and meta-analyses. Nutrients. 2019;11:2209.
• Lichtenstein AH, Appel LJ, Vadiveloo M, Hu FB, Kris-Etherton PM, Rebholz CM, et al. 2021 Dietary Guidance to improve cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2021;144:e472–87. This Scientific Statement provides dietary guidance to benefit cardiovascular health and discusses overcoming challenges in population-wide adoption of the recommendation.
Fleary SA, Nigg CR. Trends in health behavior patterns among US adults, 2003–2015. Ann Behav Med. 2019;53:1–15.
Saint Onge JM, Krueger PM. Health lifestyle behaviors among US adults. SSM-Population Health. 2017;3:89–98.
Hingle MD, Wertheim BC, Tindle HA, Tinker L, Seguin RA, Rosal MC, et al. Optimism and diet quality in the Women’s Health Initiative. J Acad Nutr Diet. 2014;114:1036–45.
Cano-Ibáñez N, Gea A, Ruiz-Canela M, Corella D, Salas-Salvadó J, Schröder H, et al. Diet quality and nutrient density in subjects with metabolic syndrome: Influence of socioeconomic status and lifestyle factors. A cross-sectional assessment in the PREDIMED-Plus study. Clin Nutr. 2020;39:1161–73.
Muscogiuri G, Barrea L, Aprano S, Framondi L, Di Matteo R, Laudisio D, et al. Sleep quality in obesity: does adherence to the Mediterranean diet matter? Nutrients. 2020;12:1364.
Sarma EA, Moyer A, Messina CR, Laroche HH, Snetselaar L, Van Horn L, et al. Is there a spillover effect of targeted dietary change on untargeted health behaviors? Evidence from a dietary modification trial. Health Educ Behav. 2019;46:569–81.
Carty CL, Kooperberg C, Neuhouser ML, Tinker L, Howard B, Wactawski-Wende J, et al. Low-fat dietary pattern and change in body-composition traits in the Women’s Health Initiative Dietary Modification Trial. Am J Clin Nutr. 2011;93:516–24.
Cespedes Feliciano EM, Tinker L, Manson JE, Allison M, Rohan T, Zaslavsky O, et al. Change in dietary patterns and change in waist circumference and DXA trunk fat among postmenopausal women. Obes. 2016;24:2176–84.
Assaf AR, Beresford SAA, Risica PM, Aragaki A, Brunner RL, Bowen DJ, et al. Low-fat dietary pattern intervention and health-related quality of life: the Women’s Health Initiative randomized controlled dietary modification trial. J Acad Nutr Diet. 2016;116:259–71.
Tinker LF, Perri MG, Patterson RE, Bowen DJ, McIntosh M, Parker LM, et al. The effects of physical and emotional status on adherence to a low-fat dietary pattern in the Women’s Health Initiative. J Am Diet Assoc. 2002;102:789–800.
Wahid A, Manek N, Nichols M, Kelly P, Foster C, Webster P, et al. Quantifying the association between physical activity and cardiovascular disease and diabetes: a systematic review and meta-analysis. J Am Heart Assoc. 2016;5:e002495.
U.S. Department of Health and Human Services. Physical activity guidelines for Americans. 2nd ed. Washington, DC; 2018.
Kraus WE, Powell KE, Haskell WL, Janz KF, Campbell WW, Jakicic JM, et al. Physical activity, all-cause and cardiovascular mortality, and cardiovascular disease. Med Sci Sports Exerc. 2019;51:1270.
Tian D, Meng J. Exercise for prevention and relief of cardiovascular disease: prognoses, mechanisms, and approaches. Oxid Med Cell Longev. 2019;3756750.
Piercy KL, Troiano RP. Physical activity guidelines for Americans from the US department of health and human services: cardiovascular benefits and recommendations. Circ Cardiovasc Qual Outcomes. 2018;11:e005263.
Boniol M, Dragomir M, Autier P, Boyle P. Physical activity and change in fasting glucose and HbA1c: a quantitative meta-analysis of randomized trials. Acta Diabetol. 2017;54:983–91.
Barone Gibbs B, Hivert M-F, Jerome GJ, Kraus WE, Rosenkranz SK, Schorr EN, et al. Physical activity as a critical component of first-line treatment for elevated blood pressure or cholesterol: who, what, and how?: a scientific statement from the American Heart Association. Hypertens. 2021;78:e26-37.
Brockow T, Conradi E, Ebenbichler G, Michalsen A, Resch KL. The role of mild systemic heat and physical activity on endothelial function in patients with increased cardiovascular risk: results from a systematic review. Complement Med Res. 2011;18:24–30.
Jadhav RA, Maiya GA, Hombali A, Umakanth S, Shivashankar KN. Effect of physical activity promotion on adiponectin, leptin and other inflammatory markers in prediabetes: a systematic review and meta-analysis of randomized controlled trials. Acta Diabetol. 2021;58:419–29.
Elagizi A, Kachur S, Carbone S, Lavie CJ, Blair SN. A review of obesity, physical activity, and cardiovascular disease. Curr Obes Rep. 2020;9:571–81.
Zhang X, Cash RE, Bower JK, Focht BC, Paskett ED. Physical activity and risk of cardiovascular disease by weight status among U.S adults. PLoS One. 2020;15:e0232893.
Goodpaster BH, DeLany JP, Otto AD, Kuller L, Vockley J, South-Paul JE, et al. Effects of diet and physical activity interventions on weight loss and cardiometabolic risk factors in severely obese adults: a randomized trial. JAMA. 2010;304:1795–802.
Powell KE, King AC, Buchner DM, Campbell WW, DiPietro L, Erickson KI, et al. The scientific foundation for the physical activity guidelines for Americans. J Phys Act Health. 2018;16:1–11.
Dwivedi AK, Dubey P, Cistola DP, Reddy SY. Association between obesity and cardiovascular outcomes: updated evidence from meta-analysis studies. Curr Cardiol Rep. 2020;22:1–19.
Khan SS, Ning H, Wilkins JT, Allen N, Carnethon M, Berry JD, et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 2018;3:280–7.
Hasan B, Nayfeh T, Alzuabi M, Wang Z, Kuchkuntla AR, Prokop LJ, et al. Weight loss and serum lipids in overweight and obese adults: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2020;105:3695–703.
Ge L, Sadeghirad B, Ball GDC, da Costa BR, Hitchcock CL, Svendrovski A, et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. BMJ. 2020;369:m696.
Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med Mass Medical Soc. 2002;346:393–403.
Powell-Wiley TM, Poirier P, Burke LE, Després J-P, Gordon-Larsen P, Lavie CJ, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021;143:e984-1010.
Tande DL, Magel R, Strand BN. Healthy Eating Index and abdominal obesity. Public Health Nutr. 2010;13:208–14.
Ford DW, Jensen GL, Still C, Wood C, Mitchell DC, Erickson P, et al. The associations between diet quality, body mass index (BMI) and health and activity limitation index (HALex) in the Geisinger Rural Aging Study (GRAS). J Nutr Health Aging. 2014;18:167–70.
Bradbury KE, Guo W, Cairns BJ, Armstrong MEG, Key TJ. Association between physical activity and body fat percentage, with adjustment for BMI: a large cross-sectional analysis of UK Biobank. BMJ Open. 2017;7:e011843.
St-Onge M. Sleep–obesity relation: underlying mechanisms and consequences for treatment. Obes Rev. 2017;18:34–9.
Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755–67.
Das SK, Bukhari AS, Taetzsch AG, Ernst AK, Rogers GT, Gilhooly CH, et al. Randomized trial of a novel lifestyle intervention compared with the Diabetes Prevention Program for weight loss in adult dependents of military service members. Am J Clin Nutr. 2021;114:1546–59.
Lasikiewicz N, Myrissa K, Hoyland A, Lawton CL. Psychological benefits of weight loss following behavioural and/or dietary weight loss interventions. Syst Res Rev Appetite. 2014;72:123–37.
CAS Google Scholar
U.S. Department of Health and Human Services and U.S. Department of Agriculture. Smoking cessation: a report of the Surgeon General. Atlanta; 2020.
U.S. Department of Health and Human Services. How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease: a report of the surgeon general. Centers for Disease Control and Prevention; 2010.
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2014.
Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation. 2021;143:e254-743.
Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307:1273–83.
Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368:341–50.
Tolstrup JS, Hvidtfeldt UA, Flachs EM, Spiegelman D, Heitmann BL, Bälter K, et al. Smoking and risk of coronary heart disease in younger, middle-aged, and older adults. Am J Public Health. 2014;104:96–102.
Wold LE, Tarran R, Crotty Alexander LE, Hamburg NM, Kheradmand F, St Helen G, et al. Cardiopulmonary consequences of vaping in adolescents: a scientific statement from the American Heart Association. Circ Res. 2022;131:e70–82.
Mons U, Müezzinler A, Gellert C, Schöttker B, Abnet CC, Bobak M, et al. Impact of smoking and smoking cessation on cardiovascular events and mortality among older adults: meta-analysis of individual participant data from prospective cohort studies of the CHANCES consortium. BMJ. 2015;350:h1551.
Gao J, Sun H, Liang X, Gao M, Zhao H, Qi Y, et al. Ideal cardiovascular health behaviors and factors prevent the development of hypertension in prehypertensive subjects. Clin Exp Hypertens. 2015;37:650–5.
Chow CK, Jolly S, Rao-Melacini P, Fox KAA, Anand SS, Yusuf S. Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation. 2010;121:750–8.
Bush T, Lovejoy JC, Deprey M, Carpenter KM. The effect of tobacco cessation on weight gain, obesity, and diabetes risk. Obesity. 2016;24:1834–41.
Hartmann-Boyce J, Theodoulou A, Farley A, Hajek P, Lycett D, Jones LL, et al. Interventions for preventing weight gain after smoking cessation. Cochrane Database Syst Rev. 2021;10:CD00219.
United States Public Health Service Office of the Surgeon General & National Center for Chronic Disease Prevention and Health Promotion Office on Smoking and Health. Smoking cessation: a report of the Surgeon General. 2020.
• Minian N, Corrin T, Lingam M, deRuiter WK, Rodak T, Taylor VH, et al. Identifying contexts and mechanisms in multiple behavior change interventions affecting smoking cessation success: a rapid realist review. BMC Public Health. 2020;20:1–26. In this realist review of 138 papers, the authors conclude that public health promotion interventions need to focus on modifying factors that are external from the individual, such as creating a supportive environment.
Makarem N, St-Onge M-P, Liao M, Lloyd-Jones DM, Aggarwal B. Association of sleep characteristics with cardiovascular health among women and differences by race/ethnicity and menopausal status: findings from the American Heart Association Go Red for Women Strategically Focused Research Network. Sleep Health. 2019;5:501–8.
