The Role of Diversity in Healthcare Essay
I see the role of diversity and the inclusiveness of diverse groups in healthcare as very important. Medical institutions need to aim to increase diversity, as represented by the workforce, with people of different socio-economic backgrounds, ethnicities, races, religions, cultures, genders, and sexual orientations. This has a positive impact not only on the organization but on individual patients and the community as a whole. The healthcare team needs to be as diverse as the patients who provide the service. This creates a feeling of inclusiveness both among patients and employees.
I am a female, first-generation African-American studying healthcare. Both of my parents are immigrants, who moved to the United States, and we are an average-income family. My race makes me a part of a diverse group, which I am quite proud of. I believe that my achievements, both personal and professional, could contribute not only to the improvement of a specific subject area but also to the situation with diversity in modern society.
Based on my prior experience, I could say that if a patient obtains a feeling of community and has a healthcare provider who identifies with them, the experience that the patient is going through will be more pleasant for them. When I had a work experience as a nurse, there was an old black woman that was very scared and stressed because of her diagnosis; she spoke in an African dialect, which is why she sometimes had difficulties explaining her needs. Her stress level negatively influenced her health conditions and treatment outcome. I decided to help to take care of her, after which she expressed very much gratitude for me and said that I gave her a feeling of trust. I was able to explain some of the things she could not explain to my colleagues because of the language barrier. I believe that there are many cases like this where patients need more understanding and support from people of the same group. Lack of diversity can lead to disruption of communication with patients due to differences and even cultural prejudices. Serious errors can occur if the patient is unable to speak sufficiently or express their needs.
The experience that I have gone through has greatly contributed to shaping my understanding of diversity and gave me a notion of how I could implement elements of diversity in my future work. In my future career, I would like to improve the healthcare management system in the context of the inclusion of different minority groups. I intend to improve the recruitment system and facilitate the inclusion of more talented professionals from diverse racial, ethical, and gender groups. I think that such an approach will, firstly, solve the problem of communication breakdown, such as a language barrier. Secondly, it will create a feeling of safety and support for the patients from the same diverse groups as healthcare providers. I believe that their positive emotions and calmness play a paramount role in the quality of service and care results.
- Investigation of the Causes of Salmonella
- Overworking and Work-Related Health Problems
- The Role of Negotiation Process in Disputed Situations
- Intellectual Disability and Inclusiveness
- Transition Experiences of First-Generation Latino Veterans
- The Simple Power of Hand-Washing
- Individual Right Versus the Collective Good
- The Role of Virtual Clinics During the COVID-19 Pandemic in Saudi Arabia
- Problem of Patients' Follow-Up Appointments
- UK Health and Social Care Using Related Laws
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, December 24). The Role of Diversity in Healthcare. https://ivypanda.com/essays/the-role-of-diversity-in-healthcare/
"The Role of Diversity in Healthcare." IvyPanda , 24 Dec. 2022, ivypanda.com/essays/the-role-of-diversity-in-healthcare/.
IvyPanda . (2022) 'The Role of Diversity in Healthcare'. 24 December.
IvyPanda . 2022. "The Role of Diversity in Healthcare." December 24, 2022. https://ivypanda.com/essays/the-role-of-diversity-in-healthcare/.
1. IvyPanda . "The Role of Diversity in Healthcare." December 24, 2022. https://ivypanda.com/essays/the-role-of-diversity-in-healthcare/.
Bibliography
IvyPanda . "The Role of Diversity in Healthcare." December 24, 2022. https://ivypanda.com/essays/the-role-of-diversity-in-healthcare/.
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
IvyPanda uses cookies and similar technologies to enhance your experience, enabling functionalities such as:
- Basic site functions
- Ensuring secure, safe transactions
- Secure account login
- Remembering account, browser, and regional preferences
- Remembering privacy and security settings
- Analyzing site traffic and usage
- Personalized search, content, and recommendations
- Displaying relevant, targeted ads on and off IvyPanda
Please refer to IvyPanda's Cookies Policy and Privacy Policy for detailed information.
Certain technologies we use are essential for critical functions such as security and site integrity, account authentication, security and privacy preferences, internal site usage and maintenance data, and ensuring the site operates correctly for browsing and transactions.
Cookies and similar technologies are used to enhance your experience by:
- Remembering general and regional preferences
- Personalizing content, search, recommendations, and offers
Some functions, such as personalized recommendations, account preferences, or localization, may not work correctly without these technologies. For more details, please refer to IvyPanda's Cookies Policy .
To enable personalized advertising (such as interest-based ads), we may share your data with our marketing and advertising partners using cookies and other technologies. These partners may have their own information collected about you. Turning off the personalized advertising setting won't stop you from seeing IvyPanda ads, but it may make the ads you see less relevant or more repetitive.
Personalized advertising may be considered a "sale" or "sharing" of the information under California and other state privacy laws, and you may have the right to opt out. Turning off personalized advertising allows you to exercise your right to opt out. Learn more in IvyPanda's Cookies Policy and Privacy Policy .

- DEI Calendar
- Testimonials
- Integration
- Success Stories
- Unconscious Bias
- Microaggressions
- Diversity Calendar 2024
- Interfaith Calendar 2024
- Awareness Months 2024
- Heritage Months
- Try for Free

Why Is Diversity Important in Healthcare?

Are you questioning why is diversity important in healthcare? Learn about the benefits of healthcare diversity and how to promote it.
Diversity is important for delivering effective healthcare. Research shows that patients are more likely to trust healthcare providers who reflect their own backgrounds. This trust leads to better communication and a higher likelihood that patients will follow their treatment plans, ultimately resulting in improved health outcomes.
Diversity in healthcare provides high-quality care for everyone by acknowledging and respecting diverse cultures, religious beliefs, genders, and socioeconomic statuses. It also empowers every patient and healthcare professional to have a voice in the type of care they receive and need.

- Celebrate Healthcare Observances
- Awareness Months, Events
- Schedule Quickly & Respectfully
- Add to Outlook, Sharepoint, etc
- Get Education Tool and Tips
- Avoid Bad PR & Lawsuits
Understanding Cultural Competence in Healthcare
While recognizing our differences is important, practicing cultural competence in healthcare is a priority. Mirroring the demographics of the community you serve can increase workplace morale and enhance the quality of care provided.
Hire employees from different backgrounds to ensure that every visitor to your facility can be treated by someone they identify with and can communicate easily with. This diversity fosters creative solutions and effective problem-solving.
What Is Diversity in Healthcare?
People from all races, religions, ethnicities, sexual orientations, abilities, genders, and ages require different medical care. Supporting diversity in healthcare leads to the ability to offer medical services that meet the specific needs of each patient. The more patients feel understood and represented, the better the care and outcomes they receive.
Benefits of Healthcare Diversity
Diversity in the workplace offers many benefits for all workplaces, including healthcare. These benefits include:
- Boosted Morale: Create a sense of inclusion and belonging that makes your workplace more enjoyable.
- Better Care: Hire a diverse team. This allows everyone who walks through your door to receive care from someone they feel comfortable with.
- Higher Retention: Foster a positive work culture that values happy employees. The happier healthcare workers feel, the longer they will want to stay.
- Improved Recruitment: Commit to making your healthcare workplace more diverse by recruiting new talent with the same DEI mindset.
How to Best Promote Diversity in Healthcare
While HR departments carry most of the responsibility for establishing diversity, healthcare workers can also contribute significantly.
Create an Accepting and Welcoming Work Environment
Establish a positive work culture where all voices are heard and respected and coworkers feel safe sharing their unique perspectives.
Address Bias Openly
Support your staff by having an open-door policy where employees can freely share their experiences. Victims of discrimination or bias don’t want to come forward for fear of retaliation. Supporting coworkers who experience this and being transparent about incidents helps create this safe place too.
Have Inclusive Job Descriptions
Encourage diverse applicants for your healthcare jobs by writing inclusive job descriptions that include your company’s mission statement and DEI commitment.
Participate in Diversity Training
Building diversity training requirements into your hiring and HR departments. Diversity training increases understanding, teaches staff how to respond to these differences, identifies bias, discrimination, or other workplace barriers, and improves communication.
Try Healthcare DEI Training Today
If you’re questioning why is diversity important in healthcare, our Healthcare DEI Training can help you and your team with factors you should consider for your workplace. Ensuring your healthcare team reflects diverse backgrounds can significantly improve patient care.
Discover more with our Healthcare Calendar 2024 and Healthcare Calendar 2025 for healthcare events , health awareness months, and healthcare observances all year long. Our Healthcare Diversity Training can empower your staff and help you create an inclusive workplace that supports diversity and inclusion. Read about medical awareness months 2024 for more education.
Why is diversity in healthcare important?
Promoting diversity in health care is vital as it offers countless patient benefits, including improved and optimized care, reduced care disparities, and improved access to care. This is especially important for adults who, because of their age, illness, or disability, cannot entirely independently take care of themselves.
Why is promoting diversity important in health and social care?
Good equality and diversity practices help ensure that access to services is fair and accessible to all. They treat all people as equals and focus on giving patients the dignity and respect they deserve with customized care. Cultural competence includes attitudes and policies that promote equitable services in healthcare facilities.
Why is cultural diversity in healthcare crucial?
Cultural respect helps reduce health disparities by improving access to high-quality healthcare and social care services. It is respectful of the needs of diverse patients. It can accurately and steadfastly treat people with all conditions and disorders to have a good quality of life while managing their health conditions.
Popular Diversity Calendar
- Global Diversity Calendar 2025
- Diversity Calendar Updates
- June Awareness Months 2025
- May Awareness Months 2025
- April Awareness Months 2025
Popular Diversity Training
- Implicit Bias in Healthcare: How DEI Training Can Help
- Diversity and Inclusion Training: Why It Matters
- Diversity and Inclusion Training for Leaders
- Best Topics for Diversity Training
- 5 Types of Diversity Training in the Workplace
Popular Diversity Insights
- How Inclusion Can Improve Your Business
- The Cost of Not Being Inclusive
- DEI Initiatives: Leveling Up Your Approach for Lasting Change
- Controversial Discussion Topics in a Diverse Workplace
- Inclusive Practices for Remote Teams
Diversity Newsletter
Join our thriving community of 15,000+ subscribers! Explore exclusive tools, tips, techniques & more!"
- Full Name *
- Diversity Calendar
- Online Diversity Training
- Client Testimonials
Legal Information
- HTML site-map
- XML site-map
- Privacy Policy
- Terms of Service
- DEI Insights
Diversity Resources

© 2024, DiversityResources.com Inc.

