BMC Nursing
Latest collections open to submissions.


Nursing vulnerable populations
Guest Edited by Jane Currie, Luke Molloy, and Mirko Prosen

Management and leadership in nursing
Guest Edited by Alexandre Pazetto Balsanelli and Abdelaziz Hendy

Nursing approaches to self-care, self-management, and adaptation to illness
Guest Edited by Åsa Audulv, Francisco Miguel Correia Sampaio and Clemente Neves Sousa
Editor's picks

End-of-life care for people with advanced dementia and pain: a qualitative study in Swedish nursing homes

Protective reactions of ICU nurses providing care for patients with COVID-19: a qualitative study
- Most accessed
Healthcare providers’ hospital breastfeeding practices during the COVID-19 endemic and associated factors in Thailand: a cross-sectional study
Authors: Nongyao Lawin, Sasitara Nuampa, Chananchida Somsuk, Sutthisak Srisawad, Kasem Raungrongmorakot and Sukwadee Ketsuwan
Effect of stress on study skills self-efficacy in Nursing students: the chain mediating role of general self-efficacy and self-directed learning
Authors: Xiaoyun Zhang, Lei-lei Guo, Ying Wang, Yuqing Li, Jiaofeng Gui, Xue Yang, Yujin Mei, Haiyang Liu, Jin-long Li, Yunxiao Lei, Xiaoping Li, Lu Sun, Liu Yang, Ting Yuan, Congzhi Wang, Dongmei Zhang…
Effect of an online training intervention on evidence-based practice in clinical nurses. #Evidencer Project
Authors: Antonio Jesús Ramos-Morcillo, Maria Ruzafa-Martínez, César Leal-Costa and Serafin Fernández-Salazar
The dual roles of empathy in mediating structural empowerment and compassion fatigue among Chinese nurses
Authors: Xiaoling Shen, He Bu, Jinhuan Zhang, Wenjie Duan, Haiyan Wang, Yan Tao and Zijia Qiao
Generalized anxiety disorder and job performance can predict job stress among nurses: A latent profile analysis
Authors: Liuqiao Ning, Fengzhen Li, Shihen Li, Yuenv Wang, Tingting Lin, Qianying Deng, Yingjie Fu, Jufang Li and Yun Li
Most recent articles RSS
View all articles
A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward
Authors: Abukari Kwame and Pammla M. Petrucka
A qualitative study of nursing student experiences of clinical practice
Authors: Farkhondeh Sharif and Sara Masoumi
The importance of professional values from nursing students’ perspective
Authors: Batool Poorchangizi, Fariba Borhani, Abbas Abbaszadeh, Moghaddameh Mirzaee and Jamileh Farokhzadian
Lifelong learning and nurses’ continuing professional development, a metasynthesis of the literature
Authors: Mandlenkosi Mlambo, Charlotte Silén and Cormac McGrath
Increasing cultural awareness: qualitative study of nurses’ perceptions about cultural competence training
Authors: Anu-Marja Kaihlanen, Laura Hietapakka and Tarja Heponiemi
Most accessed articles RSS
Aims and scope
Join our editorial board.

We are recruiting new Editorial Board Members to join our international editorial board, helping to provide expertise on manuscripts in the field of nursing.
Latest Tweets
Your browser needs to have JavaScript enabled to view this timeline
BMC Series Blog
Failed to load RSS feed.
Important information
Editorial board
For authors
For editorial board members
For reviewers
- Manuscript editing services
Annual Journal Metrics
Citation Impact 2023 Journal Impact Factor: 3.1 5-year Journal Impact Factor: 3.5 Source Normalized Impact per Paper (SNIP): 1.321 SCImago Journal Rank (SJR): 0.894 Speed 2023 Submission to first editorial decision (median days): 15 Submission to acceptance (median days): 161 Usage 2023 Downloads: 3,633,213 Altmetric mentions: 785
- More about our metrics
Peer-review Terminology
The following summary describes the peer review process for this journal:
Identity transparency: Single anonymized
Reviewer interacts with: Editor
Review information published: Review reports. Reviewer Identities reviewer opt in. Author/reviewer communication
More information is available here
- Follow us on Twitter
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 03 June 2022
Effectiveness of registered nurses on patient outcomes in primary care: a systematic review
- Julia Lukewich 1 ,
- Ruth Martin-Misener 2 ,
- Allison A. Norful 3 ,
- Marie-Eve Poitras 4 ,
- Denise Bryant-Lukosius 5 ,
- Shabnam Asghari 6 ,
- Emily Gard Marshall 7 ,
- Maria Mathews 8 ,
- Michelle Swab 9 ,
- Dana Ryan 1 &
- Joan Tranmer 10
BMC Health Services Research volume 22 , Article number: 740 ( 2022 ) Cite this article
16k Accesses
21 Citations
12 Altmetric
Metrics details
A Correction to this article was published on 22 June 2022
This article has been updated
Globally, registered nurses (RNs) are increasingly working in primary care interdisciplinary teams. Although existing literature provides some information about the contributions of RNs towards outcomes of care, further evidence on RN workforce contributions, specifically towards patient-level outcomes, is needed. This study synthesized evidence regarding the effectiveness of RNs on patient outcomes in primary care.
A systematic review was conducted in accordance with Joanna Briggs Institute methodology. A comprehensive search of databases (CINAHL, MEDLINE Complete, PsycINFO, Embase) was performed using applicable subject headings and keywords. Additional literature was identified through grey literature searches (ProQuest Dissertations and Theses, MedNar, Google Scholar, websites, reference lists of included articles). Quantitative studies measuring the effectiveness of a RN-led intervention (i.e., any care/activity performed by a primary care RN) that reported related outcomes were included. Articles were screened independently by two researchers and assessed for bias using the Integrated Quality Criteria for Review of Multiple Study Designs tool. A narrative synthesis was undertaken due to the heterogeneity in study designs, RN-led interventions, and outcome measures across included studies.
Forty-six patient outcomes were identified across 23 studies. Outcomes were categorized in accordance with the PaRIS Conceptual Framework (patient-reported experience measures, patient-reported outcome measures, health behaviours) and an additional category added by the research team (biomarkers). Primary care RN-led interventions resulted in improvements within each outcome category, specifically with respect to weight loss, pelvic floor muscle strength and endurance, blood pressure and glycemic control, exercise self-efficacy, social activity, improved diet and physical activity levels, and reduced tobacco use. Patients reported high levels of satisfaction with RN-led care.
Conclusions
This review provides evidence regarding the effectiveness of RNs on patient outcomes in primary care, specifically with respect to satisfaction, enablement, quality of life, self-efficacy, and improvements in health behaviours. Ongoing evaluation that accounts for primary care RNs’ unique scope of practice and emphasizes the patient experience is necessary to optimize the delivery of patient-centered primary care.
Protocol registration ID
PROSPERO: International Prospective Register of Systematic Reviews. 2018. ID=CRD42 018090767 .
Peer Review reports
Primary care is the foundation of a highly functioning health care system and provides comprehensive, patient-centered care that considers the needs and experiences of the individual patient, their families, and the well-being of the broader community [ 1 ]. Primary care providers are the first contact and principal point of continuing care for patients within the health care system, and coordinate other specialist care and services that patients may need [ 1 , 2 ]. The delivery of primary care occurs across varied settings but is most frequently provided in a clinic and, increasingly, by interprofessional teams that may consist of family physicians, registered nurses (RNs), nurse practitioners, pharmacists, and other health professionals. In primary care settings, RNs function as generalists and provide a broad range of patient services across the lifespan, including preventative screening, health education and promotion, chronic disease prevention and management, and acute episodic care [ 3 , 4 , 5 , 6 ]. Specifically, family physicians and RNs represent a key collaborative relationship within these teams, contributing to strengthened primary care delivery and improvements in the comprehensiveness, efficiency, and value of care for patients [ 7 , 8 , 9 ]. Internationally, nurses are increasingly embedded in primary care settings and are recognized as the most prominent non-physician contributor to primary care teams, although the scope and speed of implementation in this area differs across countries [ 10 , 11 ]. Primary care nursing in Australia is the fastest growing employment sector, with 63% of general practices employing a primary care nurse (and 82% of this group representing RNs) [ 12 , 13 ]. The World Health Organization’s report [ 14 ] on the state of the world’s nursing workforce emphasizes the need to strengthen the integration of RNs into primary care, as well as the need for further research to evaluate their impact. Global workforce data are unavailable given the variability in scope of practice and role terminology, and the lack of available information across countries. A recent review of the international literature identified that titles used to refer to RNs in primary care vary across countries [ 15 ]. For instance, titles for this role in Canada are ‘family practice nurse’ and ‘primary care nurse’, whereas in Australia, the United Kingdom, and Netherlands this title is known as ‘general practice nurse’ [ 15 ]. For the purpose of this manuscript, ‘primary care RN’ will be used throughout.
Most research in this area to date has focused on describing the roles and activities of primary care RNs. A systematic review conducted by Norful et al. [ 5 ] synthesized 18 studies from eight countries related to primary care RNs and identified assessment, monitoring, and follow-up of patients with chronic diseases as fundamental roles of the primary care RN. In contrast, there have been a number of reviews conducted on the effectiveness of nurse practitioners in primary care [ 16 , 17 , 18 ]. It is imperative that primary care RNs also begin to demonstrate their contributions to patient care within this setting. Research examining RN effectiveness has primarily been conducted within the acute care and long-term care settings and focused on staffing, role enactment, and work environment. Within these settings, there is substantial evidence demonstrating the positive effects of RN staffing on improving care and reducing adverse outcomes for hospitalized patients [ 24 , 25 ].
