- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
- Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
- Article Critique
- Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
- Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
- Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
- Research Paper
- Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring

Culture and Cultural Safety, Essay Example
Pages: 19
Words: 5223
Hire a Writer for Custom Essay
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
Regarding the pivotal aspects of nursing, we need to mention that it includes the prevention of disease and the treatment of the patients; what is more, it also includes the promotion of healthy lifestyle. It is obvious that caring emerged to be fully interwined with the principles of nursing. Analyzing the philosophy of nursing, one can easily see that this occupation mainly requires the respect towards all the ill, not making emphasis on certain categories of people; the thing is that when you are treating the patients, it means that the key goal that you need to follow must be the one based on your undeniable craving to satisfy the patients with the qualified help. The nature of nursing has much in common with both medicine and scientific expertness. The major task is to heal the sick by preventing the disease. It is necessary to take into account the fact that since the profession of nursing is the one, going through endless process of evolving, nurses are required to be also interested in applying new practices while treating the patients. As a result, one can come to understanding that nursing is an everlasting process of studying and enrichment in new branches of knowledge.
Considering the issue of nursing, one cannot skip with the importance of cultural security as well. It is clear that cultural security emerges to be one of the most significant components within the field of nursing in New Zealand. The construct of the aforementioned issue lies in directing nursing area as ‘safe’ and ‘effective’ for the customer or family/ whanau from dissimilar culture (Richardson & MacGibbon, 2010). Obviously, cultural safety occurs as “the effective nursing practice of a person or family from another culture, and is determined by that person or family. Culture includes, but is not restricted to, age or generation; gender; sexual orientation; occupation and socioeconomic position; ethnic descent or migrant awareness; religious or spiritual belief; and disability” (Nursing Council of New Zealand [NCNZ], 2011, p.7). Apart from the above-said, cultural safety distinguishes achievement of positive health results via reorganizing the health status of New Zealanders as well as acknowledging the values, beliefs and practices of those having various cultural backgrounds (Wepa, 2004). In accordance with NCNZ (2011), any care offered by nurses that disregards and humiliates the cultural identity of an individual appears to be culturally improper act.
The major goal behind cultural security lies in improving the health status of New Zealanders; moreover, developing the provision of health and disability services by so-called culturally safe nursing workforce. On the basis of cultural safety norms, there has to be trusting negotiations between a nurse and the patient; in addition, a nurse has to demonstrate the power contacts between a nurse and the patients (NCNZ, 2011). It is worth accepting ethnicity based disparities, so that an unfair practice can be minimized. In New Zealand, the policy of Treaty of Waitangi is utilized to negotiations between Mâori and Pakeha, as well to other national minorities. The number of health disparities among the Maori people is mostly related to shortage of availability of culturally adequate health care services (Ren, 2009). To offer culturally secure treatment to people from various cultures, in contemporary nursing field health professionals tend to take into account three pivotal norms of the Treaty of Waitangi, which are relationship, participation and defence (Kingi, 2007).
Relationship occurs as cooperating together with the customer and certain community in order to improve positive health outcomes (MidCentral District Health Board [MDHB], 2008). To be precise, it is worth saying that in partnership the customers are obliged to provide informed decisions and they are also engaged in all the processes which refer to their health, disease, and care. A peculiar thing is that it is not just about engaging patients in making their choices so as to provide an anticipated decision. Being involved in partnership incorporates providing the information to patients, which is vivid and adequate in a way they are likely to understand, so they are able to make an informed choice with regards to their treatment and care as well give some questions. Trusted relationship appears when people’s problems and likes are heard and answered (NCNZ, 2012a).
Participation engages the patients in decision making process, projecting and provision of health and disability services (MDHB, 2008). Active participation of health consumers appears to be important to improve the patient’s insight as well as satisfaction with provided nursing treatment, contributing to advanced care outcomes and improvement of their health state (Sahlsten, Larsson, Sjostrom, Lindencrona and Plos, 2007). For qualified culturally safe nursing treatment and to match patient preferences, it is important for nurses to become aware of the patient’s attitude towards the issue of participation (Larsson, Sahlsten, Sjostrom, Lindencrona & Plos, 2007). Sufficient and obvious information provided by a nurse enhances the active participation of health consumers, whereas the shortage of knowledge results in obstructions to active participation (Florin, 2007).
In protection, it is significant for nurses to provide their services in a manner that appreciates and protects cultural constructs, values and principles of patients from another cultural environment (MDHB, 2008). It is also extremely vital to defend patients’ privacy, since it is likely to build the trusting relationship between them and health care experts and the patients. Privacy/confidentiality policy is not only about health records; it also applies to all other individually recognisable health data, including genetic information, clinical survey and treatment records, mental health disorder treatment notifications ,suicide notes, terminally diseased notes, patient’ personal data and also the protection of cultural beliefs. This information has to be accessible to nurses who are directly responsible for looking after the health consumers (NCNZ, 2011). To provide culturally safe treatment, health professionals are obliged to protect patients’ rights and privacy. This is the ethical and legal accountability of health care experts (NCNZ, 2011).
In the given scenario, three items which inhibit the provision of nursing care are breach of privacy and confidentiality, horizontal outrage and discrimination against and disrespect towards the health consumers. These three items are an integral part of culturally unsafe tendency, since they are ignoring the patient’s rights. “Unsafe cultural practice comprises any action which diminishes, demeans or disempowers the cultural identity and well-being of an individual” (NCNZ, 2011, p.7).
The breach of privacy of the patient’s individual details and confidentiality appears to be the most significant dimension that is impacting the delivery of proficient nursing treatment in the given scenario. The nurses are loudly advancing the arguments about their right to reject to look after a patient who, for instance, has history of sexual abuse offence. As the health consumer is directly across from the nurse’s station, there is a definite probability that he heard the communication. Also there is a possibility that other patients, attendants and allied staff participants overheard the conversation, breaching the patient’s confidentiality. In accordance with the Code of Conduct for nurses, principle five (NCNZ, 2012b), it is the duty of health professionals to defend the privacy of health consumers’ personal information. Any information related to a patient should be utilized for professional aims only. Nurses should tell the health consumers if there is need to unravel the information to other health team departments, and obtain informed consent from the patient to uncover that information. However, in case there is any serious risk to the health consumer or public safety, a decision can be made without the patient’s consent. Health consumers’ personal information or health records should be preserved securely and only accessed for the purpose of providing treatment or any legal aspects. Nurses do not have to discuss practice issues in public such as, for example, social media in order to maintain health consumers’ confidentiality and privacy. Despite the fact that the name of a health consumer might be unrevealed, still they could be identified (NCNZ, 2012b).
The nurse-patient negotiations appear to be the most important part of nursing concept. The construct of trust is one of the most significant components in the nurse-patient negotiations. It can be easily figured out as well as easily broken. A trusting nurse-patient partnership apparently depends on communication. Health consumers may like to share their problems with a health professional and may see the nurse as someone who will not judge them and unveil their personal stories with some other people. If the expectations of the patient are not answered by the health professionals, and the health consumer indicates that their information is disclosed to other members of the personnel patient’s trust along with the relationship will be broken once and for all time. On the other hand, the increase of trust partnership between patients and nurses will modify the image of nurses in society as a positive element (Said, 2013). As a result, nurses should not uncover information unless it is mandatory, such as legally or for patient care.
Another issue that is influencing professional nursing treatment in this scenario is discrimination and disregard of a patient. According to the initial principle of the Code of Conduct for nurses, health professionals should respect the dignity and individuality of health consumers (NCNZ, 2012b). This constituent vividly states that nurses should practise in a way that respect and does not discriminate against any patient from any culture, age, gender, sexual orientation and political opinion (NCNZ, 2012b). In this scenario, nurses are discriminating against the patient because he has history of sexual abuse offences. They did not think of the patient’ self-respect and about making a therapeutic relationship with him. They do not support a principle of professionalism, since they are failing to provide culturally safe care by disregarding the health consumers, as they may have overheard the conversation. Health professionals are being judgemental and unwilling to offer nursing care for these patients in the scenario, which may result in the patients’ neglect. It is the accountability of health professionals to look after the patients not showing any signs of discrimination or label (NCNZ, 2012b). Moreover, all nurses are obliged to abide standards of moral relationship and ethics, and have to be non-judgemental (New Zealand Nurses Organisation [NZNO], 2010).
The third aspect that is inhibiting the provision of professional nursing treatment in this scenario is horizontal outrage towards a new graduate nurse by instigating her not to look after the patient. Horizontal outrage originates a negative work atmosphere impairing teamwork and compromising health consumers’ care (Araujo & Sofield, 2011). Horizontal outrage occurs as any unwanted abuse, assaultive and harmful behaviour by a health rofessional or a team of nurses toward a colleague via assaultive viewpoints, actions and sayings within the workplace (Becher & Visovsky, 2012).
In this scenario, senior health professionals are demonstrating a kind of bullying as they pressurised the new graduate nurse to accept the choices of the other nurses. As a new graduate nurse, I may consider senior nurses to limit my rights to voice my attitude towards this issue In view of Kelly and Tazbir, 2013, peer pressure is one of workplace bullying divisions which is likely to compromise health consumers’ care. I am likely to feel fear, and anxiety in this case and I must agree with my senior colleagues’ ideas as I would not want to be an outcast within a new workplace. A feeling of fear, concern and separation can result in emotional disorders, which later lead to poor attentiveness and fallacies. On this phase, I am likely to ruin patient’s security. Workplace bullying results in stress, hazardous culturally nursing actions and improper partnership with health consumers and team members (Yildrim, 2009). In accordance with the Code of Conduct’s sixth principle, health professionals have to work honestly with colleagues and in a co-operative way in order to match health consumers’ requirements (NCNZ, 2012b).
Health professionals have to be capable of showing their skills and judgement to cope with professional, lawful and ethical accountabilities dimensions and competent enough to recognize an atmosphere that is culturally tolerant in respect of health consumers (NCNZ, 2012c). After what took place in the scenario, being a registered health professional, I figured out that senior nurses maintain improper nursing acts that are not culturally hazardous for health consumers and the nurses. They are breaching the confidentiality and disregarding the health consumers. What is more, there is also horizontal outrage towards a new nurse as senior nurses encourage her to maintain their choices. In such a case, I have accountability as a registered nurse to follow professional principles of nursing practice in order to provide the patients’ safety.
The senior health professionals are violating the confidentiality of the patient’s individual data. They are rejecting to provide health care services for a health consumer who possesses history of sexual abuse offences. The health professionals are obliged to defend and honour the confidentiality of health consumers’ individual information especially about sensitive issues (Privacy commissioner, 2008). In such a case, initially I will shut the door as a health consumer is close to the nursing station. Furthermore, I will tell the health professionals about this, since health consumers are likely to expect that their information will not be shared with the other people. During treatment period, health professionals reassure the health consumer that their information will be protected (NCNZ, 2012b). By loudly communicating about the health consumer’s criminal history, health professionals are breaching the norms of trust. What is more, I will care for this health consumer by obeying professional principles of nursing practice and reassure patient’s security and quality treatment. Evidently, there is high probability that other health consumers, allied personnel and attendant are likely to have overheard the communication. They emerge to be likely to start disrespecting the health consumer that compromises the patient’s safety, respectively. It is the accountability of health professionals to indicate, inform and deal with the cases that impact health consumer and the members of personnel (NCNZ, 2012c) Nurses are responsible for their practice as well as the choices so they have to perform ethically (NCNZ, 2012c).
In the scenario, health professionals are also humiliating and disregarding the health consumer, since they are thought to be involved in sexual abuse offences. It appears to be the right of the health consumer to be treated with respect; the patient also has the right to complain (Health and Disability Commissioner [HDC], 2009). In such a case, as I am aware that health consumer may have heard the communication. I will provide him with an opportunity to fill a complaint form in case he/she wants; I will also fill the incident form and inform to the charge health professional, since it is compulsory to take some measures. Health professionals have to figure out the legal aspects in the practice and report on this matter to the appropriate people. Health professionals must serve in accordance with relevant legislation/norms/principles and follow health consumers’ rights (NCNZ, 2012c). Disregard/humiliation in respect of the health consumer by health care personnel is very vexing for the health consumer. It is a threat to health consumers’ security and health, since it inhibits patient’s agreement with health care. Usually, people like to commit suicides in case they have low self-esteem; this factor emerges to be extremely depressing for them. It is so destructive for health consumers and their family (Leape, Shore & Dienstag, 2012). Consequently, it is my accountability as a registered health professional to keep health consumers safe by looking after them.
In the given scenario, I have to keep myself safe from horizontal outrage from senior health professionals. Horizontal outrage is likely to result in depression, fear and seriously lowered self-esteem that will lead to poor nursing practice and interpersonal negotiations (Longo, 2010). First of all, I will follow my accountabilities in accordance with lawful and ethical limits by recognizing health consumers’ rights as well providing culturally safe treatment to them. I will also report it as at the earliest convenience after the incident took place. Health professionals have to keep clear and straightforward notes, any entries in health consumers’ notes have to be mentioned, dated and timed. Health consumers are obliged to make certain that all health consumers’ notes are preserved securely for their confidentiality (NCNZ, 2012 b). Being a registered health professional, I should be conscious about my rights, practices and principles of hospital for workplace bullying for my safety, and to master the ability to deal with these cases. Health professionals have to become aware about the workplace protocols in order to manage the issue of outrage acts and keep themselves safe, respectively (Murray, 2009). What is more, I will request help and explanation from the charge health professional and nurse instructor. I will also fill an incidence form on horizontal outrage. It is extremely significant to report incident to charge health professional (Longo, 2010).
The workplace principles in healthcare system appear to the matter of great importance for individual-centred clinically efficient treatment, whereas, an improper workplace atmosphere results in dramatic impact on the health situation (Manley, Sanders, Cardiff & Webster, 2011). The alterations I would be eager to initiate are preventing horizontal outrage, embodying inter-professional cooperation and advanced performance. To deliver these modifications in workplace environment, I chose Kurt Lewin management approach.
The Kurt Lewin’s management model consists of three phases, which are unfreezing, moving and refreezing (Mclean, 2011). In the first phase of modification (unfreezing), a problem is indicated and measures are prepared in order to accept that alteration. This very phase also encloses breaking the current approaches to working before constructing a new principle of performance (Mcgarry, Cashin & Fowler, 2012). The further phase is the process in which modification is embodied (Huber, 2014). It is important in this process to be sure that new methods of practising can provide more positive results than the existing ways (Chang & Daly, 2012). The final phase (refreezing) is utilized for evaluation of new modifications for its efficacy (Sutherland, 2013).
The first change I am eager to make is how to avoid horizontal outrage. Horizontal outrage, or destructive behaviours between nursing personnel, can result in enormous harm to health consumers and the personnel security as well as wellbeing (Longo, 2010). In the scenario, I think that senior health professionals make me accept their decisions and they are not permitting me to encapsulate my attitude towards particular issues; obviously, it is bullying. In the unfreezing stage, new graduate health professionals have to be aware of zero tolerance principles on bullying (Sayre, 2010). Each individual possesses the right to have a workplace that is fair; each person has the right to be treated with some reverence (NCNZ, 2012c). The clinical manager has a significant role to create a harmonious atmosphere which is based on a high level of proficiency with no signs of no bullying (Cleary, Hunt, Walter & Robertson, 2009). The moving stage is the embodiment of the project, so in this stage, personnel will be taught about strict zero tolerance principles in the workplace environment and the significance of teamwork, which is likely to lead to gradual prevention of horizontal outrage and confusions (Ekici & Beder, 2014). Health professionals have to be educated how to preserve regard and dignity of other members of the personnel taking into consideration culture distinctions (Rocker, 2008). During the refreezing phase, management and health professionals have to estimate the efficacy of rearrangement (Sayre, 2010). It is extremely significant to become aware of whether the modifications have either positive or negative influence (Clarkson, Flores, Johnson & Lonadier, 2012).
The second transformation would be the embodiment of inter-professional cooperation. Efficient inter-professional partnership is an integral element of nursing. It is the cooperation between the members of personnel, health consumers and their families in an honest and accountable way. This facilitates the process of building trust amongst the health consumers (Barwell, Arnold & Berry, 2013). Efficient cooperation between health professionals care personnel is vital for health consumers’ safety and person-centered treatment. As a result, they can express their viewpoints about patient’s health state, care options for necessary health outcomes (Nadzam, 2009). In this scenario, instead of supporting professional cooperation, health professionals are loudly discussing the reluctance to look after the health consumers. To provide quality treatment that is patient-cantered and culturally adequate, health professionals have to take into account the issue of professional negotiations (Arnold & Boggs, 2011).
In the initial stage of Lewin’s change management model, health professionals have to be addressed by responsible nurse or clinical manager concerning their improper cooperation that is worth being improved. Within the moving stage, unprofessional cooperation can be settled on a solution by ongoing teaching policies. The hospital principles also facilitate the process of health professionals’ understanding of the need to cooperate, since one of the reasons behind inappropriate language is the shortage of professional skills (Wachtel, 2011). During the refreezing process, health professionals will assess their learning from teaching projects and keep obeying the guidelines of the nursing practice. Positive cooperation impacts the efficacy of health consumers’ treatment and makes the performance of the teamwork much better (Sully & Dallas, 2010).
The third amendment would be efficient teamwork, since it possesses a critical factor in nursing practice (West, 2012). Effectual teamwork is important for the highly qualified and safe health consumers’ treatment. It makes nursing practice more efficient and improves final outcomes. Moreover, it helps the personnel to become aware of their peers (Ward, 2013). In this scenario, I come to understanding that there is no maintenance and co-operation between health professionals; they cannot come to mutual agreement. In the unfreezing stage, health professionals have to master the significance of understanding, cooperation with each other. Formal education projects are likely to assist in learning the way of collaboration in the workplace. Health professionals are obligated to become aware of the way how the shortage of teamwork between the staff members can lead to a negative influence on health consumers (Barwell et al., 2013). In the moving stage, health professionals will pass ongoing teaching programmed based on effectual teamwork. In the final stage, health professionals will estimate their awareness of the programmer.
The factors showing my nursing practice are cultural expertise, person-centered clinical supervision, health consumers’ feedback and the utilization of the the principles of the Treaty of Waitangi. Clinical monitoring occurs as very helpful for health professionals in proficient maintenance as well as learning how to become accountable for their individual performance. Clinical inspection is regarded as one of the best methods helping new graduate health professionals in offering culturally risk-free nursing treatment to health consumers (Rassool, 2008). Their performance can be closely inspected by a clinical manager who can recommend the junior personnel whether the treatment offered was culturally harmless or not (Hole, 2009). In other words, to reach culturally secure treatment in nursing practice, any comments, viewpoints, and assumptions from a clinical inspector are very useful (Chang & Daly, 2012). Being a new graduate health professional, I will request feedback and some comments from a clinical inspector in order to find out whether I provide culturally risk-free practice or not; these feedbacks are likely to help me rearrange my future performance. Clinical inspection emerges to be very important and for the nurses (Dawson, Phillips & Legget, 2012); it is likely to help junior personnel to undergo various problems whilst practicing as well (Lynch, Hancox, Happel, & Parker, 2009).
Feedback from health consumers is really helpful to the health professionals to assess the treatment offered. In accordance with NCNZ (2012c), expertises (1.5 and 2.6), efficacy of nursing care can be evaluated on the basis of health consumers’ feedback, since it is not the health professionals, or team members, it is the customer who receives the treatment (McMurray & Clendon, 2010). Thus, I will request feedback and comments from my clients to make certain that the treatment I offer was actually culturally secure. Once health consumers cannot provide feedback, I will ask another family member to answer my request. I will also provide therapeutic partnership with health consumers. Good collaboration and trust are extremely significant when building an effective therapeutic communication (Richard & Tabatha, 2010).
To assure culturally secure practice and patient-centered treatment, the awareness of the three principles of Treaty of Waitangi, which are partnership, participation and protection cannot be underestimated (NCNZ, 2011). Therefore, I will show these fundamental components during my nursing practice by constructing the cooperation with the health consumers and their family members; I will also demonstrate my striving to instigate them to take part in decision making process as well as care planning for successful health results. By accomplishing these steps, I will get to know their health and disease state in a more detailed way. For instance, I can find out if the clients are allergic to any remedy and. I will also take into consideration their rights of confidentiality, regard, reported consent and informed decisions. Moreover, I will ensure the health consumers that I follow the privacy and confidentiality principles. I will honour their values and beliefs. For instance, in some religions, meat is not permitted to eat; and if I ignore the patients’ traditions, I will demonstrate my disrespect. As a result, I need to be aware of the health consumers’ meals’ choices, pray peculiarities, clothing and other dimensions. I should esteem all cultures, customs, values and beliefs in order to provide highly-qualified nursing practice. All the aforementioned strategies are likely to assist in demonstrating that my practice occurs as culturally secure.
Naturally, the issue of discrimination in nursing is likely to affect both sexes, involving the unfair determination or decision making based on person’s gender as well as racial identity. Some modern scientists report that almost fifteen percent of patients suffer from discrimination while being treated by nurses. There exists the biased practice that different ethnicities are estimated in accordance with their viewpoints; moreover, the nurses tend to take into consideration the appearance of their patients, disregarding the norms ethics and human rights.
In conclusion, although the issue of discrimination in nursing is responded by the implementation of the number of anti-discrimination laws, it still can be faced in many today’s hospitals. This discrimination is typical of both sexes: males and females. The sex discrimination in nursing can be traumatic to human psyche. The person can be psychologically and emotionally destroyed when he or she is discriminated by the nurse. Apart from that, the sex as well as racial discrimination provides the misbalance within the nursing staff and usually results in unhealthy environment. The negative interaction between departments and the increased number of conflicts may contribute badly to the hospital performance. Despite the existence of gender and race discrimination in many hospitals, there should always be given adequate attention by means of regulatory laws. The point is that in case gender or race discrimination act happens, one should never leave it yet use the complete set of laws to support ourselves.
R eferences
Araujo, S., & Sofield, L. (2011). Workplace Violence in Nursing Today. The Nursing Clinics of North America, 46(4), 457-464.
Arnold, E., & Boggs, K. U. (2011). Interpersonal relationships: Professional communication skills for nurses (6th ed.). St Louis, MO: Saunders-Elsevier.
Barwell, J., Arnold, F., & Berry, H. (2013). How Interprofessional Learning Improves Care. Nursing Times, 10(21), 14-16.
Becher, J., & Visovsky, C. (2012). Horizontal Violence in Nursing. Medsurg Nursing , 21(4), 210-232.
Chang, E., & Daly, L. (2012). Transitions in Nursing: Preparing for Professional Practice . Chatswood, Australia: Elsevier.
Clarkson, L., Flores, A., Johnson, C., & Lonadier, R. (2012). Horizontal Violence in Nursing Affecting Nurse Retention. Retrieved from http://claudettejohnson.weebly.com/uploads/2/1/4/2/21425962/research_team_purple_week_8_paper-_final.pdf
Cleary, M., Hunt, G. E., Walter, G., & Robertson, M., (2009). Dealing with Bullying in the Workplace Towards Zero Tolerance. Journal of Psychosocial Nursing, 47(12), 34-41.
Dawson, M., Phillips, B., & Leggat, S. G. (2012). Effective Clinical Supervision for Regional Allied Health Professionals: The Supervisee’s Perspective. Australian Health Review, 36, 92–97.
Ekici, D., & Beder, A. (2014). The Effects of Workplace Bullying on Physicians and Nurses. Australian Journal of Advanced Nursing, 31(4), 24-33.
Health and Disability Commissioner. (2009). The HDC Code of Health and Disability Services Consumers’ Rights Regulation 1996. Retrieved from http://www.hdc.org.nz/the-act–code/the-code-of-rights/the-code-(full)
Hole, J. (2009). The Newly Qualified Nurse’s Survival Guide (2nd ed.). Chichester, United Kingdom: Radcliffe publishing.
Huber, D. (2014). Leadership and Nursing care Management (5th ed.). St Loius, MO: Elsevier.
Kelly, P., & Tazbir, J. (2013). Essentials of Leadership and Management (3rd ed.) Sydney, Australia: Cengage Learning.
Kingi, T. R. (2007). The Treaty of Waitangi: A Framework for Maori health development. New Zealand Journal of Occupational Therapy , 54(1), 4-10.
Larsson, I. E., Sahlsten, M. J. M., Segesten, K., & Plos, K. A. E. (2011). Patients’ Perceptions of Nurses’ Behaviour That Influence Patient Participation in Nursing Care: A Critical Incident Study . Journal of Nursing Research and Practice , 1-8.
Leape, L. L., Shore, M. F., Dienstag, J. L., Mayer, R. J., Edgman-Levitan, S., Meyer, G. S., & Healy, G. B. (2012). Perspective: A Culture of Respect, part 1: The Nature and Causes of Disrespectful Behavior by Physicians. Academic Medicine, 87(7), 845-852.
Longo, J., (2010). Combating Disruptive Behaviors: Strategies to Promote a Healthy Work Environment. The Online Journal of Issues in Nursing, 15(1), 1.
Lynch, L., Hancox, L., Happel, B., Parker, J. (2009). Clinical Supervision for Nurses. Chichester, United Kingdom: Wiley Blackwell.
Manley, K., Sanders, K., Cardiff, S., & Webster, J. (2011). Effective Workplace Culture: The Attributes, Enabling Factors and Consequences of a New Concept. International Practice Development Journal , 1(2), 1-29.
Mcgarry, D., Cashin, A., & Fowler, C. (2012). Child and Adolescent Psychiatric Nursing and the ‘Plastic Man’: Reflections on the Implementation of Change Drawing Insights from Lewin’s Theory of Planned Change. Contemporary Nurse, 41(2), 263-270.
Mclean, C., (2011). Change and Transition: What Is the Difference? British Journal of School Nursing , 6(2), 78-81.
McMurray, A., & Clendon, J. (2010). Community Health and Wellness: Primary Health care in Nursing. Sydney, Australia: Elsevier.
MidCentral District Health Board. (2014). Nursing Entry to Practice (NETP) programme handbook: Acute and specialty practice. Retrieved from http://www.midcentraldhb.govt.nz/WorkingMDHB/CareerInformation/Nursing/Documents/MCH_NETP_Learning_framework_2014.pdf
Murray, J. S. (2009). Workplace Bullying in Nursing: A Problem that Can’t Be Ignored. Medsurg Nursin g, 18(5), 273-276.
Nadzam, D. M. (2009). Nurses’ Role in Communication and Patient Safety. Journal of Nursing Care Quality , 24(3), 184-188.
Nursing Council of New Zealand. (2011). Guidelines for Cultural Safety, the Treaty of Waitangi, and Maori Health in Nursing Education and Practice. Wellington, New Zealand: Author.
Nursing Council of New Zealand. (2012a). Nursing Council of NZ’s Draft Code of Conduct. Wellington, New Zealand: Author.
Nursing Council of New Zealand. (2012b). Code of Conduct for Nurses. Wellington, New Zealand: Author.
Nursing Council of New Zealand. (2012c). Competencies for Registered Nurses. Wellington, New Zealand: Author.
New Zealand Nurses Organisation. (2010 ). Code of Ethics: Towards Improving Health Outcomes in New Zealand. Wellington, New Zealand: Author.
Privacy commissioner. (2008). Health Information Privacy Code 1994 . Retrieved from https://privacy.org.nz/assets/Files/Codes-of-Practice-materials/HIPC-1994-incl.-amendments-revised-commentary.pdf
Ren, X. (2009). Reaping the Benefits of a Treaty of Waitangi Workshop. Kai Tiaki Nursing New Zealand , 15(7), 28-29.
Richardson, F., & MacGibbon, L. (2010). Cultural safety: Nurses’ Accounts of Negotiating the Order of Things. Women’s Studies Journal , 24(2), 54-65.
Richard, P. L. & Tabatha, M. (2010). Fostering Therapeutic Nurse-Patient Relationships. Journal of Nursing , 8(3), 4-9.
Said, N. B. (2013 ). Nurse-Patient Trust Relationship . Retrieved from www.researchgate.net/…NursePatient_Trust_Relationship/…/0c9605162…
Sayre, M. M. (2010 ). Improving Collaboration and Patient Safety by Encouraging Nurse to Speak up: Overcoming Personal and Organisational Obstacles through Self-Reflection. Los Angeles, CA: UCLA.
Sully, P., & Dallas, J. (2010). Essential Communication Skills for Nursing and Midwifery. London, United Kingdom: Elsevier.
Sutherland, K. (2013). Applying Lewin’s Change Management Theory to the Implementation of Bar-Coded Medication Administration. Canadian Journal of Nursing Informatics, 8(1), 1-6.
Wachtel, L. P. (2011). Therapeutic Communication: Knowing What to Say When (2nd ed.). New York, NY: Guilford Press.
Ward, J. (2013). The Importance of Teamwork in Nursing.
West, M. A. (2012). Effective Teamwork: Practical Lessons from Organizational Research (3 rd ed.). Chichester, United Kingdom: BPS Blackwell.
Yildrim, D. (2009). Bullying among Nurses and Its Effects . International Nursing Review, 56,504-511.
Stuck with your Essay?
Get in touch with one of our experts for instant help!
Marjane’s Interaction With Western Culture, Essay Example
America: The New World in Transition, Essay Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Essay Samples & Examples
Voting as a civic responsibility, essay example.
Pages: 1
Words: 287
Utilitarianism and Its Applications, Essay Example
Words: 356
The Age-Related Changes of the Older Person, Essay Example
Pages: 2
Words: 448
The Problems ESOL Teachers Face, Essay Example
Pages: 8
Words: 2293
Should English Be the Primary Language? Essay Example
Pages: 4
Words: 999
The Term “Social Construction of Reality”, Essay Example
Words: 371
The Cultural Safety Concept: Gibbs’ Reflective Cycle Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Description of the theory of cultural safety, distinguishing characteristics of cultural safety.
Cultural safety has a particularly important place for consideration in many spheres of human activity. This concept implies an awareness of the importance of culture in shaping individuals’ experiences of health and healthcare. In other words, it relies on the understanding that medical services should be provided with the cultural beliefs, values, and practices of various patients in mind. In addition, the concept of cultural safety implies taking into account the historical and modern context in which a particular community is located.
Particular importance should be given to the discussion of cultural safety’s three tenets. The first of these is the balance of power, which is based on the unequal distribution of authority between healthcare providers and patients. This is especially critical for those communities that are considered marginalized or oppressed. Within this aspect, cultural safety implies addressing this problem in healthcare and providing patients with the opportunity to be educated in the field of medical services (Curtis et al., 2019). Thus, they will be able to make informed decisions about their health on their own.
The second tenant becomes cultural humility, which implies the ability of medical professionals to realize the possible cultural biases that they have. The identification of these indicators will make it possible to provide the most comprehensive care to patients and strengthen diversity and inclusion in healthcare (Curtis et al., 2019). Moreover, it will help in creating a more open and respectful environment in the healthcare organization. The third tenant is anti-opposition, which draws attention to systemic opposition and discrimination (Curtis et al., 2019). The main negative effect of this aspect is the deterioration of conditions for receiving health services from marginalized communities. Cultural Security aims to continue work to counteract these negative effects. This initiative is represented through advocacy for policies and practices that promote equity and inclusion.