Privacy Overview
- Online Training
Don’t miss our webinar! Learn how to be a better ally using the Diversity Calendar. Register Now

Pricing is by number of employees
- How many employees would you like to train, please? *
Please fill Your detail.
Sign in to Diversity Resources
- Forgot password
Home — Essay Samples — Social Issues — Diversity — Diversity in Nursing: A Critical Analysis
Diversity in Nursing: a Critical Analysis
- Categories: Diversity
About this sample

Words: 879 |
Published: Sep 12, 2023
Words: 879 | Pages: 2 | 5 min read
Table of contents
Recruitment: fostering a diverse nursing workforce, cultural competence: navigating a diverse patient population, patient care: the impact of diversity on health outcomes.

Cite this Essay
To export a reference to this article please select a referencing style below:
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof Ernest (PhD)
Verified writer
- Expert in: Social Issues

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 384 words
1 pages / 617 words
4 pages / 1973 words
2 pages / 1090 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Diversity
Our culture molds us, molds our behavior, and our sense of self. Our way of life is defined by the shared language, ideas, values, conventions, behaviors, and material items that are passed down from generation to generation. We [...]
Diversity comes in numerous forms such as gender, race, age, sexual orientation, cultural, and a lot more. The Army’s definition of diversity is the different attributes, experiences, and backgrounds of our Soldiers, civilians [...]
Culture and diversity play a significant role in healthcare delivery and outcomes. In order to provide high-quality care to patients from various cultural backgrounds, it is crucial for healthcare professionals to understand the [...]
In conclusion, "Deaf Like Me" is a testament to the power of communication, understanding, and empathy. Through their personal journey, the Spradleys invite us to reflect on the challenges faced by the Deaf community and [...]
Education is a dynamic field where educators strive to make a profound impact on children's lives, shaping their futures and fostering inclusive learning environments. Within this context, the concept of diversity in the [...]
The debate over importance of workplace diversity is not new. It has been in discussion for last 6 decades. Many researchers, academicians, human resource professionals and entrepreneurs have debated about its benefits, [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

– Medical School Blog
The Importance of Diversity in Health Care: Medical Professionals Weigh In

To provide the best possible care for all patients and help minimize racial disparities, medical professionals need to acknowledge and recognize differences among varying populations. Diversity among physicians—pertaining to socioeconomic status, race, gender identity, and so on—is key. Many physicians already recognize that a commitment to diversity is critical, yet there is still progress to be made.
To learn more about diversity in health care from the inside out, take a look at what some physicians have to say on the topic.
Exploring diversity in medicine so far
By looking at the statistics in the chart below, the medical field is still primarily white males with a smaller contingent of of females and other ethnic groups. It’s pretty clear that the medical field has a long way to go.

“Diversity in Medicine: Facts and Figures 2019” from the Association of American Medical Colleges (AAMC) touches on gender distribution among doctors , revealing that nearly two-thirds of physicians are male. However, that figure may even out over time. AAMC data comparing applicants and enrolled medical students by sex shows that females now outnumber males in US medical schools.
The same report also includes a breakdown of active physicians by race and ethnicity , which shows that more than half of practicing physicians are white, 17 percent are Asian, 6 percent are Hispanic, and 5 percent are Black. This is something that comes as no surprise to Dr. Antonio Webb, an orthopedic spine surgeon, who notes that one AAMC report found there were fewer Black male medical students in 2014 than there were in 1978. He says that when he was a child, he didn’t know any doctors who looked like him.
“My parents weren’t physicians, and I didn’t really have any mentors,” he recalls. “I kind of carved my own path—there was no YouTube back then.”
Additionally, the majority of medical students come from affluent, higher socioeconomic status backgrounds. According to An Updated Look at the Economic Diversity of U.S. Medical Students from the AAMC, more than 75 percent of medical students are from families who are in the top two quintiles for household income as identified by US census data.
While research on sexual and gender orientation as well as religious affiliation among physicians is limited, diversity in these realms is also important for developing good bedside manner and providing quality care.
How diversity in health care benefits patients
A lack of diversity in the workforce limits the capabilities of medicine, containing it within a single ethnic lens and a particular set of values. The medical workforce should instead reflect the variety of patients for which they provide care.
“It is important for physicians to be diverse in large part because our patients are diverse,” explains Dr. Lisa Doggett, a family physician. “If we can understand our patients’ belief systems and values, we will be able to provide better care for them.”
For instance, patients’ religious beliefs can similarly affect the quality of care they receive. A recent paper on cultural competence in medicine reveals the many ways in which an individual’s beliefs can affect them as a patient. Additionally, the medical research community acknowledges that health disparities among LGTBQ individuals are a significant issue. Just consider this reflection from one transgender patient.
“The more diverse the people are who provide medical care, the better they can respectfully and knowledgeably assist their patients.”
“As a transgender person, it’s very difficult to access health care with competent providers knowledgeable about transgender health care,” explains Jordan Rubenstein of Ellevest . “The more diverse the people are who provide medical care, the better they can respectfully and knowledgeably assist their patients.”

When a patient cannot find providers that resemble them, their beliefs, their culture, or other facets of their life, they run the risk of not being understood or being able to receive the appropriate treatment. One clear example of this is the extreme divide in health outcomes for expecting mothers based on race. The Centers for Disease Control and Prevention (CDC) reveals Black and native women are two to three times more likely to die of pregnancy complications than white women.
A more diverse physician workforce also makes needed care more accessible to patients who might otherwise be overlooked—research on primary care physician distribution shows that practitioners who are from minority racial and ethnic groups are much more likely to work in underserved communities than their white counterparts.
How diversity in health care benefits providers
Physicians themselves could enjoy a better quality of life as a result of a more diverse health care workforce. Doctors who are part of an underrepresented group are often able to build incredibly strong relationships with the minority individuals they serve.
“I find that I can better relate to my patients,” Dr. Webb says.
Dr. Jaydeep Tripathy, a UK-based primary care physician at DoctorSpring , notes there are other benefits to working with people from a variety of backgrounds as well. “Diversity in the workplace, in my opinion, fosters a greater sense of identity and culture, making me feel better and more rewarded at work,” he says.
This diversity can go a long way toward improving morale and reminding physicians why they became doctors in the first place. It also encourages physicians to expand their horizons.
“We run the risk of becoming shortsighted or boxed in to a particular way of thinking when everyone is the same,” Dr. Doggett explains. “We lose a certain richness and opportunity to learn from one another. We, as individual clinicians, are certainly affected when there is a lack of diversity, but our patients are impacted even more.”
Diversity in health care starts at the beginning

To truly work toward a more diverse, more equitable health care system, it’s critical to reach potential physicians as early as possible. “There should be more of a focus on exposing kids to careers in medicine,” Dr. Webb says, who is actively involved in this effort through his video interview series . “Hospitals and schools can create more pipeline programs,” he adds.
Additionally, diversity efforts must continue into medical school , which can be achieved through a more holistic admissions process. When classes are more diverse, all students benefit from broadened perspectives. Diverse classrooms help students improve active thinking, intellectual engagement, social skills, empathy, and racial understanding—all critical components to a physician’s education. Research even shows that cross-cultural interactions during medical school help students feel better prepared to serve diverse populations later on.
“Doctors are required to be competent not only in medicine but also in communication and caring for people with different disease burdens, socio-cultural realities, expectations, values, and beliefs,” explains Dr. Satesh Bidaisee , a professor of public health and preventive medicine and assistant dean for the School of Graduate Studies at St. George’s University. “Doctors of today need a global competence to understand the diverse populations they serve.” He feels it’s the responsibility of medical schools to provide this competence for students, who in turn will provide nuanced care for patients of all walks of life.
Diversity in health care matters
Diversity in health care helps ensure all backgrounds, beliefs, ethnicities, and perspectives are adequately represented in the medical field. It’s about providing the best possible care for all patients.
If you’re interested in a career in medicine and want to gain an edge with a global perspective, then learn more by reading our article, “ 6 Little-Known Perks of Attending an International Medical School .”
*This article was originally published in December 2018. It has since been updated to reflect information relevant to 2021.
Related Articles

Pathology: What it is and why it’s a fascinating specialty

Medical board certification

Medical fellowships and medical specialties
Take The Next Step
Start your journey toward becoming a doctor.
Our School of Medicine offers rolling admissions for our January, April, and August classes.
Watch this short video to learn about the SGU School of Medicine and fill out the form out the form to speak with a practicing graduate, a current student, or an admissions officer.
US residencies in 2024 1
US residency placement rate for graduates over the last five years 2
USMLE Step 1 pass rate for first-time test-takers over the last three years 3
USMLE Step 2CK pass rate for first-time test-takers over the last three years 4
1 Data as of March 2024.
2 As the medical school graduating the largest number of students per year, SGU places the largest number of graduates into residency programs each year, based on internal SGU graduate/expected graduate and residency placement data as of March 2024.
3 Average of 2019, 2020, 2021 scores. First-time pass rate is defined as the number of students passing USMLE Step 1 on their first attempt divided by the total number of students taking USMLE Step 1 for the first time. In order to be certified to take USMLE Step 1, students are required to pass all basic sciences courses.
4 Average of academic years 2019, 2020, 2021 scores. First-time pass rate is defined as the number of students passing USMLE Step 2 CK on their first attempt divided by the total number of students taking USMLE Step 2 CK for the first time. USMLE Step 2 CK is typically taken upon completion of third-year core clinical rotations.
Request More Information
US Residencies in 2024 1
US residency placement rate for graduates over the last five years 2
USMLE Step 2CK pass rate for first-time test takers over the last three years 4

Contact SGU
+1 (631) 665-8500 ext. 1380, st. george’s university university centre grenada, west indies.
Office of Admission St. George’s University c/o University Support Services, LLC The North American Correspondent 3500 Sunrise Highway, Building 300
Programs Doctor of Medicine Doctor of Medicine/Master of Science (MD/MSC) Doctor of Medicine/Master of Public Health (MD/MPH) Medical PHD Degree
Copyright: St. George’s University – 2023
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Diversity and discrimination in health care.
Brandon M. Togioka ; Derick Duvivier ; Emily Young .