Furthermore, select countries including Australia, Canada, New Zealand, and the United Kingdom have developed national standards of practice or competencies to define the scope and depth of practice for primary care RNs [ 4 , 19 , 20 , 21 , 22 , 23 ]. National competencies for primary care RNs were recently published in Canada [ 7 ]. These competencies articulate the unique scope of practice and contributions to patient care for primary care RNs across six overarching domains, namely, (1) Professionalism, (2) Clinical Practice, (3) Communication, (4) Collaboration and Partnership, (5) Quality Assurance, Evaluation and Research, and (6) Leadership.
Theoretical foundation
Determining effectiveness normally requires an examination of an intervention (e.g., primary care nursing) on a particular outcome. Incorporation of the patient perspective offers a more complete understanding of the challenges patients face within our healthcare system, especially those with long-term chronic diseases. Measuring the patient experience, which is a strong predictor of quality and value of care, should be done systematically [ 26 ]. The Organization for Economic Cooperation and Development (OECD) Patient Reported Indicator Surveys (PaRIS) Conceptual Framework was developed through a comprehensive process involving extensive international collaborations and provides a roadmap and survey tools (i.e., patient and provider questionnaires) to focus the evaluation of health care interventions on patient-reported metrics [ 27 ]. This framework provides a fuller evaluation of performance by complimenting other metrics (e.g., system/cost outcomes), while also focusing attention on the needs of the patient. The main domains of the framework include: patient reported experience measures (PREMs), patient reported outcome measures (PROMs), and health behaviours (e.g., physical activity, diet, tobacco use, alcohol use). Within primary care, the PaRIS Framework can serve as a guide for routine collection of these outcomes to facilitate quality improvement and patient-centered care [ 27 ]. A growing body of research in this area has adapted the use of this model to serve as an organizational and methodological framework. For example, multiple studies have used this framework as a method of investigating the suitability and feasibility of questionnaire and survey instruments when addressing patient perspectives [ 28 , 29 ] or in the evaluation of health-related quality of life measures from the patient’s perspective [ 30 ]. A recently published systematic review that explored the opportunities and challenges of routine collection of PREMs and PROMs data for melanoma care within primary care settings found that these measures can address important care gaps and facilitate research and assessment [ 31 ]. Similarly, a study employing qualitative methods found that the use of patient-reported measures by practitioners enhanced patients’ ability to self-manage, communicate, engage, and reflect during consultations [ 32 ]. A recent environmental scan of the PROMs landscape was conducted within Canada and internationally, indicating a lack of standardized programs for routine collection and reporting of patient outcomes. Consequently, the need for enhanced PROMs information has been identified as an area of high priority [ 33 ].
Although existing literature provides some information about the contributions of primary care RNs towards outcomes of care, a systematic review synthesizing the effectiveness of the primary care RN workforce is needed. Prior to beginning the study, the Cochrane Database of Systematic Reviews, the Joanna Briggs Institute (JBI) Library of Systematic Reviews, and the Prospective Register of Systematic Reviews (PROSPERO) were searched and no existing registered protocols or previous systematic reviews on this topic were identified. Evaluating PREMs, PROMs, and health behaviours, as well as other patient-level outcomes, is necessary to accurately demonstrate the contribution of primary care RNs, hold them accountable for their care, and generate evidence to inform decisions and policies that impact their implementation and optimization [ 34 , 35 ]. Therefore, the purpose of this systematic review is to summarize evidence examining primary care RNs’ impact on patient outcomes, including physiologic changes (via biomarkers), PREMs, PROMs, and health behaviours.
A systematic review of effectiveness was conducted using JBI Systematic Review methodology [ 36 ] and findings were reported in accordance with the 2009 (and where possible, the 2021) Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) framework [ 37 , 38 ]. Covidence software was used to manage and organize the literature [ 39 ] and enable a team approach for study and data review. The protocol for this systematic review is registered on PROSPERO (registration ID CRD42018090767). This paper presents a summary of findings from studies that report on patient outcomes, including biomarkers, PREMs, PROMs, and health behaviours. A full description of the methods and findings from studies that measured care delivery and system outcomes are reported in the companion paper “Effectiveness of Registered Nurses on System Outcomes in Primary Care: A Systematic Review” [ 40 ].

Search strategy
The search strategy aimed to include both published and unpublished literature. Following a limited search in CINAHL and Medline that identified optimal search terms, two members of the research team performed a comprehensive search of relevant electronic databases (see Supplementary File 1). Grey literature was identified using ProQuest Dissertations and Theses, MedNar, Google Scholar, the websites of relevant nursing organizations (e.g., International Council of Nurses, Community Health Nurses of Canada), and reference lists of included articles. There were no location or publication date restrictions on search criteria. Studies published in any year up to and including the date of article retrieval (January, 2022) were considered. Ongoing searches for grey literature included studies with publication dates up to January, 2022.
Inclusion criteria
Studies considered for inclusion reported on any quantitative study published in English with outcomes that directly measured, or were related to, an intervention attributable to a primary care RN. Only studies focused on RNs or equivalent (e.g., practice nurse, general nurse) [ 15 ] were included; if the RN designation was unclear or could not be determined based on the region of publication, the study was excluded. Studies that involved primary care RNs who underwent considerable advanced/focused training or those that exclusively examined structural variables were excluded. Full details regarding inclusion criteria are published in the companion paper [ 40 ].
Reviewers included two study authors (DR and JL) and two trained research assistants (AR and OP). All identified titles and abstracts were screened independently by two reviewers for potential study eligibility. Two reviewers independently screened full-text articles for relevance, applying pre-established eligibility criteria. Any disagreements were resolved through discussion, or by a third reviewer.
Risk of bias
The risk of bias and quality of each study was assessed using the Integrated Quality Criteria for Review of Multiple Study Designs (ICROMS) tool (see scoring matrix located in Supplementary File 2) [ 41 ]. All full-text articles that met eligibility criteria were appraised for quality by two independent reviewers. All studies that met inclusion/exclusion criteria also met the minimum ICROMS score to be included in the review.
Data extraction and synthesis
All eligible full-text studies underwent data extraction using a tool pre-designed and tested by the research team and based on the Cochrane Public Health Group Data Extraction Template [ 42 ]. Data extracted from the articles included: country and year of publication, study aim and design, description of primary care setting, patient sample sizes and demographics, details of study intervention and primary care RN involvement/role, outcome measures used to evaluate these interventions, and study results. To address the broad range of terms and descriptors used across included studies (e.g., traditional care, standard care, basic support, care delivered by anyone other than a primary care RN) and to provide clarity in the presentation of our results, we refer to all control groups as “usual care” or the “comparator group”. Outcomes were grouped in accordance with the OECD PaRIS Conceptual Framework Classification [ 27 ] into one of three categories defined by this model (i.e., PREMS, PROMs, health behaviours), and an additional category added by the research team (i.e., biomarkers) (see Table 1 ). Biomarkers consist of outcomes related to changes in patient health status as measured by clinical assessment (e.g., hemoglobin A1c [HbA1c] values, blood pressure, body weight). PREMs are defined as patient experience indicators related to health care access, autonomy in care, and overall satisfaction with care received, and are often assessed through self-report questionnaires or population-based surveys [ 27 ]. These outcomes can be summarized further based on patient experiences surrounding access (e.g., first point of contact), comprehensiveness of care, self-management support, trust, and overall perceived quality of care. PROMs are described as outcomes relating to a patient’s self-reported physical, mental, and social health status and can be categorized as either generic or condition-specific and applied to a broad patient population [ 27 ]. Outcomes identified on this level can be further categorized into functional status (e.g., disability, physical, mental, social function), symptoms, and health-related quality of life. The remaining outcomes were categorized according to the health behaviors classification, which includes lifestyle behaviors and actions that can contribute to a patient’s overall health status (e.g., physical activity, smoking status, dietary intake) [ 27 ]. Due to the diversity of included designs, interventions, and outcomes across studies, narrative synthesis was used to present study findings.
Figure 1 presents a PRISMA diagram outlining the results of the literature search.