To gain a better understanding of what cultural security is, it is important to know how it differs from two more commonly used terms in the U.S.: cultural humility and cultural competence. These terms can often be confused due to the fact that they all relate to phenomena in healthcare such as diversity, equity, and inclusion. The leading difference between cultural security and cultural humility and cultural competence is that it focuses on creating an environment where patients from diverse cultural backgrounds and experiences feel safe and secure (Curtis et al., 2019). On the other hand, humanity and competence focus on the healthcare provider’s ability to be self-reflective and have the knowledge and skills to care for patients from different cultures effectively. Another difference in cultural security is the emphasis on issues that exist in society. It focuses on the systemic opposition and discrimination that marginalized communities experience in modern society. Thus, it makes an attempt to transform the healthcare system on a larger and global level.
In conclusion, cultural safety has a valuable place in the field of healthcare. This phenomenon contributes to the limitation of such negative consequences of marginalization and oppression of cultural minorities as discrimination and prejudice. This contributes to strengthening aspects such as diversity and inclusion, which have a critical role in expanding the availability of health services. In the work of nurses, cultural safety is necessary to ensure that all patients receive care that is respectful, equitable, and culturally responsive to their needs.
Curtis, E., Jones, R., Tipene-Leach, D., Walker, C., Loring, B., Paine, S. J., & Reid, P. (2019). Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition . International Journal for Equity in Health, 18 (1), 1-17. Web.
- Nursing: Caregivers of Elderly Patients
- Nursing Care Theories: Henderson’s Theory
- "The Epic of Gilgamesh" by Ryan Gibbs
- The Topic of Diagnostic Measures
- Ethos, Pathos and Logos in "The Exploitation" by Adam Rulli-Gibbs
- Psychological Concerns Among Oncology Nurses
- Innovative Changes in New Jersey's Nursing Program
- The Issue of the Medication Errors
- The Concept of Cultural Relativism in Nursing
- A Path to Achieve Health Equity
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 11). The Cultural Safety Concept: Gibbs' Reflective Cycle. https://ivypanda.com/essays/the-cultural-safety-concept-gibbs-reflective-cycle/
"The Cultural Safety Concept: Gibbs' Reflective Cycle." IvyPanda , 11 Feb. 2024, ivypanda.com/essays/the-cultural-safety-concept-gibbs-reflective-cycle/.
IvyPanda . (2024) 'The Cultural Safety Concept: Gibbs' Reflective Cycle'. 11 February.
IvyPanda . 2024. "The Cultural Safety Concept: Gibbs' Reflective Cycle." February 11, 2024. https://ivypanda.com/essays/the-cultural-safety-concept-gibbs-reflective-cycle/.
1. IvyPanda . "The Cultural Safety Concept: Gibbs' Reflective Cycle." February 11, 2024. https://ivypanda.com/essays/the-cultural-safety-concept-gibbs-reflective-cycle/.
Bibliography
IvyPanda . "The Cultural Safety Concept: Gibbs' Reflective Cycle." February 11, 2024. https://ivypanda.com/essays/the-cultural-safety-concept-gibbs-reflective-cycle/.
- Open access
- Published: 14 November 2019
Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition
- Elana Curtis ORCID: orcid.org/0000-0002-9957-7920 1 ,
- Rhys Jones 1 ,
- David Tipene-Leach 2 ,
- Curtis Walker 3 ,
- Belinda Loring 1 ,
- Sarah-Jane Paine 1 &
- Papaarangi Reid 1
International Journal for Equity in Health volume 18 , Article number: 174 ( 2019 ) Cite this article
373k Accesses
534 Citations
178 Altmetric
Metrics details
Eliminating indigenous and ethnic health inequities requires addressing the determinants of health inequities which includes institutionalised racism, and ensuring a health care system that delivers appropriate and equitable care. There is growing recognition of the importance of cultural competency and cultural safety at both individual health practitioner and organisational levels to achieve equitable health care. Some jurisdictions have included cultural competency in health professional licensing legislation, health professional accreditation standards, and pre-service and in-service training programmes. However, there are mixed definitions and understandings of cultural competency and cultural safety, and how best to achieve them.
A literature review of 59 international articles on the definitions of cultural competency and cultural safety was undertaken. Findings were contextualised to the cultural competency legislation, statements and initiatives present within Aotearoa New Zealand, a national Symposium on Cultural Competence and Māori Health, convened by the Medical Council of New Zealand and Te Ohu Rata o Aotearoa – Māori Medical Practitioners Association (Te ORA) and consultation with Māori medical practitioners via Te ORA.
Health practitioners, healthcare organisations and health systems need to be engaged in working towards cultural safety and critical consciousness. To do this, they must be prepared to critique the ‘taken for granted’ power structures and be prepared to challenge their own culture and cultural systems rather than prioritise becoming ‘competent’ in the cultures of others. The objective of cultural safety activities also needs to be clearly linked to achieving health equity. Healthcare organisations and authorities need to be held accountable for providing culturally safe care, as defined by patients and their communities, and as measured through progress towards achieving health equity.
Conclusions
A move to cultural safety rather than cultural competency is recommended. We propose a definition for cultural safety that we believe to be more fit for purpose in achieving health equity, and clarify the essential principles and practical steps to operationalise this approach in healthcare organisations and workforce development. The unintended consequences of a narrow or limited understanding of cultural competency are discussed, along with recommendations for how a broader conceptualisation of these terms is important.
Introduction
Internationally, Indigenous and minoritorised ethnic groups experience inequities in their exposure to the determinants of health, access to and through healthcare and receipt of high quality healthcare [ 1 ]. The role of health providers and health systems in creating and maintaining these inequities is increasingly under investigation [ 2 ]. As such, the cultural competency and cultural safety of healthcare providers are now key areas of concern and issues around how to define these terms have become paramount, particularly within a Aotearoa New Zealand (NZ) context [ 3 ]. This article explores international literature to clarify the concepts of cultural competency and cultural safety in order to better inform both local and international contexts.
In NZ, Māori experience significant inequities in health compared to the non-Indigenous population. In 2010–2012, Māori life expectancy at birth was 7.3 years less than non-Māori [ 4 ] and Māori have on average the poorest health status of any ethnic group in NZ [ 5 , 6 ]. Although Māori experience a high level of health care need, Māori receive less access to, and poorer care throughout, the full spectrum of health care services from preventative to tertiary care [ 7 , 8 ]. This is reflected in lower levels of investigations, interventions, and medicines prescriptions when adjusted for need [ 8 , 9 ]. Māori are consistently and significantly less likely to: get understandable answers to important questions asked of health professionals; have health conditions explained in understandable terms; or feel listened to by doctors or nurses [ 10 ]. The disturbing health and social context for Māori and significant inequities across multiple health and social indicators described above provide the ‘needs-based’ rationale for addressing Māori health inequities [ 8 ]. There are equally important ‘rights-based’ imperatives for addressing Indigenous health and health equity [ 11 ], that are reinforced by the United Nations Declaration on the Rights of Indigenous Peoples [ 12 ] and Te Tiriti o Waitangi (Treaty of Waitangi) in NZ.
There are multiple and complex factors that drive Indigenous and ethnic health inequities including a violent colonial history that resulted in decimation of the Māori population and the appropriation of Māori wealth and power, which in turn has led to Māori now having differential exposure to the determinants of health [ 13 ] [ 14 ] and inequities in access to health services and the quality of the care received. Framing ethnic health inequities as being predominantly driven by genetic, cultural or biological differences provides a limited platform for in-depth understanding [ 15 , 16 ]. In addition, whilst socio-economic deprivation is associated with poorer health outcomes, inequities remain even after adjusting for socio-economic deprivation or position [ 17 ]. Health professionals and health care organisations are important contributors to racial and ethnic inequities in health care [ 2 , 13 ]. The therapeutic relationship between a health provider and a patient is especially vulnerable to the influence of intentional or unintentional bias [ 18 , 19 ] leading to the “paradox of well-intentioned physicians providing inequitable care [ 20 ]. Equitable care is further compromised by poor communication, a lack of partnership via participatory or shared decision-making, a lack of respect, familiarity or affiliation and an overall lack of trust [ 18 ]. Healthcare organisations can influence the structure of the healthcare environment to be less likely to facilitate implicit (and explicit) bias for health providers. Importantly, it is not lack of awareness about ‘the culture of other groups’ that is driving health care inequities - inequities are primarily due to unequal power relationships, unfair distribution of the social determinants of health, marginalisation, biases, unexamined privilege, and institutional racism [ 13 ]. Health professional education and health institutions therefore need to address these factors through health professional education and training, organisational policies and practices, as well as broader systemic and structural reform.
Eliminating Indigenous and ethnic health inequities requires addressing the social determinants of health inequities including institutional racism, in addition to ensuring a health care system that delivers appropriate and equitable care. There is growing recognition of the importance of cultural competency and cultural safety at both individual health practitioner and organisational levels to achieve equitable health care delivery. Some jurisdictions have included cultural competency in health professional licensing legislation [ 21 ], health professional accreditation standards, and pre-service and in-service training programmes [ 22 , 23 , 24 , 25 ]. However, there are mixed definitions and understandings of cultural competency and cultural safety, and how best to achieve them. This article reviews how concepts of cultural competency and cultural safety (and related terms such as cultural sensitivity, cultural humility etc) have been interpreted. The unintended consequences of a narrow or limited understanding of cultural competency are discussed, along with recommendations for why broader conceptualisation of these terms is needed to achieve health equity. A move to cultural safety is recommended, with a rationale for why this approach is necessary. We propose a definition for cultural safety and clarify the essential principles of this approach in healthcare organisations and workforce development.
Methods and positioning
This review was originally conducted to inform the Medical Council of New Zealand, in reviewing and updating its approach to cultural competency requirements for medical practitioners in New Zealand Aotearoa. The review and its recommendations are based on the following methods:
An international literature review on cultural competency and cultural safety.
A review of cultural competency legislation, statements and initiatives in NZ, including of the Medical Council of New Zealand (MCNZ).
Inputs from a national Symposium on Cultural Competence and Māori Health, convened for this purpose by the MCNZ and Te Ohu Rata o Aotearoa – Māori Medical Practitioners Association (Te ORA) [ 26 ].
Consultation with Māori medical practitioners (through Te ORA).
The authors reflect expertise that includes Te ORA membership, membership of the Australasian Leaders in Indigenous Medical Education (LIME) (a network to ensure the quality and effectiveness of teaching and learning of Indigenous health in medical education), medical educationalist expertise and Indigenous medical practitioner and public health medicine expertise across Australia and NZ. This experience has been at the forefront of the development of cultural competency and cultural safety approaches within NZ. The analysis has been informed by the framework of van Ryn and colleagues [ 27 ] which frames health provider behaviour within a broader context of societal racism. They note the importance of shifting “ the framing of the problem, from ‘the impact of patient race’ to the more accurate ‘impact of racism’….on clinician cognitions, behaviour, and clinical decision making” [ 27 ].
This review and analysis has been conducted from an Indigenous research positioning that draws from Kaupapa Māori theoretical and research approaches. Therefore, the positioning used to undertake this work aligns to effective Kaupapa Māori research practice that has been described by Curtis (2016) as: transformative; beneficial to Māori; under Māori control; informed by Māori knowledge; aligned with a structural determinants approach to critique issues of power, privilege and racism and promote social justice; non-victim-blaming and rejecting of cultural-deficit theories; emancipatory and supportive of decolonisation; accepting of diverse Māori realities and rejecting of cultural essentialism; an exemplar of excellence; and free to dream [ 28 ].
The literature review searched international journal databases and the grey literature. No year limits were applied to the original searching. Databases searched included: Medline, Psychinfo, Cochrane SR, ERIC, CINAHL, Scopus, Proquest, Google Scholar, EbscoHost and grey literature. Search terms included MeSH terms of cultural competence (key words: cultural safety, cultural awareness, cultural competence, cultural diversity, cultural understanding, knowledge, expertise, skill, responsiveness, respect, transcultural, multicultural, cross-cultur*); education (key words: Educat*, Traini*, Program*, Curricul*, Profession*, Course*, Intervention, Session, Workshop, Skill*, Instruc*, program evaluation); Health Provider (key words: provider, practitioner, health professional, physician, doctor, clinician, primary health care, health personnel, health provider, nurse); Health Services Indigenous (key words: health services Indigenous, ethnic* Minorit*, Indigenous people*, native people). A total of 51 articles were identified via the search above and an additional 8 articles were identified via the authors’ opportunistic searching. A total of 59 articles published between 1989 and 2018 were used to inform this review. Articles reviewed were sourced from the USA, Canada, Australia, NZ, Taiwan and Sweden (Additional file 1 Table S1).
In addition to clarifying concepts of cultural competence and cultural safety, a clearer understanding is required of how best to train and monitor for cultural safety within health workforce contexts. An assessment of the availability and effectiveness of tools and strategies to enhance cultural safety is beyond the scope of this review, but is the subject of a subsequent review in process.
Reviewing cultural competency
Cultural competency is a broad concept that has various definitions drawing from multiple frameworks. Overall, this concept has varying interpretations within and between countries (see Table 1 for specific examples). Introduced in the 1980s, cultural competency has been described as a recognised approach to improving the provision of healthcare to ethnic minority groups with the aim of reducing ethnic health disparities [ 31 ].
One of the earliest [ 49 ] and most commonly cited definitions of cultural competency is sourced from a 1989 report authored by Cross and colleagues in the United States of America [ 29 ] (p.13):
Cultural competence is a set of congruent behaviours, attitudes, and policies that come together in a system, agency, or among professionals and enable that system, agency, or those professionals to work effectively in cross-cultural situations.
Cross et al. [ 29 ] contextualized cultural competency as part of a continuum ranging from the most negative end of cultural destructiveness (e.g. attitudes, policies, and practices that are destructive to cultures and consequently to the individuals within the culture such as cultural genocide) to the most positive end of cultural proficiency (e.g. agencies that hold culture in high esteem, who seek to add to the knowledge base of culturally competent practice by conducting research and developing new therapeutic approaches based on culture). Other points along this continuum include: cultural incapacity , cultural blindness and cultural pre-competence (Table 1 ).
By the time that cultural competency became to be better understood in the late 1990s, there had been substantial growth in the number of definitions, conceptual frameworks and related terms [ 31 , 50 , 51 , 52 ]. Table 1 provides a summary of the multiple, interchangeable, terms such as: cultural awareness ; cultural sensitivity ; cultural humility ; cultural security ; cultural respect ; cultural adaptation ; and transcultural competence or effectiveness . Unfortunately, this rapid growth in terminology and theoretical positioning(s), further confused by variations in policy uptake across the health sector, reduced the potential for a common, shared understanding of what cultural competency represents and therefore what interventions are required. Table 2 outlines the various definitions of cultural competency from the literature.
Cultural competence was often defined within an individually-focused framework, for example, as:
the ability of individuals to establish effective interpersonal and working relationships that supersede cultural differences by recognizing the importance of social and cultural influences on patients, considering how these factors interact, and devising interventions that take these issues into account [ 53 ] (p.2).
Some positionings for cultural competency have been critiqued for promoting the notion that health-care professionals should strive to (or even can) master a certain level of functioning, knowledge and understanding of Indigenous culture [ 61 ]. Cultural competency is limited when it focuses on acquiring knowledge, skills and attitudes as this infers that it is a ‘static’ level of achievement [ 58 ]:
“cultural competency” is frequently approached in ways which limit its goals to knowledge of characteristics, cultural beliefs, and practices of different nonmajority groups, and skills and attitudes of empathy and compassion in interviewing and communicating with nonmajority groups. Achieving cultural competence is thus often viewed as a static outcome: One is “competent” in interacting with patients from diverse backgrounds much in the same way as one is competent in performing a physical exam or reading an EKG. Cultural competency is not an abdominal exam . It is not a static requirement to be checked off some list but is something beyond the somewhat rigid categories of knowledge, skills, and attitudes ( p.783).
By the early 2000s, governmental policies and cultural competency experts [ 50 , 54 ] had begun to articulate cultural competency in terms of both individual and organizational interventions, and describe it with a broader, systems-level focus, e.g.:
the ability of systems to provide care to patients with diverse values, beliefs and behaviours, including tailoring delivery to meet patients’ social, cultural, and linguistic needs [ 54 ] (p. v).
Moreover, some commentators began to articulate the importance of critical reflection to cultural competency. For example, Garneau and Pepin [ 55 ] align themselves more closely to the notion of cultural safety when they describe cultural competency as:
a complex know-act grounded in critical reflection and action, which the health care professional draws upon to provide culturally safe, congruent, and effective care in partnership with individuals, families, and communities living health experiences, and which takes into account the social and political dimensions of care [ 55 ] (p. 12).
Reviewing cultural safety
A key difference between the concepts of cultural competency and cultural safety is the notion of ‘power’. There is a large body of work, developed over many years, describing the nuances of the two terms [ 34 , 36 , 38 , 43 , 46 , 49 , 59 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 ]. Similar to cultural competency, this concept has varying interpretations within and between countries. Table 3 summarises the definitions and use of cultural safety from the literature. Cultural safety foregrounds power differentials within society, the requirement for health professionals to reflect on interpersonal power differences (their own and that of the patient), and how the transfer of power within multiple contexts can facilitate appropriate care for Indigenous people and arguably for all patients [ 32 ].
The term cultural safety first was first proposed by Dr. Irihapeti Ramsden and Māori nurses in the 1990s [ 74 ], and in 1992 the Nursing Council of New Zealand made cultural safety a requirement for nursing and midwifery education [ 32 ]. Cultural safety was described as providing:
a focus for the delivery of quality care through changes in thinking about power relationships and patients’ rights [ 32 ] . (p.493).
Cultural safety is about acknowledging the barriers to clinical effectiveness arising from the inherent power imbalance between provider and patient [ 65 ]. This concept rejects the notion that health providers should focus on learning cultural customs of different ethnic groups. Instead, cultural safety seeks to achieve better care through being aware of difference, decolonising, considering power relationships, implementing reflective practice, and by allowing the patient to determine whether a clinical encounter is safe [ 32 , 65 ] .
Cultural safety requires health practitioners to examine themselves and the potential impact of their own culture on clinical interactions. This requires health providers to question their own biases, attitudes, assumptions, stereotypes and prejudices that may be contributing to a lower quality of healthcare for some patients. In contrast to cultural competency, the focus of cultural safety moves to the culture of the clinician or the clinical environment rather than the culture of the ‘exotic other’ patient.
There is debate over whether cultural safety reflects an end point along a continuum of cultural competency development, or, whether cultural safety requires a paradigm shift associated with a transformational jump in cultural awareness. Dr. Irihapeti Ramsden [ 75 ] originally described the process towards achieving cultural safety in nursing and midwifery practice as a step-wise progression from cultural awareness through to cultural sensitivity and on to cultural safety. However, Ramsden was clear that the terms cultural awareness and cultural sensitivity were separate concepts and that they were not interchangeable with cultural safety. Despite some authors interpreting Ramsden’s original description of cultural safety as involving three steps along a continuum [ 35 ] other authors view a move to cultural safety as more of a ‘paradigm shift’ [ 63 ]:
where the movement from cultural competence to cultural safety is not merely another step on a linear continuum, but rather a more dramatic change of approach. This conceptualization of cultural safety represents a more radical, politicized understanding of cultural consideration, effectively rejecting the more limited culturally competent approach for one based not on knowledge but rather on power [ 63 ]. (p.10).
Regardless of whether cultural safety represents movement along a continuum or a paradigm shift, commentators are clear that the concept of cultural safety aligns with critical theory, where health providers are invited to “examine sources of repression, social domination, and structural variables such as class and power” [ 71 ] (p.144) and “social justice, equity and respect” [ 76 ] (p.1). This requires a movement to critical consciousness, involving critical self-reflection: “ a stepping back to understand one’s own assumptions, biases, and values, and a shifting of one’s gaze from self to others and conditions of injustice in the world.” [ 58 ] (p.783).
Why a narrow understanding of cultural competency may be harmful
Unfortunately, regulatory and educational health organisations have tended to frame their understanding of cultural competency towards individualised rather than organisational/systemic processes, and on the acquisition of cultural-knowledge rather than reflective self-assessment of power, priviledge and biases. There are a number of reasons why this approach can be harmful and undermine progress on reducing health inequities.
Individual-level focused positionings for cultural competency perpetuate a process of “othering”, that identifies those that are thought to be different from oneself or the dominant culture. The consequences for persons who experience othering include alienation, marginalization, decreased opportunities, internalized oppression, and exclusion [ 77 ]. To foster safe and effective health care interactions, those in power must actively seek to unmask othering practices [ 78 ].
“Other-focused” approaches to cultural competency promote oversimplified understandings of other cultures based on cultural stereotypes, including a tendency to homogenise Indigenous people into a collective ‘they’ [ 79 ]. This type of cultural essentialism not only leads to health care providers making erroneous assumptions about individual patients which may undermine the provision of good quality care [ 31 , 53 , 58 , 63 , 64 ], but also reinforces a racialised, binary discourse, used to repeatedly dislocate and destabilise Indigenous identity formations [ 80 ]. By ignoring power, narrow approaches to cultural competency perpetuate deficit discourses that place responsibility for problems with the affected individuals or communities [ 81 ], overlooking the role of the health professional, the health care system and broader socio-economic structures. Inequities in access to the social determinants of health have their foundations in colonial histories and subsequent imbalances in power that have consistently benefited some over others. Health equity simply cannot be achieved without acknowledging and addressing differential power, in the healthcare interaction, and in the broader health system and social structures (including in decision making and resource allocation) [ 82 ].
An approach to cultural competency that focuses on acquiring knowledge, skills and attitudes is problematic because it suggests that competency can be fully achieved through this static process [ 58 ]. Cultural competency does not have an endpoint, and a “tick-box” approach may well lull practitioners into a falsely confident space. These dangers underscore the importance of framing cultural safety as an ongoing and reflective process, focused on ‘critical consciousness’. There will still be a need for health professionals to have a degree of knowledge and understanding of other cultures, but this should not be confused with or presented as efforts to address cultural safety. Indeed, as discussed above, this information alone can be dangerous without deep self-reflection about how power and privilege have been redistributed during those processes and the implications for our systems and practice.
By neglecting the organisational/systemic drivers of health care inequities, individual-level focused positionings for cultural competency are fundementally limited in their ability to impact on health inequities. Healthcare organisations influence health provider bias through the structure of the healthcare environment, including factors such as their commitment to workforce training, accountability for equity, workplace stressors, and diversity in workforce and governance [ 27 ]. Working towards cultural safety should not be viewed as an intervention purely at the level of the health professional – although a critically conscious and empathetic health professional is certainly important. The evidence clearly emphasises the important role that healthcare organisations (and society at large) can have in the creation of culturally safe environments [ 31 , 32 , 46 , 60 , 69 ]. Cultural safety initiatives therefore should target both individual health professionals and health professional organisations to intervene positively towards achieving health equity.
Perhaps not surprisingly, the concept of cultural safety is often more confronting and challenging for health institutions, professionals, and students than that of cultural competency. Regardless, it has become increasingly clear that health practitioners, healthcare organisations and health systems all need to be engaged in working towards cultural safety and critical consciousness. To do this, they must be prepared to critique the ‘taken for granted’ power structures and be prepared to challenge their own culture, biases, privilege and power rather than attempt to become ‘competent’ in the cultures of others.
Redefining cultural safety to achieve health equity
It is clear from reviewing the current evidence associated with cultural competency and cultural safety that a shift in approach is required. We recommend an approach to cultural safety that encompasses the following core principles:
Be clearly focused on achieving health equity, with measureable progress towards this endpoint;
Be centred on clarified concepts of cultural safety and critical consciousness rather than narrow based notions of cultural competency;
Be focused on the application of cultural safety within a healthcare systemic/organizational context in addition to the individual health provider-patient interface;
Focus on cultural safety activities that extend beyond acquiring knowledge about ‘other cultures’ and developing appropriate skills and attitudes and move to interventions that acknowledge and address biases and stereotypes;
Promote the framing of cultural safety as requiring a focus on power relationships and inequities within health care interactions that reflect historical and social dynamics.
Not be limited to formal training curricula but be aligned across all training/practice environments, systems, structures, and policies.
We recommend that the following definition for cultural safety is adopted by healthcare organisations:
“Cultural safety requires healthcare professionals and their associated healthcare organisations to examine themselves and the potential impact of their own culture on clinical interactions and healthcare service delivery. This requires individual healthcare professionals and healthcare organisations to acknowledge and address their own biases, attitudes, assumptions, stereotypes, prejudices, structures and characteristics that may affect the quality of care provided. In doing so, cultural safety encompasses a critical consciousness where healthcare professionals and healthcare organisations engage in ongoing self-reflection and self-awareness and hold themselves accountable for providing culturally safe care, as defined by the patient and their communities, and as measured through progress towards acheiveing health equity. Cultural safety requires healthcare professionals and their associated healthcare organisations to influence healthcare to reduce bias and achieve equity within the workforce and working environment”.
In operationalising this approach to cultural safety, organisations (health professional training bodies, healthcare organisations etc) should begin with a self-review of the extent to which they meet expectations of cultural safety at a systemic and organizational level and identify an action plan for development. The following steps should also be considered by healthcare organisations and regulators to take a more comprehensive approach to cultural safety:
Mandate evidence of engagement and transformation in cultural safety activities as a part of vocational training and professional development;
Include evidence of cultural safety (of organisations and practitioners) as a requirement for accreditation and ongoing certification;
Ensure that cultural safety is assessed by the systematic monitoring and assessment of inequities (in health workforce and health outcomes);
Require cultural safety training and performance monitoring for staff, supervisors and assessors;
Acknowledge that cultural safety is an independent requirement that relates to, but is not restricted to, expectations for competency in ethnic or Indigenous health.
Cultural competency, cultural safety and related terms have been variably defined and applied. Unfortunately, regulatory and educational health organisations have tended to frame their understanding of cultural competency towards individualised rather than organisational/systemic processes, and on the acquisition of cultural-knowledge rather than reflective self-assessment of power, priviledge and biases. This positioning has limited the impact on improving health inequities. A shift is required to an approach based on a transformative concept of cultural safety, which involves a critique of power imbalances and critical self-reflection.
We propose principles and a definition for cultural safety that addresses the key factors identified as being responsible for ethnic inequities in health care, and which we therefore believe is fit for purpose in Aotearoa New Zealand and internationally. We hope this will be a useful starting point for users to further reflect on the work required for themselves, and their organisations, to contribute to the creation of culturally safe environments and therefore to the elimination of Indigenous and ethnic health inequities. More work is needed on how best to train and monitor for cultural safety within health workforce contexts.
Availability of data and materials
Not applicable.
Abbreviations
Leaders in Indigenous Medical Education network
Medical Council of New Zealand
Aotearoa New Zealand
Te Ohu Rata o Aotearoa – Māori Medical Practitioners Association
Anderson I, et al. Indigenous and tribal peoples’ health (the lancet–Lowitja Institute global collaboration): a population study. Lancet. 2016;388(10040):131–57.
Article PubMed Google Scholar
Smedley B, Stith A, Nelson A. Eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. 2002. National Academy Press: Washington.
Pigou, P. and N. Joseph, Programme Scope: Cultural competence, partnership and health equity . 2017, New Zealand Medical Council of New Zealand and Te Ohu Rata O Aotearoa: Wellington. p. 1–9.
Statistics New Zealand. Life Expectancy . NZ Social Indicators 2015 [cited 2016 January 7]; Available from: http://www.stats.govt.nz/browse_for_stats/snapshots-of-nz/nz-social-indicators/Home/Health/life-expectancy.aspx .
Jansen P, Jansen D. Māori and health , in Cole's medical practice in New Zealand , I.M. St George, editor. 2013. Medical Council of New Zealand: Wellington.
Ministry of Health, Tatau Kahukura: Māori Health Chart Book . 2006, Ministry of Health: Wellington.
Davis P, et al. Quality of hospital care for Maori patients in New Zealand: retrospective cross-sectional assessment. Lancet. 2006;367(9526):1920–5.
Ministry of Health, Tatau Kahukura: Māori Health Chart Book 2015 (3rd edition) . 2015, Ministry of Health: Wellington.
Metcalfe S, et al. Te Wero tonu-the challenge continues: Māori access to medicines 2006/07-2012/13 update. - PubMed - NCBI. N Z Med J. 2018;131(1485):27–47.
PubMed Google Scholar
Health Quality & Safety Commission, A Window on the Quality of New Zealand’s Health Care 2017. 2017, Wellington, New Zealand: Health Quality & Safety Commission.
Reid P, et al. Achieving health equity in Aotearoa: strengthening responsiveness to Māori in health research. The New Zealand Medical Journal. 2017;130(1465):96–103.
United Nations. United Nations Declaration on the Rights of Indigenous peoples , U. Nations, editor. 2008. United Nations: Geneva.
Robson B, Harris R. Eds. Hauora: Māori Standards of Health IV. A study of the years 2000-2005 . 2007. Te Rōpū Rangahau Hauora a Eru Pōmare: Wellington.
World Health Organisation, Commission on Social Determinants of Health. Final report . 2008, World Health Organization: Geneva.
Reid, P. and B. Robson, Understanding Health Inequities , in Hauora: Māori Standards of Health IV. A study of the years 2000–2005 , B. Robson and R. Harris, Editors. 2007, Te Rōpū Rangahau Hauora a Eru Pōmare: Wellington. p. 3–10.
Krieger, N., Theories for social epidemiology in the 21st century: an ecodocial perspective. Int J Epidemiol, 2001: p. 668–677.
Reid P, Robson B, Jones CP. Disparities in health: common myths and uncommon truths. Pacific Health Dialog. 2000;7(1):38–47.
CAS PubMed Google Scholar
Cooper L, et al. Delving below the surface. Understanding how race and ethnicity influence relationships in health care. J Gen Intern Med. 2006;21(Suppl. 1):21–7.
Article Google Scholar
van Ryn M, Fu S. Paved with good intentions: do public health and human service providers contribute to racial/ethnic disparities in health? Am J Public Health. 2003;93(2):248–55.
Article PubMed PubMed Central Google Scholar
van Ryn M, Saha S. Exploring unconscious Bias in disparities research and medical education. J Am Med Assoc. 2011;306(9):995–6.
Google Scholar
Health Practitioners Competence Assurance Act 2003 , in 2003 No 48 . 2003: New Zealand.
Canadian Nurses Association, Position statement: promoting culturally competent care . 2004, Canadian nurses association,. Ottawa.
Medical Council of New Zealand, Statement on cultural competence . 2006, Medical Council of New Zealand: Wellington.
Medical Board of Australia, Good medical practice: a code of conduct for doctors in Australia. . 2014, Medical Board of Australia.
Nursing Council of New Zealand, Guidelines for Cultural Safety, the Treaty of Waitangi and Maori Health in Nursing Education and Practice . 2011, Nursing Council of New Zealand,.
Reid, P. and R. Jones, Cultural Competence and Māori Health. MCNZ/Te ORA Cultural Competence Symposium held on 17th November 2017 (powerpoint) . 2017: Wellington.
van Ryn M, et al. The impact of racism on clinician cognition, behavior, and clinical decision making. Du Bois Review: Social Science Research on Race. 2011;8(1):199–218.
Curtis E. Indigenous positioning in health research: the importance of Kaupapa Māori theory informed practice. AlterNative: An International Journal of Indigenous Peoples. 2016;12(4):396.
Cross, T., B. Bazron, and M. lsaccs, Towards a Culturally Competent System of Care: A Monograph on Effective Services for Minority Children Who Are Severely Emotionally Disturbed. CASSP technical assistance Centre. Washington DC: Georgetown University Child Development Center; 1989.