Affiliations
Last Update: May 2, 2024 .
- Continuing Education Activity
The United States is a diverse country and a place for people of all backgrounds. However, discrimination against individuals and groups belonging to minority identities persists, leading to negative outcomes for patients and healthcare professionals. Clinicians are responsible for addressing inequity in the medical profession, a part of the American healthcare system. Several decades ago, diversity and discrimination were considered terms within social justice or social movements. However, in recent years, there has been a notable shift in focus within the healthcare field towards understanding and addressing social determinants of health. Remaining cognizant of these cultural shifts is relevant for healthcare community members at all levels to remain productive and contribute within the field.
This activity reviews the concepts of diversity and discrimination and highlights the interprofessional team's role in improving care for patients from diverse backgrounds through medical education. Participating clinicians are equipped with historical milestones, past and present events, and recommendations to inform policy that aims to increase diversity and decrease discrimination within healthcare settings.
- Identify different manifestations of diversity and discrimination, and analyze their impacts on health care.
- Interpret the different levels within the healthcare system on which bias and discrimination occur.
- Evaluate relationships between bias and negative patient outcomes in the healthcare system.
- Implement interprofessional guidance that healthcare systems can adopt to increase diversity and reduce disparities.
- Introduction
Diversity is broadly defined as the inclusion of varied attributes or characteristics. In the medical community, diversity often includes healthcare professionals, trainees, educators, researchers, and patients from diverse backgrounds, including race, ethnicity, gender, disability, social class, socioeconomic status, sexual orientation, gender identity, primary spoken language, and geographic region.
Discrimination in health care is defined as negative actions or lack of consideration directed towards an individual or group based on preconceived notions about their identity. Individuals do not have to belong to a marginalized group themselves to experience discrimination against that group. Discrimination can occur based on perceived membership. Furthermore, harm does not need to occur for discrimination to exist. A group may be discriminated against if it consistently receives lower-quality healthcare services compared to another group solely because of their race, ethnicity, gender, disability, social class, socioeconomic status, sexual orientation, gender identity, primary spoken language, or location of residence.
Although discrimination can manifest for various reasons, this activity focuses mainly on gender, ethnicity, and race-based discrimination in the healthcare workforce. Discrimination occurs in all workforce segments, not limited solely to health care. However, health care presents a unique scenario because both care providers and recipients may face discrimination simultaneously, underscoring an inherent power dynamic. [1]
- Issues of Concern
The 2 main types of discriminatory acts are macroaggressions and microaggressions. Macroaggressions are more overt and radical forms of discrimination deeply rooted in a society or within a system. Examples of macroaggressions include the forced relocation of Japanese-Americans into internment camps during World War II, laws preventing equal suffrage rights for women, and the Tuskegee study, where Black men were intentionally misled and denied standard treatment for syphilis.
Laws such as Title VII of the Civil Rights Act and the Americans with Disabilities Act (ADA) prohibiting unequal treatment based on race, sex, and disability have decreased overt racism within healthcare settings. In areas where overt racism has declined, awareness of microaggressions has increased. Microaggression can be defined as short, everyday insults or snubs that can be barely perceptible or difficult to define but convey a negative message to individuals because of their identity or affiliation with marginalized groups. [2] Microaggressions, often unintentional and rooted in unconscious biases, can be challenging to identify, easily concealed, and delivered involuntarily through verbal or non-verbal communication. [3] [4] Microaggressions are often delivered during one-on-one interactions, whereas macroaggressions are rooted in systems. [5]
Despite their insidious nature, microaggressions have perceptible negative impacts on the quality of life of oppressed individuals or groups. Increased exposure to microaggressions increases the likelihood of feeling discriminated against. Microaggressions may damage the mental health of oppressed individuals, causing lower self-esteem, poorer self-care, and increasing susceptibility to substance abuse, depression, suicidal ideation, and anxiety. [6] [7] [8] [9] Growing evidence suggests that repeated exposure to microaggressions is associated with a higher incidence of hypertension, increased frequency of hospital admission, and more severe diabetes-specific distress. [10] [11]
The killing of George Floyd in 2020 in a succession of incidents of police brutality, in conjunction with the disproportionate burden of COVID-19 in communities of color, has elevated the national consciousness regarding diversity and discrimination. [12] Americans are more aware that structural racism is causing healthcare disparities. [13] Research demonstrates that discrimination and bias exacerbate and create new healthcare disparities. [14] As a result, the national conversation surrounding racism has resulted in the recognition of racism as a public health crisis. [15] As the national discussion surrounding diversity, discrimination, and structural racism continues, several matters have been brought to the forefront, as discussed below.
A Multicultural Society Requires a More Diverse Workforce
As our country's racial and ethnic diversity increases, the need to diversify our healthcare workforce increases. The need to diversify health care has been present since the inception of the first women and individuals of color entering higher medical education. [16] The Flexner report significantly slowed the inclusion of Black physicians in the American medical system. [17] [18] Flexner concluded that medical education within African American schools was deficient, resulting in the closure of 5 of 7 African American medical schools. [19] Since then, the ability of Black and Brown clinicians to reach higher workforce levels has increased, but discrimination is still prevalent, intersecting with several marginalized identities. Many years later, when COVID-19 disrupted the American healthcare system, a rise in discrimination towards Asians and Asian Americans necessitated a focus on increasing social support from students to the professional level. [20] Concerning diversity outside of race, individuals belonging to gender-diverse and disabled groups face significant exclusion. [21] [22]
Progression From Individual to Structural Racism
Racism is a social construct that emphasizes phenotype. According to the National Museum of African American History & Culture, individual racism, interpersonal racism, institutional racism, and structural racism are delineated. Individual racism is most directly related to the biases that we hold, and interpersonal racism is an expression of these biases between individuals. Institutional racism is reflected in the policies and procedures of an organization. Structural racism is the cumulative effect of these forces across systems and between institutions or organizations. The promotion of health equity and a decrease in health disparities requires addressing individual and interpersonal racism and dismantling institutional and structural racism. However, the complexity of such endeavors should be recognized, given the hundreds of years of history where individual and structural racism have prevailed within health care. [23] [24] The decision regarding Dobbs v. Jackson in 2022 that overturned Roe v. Wade reignited the conversation surrounding the relationship between the healthcare system and reproductive health. [25] In 2023, the ruling against affirmative action for college admissions had an unknown impact on higher medical education in the following years. [26] The conversation in many sectors about the potential effects of structural racism, particularly concerning artificial intelligence, is prevalent in 2024. [27]
Bias, Stereotype Threat, and Negative Outcomes
Increasing awareness in the United States involves recognizing that implicit bias contributes to poorer healthcare outcomes for patients of color. [28] Racist behavior negatively impacts patient well-being. In addition, stereotype threat is a psychological state where individuals underperform due to their fear of fulfilling negative stereotypes. The hypothesis is that stereotype threat impairs the performance of minority students on standardized tests such as the Medical College Admission Test (MCAT) and the United States Medical Licensing Examination (USMLE). [29] Stereotype threat has been found to cause psychological harm among students and trainees of color. [30] Several efforts continue to examine the approaches to teaching trainees about healthcare disparities. [31] [32]
- Clinical Significance
Individual racism is a personal belief in the superiority of one's race over another, often leading to discriminatory behavior driven by implicit and explicit biases. Historically, racist beliefs regarding biological differences between Black and White people were used to justify slavery and medical experimentation on men and women of color. The legacy of this false belief in fundamental and innate biological differences between Black and White people is still present in medical practice, leading to health disparities such as the undertreatment of pain in Black patients.
A research study published in the Proceedings of the National Academy of Sciences of the United States demonstrates the connection between false beliefs about biological differences between Black and White people and racial bias in pain assessment and treatment recommendations. In this 2-part study, medical students and residents endorsed beliefs suggesting biological differences between Black and White patients. These beliefs included that the nerve endings of Black people are less sensitive compared to White people and that the skin of Black people is thicker compared to White people. Furthermore, medical students and residents who held these beliefs rated the pain of Black people lower compared to that of White people and, therefore, made less accurate treatment recommendations. [28] Historically, similar beliefs were endorsed by the Nazis during the Holocaust regarding tolerance of pain levels that led to some of the most brutal documented recollections of medical experimentation based on identity. [33] [34] [33]
Structural racism is rooted in societal, historical, and cultural norms that support racial group inequality. As an institution, medicine has adopted and implemented practices and policies that promote structural racism. Race-adjusted algorithms are based on the historic racist belief that Black people are physiologically different. For instance, race-corrected estimations of glomerular filtration rate are based on the unscientifically supported belief that Black people are more muscular and have higher creatinine levels. Consequently, this may result in a higher reported estimated glomerular filtration rate, interpreted as a better renal function for anyone identified as Black. As a result, there may be delays in diagnosing renal disease and reduce access to transplantation. [35]
At a systems level, the failure to identify the health implications of discrimination may result in developing a system promoting health disparities. For example, an algorithmic bias was identified in a medical artificial intelligence program that considered past healthcare costs when predicting clinical risk. Consequently, due to White patients having greater healthcare expenditures compared to Black patients, they were determined to have higher risk scores compared to Black patients. These scores may have led to more referrals for White patients to specialty services, perpetuating both spending discrepancies and race bias in health care. [36] In the United States, maternal mortality rates are disproportionately high, and patients who identify as female face numerous barriers to accessing equitable medical care, ranging from the use of imaging modalities, surgical recommendations, and perception of self-efficacy in decision-making to the final diagnosis, now termed gender-affirming health care. [37] Disability-conscious health care is also emerging in the continued movement toward equity in clinical practice. [38]
