Saturday, 2 November
Search for news, browse news stories.
- All opinion
- All featured

Woman jailed over abortion – an explainer on what UK law actually says
This article, written by Claire Pierson , Senior Lecturer in Politics, was originally published in The Conversation:
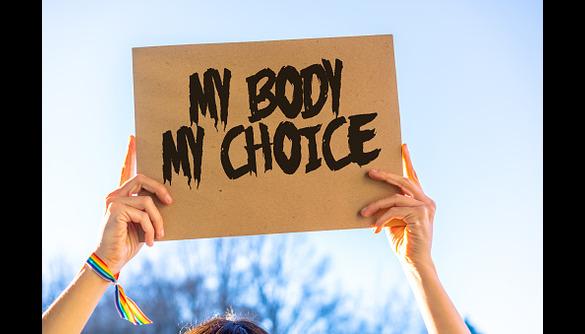
Many people assume that because abortion is relatively accessible in England, it is not a crime. The fact that a woman has now received a 28-month prison sentence for taking abortion pills past the legal time limit shows that this assumption is wrong.
Abortion remains within the criminal law to some extent in almost every country globally, despite the fact that it is a safe and relatively common procedure. Laws can criminalise women and pregnant people, healthcare providers or anyone who helps a woman get an abortion. The sentencing in Poland of activist Justyna Wydrzyńska is one example. In March 2023, she received eight months community service for aiding an abortion seeker.
The 28-month sentence for the 44-year-old mother of three in England reflects the desperate need for a change to the law, in the form of decriminalisation.
In England and Wales, abortion is considered legal when it is performed by a registered medical practitioner, authorised by two doctors and meets certain conditions, such as risk to physical or mental health or risk of fetal anomaly. Abortion can only be performed after 24 weeks gestation in very limited circumstances.
The 1967 Abortion Act determines the situations in which an abortion is not a criminal act and the gestational time limits when one can be performed. The act was written in response to healthcare providers’ concerns about unsafe “backstreet” abortions, rather than out of concern for women’s bodily rights or autonomy.
Lawmakers did not want to make abortion available on request, therefore the sections of the 1861 Offences Against the Person Act which criminalise abortion were not repealed. Sections 58 and 59 make it a criminal offence to administer or supply drugs or use instruments to procure an abortion. The offences carry a maximum sentence of life imprisonment.
While the 1967 Abortion Act applies in Scotland, the Offences Against the Person Act does not. There, abortion is considered a crime in common law, developed by court precedent.
The recent prosecution is not an anomaly. In the past eight years, police in England and Wales have investigated at least 17 people for procuring their own abortion outside the law. The legacy of the 1861 act as a Victorian colonial era law continues to be felt globally, and still applies in countries such as the Gambia, Malawi and Jamaica.
Decriminalising abortion
Northern Ireland is the only region of the UK where abortion is decriminalised . The 1967 act was never extended to Northern Ireland.
After years of activist lobbying and an international inquiry by the UN committee for the elimination of discrimination against women, Westminster repealed sections 58 and 59 of the Offences Against the Person Act in 2019 – but only in Northern Ireland. The Abortion (Northern Ireland) Regulations 2020 now govern abortion access.
But while the law in Northern Ireland is now more liberal, issues remain around access to abortion services. Healthcare providers have had to organise themselves to provide medical abortions, rather than receiving government support and people seeking surgical abortions still have to travel to England.
The World Health Organization (WHO) and international human rights bodies have recommended that, at minimum, abortion be removed from the criminal law and decriminalised around the world.
The WHO defines this as “the complete decriminalisation of abortion for all relevant actors: removing abortion from all penal/criminal laws, not applying other criminal offences (e.g., murder, manslaughter) to abortion, and ensuring there are no criminal penalties for having, assisting with, providing information about or providing abortion”.
This approach recognises that making abortion a crime does not prevent abortion, nor does it protect people from having unsafe abortions. What it does do is impede access and influence how people who have abortions are viewed. Higher levels of stigma are often seen in regions with stricter abortion laws.
This article is republished from The Conversation under a Creative Commons license. Read the original article .
- Expert Opinion
- Featured Opinion
- The Conversation
- University home page
- Department of Politics
- Faculty of Humanities and Social Sciences
- School of Histories Languages and Cultures
London School of Hygiene & Tropical Medicine

