235 Smoking Essay Topics & Examples
Looking for smoking essay topics? Being one of the most serious psychological and social issues, smoking is definitely worth writing about.

🏆 Best Smoking Essay Examples & Topic Ideas
🥇 good titles for smoking essay, 👍 best titles for research paper about smoking, ⭐ simple & easy health essay titles, 💡 interesting topics to write about health, ❓ essay questions about smoking.
In your essay about smoking, you might want to focus on its causes and effects or discuss why smoking is a dangerous habit. Other options are to talk about smoking prevention or to concentrate on the reasons why it is so difficult to stop smoking. Here we’ve gathered a range of catchy titles for research papers about smoking together with smoking essay examples. Get inspired with us!
Smoking is a well-known source of harm yet popular regardless, and so smoking essays should cover various aspects of the topic to identify the reasons behind the trend.
You will want to discuss the causes and effects of smoking and how they contributed to the persistent refusal of large parts of the population to abandon the habit, even if they are aware of the dangers of cigarettes. You should provide examples of how one may become addicted to tobacco and give the rationales for smokers.
You should also discuss the various consequences of cigarette use, such as lung cancer, and identify their relationship with the habit. By discussing both sides of the issue, you will be able to write an excellent essay.
Reasons why one may begin smoking, are among the most prominent smoking essay topics. It is not easy to begin to enjoy the habit, as the act of smoke inhalation can be difficult to control due to a lack of experience and unfamiliarity with the concept.
As such, people have to be convinced that the habit deserves consideration by various ideas or influences. The notion that “smoking is cool” among teenagers can contribute to the adoption of the trait, as can peer pressure.
If you can find polls and statistics on the primary factors that lead people to tweet, they will be helpful to your point. Factual data will identify the importance of each cause clearly, although you should be careful about bias.
The harmful effects of tobacco have been researched considerably more, with a large body of medical studies investigating the issue available to anyone.
Lung cancer is the foremost issue in the public mind because of the general worry associated with the condition and its often incurable nature, but smoking can lead to other severe illnesses.
Heart conditions remain a prominent consideration due to their lethal effects, and strokes or asthma deserve significant consideration, as well. Overall, smoking has few to no beneficial health effects but puts the user at risk of a variety of concerns.
As such, people should eventually quit once their health declines, but their refusal to do so deserves a separate investigation and can provide many interesting smoking essay titles.
One of the most prominent reasons why a person would continue smoking despite all the evidence of its dangers and the informational campaigns carried out to inform consumers is nicotine addiction.
The substance is capable of causing dependency, a trait that has led to numerous discussions of the lawfulness of the current state of cigarettes.
It is also among the most dangerous aspects of smoking, a fact you should mention.
Lastly, you can discuss the topics of alternatives to smoking in your smoking essay bodies, such as e-cigarettes, hookahs, and vapes, all of which still contain nicotine and can, therefore, lead to considerable harm. You may also want to discuss safe cigarette avoidance options and their issues.
Here are some additional tips for your essay:
- Dependency is not the sole factor in cigarette consumption, and many make the choice that you should respect consciously.
- Cite the latest medical research titles, as some past claims have been debunked and are no longer valid.
- Mortality is not the sole indicator of the issues associated with smoking, and you should take chronic conditions into consideration.
Find smoking essay samples and other useful paper samples on IvyPanda, where we have a collection of professionally written materials!
- How Smoking Is Harmful to Your Health The primary purpose of the present speech is to inform the audience about the detrimental effects of smoking. The first system of the human body that suffers from cigarettes is the cardiovascular system.
- Should Cigarettes Be Banned? Essay Banning cigarette smoking would be of great benefit to the young people. Banning of cigarette smoking would therefore reduce stress levels in people.
- Should Smoking Be Banned in Public Places? Besides, smoking is an environmental hazard as much of the content in the cigarette contains chemicals and hydrocarbons that are considered to be dangerous to both life and environment.
- Conclusion of Smoking Should Be Banned on College Campuses Essay However, it is hard to impose such a ban in some colleges because of the mixed reactions that are held by different stakeholders about the issue of smoking, and the existing campus policies which give […]
- Smoking: Problems and Solutions To solve the problem, I would impose laws that restrict adults from smoking in the presence of children. In recognition of the problems that tobacco causes in the country, The Canadian government has taken steps […]
- Causes and Effects of Smoking Some people continue smoking as a result of the psychological addiction that is associated with nicotine that is present in cigarettes.
- Smoking Cigarette Should Be Banned Ban on tobacco smoking has resulted to a decline in the number of smokers as the world is sensitized on the consequences incurred on 31st May.
- Smoking and Its Effects on Human Body The investigators explain the effects of smoking on the breath as follows: the rapid pulse rate of smokers decreases the stroke volume during rest since the venous return is not affected and the ventricles lose […]
- Social Marketing: The Truth Anti-Smoking Campaign The agreement of November 1998 between 46 states, five territories of the United States, the District of Columbia, and representatives of the tobacco industry gave start to the introduction of the Truth campaign.
- Smoking and Its Negative Effects on Human Beings Therefore, people need to be made aware of dental and other health problems they are likely to experience as a result of smoking.
- Advertisements on the Effect of Smoking Do not Smoke” the campaign was meant to discourage the act of smoking among the youngsters, and to encourage them to think beyond and see the repercussions of smoking.
- Smoking Cessation Programs Through the Wheel of Community Organizing The first step of the wheel is to listen to the community’s members and trying to understand their needs. After the organizer and the person receiving treatment make the connection, they need to understand how […]
- On Why One Should Stop Smoking Thesis and preview: today I am privileged to have your audience and I intend to talk to you about the effects of smoking, and also I propose to give a talk on how to solve […]
- “Thank You For Smoking” by Jason Reitman Film Analysis Despite the fact that by the end of the film the character changes his job, his nature remains the same: he believes himself to be born to talk and convince people.
- Summary of “Smokers Get a Raw Deal” by Stanley Scott Lafayette explains that people who make laws and influence other people to exercise these laws are obviously at the top of the ladder and should be able to understand the difference between the harm sugar […]
- Hookah Smoking and Its Risks The third component of a hookah is the hose. This is located at the bottom of the hookah and acts as a base.
- Teenage Smoking and Solution to This Problem Overall, the attempts made by anti-smoking campaigners hardly yield any results, because they mostly focus on harmfulness of tobacco smoking and the publics’ awareness of the problem, itself, but they do not eradicate the underlying […]
- Health Promotion for Smokers The purpose of this paper is to show the negative health complications that stem from tobacco use, more specifically coronary heart disease, and how the health belief model can help healthcare professionals emphasize the importance […]
- Gender-Based Assessment of Cigarette Smoking Harm Thus, the following hypothesis is tested: Women are more likely than men to believe that smoking is more harmful to health.
- Hazards of Smoking and Benefits of Cessation Prabhat Jha is the author of the article “The Hazards of Smoking and the Benefits of Cessation,” published in a not-for-profit scientific journal, eLife, in 2020.
- The Impact of Warning Labels on Cigarette Smoking The regulations requiring tobacco companies to include warning labels are founded on the need to reduce nicotine intake, limit cigarette dependence, and mitigate the adverse effects associated with addiction to smoking.
- Psilocybin as a Smoking Addiction Remedy Additionally, the biotech company hopes to seek approval from FDA for psilocybin-based therapy treatment as a cigarette smoking addiction long-term remedy.
- Investing Savings from Quitting Smoking: A Financial Analysis The progression of interest is approximately $50 per year, and if we assume n equal to 45 using the formula of the first n-terms of the arithmetic progression, then it comes out to about 105 […]
- Smoking as a Community Issue: The Influence of Smoking A review of the literature shows the use of tobacco declined between 1980 and 2012, but the number of people using tobacco in the world is increasing because of the rise in the global population.
- Smoking Public Education Campaign Assessment The major influence of the real cost campaign was to prevent the initiation of smoking among the youth and prevent the prevalence of lifelong smokers.
- Quitting Smoking and Related Health Benefits The regeneration of the lungs will begin: the process will touch the cells called acini, from which the mucous membrane is built. Therefore, quitting the habit of smoking a person can radically change his life […]
- Smoking and Stress Among Veterans The topic is significant to explore because of the misconception that smoking can alleviate the emotional burden of stress and anxiety when in reality, it has an exacerbating effect on emotional stress.
- Smoking as a Predictor of Underachievement By comparing two groups smoking and non-smoking adolescents through a parametric t-test, it is possible to examine this assumption and draw conclusions based on the resulting p-value.
- Smoking and the Pandemic in West Virginia In this case, the use of the income variable is an additional facet of the hypothesis described, allowing us to evaluate whether there is any divergence in trends between the rich and the poor.
- Anti-Smoking Policy in Australia and the US The anti-smoking policy is to discourage people from smoking through various means and promotion of a healthy lifestyle, as well as to prevent the spread of the desire to smoke.
- Smoking Prevalence in Bankstown, Australia The secondary objective of the project was to gather and analyze a sufficient amount of auxiliary scholarly sources on smoking cessation initiatives and smoking prevalence in Australia.
- Drug Addiction in Teenagers: Smoking and Other Lifestyles In the first part of this assignment, the health problem of drug addiction was considered among teens and the most vulnerable group was established.
- Aspects of Anti-Smoking Advertising Thus, it is safe to say that the authors’ main and intended audience is the creators of anti-smoking public health advertisements.
- Anti-Smoking Communication Campaign’s Analysis Defining the target audience for an anti-smoking campaign is complicated by the different layers of adherence to the issue of the general audience of young adults.
- Smoking Cessation Project Implementation In addition, the review will include the strengths and weaknesses of the evidence presented in the literature while identifying gaps and limitations.
- Smoking Cessation and Health Promotion Plan Patients addicted to tobacco are one of the major concerns of up-to-date medicine as constant nicotine intake leads to various disorders and worsens the health state and life quality of the users.
- Maternal and Infant Health: Smoking Prevention Strategies It is known that many women know the dangers of smoking when pregnant and they always try to quit smoking to protect the lives of themselves and the child.
- A Peer Intervention Program to Reduce Smoking Rates Among LGBTQ Therefore, the presumed results of the project are its introduction into the health care system, which will promote a healthy lifestyle and diminish the level of smoking among LGBTQ people in the SESLHD.
- Peer Pressure and Smoking Influence on Teenagers The study results indicate that teenagers understand the health and social implications of smoking, but peer pressure contributes to the activity’s uptake.
- Smoking: Benefits or Harms? Hundreds of smokers every day are looking for a way to get rid of the noose, which is a yoke around the neck, a cigarette.
- The Culture of Smoking Changed in Poland In the 1980-90s, Poland faced the challenge of being a country with the highest rates of smoking, associated lung cancer, and premature mortality in the world.
- The Stop Smoking Movement Analysis The paper discusses the ideology, objective, characteristics, context, special techniques, organization culture, target audience, media strategies, audience reaction, counter-propaganda and the effectiveness of the “Stop Smoking” Movement.”The Stop Smoking” campaign is a prevalent example of […]
- Health Promotion Plan: Smokers in Mississippi The main strategies of the training session are to reduce the number of smokers in Mississippi, conduct a training program on the dangers of smoking and work with tobacco producers.
- Smoking Health Problem Assessment The effects of smoking correlate starkly with the symptoms and diseases in the nursing practice, working as evidence of the smoking’s impact on human health.
- Integration of Smoking Cessation Into Daily Nursing Practice Generally, smoking cessation refers to a process structured to help a person to discontinue inhaling smoked substances. It can also be referred to as quitting smoking.
- E-Cigarettes and Smoking Cessation Many people argue that e-cigarettes do not produce secondhand smoke. They believe that the e-fluids contained in such cigarettes produce vapor and not smoke.
- Introducing Smoking Cessation Program: 5 A’s Intervention Plan The second problem arises in an attempt to solve the issue of the lack of counseling in the unit by referring patients to the outpatient counseling center post-hospital discharge to continue the cessation program.
- Outdoor Smoking Ban in Public Areas of the Community These statistics have contributed to the widespread efforts to educate the public regarding the need to quit smoking. However, most of the chronic smokers ignore the ramifications of the habit despite the deterioration of their […]
- Nicotine Replacement Therapy for Adult Smokers With a Psychiatric Disorder The qualitative research methodology underlines the issue of the lack of relevant findings in the field of nicotine replacement therapy in people and the necessity of treatment, especially in the early stages of implementation.
- Smoking and Drinking: Age Factor in the US As smoking and drinking behavior were both strongly related to age, it could be the case that the observed relationship is due to the fact that older pupils were more likely to smoke and drink […]
- Smoking Cessation Clinic Analysis The main aim of this project is to establish a smoking cessation clinic that will guide smoker through the process of quitting smoking.
- Cigarette Smoking Among Teenagers in the Baltimore Community, Maryland The paper uses the Baltimore community in Maryland as the area to focus the event of creating awareness of cigarette smoking among the teens of this community.
- Advocating for Smoking Cessation: Health Professional Role Health professionals can contribute significantly to tobacco control in Australia and the health of the community by providing opportunities for smoking patients to quit smoking.
- Lifestyle Management While Quitting Smoking Realistically, not all of the set goals can be achieved; this is due to laxity in implementing them and the associated difficulty in letting go of the past lifestyle.
- Smoking in the Actuality The current use of aggressive marketing and advertising strategies has continued to support the smoking of e-cigarettes. The study has also indicated that “the use of such e-cigarettes may contribute to the normalization of smoking”.
- Analysis of the Family Smoking Prevention and Tobacco Control Act The law ensures that the FDA has the power to tackle issues of interest to the public such as the use of tobacco by minors.
- “50-Year Trends in Smoking-Related Mortality in the United States” by Thun et al. Thun is affiliated with the American Cancer Society, but his research interests cover several areas. Carter is affiliated with the American Cancer Society, Epidemiology Research Program.
- Pulmonology: Emphysema Caused by Smoking The further development of emphysema in CH can lead to such complications caused by described pathological processes as pneumothorax that is associated with the air surrounding the lungs.
- Smoking and Lung Cancer Among African Americans Primarily, the research paper provides insight on the significance of the issue to the African Americans and the community health nurses.
- Health Promotion and Smoking Cessation I will also complete a wide range of activities in an attempt to support the agency’s goals. As well, new studies will be conducted in order to support the proposed programs.
- Maternal Mental Health and Prenatal Smoking It was important to determine the variables that may lead to postpartum relapse or a relapse during the period of pregnancy. It is important to note that the findings are also consistent with the popular […]
- Nursing Interventions for Smoking Cessation For instance, the authors are able to recognize the need to classify the level of intensity in respect to the intervention that is employed by nurses towards smoking cessation.
- Smoking and Cancer in the United States In this research study, data on tobacco smoking and cancer prevalence in the United States was used to determine whether cancer in the United States is related to tobacco smoking tobacco.
- Marketing Plan: Creating a Smoking Cessation Program for Newton Healthcare Center The fourth objective is to integrate a smoking cessation program that covers the diagnosis of smoking, counseling of smokers, and patient care system to help the smokers quit their smoking habits. The comprehensive healthcare needs […]
- Risks of Smoking Cigarettes Among Preteens Despite the good news that the number of preteen smokers has been significantly reducing since the 1990s, there is still much to be done as the effects of smoking are increasingly building an unhealthy population […]
- Public Health Education: Anti-smoking Project The workshop initiative aimed to achieve the following objectives: To assess the issues related to smoking and tobacco use. To enhance the health advantages of clean air spaces.
- Healthy People Program: Smoking Issue in Wisconsin That is why to respond to the program’s effective realization, it is important to discuss the particular features of the target population in the definite community of Wisconsin; to focus on the community-based response to […]
- Health Campaign: Smoking in the USA and How to Reduce It That is why, the government is oriented to complete such objectives associated with the tobacco use within the nation as the reduction of tobacco use by adults and adolescents, reduction of initiation of tobacco use […]
- Smoking Differentials Across Social Classes The author inferred her affirmations from the participant’s words and therefore came to the right conclusion; that low income workers had the least justification for smoking and therefore took on a passive approach to their […]
- Cigarette Smoking Side Effects Nicotine is a highly venomous and addictive substance absorbed through the mucous membrane in the mouth as well as alveoli in the lungs.
- Long-Term Effects of Smoking The difference between passive smoking and active smoking lies in the fact that, the former involves the exposure of people to environmental tobacco smoke while the latter involves people who smoke directly.
- Smoking Cessation Program Evaluation in Dubai The most important program of this campaign is the Quit and Win campaign, which is a unique idea, launched by the DHCC and is in the form of an open contest.
- Preterm Birth and Maternal Smoking in Pregnancy The major finding of the discussed research is that both preterm birth and maternal smoking during pregnancy contribute, although independently, to the aortic narrowing of adolescents.
- Enforcement of Michigan’s Non-Smoking Law This paper is aimed at identifying a plan and strategy for the enforcement of the Michigan non-smoking law that has recently been signed by the governor of this state.
- Smoking Cessation for Patients With Cardio Disorders It highlights the key role of nurses in the success of such programs and the importance of their awareness and initiative in determining prognosis.
- Legalizing Electronic Vaping as the Means of Curbing the Rates of Smoking However, due to significantly less harmful effects that vaping produces on health and physical development, I can be considered a legitimate solution to reducing the levels of smoking, which is why it needs to be […]
- Inequality and Discrimination: Impact on LGBTQ+ High School Students Consequently, the inequality and discrimination against LGBTQ + students in high school harm their mental, emotional, and physical health due to the high level of stress and abuse of various substances that it causes.
- Self-Efficacy and Smoking Urges in Homeless Individuals Pinsker et al.point out that the levels of self-efficacy and the severity of smoking urges change significantly during the smoking cessation treatment.
- “Cigarette Smoking: An Overview” by Ellen Bailey and Nancy Sprague The authors of the article mentioned above have presented a fair argument about the effects of cigarette smoking and debate on banning the production and use of tobacco in America.
- “The Smoking Plant” Project: Artist Statement It is the case when the art is used to pass the important message to the observer. The live cigarette may symbolize the smokers while the plant is used to denote those who do not […]
- Dangers of Smoking While Pregnant In this respect, T-test results show that mean birthweight of baby of the non-smoking mother is 3647 grams, while the birthweight of smoking mother is 3373 grams. Results show that gestation value and smoking habit […]
- The Cultural Differences of the Tobacco Smoking The Middle East culture is connected to the hookah, the Native American cultures use pipes, and the Canadian culture is linked to cigarettes.
- Ban on Smoking in Enclosed Public Places in Scotland The theory of externality explains the benefit or cost incurred by a third party who was not a party to the reasoning behind the benefit or cost. This will also lead to offer of a […]
- How Smoking Cigarettes Effects Your Health Cigarette smoking largely aggravates the condition of the heart and the lung. In addition, the presence of nicotine makes the blood to be sticky and thick leading to damage to the lining of the blood […]
- Alcohol and Smoking Abuse: Negative Physical and Mental Effects The following is a range of effects of heavy alcohol intake as shown by Lacoste, they include: Neuropsychiatric or neurological impairment, cardiovascular, disease, liver disease, and neoplasm that is malevolent.
- Smoking Prohibition: Local Issues, Personal Views This is due to the weakening of blood vessels in the penis. For example, death rate due to smoking is higher in Kentucky than in other parts of the country.
- Ban Smoking in Cars Out of this need, several regulations have been put in place to ensure children’s safety in vehicles is guaranteed; thus, protection from second-hand smoke is an obvious measure that is directed towards the overall safety […]
- Smoking: Causes and Effects Considering the peculiarities of a habit and of a disease, smoking can be considered as a habit rather than a disease.
- Smoking and Its Effect on the Brain Since the output of the brain is behavior and thoughts, dysfunction of the brain may result in highly complex behavioral symptoms. The work of neurons is to transmit information and coordinate messengers in the brain […]
- Smoking Causes and Plausible Arguments In writing on the cause and effect of smoking we will examine the issue from the point of view of temporal precedence, covariation of the cause and effect and the explanations in regard to no […]
- Smoking Qualitative Research: Critical Analysis Qualitative research allows researchers to explore a wide array of dimensions of the social world, including the texture and weave of everyday life, the understandings, experiences and imaginings of our research participants, the way that […]
- Motivational Interviewing as a Smoking Cessation Intervention for Patients With Cancer The dependent variable is the cessation of smoking in 3 months of the interventions. The study is based on the author’s belief that cessation of smoking influences cancer-treated patients by improving the efficacy of treatment.