Kaar JL, Luberto CM, Campbell KA, Huffman JC. Sleep, health behaviors, and behavioral interventions: reducing the risk of cardiovascular disease in adults. World J Cardiol. 2017;9:396.
Huang T, Mariani S, Redline S. Sleep irregularity and risk of cardiovascular events: the multi-ethnic study of atherosclerosis. J Am Coll Cardiol. 2020;75:991–9.
Lao XQ, Liu X, Deng H-B, Chan T-C, Ho KF, Wang F, et al. Sleep quality, sleep duration, and the risk of coronary heart disease: a prospective cohort study with 60,586 adults. J Clin Sleep Med. 2018;14:109–17.
Tao F, Cao Z, Jiang Y, Fan N, Xu F, Yang H, et al. Associations of sleep duration and quality with incident cardiovascular disease, cancer, and mortality: a prospective cohort study of 407,500 UK biobank participants. Sleep Med. 2021;81:401–9.
Zuraikat FM, Makarem N, Redline S, Aggarwal B, Jelic S, St-Onge M-P. Sleep regularity and cardiometabolic heath: is variability in sleep patterns a risk factor for excess adiposity and glycemic dysregulation? Curr Diab Rep. 2020;20:1–9.
Kim JH, Hayek SS, Ko Y-A, Liu C, Tahhan AS, Ali S, et al. Sleep duration and mortality in patients with coronary artery disease. Am J Cardiol. 2019;123:874–81.
Domínguez F, Fuster V, Fernández-Alvira JM, Fernández-Friera L, López-Melgar B, Blanco-Rojo R, et al. Association of sleep duration and quality with subclinical atherosclerosis. J Am Coll Cardiol. 2019;73:134–44.
Zuraikat FM, Makarem N, Liao M, St-Onge M, Aggarwal B. Measures of poor sleep quality are associated with higher energy intake and poor diet quality in a diverse sample of women from the Go Red for Women Strategically Focused Research Network. J Am Heart Assoc. 2020;9:e014587.
St-Onge M-P, Zuraikat FM. Reciprocal roles of sleep and diet in cardiovascular health: a review of recent evidence and a potential mechanism. Curr Atheroscler Rep. 2019;21:1–9.
Al Khatib HK, Harding SV, Darzi J, Pot GK. The effects of partial sleep deprivation on energy balance: a systematic review and meta-analysis. Eur J Clin Nutr. 2017;71:614–24.
Godos J, Grosso G, Castellano S, Galvano F, Caraci F, Ferri R. Association between diet and sleep quality: a systematic review. Sleep Med Rev. 2021;57:101430.
Atoui S, Chevance G, Romain A-J, Kingsbury C, Lachance J-P, Bernard P. Daily associations between sleep and physical activity: a systematic review and meta-analysis. Sleep Med Rev. 2021;57:101426.
Zhu G, Catt M, Cassidy S, Birch-Machin M, Trenell M, Hiden H, et al. Objective sleep assessment in >80,000 UK mid-life adults: associations with sociodemographic characteristics, physical activity and caffeine. PLoS ONE. 2019;14:e0226220.
Cox RC, Olatunji BO. Sleep in the anxiety-related disorders: a meta-analysis of subjective and objective research. Sleep Med Rev. 2020;51:101282.
Steptoe A, Kivimäki M. Stress and cardiovascular disease. Nat Rev Cardiol. 2012;9:360–70.
Dar T, Radfar A, Abohashem S, Pitman RK, Tawakol A, Osborne MT. Psychosocial stress and cardiovascular disease. Curr Treat Options Cardiovasc Med. 2019;21:23.
Hamer M, Kivimaki M, Stamatakis E, Batty GD. Psychological distress as a risk factor for death from cerebrovascular disease. CMAJ. 2012;184:1461–6.
Hamer M, Molloy GJ, Stamatakis E. Psychological distress as a risk factor for cardiovascular events. Pathophysiological and Behavioral Mechanisms. J Am Coll Cardiol. 2008;52:2156–62.
Rosengren A, Hawken S, Ôunpuu S, Sliwa PK, Zubaid M, Almahmeed WA, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11,119 cases and 13 648 controls from 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:953–62.
Kivimäki M, Steptoe A. Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol. 2018;15:215–29.
An K, Salyer J, Brown RE, Kao HFS, Starkweather A, Shim I. Salivary biomarkers of chronic psychosocial stress and CVD risks: a systematic review. Biol Res Nurs. 2016;18:241–63.
Nef HM, Möllmann H, Akashi YJ, Hamm CW. Mechanisms of stress (Takotsubo) cardiomyopathy. Nat Rev Cardiol. 2010;7:187–93.
Brotman DJ, Golden SH, Wittstein IS. The cardiovascular toll of stress. Lancet. 2007;370:1089–100.
Silverman MN, Sternberg EM. Glucocorticoid regulation of inflammation and its functional correlates: from HPA axis to glucocorticoid receptor dysfunction. Ann N Y Acad Sci. 2012;1261:55–63.
Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci USA. 2012;109:5995–9.
Strike PC, Magid K, Whitehead DL, Brydon L, Bhattacharyya MR, Steptoe A. Pathophysiological processes underlying emotional triggering of acute cardiac events. Proc Natl Acad Sci U S A. 2006;103:4322–7.
Chinnaiyan KM. Role of stress management for cardiovascular disease prevention. Curr Opin Cardiol. 2019;34:531–5.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2016;37:2315–81.
Isasi CR, Parrinello CM, Jung MM, Carnethon MR, Birnbaum-Weitzman O, Espinoza RA, et al. Psychosocial stress is associated with obesity and diet quality in Hispanic/Latino adults. Ann Epidemiol. 2015;25:84–9.
Khaled K, Tsofliou F, Hundley V, Helmreich R, Almilaji O. Perceived stress and diet quality in women of reproductive age: a systematic review and meta-analysis. Nutr J. 2020;19:92.
De Vriendt T, Clays E, Huybrechts I, De Bourdeaudhuij I, Moreno LA, Patterson E, et al. European adolescents’ level of perceived stress is inversely related to their diet quality: The Healthy Lifestyle in Europe by Nutrition in Adolescence Study. Br J Nutr. 2012;108:371–80.
Michels N, Man T, Vinck B, Verbeyst L. Dietary changes and its psychosocial moderators during the university examination period. Eur J Nutr. 2020;59:273–86.
Schweren LJS, Larsson H, Vinke PC, Li L, Kvalvik LG, Arias-Vasquez A, et al. Diet quality, stress and common mental health problems: a cohort study of 121,008 adults. Clin Nutr. 2021;40:901–6.
Mouchacca J, Abbott GR, Ball K. Associations between psychological stress, eating, physical activity, sedentary behaviours and body weight among women: a longitudinal study. BMC Public Health. 2013;13:828.
Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sport Med. 2014;44:81–121.
Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. 2008;1141:105–30.
Brady KT, Sonne SC. The role of stress in alcohol use, alcoholism treatment, and relapse. Alcohol Res Health. 1999;23:263–71.
Anthenelli RM. Overview: stress and alcohol use disorders revisited. Alcohol Res Health. 2012;34:387–90.
Torres OV, O’Dell LE. Stress is a principal factor that promotes tobacco use in females. Prog Neuropsychopharmacol Biol Psychiatry. 2016;65:260–8.
Lo Martire V, Caruso D, Palagini L, Zoccoli G, Bastianini S. Stress & sleep: a relationship lasting a lifetime. Neurosci Biobehav Rev. 2020;117:65–77.
Kalmbach DA, Anderson JR, Drake CL. The impact of stress on sleep: pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J Sleep Res. 2018;27:e12710.
Åkerstedt T. Psychosocial stress and impaired sleep. Scand J Work Environ Health. 2006;32:493–501.
Kim E-J, Dimsdale JE. The effect of psychosocial stress on sleep: a review of polysomnographic evidence. Behav Sleep Med. 2007;5:256–78.
Geiker NRW, Astrup A, Hjorth MF, Sjödin A, Pijls L, Markus CR. Does stress influence sleep patterns, food intake, weight gain, abdominal obesity and weight loss interventions and vice versa? Obes Rev. 2018;19:81–97.
Sothmann MS, Buckworth J, Claytor RP, Cox RHE, White-Welkley J, Dishman RK. Exercise training and the cross-stressor adaptation hypothesis. Exerc Sport Sci Rev. 1996;24:267–88.
Hamer M. Psychosocial stress and cardiovascular disease risk: the role of physical activity. Psychosom Med. 2012;74:896–903.
Aldana SG, Sutton LD, Jacobson BH, Quirk MG. Relationships between leisure time physical activity and perceived stress. Percept Mot Skills. 1996;82:315–21.
McEwen BS, Karatsoreos IN. Sleep deprivation and circadian disruption: stress, allostasis, and allostatic load. Sleep Med Clin. 2015;10:1–10.
Glanz K, Schwartz MD. Stress, coping, and health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: theory, research, and practice. Jossey-Bass; 2008. pp. 211–36.
Johnson BT, Scott-Sheldon LAJ, Carey MP. Meta-synthesis of health behavior change meta-analyses. Am J Public Health. 2010;100:2193–8.
Murawski B, Wade L, Plotnikoff RC, Lubans DR, Duncan MJ. A systematic review and meta-analysis of cognitive and behavioral interventions to improve sleep health in adults without sleep disorders. Sleep Med Rev. 2018;40:160–9.
Fulwiler C, Brewer JA, Sinnott S, Loucks EB. Mindfulness-based interventions for weight loss and CVD risk management. Curr Cardiovasc Risk Rep. 2015;9:46.
Mason AE, Epel ES, Kristeller J, Moran PJ, Dallman M, Lustig RH, et al. Effects of a mindfulness-based intervention on mindful eating, sweets consumption, and fasting glucose levels in obese adults: data from the SHINE randomized controlled trial. J Behav Med. 2016;39:201–13.
Salmoirago-Blotcher E, Hunsinger M, Morgan L, Fischer D, Carmody J. Mindfulness-based stress reduction and change in health-related behaviors. J Evid Based Complementary Altern Med. 2013;18:243–7.
Christaki E, Kokkinos A, Costarelli V, Alexopoulos EC, Chrousos GP, Darviri C. Stress management can facilitate weight loss in Greek overweight and obese women: a pilot study. J Hum Nutr Diet. 2013;26(Suppl. 1):132–9.
Cox TL, Krukowski R, Love SRJ, Eddings K, DiCarlo M, Chang JY, et al. Stress management-augmented behavioral weight loss intervention for African American women: a pilot, randomized controlled trial. Health Educ Behav. 2013;40:78–87.
Rigotti NA. Treatment of tobacco use and dependence. N Engl J Med. 2002;346:506–12.
Tang YY, Tang R, Posner MI. Brief meditation training induces smoking reduction. Proc Natl Acad Sci U S A. 2013;110:13971–5.
Davis JM, Fleming MF, Bonus KA, Baker TB. A pilot study on mindfulness based stress reduction for smokers. BMC Complement Altern Med. 2007;7:2.
Cropley M, Ussher M, Charitou E. Acute effects of a guided relaxation routine (body scan) on tobacco withdrawal symptoms and cravings in abstinent smokers. Addiction. 2007;102:989–93.