Ramsden, I., Cultural Safety and Nursing Education in Aotearoa and Te Waipounamu. A thesis submitted to the Victoria University of Wellington in fulfilment of the requirements for the degree of Doctor of Philosophy in Nursing , in Department of Nursing . 2002, Victoria University of Wellington Wellington. p. 211.
Truong M, Paradies Y, Priest N. Interventions to improve cultural competency in healthcare: a systematic review of reviews. BMC Health Serv Res. 2014;14:99.
Papps E, Ramsden I. Cultural safety in nursing: the New Zealand experience. Int J Qual Health Care. 1996;8(5):491–7.
Article CAS PubMed Google Scholar
Alizadeh S, Chavan M. Cultural competence dimensions and outcomes: a systematic review of the literature. Health & Social Care in the Community. 2016;24(6):e117–30.
Darroch F, et al. The United States does CAIR about cultural safety: examining cultural safety within indigenous health contexts in Canada and United States. J Transcult Nurs. 2017;28(3):269–77.
Eriksson, C. and L. Eriksson, Inequities in health care: lessons from New Zealand : A qualitative interview study about the cultural safety theory . 2017. p. 31.
Milne, T., D.K. Creedy, and R. West, Development of the Awareness of Cultural Safety Scale: A pilot study with midwifery and nursing academics. Nurse Education Today, 2016. 44(Supplement C): p. 20–25.
Tervalon M, Murray-García J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved. 1998;9(2):117–25.
McLennan V, et al. Creating culturally safe vocational rehabilitation services for indigenous Australians: a brief review of the literature. Australian Journal of Rehabilitation Counselling. 2016;22(2):93–103.
Hook JN, et al. Cultural humility: measuring openness to culturally diverse clients. J Couns Psychol. 2013;60(3):353–66.
Miller S. Cultural humility is the first step to becoming global care providers. JOGNN - Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2009;38(1):92–3.
Phiri J, Dietsch E, Bonner A. Cultural safety and its importance for Australian midwifery practice. Collegian. 2010;17(3):105–11.
Downing R, Kowal E, Paradies Y. Indigenous cultural training for health workers in Australia. Int J Qual Health Care. 2011;23(3):247–57.
Grote E. Principles and practices of cultural competency: a review of the literature. Indigenous Higher Education Advisory Council (IHEAC), Australian Government, Department of Education Employment and Workplace Relations: Canberra; 2008.
Healey P, et al. Cultural adaptations to augment health and mental health services: a systematic review. BMC Health Serv Res. 2017;17(1):1–26.
Gibbs KA. Teaching student nurses to be culturally safe: can it be done? J Transcult Nurs. 2005;16(4):356–60.
Kirmayer LJ. Rethinking cultural competence. Transcultural Psychiatry. 2012;49(2):149–64.
Blanchet-Cohen, N. And C. Richardson/Kinewesquao, Foreword: fostering cultural safety across contexts. AlterNative: An International Journal of Indigenous Peoples, 2017. 13(3): p. 138–141.
Wepa D. An exploration of the experiences of cultural safety educators in New Zealand: an action research approach. J Transcult Nurs. 2003;14(4):339–48.
Shen Z. Cultural competence models and cultural competence assessment instruments in nursing: a literature review. J Transcult Nurs. 2015;26(3):308–21.
Horvat L, et al. Cultural competence education for health professionals. Cochrane Database Syst Rev. 2014;5:CD009405.
Lin CJ, Lee CK, Huang MC. Cultural competence of healthcare providers: a systematic review of assessment instruments. J Nurs Res. 2017;25(3):174–86.
Leininger M. Culture care theory: a major contribution to advance transcultural nursing knowledge and practices. J Transcult Nurs. 2002;13(3):189–92.
Beach MC, et al. Cultural competence: a systematic review of health care provider educational interventions. Med Care. 2005;43(4):356–73.
Betancourt J, Green A, Carillo J. Cultural Competence in Health Care: Emerging Frameworks and Practical Approaches . 2002. The Commonwealth Fund: New York.
Garneau AB, Pepin J. Cultural competence: a constructivist definition. J Transcult Nurs. 2015;26(1):9–15.
Betancourt J, et al. Cultural competence and health care disparities: key perspectives and trends. Health Aff. 2005;24(2):499–505.
Maier-Lorentz MM. Transcultural nursing: its importance in nursing practice. J Cult Divers. 2008;15(1):37–43.
Kumagai A, Lypson M. Beyond cultural competence: critical consciousness, social justice, and multicultural education. Acad Med. 2009;84(6):782–7.
Ratima M, Waetford C, Wikaire E. Cultural competence for physiotherapists: reducing inequalities in health between Maori and non-Maori. N Z J Physiother. 2006;34(3):153–9.
DeSouza R. Wellness for all: the possibilities of cultural safety and cultural competence in New Zealand. J Res Nurs. 2008;13(2):125–35.
Duke, J.A.N., M. Connor, And R. McEldowney, Becoming a culturally competent health practitioner in the delivery of culturally safe care: a process oriented approach Journal of Cultural Diversity, 2009. 16(2): p. 40–49.
Ringer J. Cultural safety and engagement: keys to improving access to care. Healthcare Management Forum. 2017;30(4):213–7.
Brascoupé, S. And C.B.a.M.a. waters, Cultural Safety: Exploring the Applicability of the Concept of Cultural Safety to Aboriginal Health and Community Wellness. J Aborig Health, 2009. 5(2): p. 6–41.
Polaschek NR. Cultural safety: a new concept in nursing people of different ethnicities. J Adv Nurs. 1998;27:452–7.
Laverty M, McDermott DR, Calma T. Embedding cultural safety in Australia’s main health care standards. Med J Aust. 2017;207(1):15–6.
Richardson, A., J. Yarwood, and S. Richardson, Expressions of cultural safety in public health nursing practice. Nurs Inq, 2017. 24(1).
Wilson D, Neville S. Culturally safe research with vulnerable populations. Contemp Nurse. 2009;33(1):69–79.
Blanchet Garneau, A., et al., Applying cultural safety beyond Indigenous contexts: Insights from health research with Amish and Low German Mennonites. Nurs Inq, 2018. 25(1).
Main C, McCallin A, Smith N. Cultural safety and cultural competence: what does this mean for physiotherapists? N Z J Physiother. 2006;34(3):160–6.
Rowan, M.S., et al., Cultural competence and cultural safety in Canadian Schools of Nursing: A mixed methods study. Int J Nurs Educ Scholarsh, 2013. 10(1).
Doutrich D, et al. Cultural safety in New Zealand and the United States: looking at a way forward together. J Transcult Nurs. 2012;23(2):143–50.
McGough S, Wynaden D, Wright M. Experience of providing cultural safety in mental health to aboriginal patients: a grounded theory study. Int J Ment Health Nurs. 2018;27(1):204–13.
Browne A, Varcoe C, Smye V, Reimer-Kirkham S, Lynam J, Wong S. Cultural safety and the challenges of translating critically oriented knowledge in practice. Nurs Philos. 2009;10:167–79.
Ramsden, I., Towards cultural safety , in Cultural Safety in Aotearoa New Zealand. Second edition , D. Wepa, Editor. 2015, Cambridge University Press: Melbourne. p. 5–25.
Ramsden I. Cultural Safety and Nursing Education in Aotearoa and Te Waipounamu , in Nursing . Victoria University of Wellington: Wellington; 2002.
McGough, S., D. Wynaden, and M. Wright, Experience of providing cultural safety in mental health to aboriginal patients: a grounded theory study . International Journal of Mental Health Nursing, 2017.
Canales MK. Othering: toward an understanding of difference. Adv Nurs Sci. 2019;22(4):16–31.
Johnson JL, et al. Othering and being othered in the context of health care services. - PubMed - NCBI. Health Commun. 2019;16(2):255–71.
MacNaughton G, Davis K. Beyond 'Othering': rethinking approaches to teaching young Anglo-Australian children about indigenous Australians; 2001.
McGrath S. Binary discourses and 'othering' indigenous Australians; 2017.
Fogarty W, et al. Deficit discourse and indigenous health: how narrative framings of aboriginal and Torres Strait islander people are reproduced in policy. Melbourne: The Lowitja Institute; 2018.
Givens, M., et al., Power: the Most fundamental cause of health inequity? . Health Affairs Blog, 2018.
Download references
Acknowledgements
BJ Wilson (for undertaking the original literature searching), Matire Harwood (for early oversight of the literature review searching undertaken by BJ Wilson), Te ORA members who reviewed the original Te ORA contract report.
Some of the data sources used to inform this article were funded via a MCNZ contract with Te ORA (i.e. literature review, symposium and review of MCNZ resources). Both the MCNZ and Te ORA pre-agreed to allow the submission of internal contractual work outputs to peer-reviewed journals.
Author information
Authors and affiliations.
Te Kupenga Hauora Māori, Faculty of Medical and Health Sciences, University of Auckland, Auckland, New Zealand
Elana Curtis, Rhys Jones, Belinda Loring, Sarah-Jane Paine & Papaarangi Reid
Faculty of Education, Humanities and Health Sciences, Eastern Institute of Technology, Napier, New Zealand
David Tipene-Leach
Te Kaunihera Rata of Aotearoa, Medical Council of New Zealand, Wellington, New Zealand
Curtis Walker
You can also search for this author in PubMed Google Scholar
Contributions
EC led the overall manuscript design and development, reviewed and analysed the literature on the concepts of cultural competency and cultural safety and drafted the Introduction, Methods and Positioning, Reviewing Cultural Competency, Reviewing Cultural Safety (and associated tables) and Redefining Cultural Safety to Achieving Health Equity sections within the manuscript. RJ provided background cultural safety expertise, reviewed the original Te ORA contract work and reviewed the manuscript design/development and contributed to draft manuscripts. DTL provided background cultural safety expertise and leadership of the Te ORA contract work that led to this manuscript, reviewed the manuscript design/development and contributed to draft manuscripts. CW provided background cultural safety expertise and leadership of the MCNZ and Te ORA contract work that led to this manuscript, reviewed the manuscript design/development and contributed to draft manuscripts. BL reviewed the manuscript design/development and contributed to draft manuscripts with specific input provided for the Abstract, Why a Narrow Understanding of Cultural Competency May Be Harmful and Conclusion sections of the manuscript. SJP provided supervision of the literature review design and analysis, reviewed the manuscript design/development and contributed to draft manuscripts. PR provided background cultural safety expertise, reviewed the original Te ORA contract work and reviewed the manuscript design/development and contributed to draft manuscripts. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Elana Curtis .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: table s1..
Summary of evidence sources identified from the literature review.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Curtis, E., Jones, R., Tipene-Leach, D. et al. Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. Int J Equity Health 18 , 174 (2019). https://doi.org/10.1186/s12939-019-1082-3
Download citation
Received : 21 June 2019
Accepted : 31 October 2019
Published : 14 November 2019
DOI : https://doi.org/10.1186/s12939-019-1082-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cultural safety
- Cultural competency
- Disparities
International Journal for Equity in Health
ISSN: 1475-9276
- General enquiries: [email protected]
Cultural Competency/Humility/Safety Reflection Paper
Introduction.
The ability of healthcare practitioners to comprehend the specific cultural needs of their patients and to offer appropriate care in accordance with those requirements is referred to as “cultural competence.” Cultural competence is an essential part of providing medical care. Providers of medical care need to adopt a strategy that is culturally sensitive and takes into account, as well as respects, the beliefs, values, and practices of their patients (Jongen et al.,2018). Providing care that considers a patient’s culture is essential since it improves their trust, contentment, and overall outcomes. In addition, it is essential to note that cultural humility, another essential component of cultural competence, refers to the capacity to keep an open and flexible attitude toward differences in cultural norms and continuously self-reflect on one’s preconceived notions and biases. It is essential to note that cultural humility. The purpose of this paper is to critically reflect on a cultural situation or incident that occurred during my clinical placement, apply the fundamental concepts of cultural competence and humility to the situation, and explore the implications of cultural competence for the healthcare system, the nursing profession, patient outcomes, and future nursing practice. This paper will also apply the fundamental concepts of cultural competence and humility to the situation.
Clinical Situation
During my night shift at NURS 450 clinical placement, I provided care for a 53-year-old Indigenous woman, Lily (Pseudonym), who was brought into the emergency room by the EMS following a suicide attempt. Lily lost her husband a year ago, and it was his first anniversary of death. Lily had a long history of mental health-related issues, including 22 years of depression. Lily was agitated and fearful as she was refusing to speak to the health care staff at first. She had some disorganized ideas, such as accidentally falling out of a window or getting eaten by wild animals at the hospital. Lily attempted suicide by trying to hang herself. Lily was put in a room in the unit and was given a call bell in case she needed anything.
The physician consulted the psychiatrist on call to come to assess the patient for possible admission to the mental health unit. The psychiatrist asked for the patient’s name and history, however, after reading her name, the psychiatrist told the nurses that Lily is a “frequent flyer” and is well known to the mental health unit. Once psychiatrists evaluated the patient, the psychiatrist decided to discharge the patient with a prescription for two new medications. Once the psychiatrist was done evaluating Lily, I advocated for the patient by speaking to the psychiatrist about the patient’s current situation. The psychiatrist said the Government of Canada and the health care system try to help Indigenous people, but it’s on them that they don’t want to do better for themselves. System-wide change begins with every individual that works in health by implementing the protocol of cultural safety and humility. First Nations are a part of the system-wide change by taking ownership of their health and wellness journeys (FNHA’s policy statement on Cultural Safety and humility). The psychiatrist wasn’t too worried about the patient and discharged her with a prescription for 2 new antipsychotic medications.
During the same shift, the EMS brought the patient to the emergency room again with a polysubstance overdose from the new medications prescribed that morning. When the patient came back with EMS, the psychiatrist was called to come in again. At this time, the healthcare team (RN, student, physician, and psychiatrist) had a brief discussion regarding patient care, and they were able to review their judgments, biases, actions, and choices that ultimately led to increased accountability, safe patient care, and promoting patient health.
This patient was indigenous, and there are many stigmas regarding Indigenous people and mental health-related issues. Indigenous people are often nervous when talking to nurses, possibly due to fear of being judged. Discrimination against the Indigenous population in the healthcare system has been a significant issue for a long time.
In the 1950s, the government of Canada established a national healthcare system to ensure that all Canadians had access to the appropriate medical and hospital treatment they needed. (Lavoie, 2018). The federal government safeguards the health care plan, but the respective provincial governments manage the health and social services themselves. Yet, because the federal government is responsible for Indians who are recognized as such under the Indian Act, implementing this proposal is not in the best interest of the indigenous population. Because the responsibility for providing medical and social services lies with the provincial government, indigenous groups on reserves are forced to endure hardship.
Madeleine Leininger recognized the significance of compassionate cultural care as an essential component in nursing. Leininger made this observation on the nursing profession while working as a nurse. She found that nursing needed the cultural and care expertise essential in inpatient care to support patients’ well-being. The goal of Leininger’s Culture Care Theory is to provide culturally competent nursing care by means of supportive, facilitative, and empowering actions that are generally tailored to meet the cultural preferences, beliefs, and lifestyles of individuals, groups, or organizations (Seamon, 2019). In order for the nurse to discover the cultural care values and expressions concerning kinship (social), religion, and philosophy, as well as political and legal, technological, economic, and educational care and health factors, the nurse must maintain an extremely active listening, observing, and participating role with cultural informants. According to the Culture Care Theory, nursing is a humanistic profession that focuses on compassionate care and caring activities to encourage, promote, and educate patients to maintain their health in culturally meaningful ways. This understanding of nursing is grounded in the Culture Care Theory (Foronda, 2019).
Care and cultural values that are right for the patient can be evaluated to synchronize Madeleine Leininger’s culture care theory into practice in healthcare. It’s all in how the nurse deals with, treats, and helps the patient. Providing culturally compatible care with or appropriate to the patient’s culture is one way to accomplish integration. The nurses will benefit from this approach since it allows them to address patient concerns from the patient’s own cultural perspective. At the time of admission, the nurses should evaluate any culturally-specific home remedies the patient may have been using and decide whether or not to incorporate them into the patient’s regular treatment. Healthcare services that rely on western medicine and traditional public health techniques often ignore the social and economic factors that significantly impact individuals’ health, and they seldom modify their practices to account for cultural norms(Curtis et al., 2019). Integrating spiritual practices into care has been shown to affect health outcomes positively. Including the patient’s loved ones, with their permission, can provide them with emotional support while also demonstrating respect for the patient’s culture. And if the patient is resistant to a certain treatment, the nurse can still adjust without betraying their values by creating a cultural care plan. The nurse-patient interaction might benefit from a superficial familiarity with a patient’s culture.
Implications of Cultural Humility/Competency/Safety In;
the health system.
Improved health outcomes for culturally varied people are one of the implications of cultural humility, cultural competence, and cultural safety in the health care system. Reducing healthcare inequities, improving patient satisfaction, and enhancing provider-patient communication and relationships are the means through which this goal can be accomplished. Language obstacles, cultural beliefs, and access to care are only some of the social determinants of health that can be addressed with the help of cultural humility and safety practices (Hughes et al., 2019). These factors all have an effect on health outcomes. Another benefit of cultivating cultural humility, competence, and safety within the Health Care System is that it encourages a more varied and inclusive culture in the workplace. Understanding and appreciating cultural diversity among healthcare professionals and staff contributes to a more positive work environment, which in turn leads to a reduced staff turnover rate. Also, it has been demonstrated that healthcare personnel who are culturally competent suffer fewer incidences of burnout, which ultimately results in a higher quality of care being offered to patients.
In the context of interprofessional care and cooperation, having cultural humility, competence, and safety has extra implications, one of which is that it improves communication, coordination, and collaboration among team members (Slim & Reuter-Yuill, 2021). Providers who demonstrate cultural humility and safety are more able to comprehend the perspectives and experiences of their colleagues, which in turn fosters a more collaborative and successful approach to patient care. This ultimately results in better patient outcomes and more effective utilization of available resources.
The Nursing Profession
Nursing is a discipline that professes to address the human person holistically, focusing on all person dimensions: body, mind, and spirit (Lemmer, 2005). Care of the spirit is a professional nursing responsibility and an intrinsic part of holistic nursing. The holistic nursing perspective requires nurses to view each person as a biopsychosocial being with a spiritual core. These nurses must be sure to address the spirit and other dimensions to provide holistic care.
The implication of cultural humility/competency/safety for the nursing profession is that it fosters tremendous respect for the diversity of patients and their cultures. Culturally competent nurses can establish a rapport with their patients, which leads to better communication, trust, and respect. This, in turn, leads to increased patient satisfaction and adherence to treatment plans, which ultimately improves health outcomes. Another implication of cultural humility/competency/safety for the nursing profession is that it promotes self-reflection and continued learning. Culturally competent nurses recognize the need for ongoing education and training to address the needs of diverse patient populations. They engage in reflective practice and seek feedback from patients, colleagues, and other healthcare providers to continually improve their cultural competence.
Patient Outcomes
Promoting patient-centred care is one of the implications of cultural humility, cultural competence, and cultural safety for patient outcomes. When providing care, culturally competent practitioners place the patient’s values, beliefs, and preferences at the forefront of their work. This results in a more individualized treatment plan that is more likely to be successful (C et al., 2016). This strategy raises patient satisfaction and improves treatment adherence, eventually resulting in better health outcomes. One of the implications of cultural humility, cultural competence, and cultural safety for patient outcomes is the reduction of inequities in healthcare. Healthcare personnel can understand and meet the specific healthcare requirements of various populations when they have cultural competence (Stubbe, 2020).This results in more equitable access to and utilization of healthcare services. As a direct consequence of this, these populations will experience improvements in their health.
My Future Nursing Practice
Cultural humility, competency, and safety are all important concepts for healthcare providers, including nurses, to understand and practice. These concepts have several implications for my future nursing practice: This includes Recognizing and respecting cultural differences: Cultural humility requires healthcare providers to recognize and respect each patient’s unique cultural beliefs, values, and practices. As a nurse, I will need to take the time to learn about my patients’ cultural backgrounds and understand how these may affect their health and healthcare needs.
Secondly is Developing cultural competence: According to Greene-Moton & Minkler, 2019, Cultural competency refers to effectively working with patients from diverse cultural backgrounds. This includes understanding how culture can affect health beliefs and practices and communicating effectively with patients who may have different cultural norms around communication and decision-making. Moreover, providing culturally safe care: Cultural safety means that patients feel safe and respected in the healthcare setting, regardless of their cultural background. As a nurse, I will need to create an environment where patients feel comfortable expressing their cultural beliefs and values and where their cultural needs are met. Furthermore is avoiding cultural biases and stereotypes: Cultural humility requires healthcare providers to reflect on their own cultural biases and stereotypes and to recognize how these may impact their interactions with patients. As a nurse, I must be aware of my cultural background and beliefs and strive to provide unbiased care to all patients. Finally, I will strive to understand my patient’s cultural backgrounds and language and to provide care in a manner that is tailored to their individual needs. I will strive to create a safe and supportive environment for my patients to communicate and participate in their healthcare and to be open to feedback and criticism from my patients. By incorporating these elements into my practice, I can ensure that I am providing quality care that respects my patient’s cultural and linguistic differences and that I am providing a safe and supportive environment for my patients to communicate and participate in their healthcare.
The paper discusses the case of a patient I encountered in my clinical placement and emphasizes the importance of cultural safety and humility in healthcare. The paper highlights the need for healthcare providers to understand and appreciate cultural differences to provide quality care that respects patients’ cultural and linguistic differences. Madeleine Leininger’s culture care theory is presented to integrate cultural values into patient care. The paper emphasizes the need for system-wide change and for First Nations to take ownership of their health and wellness journeys. The paper also discusses the implications of cultural humility/competency/safety in the healthcare system, including improved health outcomes for culturally diverse populations, a more inclusive and diverse workplace culture, and a higher quality of care provided to patients. In conclusion, the paper emphasizes the importance of providing culturally safe care, avoiding cultural biases and stereotypes, and striving to understand patients’ cultural backgrounds and language to provide tailored care.
MacKenzie, L., & Hatala, A. (2019). Addressing culture within healthcare settings: the limits of cultural competence and the power of humility. Canadian Medical Education Journal , 10 (1), e124–e127. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6445323/
C, F., Dl, B., Mm, R., & K, O. (2016, May 1). Cultural Humility: A Concept Analysis . Journal of Transcultural Nursing : Official Journal of the Transcultural Nursing Society. https://pubmed.ncbi.nlm.nih.gov/26122618/
FNHA’s Policy Statement on Cultural Safety and Humility . (n.d.). https://www.fnha.ca/documents/fnha-policy-statement-cultural-safety-and-humility.pdf
Foronda, C. (2019). A Theory of Cultural Humility. Journal of Transcultural Nursing , 31 (1), 104365961987518. https://doi.org/10.1177/1043659619875184
Greene-Moton, E., & Minkler, M. (2019). Cultural competence or cultural humility? Moving beyond the debate. Health Promotion Practice , 21 (1), 152483991988491. https://doi.org/10.1177/1524839919884912
Stubbe, D. E. (2020). Practicing Cultural Competence and Cultural Humility in the Care of Diverse Patients. FOCUS , 18 (1), 49–51. https://doi.org/10.1176/appi.focus.20190041
Curtis, E., Jones, R., Tipene-Leach, D., Walker, C., Loring, B., Paine, S.-J., & Reid, P. (2019). Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. International Journal for Equity in Health , 18 (1), 1–17. https://doi.org/10.1186/s12939-019-1082-3
Hughes, V., Delva, S., Nkimbeng, M., Spaulding, E., Turkson-Ocran, R.-A., Cudjoe, J., Ford, A., Rushton, C., D’Aoust, R., & Han, H.-R. (2019). Not missing the opportunity: Strategies to promote cultural humility among future nursing faculty. Journal of Professional Nursing , 36 (1), 28–33. https://doi.org/10.1016/j.profnurs.2019.06.005
Jongen, C., McCalman, J., Bainbridge, R., & Clifford, A. (2018). Cultural competence in health: a review of the evidence.
Lavoie, J. G. (2018). Medicare and the care of First Nations, Métis and Inuit. Health Economics, Policy and Law , 13 (3-4), 280–298. https://doi.org/10.1017/s1744133117000391
Seamon, R. (2019). Addressing Appalachian Health Disparities: Applying Madeleine Leininger’s Culture Care Theory to Health Care in Appalachia. ASA Annual Conference . https://mds.marshall.edu/asa_conference/2019/session8/3/
Slim, L., & Reuter-Yuill, L. M. (2021). A Behavior-Analytic Perspective on Interprofessional Collaboration. Behavior Analysis in Practice . https://doi.org/10.1007/s40617-021-00602-7
Cite This Work
To export a reference to this article please select a referencing style below:
Related Essays
Policy on advancing telehealth beyond covid-19 act of 2022, should covid-19 vaccines be mandatory, nursing communication in acute care setting, unmanned aerial vehicles (uavs) imagery for precision agriculture through machine learning techniques, improving network security, case study: local government planning & zoning assignment, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail
Reflection as a Tool of Culturally Safe Practice
- First Online: 31 July 2021
Cite this chapter

- Pauline B. Thompson 3 &
- Kerry Taylor 4
Part of the book series: Sustainable Development Goals Series ((SDGS))
2060 Accesses
3 Citations
Reflection as a tool of culturally safe practice describes this key component of culturally safe practice and provides some strategies for reflection on previously held assumptions, beliefs, and attitudes. Reflection is a powerful tool for learning, development, and growth and is a key component of culturally safe practice. Through reflection, in and on practice, health professionals have an opportunity to examine their interactions with the goal of providing culturally safe and effective care. Reflection is applied to help health and human service professionals to decolonize and move toward culturally safe practice. Finally, we examine the relevance of this topic to your practice, and the transferability of reflective practice that is regardful in any setting.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Bassot, B. (2016). The reflective practice guide: An interdisciplinary approach to critical reflection . Routledge.
Google Scholar
Browne, A. J., Varcoe, C., Smye, V., Reimer-Kirkham, S., Lynam, M. J., & Wong, S. (2009). Cultural safety and the challenges of translating critically oriented knowledge in practice. Nursing Philosophy, 10 (3), 167–179.
Bulman, C., & Shutz, S. (2004). Reflective practice in nursing (3rd ed.). Boston: Blackwell.
Curtis, E., Jones, R., Tipene-Leach, D., Curtis, W., Belinda, L., Sarah-Jane, P., & Papaarangi, R. (2019). Why cultural safety rather than cultural competency is required to achieve health equity: A literature review and recommended definition. International Journal of Equity in Health, 18 , 174. https://doi.org/10.1186/s12939-019-1082-3 .
Elliot, M. (2004). Reflective thinking: Turning a critical incident into a topic for research . https://www.nursingtimes.net/clinical-archive/leadership/reflective-thinking-turning-a-critical-incident-into-a-topic-for-research-01-01-2004/ .
Frankel, R., & Stein, T. (1999). Getting the most out of the clinical encounter: The four habits model. The Permanente Journal, 3 , 79–88.
Freire, P. (1972). Pedagogy of the oppressed . Penguin.
Gabb, D., & McDermott, D. (2007). What do Indigenous experiences and perspectives mean for transcultural mental health? Towards a new model of transcultural teaching for health professionals. In R. Ranzijn, K. McConnochie & W. Nolan (Eds.), Psychology and indigenous Australians—Teaching, practice and theory . Cambridge Scholars Publishing.
Grant, J., & Guerin, P. (2018). Mixed and misunderstandings: An exploration of the meaning of racism with maternal, child and family health nurses in South Australia. Journal of Advanced Nursing . https://doi.org/10.1111/jan.13789 .
Article PubMed Google Scholar
Howatson-Jones, L. (2016). Reflective practice in nursing (3rd ed.). Sage.
Johns, C. (Ed.). (2017). Becoming a reflective practitioner (5th Ed.) Wiley-Blackwell.
Johns, C., & Freshwater, D. (2005). Transforming nursing through reflective practice (2nd ed.). Wiley-Blackwell.
McEldowney, R., Richardson, F., Turia, D., Laracy, K., Scott, W., & MacDonald, S. (2006). Opening our eyes—Shifting our thinking. The process of teaching and learning about reflection in cultural safety education and practice: An evaluation study . Kapiti Print Media Ltd, Victoria University of Wellington and Whitireia Community Polytechnic.
Mezirow, J. (1991). Transformative dimensions of adult learning . Jossey-Bass.
Oelke, N. D., Thurston, W. E., & Arthur, N. (2013). Intersections between interprofessional practice, cultural competency and primary healthcare. Journal of Interprofessional Care, 27 (5), 367–372. https://doi.org/10.3109/13561820.2013.785502 . Epub 2013 May 17. PMID: 23683058.
Ramsden, I. (2002). Cultural Safety and Nursing Education in Aotearoa and Te Waipounamu . Wellington: University of Wellington.
Rosen, D., McCall, J., & Goodkind, S. (2017). Teaching critical self-reflection through the lens of cultural humility: An assignment in a social work diversity course. Social Work Education, 36 (3), 289–298. https://doi.org/10.1080/02615479.2017.1287260 .
Article Google Scholar
Schön, D. (1983). The reflective practitioner: How professionals think in action . Temple Smith.
Wepa, D. (Ed.). (2015). Cultural Safety in Aotearoa New Zealand (2nd ed.). Cambridge: Cambridge University Press. https://doi.org/10.1017/CBO9781316151136 .
Download references
Author information
Authors and affiliations.
Psychology, Pennsylvania State University, Media, PA, USA
Pauline B. Thompson
College of Medicine and Public Health, Flinders University, Adelaide, SA, Australia
Kerry Taylor
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Pauline B. Thompson .
Rights and permissions
Reprints and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Thompson, P.B., Taylor, K. (2021). Reflection as a Tool of Culturally Safe Practice. In: A Cultural Safety Approach to Health Psychology. Sustainable Development Goals Series. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-76849-2_13
Download citation
DOI : https://doi.org/10.1007/978-3-030-76849-2_13
Published : 31 July 2021
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-030-76848-5
Online ISBN : 978-3-030-76849-2
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Critical Reflection
Throughout these modules, we will invite you to practice cultural safety through critical self-reflection exercises.
Self-reflection is an integral feature of culturally safe practice. These questions will be approached differently by everyone, and personal responses may change as you continue your cultural safety journey. Be curious about the thoughts, feelings, ideas, emotions that arise when undertaking these critical reflection exercises. These can be key pieces of information that reinforce, challenge, expand, or lead to further inquiry about your worldviews and lived experiences.
How to practice self-reflection
- Individually. Use the critical reflection exercises to examine and acknowledge your thoughts and reflection.
- Collectively. The critical reflections can be shared and discussed using the annotation functionality in this book, through group discussion or through Teaching in Circles (TiC).
Teaching in Circles is based on ‘ Australian Indigenous practice of Yarning ’ (Barlo et al., 2020; Dean, 2010).
Yarning is an ‘ Indigenous mode of sharing and delivering knowledges and experiences that reflects and respects our world views and ways of knowing, being and doing business and reciprocity and cultural form of conversation .’ (Doran & Wrigley, 2022)
It aligns with the principles of equal relationships, cooperation, respectful engagement, and support. It aims to create a safe space, to build connections, and enable conversations, particularly difficult ones around cultural safety and power sharing.
It encourages active listening and accountability in what and how participants hear, share, and respond.