- Factors Affecting the Success in Quitting Smoking of Smokers in West Perth, WA Australia Causing a wide array of diseases, health smoking is the second cause of death in the world. In Australia, the problem of smoking is extremely burning due to the high rates of diseases and deaths […]
- Media Effects on Teen Smoking But that is not how an adult human brain works, let alone the young and impressionable minds of teenagers, usually the ads targeted at the youth always play upon elements that are familiar and appealing […]
- Partnership in Working About Smoking and Tobacco Use The study related to smoking and tobacco use, which is one of the problematic areas in terms of the health of the population.
- Causes and Effects of Smoking in Public The research has further indicated that the carcinogens are in higher concentrations in the second hand smoke rather than in the mainstream smoke which makes it more harmful for people to smoke publicly.
- Quitting Smoking: Motivation and Brain As these are some of the observed motivations for smoking, quitting smoking is actually very easy in the sense that you just have to set your mind on quitting smoking.
- Health Effects of Tobacco Smoking in Hispanic Men The Health Effects of Tobacco Smoking can be attributed to active tobacco smoking rather than inhalation of tobacco smoke from environment and passive smoking.
- Smoking in Adolescents: A New Threat to the Society Of the newer concerns about the risks of smoking and the increase in its prevalence, the most disturbing is the increase in the incidences of smoking among the adolescents around the world.
- Smoking and Youth Culture in Germany The report also assailed the Federal Government for siding the interest of the cigarette industry instead of the health of the citizens.
- New Jersey Legislation on Smoking The advantages and disadvantages of the legislation were discussed in this case because of the complexity of the topic at hand as well as the potential effects of the solution on the sphere of public […]
- Environmental Health: Tabaco Smoking and an Increased Concentration of Carbon Monoxide The small size of the town, which is around 225000 people, is one of the reasons for high statistics in diseases of heart rate.
- Advanced Pharmacology: Birth Control for Smokers The rationale for IUD is the possibility to control birth without the partner’s participation and the necessity to visit a doctor just once for the device to be implanted.
- Legislation Reform of Public Smoking Therefore, the benefit of the bill is that the health hazard will be decreased using banning smoking in public parks and beaches.
- Smoking Bans: Protecting the Public and the Children of Smokers The purpose of the article is to show why smoking bans aim at protecting the public and the children of smokers.
- Clinical Effects of Cigarette Smoking Smoking is a practice that should be avoided or controlled rigorously since it is a risk factor for diseases such as cancer, affects the health outcomes of direct and passive cigarette users, children, and pregnant […]
- Public Health and Smoking Prevention Smoking among adults over 18 years old is a public health issue that requires intervention due to statistical evidence of its effects over the past decades.
- Smoking Should Be Banned Internationally The questions refer to the knowledge concerning the consequences of smoking and the opinions on smoking bans. 80 % of respondents agree that smoking is among the leading causes of death and 63, 3 % […]
- Microeconomics: Cigarette Taxes and Public Smoking Ban The problem of passive smoking will be minimized when the number of smokers decreases. It is agreeable that the meager incomes of such families will be used to purchase cigarettes.
- Tobacco Debates in “Thank You for Smoking” The advantage of Nick’s strategy is that it offers the consumer a role model to follow: if smoking is considered to be ‘cool’, more people, especially young ones, will try to become ‘cool’ using cigarettes.
- Alcohol and Smoking Impact on Cancer Risk The research question is to determine the quantity of the impact that different levels of alcohol ingestion combined with smoking behavioral patterns make on men and women in terms of the risks of cancer.
- Indoor Smoking Restriction Effects at the Workplace Regrettably, they have neglected research on the effect of the legislation on the employees and employers. In this research, the target population will be the employees and employers of various companies.
- Hypnotherapy Session for Smoking Cessation When I reached the age of sixty, I realized that I no longer wanted to be a smoker who was unable to take control of one’s lifestyle.
- Smoking Among Teenagers as Highlighted in Articles The use of tobacco through smoking is a trend among adolescents and teenagers with the number of young people who involve themselves in smoking is growing each day.
- Smoking Experience and Hidden Dangers When my best college friend Jane started smoking, my eyes opened on the complex nature of the problem and on the multiple negative effects of smoking both on the smoker and on the surrounding society.
- South Illinois University’s Smoking Ban Benefits The purpose of this letter is to assess the possible benefits of the plan and provide an analysis of the costs and consequences of the smoking ban introduction.
- Smoking Cessation in Patients With COPD The strategy of assessing these papers to determine their usefulness in EBP should include these characteristics, the overall quality of the findings, and their applicability in a particular situation. The following article is a study […]
- Smoking Bans: Preventive Measures There have been several public smoking bans that have proved to be promising since the issue of smoking prohibits smoking in all public places. This means it is a way of reducing the exposure to […]
- Ban Smoking Near the Child: Issues of Morality The decision to ban smoking near the child on father’s request is one of the demonstrative examples. The father’s appeal to the Supreme Court of California with the requirement to prohibit his ex-wife from smoking […]
- The Smoking Ban: Arguments Comparison The first argument against banning smoking employs the idea that smoking in specially designated areas cannot do harm to the health of non-smokers as the latter are supposed to avoid these areas.
- Smoking Cessation and Patient Education in Nursing Pack-years are the concept that is used to determine the health risks of a smoking patient. The most important step in the management plan is to determine a date when the man should quit smoking.
- Philip Morris Company’s Smoking Prevention Activity Philip Morris admits the existence of scientific proof that smoking leads to lung cancer in addition to other severe illnesses even after years of disputing such findings from health professionals.
- Tobacco Smoking and Its Dangers Sufficient evidence also indicates that smoking is correlated with alcohol use and that it is capable of affecting one’s mental state to the point of heightening the risks of development of disorders.
- Virginia Slims’ Impact on Female Smokers’ Number Considering this, through the investigation of Philip Morris’ mission which it pursued during the launch of the Virginia Slims campaign in 1968-1970 and the main regulatory actions undertaken by the Congress during this period, the […]
- Tuberculosis Statistics Among Cigarette Smokers The proposal outlines the statistical applications of one-way ANOVA, the study participants, the variables, study methods, expected results and biases, and the practical significance of the expected results.
- Smoking Habit, Its Causes and Effects Smoking is one of the factors that are considered the leading causes of several health problems in the current society. Smoking is a habit that may be easy to start, but getting out of this […]
- Smoking Ban and UK’s Beer Industry However, there is an intricate type of relationship between the UK beer sector, the smoking ban, and the authorities that one can only understand by going through the study in detail The history of smoking […]
- Smokers’ Campaign: Finding a Home for Ciggy Butts When carrying out the campaign, it is important to know what the situation on the ground is to be able to address the root cause of the problem facing the population.
- Behavior Modification Technique: Smoking Cessation Some of its advantages include: its mode of application is in a way similar to the act of smoking and it has very few side effects.
- Quitting Smoking: Strategies and Consequences Thus, for the world to realize a common positive improvement in population health, people must know the consequences of smoking not only for the smoker but also the society. The first step towards quitting smoking […]
- Effects of Thought Suppression on Smoking Behavior In the article under analysis called I suppress, Therefore I smoke: Effects of Thought Suppression on Smoking Behavior, the authors dedicate their study to the evaluation of human behavior as well as the influence of […]
- Smoking Cessation Methods These methods are a part of NRT or nicotine replacement therapy, they work according to the principle of providing the smoker with small portions of nicotine to minimize the addiction gradually and at the same […]
- Understanding Advertising: Second-Hand Smoking The image of the boy caught by the smoke is in the center of the picture, and it is in contrast with the deep black background.
- People Should Quit Smoking Other counseling strategies such as telephone calls and social support also serves the ultimate goal of providing a modern approach in which counseling can be tailored to suit the counseling needs of an individual smoker. […]
- Importance of Quitting Smoking As such, quitting smoking is important since it helps relief the worry and the fear associated with possibility of developing cancer among other smoking-related illnesses. It is therefore important to quit smoking if the problems […]
- Cigarette Smoking in Public Places Those who argue against the idea of banning the smoking are of the opinion that some of them opt to smoke due to the stress that they acquire at their work places.
- Ban of Tobacco Smoking in Jamaica The first part of the paper will address effects of tobacco smoking on personal health and the economy. Cognizant of its international obligation and the aforementioned health effects of tobacco smoke, Jamaica enacted a law […]
- Anti-Smoking Campaign in Canada This is not the first attempt that the federal government of Canada intends to make in reducing the prevalence of smoking in the country.
- Electronic Cigarettes: Could They Help University Students Give Smoking Up? Electronic Cigarettes An electronic cigarette is an electronic device that simulates the act of smoking by producing a mist which gives the physical sensation and often the flavor and the nicotine just as the analog […]
- The Change of my Smoking Behavior With the above understanding of my social class and peer friends, I was able to create a plan to avoid them in the instances that they were smoking.
- Psychosocial Smoking Rehabilitation According to Getsios and Marton most of the economic models that evaluate the effects of smoke quitting rehabilitation consider the influence of a single quit attempt.
- Combating Smoking: Taxation Policies vs. Education Policies This is a considerable provision in the realms of health; hence, the efforts created by the government to curb this trend should be supported fully. In this regard, there is need to reduce the mentioned […]
- The Program to Quit Smoking The second stage of the evaluation proves revealed the benefits of the program for the hospital in terms of discount rates for employees, age categories involved in the program. This process consists in selection of […]
- Smoking Culture in Society Smoking culture refers to the practice of smoking tobacco by people in the society for the sheer satisfaction and delight it offers.
- Possible Smoking Policies in Florida Majority also think that went it comes to workplaces hotels and bars it would be more appropriate to provide specific smoking zones as opposed to total bans The implications of the policy adopted therefore affect […]
- Smoking Ban in the State of Florida These are the Total Ban Policy, the Partial Ban policy and the Liberated Smoking policy. The policy is authoritarian and ignores the interests of the smokers.
- Core Functions of Public Health in the Context of Smoking and Heart Disease In the relation to our problem, heart attacks and smoking, it is important to gather the information devoted to the number of people who suffered from heart attacks and indicate the percentage rate of those […]
- Putting Out the Fires: Will Higher Taxes Reduce the Onset of Youth Smoking? According to the article under consideration, increase in price of cigarettes can positively or negatively affect the rate of smoking among the youth.
- Smoking Bans in US The issue of whether to ban smoking indoors by the governments of various countries is popular as they try to take a step towards curbing the harmful effects of smoking.
- Smoking as Activity Enhancer: Schizophrenia and Gender Once learning the effects which nicotine has on people’s health and the relation between gender and schizophrenia, one can possibly find the ways to prevent the latter and to protect the people in the high-risk […]
- Health Care Costs for Smokers Higher Tobacco taxes Some of the smokers have the same viewpoint that the current level of taxes imposed on the tobacco is high, 68%, and most of them, 59%, are in agreement for the increase […]
- Medical Coverage for Smoking Related Diseases However, one of the most oblivious reasons is that it is a deterrent to this behavior, which is harmful to the life of the smoker.
- The Realm of reality: Smoking In a nutshell, it can be argued that the definition of a man or a woman is different and not the same as in earlier days.
- Ethical Problem of Smoking Since the job is urgent and therefore needed in a few days time, I would request her to work on the job with the promise that I will communicate her complaints to Frank and Alice […]
- The Rate of Smoking Among HIV Positive Cases. To determine if use of group work among HIV positive smokers will be an effective strategy in reducing smoking habit among the target cases, then it is essential that this study establish if use of […]
- Studying the Government’s Anti-Smoking Measures The methodology of study includes the review of the articles devoted to the anti-smoking measures of the Federal Government and application of economic theories to them.
- Smoking Should Be Banned In the United States For numerous decades, smoking has remained the most disastrous problem in the universe in spite of the full awareness of the risk accompanied with its use.
- Effectiveness of Cognitive Behavioral Theory on Smoking Cessation The study concluded that CBT intervention was effective for African American smoking cessation. As a result, the study concluded that CBT intervention was effectual for smoking cessation among African Americans.
- Effectiveness of the Cognitive Behavioral Therapy for Smoking Cessation It is important to answer the question about the effectiveness of the CBT for smoking cessation with references to the racial and ethnic differences influencing the effectiveness of the CBT and to the comparison of […]
- Wayco Company’s Non-smoking Policy The policy should not go beyond the work place because this would be tantamount to infringing on the privacy of the employees when this does not in any way affect their work performance.
- Adverse Aspects of Smoking
- Negative Impacts of Smoking on Individuals and Society
- Smoking: Effects, Reasons and Solutions
- Smoking Ban in the United States of America
- Dangers of Smoking Campaign
- Smoking Ban in New York
- Trends in Smoking Prevalence by Race/Ethnicity
- Business Ethics: Smoking Issue
- Should Smoking Tobacco Be Classified As an Illegal Drug?
- Where Does the Path to Smoking Addiction Start?
- Public Health Communication: Quit Smoking
- Are Estimated Peer Effects on Smoking Robust?
- Are There Safe Smoking and Tobacco Options?
- What Are the Health Risks of Smoking?
- Does Cigarette Smoking Affect Body Weight?
- Does Cigarette Smuggling Prop Up Smoking Rates?
- What Foods Help You Quit Smoking?
- How Can People Relax Without Smoking?
- Does Education Affect Smoking Behaviors?
- Is Vaping Worse Than Smoking?
- Do Movies Affect Teen Smoking?
- What Is Worse: Drinking or Smoking?
- Does Smoking Affect Breathing Capacity?
- Does Smoking Cause Lung Cancer?
- Does Having More Children Increase the Likelihood of Parental Smoking?
- Does Smoking Cigarettes Relieve Stress?
- Does Time Preference Affect Smoking Behavior?
- How Does Smoking Affect Cardiovascular Endurance?
- How Hypnosis Can Help You Quit Smoking?
- How Does Smoking Affect Brain?
- How Nicotine Affects Your Quit Smoking Victory?
- How Does Secondhand Smoking Affect Us?
- Why Is Smoking Addictive?
- How Smoking Bans Are Bad for Business?
- Why Smoking Should Not Be Permitted in Restaurants?
- Why Public Smoking Should Be Banned?
- Why Has Cigarette Smoking Become So Prominent Within the American Culture?
- What Makes Smoking and Computers Similar?
- Does Smoking Affect Schooling?
- What Effects Can Cigarette Smoking Have on the Respiratory System?
- What Are the Most Prevalent Dangers of Smoking and Drinking?
- Social Security Paper Topics
- Drug Titles
- Cannabis Essay Titles
- Global Issues Essay Topics
- Cardiovascular Diseases Titles
- Marijuana Ideas
- NHS Research Ideas
- Hypertension Topics
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 29). 235 Smoking Essay Topics & Examples. https://ivypanda.com/essays/topic/smoking-essay-examples/
"235 Smoking Essay Topics & Examples." IvyPanda , 29 Feb. 2024, ivypanda.com/essays/topic/smoking-essay-examples/.
IvyPanda . (2024) '235 Smoking Essay Topics & Examples'. 29 February.
IvyPanda . 2024. "235 Smoking Essay Topics & Examples." February 29, 2024. https://ivypanda.com/essays/topic/smoking-essay-examples/.
1. IvyPanda . "235 Smoking Essay Topics & Examples." February 29, 2024. https://ivypanda.com/essays/topic/smoking-essay-examples/.
Bibliography
IvyPanda . "235 Smoking Essay Topics & Examples." February 29, 2024. https://ivypanda.com/essays/topic/smoking-essay-examples/.
IvyPanda uses cookies and similar technologies to enhance your experience, enabling functionalities such as:
- Basic site functions
- Ensuring secure, safe transactions
- Secure account login
- Remembering account, browser, and regional preferences
- Remembering privacy and security settings
- Analyzing site traffic and usage
- Personalized search, content, and recommendations
- Displaying relevant, targeted ads on and off IvyPanda
Please refer to IvyPanda's Cookies Policy and Privacy Policy for detailed information.
Certain technologies we use are essential for critical functions such as security and site integrity, account authentication, security and privacy preferences, internal site usage and maintenance data, and ensuring the site operates correctly for browsing and transactions.
Cookies and similar technologies are used to enhance your experience by:
- Remembering general and regional preferences
- Personalizing content, search, recommendations, and offers
Some functions, such as personalized recommendations, account preferences, or localization, may not work correctly without these technologies. For more details, please refer to IvyPanda's Cookies Policy .
To enable personalized advertising (such as interest-based ads), we may share your data with our marketing and advertising partners using cookies and other technologies. These partners may have their own information collected about you. Turning off the personalized advertising setting won't stop you from seeing IvyPanda ads, but it may make the ads you see less relevant or more repetitive.
Personalized advertising may be considered a "sale" or "sharing" of the information under California and other state privacy laws, and you may have the right to opt out. Turning off personalized advertising allows you to exercise your right to opt out. Learn more in IvyPanda's Cookies Policy and Privacy Policy .
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Nicotine addiction and smoking: health effects and interventions.
Sunny P. Aslam ; Stephen W. Leslie ; Jason Morris .
Affiliations
Last Update: August 8, 2024 .
- Continuing Education Activity
The Surgeon General reports that nicotine addiction produces 480,000 fatalities each year in the United States, with more casualties than all other addictions combined. Around 23% of the world's population inhales cigarettes, and the prevalence of electronic inhalation or "vaping" of nicotine has skyrocketed in recent years, particularly in young people. Studies have linked tobacco smoking to a range of devastating illnesses, including coronary artery disease, chronic obstructive pulmonary disease, cancers in every human organ system, and decreased reproductive health.
Diagnosing nicotine addiction involves assessing patient history and behaviors and using screening tools. Treatment plans are personalized, combining behavioral counseling with pharmacotherapy options like nicotine replacement therapies, bupropion, or varenicline. Support systems such as support groups and quitlines offer ongoing encouragement. Relapse prevention strategies and continued follow-up are essential for maintaining cessation efforts and achieving long-term success in abstaining from tobacco use.
This activity for healthcare professionals is designed to enhance learners' proficiency in evaluating and managing nicotine addiction. Participants gain a deeper insight into the condition's risk factors, complications, and evidence-based diagnostic and management strategies. Greater competence enables learners to work effectively within an interprofessional team caring for patients with nicotine addiction.
- Identify the primary risk factors and signs of nicotine addiction in patients through comprehensive history taking and clinical evaluation.
- Differentiate between nicotine addiction and other substance use disorders using established diagnostic criteria and screening tools.
- Implement individualized treatment plans combining behavioral counseling and pharmacotherapy to support patients in quitting nicotine use.
- Collaborate with the interprofessional team to educate, treat, and monitor patients with nicotine addiction to improve patient outcomes.
- Introduction
Tobacco leaves were originally harvested and smoked by Native Americans and introduced in Europe by Christopher Columbus in the 15th century. The botanical name for tobacco, Nicotiana tabacum , is derived from Jean Nicot, who sent the tobacco leaf to the Queen of France in the 16th century. Packaged cigarettes and cigars rapidly gained popularity during the late 18th century. Tobacco was suspected of being linked to throat and mouth cancers in the early 20th century, but the 1964 "Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service" significantly changed public opinion against nicotine. Since then, tobacco has been a prominent topic in most annual Surgeon General reports.