Chen TL, Chang SC, Hsieh HF, Huang CY, Chuang JH, Wang HH. Effects of mindfulness-based stress reduction on sleep quality and mental health for insomnia patients: a meta-analysis. J Psychosom Res. 2020;135: 110144.
Kim SM, Park JM, Seo HJ. Effects of mindfulness-based stress reduction for adults with sleep disturbance: a protocol for an update of a systematic review and meta-analysis. Syst Rev. 2016;5:51.
Moen P, Kelly EL, Tranby E, Huang Q. Changing work, changing health: can real work-time flexibility promote health behaviors and well-being? J Health Soc Behav. 2011;52:404–29.
Download references
Author information
Penny M. Kris-Etherton and Philip A. Sapp contributed equally to the writing of this paper.
Authors and Affiliations
Department of Nutritional Sciences, The Pennsylvania State University, 319 Chandlee Lab, University Park, PA, 16802, USA
Penny M. Kris-Etherton, Philip A. Sapp, Terrance M. Riley, Kristin M. Davis, Tricia Hart & Olivia Lawler
Department of Biobehavioral Health, The Pennsylvania State University, University Park, PA, 16802, USA
Kristin M. Davis
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Penny M. Kris-Etherton .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Nutrition .
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Kris-Etherton, P.M., Sapp, P.A., Riley, T.M. et al. The Dynamic Interplay of Healthy Lifestyle Behaviors for Cardiovascular Health. Curr Atheroscler Rep 24 , 969–980 (2022). https://doi.org/10.1007/s11883-022-01068-w
Download citation
Accepted : 16 August 2022
Published : 24 November 2022
Issue Date : December 2022
DOI : https://doi.org/10.1007/s11883-022-01068-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Healthy dietary pattern
- Physical activity
- Healthy weight
- Quality sleep
- Stress management
- Cardiovascular health
- Find a journal
- Publish with us
- Track your research
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Entering Medicine as a Physician and a Patient
- 1 Department of Dermatology, Boston University, Boston, Massachusetts
On Sunday, April 19, 2020, I died. My now wife, Emma, woke up to me seizing at 7 am . I was an otherwise healthy, active medical student entering my fourth year of medical school, preparing to apply to residency. She woke up to my gasps, rolled me on my side to try to clear the vomit from my mouth, and with limited medical background yet recognizing my agonal breathing, rolled me to my back, called 911, and started CPR. Seven minutes later, the paramedics arrived. Panicked and unable to let the paramedics into our Boston brownstone 4 stories below, she implored the operator to have them break down the door. They wouldn’t. She left my lifeless body, ran down 4 flights, let the paramedics in, and by the time they arrived at the scene, I was pulseless. They moved my large, 6-ft 4-in frame to the kitchen floor and attempted resuscitation. After 45 minutes, they achieved a pulse, transitioned me to the elevator and into an ambulance, and ushered Emma into a police cruiser to ride to the hospital, stopping twice on the mile-and-a-half drive to restart CPR. By the time we arrived at the hospital, they would not allow Emma in. It was the height of the COVID-19 pandemic, and after all, who was she and how did she know me? We had only been living together for the larger part of the last 6 years. My mom flew in from Chicago that afternoon, and they made an exception to let her see me in case it was the last time she would see her son alive.
Read More About
Gibson FT. Entering Medicine as a Physician and a Patient. JAMA Neurol. Published online April 15, 2024. doi:10.1001/jamaneurol.2024.0804
Manage citations:
© 2024
Artificial Intelligence Resource Center
Neurology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- The Cass review: an...
The Cass review: an opportunity to unite behind evidence informed care in gender medicine
- Related content
- Peer review
- Kamran Abbasi , editor in chief
- kabbasi{at}bmj.com
- Follow Kamran on Twitter @KamranAbbasi
At the heart of Hilary Cass’s review of gender identity services in the NHS is a concern for the welfare of “children and young people” (doi: 10.1136/bmj.q820 ). 1 Her stated ambition is to ensure that those experiencing gender dysphoria receive a high standard of care. This will be disputed, of course, by people and lobbying groups angered by her recommendations, but it is a theme running through the review. Cass, a past president of the UK’s Royal College of Paediatrics and Child Health, seeks to provide better care for children and adolescents on one of the defining issues of our age. Her conclusion is alarming for anybody who genuinely cares for child welfare: gender medicine is “built on shaky foundations” (doi: 10.1136/bmj.q814 ). 2
That verdict is supported by a series of review papers published in Archives of Disease in Childhood , a journal published by BMJ and the Royal College of Paediatrics and Child Health (doi: 10.1136/archdischild-2023-326669 doi: 10.1136/archdischild-2023-326670 doi: 10.1136/archdischild-2023-326499 doi: 10.1136/archdischild-2023-326500 ). 3 4 5 6 The evidence base for interventions in gender medicine is threadbare, whichever research question you wish to consider—from social transition to hormone treatment.
For example, of more than 100 studies examining the role of puberty blockers and hormone treatment for gender transition only two were of passable quality. To be clear, intervention studies—particularly of drug and surgical interventions—should include an appropriate control group, ideally be randomised, ensure concealment of treatment allocation (although open label studies are sometimes acceptable), and be designed to evaluate relevant outcomes with adequate follow-up.
One emerging criticism of the Cass review is that it set the methodological bar too high for research to be included in its analysis and discarded too many studies on the basis of quality. In fact, the reality is different: studies in gender medicine fall woefully short in terms of methodological rigour; the methodological bar for gender medicine studies was set too low, generating research findings that are therefore hard to interpret. The methodological quality of research matters because a drug efficacy study in humans with an inappropriate or no control group is a potential breach of research ethics. Offering treatments without an adequate understanding of benefits and harms is unethical. All of this matters even more when the treatments are not trivial; puberty blockers and hormone therapies are major, life altering interventions. Yet this inconclusive and unacceptable evidence base was used to inform influential clinical guidelines, such as those of the World Professional Association for Transgender Health (WPATH), which themselves were cascaded into the development of subsequent guidelines internationally (doi: 10.1136/bmj.q794 ). 7
The Cass review attempted to work with the Gender Identity Development Service (GIDS) and the NHS adult gender services to “fill some of the gaps in follow-up data for the approximately 9000 young people who have been through GIDS to develop a stronger evidence base.” However, despite encouragement from NHS England, “the necessary cooperation was not forthcoming.” Professionals withholding data from a national inquiry seems hard to imagine, but it is what happened.
A spiralling interventionist approach, in the context of an evidence void, amounted to overmedicalising care for vulnerable young people. A too narrow focus on gender dysphoria, says Cass, neglected other presenting features and failed to provide a holistic model of care. Gender care became superspecialised when a more general, multidisciplinary approach was required. In a broader sense, this failure is indicative of a societal failure in child and adolescent health (doi: 10.1136/bmj.q802 doi: 10.1136/bmj-2022-073448 ). 8 9 The review’s recommendations, which include confining prescription of puberty blockers and hormonal treatments to a research setting (doi: 10.1136/bmj.q660 ), now place the NHS firmly in line with emerging practice internationally, such as in Scandinavia (doi: 10.1136/bmj.p553 ). 10 11
Cass proposes a future model of regional multidisciplinary centres that provide better access and, importantly, standardised care for gender dysphoria, including a smoother transition between adolescent and adult services. Staff will need training. All children and young people embarking on a care pathway will be included in research to begin to rectify the problems with the evidence base, with long term outcomes being an important area of focus. An already stretched workforce will need to extend itself further (doi: 10.1136/bmj.q795 doi: 10.1136/bmj-2024-079474 ). 12 13 In the meantime, some children and young people will turn to the private sector or online providers to meet their needs. The dangers in this moment of service transition are apparent.
But it’s also a moment of opportunity. Families, carers, advocates, and clinicians—acting in the best interests of children and adolescents—face a clear choice whether to allow the Cass review to deepen division or use it as a driver of better care. The message from the evidence reviews in Archives of Disease in Childhood is as unequivocal as it could be. Cass’s review is independent and listened to people with lived experience. Without doubt, the advocacy and clinical practice for medical treatment of gender dysphoria had moved ahead of the evidence—a recipe for harm.
People who are gender non-conforming experience stigmatisation, marginalisation, and harassment in every society. They are vulnerable, particularly during childhood and adolescence. The best way to support them, however, is not with advocacy and activism based on substandard evidence. The Cass review is an opportunity to pause, recalibrate, and place evidence informed care at the heart of gender medicine. It is an opportunity not to be missed for the sake of the health of children and young people. It is an opportunity for unity.
- Mitchell A ,
- Langton T ,
- Heathcote C ,
- Hewitt CE ,
- Hardiman L ,
- Wilkinson E
- Dixon-Woods M ,
- Summers C ,
- climate change