Accountability requires self-reflection and acknowledgment of mistakes, an apology and consideration of what could be done differently.
Teaching in Circles supports the experiential understanding of cultural safety.
Teaching in Circle practice includes:
- A circular group formation, all participants can see each other
- Participants can choose to speak without interruption, or only listen
- non-judgement
- accountability
- No barriers to discussion such as note taking, devices, computers
Critical Reflection Exercise 1
Read the following article, then reflect on the reading using the following questions.
Doran, F. & Wrigley, B. (2022) Cultural Safety: teachers’ engagement with an Indigenous pedagogical method in undergraduate nursing education, Contemporary Nurse, 58:1, 58-70, DOI: 10.1080/10376178.2022.2044873
- What do you already know and do about cultural safety?
- What has been your experience of cultural safety?
- How confident do you feel about teaching and talking about cultural safety?
- Did you have any myths or misconceptions about cultural safety?
- What does self-reflective practice look like to you?
- What are your thoughts, feelings, beliefs, and attitudes about self -reflective practice?
Barlo, S. , Boyd, W. , Hughes, M. , Wilson, S. , & Pelizzon, A. ( 2020 ). Yarning as protected space: Relational accountability in research . Alternative: An International Journal of Indigenous Peoples , 17 (1), 40 – 48 . https://doi.org/10.1177/1177180120986151
Dean, C. ( 2010 ). A yarning place in narrative histories . History of Education Review , 39 (2), 6 – 13 . https://doi.org/10.1108/08198691201000005
Doran, F. & Wrigley, B. (2022) Cultural Safety: teachers’ engagement with an Indigenous pedagogical method in undergraduate nursing education, Contemporary Nurse , 58:1, 58-70, DOI: 10.1080/10376178.2022.2044873
Cultural Safety in Health and Teaching Practice Copyright © 2022 by QUT, Faculty of Health, Cultural Safety Indigenous Perspectives Working Group; Yasmin Antwertinger; Mary-Claire Balnaves; Marian Boman; Debbie Duthie; Lana Elliott; Catherine Haden; Shelley Hopkins; Trish Obst; Tony Parker; Helen Vidgen; and Shane Warren is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
Language selection
- Français fr
Common Definitions on Cultural Safety: Chief Public Health Officer Health Professional Forum

Download in PDF format (748 KB, 11 pages)
Organization: Public Health Agency of Canada
Date published: 2023-06-20
Related links
- Principles for Engaging with First Nations, Inuit and Métis: Chief Public Health Officer Health Professional Forum
On this page
About the cpho health professional forum and indigenous health sub-group.
- Continuum of cultural safety and humility
Definitions
Acknowledgements.
For Indigenous Peoples, racism, discrimination and stigma, which contribute to the lack of culturally safe care and support services, have created significant inequities in health in comparison to non-Indigenous Canadians. These health inequities between Indigenous Peoples and non-Indigenous Canadians have only been exacerbated by the COVID-19 pandemic. Through Canada's commitment to end racism and systemic discrimination within the health system, there has been an emergence of various terms, such as cultural safety and cultural humility. These terms describe the key elements for creating an environment where Indigenous Peoples are respected, and health services are provided in an equitable and safe manner, without discrimination.
The following Common Definitions on Cultural Safety have been developed by the Chief Public Health Officer (CPHO) Health Professional Forum's (the Forum) Indigenous Health Sub-Group. They provide clarity on the meaning of these terms, and help ensure that health professionals looking to engage meaningfully in health and healthcare improvement for Indigenous Peoples are aware of appropriate terminology.
Meaningful engagement with First Nations, Inuit, and Métis must follow a distinctions-based approach and reflect the unique interests, priorities and circumstances of each People. As such, the Forum's Indigenous Health Sub-Group has engaged, and will continue to engage with First Nations, Inuit and Métis on this resource to ensure that it reflects the perspective of Indigenous Peoples and communities in Canada.
Formed in 2018 and comprised of 19 national health organizations, the Chief Public Health Officer (CPHO) Health Professional Forum (the Forum) brings together national health organizations to collaborate and take action on public health issues of national importance. Indigenous health, including cultural competency and safety, has been recognized by the Forum as a key priority area for collaboration. The Forum's Indigenous Health Sub-Group was formed to share and build upon the work of member organizations to advance Indigenous cultural competence, awareness, safety and humility among health professionals.
CPHO Health Professional Forum members
- Association of Medical Microbiology and Infectious Diseases Canada
- Canadian Association of Social Workers
- Canadian Dental Association
- Canadian Indigenous Nurses Association
- Canadian Medical Association
- Canadian Nurses Association
- Canadian Paediatric Society
- Canadian Pharmacists Association
- Canadian Psychological Association
- Canadian Public Health Association
- College of Family Physicians of Canada
- Community Health Nurses of Canada
- HealthCareCAN
- Indigenous Physicians Association of Canada
- Infection Prevention and Control Canada
- Public Health Agency of Canada
- Public Health Physicians of Canada
- Royal College of Physicians and Surgeons of Canada
- Society of Obstetricians and Gynecologists of Canada
Indigenous Health Sub-Group members
- Assembly of First Nations
- Canadian Indigenous Nurses Association (co-lead)
- Health Canada
- Indigenous Services Canada
- Métis National Council
- National Collaborating Centre for Indigenous Health
- Royal College of Physicians and Surgeons of Canada (co-lead)
Continuum of cultural safety and humility Footnote 1
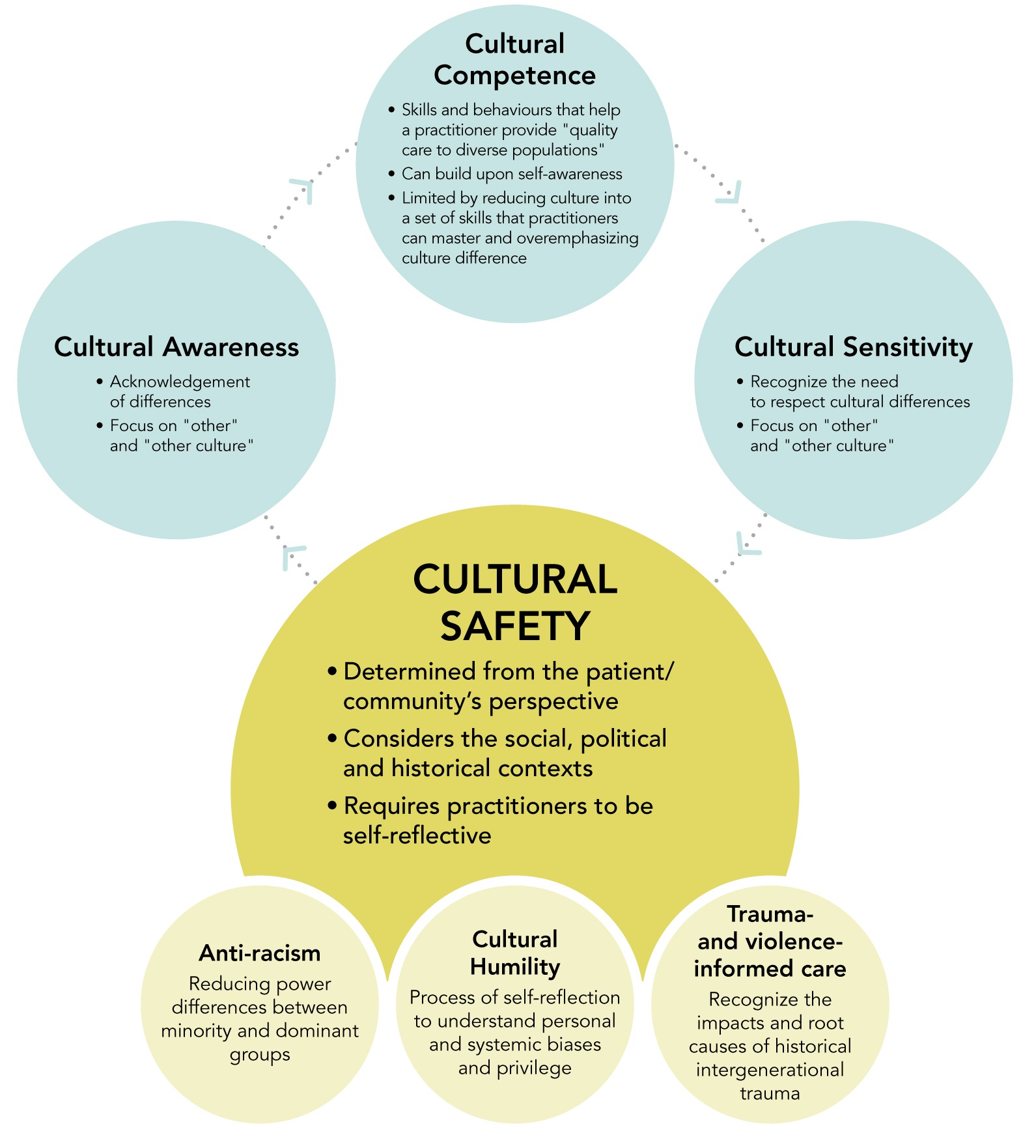
This figure shows that cultural safety must be viewed as a continuum of knowledge, attitudes and behaviours, beginning with cultural awareness.
Cultural safety is an on-going process, one in which health professionals must continuously revisit their own knowledge, attitudes, behaviours and processes to meet the needs of Indigenous peoples.
As time progresses, this process must be continuously revisited as new understanding of what cultural safety means develops. These new developments may emerge from influences such as cultural humility, anti-racism and trauma- and violence-informed care.
All three bubbles ultimately lead to cultural safety. Cultural safety is the end-goal in this pathway, how we understand that being culturally safe is a continuous process, as new understandings of what being culturally safe means are developed. Thus, cultural safety has a different shade and larger bubble than the others do. However, it feeds back into the cycle because the learning process is ongoing.
The three bubbles of anti-racism, cultural humility and trauma- and violence-informed care are not part of the cycle. They are potential influences that change our understanding of cultural safety and hence create the cycle that is never-ending. We had them touch the bubble of cultural safety to show that they impact only this bubble.
Cultural awareness
The acknowledgment of difference. It is the first step in understanding cultural differences and involves observing those differences. Cultural awareness focuses on the 'other' and the 'other culture.' Cultural awareness does not consider political or socio-economic influences on cultural difference, nor does it require an individual to reflect on his/her own cultural perspectives.
- Canadian Indigenous Nurses Association (2013). "Cultural Safety in First Nations, Inuit and Métis Public Health"
Cultural sensitivity
Recognizing the need to respect cultural differences. Cultural sensitivity involves exhibiting "behaviours that are considered polite and respectful by the [person of the other culture]." Similar to cultural awareness, cultural sensitivity focuses on the 'other' and the 'other culture.' Cultural sensitivity also does not require an individual to reflect on his/her own culture.
Cultural competency
The ability to self-reflect on one's own cultural values and how these impact the way one provides care, as well as continually learning to gain a deeper understanding of another's culture. It includes each health professional's ability to assess and respect the values, attitudes and beliefs of persons from other cultures and respond appropriately in planning, implementing, and evaluating a plan of care that incorporates health-related beliefs and cultural values, knowledge of disease incidence and prevalence, and treatment efficacy.
- Canadian Nurses Association (2018). "Promoting Cultural Competence in Nursing
Cultural humility
Cultural humility is a way in which health care providers practice that enable cultural safety . It is a process of self-reflection to understand personal and systemic biases, and privilege to develop and maintain respectful processes and relationships based on mutual trust. Cultural humility involves humbly acknowledging oneself as a learner when it comes to understanding another's experience, and dismantling power imbalances.
- BC First Nations Health Authority (2016). Creating a Climate for Change: Cultural Safety and Humility in Health Services for First Nations and Aboriginal Peoples in British Columbia
Cultural safety
Cultural safety is about the experience of the patient. It is an outcome based on respectful engagement that recognizes and strives to address power imbalances inherent in the healthcare system. It results in an environment free of racism and discrimination, where people feel safe when receiving health care.
Cultural conflict
Stems from differences in beliefs and values between one culture and another. It is the result of conscious or sub-conscious imposition of one culture's beliefs and values on another culture because of an inherent belief in their superiority.
Unearned disadvantage. Oppression is also concerned with whether a given society, economic system, or institution unjustly benefits certain groups.
- Association of Medical Microbiology and Infectious Disease Canada (2019). as referenced in Peggy McIntosh (1988). "White Privilege and Male Privilege: A Personal Account of Coming to See Correspondence through Work in Women's Studies
Unearned advantage. Privilege is concerned with whether a given society, economic system, or institution unjustly benefits certain groups.
Racial prejudice or discrimination. The belief that ones own race is superior to another, based specifically on ones particular racial or ethnic group.
- Royal College of Physicians and Surgeons (2019). "Indigenous Health Values and Principles Statement", Second Edition.
Anti-racism
Any approach that reduces power differences by benefitting minority racial[ized] groups and/or disadvantaging dominant racial[ized] groups.
- National Collaborating Centre for Indigenous Health (2013). "Understanding Racism."
Structural or systemic racism
Political, social and economic structures and institutions, where a dominant group is established and its power is reinforced through inequitable laws, policies, rules and regulations, as well as access to resources. Within these structures, stereotypes about Indigenous Peoples bring about prejudices which produces discrimination, which leads to oppression
- National Collaborating Centre for Indigenous Health (2014).
- "Aboriginal Experiences with Racism and Its Impacts."
Trauma-informed care
A trauma informed care provider understands the impacts and root causes of historical intergenerational trauma (i.e. residential school experiences), recognizes the symptoms of trauma in patients and integrates this knowledge into policies, procedures, practices and settings; "trauma informed care is their commitment to provide services in a manner that is welcoming and appropriate to the special needs of those affected by trauma."
- National Collaborating Centre for Indigenous Health (2017). "What's New is Really Old: Trauma Informed Health Practices Through an Understanding of Historic Trauma" & Royal College of Physicians and Surgeons "Indigenous Health Primer (2019)
Stigma is comprised of negative, unfounded attitudes or beliefs (prejudice) towards an individual, based on their real or perceived membership of a stigmatized group. Stigma is often accompanied by negative action/behaviours (discrimination).
- Government of Canada (2019).
- "Stigma: Why Words Matter" (2019)
This document was developed in collaboration with members of the CPHO Health Professional Forum:
- Canadian Geriatrics Society
- Canadian Medical Association Canadian Nurses Association
In addition, we gratefully acknowledge the leadership and contributions of the Indigenous Health Sub-Group of the CPHO Health Professional Forum, which, in addition to Forum members, includes the following organizations:
- Pauktuutit Inuit Women of Canada
This graphic has been adapted from Baba, L. (2013). Cultural safety in First Nations, Inuit and Métis public health: Environmental scan of cultural competency and safety in education, training and health services. Prince George, British Columbia, Canada: National Collaborating Centre for Indigenous Health. BC First Nations Health Authority. "Cultural Humility." 2019. Retrieved from https://www.fnha.ca/wellness/wellness-and-the-first-nations-health-authority/cultural-safety-and-humility; Brascoupé, S. and Waters, C. (2009). Cultural safety: Exploring the applicability of the concept of cultural safety to Aboriginal health and community wellness. Journal of Aboriginal Health. Retrieved from www.researchgate.net/
Return to footnote 1 referrer
Page details
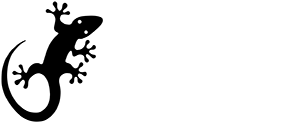
- Cultural Safety for Health Professionals
Welcome to the Health InfoNet’s Portal on Cultural Safety for Health Professionals. The portal aims to support health professionals in their practice to deliver culturally safe, accessible and responsive healthcare that is free from racism.
Links are provided here to Aboriginal and Torres Strait Islander health and cultural safety publications, policies, resources (health promotion and health practice), programs, organisations and workforce support information as well as content relevant to specific health professional disciplines. These disciplines align with the Australian Health Practitioner Regulation Agency’s 16 registered professions.
We are grateful to the First Peoples Health Unit at Griffith University in Queensland who provided funding for the original setting up of this Portal. The Health InfoNet continues to support the Portal, without specific funding, as a service to Allied health professionals working in Aboriginal and Torres Strait Islander health throughout Australia.
Aboriginal and Torres Strait Islander Health Practitioner
Chinese medicine practitioner, chiropractor, dental practitioner, medical practitioner, medical radiation practitioner, optometrist, occupational therapist, physiotherapist, psychologist, all health professionals, cultural safety for health professionals content, key resources.
- Publications
- Organisations
Workforce information
Like to see more.
The funds provided by the Australian Department of Health and Aged Care enable good coverage of many areas, particularly those within the direct responsibility of the health system. However there are other health topics which require additional funding.
We seek your assistance to fund this topic to support us in helping to improve health outcomes for Aboriginal and Torres Strait Islander people.

Melanie Robinson - Pilbara Travels
Stay connected, yarning places.
View our Disclaimer and Privacy statement
The Australian Indigenous Health InfoNet acknowledges the Traditional Owners of the lands and waters of Australia and the Torres Strait.
We respect all Aboriginal and Torres Strait Islander people—their customs and their beliefs. We also pay our respects to Elders past, present and emerging, with particular acknowledgement to the Whadjuk people of the Noongar nation, the Traditional Owners of the lands where our offices are located.

- Overview of Aboriginal and torres Strait Islander health
- Summary of Aboriginal and Torres Strait Islander health
- Reviews and Summaries
- Multimedia knowledge exchange products
- Latest information and statistics
- Cultural Ways
- Special topics
- Cardiovascular Health
- Coronavirus (COVID-19)
- Infectious Conditions
- Kidney Health
- Oral Health
- Respiratory Health
- Sexual Health
- Social and Emotional Wellbeing
- Alcohol and Other Drugs Knowledge Centre
- Child Protection
- Digital Services
- Family Safety
- Strong Communities
- Environmental Health
- Immunisation
- Physical Activity
- Social and Cultural Determinants
- Closing the Gap
- Community Controlled Health Sector
- Hospital Care
- Palliative Care and End-of-Life Care
- Primary Health Care
- Adolescents
- Older People
- Australian Capital Territory
- New South Wales
- Northern Territory
- South Australia
- Western Australia
- Aboriginal and Torres Strait Islander Health Professionals
- Our Mission
- Quality Assurance
- History timeline
- Tribute to Neil Thomson
- Advisory Board
- Consultants
- Stakeholders
- HealthInfoNet Director’s Communique
- Media Releases
- Take a tour videos
- Knowledge Exchange products
- Art Gallery
- Open access
- Published: 04 July 2022

A qualitative exploration of cultural safety in nursing from the perspectives of Advanced Practice Nurses: meaning, barriers, and prospects
- Jacqueline Pirhofer 1 ,
- Johannes Bükki 1 , 2 ,
- Mojtaba Vaismoradi 3 ,
- Manela Glarcher 1 &
- Piret Paal 1
BMC Nursing volume 21 , Article number: 178 ( 2022 ) Cite this article
19k Accesses
1 Altmetric
Metrics details
Cultural safety requires healthcare professionals and organisations to improve healthcare, facilitate patient access to healthcare, and achieve equity within the workforce.
This ethnomethodological study, which consisted of two phases, explored the concept of cultural safety from the perspective of Advanced Practice Nurses. Semi-structured interviews and the nominal group technique were used to prioritise challenges related to cultural safety, identify barriers to clinical practise and assess educational needs. The data collected was subjected to thematic analysis.
Nurses working in Austria, Germany and Switzerland were recruited ( N = 29). Accordingly, the phenomenon of cultural safety in health care is not generally known and there is little prior knowledge about it. The most frequently discussed themes were communication difficulties, lack of knowledge, the treatment of people with insufficient language skills and expectations of treatment goals and outcomes, which can lead to conflicts and accusations of unequal treatment due to diverse cultural backgrounds.
Diverse cultures are encountered in German-speaking healthcare settings. Cultural safety is also about healthcare staff, as nurses with different socialisations encounter prejudice, discrimination and racism. Although the issue of power was not discussed, academic nurses were willing to make an effort to change. Only a minority were aware that lasting change requires challenging one’s own cultural structures and adapted behaviours, rather than pushing for the mere acquisition of cultural competence. Organisations were encouraged to introduce self-reflection sessions and provide better access to translation services to improve equity and support nurses.
Peer Review reports
The right to health was recognised as a human right in the 1966 International Covenant on Economic, Social, and Cultural Rights. According to the United Nations Office of the High Commissioner for Human Rights (OHCHR), healthcare services must be culturally appropriate and acceptable [ 1 ]. The International Council of Nurses (ICN) Code of Ethics states: “Inherent in nursing is a respect for human rights, including cultural rights.” [ 2 ]. As nursing care is delivered within a social context, it is affected by healthcare contexts and policies. The importance of culturally appropriate and acceptable healthcare is steadily increasing with the increasing pluralism, diversity, and complexity of ethnic and cultural groups [ 3 ].
Health equity aims to eliminate disparities and achieve optimal health. Existing guidelines mention the discrimination of people who do not have territorial or social access to health care services. In this context, the culturally acceptable meaning of access is still debated [ 4 ]. Access to healthcare services is affected by geography, ethnicity, sex, and socioeconomic status. Globally, in-country mobility and rural–urban migration patterns add to growing diversity. Hence, accessible healthcare is an issue that is not only available in indigenous populations but also among people with different migration patterns and their descendants. Subpopulations have specific risks and exposures that must be addressed in healthcare. In the United States, the National Institutes of Health (NIH) introduced standards to enhance culturally and linguistically appropriate services (CLAS) to be adapted to any healthcare setting to improve equity and eliminate healthcare disparities [ 5 ]. The new European Agenda for Culture of the European Council calls on research on cultural crossovers, assessing the impacts of culture in different fields, including health and well-being [ 6 ].
Even in countries where cultural safety accreditation standards and policies exist, they may not necessarily be implemented [ 7 ]. Perry et al. (2015) have demonstrated that during the clinical assessment of patients from culturally and linguistically diverse backgrounds, nurses frequently rely on patients’ poor language skills, use family members or patients’ friends as interpreters, and/or do not discuss the cultural aspects of health for fear of offending patients [ 8 ]. Healthcare providers establish interventions for their individual and professional definitions of ‘appropriate’ care. There is an ingrained assumption that healthcare professionals are solely responsible for this because of their expertise. Discussions on patient autonomy, partnership, and informed consent are ongoing. However, the premise of equal treatment for all patients is insufficient, as it simply ignores existing differences [ 9 ]. To ensure high-quality care, detailed biography and needs/resource assessments are required. Patients need space for self-definition, including their respective life experiences and experiences of the care process [ 10 ]. Accordingly, governments have committed to improving access to healthcare, enriching health service delivery, improving the quality of service and patient safety, and increasing the efficiency and coordination of care [ 11 ].
Safe healthcare services should be adequate in several dimensions such as culture. Culture is a highly context-dependent concept explained as “a patterned behavioural response that develops over time as a result of imprinting the mind through social and religious structures and intellectual and artistic manifestations.” [ 12 ]. Unless this definition of culture is acknowledged in healthcare, socio-cultural practices that are ethically, socio-politically, economically questionable, and even oppressive are perpetuated [ 13 , 14 ]. It consists of all strong indicators for seeking novel approaches to heed culturally safe patient care. Curtis et al. (2019) thoroughly discussed why cultural safety rather than cultural competency is required to achieve health equity. Based on their findings, they proposed the following definition of ‘cultural safety’:
Cultural safety deals with the balance of power between professional caregivers and people receiving care. Accordingly, professional caregivers must recognise that a person’s dignity and right to self-determination have to be acknowledged and prioritised; address their own biases, attitudes, assumptions, stereotypes, prejudices, structures, and characteristics that may affect the quality of care; and engage in self-reflection. Healthcare organisations and authorities need to be held accountable for providing culturally safe care, as defined by patients and their communities, and as measured through progress towards achieving health equity. Cultural safety requires healthcare professionals and their associated organisations to influence healthcare to reduce bias and achieve equity within the workforce and working environment [ 15 ].
Wilson et al. (2022) critically analysed cultural safety education and its translation into practice, focusing on indigenous health education programs. They demonstrated that even in countries where cultural safety is a well-established concept, the change in practice is complex, requiring leadership for a multi-system approach, critical pedagogy, and commitment by nurses. Educational programs for building consciousness are required to have an impact. Education is a change agent; however, it is only one part of the complex and interdependent change process to achieve culturally safe patient care. Understanding how nurses practice cultural safety in local contexts is essential to forge changes at the individual, educational, and organizational levels [ 16 ].
Comprehensively assessing cultural safety may improve our understanding of these phenomena, identify areas for improvement, and promote cultural re-engineering strategies that improve patient safety [ 17 , 18 ]. In this study, we explored the culturally safe practices of ADVANCED PRACTICE NURSES (APN) in the German language context. According to the ICN, an advanced practice nurse is “a registered nurse who has acquired the expert knowledge base, complex decision-making skills, and clinical competencies for expanded practice, the characteristics of which are shaped by the context or country in which [she or he] is credentialed to practice.” [ 19 ]. Their focus is on direct clinical practice, addressing the health needs of populations, individuals, and families with additional expertise in health promotion and disease prevention [ 20 ]. In German-speaking countries, the integrative model of APN proposed by Hamric and Hanson [ 21 ] is widely used to describe APN core competencies, namely guidance and coaching, counselling, evidence-based practice, leadership, and collaboration [ 22 ]. It is important to understand that the educational model is an agreement between tertiary institutions to promote and professionalise nursing practice. The role of the APN is not recognised by any regulatory or government body in the respective countries [ 23 , 24 , 25 , 26 , 27 ]. In Austria, Germany and Switzerland, nurses can obtain a Master’s degree, but there are no career paths or clearly defined roles for APNs. Unlike APNs, the Registered Nurse designation (RN) is a governmental attempt to register practicing nurses, and since there is no re presentative body for nurses, there are no requirements other than to join the register. Compared to RNs or Advanced Practice Registered Nursing (APRN) roles, APNs are academically educated nurses, thus by fulfilling an expanded nursing role and performing broad competencies in healthcare, they may be able to create awareness and serve as role models for cultural safety. Therefore, this study aims to explore the concept of cultural safety from an APNs’ point of view by identifying existing barriers, opportunities, and practices.
This qualitative exploration consisted of two phases: semi-structured interviews to develop new knowledge of the research phenomenon and a nominal group meeting to discuss the findings, collect more detailed data, and validate the information power of the data collected in Phase 1.
This ethnomethodological study helps improve our understanding of the construction of order and reality through the production and interpretation of meanings from the perspective of acting persons [ 28 ]. People act as a matter of routine, and the goal of ethnomethodology is to explain people’s behaviours and actions as evidence. This approach sets out to use theoretical resources and empirical research to understand processes and, as a second step, contributes to the change in context [ 29 ].
Phase 1. Semi-structured interviews
To gain new insights into cultural safety, which is not an established theory, adequate information power was considered in the sampling strategy [ 30 ]. Interviews were conducted between November 2020 and March 2021 with nurses working in Austria, Germany or Switzerland. Second-year Master’s students (120 ETCS) and APNs with Master’s degrees were recruited. For Phase 1, the interviewer (JP) tried to recruit only students through personal contact. Since participants could not be reached in this way, we decided to expand the sample to include APNs with university degrees. Our failure to recruit students was partly due to Covid-19-related stressors and constraints and partly due to a lack of interest in the research topic.
Extended, in-depth, and specialised nursing practice takes place through direct interactions with/among individuals/families or groups [ 31 , 32 ]. APNs are expected to engage in sociocultural reflection, adopt new concepts, and rethink their cultural practices. The participants differed in age, professional experience, and specialty. Thus, this study benefitted from a broad range of experiences. Data regarding their religious and ethnic backgrounds were obtained but were not reported because of anonymity and confidentiality.
Participants were recruited via email using the purposive sampling method. The invitation contained an explanation, research questions, the purpose of data collection, and a declaration of consent. If interested, participants were asked to return the signed information sheet. An appointment was made for the interview, which was conducted through online video conferences. This turned out to be extremely helpful, especially since access to nursing staff from other countries was facilitated, and research could also be carried out in accordance with the pandemic rules. To ensure that no third parties were present, the interviewer switched on her camera and showed the interviewees their premises. Casual introductory conversations were held before the sound and video recordings. All interviews were conducted in German. The interviews lasted between 21 and 51 min (Table 1 ).
The interviews were transcribed verbatim immediately after each interview [ 33 ]. Longer pauses for breath have been placed in brackets and integrated into the text (1–3 s pause). Striking stresses have been written in bold. Striking sounds were written in brackets, e.g. (mhmm) and (aah). Striking, non-linguistic processes are marked with asterisks, e.g. *raises his voice* and *laughs*. Data collection and analysis were performed concurrently. The collected data were subjected thematic analysis [ 34 ]. Thematic analysis is a flexible research strategy as no linear data analysis process is assumed. This type of analysis suited our study because there have been no previous studies on this topic from the German-speaking context. The first author, who conducted the interviews and transcribed them, created and managed the initial codes through open coding using the MaxQDA software. Codes were constantly compared, sorted, and classified based on their similarities and differences. Themes and subthemes were developed iteratively by comparing codes that were reviewed and refined by the research team. The authors collaborated during the data analysis process until the themes were finalised [ 34 , 35 ].
Rigor and trustworthiness
Two experts in qualitative thematic analysis (JP and PP) assessed the study’s compliance with the guidelines for establishing trustworthiness. To ensure credibility and reliability, a sample of transcripts was independently reviewed and coded by JP and PP. A consensus debriefing was conducted to explore the relationships between the interview and the background context to increase reflexivity and validate findings. For credibility, individual transcripts, along with a brief report of the study findings, were sent back to the participants. None of the respondents made any requests for change, indicating that our findings reflected their perspectives. The bilingual authors ensured the validity of the translation of the outcomes from German to English for publication.
Phase 2. Nominal group meeting
Phase 1 served as the main phase of data collection for this study. However, Phase 2 was required to present, discuss and verify the data collected in the previous phase. It also served to check the validity of the data collected in Phase 1. Therefore, the nominal group technique was used. The nominal group technique (NGT) is a useful method for capturing priorities in health care and considers themes identified by the whole group [ 36 ]. The participants were second-year Master’s students (Table 2 ) who were asked to prioritise challenges related to cultural safety, name their importance, explore barriers to clinical practice and identify their educational needs based on the data collected in Phase 1. Students who had attended the lecture on cultural encounters in nursing were recruited and presented with the results of the previous phase and then asked to share their views.
A Padlet dashboard ( www.padlet.com ) was created as part of the instructional session and the link was sent to the participants. They were able to use the comment function to document and record all ideas. The process took approximately 15 min to complete. During this process, participants were also able to ask questions about the topic. Multiple responses were provided. It addressed the educational needs of the APNs to improve the existing curriculum. Participants were asked three questions related to cultural safety: 1. What factors stand out to me, which are particularly challenging? 2. What are the prospects for transformation in nursing care? 3. What aspects should be integrated into nursing education? To discern patterns, similar codes were grouped and summarised in a table. Next, they were analysed using thematic analysis [ 34 ] and presented as a tree diagram combining the study findings from Phases 1 and 2.
Participants
A total of 29 students and graduates participated in this study consisting of ten students and graduates in Phase 1 and 19 students in Phase 2. The majority (78%) of the participants were women. Their mean work experience was 7.9 years (range = 0–25). Of all the participants, 62% ( n = 18) worked in inpatient wards, 17% ( n = 5) in the outpatient setting, 10% ( n = 3) in the intensive care unit, one in central practice coordination, and one was on parental leave.