The original report was an objective review of literature that pointed to tobacco use as being causal to several deadly health conditions. Much research has been conducted since, and many new findings regarding the disease-causing aspects of tobacco smoking have been elucidated. Despite the widely published results of this research, tobacco-related illnesses remain the leading cause of preventable death in the United States. [1] [2] [3] While cigarette use rates have decreased, electronic cigarette use has increased, particularly among the youth. [4]
Most people who smoke start in their teenage years. These individuals often have family or friends who also smoke. The tobacco industry advertises heavily and markets directly to teenagers. Television commercials and social media portray tobacco use as acceptable, even glamorous. Vaping and e-cigarettes provide attractive alternatives, especially for younger individuals. [5] Strong associations have been found between adverse childhood events, nicotine, and cannabis use. [6]
- Epidemiology
About 23% of the global population is addicted to cigarettes, including 32% of men and 7% of women. Eastern and Southeast Asia have the highest smoking prevalence in the world at 45%, while the Caribbean and North America have the lowest prevalence at 20%. [7] In 2021, 18.7% of adults in the United States reported using tobacco products. [8] Cigarettes (11.5%) and e-cigarettes (4.5%) were most often used. Furthermore, 24.1% of men and 13.6% of women use a tobacco product. By age group, tobacco users represent 17% of adults aged 18 to 24, 22.1% of adults aged 25 to 44, 21.1% of adults aged 45 to 64, and 11% of adults 65% and older.
- Pathophysiology
Nicotine addiction works by activating the brain's reward system, particularly the ventral tegmental area in the midbrain, similar to other addictive drugs and alcohol. This activation stimulates the release of dopamine in the brain's reward pathways, creating pleasurable sensations that reinforce the desire to use nicotine repeatedly. Over time, the brain adapts to these increased dopamine levels, leading to tolerance, where more nicotine is needed to achieve the same effects. Additionally, withdrawal symptoms such as irritability, anxiety, and strong cravings occur when nicotine levels drop, making it challenging for individuals to quit. These neurobiological mechanisms contribute to the powerful and persistent nature of nicotine addiction. [9]
Meanwhile, some of the exact mechanisms for tobacco smoking-related illnesses have yet to be elucidated. However, several studies have linked tobacco smoking to a plethora of devastating illnesses, including coronary artery disease (CAD), cancers in every human organ system, chronic obstructive pulmonary disease (COPD), and decreased reproductive health. [10] [11] [12] Several potential mechanisms have been described linking tobacco smoking with CAD. Inhaled tobacco smoke increases the amount of exogenous and endogenous free radicals in the body, increasing oxidative stress. Greater oxidative stress leads to vasomotor dysfunction, increased prothrombotic and decreased fibrinolytic factors, leukocyte and platelet activation, greater lipid peroxidation, increased adhesion and inflammatory molecules, and smooth muscle proliferation. Researchers postulate that a combination of these factors leads to the development of CAD in tobacco smokers. [13]
Tobacco smoking correlates with an increased risk of developing at least 17 classes of human cancers. Tobacco smoke contains about 60 known carcinogens that can damage deoxyribonucleic acid (DNA) by forming DNA adducts. If not properly repaired, these adducts cause mutations that are passed on to daughter cells during cell division. These mutations accumulate over time, disrupting normal cell reproduction and leading to tumor formation. [14] [15] COPD has also been shown to correlate heavily with tobacco smoking. Reactive oxidants in cigarette smoke create a chronic inflammatory state in the lungs, which can persist even after smoking cessation. This inflammation leads to lung remodeling and can eventually cause significant structural changes. An autoimmune component in lung disease has also been proposed, where autoantibodies react to antigens formed directly or indirectly from tobacco smoking. [16]
Tobacco smoking has several deleterious effects on human reproductive health. In men, smoking has been linked to decreased semen volume, sperm density, and total sperm count. [17] In women, tobacco smoking has been shown to disrupt the normal menstruation cycle and decrease ovarian reserve. [18] Smoking tobacco while pregnant is also associated with low birth weight and cryptorchidism. [19] [20]
- Toxicokinetics
Tobacco smoke is comprised of a mixture of more than 4000 different compounds. Mainstream smoke, the smoke directly inhaled from the end of the cigarette into the smoker’s lungs, is hotter, denser, and contains more compounds than the sidestream smoke emanating from the cigarette's lit end. Mainstream smoke is the most dangerous type of cigarette smoke, although sidestream smoke has also been linked to significant illnesses.
Many compounds found in tobacco smoke form via the process of combustion as the cigarette burns between 600 °F and 900 °F. The particles rapidly increase in size after the smoke is drawn from the cigarette due to humidification from the moist air in the upper respiratory tract. Mainstream smoke subsequently condenses as it transits into the lungs, leaving an estimated 50% to 95% of these molecules deposited in the bronchi, bronchioles, and alveoli. [21]
- History and Physical
Tobacco smoking history should be routinely obtained from patients. The scent of tobacco smoke is a great cue to ask patients about nicotine use and any wishes to quit. Pack-year history provides an estimated number of cigarettes a patient has consumed over a lifetime and is calculated as packs smoked per day multiplied by the total number of years smoked. Obtaining a pack-year history has shown to be of some value when determining the presence and severity of smoking-related illnesses such as CAD and COPD, as smoking-related cancers have all been linked to increased pack-year history. [22] [23] [24]
Many physical exam findings can be directly or indirectly related to tobacco smoking. The oropharyngeal examination often reveals periodontal disease and tooth loss. Tongue and oropharyngeal cancers may even be visualized. Lung auscultation may reveal decreased or asynchronous breath sounds. The cardiac examination often demonstrates an increased resting heart rate compared to nonsmokers. Tobacco stains may be present on the skin of the face and fingers. Decreased peripheral pulses may be appreciated due to smoking-related peripheral vascular disease. [25] [26] [27]
Assisting patients with smoking cessation is one of the most important primary care tasks, and the benefits of assessing patients’ smoking behavior are well established. The US Preventive Services Task Force (USPSTF) recommends using the 5 As:
- Ask about smoking. Office systems should ensure that smoking status is documented at every visit.
- Advise to quit. Use clear, personalized messages. Even brief advice from a physician can improve quit rates compared with patients who receive no advice.
- Assess willingness to quit. Patients assessed as not yet willing to quit may be asked why or what barriers are in their way.
- Assist in quitting. Ask willing patients to set a quit date.
- Arrange follow-up and support.
Behavioral interventions, either alone or combined with pharmacotherapy, substantially improve smoking cessation rates, supported by substantial evidence. Both behavioral interventions and pharmacotherapy are effective and recommended, and combinations of interventions are most effective. The best and most effective interventions are those that are feasible for the individual. [28] [29]
Asking about nicotine use and focusing on efforts to help a patient quit or cut down is the focus of the evaluation. Referral from a clinician may be needed to treat comorbid pulmonary, cardiac, psychiatric, or other complications. Blood work and radiology, in particular, may be utilized. Addressing comorbid addictions or psychiatric disorders is also vital.
- Treatment / Management
Nicotine is one of the most addictive substances known, making it extremely difficult to give up. Repeated attempts at quitting nicotine, often involving both behavioral interventions and medications, are needed.
Behavioral Interventions
Behavioral interventions found to be effective in aiding adults in smoking cessation include psychotherapy, in-person counseling, telephone counseling, and self-help materials. These interventions may increase smoking cessation rates from a baseline of 5% to 11% in control groups to 7% to 13% in intervention groups. Both minor and intensive in-person interventions increase the proportion of persons who successfully quit smoking and remain abstinent.
However, more or longer sessions improve cessation rates. According to Public Health Service guidelines, individuals should undergo at least 4 in-person counseling sessions. Interventions delivered by various types of providers, including physicians, nurses, psychologists, social workers, and cessation counselors, can be effective. Telephone counseling interventions should provide at least 3 telephone calls conducted by trained professional counselors or healthcare providers. Effective self-help materials are tailored to the individual and are primarily print-based. [29]
Pharmacotherapy
Pharmacotherapy interventions approved by the Food and Drug Administration (FDA) for treating tobacco dependence in adults include sustained-release bupropion, varenicline, and nicotine replacement therapy (NRT). [30] [31] The effects of these modalities and the studies supporting their benefits are explained below.
Varenicline
The EAGLES trial established varenicline as the most effective and safest treatment for nicotine addiction when combined with counseling in the general population and those with psychiatric comorbidities. [32] Bupropion and nicotine-based medications (ie, gum, lozenges, inhaler, nasal spray, and patch) showed equal efficacy. Recent evidence includes a potential role for cytisine. [33] In patients willing to quit, a combination of counseling and one or more medications has proven more effective than just counseling or medication alone. [34] [35] [36]
Varenicline is a selective α4-β2 nicotinic receptor partial agonist that reduces cravings and withdrawal symptoms while blocking the binding of inhaled nicotine. Smoking cessation rates have been shown to increase from 12% in control groups to 28% in those using varenicline. The FDA removed a black box warning for mental health side effects from varenicline in December 2016. A Cochrane review found some increase in significant adverse events compatible with both benefit and harm. [37] Multiple other studies showed varenicline, bupropion, and nicotine replacement do not increase the risk of major cardiovascular events. [38] [39]
Sustained-Release Buproprion
Smoking cessation may increase from 11% in control groups to 19% in those using sustained-release bupropion. Bupropion was first developed as an antidepressant. However, The drug is also effective as a smoking cessation aid. Some studies show that NRT combined with sustained-release bupropion may be more effective than sustained-release bupropion alone, but not necessarily NRT alone.
Nicotine Replacement Therapy
Nicotine in itself is not carcinogenic. This compound acts on the craving-and-seeking pathway, as in all other addicting substances. The goal of nicotine replacement is to relieve cravings and reduce nicotine withdrawal symptoms. Rates of smoking cessation may increase from 10% in control groups to 17% in persons using any form of NRT, and using 2 types of NRT is more effective than using a single type. Evidence proves that combining a nicotine patch, which slowly releases the substance, with a rapid-delivery form of NRT (eg, gums, lozenges, nasal spray, and inhalers) is more effective than using a single type.
Combined Behavioral and Medication Therapy
Combining behavioral and medication therapy may increase smoking cessation rates from 8% to 14% compared to minimal behavioral interventions such as brief advice on quitting. Combination interventions usually include behavioral components delivered by specialized smoking cessation counselors combined with NRT. Combination interventions comprise several sessions (more than 4) and are more successful with more sessions. Adding behavioral interventions to pharmacotherapy also increases cessation rates from 18% in persons receiving pharmacotherapy alone to 21% in patients using a mix of pharmacotherapy and behavioral support.
Electronic Cigarettes for Smoking Cessation
In a Cochrane review, electronic cigarettes with nicotine increased smoking cessation rates compared with placebo, with cessation rates similar to that of nicotine patches. The most common reason for using electronic cigarettes has been to quit or reduce cigarette smoking. However, little is known about electronic cigarettes' ingredients or long-term effects. Initial studies show that electronic cigarettes contain other harmful chemicals besides nicotine, including carcinogens and lung irritants. The USPSTF found insufficient evidence for the use of electronic cigarettes as a smoking cessation tool in adults. One randomized trial of 1,246 smokers found electronic cigarettes led to less use of tobacco than counseling alone. [40]
Pregnant Women
Smoking during pregnancy contributes to preterm deliveries, low-birthweight term deliveries, sudden infant death syndrome, and preterm birth-related deaths. Approximately 23% of women smoke during the last 3 months before conception. Data from 2011 showed that 10% of women smoked during the last 3 months of pregnancy. According to the USPSTF, behavioral interventions substantially improve the achievement of tobacco smoking abstinence in pregnant women, increase infant birth weight, and reduce the risk of preterm birth.
Sustained-release bupropion and varenicline showed no strong evidence of positive or negative fetal outcomes in one study of pregnant women. [41] In a comparison of pregnant smokers, varenicline was 3 times more effective than nicotine replacement. [42] Varenicline showed no increase in negative fetal outcomes in a large Danish cohort. [43] Although a few studies suggest a potential benefit of NRT on perinatal outcomes in pregnancy, nicotine is classified as a pregnancy category D medication, indicating evidence of fetal risk. Both bupropion sustained-release and varenicline are pregnancy class C medications. [44]
- Differential Diagnosis
Differentials of nicotine dependence include substance use disorders, which may present with similar withdrawal and craving symptoms, and mental health conditions like generalized anxiety disorder and major depressive disorder, with symptoms that can overlap with nicotine withdrawal. Individuals with attention-deficit/hyperactivity disorder may use nicotine to self-medicate, while panic disorder can mimic withdrawal symptoms. Additionally, other behavioral addictions, such as gambling or internet addiction, may exhibit similar compulsive behavior and reward-seeking patterns.
Cigarette smoking produces a host of health problems, all of which are considered indirect effects of nicotine addiction. These conditions include but are not limited to the following:
- α-1 antitrypsin deficiency
- Angina pectoris
- Non-small cell lung cancer
- Small cell lung cancer
A thorough history and targeted questioning can help distinguish nicotine addiction from other conditions and guide treatment strategies.
- Pertinent Studies and Ongoing Trials
Integrating tobacco cessation has become a key focus in developing medical school curricula. [45] Short but sustained training programs are the most effective.
Tobacco smoking is extremely hazardous to human health. Smokers have a death rate approximately 3 times higher than those who have never smoked. The excess mortality of smokers is mostly attributed to vascular illnesses such as CAD, respiratory illnesses such as COPD, and at least 17 different classes of tobacco-smoking-related cancers. Evidence shows that smokers lose at least 10 years of life expectancy on average. Quitting smoking before age 40 has been shown to reduce smoking-related death by about 90%. [46]
- Complications
Physicians should make it a priority to help patients stop smoking. Smoking even a few cigarettes a day or only occasionally increases a person's chance of developing lung cancer. Smoking cessation has immediate benefits that begin hours after a person stops smoking, including lowering blood pressure, decreased cough and phlegm production, and increased lung capacity. Quitting smoking reduces a patient's risk of developing cancer, heart disease, and chronic lung disease in the long term. The earlier a person stops smoking, the more their risk of developing lung cancer is reduced.
However, quitting smoking at any age is beneficial, and the benefits of smoking cessation are cumulative over time. People who stop smoking before age 40 reduce their chances of dying from smoking-related diseases by 90%. Even people already diagnosed with cancer benefit from smoking cessation. With some forms of cancer, quitting smoking at the time of diagnosis can reduce the chances of cancer-related death by as much as 40%. [47] [48]
- Consultations
Consultations with psychiatry and addiction specialists and referrals from primary care to medical specialties like pulmonology and cardiology can be helpful.
- Deterrence and Patient Education
Primary care and many public health programs form the base of efforts to combat nicotine addiction. Through comprehensive patient education, emphasizing the risks of smoking and the benefits of cessation, healthcare providers play a pivotal role in promoting healthier behaviors. These efforts include offering counseling, prescribing cessation aids, and advocating for smoke-free environments to reduce exposure and support long-term success in quitting tobacco use.
- Pearls and Other Issues
Screening, persistence, and aggressive treatment with medications and counseling are effective in treating the world's most deadly addiction. Early identification through thorough screening in healthcare settings allows for timely interventions. Persistence in supporting patients through the challenges of quitting, combined with tailored pharmacotherapy and behavioral counseling, enhances cessation outcomes. These approaches address both the physiological and psychological aspects of nicotine addiction, promoting sustained abstinence and improved overall health.
- Enhancing Healthcare Team Outcomes
Tobacco smoking is a life-threatening addiction that, if untreated, can cause damage to every organ system in the human body. The best way to avoid a tobacco smoking-related illness is never to start smoking, and the next-best way is to stop smoking cigarettes as soon as possible. Helping a patient quit smoking is currently one of the most beneficial preventive medicine interventions. Nearly every healthcare team member may play an important role in assisting with smoking cessation. Nurses play a large role in assisting clinicians in tobacco cessation programs. Some hospitals train nurses to deliver behavioral and pharmaceutical interventions to inpatient smokers. These interventions have shown great promise in significantly reducing smoking in certain populations. [49]
Clinicians are also at the front lines in the fight against tobacco smoking. Evidence shows that individually focused counseling when delivered by a physician, can aid a patient's smoking cessation efforts. Clinician-prescribed or recommended over-the-counter medications have also been shown to play an effective role in treating these patients. [50] The best outcomes in convincing patients to quit smoking are achieved through an interprofessional team working together to educate the patient.
Clinical scientists also play a highly important role in the fight to end tobacco addiction and tobacco-related diseases. Clinical scientists continue to investigate and discover the physiology of tobacco-related illnesses, the effectiveness of tobacco cessation medications and interventions, and tobacco smoking-related conditions across a broad spectrum of populations. Scientific research has revealed much about tobacco smoking, yet much still remains to be discovered. An interprofessional team approach to smoking cessation promises better patient outcomes.
- Review Questions
- Access free multiple choice questions on this topic.
- Click here for a simplified version.
- Comment on this article.
Disclosure: Sunny Aslam declares no relevant financial relationships with ineligible companies.
Disclosure: Stephen Leslie declares no relevant financial relationships with ineligible companies.
Disclosure: Jason Morris declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Aslam SP, Leslie SW, Morris J. Nicotine Addiction and Smoking: Health Effects and Interventions. [Updated 2024 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Nicotine Addiction and Smoking: Health Effects and Interventions (Nursing). [StatPearls. 2024] Nicotine Addiction and Smoking: Health Effects and Interventions (Nursing). Aslam SP, Leslie SW, Morris J, Bomgaars DL. StatPearls. 2024 Jan
- [The history of antitobacco actions in the last 500 years. part. 1. Non-medical actions]. [Przegl Lek. 2006] [The history of antitobacco actions in the last 500 years. part. 1. Non-medical actions]. Grzybowski A. Przegl Lek. 2006; 63(10):1126-30.
- [The history of antitobacco actions in the last 500 years. Part. II. Medical actions]. [Przegl Lek. 2006] [The history of antitobacco actions in the last 500 years. Part. II. Medical actions]. Grzybowski A. Przegl Lek. 2006; 63(10):1131-4.
- Review Public Health Policies on E-Cigarettes. [Curr Cardiol Rep. 2019] Review Public Health Policies on E-Cigarettes. Bhalerao A, Sivandzade F, Archie SR, Cucullo L. Curr Cardiol Rep. 2019 Aug 28; 21(10):111. Epub 2019 Aug 28.
- Review A critique of the US Surgeon General's conclusions regarding e-cigarette use among youth and young adults in the United States of America. [Harm Reduct J. 2017] Review A critique of the US Surgeon General's conclusions regarding e-cigarette use among youth and young adults in the United States of America. Polosa R, Russell C, Nitzkin J, Farsalinos KE. Harm Reduct J. 2017 Sep 6; 14(1):61. Epub 2017 Sep 6.
Recent Activity
- Nicotine Addiction and Smoking: Health Effects and Interventions - StatPearls Nicotine Addiction and Smoking: Health Effects and Interventions - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 10 October 2022
Health effects associated with smoking: a Burden of Proof study
- Xiaochen Dai ORCID: orcid.org/0000-0002-0289-7814 1 , 2 ,
- Gabriela F. Gil 1 ,
- Marissa B. Reitsma 1 ,
- Noah S. Ahmad 1 ,
- Jason A. Anderson 1 ,
- Catherine Bisignano 1 ,
- Sinclair Carr 1 ,
- Rachel Feldman 1 ,
- Simon I. Hay ORCID: orcid.org/0000-0002-0611-7272 1 , 2 ,
- Jiawei He 1 , 2 ,
- Vincent Iannucci 1 ,
- Hilary R. Lawlor 1 ,
- Matthew J. Malloy 1 ,
- Laurie B. Marczak 1 ,
- Susan A. McLaughlin 1 ,
- Larissa Morikawa ORCID: orcid.org/0000-0001-9749-8033 1 ,
- Erin C. Mullany 1 ,
- Sneha I. Nicholson 1 ,
- Erin M. O’Connell 1 ,
- Chukwuma Okereke 1 ,
- Reed J. D. Sorensen 1 ,
- Joanna Whisnant 1 ,
- Aleksandr Y. Aravkin 1 , 3 ,
- Peng Zheng 1 , 2 ,
- Christopher J. L. Murray ORCID: orcid.org/0000-0002-4930-9450 1 , 2 &
- Emmanuela Gakidou ORCID: orcid.org/0000-0002-8992-591X 1 , 2
Nature Medicine volume 28 , pages 2045–2055 ( 2022 ) Cite this article
29k Accesses
60 Citations
169 Altmetric
Metrics details
- Risk factors
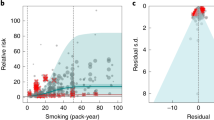
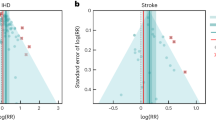
Matters Arising to this article was published on 14 April 2023
As a leading behavioral risk factor for numerous health outcomes, smoking is a major ongoing public health challenge. Although evidence on the health effects of smoking has been widely reported, few attempts have evaluated the dose–response relationship between smoking and a diverse range of health outcomes systematically and comprehensively. In the present study, we re-estimated the dose–response relationships between current smoking and 36 health outcomes by conducting systematic reviews up to 31 May 2022, employing a meta-analytic method that incorporates between-study heterogeneity into estimates of uncertainty. Among the 36 selected outcomes, 8 had strong-to-very-strong evidence of an association with smoking, 21 had weak-to-moderate evidence of association and 7 had no evidence of association. By overcoming many of the limitations of traditional meta-analyses, our approach provides comprehensive, up-to-date and easy-to-use estimates of the evidence on the health effects of smoking. These estimates provide important information for tobacco control advocates, policy makers, researchers, physicians, smokers and the public.