The SACHA Study
Creating an evidence base to guide new directions in abortion care in the UK.
The SACHA Study is the largest research project on abortion to be carried out to date in the UK. More than 20 researchers from seven countries have come together forming the SACHA Consortium.
Changes are taking place in the abortion landscape that will impact patients, practitioners and policymakers. Around three in four abortions carried out in the UK are now done by taking pills, and only one in four by surgery. Early medical abortion, involving taking mifepristone and misoprostol, can now be managed as part of routine healthcare in the first 10 weeks of pregnancy.
Recent updates
[email protected] [email protected]
The SACHA Consortium is a large group of practitioners, policymakers and researchers, united by the common aim of ensuring that new directions in abortion care are soundly based on robust empirical evidence. Their expertise encompasses healthcare, including nursing and midwifery, sexual and reproductive health, general practice, commissioning, public health and policy, social science, epidemiology, information technology and the law.
Institutions collaborating on the SACHA Study, led by Prof Kaye Wellings and Dr Rebecca French at the London School of Hygiene and Tropical Medicine, include the British Pregnancy Advisory Service, the Karolinska Institute (Sweden), King's College London, Lambeth Local Authority, University of British Columbia (Canada), University of Edinburgh, University of Kent, University of Melbourne (Australia), University of Oxford and University of Plymouth. Between them, the team members have provided the evidence base for most of the large national sexual and reproductive health interventions in the UK in the last three decades.
Study background
Changes are taking place in the abortion landscape that will impact patients, practitioners and policymakers. Around three in four abortions carried out in the UK are now done by taking pills, and only one in four by surgery. Early medical abortion, involving taking mifepristone and misoprostol, can now be managed as part of routine healthcare in the first 10 weeks of pregnancy. Since 2018, women have been able to take the second abortion pill, misoprostol, at home, and manage the abortion themselves. During nationwide lockdowns, abortion services have mainly been delivered through telemedicine and self-managed by patients, who have been able to administer both pills themselves.
Moves are afoot to change the law on abortion provision. The 1967 Abortion Act in Britain legalised, but did not decriminalise, abortion. It is still a criminal offence to have an abortion unless two doctors have signed to confirm certain conditions have been met. Many are now calling for the law to be changed, arguing that, since the procedure is safer than continuing the pregnancy, it should be governed by healthcare regulations and not the law. Both the UN and the WHO have called for abortion law reform. In Northern Ireland, the law was changed in 2019, so that women and healthcare workers no longer face prosecution if they end a pregnancy without medical approval. The same may well happen in the rest of the UK.
At the same time, the drive for abortion provision to be brought in line with modern healthcare practice is gathering pace. Clinical pathways and models of abortion care being considered reflect the need for patient-centred approaches, shared decision-making and supported self-management - all of which are supported by increasing use of telemedicine and digital resources. Thought is being given to what support is needed by women self-managing abortion and what role can health professionals such as GPs, pharmacists, nurses and midwives play in provision.
The changes could have real benefits. Patients would have more control over what happens to them. Research from other countries has shown that effective, safe and acceptable abortion care can be provided by non-abortion specialist healthcare workers. But reliable evidence is needed to underpin the reforms in the UK. Efforts are being made to develop new ways to improve abortion care in other parts of the world, but more needs to be known before deciding what is the right fit for the UK. The SACHA Study has been funded by the UK's National Institute of Health Research to gather information that will have a direct impact on clinical policy and practice, and will help shape abortion care for the future.