Phase 1: semi-structured interviews
Three main themes were developed during the data analysis process: ‘meaning of cultural safety’, ‘barriers to cultural safety’, and ‘prospects of cultural safety’. The themes and their related subthemes are described below, using direct quotations from the participants (Table 3 ).
Meaning of cultural safety
Cultural safety was common in healthcare settings, but there was little prior knowledge about it: if I were to hear (aah) cultural safety, in everyday care and everyday life, and in general, I would first say it is not yet a widespread topic or terminology. This is not a taken-for-granted terminology. This is not the present conceptualisation of everyday nursing care. (Participant 3, Line 34).
A uniform understanding of the phenomenon of cultural safety was reported, with cornerstones on individuality and the need for security, regardless of origin, culture, or other demographic determinants. Its primary goal was to provide the best possible individualised care. Therefore, under cultural safety, I understand that no matter what a person is like, in terms of sexual orientation, occupation, and socioeconomic status, is safe in this environment . (P1, L. 60).
The acceptance of both society and personnel was inevitable and any marginalisation had to be hindered: so, that he [the patient] can just live out the way, he is and move around in this can move within this protected framework without having to make cuts. (P1, L. 60).
Impact on the patients
The situation of the patients in the hospital should never be recognised as neutral. Patients might experience pain, psychological overload, or even trauma. Nursing care should focus on cultural and personal needs that positively influence therapeutic relationships. Physical discomfort often occurs along with emotional discomfort. Therefore, feelings of insecurity prevailed before the establishment of a nursing relationship.
A commonly shared opinion was that cultural safety influenced achieving the therapy goals, well-being, quality of life, recovery process, and psyche of the patient: I could imagine, they feel taken care of. More understood. Respected, even integrated. So, or so perceived. They feel more comfortable, and the feeling of comfort is also a safety aspect, and therefore, contributes to recovery. (P8, L. 60).
Self-assessment of APNs
Do you provide culturally safe care? Nine out of ten participants answered, No . They tried it, but never reached the perfect condition. So, my answer to this question can be balanced; I think, I do my work 100 percent perfect all the time. I would strongly argue that no nurse can be 100 percent culturally safe. (P3, L. 38).
I try. However, I make mistakes that I am not aware of. So, like patronising the patient, yes, he wants it that way. That happens. However, this is simply unconscious. I would say that I would never do it purposely. However, it happens in everyday life and through habits. (P7, L. 50)
Cultural safety was difficult to achieve because it was not an endpoint, but a continuous process. Continuous training was highlighted because basic education was not sufficient: I do not really know much about it, I mean, of course, in the school you have heard about the differences of (mhmm) certain things, but I do not think I am really informed about it, no. (P6, L. 46).
Prospective development
Some participants stated that currently no progress was under way regarding cultural safety: I do not think, no, that it will develop in the direction now, because nursing has quite different construction sites. (P1, L. 32).
Current research has indicated novel approaches to generate a benefit for nursing, but the transfer of knowledge into practice is slow. Special attention must be paid to this sector to meet future care demands, and we must massively upgrade and improve it. I mean, with migration, that is, what we are experiencing all around us. This will certainly be a challenge for the next few years. (P9, L. 42).
Barriers to cultural safety
Different aspects of each culture are often transformed automatically into stereotypes by nurses to make their work easier. In principle, a difficult patient is not difficult; he simply has needs that could not be met until now. You just must talk to them out of it, or they need something different in general. (P10, L. 34).
It is typically triggered by cultural background, making it difficult to process information. Due to staff shortages, nursing staff are increasingly reaching imposed limits and barriers. An adjustment should take place by which nurses and patients must approach each other to generate suitable solutions for the future: But I think a certain form of adaptation, I would wish for on both sides. The adaptation of a hospital takes place in the form of interpreter services or special meals … (P8, L. 42).
- Discrimination
It was stated that prejudices were shaped or formed by situations in the past and by the media: I think that often you get into this predicament that you might say something not so sensitive, (aah) although you do not want to discriminate, but (aah) it can happen in the sense of a faux pas. (P3, L. 28).
This discourse occurred only when people from diverse cultural backgrounds were involved. Explicit discrimination rarely occurred, but they confessed that devaluation in the form of jokes occurred in various settings. "Balkan syndrome" as a unique experience of pain and a louder and more pronounced suffering was specified: Yes. [3–5 s pause] Either way, of course, there is the classic saying ‘Balkan Syndrome’. If you go out now, for example, in the direction of a patient with an ex-Yugoslav background. (aah) Yes, I do not like it. When I hear something like this, I always point it out to my colleagues. (P2, L. 36).
Despite some participants denying any racism, others reported racist behaviours, such as a complete lack of appreciation for certain patients. Prejudices towards people with diverse cultural backgrounds were mentioned: For me, it is also always difficult to comprehend when it is in practice that other caregivers (mhmm) condemn or change their behaviours because of that–towards the patients. (P7, L. 22).
Importance of communication
Verbal communication is a vital tool for establishing contact with patients, building relationships, receiving information, and communicating, which is exceedingly difficult. I consider communication to be one of the highest assets in professional nursing. You cannot communicate; they say so nicely. (P3, L. 30).
A big caring issue was nurses rejecting patients: Quite often, the language barrier was a huge problem. Many nurses are already averse or [takes a long pause for breath] from the patient alone when a language barrier is present. (P7, L. 36).
This caused patients sometimes not to receive care they were entitled to. Often, the patients are simply left out of the rounds by the doctors. (P7, L. 42).
The language barrier created a heteronomy that was not conducive to patient care: I also see it critically that if you live in a country and get sick and cannot express yourself, then it’s an enormously dependent relationship and then it is somehow difficult to guarantee medical care. (P8, L. 42).
Visiting relatives
Families expressed their appreciation by visiting an ill family member. For certain ethnic groups, such visits were of high value: if you look at ethnic origin [3–5 s pause], with southerners, family is always a very present theme. (P3, L. 34).
The whole family always wants to be present, preferably so that they can show affection, so that they can feel connected to the patient, so that they can provide for better recovery and positively favour the whole thing. Moreover, they have high conflict potential. (P3, L. 42)
This was a burden when too many relatives were present in the patient’s room. A negative aspect was the increased noise that prevailed in rooms or wards. Others expressed an understanding towards visitations and criticised the disapproving attitude of nursing staff: Families like this do not come with bad intentions; it is about a community about celebrating something normal. (ahm) I have always found that it is very beneficial for patients. And exactly, found it a pity when the nursing staff then spoke so deprecatingly. (P8, L. 38).
Gender roles
Gender roles and body image are complex entities in many cultures, and individual considerations of sociocultural aspects are considered important. Of course, there is also the whole relationship between body image and body care. One must also always pay attention to the fact that one does not necessarily bring a male colleague to a Muslim woman in the room, or you must agree to this beforehand. The same is true, but also vice versa . Men from diverse cultural backgrounds can also be helped by other men. This is something you must pay attention to. (P2, L. 32).
Eating was seen as a cultural sign of becoming well again: food plays a crucial role because in our society (long breath), when it now goes towards the end of life, food (aah) no longer has such a significant importance as in other cultures. In other cultures, it often seems to me that they try to continue to give the patient food, and if he eats, then that is a good sign. Since then, he has become healthy again. You also notice cultural differences. (P2, L. 32).
The caregivers tended to associate special dietary requirements, such as the rejection of pork, negatively. This seemed burdensome, adding to the workload. For example, the food without pork, oh God, now you must order the food again. It is always an effort that is seen and less positive. (P7, L. 40).
The participants had a basic understanding of patients’ fears, including the fear of making situations in the hospital difficult for people with diverse cultural backgrounds; when I imagine how a patient feels, who may not be in the hospital very often, and who does not understand the language, and especially now at Corona times, when no one is allowed in the hospital, and then maybe she does not know how to use her cell phone because she is very old, then it is a disaster, I can imagine. (P1, L. 48).
It also helped me to see certain situations with different eyes. That is, not everything is the way it comes across. However, people behave in such a way because they are afraid of the reactions of another person. They tried to protect themselves. (P5, L. 22)
Several reasons including time for not being able to provide culturally safe care were mentioned: [3–5 s pause, unintelligible] It is often difficult to take time with a patient (aah) who may not understand me. Yes, this makes this difficult to achieve. (P2, L. 54).
Thus, there is more time. Time for the patient. Especially in acute hospitals (mhmm), the time to deal with it. I think a lot about palliative situations or of deceased patients when relatives come. It is just the case that, if they need something, they should get in touch. However, you do not clarify in advance how things are done or what their wishes are. (P7, L. 22)
The participants acknowledged the need to learn about others’ religions. When I think back to Germany, where the Muslim community is very widely represented, one can also be in lively contact with this community. During a hospital stay, you learn an enormous amount, and then you also develop this sensitivity for certain subtleties accordingly, which is now, for example, in connection with religion. (P3, L. 22).
Religion was set as it only represented one part of a person; despite religious affiliation, a reduction in religion is not desirable. A human being should always be recognised as an individual. Therefore, every person, (aah), has his or her character; hence, he or she must be considered an individual, and this also applies to religion. Religion is only a part, a fraction of which, what a human being is from its whole, or the total. (P3, L. 24).
Cultural diversities led to conflicts that, under certain circumstances, should be addressed: it is important, especially when certain conflicts blossom, to address them directly and to try to present one’s interests or one’s view clearly and to act accordingly in a patient-oriented manner, that is, according to the motto patient first, and accordingly to reflect on one’s own potential conflicts and on them within the team with a critical view of one’s personality or one’s interests. (P3, L. 26).
Due to diverse personalities, team cultures were variable, and conflicts might arise. Therefore, self-reflection was deemed essential: And (aah) on the other hand, it is incredibly important to reflect on oneself at the end of the day and to take the best from these conflicts and try to grow from them afterwards. It is part of your feedback to each other within the team at some point. (P3, L. 26).
Prospects of cultural safety
Staff, employers, and relatives were considered relevant actors in improving cultural safety.
Possibilities of nursing staff
It was essential to put aside one’s impartiality toward foreign cultures and to act as a professional. Professional and culturally safe care presupposes certain soft skills; therefore, we need greater sensitivity, understanding, and empathy. That is a process. [3–5 s pause], we are on the right path. I am positive about this. However, you can do much more. (P5, L. 50).
Quality management is important to continuously improve cultural safety. A valuable tool was feedback, which was a good keyword in this context [long pause for breath] because it offers the possibility to make one or another person more aware. (P3, L. 26).
The patient’s feedback was also a suitable medium: And there I plead that the patient also gives some feedback and lets us say there are various mechanisms that you can use, like an (aah) feedback sheet after a hospital stay . (P3, L. 28).
Four out of ten nurses mentioned reflection as an important perspective in achieving culturally safe care: And (aah) on the other hand, it is incredibly important that you reflect on yourself at the end of the day and, in the case of these conflicts, to take the best of them and try to grow a little bit afterward. It is part of that that your feedback is to each other within the team at some point. (P3, L. 26) Every nurse should be concerned with themselves: How do I want the patient to be treated? Think about how I would like to be treated? (P10, L. 34).
Close observation and adaptation were also stated: I think in our profession we should always be able to observe well. Moreover, they have certain adaptability. Regardless of what our own interests and values and principles are, which sometimes may not be compatible or correlate with one another. (P3, L. 24).
Empathy is a central pillar of a successful patient relationship: Understanding, I think, is a crucial point. (mhmm) [long pause for breath] *clear throat* I find the topic so difficult because it should be simple and easy. (P4, L. 50).
There needed to be awareness or education regarding cultural aspects. What certainly needs to happen is that all caregivers or medical professionals have a little more input about something like that, because I can only talk about myself now, I only know the standard things. (P6, L. 53).
The relationship between the patient and caregiver was important during the hospital stay, and the relationship is, for me let us say, the fundamental aspect of nursing care . (P9, L. 28).
A detailed assessment at the beginning of each stay was a crucial step for all further measures: Yes, take a history, also illuminate the cultural background, where he comes from, and how he grew up. (ah) [Long pause for breath] What are the family circumstances? A detailed assessment is important. (P2, L. 42).
History taking and the initial interview are always a good start for me, so to get to know, no matter which person is in front of me now. I would make a difference, but it is about gathering information about the person and the person and documenting things that are important to him or her (long pause for breath), and then it is also a matter of disseminating that further within the team. For this purpose, communication must be possible. (P8, L. 44)
Prejudices should be put aside on the part of the caregiver to approach the person in a completely unprejudiced manner to establish a communicative relationship. I believe that if the patient trusts us, it is important that we all (aah) so that we try to understand. (a) We cannot expect everybody to understand us. (P5, L. 52).
Some respondents stated that cultural characteristics had no role in establishing a professional relationship, while others claimed the opposite: it would certainly be professional if you knew the culture or the patient’s origin and if you simply responded to the individual needs. However, this often gets lost in everyday life and in stress through the automatic process that we simply know. (P7, L. 48).
Acknowledging individuality might even make work with people of diverse cultures more rewarding. And then I realised, gosh, how much I enjoy it when people like me, when I like the people like, when they build relationships . (P9, L. 30).
The participants’ curiosity about foreign cultures was considered an advantage to increase their knowledge and broaden their horizon: I always find something like that quite cool, because I always ask people how it is at their homes when I have the time because you never stop learning and I always find new cultural aspects, religious aspects, ethnic aspects, and things to get to know. (P1, L. 32) It is, yes, interesting to get to know a new culture. This represents an increase in knowledge. It encourages you to question your actions and reflect on yourself. (P2, L. 34).
To overcome the language barrier, participants exploited diverse opportunities and secured a trustful relationship with their patients. The team evaluated whether someone spoke the respective language to take responsibility for caregiving. Additionally, relatives were used as interpreters. A list of standard questions and a small dictionary from the ward were used. Since employees can hardly cover the entire repertoire of languages, support by interpreting services could be received by nurses, and when it comes to relevant, even more relevant things, such as psychological problems or explanations, there is a video interpreting service in the house, which you can request. We use that very often . (P2, L. 26).
Language assistance can be provided through various media and applications. Cell phones enable them to translate sentences quickly and easily . Everyone has a cell phone, everyone can type in ‘how are you or do you want something to drink or eat’ [long breath], and the device translates it automatically. Reading is something that most people can do, but it also has a voice function. This was a simple strategy. (P7, L. 44).
Some communication may not be restricted to the linguistic level. Facial expressions and gestures were interpreted in addition to vital signs to obtain indications of the patient’s condition. Even if language is a barrier, there are still gestures and facial expressions that do not always present themselves as barriers. (P3, L. 30).
Possibilities of the organizations
Healthcare institutions need to coin the term cultural safety and create an overarching awareness of it. Employers should exemplify it and translate it to the mission statement: Yes, we have a prayer room anyway and that is not the end of culture, and a hospital must stand up for it and that is not yet the case. I know the mission statements of the two hospitals, and there it says, for example, I do not know whether sexual orientation is specifically mentioned. These topics were completely indifferent. (P1, L. 52).
The nurses suggested holding language courses for employees, building prayer rooms, expanding chaplaincy, and organising cultural festivals. There was a need for easier access to information and introducing a qualified care expert as a contact person, which shows that they welcome information material in different languages, for example, so that the patient then clearly notices: Oops, they are prepared for me and my culture . (P9, L. 36).
Education and training are frequently mentioned as a means of improving cultural safety in hospitals. Education on cultural issues was offered routinely, but cultural safety was not covered mostly by the curricula, which was also part of it for me. With further training and (aah) further training, especially through the introduction of nursing experts, which for me can play a significant role in improving such topics and can play a key role in taking up such topics and bringing them in accordingly to train the team to implement and connect these conceptualisations, disseminate and verbalise, and complete and communicate. (P3, L. 40).
A multicultural care team has great benefits for patients and the entire health care sector; therefore, it is enormously useful because I think yes, as culturally diverse as we are in the care team, as diverse are the patients who come. (P9, L. 22).
Teams with a high degree of diversity had diverse resources ranging from language skills to religious understanding: We are a multicultural team and I think that can be transferred to the Austrian care landscape accordingly. This means that we have so many resources and so many human, cultural, and religious resources that we can use to provide adequate, humane, goal-oriented, and professional care (aah). (P3, L. 34).
A diverse nursing team had easier access to the patient, but also the general openness towards foreign cultures increased; we have a lot of foreign staff who have been here for a long time, for example, from Slovenia, Slovakia, and Croatia, so they are all mixed up, which is why we are a bit more open . (P6, L. 40).
A team of culturally diverse employees could be better prepared to grasp the importance of cultural safety, since they might have been in unpleasant situations themselves and could share these experiences with their colleagues, which enriches the whole [team]. Me. That is great. I feel so comfortable. (P9, L. 22).
Proactive involvement of family members
Family members and relatives were enriched in developing a caring relationship. Strong family cohesions were created during visits. Yes, what is often the case with us is that you can see how the family sticks together; for example, there are always visitors, especially in the palliative setting, how much they care for their relatives. That is a big cohesion, so that is with us Austrians, if I say it now so casually, not so big, as there, the family is written in capital letters. (P6, L. 36).
The participants should pay attention to integrating and involving families in the care process, and I have always received positive feedback from these families. So I have noticed that it is less often a single person, but that it was more often a family that was cared for. (P8, L. 28).
Those patients who had a powerful sense of family could benefit from it as it contributed to recovery: Well, I do find, [long pause for breath] that one often sees that the visit of the relatives to the patients can already make a difference. (P7, L. 37).
Phase 2: nominal group meeting
The most dominant themes of the nominal group interview were ‘communication difficulties,’ ‘lack of knowledge and understanding of how to treat people who do not have sufficient language skills,’ ‘having a different perception of nursing care,’ or ‘expectations towards treatment goals and outcomes,’ which could lead to conflicts.
After analysing and combining the results of Phases 1 and 2, three themes were developed: ‘physical distance and contact’, ‘pain management (and perception)’, and ‘personal hygiene requirements’. Five subthemes of ‘the socialisation of nurses,’ ‘different care goals,’ and ‘allocations of unequal treatment based on culture,’ were added to the theme ‘conflicts. A lack of knowledge regarding religious rituals and grief management was added to the theme of ‘religion.’ All of these additions constituted the category of barriers to cultural safety. In terms of prospects of cultural safety, the value-free approach was added as a subtheme to the theme ‘possibly of nursing staff’. The possibilities of the organisation were expanded with three subthemes: ‘translation services,’ reflection rounds,’ and ‘introducing experts in cultural safety to the wards.’ The findings are presented as a tree diagram, combining the findings from phases 1 and 2 (Fig. 1 ).

Cultural Safety: meaning, barriers, prospects
All participants in the nominal group pointed out the need for information, knowledge, and continuing education. It became evident that the APNs expected the nursing curriculum and continuous education to increase their knowledge about cultural differences and religious traditions and provide practical communication strategies to overcome cultural barriers. Challenging nurses’ cultural biases and adapted behaviours via self-reflection were suggested less frequently. Organisations are expected to acknowledge the need for cultural safety through diversity management, reflection rounds, and evaluations. Participants’ requirements and expectations towards education are shown in Fig. 2 .
Requirements and expectations toward nursing curriculum and continuing education
In 2016, Bozorgzad et al. wrote: “Healing occurs in a safe milieu, and patients feel safe when service providers view them as whole persons, recognizing the multiple underlying factors that cause illness. Cultural safety can lead to service delivery in this way, but most nurses have no clear understanding of this concept.” [ 37 ]. The findings of this study confirm that the APNs do not have a clear understanding of the phenomenon of cultural safety. The admitted APNs were equally ambivalent and lacked knowledge of established concepts, such as transcultural nursing, equity, cultural awareness, cultural safety, or respective competencies. They expected the nursing curriculum and continuous education to increase their cultural competencies, but they did not understand that the concept of cultural safety goes far beyond the acquisition of information, such as religious or dietary needs. Some of the APNs eagerly proposed their definitions of cultural safety, arguing that cultural safety acknowledges the importance of patient-family centred approaches and may help avoid stereotyping patients and their families based on their language, culture, religion, or ethnicity. Similarly, the international literature suggests that approaching the patient, emphasizing on the humanistic aspects of care in terms of hope and life, reducing the feeling of loneliness during hospitalization, paying attention to patients’ needs, sympathizing, and respecting them, and taking their concerns seriously can promote the feeling of safety among hospitalized patients [ 38 ].
Heeding cultural safety concerns healthcare staff as much as it concerns patients. Patient safety programs often underestimate the relationship between culture, language, and safety and quality of care [ 39 ]. This calls for organizational change that ensures appropriate communication with patients and their families, and supports policies that put in place improvement strategies [ 40 , 41 , 42 ], such as reflection rounds or cultural safety briefings at their workplaces [ 43 , 44 , 45 ]. Ideally, the education and deployment of nursing experts with a focus on cultural issues would be helpful [ 46 ]. Discrimination and even indifference towards patients who do not speak the language may have damaging consequences for patients, affecting their emotional, spiritual and physical wellbeing [ 47 ]. Our study findings indicate that patients who were unable to communicate due to poor language skills were systematically left without care. This is a clear example of a lack of access to healthcare and a lack of health equity in healthcare facilities. Taking care of people who do not understand the language or who are poorly educated takes more time and can be emotionally draining. Compensation and support should be offered to nurses taking over a mediating role. Culturally diverse nurses are considered assets in terms of language skills and cultural competencies when cultural clashes emerge. However, in our study, culturally diverse APNs admitted their familiarity with prejudices, discrimination, and racism, which was presented as a taboo topic. Whereas, patient safety culture and the second victim phenomenon has been described as causing distress in nurses [ 48 ], this study emphasises the first victim experience in culturally diverse nurses.
Power represents an essential distinction between cultural competence and cultural safety [ 15 , 16 , 37 ]. Healthcare providers should reflect on interpersonal power differences and acknowledge the power differences between nurses and patients. The topic of power was not discussed in our explorative study, which could be because of the traditional development of nursing in German-speaking countries. Nursing as an independent and academic discipline has developed very slowly in Austria, Germany, and Switzerland, compared to the international context. In Austria, basic training in nursing was shifted to the tertiary level with a change in the law in 2016 [ 49 ], university and academic training in nursing is still a much-discussed topic. The service to the patient according to the principle of Christian charity is in the foreground, strictly maintaining the attitude that the doctors order the interventions and the nurses perform them. In many cases, there is still a lack of awareness of one’s own professional role and the power it entails in the relationship between patient and nurse.
The issue of visiting relatives divided the APNs. Large families were perceived as a source of support and taking on caring responsibilities, but others saw it as a hindrance due to noise and disturbance. Despite ongoing criticism of the exhaustion of family members as interpreters [ 50 ], relatives were perceived as helpful in overcoming communication barriers. Supporting relational, culturally safe care focuses on building the conversation, engaging the family, closing the conversation gap and improving health literacy to reduce power imbalances [ 15 ]. Some nurses found it personally and professionally fulfilling to be proactive in informing, involving and communicating with family members to better understand the patient’s needs.
Nurses need to evaluate and question their cultural backgrounds and adapt their behaviours rather than pushing for the mere acquisition of competencies in different cultures and religions [ 16 ]. APNs admitted that they do not provide culturally safe care, but unanimously asserted that they strive to provide such care. They cited several characteristics of safe patient care in terms of removing language barriers and overcoming misunderstandings as the first step in building a professional nursing relationship. It became clear that reflecting on one’s own values, attitudes, assumptions, prejudices and stereotypes is essential for culturally safe care. Nurses mentioned that self-reflection must be an ongoing process to ensure culturally safe care on a continuous basis. Our study described many components that can contribute to improving cultural safety. Previously introduced concepts such as transcultural care, cultural sensitivity, cultural awareness and competencies were interpreted as prerequisites for cultural safety. Other important aspects were professional flexibility, openness and tolerance of nurses in caring for culturally diverse patients and their families. In addition, APNs argued that an atmosphere free of intimidation and fear promotes overall health [ 38 , 48 ]. Accordingly, the concept of cultural safety offers the possibility of ensuring better access to healthcare for culturally diverse patients and their families in pluralistic societies [ 51 ].
Strengths and limitations to the study
This is the first study on cultural safety in a European context, which underlines the novelty of the research topic. The simultaneous use of interviews and nominal groups for data collection from APNs working in health facilities in three countries helped to improve the variation and depth of data collection and certainly represents our research strength. In terms of informativeness, this qualitative study benefited from it through the use of the nominal group meeting in Phase 2 to validate the findings of Phase 1 and contribute to the development of new knowledge.
Online interviews cannot replace face-to-face interactions, but they offer a viable alternative [ 52 ]. A comparison of online interviews and face-to-face interviews shows that participants are more open and expressive online, while maintaining a relationship requires more effort [ 53 ].
Conclusions
Communication difficulties, insufficient language skills, different perceptions and expectations of care and treatment outcomes were mentioned as important aspects of cultural safety in German-speaking health facilities. There is a need for self-reflection sessions and translation services for nurses responsible for the care of patients with diverse cultural backgrounds in order to improve equality and the feeling of safety during the hospital stay. In addition, the presence of prejudice, discrimination and even racism in the healthcare culture should be assessed and remedial strategies developed and implemented using diversity management and leadership. Education and training are needed to bridge the gap between the perceived educational needs of nurses and the requirements of safe care, and to address challenging personal behaviours in the multicultural healthcare environment. Future studies should examine the impact of cultural safety improvement programmes on patient care outcomes.
Availability of data and materials
The anonymous data and the analysis process used in this study are available from the corresponding author upon reasonable request.
UN Office of the High Commissioner for Human Rights. Fact Sheet No. 31, The Right to Health. 2008. ( https://www.refworld.org/docid/48625a742.html June 2008, No. 31, Retrieved May 2, 2021).
Google Scholar
International Council of Nurses. The ICN Code of Ethics for Nurses. 2021. ( https://www.icn.ch/system/files/2021-10/ICN_Code-of-Ethics_EN_Web_0.pdf Retrieved February 10, 2022).
Papps E, Ramsden I. Cultural Safety in Nursing: the New Zealand Experience. Int J Qual Health Care. 1996;8(5):491–7. https://doi.org/10.1093/intqhc/8.5.491 .
Article CAS PubMed Google Scholar
Sy A. Who Defines Culturally Acceptable Health Access? Universal rights, healthcare politics and the problems of two Mbya-Guarani communities in the Misiones Province, Argentina. Health Cult Soc. 2013;4:1–19. https://doi.org/10.5195/hcs.2013.24 .
Article Google Scholar
National Committee for Quality Assurance. A Practical Guide to Implementing the National CLAS Standards: For Racial, Ethnic and Linguistic Minorities, People with Disabilities and Sexual and Gender Minorities. 2016. ( https://www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/CLAS-Toolkit-12-7-16.pdf Retrieved May 2, 2021).
European Council. A New European Agenda for Culture. 2018. ( https://ec.europa.eu/culture/document/new-european-agenda-culture-swd2018-267-final Retrieved May 2, 2021).
Power T, Geia L, Adams K, Drummond A, Saunders V, Stuart L, Deravin L, Tuala M, Roe Y, Sherwood J, Rowe Minniss F, West R. Beyond 2020: addressing racism through transformative indigenous health and cultural safety education. J Clin Nurs. 2021;30(7–8):e32–5. https://doi.org/10.1111/jocn.15623 .
Article PubMed Google Scholar
Perry A, Woodland L, Brunero S. eSimulation: a novel approach to enhancing cultural competence within a health care organisation. Nurse Educ Pract. 2015;15(3):218–24. https://doi.org/10.1016/j.nepr.2014.11.013 .
Richardson S, Williams T. Why is cultural safety essential in health care? Med Law. 2007;26:699–707.
PubMed Google Scholar
Bundesrepublik für Migration, Flüchtlinge und Integration. Memorandum für eine kultursensible Altenhilfe Ein Beitrag zur Interkulturellen Öffnung am Beispiel der Altenpflege. 2009. ( https://www.demenz-und-migration.de/fileadmin/user_upload/pdf/memorandum_fuer_eine_kultursensible_Altenhilfe.pdf Retrieved May 2, 2021).
World Health Organization. Declaration of Astana: Global Conference on Primary Health Care. 2019. ( https://apps.who.int/iris/handle/10665/328123 Retrieved May 2, 2021).
Helman, C.G. Culture, Health and Illness. 4th Ed. London: Hodder Arnold. 2000.
Paal, P. Culturally sensitive palliative care research: what should we do with ‘those people’, or what should we do with ourselves? In: K. Kuehlmeyer, C. Klingler & R. Huxtable (eds.) Ethical, Legal and Social Aspects of Healthcare for Migrants: Perspectives from the UK and Germany. London&New York: Routledge. 2018. p. 162–75.
Cubillos, F.A. Pflege in einer internationalen und transkulturellen Gesellschaft. In: A. Merx (ed.) Charta der Vielfalt: WELTOFFEN = ZUKUNFTSFÄHIG?! Diversity Management & Internationalität (pp. 62–64). Retrieved May 2, 2021, from: https://www.charta-der-vielfalt.de/fileadmin/user_upload/Studien_Publikationen_Charta/Weltoffen_Zukunftsf%C3%A4hig_CdV-Dossier.pdf
Curtis E, Jones R, Tipene-Leach D, Walker C, Loring B, Paine SJ, Reid P. Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. Int J Equity Health. 2019;18:174. https://doi.org/10.1186/s12939-019-1082-3 .
Article PubMed PubMed Central Google Scholar
Wilson C, Crawford K, Adams K. Translation to practice of cultural safety education in nursing and midwifery: A realist review. Nurse Educ Today. 2022;110:105265. https://doi.org/10.1016/j.nedt.2022.105265 .
Dicuccio MH. The Relationship Between Patient Safety Culture and Patient Outcomes: A Systematic Review. J Patient Saf. 2015;11(3):135–42. https://doi.org/10.1097/PTS.0000000000000058 .
Pumar-Méndez MJ, Attree M, Wakefield A. Methodological aspects in the assessment of safety culture in the hospital setting: A review of the literature. Nurse Educ Today. 2014;34(2):162–70. https://doi.org/10.1016/j.nedt.2013.08.008 .
International Council of Nurses. The scope of practice, standards and competencies of the advanced practice nurse. ICN Regulatory Series. Geneva: ICN; 2008.
International Council of Nurses. Guidelines on advanced practice nursing 2020. International Council of Nurses (ICN). 2020. Retrieved February 10, 2022, from: https://www.icn.ch/system/files/documents/2020-04/ICN_APN%20Report_EN_WEB.pdf
Hamric AB, Spross JA, Hanson CM. Advanced Practice Nursing: An Integrative Approach. 4th ed. Oxford: Elsevier; 2008.
Glarcher M, Lex KM. Advanced Nursing Practice in Austria under consideration of outcome measurement. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen (ZEFQ). 2020. https://doi.org/10.1016/j.zefq.2020.06.012 .
Book Google Scholar
Spichiger E, Zumstein-Shaha M, Schubert M, Herrmann L. Gezielte Entwicklung von Advanced Practice Nurse-Rollen für spezifische Patient(inn)engruppen in einem Schweizer Universitätsspital. Pflege. 2018;31(1):41–50.
Bachner F, Bobek J, Habimana K, Ladurner J, Lepuschütz L, Ostermann H, Rainer L, Schmidt AE, Zuba M, Quentin W, Winkelmann J. Austria: Health system review. Health Syst Trans. 2018;20(3):1–256.
