An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection


An overview for biomedical waste management during pandemic like COVID-19
V. s. kanwar.
1 Chitkara University School of Engineering and Technology, Chitkara University, Solan, Himachal Pradesh India
2 Chitkara University School of Computer Applications, Chitkara University, Solan, Himachal Pradesh India
A. L. Srivastav
3 Central Pollution Control Board, Lucknow, India
Amid COVID-19, world has gone under environmental reformation in terms of clean rivers and blue skies, whereas, generation of biomedical waste management has emerged as a big threat for the whole world, especially in the developing nations. Appropriate biomedical waste management has become a prime concern worldwide in the pandemic era of COVID-19 as it may affect environment and living organisms up to a great extent. The problem has been increased many folds because of unexpected generations of hazardous biomedical waste which needs extraordinary attentions. In this paper, the impacts and future challenges of solid waste management especially the biomedical waste management on environment and human beings have been discussed amid COVID-19 pandemic. The paper also recommends some guidelines to manage the bulk of medical wastes for the protection of human health and environment. The paper summarizes better management practices for the wastes including optimizing the decision process, infrastructure, upgrading treatment methods and other activities related with the biological disasters like COVID-19. As achieved in the past for viral disinfection, use of UV- rays with proper precautions can also be explored for COVID-19 disinfection. For biomedical waste management, thermal treatment of waste can be an alternative, as it can generate energy along with reducing waste volume by 80–95%. The Asian Development Bank observed that additional biomedical waste was generated ranged from 154 to 280 tons/day during the peak of COVID-19 pandemic in Asian megacities such as Manila, Jakarta, Wuhan, Bangkok, Hanoi, Kuala Lumpur.
Introduction
COVID-19 (or Coronavirus disease 2019) originated from the animals (meat/fisheries market of the Wuhan city, China) can cause severe infections to the human respiration system (Cascella et al. 2020 ; Roujian et al. 2020 ; Zhu et al. 2020 ; Xu et al. 2020 ). Firstly, it was diagnosed in the end of December, 2019 in Wuhan city of China when like pneumonia symptoms were observed in the local residents of Wuhan (WHO 2020a ; Lokhandwala and Gautam 2020 ; Sohrabi et al. 2020 ). Other health problems were also got detected because of CIVID-19 infections including breath shortness, fever, pain in muscles and head (Huang et al. 2020 ). WHO declared worldwide human health emergency (pandemic) due to fast rate of COVID-19 infections as it took around 3 months durations only to reach in 100 nations. Moreover, 10 million people of the world got infected with COVID-19 till the last of May, 2020, whereas up to last week of June, 2020, COVID-19 infections reached in 216 countries (WHO 2020b ). Even top economic nations of the world (USA, Germany, France, Spain, Japan, Singapore, Italy etc.) were stuck in the raising COVID-19 infections among the community people (Amanat and Krammer 2020 ). However, USA was and still on the top in terms of highest numbers of both infections and deaths due this pandemic (CDC 2020 ). In Asia, India is on the top position reading deaths as well infections due to corona virus (MoHFW 2020 ). In the absence of vaccine, testing of COVID-19 has become very important to prevent its further infections and reverse-transcription polymerase chain reaction, medical imaging and computed tomography are the recommended methods of detection (Ardakani et al. 2020 ). Despite of infecting huge population, the fatality rate of COVID-19in India is less than Middle East respiratory syndrome (MERS, year 2012) and severe acute respiratory syndrome (SARS CoV-1 year 2003) and more than the Spanish flu (year 1918) as shown in Fig. 1 .

Human fatality rates of different viral infections (
Source : Modified from Goel et al. 2020 )
From Fig. 1 , it was observed that in year 2012, MERS had affected people of 27 countries of the world with maximum fatality rate of 34.3% followed by SARS CoV-1 in year 2003 with 15%. In 1918, the fatality rate of Spanish flu was rescored as 10% which is less than COVID-19 (12.3%) (Callaway et al. 2020 ; Goel et al. 2020 ). However, according to Gates ( 2020 ), it can kill only 1% of total infected persons including old aged people as well as adults, if they were already suffering with some serious health disorders. However, it can spread easily among the humans as compared to other illness (Goel et al. 2020 ). Because of this reason, initially, rate of infection was slow and later through community transmission; it has reached in every part of the world (Anderson et al. 2020 ; Shammi et al. 2020 ).