Kaye Wellings
Prof Kaye Wellings is a social scientist and known, nationally and internationally, for her research into sexual and reproductive health. She is Professor of Sexual and Reproductive Health at LSHTM and was founding head of the Centre for Sexual and Reproductive Health Research from 1995 to 2017. Kaye founded the National Survey of Sexual Attitudes and Lifestyles with Natcen in 1987 and co-led the study until 2015. Kaye is an elected Fellow of the UK Faculty of Public Health, the Faculty of Sexual and Reproductive Health, the Royal College of Obstetricians and Gynaecologists and of the Academy of Social Sciences. She sits on a number of advisory committees in Europe and North America, works closely with the WHO, and is a trustee of the Population Council. Co-leading Work Package 4.

Rebecca French
Associate professor.
Dr Rebecca French Associate Professor, LSHTM. Public Health specialist brings experience of public health and policy-related research and evaluation including research in sexual and reproductive health service delivery and use of new technologies. Chair of the RCOG Clinical Studies Group on Sexual & Reproductive Health. Responsible jointly, with Prof Kaye Wellings, for overall management and strategic direction of the study. Co-leading Work Package 3.

Melissa Palmer
Assistant professor.
Dr Melissa Palmer, Assistant Professor at LSHTM. Brings experience of both quantitative and qualitative research, including evaluation of E-Health interventions, analysis of routine data and large-scale survey data. Will contribute across the study to fieldwork, data analysis and reporting. Co-leading Work Package 2.

Rachel Scott
Dr Rachel Scott Assistant Professor at LSHTM. Brings qualitative and quantitative expertise and experience, including comparative research on abortion (Britain vs France; US vs Britain); representations of abortion (West Africa) and an intervention trial of the effect of post-abortion contraceptive counselling. Will contribute across the study to fieldwork, data analysis and reporting. Co-leading Work Package 2.

Rebecca Meiksin
Research fellow.
Rebecca Meiksin Research Fellow in Social Science at LSHTM. Experience of qualitative and quantitative research as well as practice experience in supporting women seeking abortion. Brings experience of conducting qualitative and quantitative systematic reviews and of realist methods. Contributes to study fieldwork, data analysis and reporting.

Maria Lewandowska
Research assistant.
Maria Lewandowska is a Research Assistant in the Department of Public Health, Environments and Society at LSHTM. She completed her MSc in Reproductive and Sexual Health Research at the School and wrote her thesis looking at the impact of the approval of home administration of misoprostol in medical abortions in England, using quantitative methods. Involved in the quantitative and qualitative components of the study.
Natasha Salaria
Natasha Salaria is a Research Assistant in the Department of Public Health, Environments and Society at LSHTM. She completed her MSc in Reproductive Science and Women’s Health at UCL and brings quantitative and qualitative experience along with strategic communications and dissemination of research. Will be involved in the quantitative and qualitative components of the study including fieldwork, data analysis and reporting on Work Packages 3 and 4. Natasha is also a mental health first aider at the School.

Paula Baraitser
Dr Paula Baraitser Consultant in sexual health at King’s College Hospital, Senior Lecturer in Global Health, KCL. Director of community interest company, SH:24. Brings experience in the development and evaluation of sexual health services, particularly online; extensive experience of use of new technologies to improve SRH. Co-leading Work Package 1.


Sharon Cameron
Consultant gynaecologist.
Prof Sharon Cameron Consultant Gynaecologist NHS Lothian & Lead for Abortion Care & Sexual and reproductive Health. Editor in chief BMJ Sexual & Reproductive Health. Brings research experience in conducting and evaluating initiatives to improve women’s SRH, including expansion of health care provision outside existing models of service delivery, self-management of abortion, development of effective methods of follow up after medical abortion and SRH services from community pharmacies. Co-leading Work Package 5.

Caroline Free
Prof Caroline Free Professor of Primary Care and Epidemiology, LSHTM, General Practitioner and Honorary Consultant in SRH at KCH. Brings research and development experience in primary care interventions, particularly M-health and sexual and reproductive health. Co-leading Work Package 1: Realist Review.

Louise Keogh
Prof Louise Keogh Professor, Health Sociology, Melbourne School of Population and Global Health. University of Melbourne. Experienced qualitative researcher who has studied the impact of decriminalisation of abortion in Victoria and has recently received funding to explore a new model for the regulation of conscientious objection to abortion in Australia. Louise will be actively involved in facilitating fieldwork in Australia, in the recruitment of participants, the identification of published and grey literature on abortion in Australia and in carrying out fieldwork.

