An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List


Coping With Racism: A Selective Review of the Literature and a Theoretical and Methodological Critique
Elizabeth brondolo , ph.d., nisha brady , m.a., melissa pencille, danielle beatty , ph.d., richard j contrada.
- Author information
- Article notes
- Copyright and License information
Issue date 2009 Feb.
Racism is a stressor that contributes to racial/ethnic disparities in mental and physical health and to variations in these outcomes within racial and ethnic minority groups. The aim of this paper is to identify and discuss key issues in the study of individual-level strategies for coping with interpersonal racism. We begin with a discussion of the ways in which racism acts as a stressor and requires the mobilization of coping resources. Next, we examine available models for describing and conceptualizing strategies for coping with racism. Third, we discuss three major forms of coping: racial identity development, social support seeking and anger suppression and expression. We examine empirical support for the role of these coping strategies in buffering the impact of racism on specific health-related outcomes, including mental health (i.e., specifically, self-reported psychological distress and depressive symptoms), self-reported physical health, resting blood pressure levels, and cardiovascular reactivity to stressors. Careful examination of the effectiveness of individual-level coping strategies can guide future interventions on both the individual and community levels.
Racism is a stressor that contributes to racial/ethnic disparities in mental and physical health and to variations in health outcomes within racial and ethnic minority groups ( Anderson 1989 ; Clark et al. 1999 ; Mays et al. 2007 ; Paradies 2006 ; Williams and Williams-Morris 2000 ). Racism, in particular, self-reported ethnic or racial discrimination is a highly prevalent phenomenon. Members of most ethnic or racial minority groups report exposure over the course of their lifetime, and recent research indicates that episodes of ethnicity-related maltreatment occur on a weekly basis for some groups (Brondolo et al. 2009). The evidence points consistently to a relationship between self-reported racism and mental health impairments, specifically negative mood and depressive symptoms ( Brondolo et al. 2008 ; Kessler Mickelson and Williams 1999 ; Paradies 2006 ). Some evidence has linked self-reported racism to hypertension and a more consistent body of evidence has linked racism to risk factors for hypertension and/or coronary heart disease ( Brondolo et al. 2003 , 2008 ; Harrell et al. 2003 ; Lewis et al. 2006 ; Peters 2004 ; Steffen and Bowden 2006 ). Racism has also been linked to several other health conditions ( Paradies 2006 ), and to perceived health, which is itself a predictor of all-cause mortality ( Borrell et al. 2007 ; Jackson et al. 1996 ; Schulz et al. 2006 ).
Since racism persists within the US, it is critical to identify the strategies individuals use to cope with this stressor and to evaluate the effectiveness of these strategies. As noted by Fischer & Shaw (1999) , in 1996 the National Advisory Mental Health Council highlighted the importance of investigating individual-level factors that buffer the health effects of discrimination ( Fischer and Shaw 1999 ). Although the knowledge base has grown since 1996, there is an ongoing need for greater understanding of the ways in which individuals can mitigate the health risks associated with racial/ethnic discrimination.
The aim of this paper is to identify and discuss key issues in the study of individual-level strategies for coping with interpersonal racism. It is important to note that we do not intend this review to communicate the idea that the burden of coping with racism should be placed on the shoulders of targeted individuals alone. Eliminating racism and the effects of racism on health will require interventions at all levels: from the individual to the family, community, and nation. Nonetheless, careful examination of the effectiveness of individual-level coping strategies is needed to guide future interventions at both the individual and other levels.
We begin with a discussion of the ways in which racism acts as a stressor and requires the mobilization of coping resources. Next, we examine available models for describing and conceptualizing strategies for coping with racism. Third, we discuss three major approaches to coping: racial identity development, social support seeking, and anger suppression and expression. These coping approaches have received sufficient research attention to permit a systematic review of evidence regarding their effectiveness for both mental and physical health outcomes. In addition, these coping approaches are intuitively plausible as potential buffers of the effects of racism on health, and if shown to be effective, would lend themselves to skills and information-based intervention approaches. We examine empirical support for the role of these coping approaches in buffering the impact of racism on mental health-related outcomes (i.e., specifically, self-reported psychological distress and depressive symptoms), self-reported physical health, resting blood pressure levels, and cardiovascular reactivity to stressors. These outcomes were chosen because they have been among those most consistently identified as correlates of racism ( Paradies 2006 ). Finally, we discuss theoretical and methodological issues that are important to consider when conducting and evaluating research on strategies for coping with racism. Although much of the research on coping with racism has focused on African American samples, we have included the available data on other groups, including individuals of Asian and Latino(a) descent as well.
Definitions
Clark et al. (1999 , p. 805) define racism as “the beliefs, attitudes, institutional arrangements, and acts that tend to denigrate individuals or groups because of phenotypic characteristics or ethnic group affiliation”. Contrada and others (2000, 2001) use the more general term ethnic discrimination to refer to unfair treatment received because of one’s ethnicity, where “ethnicity” refers to various grouping of individuals based on race or culture of origin. We consider racism a special form of social ostracism in which phenotypic or cultural characteristics are used to assign individuals to an outcast status, rendering them targets of social exclusion, harassment, and unfair treatment.
Racism exists at multiple levels, including interpersonal, environmental, institutional, and cultural ( Harrell 2000 ; Jones 1997 , 2000 ; Krieger 1999 ). However, the bulk of empirical research on coping with racism focuses on strategies for coping with interpersonal racism. Interpersonal racism has been defined by Krieger as “directly perceived discriminatory interactions between individuals whether in their institutional roles or as public and private individuals” ( Krieger 1999 , p. 301). Racism may have deleterious effects even when the target does not consciously perceive the maltreatment or attribute it to racism. However, this review considers the effectiveness of individual-level coping strategies employed to address episodes of racism that are both directly experienced and perceived. This focus on an interpersonal approach to examining racism is consistent with much recent work by Smith and colleagues examining the health effects of other psychosocial stressors (e.g., poverty) within an interpersonal context (see, for example, Gallo et al. 2006 ; Ruiz et al. 2006 ; Smith et al. 2003 ).
Types of ethnicity-related maltreatment
Racism/ethnic discrimination can encompass a wide range of acts including social exclusion, workplace discrimination, stigmatization, and physical threat and harassment ( Brondolo et al. 2005a ; Contrada et al. 2001 ). Social exclusion includes a variety of different interactions in which individuals are excluded from social interactions, rejected, or ignored because of their ethnicity or race. Stigmatization can include both verbal and non-verbal behavior directed at the targeted individual that communicates a message that demeans the targeted person (e.g., communicates the idea that the targeted individual must be lazy or stupid because he or she belongs to a particular racial or ethnic group). Workplace discrimination includes acts directed at individuals of a particular race or ethnicity that range from the expression of lowered expectations to a refusal to promote or hire. Threat and harassment can include potential or actual damage to an individual or his or her family or property because of ethnicity or race. Any of these discriminatory acts can be overt, such that the racial bias is made explicit (e.g., when accompanied by racial slurs), or the acts can be covert such that racial bias may not be directly stated but is implicit in the communication ( Taylor and Grundy 1996 ).
Racism as a stressor
A number of conceptual models, including those which consider racism within stress and coping frameworks, have described the ways that racism may confer risk for health impairment ( Anderson et al. 1989 ; Clark et al. 1999 ; Harrell et al. 1998 ; Krieger 1999 ; Mays et al. 2007 ; Outlaw 1993 ; Williams et al. 2003 ). In general, each model emphasizes the need to consider the acute effects of individual incidents of ethnicity-related maltreatment, as well as factors that sustain the damaging effects of these events. They highlight the importance of considering racism as a unique stressor, and as a factor that may interact with other potential race and non-race-related stressors, including low socioeconomic status and neighborhood crime. Racism itself and the environmental conditions associated with racism (e.g., neighborhood segregation) limit access to coping resources. The cumulative effects of acute and sustained stress exposure, combined with limited coping resources are likely to cause perturbations in neuroendocrine and autonomic systems that respond to acute stressors and that maintain or re-establish physiological homeostasis ( Gallo and Matthews 2003 ; McEwen and Lasley 2003 , 2007 ).
From the perspective of the targeted individual, racism is a complex stressor, requiring a range of different coping resources to manage both practical and emotional aspect of the stressor. Features of the racist incident, as well as the corresponding coping demands, may vary depending upon the physical, social, and temporal context of exposure. Targets must cope with the substance of racism, such as interpersonal conflict, blocked opportunities, and social exclusion. They must also manage the emotional consequences, including painful feelings of anger, nervousness, sadness, and hopelessness, and their physiological correlates. Targets may also need to manage their concerns about short and long term effects of racism on other members of their group, including their friends and family members. Indirect effects of racism (e.g., poverty, environmental toxin exposure, changes in family structure) may require additional coping efforts ( Mays et al. 1996 ). A theme that may cut across and link many or even most of the coping tasks posed by racism is the management of damage to self-concept and social identity ( Mellor 2004 ).
Episodes of ethnicity or race-based maltreatment can occur in a number of different venues. The effectiveness of the coping response may vary depending on the context in which the maltreatment occurs. Factors that may influence the choice and effectiveness of a coping strategy include variations in the intensity and nature of the threat, the perceived degree of intentionality of the perpetrator, the potential consequences of the act and of the coping response, the availability of resources to assist the target, and perceptions of the need to repeatedly muster different coping resources and the appraisal of one’s ability to do so ( Richeson and Shelton 2007 ; Scott 2004 ; Scott and House 2005 ; Swim et al. 2003 ).
Different types of coping may be needed at different points in time: in anticipation of potential exposure to ethnicity-related maltreatment, at the time of exposure, following the episode, and when considering longer term implications of persistent or recurring exposure. The strategies that are effective for quickly terminating a specific episode of maltreatment are not necessarily the same as those needed to manage the possibility of longer term exposure. A variety of coping strategies may be needed at each point.
Consequently, one of the most serious challenges facing minority group members is the need to develop a broad range of racism-related coping responses to permit them to respond to different types of situations and to adjust the response depending on factors that might influence the effectiveness of any particular coping strategy. Targets must also develop the cognitive flexibility to implement an appropriate and effective strategy in each of the wide range of situations in which they may be exposed to discrimination, judge the relative costs and benefits of these strategies, and deploy them as needed over prolonged periods of time. This level of coping flexibility is beneficial, but difficult to achieve ( Cheng 2003 ). The perception that one’s coping capacity is not adequate to meet the demands increases the likelihood that ethnicity-related maltreatment will be experienced as a chronic stressor.
Coping with racism: models and measures
There are a number of early models ( Allport 1954 ; Harrell 1979 ) of the different strategies individuals used to respond to racism that have been reviewed in Mellor (2004) . Some of the difficulties with these models are a function of more general problems with models of coping that have been well reviewed elsewhere ( Skinner et al. 2003 ). Other concerns are more specific to the difficulties of developing models for coping with racism.
Most models fail to explicitly incorporate strategies designed to manage the interpersonal conflict associated with ethnicity-related maltreatment as well as with its emotional sequelae. They do not always include strategies both for coping with an acute event (i.e., responding to the perpetrator during episodes of ethnicity-related maltreatment) and for coping with the awareness that race-related maltreatment is likely to be an ongoing stressor. Additionally, it can also be difficult to determine if the coping strategies included in the models are intended to address racism specifically or the various consequences of discrimination, such as unemployment, denial of a job promotion, or poverty.
More recent work has utilized dimensions of coping that are more explicitly tied to theories of stress and coping, including problem-focused coping, emotion-focused coping, approach versus avoidance coping, and social support ( Danoff-Burg et al. 2004 ; Scott 2004 ; Scott and House 2005 ; Thompson Sanders 2006 ). However, as Mellor (2004) points out, many of the strategies included in models of coping responses can only be loosely organized according to available rubrics for categorizing coping strategies. For example, it is unclear how to classify spirituality and Africultural coping, which appear to represent multifaceted strategies with some aspects involving problem-focused coping and others involving emotion-focused coping ( Constantine et al. 2002 ; Lewis-Coles and Constantine 2006 ; Utsey et al. 2000a ). There have been inconsistencies even within specific coping domains. For example, seeking social support when confronted by racism has been considered an approach coping strategy ( Scott 2004 ; Scott and House 2005 ; Thompson Sanders 2006 ), a problem-focused coping strategy ( Noh and Kaspar 2003 ; Plummer and Slane 1996 ), an emotion-focused strategy (such as when seeking emotional social support) ( Tull et al. 2005 ), an avoidance strategy (if it involves venting, but no direct confrontation), and a strategy in an entirely separate category ( Danoff-Burg et al. 2004 ; Swim et al. 2003 ; Utsey et al. 2000b ).
Mellor (2004) suggests an alternate framework for organizing racism-related coping that focuses on the function of the coping strategies versus the content of their focus. His model highlights the importance of distinguishing between tasks that serve to prevent personal injury (e.g., denial, acceptance) from those that are intended to remediate, prevent, or punish racism (e.g., assertiveness, aggressive retaliation). This functional approach may be an important step toward developing more effective models of coping with racism, particularly if the purpose is closely linked to the various specific challenges that face targets of discrimination.
Measurement issues
The development of more comprehensive models is further limited by the small number of instruments available to assess racism-related coping. The Perceived Racism Scale ( McNeilly et al. 1996 ) is one of the only instruments available to assess strategies for coping with racism. It is intended for use with African Americans and measures both exposure to experiences of ethnicity-related maltreatment and coping responses to the exposure. For each venue or domain in which racist events might occur (i.e., job-seeking, educational settings, the health-care system), participants are asked to indicate the cognitive, affective, and behavioral responses used to cope with each experience. Other researchers have used generic coping scales (e.g., the Ways of Coping or the Spielberger Anger Expression Inventory) and modified the presentation to inquire about coping in response to race-related maltreatment (e.g., Brondolo et al. 2005b ).
Each of these measures is subject to the limitations of traditional self-reported trait coping indices ( Lazarus 2000 ). It is difficult to evaluate the timing or circumstances in which the coping response is used. For example, when the Self-Report Coping Scale ( Causey and Dubow 1992 ) is applied to the study of racism-coping (e.g., Scott and House 2005 ), participants indicate the degree to which they use strategies such as externalizing (i.e., getting mad or throwing things) as a response to race-related stress. It is unclear if the item refers to expressing anger at the perpetrator of the racist acts (possibly a problem-focused or approach coping strategy) or discharging anger later when thinking about specific incidents (possibly an emotion-focused coping strategy).
Careful delineation of the timing and function of the coping strategy is valuable, because there may be some strategies that are effective in the short run, but counterproductive if used persistently over time. For example, “keeping it to myself” may be a safe strategy to use as an immediate course of action in a situation in which the target may face immediate retaliation, but may be deleterious once the acute maltreatment has ended. Similarly, there may be strategies that are effective and acceptable in some settings, but not others. Measures which include items assessing both immediate and longer term responses and inquire about the circumstances of exposure to maltreatment are needed.
How do people cope with racism?
There are no population-based epidemiological data on the strategies most commonly used to cope with episodes of ethnicity-related maltreatment at the time of the event. There are very limited population-based data on the strategies used to manage discrimination in general. In a population-based sample of over 4,000 Black and White men and women, participants were asked about the ways they handled episodes of racial discrimination ( Krieger and Sidney 1996 ). Most (69–78% depending on race and gender group) indicated they would “try to do something and talk to others.” Only 17–19% indicated that they would “accept it as a fact of life and talk to others.” Most individuals (86–97%) indicated that they would talk to others whether they took action in response to racism or accepted the racist behavior ( Krieger and Sidney 1996 ). In contrast to the tendency of Black and White Americans to indicate that they would try to do something about racism, other research suggests that Asian immigrants in Canada would prefer to “regard it as a fact of life, avoid it or ignore it” ( Noh et al. 1999 ). The ethnic and national differences in response suggest that the moderating effects of culture and immigration status on racism and coping must be further evaluated in larger ethnically diverse population-based studies.
Evaluating different coping approaches
In the next three sections, we review in detail the data on the effectiveness of three coping approaches that have been considered as responses to racism: racial identity development, social support seeking, and confrontation/anger coping. We restrict the reviews to published, peer-reviewed papers. For each topic area, studies for consideration were identified by accessing all major databases including PsychInfo, ERIC, MEDLINE, and Sociology Abstracts, using both ProQuest and EBSCO search engines. We included thesaurus terms racism, ethnic discrimination, racial discrimination, race discrimination, race-related stress . For a general review, we included the terms: coping, active coping, approach coping, stress-management . For the specific review on racial and ethnic identity, we included the terms: racial identity, ethnic identity, and racial socialization. For the section on social support, we included terms: support, social support, support coping, active coping, approach coping . For the section on anger, we included the terms: confrontation, anger, anger expression, anger suppression, anger management, anger-in, anger-out . We further searched the reference sections of each paper to identify additional studies. We also examined all published work of each author of each paper to determine if additional studies could be identified. Examining the empirical data on these three coping approaches highlights in specific detail some of the methodological issues involved in research investigating effective strategies for coping with racism.
Our evaluation of coping effectiveness focuses on stress-buffering effects. A coping response may be said to buffer stress when, among individuals exposed to the stressor, those who engage in that response (or who engage in it to a greater degree) are less likely to experience a negative outcome than those who do not (or who engage in it to a lesser degree). The relative benefit associated with performing the coping response should be smaller or not at all in evidence among those who are not exposed to the stressor. It should be noted that stress-buffering is not the only manner in which a coping response might confer an advantage. Other models are plausible, including mediational models that describe a causal chain in which exposure to stress promotes performance of the coping response which, in turn, promotes more positive outcomes. However, a focus on stress-buffering is warranted since the aim of the paper is to identify those strategies which might be effective in ameliorating the health effects of exposure to racism, and could form the basis of coping-based interventions. Figure 1 provides a graphical illustration of these different possible pathways.
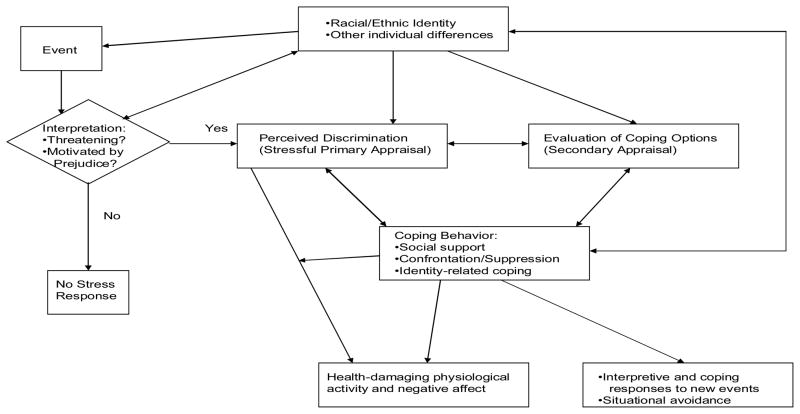
Different pathways through which coping approaches may offset the effects of racism on mental and physical health.
Racial/ethnic identity as a buffer of the effects of racism on distress
Based on Phinney (1990 , 1996) , Cokley (2007 , p. 225) defines ethnic identity as “the subjective sense of ethnic group membership that involves self-labeling, sense of belonging, preference for the group, positive evaluation of the ethnic group, ethnic knowledge, and involvement in ethnic group activities.” Similarly, racial identity has been defined as “a sense of group or collective identity based on one’s perception that he or she shares a common racial heritage with a particular racial group” ( Helms 1990 , p. 3). There are differences of opinion about the degree to which ethnic and racial identity represent distinct constructs ( Cross and Strauss 1998 ; Helms 1990 ; Phinney and Ong 2007 ). Definitions of both constructs include a focus on shared history, values, and a common heritage. However, those who advocate the study of racial identity as a separate construct suggest that it entails a complex developmental process, reflecting the individual’s attempts to resolve the problems associated with racism directed both at the individual and at the group as a whole.
How could racial or ethnic identity serve as a coping strategy?
Racial and ethnic identity are generally considered individual difference variables, (i.e., an underlying set of schemas that help individuals make sense of and respond to their experiences as a member of their ethnic or racial group) ( Cross and Strauss 1998 ; Helms 1990 ; Phinney and Ong 2007 ). However, researchers explicitly link the process of developing an ethnic identity to other acts that can have stress-buffering effects ( Phinney et al. 2001 ). Some research explicitly frames ethnic identity as a variable possessing characteristics similar to other potential coping responses, capable of buffering the effects of stress exposure (see for example, Lee 2003 ). Despite the ambiguity about the degree to which racial identity can be considered within the domain of coping resources, research on racial identity has a potential impact on public health. If racial identity is mutable, and aspects of racial identity are effective in modifying psychological or psychophysiological responses to racism, those aspects of identity could be incorporated into health communications and could guide racial socialization practices.
Racial/ethnic identity may serve as a coping mechanism in several different ways. Specifically, some aspects of racism may influence the salience of race-related maltreatment and affect the subsequent appraisals of and coping responses to these events ( Oyserman et al. 2003 , Quintana 2007 ). A well-developed racial identity may be associated with historical and experiential knowledge about one’s own group and its social position. In turn this knowledge may help a targeted individual distinguish between actions directed at the person as an individual versus those directed at the person as a member of a particular group ( Cross 2005 ). This can protect targeted individuals from injuries to self-esteem or distress when they are exposed to negative events that may be a function of ethnic discrimination rather than individual characteristics of behavior ( Branscombe et al. 1999 ; Mossakowski 2003 ; Sellers and Shelton 2003 ). Racial socialization could provide an individual with an opportunity to consider possible approaches to this maltreatment and could serve to expedite the implementation of coping responses ( Hughes et al. 2006 ). Ethnic connection and belonging could ameliorate some of the pain of ostracism from other groups.
Appreciating the potential benefits of a well-developed sense of ethnic or racial identity, investigators have generated a large body of research that has examined the nature of racial and ethnic identity, and a smaller body of research that has tested the hypothesis that a strong positive racial or ethnic identity might buffer the effects of racism on mental health/psychological distress. However, the findings to date have been conflicted and present a number of methodological problems that need resolution.
Our review identified 12 published peer-reviewed papers that explicitly tested the hypothesis that ethnic or racial identity buffers the effects of exposure to racism on psychological distress or depression ( Banks and KohnWood 2007 ; Bynum et al. 2007 ; Fischer and Shaw 1999 ; Greene et al. 2006 ; Lee 2003 , 2005 ; Mossakowski 2003 ; Noh et al. 1999 ; Sellers et al. 2003 , 2006 ; Sellers and Shelton 2003 ; Wong et al. 2003 ). Details of the studies, including the samples, measures, and results, are presented in Table 1 . The effects of ethnic identity as a buffer of the relationship of racism to depressive symptoms or psychological distress were tested in samples of African Americans, Filipinos, Koreans, South Asian Indians, and Latino(a)s, with most, but not all, studies employing samples of convenience.
Studies of the buffering effects of racial identity on the relationship of racism to mental physical health indices
Note. AA = African American; MH = mental health; sx = symptoms; discrim. = discrimination; EI = ethnic identity. MIBI = Multidimensional Inventory of Black Identity ( Sellers, Smith, Shelton, Rowley, & Chavous, 1998 ). RaLES Daily Exper. = Daily Life Experiences subscale from the Racism and Life Experience Scales ( Harrell, 1997 ). CES-D = Center for Epidemiological Studies Depression Scale ( Radloff, 1977 ). TERS = Teenager Experience with Racial Socialization Scale ( Stevenson et al., 2002 ). BSI = Brief Symptom Inventory ( Deragotis & Melisarotis, 1983 ). PSS = Perceived Stress Scale ( Cohen & Williamson, 1988 ). RaLES-R - Brief Racism Scale = Brief Racism Scale from the Racism and Life Experiences Scales-Revised ( Harrell, 1997a , 1997b ). SORS-A = Scale of Racial Socialization for Adolescents ( Stevenson, 1994 ). SRE = Schedule of Racist Events ( Landrine & Klonoff, 1996 ). MHI = Mental Health Inventory ( Veit & Ware, 1983 ). MEIM = Multigroup Ethnic Identity Measure ( Phinney, 1992 ); EI = ethnic identity. PDS = Perceived Personal Ethnic Discrimination ( Finch et al., 2000 ). SCL-90 = Symptom Checklist – 90 – Revised ( Deragotis, 1994 ). DLE = Daily Life Experience subscale of the Racism and Life Experience scales ( Harrell, 1994 ). STAI = State–Trait Anxiety Inventory ( Spielberger, 1983 ).
For each main effect tested, the component of racial identity evaluated is listed. The results are categorized as follows: (NO) = No significant main effect; (YES-POS) = Significant main effect such that increasing scores on listed components of racial identity are associated with lower symptom reports; (YES-NEG) = Significant main effects such that increasing scores on listed components of racial identity are associated with greater symptom reports.
For each interaction action tested, the variables are presented as follows: measure of racial identity/measure of racism/measure of depressive symptoms or distress. The results are categorized as follows: (NO) = No significant interaction (buffering) effect; (YES-I) = Significant interaction effect, such that the relationship of racism to symptoms is stronger for those with high scores on listed components of racial identity; (YES-B) = Significant interaction effect, such that the relationship of racism to symptoms is weaker for those with high scores on listed components of racial identity. In this case, racial identity serves as a buffer.
These studies assessed different aspects of ethnic or racial identity and used several different strategies for measuring these dimensions. Some investigators used measures of pride or belonging, including the Multi-Ethnic Identity Measure (MEIM; Phinney 1992 ) or the private regard subscale of the Multidimensional Inventory of Black Identity (MIBI; Sellers et al. 1997 ). Other investigations included measures of racial centrality, a construct involving the degree to which one’s race or ethnicity forms an important part of self-concept ( Sellers et al. 1997 ). Still other studies included aspects of racial identity that refer to the development of preparation for discrimination, including measures of racial socialization. Three studies ( Greene et al. 2006 ; Sellers et al. 2003 ; Wong et al. 2003 ) used longitudinal designs to examine the degree to which racial identity buffers racism-related changes in depression. The remainder used cross sectional, correlational designs. In all the studies, participants completed measures of racial identity, perceived racism and a measure of depression or psychological distress. To test the buffering effects of racial identity, all researchers directly examined the statistical interactions of racial identity and racism on measures of distress, with the exception of those who used path analytic models ( Sellers et al. 2003 ).