Factors responsible for the transmission of COVID-19
As per the studies, it has been found that several days are required for complete inactivation of COVID-19 virus (Casanova et al. 2009 ; Qu et al. 2020 ). It is quite evident corona virus is mostly spreading through physical contacts between the individuals knowingly or unknowingly. However, it can also infect the healthy people through the skin, mouth, nose and eyes of any COVID-19 patient after direct or indirect interactions. The virus can survive on the various types of surfaces (medical wastes, plastic etc.) or environment for a specific time (Weber et al. 2016 ; Qu et al. 2020 ). Further, the chances of viral infection may be governed by several factors including stability of virus containing aerosols in the air (usually 3 h is reported), active periods of the virus on the surfaces like steel (7 days), glasses and currency papers (4 days). Even after applying soap on the hands, additional five minutes are required to inactivate the virus. Hence, it is advisable that one should avoid touching any part of the face within 5 min of hand wash (Goel et al. 2020 ).Other factors of COVID-19 transmission may also be considered as sneezing, coughing, and talking with any infected person. In many studies, presence of COVID-19 virus has been diagnosed in the excreta, tear, urine and other body secretions of the infected people (Zhang et al. 2020 ; Xia et al. 2020 ; Peng et al. 2020 ). In Japan, a study has shown that COVID-19 transmission is also possible through the lighter water droplets containing virus. As lighter water droplets (or aerosols) when come in the contact of any COVID-19 infected person and thereafter it can transmit into healthy people. However, this type of airborne infection depends upon the local weather conditions (wet or dry) (Chin and Poon 2020 ; Wölfel et al. 2020 ). Moreover, a theory of asymptomatic or oligosymptomatic infections are also reported in the literatures (Wölfel et al. 2020 ). There are different types of which can trigger in the transmission of the COVID-19 (Fig. (Fig.2 2 ).

Responsible factors for the human transmission of COVID-19
Most importantly, poor people (may be due to insanitary practices), elderly persons, workers of waste management authorities are in high risk zone of COVID-19 infection. However, their restricted movement can reduce the chance of pandemic outbreak (United Nations 2020 ). Because of this reason, in USA and Singapore, recycling of waste materials has been discontinued or carried out with less frequency to reduce the risk of further transmission of COVID-19 among the sanitary workers (Zambrano-Monserrate et al. 2020 ; National Environmental Agency, Singapore 2020 ). In developing world, situation has become very critical during this pandemic because of unemployment during lockdown and panic of infection among waste management people, and ultimately, it may affect the economy of the nations too (World Bank 2020 ). According to Nghiem et al. ( 2020 ) and Kulkarni and Anantharama ( 2020 ) it can be managed by adopting best practices of waste management to safeguard the health of these workers during handling of contagious wastes. Major objective of the present research paper is to explore the practices which can be helpful in the management of biomedical wastes during pandemic like COVID-19. Moreover, alternatives options and challenges of future have also been discussed.
Impacts of COVID-19 pandemic
(i) impact on the human health.
Human respiration system is the main target of this COVID-19 virus. Moreover, this has become more dangerous for the elderly people or the people who are suffering with sever diseases related with cardiac system, diabetes, cancer, or else (Dhama et al. 2020 ; Rodriguez-Morales et al. 2020 ; Mahajan and Kaushal 2020 ). However, it has also found that children are not a common victim of the COVID-19 virus (Huang et al. 2020 ) because usually they do not go outside the home as well as less travelling exercise (Lee et al. 2020 ). Chen et al. ( 2020 ) reported that only in China health recovery of the citizens was so better due to an improvement in air quality amid COVID-19 lockdown periods. Therefore, due to lockdown, the pollution load of environmental systems (atmosphere, hydrosphere and lithosphere) has decreased worldwide and this may be helpful for the protection of public health. Figure 3 shows the confirmed infections of COVID-19 in top ten countries as on Sept. 30, 2020.

Total COVID-19 infections in top 10 mostly affected countries (WHO 2020b ) (assessed on the 30.09.2020)
From Fig. 3 , it appears that till Sept. 30, most affected countries with COVID-19 infections are USA, Indian, Brazil, Russia and Columbia. Similar problems have been observed in the Bangladesh during lockdown periods amid COVID-19 pandemic (Hopman et al. 2020 ). Transmission of corona virus through air is also reported (Bourouiba 2020 ) and can be prevented by using face mask at crowded places (Klemeš et al. 2020 ). Moreover, during the crisis maintaining employment opportunities along with public health protection has become top priorities of the government authorities. For public health protection, there are many issues should be handles with due care like advancement of medical standards, easy availability of testing facility, revisions of policies for local public etc. (WHO 2020b ; Sharma et al. 2020 ). In addition to these, many psychological disorders have been observed especially among patients due to this pandemic as studied in United Kingdom (Ford et al. 2020 ; Holmes et al. 2020 ). Figure 4 summarises the diverse types of impacts observed during the COVID-19 outbreak.

Impact of COVID-19 on the environment and human beings
Elderly people are found at the larger risks of COVID-19 and during quarantine period, there is a great chance of developing mental disorders (for example, anxiety, guiltiness, dementia, depression etc.) because of loneliness (Armitage and Nellums 2020 ; Holmes et al. 2020 ; Ahorsu et al. 2020 ; Shammi et al. 2020 ).These mental problems may be responsible for the increase in number of suicide cases in the society (Duan and Zhu 2020 ). However, few medicines are recommended in case of emergency situation for COVID-19 patients (Singh et al. 2020 ). Recently, Goel et al. ( 2020 ) reported that silver coated grapheme oxide sheets and chiral gold nanohybrids for the inhibition as well as detection of the different types of viruses including corona virus. According to Chan ( 2020 ) application of different types of nano-materials should also be explored against the coronavirus. Because of unavailability of proper medication, “social lockdown” or “social distancing” has been imposed to stop the transmission of COVID-19 virus across the world (Paital et al. 2020 ; Zambrano-Monserrate et al. 2020 ; Lokhandwala and Gautam 2020 ; Somani et al. 2020 ). During lockdown, restrictions were imposed on every type of public meetings, industries and automobiles to maintain social distancing. Due to shutdown of factories and vehicles many positive changes have been observed in the cosmopolitan environment.