Weiss, S., Ditto, M., Füszl, S., Lanske, P., Lust, A., Oberleitner-Tschan, C., Wenda, S. Healthcare professions in Austria. Federal Ministry of Health and Women’s Affairs, Division II, 2017. Retrieved May 23, 2022, form: https://broschuerenservice.sozialministerium.at/Home/Download?publicationId=600
Schäfer, D. Die Zukunft der „Advanced Practice Nurse“ in Österreich. Pflege Professionell, 2018. 25.06.2018, Retrieved May 23, 2022, from: https://pflege-professionell.at/die-zukunft-der-advanced-practice-nurse-in-oesterreich
DeutscherBerufsverbandfürPflegeberufe - DBfKBundesverbande.V. Advanced Practice Nursing Pflegerische Expertise für eine leistungsfähige Gesundheitsversorgung. 2019. ( https://www.dbfk.de/media/docs/download/Allgemein/Advanced-Practice-Nursing-Broschuere-2019.pdf Retrieved May 23, 2022).
Lamnek S, Krell, C. Qualitative Sozialforschung: Mit Online-Materialien. 6th Ed. Psychologie Verlagsunion. Weinheim: Peltz; 2016.
Flick U, Kardoff E, Steinke I. Qualitative Forschung. Hamburg: Rowohlt Taschenbuchverlag; 2019.
Malterud K, Siersma VD, Guassora AD. Sample Size in Qualitative Interview Studies: Guided by Information Power. Qual Health Res. 2016;26(13):1753–60. https://doi.org/10.1177/1049732315617444 .
International Council of Nurses. Definition and Characteristics of the Role. 2009. ( https://international.aanp.org/Practice/APNRoles Retrieved May 2, 2021).
Ammouri A, Tailakh A, Muliira J, Geethakrishnan R, Al Kindi S. Patient safety culture among nurses. Int Nurs Rev. 2015;62:102–10. https://doi.org/10.1111/inr.12159 .
Kuckartz, U. Qualitative Inhaltsanalyse. Methoden, Praxis, Computerunterstützung. Weinheim und Basel: Beltz Juventa; 2016.
Clarke V, Braun V. Thematic analysis. J Posit Psychol. 2017;12(3):297–8. https://doi.org/10.1080/17439760.2016.1262613 .
Vaismoradi M, Jones J, Turunen H, Snelgrove S. Theme development in qualitative content analysis and thematic analysis. J Nurs Educ Pract. 2016;6(5):100–10. https://doi.org/10.5430/jnep.v6n5p100 .
Mcmillan S, Kelly F, Sav A, Kendall E, King MA, Whitty JA, Wheeler AJ. Using the nominal group technique: How to analyse across multiple groups. Health Serv Outcomes Res Methodol. 2014;14:92–108. https://doi.org/10.1007/s10742-014-0121-1 .
Bozorgzad P, Negarandeh R, Raiesifar A, Poortaghi S. Cultural Safety: An Evolutionary Concept Analysis. Holist Nurs Pract. 2016;30(1):33–8. https://doi.org/10.1097/HNP.0000000000000125 .
Vaismoradi M, Salsali M, Turunen H, Bondas T. Patients’ understandings and feelings of safety during hospitalization in Iran: A qualitative study. Nurs Health Sci. 2011;13:404–11. https://doi.org/10.1111/j.1442-2018.2011.00632.x .
Johnstone M-J, Kanitsaki O. Culture, language, and patient safety: making the link. Int J Qual Health Care. 2006;18(5):383–8. https://doi.org/10.1093/intqhc/mzl039 .
Hudelson P, Vilpert S. Overcoming language barriers with foreign-language speaking patients: a survey to investigate intra-hospital variation in attitudes and practices. BMC Health Serv Res. 2009;9:187. https://doi.org/10.1186/1472-6963-9-187 .
Verbakel NJ, Langelaan M, Verheij TJM, Wagner C, Zwart DL. Improving Patient Safety Culture in Primary Care: A Systematic Review. J Patient Saf. 2016;12(3):152–8. https://doi.org/10.1097/PTS.0000000000000075 .
Gurková E, Zeleníková R, Friganovic A, Uchmanowicz I, Jarošová D, Papastavrou E, Žiaková K. Hospital safety climate from nurses’ perspective in four European countries. Int Nurs Rev. 2020;67:208–17. https://doi.org/10.1111/inr.12561 .
Flanagan E, Chadwick R, Goodrich J, Ford C, Wickens R. Reflection for all healthcare staff: A national evaluation of Schwartz Rounds. J Interprof Care. 2020;34(1):140–2. https://doi.org/10.1080/13561820.2019.1636008 .
Ryan S, Ward M, Vaughan D, Murray B, Zena M, O’Connor T, Nugent L, Patton D. Do safety briefings improve patient safety in the acute hospital setting? A systematic review. J Adv Nurs. 2018;75:2085–98. https://doi.org/10.1111/jan.13984 .
Weaver SJ, Lubomksi LH, Wilson RF, Pfoh ER, Martinez KA, Dy SM. Promoting a Culture of Safety as a Patient Safety Strategy A Systematic Review. Ann Intern Med. 2013;158(5):369–72. https://doi.org/10.7326/0003-4819-158-5-201303051-00002 .
Salmela S, Koskinen C, Eriksson K. Nurse leaders as managers of ethically sustainable caring cultures. J Adv Nurs. 2017;73(4):871–82. https://doi.org/10.1111/jan.13184 .
Schrank B, Rumpold T, Amering M, Masel EK, Watzke H, Schur S. Pushing boundaries — culture-sensitive care in oncology and palliative care: a qualitative study. Psychooncology. 2017;26:763–9. https://doi.org/10.1002/pon.4217 .
Quillivan RR, Burlison JD, Browne EK, Scott SD, Hoffman JM. Patient Safety Culture and the Second Victim Phenomenon: Connecting Culture to Staff Distress in Nurses. Jt Comm J Qual Patient Saf. 2016;42(8):377-AP2. https://doi.org/10.1016/S1553-7250(16)42053-2 .
Schaeffer, D. Nursing science and research: quo vadis? In E. Seidl & I. Walter (Eds.), Current nursing research. Studies-Comments-Reports. Pflegewissenschaft heute, 7. Wien, München, Bern: Maudrich. 2002. p. 129–50.
Barclay JS, Blackhall LJ, Tulsky JA. Communication Strategies and Cultural Issues in the Delivery of Bad News. J Palliat Med. 2007;10:958–77. https://doi.org/10.1089/jpm.2007.9929 .
Latif AS. The Importance of Understanding Social and Cultural Norms in Delivering Quality Health Care—A Personal Experience Commentary. Trop Med Infect Dis. 2020;5(1):22. https://doi.org/10.3390/tropicalmed5010022 .
Article PubMed Central Google Scholar
LaIacono V, Symonds P, Brown DHK. Skype as a Tool for Qualitative Research Interviews. Sociol Res Online. 2016;21:103–17. https://doi.org/10.5153/sro.3952 .
Gray LM, Wong-Wylie G, Rempel GR, Cook K. Expanding Qualitative Research Interviewing Strategies: Zoom Video Communications. Qual Rep. 2020;25(9):1292–301. https://doi.org/10.46743/2160-3715/2020.4212 .
Download references
Acknowledgements
The authors appreciate the sincere participation of the APNs and sharing their perspectives.
The authors received no financial support for the research, authorship, and/or publication of this article. The open access fee was paid by Parcelsus Medical University in Salzburg, Austria.
Author information
Authors and affiliations.
Institute of Nursing Science and Practice, Paracelsus Medical University, Strubergasse 21, 5020, Salzburg, Austria
Jacqueline Pirhofer, Johannes Bükki, Manela Glarcher & Piret Paal
Diakonie-Klinikum Stuttgart, Rosenbergstrasse 38, 70176, Stuttgart, Germany
Johannes Bükki
Faculty of Nursing and Health Sciences, Nord University, 8049, Bodø, Norway
Mojtaba Vaismoradi
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualisation and methodology, PP; formal analysis, JP and PP; investigation, JP; writing—original draft preparation, review, and editing, JP, PP, JB, MG, MV, PP; supervision, PP. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Piret Paal .
Ethics declarations
Ethics approval and consent to participate.
According to the Ethics Committee of the Medical Faculty of Johannes Kepler University (Linz/Austria), formal approval for this study was not needed as vulnerable persons were not involved (decree code: 09.09.2020). The participants were informed both orally and in writing about the purpose of the study and their voluntary participation. The participants were asked to sign an informed consent form. Permission to record their voices was obtained prior to data collection. Written informed consent for publication was obtained from all the participants. The participants could withdraw from the study at all times, and all efforts were made to ensure anonymity and confidentiality of the collected data. Our research was reported in accordance with the COnsolidated Criteria for REporting Qualitative Research (COREQ) checklist.
Consent for publication
Not Applicable.
Competing interests
The authors certify that they have no affiliations with or involvement in any organisation or entity with any financial or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pirhofer, J., Bükki, J., Vaismoradi, M. et al. A qualitative exploration of cultural safety in nursing from the perspectives of Advanced Practice Nurses: meaning, barriers, and prospects. BMC Nurs 21 , 178 (2022). https://doi.org/10.1186/s12912-022-00960-9
Download citation
Received : 01 December 2021
Accepted : 27 June 2022
Published : 04 July 2022
DOI : https://doi.org/10.1186/s12912-022-00960-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cultural safety
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
24/7 writing help on your phone
To install StudyMoose App tap and then “Add to Home Screen”
Cultural safety in nursing
Save to my list
Remove from my list

Cultural safety in nursing. (2016, Jul 29). Retrieved from https://studymoose.com/cultural-safety-in-nursing-essay
"Cultural safety in nursing." StudyMoose , 29 Jul 2016, https://studymoose.com/cultural-safety-in-nursing-essay
StudyMoose. (2016). Cultural safety in nursing . [Online]. Available at: https://studymoose.com/cultural-safety-in-nursing-essay [Accessed: 28 Aug. 2024]
"Cultural safety in nursing." StudyMoose, Jul 29, 2016. Accessed August 28, 2024. https://studymoose.com/cultural-safety-in-nursing-essay
"Cultural safety in nursing," StudyMoose , 29-Jul-2016. [Online]. Available: https://studymoose.com/cultural-safety-in-nursing-essay. [Accessed: 28-Aug-2024]
StudyMoose. (2016). Cultural safety in nursing . [Online]. Available at: https://studymoose.com/cultural-safety-in-nursing-essay [Accessed: 28-Aug-2024]
- Patient Safety in Rural Nursing Because of Nursing Shortage Pages: 7 (1814 words)
- Car Safety Features - Safety on the Road Pages: 6 (1738 words)
- Impact of Nursing Leadership on Nursing Job Satisfaction Pages: 6 (1578 words)
- Professional Identity in Nursing and Nursing Philosophy Pages: 3 (727 words)
- Nursing: Clinical Reflection of the Nursing Students' Performance Pages: 4 (936 words)
- Professional Nursing Organizations and Regulatory Agencies in Nursing Practice Pages: 4 (1194 words)
- Nursing as an Art and Science: Nursing Concepts, Barriers, Facilitators Pages: 4 (1077 words)
- Factors That Influence The Clinical Learning Experience Of Nursing Students At a Caribbean School Of Nursing Pages: 4 (1020 words)
- Cultural Diversity in Nursing Pages: 5 (1377 words)
- The Nursing Profession - a Study of Cultural Diversity and Spirituality Issues Pages: 8 (2229 words)
👋 Hi! I’m your smart assistant Amy!
Don’t know where to start? Type your requirements and I’ll connect you to an academic expert within 3 minutes.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Reflexive Practice as an Approach to Improve Healthcare Delivery for Indigenous Peoples: A Systematic Critical Synthesis and Exploration of the Cultural Safety Education Literature
Jessica dawson.
1 School of Psychology, University of Adelaide, Adelaide, SA 5000, Australia
2 Poche SA+NT, Flinders University, Bedford Park, SA 5042, Australia
Keera Laccos-Barrett
3 College of Nursing & Health Sciences, Flinders University, Bedford Park, SA 5042, Australia; [email protected]
Courtney Hammond
4 School of Public Health, University of Adelaide, Adelaide, SA 5000, Australia; [email protected]
5 Wardliparingga Aboriginal Health Equity Unit, SAHMRI, Adelaide, SA 5000, Australia
Alice Rumbold
6 Women and Kids Theme, SAHMRI, Adelaide, SA 5000, Australia; [email protected]
7 Adelaide Medical School, The University of Adelaide, Adelaide, SA 5000, Australia
Associated Data
All data are publicly available as this is a review article. Data are summarised in Table 1 (Summary of key characteristics of the educational interventions included).
Cultural safety is increasingly being taught in tertiary programmes of study for health professionals. Reflexivity is a key skill required to engage in culturally safe practice, however, there is currently limited literature examining how reflexivity is taught or assessed within cultural safety curricula. A systematic review of the literature up until November 2021 was conducted, examining educational interventions which aimed to produce culturally safe learners. Studies were limited to those with a focus on Indigenous health and delivered in Australia, Aotearoa New Zealand, Canada, and the United States. A total of 46 documents describing 43 different educational interventions were identified. We found that definitions and conceptualisations of reflexivity varied considerably, resulting in a lack of conceptual clarity. Reflexive catalysts were the primary pedagogical approaches used, where objects, people, or Indigenous pedagogies provided a counterpoint to learners’ knowledges and experiences. Information regarding assessment methods was limited but indicates that the focus of existing programmes has been on changes in learner knowledge and attitudes rather than the ability to engage in reflexivity. The results demonstrate a need for greater conceptual clarity regarding reflexivity as it relates to cultural safety, and to develop methods of assessment that focus on process rather than outcomes.
1. Introduction
The beliefs, attitudes, and biases that healthcare professionals hold can substantially influence the way they interact with and provide care to people. This is particularly relevant to the health and well-being of Aboriginal and Torres Strait Islander Australians, where healthcare professional attitudes are seen as a major factor in whether care is considered safe, adequate, and acceptable [ 1 , 2 , 3 ]. Dismissive, rude, and outright racist behaviours have been reported by Aboriginal and Torres Strait Islander people in their encounters with non-Indigenous healthcare professionals. These experiences can result in inadequate or negligent care provision and deter recipients of care from further engaging with a healthcare system that is perceived as culturally unsafe [ 4 , 5 , 6 ]. In turn, this can have significant flow-on effects for healthcare access and outcomes and contributes to the health inequities experienced by Aboriginal and Torres Strait Islander people. Parallels can be seen in Aotearoa New Zealand, Canada, and the United States, where racial discrimination and culturally unsafe care contribute to inequities in healthcare access and outcomes for Indigenous peoples [ 7 , 8 , 9 ].
Cultural safety is recognised as an approach to healthcare with the potential to improve the experience of care for Indigenous peoples in Australia, Aotearoa New Zealand, Canada, and the United States. The concept of cultural safety was originally developed in Aotearoa New Zealand by Māori nurses and midwives, to address the racism experienced by Māori patients being cared for by a largely non-Indigenous health workforce [ 10 , 11 ]. Cultural safety in healthcare delivery recognises the centrality of culture to health and well-being and seeks to ensure that healthcare is respectful and non-discriminatory. To provide culturally safe care, healthcare professionals need to engage in critical reflexivity, whereby they examine their own cultural identity, positioning and power, the values, attitudes, and biases they carry, and the potential consequences of these for the people they provide care to [ 12 , 13 , 14 , 15 ].
The importance of cultural safety as an approach to healthcare provision is now well established, with a substantial body of literature exploring the application of cultural safety across a range of health professions, including nursing and midwifery [ 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 ], medicine [ 24 , 25 , 26 , 27 , 28 ], psychology [ 29 ], physiotherapy [ 30 ], occupational therapy [ 31 , 32 ], and nutrition [ 33 ]. As such it is increasingly being included in health sciences curricula at the tertiary level in Australia, Aotearoa New Zealand, Canada, and the United States [ 34 ] and developed as short continuing professional education courses (for example, [ 35 , 36 , 37 ]). While there is a growing body of literature exploring best practice approaches to the development and delivery of cultural safety education, this predominantly focuses on overall curriculum structure and content (for example [ 20 , 31 , 38 ]). Currently, however, there is little guidance on the most appropriate pedagogical approaches to teach students how to be reflexive, or on how educators should assess student learning outcomes concerning reflexivity. Given the centrality of reflexivity to culturally safe practice, we argue that there is a need to develop best practice approaches to the teaching and assessment of reflexivity within cultural safety education.
Reflexivity and Cultural Safety
The way reflexivity is defined, conceptualised, and operationalised varies both across and within fields and disciplines, depending on the purpose to which it is being put [ 39 , 40 ]. At its core, reflexivity involves an awareness and examination of the ontological and epistemological foundations that inform our existence and shape our thoughts and behaviours [ 39 , 41 ]. Notably, reflexivity is concerned with the self in relation to others; that is, how our ways of knowing, being, and doing shape our interpretation of and behaviour towards people [ 40 , 42 ]. Despite its centrality to culturally safe practice, reflexivity has not been specifically defined or conceptualised in this context. In her account of reflexive, culturally safe research, Wilson draws on the broader research literature to define reflexivity as a tool “to gain greater understanding of the self/other positionalities and the experience of research” [ 42 ] (p. 219). How this might be adapted into healthcare contexts and included in cultural safety education is yet to be determined.
In the context of cultural safety, reflexivity serves several purposes, and each presents challenges for educators and students alike. Perhaps the most cited purpose of reflexivity is the examination of own cultural worldviews and values and how these might influence delivery of care to people from different cultural backgrounds [ 43 , 44 ]. Notably, there is an acknowledgement that ‘culture’ is a complex intersection of factors such as race, ethnicity, gender, age, socioeconomic status, disability status, geographical location, and sexual orientation, among others [ 34 , 43 , 44 ]. Arguably, this complexity presents students with a significant challenge of understanding their own intersectional nature. Given the tendency of cultural safety education to focus on Indigenous health, there is a risk that this type of curricula reinforces a false dichotomy of Indigenous and non-Indigenous identity, resulting in a curriculum more akin to cultural competency training [ 13 , 45 ]. It also risks diminishing the complexity of Indigenous identity, which encompasses more than ethnicity on its own [ 46 , 47 ]. Further, as Lumsden [ 39 ] (p. 3) notes, there is an inherent risk that reflexivity can easily become entangled in notions of individual identity, “while failing to recognize the wider disciplinary, institutional, and political context(s) in which reflexivity…takes place, and in which knowledge is constructed, situated, and (re)negotiated”. In cultural safety education, and specifically in the context of Indigenous health, considerations of these broader contexts and the sites and methods of knowledge (re)production are essential.
The development of reflexive skills and the exploration of own cultural identity most often occurs in conjunction with learning about the social determinants of Indigenous health. In colonised countries like Australia, Aotearoa New Zealand, Canada, and the United States, this includes developing an understanding of historical and ongoing processes of colonisation, and the resulting interpersonal and institutional racism, whiteness, and power differentials. Students also need to develop an understanding of how these factors intersect with other social determinants such as education, employment, housing, and food security to produce the health inequities that Indigenous people experience [ 13 , 43 , 48 ]. In part, this learning is intended to help students understand that health is the product of social, economic, political, and historical forces [ 44 ]. It is also an opportunity for students to become aware of and challenge their own internalised stereotypes, assumptions, and biases through exposure to new learning. Yet this can be a challenging process for students, one which has been consistently shown to produce feelings of discomfort for students [ 48 , 49 , 50 ]. These feelings of discomfort can range from disengagement in class to outright hostility towards content, learning, and educators. This discomfort, if carefully managed, can produce transformative learning experiences for students. Conversely, poorly managed discomfort may serve to reinforce negative attitudes towards learning, content, and Indigenous people themselves [ 48 , 49 , 50 ].
Additionally, students are expected to engage in this complex, deeply personal, and potentially uncomfortable learning process in the context of a tertiary educational institution. While educators might strive to provide genuinely transformative learning experiences, the reality for students is that they need to pass their studies. Faced with the task of engaging reflexively, there is a risk that students will simply provide the responses they think educators want. This has been acknowledged as a potential issue in the literature [ 39 , 49 , 51 , 52 , 53 ] but has not been explored in-depth regarding whether and to what extent this occurs within cultural safety education.
While there is a growing body of literature on cultural safety education, at present, there is little guidance on the best approach to teach or assess reflexivity in the context of cultural safety. Currently, most cultural safety education literature falls into three broad categories: qualitative explorations of student learning experiences [ 18 , 22 , 30 , 54 , 55 , 56 , 57 , 58 ], evaluations of student learning outcomes [ 17 , 19 , 23 , 26 , 29 , 32 , 33 , 50 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 ], and descriptions of curricula development and delivery [ 16 , 20 , 21 , 25 , 28 , 31 , 38 , 67 , 68 , 69 , 70 , 71 , 72 , 73 ]. In evaluations of curricula and learning outcomes, student reflective journals are a common source of data. However, these articles tend to focus on whether and how the curricula have produced transformative learning, with little information provided on the specific pedagogical approaches used to teach students reflexivity, nor how assessments are structured to capture the reflexive process.
The dearth of literature on teaching and assessment of reflexivity may be reflective of the diversity of definitions, conceptualisations, and ways of operationalising it as a concept. Lumsden [ 39 ] warns against using standardised instructions for learning how to engage in reflexivity, as this implies a ‘correct’ and ‘incorrect’ way of going about the process, and risks reducing it to a checklist approach. In the absence of such instruction, how do educators help students develop the skill of reflexivity? Further, in the tertiary education system, where educators are required to assess the learning outcomes of students in a standardised manner, how do they assess whether students have effectively demonstrated these skills? The current research aims to address these questions through a systematic synthesis and exploration of the Indigenous cultural safety literature, with a specific focus on reflexivity, and aims to address the following questions:
- How is reflexivity conceptualised within cultural safety educational interventions?
- Where and how is reflexivity included as part of learning outcomes in educational interventions?
- What types of pedagogical approaches are used in cultural safety educational interventions to help students develop reflexive skills?
- How is the development of reflexivity as a skill assessed?
2. Materials and Methods
2.1. data sources and search strategies.
An initial systematic search of the following databases was conducted: CINAHL, PubMed, Scopus, Informit, PsycINFO, and Embase. Consultation with a research librarian determined that, due to the specificity of the search parameters and the limitations this placed on using indexing terms, a simplified set of search terms was most appropriate. Therefore, all searches across the databases used the following search terms: “cultural safety” and “culturally safe”. Where the databases provided the option, searches were limited geographically to Australia, Aotearoa New Zealand, Canada, and the United States of America, and to articles in English.
Additionally, a targeted internet search was also conducted, specifically to capture data produced by Indigenous and other non-government organisations (NGOs) as well as any available information on CPE. These data sources represent an important but often overlooked source of information not captured in other literature reviews, as they are often direct accounts of the educational process and often centre Indigenous experiences, knowledges, and aspirations.
2.2. Eligibility Criteria
Data sources were included if they described an educational programme or intervention that fitted the following inclusion criteria: (1) aimed to develop culturally safe learners; (2) was delivered as either part of an undergraduate or postgraduate degree or as continuing professional education (CPE); (3) had a focus on Indigenous health outcomes; and (4) was delivered in Australia, Aotearoa New Zealand, Canada, or the United States of America. The latter criteria were employed as these countries share similar historical and ongoing colonial processes, with resulting similarities in health inequities experienced by Indigenous peoples. The inclusion criteria were designed to allow for the inclusion of all cultural safety education literature and the identification of variations in how and where reflexivity was included or excluded.
Data sources were excluded if they were published in a language other than English, described an educational approach other than cultural safety, or a full-text article was not available.
2.3. Article Review
The initial search of the databases returned a total of 2860 results, which were exported into Endnote [ 74 ]. Duplicates were removed ( n = 1125), leaving 1735 results. Initial screening of titles was carried out by the lead author (JD), and identified a further 852 for removal, due to either irrelevance (for example, most of those excluded discussed a “culture of safety” rather than cultural safety), or duplicates missed by the Endnote sorting function.
Titles and abstracts of the remaining articles ( n = 883) were reviewed by JD and CH according to the inclusion/exclusion criteria; 738 articles were excluded, leaving 145 articles for full-text review. Full-text review resulted in the identification of another two articles, bringing the total number of articles reviewed to 147. JD conducted all full-text reviews, with a 10% cross-check provided by CH. Where agreement could not be reached on an article, it was discussed with AR until a decision could be made. An additional 29 articles were identified in the grey literature. An updated search conducted in 2021 identified an additional 17 articles for inclusion.
It should be noted that the targeted internet search identified a wide range of cultural safety training modules available via organisational websites, such as Australian Indigenous Doctors’ Association (Australia) and San’yas (Canada). Most of these organisational websites contained publicly available information about the expected learning outcomes of the training module but were excluded from analysis due to insufficient information on other aspects of learning.
2.4. Data Extraction
Data in the current research are descriptive and primarily sourced from the introduction and background sections of articles where information about the educational intervention is provided as a preface to evaluation or measurement of student learning and outcomes. Data were analysed using a two-stage thematic analysis process. In the first stage, data were coded under four major themes drawn from the research questions: definition and conceptualisation of reflexivity; where and how reflexivity is included in learning outcomes; pedagogical approaches used to develop reflexivity; and assessment methods used to measure reflexivity development. The second stage of analysis used inductive thematic analysis, where learning is generated from the data itself rather than guided by existing theoretical frameworks [ 75 ]. Data in each of the major themes were iteratively analysed and coded according to the sub-themes that emerged.
Additionally, discursive analysis [ 75 ] was used to provide a more nuanced understanding of how language practices shape the definition, conceptualisation, and practice of reflexivity within cultural safety education. Analysis of how reflexivity is defined drew on constructivist theory [ 76 ] to examine how language shapes our understanding of both the nature and purpose of reflexivity. Analysis of how reflexivity is conceptualised primarily drew on existing cultural safety and reflexivity literature (for example, [ 13 , 38 , 39 , 43 ]), and analysis of the pedagogical approaches drew on the object-based learning literature [ 77 , 78 ]. Throughout the analysis, we also drew on the work of Indigenous educators who operate at the cultural interface [ 79 ] and whose writings and approach to teaching are informed by Indigenous ways of knowing, being, and doing [ 53 , 55 , 80 , 81 ].
Data and analysis were managed using NVivo12 software [ 82 ].
3.1. Summary of Educational Interventions
A total of 46 documents were analysed, describing 43 different educational interventions. The majority ( n = 35) of documents described university-based educational interventions [ 16 , 18 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 38 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 62 , 63 , 64 , 66 , 68 , 69 , 70 , 73 , 80 , 81 , 83 , 84 ], with one set of documents describing a short vocational training course [ 85 , 86 , 87 ], and the remainder ( n = 8) describing continuing professional education (CPE) courses for practicing health professionals [ 17 , 19 , 20 , 36 , 69 , 73 , 88 , 89 ]. Just over half of the documents analysed ( n = 28) were from Australia [ 17 , 18 , 20 , 22 , 23 , 24 , 27 , 28 , 29 , 30 , 33 , 36 , 38 , 54 , 55 , 56 , 57 , 62 , 64 , 66 , 67 , 73 , 81 , 84 , 85 , 86 , 87 , 90 ], with the rest from Aotearoa New Zealand ( n = 5) [ 25 , 61 , 71 , 72 , 89 ], and Canada ( n = 13) [ 16 , 19 , 21 , 26 , 31 , 32 , 59 , 60 , 64 , 70 , 73 , 85 , 86 ]; there were no documents from the United States. Table 1 provides a summary of key characteristics of the documents included for analysis.