America’s Young Farmers Are Burning Out. I Quit, Too

I n 2023, Scott Chang-Fleeman—a young farmer like me—put down his shovel. A post on his Instagram read, “Shao Shan Farm, in its current form, is going on indefinite hiatus.” From the outside, the burgeoning farm had the makeup of one that could stand the test of time. In reality, his experience of farm ownership was wrought with challenges.
A farmer in his late 20s, Chang-Fleeman started Shao Shan Farm in 2019 to reconnect with his roots and provide a source of locally grown heritage Asian vegetables to the Bay Area. He quickly secured a clientele and fan base—two of the greatest hurdles of starting a farm—and became the go-to for San Francisco’s high-end Asian eateries.
But after four years of creative pivots to withstand unexpected hurdles that included financial stress, severe drought, and a global pandemic, Chang-Fleeman made a choice that many young farmers are considering: to leave farming behind. Why he left and what could have kept him on the land are critical questions we must address if we are to have a sustainable and food-secure future.
The USDA Census of Agriculture reported that in 2017, nearly 1 in 4 of the 3.4 million agricultural producers in the US were new and beginning farmers. Many of these new farmers are doing exactly what it seems American agriculture needs: starting small farms. According to the most recent data from the Agricultural Resource Management Survey (ARMS) in 2019 , farms with annual sales of less than $100,000 accounted for about 85% of all U.S. farms. And though not all of these small-scale farms are necessarily organic, small farms are more likely to grow a diversity of crop types, use methods that reduce negative impacts on the climate, increase carbon sequestration, and tend to be more resilient in the face of climate change.
Read More: How Extreme Weather Is Affecting Small Farmers Across the U.S.
There has been a growing interest among younger people in recent years in sustainable and organic farming practices, as well as in local food systems. This interest has led people in their 20s and 30s to enter into small-scale farming, particularly in niche markets such as organic produce, specialty crops, and direct-to-consumer sales.
As a result, both congressional Democrats and Republicans have maintained that encouraging young people to farm is of utmost importance in ensuring the stability of our food system. But getting young people into farming may not be the problem. Keeping them on the farm may be the hardest part.
I should know. I quit too.

Chang-Fleeman got his start in agriculture right out of college, where he spent several years working at the on-campus farm. As a third-generation Chinese American, he noticed a distinct lack of Asian vegetables at local farmers markets, particularly those that were grown organically, and suspected there would be a demand should a supply exist. He started trialing some varieties, and his suspicions were quickly affirmed when samples of his choy sum caught the attention of chef Brandon Jew of Mister Jiu’s, a contemporary Chinese eatery with a Michelin star in the heart of San Francisco’s Chinatown. Jew provided some seed funds for what was to become Shao Shan Farm in 2019.
During the first year running his farm, Chang-Fleeman focused his sales on his relationships with local restaurants, while attending some farmers' markets sales to supplement income. But when the COVID-19 pandemic hit in early 2020, he lost all of his restaurant accounts overnight.
Like many farmers at that time, he pivoted to a CSA model, offering farm boxes that provide a household with an assortment of vegetables for the week.
“So literally over a night, I reworked my crop plan” he told me. “Just to get through that year, or through that season, not knowing how long [the pandemic was going to] last.”
As if a global pandemic wasn’t enough, in 2021, California entered a drought, and he lost the ability to irrigate his crops come mid-summer, which meant a hard stop for production.
“I was hoping to hit some sort of a rhythm, and every year felt a bit like starting from scratch,” Chang-Fleeman reflected.
Throughout farm ownership, he worked side jobs to compensate for the slow build of business income and the fact that he could only afford to pay himself a monthly salary of $2,000. He regularly worked 90 hours a week. At the same time, farm expenses were on the rise.
“The cost of our packaging went up like three times in one year and the cost of the produce didn't change,” he explained. “Our operating expenses went up like 30%, after COVID.”
In four short years, Chang-Fleeman experienced an avalanche of extenuating circumstances that would bring most farm businesses to their knees. But the thing that finally catalyzed the closing of his business was burnout. He relayed the experience of the exhaustion and stress building over time until he reached a breaking point. “If I don’t stop now, it’s going to kill me,” he recalled thinking.
Chang-Fleeman’s burnout reminded me of my own story. In the fall of 2018, I took what ended up being a two-month medical leave from an organic farm I managed in Northern California in order to try to try to resolve a set of weird symptoms that included dizzy spells and heart palpitations. If you know anything about farming, fall is not the time to be absent. It’s peak harvest time and the culmination of all of your work is underway. But as my medical anomaly continued to worsen, I came no closer to getting back to work. After many doctor visits, several trips to the specialist, a flurry of blood tests, and a week of heart monitoring, it took one Xanax to solve the mystery.
Read More: ‘ They’re Trying to Wipe Us Off the Map.’ Small American Farmers Are Nearing Extinction
The prolonged physical stress that I had been harboring at work had triggered the onset of panic disorder, a nervous system affliction that had led me into a near-chronic state of fight or flight mode, causing a swath of physical symptoms not typically associated with “anxiety.”
For me, this was a wake-up call. I turned to a slew of Western and naturopathic remedies to alleviate my symptoms, but ultimately, removing the stressors of farm management was the thing that allowed me to, mostly, reach a nervous system balance. Even still, six years later, I’m constantly navigating the ‘new normal’ of this diagnosis.
A pilot study conducted by agriculture researcher Josie Rudolphi and her colleagues in 2020 found that of 170 participants, approximately 71% met the criteria for Generalized Anxiety Disorder. By comparison, in the US, an estimated 18% of adults experience an anxiety disorder. Rudolphi’s work indicates that these disorders maybe three times more prevalent in young farmer and rancher populations.
This rang true as I went from farm to farm trying to figure out what so often goes wrong in a new farm operation. Again and again mental health was a through-line. Collette Walsh, owner of a cut-flower operation in Braddock, PA, put it to me bluntly: "I usually get to a point in late August or early September, where there’s a week where I just cry.”
How can we build a farming economy that helps young farmers not only stay, but also thrive on the land? The Farm Bill , a federal package of legislation that provides funding for agricultural programs, is one route. As the reboot of the Farm Bill approaches, it’s a critical time to ask these questions and advocate for policies that support young farmers and the barriers they’re facing in maintaining a long-lasting career in agriculture.
Take for instance, Jac Wypler, Farmer Mental Health Director at the National Young Farmer Coalition (Young Farmers), who oversees the Northeast region’s Farmer and Rancher Stress Assistance Network (FRSAN). The organization was established by the Farm Bill in 2018 to develop a service provider network for farmers, ranchers, and other agricultural workers that was dedicated to mental well-being. Through the network of service providers she directs, called “Cultivemos,” Wypler and her colleagues utilize a multi-tiered approach to address mental health in farming spaces. Cultivemos partners provide direct support in moments of stress and crisis as well as peer-to-peer support spaces.
An expanded (and subsidized) program that scales efforts like Cultivemos to a size commensurate with the young work force is clearly needed. But it’s only part of the picture.
“While we believe that it is important to make sure that farms, farmers, and farmworkers are getting direct support around their mental health,” Wypler explained. “We need to alleviate what is causing them stress.”
Cultivemos works to address the structural root causes of stress which can include climate change, land prices, and systemic racism, to name a few. They focus on communities that are disproportionately harmed by these structural root causes, specifically Black, Indigenous, and other farmers of color. Finally, they seek to make this impact by regranting funding directly into the hands of these farmers.
“The way I think of regranting is that the USDA and these large institutions are the Mississippi River of funding.” Wypler says. “We’re trying to get the funding into these smaller rivers and tributaries to disperse these funds and shift that power dynamic and leadership dynamic.”
The next Farm Bill cycle will be critical in ensuring this work is continued. In November of 2023, lawmakers signed a stopgap funding bill that allows for a one-year extension on the 2018 Farm Bill. Lawmakers are currently in deliberations over the bill until September when it will be up for a vote. Young Farmers underscores the importance of the appropriations process, which is when program areas that are authorized in the farm bill are allocated funding.