(ii) Impact on the environmental systems
In twenty-first century, there are many challenges for whole world including severe environmental quality diminution (Chakraborty and Maity 2020 ) due to over industrialization as well as unorganized fast urbanization as it requires huge demand of natural resources. Because of overexploitation of resources, ecological systems have been deteriorated which includes air pollution, water quality degradation, soil contamination, global warming, threat to the biodiversity, human health problems etc. (Bremer et al. 2019 ). Amid COVID-19 pandemic, world has gone into complete lockdown except essential commodities which imposed ban on the opening of industries as well as movement of the vehicles. Hence, during lockdown periods emission of harmful gases and wastewater discharges were decreased significantly and considerable environmental healing was observed across the world (Australia, China, France, Germany, India, Italy, Iran, Spain, South Korea, Taiwan, Turkey, United Kingdom and USA) since March 2020 (Chakraborty and Maity 2020 ; Elavarasan and Pugazhendhi 2020 ; Atalan 2020 ). As it has been observed that air pollution is responsible for > 7 million human deaths in whole world and out of it, 1.2 million deaths were reported in only in India (WHO 2018 ; Polk 2019 ). Significant reduction in the concentration of air pollutants (particulate matters and greenhouse gases) was reported from the various parts of the world like Kazakhstan (Kerimray et al. 2020 ), India (Mahato et al. 2020 ) and Brazil (Dantas et al. 2020 ). Besides, industries and automobiles, operations of aeroplanes were also affected during lockdown and it was also helped in the reduction of greenhouse gases in the atmosphere (Corletta et al. 2020 ). However, level of indoor air pollutants (including black carbon of smoke) was increased amid lockdown as most of the people were got stuck inside their homes (NASA 2020 ). Availability of adequate natural ventilation (not any artificial systems like air conditioner etc.) inside the homes could dilute the concentrations of indoor air pollutants (Bhatia and Bhaskar 2020 ; Somani et al. 2020 ). Moreover, concentrations of greenhouse gases were also remarkably decreased during lockdown periods, for example 2600 metric tons of carbon dioxide was decreased across the global amid COVID-19 pandemic (Global Climate Report 2019 ) due to less energy demand as around 64% of total electrical energy is getting produced from the natural gas and coals (Somani et al. 2020 ). In India, the carbon dioxide emission was decreased in between 15 and 30% during March to April, 2020 (Myllavirta and Dahiya 2020 ). Similarly, due to closure of machines and restricted vehicle movements, level of noise also got decreased as reported in many countries such as China (19%), USA (36%) and United Kingdom (54%) (Somani et al. 2020 ). Moreover, decrease in oceanic noise levels were also observed during lockdown due to limited waterways traffic and it could have provided a better environment for aquatic lives (Ian Randall 2020 ). In India, around 40–75% noise level reductions were reported from the various states or cities (for example, Karnataka, Delhi, Bengaluru, Kolkata ) due to non-movements of the trains (Somani et al. 2020 ) as trains and other vehicles are the principal causes of noise pollution in megacities of India (Mishra et al. 2010 ). Furthermore, biodiversity conservation via revival of natural shelters for marine organisms (turtles), other aquatic lives, birds, wild life animals were found to be very rapid due to less movement of human beings (Corletta et al. 2020 ; Zambrano-Monserrate et al. 2020 ) as the reports were published in the countries like Mexico, Spain, India as well as Ecuador (Zambrano-Monserrate et al. 2020 ; Somani et al. 2020 ). Self-purification capacities of many rivers/lakes increased amid lockdown because of less wastewater discharge as most of the pollution in surface water reservoirs is due to the raw sewage mixing into them (Sinha et al. 2016 ; CPCB 2020a ; Corletta et al. 2020 ; Zambrano-Monserrate et al. 2020 ). In India, amid lockdown, water quality of rivers Ganga and Yamuna were improved for bathing and aquaculture purpose as observed by the Central Pollution Control Board (CPCB) than previous years (CPCB 2020a ). Most importantly, Uttarakhand Pollution Control Board of India stated that Ganga river water at Haridwar (location: Har-ki-Pauri) was improved for drinking purpose after more than 30 years (Katariya 2020 ). Similarly, (Yunus et al. 2020 ) reported ~ 15.6% water pollution reduction in the Venbanad Lake of Kerala province of India. These improvements were observed in many Indian states ( Uttrakhand, UttarPradesh, West Bengal, Karnataka, Tamilnadu ) because of very less number of visitors, drastic decrease in the volume of the untreated effluents (~ 500%) during lockdown periods (Somani et al. 2020 ).