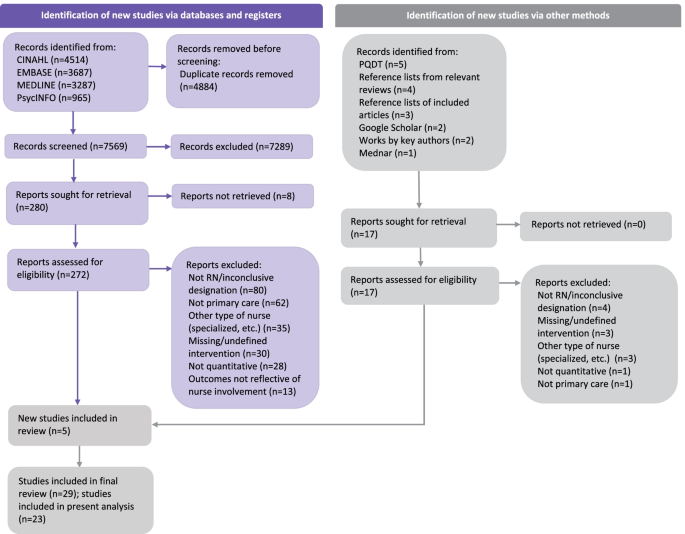
PRISMA Diagram of Literature Search. *This paper reports on studies that measured patient outcomes. Findings from studies that measured care delivery and system outcomes are reported in the companion paper "Effectiveness of registered nurses on system outcomes in primary care: a systematic review" [ 40 ]
Study characteristics
Of the 29 articles included in the final review, 23 reported on patient outcomes (included in the present analysis) [ 40 ]. Table 2 presents a detailed summary of the study characteristics for each of these articles. Studies were published between the years 1996–2021 and conducted in the United Kingdom ( n = 9), United States ( n = 6), Australia ( n = 5), and New Zealand ( n = 3). Study designs included randomized controlled trials ( n = 9), observational ( n = 8) (e.g., survey, secondary data analysis), cohort ( n = 1), non-controlled ( n = 2) and controlled before-after ( n = 1), and two studies with mixed-methods designs that combined a non-controlled before-after with a non-randomized controlled trial ( n = 1) or with an observational design ( n = 1). Sample sizes ranged from 81–2850 patients. Quality scores, as assessed by the ICROMS tool, varied between studies. Four studies were scored at the minimum threshold for their study design [ 46 , 56 , 61 , 65 ], six studies scored 1–2 points above threshold [ 44 , 45 , 48 , 49 , 53 , 57 ], and thirteen studies exceeded the minimum cut-off score by 3 or more points [ 43 , 47 , 50 , 51 , 52 , 54 , 55 , 58 , 59 , 60 , 62 , 63 , 64 ].
Overview of RN interventions
The nature of interventions examined in this review differed across studies. The most common interventions were related to chronic disease prevention and management, specifically, case management or targeted chronic disease management care (e.g., diabetes, obesity, hypertension, hypocholesteremia) ( n = 7) [ 43 , 44 , 45 , 46 , 47 , 48 , 49 ] and primary and secondary preventative care for patients at risk of chronic disease (e.g. prediabetes, coronary heart disease) ( n = 3) [ 50 , 51 , 52 ]. Other studies examined primary care RN-delivered smoking cessation support ( n = 4) [ 53 , 54 , 55 , 56 ], back pain education and management [ 57 ], pelvic floor muscle training [ 58 ], consultations aimed at increasing patient physical activity levels [ 59 , 60 ], and a telecare program for patients with diagnosed depression [ 61 ]. Four studies examined the impact of RN care in general (at an organizational-level); three of which focused on consultations with patients in general practice [ 62 , 63 , 64 ] and another which examined the impacts of a nurse-operated telephone consultation/triage service [ 65 ].
In thirteen studies, primary care RNs carried out the intervention independently without the support of other staff/providers [ 45 , 46 , 49 , 51 , 53 , 54 , 55 , 57 , 58 , 59 , 60 , 62 , 63 ], and in 10 studies, they carried out the intervention interdependently, in collaboration with health care providers (e.g., physicians, clinical pharmacy specialists [CPS], dieticians) or members of the research team (e.g., trial nurse facilitator) [ 43 , 44 , 47 , 48 , 50 , 52 , 56 , 61 , 64 , 65 ]. Three of these 10 studies involved evaluating RNs at the general practice-level and therefore are assumed to be evaluating an interdependent role involving support of other health care providers [ 47 , 61 , 64 ]. The presence and type of comparator group also differed across study designs. Specifically, five of the included studies compared a nurse-led intervention to the same intervention led by other health care providers [ 46 , 52 , 54 , 55 , 58 ]. Other studies compared nurse-led interventions with that of ‘usual care’ not associated with nurse involvement ( n = 4) [ 43 , 50 , 57 , 60 ], or with ‘usual care’ that was associated with reduced or alternative levels of nurse involvement ( n = 5) [ 44 , 49 , 53 , 56 , 59 ]. The remaining studies examined the effectiveness of a primary care RN-delivered intervention on specific outcomes of care using an observational or before-after design ( n = 5) [ 48 , 51 , 61 , 62 , 65 ], or did not contain a specific intervention, but rather, examined the impact of varying roles and practice characteristics of the primary care RN in general practice ( n = 4) [ 45 , 47 , 63 , 64 ].
Overview of outcomes
A total of 46 patient outcomes were identified across included studies (Table 3 ). Physiologic disease control outcomes, which were measured via biomarkers, included quality of care for diabetes (e.g., HbA1c, fasting blood glucose) [ 43 , 44 , 50 , 51 ], obesity (e.g., body mass index [BMI], waist circumference) [ 44 , 47 , 50 , 51 , 59 , 60 ], pelvic floor strength and endurance [ 58 ], hypercholesterolemia (e.g., total cholesterol) [ 49 ], and hypertension (e.g., blood pressure) [ 43 , 44 , 48 , 50 , 51 ]. Patient experience outcomes identified under the PREMs category included patient satisfaction with access to care (RN versus physician as first point of contact) [ 64 ], quality of self-management support (e.g., smoking cessation counseling, chronic disease services) [ 56 , 62 ], comfort/trust with primary care RN roles [ 45 ], and overall satisfaction or perceived quality of care with provider consultations, treatment, or advice/support received [ 45 , 51 , 55 , 57 , 63 , 65 ]. Patient reported outcomes identified within the PROMs category consisted of physical and social functional status [ 43 , 57 ], level of disability (e.g., activity levels, bed rest, work loss) [ 57 , 61 ], changes in self-reported anxiety, depression, or pain [ 59 , 60 , 61 ], adverse health events (e.g., falls, fractures, severe hypoglycemia) [ 43 , 59 , 60 ], and health-related qualify of life (e.g., physical activity, social activity) [ 43 , 46 , 51 , 52 , 60 ]. Lastly, outcomes grouped under the health behaviors classification included reduction and/or cessation of tobacco use [ 51 , 53 , 54 , 55 , 56 ], changes to physical activity (e.g., level of aerobic exercise, daily step count) [ 51 , 57 , 59 , 60 ], and improvements in dietary intake [ 49 ].
Physiologic disease control via biomarkers
Ten studies measured clinical patient outcomes when comparing interventions that involved primary care RNs to that of usual care or an intervention delivered by a comparator group. Clinical biomarkers included those for diabetes (HbA1c, fasting blood glucose), obesity (BMI, total fat mass), hypertension (blood pressure), and cardiovascular risk (total cholesterol). Of the ten studies, four examined diabetic control. After one year, Aubert et al [ 43 ]. reported significant differences in HbA1c values; patients in the primary care RN case management group had a larger mean reduction (-1.7 percentage points) over 12 months in comparison to usual care (-0.6 percentage points) (difference -1.1, 95% CI: -1.62 to 0.58; p < 0.001). Additionally, patients in the intervention group had a greater decrease in fasting blood glucose than the usual care group (-48.3 mg/dL versus -14.5 mg/dL; difference -33.8, 95% CI: -56.12 to 11.48; p = 0.003). Bellary et al [ 44 ]. found a small but non-significant reduction in HbA1c among their patient sample after two years. One additional study that conducted a retrospective data analysis of clinical outcome data from patients attending an independently RN-led primary care clinic, did not detect significant changes in HbA1c between initial intake at baseline and follow-up visits at various intervals (reported as 3 months to “several years” depending on the individual) [ 51 ].
Seven studies examined obesity-related outcomes such as BMI, weight, and total fat mass. In their adjusted regression models, Karnon et al [ 47 ]. reported that high level involvement of primary care RNs in the provision of obesity-related clinical activities (in comparison to low level involvement) yielded significantly larger mean reductions in BMI (mean difference -1.10, 95% CI: -0.45 to -1.76; p = 0.001) after one year, however, there were no significant improvements in terms of the proportion of patients losing weight (mean difference 0.09, 95% CI: -0.07 to 0.25; p = 0.259). Coppell et al [ 50 ]. found a significant weight reduction (-1.3 kg) in the primary care RN-led prediabetes intervention arm compared to usual care (gained 0.8 kg) (2.2 kg difference; p < 0.001). Mean BMI and waist circumference also decreased in the intervention arm compared to an increase in the control group, however, these differences were not significant. Likewise, a third study reported that fat mass was slightly reduced at 12 months, but differences between the intervention and control groups were equivalent when the primary care RN group was compared to both postal intervention ( p = 0.54) and usual care ( p = 0.30) [ 60 ]. There were no significant reductions in BMI or waist circumference in the remaining four studies [ 43 , 44 , 51 , 59 ].
Five studies investigated the impact of enhanced nurse involvement in primary care delivery on blood pressure. Bellary et al [ 44 ]. reported significant differences between groups in diastolic blood pressure (-1.91, 95% CI: -2.88 to -0.94 mm Hg; p = 0.0001) and mean arterial pressure (1.36, 95% CI: -2.49 to -0.23 mm Hg; p = 0.018), favoring the intervention (additional time spent with a primary care RN). In a second study conducted by O’Neill et al. in which the RN independently assessed blood pressure and collaborated with either a CPS or physician in hypertension case management, [ 48 ] there was a greater decrease in systolic blood pressure in patients who received care from CPS and primary care RN teams (-14 mm Hg) compared to patients receiving care from physician-directed primary care RNs (-10 mm Hg) ( p = 0.04), however, there were no significant changes in diastolic blood pressure between groups. The remaining three studies found no significant changes in blood pressure when comparing a primary care RN-led intervention to that of usual care [ 43 , 50 ] or from initial baseline to follow-up [ 51 ].