Back-to-the-landism has waxed and waned throughout the last hundred years, booming in the pre-Depression years of the 1930s, dying in the war years and then storming back in the 60s and 70s. When my generation’s own farming revolution came along in the early 2000s, I was similarly swept up. I imagined when I chose to farm that the path would be lifelong. What I hadn’t accounted for, as a determined, starry-eyed changemaker, was the toll that a decade of farming through wildfires, evacuations, floods, power outages, and a global pandemic would take on my mental health.
Don’t get me wrong: I was happy working hard with my two feet planted firmly on the land. In a better world I and people like Scott Chang-Fleeman would have kept getting our hands dirty, making an honest, if modest, living providing good and wholesome food in synch with the rhythms of the planet.
But to borrow a word from the world of ecology, being a young farmer in today’s economy is “unsustainable.” The numbers don’t work economically and, eventually, any mind trying to square this un-squarable circle is going to break. The economic, physical and mental challenges are all interconnected.
It’s hard to find an American, Republican or Democrat, red or blue state resident that doesn’t want more young hands on the land. We all rightly see agriculture as a pathway to personal fulfillment and a way to make our food supply healthier and more secure. But words and intentions can only do so much. We must answer these very real problems with very real subsidy.
If we don’t, my generation might be the last to think of going “back-to-the-land” as something actually worth doing.
More Must-Reads From TIME
- The 100 Most Influential People of 2024
- The Revolution of Yulia Navalnaya
- 6 Compliments That Land Every Time
- Stop Looking for Your Forever Home
- If You're Dating Right Now , You're Brave: Column
- The AI That Could Heal a Divided Internet
- Fallout Is a Brilliant Model for the Future of Video Game Adaptations
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]

Upcoming information sessions from the School of Medicine
If you’re looking to explore graduate programs in healthcare at Case Western Reserve University, the School of Medicine is hosting information sessions to help you identify opportunities, answer questions and apply.
Virtual Open House: Master of Science in Clinical Research
Join a virtual open house to learn more about the Master of Science in Clinical Research program. This session will be hosted by the Department of Population and Quantitative Health Sciences. Through this program, students are encouraged to pose thought-provoking questions and employ cutting-edge methods to tackle the most complex challenges in clinical research.
This virtual session will take place on Sunday, April 21, 7:30-8:30 p.m.
Virtual Open House: Master of Public Health
Attend a brief presentation followed by a Q&A session to learn more about the Master of Public Health program.
This program guarantees a thorough understanding of various public health methodologies, combined with hands-on practical experiences. Students will have the flexibility to tailor their education by choosing from five concentrations or many dual degree options. The on-site program offers the possibility of completion in as little as 16 to 21 months.
Master of Science in Regenerative Medicine and Entrepreneurship: Student Perspectives
Join this webinar featuring a panel of students in the Master of Science in Regenerative Medicine and Entrepreneurship program. Searching for, applying to and choosing a graduate program can be a daunting task. Sometimes, it is more helpful to hear from current students who once went through the same process.
This virtual session will take place on Tuesday, April 23, 3:30 to 4 p.m.
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- March Madness
- AP Top 25 Poll
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
An NPR editor who wrote a critical essay on the company has resigned after being suspended
FILE - The headquarters for National Public Radio (NPR) stands on North Capitol Street on April 15, 2013, in Washington. A National Public Radio editor who wrote an essay criticizing his employer for promoting liberal reviews resigned on Wednesday, April 17, 2024, a day after it was revealed that he had been suspended. (AP Photo/Charles Dharapak, File)

- Copy Link copied
NEW YORK (AP) — A National Public Radio editor who wrote an essay criticizing his employer for promoting liberal views resigned on Wednesday, attacking NPR’s new CEO on the way out.
Uri Berliner, a senior editor on NPR’s business desk, posted his resignation letter on X, formerly Twitter, a day after it was revealed that he had been suspended for five days for violating company rules about outside work done without permission.
“I cannot work in a newsroom where I am disparaged by a new CEO whose divisive views confirm the very problems” written about in his essay, Berliner said in his resignation letter.
Katherine Maher, a former tech executive appointed in January as NPR’s chief executive, has been criticized by conservative activists for social media messages that disparaged former President Donald Trump. The messages predated her hiring at NPR.
NPR’s public relations chief said the organization does not comment on individual personnel matters.
The suspension and subsequent resignation highlight the delicate balance that many U.S. news organizations and their editorial employees face. On one hand, as journalists striving to produce unbiased news, they’re not supposed to comment on contentious public issues; on the other, many journalists consider it their duty to critique their own organizations’ approaches to journalism when needed.
In his essay , written for the online Free Press site, Berliner said NPR is dominated by liberals and no longer has an open-minded spirit. He traced the change to coverage of Trump’s presidency.
“There’s an unspoken consensus about the stories we should pursue and how they should be framed,” he wrote. “It’s frictionless — one story after another about instances of supposed racism, transphobia, signs of the climate apocalypse, Israel doing something bad and the dire threat of Republican policies. It’s almost like an assembly line.”
He said he’d brought up his concerns internally and no changes had been made, making him “a visible wrong-thinker at a place I love.”
In the essay’s wake, NPR top editorial executive, Edith Chapin, said leadership strongly disagreed with Berliner’s assessment of the outlet’s journalism and the way it went about its work.
It’s not clear what Berliner was referring to when he talked about disparagement by Maher. In a lengthy memo to staff members last week, she wrote: “Asking a question about whether we’re living up to our mission should always be fair game: after all, journalism is nothing if not hard questions. Questioning whether our people are serving their mission with integrity, based on little more than the recognition of their identity, is profoundly disrespectful, hurtful and demeaning.”
Conservative activist Christopher Rufo revealed some of Maher’s past tweets after the essay was published. In one tweet, dated January 2018, Maher wrote that “Donald Trump is a racist.” A post just before the 2020 election pictured her in a Biden campaign hat.
In response, an NPR spokeswoman said Maher, years before she joined the radio network, was exercising her right to express herself. She is not involved in editorial decisions at NPR, the network said.
The issue is an example of what can happen when business executives, instead of journalists, are appointed to roles overseeing news organizations: they find themselves scrutinized for signs of bias in ways they hadn’t been before. Recently, NBC Universal News Group Chairman Cesar Conde has been criticized for service on paid corporate boards.
Maher is the former head of the Wikimedia Foundation. NPR’s own story about the 40-year-old executive’s appointment in January noted that she “has never worked directly in journalism or at a news organization.”
In his resignation letter, Berliner said that he did not support any efforts to strip NPR of public funding. “I respect the integrity of my colleagues and wish for NPR to thrive and do important journalism,” he wrote.
David Bauder writes about media for The Associated Press. Follow him at http://twitter.com/dbauder


Taco Relish
15+ Household Items We Didn't Realize Need To Be Tossed
Posted: April 10, 2024 | Last updated: April 11, 2024

Over the years, homes can become filled with items that no longer serve any purpose. Piles of papers, unworn clothes, and tasteless spices are harmless, but a waste of space. Conversely, aged pillows, old air filters, and tattered towels can compromise the overall hygiene of your home. From appliance manuals to expired medicine, you may be surprised how many household items are waiting to be thrown out.
Do you know how often you should be replacing your pillows? Keep reading to see a list of things it may be time to toss.
Old Papers Need To Get Shredded
From old receipts to childhood birthday cards, papers can pile up over the years. Before you know it, there's a stack of papers pouring out of every cabinet, closet, and drawer in the office.
Be sure to carve out some time every so often to go through old documents and shred ones that are no longer necessary. For sentimental items, consider cutting out any handwritten messages and condensing them in a scrapbook or a collage.

Expired Medicine Is Easy To Forget About
We all have that shelf in the house that's riddled with leftover flu and allergy medicine that got crammed into the back corner and forgotten about. By the time you needed it again, you forgot you even had it an bought an entirely new box.
By now, you might have several medications that are either in a deteriorating package or are unidentifiable, separated from its original box. Before you go offering someone a Tylenol from 1989, go through your medication and toss the questionable ones out!

Old Spices Lose Their Taste
Spices can get a little pricey, so you want to hold on to them as long as possible. For those of us who don't cook often, we may have a few spices we rely on every day, and several others in the back that we never touch.
For those ones in the back, you may want to give them a whiff. Generally speaking, spices don't become dangerous to consume. However, they do lose their taste, at which point they serve no other purpose than taking up space in the cabinet.

Unworn Clothing Can Be Donated
As your fashion evolves, you may find yourself holding on to items that you haven't worn in half a decade. When going through your closet, it can be easy to think you'll wear something, only to go another year without touching it.
As a rule of thumb, try to get rid of any clothes you haven't worn in six months. This way, you can't use the excuse that it just isn't warm or cold enough yet. Donate gently used articles of clothing and toss the rest.