The root cause of discrimination based on race, gender, or other identifying social constructs has led to racism, inequality, and inequity concerning the process of patient history intake, evaluation, and diagnostic testing. Within each specialty, the effect of discriminatory beliefs is exhaustive, but some commonalities can be observed. Considering the past pitfalls of experimentation on marginalized groups and restructuring the approach to medical education in the present is the path presented in this activity.
- Other Issues
Medical Education on Diversity in Healthcare
This section is intended primarily for healthcare professional educators. However, all educators may benefit from both peer- and self-education.
The Liaison Committee on Medical Education and the Commission on Osteopathic College Accreditation require medical schools to promote diversity and prohibit discrimination. However, researchers have yet to confirm whether such actions affect health outcomes. A search in PubMed for education studies about diversity for healthcare professionals did not yield results generalizable to the effectiveness of any specific strategy. Before considering healthcare outcomes, an intermediate step is raising the awareness of bias to modify perceptions and behaviors at the student level; research in this area is abundant and described below.
Valuing cultures other than oneself involves a willingness to learn and self-reflect continuously. When discussing the ability of education to change perceptions and behaviors, the terms cultural humility, cultural awareness, and cultural sensitivity are more appropriate compared to cultural competency, as competency implies having attained a finite body of knowledge. [39] The former terms present the knowledge as existing on a continuum that requires progress toward inclusion.
Educational Approaches
Inclusive education emphasizes that healthcare professionals should consider patients in their unique individual contexts and acknowledge that a situation may be experienced differently by different patients. What matters in making informed decisions are an individual's health perspectives, requirements, and experiences, not their ethnicity, race, or social status. [40] A critical skill for all healthcare professionals is to understand patients not by employing any particular label but instead by employing an attitude of curiosity about how each patient’s experiences and context shape their views and behaviors.
Developing a healthcare professional's critical consciousness, defined as a reflective awareness of the self, others, and the world and a commitment to addressing issues of societal relevance in health care, is believed to be an effective approach to education about diversity than teaching facts or emphasizing the use of an individualized approach to patient care. [41] Healthcare professionals should also undergo training in recognizing their own implicit biases and biases of the institutions and systems in which they work. This training includes understanding the composition of the leadership workforce and how decisions are made within their workplaces.
Recent review articles provide general guidance and practical examples for educators.
- In 2007, Smith et al developed recommendations for curricula on health disparities and suggested that the broad goal of such curricula should be to eliminate health disparities.
- In 2016, Dogra et al published a curriculum guide and reviewed examples of education about diversity. They recommended integrating education concerning diversity throughout the curriculum and highlighted the importance of self-reflection in learning and teaching related concepts.
- A multidisciplinary approach incorporating many education modalities typically enhances knowledge retention. Similar to Objective Structured Clinical Examinations (OSCEs), simulations, in particular, may resemble real-life clinical encounters as applicable to situations of discrimination. [42] [43]
Despite the lack of large-scale evidence for best practices, many smaller studies focused on particular target populations or particular interventions. Some evidence suggests that multimodal, active learning formats, such as a combination of faculty role modeling, interprofessional rounds, and OSCEs, can yield gains in learners' knowledge, skills, and attitudes. [44] Lectures are useful but have potential pitfalls and should be followed by hands-on practice with feedback and formative evaluation. The discussion format is likely more effective compared to lectures alone in helping learners explore and develop their attitudes on cultural issues.
When education about diversity is integrated longitudinally throughout a curriculum, appointing someone to oversee all curricular modules can maximize cohesion and minimize redundancy. Smith et al proposed that a curriculum committee not assign all teaching roles to faculty persons of minority demographics because that arrangement can imply that issues related to discrimination are only a problem for minorities to navigate rather than the responsibility of all healthcare professionals. [32]
Diversity education is a unique curricular topic. Healthcare team members at all expertise levels, from trainees to experienced clinicians, require the same foundation that builds a skill set. If education is considered a shared responsibility, professionals from diverse backgrounds can engage in mutual learning and collaboration.
Healthcare professionals have made many false assumptions about the relationship between cultural variables and medical outcomes, unnecessarily reinforcing negative stereotypes. Teaching typical characteristics of minority groups frequently promotes stigmatization without promoting healthcare outcomes. This approach makes culture a proxy that prevents healthcare professionals from noting the person behind the patient. Categorizing patients based on cultural characteristics assumes that culture and its impact on persons' responses are fixed. Healthcare professionals should instead realize that patients have dynamic views that vary based on their immediate contexts and recognize that identity classifications such as gender, age, class, disability, sexuality, race, and ethnicity are multifaceted.
Faculty preparation is crucial for effectively teaching diversity education; educators who are well-intentioned but unprepared can inadvertently promote students' and patients' stereotyping. Microaggressions embedded in curricular content create an unsafe climate for cultural minority students. Emphasizing minority patient characteristics as inconsistent with the privileged majority's norm marginalizes minority patients and paints them as a problematic other. [40]
Finally, educators should realize that they teach a curriculum implicitly or explicitly. While the planned curriculum describes what educators perceive, the experienced curriculum describes what students perceive. What educators teach students unintentionally is the hidden curriculum, described as a set of influences that function at the level of organizational structure and culture. [45] The hidden curriculum can have positive effects, such as when an educator role models cultural humility. The hidden curriculum can also have negative effects, such as using clinical vignettes that promote stereotypes and undermining cultural sensitivity training in other parts of the curriculum. [46] In addition, a lack of diversity among faculty or institutional leaders can project through the hidden curriculum that minorities do not have a role in higher career positions. [31]
Education regarding diversity is not a time-bound goal but rather a journey. The education should provide learners with the opportunity to become actively engaged in fostering a level of critical awareness of the healthcare provider's position of power and privilege in society. [47] Inclusiveness in a curriculum does not involve adding a few learning activities to the existing curriculum but rather involves a culture shift. [48]
- Enhancing Healthcare Team Outcomes
Based on existing literature and the results of several studies, the hypothesis positing an inverse relationship between discrimination and diversity is recognized. The prevailing belief within the medical community is that discrimination decreases and equity increases if the percentage of underrepresented minorities reaches a critical mass. Evidence suggests that although diversity is a goal, it alone does not create equity. Although more than half the pediatricians and gynecologists in the United States are now women, leadership positions within departments remain predominantly occupied by men. [5] Men are likelier to be selected for editorial board membership and achieve status as an associate or full professor, department chair, or medical school dean. Men also earn more at each academic rank. [49] Therefore, diversity does not necessarily impact the distribution of resources within the teaching system.
These results are similar to those found in the nursing profession. The male advantage in nursing has been described as a glass escalator, in which men are put on a fast track and almost pushed to achieve positions that include greater responsibility, higher salaries, and more organizational benefits. [50] Thus, although diversity is necessary and important, equity is needed to decrease disparities and mitigate the impact of discrimination.
Although increasing diversity may not eliminate all problems related to healthcare disparities and discrimination, we strongly encourage healthcare systems to promote diversity among clinicians. A larger talent pool, including clinicians with heterogeneous customs, experiences, and problem-solving tactics, can create more innovative approaches to systems-based problems. Individuals within a group may best solve healthcare issues that are more prevalent within that group. Diverse viewpoints enhance patient care and clinical research design, which may lead to improved inclusion.
Numerous studies have shown that increased clinician diversity is associated with improved healthcare quality. Concordant care, defined as a patient and clinician sharing a common attribute such as race, ethnicity, or gender, has been associated with improved quality of care. Race-concordant patient-physician relationships are associated with improved communication, longer patient visits, greater medication adherence, and higher patient satisfaction scores. [51] [52] Language and gender-concordant patient-physician relationships have similarly been associated with improved home medication compliance and outcomes. [53] [54] Such results suggest that patient-physician concordance may facilitate communication and trust.
Poor access to quality care continues to impact minority and low-income individuals in the United States disproportionately. A potential solution is to focus on recruiting and retaining underrepresented healthcare professionals. Underrepresented minority physicians are more likely to serve in areas with a physician shortage and serve underserved groups, including minorities, low-income individuals, and the uninsured. [55] [56] [57]
The following measures are encouraged to be considered by healthcare groups and systems to improve the recruitment and retention of employees from underrepresented groups:
- Eliminate financial barriers to higher education for socioeconomically disadvantaged groups by developing scholarships, grants, and tuition assistance.
- Create mentorship and pipeline programs to increase the number of underrepresented minorities in healthcare careers. When possible, these mentorship pairings should align with the race and gender of participants.
- Provide opportunities for coaching and leadership training for healthcare professionals from underrepresented groups.
- Use transparent processes to select committee members and leaders with diverse backgrounds and viewpoints.
- Provide pay transparency and objective measures for promotion and salary increase.
The following actions are encouraged to be considered by healthcare groups and systems to quell discrimination and accelerate the remedy of healthcare disparities:
- Acknowledge that past discrimination and current implicit biases lead to inequities related to race, gender, ethnicity, sexual orientation, and disability, which still exist in healthcare settings. Progress is limited by denying the existence of discrimination and bias.
- Educate healthcare professionals on the impact of health disparities and structural racism on patient outcomes. Equip healthcare trainees and practicing clinicians with tools and resources to confront macroaggressions and microaggressions.
- Create a zero-tolerance policy for harassment and discrimination that includes a safe reporting mechanism for both the victim and the reporter.
- Increase support for research on healthcare disparities.
- Consider diversity as a subject integrated into medical education rather than an adjunct.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Brandon Togioka declares no relevant financial relationships with ineligible companies.
Disclosure: Derick Duvivier declares no relevant financial relationships with ineligible companies.
Disclosure: Emily Young declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Togioka BM, Duvivier D, Young E. Diversity and Discrimination in Health Care. [Updated 2024 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Palliative care experiences of adult cancer patients from ethnocultural groups: a qualitative systematic review protocol. [JBI Database System Rev Implem...] Palliative care experiences of adult cancer patients from ethnocultural groups: a qualitative systematic review protocol. Busolo D, Woodgate R. JBI Database System Rev Implement Rep. 2015 Jan; 13(1):99-111.
- Diversity, Equity, and Inclusion Among Anesthesiology Trainees. [Womens Health Rep (New Rochell...] Diversity, Equity, and Inclusion Among Anesthesiology Trainees. Patel S, Lin KK, Milam AJ, Yu S, Raynor G, Narjeet K, Verdiner R, Girardo ME, Misra L. Womens Health Rep (New Rochelle). 2022; 3(1):414-419. Epub 2022 Apr 7.
- Essential Principles to Create an Equitable, Inclusive, and Diverse EMS Workforce and Work Environment: A Position Statement and Resource Document. [Prehosp Emerg Care. 2023] Essential Principles to Create an Equitable, Inclusive, and Diverse EMS Workforce and Work Environment: A Position Statement and Resource Document. Owusu-Ansah S, Tripp R, N Weisberg S, P Mercer M, Whitten-Chung K, NAEMSP Diversity, Equity, & Inclusion Committee. Prehosp Emerg Care. 2023; 27(5):552-556. Epub 2023 Mar 24.
- Review Comparing Preferences for Depression and Diabetes Treatment among Adults of Different Racial and Ethnic Groups Who Reported Discrimination in Health Care [ 2021] Review Comparing Preferences for Depression and Diabetes Treatment among Adults of Different Racial and Ethnic Groups Who Reported Discrimination in Health Care Cook BL, Progovac AM, Cortés DE, McCormick D, Flores M, Adams LB, Creedon TB, Carson N, Lee E, Lu F, et al. 2021 Jan
- Review Disability, mental health, sexual orientation and gender identity: understanding health inequity through experience and difference. [Health Res Policy Syst. 2018] Review Disability, mental health, sexual orientation and gender identity: understanding health inequity through experience and difference. Nakkeeran N, Nakkeeran B. Health Res Policy Syst. 2018 Oct 9; 16(Suppl 1):97. Epub 2018 Oct 9.
Recent Activity
- Diversity and Discrimination in Health Care - StatPearls Diversity and Discrimination in Health Care - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Systematic review in relation to support of diversity in nursing homes
Javier mesas-fernández, jordi tous-pallarès, ivette margarita espinoza-díaz.
- Author information
- Article notes
- Copyright and License information
Edited by: Laura Haynes , University of Connecticut, United States
Reviewed by: Erica C. Lorenzo , UCONN Health, United States
Daniele Melo Sardinha , Evandro Chagas Institute, Brazil
*Correspondence: Javier Mesas-Fernández, [email protected]
Received 2024 Feb 21; Accepted 2024 Aug 27; Collection date 2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
Introduction
Given the increasing global population of older adults, it is essential and inevitable that healthcare centers and nursing homes address and accommodate diversity in their support systems as interventions for healthy aging. The active aging and the inclusion of all people regardless of their religion, origin, and/or sexual orientation is essential to create a climate of safety. Discrimination must be addressed from all angles, at the social level, at the business level and by all workers in nursing homes.
Methodology and results
This study provides a comprehensive review of existing literature to systematize information on diversity among older adults in healthcare centers and nursing homes. Out of 1.458 articles identified, 10 were analyzed in depth, revealing that addressing diversity among older adults is crucial to overall mental and physical healthy aging. The findings underscore the need for a multidisciplinary approach and effective management through the Person-Centered Care Model (PCCM).
Discussion and conclusion
This study highlights the critical role of the Person-Centered Care Model (PCCM) in addressing diversity in aging needs. It highlights the necessity of tailoring care based on individual life histories and experiences. Additionally, it calls for the implementation of inclusive policies in nursing homes and emphasizes the need for professional training on diversity to ensure these facilities are safe and supportive for all residents.
Keywords: diversity, nursing homes, elderly, person-centered care model (PCCM), discrimination
1 Introduction
It is necessary to offer a more inclusive concept about aging, which accepts and adopts diversity in all its forms, considering the biological, psychological, and social aspects of the person, and not only from the economic point of view. It is important to expand the active aging model. This action must go hand in hand with an effort to carry out actions and activities where the differences of each human being are highlighted and enhanced ( Villar Possada et al., 2018 ).
Diversity in aging is a phenomenon that needs to be dealth with and discussed since it poses a series of challenges that require attention in the new realities within nursing homes. The importance of studying the phenomenon from a comprehensive vision is highlighted due to the challenges, opportunities, transformations, and concerns that this phenomenon represents in society.
According to Sánchez Barrera et al. (2019) , the aging process is surrounded by a range of beliefs, myths, prejudices, policies, and perceptions, emphasizing the need for a more in-depth exploration of this topic. The increasing global population of older adults is viewed as a social achievement due to longer life expectancy. However, this also presents a significant challenge: transforming the concept of healthy aging from a rare privilege into an opportunity that embraces all forms of diversity. The challenge is that of healthy aging, passing from the belief that it is an exception and a privilege, including all types of diversities, to be an opportunity. Support for diversity is a necessity. The inclusion of all people regardless of their religion, origin, and/or affective-sexual diversity is essential to create a climate of safety.
In relation to older people, diversity is a key concept to understand and adequately address the needs and realities of this population. Diversity refers to the approach to equality that seeks to celebrate the differences between people ( Klein, 2016 ). Older people are not a homogeneous group but present a great variety in terms of their characteristics and needs. Some are active and healthy, while others may have functional and/or cognitive diversity. In addition, older people also have differences among themselves in terms of culture, wealth, social status, gender, affective, sexual, etc. In the same way as the rest of the population.
Diversity refers to the presence of people with different physical, social, and personal characteristics in a group or organization. These characteristics include race, ethnicity, age, gender, sexual identity, religion, physical and mental ability, language, income, and education. One’s concept of diversity is linked to one’s experiences of diversity, one’s own social, political, educational values and perspectives, etc. ( Nash, 2001 ).
Sexuality in human beings is something innate. There is no limit to this dimension since it is part of our communication. On many occasions, and mistakenly, sexuality is related to sexual activity itself. Sexuality as a dimension covers aspects such as identity, intimacy, attitudes, gender roles, sexual orientation, desire, etc. In relation to the affective-sexual diversity, on the other hand, refers to the different ways of expressing affection, desire, and erotic and/or loving practices. That is, to all the possibilities of accepting, assuming and living affectivity and sexuality, whether for people of the same sex, the opposite sex or both ( Morales-Rodríguez, 2021 ).
According to Boyon (2021) , through the Ipsos report carried out in 2021 on 19,069 people, various issues regarding the LGTBI + elderly group are made clear:
- By the year 2050, it is expected that there will be about 2,000 million older people throughout the planet; 22% of the planet’s inhabitants will be over 65 years old by that date. It is estimated that, of those 2,000 million people, approximately, 200 million will be LGTBI+.
- Spain is the third country in the world, the first in Europe, with the highest percentage of the population that declares themselves non-heterosexual (12% in total; of which 6% say they are bisexual, 5% gay and the other 1% pansexual).
The lack of specific data can make it difficult to articulate different public policies aimed at improving the lives of older people. Due to this, as Equala (2023) indicates, in recent years an incipient effort has been made to generate indicators that allow us to understand the reality of LGTBI + people.
In relation to the problem of racism and religion, in society, this could create two fundamental aspects that need to be considered. Firstly, the importance of religion in older people and, consequently, in nursing homes. Secondly, the possibility of racist attitudes being replicated in the centers by users and staff. For Kaplan and Berkman (2022) , there is a relationship between the concepts of religion and spirituality, which, although they are similar, are not identical. They refer to religion as a more formal and structured concept, and includes more traditional activities, the performance of rituals and putting them into practice. On the other hand, when they talk about spirituality, they do so by mentioning the immaterial and intangible, which does not have to be related to a specific group.
According to Farrell et al. (2022) constructs of racism and ageism can have negative effects on health outcomes that can be magnified when race and age intersect, including recent events such as the COVID-19 pandemic.
The Person-Centered Care Model (PCCM) proposes an approach considering the care of the person, their dignity and their wishes, in addition, it pays special attention to their decisions, tastes and preferences, understanding that each person has a unique identity that is differentiated from the rest.
All of this with the objective that every older person, regardless of their dependency, develops their own vital process. Maintaining dignity throughout this process is essential to promoting their quality of life.
Care encompasses those individual and social practices designed to ensure the survival and wellbeing of human beings. Caring means supporting people in their autonomy and helping them to function in daily life ( HelpAge Spain International, 2021 ). People who need care have the right to exercise control directly or indirectly over their lives and care. The need for new forms of care that focus on putting the person at the center is becoming evident.
The diversity of the older population is a key factor in providing services and care tailored to the individual needs of each person. PCCM is particularly relevant in this sense, as it promotes the personalization and adaptation of services and care to the individual needs and preferences of each person.