These studies provide only very limited evidence for the hypothesis that racial or ethnic identity buffers the effects of racism on psychological distress. Of the 12 studies specifically examining effects of racism on distress or depression, only two found evidence of a buffering effect of racial identity on at least one measure of distress ( Fischer and Shaw 1999 ; Mossakowski 2003 ). One study was a population-based study investigating these issues in Filipino-American adults ( Mossakowski 2003 ). In this study, ethnic identity acted as a buffer only for the predictive effects of a single item measure of discrimination on depressive symptoms. Ethnic identity did not appear to buffer the effects of everyday maltreatment on depressive symptoms. The other study reporting buffering effects on depressive symptoms was a study of African American young adults ( Fischer and Shaw 1999 ). Six studies ( Bynum et al. 2007 ; Fischer and Shaw 1999 ; Lee 2003 , 2005 ; Sellers et al. 2003 ; Wong et al. 2003 ) reported no buffering effects for either distress or depression. Four studies found some evidence that an aspect of ethnic identity (i.e., pride; Lee 2005 ); public regard ( Sellers et al. 2006 ); commitment/centrality ( Noh et al. 1999 ) or positive attitudes towards other cultures ( Banks and Kohn-Wood 2007 ) may intensify the relationship of racism to distress. 1
In contrast, positive main effects of racial identity on distress were obtained in several studies examining dimensions related to ethnic pride or attachment (e.g., positive attachment to one’s ethnic group (i.e., including the MEIM; Phinney 1992 ), the private regard component of the MIBI or the cultural pride dimension of racial socialization or connection to ethnic group) ( Bynum et al. 2007 ; Lee 2005 ; Mossakowski 2003 ; Sellers et al. 2006 ; Wong et al. 2003 ). However, some studies obtained null ( Fischer and Shaw 1999 ; Lee 2003 ; Noh et al. 1999 ; Wong et al. 2003 ) or reverse effects ( Bynum et al. 2007 ). The effects for dimensions such as centrality were more mixed, with some studies reporting that greater racial centrality was associated with less negative mood ( Sellers et al. 2003 ), whereas another study failed to find the same connection ( Sellers et al. 2006 ). In one study a measure that more explicitly assess those aspects of identity that address preparedness for discrimination was associated with increased distress ( Bynum et al. 2007 ).
These main effects analyses suggest that the pride and belonging dimensions of racial identity may produce a more general feeling of well-being. Aspects of racial identity may buffer the effects of other stressors common to the research participants that were not assessed in the study. However, the effects of these positive racial identity dimensions were not sufficient to offset the impact of perceived racism, and in particular everyday maltreatment, on distress and depressive symptoms.
Findings from Lee (2005) suggest a complex relationship of centrality and pride to depression. In this study of Asian young adults, there was a significant main effect of Ethnic Identity (EI)-Pride, such that those with relatively high scores on the ethnic pride dimension of the MEIM (derived from a factor analysis conducted in the same sample) had fewer depressive symptoms than those with low scores. However, among those with high EI-Pride scores, the effects of racism on depressive symptoms were stronger than for those who did not feel a great deal of pride in their ethnic group. This suggests that enhancing pride may reduce depression overall, but may be related to greater symptom reports when individuals are exposed to racism. Racial identity as a buffer of cardiovascular reactivity to race-related stress
There are also two studies that examined racial identity as a moderator or buffer of the relationship of race-related stress to an index of cardiovascular response. These measures of cardiovascular reactivity (CVR) appear to be markers for processes involved in the development of hypertension and coronary heart disease. However, it is difficult to evaluate the meaning of reactivity data in some of these studies, since there are some limitations to the presentations of the existing studies. Clark and Gochett (2006) reported finding an inverse relationship between private regard and cardiac output and stroke volume (measures of sympathetic nervous system influences on the heart) before, during, and after racial and non-racial stressors. The authors interpreted the inverse relationship to suggest higher levels of arousal for those high in private regard; however, analyses directly examining the relationship of identity to the change from baseline are not reported. Similarly, Torres and Bowens (2000) reported positive correlations of the Black Racial Identity Attitude Scale (RIAS-B) internalization attitudes (indicating more acceptance of both Black and Caucasian groups) with systolic blood pressure (SBP) reactivity to both race and non-race related stressors. These findings may indicate that individuals with Black oriented identities (i.e., those who are low on internalization) are better prepared to confront episodes of racism as they expect this maltreatment. However, the data are difficult to interpret, as greater increases in SBP may also indicate greater task engagement and no measures were made of level of effort or involvement. Without data on subjective response to the task, it is difficult to interpret these findings.
In contrast, in a study of the main effect of racial identity on both resting and ambulatory blood pressure (BP), Thompson et al. (2002) found that a transitional racial identity, marked by an intense involvement in in-group activities and an “idealization of African American and African American culture and a devaluation of White culture,” was associated with higher levels of resting and ambulatory BP. The authors suggest that a transitional identity may intensify the perception of racial bias and make race-related conflict more salient, increasing the frequency with which individuals experience interpersonal stress. However, no data were available on the race-related social interactions experienced by the participants.
What accounts for the mixed findings on the effects of racial identity?
The effects of racial identity on mental and physical health are complex, and the data do not support a uniformly positive effect of each aspect of racial or ethnic identity on mental health. The bulk of the evidence suggests that ethnic pride may be associated with fewer depressive symptoms overall, but the results indicate that pride and other aspects of ethnic/racial identity are not sufficient to buffer the effects of racism on depressive symptoms for most (but not all) samples. It is important to note that some aspects of racial identity appear to intensify the relationship of racism to depression.
Ethnic pride may not buffer the pain of race-based ostracism, since social rejection is painful, even when other sources of social connection are available ( Baumeister et al. 2005 ; MacDonald and Leary 2005 ). Further, race-based social rejection or exclusion may heighten the awareness of race-related stereotypes and elicit concerns about stereotype threat. In turn these concerns may evoke feelings of anxiety and shame ( Cohen and Garcia 2005 ; Steele 1997 ). Messages of cultural pride may not be adequate to counteract the emotional consequences of demeaning treatment.
There is also some evidence that ostracism is associated with a decrease in self-awareness and self-regulation ( Baumeister et al. 2005 ; MacDonald and Leary 2005 ). This blunting of self-awareness may help the individual block some of the injury to self-esteem associated with social rejection. However, reductions in self-awareness in response to personal threat may also limit the individual’s ability to access self-related schemas (e.g., racial identity or ethnic pride) that might facilitate coping. Laboratory studies are needed to assess the effects of priming racial salience on responses to acute race-related stressors and to evaluate the effects of increasing versus decreasing self-awareness during these manipulations ( Baumeister et al. 2005 ).
The effects of racial centrality appear to be more variable than the effects of racial/ethnic pride and belonging. There may be circumstances in which drawing attention to race and heightening awareness of potential exposure to racism protect individuals from its harmful effects ( Fischer and Shaw 1999 ), but there is also evidence that racial centrality can intensify distress ( Sellers et al. 2006 ). The awareness that one may be targeted for racism may help individuals gather the strength they need to avoid being denied rights or misjudging their own competence, but this awareness can also be exhausting, elicit distress and anger, and erode some relationships. This is consistent with data on the use of avoidance coping in African Americans reported by Thompson Sanders (2006) . Further work is needed to identify the types and timing of the complex of racial socialization messages that increase awareness without destroying hope or inflicting a costly emotional burden. The nature of these messages may vary by socioeconomic status and parental involvement, and some personality dimensions ( Scott 2003 , 2004 ), and the role of these potential moderators has also not been adequately explored.
There is some evidence that racial identity buffers the effects of racism on self-esteem and some measures of academic performance (e.g., Oyserman et al. 2001 ; Wong et al. 2003 ). Failure to find substantial buffering effects for depression and distress may be a function of the need to match the type of coping strategy with the expected outcome. Racial identity is related to self-concept and pride, and as a consequence may have effects primarily on aspects of functioning that are tied to self-concept versus more global affective states.
The data on the effectiveness of racial identity as a buffer of the relationship of racism to BP or BP reactivity is too limited to support firm conclusions. The findings suggest, however, that measures of racial identity may tap psychological dimensions that influence coping with stressors on a day-to-day basis. These schemas may influence the degree to which individuals are able to engage in challenge or feel they must defend themselves from threat. Both engagement and defensiveness influence cardiovascular dynamics. Continued research on the ways in which racial identity affects appraisals of laboratory tasks and everyday events, and in turn influence cardiovascular and neuroendocrine responses, would be very useful.
Social support as a buffer of the effects of racism on mental and physical health
Social support has been defined as the presence or availability of network members who express concern, love, and care for an individual and provide coping assistance ( Sarason et al. 1983 ). Seeking social support involves communication with others (e.g., family, friends, and community members) about events or experiences. Within the Black community, seeking social support has sometimes been more specifically labeled as “leaning on shoulders” ( Shorter-Gooden 2004 ). This term refers to seeking out and talking to others as a means of coping with racial discrimination.
How might social support buffer the effects of racism on distress?
It is widely accepted that social support is beneficial for physical and psychological health ( Allgower et al. 2001 ; Barnett and Gotlib 1988 ; Symister and Friend 2003 ). A supportive social network promotes a sense of security and connectedness, helping the individual to understand that discrimination is a shared experience. Group members can serve as models, guiding the individual in effective methods for responding to and coping with discrimination. Placing the event in a collective context can also help the individual to feel more connected to his or her ethnic/racial group and can activate racial identity ( Harrell 2000 ; Mellor 2004 ). Greater participation in social activities may help to distract individuals and provide them with positive experiences that may buffer the negative impact of a range of stressors including racism ( Finch and Vega 2003 ).
Seeking social support is commonly used as a coping strategy following a racist incident ( Krieger 1990 ; Krieger and Sidney 1996 ; Lalonde et al. 1995 ; Mellor 2004 ; Shorter-Gooden 2004 ; Swim et al. 2003 ; Thompson Sanders 2006 ; Utsey et al. 2000b ). In Black college students, Swim et al. (2003) found that 68% of the sample discussed a racist incident with their family, friends, or others. In two separate studies, Krieger found that the vast majority of Black individuals sampled reported “talking to others” in response to racial discrimination ( Krieger 1990 ; Krieger and Sidney 1996 ). Furthermore, a majority of Black Canadians reported “seeking advice” and “telling others about the discrimination” in response to a hypothetical situation involving housing rejection based on ethnic discrimination ( Lalonde et al. 1995 ). Although social support is hypothesized to serve as an effective strategy for coping with racism, there has been surprisingly limited empirical research testing this hypothesis.
We are aware of only three empirical tests of the hypothesis that social support buffers the effects of racism on distress ( Fischer and Shaw 1999 ; Noh and Kaspar 2003 ; Thompson Sanders 2006 ), and four studies examining the hypothesis that social support buffers the effects of racism on physical health-related measures (i.e., self-reported health or cardiovascular reactivity to stress) ( Clark 2003 ; Clark and Gochett 2006 ; Finch and Vega 2003 ; McNeilly et al. 1995 ). Diverse ethnic groups were included in the studies. Some studies assessed the tendency to seek social support or guidance in response to racist events ( Noh and Kaspar 2003 ; Thompson Sanders 2006 ), whereas others examined the availability of support (i.e., size of network) or quality of general social support ( Clark 2003 ; Finch and Vega 2003 ; Fischer and Shaw 1999 ; McNeilly et al. 1995 ). Further details of the studies are presented in Table 2 .
Studies of the buffering effects of social support on the relationship of racism to mental or physical health indices
Note. sx = symptoms; discrim. = discrimination. SBP = systolic blood pressure; DBP = diastolic blood pressure. BP = blood pressure. SRE = Schedule of Racist Events ( Landrine & Klonoff, 1996 ). MHI = Mental Health Inventory ( Veit & Ware, 1983 ). CES-D-K = Korean version of the Center for Epidemiologic Studies Depression Scale ( Noh et al., 1998 ; Radloff, 1977 ). CRI = Coping Responses Inventory–Adult Form ( Moos, 1993 ).
For main effects analysis, the type of support and specific outcome measure are listed as follows: type of support/outcome. The results are categorized as follows: (NO) = No main effect; (YES-POS) = Significant main effects such that increasing scores on listed dimensions of social support are associated with lower symptom reports; (YES-NEG) = Significant main effects such that increasing scores on listed dimensions of social support are associated with greater symptom reports.
(NO) = No buffering effect; (YES-I) = Significant interaction effect, such that the relationship of racism to symptoms is stronger for those with high scores on listed dimensions of social support. (YES-B) = Significant interaction effect, such that the relationship of racism to symptoms is weaker for those with high scores on listed dimensions of social support.
. For both SBP and DBP, the SSN is negatively related to BP reactivity for those reporting low levels of racism and positively related for those reporting high levels of racism.
The three studies examining the buffering effects of seeking social support on the relationship of racism to distress failed to find positive effects ( Fischer and Shaw 1999 ; Noh and Kaspar 2003 ; Thompson Sanders 2006 ). However, two of these three studies found main effects of social support on depressive symptoms.
The effects are more mixed among the four studies examining the buffering effects of support on a health-related outcome. Finch and Vega (2003) found robust effects of instrumental support on perceived health in a population-based sample of Mexican Americans. Discrimination was not related to health among those with high levels of support, but was associated with poorer health for those with low levels of support. Two studies found buffering effects of support seeking, but only for those who were exposed to low levels of racism ( Clark 2003 ; Clark and Gochett 2006 ). Specifically, Clark (2003) reported that self-reported quantity and quality of social support were associated with reduced DBP reactivity to a non-racial stressor (i.e., mental arithmetic), but only for those who had experienced relatively low levels of racism over the course of their lives. Similarly, in a school-based study, Clark and Gochett (2006) found that youth who indicated that they would “talk to others” had a lower incidence of elevated BP (above 90th percentile) than those who did not endorse this item, but these effects were seen only among those who experienced low levels of racism. In contrast, among those exposed to high levels of racism, “talking to others” was associated with a higher prevalence of elevated BP. Finally, in a laboratory study, McNeilly et al. (1995) reported that providing support (in the form of a supportive confederate) did not reduce cardiovascular reactivity in response to racist provocation (i.e., debating about race-related topics), but did reduce self-reported anger. There are two additional studies that examined the relationship of support to race-related stress in African Americans, but they did not directly test the hypothesis that social support buffers the effects of racism on psychological distress ( Scott and House 2005 ; Utsey et al. 2000a, b ).
Despite the generally null findings of the quantitative studies, two qualitative reports about seeking social support in response to ethnic or racial discrimination suggest beneficial effects. In a diary study of perceived discrimination, participants reported that it was helpful to discuss racist incidents with another person ( Swim et al. 2003 ). Similarly, African American men participating in an African-centered support group for confronting racism reported decreases in levels of anger and frustration. They also reported engaging in fewer interpersonal conflicts with significant others after attending the support group ( Elligan and Utsey 1999 ).
What accounts for the mixed findings on social support?
Overall, the quantitative literature provides minimal support for the hypothesis that social support (either seeking social support or having a supportive network) buffers the impact of racism on psychological health. It also provides very mixed support for the notion that social support buffers racism effects on indices of physical health. There is some suggestion that social support may be helpful at low levels of stress exposure, but exacerbates difficulties at high levels of exposure. Yet, these results are contrary to anecdotal reports or findings from qualitative studies, and largely contrast with the findings from other literatures on the buffering effects of support in the face of other stressors (mostly medical illnesses). What accounts for these variations?
Measures and research design
General difficulties with the social support research have been outlined by Uchino (2006) . Variations in the conceptualization and measurement of social support make the results of studies examining the effects of support as a buffer of the effects of racism on distress or health difficult to interpret. In the studies reviewed, four separate support-related constructs have been studied: seeking support to obtain guidance for ways to manage racism; general support network size, general support network quality, and the proportion of relationships with people of the same ethnicity. The quality of the measurement instruments also varies, with some studies assessing social support seeking using two questions in a self-report survey or diary ( Noh and Kaspar 2003 ; Swim et al. 2003 ).
The research designs of some studies also have some limitations, as cross sectional correlational designs fail to reveal the direction of the effects. In the Clark and Gochett (2006) study, there are some correlations between exposure to higher levels of racism and seeking support, suggesting that the level of support seeking is in fact a function of the degree of stress exposure. Prospective cohort and laboratory studies may be necessary to more clearly distinguish the direction of the relationship between support and distress. Different types of support may be necessary at different points in time, and no studies have examined perceived needs for support at different stages in the experience of ethnicity-related maltreatment. For example, concrete advice and emotional support may be needed at the time of the incident, whereas support focused on meaning and hope may be needed as individuals confront the possibility of more sustained exposure.
Social constraint and facilitation
Some of the failure to find positive effects associated with social support may be a function of issues related to both social constraint and social facilitation. Lepore and Revenson (2007) propose that social constraints limit the effectiveness of certain social support interventions. Seeking support for race-related maltreatment may entail discussions that are anxiety provoking for both the seekers and givers of support. For members of stigmatized groups, discussions of racism may evoke recollections that feel uncontrollable and are stressful. For members of a majority out-group, stereotype threat may be evoked if individuals become concerned about appearing cruel, uncaring, or insensitive when discussing race-related conflict ( Richeson and Shelton 2007 ). Anxiety on the part of both the in-group and out-group members may inhibit effective communication about race-related incidents. When individuals receive messages that tend to minimize or deny aspects of their experience, support seeking may be ineffective and associated with increased versus decreased distress ( Badr and Taylor 2006 ). Research on the dynamics of interracial communication may provide guidance for further research on the types of communication that can minimize social constraints and facilitate inter-racial communication ( Czopp et al. 2006 ; Richeson and Shelton 2005 ).
As Utsey et al. (2002) points out, social facilitation may increase distress when individuals discuss discrimination with other members of their group. The experience of sharing episodes of ethnicity-related maltreatment may arouse greater anger as individuals exchange accounts of their experiences. If the situations appear hopeless or if individuals in the discussion have had negative experiences managing race-related interactions themselves, other negative emotions, including fear, frustration, grief, shame and loss, may also be evoked. Further research is needed to determine how variations in the circumstances in which support is sought and in the content of support message confer different costs and benefits to the target of discrimination. It will be important to understand how best to acknowledge the difficulties and pain associated with exposure to discrimination without eliminating hope or generating additional stress.
Confrontation and anger expression
Race-related maltreatment evokes anger ( Brondolo et al. 2008 ; Broudy et al. 2007 ; Landrine and Klonoff 1996 ). Consequently, many models of coping with racism recognize the need to address the anger evoked by ethnicity-related maltreatment ( Mellor 2004 ), and some of the seminal studies of the effects of racial stress examined anger coping ( Harburg et al. 1979 , 1991 ). Anger coping strategies used in response to ethnicity-related maltreatment may address two goals. The first involves using anger coping strategies, including confrontation, to influence the outcome of the race-related conflict. For example, the expression of anger can be used to motivate the perpetrator to change his or her behavior or to motivate others to take action ( Swim et al. 2003 ). The second goal of anger coping strategies is to manage the emotional burden created by the anger.
Researchers have used several different approaches to assess constructs related to anger expression and confrontation. In some cases, anger coping that involves directly protesting maltreatment has been subsumed under the term confrontation coping ( Noh et al. 1999 ). In other cases, researchers have directly examined the effects of different strategies for anger expression, including outward anger expression (Anger-Out) or anger suppression (Anger-In) (e.g., Dorr et al. 2007 ).
Despite the obvious importance of studying the effects of anger coping, there have been relatively few studies directly addressing these issues. Specifically, there have been two survey studies that examine the effects of confrontation coping as a buffer of the relationship of racism to distress ( Noh et al. 1999 ; Noh and Kaspar 2003 ). There have been five studies examining the effects of anger coping or confrontation as a means of managing racist interactions on BP ( Armstead and Clark 2002 ; Dorr et al. 2007 ; Krieger 1990 ; Krieger and Sidney 1996 ; Steffen et al. 2003 ). Details of these studies are presented in Table 3 .
Studies of the buffering effects of anger expression on the relationship of racism to mental and physical health indices
Note. HTN = Hypertension. ABP = ambulatory blood pressure. BP = blood pressure. SBP = systolic blood pressure. DBP = diastolic blood pressure. MAS = Multidimensional Anger Scale ( Siegel, 1986 ). PRS = Perceived Racism Scale ( McNeilly et al., 1996 ).
For the main effects analyses the results are listed as follows: type of anger expression/outcome. The results are categorized as follows: NA = not applicable, with no main effect tested. (YES-POS) = Significant main effects such that increasing scores on listed dimensions of anger expression are associated with higher levels of ABP.
For the interaction effects, the results are listed as follows: type of anger expression/type of discrimination/outcome. The results are categorized as follows: (NO) = No buffering effect; (YES-I) = Significant interaction effect, such that the relationship of racism to symptoms is stronger for those with high scores on listed dimension of anger expression. (YES-B) = Significant interaction effect, such that the relationship of racism to BP is weaker for those with high scores on listed dimensions of anger expression.
In two population-based samples of Asian immigrants, Noh and colleagues examined confrontation coping using measures which include an item assessing direct protests to the perpetrator. In the South Asian sample (i.e., composed largely of Chinese and Vietnamese), Noh and Kaspar (2003) reported no effects of confrontation on the relationship of perceived discrimination to depression. In contrast, in a study of Korean immigrants, the authors reported that personal confrontation coping (i.e., directly protesting or talking to the perpetrator) moderated the effects of discrimination on depression, such that those who were more likely to confront reported less depression in the face of discrimination than those who indicate they are less likely to confront ( Noh et al. 1999 ).
A recent diary study by Hyers (2007) examined costs and benefits associated with confrontation coping, although no measure was made of depression or health. She considered outcomes including rumination-related behaviors (i.e., feelings of emotional upset, regret, wishing to respond differently in the future) and experiences of self-efficacy (i.e., “the perpetrator was educated”) as well as interpersonal conflict. These intermediate outcomes may be predictors of depression over the long run, and potentially serve to maintain the stress associated with the episodes of racism. Hyers reported that when women responded to incidents of racism or sexism with confrontation coping, they were less likely to ruminate and more likely to feel they had been efficacious. Those who did not confront were more likely to report a benefit of avoiding interpersonal conflict; however, it is not clear if the women who did confront actually experienced more conflict.
In five studies using different methodologies, the effects of anger coping on BP levels or reactivity and recovery were examined ( Armstead et al. 1989 ; Dorr et al. 2007 ; Krieger 1990 ; Krieger and Sidney 1996 ; Steffen et al. 2003 ). The results were fairly consistent and are detailed in Table 3 . The main effects analyses indicate that suppressing anger in the face of discrimination is associated with higher levels of BP or poorer cardiovascular recovery from race-related stress exposure. However, there is also some evidence that, for African Americans, expressing anger may be associated with poorer cardiovascular recovery as well.
In two population-based samples, Krieger and colleagues examined the effects of exposure to discrimination and responses to discrimination, contrasting the effects of “doing something about it” with “accepting it as a fact of life”. Among a small sample of Black women, those who reported “doing something about it (discrimination)” were less likely to have a hypertension diagnosis than those who “accepted and kept quiet about it” ( Krieger 1990 ). In Krieger and Sidney (1996) , a large scale population-based study of Black and White individuals, the blood pressure levels of those who reported “doing something about it” were lower than those of individuals who reported “accepting it.” Statistical tests of moderation were not performed, making it difficult to determine if buffering effects were present.
Steffen et al. (2003) reported that trait anger suppression was independently associated with ambulatory DBP in a convenience sample of African Americans. However, neither anger suppression nor expression moderated the effects of racism on ambulatory BP. Armstead et al. (1989) and Dorr et al. (2007) conducted laboratory studies examining the relationship of anger coping to BP response to a racist stressor. Armstead et al. (1989) reported that for Blacks anger suppression was marginally associated with greater SBP at baseline. A style of anger coping in which anger is outwardly expressed was marginally associated with baseline levels of mean arterial pressure and reduced SBP and DBP reactivity to the racist stressor.
In the Dorr et al. study (2007) , African American and European American participants engaged in race and nonrace-related debates facing a European American confederate. Following the tasks participants were given opportunities to express versus inhibit anger. The authors reported that for both African Americans and European Americans, anger inhibition was associated with slower recovery of indices of total peripheral resistance, a measure of vascular response. For African Americans, BP and HR recovery was slower when they were allowed to express their anger than when they were asked to inhibit it, and recovery was also slower than the recovery of EA who were able to express their anger. These effects suggest that anger suppression exacerbates vascular recovery to stress for both groups; whereas outward anger expression exacerbates cardiac and other CV indices of recovery to stress for Blacks.
The authors suggest that one possible explanation for these findings is that anger suppression can lead to rumination if issues are not resolved satisfactorily. However, anger expression may lead to anxiety about retaliation or abandonment if social relations are threatened by direct expression of anger. Both rumination and persistent anxiety may be associated with sustained physiological activation following stress exposure ( Brosschot et al. 2006 ).
What accounts for the variations in the effects of confrontation as a buffer of the effects of racism on depression?
The specific effects of confrontation coping are difficult to interpret, since confrontation coping is subsumed under the general heading of approach coping or problem solving coping and includes items measuring social support seeking as well as “going to the authorities”. Second, the type of confrontation (i.e., hot and angry versus cold and unemotional) is generally not specifically examined, yet laboratory research suggests that the effects of the confrontation depend in part on the emotional quality of the confrontation ( Czopp et al. 2006 ).
Although the limited literature suggests that most Black and White individuals report trying to “do something” about racism ( Krieger and Sidney 1996 ; Plummer and Slane 1996 ; Thompson Sanders 2006 ), diary studies suggest that individuals report thinking about confrontation or indirectly or non-verbally expressing their anger more often than they actually engage in direct anger expression ( Hyers 2007 ). Measures are needed that separate intent from action or more explicitly identify the specific actions taken.