Similar content being viewed by others
A systematic review and network meta-analysis of population-level interventions to tackle smoking behaviour
The Burden of Proof studies: assessing the evidence of risk
Health effects associated with exposure to secondhand smoke: a Burden of Proof study
Among both the public and the health experts, smoking is recognized as a major behavioral risk factor with a leading attributable health burden worldwide. The health risks of smoking were clearly outlined in a canonical study of disease rates (including lung cancer) and smoking habits in British doctors in 1950 and have been further elaborated in detail over the following seven decades 1 , 2 . In 2005, evidence of the health consequences of smoking galvanized the adoption of the first World Health Organization (WHO) treaty, the Framework Convention on Tobacco Control, in an attempt to drive reductions in global tobacco use and second-hand smoke exposure 3 . However, as of 2020, an estimated 1.18 billion individuals globally were current smokers and 7 million deaths and 177 million disability-adjusted life-years were attributed to smoking, reflecting a persistent public health challenge 4 . Quantifying the relationship between smoking and various important health outcomes—in particular, highlighting any significant dose–response relationships—is crucial to understanding the attributable health risk experienced by these individuals and informing responsive public policy.
Existing literature on the relationship between smoking and specific health outcomes is prolific, including meta-analyses, cohort studies and case–control studies analyzing the risk of outcomes such as lung cancer 5 , 6 , 7 , chronic obstructive pulmonary disease (COPD) 8 , 9 , 10 and ischemic heart disease 11 , 12 , 13 , 14 due to smoking. There are few if any attempts, however, to systematically and comprehensively evaluate the landscape of evidence on smoking risk across a diverse range of health outcomes, with most current research focusing on risk or attributable burden of smoking for a specific condition 7 , 15 , thereby missing the opportunity to provide a comprehensive picture of the health risk experienced by smokers. Furthermore, although evidence surrounding specific health outcomes, such as lung cancer, has generated widespread consensus, findings about the attributable risk of other outcomes are much more heterogeneous and inconclusive 16 , 17 , 18 . These studies also vary in their risk definitions, with many comparing dichotomous exposure measures of ever smokers versus nonsmokers 19 , 20 . Others examine the distinct risks of current smokers and former smokers compared with never smokers 21 , 22 , 23 . Among the studies that do analyze dose–response relationships, there is large variation in the units and dose categories used in reporting their findings (for example, the use of pack-years or cigarettes per day) 24 , 25 , which complicates the comparability and consolidation of evidence. This, in turn, can obscure data that could inform personal health choices, public health practices and policy measures. Guidance on the health risks of smoking, such as the Surgeon General’s Reports on smoking 26 , 27 , is often based on experts’ evaluation of heterogenous evidence, which, although extremely useful and well suited to carefully consider nuances in the evidence, is fundamentally subjective.
The present study, as part of the Global Burden of Diseases, Risk Factors, and Injuries Study (GBD) 2020, re-estimated the continuous dose–response relationships (the mean risk functions and associated uncertainty estimates) between current smoking and 36 health outcomes (Supplementary Table 1 ) by identifying input studies using a systematic review approach and employing a meta-analytic method 28 . The 36 health outcomes that were selected based on existing evidence of a relationship included 16 cancers (lung cancer, esophageal cancer, stomach cancer, leukemia, liver cancer, laryngeal cancer, breast cancer, cervical cancer, colorectal cancer, lip and oral cavity cancer, nasopharyngeal cancer, other pharynx cancer (excluding nasopharynx cancer), pancreatic cancer, bladder cancer, kidney cancer and prostate cancer), 5 cardiovascular diseases (CVDs: ischemic heart disease, stroke, atrial fibrillation and flutter, aortic aneurysm and peripheral artery disease) and 15 other diseases (COPD, lower respiratory tract infections, tuberculosis, asthma, type 2 diabetes, Alzheimer’s disease and related dementias, Parkinson’s disease, multiple sclerosis, cataracts, gallbladder diseases, low back pain, peptic ulcer disease, rheumatoid arthritis, macular degeneration and fractures). Definitions of the outcomes are described in Supplementary Table 1 . We conducted a separate systematic review for each risk–outcome pair with the exception of cancers, which were done together in a single systematic review. This approach allowed us to systematically identify all relevant studies indexed in PubMed up to 31 May 2022, and we extracted relevant data on risk of smoking, including study characteristics, following a pre-specified template (Supplementary Table 2 ). The meta-analytic tool overcomes many of the limitations of traditional meta-analyses by incorporating between-study heterogeneity into the uncertainty of risk estimates, accounting for small numbers of studies, relaxing the assumption of log(linearity) applied to the risk functions, handling differences in exposure ranges between comparison groups, and systematically testing and adjusting for bias due to study designs and characteristics. We then estimated the burden-of-proof risk function (BPRF) for each risk–outcome pair, as proposed by Zheng et al. 29 ; the BPRF is a conservative risk function defined as the 5th quantile curve (for harmful risks) that reflects the smallest harmful effect at each level of exposure consistent with the available evidence. Given all available data for each outcome, the risk of smoking is at least as harmful as the BPRF indicates.
We used the BPRF for each risk–outcome pair to calculate risk–outcome scores (ROSs) and categorize the strength of evidence for the association between smoking and each health outcome using a star rating from 1 to 5. The interpretation of the star ratings is as follows: 1 star (*) indicates no evidence of association; 2 stars (**) correspond to a 0–15% increase in risk across average range of exposures for harmful risks; 3 stars (***) represent a 15–50% increase in risk; 4 stars (****) refer to >50–85% increase in risk; and 5 stars (*****) equal >85% increase in risk. The thresholds for each star rating were developed in consultation with collaborators and other stakeholders.
The increasing disease burden attributable to current smoking, particularly in low- and middle-income countries 4 , demonstrates the relevance of the present study, which quantifies the strength of the evidence using an objective, quantitative, comprehensive and comparative framework. Findings from the present study can be used to support policy makers in making informed smoking recommendations and regulations focusing on the associations for which the evidence is strongest (that is, the 4- and 5-star associations). However, associations with a lower star rating cannot be ignored, especially when the outcome has high prevalence or severity. A summary of the main findings, limitations and policy implications of the study is presented in Table 1 .
We evaluated the mean risk functions and the BPRFs for 36 health outcomes that are associated with current smoking 30 (Table 2 ). Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines 31 for each of our systematic reviews, we identified studies reporting relative risk (RR) of incidence or mortality from each of the 36 selected outcomes for smokers compared with nonsmokers. We reviewed 21,108 records, which were identified to have been published between 1 May 2018 and 31 May 2022; this represents the most recent time period since the last systematic review of the available evidence for the GBD at the time of publication. The meta-analyses reported in the present study for each of the 36 health outcomes are based on evidence from a total of 793 studies published between 1970 and 2022 (Extended Data Fig. 1 – 5 and Supplementary Information 1.5 show the PRISMA diagrams for each outcome). Only prospective cohort and case–control studies were included for estimating dose–response risk curves, but cross-sectional studies were also included for estimating the age pattern of smoking risk on cardiovascular and circulatory disease (CVD) outcomes. Details on each, including the study’s design, data sources, number of participants, length of follow-up, confounders adjusted for in the input data and bias covariates included in the dose–response risk model, can be found in Supplementary Information 2 and 3 . The theoretical minimum risk exposure level used for current smoking was never smoking or zero 30 .
Five-star associations
When the most conservative interpretation of the evidence, that is, the BPRF, suggests that the average exposure (15th–85th percentiles of exposure) of smoking increases the risk of a health outcome by >85% (that is, ROS > 0.62), smoking and that outcome are categorized as a 5-star pair. Among the 36 outcomes, there are 5 that have a 5-star association with current smoking: laryngeal cancer (375% increase in risk based on the BPRF, 1.56 ROS), aortic aneurysm (150%, 0.92), peripheral artery disease (137%, 0.86), lung cancer (107%, 0.73) and other pharynx cancer (excluding nasopharynx cancer) (92%, 0.65).
Results for all 5-star risk–outcome pairs are available in Table 2 and Supplementary Information 4.1 . In the present study, we provide detailed results for one example 5-star association: current smoking and lung cancer. We extracted 371 observations from 25 prospective cohort studies and 53 case–control studies across 25 locations (Supplementary Table 3 ) 5 , 6 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 . Exposure ranged from 1 pack-year to >112 pack-years, with the 85th percentile of exposure being 50.88 pack-years (Fig. 1a ).
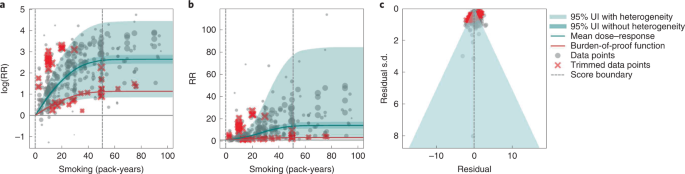
a , The log(RR) function. b , RR function. c , A modified funnel plot showing the residuals (relative to 0) on the x axis and the estimated s.d. that includes reported s.d. and between-study heterogeneity on the y axis.
We found a very strong and significant harmful relationship between pack-years of current smoking and the RR of lung cancer (Fig. 1b ). The mean RR of lung cancer at 20 pack-years of smoking was 5.11 (95% uncertainty interval (UI) inclusive of between-study heterogeneity = 1.84–14.99). At 50.88 pack-years (85th percentile of exposure), the mean RR of lung cancer was 13.42 (2.63–74.59). See Table 2 for mean RRs at other exposure levels. The BPRF, which represents the most conservative interpretation of the evidence (Fig. 1a ), suggests that smoking in the 15th–85th percentiles of exposure increases the risk of lung cancer by an average of 107%, yielding an ROS of 0.73.
The relationship between pack-years of current smoking and RR of lung cancer is nonlinear, with diminishing impact of further pack-years of smoking, particularly for middle-to-high exposure levels (Fig. 1b ). To reduce the effect of bias, we adjusted observations that did not account for more than five confounders, including age and sex, because they were the significant bias covariates identified by the bias covariate selection algorithm 29 (Supplementary Table 7 ). The reported RRs across studies were very heterogeneous. Our meta-analytic method, which accounts for the reported uncertainty in both the data and between-study heterogeneity, fit the data and covered the estimated residuals well (Fig. 1c ). After trimming 10% of outliers, we still detected publication bias in the results for lung cancer. See Supplementary Tables 4 and 7 for study bias characteristics and selected bias covariates, Supplementary Fig. 5 for results without 10% trimming and Supplementary Table 8 for observed RR data and alternative exposures across studies for the remaining 5-star pairs.
Four-star associations
When the BPRF suggests that the average exposure of smoking increases the risk of a health outcome by 50–85% (that is, ROS > 0.41–0.62), smoking is categorized as having a 4-star association with that outcome. We identified three outcomes with a 4-star association with smoking: COPD (72% increase in risk based on the BPRF, 0.54 ROS), lower respiratory tract infection (54%, 0.43) and pancreatic cancer (52%, 0.42).
In the present study, we provide detailed results for one example 4-star association: current smoking and COPD. We extracted 51 observations from 11 prospective cohort studies and 4 case–control studies across 36 locations (Supplementary Table 3 ) 6 , 8 , 9 , 10 , 78 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 . Exposure ranged from 1 pack-year to 100 pack-years, with the 85th percentile of exposure in the exposed group being 49.75 pack-years.
We found a strong and significant harmful relationship between pack-years of current smoking and RR of COPD (Fig. 2b ). The mean RR of COPD at 20 pack-years was 3.17 (1.60–6.55; Table 2 reports RRs at other exposure levels). At the 85th percentile of exposure, the mean RR of COPD was 6.01 (2.08–18.58). The BPRF suggests that average smoking exposure raises the risk of COPD by an average of 72%, yielding an ROS of 0.54. The results for the other health outcomes that have an association with smoking rated as 4 stars are shown in Table 2 and Supplementary Information 4.2 .
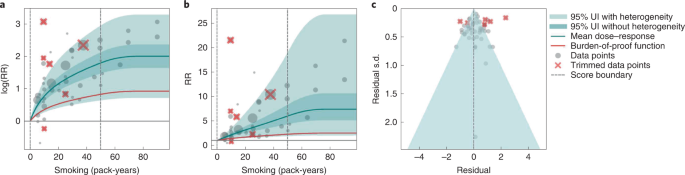
a , The log(RR) function. b , RR function. c , A modified funnel plot showing the residuals (relative to 0) on th e x axis and the estimated s.d. that includes the reported s.d. and between-study heterogeneity on the y axis.
The relationship between smoking and COPD is nonlinear, with diminishing impact of further pack-years of current smoking on risk of COPD, particularly for middle-to-high exposure levels (Fig. 2a ). To reduce the effect of bias, we adjusted observations that did not account for age and sex and/or were generated for individuals aged >65 years 116 , because they were the two significant bias covariates identified by the bias covariate selection algorithm (Supplementary Table 7 ). There was large heterogeneity in the reported RRs across studies, and our meta-analytic method fit the data and covered the estimated residuals well (Fig. 2b ). Although we trimmed 10% of outliers, publication bias was still detected in the results for COPD. See Supplementary Tables 4 and 7 for study bias characteristics and selected bias covariates, Supplementary Fig. 5 for results without 10% trimming and Supplementary Table 8 for reported RR data and alternative exposures across studies for the remaining health outcomes that have a 4-star association with smoking.
Three-star associations
When the BPRF suggests that the average exposure of smoking increases the risk of a health outcome by 15–50% (or, when protective, decreases the risk of an outcome by 13–34%; that is, ROS >0.14–0.41), the association between smoking and that outcome is categorized as having a 3-star rating. We identified 15 outcomes with a 3-star association: bladder cancer (40% increase in risk, 0.34 ROS); tuberculosis (31%, 0.27); esophageal cancer (29%, 0.26); cervical cancer, multiple sclerosis and rheumatoid arthritis (each 23–24%, 0.21); lower back pain (22%, 0.20); ischemic heart disease (20%, 0.19); peptic ulcer and macular degeneration (each 19–20%, 0.18); Parkinson's disease (protective risk, 15% decrease in risk, 0.16); and stomach cancer, stroke, type 2 diabetes and cataracts (each 15–17%, 0.14–0.16).
We present the findings on smoking and type 2 diabetes as an example of a 3-star risk association. We extracted 102 observations from 24 prospective cohort studies and 4 case–control studies across 15 locations (Supplementary Table 3 ) 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 , 141 , 142 , 143 , 144 . The exposure ranged from 1 cigarette to 60 cigarettes smoked per day, with the 85th percentile of exposure in the exposed group being 26.25 cigarettes smoked per day.
We found a moderate and significant harmful relationship between cigarettes smoked per day and the RR of type 2 diabetes (Fig. 3b ). The mean RR of type 2 diabetes at 20 cigarettes smoked per day was 1.49 (1.18–1.90; see Table 2 for other exposure levels). At the 85th percentile of exposure, the mean RR of type 2 diabetes was 1.54 (1.20–2.01). The BPRF suggests that average smoking exposure raises the risk of type 2 diabetes by an average of 16%, yielding an ROS of 0.15. See Table 2 and Supplementary Information 4.3 for results for the additional health outcomes with an association with smoking rated as 3 stars.
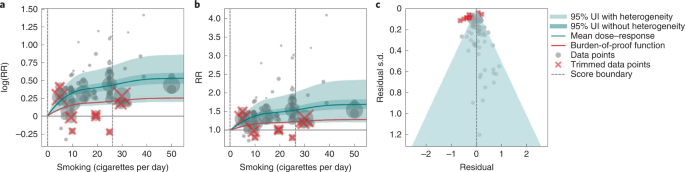
a , The log(RR) function. b , RR function. c , A modified funnel plot showing the residuals (relative to 0) on the x axis and the estimated s.d. that includes the reported s.d. and between-study heterogeneity on the y axis.
The relationship between smoking and type 2 diabetes is nonlinear, particularly for high exposure levels where the mean risk curve becomes flat (Fig. 3a ). We adjusted observations that were generated in subpopulations, because it was the only significant bias covariate identified by the bias covariate selection algorithm (Supplementary Table 7 ). There was moderate heterogeneity in the observed RR data across studies and our meta-analytic method fit the data and covered the estimated residuals extremely well (Fig. 3b,c ). After trimming 10% of outliers, we still detected publication bias in the results for type 2 diabetes. See Supplementary Tables 4 and 7 for study bias characteristics and selected bias covariates, Supplementary Fig. 5 for results without 10% trimming and Supplementary Table 8 for observed RR data and alternative exposures across studies for the remaining 3-star pairs.
Two-star associations
When the BPRF suggests that the average exposure of smoking increases the risk of an outcome by 0–15% (that is, ROS 0.0–0.14), the association between smoking and that outcome is categorized as a 2-star rating. We identified six 2-star outcomes: nasopharyngeal cancer (14% increase in risk, 0.13 ROS); Alzheimer’s and other dementia (10%, 0.09); gallbladder diseases and atrial fibrillation and flutter (each 6%, 0.06); lip and oral cavity cancer (5%, 0.05); and breast cancer (4%, 0.04).
We present the findings on smoking and breast cancer as an example of a 2-star association. We extracted 93 observations from 14 prospective cohort studies and 9 case–control studies across 14 locations (Supplementary Table 3 ) 84 , 87 , 145 , 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 , 162 , 163 , 164 , 165 . The exposure ranged from 1 cigarette to >76 cigarettes smoked per day, with the 85th percentile of exposure in the exposed group being 34.10 cigarettes smoked per day.
We found a weak but significant relationship between pack-years of current smoking and RR of breast cancer (Extended Data Fig. 6 ). The mean RR of breast cancer at 20 pack-years was 1.17 (1.04–1.31; Table 2 reports other exposure levels). The BPRF suggests that average smoking exposure raises the risk of breast cancer by an average of 4%, yielding an ROS of 0.04. See Table 2 and Supplementary Information 4.4 for results on the additional health outcomes for which the association with smoking has been categorized as 2 stars.
The relationship between smoking and breast cancer is nonlinear, particularly for high exposure levels where the mean risk curve becomes flat (Extended Data Fig. 6a ). To reduce the effect of bias, we adjusted observations that were generated in subpopulations, because it was the only significant bias covariate identified by the bias covariate selection algorithm (Supplementary Table 7 ). There was heterogeneity in the reported RRs across studies, but our meta-analytic method fit the data and covered the estimated residuals (Extended Data Fig. 6b ). After trimming 10% of outliers, we did not detect publication bias in the results for breast cancer. See Supplementary Tables 4 and 7 for study bias characteristics and selected bias covariates, Supplementary Fig. 5 for results without 10% trimming and Supplementary Table 8 for observed RR data and alternative exposures across studies for the remaining 2-star pairs.
One-star associations
When average exposure to smoking does not significantly increase (or decrease) the risk of an outcome, once between-study heterogeneity and other sources of uncertainty are accounted for (that is, ROS < 0), the association between smoking and that outcome is categorized as 1 star, indicating that there is not sufficient evidence for the effect of smoking on the outcome to reject the null (that is, there may be no association). There were seven outcomes with an association with smoking that rated as 1 star: colorectal and kidney cancer (each –0.01 ROS); leukemia (−0.04); fractures (−0.05); prostate cancer (−0.06); liver cancer (−0.32); and asthma (−0.64).