Summary of key characteristics of the educational interventions included.
| Reference Country | Learner Level and Field of Study | Site and Type of Educational Intervention | Duration. Delivery Method | Level of Indigenous Involvement |
|---|---|---|---|---|
| Arnold et al. (2008) [ ] Canada | Undergraduate nursing students. | University. Reciprocal partnership, including community placements. | Not specified. Face-to-face. | Initiated, co-designed, and co-delivered. |
| Bernhardt et al. (2011) [ ] Canada | Undergraduate speech-language pathology and audiology students. | University. Unit of study, including community placement. | 8-month teaching period. 26 h in-class teaching time. 26 h out of class time. Face-to-face with some online components. | Advisory Group established. Co-designed and co-delivered. |
| Bolton and Andrews (2018) [ ] Australia | Doctor of physiotherapy students. | University. Field trip within a unit of study. | Not specified. Face-to-face. | Co-designed and co-delivered. |
| Carriage et al. (2017) [ ] Australia | Fifth-year medical students. | University. Rural and remote placements. | Half-day lecture followed by 5-week placement. Face-to-face. | Aboriginal Medical Service host organisations, including cultural mentoring. |
| Chiodo et al. (2014) [ ] Australia | Undergraduate psychology students. | University. Unit of study. | 6-week teaching period. 2 h weekly lectures. 1 h weekly tutorials. Face-to-face. | Includes a ‘diverse teaching group’ and involvement of ‘Indigenous guest speakers.’ |
| Crampton et al. (2003) [ ] Aotearoa New Zealand | Third-year medical students. | University. Cultural immersion placement. | 1 week Face-to-face. | Consultation and collaboration with local community. |
| Delbridge et al. (2021) [ ] Australia | Undergraduate and postgraduate health professions students. | University. 2 discipline specific PBL modules. 1 inter-professional simulation session. | PBL modules: Pre-workshop online learning, 1 h seminar, and 3 h workshop. Simulation: Pre-session online learning, length of session not specified. Face-to-face with some online components | Co-designed involving expert knowledge holders. |
| Demers et al. (2021) [ ] Canada | Undergraduate occupational therapy students. | University. Fieldwork placement. | Pre-placement self-paced learning. 8-week placement. Face-to-face with some online components. | Partnership was initiated by a community-based Indigenous OT. |
| Dowell et al. (2001) [ ] Aotearoa New Zealand | Third-year medical students. | University. Cultural immersion placement; part of a unit of study. | 1 week Face-to-face. | Consultation and collaboration with local community. |
| Durey et al. (2017) [ ] Australia | Health professionals (radiation oncology). | CPE. Workshop. | 2 h workshop. Face-to-face. | Co-presentation. |
| Duthie et al. (2013) [ ] Australia | Master of social work students. | University. Field experience; part of a unit of study. | 1 day. Face-to-face. | Co-designed and co-delivered. |
| Fleming et al. (2017) [ ] Australia | Midwifery academic educators. | CPE. Workshops and yarning circles. | 2 half-day workshops and 5 yarning circles; held over a 12-week semester. Face-to-face. | Co-designed and co-delivered. |
| Gray et al. (2020) [ ] Australia | Undergraduate allied health students. | University. Workshop. | 1 day. Face-to-face. | Co-designed and co-delivered. |
| Hardcastle and Bradford (2007) [ ] Australia | Nurses and other health professionals. | CPE. Online module. | 6 self-paced learning modules. Online (web-based training programme). | Initiated, co-designed, and co-delivered. |
| Hart et al. (2015) [ ] Australia | Undergraduate nursing students. | University. Pre-placement unit. Placement (urban, rural, and remote locations). | Pre-placement semester unit of study. Placement (5 weeks). Face-to-face. | Collaboration and consultation with Aboriginal Medical Services to set up placements. |
| Herzog (2017) [ ] Canada | Fourth-year medical students. | University. Elective unit of study. | 4 weeks. Face-to-face. | Development and delivery of learning. |
| Herzog et al. (2021) [ ] Canada | Second-year medical students. | University. Class activity. | Not specified. Face-to-face | Not specified. |
| Hudson and Maar (2014) [ ] Canada | First-year medical students. | University. Pre-placement preparation. Placement in community. | 4 weeks (total) 2-week placement in Aboriginal community. 2-week follow-up on campus. Face-to-face with some online components. | Co-designed, co-delivered, and co-evaluation. |
| Hulko et al. (2021) [ ] Canada | Health professionals (nurses working with dementia patients). | CPE. Module. | Self-paced, equivalent to 8–10 h completed over 8 weeks. Online and face-to-face components. | Co-designed and co-delivered. |
| Jackson et al. (2013) [ ] Australia | Masters-level postgraduate health professions students. | University. Workshop within a compulsory subject. | 1 day; 7 discrete sessions. Face-to-face. | Co-designed and co-delivered. |
| Jamieson et al. (2017) [ ] Canada | First-year occupational therapy students. | University. Modules included in a first year OT course. | 3 × 1 h modules. Face-to-face. | Co-designed and co-delivered. |
| Joyce (1996) [ ] Aotearoa New Zealand | Undergraduate nursing students. | University. Scaffolded and integrated curriculum across undergraduate programme. | 3-year curriculum. Approximately 252 h total across 3600 h of teaching. Face-to-face. | Co-delivery of teaching. |
| Kelly et al. (2016) [ ] Australia | Renal health training for new and current nursing staff. | CPE. Workshop (pilot and evaluation). | Aim is to offer a 1-day workshop. Face-to-face. | Not specified. |
| Kickett et al. (2014) [ ] Australia | First-year health sciences students. | University. Integrated curricula. | 12-week semester. 2 h weekly tutorials. Offered in two formats: fully online; and face-to-face with some online components. | Co-coordination. Delivery of teaching. |
| Lucas et al. (2021) [ ] Australia | Master of pharmacy students. | University. Immersive workshop. | 8 h. Face-to-face. | Co-designed and co-delivered. |
| Maar et al. (2020) [ ] Canada | Pre-clerkship medical students. | University. Simulated clinical scenarios. | 15-min interview and 20-min debrief interview. Face-to-face. | Co-designed and co-delivered. |
| Mahara et al. (2011) [ ] Canada | Baccalaureate nursing students. | University. Proposed curriculum. Scaffolded and integrated curriculum across the programme; includes a community placement. | 4-year curriculum. Total amount of time not specified. Proposed activities would be face-to-face. | Conceptualisation, planning, and development. |
| McCartan et al. (2021) [ ] Australia | First-year nutrition science students. | University. Integrated curriculum across first year. | Integrated across 4 semester-long first-year subjects. Face-to-face. | Co-designed. |
| Mills et al. (2022) [ ] Australia | Undergraduate health sciences students. | University. Semester-long unit of study. | Four 3 h workshops across a 12-week unit. 1 face-to-face workshop; 3 online workshops (due to COVID-19). | Co-designed and co-delivered. |
| Min et al. (2020) [ ] Canada | Third- and fourth-year pharmacy students. | University. One-semester unit of study; includes experiential learning activities. | 3 h per week; 36 h total. Face-to-face. | Co-designed and co-delivered. |
| Nash et al. (2006) [ ] Australia | Undergraduate nursing students. | University. Scaffolded and integrated curricula across the programme of study. | Seven units across the programme had content embedded; five were practical placements. Face-to-face with online components. | Consultation and collaboration in the development. |
| NSW Government Family and Community Services (2007) [ , , ] Australia | Not specified. | Vocational training. Units of study within a Certificate III in Aged Care. | 5-day workshop. Face-to-face. | Contributed to resource development. Required as assessor(s). |
| Oosman et al. (2019) [ ] Canada | Master of physical therapy students. | University. Pre-placement orientation session. Placement in community. | Varied length, 2–4-week placements. 2 days per week in a health facility, 3 days per week in community. Face-to-face. | Design and delivery of community practicum. |
| Paul et al. (2019) [ ] Australia | Medical students, first to fourth year. | University. Vertically and horizontally integrated curriculum. | Activities included in the curriculum vary between 1 h (smoking ceremony and welcome to country) and 8-weeks (rural GP and psychiatry rotation). Face-to-face. | Aboriginal health team responsible for coordination, development, implementation, and evaluation. |
| Power et al. (2020) [ ] Australia | Third-year nursing students. | University. Elective clinical placement. | Not specified. Face-to-face. | Written and facilitated. |
| Ramsden (1992) [ ] Aotearoa New Zealand | Undergraduate nursing and midwifery students. | University. Proposed curriculum framework. | Not specified, but curricula to be scaffolded and embedded throughout the programmes. Not specified. | Conceptualisation of framework. |
| Richardson et al. (2017) [ ] Canada | Child and youth mental health workers. | CPE. Short course. | 5-day training programme. Face-to-face. | Co-designed and co-delivered. |
| Royal Australian College of General Practitioners (2011) [ ] Australia | Medical practitioners. | CPE. Framework for delivery; to be developed and delivered on a case-by-case basis by accredited trainers. | Minimum 6 h, up to 10 h of structured learning. Must also include preparatory activities. Mandatory 6 h face-to-face; can also include online components. | Planning, delivery, and evaluation of the programme. |
| Ryder et al. (2013) [ ] Australia | Second- and third-year medical students. | University. Structured clinical simulations. | 3 h session. Face-to-face. | Co-designed and co-delivered. |
| Sjoberg and McDermott (2016) [ ] Australia | Health professions students (undergraduate and postgraduate). | University. Assessment included within a semester-long unit of study. | Not specified. Face-to-face. | Development. |
| Thackrah and Thomson (2013) [ ] Australia | First-year midwifery students. | University. Semester-long unit of study. | 12-week semester. 2 contact hours per week. Face-to-face. | Co-designed and co-delivered. |
| The Royal New Zealand College of General Practitioners (n.d.) [ ] Aotearoa New Zealand | Practicing general practitioners. | CPE. Online training module. | Self-paced training module. Online. | Development and presentation. |
| Thorpe and Burgess (2012) [ ] Australia | Undergraduate preservice teachers. | University. Semester-long unit of study. | 12-week semester. Weekly contact time not specified. Face-to-face. | Co-designed and co-delivered. |
| West et al. (2021) [ ] Australia | Final year undergraduate podiatry students. | University. Immersive clinical placement. | Minimum of four 1-day placements over the final year of study. Face-to-face | Clinic is staffed by Aboriginal health professionals. |
3.2. Definitions of Cultural Safety
While an exploration of cultural safety definitions was not a central aim of this study, it was notable that several definitions included did not contain any reference to reflexivity or similar processes, such as critical reflection or self-awareness. Six of the documents included for analysis made no reference to reflexivity or similar in either the definition of cultural safety or in the educational intervention [ 19 , 24 , 27 , 28 , 73 , 88 ]. One of these documents referred to practicing cultural safety skills learned in a previous topic via structured simulation workshops [ 28 ], but the cultural safety skills are not outlined so it is unclear whether this includes reflexivity. An additional eight documents included in the analysis did not include reflexivity in the definition or conceptualisation of cultural safety but did include reflexivity as part of the educational intervention described [ 23 , 32 , 33 , 56 , 57 , 64 , 67 , 68 ].
3.3. Definition of Reflexivity
Inductive thematic analysis of the data found a lack of consistency in the terminology used to name and describe the reflexive process within cultural safety educational interventions. Of the 46 documents analysed, 40 described some form of reflexive process. Ten documents specifically referred to a process of ‘reflexivity’, either as part of the cultural safety definition [ 17 , 18 , 25 , 26 , 29 , 30 , 31 , 84 ] or as part of the educational intervention [ 23 , 38 ]. The remaining 30 documents used variations of the following terms: (self) awareness [ 20 , 54 , 57 , 58 , 59 , 63 , 64 , 69 , 80 , 91 ]; (critical and/or self) reflection [ 21 , 22 , 32 , 33 , 36 , 55 , 56 , 57 , 58 , 63 , 64 , 66 , 67 , 68 , 73 , 80 , 81 , 83 , 84 , 85 , 86 , 87 , 91 ]; (self) examination [ 16 , 61 , 65 , 71 , 72 , 75 ]. None of the documents analysed used the term reflexivity as a standalone concept; the ten documents that used the term reflexivity did so interchangeably with the other terms listed above.
Where documents described the process of reflexivity, a variety of terms was used. The most common descriptors included ‘reflect on’ [ 21 , 22 , 23 , 27 , 30 , 31 , 32 , 33 , 36 , 56 , 64 , 66 , 67 , 68 , 73 , 80 , 90 ]; ‘examine’ [ 16 , 17 , 25 , 61 , 71 , 72 ]; ‘become aware of’ [ 17 , 18 , 36 , 63 , 68 , 75 , 88 ]; ‘explore’ [ 17 , 18 , 36 , 63 , 68 , 75 , 88 ]; ‘consider’ [ 29 , 56 , 67 , 68 ]; ‘understanding’ [ 36 , 58 , 87 ]; and ‘identify’ [ 21 , 64 , 67 , 72 , 89 ]. What is notable about these descriptors is that most—including all the most commonly used—describe a passive process of identification, observation, and awareness. In contrast, some descriptors contain a call to action, for example, the requirement to use this new knowledge and understanding of self to enact attitude change [ 23 , 36 , 56 , 71 , 72 ], and to contest and deconstruct previous understandings [ 29 , 73 ].
3.4. Conceptualisations of Reflexivity
Four sub-themes emerged relating to how the purpose and focus of reflexivity was conceptualised. These sub-themes included self-identity; held beliefs; relationality; and context, with each sub-theme encompassing a suite of factors that learners were expected to reflect on. These factors are outlined in Table 2 , below, although it should be noted that conceptualisations of reflexivity varied considerably across the data and inclusion of a sub-theme did not guarantee inclusion of all factors. All documents included for analysis conceptualised reflexivity using at least one sub-theme, but usually two or more sub-themes were present.
How the purpose and focus of reflexivity is conceptualised: sub-themes identified in the data.
| Self-Identity | Held Beliefs | Relationality | Context |
|---|---|---|---|
| Identity Culture and ethnicity Worldview Values | Assumptions Biases and stereotypes Internalised racism Power and privilege | Impact of self-identity and held beliefs on relationships with others | Impact of context on self-identity, held beliefs, and relationality |
3.4.1. Sub-Theme 1: Self-Identity
The sub-theme of self-identity was primarily concerned with students reflecting on their own identity, culture, worldviews, and values, and was seen in 30 of the documents analysed [ 16 , 17 , 18 , 20 , 21 , 22 , 23 , 26 , 28 , 29 , 30 , 31 , 32 , 33 , 36 , 57 , 58 , 59 , 60 , 62 , 63 , 64 , 66 , 67 , 69 , 70 , 71 , 73 , 83 , 87 ]. The primary purpose of reflecting on self-identity was broadly described as developing an understanding that identity, culture, worldviews, and values are not universal, exemplified in the following extracts:
“Participants were therefore encouraged to…explore their own culture, values, and beliefs [and] acknowledge difference” [ 17 ] (p. 248)
“[Cultural safety] requires registered nurses to reflect on their own cultural identity and practice in a way that affirms the culture of clients and co-workers” [ 21 ] (p. 3)
Further, learners were required to develop an understanding that their own self-identity shapes and influences understanding, attitudes, and behaviours, as demonstrated in the following extracts:
“This includes understanding your own worldview and how your values and beliefs influence the way you perceive other people” [ 57 ] (p. 88)
“[Students will] reflect on their own cultural background and their life experiences including the development of values and attitudes that have shaped their thinking and behaviours” [ 23 ] (p. 120)
3.4.2. Sub-Theme 2: Held Beliefs
Thirty-five of the documents analysed described the sub-theme of held beliefs, where learners were required to identify and articulate their current knowledge, attitudes, biases, power, and privilege specifically in relation to Indigenous peoples [ 16 , 17 , 19 , 20 , 21 , 22 , 23 , 25 , 26 , 29 , 30 , 31 , 33 , 36 , 38 , 54 , 55 , 57 , 58 , 59 , 60 , 62 , 63 , 64 , 66 , 67 , 69 , 70 , 73 , 80 , 81 , 83 , 87 , 90 , 91 ]. In most of these educational interventions, learners were required to reflect on both self-identity and held beliefs, and these were conceptualised as related. However, eight of the educational interventions only included a requirement to identify, reflect on, and in some cases actively critique held beliefs [ 19 , 25 , 55 , 56 , 68 , 86 , 88 , 89 ].
A closer examination of the language used to describe the sub-theme of held beliefs found that the process and focus of reflexivity was often couched in neutral terms that glossed over the inherent racism underpinning beliefs and attitudes, as seen in the following extracts:
“…highlighted the importance of health providers reflecting on and questioning their own assumptions about Aboriginal people that can impact on the care they provide”. [ 90 ] (p. 3, emphasis added)
“…learners were encouraged to reflect on their own cultural values or emotional responses to diverse histories, cultures, worldviews, values, and contemporary events related to Indigenous people” [ 32 ] (p. e2, emphasis added)
Notably, across the educational interventions, there was minimal expectation that learners would reflect on their future or current professional culture, and the norms, beliefs, and values that would inform their practice. Three exceptions to this are Demers et al. [ 31 ], Kelly et al. [ 20 ], and Ramsden [ 70 ]. Demers et al., note that cultural safety “requires exploration of cultures and identities, on both a personal and professional level” [ 31 ] (p. 184). Similarly, Kelly et al., argue that culturally safe nurses are “aware of their own culture and that of the hospital” [ 20 ] (p. 110), and Ramsden states that nurses and midwives must become aware of “the cultural boundaries which surround [the] traditional nursing and midwifery role” [ 70 ] (p. 23).
3.4.3. Sub-Theme 3: Relationality
Half of the educational interventions ( n = 23) described the sub-theme of relationality [ 16 , 17 , 18 , 20 , 21 , 22 , 25 , 29 , 31 , 36 , 54 , 57 , 58 , 59 , 60 , 64 , 66 , 67 , 69 , 70 , 73 , 87 , 91 ]. In this sub-theme, learners were required to reflect on how self-identity and held beliefs impact on engagement with and care for others, and how this contributes to poor health and social outcomes, as exemplified by the following extracts:
“…students reflected on their own place-based identity (i.e., who they were, where they came from) and recognized how their own personal biases were unintentionally but significantly brought into practice and how those biases influenced their work and social interactions” [ 31 ] (p. 187)
“…notice our own cultural practices and individual behaviours and the impact these may have on Aboriginal and Torres Strait Islander people” [ 87 ] (p. 23)
3.4.4. Sub-Theme 4: Context
The fourth sub-theme identified in the data was context and was included in 10 of the educational interventions analysed [ 16 , 22 , 23 , 29 , 31 , 55 , 59 , 60 , 67 , 75 ]. Context was described as a process of reflecting on how self-identity, held beliefs, and relationality have been shaped by historical, social, political, and economic forces. Like relationality, reflection on context takes the process of reflexivity beyond introspection and allows a more critical analysis of the self as socially located. In some cases, this was a passive analysis, as in the following extract:
“Become aware of their own social conditioning, their (often privileged) status, and how their conditioning and status can affect their interactions with clients” [ 59 ] (p.179)
In contrast, other conceptualisations of reflexivity recognised the opportunity to actively challenge and deconstruct [ 29 ] this social conditioning, a process that Sjoberg and McDermott refer to as “disassembling planks of belief” [ 73 ] (p. 30).
All educational interventions included content on contextual factors such as colonisation, racism, and sociopolitical processes, and their impact on the health and wellbeing of Indigenous peoples. It is notable that while there is ubiquitous recognition of how colonialism and racism have impacted on Indigenous health and well-being, there is comparatively less recognition of how these factors have shaped non-Indigenous self-identity, held beliefs, and relationality.
The varying conceptualisations of reflexivity can be seen as existing on a spectrum, ranging from basic reflection on self-identity at one end, to more critical reflection on self-beliefs and relationality in the middle, and reflexive analysis of the self as contextually situated at the other end. This can be seen in Figure 1 , below:

Spectrum of reflexive practice.
3.5. Where and How Reflexivity Is Included as a Learning Outcome
None of the educational interventions included learning outcomes that explicitly required students to develop knowledge of or ability to engage in reflexivity. Instead, reflexivity was operationalised as a method for achieving other learning outcomes, such as developing awareness and knowledge of self-identity, held beliefs, relationality, and/or context. Of the documents included for analysis, only 15 explicitly stated the learning outcomes of the educational intervention, and of these, 10 included learning outcomes relating to reflexivity [ 17 , 29 , 54 , 55 , 56 , 59 , 64 , 70 , 85 , 91 ]. An example of this can be seen in the following extract, which outlines two of the learning aims of a one-day workshop for Australian postgraduate health sciences students:
Specific aims of the day were to facilitate students in: “Recognising and acknowledging their own views and frames of reference in relation to Indigenous Australians”; “Critically reflecting on the impact of ongoing colonisation and its pervasive discourse on the health and well-being of Indigenous Australians”. [ 55 ] (p. 106)
In most of the other documents included for analysis ( n = 31), expected learning outcomes could be inferred from the description of the educational intervention. For example, the extract below describes the intended learning outcomes of a community placement for master of physical therapy students in Canada:
“Our goal was to study whether expanding the clinic beyond the classroom and into a Métis community would make the students more aware of their own identity and worldviews, how they may be different from those in that community, and how they shape their stereotypes and misperceptions of peoples from other cultures”. [ 58 ] (p. 147)
The conceptualisation of reflexivity as an approach to learning can be traced back to Ramsden’s early work on cultural safety education. The learning objectives outlined by Ramsden specifically require students to “examine their own reality and…attitudes”, “be open minded and flexible in their attitudes toward people”, and to become “self-aware” [ 70 ] (p. 22), learning requirements that are reflected throughout the cultural safety education literature. While there were a range of pedagogical approaches used to facilitate reflexivity, there is no mention of whether students were explicitly taught about the concept and purpose of reflexivity, or how to go about being reflexive. It may be that some of the facilitated activities included instruction on the concept and process, but this is not outlined in any of the literature included for analysis.
3.6. Pedagogical Approaches to Facilitate Reflexivity
The analysis revealed that reflexivity was facilitated through a range of pedagogical approaches, all of which involved some type of reflexive catalyst [ 78 ]. These catalysts were used as a counterpoint to the learner’s own lived experiences and worldviews, with the intention that exposure to difference would result in some level of reflexivity. Pedagogical approaches can be seen as grouped into three broad categories, depending on the type of catalyst used: objects, people, and Indigenous pedagogical practices.
3.6.1. Objects
Object catalysts were described in 27 of the educational interventions analysed, and included things like readings, case studies, stories, visual art, and films [ 17 , 20 , 23 , 24 , 29 , 30 , 31 , 32 , 33 , 36 , 38 , 56 , 59 , 62 , 63 , 64 , 66 , 67 , 68 , 69 , 71 , 73 , 84 , 85 , 87 , 90 , 91 ]. Reflexive engagement with object catalysts was most often depicted as small or large group discussions, where new knowledge and understanding was co-produced through the sharing of beliefs, experiences, and interpretations. Examples of this can be seen in the following extracts:
“… the session includes a semi-formal lecture in a quieter space of the gallery … student literature reviews, gallery exploration, and a group reflective discussion”. [ 30 ] (p. 37)
“The tutorial format was tightly structured and included the viewing of a vodcast (prepared specifically for the unit and featuring Aboriginal speakers), discussion of issues arising, case studies, and periodic presentations by students. … Guidelines [were] developed by students [to facilitate classroom discussions, to ensure] that consideration be given to experiences and background that may influence attitudes expressed”. [ 23 ] (pp. 115–116)
3.6.2. People
Twenty-six educational interventions analysed included people as a reflexive catalyst [ 16 , 17 , 18 , 19 , 21 , 22 , 24 , 25 , 26 , 27 , 28 , 31 , 36 , 38 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 62 , 63 , 69 , 80 , 81 , 83 , 84 ]. Immersive, community-based placements or field trips were the most common ( n = 16), where predominantly non-Indigenous students visited (and sometimes stayed in) Indigenous communities or health services [ 16 , 18 , 22 , 24 , 25 , 26 , 27 , 31 , 54 , 57 , 58 , 59 , 60 , 63 , 81 , 83 ]. The educational interventions that took this approach shared similar theoretical underpinnings, where exposure to difference was described as an opportunity for reflection and growth. The extract below is exemplary of this theory:
“Cultural immersion is an experiential approach to learning about culture and social situations. In medical education this type of approach is beginning to be recognized for its potential to raise consciousness among students; expose tacit inappropriate biases, including racism; help students learn about themselves and other cultures; and assist students in their preparation for work in culturally diverse settings”. [ 26 ] (p. 3)
In 13 of the educational interventions analysed, Indigenous educators were positioned as the reflexive catalysts, either as core teaching staff [ 17 , 36 , 56 , 57 , 68 , 71 , 90 ] or in ad hoc roles such as guest speakers [ 19 , 21 , 60 , 64 ] or patient simulation actors [ 28 , 63 , 86 ]. Indigenous educators were frequently described as providing learners with an opportunity to challenge their own stereotypes and beliefs about Indigenous peoples, as exemplified in the following extract:
“Having the opportunity to be taught by and interact with an Indigenous academic is thought to have a major role in reducing stereotypes and negative attitudes about Indigenous Australians … Our objective was to present an Indigenous informed perspective filling in the gaps of knowledge that have resulted from silencing Indigenous peoples, their stories and experiences. We wanted to provide students with some positive and affirming images of the strength and resilience of Australian Indigenous peoples”. [ 55 ] (pp. 105–107)
Simulated patient scenarios involving Indigenous people as ‘patients’ were all described as an opportunity for learners to practice and refine communication skills and develop their cultural safety skills. This was seen as providing a safe, controlled environment for both learners and ‘patients’ where feedback could be provided to facilitate learner reflection [ 28 , 63 , 86 ].
3.6.3. Indigenous Pedagogical Practices
Eighteen of the educational interventions analysed described the inclusion of Indigenous pedagogies as a method of facilitating learner reflexivity [ 16 , 17 , 18 , 19 , 27 , 30 , 32 , 38 , 54 , 56 , 60 , 64 , 68 , 71 , 73 , 81 , 83 , 84 ]. In some educational interventions this was an integral aspect of immersive community placements, where learners engaged in a variety of cultural and community events [ 16 , 18 , 27 , 55 , 61 , 85 ]. In other educational interventions, this was described as a process of engaging with Indigenous ways of knowing, being, and doing through activities such as talking (or yarning) circles [ 17 , 57 , 70 , 73 ], storytelling [ 19 , 30 , 32 , 68 , 90 ], and ‘Indigenised spaces’ [ 30 , 65 , 87 ]. In these educational interventions, Indigenous pedagogies were described as providing a counterpoint to deficit-based understandings that may be held by learners, or to legitimate Indigenous knowledges, as demonstrated in the following extracts:
“field experiences can provide students with a first-hand account of the ‘ways of knowing, being, and doing’ …that is, communicating with and listening to Aboriginal Elders, practitioners and community members provides a deeper analysis of social work practice through assessing the cultural context, yarning and storying” [ 54 ] (p. 199)
“A yarning circle approach was used to privilege First Peoples’ culture and voice. First Peoples have recognised yarning as a method of sharing stories, information and knowledge for generations”. [ 17 ] (pp. 247–248)
3.7. Assessment of Reflexivity
Of the 46 educational interventions analysed, only 22 provided information on the assessment of reflexivity, and in most instances only a brief description of the assessment task(s) was provided [ 18 , 22 , 23 , 24 , 26 , 27 , 29 , 33 , 38 , 54 , 55 , 56 , 58 , 59 , 63 , 66 , 69 , 73 , 81 , 84 , 85 , 91 ]. The most common forms of assessment were written reflections in the form of journals [ 23 , 24 , 29 , 57 , 60 , 87 ], essays [ 22 , 59 , 67 , 68 , 75 ], and portfolios [ 26 , 27 , 33 ]. Other forms of assessment included structured reflective questions [ 54 , 85 ], oral presentations [ 18 ], and arts-based reflection activities [ 59 , 63 ].
A common theme throughout assessments is the requirement for students to reflect on their learning, and how this applies to them personally and professionally, as demonstrated by the following extracts:
“Students subsequently submitted a critical self-reflection exploring their personal learnings, including reflections on assumptions, discomfort and realisations” . [ 38 ] (p. 6)
“The idea that students would be given a ‘real world’ experience, be required to reflect on what they had observed and what they had learnt, with supporting literature, was vital to identifying elements of changing attitudes and effectiveness of learning. Furthermore, students then had to plan how they would use their new knowledge in future practice contexts”. [ 54 ] (p. 201)
The above extracts demonstrate the two different ways that learners were required to reflect on their learning. In the first extract [ 38 ], the purpose of the assessment is described as assessing what students have learned about themselves, demonstrating an inward focus on self-identity and held beliefs. In the second extract [ 54 ], assessment is described as having a more applied focus; students must reflect on what they have learned and consider the implications for practice.
Two documents included for analysis focused specifically on the assessment of reflexivity in their respective educational interventions, with descriptions of how these assessments connect to learning outcomes and are supported via learning activities. Sjoberg and McDermott [ 73 ] discuss what they call the ‘deconstruction exercise’, where students are required to critically examine and ‘deconstruct’ their chosen question rather than answer it directly. The aim is to expose the racialised assumptions and stereotypes that inform the question and how this links to broader social, historical, and political contexts. By externalising this critique, Sjoberg and McDermott argue that the deconstruction exercise provides learners with an “opportunity to reflect on the everyday language in which they may be immersed, to see behind the dominant Australian lexicon to the colonial, discursive position from which it has been constructed” [ 73 ] (p. 31).
Power et al. [ 22 ] describe a reflective essay assignment in which students were required to complete three online reflections before, during, and after their 3-week placement. Students were provided with ‘trigger questions’ to prompt their online reflections, and these reflections formed the basis of their submitted reflective essay. The trigger questions step students through the reflective process, prompting them to think about their current knowledge and expectations (pre-placement), new learnings about themselves (mid-placement), and how this applies to future practice (post-placement).
What is notable about the educational interventions described by Sjoberg and McDermott [ 73 ] and Power et al. [ 22 ] is that learners are supported to complete these assessments in several ways, including clear links made to topic content, scaffolded activities to support reflexive skill development, and prompting questions to guide the reflexive process. Several other educational interventions described similar approaches to support learner reflexivity, although only limited information was provided. For example, Chiodo et al. note that learners were required to keep a reflective journal in which they “reflect upon the topics covered in class and in the set reading material … to think about what the issues/concepts/theories…meant for them both in their personal and professional lives” [ 29 ] (p. 184). Here, assessment requirements are clearly tied to learning content and instructions regarding the focus of reflexivity; this was described in eight documents analysed [ 22 , 26 , 29 , 55 , 64 , 67 , 68 , 75 ].
4. Discussion
The current study analysed a total of 46 documents, which described 43 different educational interventions. Definitions and conceptualisations of reflexivity varied; in many definitions, reflexivity was conceptualised as a passive process of observation rather than an active process of analysis, critique, and change. Four sub-themes were identified: self-identity, held beliefs, relationality, and context, with conceptualisations of reflexivity drawing on varying combinations of these sub-themes.
In all educational interventions analysed, reflexivity was considered an approach to learning rather than a learning outcome itself. Only 15 of the documents included for analysis specifically outlined syllabus learning outcomes, so it is possible that the other educational interventions include learning outcomes related to the development of reflexivity as a skill. Pedagogical approaches relied on three types of reflexive catalysts: objects, people, and Indigenous pedagogies. The use of reflexive catalysts was premised on the assumption that exposure to difference would engender understanding and respect for perspectives, beliefs, and experiences different to those of the learners. There was limited information available on the assessment of reflexivity, although most assessments focused on new knowledges and understandings gained through the educational intervention, including knowledge of self, and how these apply to students’ personal and professional lives.
It is noteworthy that 14 of the documents analysed included a definition of cultural safety that did not include reflexivity as a core aspect of culturally safe practice, with eight of those documents positioning reflexivity as additional to cultural safety, and six documents making no reference to reflexivity at all. Definitions that lack reference to reflexivity tend to align more with cultural competency models, which emphasises learning about other cultures and has been criticised as taking a more tick-box approach that risks essentialising culture and reinforcing stereotypes [ 13 , 45 ]. Cultural safety specifically moves away from this model of learning, with the emphasis placed on students learning about themselves and their own culture, and how power imbalances impact healthcare provision. Notably, there were several documents included in the analysis that used the terms ‘cultural safety’, ‘cultural awareness’, and ‘cultural competency’ interchangeably (for example, [ 21 , 23 ]) or conceptualised them as aspects or stages of the same process (for example, [ 17 , 36 , 86 ]). This potentially highlights a lack of understanding of core cultural safety concepts, and arguably, results in less effective teaching.
Variations in how cultural safety is conceptualised may provide some explanation for the variations in how reflexivity was defined and conceptualised. As noted by Lumsden [ 39 ], definitions of reflexivity differ according to context and purpose. The analysis showed that where the purpose of the educational intervention was to increase recognition and respect for diversity, reflexivity tended to be conceptualised as a process of understanding self-identity, held beliefs, and in some cases, relationality [ 16 , 17 , 18 , 19 , 20 , 22 , 23 , 25 , 26 , 28 , 29 , 30 , 31 , 32 , 33 , 36 , 38 , 54 , 55 , 57 , 58 , 59 , 60 , 62 , 63 , 64 , 66 , 67 , 69 , 70 , 73 , 80 , 81 , 83 , 87 , 90 , 91 ]. Where educational interventions were conceptualised as a way to address colonialism, privilege, and power imbalances, reflexivity was defined as a process of identifying and critiquing self-beliefs and the structural, institutional, and discursive factors that contribute to them [ 16 , 22 , 23 , 29 , 31 , 55 , 59 , 60 , 67 , 75 ].
As outlined in Figure 1 , reflexivity could be conceptualised as existing on a spectrum. At one end, reflexivity was concerned with acknowledging and exploring self-identity and held beliefs, while at the other end, reflexivity was concerned with contextualising the self as socially located. Most of the documents analysed fell into the ‘basic’ or ‘critical’ reflection portions of the spectrum, with a greater focus on identification and understanding of self-identity and held beliefs, and to a lesser extent relationality. Expectations that students will identify and critique their self-identity and held beliefs would arguably be a contributing factor to student feelings of discomfort and resistance [ 48 , 49 , 50 ]. While discomfort is a necessary part of transformative learning, this discomfort needs to be carefully managed [ 49 , 50 , 54 ]. We would argue that a greater focus on the social, historical, political, and discursive forces which inform and shape students’ self-identity and held beliefs are an important part of the reflexive process. This would provide students the opportunity to understand that these are not immutable aspects of their own identity, but rather changeable aspects that have been shaped by problematic, inequitable, and racist systems [ 73 ]. If adequately managed, students may feel empowered to change problematic beliefs and attitudes while critiquing the systems that produced them.