Patricia Lohr
Medical director.
Dr Patricia Lohr Medical Director, British Pregnancy Advisory Service (BPAS) and Director, Centre for Reproductive Research and Communication. Advisor on abortion education to British Society of Abortion Care Providers and Royal College of Obstetricians and Gynaecologists. Direct clinical abortion service experience and extensive experience of trialling interventions to improve provision. Patricia will advise on all service-related aspects of the study. Co-leading Work Package 4.
Clare Murphy
Chief executive officer.
Clare Murphy Chief Executive Officer at British Pregnancy Advisory Service. In addition to contributing to Work Package 4, Clare will work with the LSHTM lead on dissemination of study findings and public engagement and will manage lay involvement in the study.

Wendy Norman
Dr Wendy Norman Associate Professor, and Public Health Agency of Canada Chair in Family Planning, Faculty of Medicine, University of British Columbia. Family Physician. Brings extensive expertise in innovation approaches to abortion provision and pivotal experience in shaping policy and practice post-decriminalisation in Canada. Wendy will facilitate and guide the fieldwork and desk research in Canada.

Jennifer Reiter
Lead commissioner for sexual health.
Jennifer Reiter is Lead Commissioner for Sexual Health (including abortion services) at London Borough of Lambeth. She has also commissioned sexual and reproductive health services for London Borough of Camden and HIV Prevention England. In the UK she previously served as Secretary for Abortion Support Network. In the US she delivered education, outreach and training for Planned Parenthood chapters in Wisconsin and Illinois. For the SACHA study, she will provide guidance into the commissioning of services and will facilitate the participation of commissioners in the study and enlist their support in disseminating the outputs. Co-leading Work Package 5.

Sally Sheldon
Prof Sally Sheldon Professor of Law at Kent Law School. Brings health care law and ethics, with specific reference to reproductive health/abortion. Sally will provide the necessary perspectives on legal aspects of abortion provision across the study. Co-leading Work Package 5.

Prof Jill Shawe Professor of Maternal and Family Health School of Nursing & Midwifery, University of Plymouth. Sexual & Reproductive Health Nurse and Midwife. Brings experience of research into women’s health care and the role of nurse/midwife in sexual and reproductive health and inequalities in access. Co-leading Work Package 3.