Total cholesterol was measured in four studies. Pine et al [ 49 ]. reported that the mean total cholesterol level decreased by 0.29 mmol/L (11.2 mg/dL) (4.3%) from the initial physician visit to the first primary care RN visit. Following five counseling sessions by a primary care RN, the mean total cholesterol levels of all patients decreased (-0.14 mmol/L; p = 0.4). However, during the follow-up comparison study, there were no significant differences in total cholesterol improvement between the nurse-counseling intervention group and the comparison patients, and total cholesterol levels in both groups improved significantly ( p = 0.002). The remaining three studies reported equivalent results in regards to total cholesterol reduction [ 43 , 44 , 50 ].
Patient experience outcomes via PREMS
Nine articles reported on patient experience outcomes via PREMs: overall perceived quality of care [ 45 , 51 , 55 , 63 , 65 ], self-management support [ 56 , 62 ], access (first point of primary care contact) [ 64 ], comprehensiveness [ 57 ], and trust [ 45 ].
In regard to overall perceived quality of care, Halcomb and colleagues [ 45 ] found that Australian patients were very satisfied and comfortable with chronic disease care delivered by a primary care RN. This was particularly true for patients with diabetes who reported being almost three times more comfortable (38% versus 14%, p = 0.016) with their encounter than patients who consulted for other chronic health conditions. A similar study in New Zealand also revealed high satisfaction with primary care RN-delivered services overall, with increased satisfaction associated with an increased number of visits (i.e., those who had more than four previous visits to the primary care RN) after controlling for demographic factors [ 63 ]. Longer consultation time with a primary care RN resulted in higher patient satisfaction (OR = 2.50, 95% CI: 1.43 to 4.35; p < 0.01) and patient enablement (OR = 2.55, 95% CI: 1.45 to 4.50; p < 0.01) than shorter consultation time [ 62 ]. Moreover, patients who attended practices where primary care RNs worked with broad scopes of practice and high levels of autonomy were more satisfied (OR = 1.76, 95% CI: 1.09 to 2.82; p = 0.04) and more enabled (OR = 2.56, 95% CI: 1.40 to 4.68; p < 0.01) than patients who attended practices where nurses worked with more limited scopes of practice and lower levels of autonomy [ 62 ].
Patients also reported improved health, better understanding of disease diagnosis, medication, and treatment plan, and more motivation for self-management as a result of primary care RN-led lifestyle clinics focused on diabetes, smoking cessation, women’s health, cardiovascular risk, respiratory/asthma, and diet/nutrition [ 51 ]. Furthermore, patients reported positive experiences with primary care RN-led telephone consultations for acute illness [ 65 ], back pain education [ 57 ], and smoking cessation support [ 55 , 56 ]. For instance, Cherkin et al. [ 57 ] reported higher satisfaction ( p < 0.01) and higher perceived knowledge ( p < 0.001) for patients who received a primary care RN-led educational intervention for back pain than those in the usual care group. Nearly all patients (98%, n = 385) in an Australian study [ 56 ] that examined smoking cessation behavioral support from a primary care RN rated the support provided as helpful (19%) or very helpful (79%) and indicated that they may have been more successful with smoking cessation if they had been able to have more sessions with the RN. With respect to access to care, a study by Caldow et al [ 64 ]. found that patients expressed satisfaction and preference with primary care RN versus physician consultations for minor illness as first point of contact if this resulted in a reduced waiting time, suggesting that patients would be accepting of an expanded nursing role in primary care.
Patient reported outcomes via PROMs
Patient reported outcome measures via PROMs were examined across eight studies and included health-related quality of life [ 43 , 46 , 51 , 52 , 60 ], symptoms [ 59 , 60 , 61 ], self-efficacy [ 60 ], and functional status [ 57 ].
Health-related quality of life, as measured through patient self-report, was assessed in five studies [ 43 , 46 , 51 , 52 , 60 ]. In a 12-month randomized controlled trial conducted by Aubert et al., [ 43 ] a primary care RN-led case management model of adult diabetes care was compared with that of usual care in a primary care setting. Health-related quality of life was assessed by a validated questionnaire developed by the Centers for Disease Control and Prevention for the Behavioral Risk Factor Surveillance System to assess patient perception of health status across four domains. The results demonstrated an improved perception of health status in both groups, with patients in the intervention group more than twice as likely to report improvement in health status score (mean change = 0.47) as those in the usual care group (mean change = 0.20) ( difference= 0.27; 95% CI: -0.03 to 0.57; p = 0.02). In contrast, the other four studies [ 46 , 51 , 52 , 60 ] examining health-related quality of life did not report significant differences in regards to these outcomes, including two cluster randomized controlled trials [ 46 , 52 , 60 ]. One study assessed the effectiveness of three different methods of secondary prevention care of coronary heart disease (recall to a primary care RN; recall to a physician; audit and feedback) [ 52 ], while the other compared the efficacy of a primary care RN-supported physical activity intervention to that of usual care [ 60 ]. Both studies reported equivalent scores between groups on all dimensions of patient self-reported quality of life measurements. Lastly, an observational study by Marshall et al [ 51 ]. used patient satisfaction surveys to assess perceptions of Nurse-Led Healthy Lifestyle Clinics (NLHLC) in New Zealand. Using scores from the Dartmouth Primary Care Cooperative (COOP) Information charts [ 66 ], it was noted that there were no statistically significant differences in the COOP dimensions related to self-perceived quality of life from first clinic visit to last clinic visit. However, significant improvements were noted in relation to the COOP variables related to patient-perceived social activity (mean difference = -0.20; p = 0.049), change in health (mean difference = -0.42; p = 0.001), and overall health (mean difference = -0.21; p = 0.025).
Patient self-reported symptoms were measured in three studies [ 59 , 60 , 61 ] and included outcomes related to both mental and physical health (anxiety, depression, pain), as well as the occurrence of adverse health events (injuries, fractures, cardiovascular events, deaths, and deterioration of any pre-existing health problems). In an observational study of a nurse telecare intervention for adults with depression in the United States, Pearson et al [ 61 ]. found a significant improvement in mean scores on the SF-12 Mental Functioning Scale between baseline (mean = 29.9) and 6-months post-intervention (mean = 48.2) ( p < 0.0001). During the same time interval, significant differences were noted on the Hamilton Depression Rating scale (14.6 to 6.5; p < 0.001), as well as the mean scores on the Work Limitations Questionnaire (70.4 to 87.2; p < 0.001), which both represent an improvement in functioning. Paired t-test results for the difference in mean scores on all three instruments were statistically significant ( p = 0.0001) and the majority of patients (63%) experienced at least a 50% reduction in the Hamilton Depression Rating score at 6-months. The remaining studies to examine self-reported symptoms as an outcome were two randomized controlled studies that measured the effects of a primary care RN-delivered intervention on patient physical activity [ 59 , 60 ]. Both studies assessed changes to patient self-reported levels of depression, anxiety, and pain and incidents of adverse health events. The results of both studies reported no statistically significant between-group differences in mean scores of either symptom at 3- or 12-months post-intervention. Additionally, while total number of adverse events did not differ between groups for either study, Harris et al [ 60 ]. found a significant reduction in cardiovascular events among the intervention group over the 12 month period ( p = 0.04).
Patient self-efficacy was examined in a three-arm cluster randomized controlled study conducted by Harris et al [ 60 ]., in which patient-reported levels of exercise self-efficacy were examined at 3- and 12-months following a physical activity intervention. Exercise self-efficacy in this study was characterized by a patient’s willingness to set goals, create action plans, engage in self-monitoring, and seek out social support, and are directly related to long-term physical activity adherence. Findings indicated that exercise self-efficacy was significantly increased in both intervention groups at 3-months for postal group (pedometer delivered by mail) versus control (Effect Size [ES] = 1.1, 95% CI: 0.2 to 2.0; p = 0.01), primary care RN group versus control (ES = 2.3, 95% CI: 1.4 to 3.2; p < 0.001), and primary care RN group versus postal group (ES = 1.2, 95% CI: 0.3 to 2.1; p = 0.01). For primary care RN group versus control group, the difference remained significant at the 12-month follow-up (ES = 1.2, 95% CI: 0.3 to 2.2; p = 0.01), but not for the postal group versus control ( p = 0.2) or the primary care RN group versus postal group ( p = 0.22).
The sole study to evaluate functional status was a randomized controlled trial conducted by Cherkin et al [ 57 ]. comparing usual care, usual care plus an educational booklet, and usual care plus an educational session with a primary care RN and an educational booklet to improve outcomes of low back pain in primary care. None of the interventions had a statistically significant effect on functional status, including days of limited activity, bed rest, or work loss resulting from back pain one week after the intervention or at any subsequent follow-up.