Challenges of biomedical waste generation and its proper management amid COVID-19 pandemic
Apart from some environmental benefits, great negative impacts will be observed across the globe due to COVID-19 pandemic including public health crisis (WHO 2020a ) including hurdles in the recycling of the wastes (Calma 2020 ), economical emergency and unemployment (Atalan 2020 ), proper management and disposal of hospital wastes and need of extra disinfectants (Zambrano-Monserrate et al. 2020 ). Certainly, COVID-19 pandemic is one of the greatest challenges for everyone such as the scientists, industrialists, doctors, paramedical staffs, police, municipal authorities, government authorities as well as local public of the world. Since its beginning in 2019 from China, researchers of the world are working 24 h a day to develop effective medication/or vaccine against it. However, no any solution is reported till now against this virus (Vellingiri et al. 2020 ). Because of high mutagenic characters and continuous morphological changes in the COVID-19, development of its vaccine is facing difficulties (American Society of Microbiology 2020 ). Therefore, governments of most of the nations have imposed compulsory national lockdowns to keep safe their citizens except essential supplies of the goods and medicines. Apart from it, individual physical distancing and self-quarantine were also recommended for each person to ensure wellbeing (Balachandar et al. 2020 ). On the other hand, because of the lockdown, worldwide huge economical loss is expected in near future (Somani et al. 2020 ) due to closure of industries and manufacturing units (United Nations Industrial Development Organization 2020 ). Because of shutting industries, product supply chain of goods has been ruined (Kahlert and Bening 2020 ; Kulkarni and Anantharama 2020 ). In addition to huge economical loss, health workers and hospitals of the world (both developed and developing countries) are under tremendous pressure due to exponential rate of COVID-19 infections. Moreover, critical patients are not getting proper care due to unavailability of intensive care units in most of the hospitals. Health workers are using personal protective equipments (for example, face mask, transparent face shield, gloves etc.) to protect themselves from this virus and providing these safety devices are also a challenge for the authorities (Dargaville et al. 2020 ). Some misconceptions have been spread into the society that intake of lemon beverages, wine etc. can be used as medications against Coronavirus (Shammi et al. 2020 ). Moreover, in most of the countries, numbers of unemployed personas have been increased due to the pandemic (Kulkarni and Anantharama 2020 ). In order to handle these challenges, many governments are planning effective strategies for the sustainable development of the world after COVID-19 era (Rosenbloom and Markard 2020 ).
Owing to lockdown amid COVID-19 pandemic, world has gone under environmental reformation in terms of clean rivers and blue skies, whereas, this pandemic has created lots of problems in the management of solid waste (Gardiner 2020 ). Appropriate solid waste management has been a big challenge for the world especially to the developing nations. COVID-19 pandemic has boosted this problem many folds because of unexpected generations of waste materials (especially biomedical waste: a type of hazardous waste). It needs to be given extraordinary attentions by the waste management authorities and governments (Ferronato and Torretta 2019 ; Kaufman and Chasan 2020 ) as the compositions and volumes of the waste materials has been changed (Mallapur 2020 ). Moreover, Fan et al. ( 2021 ) reported that during COVID-19 pandemic many challenges have been emerged while managing waste materials because of changes observed in the volume, types, composition, disposal rate, frequency of collection, availability of treatment options, funds availability etc. as shown in Fig. 5 .

Common challenges of infected waste management during pandemic (
modified from Fan et al. 2021 )
In order to prevent transmission of COVID-19, lockdown was imposed in many countries which increased online shopping for the household products especially in developed countries. This panic situation has created a big concern of proper waste management in terms of collection, recycle, treatment as well as disposal (Zambrano-Monserrate et al. 2020 ; Nghiem et al. 2020 ). Moreover, Rahman et al. ( 2020 ) observed that hospital waste can cause severe environmental as well as public health problems as 5.2 million people of the world are dying annually due to mismanagement of hospital waste materials. During the pandemic, the composition of medical waste has changed drastically as it contains huge quantities of discarded masks, gloves, PPE kits etc. (UNEP 2020 ; Somani et al. 2020 ) and it could be dangerous for the society (especially workers of waste management authorities) in terms of increasing transmission due to mishandling of such types of infected wastes (Sharma et al. 2020 ). Similar, concern was also expressed by Occupational Safety and Health Administration (OSHA) regarding further infections among the workers of waste management authorities (OSHA 2020 ). Further, wastage of plastic waste also got increased across the world which is being used by pharmaceutical industries for packaging purpose (WHO 2020d ). Therefore, World Health Organization, Central Pollution Control Board (India), OSHA and other prestigious international organizations have developed new guidelines to manage the waste materials (especially hospital wastes) during COVID-19 (Somani et al. 2020 ; Kulkarni and Anantharama 2020 ). According to WHO, > 80% wastes of the hospitals were found in the category