Population aging is a global phenomenon, with middle-income and low-income countries experiencing the most rapid growth in individuals over 60, increasing from 16% in 2019 to 36% in recent years ( World Health Organization, 2021 ). This trend highlights the pressing issue of ageism, which manifests in societal stereotypes, prejudices, and discriminatory practices ( World Health Organization, 2021 ). As the older adult population continues to rise, the demand for healthcare centers and nursing homes will increase, necessitating a focus on diversity as a foundational element. It is imperative to ensure that individuals with diverse characteristics and needs have access to appropriate resources and environments that promote their wellbeing. Embracing diversity and implementing individualized care models are crucial for enhancing nursing home services. A comprehensive review of management practices, including attention to internal policies, protocols, records, and diversity training for professionals, is essential for improving care in these settings.
This article contributes significantly to the field of research by highlighting the need for a more inclusive concept of ageing, which addresses diversity in all its forms and considers the biological, psychological and social aspects of older people. Research indicates that ageing should be an accessible opportunity for all, regardless of their affective-sexual, cultural, religious or socioeconomic diversity.
2 Methodology
This systematic review is based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). The PICO framework is used to structure the systematic review approach and is related to diversity in older adults living in healthcare facilities and nursing homes. A non-experimental design was utilized to perform a systematic review of the literature concerning diversity in older adults living in nursing homes. This method involved aggregating and analyzing contributions from various peer-reviewed literatures to determine current levels of support for diversity in nursing homes. This analysis was also used to inform best interventional practices to provide nursing home residents with a supportive healthy environment centered around PCCM.
Carrying out systematic research requires the establishment of three phases, these are developed and articulated sequentially to guarantee the identification and selection of documents ( Table 1 ).
Phases to guarantee the identification and selection of documents.
2.1 PICO question
The work developed and the methodology presented below are based on the question in relation to the PICO question, which is posed in the following table ( Table 2 ). Table 2 details the PICO question, which outlines the objectives of this study.
PICO question.
This table is transferred to the definition of the following PICO question:
How does attention to diversity influence the quality of life in older people?
2.2 Study selection criteria
- Inclusion criteria:
• Scientific articles and magazines published in the last 5 years.
• Publications in which the active aging approach, its components, policies, and strategies have been addressed, both in Spanish and English.
• Articles under a qualitative design
• Scientific documents and research that are complete.
• Texts that have been developed from national and international cases.
• Scientific articles and magazines, both national and international.
- Exclusion criteria:
• Type of study: meta-analysis and systematic reviews; opinion articles and duplicates.
• Sample population (age <60).
• Documents that do not contain keywords in the title, summary and/or keywords.
Consequently, it was determined through the checklist that through the PRISMA 2020 declaration, that the research sources must contain specific sections such as: section/topic; qualification; summary; introduction; methods of inquiry and the resolutions that other researchers managed to achieve in their investigative process and that were contrasted in the discussion section.
2.2.1 Information sources and search method
The following databases were searched: Pubmed (US National Library of Medicine), Cochrane Library, Scielo, Web of Science (Institute of Scientific Information) and Scopus.
For the search, different keywords were combined:
- Terms Mesh: quality of life, nursing homes, intersectionality.
- Terms DeCs: calidad de vida, residencias de personas mayores e interseccionalidad.
In addition, terms that are not included in the Mesh terms were used, they were the following: diversity, gerontology, and elderly people. These terms were combined with the Boolean operators “AND” and “OR”, in this way the search is directed to the desired articles. Finally, the following search is carried out in the different databases:
(religious OR spiritual OR cultural OR gender OR sexual) AND diversity AND (“quality of life” OR “wellbeing” OR “wellbeing” OR care) AND (“elderly people” OR “nursing homes” OR elder OR “old people”).
The present systematic review has been registered in PROSPERO with the following number: 543543 - Systematic review in relation to diversity in nursing homes.
Of all the articles obtained in the searches, a total of 1,458 articles; duplicate articles in the different databases and systematic reviews were discarded. A total of 1,311 articles were discarded, so 147 articles were selected for a first reading of the title and summary.
2.2.2 Search list
The search in the databases was carried out between the months of May and July 2023, with the last search being carried out on 23 July 2023.
2.2.3 Web of science
- The search was carried out within “Topic,” with the following combination:
- (religious OR spiritual OR cultural OR gender OR sexual) AND diversity AND (“quality of life” OR “wellbeing” OR “wellbeing” OR care) AND (“elderly people” OR “nursing homes” OR elder OR “old people”) AND “intersectionality”.
- A total of 598 articles were obtained. The filters were introduced: Spanish and English language, complete and open availability, and publication date between 2013 and 2023. The following “Meso topics” were used: 6.178 (Gender & Sexuality), 1.14 (Nursing), 6.73 (Social Phsycology), 1.155 (Medical Ethics), 6.86 (Human Geography), 1.66 (Hiv), 6.256 (Religion) 6.24 (Psychiatry & Psychology). A total of 45 articles were obtained for reading the title and abstract.
2.2.4 Scopus
- The search was carried out within “Article title, abstract, keywords” with the following combination:
- TITLE-ABS-KEY (religious OR spiritual OR cultural OR gender OR sexual) AND diversity AND (“quality of life” OR “wellbeing” OR wellbeing” OR care)AND “elderly people” OR “nursing homes” OR elder OR “old people” AND “intersectionality”
- A total of 266 articles were obtained. Filters were introduced: Spanish and English language; publication date between 2019 and 2023; availability of the complete free open document; document type: article; In the subject area, documents related to Medicine, Nursing, Social Sciences, Arts and Humanities and Multidisciplinary were filtered, discarding the areas of Agriculture and Biological Sciences, Environmental Sciences and Neuroscience. A total of 22 articles were obtained, selected for reading the title and abstract.
2.2.5 Pubmed
- The search was carried out within “Title/abstract” with the following combination:
- (religious OR spiritual OR cultural OR gender OR sexual) AND diversity AND (“quality of life” OR “wellbeing” [Mesh] OR “wellbeing” OR care) AND (“elderly people” OR “nursing homes” [Mesh] OR elder OR “old people”).
- A total of 377 results were obtained. After entering all the eligibility criteria: publication date from 2019 to 2023, availability of the full open text, Spanish or English language, a total of 9 studies were obtained for reading the title and abstract.
2.2.6 Cochrane library
- The result of the search combination in the “Title, summary, keyword” section was:
- (religious OR spiritual OR cultural OR gender OR sexual) AND diversity AND (“quality of life” OR “well being” OR “well-being” OR care) AND (“elderly people” OR “nursing homes” OR elder OR “old people”) AND “intersectionality”
- The search was carried out in the essays section. A total of 126 trials were obtained. After entering the filters: English language; publication date: between 2019 and 2023, a total of 64 articles were obtained for reading the title and abstract.
2.2.7 Scielo
- The search was carried out within “Topic” with the following combination:
- (religious OR spiritual OR cultural OR gender OR sexual) AND diversity AND (“quality of life” OR “well being” OR “well-being” OR care) AND (“elderly people” OR “nursing homes” OR elder OR “old people”) AND “intersectionality”.
- A total of 18 results were obtained. After entering all the eligibility criteria: publication date from 2019 to 2023, availability of the full open text, Spanish or English language, a total of 7 studies were obtained for reading the title and abstract.
The search flowchart used during the systematic review is shown in detail below ( Figure 1 ).
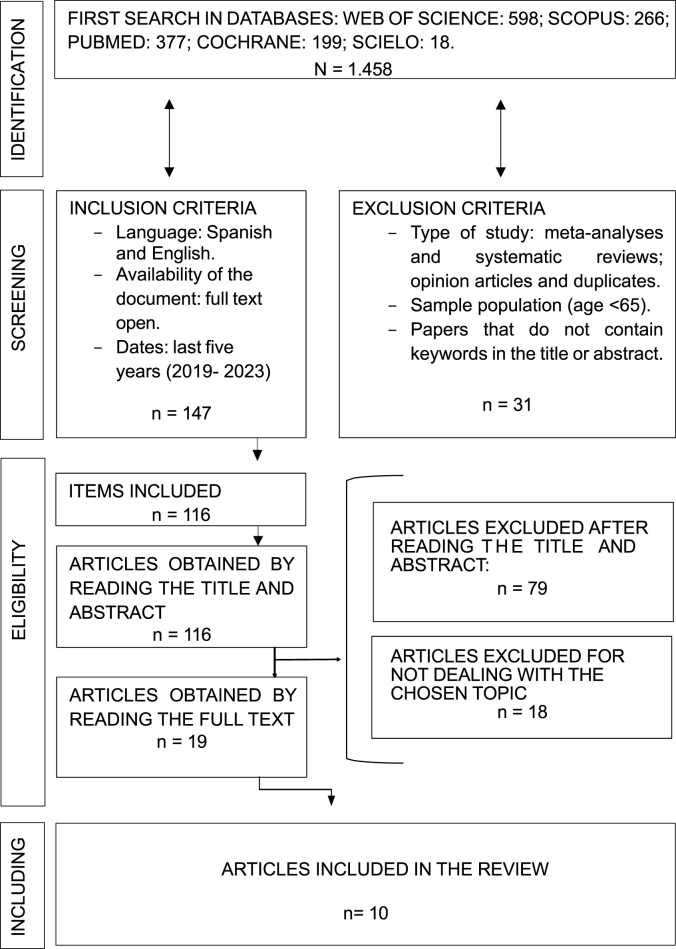
Process to determine qualifying literature to include in systematic review.
2.8 Methodological quality assessment
A quality assessment of the articles included in the review was carried out by the Center for Evidence-Based Medicine (CEBM), Oxford. It is characterized by evaluating the evidence according to the thematic area or clinical scenario and the type of study that involves the clinical problem in question. It has the advantage of grading the evidence according to the best design for each clinical scenario, granting it intentionality and adding the systematic reviews (SR) in the different areas ( Tables 3 , 4 ).
CEBM Recommendation degree and levels of evidence.
Source: Adapted from “Levels of evidence and grades of recommendation” of Gorodosti (2008) .
CEBM scale for articles included in the review peer-reviewed literature.
3.1 Articles examining diversity in aging and assessing aspects of support for diverse populations in healthcare facilities and nursing homes
Of the 19 articles, based on the criteria, 10 articles were selected to be included in the analysis.
The data regarding the authors, year of publication, country, translation of the original title, type/sample and the main findings obtained from the 10 included articles are represented in a tabulated manner ( Supplementary Table S5 ).
4 Discussion and conclusion
The data collected has made it possible to update the available scientific evidence on diversity and older people. It has been found that the individualized attention favors older people, but the limited research on this subject of study indicates the need for further research.
In terms of understanding the needs of older adults in relation to multicultural diversity, it can be confirmed by Hutchinson et al. (2022) that culturally and linguistically diverse older people attach great importance to the six dimensions of the Quality of Life - Aged Care Consumer (QOL-ACC). These quality-of-life dimensions refer to mobility, pain management, independence, emotional wellbeing, social connections and activities. Two other dimensions were added at the request of professionals as relevant, “identity” and “purpose,” which were found to be important for culturally and linguistically diverse older adults (CALD) but were not found to be generically the most important. Based on a study conducted by Palacios-Ceña et al. (2016) , Hutchinson et al. (2022) highlight that meaningful activities are part of identity and promote a sense of belonging. Following on from the article by Hutchinson et al. (2022) , two final issues are highlighted, firstly, how the global COVID-19 pandemic affected the quality of life of older people, especially their personal and social relationships as they were unable to go outdoors. Secondly, it then reaffirms the importance of identity, purpose and meaning in CALD elders and its benefit on quality of life through participation in meaningful activities.
Regarding reviewing the information on the need to include interventions on diversity care in nursing homes, it can be seen, both in the study by Ward et al. (2019) and Daley et al. (2020) , that interventions on diversity care for older people are essential. The article number 1 reviews geriatric assessments in multicultural immigrant populations. The authors affirm the need for comprehensive geriatric assessments in nursing homes, which consider criteria related to multiculturalism and whose aim is to improve quality of life. To this end, a rubric for good practice is created. The article number 2 deals with LGTBI + elderly people in home care and establishes two relevant findings. Firstly, the importance of creating a structure based on the life stories and the perspective of each service user to improve their access, and the invisibility of LGTBI + older people in organizations. In turn, the same article showed that older transgender people avoid home care services for fear of rejection. Nursing homes as social and healthcare spaces must be aware of this fact, and according to Willis et al. (2020) , to build accessible spaces, it is essential to establish a gender affirmative model of care.