We use smoking and prostate cancer as examples of a 1-star association. We extracted 78 observations from 21 prospective cohort studies and 1 nested case–control study across 15 locations (Supplementary Table 3 ) 157 , 160 , 166 , 167 , 168 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 , 184 , 185 . The exposure among the exposed group ranged from 1 cigarette to 90 cigarettes smoked per day, with the 85th percentile of exposure in the exposed group being 29.73 cigarettes smoked per day.
Based on our conservative interpretation of the data, we did not find a significant relationship between cigarettes smoked per day and the RR of prostate cancer (Fig. 4B ). The exposure-averaged BPRF for prostate cancer was 0.94, which was opposite null from the full range of mean RRs, such as 1.16 (0.89–1.53) at 20 cigarettes smoked per day. The corresponding ROS was −0.06, which is consistent with no evidence of an association between smoking and increased risk of prostate cancer. See Table 2 and Supplementary Information 4.5 for results for the additional outcomes that have a 1-star association with smoking.
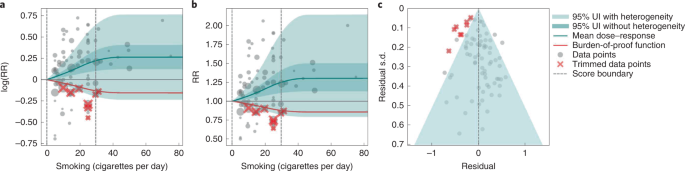
The relationship between smoking and prostate cancer is nonlinear, particularly for middle-to-high exposure levels where the mean risk curve becomes flat (Fig. 4a ). We did not adjust for any bias covariate because no significant bias covariates were selected by the algorithm (Supplementary Table 7 ). The RRs reported across studies were very heterogeneous, but our meta-analytic method fit the data and covered the estimated residuals well (Fig. 4b,c ). The ROS associated with the BPRF is −0.05, suggesting that the most conservative interpretation of all evidence, after accounting for between-study heterogeneity, indicates an inconclusive relationship between smoking exposure and the risk of prostate cancer. After trimming 10% of outliers, we still detected publication bias in the results for prostate cancer, which warrants further studies using sample populations. See Supplementary Tables 4 and 7 for study bias characteristics and selected bias covariates, Supplementary Fig. 5 for results without 10% trimming and Supplementary Table 8 for observed RR data and alternative exposures across studies for the remaining 1-star pairs.
Age-specific dose–response risk for CVD outcomes
We produced age-specific dose–response risk curves for the five selected CVD outcomes ( Methods ). The ROS associated with each smoking–CVD pair was calculated based on the reference risk curve estimated using all risk data regardless of age information. Estimation of the BPRF, calculation of the associated ROS and star rating of the smoking–CVD pairs follow the same rules as the other non-CVD smoking–outcome pairs (Table 1 and Supplementary Figs. 2 – 4 ). Once we had estimated the reference dose–response risk curve for each CVD outcome, we determined the age group of the reference risk curve. The reference age group is 55–59 years for all CVD outcomes, except for peripheral artery disease, the reference age group for which is 60–64 years. We then estimated the age pattern of smoking on all CVD outcomes (Supplementary Fig. 2 ) and calculated age attenuation factors of the risk for each age group by comparing the risk of each age group with that of the reference age group, using the estimated age pattern (Supplementary Fig. 3 ). Last, we applied the draws of age attenuation factors of each age group to the dose–response risk curve for the reference age group to produce the age group-specific dose–response risk curves for each CVD outcome (Supplementary Fig. 4 ).
Using our burden-of-proof meta-analytic methods, we re-estimated the dose–response risk of smoking on 36 health outcomes that had previously been demonstrated to be associated with smoking 30 , 186 . Using these methods, which account for both the reported uncertainty of the data and the between-study heterogeneity, we found that 29 of the 36 smoking–outcome pairs are supported by evidence that suggests a significant dose–response relationship between smoking and the given outcome (28 with a harmful association and 1 with a protective association). Conversely, after accounting for between-study heterogeneity, the available evidence of smoking risk on seven outcomes (that is, colon and rectum cancer, kidney cancer, leukemia, prostate cancer, fractures, liver cancer and asthma) was insufficient to reject the null or draw definitive conclusions on their relationship to smoking. Among the 29 outcomes that have evidence supporting a significant relationship to smoking, 8 had strong-to-very-strong evidence of a relationship, meaning that, given all the available data on smoking risk, we estimate that average exposure to smoking increases the risk of those outcomes by >50% (4- and 5-star outcomes). The currently available evidence for the remaining 21 outcomes with a significant association with current smoking was weak to moderate, indicating that smoking increases the risk of those outcomes by at least >0–50% (2- and 3-star associations).
Even under our conservative interpretation of the data, smoking is irrefutably harmful to human health, with the greatest increases in risk occurring for laryngeal cancer, aortic aneurysm, peripheral artery disease, lung cancer and other pharynx cancer (excluding nasopharynx cancer), which collectively represent large causes of death and ill-health. The magnitude of and evidence for the associations between smoking and its leading health outcomes are among the highest currently analyzed in the burden-of-proof framework 29 . The star ratings assigned to each smoking–outcome pair offer policy makers a way of categorizing and comparing the evidence for a relationship between smoking and its potential health outcomes ( https://vizhub.healthdata.org/burden-of-proof ). We found that, for seven outcomes in our analysis, there was insufficient or inconsistent evidence to demonstrate a significant association with smoking. This is a key finding because it demonstrates the need for more high-quality data for these particular outcomes; availability of more data should improve the strength of evidence for whether or not there is an association between smoking and these health outcomes.
Our systematic review approach and meta-analytic methods have numerous benefits over existing systematic reviews and meta-analyses on the same topic that use traditional random effects models. First, our approach relaxes the log(linear) assumption, using a spline ensemble to estimate the risk 29 . Second, our approach allows variable reference groups and exposure ranges, allowing for more accurate estimates regardless of whether or not the underlying relative risk is log(linear). Furthermore, it can detect outliers in the data automatically. Finally, it quantifies uncertainty due to between-study heterogeneity while accounting for small numbers of studies, minimizing the risk that conclusions will be drawn based on spurious findings.
We believe that the results for the association between smoking and each of the 36 health outcomes generated by the present study, including the mean risk function, BPRF, ROS, average excess risk and star rating, could be useful to a range of stakeholders. Policy makers can formulate their decisions on smoking control priorities and resource allocation based on the magnitude of the effect and the consistency of the evidence relating smoking to each of the 36 outcomes, as represented by the ROS and star rating for each smoking–outcome association 187 . Physicians and public health practitioners can use the estimates of average increased risk and the star rating to educate patients and the general public about the risk of smoking and to promote smoking cessation 188 . Researchers can use the estimated mean risk function or BPRF to obtain the risk of an outcome at a given smoking exposure level, as well as uncertainty surrounding that estimate of risk. The results can also be used in the estimation of risk-attributable burden, that is, the deaths and disability-adjusted life-years due to each outcome that are attributable to smoking 30 , 186 . For the general public, these results could help them to better understand the risk of smoking and manage their health 189 .
Although our meta-analysis was comprehensive and carefully conducted, there are limitations to acknowledge. First, the bias covariates used, although carefully extracted and evaluated, were based on observable study characteristics and thus may not fully capture unobserved characteristics such as study quality or context, which might be major sources of bias. Second, if multiple risk estimates with different adjustment levels were reported in a given study, we included only the fully adjusted risk estimate and modeled the adjustment level according to the number of covariates adjusted for (rather than which covariates were adjusted for) and whether a standard adjustment for age and sex had been applied. This approach limited our ability to make full use of all available risk estimates in the literature. Third, although we evaluated the potential for publication bias in the data, we did not test for other forms of bias such as when studies are more consistent with each other than expected by chance 29 . Fourth, our analysis assumes that the relationships between smoking and health outcomes are similar across geographical regions and over time. We do not have sufficient evidence to quantify how the relationships may have evolved over time because the composition of smoking products has also changed over time. Perhaps some of the heterogeneity of the effect sizes in published studies reflects this; however, this cannot be discerned with the currently available information.
In the future, we plan to include crude and partially adjusted risk estimates in our analyses to fully incorporate all available risk estimates, to model the adjusted covariates in a more comprehensive way by mapping the adjusted covariates across all studies comprehensively and systematically, and to develop methods to evaluate additional forms of potential bias. We plan to update our results on a regular basis to provide timely and up-to-date evidence to stakeholders.
To conclude, we have re-estimated the dose–response risk of smoking on 36 health outcomes while synthesizing all the available evidence up to 31 May 2022. We found that, even after factoring in the heterogeneity between studies and other sources of uncertainty, smoking has a strong-to-very-strong association with a range of health outcomes and confirmed that smoking is irrefutably highly harmful to human health. We found that, due to small numbers of studies, inconsistency in the data, small effect sizes or a combination of these reasons, seven outcomes for which some previous research had found an association with smoking did not—under our meta-analytic framework and conservative approach to interpreting the data—have evidence of an association. Our estimates of the evidence for risk of smoking on 36 selected health outcomes have the potential to inform the many stakeholders of smoking control, including policy makers, researchers, public health professionals, physicians, smokers and the general public.
For the present study, we used a meta-analytic tool, MR-BRT (metaregression—Bayesian, regularized, trimmed), to estimate the dose–response risk curves of the risk of a health outcome across the range of current smoking levels along with uncertainty estimates 28 . Compared with traditional meta-analysis using linear mixed effect models, MR-BRT relaxes the assumption of a log(linear) relationship between exposure and risk, incorporates between-study heterogeneity into the uncertainty of risk estimates, handles estimates reported across different exposure categories, automatically identifies and trims outliers, and systematically tests and adjusts for bias due to study designs and characteristics. The meta-analytic methods employed by the present study followed the six main steps proposed by Zheng et al. 28 , 29 , namely: (1) enacting a systematic review approach and data extraction following a pre-specified and standardized protocol; (2) estimating the shape of the relationship between exposure and RR; (3) evaluating and adjusting for systematic bias as a function of study characteristics and risk estimation; (4) quantifying between-study heterogeneity while adjusting for within-study correlation and the number of studies; (5) evaluating potential publication or reporting biases; and (6) estimating the mean risk function and the BPRF, calculating the ROS and categorizing smoking–outcome pairs using a star-rating scheme from 1 to 5.
The estimates for our primary indicators of this work—mean RRs across a range of exposures, BRPFs, ROSs and star ratings for each risk–outcome pair—are not specific to or disaggregated by specific populations. We did not estimate RRs separately for different locations, sexes (although the RR of prostate cancer was estimated only for males and of cervical and breast cancer only for females) or age groups (although this analysis was applied to disease endpoints in adults aged ≥30 years only and, as detailed below, age-specific estimates were produced for the five CVD outcomes).
The present study complies with the PRISMA guidelines 190 (Supplementary Tables 9 and 10 and Supplementary Information 1.5 ) and Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) recommendations 191 (Supplementary Table 11 ). The study was approved by the University of Washington Institutional Review Board (study no. 9060). The systematic review approach was not registered.
Selecting health outcomes
In the present study, current smoking is defined as the current use of any smoked tobacco product on a daily or occasional basis. Health outcomes were initially selected using the World Cancer Research Fund criteria for convincing or probable evidence as described in Murray et al. 186 . The 36 health outcomes that were selected based on existing evidence of a relationship included 16 cancers (lung cancer, esophageal cancer, stomach cancer, leukemia, liver cancer, laryngeal cancer, breast cancer, cervical cancer, colorectal cancer, lip and oral cavity cancer, nasopharyngeal cancer, other pharynx cancer (excluding nasopharynx cancer), pancreatic cancer, bladder cancer, kidney cancer and prostate cancer), 5 CVDs (ischemic heart disease, stroke, atrial fibrillation and flutter, aortic aneurysm and peripheral artery disease) and 15 other diseases (COPD, lower respiratory tract infections, tuberculosis, asthma, type 2 diabetes, Alzheimer’s disease and related dementias, Parkinson’s disease, multiple sclerosis, cataracts, gallbladder diseases, low back pain, peptic ulcer disease, rheumatoid arthritis, macular degeneration and fracture). Definitions of the outcomes are described in Supplementary Table 1 .
Step 1: systematic review approach to literature search and data extraction
Informed by the systematic review approach we took for the GBD 2019 (ref. 30 ), for the present study we identified input studies in the literature using a systematic review approach for all 36 smoking–outcome pairs using updated search strings to identify all relevant studies indexed in PubMed up to 31 May 2022 and extracted data on smoking risk estimates. Briefly, the studies that were extracted represented several types of study design (for example, cohort and case–control studies), measured exposure in several different ways and varied in their choice of reference categories (where some compared current smokers with never smokers, whereas others compared current smokers with nonsmokers or former smokers). All these study characteristics were catalogued systematically and taken into consideration during the modeling part of the analysis.
In addition, for CVD outcomes, we also estimated the age pattern of risk associated with smoking. We applied a systematic review of literature approach for smoking risk for the five CVD outcomes. We developed a search string to search for studies reporting any association between binary smoking status (that is, current, former and ever smokers) and the five CVD outcomes from 1 January 1970 to 31 May 2022, and included only studies reporting age-specific risk (RR, odds ratio (OR), hazard ratio (HR)) of smoking status. The inclusion criteria and results of the systematic review approach are reported in accordance with PRISMA guidelines 31 . Details for each outcome on the search string used in the systematic review approach, refined inclusion and exclusion criteria, data extraction template and PRISMA diagram are given in Supplementary Information 1 . Title and/or abstract screening, full text screening and data extraction were conducted by 14 members of the research team and extracted data underwent manual quality assurance by the research team to verify accuracy.
Selecting exposure categories
Cumulative exposure in pack-years was the measure of exposure used for COPD and all cancer outcomes except for prostate cancer, to reflect the risk of both duration and intensity of current smoking on these outcomes. For prostate cancer, CVDs and all the other outcomes except for fractures, we used cigarette-equivalents smoked per day as the exposure for current smoking, because smoking intensity is generally thought to be more important than duration for these outcomes. For fractures, we used binary exposure, because there were few studies examining intensity or duration of smoking on fractures. The smoking–outcome pairs and the corresponding exposures are summarized in Supplementary Table 4 and are congruent with the GBD 2019 (refs. 30 , 186 ).
Steps 2–5: modeling dose–response RR of smoking on the selected health outcomes
Of the six steps proposed by Zheng et al. 29 , steps 2–5 cover the process of modeling dose–response risk curves. In step 2, we estimated the shape (or the ‘signal’) of the dose–response risk curves, integrating over different exposure ranges. To relax the log(linear) assumption usually applied to continuous dose–response risk and make the estimates robust to the placement of spline knots, we used an ensemble spline approach to fit the functional form of the dose–response relationship. The final ensemble model was a weighted combination of 50 models with random knot placement, with the weight of each model proportional to measures of model fit and total variation. To avoid the influence of extreme data and reduce publication bias, we trimmed 10% of data for each outcome as outliers. We also applied a monotonicity constraint to ensure that the mean risk curves were nondecreasing (or nonincreasing in the case of Parkinson’s disease).
In step 3, following the GRADE approach 192 , 193 , we quantified risk of bias across six domains, namely, representativeness of the study population, exposure, outcome, reverse causation, control for confounding and selection bias. Details about the bias covariates are provided in Supplementary Table 4 . We systematically tested for the effect of bias covariates using metaregression, selected significant bias covariates using the Lasso approach 194 , 195 and adjusted for the selected bias covariates in the final risk curve.
In step 4, we quantified between-study heterogeneity accounting for within-study correlation, uncertainty of the heterogeneity, as well as small number of studies. Specifically, we used a random intercept in the mixed-effects model to account for the within-study correlation and used a study-specific random slope with respect to the ‘signal’ to capture between-study heterogeneity. As between-study heterogeneity can be underestimated or even zero when the number of studies is small 196 , 197 , we used Fisher’s information matrix to estimate the uncertainty of the heterogeneity 198 and incorporated that uncertainty into the final results.
In step 5, in addition to generating funnel plots and visually inspecting for asymmetry (Figs. 1c , 2c , 3c and 4c and Extended Data Fig. 6c ) to identify potential publication bias, we also statistically tested for potential publication or reporting bias using Egger’s regression 199 . We flagged potential publication bias in the data but did not correct for it, which is in line with the general literature 10 , 200 , 201 . Full details about the modeling process have been published elsewhere 29 and model specifications for each outcome are in Supplementary Table 6 .
Step 6: estimating the mean risk function and the BPRF
In the final step, step 6, the metaregression model inclusive of the selected bias covariates from step 3 (for example, the highest adjustment level) was used to predict the mean risk function and its 95% UI, which incorporated the uncertainty of the mean effect, between-study heterogeneity and the uncertainty in the heterogeneity estimate accounting for small numbers of studies. Specifically, 1,000 draws were created for each 0.1 level of doses from 0 pack-years to 100 pack-years or cigarette-equivalents smoked per day using the Bayesian metaregression model. The mean of the 1,000 draws was used to estimate the mean risk at each exposure level, and the 25th and 95th draws were used to estimate the 95% UIs for the mean risk at each exposure level.
The BPRF 29 is a conservative estimate of risk function consistent with the available evidence, correcting for both between-study heterogeneity and systemic biases related to study characteristics. The BPRF is defined as either the 5th (if harmful) or 95th (if protective) quantile curve closest to the line of log(RR) of 0, which defines the null (Figs. 1a , 2b , 3a and 4a ). The BPRF represents the smallest harmful (or protective) effect of smoking on the corresponding outcome at each level of exposure that is consistent with the available evidence. A BPRF opposite null from the mean risk function indicates that insufficient evidence is available to reject null, that is, that there may not be an association between risk and outcome. Likewise, the further the BPRF is from null on the same side of null as the mean risk function, the higher the magnitude and evidence for the relationship. The BPRF can be interpreted as indicating that, even accounting for between-study heterogeneity and its uncertainty, the log(RR) across the studied smoking range is at least as high as the BPRF (or at least as low as the BPRF for a protective risk).
To quantify the strength of the evidence, we calculated the ROS for each smoking–outcome association as the signed value of the log(BPRF) averaged between the 15th and 85th percentiles of observed exposure levels for each outcome. The ROS is a single summary of the effect of smoking on the outcome, with higher positive ROSs corresponding to stronger and more consistent evidence and a higher average effect size of smoking and a negative ROS, suggesting that, based on the available evidence, there is no significant effect of smoking on the outcome after accounting for between-study heterogeneity.
For ease of communication, we further classified each smoking–outcome association into a star rating from 1 to 5. Briefly, 1-star associations have an ROS <0, indicating that there is insufficient evidence to find a significant association between smoking and the selected outcome. We divided the positive ROSs into ranges 0.0–0.14 (2-star), >0.14–0.41 (3-star), >0.41–0.62 (4-star) and >0.62 (5-star). These categories correspond to excess risk ranges for harmful risks of 0–15%, >15–50%, >50–85% and >85%. For protective risks, the ranges of exposure-averaged decreases in risk by star rating are 0–13% (2 stars), >13–34% (3 stars), >34–46% (4 stars) and >46% (5 stars).
Among the 36 smoking–outcome pairs analyzed, smoking fracture was the only binary risk–outcome pair, which was due to limited data on the dose–response risk of smoking on fracture 202 . The estimation of binary risk was simplified because the RR was merely a comparison between current smokers and nonsmokers or never smokers. The concept of ROS for continuous risk can naturally extend to binary risk because the BPRF is still defined as the 5th percentile of the effect size accounting for data uncertainty and between-study heterogeneity. However, binary ROSs must be divided by 2 to make them comparable with continuous ROSs, which were calculated by averaging the risk over the range between the 15th and the 85th percentiles of observed exposure levels. Full details about estimating mean risk functions, BPRFs and ROSs for both continuous and binary risk–outcome pairs can be found elsewhere 29 .