of noncontiguous wastes which can be treated and managed similar as municipal waste materials (WHO 2020d ). Normally, biomedical wastes are waste generated from the hospitals and veterinary medical premises including syringe, pathological materials, pharmaceutics etc. (Sharma et al. 2020 ; Somani et al. 2020 ). Due to COVID-19 pandemic, huge mass of plastic wastes has been increased across the world as it is being used in personal protection kits (for example, gloves, masks, face shield, ventilator etc.) (Klemeš et al. 2020 ). In India, waste management authorities are in more trouble due to fear of infection as safety measures are not good in the comparison of developed countries. During, lockdown in India, the bulk of biomedical waste was found to be greater than the municipal solid wastes (Somani et al. 2020 ). Significant reduction in municipal solid waste quantity was attributed to the shutdown of markets, shops, hotels, commercial premises, offices, transport etc. (Somani et al. 2020 ), whereas, huge amount of biomedical waste was generated probably because of high numbers of the COVID-19 infected persons admitted in the hospitals. In USA, huge quantities of food waste were generated during lockdown as most of the commercial institutes (like hotels, restaurants, mess etc.) had already purchased the raw materials (Kulkarni and Anantharama 2020 ). During lockdown, similar observations of change in the quantity and composition of waste materials have been reported from North America (SWANA 2020 ) and China (Klemeš et al. 2020 ). According to Klemeš et al. ( 2020 ), only in Hubei (China), around 370% increase in biomedical waste after COVID-19 infections. However, the quantity of municipal solid waste was generated less than 30% during pandemic. Nghiem et al. ( 2020 ) and Zambrano-Monserrate et al. ( 2020 ) have also studied the change in the waste composition (and quantity) along with their negative impacts of change in waste generation on the environment and health workers. They found that transmission of virus in community has significantly affected waste recycling facilities around the world. For instance, in United Kingdom, 46% material recovery process was stopped due to lockdown amid COVID-19 pandemic and similarly 31% recycling units of USA were also closed in the similar situations (Somani et al. 2020 ).
Contagious biomedical wastes can spread disease in living organisms and their mishandling may also be responsible for soil contamination, water pollution (both groundwater and surface water), injuries and death of ecofriendly microbes (Datta et al. 2018 ). Incineration is one of the preferred options for the waste management especially biomedical (or infectious) wastes in developed countries as shown in Fig. 6 .

Proportion of incineration for energy recovery in developed countries before COVID-19 pandemic
From the above figure, it is visible that Japan used to treat municipal solid waste through 74% incineration, 17% recycling and only 3% as landfill disposal before the pandemic (Mollica and Balestieri 2020 ). In Wuhan (China), normally 40 tons of biomedical waste was generated every day and after COVID-19 infections, it was reached up to 240 tons/day. Therefore, the increase in infectious wastes was around 6 times more as compared to normal days. This huge bulk of medical waste created big challenge to the management authorities as Wuhan administration could incinerate only 49 tons (maximum) of waste every day. Moreover, this will not be economical for any country as the costs of incineration for hazardous and municipal solid wastes in China were calculated as 281.7–422.6 USD/tons and 14.1 USD/tons, respectively (Tang 2020 ; Klemeš et al. 2020 ). According to WHO ( 2017 ), usually, 85% biomedical wastes are not hazardous in nature, rest 10% may be infectious along with 5% radioactive wastes. Before pandemic, except USA (12.7% only) (United States Environmental Protection Agency 2017 ), many developed countries incinerate their waste materials to recover energy such as 50% municipal waste incinerated in Denmark, Finland, Norway and Sweden (Istrate et al. 2020 ); 40% in Austria (Kyriakis et al. 2019 ); 76% in United Kingdom (DEFRA Government of UK 2020 ). However, recycling of the waste reported 32% in Austria (including composting) (Kyriakis et al. 2019 ); 45% in United Kingdom (DEFRA Government of UK 2020 ), and 35.2% in USA (both recycling and composting) (United States Environmental Protection Agency 2017 ). Therefore, it can be seen from the above results that collection and recycling of waste materials has been disturbed due COVID-19 pandemic. Moreover, pandemic has caused huge economical losses by many ways to the affected countries along with an unseen fear of its infections. Datta et al. ( 2018 ) studied that in India by the year 2017, 500 MT/day biomedical wastes were generated and infrastructure of managing biomedical waste is not good. Hence, based on the data of biomedical waste generated in Wuhan (> 6 times) during pandemic, India this situation is expected. However, till now biomedical waste generation data is not available for whole India (Somani et al. 2020 ). Further, according to one Indian leading newspaper in Gurugram (India), only in 2 months of pandemic, the quantity of biomedical wastes has increased around 40 times as compared to normal months. Similarly, before pandemic 550–600 kg biomedical waste was generated every day in Ahmadabad. Now, it has already increased up to 1000 kg/day during pandemic with an expectation of reaching up to 3000 kg/day especially in the red zones (COVID-19 containment zones (TOI 2020 ; Somani et al. 2020 ). Tables Tables1 1 and and2 2 shows the biomedical waste generation in some Asian cities and Indian cities/states.