Health behaviors
Of all the studies included ( n = 23), nine considered health behavior outcomes. Among the studies examining the impact of a primary care RN-led intervention on health behaviors, it was found that tobacco use was the most documented health behavior ( n = 5) [ 51 , 53 , 54 , 55 , 56 ]. Tobacco use was examined by looking at both abstinence from smoking, as well as daily reductions or changes to smoking behaviour, and this was measured at multiple follow-up periods throughout the duration of the intervention. All five studies demonstrated positive changes in smoking-related health behaviors following either an independent [ 51 , 53 , 54 , 55 ] or interdependent [ 56 ] primary care RN intervention. For example, Byers et al [ 54 ]. compared a primary care RN-led intervention with a physician-led intervention to support smoking cessation. The results show that support provided by the primary care RN was equivalent to that provided by the comparator group (29.1% versus 18.2% quit rate, respectively; p = 0.077) in supporting the patient to quit smoking. Marshall et al [ 51 ]. looked at primary care RN-led healthy habits lifestyle clinics for patients with or at risk of chronic disease within targeted populations with known health inequalities. Following the intervention, 94% of patients reported having a better understanding of their diagnosis, medication and treatement plan, and an increase in motivation to self-manage their health needs. Other studies have examined the impact of nursing interventions on patient-reported levels of physical activity [ 57 , 59 , 60 ]. Only one study considered adherence to healthy eating as a health outcome following a RN-led intervention in primary care [ 49 ]. In this study, Pine and colleagues evaluated the effect of a nursing intervention to support cholesterol lowering for patients diagnosed with hypercholesterolemia. To do this, primary care RNs provided a total of five counseling visits focused on nutritional education and physical activity (1-month after referral, and at 3-, 5-, 7-, and 12-months) to 82 patients with total cholesterol higher than 6.21 mmol/l. Intervention patients were already following a diet consistent with the program at baseline, however, the mean score for Section 1 of the Eating Pattern Assessment Tool (questions related to foods with serum cholesterol-raising potential) improved from 23.4 at the first visit to 20.4 at the final visit ( p < 0.001).
This systematic review presents a comprehensive synthesis of literature examining the impact of primary care RNs on patient outcomes. The findings suggest that outcomes resulting from care provided by primary care RNs are comparable and complementary to care provided by other primary care providers, specifically with respect to chronic disease prevention and management, smoking cessation, and wellness counseling. This review supports that primary care RNs deliver appropriate and high-quality patient care. There was a high level of patient satisfaction reported regarding experiences with RN-led care. Patients appear to be comfortable with RNs providing primary care services and taking on expanded roles in primary care. This is consistent with findings from other studies that have examined patient satisfaction and comfort with RN roles in primary care practices across multiple countries [ 67 , 68 , 69 , 70 ]. Our findings are aligned with existing evidence that has linked patient experiences of care to the level of autonomy and scope of practice of the RN in the clinical setting. A recently published study from Canada evaluated patient experiences in primary care organizations and determined that patient-reported experience was significantly enhanced in clinics in which RNs systematically followed patients and used their scope of practice to their full potential [ 71 ].
Patient experience is a strong indicator of patient-perceived quality of care and fundamental to achieving desired patient outcomes for a range of physical and mental health domains [ 72 , 73 , 74 , 75 , 76 ]. The recently developed PaRIS Framework served as a valuable tool for organizing patient-reported outcomes, however, it did not capture all patient outcomes identified within the studies included in this review. For example, clinical biomarkers, such as HbA1c and fasting blood glucose (used as a measure of diabetes care quality), were not considered in the PaRIS Framework and therefore added by the study authors during the analysis phase as an additional patient outcome category. Similarly, studies evaluating RN interventions in primary care did not consider many components of the PaRIS Framework, such as delivery system design (e.g., clinic remuneration, remote consultations), individual and sociodemographic factors (e.g., patient demographic characteristics), and health and health care capabilities, and only measured select components from the patient-reported experiences of care, health behaviours, and patient-reported outcome domains. For instance, many articles did not provide information regarding RN characteristics, such as level of education, years of experience, or specific roles/tasks that they performed in-clinic prior to the intervention that might have impacted outcomes observed. In addition, conceptual definitions of outcomes within included studies may vary and not align with meanings as defined within the PaRIS Framework. A taxonomy for RN outcomes may be useful and should be considered in future revisions and applications of the OECD PaRIS Framework.
The included studies evaluated a variety of primary care RN interventions but did not capture all roles that encompass their broad scope of practice. Commonly offered services by primary care RNs that have yet to be comprehensively evaluated include prenatal and well-baby care, therapeutic interventions (e.g., wound care, treatment of infections), preventative care (e.g., immunizations, health promotion and education) and care coordination (e.g., nursing surveillance, system navigation). Although self-management supports (e.g., smoking cessation, physical activity, diabetes, nutrition, pain management, healthy lifestyle promotion, chronic disease prevention) were examined in a few studies [ 43 , 44 , 49 , 50 , 51 , 53 , 54 , 55 , 56 , 57 , 59 , 60 ], further evaluation of self-management and behaviour support interventions (included within the PaRIS Framework) offered by RNs in primary care is needed. Moreover, recently developed competencies identify that, in addition to clinical practice activities centered around patient care provision, primary care RNs engage in a wide range of non-clinical roles, such as leadership, research, and interprofessional collaboration. These non-clinical domains of practice for primary care RNs require further understanding and evaluation.
There is a general apprehension among some medical practitioners that if RNs assume more responsibilities or enhanced roles within primary care settings, high-quality care and patient safety will be compromised [ 77 , 78 ]. Findings from this study show that patient care is equivalent to that of “usual care” and in many cases, produced better patient outcomes when the intervention was provided by a primary care RN. This aligns with literature in the acute care and long-term care settings [ 24 , 25 ]. The findings from our review call into question concerns that RN-provided care increases risk or reduces quality of care and equally, lends support towards the efficacy of primary care RN care provision on improvements to patient outcomes. Additionally, primary care RNs are required to practice within their legislated and regulated scope of practice, regardless of the practice setting or types of clinical roles performed [ 79 , 80 ].
Generally, there are methodological challenges associated with examining the contributions of a specific health care provider within the context of a team [ 81 , 82 , 83 ]. As the focus of practice and research moves towards interdisciplinary teams, it is increasingly difficult to isolate and evaluate the impact of primary care RN interventions. In addition, the roles of primary care RNs and team compositions vary across practice settings. Although this review exclusively examined studies in which an intervention was delivered by a RN, many studies were excluded because of unclear terminology surrounding the nursing designation/role (i.e., unable to discern whether nurse in study was a RN or equivalent). Furthermore, the review included only nine randomized controlled trials, which provide the strongest level of evidence, that specifically compared RN-led interventions to care delivered by other health care professionals and/or usual care [ 43 , 52 , 53 , 57 , 58 , 59 , 60 , 84 , 85 ]. Comparator groups in studies varied considerably, impacting the ability to make comparisons across studies and limiting the generalizability of findings from this study. Despite these challenges, this review provides preliminary evidence on patient outcomes used to evaluate a variety of different RN interventions in a multidimensional health care environment. The findings from this study, coupled with an existing framework (e.g., OECD PaRIS Framework) serve as a tool to map roles and activities to outcomes and guide future evaluation of primary care RNs. Overall, as the presence of RNs in primary care increases globally, further evaluation research implementing control/comparison groups into study design and controlling for confounding factors (e.g., nurse characteristics) is needed to strengthen the evidence related to the effectiveness of RNs in primary care.
Strengths and limitations
This review provides preliminary evidence regarding the effectiveness of RNs on patient outcomes in primary care. Traditional means of measuring the effectiveness of care provision in the healthcare sector have focused mainly on the use of clinical data. A strength of this systematic review is its patient-oriented approach that assesses health outcomes from the patient perspective [ 27 , 86 ]. Additional strengths of this systematic review include the application of a comprehensive search strategy and use of the PRISMA checklist in the screening process. However, despite utilizing a comprehensive search strategy, it is possible that not all relevant studies were retrieved and included in this review. Furthermore, although we conducted an appraisal using an established quality assessment tool (i.e., ICROMS), this tool presented certain challenges. For instance, although a strength of this tool is that it offered criteria to assist with the process of assigning quality scores, there is a degree of subjectivity involved in the appraisal process. In addition, the minimum cut-off scores varied across study designs and therefore, made comparisons of the quality between different types of studies difficult. Similarly, the score itself is difficult to interpret without an understanding of the tool and design matrix (limitations of articles are summarized in Supplementary Table 3). The ICROMS tool was also not designed to specifically appraise mixed methods or observational designs. The lack of consistent and available data regarding terminology used to describe RNs, or equivalent nursing titles, across countries limited the ability to include studies published in certain regions. Only studies published in the English language were included, which may limit generalizability to certain countries. High-quality research employing robust study designs (e.g., randomized controlled trials) need to be conducted to further understand the impact of RNs on patient outcomes in primary care.
Primary care RNs can provide patient care that is comparable and complementary to that of other primary care providers, specifically with respect to patient satisfaction, enablement, self-reported quality of life, self-efficacy, and improvements in health behaviours. This review provides preliminary evidence regarding the effectiveness of RNs on patient outcomes in primary care. Findings are applicable to researchers and other stakeholders engaged in primary care reform and can inform further integration and optimization of this role, as well as contribute to future research.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Change history
22 june 2022.