Estimating the age-specific risk function for CVD outcomes
For non-CVD outcomes, we assumed that the risk function was the same for all ages and all sexes, except for breast, cervical and prostate cancer, which were assumed to apply only to females or males, respectively. As the risk of smoking on CVD outcomes is known to attenuate with increasing age 203 , 204 , 205 , 206 , we adopted a four-step approach for GBD 2020 to produce age-specific dose–response risk curves for CVD outcomes.
First, we estimated the reference dose–response risk of smoking for each CVD outcome using dose-specific RR data for each outcome regardless of the age group information. This step was identical to that implemented for the other non-CVD outcomes. Once we had generated the reference curve, we determined the age group associated with it by calculating the weighted mean age across all dose-specific RR data (weighted by the reciprocal of the s.e.m. of each datum). For example, if the weighted mean age of all dose-specific RR data was 56.5, we estimated the age group associated with the reference risk curve to be aged 55–59 years. For cohort studies, the age range associated with the RR estimate was calculated as a mean age at baseline plus the mean/median years of follow-up (if only the maximum years of follow-up were reported, we would halve this value and add it to the mean age at baseline). For case–control studies, the age range associated with the OR estimate was simply the reported mean age at baseline (if mean age was not reported, we used the midpoint of the age range instead).
In the third step, we extracted age group-specific RR data and relevant bias covariates from the studies identified in our systematic review approach of age-specific smoking risk on CVD outcomes, and used MR-BRT to model the age pattern of excess risk (that is, RR-1) of smoking on CVD outcomes with age group-specific excess RR data for all CVD outcomes. We modeled the age pattern of smoking risk on CVDs following the same steps we implemented for modeling dose–response risk curves. In the final model, we included a spline on age, random slope on age by study and the bias covariate encoding exposure definition (that is, current, former and ever smokers), which was picked by the variable selection algorithm 28 , 29 . When predicting the age pattern of the excess risk of smoking on CVD outcomes using the fitted model, we did not include between-study heterogeneity to reduce uncertainty in the prediction.
In the fourth step, we calculated the age attenuation factors of excess risk compared with the reference age group for each CVD outcome as the ratio of the estimated excess risk for each age group to the excess risk for the reference age group. We performed the calculation at the draw level to obtain 1,000 draws of the age attenuation factors for each age group. Once we had estimated the age attenuation factors, we carried out the last step, which consisted of adjusting the risk curve for the reference age group from step 1 using equation (1) to produce the age group-specific risk curves for each CVD outcome:
We implemented the age adjustment at the draw level so that the uncertainty of the age attenuation factors could be naturally incorporated into the final adjusted age-specific RR curves. A PRISMA diagram detailing the systematic review approach, a description of the studies included and the full details about the methods are in Supplementary Information 1.5 and 5.2 .
Estimating the theoretical minimum risk exposure level
The theoretical minimum risk exposure level for smoking was 0, that is, no individuals in the population are current or former smokers.
Model validation
The validity of the meta-analytic tool has been extensively evaluated by Zheng and colleagues using simulation experiments 28 , 29 . For the present study, we conducted two additional sensitivity analyses to examine how the shape of the risk curves was impacted by applying a monotonicity constraint and trimming 10% of data. We present the results of these sensitivity analyses in Supplementary Information 6 . In addition to the sensitivity analyses, the dose–response risk estimates were also validated by plotting the mean risk function along with its 95% UI against both the extracted dose-specific RR data from the studies included and our previous dose–response risk estimates from the GBD 2019 (ref. 30 ). The mean risk functions along with the 95% UIs were validated based on data fit and the level, shape and plausibility of the dose–response risk curves. All curves were validated by all authors and reviewed by an external expert panel, comprising professors with relevant experience from universities including Johns Hopkins University, Karolinska Institute and University of Barcelona; senior scientists working in relevant departments at the WHO and the Center for Disease Control and Prevention (CDC) and directors of nongovernmental organizations such as the Campaign for Tobacco-Free Kids.
Statistical analysis
Analyses were carried out using R v.3.6.3, Python v.3.8 and Stata v.16.
Statistics and reproducibility
The study was a secondary analysis of existing data involving systematic reviews and meta-analyses. No statistical method was used to predetermine sample size. As the study did not involve primary data collection, randomization and blinding, data exclusions were not relevant to the present study, and, as such, no data were excluded and we performed no randomization or blinding. We have made our data and code available to foster reproducibility.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The findings from the present study are supported by data available in the published literature. Data sources and citations for each risk–outcome pair can be downloaded using the ‘download’ button on each risk curve page currently available at https://vizhub.healthdata.org/burden-of-proof . Study characteristics and citations for all input data used in the analyses are also provided in Supplementary Table 3 , and Supplementary Table 2 provides a template of the data collection form.
Code availability
All code used for these analyses is publicly available online ( https://github.com/ihmeuw-msca/burden-of-proof ).
Doll, R. & Hill, A. B. Smoking and carcinoma of the lung. Br. Med. J. 2 , 739–748 (1950).
Article CAS PubMed PubMed Central Google Scholar
Di Cicco, M. E., Ragazzo, V. & Jacinto, T. Mortality in relation to smoking: the British Doctors Study. Breathe 12 , 275–276 (2016).
Article PubMed PubMed Central Google Scholar
World Health Organization. WHO Framework Convention on Tobacco Control 36 (WHO, 2003).
Dai, X., Gakidou, E. & Lopez, A. D. Evolution of the global smoking epidemic over the past half century: strengthening the evidence base for policy action. Tob. Control 31 , 129–137 (2022).
Article PubMed Google Scholar
Dikshit, R. P. & Kanhere, S. Tobacco habits and risk of lung, oropharyngeal and oral cavity cancer: a population-based case-control study in Bhopal, India. Int. J. Epidemiol. 29 , 609–614 (2000).
Article CAS PubMed Google Scholar
Liaw, K. M. & Chen, C. J. Mortality attributable to cigarette smoking in Taiwan: a 12-year follow-up study. Tob. Control 7 , 141–148 (1998).
Gandini, S. et al. Tobacco smoking and cancer: a meta-analysis. Int. J. Cancer 122 , 155–164 (2008).
Deng, X., Yuan, C. & Chang, D. Interactions between single nucleotide polymorphism of SERPINA1 gene and smoking in association with COPD: a case–control study. Int. J. Chron. Obstruct. Pulmon. Dis. 12 , 259–265 (2017).
Leem, A. Y., Park, B., Kim, Y. S., Jung, J. Y. & Won, S. Incidence and risk of chronic obstructive pulmonary disease in a Korean community-based cohort. Int. J. Chron. Obstruct. Pulmon. Dis. 13 , 509–517 (2018).
Forey, B. A., Thornton, A. J. & Lee, P. N. Systematic review with meta-analysis of the epidemiological evidence relating smoking to COPD, chronic bronchitis and emphysema. BMC Pulmon. Med. 11 , 36 (2011).
Article Google Scholar
Tan, J. et al. Smoking, blood pressure, and cardiovascular disease mortality in a large cohort of Chinese men with 15 years follow-up. Int. J. Environ. Res. Public Health 15 , E1026 (2018).
Doll, R., Peto, R., Boreham, J. & Sutherland, I. Mortality in relation to smoking: 50 years’ observations on male British doctors. Br. Med. J. 328 , 1519 (2004).
Huxley, R. R. & Woodward, M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet 378 , 1297–1305 (2011).
Hbejan, K. Smoking effect on ischemic heart disease in young patients. Heart Views 12 , 1–6 (2011).
Chao, H. et al. A meta-analysis of active smoking and risk of meningioma. Tob. Induc. Dis. 19 , 34 (2021).
Shi, H., Shao, X. & Hong, Y. Association between cigarette smoking and the susceptibility of acute myeloid leukemia: a systematic review and meta-analysis. Eur. Rev. Med Pharm. Sci. 23 , 10049–10057 (2019).
CAS Google Scholar
Macacu, A., Autier, P., Boniol, M. & Boyle, P. Active and passive smoking and risk of breast cancer: a meta-analysis. Breast Cancer Res. Treat. 154 , 213–224 (2015).
Pujades-Rodriguez, M. et al. Heterogeneous associations between smoking and a wide range of initial presentations of cardiovascular disease in 1 937 360 people in England: lifetime risks and implications for risk prediction. Int. J. Epidemiol. 44 , 129–141 (2015).
Kanazir, M. et al. Risk factors for hepatocellular carcinoma: a case-control study in Belgrade (Serbia). Tumori 96 , 911–917 (2010).
Pytynia, K. B. et al. Matched-pair analysis of survival of never smokers and ever smokers with squamous cell carcinoma of the head and neck. J. Clin. Oncol. 22 , 3981–3988 (2004).
Barengo, N. C., Antikainen, R., Harald, K. & Jousilahti, P. Smoking and cancer, cardiovascular and total mortality among older adults: the Finrisk Study. Prev. Med. Rep. 14 , 100875 (2019).
Guo, Y. et al. Modifiable risk factors for cognitive impairment in Parkinson’s disease: a systematic review and meta-analysis of prospective cohort studies. Mov. Disord. 34 , 876–883 (2019).
Aune, D., Vatten, L. J. & Boffetta, P. Tobacco smoking and the risk of gallbladder disease. Eur. J. Epidemiol. 31 , 643–653 (2016).
Qin, L., Deng, H.-Y., Chen, S.-J. & Wei, W. Relationship between cigarette smoking and risk of chronic myeloid leukaemia: a meta-analysis of epidemiological studies. Hematology 22 , 193–200 (2017).
Petrick, J. L. et al. Tobacco, alcohol use and risk of hepatocellular carcinoma and intrahepatic cholangiocarcinoma: the Liver Cancer Pooling Project. Br. J. Cancer 118 , 1005–1012 (2018).
United States Department of Health, Education and Welfare. Smoking and Health. Report of the Advisory Committee on Smoking and Health to the Surgeon General of the United States Public Health Service https://www.cdc.gov/tobacco/data_statistics/sgr/index.htm (US DHEW, 1964).
United States Public Health Service Office of the Surgeon General & National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking Cessation: A Report of the Surgeon General . (US Department of Health and Human Services, 2020).
Zheng, P., Barber, R., Sorensen, R. J. D., Murray, C. J. L. & Aravkin, A. Y. Trimmed constrained mixed effects models: formulations and algorithms. J. Comput. Graph Stat. 30 , 544–556 (2021).
Zheng, P. et al. The Burden of Proof studies: assessing the evidence of risk. Nat. Med. in press (2022).
Reitsma, M. B. et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet 397 , 2337–2360 (2021).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Br. Med. J. 339 , b2535 (2009).
Liu, Z. Y., He, X. Z. & Chapman, R. S. Smoking and other risk factors for lung cancer in Xuanwei, China. Int. J. Epidemiol. 20 , 26–31 (1991).
Brownson, R. C., Reif, J. S., Keefe, T. J., Ferguson, S. W. & Pritzl, J. A. Risk factors for adenocarcinoma of the lung. Am. J. Epidemiol. 125 , 25–34 (1987).
Marugame, T. et al. Lung cancer death rates by smoking status: comparison of the Three-Prefecture Cohort study in Japan to the Cancer Prevention Study II in the USA. Cancer Sci. 96 , 120–126 (2005).
Dosemeci, M., Gokmen, I., Unsal, M., Hayes, R. B. & Blair, A. Tobacco, alcohol use, and risks of laryngeal and lung cancer by subsite and histologic type in Turkey. Cancer Causes Control 8 , 729–737 (1997).
Freedman, N. D. et al. Impact of changing US cigarette smoking patterns on incident cancer: risks of 20 smoking-related cancers among the women and men of the NIH-AARP cohort. Int. J. Epidemiol. 45 , 846–856 (2016).
Bae, J.-M. et al. Lung cancer incidence by smoking status in Korean men: 16 years of observations in the Seoul Male Cancer Cohort study. J. Korean Med. Sci. 28 , 636–637 (2013).
Everatt, R., Kuzmickienė, I., Virvičiūtė, D. & Tamošiūnas, A. Cigarette smoking, educational level and total and site-specific cancer: a cohort study in men in Lithuania. Eur. J. Cancer Prev. 23 , 579–586 (2014).
Nordlund, L. A., Carstensen, J. M. & Pershagen, G. Are male and female smokers at equal risk of smoking-related cancer: evidence from a Swedish prospective study. Scand. J. Public Health 27 , 56–62 (1999).
Siemiatycki, J., Krewski, D., Franco, E. & Kaiserman, M. Associations between cigarette smoking and each of 21 types of cancer: a multi-site case–control study. Int. J. Epidemiol. 24 , 504–514 (1995).
Chyou, P. H., Nomura, A. M. & Stemmermann, G. N. A prospective study of the attributable risk of cancer due to cigarette smoking. Am. J. Public Health 82 , 37–40 (1992).
Potter, J. D., Sellers, T. A., Folsom, A. R. & McGovern, P. G. Alcohol, beer, and lung cancer in postmenopausal women. The Iowa Women’s Health Study. Ann. Epidemiol. 2 , 587–595 (1992).
Chyou, P. H., Nomura, A. M., Stemmermann, G. N. & Kato, I. Lung cancer: a prospective study of smoking, occupation, and nutrient intake. Arch. Environ. Health 48 , 69–72 (1993).
Pesch, B. et al. Cigarette smoking and lung cancer–relative risk estimates for the major histological types from a pooled analysis of case–control studies. Int. J. Cancer 131 , 1210–1219 (2012).
Jöckel, K. H. et al. Occupational and environmental hazards associated with lung cancer. Int. J. Epidemiol. 21 , 202–213 (1992).
Jöckel, K. H., Ahrens, W., Jahn, I., Pohlabeln, H. & Bolm-Audorff, U. Occupational risk factors for lung cancer: a case-control study in West Germany. Int. J. Epidemiol. 27 , 549–560 (1998).
Lei, Y. X., Cai, W. C., Chen, Y. Z. & Du, Y. X. Some lifestyle factors in human lung cancer: a case-control study of 792 lung cancer cases. Lung Cancer 14 , S121–S136 (1996).
Pawlega, J., Rachtan, J. & Dyba, T. Evaluation of certain risk factors for lung cancer in Cracow (Poland)—a case–control study. Acta Oncol. 36 , 471–476 (1997).
Mao, Y. et al. Socioeconomic status and lung cancer risk in Canada. Int. J. Epidemiol. 30 , 809–817 (2001).
Barbone, F., Bovenzi, M., Cavallieri, F. & Stanta, G. Cigarette smoking and histologic type of lung cancer in men. Chest 112 , 1474–1479 (1997).
Matos, E., Vilensky, M., Boffetta, P. & Kogevinas, M. Lung cancer and smoking: a case–control study in Buenos Aires, Argentina. Lung Cancer 21 , 155–163 (1998).
Simonato, L. et al. Lung cancer and cigarette smoking in Europe: an update of risk estimates and an assessment of inter-country heterogeneity. Int. J. Cancer 91 , 876–887 (2001).
Risch, H. A. et al. Are female smokers at higher risk for lung cancer than male smokers? A case–control analysis by histologic type. Am. J. Epidemiol. 138 , 281–293 (1993).
Sankaranarayanan, R. et al. A case–control study of diet and lung cancer in Kerala, south India. Int. J. Cancer 58 , 644–649 (1994).
Band, P. R. et al. Identification of occupational cancer risks in British Columbia. Part I: methodology, descriptive results, and analysis of cancer risks, by cigarette smoking categories of 15,463 incident cancer cases. J. Occup. Environ. Med. 41 , 224–232 (1999).
Becher, H., Jöckel, K. H., Timm, J., Wichmann, H. E. & Drescher, K. Smoking cessation and nonsmoking intervals: effect of different smoking patterns on lung cancer risk. Cancer Causes Control 2 , 381–387 (1991).
Brockmöller, J., Kerb, R., Drakoulis, N., Nitz, M. & Roots, I. Genotype and phenotype of glutathione S-transferase class mu isoenzymes mu and psi in lung cancer patients and controls. Cancer Res. 53 , 1004–1011 (1993).
PubMed Google Scholar
Vena, J. E., Byers, T. E., Cookfair, D. & Swanson, M. Occupation and lung cancer risk. An analysis by histologic subtypes. Cancer 56 , 910–917 (1985).
Cascorbi, I. et al. Homozygous rapid arylamine N -acetyltransferase (NAT2) genotype as a susceptibility factor for lung cancer. Cancer Res. 56 , 3961–3966 (1996).
CAS PubMed Google Scholar
Chiazze, L., Watkins, D. K. & Fryar, C. A case–control study of malignant and non-malignant respiratory disease among employees of a fiberglass manufacturing facility. Br. J. Ind. Med 49 , 326–331 (1992).
CAS PubMed PubMed Central Google Scholar
Ando, M. et al. Attributable and absolute risk of lung cancer death by smoking status: findings from the Japan Collaborative Cohort Study. Int. J. Cancer 105 , 249–254 (2003).
De Matteis, S. et al. Are women who smoke at higher risk for lung cancer than men who smoke? Am. J. Epidemiol. 177 , 601–612 (2013).
He, Y. et al. Changes in smoking behavior and subsequent mortality risk during a 35-year follow-up of a cohort in Xi’an, China. Am. J. Epidemiol. 179 , 1060–1070 (2014).
Nishino, Y. et al. Cancer incidence profiles in the Miyagi Cohort Study. J. Epidemiol. 14 , S7–S11 (2004).
Papadopoulos, A. et al. Cigarette smoking and lung cancer in women: results of the French ICARE case–control study. Lung Cancer 74 , 369–377 (2011).
Shimazu, T. et al. Alcohol and risk of lung cancer among Japanese men: data from a large-scale population-based cohort study, the JPHC study. Cancer Causes Control 19 , 1095–1102 (2008).
Tindle, H. A. et al. Lifetime smoking history and risk of lung cancer: results from the Framingham Heart Study. J. Natl Cancer Inst. 110 , 1201–1207 (2018).
PubMed PubMed Central Google Scholar
Yong, L. C. et al. Intake of vitamins E, C, and A and risk of lung cancer. The NHANES I epidemiologic followup study. First National Health and Nutrition Examination Survey. Am. J. Epidemiol. 146 , 231–243 (1997).
Hansen, M. S. et al. Sex differences in risk of smoking-associated lung cancer: results from a cohort of 600,000 Norwegians. Am. J. Epidemiol. 187 , 971–981 (2018).
Boffetta, P. et al. Tobacco smoking as a risk factor of bronchioloalveolar carcinoma of the lung: pooled analysis of seven case-control studies in the International Lung Cancer Consortium (ILCCO). Cancer Causes Control 22 , 73–79 (2011).
Yun, Y. D. et al. Hazard ratio of smoking on lung cancer in Korea according to histological type and gender. Lung 194 , 281–289 (2016).
Suzuki, I. et al. Risk factors for lung cancer in Rio de Janeiro, Brazil: a case–control study. Lung Cancer 11 , 179–190 (1994).
De Stefani, E., Deneo-Pellegrini, H., Carzoglio, J. C., Ronco, A. & Mendilaharsu, M. Dietary nitrosodimethylamine and the risk of lung cancer: a case–control study from Uruguay. Cancer Epidemiol. Biomark. Prev. 5 , 679–682 (1996).
Google Scholar
Kreuzer, M. et al. Risk factors for lung cancer in young adults. Am. J. Epidemiol. 147 , 1028–1037 (1998).
Armadans-Gil, L., Vaqué-Rafart, J., Rosselló, J., Olona, M. & Alseda, M. Cigarette smoking and male lung cancer risk with special regard to type of tobacco. Int. J. Epidemiol. 28 , 614–619 (1999).
Kubík, A. K., Zatloukal, P., Tomásek, L. & Petruzelka, L. Lung cancer risk among Czech women: a case–control study. Prev. Med. 34 , 436–444 (2002).
Rachtan, J. Smoking, passive smoking and lung cancer cell types among women in Poland. Lung Cancer 35 , 129–136 (2002).
Thun, M. J. et al. 50-year trends in smoking-related mortality in the United States. N. Engl. J. Med. 368 , 351–364 (2013).
Zatloukal, P., Kubík, A., Pauk, N., Tomásek, L. & Petruzelka, L. Adenocarcinoma of the lung among women: risk associated with smoking, prior lung disease, diet and menstrual and pregnancy history. Lung Cancer 41 , 283–293 (2003).