It is also necessary to consider the context in which the conflict occurs when evaluating the effects of anger coping or confrontation. Individuals will hesitate to express anger directly if they believe there will be retaliatory consequences for this anger expression. In any given interaction, individuals with relatively lower levels of power or status are more likely to suppress anger than high power individuals ( Gentry et al. 1973 ). The location of the conflict (i.e., work or social arena) may also influence the choice of coping strategies ( Brondolo et al. 2005b ). Cultural variations in the importance of maintaining relationships may also affect the outcomes associated with confrontation ( Noh et al. 1999 ; Suchday and Larkin 2004 ). Research is needed to clearly differentiate among different types of confrontation strategies and to identify situational and cultural variations in the types of strategies used and their effectiveness.
Some of the health effects of different individual-level coping strategies are likely to be a function of the efficacy of the coping strategies themselves. If the strategies for confrontation and anger coping are effective on some dimensions (e.g., reducing overt expressions of prejudice), but costly on others (e.g., social relations), individuals may not perceive themselves as having appropriate coping resources, making it more likely that they will perceive interracial or race-based maltreatment as stressful. Evaluating a broad range of outcome measures from the target’s perspective (e.g., mental and physical health, rumination, satisfaction with outcome, perceived benefits) is critical. Investigating the perceptions of these different coping strategies from the perspective of others is also important. The growing literature on other’s perceptions of confrontation and other coping strategies ( Czopp et al. 2006 ; Kawakami et al. 2007 ) can provide guidance for future studies on anger coping. More knowledge regarding the perceptions of different coping strategies by individuals of other ethnicities/races can help guide individuals as they weigh the costs and benefits of various responses.
Summary and future directions
The strongest and clearest conclusion that can be drawn from this review is that there is a significant need for further research on strategies for coping with racism. No coping strategy has emerged as a clearly successful strategy for offsetting the mental or physical health impacts of racism. Instead, each approach has some demonstrated strengths, but also considerable side effects or limitations.
Ethnic and racial identity develop to meet multiple needs, including enhancing one’s pride and commitment to one’s cultural group as well as helping individuals develop meaningful strategies for managing discrimination based on racial or ethnic bias. Studies suggest that racial identity, particularly racial or ethnic pride and belonging may have beneficial effects in some circumstances. But these components of identity are not sufficient to ameliorate the effects of racism on the development of depressive symptoms and may increase the detection of threat and the perception of harm.
Involvement with only one type of identity may restrict the individuals’ ability to consider multiple perspectives and learn a range of coping options. Instead, in an increasingly multicultural society, it will be important to understand the best ways to help individuals master the complex psychological tasks involved in maintaining individual, group and national identities, particularly when the values at one level contrast with the values at another. Oyserman has specifically suggested that a “possible selves” approach, encouraging individuals to incorporate aspects of different types of group identities, may be of benefit ( Oyserman et al. 2007 ).
It may be that the strength of this approach is not only in gaining the benefits of having multiple roles, but in the process of mastering the underlying cognitive-affective processes that subserve these identities. Learning to think about oneself as a member of many different groups requires considering multiple perspectives and developing the ability to shift the focus of one’s attention even when experiencing strong emotion. Additionally, individuals must learn to integrate specific individualized information (e.g., about stressors and resources specific to the individual) with larger category-based information (e.g., about stressors and resources conferred because of group membership). In the process of developing an awareness of many possible identities, individuals may also strengthen their own capacity for effective coping in a range of circumstances and increase their ability to draw support from a number of different groups. Similarly, social support appears to be beneficial in a variety of circumstances, but the available data do not support a direct role for non-specific social support as a buffer of the effects of racism on distress. A greater understanding of the types of support beneficial for different phases and dimensions of the experience of racism will be needed to facilitate the development of support-based interventions including, for example, group based stress-management programs.
The clinical literature ( Elligan and Utsey 1999 ; Utsey et al. 2002 ) may provide some guidance for the specific types of support that may be valuable at different points in time. It may be necessary to include communication that is aimed at validating the individual’s experience (i.e., the perception that race-based maltreatment may have occurred), while also offering opportunities to review the circumstances and identify factors that elicited perceptions of threat. This type of support is needed to decrease defensiveness and increase the capacity to clearly articulate specific concerns and develop appropriate strategies to manage the specific threat. But acute problem-focused support may not be sufficient. Support may also be needed to address and ameliorate the painful nature of racism, providing an opportunity to address not only the feelings of anger, but of shame and anxiety as well. Finally, still other forms of support may be needed to provide hope and the motivation and direction to reduce racism and its effects over the long term.
The psychobiological effects of anger suppression among African Americans are among the most consistent findings in the literature on coping with racism. These data suggest that suppressing anger in the face of discrimination is associated with elevated BP or greater BP responses, but the studies have included only African Americans or European Americans. Other data suggest that there may be cultural moderators of these effects, since the association between anger suppression and distress varies depending on the individual’s ethnicity or race.
Yet, it is unclear what the effective alternatives to anger suppression and aggressive confrontation might be. We need better and more detailed answers to the questions: What is the most effective method to protest ethnicity-related maltreatment? How can anger be used to effectively communicate the seriousness of injustice without exhausting the targets of injustice? If individuals suppress anger at the time of the maltreatment, how can they reintroduce the discussion and communicate their concerns and remedy the injustice later? Understanding the predictors of anger suppression and confrontation both at the time of the incident and over the long run is likely to yield insight into the costs and benefits of these different approaches and to suggest more effective strategies.
Since racism and strategies for coping with racism occur within an interpersonal context, it is important to understand how different behaviors are perceived by others. Czopp et al. (2006) indicates that confrontation coping can be very effective in changing a perpetrator’s beliefs and behavior. The different features of the confrontation (e.g., the ethnicity of the confronter, the emotional tone of the message) are associated with variations in the effectiveness of the confrontation in changing behavior and eliciting negative reactions. The literature on coping with racism must be closely integrated with the empirical literature on the perceptions of targeted individuals by members of other racial or ethnic groups ( Kawakami et al. 2007 ). With this knowledge, individuals can make better predictions about the likely outcomes of their efforts to combat racism and to become increasingly effective in their communication.
Cultural norms have changed regarding the acceptability of overtly discriminatory behavior. Social modeling via the media and other methods has been used to communicate more egalitarian values and to deride racist behavior. It may be useful to use similar methods to generate and model strategies for communicating concern and anger about more subtle discriminatory or stigmatizing actions.
There are conceptual and methodological problems with the existing literature that are common to a new research area confronting a complex and disturbing problem. Some difficulties are related to problems in conceptualizing racism-related coping, and developing models that incorporate the different types of strategies needed to accommodate variations in demand across time and across contexts. To date, very few studies have examined the degree to which the effects of racism-related coping strategies vary by context or timing, and very few have examined the degree to which individual difference variables, including the presence of other background stressors or personality dimensions, shape the type of coping choice ( Brondolo et al. 2008 ; Scott 2004 ) or moderate its effectiveness ( Danoff-Burg et al. 2004 ; Scott 2004 ).
Surprisingly, almost no studies have examined variations in the effectiveness of the strategies by the stage of the incident (i.e., in preparation for future difficulties, at the time of the incident or following the termination of the conflict). Additionally, investigations have not adequately separated out the types of strategies most effective for managing the practical consequences of exposure versus the emotional consequences of confronting unjust social exclusion. The development of new measures of racism-related coping that incorporate issues of timing, context, and intent are needed.
Research is also needed to investigate the differential effects of any particular strategy on functioning, affect and health. Some coping strategies, for example, may be effective in limiting exposure to racism, but may have detrimental effects on mental and physical health. Outcomes must also include assessments of the target’s perceptions of effectiveness as well.
Because coping strategies may have side effects, there is a need for more research involving multiple outcome measures. Confrontational coping may have the side effect of creating or exacerbating interpersonal conflict. Anger suppression may have the side effect of increasing rumination. Social support seeking can be distracting or confusing. The results of studies reporting effects that are limited to one or two outcome domains may be misleading regarding the overall effectiveness of the coping responses examined.
In this review, we have chosen to consider a coping strategy as effective if it ameliorates some of the deleterious health effects of racism, specifically effects on depression symptoms or risk factors for hypertension. However, there may be other dimensions of effectiveness worth considering: Does the strategy for coping with racism reduce the incidence of racism over the long run? Does it achieve the personal goals of the target (i.e., to get a job, to avoid exclusion) even it if incurs some consequences as well? Does it decrease fear?
A fuller understanding of the potential benefits of strategies for coping with racism will be facilitated by intervention research. Ultimately, these will have the broadest impact if delivered and evaluated on a community, institutional, or national scale. Public education messages and school-based health promotion activities have the potential of reaching a large and diverse audience. But they will only be as effective as the coping responses that they attempt to promote.
We focused on stress-buffering, which is only one model of the manner in which coping responses may ameliorate the effects of exposure to racism. As shown in Fig. 1 , other plausible models include mediational models that posit simultaneous causal effects of stress on coping and of coping on outcomes. Some of the strategies that we have examined, such as anger expression or racial identity development, may be better considered as responses that emerge as a function of discrimination rather than as coping responses that develop independently of exposure. Developing different strategies may require a substantial effort on the part of the target. Both buffering and mediational models are best examined in large-scale, longitudinal studies, which are in short supply in the published literature.
Early models of coping may have reflected the more general societal view that racial and ethnic discrimination were an immutable feature of life. As legal, economic, and social conditions change, the possibilities for coping with ethnic and racial discrimination will change as well. As new solutions and opportunities develop, the models of these coping strategies will also evolve.
Research on strategies for coping with racism is necessary to empower targeted individuals to develop and choose methods that are effective at reducing discrimination, increasing hope, and buffering the impact of racism on health. As we come to understand a fuller range of consequences of each strategy, we can provide better guidance to help individuals make more informed choices about the ways they wish to cope with racism and protect their health. We hope that this knowledge and the detailed description of the ways in which racism is experienced by the targets will contribute to the elimination of discriminatory behavior.
Two additional studies report buffering effects on perceived stress, but not depressive symptoms ( Sellers et al., 2003 ; Sellers et al., 2006 ). Four studies reported buffering effects of racial/ethnicity identity on self-esteem or academic orientation, achievement or efficacy, even when the authors reported that they did not find buffering effects on measures of distress or depression ( Sellers et al., 2003 ; Wong et al., 2003 ) or did not examine effects on depression ( Oyserman & Fryberg, 2006 ; Romero & Roberts, 2003 ). There are also laboratory studies examining the effects of identity on emotional responses to racism-type manipulations ( Ellemers, 1997 ). These provide important insights into the nature of group and individual processes on identity development, but it is not clear that the measures used in these studies are of relevance to the hypothesis that racial/ethnic identity buffers the effects of exposure to racism on clinically significant distress.
Contributor Information
Elizabeth Brondolo, St. John’s University
Nisha Brady, St. John’s University
Melissa Pencille, St. John’s University.
Danielle Beatty, University of Pittsburgh Medical Center
Richard J. Contrada, Rutgers, The State University of New Jersey
- Allgower A, Wardle J, Steptoe A. Depressive symptoms, social support, and personal health behaviors in young men and women. Health Psychology. 2001;20(3):223–227. [ PubMed ] [ Google Scholar ]
- Allport GW. The nature of prejudice. Oxford, England: Addison-Wesley; 1954. [ Google Scholar ]
- Anderson NB. Racial Differences in Stress-Induced Cardiovascular Reactivity and Hypertension: Current Status and Substantive Issues. American Psychological Association. 1989;105(1):89–105. doi: 10.1037/0033-2909.105.1.89. [ DOI ] [ PubMed ] [ Google Scholar ]
- Anderson NB, Myers HF, Pickering T, Jackson JS. Hypertension in blacks: Psychosocial and Biological perspectives. Journal of Hypertension. 1989;7:161–172. [ PubMed ] [ Google Scholar ]
- Armstead CA, Clark R. Assessment of self-reported anger expression in pre- and early-adolescent African Americans: Psychometric considerations. Journal of Adolescence. 2002;25(4):365–371. doi: 10.1006/jado.2002.0481. [ DOI ] [ PubMed ] [ Google Scholar ]
- Armstead CA, Lawler KA, Gorden G, Cross J, Gibbons J. Relationship of racial stressors to blood pressure responses and anger expression in Black college students. Health Psychology. 1989;8(5):541–556. doi: 10.1037//0278-6133.8.5.541. [ DOI ] [ PubMed ] [ Google Scholar ]
- Badr H, Taylor CLC. Social constraints and spousal communication in lung cancer. Psycho-Oncology. 2006;15(8):673–683. doi: 10.1002/pon.996. [ DOI ] [ PubMed ] [ Google Scholar ]
- Banks KH, Kohn-Wood L. The influence of racial identity profiles on the relationship between racial discrimination and depressive symptoms. Journal of Black Psychology 2007 [ Google Scholar ]
- Barnett PA, Gotlib IH. Psychosocial functioning and depression: Distinguishing among antecedents, concomitants, and consequences. American Psychological Association. 1988;104(1):97–126. doi: 10.1037/0033-2909.104.1.97. [ DOI ] [ PubMed ] [ Google Scholar ]
- Baumeister RF, DeWall CN, Ciarocco NJ, Twenge JM. Social exclusion impairs self-regulation. Journal of Personality & Social Psychology. 2005;88(4):589–604. doi: 10.1037/0022-3514.88.4.589. [ DOI ] [ PubMed ] [ Google Scholar ]
- Borrell LN, Jacobs DR, Jr, Williams DR, Pletcher MJ, Houston TK, Kiefe CI. Self-reported racial discrimination and substance use in the coronary artery risk development in adults study. American Journal of Epidemiology. 2007;20:1–12. doi: 10.1093/aje/kwm180. [ DOI ] [ PubMed ] [ Google Scholar ]
- Branscombe NR, Schmitt MT, Harvey RD. Perceiving pervasive discrimination among African-Americans: Implications for group identification and well-being. Journal of Personality and Social Psychology. 1999;77(1):135–149. [ Google Scholar ]
- Brondolo E, Beatty D, Cubbin C, Weinstein M, Saegert S, Wellington RL, et al. Sociodemographic variations in self-reported racism in a community sample of blacks and latino(a)s. Journal of Applied Social Psychology (in press) [ Google Scholar ]
- Brondolo E, Brady N, Thompson S, Tobin JN, Cassells A, Sweeney M, et al. Perceived racism and negative affect: Analyses of trait and state measures of affect in a community sample. Journal of Social and Clinical Psychology. 2008;27(2):150–173. doi: 10.1521/jscp.2008.27.2.150. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brondolo E, Kelly KP, Coakley V, Gordon T, Thompson S, Levy E, et al. The Perceived Ethnic Discrimination Questionnaire: development and preliminary validation of a community version. Journal of Applied Social Psychology. 2005;35(2):335–365. [ Google Scholar ]
- Brondolo E, Rieppi R, Erickson SA, Bagiella E, Shapiro PA, McKinley P, et al. Hostility, interpersonal interactions, and ambulatory blood pressure. Psychosomatic Medicine. 2003;65:1003–1011. doi: 10.1097/01.psy.0000097329.53585.a1. [ DOI ] [ PubMed ] [ Google Scholar ]
- Brondolo E, Thompson S, Brady N, Appel R, Cassells A, Tobin JN, et al. The relationship of racism to appraisals and coping in a community sample. Ethnicity and Disease. 2005;15(4 Suppl 5):S5-14–19. [ PubMed ] [ Google Scholar ]
- Brondolo E, Thompson S, Brady N, Appel R, Cassells A, Tobin JN, et al. The relationship of racism to appraisals and coping in a community sample. Ethnicity and Disease. 2006;15(S5):14–19. [ PubMed ] [ Google Scholar ]
- Brosschot JF, Gerin W, Thayer JF. The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychosomatic Research. 2006;60(2):113–124. doi: 10.1016/j.jpsychores.2005.06.074. [ DOI ] [ PubMed ] [ Google Scholar ]
- Broudy R, Brondolo E, Coakley V, Brady N, Cassells A, Tobin J, et al. Perceived ethnic discrimination in relation to daily moods and negative social interactions. Journal of Behavioral Medicine. 2007;30(1):31–43. doi: 10.1007/s10865-006-9081-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- Bynum MS, Burton ET, Best C. Racism experiences and psychological functioning in African American college freshmen: Is racial socialization a buffer? Cultural Diversity and Ethnic Minority Psychology. 2007;13(1):64–71. doi: 10.1037/1099-9809.13.1.64. [ DOI ] [ PubMed ] [ Google Scholar ]
- Causey DL, Dubow EF. Development of a self-report coping measure for elementary school children. Journal of Clinical Child Psychology. 1992;21(1):47–59. [ Google Scholar ]
- Cheng C. Cognitive and motivational processes underlying coping flexibility: A dual-process model. Journal of Personality and Social Psychology. 2003;84(2):425–438. [ PubMed ] [ Google Scholar ]
- Clark R. Self-reported racism and social support predict blood pressure reactivity in Blacks. Annals of Behavioral Medicine. 2003;25(2):127–136. doi: 10.1207/S15324796ABM2502_09. [ DOI ] [ PubMed ] [ Google Scholar ]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans. American Psychologist. 1999;54(10):805–816. doi: 10.1037//0003-066x.54.10.805. [ DOI ] [ PubMed ] [ Google Scholar ]
- Clark R, Gochett P. Interactive effects of perceived racism and coping responses predict a school-based assessment of blood pressure in Black youth. Annals of Behavioral Medicine. 2006;32(1):1–9. doi: 10.1207/s15324796abm3201_1. [ DOI ] [ PubMed ] [ Google Scholar ]
- Cohen GL, Garcia J. “I am us”: Negative stereotypes as collective threats. Journal of Personality & Social Psychology. 2005;89(4):566–582. doi: 10.1037/0022-3514.89.4.566. [ DOI ] [ PubMed ] [ Google Scholar ]
- Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. Newbury Park, CA: Sage; 1988. [ Google Scholar ]
- Cokley K. Critical issues in the measurement of ethnic and racial identity: A referendum on the state of the field. Journal of Counseling Psychology. 2007;54(3):224–234. [ Google Scholar ]
- Constantine MG, Donnelly PC, Myers LJ. Collective self-esteem and africultural coping styles in African American adolescents. Journal of Black Studies. 2002;32(6):698–710. [ Google Scholar ]
- Contrada RJ, Ashmore RD, Gary ML, Coups E, Egeth JD, Sewell A, et al. Measures of ethnicity-related stress: Psychometric properties, ethnic group differences, and associations with well-being. Journal of Applied Social Psychology. 2001;31:1775–1820. [ Google Scholar ]
- Cross WE., Jr . Ethnicity, race, and identity. Chicago, IL: University of Chicago Press; 2005. [ Google Scholar ]
- Cross WE, Jr, Strauss L. The everyday functions of African American identity. In: Swim JK, Stangor C, editors. Prejudice: The target’s perspective. San Diego, CA: Academic Press; 1998. pp. 267–279. [ Google Scholar ]
- Czopp AM, Monteith MJ, Mark AY. Standing up for a change: reducing bias through interpersonal confrontation. Journal of Personality and Social Psychology. 2006;90(5):784–803. doi: 10.1037/0022-3514.90.5.784. [ DOI ] [ PubMed ] [ Google Scholar ]
- Danoff-Burg S, Prelow HM, Swenson RR. Hope and life satisfaction in Black college students coping with race-related stress. Journal of Black Psychology. 2004;30(2):208–228. [ Google Scholar ]
- Deragotis LR. Symptom Checklist-90-R: Administration, scoring and procedures manual. 3. Minneapolis, MN: National Computer Systems, Inc; 1994. [ Google Scholar ]
- Deragotis LR, Meisarotis N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [ PubMed ] [ Google Scholar ]
- Dorr N, Brosschot JF, Sollers JJ, III, Thayer JF. Damned if you do, damned if you don’t: The differential effect of expression and inhibition of anger on cardiovascular recovery in Black and White males. International Journal of Psychophysiology. 2007;66(2):125–134. doi: 10.1016/j.ijpsycho.2007.03.022. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ellemers N, Spears R, Doosje B. Sticking together of falling apart: In-group identification as a psychological determinant of group commitment versus individual mobility. Journal of Personality and Social Psychology. 1997;72(3):617–626. [ Google Scholar ]
- Elligan D, Utsey SO. Utility of an African-centered support group for African American men confronting societal racism and oppression. Cultural Diversity and Ethnic Minority Psychology. 1999;41(3):295–313. doi: 10.1037/1099-9809.5.2.156. [ DOI ] [ PubMed ] [ Google Scholar ]
- Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. Journal of Health and Social Behavior. 2000;41(3):295–313. [ PubMed ] [ Google Scholar ]
- Finch BK, Vega WA. Acculturation stress, social support, and self-rated health among Latinos in California. Journal of Immigrant Health. 2003;5(3):109–117. doi: 10.1023/a:1023987717921. [ DOI ] [ PubMed ] [ Google Scholar ]
- Fischer AR, Shaw CM. African Americans’ mental health and perceptions of racist discrimination: The moderating effects of racial socialization experiences and self-esteem. The Journal of Counseling Psychology. 1999;46(3):395–407. [ Google Scholar ]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003;129(1):10–51. doi: 10.1037/0033-2909.129.1.10. [ DOI ] [ PubMed ] [ Google Scholar ]
- Gallo LC, Smith TW, Cox C. Socioeconomic status, psychosocial processes, and perceived health: An interpersonal perspective. Annals of Behavioral Medicine. 2006;31:109–119. doi: 10.1207/s15324796abm3102_2. [ DOI ] [ PubMed ] [ Google Scholar ]
- Gentry WD, Harburg E, Hauenstein L. Effects of anger expression/inhibition/and guilt on elevated diastolic blood pressure in high/low stress and Black/White females. 1973. pp. 115–116. [ Google Scholar ]
- Greene ML, Way N, Pahl K. Trajectories of perceived adult and peer discrimination among Black, Latino, and Asian American adolescents: Patterns and psychological correlates. Developmental Psychology. 2006;42(2):218–238. doi: 10.1037/0012-1649.42.2.218. [ DOI ] [ PubMed ] [ Google Scholar ]
- Harburg E, Blakelock EH, Roeper P. Resentful and reflective coping with arbitrary authority and blood pressure: Detroit. Psychosomatic Medicine. 1979;41(3):189–202. doi: 10.1097/00006842-197905000-00002. [ DOI ] [ PubMed ] [ Google Scholar ]
- Harburg E, Gleiberman L, Russell M, Cooper ML. Anger-coping styles and blood pressure in Black and White males: Buffalo, New York. Psychosomatic Medicine. 1991;53(2):153–164. doi: 10.1097/00006842-199103000-00005. [ DOI ] [ PubMed ] [ Google Scholar ]
- Harrell JP. Analyzing Black coping styles: A supplemental diagnostic system. Journal of Black Psychology. 1979;5(2):99–108. [ Google Scholar ]
- Harrell JP, Hall S, Taliaferro J. Physiological responses to racism and discrimination: An assessment of the evidence. American Journal of Public Health. 2003;93(2):243–248. doi: 10.2105/ajph.93.2.243. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Harrell JP, Merritt MN, Kalu J. Racism, stress and disease. In: Jones RL, editor. African American mental health: Theory, research, and intervention. Hampton, VA: Cobb & Henry Publishers; 1998. pp. 247–280. [ Google Scholar ]
- Harrell SP. A multidimensional conceptualization of racism-related stress: Implications for the well-being of people of color. American Journal of Orthopsychiatry. 2000;70(1):42–57. doi: 10.1037/h0087722. [ DOI ] [ PubMed ] [ Google Scholar ]
- Harrell SP. Unpublished manuscript. 1994. The Racism and Life Experience Scale. [ Google Scholar ]
- Harrell SP. Unpublished manuscript. 1997a. The Racism and Life Experiences Scales. [ Google Scholar ]
- Harrell SP. Unpublished manuscript. 1997b. Development and initial validation of scales to measure racism-related stress. [ Google Scholar ]
- Helms JE. An overview of Black racial identity theory. In: Helms JE, editor. Black and White racial identity: Theory, research, and practice. Westport, Conn: Praeger; 1990. pp. 9–32. [ Google Scholar ]
- Horowitz M, Wilner H, Alvarez W. Impact of Events Scale: A measure of subjective stress. Psychosomatic Medicine. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hughes D, Rodriguez J, Smith EP, Johnson DJ, Stevenson HC, Spicer P. Parents’ ethnic-racial socialization practices: A review of research and directions for future study. Developmental Psychology. 2006;42(5):747–770. doi: 10.1037/0012-1649.42.5.747. [ DOI ] [ PubMed ] [ Google Scholar ]
- Hyers LL. Resisting prejudice every day: Exploring women’s assertive responses to anti-Black racism, anti-semitism, heterosexism, and sexism. Sex Roles. 2007;56(1–2):1–12. [ Google Scholar ]
- Jackson JS, Brown TN, Williams DR, Torres M, Sellers SS, Brown K. Racism and the physical and mental health status of African Americans: A thirteen year national panel study. Ethnicity and Disease. 1996;6:132–147. [ PubMed ] [ Google Scholar ]
- Jones CP. Levels of racism: A theoretic framework and a gardener’s tale. American Journal of Public Health. 2000;90(8):1212–1215. doi: 10.2105/ajph.90.8.1212. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jones JM. Prejudice and racism. 2. New York: McGraw Hill; 1997. [ Google Scholar ]