A Correction to this paper has been published: https://doi.org/10.1186/s12913-022-08204-x
Abbreviations
Registered Nurses
Patient Reported Indicator Survey
Patient-reported experience measures
Patient-reported outcome measures
Joanna Briggs Institute
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
Prospective Register of Systematic Reviews
Integrated Quality Criteria for Review of Multiple Study Designs
Hemoglobin A1c
Body mass index
Clinical Pharmacy Specialist
Primary Care Cooperative
Nurse-Led Healthy Lifestyle Clinic
Organization for Economic Cooperation and Development
Effect Size
National Academies of Sciences, Engineering, and Medicine. Implementing high-quality primary care: rebuilding the foundation of health care. The National Academies Press. 2021. https://www.nap.edu/read/25983 . Accessed 08 Nov 2021.
Muldoon LK, Hogg WE, Levitt M. Primary care (PC) and primary health care (PHC): what’s the difference? Can J Pub Health. 2006;87(5):409–11.
Article Google Scholar
Halcomb E, Stephens M, Bryce J, Foley E, Ashley C. Nursing competency standards in primary health care: an integrative review. J Clin Nurs. 2016;25:1193–205.
Lukewich J, Allard M, Ashley L, Aubrey-Bassler K, Bryant-Lukosius D, Klassen T, et al. National competencies for registered nurses in primary care: a Delphi study. West J Nurs Res. 2020;42(12):1078–87. https://doi.org/10.1177/0193945920935590 .
Article PubMed PubMed Central Google Scholar
Norful A, Martsolf G, de Jacq K, Poghosyan L. Utilization of registered nurses in primary care teams: a systematic review. Int J Nurs Stud. 2017;74:15–23. https://doi.org/10.1016/j.ijnurstu.2017.05.013 .
Poitras ME, Chouinard MC, Gallagher F, Fortin M. Nursing activities for patients with chronic disease in primary care settings: a practice analysis. Nurs Res. 2018;67(1):35–42. https://doi.org/10.1097/NNR.0000000000000253 .
Article PubMed Google Scholar
College of Family Physicians of Canada. Patient-centred primary care in Canada: bring it on home. CFPC. 2009. https://www.cfpc.ca/CFPC/media/Resources/Health-Care-Delivery/Bring-it-on-Home-FINAL-ENGLISH.pdf . Accessed 09 Nov 2021.
Schottenfeld L, Petersen D, Peikes D, et al. Creating patient-centered team-based primary care. Agency for Healthcare Research and Quality. 2016. https://pcmh.ahrq.gov/sites/default/files/attachments/creating-patient-centered-team-based-primary-care-white-paper.pdf . Accessed 08 Nov 2021.
Smolowitz J, Speakman E, Wojnar D, Whelan EM, Ulrich S, Hayes C, et al. Role of the registered nurse in primary health care: meeting health care needs in the 21st century. Nurs Outlook. 2015;63(2):130–6. https://doi.org/10.1016/j.outlook.2014.08.004 .
Organization for Economic Cooperation and Development (OECD). Health at a glance 2019: OECD Indicators. OECD Publishing. 2019. https://www.oecd-ilibrary.org/docserver/4dd50c09-en.pdf?expires=1631157370&id=id&accname=guest&checksum=AA4126CD8BEAEF8E2B96A614027E7B0D . Accessed 08 Nov 2021.
Freund T, Everett C, Griffiths P, Hudon C, Naccarella L, Laurant M. Skill mix, roles and remuneration in the primary care workforce: who are the healthcare professionals in the primary care teams across the world? Int J Nurs Stud. 2015;52:727–43. https://doi.org/10.1016/j.ijnurstu.2014.11.014 .
Australian Institute of Health and Welfare. A profile of primary health care nurses. Australian Government. 2020. https://www.aihw.gov.au/reports/primary-health-care/a-profile-of-primary-care-nurses/contents/primary-health-care-nurses . Accessed 08 Nov 2021.
Australian Primary Health Care Association . General practice nursing. APNA. 2021 https://www.apna.asn.au/profession/what-is-primary-health-care-nursing/general-practice-nursing . Accessed 08 Nov 2021.
World Health Organization. State of the world's nursing: investing in education, jobs and leadership. WHO. 2020. https://www.who.int/publications/i/item/9789240003279 . Accessed 07 Nov 2021.
Barrett C, Ryan D, Poitras ME, Norful AA, Martin-Misener R, Tranmer J, et al. Job titles and education requirements of registered nurses in primary care: an international document analysis. Int J Nurs Stud Adv. 2021:e1–35. doi: https://doi.org/10.1016/j.ijnsa.2021.100044 .
Canadian Nurses Association. Effectiveness of registered nurses and nurse practitioners in supporting chronic disease self-management. CNA. 2012.
Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002;324(7341):819–23.
Martin-Misener R, Harbman P, Donald F, Reid K, Kilpatrick K, Carter N, et al. The cost-effectiveness of nurse practitioners in primary and specialised ambulatory care: a systematic review. BMJ Open. 2015;5(6): e007167. https://doi.org/10.1136/bmjopen-2014-007167 .
Australian Nursing and Midwifery Federation. National practice standards for nurses in general practice. Australian Nursing and Midwifery Federation- Federal Office. 2014. http://www.anmf.org.au/documents/National_Practice_Standards_for_Nurses_in_General_Practice.pdf . Accessed 08 Nov 2021.
Canadian Family Practice Nurses Association. National competencies for registered nurses in primary care. CFPNA. 2019. https://www.cfpna.ca/copy-of-resources-1 . Accessed 08 Nov 2021.
Mid-Central District Health Board, New Zealand Nurses Organisation, The New Zealand College of Primary Health Care Nurses. Aotearoa New Zealand primary health care nursing standards of practice. New Zealand Nurses Organization. 2019. https://www.nzno.org.nz/Portals/0/publications/Primary%20Health%20Care%20Nursing%20Standards%20of%20Practice%202019.pdf?ver=XYUZI2v-cpVH28Oy1rhfdw%3d%3d . Accessed 08 Nov 2021.
The Queen’s Nursing Institute. The QNI standards of education and practice for nurses new to general practice nursing. QNI. 2020. https://www.qni.org.uk/wp-content/uploads/2020/05/Standards-of-Education-and-Practice-for-Nurses-New-to-General-Practice-Nursing-1.pdf . Accessed 08 Nov 2021.
The Queen’s Nursing Institute, The Queen’s Nursing Institute Scotland. The QNI/QNIS voluntary standards for general practice nursing education and practice. QNI & QNIS. 2017. https://www.qni.org.uk/wp-content/uploads/2016/09/GPN-Voluntary-Standards-for-Web.pdf . Accessed 09 Nov 2021.
Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care. 2007;45(12):1195–204.
Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346(22):1715–22. https://doi.org/10.1056/NEJMsa012247 .
Berkowitz B. The patient experience and patient satisfaction: measurement of a complex dynamic. OJIN. 2016;21(1): e1. https://doi.org/10.3912/ojin.vol21no01man01 .
Organization for Economic Cooperation and Development. Measuring what matters: the patient-reported indicator surveys. OECD Publishing. 2019. https://ec.europa.eu/health/sites/default/files/systems_performance_assessment/docs/pagoda_en.pdf . Accessed 08 Nov 2021.
Gerrard G, Jones R, Hierons RJ. How did we do? An investigation into the suitability of patient questionnaires (PREMs and PROMs) in three primary care oral surgery practices. Br Dent J. 2017;223(1):27–32.
Article CAS Google Scholar
Depla AL, Ernst-Smelt HE, Poels M, Crombag NM, Franx A, Bekker MN. A feasibility study of implementing a patient-centered outcome set for pregnancy and childbirth. Health Sci Rep. 2020;3(3): e168. https://doi.org/10.1002/hsr2.168 .
Aiyegbusi OL, Kyte D, Cockwell P, Anderson N, Calvert M. A patient-centered approach to measuring quality in kidney care: patient-reported outcome measures and patient-reported experience measures. Curr Opin Nephrol Hypertens. 2017;26(6):442–9. https://doi.org/10.1097/MNH.0000000000000357 .
Blood Z, Tran A, Caleo L, Saw R, Dieng M, Shackleton M, et al. Implementation of patient-reported outcome measures and patient-reported experience measures in melanoma clinical quality registries: a systematic review. BMJ Open. 2021;11(2): e040751. https://doi.org/10.1136/bmjopen-2020-040751 .
Wheat H, Horrell J, Valderas JM, Close J, Fosh B, Lloyd H. Can practitioners use patient reported measures to enhance person centred coordinated care in practice? A qualitative study. Health Qual Life Outcomes. 2018;16(1): e223. https://doi.org/10.1186/s12955-018-1045-1 .
Canadian Institutes for Health Information. PROMs background document. CIHI. 2015. https://www.cihi.ca/sites/default/files/proms_background_may21_en-web_0.pdf . Accessed 09 Nov 2021.
Dubois CA, D’Amour D, Pomey MP, Girard F, Brault I. Conceptualizing performance of nursing care as a prerequisite for better measurement: a systematic and interpretive review. BMC Nurs. 2013;12:7. https://doi.org/10.1186/1472-6955-12-7 .