Hansen, M. S., Licaj, I., Braaten, T., Lund, E. & Gram, I. T. The fraction of lung cancer attributable to smoking in the Norwegian Women and Cancer (NOWAC) Study. Br. J. Cancer 124 , 658–662 (2021).
Zhang, P. et al. Association of smoking and polygenic risk with the incidence of lung cancer: a prospective cohort study. Br. J. Cancer 126 , 1637–1646 (2022).
Weber, M. F. et al. Cancer incidence and cancer death in relation to tobacco smoking in a population-based Australian cohort study. Int. J. Cancer 149 , 1076–1088 (2021).
Guo, L.-W. et al. A risk prediction model for selecting high-risk population for computed tomography lung cancer screening in China. Lung Cancer 163 , 27–34 (2022).
Mezzoiuso, A. G., Odone, A., Signorelli, C. & Russo, A. G. Association between smoking and cancers among women: results from the FRiCaM multisite cohort study. J. Cancer 12 , 3136–3144 (2021).
Hawrysz, I., Wadolowska, L., Slowinska, M. A., Czerwinska, A. & Golota, J. J. Adherence to prudent and mediterranean dietary patterns is inversely associated with lung cancer in moderate but not heavy male Polish smokers: a case–control study. Nutrients 12 , E3788 (2020).
Huang, C.-C., Lai, C.-Y., Tsai, C.-H., Wang, J.-Y. & Wong, R.-H. Combined effects of cigarette smoking, DNA methyltransferase 3B genetic polymorphism, and DNA damage on lung cancer. BMC Cancer 21 , 1066 (2021).
Viner, B., Barberio, A. M., Haig, T. R., Friedenreich, C. M. & Brenner, D. R. The individual and combined effects of alcohol consumption and cigarette smoking on site-specific cancer risk in a prospective cohort of 26,607 adults: results from Alberta’s Tomorrow Project. Cancer Causes Control 30 , 1313–1326 (2019).
Park, E. Y., Lim, M. K., Park, E., Oh, J.-K. & Lee, D.-H. Relationship between urinary 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol and lung cancer risk in the general population: a community-based prospective cohort study. Front. Oncol. 11 , 611674 (2021).
De Stefani, E., Deneo-Pellegrini, H., Mendilaharsu, M., Carzoglio, J. C. & Ronco, A. Dietary fat and lung cancer: a case–control study in Uruguay. Cancer Causes Control 8 , 913–921 (1997).
Wünsch-Filho, V., Moncau, J. E., Mirabelli, D. & Boffetta, P. Occupational risk factors of lung cancer in São Paulo, Brazil. Scand. J. Work Environ. Health 24 , 118–124 (1998).
Hu, J. et al. A case-control study of diet and lung cancer in northeast China. Int. J. Cancer 71 , 924–931 (1997).
Jia, G., Wen, W., Massion, P. P., Shu, X.-O. & Zheng, W. Incorporating both genetic and tobacco smoking data to identify high-risk smokers for lung cancer screening. Carcinogenesis 42 , 874–879 (2021).
Rusmaully, J. et al. Risk of lung cancer among women in relation to lifetime history of tobacco smoking: a population-based case–control study in France (the WELCA study). BMC Cancer 21 , 711 (2021).
Jin, K. et al. Tobacco smoking modifies the association between hormonal factors and lung cancer occurrence among post-menopausal Chinese women. Transl. Oncol. 12 , 819–827 (2019).
Tse, L. A., Wang, F., Wong, M. C.-S., Au, J. S.-K. & Yu, I. T.-S. Risk assessment and prediction for lung cancer among Hong Kong Chinese men. BMC Cancer 22 , 585 (2022).
Huang, C.-C. et al. Joint effects of cigarette smoking and green tea consumption with miR-29b and DNMT3b mRNA expression in the development of lung cancer. Genes 13 , 836 (2022).
Hosseini, M. et al. Environmental risk factors for lung cancer in Iran: a case–control study. Int. J. Epidemiol. 38 , 989–996 (2009).
Naghibzadeh-Tahami, A. et al. Is opium use associated with an increased risk of lung cancer? A case–control study. BMC Cancer 20 , 807 (2020).
Shimatani, K., Ito, H., Matsuo, K., Tajima, K. & Takezaki, T. Cumulative cigarette tar exposure and lung cancer risk among Japanese smokers. Jpn J. Clin. Oncol. 50 , 1009–1017 (2020).
Lai, C.-Y. et al. Genetic polymorphism of catechol- O -methyltransferase modulates the association of green tea consumption and lung cancer. Eur. J. Cancer Prev. 28 , 316–322 (2019).
Schwartz, A. G. et al. Hormone use, reproductive history, and risk of lung cancer: the Women’s Health Initiative studies. J. Thorac. Oncol. 10 , 1004–1013 (2015).
Kreuzer, M., Gerken, M., Heinrich, J., Kreienbrock, L. & Wichmann, H.-E. Hormonal factors and risk of lung cancer among women? Int. J. Epidemiol. 32 , 263–271 (2003).
Sreeja, L. et al. Possible risk modification by CYP1A1, GSTM1 and GSTT1 gene polymorphisms in lung cancer susceptibility in a South Indian population. J. Hum. Genet. 50 , 618–627 (2005).
Siemiatycki, J. et al. Are the apparent effects of cigarette smoking on lung and bladder cancers due to uncontrolled confounding by occupational exposures? Epidemiology 5 , 57–65 (1994).
Chan-Yeung, M. et al. Risk factors associated with lung cancer in Hong Kong. Lung Cancer 40 , 131–140 (2003).
Lawania, S., Singh, N., Behera, D. & Sharma, S. Xeroderma pigmentosum complementation group D polymorphism toward lung cancer susceptibility survival and response in patients treated with platinum chemotherapy. Future Oncol. 13 , 2645–2665 (2017).
De Stefani, E. et al. Mate drinking and risk of lung cancer in males: a case-control study from Uruguay. Cancer Epidemiol. Biomark. Prev. 5 , 515–519 (1996).
Pérez-Padilla, R. et al. Exposure to biomass smoke and chronic airway disease in Mexican women. A case-control study. Am. J. Respir. Crit. Care Med. 154 , 701–706 (1996).
Zhang, X.-R. et al. Glucosamine use, smoking and risk of incident chronic obstructive pulmonary disease: a large prospective cohort study. Br. J. Nutr . https://doi.org/10.1017/S000711452100372X (2021).
Johannessen, A., Omenaas, E., Bakke, P. & Gulsvik, A. Incidence of GOLD-defined chronic obstructive pulmonary disease in a general adult population. Int. J. Tuberc. Lung Dis. 9 , 926–932 (2005).
Fox, J. Life-style and mortality: a large-scale census-based cohort study in Japan. J. Epidemiol. Community Health 45 , 173 (1991).
Article PubMed Central Google Scholar
Thomson, B. et al. Low-intensity daily smoking and cause-specific mortality in Mexico: prospective study of 150 000 adults. Int. J. Epidemiol. 50 , 955–964 (2021).
van Durme, Y. M. T. A. et al. Prevalence, incidence, and lifetime risk for the development of COPD in the elderly: the Rotterdam study. Chest 135 , 368–377 (2009).
Li, L. et al. SERPINE2 rs16865421 polymorphism is associated with a lower risk of chronic obstructive pulmonary disease in the Uygur population: a case–control study. J. Gene Med. 21 , e3106 (2019).
Ganbold, C. et al. The cumulative effect of gene-gene interactions between GSTM1 , CHRNA3 , CHRNA5 and SOD3 gene polymorphisms combined with smoking on COPD risk. Int. J. Chron. Obstruct. Pulmon. Dis. 16 , 2857–2868 (2021).
Omori, H. et al. Twelve-year cumulative incidence of airflow obstruction among Japanese males. Intern. Med. 50 , 1537–1544 (2011).
Manson, J. E., Ajani, U. A., Liu, S., Nathan, D. M. & Hennekens, C. H. A prospective study of cigarette smoking and the incidence of diabetes mellitus among US male physicians. Am. J. Med. 109 , 538–542 (2000).
Lv, J. et al. Adherence to a healthy lifestyle and the risk of type 2 diabetes in Chinese adults. Int. J. Epidemiol. 46 , 1410–1420 (2017).
Waki, K. et al. Alcohol consumption and other risk factors for self-reported diabetes among middle-aged Japanese: a population-based prospective study in the JPHC study cohort I. Diabet. Med. 22 , 323–331 (2005).
Meisinger, C., Döring, A., Thorand, B. & Löwel, H. Association of cigarette smoking and tar and nicotine intake with development of type 2 diabetes mellitus in men and women from the general population: the MONICA/KORA Augsburg Cohort Study. Diabetologia 49 , 1770–1776 (2006).
Huh, Y. et al. Association of smoking status with the risk of type 2 diabetes among young adults: a nationwide cohort study in South Korea. Nicotine Tob. Res. 24 , 1234–1240 (2022).
Sawada, S. S., Lee, I.-M., Muto, T., Matuszaki, K. & Blair, S. N. Cardiorespiratory fitness and the incidence of type 2 diabetes: prospective study of Japanese men. Diabetes Care 26 , 2918–2922 (2003).
Will, J. C., Galuska, D. A., Ford, E. S., Mokdad, A. & Calle, E. E. Cigarette smoking and diabetes mellitus: evidence of a positive association from a large prospective cohort study. Int. J. Epidemiol. 30 , 540–546 (2001).
Nakanishi, N., Nakamura, K., Matsuo, Y., Suzuki, K. & Tatara, K. Cigarette smoking and risk for impaired fasting glucose and type 2 diabetes in middle-aged Japanese men. Ann. Intern. Med. 133 , 183–191 (2000).
Sairenchi, T. et al. Cigarette smoking and risk of type 2 diabetes mellitus among middle-aged and elderly Japanese men and women. Am. J. Epidemiol. 160 , 158–162 (2004).
Hou, X. et al. Cigarette smoking is associated with a lower prevalence of newly diagnosed diabetes screened by OGTT than non-smoking in Chinese men with normal weight. PLoS ONE 11 , e0149234 (2016).
Hu, F. B. et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N. Engl. J. Med. 345 , 790–797 (2001).
Teratani, T. et al. Dose-response relationship between tobacco or alcohol consumption and the development of diabetes mellitus in Japanese male workers. Drug Alcohol Depend. 125 , 276–282 (2012).
Kawakami, N., Takatsuka, N., Shimizu, H. & Ishibashi, H. Effects of smoking on the incidence of non-insulin-dependent diabetes mellitus. Replication and extension in a Japanese cohort of male employees. Am. J. Epidemiol. 145 , 103–109 (1997).
Patja, K. et al. Effects of smoking, obesity and physical activity on the risk of type 2 diabetes in middle-aged Finnish men and women. J. Intern. Med. 258 , 356–362 (2005).
White, W. B. et al. High-intensity cigarette smoking is associated with incident diabetes mellitus in Black adults: the Jackson Heart Study. J. Am. Heart Assoc. 7 , e007413 (2018).
Uchimoto, S. et al. Impact of cigarette smoking on the incidence of Type 2 diabetes mellitus in middle-aged Japanese men: the Osaka Health Survey. Diabet. Med . 16 , 951–955 (1999).
Rimm, E. B., Chan, J., Stampfer, M. J., Colditz, G. A. & Willett, W. C. Prospective study of cigarette smoking, alcohol use, and the risk of diabetes in men. Br. Med. J. 310 , 555–559 (1995).
Article CAS Google Scholar
Hilawe, E. H. et al. Smoking and diabetes: is the association mediated by adiponectin, leptin, or C-reactive protein? J. Epidemiol. 25 , 99–109 (2015).
InterAct, Consortium et al. Smoking and long-term risk of type 2 diabetes: the EPIC-InterAct study in European populations. Diabetes Care 37 , 3164–3171 (2014).
Jee, S. H., Foong, A. W., Hur, N. W. & Samet, J. M. Smoking and risk for diabetes incidence and mortality in Korean men and women. Diabetes Care 33 , 2567–2572 (2010).
Rasouli, B. et al. Smoking and the risk of LADA: results from a Swedish population-based case-control study. Diabetes Care 39 , 794–800 (2016).
Wannamethee, S. G., Shaper, A. G. & Perry, I. J., British Regional Heart Study. Smoking as a modifiable risk factor for type 2 diabetes in middle-aged men. Diabetes Care 24 , 1590–1595 (2001).
Radzeviciene, L. & Ostrauskas, R. Smoking habits and type 2 diabetes mellitus in women. Women Health 58 , 884–897 (2018).
Carlsson, S., Midthjell, K. & Grill, V., Nord-Trøndelag Study. Smoking is associated with an increased risk of type 2 diabetes but a decreased risk of autoimmune diabetes in adults: an 11-year follow-up of incidence of diabetes in the Nord-Trøndelag study. Diabetologia 47 , 1953–1956 (2004).
Akter, S. et al. Smoking, smoking cessation, and the risk of type 2 diabetes among Japanese adults: Japan Epidemiology Collaboration on Occupational Health Study. PLoS ONE 10 , e0132166 (2015).
Pirie, K. et al. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet 381 , 133–141 (2013).
Park, C.-H. et al. [The effect of smoking status upon occurrence of impaired fasting glucose or type 2 diabetes in Korean men]. J. Prev. Med. Public Health 41 , 249–254 (2008).
Doi, Y. et al. Two risk score models for predicting incident Type 2 diabetes in Japan. Diabet. Med. 29 , 107–114 (2012).
van den Brandt, P. A. A possible dual effect of cigarette smoking on the risk of postmenopausal breast cancer. Eur. J. Epidemiol. 32 , 683–690 (2017).
Dossus, L. et al. Active and passive cigarette smoking and breast cancer risk: results from the EPIC cohort. Int. J. Cancer 134 , 1871–1888 (2014).
Kawai, M., Malone, K. E., Tang, M.-T. C. & Li, C. I. Active smoking and the risk of estrogen receptor-positive and triple-negative breast cancer among women ages 20 to 44 years. Cancer 120 , 1026–1034 (2014).
Reynolds, P. et al. Active smoking, household passive smoking, and breast cancer: evidence from the California Teachers Study. J. Natl Cancer Inst. 96 , 29–37 (2004).
Ellingjord-Dale, M. et al. Alcohol, physical activity, smoking, and breast cancer subtypes in a large, nested case-control study from the Norwegian Breast Cancer Screening Program. Cancer Epidemiol. Biomark. Prev. 26 , 1736–1744 (2017).
Arthur, R. et al. Association between lifestyle, menstrual/reproductive history, and histological factors and risk of breast cancer in women biopsied for benign breast disease. Breast Cancer Res. Treat. 165 , 623–631 (2017).
Luo, J. et al. Association of active and passive smoking with risk of breast cancer among postmenopausal women: a prospective cohort study. Br. Med. J. 342 , d1016 (2011).
White, A. J., D’Aloisio, A. A., Nichols, H. B., DeRoo, L. A. & Sandler, D. P. Breast cancer and exposure to tobacco smoke during potential windows of susceptibility. Cancer Causes Control 28 , 667–675 (2017).
Gram, I. T. et al. Breast cancer risk among women who start smoking as teenagers. Cancer Epidemiol. Biomark. Prev. 14 , 61–66 (2005).
Gammon, M. D. et al. Cigarette smoking and breast cancer risk among young women (United States). Cancer Causes Control 9 , 583–590 (1998).
Magnusson, C., Wedrén, S. & Rosenberg, L. U. Cigarette smoking and breast cancer risk: a population-based study in Sweden. Br. J. Cancer 97 , 1287–1290 (2007).
Chu, S. Y. et al. Cigarette smoking and the risk of breast cancer. Am. J. Epidemiol. 131 , 244–253 (1990).
Lemogne, C. et al. Depression and the risk of cancer: a 15-year follow-up study of the GAZEL cohort. Am. J. Epidemiol. 178 , 1712–1720 (2013).
Morabia, A., Bernstein, M., Héritier, S. & Khatchatrian, N. Relation of breast cancer with passive and active exposure to tobacco smoke. Am. J. Epidemiol. 143 , 918–928 (1996).
Conlon, M. S. C., Johnson, K. C., Bewick, M. A., Lafrenie, R. M. & Donner, A. Smoking (active and passive), N -acetyltransferase 2, and risk of breast cancer. Cancer Epidemiol. 34 , 142–149 (2010).
Ozasa, K., Japan Collaborative Cohort Study for Evaluation of Cancer. Smoking and mortality in the Japan Collaborative Cohort Study for Evaluation of Cancer (JACC). Asian Pac. J. Cancer Prev. 8 , 89–96 (2007).
Jones, M. E., Schoemaker, M. J., Wright, L. B., Ashworth, A. & Swerdlow, A. J. Smoking and risk of breast cancer in the Generations Study cohort. Breast Cancer Res. 19 , 118 (2017).
Bjerkaas, E. et al. Smoking duration before first childbirth: an emerging risk factor for breast cancer? Results from 302,865 Norwegian women. Cancer Causes Control 24 , 1347–1356 (2013).
Gram, I. T., Little, M. A., Lund, E. & Braaten, T. The fraction of breast cancer attributable to smoking: the Norwegian women and cancer study 1991–2012. Br. J. Cancer 115 , 616–623 (2016).
Li, C. I., Malone, K. E. & Daling, J. R. The relationship between various measures of cigarette smoking and risk of breast cancer among older women 65–79 years of age (United States). Cancer Causes Control 16 , 975–985 (2005).
Xue, F., Willett, W. C., Rosner, B. A., Hankinson, S. E. & Michels, K. B. Cigarette smoking and the incidence of breast cancer. Arch. Intern. Med. 171 , 125–133 (2011).
Parker, A. S., Cerhan, J. R., Putnam, S. D., Cantor, K. P. & Lynch, C. F. A cohort study of farming and risk of prostate cancer in Iowa. Epidemiology 10 , 452–455 (1999).
Sawada, N. et al. Alcohol and smoking and subsequent risk of prostate cancer in Japanese men: the Japan Public Health Center-based prospective study. Int. J. Cancer 134 , 971–978 (2014).
Hiatt, R. A., Armstrong, M. A., Klatsky, A. L. & Sidney, S. Alcohol consumption, smoking, and other risk factors and prostate cancer in a large health plan cohort in California (United States). Cancer Causes Control 5 , 66–72 (1994).
Cerhan, J. R. et al. Association of smoking, body mass, and physical activity with risk of prostate cancer in the Iowa 65+ Rural Health Study (United States). Cancer Causes Control 8 , 229–238 (1997).
Watters, J. L., Park, Y., Hollenbeck, A., Schatzkin, A. & Albanes, D. Cigarette smoking and prostate cancer in a prospective US cohort study. Cancer Epidemiol. Biomark. Prev. 18 , 2427–2435 (2009).
Butler, L. M., Wang, R., Wong, A. S., Koh, W.-P. & Yu, M. C. Cigarette smoking and risk of prostate cancer among Singapore Chinese. Cancer Causes Control 20 , 1967–1974 (2009).
Lotufo, P. A., Lee, I. M., Ajani, U. A., Hennekens, C. H. & Manson, J. E. Cigarette smoking and risk of prostate cancer in the physicians’ health study (United States). Int. J. Cancer 87 , 141–144 (2000).
Hsing, A. W. et al. Diet, tobacco use, and fatal prostate cancer: results from the Lutheran Brotherhood Cohort Study. Cancer Res. 50 , 6836–6840 (1990).
Veierød, M. B., Laake, P. & Thelle, D. S. Dietary fat intake and risk of prostate cancer: a prospective study of 25,708 Norwegian men. Int. J. Cancer 73 , 634–638 (1997).
Meyer, J., Rohrmann, S., Bopp, M. & Faeh, D. & Swiss National Cohort Study Group. Impact of smoking and excess body weight on overall and site-specific cancer mortality risk. Cancer Epidemiol. Biomark. Prev . 24 , 1516–1522 (2015).
Putnam, S. D. et al. Lifestyle and anthropometric risk factors for prostate cancer in a cohort of Iowa men. Ann. Epidemiol. 10 , 361–369 (2000).