Recycle Old Technology
With new technological devices coming out faster than ever, you may be wondering what to do with your old cell phones, laptops, monitors, and more. If your junk drawer is full of floppy disks and MP3 players, it's time to recycle some old devices.
From a ball of old earphones that you'll never untangle to dinosaur computers, you'll be surprised all the items an e-waste recycling program will accept. A simple Google search will bring up locations near you.

Appliance Manuals Aren't Needed
Remember the good-old-days of having to watch a DVD-- or worse, read!-- in order to understand how a device worked? Even after going through the manual, you'd hold on to it just in case that feared day came that you didn't know how to do something.
These days, there are tons of tutorials to show you how to do just about anything online. Worst comes to worst, it doesn't take much to look up an appliance company and get their technical support hotline.
Takeout Menus Are Pointless
While takeout menus served a purpose once upon a time, these days they are perhaps the most pointless item in your home. Whether you grabbed one from a restaurant on your way out or received one in the mail, we promise you'll have nothing to lose throwing it out.
Just about every restaurant has a website these days, and if it doesn't, you may want to second-guess going there. Websites are complete with everything from the location and phone number to the menu items.

Pillows Don't Last More Than A Few Years
It's no surprise that pillows collect oil and sweat. So, why is it that many of us had no idea that you can throw an entire pillow in the washing machine? While many are machine-safe, some do need to be hand-washed.
Either way, pillows should be cleaned every six months, at least. Even those who take the utmost care of their high-quality pillows will need to replace them after a few years since they lose their support over time.

You Need A New Toothbrush Every Few Months
Some of us can't even remember the last time we bought a new toothbrush. Yet, dentists generally recommend getting a new one every three to four months! That's because the bristles can lose their effectiveness over time and begin to harbor bacteria.
If your toothbrush looks like something you'd use to scrub the grime off of pots and pans, it's well past the time to get a new one. For automated toothbrushes, just be sure to replace the head every few months.

Expired Condiments Can Make A Sticky Mess
Condiments are sneaky because they often last for years, making it easy to forget about them. Just think of that bottle of soy sauce that's been in your fridge door for the past three years.
From A1 to hot sauce, there are plenty of condiments that last long but are used rarely. These lightly-used sauces somehow find a way to leak out of the bottle and become a sticky mess, so be sure to check their dates and toss them when necessary.

Planners And Calendars Aren't Necessary
Some of us are still holding on to the days before smartphones held all of our important information. From contact books to calendars and planners, these clutter-makers are a waste of space and paper.
If you must have things handwritten, at least be sure to get rid of the calendars and planners from yesteryear. We love cute kitten calendars as much as the next animal-lover, but they don't count as sentimental photos worth holding on to.

Wire Hangers Don't Support Clothes Well
Wire hangers have lost popularity in recent years, if for no other reason than the epic scene in Mommy Dearest . In all seriousness, they are flimsy when it comes to heavy garments like coats.
Conversely, when it comes to lighter articles of clothing like t-shirts, wire hangers leave lines in the clothes that can linger throughout the day. For this reason, many turn to wooden or plastic hangers as a more practical and sturdier alternative.

Old Costumes Don't Come In Handy
Halloween can be a blast, but it does require you to purchase or make a costume you'll probably never wear again. After all, your costume loses its impressiveness the minute someone recognizes it as the same thing you wore last year.
Then there are the costumes you wore at a theme party or in your high school play. These outfits are often cheaply made with the full knowledge that they will likely be worn once. Donate them.
If You Don't Enjoy Cooking, Nix The Cookbooks
Whether it caught your eye at a bookstore or was a White Elephant gift, many of us have ended up with a cookbook we've hardly opened. By the time they make it to your kitchen, their only purpose is to remind you of the recipes you'll probably never cook.
If your cookbooks have collected dust over the years because you don't actually like cooking, it may be time to get honest about who you are. There's no shame in donating or re-gifting something you have no real desire to use.
Old Towels Can Harbor Bacteria
Towels can appear to be in decent shape, but their smell can give them away. Over time, their fibers can start to harbor bacteria that not even the washing machine will remove. If your towel has a musty smell after just one use, it may be time to replace it.
To be sure, try washing the towel once with vinegar and again with detergent. If you still can't get more than a singlr use or two out of it, it's time for some new towels.

Old Sponges Don't Clean Items
It seems counterintuitive that a soapy sponge could be adding bacteria to an item, but that's precisely what happens when you don't replace them. After a couple of weeks, sponges become full of bacteria.
As you wash the counter or dishes, the sponge releases this bacteria. While antibacterial soap can combat the dirty sponge to some extent, it becomes counterproductive. For a more sanitary clean, use bleach to sanitize your sponges and replace them every couple of weeks.
Let Someone Else Read The Books You Won't Reread
Some of us are quite nostalgic about books, and there's nothing wrong with that. However, if most of the books on your shelves are those you know you won't reread, it may be time to donate them.
With all the time and effort that goes into making books, they deserve to be read. Keep the books you refer back to often or think you'd enjoy rereading. As for all the rest, give them away to a library or someone who may enjoy them.

Lingering Keys Probably Don't Unlock Anything
If you've ever found a key lying around in a drawer somewhere, you may have had that feeling deep down that you better hang on to it just in case. But what exactly is the "case" you're waiting for?
By the time you've forgotten what the key was for, odds are you've already gotten rid of the lock. Maybe it was an old mailbox or a spare key to a former home. Regardless, you're better off recycling it than holding on to a pointless piece of metal.
More for You
Ukraine May Have Just Crossed Putin's Nuclear Red Line
The Best Met Gala Entrances, from Lady Gaga to Rihanna
Your senses will shut down in a specific order when you’re about to die
Road closures as rail line bridge work begins
Paedophiles to lose parental rights under new law
Rory McIlroy's LIV Golf fears come true as Masters viewing figures paint grim picture
Kawhi Leonard going viral after underwhelming response to receiving his Olympic jersey
Popular California Pizza Chain Announces Sudden Closure of 27 Locations
I’m an Average Middle-Class Retiree: Here’s How Much Savings I Have
The Coolest Car From the Year You Were Born (1945-1995)
Your Blood Type Affects Your Risk of Early Stroke, Scientists Discover
Netanyahu says 9 chilling words as Iran's president vows to completely destroy Israel
Nobel-winning molecular biologist on the consequences of aging
Sailor Moon's New Photo Release Reveals Cast in Full Costume for Show Debut
Costco’s New Comfort Food Meal Kit Is a Total Treasure
‘The Ministry of Ungentlemanly Warfare' Review: Henry Cavill and Alan Ritchson in Guy Ritchie's Slapdash Tale of WWII Derring-Do
Peanuts by Charles Schulz
Republicans Suddenly Cancel Multiple Bills
Average US annual salary by age revealed – see how you compare
Parents sue California for 'misleading' branding of parental notification policy on November ballot: report

Food as Medicine
The healing potential of food.
Food as medicine, is the prioritization of diet and nutrition (what we eat) as an important part of treating and preventing some chronic diseases. The fact that diet, healthy or otherwise, can impact an individual’s health is well-documented and acknowledged. Improvements in diet quality, like adding nutrient dense, fiber-rich foods, may reduce disease symptoms and improve quality of life. For lifestyle medicine clinicians, this is a crucial part of their therapeutic approach.
ACLM supports the use of evidence-based food as medicine interventions by health care professionals in clinical settings. We offer training in the form of CME/CE online courses and live events as well as downloadable kits, tools, and resources that help clinicians actively apply all six pillars of lifestyle medicine.

ACLM’s dietary position statement: For the treatment, reversal and prevention of lifestyle-related chronic disease, ACLM recommends an eating plan based predominantly on a variety of minimally processed vegetables, fruits, whole grains, legumes, nuts and seeds.
Connecting healthcare professionals to the training and evidence they need to:
Empower patients to restore their own health, regain passion for their career and the field of medicine, treat & reverse the chronic cycle of lifestyle-related illnesses, food as medicine training for clinicians.
There is an urgent need to raise the level of competency in food as medicine for all health care professionals. Healthful eating patterns not only impact disease progression but encourage overall well-being, influencing a patient’s success in other lifestyle pillars. It just so happens that this dietary lifestyle pattern is also what is best for the planet.
ACLM is pleased to offer a breadth of CME/CE educational courses, research, tools and resources to support health professionals and patients in their journey to use food as medicine.
Remission of Type 2 Diabetes and Reversal of Insulin Resistance
Remission of Type 2 Diabetes After Treatment With a High-Fiber, Low-Fat, Plant-Predominant Diet Intervention: A Case Series
Food As Medicine: A Calorie Density Approach to Weight Loss
Food As Medicine: Preconception, Pregnancy, and Postpartum