- Kawakami K, Phills CE, Steele JR, Dovidio JF. (Close) distance makes the heart grow fonder: Improving implicit racial attitudes and interracial interactions Through approach behaviors. Journal of Personality & Social Psychology. 2007;92(6):957–971. doi: 10.1037/0022-3514.92.6.957. [ DOI ] [ PubMed ] [ Google Scholar ]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999;40(3):208–230. [ PubMed ] [ Google Scholar ]
- Krieger N. Racial and gender discrimination: Risk factors for high blood pressure? Social Science and Medicine. 1990;30(12):1273–1281. doi: 10.1016/0277-9536(90)90307-e. [ DOI ] [ PubMed ] [ Google Scholar ]
- Krieger N. Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services. 1999;29:295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [ DOI ] [ PubMed ] [ Google Scholar ]
- Krieger N, Sidney S. Racial discrimination and blood pressure: The CARDIA study of young Black and White adults. American Journal of Public Health. 1996;86(10):1370–1378. doi: 10.2105/ajph.86.10.1370. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lalonde RN, Majumder S, Parris RD. Preferred responses to situations of housing and employment discrimination. Journal of Applied Social Psychology. 1995;25(12):1105–1119. [ Google Scholar ]
- Landrine H, Klonoff EA. The Schedule of Racist Events: A measure of racial discrimination and a study of its negative physical and mental health consequences. Journal of Black Psychology. 1996;22:144–168. [ Google Scholar ]
- Lazarus RS. Toward better research on stress and coping. American Psychologist. 2000;55:665–673. doi: 10.1037//0003-066x.55.6.665. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lee RM. Do ethnic identity and other-group orientation protect against discrimination for Asian Americans? Journal of Counseling Psychology. 2003;50(2):133–141. [ Google Scholar ]
- Lee RM. Resilience against discrimination: Ethnic identity and other-group orientation as protective factors for Korean Americans. Journal of Counseling Psychology. 2005;52(1):36–44. [ Google Scholar ]
- Lepore S, Revenson TA. Social constraints on disclosure and adjustment to cancer. Social and Personality Psychology Compass. 2007;1(1):313–333. [ Google Scholar ]
- Lewis-Coles MaEL, Constantine MG. Racism-related stress, Africultural coping, and religious problem-solving among African Americans. Cultural Diversity and Ethnic Minority Psychology. 2006;12(3):433–443. doi: 10.1037/1099-9809.12.3.433. [ DOI ] [ PubMed ] [ Google Scholar ]
- Lewis TT, Everson-Rose SA, Powell LH, Matthews KA, Brown C, Karavolos K, et al. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN Heart Study. Psychosomatic Medicine. 2006;68(3):362–368. doi: 10.1097/01.psy.0000221360.94700.16. [ DOI ] [ PubMed ] [ Google Scholar ]
- MacDonald G, Leary MR. Why does social exclusion hurt? The relationship between social and physical pain. Psychological Bulletin. 2005;131(2):202–223. doi: 10.1037/0033-2909.131.2.202. [ DOI ] [ PubMed ] [ Google Scholar ]
- Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination and health outcomes among African Americans. Annual Review of Psychology. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mays VM, Coleman LM, Jackson JS. Perceived race-based discrimination, employment status, and job stress in a national sample of Black women: Implications for health outcomes. Journal of Occupational Health Psychology. 1996;1:319–329. doi: 10.1037//1076-8998.1.3.319. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McEwen B, Lasley EN. Allostatic load: When protection gives way to damage. Advances in Mind-Body Medicine. 2003;19(1):28–33. [ PubMed ] [ Google Scholar ]
- McEwen B, Lasley EN. Allostatic load: When protection gives way to damage. In: Monat A, Lazarus RS, Reevy G, editors. The Praeger handbook on stress and coping. Vol. 1. Westport, CT: Praeger Publishers/Greenwood Publishing Group; 2007. pp. 99–109. [ Google Scholar ]
- McNeilly MD, Anderson NB, Armstead CA, Clark R, Corbett M, Robinson EL, et al. The Perceived Racism Scale: A multidimensional assessment of the experience of White racism among African Americans. Ethnicity and Disease. 1996;6:154–166. [ PubMed ] [ Google Scholar ]
- McNeilly MD, Robinson EL, Anderson NB, Pieper C, Shah A, Toth PS, et al. Effects of racist provocation and social support on cardiovascular reactivity in African American women. International Journal of Behavioral Medicine. 1995;2(4):321–338. doi: 10.1207/s15327558ijbm0204_3. [ DOI ] [ PubMed ] [ Google Scholar ]
- Mellor D. Responses to racism: A taxonomy of coping styles used by aboriginal Australians. American Journal of Orthopsychiatry. 2004;74(1):56–71. doi: 10.1037/0002-9432.74.1.56. [ DOI ] [ PubMed ] [ Google Scholar ]
- Moos RH. Coping Responses Inventory Adult Form: Professional manual. Odessa, FL: Psychological Assessment Resources; 1993. [ Google Scholar ]
- Mossakowski KN. Coping with perceived discrimination: Does ethnic identity protect mental health? Journal of Health and Social Behavior. 2003;44(3):318–331. [ PubMed ] [ Google Scholar ]
- Noh S, Beiser M, Kaspar V, Hou F, Rummens J. Perceived racial discrimination, depression, and coping: A study of Southeast Asian refugees in Canada. Journal of Health and Social Behavior. 1999;40:193–207. [ PubMed ] [ Google Scholar ]
- Noh S, Kasper V, Chen X. Measuring depression in Korean Immigrants: Assessing validity of the translated Korean version of the CES-D scale. Cross-Cultural Research: The Journal of Comparative Social Science. 1998;32(4):358–377. [ Google Scholar ]
- Noh S, Kaspar V. Perceived discrimination and depression: Moderating effects of coping, acculturation and ethnic support. American Journal of Public Health. 2003;93(2):232–238. doi: 10.2105/ajph.93.2.232. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Outlaw FH. Stress and coping: The influence of racism on the cognitive appraisal processing of African-Americans. Issues in Mental Health Nursing. 1993;14:399–409. doi: 10.3109/01612849309006902. [ DOI ] [ PubMed ] [ Google Scholar ]
- Oyserman D, Brickman D, Rhodes M. School success, possible selves, and parent school involvement. Family Relations: Interdisciplinary Journal of Applied Family Studies. 2007;56(5):479–489. [ Google Scholar ]
- Oyserman D, Fryberg S. The Possible Selves of Diverse Adolescents: Content and Function Across Gender, Race and National Origin. In: Dunkel C, Kerpelman J, editors. Possible selves: Theory, research and applications. Hauppauge, NY: Nova Science Publishers; 2006. pp. 17–39. [ Google Scholar ]
- Oyserman D, Harrison K, Bybee D. Can racial identity be promotive of academic efficacy? International Journal of Behavioral Development. 2001;25(4):379–385. [ Google Scholar ]
- Oyserman D, Kemmelmeier M, Fryberg S, Brosh H, Hart-Johnson T. Racial-ethnic self-schemas. Social Psychology Quarterly. 2003;66(4):333–347. [ Google Scholar ]
- Quintana SM. Racial and ethnic identity: Developmental perspectives and research. Journal of Counseling Psychology. 2007;54(3):259–270. [ Google Scholar ]
- Paradies Y. A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology. 2006;35:888–901. doi: 10.1093/ije/dyl056. [ DOI ] [ PubMed ] [ Google Scholar ]
- Peters RM. Racism and Hypertension Among African Americans. Western Journal of Nursing Research. 2004;26(6):612–631. doi: 10.1177/0193945904265816. [ DOI ] [ PubMed ] [ Google Scholar ]
- Phinney JS. Ethnic identity in adolescents and adults: Review of research. Psychological Bulletin. 1990;108(3):499–514. doi: 10.1037/0033-2909.108.3.499. [ DOI ] [ PubMed ] [ Google Scholar ]
- Phinney JS. The Multigroup Ethnic Identity Measure: A new scale for use with diverse groups. Journal of Adolescent Research. 1992;7:156–176. [ Google Scholar ]
- Phinney JS. When we talk about American ethnic groups, what do we mean? American Psychologist. 1996;51:918–927. [ Google Scholar ]
- Phinney JS, Horenczyk G, Liebkind K, Vedder P. Ethnic identity, immigration and well-being: An interactional perspective. Journal of Social Issues. 2001;57(3):493–510. [ Google Scholar ]
- Phinney JS, Ong AD. Conceptualization and measurement of ethnic identity: Current status and future directions. Journal of Counseling Psychology. 2007;54(3):271–281. [ Google Scholar ]
- Plummer DL, Slane S. Patterns of coping in racially stressful situations. Journal of Black Psychology. 1996;22(3):302–315. [ Google Scholar ]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [ Google Scholar ]
- Richeson JA, Shelton NJ. Brief Report: Thin slices of racial bias. Journal of Nonverbal Behavior. 2005;29(1):75–86. [ Google Scholar ]
- Richeson JA, Shelton NJ. Negotiating interracial interactions: Costs, consequences and possibilities. 2007;16:316–320. [ Google Scholar ]
- Romero AJ, Roberts RE. The impact of multiple dimensions of ethnic identity on discrimination and adolescents’ self-esteem. Journal of Applied Social Psychology. 2003;33(11):2288–2305. [ Google Scholar ]
- Ruiz JM, Hamann HA, Coyne J, Compare A. In sickness and in health: Interpersonal risk and resilience in cardiovascular disease. In: Molinari E, Compare A, Parati G, editors. Clinical psychology and heart disease. New York: Springer; 2006. pp. 233–272. [ Google Scholar ]
- Sarason IG, Levine HM, Basham RB, Sarason BR. Assessing social support: The Social Support Questionnaire. Journal of Personality and Social Psychology. 1983;44(1):127–139. [ Google Scholar ]
- Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support: Practical and theoretical implications. Journal of Social and Personal Relationships. 1987;4(4):497–510. [ Google Scholar ]
- Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, Symptoms of Depression, and Self-Rated Health Among African American Women in Detroit: Results from a Longitudinal Analysis. American Journal of Public Health. 2006;96(7):1265–1270. doi: 10.2105/AJPH.2005.064543. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Scott LD., Jr The relation of racial identity and racial socialization to coping with discrimination among African American adolescents. Journal of Black Studies. 2003;33(4):520–538. [ Google Scholar ]
- Scott LD., Jr Correlates of coping with perceived discriminatory experiences among African American adolescents. Journal of Adolescence. 2004;27(2):123–137. doi: 10.1016/j.adolescence.2003.11.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- Scott LD, Jr, House LE. Relationship of distress and perceived control to coping with perceived racial discrimination among Black youth. Journal of Black Psychology. 2005;31(3):254–272. [ Google Scholar ]
- Sellers RM, Caldwell CH, Schmeelk-Cone KH, Zimmerman MA. Racial identity racial discrimination, perceived stress, and psychological distress among African American young adults. Journal of Health and Social Behavior. 2003;44(3):302–317. [ PubMed ] [ Google Scholar ]
- Sellers RM, Copeland-Linder N, Martin PP, Lewis RL. Racial identity matters: The relationship between racial discrimination and psychological functioning in African American adolescents. Journal of Research on Adolescence. 2006;16(2):187–216. [ Google Scholar ]
- Sellers RM, Rowley SAJ, Chavous TM, Shelton NJ, Smith MA. Multidimensional inventory of Black identity: A preliminary investigation of reliability and constuct validity. Journal of Personality and Social Psychology. 1997;73(4):805–815. [ Google Scholar ]
- Sellers RM, Shelton NJ. The role of racial identity in perceived racial discrimination. Journal of Personality and Social Psychology. 2003;84(5):1079–1092. doi: 10.1037/0022-3514.84.5.1079. [ DOI ] [ PubMed ] [ Google Scholar ]
- Sellers RM, Smith MA, Shelton NJ, Rowley SAJ, Chavous TM. Multidimensional model of racial identity: A reconceptualization of African American racial identity. Personality and Social Psychology Review. 1998;2(1):18–39. doi: 10.1207/s15327957pspr0201_2. [ DOI ] [ PubMed ] [ Google Scholar ]
- Shorter-Gooden K. Multiple resistance strategies: How African American women cope with racism and sexism. Journal of Black Psychology. 2004;30(3):406–425. [ Google Scholar ]
- Siegel JM. The Multidimensional Anger Inventory. Journal of Personality and Social Psychology. 1986;51(1):191–200. doi: 10.1037/0022-3514.51.1.191. [ DOI ] [ PubMed ] [ Google Scholar ]
- Skinner EA, Edge K, Altman J, Sherwood H. Searching for the Structure of Coping: A Review and Critique of Category Systems for Classifying Ways of Coping. Psychological Bulletin. 2003;129(2):216. doi: 10.1037/0033-2909.129.2.216. [ DOI ] [ PubMed ] [ Google Scholar ]
- Smith TW, Gallo LC, Ruiz JM. Toward a social psychophysiology of cardiovascular reactivity: Interpersonal concepts and methods in the study of stress and coronary disease. In: Suls J, Wallston K, editors. Social psychological foundations of health and illness. Malden, MA: Blackwell; 2003. pp. 335–366. [ Google Scholar ]
- Spielberger CD. Manual for the State–Trait Anxiety Inventory (Form Y) Palo Alto, CA: Consulting Psychologists Press; 1983. [ Google Scholar ]
- Steele CM. A threat in the air: How stereotypes shape intellectual identity and performance. American Psychologist. 1997;52(6):613–629. doi: 10.1037//0003-066x.52.6.613. [ DOI ] [ PubMed ] [ Google Scholar ]
- Steffen PR, Bowden M. Sleep disturbance mediates the relationship between perceived racism and depressive symptoms. Ethnicity & Disease. 2006;16(1):16–21. [ PubMed ] [ Google Scholar ]
- Steffen PR, McNeilly MD, Anderson N, Sherwood A. Effects of perceived racism and anger inhibition on ambulatory blood pressure in African Americans. Psychosomatic Medicine. 2003;65(5):746–750. doi: 10.1097/01.psy.0000079380.95903.78. [ DOI ] [ PubMed ] [ Google Scholar ]
- Stevenson HC. Validation of the Scale of Racial Socialization for African American adolescents: Steps toward multidimensionality. Journal of Black Psychology. 1994;20(4):445–468. [ Google Scholar ]
- Stevenson HC, Jr, Cameron R, Herrero-Taylor T, Davis GY. Development of the Teenager Experience of Racial Socialization scale: Correlates of race-related socialization frequency from the perspective of Black youth. Journal of Black Psychology. 2002;28(2):84–106. [ Google Scholar ]
- Suchday S, Larkin KT. Psychophysiological responses to anger provocation among Asian Indian and White men. International Journal of Behavioral Medicine. 2004;11(2):71–80. doi: 10.1207/s15327558ijbm1102_2. [ DOI ] [ PubMed ] [ Google Scholar ]
- Swim JK, Hyers LL, Cohen LL, Fitzgerald DC, Bylsma WH. African American college students’ experiences with everyday racism: Characteristics of and responses to these incidents. Journal of Black Psychology. 2003;29(1):38–67. [ Google Scholar ]
- Symister P, Friend R. The influence of social support and problematic support on optimism and depression in chronic illness: A prospective study evaluating self-esteem as a mediator. Health Psychology. 2003;22(2):123–129. doi: 10.1037//0278-6133.22.2.123. [ DOI ] [ PubMed ] [ Google Scholar ]
- Taylor J, Grundy C. Measuring Black Internalization of White Stereotypes About African Americans: The Nadanolitization Scale. In: Jones RL, editor. The Handbook of Tests and Measurements for Black Populations. Hampton, VA: Cobb & Henry; 1996. pp. 217–226. [ Google Scholar ]
- Thompson HS, Kamarck TW, Manuck SB. The association between racial identity and hypertension in African-American adults: elevated resting and ambulatory blood pressure as outcomes. Ethnicity and Disease. 2002;12:20–28. [ PubMed ] [ Google Scholar ]
- Thompson Sanders VL. Coping responses and the experience of discrimination. Journal of Applied Social Psychology. 2006;36(5):1198–1214. [ Google Scholar ]
- Thompson Sanders VL. The empirical characteristics of the Multidimensional Racial Identification Scale. Revised. Journal of Research in Personality. 1995;29:208–222. [ Google Scholar ]
- Tull ES, Sheu YT, Butler C, Cornelious K. Relationships between Perceived Stress, Coping Behavior and Cortisol Secretion in Women with High and Low Levels of Internalized Racism. Journal of the National Medical Association. 2005;97(2):206–212. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. [ DOI ] [ PubMed ] [ Google Scholar ]
- Utsey SO, Adams EP, Bolden M. Development and initial validation of the Africultural coping systems inventory. Journal of Black Psychology. 2000;26(2):194–215. [ Google Scholar ]
- Utsey SO, Chae MH, Brown CF, Kelly D. Effect of ethnic group membership on ethnic identity, race-related stress and quality of life. Cultural Diversity and Ethnic Minority Psychology. 2002;8(4):366–377. doi: 10.1037/1099-9809.8.4.367. [ DOI ] [ PubMed ] [ Google Scholar ]
- Utsey SO, Ponterotto JG, Reynolds AL, Cancelli AA. Racial discrimination, coping, life satisfaction, and self-esteem among African Americans. Journal of Counseling & Development. 2000;78(1):72–80. [ Google Scholar ]
- Veit CT, Ware JE. The structure of psychological distress and well-being in general populations. Journal of Consulting and Clinical Psychology. 1983;51(5):730–742. doi: 10.1037//0022-006x.51.5.730. [ DOI ] [ PubMed ] [ Google Scholar ]
- Way N. Unpublished Document. 1997. Adult and Peer Discrimination Measure. [ Google Scholar ]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: Findings from community studies. American Journal of Public Health. 2003;93(2):200–208. doi: 10.2105/ajph.93.2.200. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Williams DR, Williams-Morris R. Racism and mental health: the African American experience. Ethnicity and Health. 2000;5:243–268. doi: 10.1080/713667453. [ DOI ] [ PubMed ] [ Google Scholar ]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [ DOI ] [ PubMed ] [ Google Scholar ]
- Wong CA, Eccles JS, Sameroff A. The influence of ethnic discrimination and ethnic identification on African American adolescents’ school and socioemotional adjustment. Journal of Personality. 2003;71(6):1197–1232. doi: 10.1111/1467-6494.7106012. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (287.9 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Racism and Health: Evidence and Needed Research
David r williams, jourdyn lawrence, brigette davis.
- Author information
- Article notes
- Copyright and License information
Address correspondence to David R. Williams, Harvard T. H. Chan School of Public Health, 677 Huntington Avenue, 6 th floor, Boston, MA 02115 ( [email protected] )
Issue date 2019 Apr 1.
In recent decades, there has been remarkable growth in scientific research examining the multiple ways in which racism can adversely affect health. This interest has been driven in part by the striking persistence of racial/ethnic inequities in health and the empirical evidence that indicates that socioeconomic factors alone do not account for racial/ethnic inequities in health. Racism is considered a fundamental cause of adverse health outcomes for racial/ethnic minorities and racial/ethnic inequities in health. This article provides an overview of the evidence linking the primary domains of racism – structural racism, cultural racism and individual-level discrimination – to mental and physical health outcomes. For each mechanism, we describe key findings and identify priorities for future research. We also discuss evidence for interventions to reduce racism and needed research to advance knowledge in this area.
There has been steady and sustained growth in scientific research on the multiple ways in which racism can affect health and racial/ethnic inequities in health. This article provides an overview of key findings and trends in this area of research. It begins with a description of the nature of racism and the principal mechanisms -- structural, cultural and individual -- by which racism can affect health. For each dimension, we review key research findings and describe needed scientific research. We also discuss evidence for interventions to reduce racism and needed research to advance knowledge in this area. Finally, we discuss crosscutting priorities across the three domains of racism.
The patterning of racial/ethnic inequities in health was an early impetus for research on racism and health ( 139 ). First, there are elevated rates of disease and death for historically marginalized racial groups, blacks (or African Americans), Native Americans (or American Indians and Alaska Natives) and Native Hawaiians and Other Pacific Islanders, who tend to have earlier onset of illness, more aggressive progression of disease and poorer survival ( 5 , 134 ). Second, empirical analyses revealed the persistence of racial differences in health even after adjustment for socioeconomic status (SES). For example, at every level of education and income, African Americans have lower life expectancy at age 25 than whites and Hispanics (or Latinos), with blacks with a college degree or more education having lower life expectancy than whites and Hispanics who graduated from high school ( 15 ). Third, research has also documented declining health for Hispanic immigrants over time with middle-aged U.S.-born Mexican Americans and Mexican immigrants resident 20 or more years in the U.S. having a health profile that did not differ from that of African Americans ( 56 ).
Racism and Health
Racism is an organized social system, in which the dominant racial group, based on an ideology of inferiority, categorizes and ranks people into social groups called “races”, and uses its power to devalue, disempower, and differentially allocate valued societal resources and opportunities to groups defined as inferior ( 13 , 140 ). Race is primarily a social category, based on nationality, ethnicity, phenotypic or other markers of social difference, which captures differential access to power and resources in society ( 133 ). Racism functions on multiple levels. The cultural agencies within a society socializes the population to accept as true the inferiority of non-dominant racial groups leading to negative normative beliefs (stereotypes) and attitudes (prejudice) toward stigmatized racial groups which undergird differential treatment of members of these groups by both individuals and social institutions ( 13 , 140 ). A characteristic of racism is that its structure and ideology can persist in governmental and institutional policies in the absence of individual actors who are explicitly racially prejudiced ( 7 ).
As a structured system, racism interacts with other social institutions, shaping them and being re-shaped by them, to reinforce, justify and perpetuate a racial hierarchy. Racism has created a set of dynamic, interdependent, components or subsystems that reinforce each other, creating and sustaining reciprocal causality of racial inequities across various sectors of society ( 106 ). Thus, structural racism exists within, and is reinforced and supported by multiple societal systems, including the housing, labor and credit markets, and the education, criminal justice, economic and healthcare systems. Accordingly, racism is adaptive over time, maintaining its pervasive adverse effects through multiple mechanisms that arise to replace forms that have been diminished ( 99 , 140 ).
Racism: A Fundamental Cause of Racial/Ethnic Inequities in Health
The persistence of racial inequities in health should be understood in the context of relatively stable racialized social structures that determine differential access to risks, opportunities, and resources that drive health. We conceptualize this system of racism, chiefly operating through institutional and cultural domains, as a basic or fundamental cause of racial health inequalities ( 74 , 99 , 133 , 136 ). According to Lieberson, fundamental causes are critical causal factors that generate an outcome while surface causes are associated with the outcome but changes in these factors do not trigger changes in the outcome ( 73 ). Instead, as long as the fundamental causes are operative, interventions on surface causes only give rise to new intervening mechanisms to maintain the same outcome. Sociologists argued that socioeconomic status (SES) is a fundamental cause of health ( 53 , 132 ), with Link and colleagues ( 74 , 100 ) providing considerable evidence in support of this perspective. In 1997, Williams argued that alongside SES and other upstream social factors, racism should be recognized as a fundamental cause of racial inequities in health ( 133 ). Evidence continues to accumulate highlighting racism as a driver of multiple upstream societal factors that perpetuate racial inequities in health for multiple non-dominant racial groups around the world ( 99 , 140 ).
Structural or Institutional Racism
We use the terms institutional and structural racism, interchangeably, consistent with much of the social science literature ( 13 , 55 , 106 ). Institutional racism refers to the processes of racism that are embedded in laws (local, state, and federal), policies, and practices of society and its institutions that provide advantages to racial groups deemed as superior, while differentially oppressing, disadvantaging, or otherwise neglecting racial groups viewed as inferior ( 13 , 104 ). We argue that the most important way through which racism affects health is through structural racism. We highlight evidence of the health impact of residential segregation but acknowledge that there are multiple other forms of institutional racism in society. For example, structural racism in the Criminal Justice System ( 84 , 130 , 142 ) can adversely affect health through multiple pathways ( 37 , 130 ).
Racial Residential Segregation
Racial residential segregation remains one of the most widely studied institutional mechanisms of racism and has been identified as a fundamental cause of racial health disparities due to the multiple pathways through which it operates to have pervasive negative consequences on health ( 7 , 38 , 60 , 136 ). Racial residential segregation refers to the occupancy of different neighborhood environments by race that was developed in the U.S. to ensure that whites resided in separate communities from blacks. Segregation was created by federal policies as well as explicit governmental support of private policies such as discriminatory zoning, mortgage discrimination, red-lining and restrictive covenants ( 107 ). This physical separation of races in distinctive residential areas (including the forced removal and relocation of American Indians) was shaped by multiple social institutions ( 83 , 136 ). Although segregation has been illegal since the Fair Housing Act of 1968, its basic structures established by the 1940s remain largely intact.
In the 2010 Census, residential segregation was at its lowest level in 100 years and the decline in segregation was observed in all of the nation’s largest metropolitan areas ( 43 ). However, the recent declines in segregation have been driven by a few blacks moving to formerly all-white residential areas with the declines in segregation having negligible impact on the very high percentage black census tracts, the residential isolation of most African-Americans, and the concentration of urban poverty ( 44 ). Although segregation is increasing for Hispanics, the segregation of African Americans remains distinctive. In the 2000 census middle class blacks were more segregated than poor Hispanics and Asians ( 81 ), and the segregation of immigrant groups has never been as high as the current segregation of African Americans ( 83 ).
Segregation and Health: Pathways
Segregation affects health in multiple ways ( 136 ). First, it is a critical determinant of SES, which is a strong predictor of variations in health. Research has found that segregation reduces economic status in adulthood by reducing access to quality elementary and high school education, preparation for higher education, and employment opportunities ( 136 ). Schools in segregated areas have lower levels of high-quality teachers, educational resources, per-student spending and higher levels of neighborhood violence, crime and poverty ( 91 ). Segregation also reduces access to employment opportunities by triggering the movement of low skill, high pay jobs from areas where racial minorities are concentrated to other areas and by enabling employers to discriminate against job applicants by using their place of residence as a predictor of whether or not the applicant would be a good employee ( 136 ) One national study found that the elimination of segregation would erase black-white differences in income, education and unemployment and reduce racial differences in single motherhood by two-thirds ( 28 ). Thus, segregation is responsible for the large and persistent racial/ethnic differences in SES. In 2016, for every dollar of income that white households received, Hispanics earned 73 cents and blacks earned 61 cents ( 110 ). And racial differences in health are stunningly larger. For every dollar of wealth that white households have, Hispanics have 7 pennies, and blacks have 6 pennies ( 120 ).