Taghizadeh, N., Vonk, J. M. & Boezen, H. M. Lifetime smoking history and cause-specific mortality in a cohort study with 43 years of follow-up. PLoS ONE 11 , e0153310 (2016).
Park, S.-Y. et al. Racial/ethnic differences in lifestyle-related factors and prostate cancer risk: the Multiethnic Cohort Study. Cancer Causes Control 26 , 1507–1515 (2015).
Nomura, A. M., Lee, J., Stemmermann, G. N. & Combs, G. F. Serum selenium and subsequent risk of prostate cancer. Cancer Epidemiol. Biomark. Prev. 9 , 883–887 (2000).
Rodriguez, C., Tatham, L. M., Thun, M. J., Calle, E. E. & Heath, C. W. Smoking and fatal prostate cancer in a large cohort of adult men. Am. J. Epidemiol. 145 , 466–475 (1997).
Rohrmann, S. et al. Smoking and risk of fatal prostate cancer in a prospective U.S. study. Urology 69 , 721–725 (2007).
Giovannucci, E. et al. Smoking and risk of total and fatal prostate cancer in United States health professionals. Cancer Epidemiol. Biomark. Prev. 8 , 277–282 (1999).
Rohrmann, S. et al. Smoking and the risk of prostate cancer in the European Prospective Investigation into Cancer and Nutrition. Br. J. Cancer 108 , 708–714 (2013).
Lund Nilsen, T. I., Johnsen, R. & Vatten, L. J. Socio-economic and lifestyle factors associated with the risk of prostate cancer. Br. J. Cancer 82 , 1358–1363 (2000).
Hsing, A. W., McLaughlin, J. K., Hrubec, Z., Blot, W. J. & Fraumeni, J. F. Tobacco use and prostate cancer: 26-year follow-up of US veterans. Am. J. Epidemiol. 133 , 437–441 (1991).
Murray, C. J. L. et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396 , 1223–1249 (2020).
Bero, L. A. & Jadad, A. R. How consumers and policymakers can use systematic reviews for decision making. Ann. Intern. Med. 127 , 37–42 (1997).
Centers for Disease Control and Prevention (CDC). Cigarette smoking among adults and trends in smoking cessation—United States, 2008. MMWR Morb. Mortal. Wkly Rep. 58 , 1227–1232 (2009).
Prochaska, J. O. & Goldstein, M. G. Process of smoking cessation: implications for clinicians. Clin. Chest Med. 12 , 727–735 (1991).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br. Med. J. 372 , n71 (2021).
Stevens, G. A. et al. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. Lancet 388 , e19–e23 (2016).
BMJ Best Practice. What is GRADE? https://bestpractice.bmj.com/info/us/toolkit/learn-ebm/what-is-grade (BMJ, 2021).
The GRADE Working Group. GRADE handbook . https://gdt.gradepro.org/app/handbook/handbook.html (The GRADE Working Group, 2013).
Efron, B., Hastie, T., Johnstone, I. & Tibshirani, R. Least angle regression. Ann. Stat. 32 , 407–499 (2004).
Tibshirani, R. Regression shrinkage and selection via the lasso. J. R. Stat. Soc. Ser. B Stat. Methodol. 58 , 267–288 (1996).
von Hippel, P. T. The heterogeneity statistic I2 can be biased in small meta-analyses. BMC Med. Res. Methodol. 15 , 35 (2015).
Kontopantelis, E., Springate, D. A. & Reeves, D. A re-analysis of the Cochrane Library data: the dangers of unobserved heterogeneity in meta-analyses. PLoS ONE 8 , e69930 (2013).
Biggerstaff, B. J. & Tweedie, R. L. Incorporating variability in estimates of heterogeneity in the random effects model in meta-analysis. Stat. Med. 16 , 753–768 (1997).
Egger, M., Smith, G. D., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. Br. Med. J. 315 , 629–634 (1997).
Lee, P. N., Forey, B. A. & Coombs, K. J. Systematic review with meta-analysis of the epidemiological evidence in the 1900s relating smoking to lung cancer. BMC Cancer 12 , 385 (2012).
Rücker, G., Carpenter, J. R. & Schwarzer, G. Detecting and adjusting for small-study effects in meta-analysis. Biometr. J. 53 , 351–368 (2011).
Wu, Z.-J., Zhao, P., Liu, B. & Yuan, Z.-C. Effect of cigarette smoking on risk of hip fracture in men: a meta-analysis of 14 prospective cohort studies. PLoS ONE 11 , e0168990 (2016).
Thun, M. J. et al. in Cigarette Smoking Behaviour in the United States: changes in cigarette-related disease risks and their implication for prevention and control (eds Burns, D.M. et al.) Tobacco Control Monograph No. 8 Ch. 4 (National Cancer Institute, 1997).
Tolstrup, J. S. et al. Smoking and risk of coronary heart disease in younger, middle-aged, and older adults. Am. J. Public Health 104 , 96–102 (2014).
Jonas, M. A., Oates, J. A., Ockene, J. K. & Hennekens, C. H. Statement on smoking and cardiovascular disease for health care professionals. American Heart Association. Circulation 86 , 1664–1669 (1992).
Khan, S. S. et al. Cigarette smoking and competing risks for fatal and nonfatal cardiovascular disease subtypes across the life course. J. Am. Heart Assoc. 10 , e021751 (2021).
Download references
Acknowledgements
Research reported in this publication was supported by the Bill & Melinda Gates Foundation and Bloomberg Philanthropies. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders. The study funders had no role in study design, data collection, data analysis, data interpretation, writing of the final report or the decision to publish.
We thank the Tobacco Metrics Team Advisory Group for their valuable input and review of the work. The members of the Advisory Group are: P. Allebeck, R. Chandora, J. Drope, M. Eriksen, E. Fernández, H. Gouda, R. Kennedy, D. McGoldrick, L. Pan, K. Schotte, E. Sebrie, J. Soriano, M. Tynan and K. Welding.
Author information
Authors and affiliations.
Institute for Health Metrics and Evaluation, University of Washington, Seattle, WA, USA
Xiaochen Dai, Gabriela F. Gil, Marissa B. Reitsma, Noah S. Ahmad, Jason A. Anderson, Catherine Bisignano, Sinclair Carr, Rachel Feldman, Simon I. Hay, Jiawei He, Vincent Iannucci, Hilary R. Lawlor, Matthew J. Malloy, Laurie B. Marczak, Susan A. McLaughlin, Larissa Morikawa, Erin C. Mullany, Sneha I. Nicholson, Erin M. O’Connell, Chukwuma Okereke, Reed J. D. Sorensen, Joanna Whisnant, Aleksandr Y. Aravkin, Peng Zheng, Christopher J. L. Murray & Emmanuela Gakidou
Department of Health Metrics Sciences, School of Medicine, University of Washington, Seattle, WA, USA
Xiaochen Dai, Simon I. Hay, Jiawei He, Peng Zheng, Christopher J. L. Murray & Emmanuela Gakidou
Department of Applied Mathematics, University of Washington, Seattle, WA, USA
Aleksandr Y. Aravkin
You can also search for this author in PubMed Google Scholar
Contributions
X.D., S.I.H., S.A.M., E.C.M., E.M.O., C.J.L.M. and E.G. managed the estimation or publications process. X.D. and G.F.G. wrote the first draft of the manuscript. X.D. and P.Z. had primary responsibility for applying analytical methods to produce estimates. X.D., G.F.G., N.S.A., J.A.A., S.C., R.F., V.I., M.J.M., L.M., S.I.N., C.O., M.B.R. and J.W. had primary responsibility for seeking, cataloguing, extracting or cleaning data, and for designing or coding figures and tables. X.D., G.F.G., M.B.R., N.S.A., H.R.L., C.O. and J.W. provided data or critical feedback on data sources. X.D., J.H., R.J.D.S., A.Y.A., P.Z., C.J.L.M. and E.G. developed methods or computational machinery. X.D., G.F.G., M.B.R., S.I.H., J.H., R.J.D.S., A.Y.A., P.Z., C.J.L.M. and E.G. provided critical feedback on methods or results. X.D., G.F.G., M.B.R., C.B., S.I.H., L.B.M., S.A.M., A.Y.A. and E.G. drafted the work or revised it critically for important intellectual content. X.D., S.I.H., L.B.M., E.C.M., E.M.O. and E.G. managed the overall research enterprise.
Corresponding author
Correspondence to Xiaochen Dai .
Ethics declarations
Competing interests.
The authors declare no competing interests.

Peer review
Peer review information.
Nature Medicine thanks Frederic Sitas and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editors: Jennifer Sargent and Ming Yang, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended data fig. 1 prisma 2020 flow diagram for an updated systematic review of the smoking and tracheal, bronchus, and lung cancer risk-outcome pair..
The PRISMA flow diagram of an updated systematic review on the relationship between smoking and lung cancer conducted on PubMed to update historical review from previous cycles of the Global Burden of Disease Study. Template is from: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/ .
Extended Data Fig. 2 PRISMA 2020 flow diagram for an updated systematic review of the Smoking and Chronic obstructive pulmonary disease risk-outcome pair.
The PRISMA flow diagram of an updated systematic review on the relationship between smoking and chronic obstructive pulmonary disease conducted on PubMed to update historical review from previous cycles of the Global Burden of Disease Study. Template is from: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/ .
Extended Data Fig. 3 PRISMA 2020 flow diagram for an updated systematic review of the Smoking and Diabetes mellitus type 2 risk- outcome pair.
The PRISMA flow diagram of an updated systematic review on the relationship between smoking and type 2 diabetes conducted on PubMed to update historical review from previous cycles of the Global Burden of Disease Study. Template is from: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/ .
Extended Data Fig. 4 PRISMA 2020 flow diagram for an updated systematic review of the Smoking and Breast cancer risk-outcome pair.
The PRISMA flow diagram of an updated systematic review on the relationship between smoking and breast cancer conducted on PubMed to update historical review from previous cycles of the Global Burden of Disease Study. Template is from: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/ .
Extended Data Fig. 5 PRISMA 2020 flow diagram for an updated systematic review of the Smoking and Prostate cancer risk-outcome pair.
The PRISMA flow diagram of an updated systematic review on the relationship between smoking and prostate cancer conducted on PubMed to update historical review from previous cycles of the Global Burden of Disease Study. Template is from: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/ .
Extended Data Fig. 6 Smoking and Breast Cancer.
a , log-relative risk function. b , relative risk function. c , A modified funnel plot showing the residuals (relative to 0) on the x-axis and the estimated standard deviation (SD) that includes reported SD and between-study heterogeneity on the y-axis.
Supplementary information
Supplementary information.
Supplementary Information 1: Data source identification and assessment. Supplementary Information 2: Data inputs. Supplementary Information 3: Study quality and bias assessment. Supplementary Information 4: The dose–response RR curves and their 95% UIs for all smoking–outcome pairs. Supplementary Information 5: Supplementary methods. Supplementary Information 6: Sensitivity analysis. Supplementary Information 7: Binary smoking–outcome pair. Supplementary Information 8: Risk curve details. Supplementary Information 9: GATHER and PRISMA checklists.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Dai, X., Gil, G.F., Reitsma, M.B. et al. Health effects associated with smoking: a Burden of Proof study. Nat Med 28 , 2045–2055 (2022). https://doi.org/10.1038/s41591-022-01978-x
Download citation
Received : 11 April 2022
Accepted : 28 July 2022
Published : 10 October 2022
Issue Date : October 2022
DOI : https://doi.org/10.1038/s41591-022-01978-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Estimating effects of whole grain consumption on type 2 diabetes, colorectal cancer and cardiovascular disease: a burden of proof study.
Nutrition Journal (2024)
Effects of passive smoking on cortical spreading depolarization in male and female mice
- Tsubasa Takizawa
- Keiko Ihara
- Jin Nakahara
The Journal of Headache and Pain (2024)
Association of cigarette smoking, smoking cessation with the risk of cardiometabolic multimorbidity in the UK Biobank
BMC Public Health (2024)
Health effects associated with chewing tobacco: a Burden of Proof study
- Gabriela F. Gil
- Jason A. Anderson
- Emmanuela Gakidou
Nature Communications (2024)
Probabilistic inference of epigenetic age acceleration from cellular dynamics
- Jan K. Dabrowski
- Emma J. Yang
- Tamir Chandra
Nature Aging (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Cancer newsletter — what matters in cancer research, free to your inbox weekly.
Home — Essay Samples — Nursing & Health — Addictions — Smoking
Essays About Smoking
Smoking essay, types of essay about smoking.
- Cause and Effect Essay: This type of essay focuses on the causes and effects of smoking. It discusses why people start smoking and the consequences of smoking on both the smoker and those around them.
- Argumentative Essay: This essay type aims to persuade the reader about the negative effects of smoking. It presents an argument and provides supporting evidence to convince the reader that smoking is harmful and should be avoided.
- Persuasive Essay: Similar to an argumentative essay, this type of essay aims to persuade the reader to quit smoking. It presents facts, statistics, and other relevant information to convince the reader to stop smoking.
Smoking Essay Example: Cause and Effect
- Identify the causes of smoking: Start by examining why people start smoking in the first place. Is it peer pressure, addiction, stress, or curiosity? Understanding the reasons why people smoke is crucial in creating an effective cause and effect essay.
- Discuss the effects of smoking: Highlight the impact smoking has on an individual's health and the environment. Discuss the risks associated with smoking, such as lung cancer, heart disease, and respiratory problems, and explain how smoking affects non-smokers through secondhand smoke.
- Use reliable sources: To make your essay more convincing, ensure that you use credible sources to back up your claims. Use scientific studies, government reports, and medical journals to support your arguments.
- Provide statistical evidence: Incorporate statistical data to make your essay more impactful. Use figures to show the number of people who smoke, the effects of smoking on the environment, and the costs associated with smoking.
- Offer solutions: Conclude your essay by suggesting solutions to the problem of smoking. Encourage smokers to quit by outlining the benefits of quitting smoking and offering resources for those who want to quit.
Smoking: Argumentative Essay
- Choose a clear position: The writer should choose a side on the issue of smoking, either for or against it, and be clear in presenting their stance.
- Gather evidence: Research and collect facts and statistics to support the writer's argument. They can find data from reliable sources like scientific journals, government reports, and reputable news organizations.
- Address counterarguments: A good argumentative essay will acknowledge opposing viewpoints and then provide a counterargument to refute them.
- Use persuasive language: The writer should use persuasive language to convince the reader of their position. This includes using rhetorical devices, such as ethos, pathos, and logos, to appeal to the reader's emotions and logic.
- Provide a clear conclusion: The writer should summarize the key points of their argument and reiterate their stance in the conclusion.
Persuasive Essay on Smoking
- Identify your audience and their beliefs about smoking.
- Present compelling evidence to support your argument, such as statistics, research studies, and personal anecdotes.
- Use emotional appeals, such as stories or images that show the negative impact of smoking.
- Address potential counterarguments and refute them effectively.
- Use strong and clear language to persuade the reader to take action.
- When choosing a topic for a smoking persuasive essay, consider a specific aspect of smoking that you would like to persuade the audience to act upon.
Hook Examples for Smoking Essays
Anecdotal hook.
Imagine a teenager taking their first puff of a cigarette, unaware of the lifelong addiction they're about to face. This scenario illustrates the pervasive issue of smoking among young people.
Question Hook
Is the pleasure derived from smoking worth the serious health risks it poses? Dive into the contentious debate over tobacco use and its consequences.
Quotation Hook
"Smoking is a habit that drains your money and kills you slowly, one puff after another." — Unknown. Explore the financial and health impacts of smoking in today's society.
Statistical or Factual Hook
Did you know that smoking is responsible for nearly 8 million deaths worldwide each year? Examine the alarming statistics and data associated with tobacco-related illnesses.
Definition Hook
What exactly is smoking, and what are the various forms it takes? Delve into the definitions of smoking, including cigarettes, cigars, pipes, and emerging alternatives like e-cigarettes.
Rhetorical Question Hook
Can we truly call ourselves a smoke-free generation when new nicotine delivery devices are enticing young people? Investigate the impact of vaping and e-cigarettes on the youth.
Historical Hook
Trace the history of smoking, from its ancient roots to its prevalence in different cultures and societies. Explore how perceptions of smoking have evolved over time.
Contrast Hook
Contrast the images of the suave, cigarette-smoking characters from classic films with the grim reality of tobacco-related diseases and addiction in the modern world.
Narrative Hook
Walk in the shoes of a lifelong smoker as they recount their journey from that first cigarette to a battle with addiction and the quest to quit. Their story reflects the struggles of many.
Shocking Statement Hook
Prepare to uncover the disturbing truth about smoking—how it not only harms the smoker but also affects non-smokers through secondhand smoke exposure. It's an issue that goes beyond personal choice.
The Effects of Smoking on Your Body
The effects of smoking on health, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
The Importance of Quitting Smoking
The history of tobacco use and its dangers, the dangers of smoke from cigarettes, a research paper on smoking cigarettes: should society ban it, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Effect of Tobacco: Why Cigarette Smoking Should Be Banned
How smoking can ruin your health, fight addiction with the help willpower, should smoking be made illegal: argumentative, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
Look of Maturity: Why Smoking is "Good" for You
Nevada's smoking freedom at stake as joelle babula argues that local government should enforce strict laws, 500 words on smoking ban: the effects, the challenges of quitting smoking, discussion on whether cigarette smoking should be banned in public places, the motif of smoking in all the pretty horses, the issue of smoking and alcohol drinking among adolescents, my personal experience of the effects of vaping, why vaping is bad for you: effects and dangers, feminist theory and communication, the toxic truth of smoking and vaping, the different harmful effects of smoking marijuana, pieces of advice that will help you to select the best vape shop in las vegas, facts of herbal cigarettes versus tobacco cigarettes, vaping: all you need to know about this trend, from cure to poison: the negative effects of tobacco, global efforts to diminish tobacco usage, the design of the zippo lighter, the detrimental effects of tobacco smoking, tobacco addiction according to bruijnzeel, relevant topics.
- Eating Disorders
- Post Traumatic Stress Disorder
- Affordable Care Act
- Postpartum Depression
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

IMAGES
VIDEO
COMMENTS
Therefore, the current study will investigate both smoking patterns (e.g., frequency, smoking context, and quitting efficacy) and smoking attitudes (e.g., smoking motives, smoker image, and perceived stigma) of
Looking for smoking essay topics? 🚭 Here we've gathered 235 catchy titles for research papers about smoking together with smoking essay examples. 😝 Get inspired with us!
This report focuses on “young people.”. In general, work was reviewed on the health consequences, epidemiology, etiology, reduction, and prevention of tobacco use for those in the young adolescent (11–14 years of age), adolescent (15–17 years of age), and young adult (18–25 years of age) age groups.
This paper reviews the extent and nature of harms caused by smoking, the benefits of stopping, patterns of smoking, psychological, pharmacological and social factors that contribute to uptake and...
Tobacco smoking is a life-threatening addiction that, if untreated, can cause damage to every organ system in the human body. The best way to avoid a tobacco smoking-related illness is never to start smoking, and the next-best way is to stop smoking cigarettes as soon as possible.
Smoking is a serious public health problem because of its close link to health conditions such as lung cancer. Smoking cessation has received significant attention in research that contributes to successful quitting, but not much is known about smokers’ reasons for and experiences of quit attempts.
We identified three outcomes with a 4-star association with smoking: COPD (72% increase in risk based on the BPRF, 0.54 ROS), lower respiratory tract infection (54%, 0.43) and pancreatic cancer...
Background: The smoking rate among young Alaska Native adults (ages 19- 29)in Southeast Alaska is 70% as compared to the statewide adult smoking rate of 21%, the Alaska Native adult rate of 41%, and the overall young adult rate of 32%.
Discuss the effects of smoking: Highlight the impact smoking has on an individual's health and the environment. Discuss the risks associated with smoking, such as lung cancer, heart disease, and respiratory problems, and explain how smoking affects non-smokers through secondhand smoke.
Interventions should aim to target high-risk young adults with poorer psychological health to treat unpleasant psychological symptoms simultaneously with smoking prevention and cessation programs.