Lifestyle Medicine and Foods as Medicine Essentials

Nutrition | Core Competencies
Food As Medicine: Nutrition for Treatment and Risk Reduction
Food As Medicine: Nutrition for Prevention and Longevity
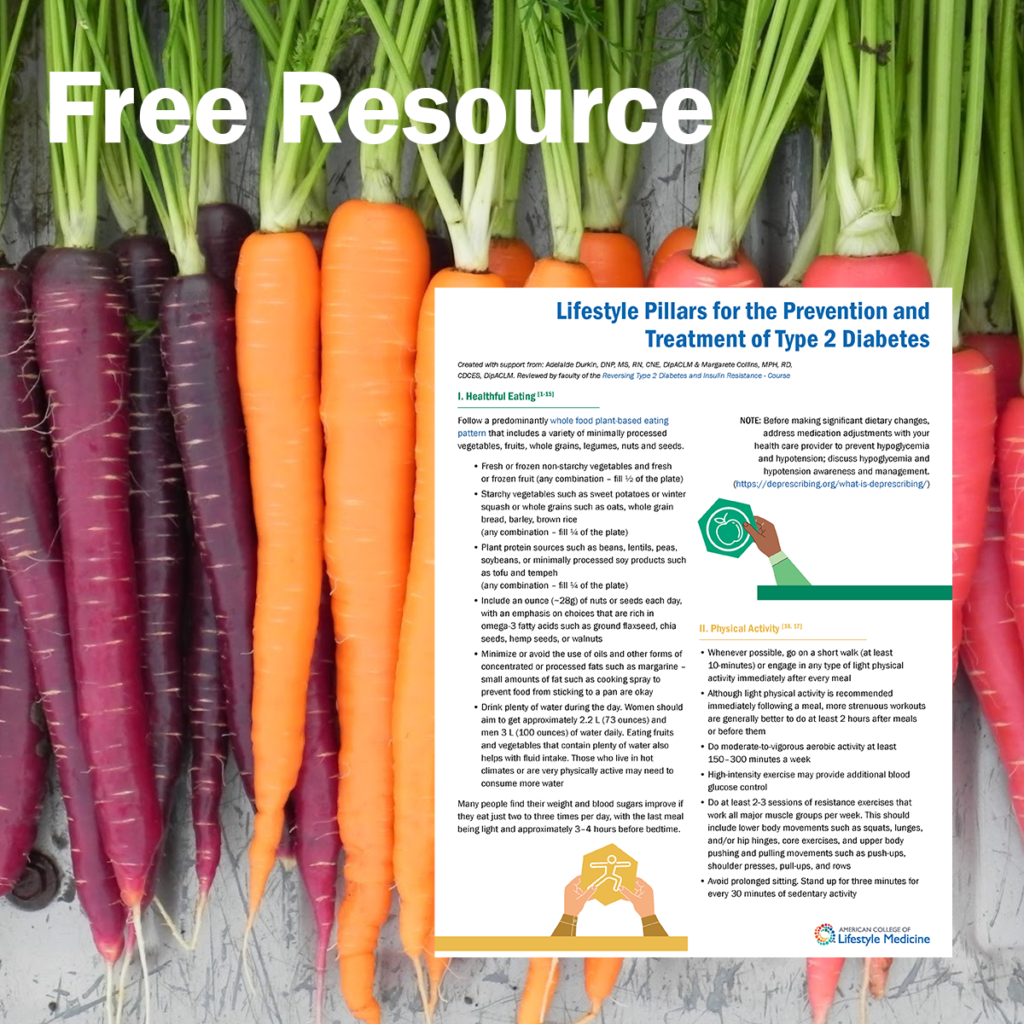
By providing your email address, you agree to future communications. Upon submission, you will be sent to a new page where we offer you a complimentary download of a useful practice tool and patient education handout. This two-page pdf provides practical tips on all 6 lifestyle medicine pillars to help with the prevention and treatment of food-related conditions.
Clinical Practice Guidelines
A recently published meta-epidemiological study from ACLM ( published in Advances in Nutrition ) synthesizes recommendations from 78 clinical practice guidelines for major chronic conditions and general health promotion.
“… These findings support both ACLM’s dietary position statement and its recent expert consensus statement that the most effective dietary intervention for achieving T2D remission is whole, plant-based foods with minimal consumption of meat and other animal products…”
Expert Consensus Statement
“Dietary Interventions to Treat Type 2 Diabetes in Adults with a Goal of Remission”
Expert consensus was achieved for 69 statements pertaining to diet and remission of T2D, dietary specifics and types of diets, adjuvant and alternative interventions, support, monitoring, adherence to therapy, weight loss, and payment and policy. Clinicians can use these statements to improve quality of care, inform policy and protocols, and identify areas of uncertainty.
Nutrition and Family Practice
In a 22-article supplement to the Journal of Family Practice introducing the field and implementation of lifestyle medicine to family medicine physicians, two articles focused on nutrition: “Nutrition and Disease Prevention” with first author Michelle E. Hauser, MD, MS, MPA, FACP, FACLM, DipABLM; and “An Approach to Nutritional Counseling” with author Thomas M. Campbell, MD, DipABOM.
Read more about the evidence supporting the use of a whole-food, plant-based eating pattern for optimal human health.

March Insider

Preventing non-traumatic amputations with lifestyle medicine

How to make food as medicine successful and sustainable

Hope and Healing: Type 2 Diabetes Remission with Lifestyle Medicine

Transforming Hospital Food From Bad to Healthy and Delicious

Patient Info on Polypharmacy Should Emphasize Lifestyle Behavior

Making the healthy choice the easy choice with lifestyle medicine
Type 2 Diabetes Remission is Possible Without Severe Calorie Restriction

FREE CURRICULUM
Providing healthcare professionals with a strong foundation in Culinary Medicine — including what constitutes a healthy diet and how to find, obtain, and prepare healthy and delicious food — is a key part of supporting patients in achieving better health outcomes and putting food as medicine into practice. Access this comprehensive, complimentary curriculum.
Food as Medicine Patient Resources
Tools and support to help patients use food as medicine are critical to patient success.
ACLM has compiled a number of downloadable print resources including our free Food as Medicine Jumpstart Guide and a Whole Food Plant Based Sample Menu Plan that contain delicious recipes, tips and advice that can be used to augment your food as medicine.
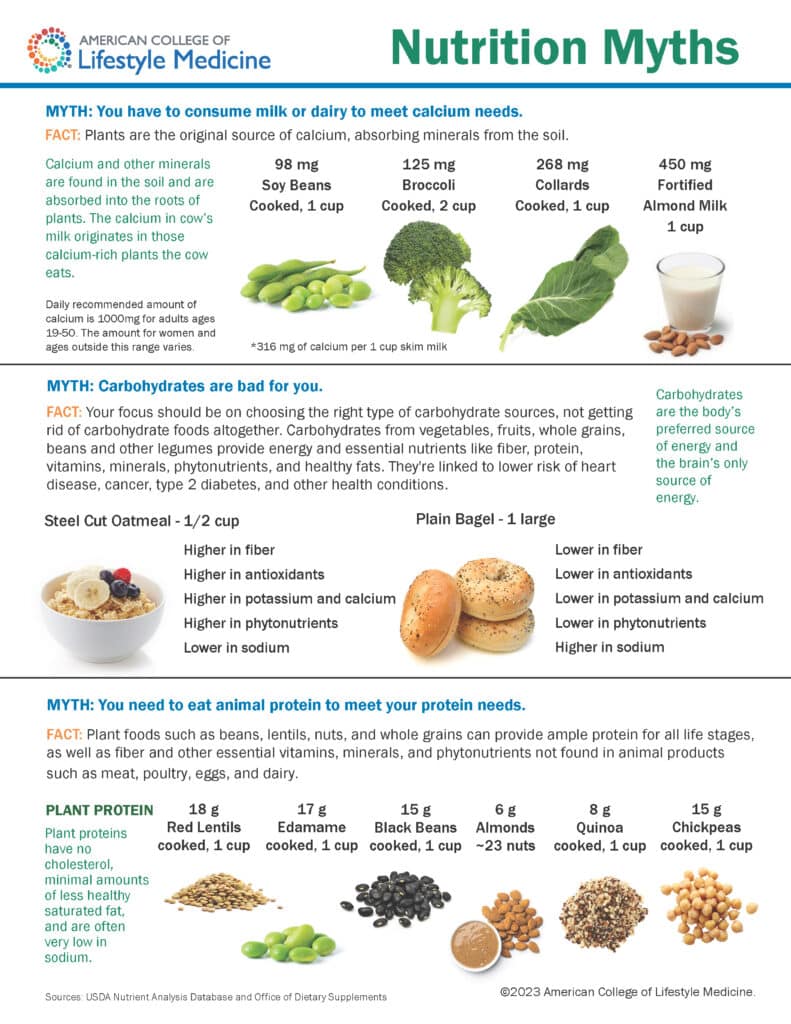
October 27 – 30, 2024 | Orlando & Online
Celebrating 20 years of Lifestyle Medicine
Every Fall, ACLM hosts the premier continuing education event focused on lifestyle medicine – the therapeutic dose of proper nutrition, regular physical activity, social connection, restorative sleep, stress management, and avoidance of risky substances.
- Manage Account
Taraji P. Henson Blown Away By ‘TIME’ 2024 Most Influential People List Honoree Fantasia: ‘The Sky’s The Limit’
The "Color Purple" star made the list alongside Jack Antonoff, Dua Lipa, Patrick Mahomes, 21 Savage, Kylie Minogue, Burna Boy and America Ferrara, among others.
By Gil Kaufman
Gil Kaufman
- Share this article on Facebook
- Share this article on Twitter
- Share this article on Flipboard
- Share this article on Pinit
- + additional share options added
- Share this article on Reddit
- Share this article on Linkedin
- Share this article on Whatsapp
- Share this article on Email
- Print this article
- Share this article on Comment
- Share this article on Tumblr