Segregation can also adversely affect health by creating communities of concentrated poverty with high levels of neighborhood disadvantage, low quality housing stock, and with both government and private sector demonstrating disinterest or divestment from these communities. In turn, the physical conditions (poor quality housing and neighborhood environments) and the social conditions (co-occurrence of social problems and disorders linked to concentrated poverty) that characterize segregated geographic areas lead to elevated exposure to physical and chemical hazards, increased prevalence and co-occurrence of chronic and acute psychosocial stressors, as well as, reduced access to a broad range of resources that enhance health ( 60 , 87 , 128 , 136 ). The living conditions created by concentrated poverty and segregation make it more difficult for residents of those contexts to practice healthy behaviors ( 7 , 60 , 128 , 136 ). Segregation also adversely affects the availability and affordability of care, contributing to lower access to high quality primary and specialty care and even pharmacy services ( 129 ).
Epidemiological Evidence Linking Segregation to Health
A 2011 review found nearly 50 empirical studies which generally found that segregation was associated with poorer health ( 128 ). A 2017 review and meta-analysis focused on 42 articles that examined the association between segregation and birth outcomes found that segregation was associated with increased risk of low birth rate weight and preterm birth for blacks ( 85 ). Other recent studies show that segregation is associated with increased risk of preterm birth for U.S.-born and foreign-born black women ( 79 ) and of stillbirth for blacks and whites, with the effects being more pronounced for blacks than for whites ( 131 ). A systematic review of 17 papers examining segregation and cancer, found that segregation was positively associated with later-stage diagnosis, elevated mortality and lower survival rates for both breast and lung cancers for blacks ( 65 ). Recent studies highlight variation in the association between segregation and health for population subgroups. One national study found that segregation was associated with poor self-rated health for blacks in high but not lower poverty neighborhoods ( 31 ). It was unrelated to poor health for whites but benefited whites indirectly by reducing the likelihood of their location in high poverty neighborhoods ( 31 ). And a 25 year longitudinal study found that cumulatively higher exposure to segregation was associated with elevated risk of incident obesity in black women but not black men ( 101 ).
Recommendations for Research on Institutional Racism
Several strategies should be implemented to further understanding of how institutional racism adversely affects health. First, there is a need to broaden our conceptualization and assessment of the multiple domains and contexts in which these structural processes are operative and empirically assess their impact on health. In a study of structural racism and myocardial infarction, Lukachko and colleagues ( 75 ) utilized four state-level measures of structural racism: political participation, employment, education and judicial treatment. The analyses revealed that state level racial disparities that disadvantaged blacks in political representation, employment and incarceration were associated with increased risk of MI in the prior year. Among whites, structural racism was unrelated to or had a beneficial effect on the risk of MI.
Second, immigration policy has been identified as a mechanism of structural racism ( 38 ) and systematic attention should be given to understanding how contemporary immigration policies adversely affect population health. Recent research suggests that anti-immigrant policies can trigger hostility toward immigrants leading to perceptions of vulnerability, threat, and psychological distress for both those who are directly targeted and those who are not ( 46 ). One study found that a large federal immigration raid was associated with an increase in low birthweight risk among infants born to Latina but not white mothers in that community a year after the raid ( 90 ). Immigration polices can also adversely affect health by leading to reduced utilization of preventive health services by both documented and undocumented immigrants ( 80 , 117 , 127 ).
Third, some of the methodological limitations of the current literature need to be addressed. Research on structural racism has been limited by the availability of data on structural levels and ecological analyses are limited in capturing the underlying processes. The available evidence suggests that the associations between segregation and health tend to vary based on the choice of a geographic unit of analysis ( 7 , 38 , 60 , 128 ). While smaller units tend to produce the most reliable estimates, the appropriate geographic level may not be consistent across all health outcomes. These analytic challenges are further exacerbated by difficulties disentangling the potential mediating and moderating effects that contribute to observed patterns. Many studies adjust for variables like poverty or other indicators of low SES and the social context which are likely a part of the pathway by which segregation exerts its effects ( 60 , 128 ). Future research needs to identify the proximal mechanisms linking segregation to health by using longitudinal data to establish temporality, and leveraging new statistical techniques ( 60 , 128 ). There is also a need for more complex system modeling approaches that seek to capture the impact of all of the dynamic historical processes that influence each other over time, at multiple levels of analysis ( 30 , 92 ).
Fourth, greater attention should be given to similarities and differences across national and cultural contexts. For example, segregation levels are rising in Europe and are positively associated with darker skinned nationalities and being Muslim but there has been little analysis of the effects of this segregation on SES and health ( 82 ). A study that compared a national sample of Caribbean blacks in the U.S. to those in the U.K. found that, in the U.S., increased black Caribbean ethnic density was associated with improved health while increased black ethnic density was associated with worse health but the opposite pattern was evident for Caribbean blacks in England ( 10 ). Comparative research could enhance our understanding of the contextual factors such as variation in the racialization of ethnic groups that could contribute to the observed associations.
Finally, we need a better understanding of the conditions under which group density can have positive versus adverse effects on health ( 86 ). A national study of Hispanics found that segregation was adversely related to poor self-rated health among US born Hispanics but it had a salutary effect on the health of the foreign-born ( 32 ). We need a clearer understanding of when and how segregation can give rise to health enhancing versus health damaging factors.
Cultural Racism
Cultural racism refers to the instillation of the ideology of inferiority in the values language, imagery, symbols and unstated assumptions of the larger society. It creates a larger ideological environment where the system of racism can flourish, and can undergird both institutional and individual level discrimination. It manifests itself through media, stereotyping and within institutions, and norms ( 49 , 140 ). It can yield inconspicuous forms of racism, such as implicit bias, as a result of the commonplace and continuous negative imagery about racial and ethnic minorities ( 140 ). Cultural forms of racism may serve as the conduit through which views regarding the limitations, stereotypes, values, images and ideologies associated with racial/ethnic minority groups are presented to society, and are consciously or subconsciously adopted and normalized ( 105 , 113 ).
The internalization of racism yields a tendency to focus on individual pathology and abilities rather than examining structural components that give rise to racial inequities. This internalization affects most members of the dominant group and a nontrivial proportion of the marginalized group as well, given that both groups are exposed to key socializing agents of the larger society that perpetuate racist beliefs ( 105 ). Research indicates that negative racial and ethnic stereotypes persist in entertainment, media, and fashion ( 18 , 140 ). A recent national survey of adults who work with children found that whites had high levels of negative racial stereotypes (lazy, unintelligent, violent and having unhealthy habits) towards non-whites, with the highest levels towards blacks followed by Native Americans and Hispanics ( 103 ).
Cultural Racism and Health
Cultural racism can affect health in multiple ways. First, cultural racism can drive societal policies that lead to the creation and maintenance of structures that provide differential access to opportunities ( 140 ). For example, a study of white residents revealed that their negative stereotypes about blacks influenced their housing decisions in ways that would maintain residential segregation ( 64 ). In this study whites rated an all-white neighborhood more positively (on the cost of housing, safety, future property value, and quality of schools) than an identical neighborhood if a black person were pictured in it.
Second, cultural racism can also lead to individual level unconscious bias that can lead to discrimination against outgroup members. In clinical encounters, these processes lead to minorities receiving inferior medical care compared to whites. Research indicates that across virtually every type of diagnostic and treatment interventions blacks and other minorities receive fewer procedures and poorer quality medical care than whites ( 112 ). Recent research documents the persistence of these patterns and reveals that higher implicit bias scores among physicians are associated with biased treatment recommendations in the care of black patients ( 123 ). Providers’ implicit bias is also associated with poorer quality of patient provider communication including provider nonverbal behavior ( 25 ).
Stereotype threat is a third pathway. This term refers to the anxieties and expectations that can be activated in stigmatized groups when negative stereotypes about their group are made salient. These anxieties can adversely affect academic performance and psychological functioning ( 114 ). Some limited evidence indicates that stereotype threat can lead to increased anxiety, reduced self-regulation and impaired decision-making that can lead to unhealthy behaviors, poor patient-provider communication, lower levels of adherence to medical advice, increased blood pressure and weight gain among stigmatized groups ( 6 , 114 , 141 ). Relatedly, a study documented that exposure of American Indian students to Native American mascots, leads to declines in self-esteem, community worth and achievement aspirations ( 35 ). Fourth, as noted, some members of stigmatized racial populations respond to the pervasive negative racial stereotypes in the culture by accepting them to be true. This endorsement of the dominant society’s beliefs about their inferiority is called internalized racism or self-stereotyping. Research indicates that it is associated with lower psychological well-being and higher levels of alcohol consumption, depressive symptoms and obesity ( 139 ).
Recommendations for Research on Cultural Racism
Future research should aim to understand how and why cultural racism, when it is measured as elevated levels of racial prejudice at the community level, is associated with poorer health for racial minorities, and sometimes all persons, who live in that community. Recent studies have found that residing in communities with high levels of racial prejudice is positively associated with overall mortality ( 20 , 67 ), heart disease mortality ( 68 ), and low birthweight ( 21 ). Community-level prejudice against immigrants has also been associated with increased mortality among US-born immigrant adults ( 89 ). However, these studies are ecological in nature and lack adjustment for individual-level factors
Second, we need to better understand how internalized racism can affect health. There is limited understanding of the conditions under which internalized racism has adverse consequences for health, the groups that are most vulnerable, and the range of health and health-related outcomes that may be affected ( 140 ). The optimal measurement of internalized racism is also a challenge. Studies have used scales of internalized racism, minority group endorsement of negative stereotypes and African Americans’ scores on anti-black bias on the IAT. It is currently unclear how these measures correlate with each other and the extent to which they may capture different aspects of internalized racism. Beyond the individual, future work should also examine internalized racism in a more collective form that could facilitate understanding of the cultural and structural pervasiveness of racism at the societal level racial ( 105 ). Research should also assess if and how racist ideologies and oppression become internalized among immigrants in the United States and how these are associated with health outcomes.
Discrimination
Discrimination is the most frequently studied domain of racism in the health literature. It exists in two forms: 1) where individuals and larger institutions, deliberately or without intent, treat racial groups differently, resulting in inequitable access to opportunities and resources (e.g., employment, education, and medical care) by race/ethnicity, and 2) self-reported discrimination, a sub-set of these experiences that individuals are aware of. These latter incidents are a type of stressful life experience that can adversely affects health, similar to other kinds of psychosocial stressors. Considerable scientific evidence, supports of the first pathway, much of it captured through audit studies (those in which researchers use individuals who are equally qualified in every respect but differ only in race or ethnicity) that document the persistence of discrimination in many contexts including employment, education, housing, credit, and criminal justice systems ( 93 ). This discrimination in social institutions contributes to the differential access to resources and opportunities and results in SES and other material disadvantages.
A large proportion of the discrimination literature focuses on the second pathway with the evidence indicating that stigmatized racial and ethnic populations and other socially marginalized groups around the world report experiences of discrimination that are inversely related to good health ( 109 , 139 , 140 ). Researchers refer to these experiences as self-reported discrimination, perceived discrimination, and racial discrimination, and we use these terms interchangeably. Self-reports of discrimination can adversely affect health through triggering negative emotional reactions that can lead to altered physiological reactions and changes in health behaviors, that can increase the risk of poor health ( 41 ). We highlight key patterns and trends in this research on discrimination and health.
A 2015 meta-analysis assessed the scientific evidence for the association between self-reported racial discrimination and health from over 300 articles published between 1983 and 2013 ( 95 ). Eighty one percent of studies were from the U.S. followed by the U.K., Australia, Canada, the Netherlands and 15 other countries. The analyses found that the association between discrimination and mental health was stronger than for physical health. This was inconsistent with a prior review that found similar effect sizes for physical and mental health ( 96 ). Interestingly, ethnicity moderated the effect of self-reported racial discrimination on health with the association between perceived racial discrimination and mental health being stronger for Asian Americans and Latino Americans compared to blacks and the association with physical health being stronger for Latinos than for blacks.
While the review by Paradies and colleagues ( 95 ) is the most comprehensive one published to date, it excluded many studies that are included in other reviews. Because of its focus on experiences of “racism”, it excluded studies using measures of discrimination, bias and unfair treatment where race or ethnicity were not explicitly noted as the reason for discrimination. This included many studies using the Everyday Discrimination Scale and the Major Experiences of Discrimination Scale ( 137 , 143 ) which use a two-stage approach where respondents are first asked about generic experiences of bias and then a follow-up question ascertains the main reason. Many studies that have used these measures have not asked or analyzed the follow-up question. Relatedly, studies were also excluded that used a version of these two instruments that were utilized in the national MIDUS study ( 59 ). It explicitly asked respondents to report only instances where they had been “discriminated against” because of their race or other specific social characteristics ( 59 ). It appears that the use of “discrimination” does not affect the reports of bias by blacks but depresses reports by whites ( 8 ). Importantly, multiple reviews have concluded that the deleterious health effects of discrimination are generally evident with the generic perception of bias or unfair treatment irrespective of which social status category the experience is attributed to ( 70 , 96 , 139 ).
Several recent reviews provide additional evidence of the pervasive negative health effects of exposure to discrimination. A 2015 review indicated that self-reported discrimination is related not only to indicators of mental health symptoms and distress but also to defined psychiatric disorders ( 70 ). Moreover, there is growing evidence that self-reported discrimination is associated with preclinical indicators of disease, including increased allostatic load, inflammation, shorter telomere length, coronary artery calcification, dysregulation in cortisol and greater oxidative stress ( 70 ). Linkages between self-reported racial discrimination and physical health outcomes have been documented in multiple recent reviews with research indicating positive associations between reports of discrimination and adverse cardiovascular outcomes ( 72 ), BMI and incidence of obesity ( 12 ), hypertension and nighttime ambulatory blood pressure ( 33 ), engaging in high-risk behaviors ( 40 ), alcohol use and misuse ( 42 ), and poorer sleep ( 111 ). Research also indicates that experiences of discrimination can shape healthcare seeking behaviors and adherence to medical regiments. A 2017 review and meta-analysis of studies on discrimination and health service utilization revealed that perceived discrimination was inversely related to positive experiences with regards to healthcare (e.g., satisfaction with care or perceived quality of care) and reduced adherence to medical regimens and delaying or not seeking healthcare ( 11 ).
Research on stress and health reveals that in addition to stressful experiences affecting health through actual exposure, the threat of exposure as captured by responses of vigilance, worry, rumination and anticipatory stress can prolong the negative effect of stressors and exacerbate the negative effects of stressful experiences on health ( 17 ). Increased attention has been given to capturing vigilance with regards to the threat of discrimination. Several recent studies have used the Heightened Vigilance scale ( 23 ) or a shortened version of it and have found that vigilance about discrimination was positively associated with depressive symptoms ( 66 ), sleep difficulties ( 50 ), and hypertension ( 52 ) and contributed to racial differences for these outcomes. Another recent study with the same measure also found that heightened vigilance was associated with increased waist circumference and BMI among black but not white women ( 51 ). However, these studies have all been cross-sectional and future research using longitudinal study designs would strengthen the evidence for vigilance as a risk factor for health.
Another trend in recent research on discrimination and health is increasing attention to its negative effects on the health and wellbeing of children and adolescents. A 2013 review of discrimination and the health of persons age zero to 18 years old found 121 studies that had examined this association ( 102 ). There were consistent positive associations between self-reported discrimination and indicators of mental health problems, negative health behaviors and physical health outcomes. There is also accumulating evidence that the adverse health effects of discrimination in childhood and adolescence are evident early in life and are a likely contributor to racial inequities in health in young adulthood. For example, a study of black adolescents found that those who reported high levels of discrimination at age 16, 17, and 18 had elevated levels of stress hormones (cortisol, epinephrine and norepinephrine), blood pressure, inflammation and BMI by age 20 ( 16 ).
Research has documented cumulative effects of discrimination on health with greater negative impact evident with increasing levels of exposure to the stress of discrimination. A longitudinal study of ethnic minorities in the United Kingdom identified a dose-response relationship between the accumulation of experiences of discrimination with the deterioration in mental health, with the greatest degree of mental health deterioration evident among those who reported two or more experiences of discrimination at both time points ( 125 ).
Recommendations for Research on Discrimination and Health
As noted, audit studies and other field experiments document the existence of discrimination in many societal institutions and contexts. More concerted efforts are needed to apply knowledge and insights from these studies on the structuring and persistence of discrimination within institutional settings to understand how such discrimination sustains racial disadvantage in ways that shape health outcomes and impact racial health inequities. More generally, despite the burgeoning literature on self-reported discrimination and health, there are some fundamental questions that remain unanswered, including the conditions under which particular aspects of discrimination are related to changes in health status for specific indicators of health status. Such analyses might shed light on findings where the pattern is not uniform. For example, cohort studies have found a positive association ( 9 ), no association ( 2 ) and an inverse association between discrimination and all-cause mortality ( 34 ). The contribution of differences in the assessment of discrimination and in the populations covered to the observed patterns is not well understood.
Prior reviews indicate that the literature on self-reported discrimination and health has been plagued with multiple measurement challenges that probably lead to an underestimation of the actual effects of discrimination on health ( 62 , 135 ). These challenges include identifying the optimal approaches for accurately and comprehensively measuring discrimination and ensuring adequate assessment of key stressful components of discriminatory experiences such as their chronicity, recurrence, severity and duration and distinguishing incidents that are traumatic from those that are not. These challenges remain urgent issues to address in future research.
A limitation of most prior research on discrimination and health is the focus on singular identities of the study participants. Emerging evidence suggests that utilizing an intersectionality framework that examines associations between discrimination and health, with the simultaneous consideration of multiple social categories (e.g., race, sex, gender, SES), leads to larger associations than when only a single social category is considered ( 71 ). Experiences of discrimination should also be considered both for an individual’s self-identified race, as well as for one’s socially assigned race ( 124 ). Recent studies also provide striking evidence of the persistence of discrimination based on skin color within multiple Latino ethicities ( 97 ) and for blacks ( 88 ) suggesting that skin color should be an essential domain of assessing discrimination in future research.
An enhanced understanding of how discrimination combines with other stressors to shape health and racial/ethnic inequities in health is also needed. Self-reported experiences of discrimination do not fully encompass psychosocial stressors linked to non-dominant racial/ethnic status nor the full contribution of racism-related stressors. A study that measured multiple dimensions of discrimination (everyday, major experiences and work discrimination) along with brief measures of childhood adversity, lifetime traumas, recent life events and chronic stressors in the domains of work, finances, relationships and neighborhood, found a graded association between the number of stressors and multiple indicators of morbidity, with each additional stressor associated with worse health ( 115 ). Moreover, stress exposure explained a substantial portion of the residual effect of race/ethnicity after adjustment had been made for SES. Fully capturing stressful exposures for vulnerable populations should also include the assessment of stressors linked to the physical, chemical, and built environment ( 139 ).
Attention should also be given to understanding the contribution of stressors that, at face value, are not linked to racism but that reflect the effects of racism on health. Research on community bereavement shows that structural conditions linked to racism lead to lower life expectancy for blacks compared to whites ( 122 ). As a result, compared to whites, black children are three times as likely to lose a mother by age 10, and black adults are more than twice as likely to lose a child by age 30, and a spouse by age 60. This elevated rate of bereavement and loss of social ties is a stressor that adversely affects levels of social ties and physical and mental health of blacks across the life course ( 119 ). The death of loved ones is included on standard assessments of life events, but its links to racism typically recognized.
Another priority for future research is to better identify the conditions under which vicarious experiences of discrimination can affect health, The term, vicarious discrimination, refers to discriminatory experiences that were not directly experienced by an individual but were faced by others in their network or with whom they identify ( 47 ). A recent systematic review of 30, mainly longitudinal, studies found that that indirect, secondhand exposure to racism was adversely related to child health ( 47 ). The range of contexts in which vicarious discrimination occurs is broad. Recent studies suggest that online discrimination through social media and frequent reports and visualization of incidents of police violence directed towards black, Latino, and Native American communities may also have negative health consequences ( 121 ). A recent, nationally-representative, quasi-experimental study found that each police killing of an unarmed black male Americans worsened mental health among blacks in the general population ( 14 ).
Increased hostility and resentment towards racial and ethnic minority groups and immigrants in the U.S. as well as political polarization associated with the recent presidential election and its aftermath also deserve more research attention ( 138 ). A recent longitudinal study of high school juniors interviewed before and after the presidential election found that many reported concern, worry or stress regarding the increasing hostility and discrimination of people because of their race, immigrant status, religion, or other social factors. A year later, higher concern about discrimination was associated with increases in cigarette smoking, alcohol use, substance use, and greater odds of depression and ADHD ( 69 ).
Future research also needs to better document the role of discrimination, and other dimensions of racism, in accounting for racial disparities in health. Studies from Australia, New Zealand, South Africa and the U.S. have found that self-reports of discrimination make an incremental contribution over and above income and education in accounting for racial/ethnic inequities in health ( 139 ). However, most studies of discrimination neglect to empirically quantify the contribution of discrimination to the patterns and trends of inequities in health.
Interventions
Future research on racism and health needs to give more sustained attention to identifying interventions to reduce and prevent racism, as well as, to ameliorate its adverse health effects. Research on interventions to address the multiple dimensions of racism is still in its infancy ( 94 , 141 ).
Addressing Institutional Racism
Reskin ( 106 ) emphasizes that because racism is a system that consists of a set of dynamically related components or subsystems, disparities in any given domain is a result of processes of reciprocal causality across multiple subsystems. Accordingly, interventions should address the interrelated mechanisms and critical leverage points through which racism operates, and explicitly design multi-level interventions to get at the multiple processes of racism simultaneously. The systemic nature of racism implies that effective solutions to addressing racism need to be comprehensive and emphasize upstream/structural/institutional interventions ( 142 ). The civil rights policies of the 1960s are prime examples of race-targeted policies that that improved socioeconomic opportunities and living conditions, narrowed the black-white economic gap between the mid 1960s and the late 1970s and reduced health inequities ( 3 , 4 , 26 , 45 , 58 ). Interventions to improve household income, education and employment opportunities, and housing and neighborhood conditions have also demonstrated health benefits ( 141 ).
Additional income to households with modest economic resources suggests that added financial resources are associated with improved health ( 141 ). The Great Smoky Mountains Study was a natural experiment that assessed the impact of extra income received by American Indian households due to the opening of a Casino, on the health of Native youth ( 27 ). The study found declining rates of deviant and aggressive behavior among adolescents whose families received additional income; and increases in formal education and declines in the incidence of minor criminal offenses in young adulthood, and the elimination of Native American-white disparities on both of these outcomes ( 1 ). The Abecedarian project that randomized economically disadvantaged children, birth to 5 years of age, most of them Black, to an early childhood nurturing program also illustrates that interventions efforts at an early age can be beneficial ( 19 ). By their mid 30s, the intervention group had lower levels of multiple risk factors for cardiovascular disease than the controls. Community initiatives and efforts to build community capacity around racism may also have the potential to improve health ( 140 , 141 ). One study demonstrated that cultural empowerment among Native communities, in the form of civil and governmental sovereignty and the presence of a building for cultural activities, had a strong inverse relationship with youth suicide ( 22 ).
Addressing Cultural Racism
Most interventions aimed at reducing cultural racism focus on addressing implicit biases or enhancing cultural competence. A recent review found that cultural competency interventions can lead to improvements in provider knowledge, skills and attitudes regarding cultural competency and health care access and utilization, but there is little evidence that these interventions affect health outcomes and health equity ( 118 ). While extensive evidence documents that healthcare students and professionals have an anti-black there are no effective interventions to reduce this bias among providers ( 76 ). However, Devine and colleagues documented that a comprehensive program that deployed multiple strategies to reduce implicit biases found a sustained reduction in implicit biases in nonblack undergraduate students three months after the program began ( 29 ). Future research needs to assess the generalizability of the effects of this intervention to other groups.
Interventions, targeted at individuals, that seek to neutralize cultural racism have shown positive socioeconomic and health benefits. Values affirmation interventions (in which youth enhance their sense of self-worth by reflecting on and writing about their most important value) and social belonging interventions (which create a sense of relatedness) have been shown to markedly improve academic performance and health of stigmatized racial groups ( 24 ). There is an emerging body of evidence that suggests that similar self-affirmation strategies can enhance an individual’s capacity to cope with stressful situations and lead to improved health behaviors ( 24 ).
Addressing Discrimination
Effective strategies can be deployed to reduce discrimination against individuals that occur within institutional contexts. For example, in the employment domain, research reveals that discrimination can be reduced and the proportion of under-represented groups markedly increased through organizational policy changes that require mandatory programs, or programs with explicit authority and accountability that are supported by organizational leadership and rigorously monitored ( 57 ). Discrimination can also be minimized in employment decisions by having applications reviewed with the names of the applicants removed from the application package ( 61 ). Many interventions targeting interpersonal discrimination focus on reductions in prejudice and stereotyping through increased interracial contact. However, evidence in support of the contact theory of prejudice indicates that reductions in prejudice and discrimination are observed only when groups meet specific conditions: they are equivalent in status, have shared goals, cooperate to achieve shared goals, and have the support of authority figures ( 98 ).
Research on interpersonal discrimination also suggests that coping strategies and resources (such as social ties, religious involvement and optimism) can mitigate at least some of the detrimental effects of racial discrimination on health ( 70 ). Racial identity is another promising strategy but studies have found both protective and exacerbating effects of identity ( 144 ). At the present time, we do not clearly understand the determinants of discrepant findings and the conditions under which specific aspects of identity have positive or negative effects for particular indicators of health for specific population subgroups.

Needed Research On Interventions
Although there is emerging evidence that a broad range of strategies may reduce certain aspects of racism and enhance racial equity, there is still a lot that we do not understand. For example, interventions that have improved neighborhood and housing conditions have been implemented on a small scale and they have yet to seriously address either residential racial segregation or the concentration of poverty in the metropolitan areas in which they have been implemented. Residential segregation has been identified as a leverage point or fundamental causal mechanism by which institutional racism creates and sustains racial economic inequities ( 106 , 136 ). Thus, dismantling the core institutional mechanisms of segregation will require scaling up interventions that address its key underlying mechanisms. Relatedly, we lack the empirical evidence to identify which mechanisms of segregation (e.g., educational opportunity, labor market, housing quality) should be tackled first, would have the largest impact, and is most likely to trigger ripple effects to other pathways.