In relation to the need for training of professionals, in article number 7 the emphasis is placed on the need for training in the field of health on gender identity diversity, avoiding cisnormativity practices. In this same area of health, it showed the disparities of people with HIV. It is evident that older homosexual and bisexual people with HIV have poorer health. There is also a depressive symptomatology, which not only affects health on a physical level, but also on a psychological level ( Emlet et al., 2020 ). Once again, this article makes special mention of the importance of using the life histories of older people as a tool to improve the quality of life in the service, as well as the low level of training of professionals in relation to LGTBI + older people.
This same author, Emlet et al. (2019) previously conducted a study through WHOAIDS analyzing the global impact of HIV on older LGTBI + people. The study showed there is an intersectionality of stigma, affecting the person in a holistic way and how there is a growth of HIV in older people. HIV broke out in 1981, that same year Acquired Immune Deficiency Syndrome (AIDS) was recognized for the first time as a new disease ( Sharp and Hahn, 2011 ). This means that the people of that generation who survived HIV, today could be 59 or more years old. This assumption is made with the aim of highlighting the need to work on this issue, as they are the closest generations to be potential users of nursing homes. According to Green et al. (2007) HIV in 1982 was more common in homosexual men and intravenous drug users, the first theories about its cause focused on “lifestyle” problems. This discourse persists in society and is directly related to depressive symptomatology in LGTBI + older people ( Emlet et al., 2020 ).
Following the analysis of Holman et al. (2020) , article number 5, about the need for the training in LGTBI + diversity for professionals in the care of the elderly helps to create a better climate. Therefore, this has a beneficial impact on the quality of life of users, strengthening ties and creating a healthy and safe environment. It is also evident that in organizations, in this case of a domiciliary nature, training in affective-sexual diversity is necessary. There are LGTB + older adults, especially transgender people, who avoid this type of resource for fear of rejection ( Daley et at., 2020 ).
The study by Nelson-Becker and Thomas (2020) concludes that resilience is a fundamental factor in expanding the sense of an integrated and dignified self. The authors stress the importance of spiritual resilience and how it involves resistance through progressive self- awareness, facilitating inner transformation. In some cases, the person feels rejected by those who profess a certain religion, this can be either through their own beliefs or because of the characteristics of the person or the community. This was consolidated in the data obtained in the surveys they received. The recognition of strengths and capacities must always be included. This allows LGTBI + older people and CALD older adults to deal with marginalization. It is essential to recognize the importance of the interventions considering the life history of the service users using PCCM as a management model. This model places an emphasis on the life history of the people and the importance of their needs. As mentioned by Nelson-Becker and Thomas (2020) , “people are resilient because they often have few other options except to despair and isolate themselves. Their tenacity to reclaim a personal sense of spirituality and find meaning in adverse situations is a testament to this resilience”.
It is vitally important to carry out interventions where older people are the center of attention. For this reason, the PCCM was established as a management model for the centers. Its realization and execution from intersectionality is of vital importance. The interventions must be carried out in the nursing homes using the PCCM, including the staff in this change so that they feel part of it. It is essential for the workers to be trained in diversity, thus reducing age discrimination, stigmas associated with religion and ethnicity and creating spaces of equality and support for emotional-sexual diversity. It should include the establishment of diverse and inclusive policies, staff diversity and sensitivity, personalized care plans, addressing it from community and family participation.
4.1 Detailed implementation strategies are crucial for the effective application of the person-centered care model (PCCM) in nursing homes
4.1.1 implementation in real time.
Implementing PCCM in real-time within nursing homes involves several steps to ensure it is practical and beneficial for residents:
a) Interdisciplinary Team Approach: Nursing homes should establish an interdisciplinary team that includes a clinical psychologist, behavioral specialist, social worker, and counselor. This team should meet with each new resident upon their arrival to develop a personalized care plan. This initial assessment should be comprehensive, considering the resident’s physical health, psychological state, social needs, and personal preferences.
b) Regular Review and Adaptation: The care plan should not be static. Regular meetings (e.g., quarterly) should be scheduled to review and adapt the care plan based on the resident’s evolving needs and preferences.
c) Training and Education: Continuous education and training for all staff members on PCCM principles and practices are essential. This training should emphasize the importance of empathy, active listening, and personalized care strategies.
4.1.2 Creating the care plan
The creation of the care plan should be a collaborative process involving multiple stakeholders:
a) Clinical Psychologist: To assess and address mental health needs, providing strategies to manage anxiety, depression, and other psychological issues.
b) Behavioral Specialist: To design behavior management plans and interventions tailored to the resident’s specific needs.
c) Social Worker: To identify and address social needs, including family dynamics, social interactions, and community engagement.
d) Counselor: To provide emotional support and counseling, helping residents cope with the transition and any personal issues.
4.1.3 Reality of personalized care in large facilities
In large nursing homes with over 100 residents, implementing and maintaining individualized care plans can indeed be challenging. However, several strategies can mitigate these challenges:
a) Delegation and Team Structure: Assigning specific residents to designated team members who are responsible for their care plan ensures accountability and continuity. This can be managed through smaller sub-teams within the larger interdisciplinary team.
b) Technology Utilization: Implementing electronic health records (EHR) and specialized software to track care plans, monitor updates, and ensure that all staff have access to up-to-date information about each resident.
c) Incremental Implementation: Start with a pilot program for a smaller group of residents, refining the process before scaling it up to the entire facility.
4.1.4 Addressing temporary and high turnover in staff
The presence of temporary staff and high turnover rates present significant barriers to consistent and personalized care:
a) Standardized Procedures: Develop detailed, standardized procedures and protocols that temporary staff can easily follow. This includes thorough documentation in the EHR that allows new staff to quickly understand each resident’s needs and preferences.
b) Orientation and Training for Temporary Staff: Implement a robust orientation program for temporary staff, focusing on the core principles of PCCM and the specific practices of the nursing home.
c) Retention Strategies: Investing in strategies to improve staff retention, such as competitive salaries, benefits, professional development opportunities, and a supportive work environment, is critical for maintaining a stable and consistent caregiving team.
4.1.5 Need for systemic reform
The current climate in many nursing homes necessitates significant reform to support such a paradigm shift:
a) Policy Advocacy: Advocate for policies that support better staffing ratios, increased funding for staff training, and incentives for nursing homes to adopt PCCM.
b) Community and Family Engagement: Engage families and the broader community in supporting nursing homes, whether through volunteer programs, donations, or advocacy efforts.
c) Continuous Improvement: Establish a culture of continuous improvement within nursing homes, where feedback from residents, families, and staff is actively sought and used to make ongoing enhancements to care practices.
In conclusion, while implementing PCCM in nursing homes presents challenges, especially in large facilities or those with high staff turnover, these challenges are not insurmountable. With a strategic approach, adequate resources, and a commitment to continuous improvement, it is possible to create a more inclusive, empathetic, and effective care environment for older adults.
4.2 Study limitations
This review has several limitations. Firstly, methodological in nature. There were many articles that could not be accessed due to their “restricted access” nature, so much information about the subject of the study has already been lost along the way. Secondly, the scarcity of published studies that evaluate results in terms of attitudes to diversity in older people, both in nursing homes and in potential users of the services.
A more exhaustive study of the literature is needed, with free access to the available literature to be able to reflect more fully the results of the articles that deal with the subject. This future line of research in turn requires the definition of a concrete and specific protocol in terms of the tools used, the number and design of the sessions and, in short, the application of an intervention in which the maximum possible number of variables that influence this type of study are controlled.
Finally, it is of interest to continue with future lines of research regarding the attitude towards diversity, along with studying the effects of the changes using the PCCM and its implications on the quality of life for older people who use the services.
Funding Statement
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
JM-F: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing–original draft, Writing–review and editing. JT-P: Data curation, Methodology, Supervision, Validation, Writing–review and editing. IE-D: Investigation, Methodology, Resources, Validation, Writing–review and editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fragi.2024.1389610/full#supplementary-material
- Boyon N. (2021). LGBT+ pride 2021 global survey. Available at: https://www.ipsos.com/en/lgbt-pride-2021-global-survey-points-generation-gap-around-gender-identity-and-sexual-attraction .
- Daley A., Brotman S., MacDonnell J. A., St Pierre M. (2020). A framework for enhancing access to equitable home care for 2SLGBTQ+ communities. Int. J. Environ. Res. public health 17 (20), 7533. 10.3390/ijerph17207533 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Emlet C. A., Fredriksen-Goldsen K. I., Kim H. J., Jung H. (2020). Accounting for HIV health disparities: risk and protective factors among older gay and bisexual men. J. aging health 32 (7-8), 677–687. 10.1177/0898264319848570 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Emlet C. A., O'Brien K. K., Fredriksen Goldsen K. (2019). The global impact of HIV on sexual and gender minority older adults: challenges, progress, and future directions. Int. J. aging and Hum. Dev. 89 (1), 108–126. 10.1177/0091415019843456 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Equala (2023). Envejecer con orgullo: Estudio sobre las personas mayores LGTBI+ en Navarra. Pamplona Gob. Navar. Available at: https://www.igualdadnavarra.es/imagenes/documentos/-500-f-es.pdf?ts=20230331081053?ts=20230331081053 . [ Google Scholar ]