Biomedical waste generation in Asian regions
| City/State | Additional medical waste generated (tons/day) | References |
|---|---|---|
| Manila (Philippines) | 280 | ADB ( ) |
| Jakarta (Indonesia) | 212 | ADB ( ) |
| Wuhan (China) | 210 | Tang ( ); Klemeš et al. ( ) |
| Bangkok (Thailand) | 210 | ADB ( ) |
| Hanoi (Vietnam) | 160 | ADB ( ) |
| Kuala Lumpur (Malaysia) | 154 | ADB ( ) |
| Ahmedabad | 0.4 | Somani et al. ( ) |
| National Capital Territory Delhi (India) | 349* | EPCA ( ) |
| Bhagpat, Gautambudh Nagar, Ghaziabad, Hapur, Meerut and Muzzafarnagar (Uttar Pradesh, India) | 247* | EPCA ( ) |
| Bhiwani, Charkhi Dadri, Faridabad, Gurgaon, Hisar, Jhajjar, Jind, Karnal, Mahendergarh, Panipat, Rewari, Sonipat and Rohtak (Haryana, India) | 162* | EPCA ( ) |
| Alwar, Bharatpur (Rajasthan, India) | 3.27* | EPCA ( ) |
*Total biomedical waste generated in the month of July, 2020
Biomedical waste generation in Indian states during pandemic. (
Source : Consolidated Status Report in the matter of O.A. NO. 72 of 2020 In re: Scientific Disposal of Bio-Medical Waste arising out of Covid-19 treatment—Compliance of BMWM Rules, 2016 before Hon’ble National Green Tribunal, Principle Bench, New Delhi) dated 17.06.2020
| City/State | Biomedical waste generation in Indian states during COVID-19 pandemic (June 2020) | |
|---|---|---|
| t/d | t/month | |
| Andaman and Nicobar Islands | 0.014 | 0.42 |
| Andhra Pradesh | 5.516 | 165.48 |
| Arunachal Pradesh | 0.112 | 3.36 |
| Assam | 0.946 | 28.38 |
| Bihar | 0.228 | 6.84 |
| Chandigarh | 0.995 | 29.85 |
| Chhattisgarh | 0.373 | 11.19 |
| Dadar Nagar Haveli | 0.015 | 0.45 |
| Delhi | 11.114 | 333.42 |
| Goa | 0.027 | 0.81 |
| Gujarat | 11.693 | 350.79 |
| Haryana | 2.511 | 75.33 |
| Himachal Pradesh | 0.127 | 3.81 |
| Jammu and Kashmir | 0.357 | 10.71 |
| Jharkhand | Information not provided | – |
| Karnataka | 2.8 | 84 |
| Kerala | 4.71 | 141.3 |
| Lakshadweep | 0.01 | 0.3 |
| Madhya Pradesh | 7.486 | 224.58 |
| Maharashtra | 17.494 | 524.82 |
| Manipur | 0.171 | 5.13 |
| Meghalaya | 0.17 | 5.1 |
| Mizoram | 0.14 | 4.2 |
| Nagaland | 0.12 | 3.6 |
| Odisha | 1.062 | 31.86 |
| Puducherry | 0.621 | 18.63 |
| Punjab | 1.6 | 48 |
| Rajasthan | 5.9 | 177 |
| Sikkim | 0.2 | 6 |
| Tamil Nadu | 10.41 | 312.3 |
| Telengana | 0.41 | 12.3 |
| Tripura | 0.015 | 0.45 |
| Uttarakhand | 0.53 | 15.9 |
| Uttar Pradesh | 7 | 210 |
| West Bengal | 6.5 | 195 |
| Total | 101 | 3030 |
From Table Table1, 1 , it can be seen that around every Asian city, the quantity of biomedical wastes has been increased many folds during the outbreak of COVID-19 in the community. In terms of maximum additional biomedical waste was generated in the capital of Philippines, i.e., Manila followed by Jakarta (Indonesia). In, Wuhan (China) and Bangkok (Thailand), 210 tons of additional biomedical waste was generated amid COVID-19 pandemic (ADB 2020 ). Improper medical waste handling may increase the number of COVID-19 infections in the community (Peng et al. 2020 ) due to presence of pathogenic microbes (Windfeld and Brooks 2015 ). Due to airborne infections of the COVID-19 virus in healthy people, use of masks, gloves, face cover etc. has been also increased up to dangerous levels in the world (Bourouiba 2020 ). At global level, 89 million masks and 76 million gloves are required against the protection from COVID-19 infection (WHO 2020c ). According to UNEP ( 2020 ), appropriate management of extra waste materials generated during COVID-19 pandemic has become a major concern for the countries. Therefore, medical wastes from the COVID-19 affected zones/hospitals need to be disinfected with careful handling. Treatment of medical waste can be carried out by using thermal techniques such as autoclaving, incineration, microwave and plasma method. However, selection above processes of waste treatment will be governed by many factors like economic feasibility, easy and safe handling, eco-friendly nature as well as harmless to the society (Liu et al. 2015 ). In order to reduce the chance of infection in the community, effective medical waste (or infectious waste) management should be adapted. Apart from collection and transport, trained manpower should be involved in this activity and disinfection of infectious waste should be compulsory (Klemeš et al. 2020 ).