Research also needs to identify if and when observed health effects of reducing racism would be larger if comprehensive, multi-level intervention strategies (instead of interventions targeted at a single level) were deployed to neutralize the negative impact of the pathogenic effects of racism. For example, we are unaware whether we would observe larger positive effects if interventions focused on upstream interventions (e.g., in housing, education and additional income) were combined with an individual-level targeted strategy such as a self-affirmation intervention ( 24 ). Relatedly, interventions need to be evaluated for the extent to which they may be differentially effective across various subgroups of the population. The cost-effectiveness of interventions also needs to be assessed for population subgroups.
Taking the systemic nature of racism seriously also highlights that it is deeply embedded in other political, economic and cultural structures of society and that many powerful societal actors are likely to be resistant to change because they currently benefit from the status quo. Research to advance an agenda to dismantle racism and its negative effects must invest in studies that delineate how to overcome societal inertia, increase empathy for stigmatized racial/ethnic populations, build political will and identify optimal communication strategies to raise public and stakeholder awareness of the societal benefits of racial equity agenda ( 142 ).
Cross-Cutting Issues
Much of the research described in this review has focused on a single mechanism of racism (structural/institutional, cultural, discrimination) through which racism may influence health. Differentiating between these mechanisms allows researchers to clarify potential pathways, measure outcomes, and explore interventions. However, the impact of addressing a single dimension of racism will be diminished by the system of racial oppression which interacts across sectors and domains of racism. Tying together interconnected data on health and racism will be critical for health disparities researchers moving forward. Some emerging topics lend themselves to this multi-dimensional, cross-cutting research—allowing investigators to better understand and address the systemic nature of racism. Priority topics include studying the effects of racism throughout the life course, understanding the potential intergenerational effects of racism, and the impact of racism on white people.
Understanding Racism across the Life Course
Life course research aims to examine how early exposures, such as lead poisoning in utero, or adversity in early childhood, can impact health in adulthood. This perspective can incorporate early context, sensitivity and latency periods, the accumulation of risk over time, and etiologic origins of disease ( 39 ). When examining racism as an exposure, understanding how individuals encounter racism across the life course is one example of a cross-cutting issue in need of more research ( 38 , 39 , 128 ). A life course approach can begin to unpack how exposures to interpersonal, cultural, and structural racism may evolve and relate to each other across developmental stages, as individuals interact with their neighborhoods and educational systems, and health care systems ( 106 ). A recent study, for example, documented a relationship between early childhood lead exposure and adult incarceration ( 108 ). It is likely that multiple mechanisms of racism could have combined, additively and interactively over time, to undergird this association ( 78 ). Life course approaches are also important for determining how and when it is most opportune to intervene on racism. The Great Smoky Mountains Study found that providing additional income to Native American households led to a reduction in adolescent risk behaviors, but only among those who were the youngest when the income supplements began, and who thus had the longest period of exposure ( 27 ). A life course approach can identify key periods of increased risk as well as opportunities for intervention and resilience.
Intergenerational Transmission of Racism’s Effects
An extension of the life course perspective is a focus on the impact of intergenerational transmission of the effects of racism, from parent to offspring. Though still in its infancy, research on the intergenerational transmission of racism could enhance and clarify observational research which posits that descendants of survivors of mass and targeted trauma experience grief and other mental, behavioral, and somatic symptoms akin to what would might be expected if the trauma was witnessed directly ( 48 ). Long-term adverse health impacts linked to Jim Crow laws illustrate the long reach of institutional racism ( 63 ). Studies of children of Holocaust survivors and multiple generations of Native Americans suggest a link between these racialized traumatic experiences and the well-being of future generations ( 119 ). Possible pathways include the effects of parenting and community norms, the transfer of resources (i.e. wealth, land), and potentially, heritable and non-heritable epigenetic changes caused by external stressors ( 126 ). Differential DNA methylation is one type of epigenetic difference that has been found among adult children of holocaust survivors, which may affect gene expression at the methylated loci ( 119 ). Concerted new research efforts are needed to provide a more nuanced understanding of how racialized experiences are embodied for future generations.
Racism and the Health of Whites
There is growing scientific interest in how the system of racism can have both positive and negative effects on the health of whites ( 77 ). Whites as a whole have better health than the historically oppressed groups in the U.S., but they are less healthy than whites in other advanced economies. Inadequate attention has been given to delineating the ways in which racism could simultaneously advantage whites compared to other racial groups in the U.S. while creating conditions that are inimical to the health of all groups, including disadvantaging large segments of the white population, and imposing ceilings that prevent many middle class whites from attaining a level of good health seen elsewhere ( 77 ). For example, racial animus towards blacks has led to white opposition to a broad range of social programs, including the Affordable Care Act, which would benefit a large proportion of whites ( 116 ). In addition, while research on internalized racism has heavily focused on its potential negative health effects on members of racial and ethnic minority groups, whites also have high levels of internalized racism (that is, internalized racial superiority) that could affect how whites respond to economic adversity perhaps contribute to increasing rates of “deaths of despair” among low SES whites ( 77 , 105 ). Research on self-reported discrimination and hqealth has also observed negative effects of such experiences among whites ( 70 ). It is not clear that all whites are equally vulnerable. One study found that discrimination adversely affected only whites who were male and who belonged to ethnic subgroups with a history of discrimination (Polish, Irish, Italian or Jewish) ( 54 ). Another study found that discrimination based on class helped to explain SES differences in allostatic load in a sample of white adolescents ( 36 ). Concerted attention should be given to the myriad ways in which various aspects of racism can have positive and negative effects on the health of whites and particular subgroups of whites.
Conclusions
The study of contemporary racism and its impact on health is complex, as manifestations of structural, cultural, and interpersonal racism adapt to changes in technology, cultural norms, and political events. This body of research illustrates the myriad ways in which the larger social environment can get under the skin to drive health and inequities in health. While there is much that we yet need to learn, the quality and quantity of research continues to increase in this area and there is an acute need for increased attention to identifying the optimal interventions to reduce and eliminate the negative effects of racism on health. Understanding and effectively addressing the ways in which racism affects health is critical to improving population health and to making progress in reducing large and often intractable racial inequities in health.
Acknowledgments
Preparation of this paper was supported by grant U19 AG 051426 from the National Institute of Aging. We wish to thank Sandra Krumholz for her assistance with preparing the manuscript.
Literature Cited
- 1. Akee RKQ, Copeland WE, Keeler G, Angold A, Costello EJ. 2010. Parents’ Incomes and Children’s Outcomes: A Quasi-experiment Using Transfer Payments from Casino Profits. American Economic Journal: Applied Economics 2: 86–115 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Albert MA, Cozier Y, Ridker PM, Palmer JR, Glynn RJ, et al. 2010. Perceptions of Race/Ethnic Discrimination in Relation to Mortality Among Black Women: Results From the Black Women’s Health Study. Archives of internal medicine 170: 896–904 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Almond D, Chay KY. 2006. The Long-Run and Intergenerational Impact of Poor Infant Health: Evidence from Cohorts Born During the Civil Rights Era manuscript, UC Berkeley Department of Economics. [ Google Scholar ]
- 4. Almond D, Chay KY, Greenstone M. 2006. Civil Rights, the War on Poverty, and Black-White Convergence in Infant Mortality in the Rural South and Mississippi, MIT Dept of Economics Working Paper Series [ Google Scholar ]
- 5. Arias E, Xu J, Jim MA. 2014. Period life tables for the non-Hispanic American Indian and Alaska Native population, 2007–2009. Am J Public Health 104 Suppl 3: S312–9 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Aronson J, Burgess D, Phelan SM, Juarez L. 2013. Unhealthy interactions: The role of stereotype threat in health disparities. American journal of public health 103: 50–56 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. 2017. Structural racism and health inequities in the USA: evidence and interventions. The Lancet 389: 1453–63 [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Barkan SE. 2018. Measuring Perceived Mistreatment: Potential Problems in Asking About “Discrimination”. Sociological Inquiry 88: 245–53 [ Google Scholar ]
- 9. Barnes LL, Mendes de Leon CF, Lewis TT, Bienias JL, Wilson RS, Evans DA. 2008. Perceived Discrimination and Mortality in a Population-based Study of Older Adults. American journal of public health 98: 1241–47 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Becares L, Nazroo J, Jackson J, Heuvelman H. 2012. Ethnic density effects on health and experienced racism among Caribbean people in the US and England: a cross-national comparison. Soc Sci Med 75: 2107–15 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Ben J, Cormack D, Harris R, Paradies Y. 2017. Racism and health service utilisation: A systematic review and meta-analysis. PloS one 12: e0189900. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Bernardo CdO, Bastos JL, González‐Chica DA, Peres MA, Paradies YC 2017. Interpersonal discrimination and markers of adiposity in longitudinal studies: a systematic review. Obesity Reviews 18: 1040–49 [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Bonilla-Silva E 1997. Rethinking racism: Toward a structural interpretation. American sociological review: 465–80
- 14. Bor J, Venkataramani AS, Williams DR, Tsai AC. 2018. Police killings and their spillover effects on the mental health of black Americans: a population-based, quasi-experimental study. In Lancet doi: 10.1016/S0140-6736(18)31130-9. [ DOI ] [ PMC free article ] [ PubMed ]
- 15. Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. 2010. Socioeconomic disparities in health in the United States: what the patterns tell us. American journal of public health 100: S186–S96 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Brody GH, Lei MK, Chae DH, Yu T, Kogan SM, Beach SRH. 2014. Perceived discrimination among African American adolescents and allostatic load: a longitudinal analysis with buffering effects. Child Dev 85: 989–1002 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Brosschot JF, Gerin W, Thayer JF. 2006. The perservative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychosomatic Research 60: 113–24 [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Burkley M, Burkley E, Andrade A, Bell AC. 2017. Symbols of pride or prejudice? Examining the impact of Native American sports mascots on stereotype application. The Journal of social psychology 157: 223–35 [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Campbell FA, Conti G, Heckman JJ, Moon SH, Pinto R, et al. 2014. Early childhood investments substantially boost adult health. Science 343: 1478–85 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Chae DH, Clouston S, Hatzenbuehler ML, Kramer MR, Cooper HLF, et al. 2015. Association between an internet-based measure of area racism and black mortality. PLoS ONE 10 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. Chae DH, Clouston S, Martz CD, Hatzenbuehler ML, Cooper HLF, et al. 2018. Area racism and birth outcomes among Blacks in the United States. Social Science & Medicine 199: 49–55 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Chandler MJ, Lalonde C. 1998. Cultural Continuity as a Hedge against Suicide in Canada’s First Nations. Transcultural Psychiatry 35: 191–219 [ Google Scholar ]
- 23. Clark R, Benkert RA, Flack JM. 2006. Large arterial elasticity varies as a function of gender and racism-related vigilance in black youth. Journal of Adolescent Health 39: 562–69 [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Cohen GL, Sherman DK. 2014. The Psychology of Change: Self-Affirmation and Social Psychological Intervention. Annual Review of Psychology 65: 222–71 [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, et al. 2012. The Associations of Clinicians’ Implicit Attitudes About Race With Medical Visit Communication and Patient Ratings of Interpersonal Care. American Journal of Public Health 102: 979–87 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Cooper RS, Steinhauer M, Schatzkin A, Miller W. 1981. Improved mortality among U.S. blacks, 1968–1978: The role of antiracist struggle. International Journal of Health Services 11: 511–22 [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Costello EJ, Erkanli A, Copeland W, Angold A. 2010. Association of Family Income Supplements in Adolescence With Development of Psychiatric and Substance Use Disorders in Adulthood Among an American Indian Population. The Journal of the American Medical Association 303: 1954–60 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Cutler DM, Glaeser EL. 1997. Are ghettos good or bad? The Quarterly Journal of Economics 112: 827–72 [ Google Scholar ]
- 29. Devine PG, Forscher PS, Austin AJ, Cox WTL. 2012. Long-term reduction in implicit race bias: A prejudice habit-breaking intervention. Journal of experimental social psychology 48: 1267–78 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. Diez Roux AV. 2011. Complex systems thinking and current impasses in health disparities research. Am J Public Health 101: 1627–34 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Do DP, Frank R, Iceland J. 2017. Black-white metropolitan segregation and self-rated health: Investigating the role of neighborhood poverty. Social Science & Medicine 187: 85–92 [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Do DP, Frank R, Zheng C, Iceland J. 2017. Hispanic Segregation and Poor Health: It’s Not Just Black and White. American journal of epidemiology 186: 990–99 [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Dolezsar CM, McGrath JJ, Herzig AJM, Miller SB. 2014. Perceived racial discrimination and hypertension: A comprehensive systematic review. Health Psychology 33: 20–34 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 34. Dunlay SM, Lippmann SJ, Greiner MA, O’Brien EC, Chamberlain AM, et al. 2017. Perceived Discrimination and Cardiovascular Outcomes in Older African Americans: Insights from the Jackson Heart Study. Mayo Clinic proceedings 92: 699–709 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 35. Fryberg SA, Markus HR, Oyserman D, Stone JM. 2008. Of warrior chiefs and Indian princesses: The psychological consequences of American Indian mascots. Basic and Applied Social Psychology 30: 208–18 [ Google Scholar ]
- 36. Fuller-Rowell TE, Evans GW, Ong AD. 2012. Poverty and Health: The Mediating Role of Perceived Discrimination. Psychological Science 23: 734–39 [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Gebremariam M, Nianogo R, Arah O. 2018. Weight gain during incarceration: systematic review and meta‐analysis. Obesity Reviews 19: 98–110 [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Gee GC, Ford CL. 2011. Structural racism and health inequities: old issues, new directions. Du Bois review: social science research on race 8: 115–32 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 39. Gee GC, Walsemann KM, Brondolo E. 2012. A life course perspective on how racism may be related to health inequities. American Journal of Public Health 102: 967–74 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 40. Gibbons FX, Stock ML. 2017. Perceived Racial Discrimination and Health Behavior: Mediation and Moderation. In The Oxford Handbook of Stigma, Discrimination, and Health, ed. Major B, Dovidio JF, Link BG, pp. 355–77. New York: Oxford University Press [ Google Scholar ]
- 41. Gibbons FX, Stock ML. 2017. Perceived Racial Discrimination and Health Behavior: Mediation and Moderation: Oxford University Press [ Google Scholar ]
- 42. Gilbert PA, Zemore SE. 2016. Discrimination and drinking: A systematic review of the evidence. Social Science & Medicine 161: 178–94 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Glaeser E, Vigdor J. 2012. The end of the segregated century: Racial separation in America’s neighborhoods, 1890–2010. Rep. 66, Manhattan Institute for Policy Research New York [ Google Scholar ]
- 44. Glaeser EL, Vigdor JL. 2001. Racial segregation in the 2000 Census: Promising news, The Brookings Institution, Washington, DC [ Google Scholar ]
- 45. Hahn R, Truman B, Williams D. 2018. Civil rights as determinants of public health and racial and ethnic health equity: Health care, education, employment, and housing in the United States. SSM-population health 4: 17–24 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 46. Hatzenbuehler ML, Prins SJ, Flake M, Philbin M, Frazer MS, et al. 2017. Immigration policies and mental health morbidity among Latinos: A state-level analysis. Soc Sci Med 174: 169–78 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 47. Heard-Garris NJ, Cale M, Camaj L, Hamati MC, Dominguez TP. 2018. Transmitting Trauma: A systematic review of vicarious racism and child health. Social Science & Medicine 199: 230–40 [ DOI ] [ PubMed ] [ Google Scholar ]
- 48. Heart MYHB, DeBruyn LM. 1998. The American Indian holocaust: Healing historical unresolved grief. American Indian and Alaska native mental health research 8: 56. [ PubMed ] [ Google Scholar ]
- 49. Hicken MT, Kravitz-Wirtz N, Durkee M, Jackson JS. 2018. Racial inequalities in health: Framing future research. Soc Sci Med 199: 11–18 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Hicken MT, Lee H, Ailshire J, Burgard SA, Williams DR. 2013. “Every shut eye, ain’t sleep”: The role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race and social problems 5: 100–12 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 51. Hicken MT, Lee H, Hing AK. 2018. The weight of racism: Vigilance and racial inequalities in weight-related measures. Social science & medicine 199: 157–66 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 52. Hicken MT, Lee H, Morenoff J, House JS, Williams DR. 2014. Racial/ethnic disparities in hypertension prevalence: reconsidering the role of chronic stress. American journal of public health 104: 117–23 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 53. House JS, Kessler RC, Herzog AR, Mero R, Kinney A, Breslow M. 1990. Age, socioeconomic status, and health. Milbank Quarterly 68: 383–411 [ PubMed ] [ Google Scholar ]
- 54. Hunte HE, Williams DR. 2009. The association between perceived discrimination and obesity in a population-based multiracial and multiethnic adult sample. Am J Public Health 99: 1285–92 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 55. Jones JM. 1997. Prejudice and racism 2nd ed. New York: McGraw Hill [ Google Scholar ]
- 56. Kaestner R, Pearson JA, Keene D, Geronimus AT. 2009. Stress, Allostatic Load, and Health of Mexican Immigrants. Social Science Quarterly 90: 1089–111 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 57. Kalev A, Dobbin F, Kelly E. 2006. Best practices or best guesses? Assessing the efficacy of corporate affirmative action and diversity policies. American sociological review 71: 589–617 [ Google Scholar ]
- 58. Kaplan GA, Ranjit N, Burgard S. 2008. Lifting Gates--Lengthening Lives: Did Civil Rights Policies Improve the Health of African-American Woman in the 1960s and 1970s? In Making Americans Healthier: Social and Economic Policy as Health Policy, ed. Schoeni RF, House JS, Kaplan GA, Pollack H, pp. 145–69. New York: Russell Sage Foundation Publications [ Google Scholar ]
- 59. Kessler RC, Mickelson KD, Williams DR. 1999. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of health and social behavior 40: 208–30 [ PubMed ] [ Google Scholar ]
- 60. Kramer MR, Hogue CR. 2009. Is segregation bad for your health? Epidemiologic reviews 31: 178–94 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 61. Krause A, Rinne U, Zimmermann KF. 2012. Anonymous job applications in Europe. IZA Journal of European Labor Studies 1: 5 [ Google Scholar ]
- 62. Krieger N 2014. Discrimination and health inequities. Int J Health Serv 44: 643–710 [ DOI ] [ PubMed ] [ Google Scholar ]
- 63. Krieger N, Chen JT, Coull BA, Beckfield J, Kiang MV, Waterman PD. 2014. Jim Crow and premature mortality among the US black and white population, 1960–2009: an age–period–cohort analysis. Epidemiology (Cambridge, MA) 25: 494–504 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 64. Krysan M, Farley R, Couper MP. 2008. In the eye of the beholder: Racial beliefs and residential segregation. Du Bois Review 5: 5–26 [ Google Scholar ]
- 65. Landrine H, Corral I, Lee JG, Efird JT, Hall MB, Bess JJ. 2017. Residential Segregation and Racial Cancer Disparities: A Systematic Review. Journal of racial and ethnic health disparities 4: 1195–205 [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. LaVeist TA, Thorpe RJ Jr., Pierre G, Mance GA, Williams DR 2014. The Relationships among Vigilant Coping Style, Race, and Depression. Journal of Social Issues 70: 241–55 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 67. Lee H, Wildeman C, Wang EA, Matusko N, Jackson JS. 2014. A heavy burden: the cardiovascular health consequences of having a family member incarcerated. Am J Public Health 104: 421–7 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 68. Leitner JB, Hehman E, Ayduk O, Mendoza-Denton R. 2016. Blacks’ Death Rate Due to Circulatory Diseases Is Positively Related to Whites’ Explicit Racial Bias. Psychol Sci 27: 1299–311 [ DOI ] [ PubMed ] [ Google Scholar ]
- 69. Leventhal AM Cho J Andrabi N Barrington-Trimis J 2018. Association of Reported Concern Over Increasing Societal Discrimination and Adverse Behavioral Health Outcomes in Late Adolescence, 2016–2017. JAMA Pediatrics, In Press [ DOI ] [ PMC free article ] [ PubMed ]
- 70. Lewis TT, Cogburn CD, Williams DR. 2015. Self-Reported Experiences of Discrimination and Health: Scientific Advances, Ongoing Controversies, and Emerging Issues. Annual Review of Clinical Psychology 11: 407–40 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 71. Lewis TT, Van Dyke ME. 2018. Discrimination and the Health of African Americans: The Potential Importance of Intersectionalities. Current Directions in Psychological Science 27: 176–82 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 72. Lewis TT, Williams DR, Tamene M, Clark CR. 2014. Self-Reported Experiences of Discrimination and Cardiovascular Disease. Curr Cardiovasc Risk Rep 8: 365. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 73. Lieberson S 1985. Making it Count: The Improvement of Social Research and Theory Berkeley: Univiversity of California Press [ Google Scholar ]
- 74. Link BG, Phelan J. 1995. Social Conditions As Fundamental Causes of Disease. Journal of Health and Social Behavior Special Issue: 80–94 [ PubMed ]
- 75. Lukachko A, Hatzenbuehler ML, Keyes KM. 2014. Structural racism and myocardial infarction in the United States. Soc Sci Med 103: 42–50 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 76. Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. 2018. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Social Science and Medicine 199: 219–29 [ DOI ] [ PubMed ] [ Google Scholar ]
- 77. Malat J, Mayorga-Gallo S, Williams DR. 2017. The effects of whiteness on the health of whites in the USA. Social Science & Medicine 199: 148–56 [ DOI ] [ PubMed ] [ Google Scholar ]
- 78. Mallett CA. 2016. The school-to-prison pipeline: A critical review of the punitive paradigm shift. Child and adolescent social work journal 33: 15–24 [ Google Scholar ]
- 79. Margerison-Zilko C, Perez-Patron M, Cubbin C. 2017. Residential segregation, political representation, and preterm birth among U.S.- and foreign-born Black women in the U.S. 2008–2010. Health Place 46: 13–20 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 80. Martinez O, Wu E, Sandfort T, Dodge B, Carballo-Dieguez A, et al. 2015. Evaluating the impact of immigration policies on health status among undocumented immigrants: a systematic review. Journal of Immigrant and Minority Health 17: 947–70 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 81. Massey DS. 2004. Segregation and stratification: a biosocial perspective. Du Bois Review 1: 7–25 [ Google Scholar ]
- 82. Massey DS. 2016. Segregation and the Perpetuation of Disadvantage. In The Oxford Handbook of the Social Science of Poverty, ed. Brady D, Burton LM New York: Oxford University Press [ Google Scholar ]
- 83. Massey DS, Denton NA. 1988. The dimensions of residential segregation. Social forces 67: 281–315 [ Google Scholar ]
- 84. Mauer M, Huling T. 1995. Young black Americans and the criminal justice system: Five years later, The Sentencing Project [ Google Scholar ]
- 85. Mehra R, Boyd LM, Ickovics JR. 2017. Racial residential segregation and adverse birth outcomes: A systematic review and meta-analysis. Social Science & Medicine 191: 237–50 [ DOI ] [ PubMed ] [ Google Scholar ]
- 86. Mendez DD, Hogan VK, Culhane JF. 2014. Institutional racism, neighborhood factors, stress, and preterm birth. Ethnicity & health 19: 479–99 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 87. Miranda ML, Maxson P, Edwards S. 2009. Environmental contributions to disparities in pregnancy outcomes. Epidemiol Rev 31: 67–83 [ DOI ] [ PubMed ] [ Google Scholar ]
- 88. Monk EP Jr. 2015. The Cost of Color: Skin Color, Discrimination, and Health among African-Americans. American Journal of Sociology 121: 396–444 [ DOI ] [ PubMed ] [ Google Scholar ]
- 89. Morey BN, Gee GC, Muennig P, Hatzenbuehler ML. 2018. Community-level prejudice and mortality among immigrant groups. Social Science and Medicine 199: 56–66 [ DOI ] [ PubMed ] [ Google Scholar ]
- 90. Novak NL, Geronimus AT, Martinez-Cardoso AM. 2017. Change in birth outcomes among infants born to Latina mothers after a major immigration raid. Int J Epidemiol 46: 839–49 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 91. Orfield G, Frankenberg E, Garces LM. 2008. Statement of American social scientists of research on school desegregation to the US Supreme Court in Parents v. Seattle School District and Meredith v. Jefferson County. The Urban Review 40: 96–136 [ Google Scholar ]
- 92. Orr MG, Kaplan GA, Galea S. 2016. Neighbourhood food, physical activity, and educational environments and black/white disparities in obesity: a complex systems simulation analysis. J Epidemiol Community Health 70: 862–7 [ DOI ] [ PubMed ] [ Google Scholar ]
- 93. Pager D, Shepherd H. 2008. The Sociology of Discrimination: Racial Discrimination in Employment, Housing, Credit, and Consumer Markets. Annual Review of Sociology 34: 181–209 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 94. Paradies Y 2005. Anti-Racism and Indigenous Australians. Analyses of Social Issues and Public Policy 5: 1–28 [ Google Scholar ]
- 95. Paradies Y, Ben J, Denson N, Elias A, Priest N, et al. 2015. Racism as a Determinant of Health: A Systematic Review and Meta-Analysis. PLOS ONE 10: 1–48 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 96. Pascoe EA, Richman LS. 2009. Perceived Discrimination and Health: A Meta-Analytic Review. Psychological Bulletin 135: 531–54 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 97. Perreira KM, Telles EE. 2014. The color of health: Skin color, ethnoracial classification, and discrimination in the health of Latin Americans. Social Science & Medicine 116: 241–50 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 98. Pettigrew TF, Tropp LR. 2006. A meta-analytic test of intergroup contact theory. Journal of Personality and Social Psychology 90: 751–83 [ DOI ] [ PubMed ] [ Google Scholar ]
- 99. Phelan JC, Link BG. 2015. Is Racism a Fundamental Cause of Inequalities in Health? Annual Review of Sociology 41: 311–30 [ Google Scholar ]
- 100. Phelan JC, Link BG, Tehranifar P. 2010. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav 51 Suppl: S28–40 [ DOI ] [ PubMed ] [ Google Scholar ]
- 101. Pool LR, Carnethon MR, Goff DC Jr., Gordon-Larsen P, Robinson WR, Kershaw KN 2018. Longitudinal Associations of Neighborhood-level Racial Residential Segregation with Obesity Among Blacks. Epidemiology 29: 207–14 [ DOI ] [ PubMed ] [ Google Scholar ]