Sidani S, Irvine D. A conceptual framework for evaluating the nurse practitioner role in acute care settings. J Adv Nurs. 1999;30(1):58–66. https://doi.org/10.1046/j.1365-2648.1999.01049.x .
Article CAS PubMed Google Scholar
Aromataris E, Munn Z, eds . Joanna Briggs Institute reviewer's manual. The Joanna Briggs Institute. 2017. https://reviewersmanual.joannabriggs.org/ . Accessed 09 Nov 2021.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1136/bmj.b2535 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. https://doi.org/10.1136/bmj.n71 .
Covidence. Covidence systematic review software [computer program]. Veritas Health Innovation. n.d. www.covidence.org
Lukewich J, Ryan D, Asghari S, Marshall EG, Mathews M, Swab M, et al. Effectiveness of registered nurses on system outcomes in primary care: a systematic review. BMC Health Services. 2022;22:440. https://doi.org/10.1186/s12913-022-07662-7
Zingg W, Castro-Sanchez E, Secci FV, Edwards R, Drumright LN, Sevdalis N, et al. Innovative tools for quality assessment: integrated quality criteria for review of multiple study designs (ICROMS). Pub Health. 2016;133:19–37. https://doi.org/10.1016/j.puhe.2015.10.012 .
Cochrane Public Health Group. Data extraction and assessment template. Cochrane. 2011.
Aubert RE, Herman WH, Waters J, Moore W, Sutton D, Peterson BL, et al. Nurse case management to improve glycemic control in diabetic patients in a health maintenance organization. A randomized, controlled trial. Ann Intern Med. 1998;129(8):605–12.
Bellary S, O’Hare JP, Raymond NT, Gumber A, Mughal S, Szczepura A, et al. Enhanced diabetes care to patients of south Asian ethnic origin (the United Kingdom Asian Diabetes Study): a cluster randomised controlled trial. Lancet. 2008;371(9626):1769–76. https://doi.org/10.1016/S0140-6736(08)60764-3 .
Halcomb EJ, Salamonson Y, Cook A. Satisfaction and comfort with nursing in Australian general practice. Collegian. 2015;22(2):199–205.
Iles RA, Eley DS, Hegney DG, Patterson E, Young J, Del Mar C, et al. Revenue effects of practice nurse-led care for chronic diseases. Aust Health Rev. 2014;38(4):363–9. https://doi.org/10.1071/AH13171 .
Karnon J, Ali Afzali HH, Gray J, Holton C, Banham D, Beilby J. A risk adjusted cost-effectiveness analysis of alternative models of nurse involvement in obesity management in primary care. Obesity. 2013;21(3):472–9. https://doi.org/10.1002/oby.20100 .
O’Neill JL, Cunningham TL, Wiitala WL, Bartley EP. Collaborative hypertension case management by registered nurses and clinical pharmacy specialists within the Patient Aligned Care Teams (PACT) model. J Gen Intern Med. 2014;29(2):S675–81. https://doi.org/10.1007/s11606-014-2774-4 .
Pine DA, Madlon-Kay DJ, Sauser M. Effectiveness of a nurse-based intervention in a community practice on patients’ dietary fat intake and total serum cholesterol level. Arch Fam Med. 1997;6:129–34.
Coppell KJ, Abel SL, Freer T, Gray A, Sharp K, Norton JK, et al. The effectiveness of a primary care nursing-led dietary intervention for prediabetes: a mixed methods pilot study. BMC Fam Pract. 2017;18(1):106. https://doi.org/10.1186/s12875-017-0671-8 .
Marshall B, Floyd S, Forrest R. Clinical outcomes and patients’ perceptions of nurse-led healthy lifestyle clinics. J Prim Health Care. 2011;3(1):48–52.
Moher M, Yudkin P, Wright L, Turner R, Fuller A, Schofield T, et al. Cluster randomised controlled trial to compare three methods of promoting secondary prevention of coronary heart disease in primary care. BMJ. 2001;322(7298):1338. https://doi.org/10.1136/bmj.322.7298.1338 .
Article CAS PubMed PubMed Central Google Scholar
Aveyard P, Brown K, Saunders C, Alexander A, Johnstone E, Munafò MR, et al. Weekly versus basic smoking cessation support in primary care: a randomised controlled trial. Thorax. 2007;62(10):898–903. https://doi.org/10.1136/thx.2006.071837 .
Byers MA, Wright P, Tilford JM, Nemeth LS, Matthews E, Mitchell A. Comparing smoking cessation outcomes in nurse-led and physician-led primary care visits. J Nurs Care Qual. 2018;33(3):272–8. https://doi.org/10.1097/NCQ.0000000000000296 .
Faulkner K, Sutton S, Jamison J, Sloan M, Boase S, Naughton F. Are nurses and auxiliary healthcare workers equally effective in delivering smoking cessation support in primary care? Nicotine Tob Res. 2016;18(5):1054–60. https://doi.org/10.1093/ntr/ntv206 .
Zwar NA, Richmond RL, Forlonge G, Hasan I. Feasibility and effectiveness of nurse-delivered smoking cessation counselling combined with nicotine replacement in Australian general practice. Drug Alcohol Rev. 2011;30(6):583–8. https://doi.org/10.1111/j.1465-3362.2010.00243.x .
Cherkin DC, Deyo RA, Street JH, Hunt M, Barlow W. Pitfalls of patient education. Limited success of a program for back pain in primary care. Spine. 1996;21(3):345–5. https://doi.org/10.1097/00007632-199602010-00019.
Waterfield A, Waterfield M, Campbell J, Freeman R. Can effective supervised pelvic floor muscle training be provided by primary care nurses? A randomized controlled trial. Int Urogynecol J. 2021;32(10):2717–25.
Harris T, Kerry SM, Victor CR, Ekelund U, Woodcock A, Iliffe S, et al. A primary care nurse-delivered walking intervention in older adults: PACE (pedometer accelerometer consultation evaluation)-Lift cluster randomised controlled trial. PLoS Med. 2015;12(2): e1001783. https://doi.org/10.1371/journal.pmed.1001783 .
Harris T, Kerry SM, Limb ES, Victor CR, Iliffe S, Ussher M, et al. Effect of a primary care walking intervention with and without nurse support on physical activity levels in 45- to 75-Year-olds: the pedometer and consultation evaluation (PACE-UP) cluster randomised clinical trial. PLoS Med. 2017;14(1): e1002210. https://doi.org/10.1371/journal.pmed.1002210 .
Pearson B, Katz S, Soucie V, Hunkeler E, Meresman J, Rooney T, et al. Evidence-based care for depression in Maine: dissemination of the Kaiser Permanente Nurse Telecare Program. Psych Quarterly. 2003;74(1):91–102. https://doi.org/10.1023/a:1021149923867 .
Desborough J, Bagheri N, Banfield M, Mills J, Phillips C, Korda R. The impact of general practice nursing care on patient satisfaction and enablement in Australia: a mixed methods study. Int J Nurs Stud. 2016;64:108–19. https://doi.org/10.1016/j.ijnurstu.2016.10.004 .
Halcomb E, Davies D, Salamonson Y. Consumer satisfaction with practice nursing: a cross-sectional survey in New Zealand general practice. Aust J Prim Health. 2015;21(3):347–53. https://doi.org/10.1071/PY13176 .
Caldow J, Bond C, Ryan M, Campbell NC, San Miguel F, Kiger A, et al. Treatment of minor illness in primary care: a national survey of patient satisfaction, attitudes and preferences regarding a wider nursing role. Health Expect. 2007;10(1):30–45. https://doi.org/10.1111/j.1369-7625.2006.00422.x .
Gallagher M, Huddart T, Henderson B. Telephone triage of acute illness by a practice nurse in general practice: outcomes of care. Br J Gen Pract. 1998;48(429):1141–5.
CAS PubMed PubMed Central Google Scholar
Nelson E, Wasson J, Kirk J, et al. Assessment of function in routine clinical practice: description of the COOP chart method and preliminary findings. J Chronic Dis. 1987;40:55–63.
Fernandez JM, Ariza-Cardiel G, Rodriguez-Martinez G, Gayo-Milla M, Martinez-Gil M, Alzola-Martin C, et al. Satisfaction with primary care nursing: use of measurement tools and explanatory factors. Rev Calid Asist. 2015;30(2):86–94. https://doi.org/10.1016/j.cali.2015.01.007 .
Randall S, Crawford T, Currie J, River J, Betihavas V. Impact of community-based nurse-led clinics on patient outcomes, patient satisfaction, patient access and cost effectiveness: a systematic review. Int J Nurs Stud. 2017;73:24–33.
Karaca A, Durna Z. Patient satisfaction with the quality of nursing care. Nurs Open. 2019;6(2):535–45. https://doi.org/10.1002/nop2.237 .
Nunu WN, Munyewende PO. Patient satisfaction with nurse-delivered primary health care services in Free State and Guateng provinces South Africa: a comparative study. Afr J Prim Health Care Fam Med. 2017;28(9):e1-8.
Google Scholar
Da Silva, Brault I, Pineault R, Chouinard MC, Prud’homme A, D’Amour D. Nursing practice in primary care and patients’ experience of care. J Prim Care Community Health. 2018;9:1–7. https://doi.org/10.1177/2150131917747186 .