Dr Geoff Wong Associate Professor in Primary Care at the Nuffield Department of Primary Care Health Sciences, University of Oxford and GP in London. Brings extensive expertise in realist synthesis and its application to understand implementation to complex health and social interventions.
The SACHA Study is the largest research project on abortion to be carried out to date in the UK. More than 20 researchers from seven countries have come together forming the SACHA Consortium with the aim of building a comprehensive evidence base for new directions in abortion care. Five interlinked work packages make up the study:
- Reviews of existing evidence on novel models of abortion care that are being tried and tested;
- Case studies capturing the experience of abortion provision reforms in Australia, Canada, and Sweden, and transferrable lessons to be learnt for the UK.
- A survey of health care practitioners such as GPs, midwives, nurses and pharmacists, to assess the potential for extending their role in abortion provision;
- In-depth interviews with women with recent experience of abortion to find out how best abortion services might be organised to meet their needs and preferences for different models of care;
- Roundtable discussion groups with key stakeholders to examine which innovations in abortion care would be most likely to work in the UK.
The study findings will be tailored to different audiences - the general public, the media, healthcare professionals, academics, policymakers and commissioners.
Items in the media citing SACHA:
- Major UK study recommends extending abortion powers to nurses (Nursing Times)
- UK abortion law should change to reflect current practice, study suggests (Medical Xpress)
- NHS nurses and midwives should be able to approve abortions, report argues (Yahoo News)
- Nurses and midwives should be able to approve abortions, UK study concludes (The Guardian)
- Need for two doctors to approve abortion ‘should be scrapped' (Irish News)
- Everything you need to know about having an abortion, according to a reproductive health expert (Glamour Magazine)
- Abortion is safe, supported, and available in the UK. Why is the law so complicated? (The Guardian)
- Scotland 'must act quickly' on abortion services as new study shows women 'overwhelmingly support' telemedicine provisions (The Scotsman)
- Women support home-use of abortion pills and telemedical model of care (News-Medical.Net)
- Scotland urged to continue at-home abortions (BBC)
We presented the findings of the SACHA Study at the All-Parliamentary Party Group on Sexual and Reproductive Health on the 7th of March 2023.
Our team presented the following research at the conference of the International Federation of Abortion and Contraception Professionals in September 2022: - COVID-19: abortion and contraception - impetus or impediment? Wellings Kaye, London School of Hygiene & Tropical Medicine, Public Health and Policy, London, UK,SACHA Consortium, LSHTM, London, UK. - Decriminalising abortion in Britain: what do patients and providers think? French RS, Salaria N, Lewandowska M, Meiksin R, Palmer M, Scott R, Lohr PA, Shawe J, Wellings K,The SACHA Study Team. London School of Hygiene & Tropical Medicine, Department of Public Health, Environments and Society, Faculty of Public Health and Policy, London, UK. - Perceptions of stigma among women receiving abortion care in Britain. Dr Rachel Scott, LSHTM, London, United Kingdom; Maria Lewandowska, LSHTM, London, United Kingdom; Dr Patricia Lohr, British Pregnancy Advisory Service, London, United Kingdom; Rebecca Meiksin, LSHTM, London, United Kingdom; Jennifer Reiter, Lambeth Council, London, United Kingdom; Dr Rebecca French, LSHTM, London, United Kingdom; Dr Melissa Palmer, LSHTM, London, United Kingdom; Professor Kaye Wellings, LSHTM, London, United Kingdom.
Read more about our research at the conference.
The results of the first research paper published by SACHA, based on qualitative interviews with women with recent experience of abortion, presented by Maria Lewandowska at the conference of the European Society of Contraception and Reproductive Health , May 2022.
- Share full article
Advertisement
Supported by
U.K. Woman Sentenced to Prison for Abortion in Eighth Month of Pregnancy
The case has prompted heated debate in England, with some arguing that abortion pills should not be available by mail and others maintaining that abortion should be fully decriminalized.