The waste management as well as waste recycling process of the developed nations has been disturbed due to this COVID-19 outbreak. Figure 7 shows the waste management practices adapted by developed countries.

Management practices for solid wastes in some developed countries (ACRPlus 2020 ; Nghiem et al. 2020 ; Kulkarni and Anantharama 2020 ). (Reprinted from Kulkarni and Anantharama 2020 with permission from Elsevier)
From Fig. 7 , it can be seen that in developed countries waste management practice involves segregation of the waste at the source of generation followed by their effective collection, transpiration, treatment and disposal. However, during COVID-19 outbreak, the waste collection guidelines were changed as segregation and collection of the wastes from the infected area is carried out after a waiting period of 72 h (ACRPlus 2020 ; Nghiem et al. 2020 ). In most of the Asian countries like Bangladesh, India, Indonesia, Malaysia, Myanmar and Thailand, municipal solid wastes are getting managed by land-filling (Yadav and Samadder 2018 ). Integrated solid waste management system can be a good alternative for the recycling of wastes and also producing energy from the waste materials (Ramachandra et al. 2018 ). Lack of scientific designing of land-fill sites for waste disposal may lead several environmental problems such as air pollution, water pollution, soil pollution, marine pollution and vector borne-diseases among humans (Pujara et al. 2019 ). Therefore, mishandling of the biomedical wastes will be more dangerous as it may cause infections in the living organisms.
Biomedical waste management is a big challenge for every country especially during this pandemic time. According to the WHO, most of the developing countries do not have advanced systems for the management of biomedical wastes (Chartier et al. 2014 ). Chartier et al. ( 2014 ) proposed a close pit (as shown in Fig. 8 a) which should have a dimension of 2 m and 3 m and can be made by clay or geo-synthetic materials used at the base. This arrangement can be used for the safe management of biomedical wastes in emergency situations such as COVId-19 pandemic.

a Layout of a pit for onsite disposal of biomedical wastes in low-income countries during COVID-19 like emergency situation (Chartier et al. 2014 ; Sharma et al. 2020 ). (Reprinted from Sharma et al. 2020 with permission from Elsevier). b COVID-19 infected waste handling procedure for low income countries
Figure 8 a gives a temporary arrangement for the effective and safe disposal of biomedical wastes in low-income countries (Chartier et al. 2014 ; Sharma et al. 2020 ). Further, Fig. 8 b can be adopted during the handling infected hospital wastes.
Figure 8 b gives a detail outline for the management of infected wastes generated during the pandemic like COVID-19. In this diagram, it can be seen that disinfection of hospital waste has become very important as recommended by many government authorities of the world. For disinfection, autoclaving and sterilization of the tools can be carried out at the temperature ranged between 121 and 149 °C or with the spraying of 0.1% of NaClO. After, disinfection processes, the medical wastes can be shredded and incinerated (~ 1000 °C temperature) followed by ultimate disposal in landfills. Further, incineration has been considered as the best method for the treatment of hazardous wastes (e.g. medical wastes) as it will condense the weight along with volume of the wastes (Rajor et al. 2012 ). Even, US Environmental Protection Agency (USEPA 2020 ) issued special guidelines for managing food wastes of residential colonies and other commercial buildings during pandemic. Similarly, Government of India issued guidelines for the management of waste products generated during sudden lockdown. These wastes included perishable agricultural products as well (FAO 2020 ). According to Klemeš et al. ( 2020 ), environment and human health can be protected well after appropriate waste management. Hospital or infectious wastes can be managed effectively through proper collection, transport, treatment and final disposal. It also requires trained health workers who should be aware about the proper disinfection process along with self-protection too. Wasted PPE kits volume can also be decreased, if these materials (like antiviral masks, face shields etc.) can be reused after disinfections (Goel et al. 2020 ).Previously, viral disinfection was achieved by using UV-C rays (at 254 nm) in 40 min (Darnell et al. 2004 ), but in case of COVID-19, it is a matter of exploration. Moreover, it was also reported that UV-C rays can lead skin and eye disorders. Therefore, it must be examined before suggesting the application of UV-C rays as a disinfectant (Goel et al. 2020 ).Thermal treatment of waste can be an alternative for their management as it will generate energy along with reducing waste volume by 80–95%, and mineralization etc. (Singh et al. 2011 ; Brunner and Rechberger 2015 ; World Bank 2018 ). Implementation of these technologies were successful in some developed and developing countries and land-filling has become a rare practice in the developed nations because of land scarcity or/and environmental pollutions. Further, due to high investments, in developing countries it is still inaccessible (Mayer et al. 2019 ). Apart from the above advantages, incineration generates the ash residues which may contain toxic metals etc. Similarly, groundwater contamination may happen due to the disposal of such residues in the landfills (Rajor et al. 2012 ). Dargaville et al. ( 2020 ) recommended some steps to reduce the wastage of PPE kits which includes:
- To explore the possibility of recycling of PPE kits (gloves, mask, face shield etc.);
- Disinfection should be ensured before recycling
- One of the best disinfection methods should be shared with everyone (especially medical workers)
- Material’s properties should be examined before recycling
- Fix the guidelines for their number of recycling
- Exchange of recycled materials should not be allowed
- Time to time expert’s (material science, clinical doctors, virologist etc.) guidelines should be shared.