- 102. Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. 2013. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Social Science & Medicine 95: 115–27 [ DOI ] [ PubMed ] [ Google Scholar ]
- 103. Priest N, Slopen N, Woolford S, Philip JT, Singer D, et al. Forthcoming. Stereotyping across intersections of race and age: Racial stereotyping among White adults working with children. PLoS One [ DOI ] [ PMC free article ] [ PubMed ]
- 104. Priest N, Williams DR. 2017. Racial Discrimination and Racial Disparities in Health. In The Oxford Handbook of Stigma, Discrimination, and Health, ed. Major B, Dovidio JF, Link BG, pp. 163–82. New York: Oxford University Press [ Google Scholar ]
- 105. Pyke KD. 2010. What is internalized racial oppression and why don’t we study it? Acknowledging racism’s hidden injuries. Sociological Perspectives 53: 551–72 [ Google Scholar ]
- 106. Reskin B 2012. The race discrimination system. Annual Review of Sociology 38: 17–35 [ Google Scholar ]
- 107. Rothstein R 2017. The color of law: A forgotten history of how our government segregated America New York; London: Liveright Publishing [ Google Scholar ]
- 108. Sampson RJ, Winter AS. 2018. Poisoned development: assessing childhood lead exposure as a cause of crime in a birth cohort followed through adolescence. Criminology 56: 269–301 [ Google Scholar ]
- 109. Schmitt MT, Branscombe NR, Postmes T, Garcia A. 2014. The consequences of perceived discrimination for psychological well-being: a meta-analytic review. Psychol Bull 140: 921–48 [ DOI ] [ PubMed ] [ Google Scholar ]
- 110. Semega JL, Fontenot Kayla R, and Kollar Melissa A. 2017. U.S. Census Bureau, Current Population Reports, P60–259, Income and Poverty in the United States: 2016 Washington D.C: U.S. Government Printing Office [ Google Scholar ]
- 111. Slopen N, Lewis TT, Williams DR. 2016. Discrimination and sleep: a systematic review. Sleep Medicine 18: 88–95 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 112. Smedley BD, Stith AY, Nelson AR. 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care Washington, DC: National Academy Press; [ PubMed ] [ Google Scholar ]
- 113. Speight SL. 2007. Internalized Racism: One More Piece of the Puzzle. The Counseling Psychologist 35: 126–34 [ Google Scholar ]
- 114. Spencer SJ, Logel C, Davies PG. 2016. Stereotype Threat. Annual Review of Psychology 67: 415–37 [ DOI ] [ PubMed ] [ Google Scholar ]
- 115. Sternthal MJ, Slopen N, Williams DR. 2011. Racial disparities in health: how much does stress really matter? Du Bois Review: Social Science Research on Race 8: 95–113 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 116. Tesler M 2012. The spillover of racialization into health care: How President Obama polarized public opinion by racial attitudes and race. American Journal of Political Science 56: 690–704 [ Google Scholar ]
- 117. Toomey RB, Umaña-Taylor AJ, Williams DR, Harvey-Mendoza E, Jahromi LB, Updegraff KA. 2014. Impact of Arizona’s SB 1070 Immigration Law on Utilization of Health Care and Public Assistance Among Mexican-Origin Adolescent Mothers and Their Mother Figures. American Journal of Public Health 104: S28–S34 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 118. Truong M, Paradies Y, Priest N. 2014. Interventions to improve cultural competency in healthcare: a systematic review of reviews. BMC Health Services Research 14: 99–99 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 119. Turecki G, Meaney MJ. 2016. Effects of the social environment and stress on glucocorticoid receptor gene methylation: a systematic review. Biological psychiatry 79: 87–96 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 120. U.S. Census Bureau. 2014. Wealth, Asset Ownership, & Debt of Household Detailed Tables: 2011 https://www.census.gov/data/tables/2011/demo/wealth/wealth-asset-ownership.html Washington DC: U.S. Department of Commerce [ Google Scholar ]
- 121. Umana-Taylor AJ, Tynes BM, Toomey RB, Williams DR, Mitchell KJ. 2015. Latino adolescents’ perceived discrimination in online and offline settings: an examination of cultural risk and protective factors. Dev Psychol 51: 87–100 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 122. Umberson D 2017. Black Deaths Matter: Race, Relationship Loss, and Effects on Survivors. J Health Soc Behav 58: 405–20 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 123. van Ryn M, Burgess DJ, Dovidio JF, Phelan SM, Saha S, et al. 2011. The impact of racism on clinician cognition, behavior, and clinical decision making. Du Bois Review 8: 199–218 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 124. Vargas ED, Winston NC, Garcia JA, Sanchez GR. 2016. Latina/o or Mexicana/o? The relationship between socially assigned race and experiences with discrimination. Sociology of Race and Ethnicity 2: 498–515 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 125. Wallace S, Nazroo J, Bécares L. 2016. Cumulative Effect of Racial Discrimination on the Mental Health of Ethnic Minorities in the United Kingdom. American Journal of Public Health 106: 1294–300 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 126. Walters KL, Mohammed SA, Evans-Campbell T, Beltrán RE, Chae DH, Duran B. 2011. Bodies don’t just tell stories, they tell histories: Embodiment of historical trauma among American Indians and Alaska Natives. Du Bois Review: Social Science Research on Race 8: 179–89 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 127. White K, Blackburn J, Manzella B, Welty E, Menachemi N. 2014. Changes in use of county public health services following implementation of Alabama’s immigration law. J Health Care Poor Underserved 25: 1844–52 [ DOI ] [ PubMed ] [ Google Scholar ]
- 128. White K, Borrell LN. 2011. Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health & place 17: 438–48 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 129. White K, Haas JS, Williams DR. 2012. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health services research 47: 1278–99 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 130. Wildeman C, Wang EA. 2017. Mass incarceration, public health, and widening inequality in the USA. The Lancet 389: 1464–74 [ DOI ] [ PubMed ] [ Google Scholar ]
- 131. Williams AD, Wallace M, Nobles C, Mendola P. 2018. Racial residential segregation and racial disparities in stillbirth in the United States. Health & place 51: 208–16 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 132. Williams DR. 1990. Socioeconomic differentials in health: A review and redirection. Social psychology quarterly: 81–99
- 133. Williams DR. 1997. Race and health: Basic questions, emerging directions. Annals of Epidemiology 7: 322–33 [ DOI ] [ PubMed ] [ Google Scholar ]
- 134. Williams DR. 2012. Miles to go before we sleep: Racial inequities in health. Journal of health and social behavior 53: 279–95 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 135. Williams DR. 2016. Improving the measurement of self-reported racial discrimination: Challenges and opportunities. In The cost of racism for people of color: Contextualizing experiences of discrimination ed. Alvarez Alvin N., Liang Christopher T. H., Neville Helen A., pp. 55–83. Washington, DC: American Psychological Association [ Google Scholar ]
- 136. Williams DR, Collins C. 2001. Racial residential segregation: a fundamental cause of racial disparities in health. Public health reports 116: 404. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 137. Williams DR, Gonzalez HM, Williams S, Mohammed SA, Moomal H, Stein DJ. 2008. Perceived discrimination, race and health in South Africa. Soc Sci Med 67: 441–52 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 138. Williams DR, Medlock MM. 2017. Health Effects of Dramatic Societal Events — Ramifications of the Recent Presidential Election. New England Journal of Medicine 376: 2295–99 [ DOI ] [ PubMed ] [ Google Scholar ]
- 139. Williams DR, Mohammed SA. 2009. Discrimination and racial disparities in health: evidence and needed research. Journal of Behavioral Medicine 32: 20–47 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 140. Williams DR, Mohammed SA. 2013. Racism and Health I: Pathways and Scientific Evidence. American Behavioral Scientist 57: 1152–73 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 141. Williams DR, Mohammed SA. 2013. Racism and Health II: A Needed Research Agenda for Effective Interventions. American Behavioral Scientist 57: 1200–26 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 142. Williams DR, Purdie-Vaughns V. 2016. Needed Interventions to Reduce Racial/Ethnic Disparities in Health. Journal of Health Politics, Policy and Law 41: 627–51 [ DOI ] [ PubMed ] [ Google Scholar ]
- 143. Williams DR, Yu Y, Jackson JS, Anderson NB. 1997. Racial Differences in Physical and Mental Health: Socio-economic Status, Stress and Discrimination. J Health Psychol 2: 335–51 [ DOI ] [ PubMed ] [ Google Scholar ]
- 144. Yip T 2018. Ethnic/Racial Identity—A Double-Edged Sword? Associations With Discrimination and Psychological Outcomes. Current Directions in Psychological Science 27: 170–75 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (357.9 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Study protocol
- Open access
- Published: 28 March 2019
The impact of racism on the future health of adults: protocol for a prospective cohort study
- James Stanley ORCID: orcid.org/0000-0002-8572-1047 1 ,
- Ricci Harris 2 ,
- Donna Cormack 2 ,
- Andrew Waa 2 &
- Richard Edwards 1
BMC Public Health volume 19 , Article number: 346 ( 2019 ) Cite this article
239k Accesses
24 Citations
266 Altmetric
Metrics details
Racial discrimination is recognised as a key social determinant of health and driver of racial/ethnic health inequities. Studies have shown that people exposed to racism have poorer health outcomes (particularly for mental health), alongside both reduced access to health care and poorer patient experiences. Most of these studies have used cross-sectional designs: this prospective cohort study (drawing on critical approaches to health research) should provide substantially stronger causal evidence regarding the impact of racism on subsequent health and health care outcomes.
Participants are adults aged 15+ sampled from 2016/17 New Zealand Health Survey (NZHS) participants, sampled based on exposure to racism (ever exposed or never exposed, using five NZHS questions) and stratified by ethnic group (Māori, Pacific, Asian, European and Other). Target sample size is 1680 participants (half exposed, half unexposed) with follow-up survey timed for 12–24 months after baseline NZHS interview. All exposed participants are invited to participate, with unexposed participants selected using propensity score matching (propensity scores for exposure to racism, based on several major confounders). Respondents receive an initial invitation letter with choice of paper or web-based questionnaire. Those invitees not responding following reminders are contacted for computer-assisted telephone interview (CATI).
A brief questionnaire was developed covering current health status (mental and physical health measures) and recent health-service utilisation (unmet need and experiences with healthcare measures). Analysis will compare outcomes between those exposed and unexposed to racism, using regression models and inverse probability of treatment weights (IPTW) to account for the propensity score sampling process.
This study will add robust evidence on the causal links between experience of racism and subsequent health. The use of the NZHS as a baseline for a prospective study allows for the use of propensity score methods during the sampling phase as a novel approach to recruiting participants from the NZHS. This method allows for management of confounding at the sampling stage, while also reducing the need and cost of following up with all NZHS participants.
Peer Review reports
Differential access to the social determinants of health both creates and maintains unjust and avoidable health inequities [ 1 ]. In New Zealand, these inequities are largely patterned by ethnicity, particularly for Māori (the indigenous peoples) and Pacific peoples, and intertwined with ethnic distributions of socioeconomic status [ 2 , 3 ]. In models of health, racism is recognised as a key social determinant that underpins systemic ethnic health and social inequities, as is evident in New Zealand and elsewhere [ 4 , 5 ].
Racism can be understood as an organised system based on the categorisation and ranking of racial/ethnic groups into social hierarchies whereby ethnic groups are assigned differential value and have differential access to power, opportunities and resources, resulting in disadvantage for some groups and advantage for others [ 4 , 6 ]. Historical power relationships underpin systems of racism [ 7 ], which in New Zealand relates specifically to our colonial history and ongoing colonial processes [ 8 ].
Racism can be expressed at structural and individual levels, with several taxonomies describing different levels of racism. Institutionalised racism, for example, has been defined as, “the structures, policies, practices, and norms resulting in differential access to the goods, services, and opportunities of society by race[/ethnicity]” (p. 10) [ 6 ]. In contrast, personally-mediated racism has been defined as, “prejudice and discrimination, where prejudice is differential assumptions about the abilities, motives, and intents of others by ‘race[/ethnicity],’ and discrimination is differential actions towards others by ‘race[/ethnicity]’” (p. 10) [ 6 ].
The multifarious expressions of racism can affect health via several recognised direct and indirect pathways. Indirect pathways include differential access to societal resources and health determinants by race/ethnicity, as evidenced by long-standing ethnic inequities in income, education, employment and living standards in New Zealand, with subsequent impacts on living environments and exposure to risk and protective factors [ 4 , 6 , 9 , 10 ]. At the individual level, experience of racism can affect health directly through physical violence and stress pathways, with negative psychological and physiological impacts leading to subsequent mental and physical health consequences. In addition, racism influences healthcare via institutions and individual health providers, leading to ethnic inequities in access to and quality of care. For example, ethnic disparities in socioeconomic status can indirectly result in differential access to care, while health provider ethnic bias can influence the quality and outcomes of healthcare interactions [ 11 ].
There has been considerable recent growth in research supporting a direct link between experience of racism and health. A recent systematic review and meta-analysis summarised the evidence for direct links between self-reported personally-mediated racism and negative physical and mental health outcomes [ 12 ], with the strongest effect sizes demonstrated for mental health. Related work has also shown that experience of racial discrimination is associated with other adverse health outcomes and preclinical indicators of disease and health risk across various ethnic groups and countries, including in New Zealand [ 9 , 13 , 14 , 15 ]. Experience of racism has also been linked to a range of negative health care-related measures [ 16 ].
However, most studies have used cross-sectional designs: very few of the articles in a recent systematic review [ 12 ] used prospective or longitudinal designs ( n = 30, 9% of total, including multiple articles from some studies), limiting our ability to draw strong causal conclusions as the direction of causality cannot be determined when racism exposure and health outcomes are measured at the same time. Additionally, cross-sectional studies may give biased estimates of the magnitude of association between experience of racism and health: for example, bias may occur if experience of ill health (outcome) increases reporting or perception of racism (exposure) [ 12 ]. This is suggested by meta-analyses where effect sizes for the association between racism and mental health were larger for cross-sectional compared to longitudinal studies [ 12 ]. Longitudinal research on the effects of racism has been particularly limited with respect to physical health outcomes and measures of healthcare access and quality [ 12 , 16 ]. Finally, existing prospective studies have largely been restricted to quite specific groups (e.g. adolescents, females, particular ethnic groups), with a limited number of studies undertaken at a national population level and few with sufficient data to explore the impact of racism on the health of Indigenous populations [ 12 ].
In New Zealand, reported experience of racism is substantially higher among Māori, Asian and Pacific ethnic groupings compared to European [ 3 , 17 ]. In our own research, we have examined cross-sectional links between reported experience of racism and various measures of adult health in New Zealand using data from the New Zealand Health Survey (NZHS), an annual national survey by the Ministry of Health including ~ 13,000 adults per annum [ 2 , 18 , 19 ]. In these studies [ 17 , 20 , 21 , 22 ] we have shown that both individual experience of racism (e.g. personal attacks or unfair treatment) and markers of structural racism (deprivation, other socioeconomic indicators) are independently associated with poor health (mental health, physical health, cardiovascular disease), health risks (smoking, hazardous alcohol consumption) and healthcare experience and use (screening, unmet need and negative patient experiences). Other New Zealand researchers have reported similar findings including studies among older Māori [ 23 ], adolescents [ 24 ], and for maternal and child health outcomes [ 25 ]. However, evidence from New Zealand prospective studies is still limited. The NZ Attitudes and Values study showed that, among Māori, experience of racism was negatively linked to subsequent wellbeing [ 26 ], and the Growing Up in New Zealand study reported that maternal experience of racism (measured antenatally) was linked to a higher risk of postnatal depression among Māori, Pacific and Asian women [ 27 ].
While empirical evidence of the links between racism and health is growing in New Zealand, it remains limited in several areas. There is consistent evidence from cross-sectional studies for the hypothesis that racism is associated with poorer health and health care. This study seeks to build on existing research to provide more robust causal evidence using a prospective design that helps to rule out reverse causality, in order to inform policy and healthcare interventions.
Theoretical and conceptual approaches
Addressing racism as a health determinant is intrinsically linked to addressing ethnic health inequities. In New Zealand, Māori health is of special relevance given Māori rights under the Treaty of Waitangi [ 28 ] and the United Nations Declaration on the Rights of Indigenous People [ 29 ], and in recognition of the inequities for Māori across most major health indicators [ 28 ]. We recognise the direct significance of this project to Māori and understand racism in its broader sense as underpinning our colonial history with ongoing contemporary manifestations and effects [ 8 ]. As such, our work is informed by critical approaches to health research that are explicitly concerned with understanding inequity and transforming systems and structures to achieve the goal of health equity. This includes decolonising and transformative research principles [ 30 ] that influence our approach to the research question, data collection, analysis and interpretation of data, and translation of research findings. The team includes senior Māori researchers as well as advisors with experience in Māori health research and policy.
Aims and research questions
The overall aim is to examine the relationship between reported experience of racism and a range of subsequent health measures. The specific objectives are:
To determine whether experience of racism leads to poorer mental health and/or physical health.
To determine the impact of racism on subsequent use and experience of health services.
Study design
The proposed study uses a prospective cohort study design. Respondents from the 2016/17 New Zealand Health Survey [ 2 , 18 , 19 ] (NZHS) provide the source of the follow-up cohort sample and the NZHS provides baseline data. The follow-up survey will be conducted between one and two years after respondents completed the NZHS. Using the NZHS data as our sampling frame provides access to exposure status (experience of racism), along with data on a substantial number of covariates (including age, gender, and socioeconomic variables) allowing us to select an appropriate study cohort for answering our research questions. Participant follow-up will be conducted by a multi-modality survey (mail, web and telephone modalities).
This study explores the impact of racism on health in the general NZ adult population (which is the target population of the NZHS that forms the baseline of the study).
Participants
Participants were selected from adult NZHS 2016/17 interviewees ( n = 13,573, aged 15+ at NZHS interview) who consented to re-contact for future research within a 2 year re-contact window (92% of adult respondents). The NZHS is a complex-sample design survey with an 80% response rate for adults [ 18 ] and oversampling of Māori, Pacific, and Asian populations (who experience higher levels of racism), which facilitates studying the impact of racism on subsequent health status. Participants who had consented to re-contact ( n = 12,530) also needed to have contact details recorded and sufficient data on exposures/confounders to be included in the sampling frame ( n = 11,775, 93.9% of consenting adults). All invited participants will be aged at least 16 at the time of follow-up, as at least one year will have passed since participation in the NZHS (where all participants were aged at least 15).
Exposure to racism was determined from the five previously validated NZHS items [ 31 ] asked of all adult respondents (see Table 1 ) about personal experience of racism across five domains (verbal and physical attack; unfair treatment in health, housing, or work). Response options for each question cover recent exposure (within the past 12 months), more historical exposure (> 12 months ago), or no exposure to racism.
Identification of exposed and unexposed individuals
Individuals were classified as exposed to racism if they answered “yes” to any question in Table 1 , in either timeframe (recent or historical: referred to as “ever” exposure). This allows for analysis restricted to the nested subset of individuals reporting recent exposure to racism (past 12 months) and those only reporting more historical exposure (> 12 months ago). The unexposed group comprised all individuals answering “No” to all five domains of experience of racism. We selected all exposed individuals for follow-up, along with a matched sample of unexposed individuals. Individuals missing exposure data were explicitly excluded.
Matching of exposed and unexposed individuals
To address potential confounding, we used propensity score matching methods in our sampling stage to remove the impact of major confounders (as measured in the NZHS) of the causal association between experience of racism and health outcomes. Propensity score methods are increasingly used in observational epidemiology as a robust method for dealing with confounding in the analysis stage [ 32 , 33 , 34 , 35 , 36 ] and have more recently been considered as a useful approach for secondary sampling of participants from existing cohorts for subsequent follow up [ 37 ].
All exposed NZHS respondents will be invited into the follow-up survey. To find matched unexposed individuals, potential participants were stratified based on self-reported ethnicity (Māori, Pacific, Asian, European and Other; using prioritised ethnicity for individuals identifying with more than one grouping) [ 38 ] and then further matched for potential sociodemographic and socioeconomic confounders using propensity score methods [ 39 , 40 ]. Stratification by ethnicity reflects the differential prevalence of racism by ethnic group, and furthermore allows ethnically-stratified estimates of the impact of racism [ 22 ].
Propensity scores were modelled using logistic regression for “ever” exposure to racism based on major confounder variables of the association between racism and poor health (Table 2 ), with modelling stratified by ethnic group. Selection of appropriate confounders was based on past work using cross-sectional analysis of the 2011/12 NZHS (e.g. [ 21 , 22 ]) and the wider literature that informed the conceptual model for the project. Some additional variables were considered for inclusion in the matching process but were removed prior to finalisation (details in Table 2 ).
Within each ethnic group stratum, exposed individuals were matched with unexposed individuals (1:1 matching) based on propensity scores to make these two groups approximately exchangeable (confounders balanced between exposure groups). The matching process [ 41 ] used nearest neighbour matching as implemented in MatchIt [ 42 ] in R 3.4 (R Institute, Vienna, Austria). As the propensity score modelling is blind to participants’ future outcome status, the final propensity score models were refined using just the baseline NZHS data to achieve maximal balance of confounders between exposure groups, without risking bias to the subsequent primary causal analyses [ 39 ]. Balance between groups was then checked on all matching variables prior to finalisation of the sampling lists.
Questionnaire development
Development of the follow-up questionnaire was informed by a literature review and a conceptual model (Figs. 1 and 2 ) of the potential pathways from racism to health outcomes (Fig. 1 ) and health service utilisation (Fig. 2 ) [ 4 , 10 , 16 , 43 , 44 ]. The literature review focussed on longitudinal studies of racism and health among adolescents and adults that included health or health service outcomes. The literature review covered longitudinal studies post-dating the 2015 systematic review by Paradies et al. [ 12 ], using similar search terms for papers between 2013 and 2017 indexed in Medline and PubMed databases, alongside additional studies from systematic reviews [ 12 , 16 ].
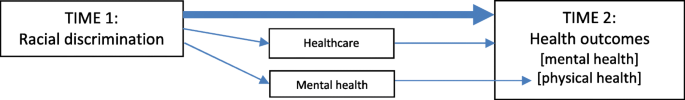
Potential pathways between racism and health outcomes. Direct pathway: Main arrow represents the direct biopsychosocial and trauma pathways between experience of racial discrimination (Time 1) and negative health outcomes (Time 2) Indirect pathways: Racial discrimination (Time 1) can impact negatively on health outcomes (Time 2) via healthcare pathways (e.g. less engagement, unmet need). Racial discrimination (Time 1) can impact negatively on physical health outcomes (Time 2) via mental health pathways
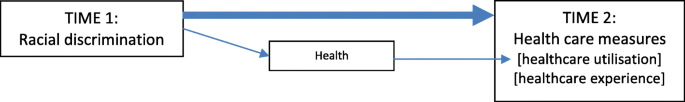
Potential pathways between racism and healthcare utilisation outcomes. Main pathway: Main arrow represents the pathway between experience of racial discrimination (Time 1) and negative healthcare measures (Time 2), via negative perceptions and expectations of healthcare (providers, organisations, systems) and future engagement. Secondary pathway: Racial discrimination (T1) can impact negatively on healthcare (Time 2) via negative impacts on health increasing healthcare need
We used several criteria for considering and prioritising variables for the questionnaire. The conceptual model also informed prioritisation of variables for the questionnaire. For outcome measures, these included: alignment with study aims and objectives; existing evidence of a relationship between racism and outcome; New Zealand evidence of ethnic inequities in outcome; previous cross-sectional relationships between racism and outcome in New Zealand data; availability of baseline measures (for health outcomes); plausibility of health effects manifesting within a 1–2 year follow-up period; and data quality (e.g. validated measures, low missing data, questions suitable for multimodal administration). Mediators and confounders were considered for variables not available in the baseline NZHS survey, as was recent experience of racism (following the NZHS interview) to provide additional measurement of exposure to recent racism. A final consideration for prioritising items for inclusion was keeping the length of the questionnaire short in order to maximise response rates (while being able to fully address the study aims). The questionnaire was extensively discussed by the research team and reviewed by the study advisors prior to finalisation.
Table 3 summarises the outcome measures by topic domain and original source (with references). The final questionnaire content can be found in the Additional file 1 , and includes: health outcome measures of mental and physical health (using SF12-v2 and K10 scales); health service measures (unmet need, satisfaction with usual medical centre, experiences with general practitioners); experience of racism in the last 12 months (adapted from items in the NZHS); and variables required to restrict data (e.g. having a usual medical centre, type of centre, having a General Practitioner [GP] visit in the last 12 months) or potential confounder and mediator variables not available at baseline (e.g. number of GP visits).
Recruitment and data collection
Recruitment is currently underway. The sampling phase provided a list of potential participants for invitation, and recruitment for the follow-up survey uses the contact details from the NZHS interview (physical address, mobile/landline telephone, and email address if available). Recruitment will take place over three tranches to (1) manage fieldwork capacity and (2) allow tracking of response rates and adaptation of contact strategies if recruitment is sub-optimal.