All educational interventions analysed included information about the social determinants of health, so it is possible that learners were assisted to reflect on the connections between their own worldviews and broader contextual factors during learning. This is common throughout the cultural safety education literature, where learning about social determinants is positioned as a method for challenging and critiquing racialised beliefs, assumptions, and stereotypes that may negatively impact on care provision [ 20 , 33 , 42 , 43 , 56 , 57 , 68 , 71 , 72 ]. However, this was not evident from the available data, where discussion of the social determinants was explicitly described as developing an understanding of their impact on health outcomes for Indigenous peoples. Arguably this works to construct social processes as unidirectional, only impacting on Indigenous peoples’ health, without acknowledgement of how learners themselves are embedded within and shaped by these processes. This potentially limits the extent to which learners can engage in reflexivity, directing greater attention to self-identity and held beliefs and how they impact on behaviours and attitudes towards others.
The pedagogical methods used to facilitate reflexivity are also worth greater examination. More than half ( n = 26) of the documents analysed used people as the catalyst for reflexivity, where exposure to people with different cultures and life experiences provided learners with a counterpoint to their own culture, beliefs, assumptions, and stereotypes. Cultural immersion theory aligns with a pedagogy of discomfort [ 49 ], in that learners are taken out of their comfort zones and confronted with new knowledges and experiences that may challenge their preconceptions. What is notable here is that, while many of the immersion-based curricula were designed and delivered by Indigenous community members, there was little consideration given to the cultural safety of this experience for the community itself. In contrast, learner needs were paramount in discussions, with a range of strategies employed to manage student discomfort and create culturally safe learning experiences. For example, Gray et al. [ 62 ] describe an Indigenous health workshop for fourth-year allied health students, in which students interviewed local Aboriginal Elders and other community members to develop culturally safe communication skills. Gray et al., note that “this process provided a ‘safe space’ for students to interact with an Indigenous Australian person” [ 62 ] (p. 3). Arguably, however, there is at least as much risk for elders and other community members in the potential exposure to the racism, dismissive attitudes, and resistance to learning that often accompanies student feelings of discomfort [ 23 , 49 , 50 ]. Gray et al. indirectly acknowledge the potential for this to occur, noting that educators are taught how to de-escalate situations, and “post-workshop debrief sessions were held for teaching staff, to allow for the ‘venting’ of concerns” [ 62 ] (p. 3).
In other immersive-based curricula, efforts were made to ensure that reciprocity was an underpinning principle, where communities received as much benefit as students did. This is exemplified by Hudson and Maar, who note that their placement experience was informed by a social accountability model, where “the obligation of medical schools is to direct education, research and service activities towards addressing priority health concerns in the community” [ 26 ] (p. 2). While laudable, it does not explicitly address the potential risks for the community members hosting students; there is an expectation that the risk to educators and other community members is worth the educational gains for students. Only two educational interventions explicitly addressed the issue of safety for Indigenous educators and community members [ 55 , 80 ], acknowledging the potential for Indigenous people to be exposed to racism. The culturally unsafe nature of the classroom for Indigenous educators is well recognised (see for example, [ 53 , 80 , 81 ]) yet there are currently limited strategies put in place to address this risk. Most educational interventions analysed had some level of Indigenous involvement in development and/or delivery (see Table 1 ), yet on its own this does not guarantee the safety of Indigenous educators or community members. There is a need for more research to develop strategies that minimise the risk for Indigenous people working in this space [ 92 ].
Finally, the lack of information on the assessment of reflexivity within cultural safety curricula highlights a significant gap in the literature. Reflexivity is a fundamental aspect of being culturally safe; presumably, then, it is important to determine whether learners have developed the necessary reflexive skills to become culturally safe. Yet assessment is often glossed over in curricula descriptions, with only brief summaries provided of what is being assessed. In all instances where information on assessments was provided, learners were expected to demonstrate reflection on learning and how this applied to them personally and professionally. There were no examples that required students to explicitly demonstrate reflexive skills; in other words, assessment was of content rather than process. Arguably there are issues with this approach; as noted previously, focusing on what students have learned about themselves is potentially problematic and could be a causative factor in student feelings of discomfort, disengagement, and resistance [ 50 , 75 , 80 ]. Additionally, the potential for students to game their reflections also calls into question the efficacy of these types of assessments. A possible solution is to shift the focus of assessment from content to process, where learners’ ability to demonstrate reflexivity is assessed, although currently there is very little research to indicate what this might look like (for example, [ 93 ]), and none within cultural safety education. Arguably then, there is a need for more research to determine how best to assess reflexive skills within cultural safety education without reducing it to either a checklist approach or a navel-gazing exercise [ 40 ].
While the results of this study are specifically concerned with reflexivity in the context of Indigenous cultural safety, cultural safety is increasingly being adopted in other discipline and population contexts. In particular, there is growing interest in how cultural safety might improve care provision and health outcomes for marginalised and disadvantaged populations, for example the LGBTIQA+ community [ 88 , 89 ], racial and cultural minority groups [ 94 , 95 ], and Indigenous populations globally [ 96 ]. In an increasingly globalized and multicultural society, the importance of cultural safety and the ability to engage reflexively is fundamental to the provision of equitable, non-discriminatory care.
Limitations
A potential limitation of the current study is the type of literature that has been included. Most articles included in the analysis were evaluations of all or part of a cultural safety curriculum, with information on the learning outcomes, pedagogical approaches, and assessment options provided in the introduction or methodology sections. Articles were included where they provided sufficient information on at least three of the four key areas of analysis. The reliance on this type of data may explain the paucity of information on assessment approaches, as this was not a key feature of curriculum evaluations, where most of the focus was on changes in learner attitudes and knowledges, or learner experiences. However, the inclusion of this literature also means that a much broader picture of cultural safety education can be gleaned, compared to only including articles that focus on curriculum description.
Another possible limitation is that literature was only sourced from Australia, Aotearoa New Zealand, Canada, and the United States. It is possible that additional insights and perspectives might have been gained from other countries, broadening our current understanding of cultural safety curricula. Given the similarities in colonial history and Indigenous experiences of health and social inequity, it was felt that the cultural safety curricula literature would be comparable across these four countries, whereas this may not be the case for other countries.
5. Conclusions
While there is a substantial body of research exploring pedagogical approaches to teaching cultural safety in the context of Indigenous health, relatively little work has been done to determine best practice approaches to teaching and assessing reflexivity as a core cultural safety skill. Indeed, the above analysis demonstrates that even within the cultural safety education literature, there is substantial variation in whether and how reflexivity is included within definitions of cultural safety, and how reflexivity itself is conceptualised. This lack of conceptual clarity presents issues for educators when trying to develop cultural safety curricula and suggests that more work is required to develop a more cohesive model of reflexivity specifically aligned with the aims of cultural safety curricula and practice. Additionally, more thought must be given to the pedagogical and assessment approaches utilised within cultural safety education. A range of strategies were utilised during learning to manage student discomfort, yet almost no attention was given to how that discomfort might manifest in the context of assessments. Likewise, while there was a substantial focus on student safety within the educational interventions, relatively few educational interventions considered the cultural safety of Indigenous educators and community members involved in the development of delivery of these programmes. Further research is required to provide greater conceptual clarity, consistency in skills development, and safety of learners and educators alike.
Acknowledgments
The authors would like to acknowledge the Kaurna people of the Adelaide Plains region, and the Peramangk People of the Adelaide Hills region on whose lands this research was conducted. We pay our respects to Elders past and present and acknowledge the ongoing connection of Aboriginal and Torres Strait Islander people to the lands, skies, and waters. This research was supported by a University of Adelaide Faculty of Health Sciences Divisional Scholarship, with continued financial support from Poche SA+NT, Flinders University.
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, J.D. and A.R.; methodology, J.D.; validation, J.D., C.H. and A.R.; formal analysis, J.D.; investigation, J.D.; data curation, J.D. and C.H.; writing—original draft preparation, J.D.; writing—review and editing, J.D., A.R. and K.L.-B.; supervision, A.R.; project administration, J.D. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Aboriginal and Torres Strait Islander cultural safety
Cultural safety is about creating an environment that is safe for Aboriginal and Torres Strait Islander people. This means there is no assault, challenge or denial of their identity and experience.
Cultural safety is about:
- Shared respect, shared meaning and shared knowledge
- The experience of learning together with dignity and truly listening
- Strategic and institutional reform to remove barriers to the optimal health, wellbeing and safety of Aboriginal people. This includes addressing unconscious bias, racism and discrimination, and supporting Aboriginal self-determination
- Individuals, organisations and systems ensuring their cultural values do not negatively impact on Aboriginal peoples, including addressing the potential for unconscious bias, racism and discrimination
- Individuals, organisations and systems ensuring self-determination for Aboriginal people. This includes sharing power (decision-making and governance) and resources with Aboriginal communities. It's especially relevant for the design, delivery and evaluation of services for Aboriginal people.
Key elements of culturally safe workplaces and services
Knowledge and respect for self: Awareness of how one's own cultural values, knowledge, skills and attitudes are formed and affect others, including a responsibility to address their unconscious bias, racism and discrimination.
Knowledge and respect for Aboriginal people: Knowledge of the diversity of Aboriginal peoples, communities and cultures, and the skills and attitudes to work effectively with them.
A commitment to redesigning organisations and systems to reduce racism and discrimination: Strategic and institutional reform to remove barriers to optimal health, wellbeing and safety outcomes for Aboriginal people.
Cultural safety is an ongoing learning journey: An ongoing and response learning framework that includes the need to unlearn unconscious bias and racism and relearn Aboriginal cultural values.
Why is cultural safety important?
Cultural safety is a fundamental human right. It's also a legislative requirement of public agencies to provide safety in the workplace.
The workplace environment, services and settings for health, wellbeing and safety must be culturally safe for all people.
For a fair and equitable society free from racism and discrimination, we must address the underlying causes of culturally unsafe practice.
Everyone's responsibility?
Everyone has a responsibility for the cultural safety of Aboriginal people in their organisation. Everyone is responsible for how they work with Aboriginal staff, health consumers and clients of community services.
Aboriginal and Torres Strait Islander cultural safety framework
The Aboriginal and Torres Strait Islander cultural safety framework has been developed to help mainstream Victorian health, human and community services and the department to create culturally safe environments, services and workplaces.
The framework provides a continuous quality improvement model to strengthen the cultural safety of individuals and organisations.
It aims to help the department and mainstream health, human and community services to strengthen their cultural safety by participating in an ongoing learning journey.
Helping mainstream Victorian health, human and community services and the department to create culturally safe environments, services and workplaces.
Aboriginal and Torres Strait Islander Cultural Safety Framework guidelines
Reviewed 08 February 2023
- Hospitals & health services
- Public hospitals in Victoria
- Patient care
- Ambulance and patient transport
- Non-emergency patient transport
- Non-emergency patient transport review
- NEPT legislation and clinical practice protocols
- Non-emergency patient transport licensing
- NEPT licensing fees
- NEPT services information and guidance
- First Aid Services
- First aid licences
- First aid services information and guidance
- First aid service fees
- Victorian State Trauma System
- Acute medicine
- Emergency care
- Surgical services
- Better at Home
- Critical care
- Hospital in the Home
- Virtual care (Telehealth)
- Perinatal and reproductive services
- Rehabilitation and complex care
- Renal health
- Renal services in Victoria
- Funding for renal services
- Different approaches to haemodialysis
- Specialist clinics
- Access to non-admitted services
- Minimum referral information
- Communication toolkit
- Integrated care
- HealthLinks: Chronic Care
- Community Health Integrated Program (CHIP) guidelines
- Service coordination in Victoria
- Victorian integrated care online resources
- Specialist clinics programs
- Specialist clinics reform
- Specialty diagnostics, therapeutics and programs
- Older people in hospital
- End of life and palliative care in Victoria
- Voluntary assisted dying
- Quality, safety and service improvement
- Digital Health
- Roadmap and Maturity Model
- Standards and guidelines
- Policies and frameworks
- Health Information Sharing Legislation Reform
- My Health Record
- Public hospital accreditation in Victoria
- Credentialing for senior medical staff in Victoria
- Clinical risk management
- Preventing infections in health services
- Healthy choices
- Victorian Perinatal Data Collection
- Rural health
- Improving Access to Primary Care in Rural and Remote Areas Initiative
- Rural x-ray services
- Rural health regions and locations
- Rural and regional medical director role
- Victorian Patient Transport Assistance Scheme
- Rural and isolated practice registered nurses
- Urgent care in regional and rural Victoria
- Private health service establishments
- Private hospitals
- Day procedure centres
- Mobile health services
- Fees for private health service establishments in Victoria
- Design resources for private health service establishments
- Professional standards in private health service establishments
- Legislation updates for private health service establishments
- Complaints about private health service establishments
- Cosmetic procedures
- Guideline for providers of liposuction
- Private hospital funding agreement
- Boards and governance
- About health service boards in Victoria
- Information and education
- Education resources for boards
- Sector leadership
- Data, reporting and analytics
- Health data standards and systems
- Funding, performance and accountability
- Statements of Priorities
- Performance monitoring framework
- Integrity governance framework and assessment tool
- Pricing and funding framework
- Patient fees and charges
- Fees and charges for admitted patients
- Non-admitted patients - fees and charges
- Other services
- Planning and infrastructure
- Medical equipment asset management framework
- Health system design, service and infrastructure planning
- Complementary service and locality planning
- Primary & community health
- Primary care
- Community pharmacist pilot
- EOI - Victorian Community Pharmacist Statewide Pilot
- Victorian Community Pharmacist Statewide Pilot – Resources for pharmacists
- Emergency Response Planning Tool
- Working with general practice
- NURSE-ON-CALL
- Priority Primary Care Centres
- Local Public Health Units
- Community health
- Community health services
- Community health pride
- Registration and governance of community health centres
- Community Health Directory
- Community Health Program in Victoria
- Community health population groups
- Dental health
- Access to public dental care services
- Victoria's public dental care fees
- Victoria's public dental care waiting list
- Dental health for SRS residents
- Dental health program reporting
- Smile Squad school dental program
- Maternal and Child Health Service
- Nursery Equipment Program
- Maternal and Child Health Service Framework
- Maternal and Child Health Service resources
- Child Development Information System
- Early parenting centres
- Maternal Child and Health Reporting, Funding and Data
- Baby bundle
- Sleep and settling
- Maternal and Child Health Workforce professional development
- Aboriginal Maternal and Child Health
- Public health
- Women's Health and Wellbeing Program
- Inquiry into Women's Pain
- Support groups and programs
- About the program
- Victorian Women's Health Advisory Council
- Cemeteries and crematoria
- Cemetery trust member appointments
- Cemetery search
- Cemeteries and crematoria complaints
- Exhumations
- Governance and finance
- Cemetery grants
- Interments and memorials
- Land and development
- Legislation governing Victorian cemeteries and crematoria
- Cemeteries and crematoria publications
- Repatriations
- Rights of interment
- Medicines and Poisons Regulation
- Patient Schedule 8 treatment permits
- Schedule 8 MDMA and Schedule 8 psilocybine
- Schedule 9 permits for clinical trials
- Documents and forms to print or download
- Legislation and Approvals
- Frequently Asked Questions - Medicines and Poisons Regulation
- Health practitioners
- Licences and permits to possess (& possibly supply) scheduled substances
- Medicinal cannabis
- Pharmacotherapy (opioid replacement therapy)
- Recent updates
- Environmental health
- Improving childhood asthma management in Melbourne's inner west
- Climate and weather, and public health
- Environmental health in the community
- Environmental health in the home
- Environmental health professionals
- Face masks for environmental hazards
- Human health risk assessments
- Lead and human health
- Per- and poly-fluoroalkyl substances (PFAS)
- Pesticide use and pest control
- Food safety
- Information for community groups selling food to raise funds
- Food businesses
- Food safety information for consumers
- Food regulation in Victoria
- Food safety library
- Food allergens
- Introducing Standard 3.2.2A: Food safety management tools
- Immunisation
- Respiratory syncytial virus (RSV) immunisation
- Seasonal influenza vaccine
- Immunisation schedule and vaccine eligibility criteria
- Ordering vaccine
- Immunisers in Victoria
- Immunisation provider information
- Cold chain management
- Adverse events following immunisation reporting
- Vaccine error management
- Vaccination for infants and children
- Vaccination for adolescents
- Vaccination program for adults
- Vaccination for special-risk groups
- Immunisation resources order form
- Victorian coverage rates for Victoria
- Infectious diseases guidelines & advice
- Infection control guidelines
- Disease information and advice
- Advice to the cruise industry: reporting infections
- Notifiable infectious diseases, conditions and micro-organisms
- Notification procedures for infectious diseases
- Infectious diseases surveillance in Victoria
- Germicidal ultraviolet light
- Protecting patient privacy in Victoria
- Population health systems
- Evidence and evaluation
- Health promotion
- Health status of Victorians
- Municipal public health and wellbeing planning
- Population screening
- Cancer screening
- Conditions not screened
- Improving outcomes in under-screened groups
- Infant hearing screening
- Newborn bloodspot screening
- Prenatal screening
- Screening registers
- Preventive health
- Type 2 diabetes and cardiovascular disease prevention
- Eye health promotion
- Injury prevention
- Healthy eating
- Oral health promotion
- Physical activity
- Sexual health
- Sex worker health
- Decriminalisation of sex work
- Automatic mutual recognition
- Domestic smoke detectors
- Lasers, IPL and LED devices for cosmetic treatments and beauty therapy
- Victoria's regulatory framework for radiation
- Tobacco reforms
- Tobacco reform legislation and regulations
- E-cigarettes and vaping
- Quitting smoking and vaping
- Smoke-free and vape-free areas
- Building entrances
- Children's indoor play centres
- Public hospitals and health centres
- Children's recreational areas
- Playground equipment
- Skate parks
- Swimming pools
- Under-age sporting events
- Enclosed workplaces
- Government buildings
- Learning environments
- Outdoor dining
- Outdoor drinking areas
- Patrolled beaches
- Train platforms and bus and tram shelters
- Under-age music or dance events
- Tobacco and e-cigarette retailers
- Making a report or complaint
- Resources and factsheets
- Alternative water supplies
- Aquatic facilities
- Blue-green algae (cyanobacteria)
- Drinking water in Victoria
- Legionella risk management
- Private drinking water
- Recreational water use and possible health risks
- Water fluoridation
- Chief Health Officer
- About the Chief Health Officer
- Chief Health Officer publications
- Health alerts and advisories
- Mental health
- Mental Health and Wellbeing Act 2022
- Mental Health and Wellbeing Act 2022 Handbook
- Community information
- Mental Health and Wellbeing Act 2022 in your language
- About Victoria's mental health services
- Area-based services
- Statewide and specialist mental health services
- Mental Health Community Support Services
- Support and intervention services
- Language services - when to use them
- Access to mental health services across areas
- Transport for people in mental health services
- Practice and service quality
- Medical Treatment Planning and Decisions Act
- Service quality
- Specialist responses
- Mental health and wellbeing reform
- Reform activity updates
- Priority areas
- Latest news
- Working with consumers and carers
- Consumer and carer engagement
- Consumer and Carer Experience Surveys
- Family support and crisis plans
- Consumer and carer financial support
- Supporting children whose parents have a mental illness
- Supporting parents with a mental illness
- Prevention and promotion
- Early intervention in mental illness
- Mental health promotion in Victoria
- Suicide prevention in Victoria
- Priorities and transformation
- Supporting the social and emotional wellbeing of Aboriginal and Torres Strait Islander Victorians
- National mental health strategy
- Rights and advocacy
- Making a complaint about a mental health service
- Chief Psychiatrist
- About the Chief Psychiatrist
- Obligations under the Mental Health and Wellbeing Act 2022
- Reporting obligations for clinical mental health and wellbeing services
- Reporting a failure to comply with the Mental Health and Wellbeing Act 2022
- Governance and committees
- Mental health and wellbeing support
- Making a complaint and seeking advocacy
- Second psychiatric opinion and process of review by Chief Psychiatrist
- Reform activities and news involving the Office of the Chief Psychiatrist
- Resources and reports
- Chief psychiatrist guidelines
- Chief Mental Health Nurse
- About Victoria's Chief Mental Health Nurse
- Best practice
- Reducing restrictive interventions
- Research and reporting
- Mental health performance reports
- Reporting requirements and business rules for clinical mental health services
- Alcohol & drugs
- Alcohol and other drug treatment services
- Overview of Victoria's alcohol and drug treatment system
- Pathways into alcohol and other drugs treatment
- Prevention and harm reduction
- Medically supervised injecting room
- Victoria's Take-Home Naloxone Program
- Community-based AOD treatment services in Victoria
- Residential treatment services
- Mildura statewide alcohol and drug residential treatment service
- Drug rehabilitation plan
- Hospital-based services
- Forensic services
- Pharmacotherapy treatment
- Services for Aboriginal people
- Services for young people
- Statewide and specialist services
- Compulsory treatment
- Family and peer support
- Public intoxication reform
- New public intoxication response services
- Policy, research and legislation
- Alcohol and drug research and data
- Legislation governing alcohol and other drug treatment
- Alcohol and other drug service standards and guidelines
- Alcohol and other drug client charter and resources
- Alcohol and other drug treatment principles
- Service quality and accreditation
- Alcohol and other drug program guidelines
- Maintenance pharmacotherapy
- Specialist Family Violence Advisor capacity building program in mental health and alcohol and other drug services - Victoria
- Alcohol and other drug workforce
- Learning and development
- Alcohol and other drug workforce Minimum Qualification Strategy
- Workforce data and planning
- Funding and reporting for alcohol and other drug services
- Funding of alcohol and other drugs services in Victoria
- Reporting requirements and business rules for alcohol and other drug services
- Drug alerts
- 25C-NBOMe and 4-FA sold as '2C-B'
- Novel stimulants sold as MDMA, cocaine or speed
- Protonitazene sold as ketamine
- High potency benzodiazepine tablets
- MDMA adulterated with PMMA
- 25B-NBOH sold as powdered 'LSD'
- Green 'UPS' pills containing N-ethylpentylone (no MDMA)
- N-ethylpentylone in cocaine
- Ageing & aged care
- Supporting independent living
- Low cost accommodation support programs
- Personal Alert Victoria
- Dementia services
- Victorian Aids and Equipment Program
- Residential aged care services
- Public sector residential aged care services
- Safety and quality in public sector residential aged care
- Physical and social environments
- Emergency preparedness in residential aged care services
- My Aged Care assessment services
- Home and Community Care Program for Younger People
- HACC data reporting
- HACC PYP fees policy and schedule of fees
- Dementia-friendly environments
- Designing for people with dementia
- Maintaining personal identity
- Personal enjoyment
- Interior design
- Dining areas, kitchens and eating
- Bedrooms and privacy
- Gardens and outdoor spaces
- Assistive technology
- Staff education and support
- Strategies, checklists and tools
- Our Strategic Plan 2023-27
- Our organisation
- Our secretary
- Leadership charter
- Our services
- Our vision and values
- Specialist offices
- Senior officers in health
- Human Research Ethics Committee (HREC)
- Gifts, benefits and hospitality policy
- Information Asset Register
- Health legislation
- Health regulation reform
- Health legislation overview
- Health Complaints legislation
- Health Records Act
- Human Tissue Act 1982
- Public Health and Wellbeing Act 2008
- Voluntary Assisted Dying Act
- Victoria's pandemic management framework
- Independent Pandemic Management Advisory Committee
- Pandemic Order Register
- Our ministers
- Our role in emergencies
- State Health Emergency Response Arrangements
- Emergency type
- Department's responsibilities in emergencies
- Health services’ responsibilities in emergencies
- Aboriginal employment
- Current vacancies
- Employment programs for students and graduates
- Rise program
- Inclusion and diversity at the Department of Health
- Health workforce
- Working in health
- Information sharing and MARAM
- Child Safe Standards
- Regulatory functions
- Reviews of decisions
- Victorian Public Healthcare Awards
- Aboriginal healthcare workers
- Mental health workforce
- Lived and living experience workforces
- Engaging with lived and living experience workforces
- Our workforce, our future
- Nursing and midwifery
- Free nursing and midwifery study
- Additional funding for nursing and midwifery positions
- Becoming a nurse or midwife
- Undergraduate nursing and midwifery scholarships
- Undergraduate student employment programs
- Nursing and midwifery graduates
- Nursing and midwifery graduate sign-on bonus
- Working as a nurse or midwife
- Enrolled nurse to registered nurse transition scholarships
- Support for new nurse practitioners
- Postgraduate scholarships for nurses and midwives
- Nurse practitioners
- Returning to nursing or midwifery
- Refresher pathway for nurses and midwives
- Re-entry pathway scholarships for nurses and midwives
- Nursing and midwifery - legislation and regulation
- Nursing and midwifery program - health sector
- Allied health workforce
- Education and training
- Enterprise agreements
- Worker health and wellbeing
- Working with us
- Grants and programs
- Freedom of Information
- Part II - Information Statements
- Procurement policies
- Protective markings
- Health and medical research
- Sponsorship application information
- Publications
- Annual reports
- Fact sheets
- Strategies, plans and charters
- Policies, standards and guidelines
- Research and reports
- Forms and templates
- Communities
- Designing for Diversity
- Vulnerable children
- Vulnerable children - responsibilities of health professionals
- Identifying and responding to children at risk
- Pathway to good health for children in care
- Older people
- Aboriginal health
- Improving health for Victorians from culturally and linguistically diverse backgrounds
- Asylum seeker and refugee health in Victoria
- News and media hub
- Media releases
- Health alerts
- Feedback and complaints
- Make a payment
- Fees, charges and penalties subject to automatic indexation
- Our campaigns
Share this page
- Facebook , opens a new window
- X (formerly Twitter) , opens a new window
- LinkedIn , opens a new window

IMAGES
COMMENTS
The construct of the aforementioned issue lies in directing nursing area as 'safe' and 'effective' for the customer or family/ whanau from dissimilar culture (Richardson & MacGibbon, 2010). Obviously, cultural safety occurs as "the effective nursing practice of a person or family from another culture, and is determined by that person ...
Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. International Journal for Equity in Health, 18 (1), 1-17. Web. This essay, "The Cultural Safety Concept: Gibbs' Reflective Cycle" is published exclusively on IvyPanda's free essay examples database.
Cultural safety is a radical paradigm shift from other approaches that maintain a focus on the interactions between patients and providers − for example, cultural sensitivity, awareness and competency − because it is based on a politicized understanding of health and of power inequities underlying the health system (Brascoupé & Waters ...
Further ensuring standards of cultural safety through adopting culturally appropriate approaches that recognise Māori as tāngata whenua, and ... binaries/54814_Example_reflective_essay.pdf Finally, some useful reflections can be found on the internet. Here are some examples:
Cross et al. [] contextualized cultural competency as part of a continuum ranging from the most negative end of cultural destructiveness (e.g. attitudes, policies, and practices that are destructive to cultures and consequently to the individuals within the culture such as cultural genocide) to the most positive end of cultural proficiency (e.g. agencies that hold culture in high esteem, who ...
Implications. Cultural safety promotes a more critical and inclusive perspective of culture. As an analytical lens in occupational therapy practice and research, it has the potential to reveal and generate broader understandings of occupation and health from individuals or groups in society who are traditionally silenced or marginalized.
Background. The right to health was recognised as a human right in the 1966 International Covenant on Economic, Social, and Cultural Rights. According to the United Nations Office of the High Commissioner for Human Rights (OHCHR), healthcare services must be culturally appropriate and acceptable [].The International Council of Nurses (ICN) Code of Ethics states: "Inherent in nursing is a ...
Cultural Safety Principles ExamplesCul. ural Safety Prin. iples - ExamplesBest, O. (2017). The cultural safety journey: An Aboriginal Austr. lian nursing and midwifery context. In O. Best & B. Fredericks (Eds.), Yatdjuligin: Aboriginal and Torres Strait Islander Nur. ing and Midwifery Care (pp. 46-66). Cambridge: Cambridge University.
The ability of healthcare practitioners to comprehend the specific cultural needs of their patients and to offer appropriate care in accordance with those requirements is referred to as "cultural competence.". Cultural competence is an essential part of providing medical care. Providers of medical care need to adopt a strategy that is ...
Cultural safety strategies. Reflection is a key strategy of cultural safety. It is an on-going process of reflecting on self, one's own culture and profession. This includes considering the power and privilege, attitudes, assumptions and beliefs about others that may be inherent in these cultures. Strategies for culturally safe practice include:
Reflection is applied to help health and human service professionals to decolonize and move toward culturally safe practice. Finally, we examine the relevance of this topic to your practice, and the transferability of reflective practice that is regardful in any setting. Reflection is a powerful tool for learning, development, and growth and is ...
Critical Reflection. Throughout these modules, we will invite you to practice cultural safety through critical self-reflection exercises. Self-reflection is an integral feature of culturally safe practice. These questions will be approached differently by everyone, and personal responses may change as you continue your cultural safety journey.
Cultural humility is a way in which health care providers practice that enable cultural safety. It is a process of self-reflection to understand personal and systemic biases, and privilege to develop and maintain respectful processes and relationships based on mutual trust. ... Brascoupé, S. and Waters, C. (2009). Cultural safety: Exploring ...
Welcome to the HealthInfoNet's Portal on Cultural Safety for Health Professionals. The portal aims to support health professionals in their practice to deliver culturally safe, accessible and responsive healthcare that is free from racism. ... (CC BY-NC-ND 3.0) licence. Excluded material owned by third parties may include, for example, design ...
Assignment title: Reflective essay Unit code and Title: NCS2202 Culture and Health Lecturer: Carol Squire Student Name: Conor Gary Osborne Student Number: 10389545 Date of Submission: Word Count: 2112 Table of Contents Health issues impacting Aboriginal and Torres Strait Islander The client in Cultural knowings framework: understanding and Social determinants of health: understanding and 2 ...
Decent Essays. 402 Words. 2 Pages. Open Document. The outcome of cultural awareness and cultural sensitivity is cultural safety (Berg, 2010). In practicing cultural safety, it is not really expected that health care workers will know all cultures; it is acknowledging and respecting people regardless of their differences and beliefs (Hughes ...
Cultural safety requires healthcare professionals and organisations to improve healthcare, facilitate patient access to healthcare, and achieve equity within the workforce. This ethnomethodological study, which consisted of two phases, explored the concept of cultural safety from the perspective of Advanced Practice Nurses. Semi-structured interviews and the nominal group technique were used ...
As a result, cultural safety assists people to understand the limitations regarding cultural competence, which is aimed at the practitioners' attitudes, knowledge, and skills (ANAC, 2000). It is also concerned with the power relationships between the nurses and the individuals they take care of as well as the experience of the recipient of care.
Cultural expression assumes many forms, including language, traditions, stress, pain, anger, sorrow, spirituality, decision making and even world philosophy (Catalano, 2006).Cultural safety is a process that involves the individual knowing of their self and their own culture, becoming aware of, respectful of, and sensitive to different cultures ...
Power et al. describe a reflective essay assignment in which students were required to complete three online reflections before, during, and after their 3-week placement. Students were provided with 'trigger questions' to prompt their online reflections, and these reflections formed the basis of their submitted reflective essay.
The concept of Cultural Safety was developed from the experience of colonisation of Indigenous Peoples, the impacts on health experience from the experience of social, historical, political, and economic diversity of a culture (Ramsden, Citation 2002) is determined by Indigenous Peoples, and involves ongoing critical reflection of the ...
Cultural safety is about creating an environment that is safe for Aboriginal and Torres Strait Islander people. This means there is no assault, challenge or denial of their identity and experience. Cultural safety is about: Strategic and institutional reform to remove barriers to the optimal health, wellbeing and safety of Aboriginal people.