By Emma Bubola
Reporting from London
A woman’s sentencing to prison this week for illegally using abortion pills to end a 32- to 34-week pregnancy is prompting a debate in England over the state of its abortion laws and whether a woman should ever be prosecuted for the procedure.
Adding to the debate is the fact that she was prosecuted under a law more than 160 years old. Some say that the law is too draconian, while others say the case illustrates the dangers of allowing abortion pills to be sent by mail.
What happened in the case?
On Monday, a court in Stoke-on-Trent, a city in central England, sentenced Carla Foster, 44, to 28 months for having caused her own miscarriage by taking abortion pills when she was in her eighth month of pregnancy.
The sentence includes up to 14 months in prison, after which she could serve the rest of her term on release if she meets certain conditions.
In early 2020, during the coronavirus pandemic, Ms. Foster, a mother of three, had moved back in with her long-term but estranged partner after becoming pregnant by another man, according to court documents.
The judge, Edward Brian Pepperall, wrote in his sentencing remarks that Ms. Foster had been in emotional turmoil as she sought to hide the pregnancy. She also repeatedly searched online for information about how to terminate her pregnancy in the first months of 2020, according to the judge.
That May, she obtained abortion drugs by mail after giving false information to Britain’s pregnancy advisory service, the judge wrote. Although abortion pills are available by mail through the service in the first 10 weeks of pregnancy, Ms. Foster’s internet searches indicated that she knew she was more than 24 weeks pregnant, the legal limit for most abortions, the court documents said.
Shortly after she took the drugs, her pregnancy ended in a stillbirth, according to the court. Paramedics were on the scene, and Ms. Foster told them that she understood that she would be required to speak to the police.
A post-mortem examination confirmed that the pregnancy was between 32 and 34 weeks, the judge wrote. A full-term pregnancy is about 40 weeks, or nine months.
Ms. Foster initially pleaded not guilty, but this March she pleaded guilty to a charge of “administering poison with intent to procure a miscarriage.”
The judge wrote in his decision that Ms. Foster was a good mother to her three children, including one with special needs, and he acknowledged that they would suffer from their mother’s imprisonment.
In handing down the sentence, the judge wrote, “The balance struck by the law between a woman’s reproductive rights and the rights of her unborn fetus is an emotive and often controversial issue.”
What are England’s abortion laws?
Abortion has been legal in England, Scotland and Wales since the Abortion Act of 1967, and access to the procedure is generally liberal, experts said.
Abortions are allowed in the first 24 weeks of pregnancy and must be approved by two doctors.
In the first 10 weeks, women can get an abortion by having two drugs prescribed to them, which in earlier years would have typically required a visit to a clinic. During the pandemic, when securing in-person services became both difficult and dangerous, the British government ruled that the drugs could be provided without an in-person appointment.
That decision was made permanent last August.
Later-term abortions are allowed in some exceptional cases, including when the woman’s health is in danger or in some cases of fetal abnormality.
Yet when Parliament passed the 1967 legislation allowing for abortions, it did not repeal an earlier law that had criminalized them. In rare cases, therefore, abortion can still be prosecuted as a criminal act.
Under a law passed in 1861, any woman who takes “poison” with an intent to cause her own fetus’s miscarriage “shall be guilty of felony” and liable “to be kept in penal servitude for life.”
That was the law under which Ms. Foster was sentenced, and hers is not an isolated case.
In his ruling, Judge Pepperall cited a 2013 decision in which a British court sentenced a woman to three and a half years in prison for causing her own miscarriage while about 38 weeks pregnant. And Stella Creasy, a lawmaker in the opposition Labour Party, said on BBC Two’s “Newsnight” current-affairs show on Monday that there had been 67 investigations under the 1861 act in the past decade.
What were the calls for decriminalization?
Caroline Nokes, a lawmaker in the governing Conservative Party who chairs the Women and Equalities Committee in the House of Commons, told the BBC after the court’s ruling that England was “relying on legislation that is very out of date.”
She said the sentencing “makes a case for Parliament to start looking at this issue in detail.”
Louise McCudden, the head of external affairs at MSI Reproductive Choices, a Britain-based women’s health organization, said in an interview that even if prosecution was rare, the law must be changed.
“Any case is too many,” she said.
Ms. Creasy, the Labour lawmaker, told BBC Two’s “Newsnight” that “Abortion is a health care issue, not a criminal matter.”
What were the calls for tighter rules?
Groups that campaign against abortion argued that the case illustrated the tragic consequences of the government’s decision to allow abortion pills to be sent by mail. They also said that Parliament should act based on the case, by further restricting the procedure.
“The government should urgently turn back the clock and end this disastrous policy of cheap, convenient, pills-by-post abortions,” Andrea Williams, the chief executive of Christian Concern, an advocacy group, said in a statement.
“At 32 weeks’ gestation, an unborn baby has a 95 percent chance of survival if delivered,” she added. “Our abortion law rightly recognizes that these precious humans deserve protection.”
James Mumford, an author who studies political theology, modern Catholic social thought, and bioethics , told BBC Two’s “Newsnight” on Monday that England had an “extreme abortion-on-demand culture.”
He called Ms. Foster’s case a natural consequence of making abortion pills available by mail, which he called an “utter disaster.”
What did medical experts say?
Some medical professionals also lobbied against sending Ms. Foster to prison, a penalty that they said might discourage other women from seeking access to abortion pills at home.
The court said it had received a letter from the president of the Royal College of Obstetricians and Gynecologists as well as other medical bodies urging a noncustodial sentence.
The judge responded that it was inappropriate for medical professionals to send such a letter, and that if they disagreed with the law, they should lobby Parliament to change it rather than judges who are charged with applying it.
Emma Bubola is a reporter based in London. More about Emma Bubola

IMAGES
VIDEO