Taylor Swift Announces New Music Video With Cryptic Clip Full of 'Tortured Poets' Easter Eggs
See latest videos, charts and news
Fantasia Barrino
Taraji p. henson, trending on billboard.
“When I met her years later, I learned that she’s a Cancer — sweet and sensitive but with a quiet strength. You can feel it in her presence, and you can hear it in her powerful voice,” Henson added. “When she sings, she transcends. It’s like she goes somewhere else and you just have to go with her.”
Oscar nominee Henson called Fantasia “living testimony” that we are all going through our own personal “storms,” saying that after the tempest has tamed the sun comes out and “whatever comes next for her will be so beautiful. She deserves everything. I see such big things for Fantasia – the sky’s the limit. Well, beyond the sky for her. It’s her time.”
This year’s list features a number of other singers (cover star Dua Lipa honored by punk godmother Patti Smith), 21 Savage (by Burna Boy), Jack Antonoff (by Maren Morris), Kylie Minogue (by Coldplay’s Chris Martin), Leslie Odom Jr. (by Kate Hudson), Burna Boy (Angélique Kidjo) and James McBride (by Ethan Hawke).
Check out this year’s full list here .
Get weekly rundowns straight to your inbox
Want to know what everyone in the music business is talking about?
Get in the know on.
Billboard is a part of Penske Media Corporation. © 2024 Billboard Media, LLC. All Rights Reserved.
optional screen reader
Charts expand charts menu.
- Billboard Hot 100™
- Billboard 200™
- Hits Of The World™
- TikTok Billboard Top 50
- Song Breaker
- Year-End Charts
- Decade-End Charts
Music Expand music menu
- R&B/Hip-Hop
Culture Expand culture menu
Media expand media menu, business expand business menu.
- Business News
- Record Labels
- View All Pro
Pro Tools Expand pro-tools menu
- Songwriters & Producers
- Artist Index
- Royalty Calculator
- Market Watch
- Industry Events Calendar
Billboard Español Expand billboard-espanol menu
- Cultura y Entretenimiento
Honda Music Expand honda-music menu

IMAGES
VIDEO
COMMENTS
Lifestyle medicine has also become an international movement with the development of the Lifestyle Medicine Global Alliance. 26. In addition, a peer-reviewed academic journal has been established, the American Journal of Lifestyle Medicine, 27 to provide a forum for individuals interested in exchanging academic information in this growing field.
Lifestyle Medicine (LM) is a rapidly growing discipline that focuses on the role of lifestyle factors in preventing, managing, and reversing chronic disease. At this point in the field's evolution, there is strong evidence that the 6 pillars of LM—a whole-food, plant-predominant eating pattern, physical activity, restorative sleep, stress management, avoidance of risky substances, and ...
Fig 1. The three core principles in the practice of Lifestyle Medicine. Lifestyle medicine describes a medical discipline that is practised by clinicians of all backgrounds at a personal level within one-to-one consultations or small groups of patients. It is most effective with strong public health policies.
American Journal of Lifestyle Medicine (AJLM) is a peer-reviewed bi-monthly resource for practitioners seeking to incorporate lifestyle practices into clinical medicine. AJLM provides commentaries and research reviews on nutrition and diet, physical activity, behavior change, cardiovascular disease, obesity, anxiety and depression, sleep problems, metabolic disease, and more.
American Journal of Lifestyle Medicine Jan • Feb 2021 James M. Rippe, MD T he year 2021 marks the 15th anniversary of the publication of the American Journal of Lifestyle ... important papers in 2020. Chief among them is the article by past president of the ACLM Dr John Kelly along with Dr Micaela Karlsen (who also serves as the
The Importance of Lifestyle for Health and Longevity. The tenets of LM are based on several, groundbreaking large observational studies. First was The Adventist Mortality Study in 1960. Researchers studied Seventh-Day Adventists in Loma Linda, California. What they found over a 25-year follow up was astonishing.
Adopting Lifestyle Medicine Adoption Challenges to Adopting Lifestyle Medicine Advancing Lifestyle Medicine Adoption This brief will 1) evaluate the promise of, and need for, health equity; 2) explain what lifestyle medicine is and why it is high-value care; 3) share how provider organizations can deliver lifestyle medicine both through their own
6 pillars of Lifestyle Medicine. The American College of Lifestyle Medicine has established six key areas that impact everyone's overall health and goals:. 1. Nutrition: We've all heard it: "You are what you eat." And eating mostly plant-based foods, such as fruits, vegetables, beans, nuts, seeds, and whole grains, is the foundation of a healthy diet.
Lifestyle Medicine is an interdisciplinary journal providing a forum for those interested in the rapidly growing specialty of lifestyle medicine, publishing articles and reviews which focus on the clinical and scientific aspects of lifestyle medicine and its incorporation into clinical practice. Research published is of relevancy to cardiologists, epidemiologists, endocrinologists, allergists ...
Lifestyle medicine is a medical specialty that uses therapeutic lifestyle interventions as a primary modality to treat chronic conditions including, but not limited to, cardiovascular diseases, type 2 diabetes, and obesity. Lifestyle medicine certified clinicians are trained to apply evidence-based, whole-person, prescriptive lifestyle change ...
A healthy lifestyle is "a way of living that lowers the risk of being seriously ill or dying early." 7 Considering what contributes to a healthy lifestyle, this usually includes "activities and habits that encourage the development of total physical, mental, and spiritual fitness, and which reduces the risk of major illness." 9 Examples ...
The practice of lifestyle medicine is described and its powerful effect on these modern instigators of premature disability and death are described and the economic benefits of prevention-based lifestyle medicine are addressed. By ignoring the root causes of disease and neglecting to prioritize lifestyle measures for prevention, the medical community is placing people at harm. Advanced nations ...
This essay defined lifestyle medicine; discussed perceptions of the expert patient and self-management of chronic conditions (enhanced by peer support, motivational interviewing, and tailored lifestyle prescriptions); and considered power imbalances within and between patients and healthcare professionals. ...
Lifestyle Medicine is an interdisciplinary journal focusing on the clinical and scientific aspects of lifestyle medicine and its incorporation into clinical practice. Abstract Introduction Despite the increasing popularity of social media, little research has been conducted on its impact on lifestyle behaviors and health outcomes among adults.
Lifestyle Medicine is the name that is being used by a growing global, grass-roots clinician and patient movement that aims to use good quality evidence for what lifestyle changes improve health (improvements in diet, physical activity, sleep, social connection, stress and reduction in alcohol and smoking cessation) with tried and tested ...
Lifestyle Medicine Performance Measures: Kelly JH, Lianov L, Shurney D, et al. Lifestyle Medicine Performance Measures: An Expert Consensus Statement Defining Metrics to Identify Remission or Long-Term Progress Following Lifestyle Medicine Treatment. American Journal of Lifestyle Medicine. 2024:15598276241230237. Link to Journal.
The 6 pillars of lifestyle medicine have strong scientific backing and plenty of supportive evidence to validate their integration into routine clinical practice. However, two barriers stand in the way of their widespread adoption: the system of healthcare and the culture of medicine. This article describes changes necessary to overcome these ...
Purpose of Review The recent rise in cardiovascular disease (CVD) deaths in the USA has sparked interest in identifying and implementing effective strategies to reverse this trend. Healthy lifestyle behaviors (i.e., healthy diet, regular physical activity, achieve and maintain a healthy weight, avoid tobacco exposure, good quality sleep, avoiding and managing stress) are the cornerstone for ...
How that will impact their life—at home, at work, with family, socially, how they sleep, and so on. Being able to care for others as a physician is a unique privilege. It is a rare circumstance to meet a stranger and to wholly trust them from the first interaction with something as sacred as your health.
The Cass review: an opportunity to unite behind evidence informed care in gender medicine. At the heart of Hilary Cass's review of gender identity services in the NHS is a concern for the welfare of "children and young people" (doi: 10.1136/bmj.q820 ). 1 Her stated ambition is to ensure that those experiencing gender dysphoria receive a ...
I n 2023, Scott Chang-Fleeman—a young farmer like me—put down his shovel. A post on his Instagram read, "Shao Shan Farm, in its current form, is going on indefinite hiatus.". From the ...
Master of Science in Regenerative Medicine and Entrepreneurship: Student Perspectives. Join this webinar featuring a panel of students in the Master of Science in Regenerative Medicine and Entrepreneurship program. Searching for, applying to and choosing a graduate program can be a daunting task.
Updated 9:27 AM PDT, April 17, 2024. NEW YORK (AP) — A National Public Radio editor who wrote an essay criticizing his employer for promoting liberal views resigned on Wednesday, a day after it was revealed that he had been suspended. Uri Berliner, a senior editor on NPR's business desk, posted his resignation letter on X, formerly Twitter.
Over the years, homes can become filled with items that no longer serve any purpose. Piles of papers, unworn clothes, and tasteless spices are harmless, but a waste of space. Conversely, aged ...
The Healing Potential of Food. Food as medicine, is the prioritization of diet and nutrition (what we eat) as an important part of treating and preventing some chronic diseases. The fact that diet, healthy or otherwise, can impact an individual's health is well-documented and acknowledged. Improvements in diet quality, like adding nutrient ...
That explains why in her essay celebrating Fantasia for TIME magazine's 2024 list of the 100 Most Influential People in the World Golden Globe-winning actress (and fellow 100 honoree) Taraji P ...
Lifestyle Medicine: From Challenges to Opportunities. "The dedication and perseverance of the healthcare workers during the pandemic challenges, through stress and burnout, inspired both hope and unity in the face of adversity.". It is our distinct honor and pleasure to serve as guest editors for this special issue of the American Journal ...