To maximise response rates, we chose to use a multi-modal survey [ 45 ]. Participants are invited to respond by a paper questionnaire included with the initial invitation letter (questionnaire returned by pre-paid post), by self-completed online questionnaire, or by computer-assisted telephone interview (CATI, on mobile or landline.) A pen is included in the study invitation to improve initial engagement with the paper-based survey [ 46 ]. Participants completing the survey are offered a NZ$20 gift card to recognise their participation. The contact information contains instructions for opting out of the study.
Those participants not responding online or by post receive a reminder postcard mailed out two weeks after the initial letter, containing a link to the web survey and a note that the participant will be contacted by telephone in two weeks’ time.
Two weeks after the reminder postcard (four weeks post-invitation) remaining non-respondents are contacted using CATI processes. For those with mobile phone numbers or email addresses, a text (SMS) or email reminder is sent two days before the telephone contact phase. Once contact is made by telephone, the interviewer asks the participant to complete the survey over the telephone at that time or organises a subsequent appointment (interview duration approximately 15 min). Interviewers make up to seven telephone contact attempts for each participant, using all recorded telephone numbers. Respondents who decline to complete the full interview at telephone follow-up are asked to consider answering two priority questions (self-rated health and any unmet need for healthcare in the last 12 months: questions 1 and 8 in Table 3 and Additional file 1 ).
Past surveys conducted in NZ have frequently noted lower response rates and hence under-representation of Māori [ 47 , 48 ]. Drawing on Kaupapa Māori research principles, we are explicitly aiming for equitable response rates of Māori to ensure maximum power for ethnically stratified analysis. This involves providing culturally appropriate invitations and interviewers for participants, and actively monitoring response rates by ethnicity during data collection to allow longer and more frequent follow-up of Māori, Pacific and Asian participants if required [ 48 , 49 ]. The use of a multi-modal survey is also expected to minimise recruitment problems inherent to any single modality (e.g. lower phone ownership or internet access in some ethnic groups).
We have contracted an external research company to co-ordinate recruitment and data collection fieldwork under our supervision (covering all contact processes described here), which follows recruitment and data management protocols set by our research team.
Statistical analysis
Propensity score methods for the sampling stage are described above: this section focuses on causal analyses for health outcomes in the achieved sample. The sampling frame selects participants based on “ever” experience of racism, which is our exposure definition.
All analyses will account for both the complex survey sampling frame (weights, strata and clusters from the NZHS) and the secondary sampling phase (selection based on propensity scores). Complex survey data will be handled using software to account for these designs (e.g. survey package [ 50 ] in R); propensity scores will be handled in the main analysis by using inverse probability of treatment weights (IPTW) combined with the sampling weights [ 51 ].
Linear regression methods will be used to compare change in continuous outcome measures (e.g. K10 score) by estimating mean score at follow-up, adjusted for baseline. Analysis of dichotomous categorical outcomes (e.g. self-rated health) will use logistic regression methods, again adjusted for baseline (for health outcomes). We will conduct analyses stratified by ethnic group to explore whether the impact of racism differs by ethnic group. Models will adjust for confounders included in creating the propensity scores (doubly-robust estimation) to address residual confounding not fully covered by the propensity score approach [ 52 ]. Analysis for other outcomes will use similar methods.
As we hypothesise that some outcomes (e.g. self-reported mental distress) will be more strongly influenced by recent experience of racism, we will also examine our main outcomes restricted to those only reporting historical (more than 12 months ago) or recent (last 12 months) racism at baseline. These historical and recent experience groups (and corresponding unexposed individuals) form nested sub-groups of the total cohort, and so analysis will follow the same framework outlined above. Experience of racism in the last 12 months (measured at follow-up) will be examined in cross-sectional analyses and in combination with baseline measures of racism to create a measure to examine the cumulative impact of racism on outcomes.
Sensitivity analyses
While the sampling invitation lists are based on matched samples, we have no control about specific individuals choosing to participate in the follow-up survey, and so the original matching is unlikely to be maintained in the achieved sample. We will conduct sensitivity analyses using re-matched data (based on propensity scores for those participating in follow-up) to allow for re-calibration of exposed and unexposed groups in the achieved sample.
To consider potential for bias due to non-response in our follow-up sample, we will compare NZHS 2016/17 cross-sectional data for responders and non-responders on baseline sociodemographic, socioeconomic, and baseline health variables.
Sample size
Based on NZHS 2011/12 responses, we anticipated a total pool of 2100 potential participants with “ever” experience of racism, with approximately 1100 expected to be Māori/Pacific/Asian ethnicity, and 10,000 with no report of racism (at least 2 unexposed per exposed individual in each ethnic group).
For the main analyses (based on “ever” experience of racism) we assumed a conservative follow-up rate of 40%, giving a final sample size of at least 840 exposed individuals. This response rate includes re-contact and agreement to participate, based on past experience recruiting NZHS participants for other studies and the relative length of the current survey questionnaire.
Initial projections (based on NZHS2011/12 data) indicated sufficient numbers of unexposed individuals for 1:1 matching based on ethnicity and propensity scores. This gives a feasible total sample size of n = 1680, providing substantial power for the K10 mental health outcome (standard deviation = 6.5: > 95% power to detect difference in change of 2 units of K10 between groups.) For the second main health outcome (change in self-rated health), this sample size will have > 85% power for a difference between 8% of those exposed to racism having worse self-reported health at follow-up (relative to baseline) compared to 5% of unexposed individuals.
For analyses of effects stratified by ethnicity, we expect > 95% power for Māori participants ( n = 280 each exposed and unexposed) for the K10 outcome (assumptions as above); change in self-rated health will have 80% power for a difference between 12% of exposed individuals having worse self-reported health at follow-up (relative to baseline) compared to 5% of unexposed individuals. Stratified estimates for Pacific and Asian groups will have poorer precision, but should still provide valid comparisons.
Ethical approval and consent to participate
The study involves recruiting participants who have already completed the NZHS interview (including questions on racial discrimination) The NZHS as conducted by the Ministry of Health has its own ethical approval (MEC/10/10/103) and participants are only invited onto the present study if they explicitly consented (at the time of completing the NZHS) to re-contact for future health research. The current study was reviewed and approved by the University of Otago’s Human Ethics (Health) Committee prior to commencement of fieldwork (reference: H17/094). Participants provided informed consent to participate at the time of completing the follow-up survey depending on response modality: implicitly through completion and return of the paper survey which stated “By completing this survey, you indicate that you understand the research and are willing to participate” (see Additional file 1 : a separate written consent document was not required by the ethics committee); in the online survey by responding “yes” to a similarly worded question that they understood the study and agreed to take part (recorded as part of data collection, and participation could not continue unless ticked), or by verbal consent in a similar initial question in the telephone interview (since written consent could not be collected in this setting). These consent methods were approved by the reviewing Ethics committee [ 53 ]. Ethical approval for the study included using the same consent processes for those participants aged 16 to 18 as for older participants.
This study will contribute robust evidence to the limited national and international literature from prospective studies on the causal links between experience of racism and subsequent health. The use of the NZHS as the baseline for the prospective study capitalises on the inclusion of racism questions in that survey to provide a unique and important opportunity to build on and substantially strengthen the current evidence base for the impact of racism on health using data spanning the entire New Zealand adult population. In addition, our use of propensity scores in the sampling phase is a novel approach to prospective recruitment of participants from the NZHS. This approach should manage confounding while reducing the need (and cost) of following up all NZHS participants, without compromising the internal validity of the results. The novel methods developed for using the NZHS as the base for a prospective cohort study will have wider application to other health priority areas. One general limitation of this approach is that baseline data (for both propensity score development and baseline health measures) is limited to the data captured in the existing larger survey. We anticipate that this study will assist in prioritising racism as a health determinant and inform the development of anti-racism interventions in health service delivery and policy making.
Current stage of research
Funding for this project began October 1st 2017. The first set of respondent invitations was mailed out on July 12th 2018; fieldwork for the final tranche of invitations was underway at the time of submission and is expected to be completed by 31 December 2018. Analysis and reporting will take place in mid-to-late 2019.
Abbreviations
Computer Assisted Telephone Interview
General Practitioner
General Social Survey
Index of Multiple Deprivation
Inverse Probability of Treatment Weights
- New Zealand
New Zealand Deprivation Index
New Zealand Health Survey
12/36-Item Short Form Survey
short message service
Commission on Social Determinants of Health. Closing the gap in a generation: health equity through actions on the social determinants of health. Geneva: World Health Organization; 2008.
Google Scholar
Ministry of Health. Annual Update of Key Results 2016/17: New Zealand Health Survey 2017 [Available from: https://www.health.govt.nz/publication/annual-update-key-results-2016-17-new-zealand-health-survey . accessed 13/09/2018].
Ministry of Social Development. The Social Report 2016: Te pūrongo oranga tangata. Wellington: Ministry of Social Development; 2016.
Williams DR, Mohammed SA. Racism and health I: pathways and scientific evidence. Am Behav Sci. 2013;57(8). https://doi.org/10.1177/0002764213487340 .
Reid P, Robson B. Understanding health inequities. In: Robson B, Harris R, editors. Hauora: Maori standards of health IV a study of the years 2000–2005. Wellington: Te Ropu Rangahau Hauora a Eru Pomare; 2007. p. 3–10.
Jones C. Confronting institutionalized racism. Phylon. 2002;50:7–22.
Article Google Scholar
Garner S. Racisms: An introduction. London/Thousand Oaks CA: Sage; 2010.
Book Google Scholar
Becares L, Cormack D, Harris R. Ethnic density and area deprivation: neighbourhood effects on Maori health and racial discrimination in Aotearoa/New Zealand. Soc Sci Med. 2013;88:76–82. https://doi.org/10.1016/j.socscimed.2013.04.007 .
Article PubMed PubMed Central Google Scholar
Paradies YC. Defining, conceptualizing and characterizing racism in health research. Crit Public Health. 2006;16(2):143–57. https://doi.org/10.1080/09581590600828881 .
Krieger N. Methods for the scientific study of discrimination and health: an ecosocial approach. Am J Public Health. 2012;102(5):936–44. https://doi.org/10.2105/AJPH.2011.300544 .
Jones CP. Invited commentary: "race," racism, and the practice of epidemiology. Am J Epidemiol. 2001;154(4):299–304; discussion 05-6.
Article CAS Google Scholar
Paradies Y, Ben J, Denson N, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0138511. https://doi.org/10.1371/journal.pone.0138511 .
Article CAS PubMed PubMed Central Google Scholar
Lewis TT, Cogburn CD, Williams DR. Self-reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annu Rev Clin Psychol. 2015;11:407–40. https://doi.org/10.1146/annurev-clinpsy-032814-112728 .
Gee GC, Ro A, Shariff-Marco S, et al. Racial discrimination and health among Asian Americans: evidence, assessment, and directions for future research. Epidemiol Rev. 2009;31:130–51. https://doi.org/10.1093/epirev/mxp009 .
Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. https://doi.org/10.1007/s10865-008-9185-0 .
Article PubMed Google Scholar
Ben J, Cormack D, Harris R, et al. Racism and health service utilisation: a systematic review and meta-analysis. PLoS One. 2017;12(12):e0189900. https://doi.org/10.1371/journal.pone.0189900 published Online First: 2017/12/19.
Harris R, Cormack D, Tobias M, et al. The pervasive effects of racism: experiences of racial discrimination in New Zealand over time and associations with multiple health domains. Soc Sci Med. 2012;74(3):408–15. https://doi.org/10.1016/j.socscimed.2011.11.004 .
Ministry of Health. Methodology report 2016/17: New Zealand health survey. Wellington: Ministry of Health; 2017.
Ministry of Health. Content guide 2016/17: New Zealand health survey. Wellington: Ministry of Health; 2017.
Harris R, Cormack D, Tobias M, et al. Self-reported experience of racial discrimination and health care use in New Zealand: results from the 2006/07 New Zealand health survey. Am J Public Health. 2012;102(5):1012–9. https://doi.org/10.2105/AJPH.2011.300626 .
Harris RB, Cormack DM, Stanley J. Experience of racism and associations with unmet need and healthcare satisfaction: the 2011/12 adult New Zealand health survey. Aust N Z J Public Health. 2018. https://doi.org/10.1111/1753-6405.12835 published Online First: 2018/10/09.
Harris RB, Stanley J, Cormack DM. Racism and health in New Zealand: prevalence over time and associations between recent experience of racism and health and wellbeing measures using national survey data. PLoS One. 2018;13(5):e0196476. https://doi.org/10.1371/journal.pone.0196476 published Online First: 2018/05/04.
Dyall L, Kepa M, Teh R, et al. Cultural and social factors and quality of life of Maori in advanced age. Te puawaitanga o nga tapuwae kia ora tonu - life and living in advanced age: a cohort study in New Zealand (LiLACS NZ). N Z Med J. 2014;127(1393):62–79.
PubMed Google Scholar
Crengle S, Robinson E, Ameratunga S, et al. Ethnic discrimination prevalence and associations with health outcomes: data from a nationally representative cross-sectional survey of secondary school students in New Zealand. BMC Public Health. 2012;12:45. https://doi.org/10.1186/1471-2458-12-45 .
Thayer ZM, Kuzawa CW. Ethnic discrimination predicts poor self-rated health and cortisol in pregnancy: insights from New Zealand. Soc Sci Med. 2015;128:36–42. https://doi.org/10.1016/j.socscimed.2015.01.003 .
Stronge S, Sengupta NK, Barlow FK, et al. Perceived discrimination predicts increased support for political rights and life satisfaction mediated by ethnic identity: a longitudinal analysis. Cult Divers Ethn Minor Psychol. 2016;22(3):359–68. https://doi.org/10.1037/cdp0000074 .
Becares L, Atatoa-Carr P. The association between maternal and partner experienced racial discrimination and prenatal perceived stress, prenatal and postnatal depression: findings from the growing up in New Zealand cohort study. Int J Equity Health. 2016;15(1):155. https://doi.org/10.1186/s12939-016-0443-4 .
Robson B, Harris R, editors. Hauora : Maori standards of health IV : a study of the years 2000–2005. Wellington: Te Rōpū Rangahau Hauora a Eru Pōmare; 2007.
UN General Assembly. United Nations Declaration on the Rights of Indigenous Peoples : resolution / adopted by the General Assembly 2007. Available from: https://undocs.org/A/RES/61/295 . Accessed 1 Nov 2018.
Smith L. Decolonizing methodologies: research and indigenous peoples. 2nd ed. London and New York: Zed Books; 2012.
Harris R, Tobias M, Jeffreys M, et al. Racism and health: the relationship between experience of racial discrimination and health in New Zealand. Soc Sci Med. 2006;63(6):1428–41. https://doi.org/10.1016/j.socscimed.2006.04.009 .
Sturmer T, Joshi M, Glynn RJ, et al. A review of the application of propensity score methods yielded increasing use, advantages in specific settings, but not substantially different estimates compared with conventional multivariable methods. J Clin Epidemiol. 2006;59(5):437–47. https://doi.org/10.1016/j.jclinepi.2005.07.004 .
Luo Z, Gardiner JC, Bradley CJ. Applying propensity score methods in medical research: pitfalls and prospects. Med Care Res Rev. 2010;67(5):528–54. https://doi.org/10.1177/1077558710361486 .
Weitzen S, Lapane KL, Toledano AY, et al. Principles for modeling propensity scores in medical research: a systematic literature review. Pharmacoepidemiol Drug Saf. 2004;13(12):841–53. https://doi.org/10.1002/pds.969 .
Shah BR, Laupacis A, Hux JE, et al. Propensity score methods gave similar results to traditional regression modeling in observational studies: a systematic review. J Clin Epidemiol. 2005;58(6):550–9. https://doi.org/10.1016/j.jclinepi.2004.10.016 .
Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. 2010;25(1):1–21. https://doi.org/10.1214/09-STS313 published Online First: 2010/09/28.
Stuart EA, Ialongo NS. Matching methods for selection of subjects for follow-up. Multivariate Behav Res. 2010;45(4):746–65. https://doi.org/10.1080/00273171.2010.503544 [published Online First: 2011/01/12].
Ministry of Health. Ethnicity Data Protocols Wellington: Ministry of Health; 2017. Available from: https://www.health.govt.nz/system/files/documents/publications/hiso-10001-2017-ethnicity-data-protocols-v2.pdf . Accessed 1 Nov 2018.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. https://doi.org/10.1080/00273171.2011.568786 .
Caliendo M, Kopeinig S. Some practical guidance for the implementation of propensity score matching. J Econ Surv. 2008;22(1):31–72. https://doi.org/10.1111/j.1467-6419.2007.00527.x .
Ho DE, Imai K, King G, et al. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Polit Anal. 2017;15(03):199–236. https://doi.org/10.1093/pan/mpl013 .
Ho DE, Imai K, King G, et al. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42(8):1–28.
Sarnyai Z, Berger M, Jawan I. Allostatic load mediates the impact of stress and trauma on physical and mental health in indigenous Australians. Australas Psychiatry. 2016;24(1):72–5. https://doi.org/10.1177/1039856215620025 published Online First: 2015/12/10.
Kaholokula J. Mauli Ola: Pathways toward Social Justice for Native Hawaiians. Townsville: LIME Network Conference; 2015.
Fowler FJ, Roman AM, Mahmood R, et al. Reducing nonresponse and nonresponse error in a telephone survey: an informative case study. J Survey Stat Methodol. 2016;4(2):246–62. https://doi.org/10.1093/jssam/smw004 .
White E, Carney PA, Kolar AS. Increasing response to mailed questionnaires by including a pencil/pen. Am J Epidemiol. 2005;162(3):261–6. https://doi.org/10.1093/aje/kwi194 [published Online First: 2005/06/24].
Fink JW, Paine SJ, Gander PH, et al. Changing response rates from Maori and non-Maori in national sleep health surveys. N Z Med J. 2011;124(1328):52–63.
Paine SJ, Priston M, Signal TL, et al. Developing new approaches for the recruitment and retention of Indigenous participants in longitudinal research: Lessons from E Moe, Māmā: Maternal Sleep and Health in Aotearoa/New Zealand. MAI Journal: A New Zealand Journal of Indigenous Scholarship. 2013;2(2):121–32.
Selak V, Crengle S, Elley CR, et al. Recruiting equal numbers of indigenous and non-indigenous participants to a 'polypill' randomized trial. Int J Equity Health. 2013;12:44. https://doi.org/10.1186/1475-9276-12-44 .
Lumley T. survey: analysis of complex survey samples v3.32 2017 [R package]. Available from: https://cran.r-project.org/web/packages/survey/index.html . Accessed 1 Nov 2018.
Lenis D, Nguyen TQ, Dong N, et al. It's all about balance: propensity score matching in the context of complex survey data. Biostatistics. 2017. https://doi.org/10.1093/biostatistics/kxx063 [published Online First: 2018/01/03].
Funk MJ, Westreich D, Wiesen C, et al. Doubly robust estimation of causal effects. Am J Epidemiol. 2011;173(7):761–7. https://doi.org/10.1093/aje/kwq439 [published Online First: 2011/03/10].
National Ethics Advisory Committee. Ethical guidelines for observational studies: observational research, audits and related activities. Revised edition. Wellington: Ministry of Health; 2012.
Atkinson J, Salmond C, Crampton P. NZDep2013 index of deprivation. Dunedin: University of Otago; 2014.
Exeter DJ, Zhao J, Crengle S, et al. The New Zealand indices of multiple deprivation (IMD): a new suite of indicators for social and health research in Aotearoa, New Zealand. PLoS One. 2017;12(8):e0181260. https://doi.org/10.1371/journal.pone.0181260 [published Online First: 2017/08/05].
Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–76.
Ware J Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Fleishman JA, Selim AJ, Kazis LE. Deriving SF-12v2 physical and mental health summary scores: a comparison of different scoring algorithms. Qual Life Res. 2010;19(2):231–41. https://doi.org/10.1007/s11136-009-9582-z .
Bastos JL, Harnois CE, Paradies YC. Health care barriers, racism, and intersectionality in Australia. Soc Sci Med. 2018;199:209–18. https://doi.org/10.1016/j.socscimed.2017.05.010 [published Online First: 2017/05/16].
Australian Bureau of Statistics. General Social Survey 2014: Household questionnaire. Canberra: Australian Bureau of Statistics; 2014.
Ministry of Health. The New Zealand Health Survey: Content Guide and questionnaires 2011–2012 Wellington: Ministry of Health; 2012 [Available from: http://www.health.govt.nz/publication/new-zealand-health-survey-content-guide-and-questionnaires-2011-2012 . accessed 31/10/2016 2016].
Download references
Acknowledgements
We would like to acknowledge the assistance of the Ministry of Health’s New Zealand Health Survey Team for facilitating access to the NZHS data and respondent lists, and for help with constructing the questionnaire (including providing the Helpline contact template).
We would also like to acknowledge the expertise and input of our project advisory team: Natalie Talamaivao (Senior Advisor, Māori Health Research, Ministry of Health), Associate Professor Bridget Robson (Director, Eru Pōmare Māori Health Research Centre, University of Otago, Wellington), and Dr. Sarah-Jane Paine (Senior Research Fellow, University of Auckland and University of Otago, Wellington). Thanks also to Ms. Ruruhira Rameka (Eru Pōmare Māori Health Research Centre, University of Otago, Wellington) for providing administrative support. Research New Zealand was contracted to undertake the data collection and other fieldwork for the follow-up survey.
This project was funded by the Health Research Council of New Zealand (HRC 17–066). The funding body approved the study but has no further role in the study design or outputs from the study.
Availability of data and materials
Data from the follow-up study is not available to other researchers as participants did not provide their consent for data sharing. The NZHS 2016/17 data used as the baseline for the study described in this protocol is available to approved researchers subject to the New Zealand Ministry of Health’s Survey Microdata Access agreement https://www.health.govt.nz/nz-health-statistics/national-collections-and-surveys/surveys/access-survey-microdata .
Author information
Authors and affiliations.
Department of Public Health, University of Otago, Wellington, 23a Mein Street, Newtown, Wellington, New Zealand
James Stanley & Richard Edwards
Eru Pōmare Māori Health Research Centre, University of Otago, Wellington, 23a Mein Street, Newtown, Wellington, New Zealand
Ricci Harris, Donna Cormack & Andrew Waa
You can also search for this author in PubMed Google Scholar
Contributions
JS and RH initiated the project and are co-principal investigators of the study, and jointly led writing of the grant application and this protocol paper. JS designed the sampling plan, led the development of the contact protocol, led the development of the statistical analysis plan, contributed to revising the questionnaire, and is guarantor of the paper. RH designed the questionnaire, contributed to development of the sampling and contact protocol, and co-led the statistical analysis plan. DC led the conceptual plan with support from RH. AW and RE contributed to the contact protocol. DC, AW and RE all contributed to writing the grant application, revising the questionnaire and sampling plans, and revising the draft protocol paper. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to James Stanley .
Ethics declarations
Ethics approval and consent to participate.
The follow-up study protocol and questionnaire were approved by the University of Otago’s Human Ethics (Health) Committee prior to commencement of fieldwork (reference: H17/094). The NZHS has its own ethical approval as granted to the New Zealand Ministry of Health (NZ Multi-Region Ethics Committee, MEC/10/10/103), and consent for re-contact was gained from participants at the time of their NZHS interview. Participants provided informed consented to participate at the time of completing the follow-up survey: implicitly through completion and return of the paper survey which stated “By completing this survey, you indicate that you understand the research and are willing to participate”; in the online survey by responding “yes” to a similarly worded question that they understood the study and agreed to take part, or by verbal consent in a similar initial question in the telephone interview.
Consent for publication
Not applicable.
Competing interests
JS, RH, DC, AW, and RE report funding from the Health Research Council of New Zealand to complete this work. JS and RH report personal fees from the Health Research Council of New Zealand for service as external members on committees (neither are employees of the HRC), outside the scope of the current work.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Questionnaire used in follow-up survey. (PDF 919 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Stanley, J., Harris, R., Cormack, D. et al. The impact of racism on the future health of adults: protocol for a prospective cohort study. BMC Public Health 19 , 346 (2019). https://doi.org/10.1186/s12889-019-6664-x
Download citation
Received : 28 November 2018
Accepted : 15 March 2019
Published : 28 March 2019
DOI : https://doi.org/10.1186/s12889-019-6664-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Prospective cohort study
- Health service utilisation
- Health inequities
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
As a legacy of African enslavement, structural racism affects both population and individual health in three interrelated domains: redlining and racialized residential segregation, mass...
In this paper, we first provide a review of sociological research that exemplifies different meanings of racism, using the work of comparative sociologists as well as U.S.-focused scholars.
First, one can find racism embedded in our everyday worlds. Second, through our preferences and selections, we maintain racialized contexts in everyday action. Third, we inhabit cultural worlds that, in turn, promote racialized ways of seeing, being in, and acting in the world.
This paper defines antiracist research and explains how it can be used to dismantle the racism embedded in research practices. We offer a conceptual framework, including 10 foundational principles for understanding and practicing antiracist research.
Research on strategies for coping with racism is necessary to empower targeted individuals to develop and choose methods that are effective at reducing discrimination, increasing hope, and buffering the impact of racism on health.
Mapping racism-specific coping mechanisms. Faced with a dearth of concrete research, this article provides a comprehensive review of the literature to summarize the research documenting the various ways Black people in racialized societies regulate their emotions and cope when faced with racism.
This article provides an overview of the evidence linking the primary domains of racism – structural racism, cultural racism and individual-level discrimination – to mental and physical health outcomes. For each mechanism, we describe key findings and identify priorities for future research.
A renewed call to confront structural and systemic racism and oppression globally, and more specifically in the United States, has emerged to confront a confluence of state-sanctioned violence against Black lives; systemic racism against Black, Indigenous, and people of color (BIPOC); abuses based upon sexual orientation, gender identity, and ...
Racial discrimination is recognised as a key social determinant of health and driver of racial/ethnic health inequities. Studies have shown that people exposed to racism have poorer health outcomes (particularly for mental health), alongside both reduced access to health care and poorer patient experiences.
A thorough analysis of racism requires an examination of both subtle forms of racism and the resurgence of overt racism and its consequences for inequality. Discover the world's research 25 ...