- Farrell T. W., Hung W. W., Unroe K. T., Brown T. R., Furman C. D., Jih J., et al. (2022). Exploring the intersection of structural racism and ageism in healthcare. J. Am. Geriatrics Soc. 70 (12), 3366–3377. 10.1111/jgs.18105 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fredriksen-Goldsen K., Teri L., Kim H. J., La Fazia D., McKenzie G., Petros R., et al. (2023). Design and development of the first randomized controlled trial of an intervention (IDEA) for sexual and gender minority older adults living with dementia and care partners. Contemp. Clin. trials 128, 107143. 10.1016/j.cct.2023.107143 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gorodosti M. (2008). Niveles de evidencia y grados de recomendación. Available at: http://svgo.es/sites/default/files/Medicina%20basada%20en%20la%20evidencia.pdf .
- Green H., Paul M., Vidal L., Leibovic L. (2007). Prophylaxis of Pneumocystis pneumonia in immunocompromised non-HIV-infected patients: systematic review and meta-analysis of randomized controlled trials. Mayo Clin. Proc. 82 (9), 1052–1059. 10.4065/82.9.1052 [ DOI ] [ PubMed ] [ Google Scholar ]
- HelpAge Spain International (2021). El derecho a los cuidados de las personas mayores. Available at: https://www.helpage.es/helpage-espana-publica-el-informeel-derecho-a-los-cuidados-de-las-personas-mayores/ .
- Holman E. G., Landry-Meyer L., Fish J. N. (2020). Creating supportive environments for LGBT older adults: an efficacy evaluation of staff training in a senior living facility. J. Gerontological Soc. Work 63 (5), 464–477. 10.1080/01634372.2020.1767254 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hutchinson C., Cleland J., McBain C., Walker R., Milte R., Swaffer K., et al. (2022). What quality of life domains are most important to older adults in residential care? J. Aging Soc. Policy 36, 21–42. 10.1080/08959420.2022.2134691 [ DOI ] [ PubMed ] [ Google Scholar ]
- Kaplan D. B., Berkman B. J. (2022). Religión y espiritualidad en los ancianos. Manual MSD versión Prof. Available at: https://www.msdmanuals.com/es-es/professional/geriatr%C3%ADa/aspectos-sociales-en-los-ancianos/religi%C3%B3n-y-espiritualidad-en-los-ancianos . 10.20318/recs.2024.8494 [ DOI ] [ Google Scholar ]
- Klein U. (2016). Gender equality and diversity politics in higher education: conflicts, challenges and requirements for collaboration. Women’s Stud. Int. Forum. 54, 147–156. 10.1016/j.wsif.2015.06.017 [ DOI ] [ Google Scholar ]
- Morales-Rodríguez F. M. (2021). Educación transversal para la inclusión y diversidad afectivo-sexual, corporal y de género: Un proyecto de innovación docente. Rev. Estud. Investig. Psicol. Educ. 8 (2), 261–281. 10.17979/reipe.2021.8.2.8703 [ DOI ] [ Google Scholar ]
- Nash M. (2001). Multiculturalismo y género. Un estudio interdisciplinar. Available at: https://www.torrossa.com/gs/resourceProxy?an=2465532&publisher=FZW027#page=21 . 21 [ Google Scholar ]
- Nelson-Becker and Thomas M. (2020). Religious/spiritual struggles and spiritual resilience in marginalised older adults. Religions 11 (9), 431. 10.3390/rel11090431 [ DOI ] [ Google Scholar ]
- Palacios-Ceña D., Gómez-Calero C., Cachón-Pérez J. M., Velarde-García J. F., Martínez-Piedrola R., Pérez-De-Heredia M. (2016). The experience of meaningful activities understood in nursing homes? A qualitative study. Geriatic- Nurs. 37 (2), 110–115. 10.1016/j.gerinurse.2015.10.015 [ DOI ] [ PubMed ] [ Google Scholar ]
- Sánchez Barrera O., Martínez Abreu J., Florit Serrate P., Gispert Abreu E., Vila Viera M. (2019). Envejecimiento poblacional: algunas valoraciones desde la antropología. Rev. Médica Electrónica 41 (3), 708–724. Available at: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1684-18242019000300708&lng=es&tlng=es . [ Google Scholar ]
- Sharp P. M. Y., Hahn B. H. (2011). Origins of HIV and the AIDS pandemic. Col spring Harb. Perspect. Med. 1 (1), 1–23. 10.1101/cshperspect.a006841 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Villar F., Serrat R., Celdrán M., Fabà J., Martínez T., Twisk J. (2020). ‘I do it my way’: long-term care staff’s perceptions of residents’ sexual needs and suggestions for improvement in their management. Eur. J. Ageing 17 (2), 197–205. 10.1007/s10433-019-00546-6 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Villar Possada F., Celdrán M., Serrat R., Canella V. (2018). Abordando la diversidad en el envejecimiento activo: Una propuesta de clasificación/Addressing diversity in active ageing: A new classification’s proposal. Aula Abierta 47 (1), 55. 10.17811/rifie.47.1.2018.55-62 Available at: https://sid-inico.usal.es/idocs/F8/ART22036/villar_posada.pdf#:∼:text=Volumen%2047%2C%20n%C3%BAmero%201%2C%20enero-marzo%2C . [ DOI ] [ Google Scholar ]
- Ward K. T., Hess M., Wu S. (2019). Geriatric assessment in multicultural immigrant populations. Geriatrics 4 (3), 40. 10.3390/geriatrics4030040 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Willis P., Dobbs C., Evans E., Raithby M., Bishop J. A. (2020). Reluctant educators and self-advocates: older trans adults' experiences of health-care services and practitioners in seeking gender-affirming services. Health Expect. 23 (5), 1231–1240. 10.1111/hex.13104 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- World Health Organization [WHO] (2021). Global report on ageism. Available at: https://www.who.int/es/teams/social-determinants-of-health/demographic-change-and-healthy-ageing/combatting-ageism/global-report-on-ageism/ .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data availability statement.
- View on publisher site
- PDF (797.0 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
VIDEO
COMMENTS
The healthcare office should maintain diversity and inclusion across ethnic, racial, gender, religious, sexual, and other dimensions. In particular, integrating workers from racial and ethnic minorities is essential in overcoming disparities in the workplace and receiving health care (Goode & Landefeld). To do this, both leadership and the ...
Culture and diversity play a significant role in healthcare delivery and outcomes. In order to provide high-quality care to patients from various cultural backgrounds, it is crucial for healthcare professionals to understand the influence of culture and diversity in healthcare settings. This essay will explore the impact of culture and ...
The Role of Diversity in Healthcare Essay. I see the role of diversity and the inclusiveness of diverse groups in healthcare as very important. Medical institutions need to aim to increase diversity, as represented by the workforce, with people of different socio-economic backgrounds, ethnicities, races, religions, cultures, genders, and sexual ...
Equality and Diversity within Healthcare. An Essay by Emma Bushnell. Note: For the purpose of this essay I will assume Salome (from the Case Study) is a person with a protected characteristic defined by The Equality Act 2010.
Diversity in healthcare provides high-quality care for everyone by acknowledging and respecting diverse cultures, religious beliefs, genders, and socioeconomic statuses. It also empowers every patient and healthcare professional to have a voice in the type of care they receive and need. Healthcare Diversity Calendar Easy Awareness & Inclusion: 365.
preference, age, ethnicity, religion, disability, and gender identity into diversity training programs. Diversity educa-tion programs continued to evolve and multiply during the 1980s as a corporate means to meet compliance standards; the value of diversity was not yet recognized.2 The true in diversity has been increasingly.
Diversity of thought, population, and indeed methodology is necessary to develop high-quality interventions for patients and families. ... issues related to health disparities can often be found in the limitations section of research papers. For example, authors may note loss to follow up because of lack of transportation, that some groups were ...
Supporting diversity in nursing helps nurse leaders promote an open, inclusive environment that promotes teamwork, better addresses health inequities and improves patient-care provider relationships. By influencing their organization's policies and actions, encouraging open communication on their team, and supporting awareness training and ...
In the modern healthcare landscape, diversity in nursing has emerged as a crucial and highly relevant topic. The nursing profession is a cornerstone of healthcare systems worldwide, and its effectiveness hinges on the diverse perspectives, backgrounds, and experiences of its practitioners. This essay explores the multifaceted dimensions of diversity in nursing, addressing its importance ...
Journal of Best Practices in Health Professions Diversity: Research, Education, and Policy Vol. 6, No. 1, Spring 2013 Provider/Patient communication growing literature delineates the impact of sociocultural factors, race, ethnicity, and A limited-English proficiency on health and clinical care (IOM, 2003). Healthcare professionals
Cultural competence describes "the ability of systems to provide care to patients with diverse values, beliefs, and behaviors, including tailoring delivery to meet patients' social, cultural, and linguistic needs." 1. Because the term cultural competence might imply an achievement or endpoint, some experts recommend using the term ...
Diversity in health care helps ensure all backgrounds, beliefs, ethnicities, and perspectives are adequately represented in the medical field. It's about providing the best possible care for all patients. If you're interested in a career in medicine and want to gain an edge with a global perspective, then learn more by reading our article ...
Diversity is broadly defined as the inclusion of varied attributes or characteristics. In the medical community, diversity often includes healthcare professionals, trainees, educators, researchers, and patients from diverse backgrounds, including race, ethnicity, gender, disability, social class, socioeconomic status, sexual orientation, gender identity, primary spoken language, and geographic ...
Cultural Diversity In Health Care Essay. In the last twenty years, the rising number of disparities in health and healthcare has increased simultaneously with the influx of minorities within the population (Baldwin, 2003) A4. As the size of an ethnically diverse population steadily continues to increase, so will the level of complexities of ...
Better Recruitment. A commitment to diversity helps when recruiting new healthcare workers and administrative staff. It allows you to cast a wider net to attract new talent and it offers a stronger hiring proposition for candidates who may consider working at your hospital or clinic.
A recent scoping review found 37 published intervention papers with only a third including ... Mcguire M, McCauley J, et al. Racial comparisons of health care and glycemic control for African American and White diabetic adults in an urban managed care organization. ... Parker RB, Stack SJ, Schneider SM, et al. Why diversity and inclusion are ...
Diversity in healthcare encompasses a wide range of characteristics, including but not limited to race, ethnicity, gender, sexual orientation, age, disability, socioeconomic status, and cultural backgrounds among both patients and healthcare professionals. It acknowledges that individuals bring unique experiences and perspectives to the ...
Health care organizations face challenges with the initiative to increase racial diversity within the nursing workforce. Despite efforts to diversify, the 2018 Bureau of Labor and Statistics showed that amongst 3.2 million registered nurses in the United States (U.S.), 75.5% are whites, 13.1 % are Black or African- American, 9% Asian and only 7.2% are Hispanic or Latino.
This study provides a comprehensive review of existing literature to systematize information on diversity among older adults in healthcare centers and nursing homes. Out of 1.458 articles identified, 10 were analyzed in depth, revealing that addressing diversity among older adults is crucial to overall mental and physical healthy aging ...
Choose one of the communities to which you belong, and describe that community and your place within it. Example: Common Application prompt #1. Some students have a background, identity, interest, or talent that is so meaningful they believe their application would be incomplete without it.
Hire verified writer. $35.80 for a 2-page paper. Diversity requires more than knowing about individual differences and it key for overcoming cross-cultural barriers in healthcare. As cultures within the U. S. continue to grow at a huge number, the understanding of how to deal with them must also grow.