Veroff D, Marr A, Wennberg D. (2013), Enhanced support for shared decision-making reduced costs of care for patients with preference-sensitive conditions. Health Aff. 2013;32(2):285–93. https://doi.org/10.1377/hlthaff.2011.0941 .
Basch E. Patient-reported outcomes – harnessing patients’ voices to improve clinical care. N Engl J Med. 2017;376(2):105–8. https://doi.org/10.1056/NEJMp1611252 .
Basch E, Deal AM, Dueck AC. Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA. 2017;318(2):197–8. https://doi.org/10.1001/jama.2017.7156 .
Greenhalgh J, Dalkin S, Gibbons E. How do aggregated patient-reported outcome measures data stimulate health care improvement? A realist synthesis. J Health Serv Res Policy. 2018;23(1):57–65. https://doi.org/10.1177/1355819617740925 .
Calvert M, O’Connor D, Basch E. Harnessing the patient voice in real-world evidence: the essential role of patient-reported outcomes. Nat Rev Drug Discov. 2019;18(10):731–2. https://doi.org/10.1038/d41573-019-00088-7 .
American Medical Association. AMA successfully fights scope of practice expansions that threaten patient safety. American Medical Association. 2020. https://www.ama-assn.org/practice-management/scope-practice/ama-successfully-fights-scope-practice-expansions-threaten . Accessed 08 Nov 2021.
Robeznieks A. Scope of practice: how the AMA fights for patient safety. American Medical Association. 2020. https://www.ama-assn.org/practice-management/scope-practice/scope-practice-how-ama-fights-patient-safety . Accessed 09 Nov 2021.
Canadian Nurses Association. Framework for the practice of registered nurses in Canada. CNA. 2015. https://www.caccn.ca/files/RN%20Framework%20Revision%20V2%2014_11_13.pdf . Accessed 09 Nov 2021.
International Council of Nurses. Scope of practice and decision-making framework toolkit: ICN regulation series. ICN. 2010. https://www.icn.ch/sites/default/files/inline-files/2010_ICN%20Scope%20of%20Nursing%20and%20Decision%20making%20Toolkit_eng.pdf . Accessed 09 Nov 2021.
Bottorff JL, Kelly M, Young J. Methodological issues in researching palliative care nursing practice. Can J Nurs Res. 2005;37(2):50–68.
PubMed Google Scholar
Lopatina E, Donald F, DiCenso A, Martin-Misener R, Kilpatrick K, Bryant-Lukosius D, et al. Economic evaluation of nurse practitioner and clinical nurse specialist roles: a methodological review. Int J Nurs Stud. 2017;72:71–82. https://doi.org/10.1016/j.ijnurstu.2017.04.012 .
Vincelette C, Thivierge-Southidara M, Rochefort CM. Conceptual and methodological challenges of studies examining the determinants and outcomes of omitted nursing care: a narrative review of the literature. Int J Nurs Stud. 2019;100: 103403. https://doi.org/10.1016/j.ijnurstu.2019.103403 .
Katz DA, Brown RB, Muehlenbruch DR, Fiore MC, Baker TB, AHRQ Smoking Cessation Guideline Study Group. Implementing guidelines for smoking cessation: comparing the efforts of nurses and medical assistants. Am J Prev Med. 2004;27(5):411–6. https://doi.org/10.1016/j.amepre.2004.07.015 .
Low N, McCarthy A, Roberts TE, Huengsberg M, Sanford E, Sterne JAC, et al. Partner notification of chlamydia infection in primary care: randomised controlled trial and analysis of resource use. BMJ. 2006;332(7532):14–9. https://doi.org/10.1136/bmj.38678.405370.7C .
Canadian Institutes for Health Information. Patient-centred measuring and reporting in Canada: launching the discussion toward a future state. CIHI. 2017. https://www.cihi.ca/sites/default/files/document/visioning-day-paper-en-web.pdf . Accessed 09 Nov 2021.
Download references
Acknowledgements
We acknowledge the following research assistants for the contributions to the systematic review screening, appraisal and data extraction process: Richard Buote, Ashley Joyce, Olivia Parsons, and Arifur Rahman.
This research was supported by funding received from Memorial University and the Department of Health & Community Services, Government of Newfoundland & Labrador.
Author information
Authors and affiliations.
Faculty of Nursing, Memorial University, 300 Prince Phillip Drive, St. John’s, NL, A1B 3V, Canada
Julia Lukewich & Dana Ryan
School of Nursing, Dalhousie University, 5869 University Ave. St, Halifax, NS, B3H 4R2, Canada
Ruth Martin-Misener
School of Nursing, Columbia University, 630 West 168th Street, New York, NY, 10032, USA
Allison A. Norful
Département de Médecine de Famille Et Médecine d’urgence, Université de Sherbrooke, 2500 Boulevard de l’Université, Sherbrooke, QC, J1K 2R1, Canada
Marie-Eve Poitras
School of Nursing, McMaster University, 1280 Main St W, Hamilton, ON, L8S 4L8, Canada
Denise Bryant-Lukosius
Department of Family Medicine, Memorial University, 300 Prince Phillip Drive, St. John’s, NL, A1B 3V6, Canada
Shabnam Asghari
Department of Family Medicine Primary Care Research Unit, Dalhousie University, 1465 Brenton Street, Suite 402, Halifax, NS, B3J 3T4, Canada
Emily Gard Marshall
Department of Family Medicine, Schulich School of Medicine & Dentistry, University of Western, 1151 Richmond Street, OntarioLondon, ON, N6A 5C1, Canada
Maria Mathews
Health Sciences Library, Faculty of Medicine, Memorial University, 300 Prince Phillip Drive, St. John’s, NL, A1B 3V6, Canada
Michelle Swab
School of Nursing, Queen’s University, 92 Barrie Street, Kingston, ON, K7L 3N6, Canada
Joan Tranmer
You can also search for this author in PubMed Google Scholar
Contributions
JL conceived of the larger project, obtained grant funding, supervised data collection and screening, interpreted and synthesized results, and drafted and revised the manuscript; DBL, RMM, AN, MEP interpreted results and drafted and revised the manuscript; MS carried out the initial search strategy, assisted with adherence to PRISMA guidelines, interpreted results, and revised the manuscript; SA, EGM, MM, JT interpreted results and revised the manuscript; DR screened, appraised and extracted data, and assisted with interpretation of results and the drafting/revising of the manuscript. All authors approved the final draft.
Corresponding author
Correspondence to Julia Lukewich .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: a typesetting error in the third paragraph of the ‘Patient experience outcomes via PREMS’ subsection under the ‘Results’ was corrected.
Supplementary Information
Additional file 1., additional file 2., additional file 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lukewich, J., Martin-Misener, R., Norful, A.A. et al. Effectiveness of registered nurses on patient outcomes in primary care: a systematic review. BMC Health Serv Res 22 , 740 (2022). https://doi.org/10.1186/s12913-022-07866-x
Download citation
Received : 10 November 2021
Accepted : 03 March 2022
Published : 03 June 2022
DOI : https://doi.org/10.1186/s12913-022-07866-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Effectiveness
- Primary healthcare
- Registered nurse
- Primary care nursing
- Systematic review
- Patient measures
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Clinical Nursing Research (CNR) is a leading international nursing journal, published eight times a year. CNR aims to publish the best available evidence from multidisciplinary teams, with the goal of reporting clinically applicable nursing science and phenomena of interest to nursing.
Exploring all aspects of nursing research, training, education, and practice, BMC Nursing is a well-established open access peer-reviewed journal. Rapid ...
The Journal's mission is to promote excellence in professional nursing, with a global perspective, by providing cutting edge, evidence-based information that embraces a holistic perspective on health and nursing. Clinical articles focus on acute care, health promotion and prevention, rehabilitation, emergencies, critical care, home health care ...
This leading peer-reviewed journal blends quality research with contemporary debates about nursing policy and practice. Each issue contains original research pa...
Online ISSN: 1538-7488. Frequency: 12 issues per year. Ranking: 32/191. Impact Factor: 2.5. eTOC Alert. AJN Featured Articles. Original Research: Exploring Black Nurses' Perceptions of Workplace Safety and Personal Health. Martin, Nia M.; Dehom, Salem O.; Cuccia, Alison F.; More. AJN, American Journal of Nursing. 124 (11):20-28, November 2024.
This mixed methods systematic review aimed to examine how evidence is used to solve leadership problems and to describe the measured and perceived effects of evidence-based leadership on nurse leaders and their performance, organizational, and clinical outcomes. We included articles using any type of research design.
BMC Nursing is an open access, peer-reviewed journal with a primary focus on evidence-based nursing care; nursing research methods; nursing service delivery, utilization, and evaluation; nursing administration and human resources.
Nursing Research is a peer-reviewed journal celebrating over 60 years as the most sought-after nursing resource; it offers more depth, more detail, and more of what today's nurses demand.
Latest published. Articles in press. Top cited. Most downloaded. Most popular. Research articleOpen access. An exploratory study of nursing tasks that induce physical and mental stress among hospital nurses. Younhee Kang, Aekyeong Jin. December 2024 View PDF. Research articleFull text access.
21 Citations. 12 Altmetric. Metrics. A Correction to this article was published on 22 June 2022. This article has been updated. Abstract. Background. Globally, registered nurses (RNs) are increasingly working in primary care interdisciplinary teams.