These are the general guidelines to be followed everywhere to reduce the quantity of medical wastes along with the human health and environmental protections (Dargaville et al. 2020 ).According to WHO, thermal treatment and/or application of conventional biocidal materials can be integrated with waste treatment systems for inactivating Coronavirus before the disposal of biomedical wastes (Kampf et al. 2020 ). Apart from these options of biomedical waste management; some extra efforts are needed to upgrade the existing waste management systems so that it can deal with emergency situations like this pandemic (COVID-19).
Some challenges observed as wastes are also generated from the mildly infected or asymptomatic people that may have viral infections. COVID-19 virus can be present in active form for different time periods (few hours to days) on the cardboards, plastic materials and metallic objects (Kampf et al. 2020 ; Doremalen et al. 2020 ; Nghiem et al. 2020 ). Somani et al. ( 2020 ) observed other waste materials which may be considered as infectious in nature, if not treated properly. These wastes are syringe, needles, masks, gloves, medicines, discarded materials from the home quarantine patients etc. Mishandling of these wastes may trigger the chance of more infections in public as well as health workers (Sharma et al. 2020 ; Kulkarni and Anantharama 2020 ).Further studies have shown that in between 21 and 23 °C temperature in presence of 40% relative humidity, the survival time of Coronavirus was 7 days. However, in atmosphere, with 65% relative humidity the activation time was drastically reduced up to 3 h with same temperature range (Doremalen et al. 2020 ). Kampf et al. ( 2020 ) reported 9 days active period of Coronavirus on the metal, glass or plastic. Further, Chin et al. ( 2020 ) found that at 70 °C, COVID-19 virus did not survive more than 5 min. National Biodefense Analysis and Countermeasures Centre, USA found in the initial studies that direct sunlight can be very effective to inactivate the Coronavirus within minutes from the many surfaces (Goel et al. 2020 ). Better management of the wastes can be carried out by optimizing the decision process, infrastructure, upgrading treatment methods and other activities related with the biological disasters like COVID-19 (Klemeš et al. 2020 ).
Provisions for biomedical waste management in India amid COVID-19
According to Bio-Medical Waste Management Rules, 2016 passed by Indian parliament data of biomedical waste generation should be updated on daily basis by the health care service providers and also, they must expose monthly information on their website (BMWM 2016 ). These rules were amended at time to time as per the need of the hour to make the effective biomedical waste management in the country. Amid COVID-19 pandemic, like other countries, Indian government has also taken many initiations for the purpose of quarantine, isolation, sampling, laboratory works etc. These initiatives were in agreement with the guidelines of various international (WHO, CDC etc.) and national agencies (MoH&FW, ICMR, CPCB etc.) such as application of separate colour storage basket or double layered bags with proper labelling, separate collection for biomedical wastes etc. During COVID-19 pandemic, some activities were recommended for the rapid and effective waste management by the Indian government to reduce the chance of further infections such as use PPE kits especially by the health workers/waste management people, providing training for their safety, record maintenance, extra working times for treatment facilities etc. (Soni 2020 ). CPCB has developed a mobile app, i.e., ‘COVID19BWM’ for the daily updation of the generation of biomedical wastes from COVID-19 related places. Moreover, 0.5% chlorine solution was recommended for the disinfection purpose where the patients wards. However, COVID-19 waste and their storage places should be disinfected with 1% sodium hypochlorite solution on daily basis (CPCB 2020b ). These guidelines were revised again (on July 17, 2020) and some significant amendments were carried out to fight with the COVID-19 virus such as rail coaches can also be used as isolation wards the materials used by COVID-19 patients included in the category of biomedical waste and their treatment should be mandatory as per the guidelines provided by CPCB and yellow bags can be used for their collection. It was mandatory that do not mix the municipal solid wastes with the waste generated from the COVID-19 infected places/homes (CPCB 2020c ). There, it can be said that despite of being a developing nation, Indian authorities are also doing lots of efforts to reduce the numbers of COVID-19 infections in the community.
Amid COVID-19, world has gone under environmental reformation in terms of clean rivers and blue skies, whereas, this pandemic has hurdled the appropriate solid waste management process and the same has emerged as a big threat for the world especially to the developing nations. Researchers have suggested some steps to reduce the wastage of biomedical waste and explored the mechanisms of safe and hygienic recycling. As advised by the WHO, developing countries, who are deficient of advanced systems for the management of biomedical wastes should follow the temporary solution of a close pit with a dimension of 2 m and 3 m and can be made by clay or geo-synthetic materials used at the base and the same arrangement can be used for the safe management of biomedical wastes in emergency situations such as COVId-19 pandemic wastes in emergency situations. The paper summarizes that better management of the wastes can be carried out by optimizing the decision process, infrastructure, upgrading treatment methods and other activities related with the biological disasters like COVID-19. National Biodefense Analysis and Countermeasures Centre, USA found in the initial studies that direct sunlight can be very effective to inactivate the Coronavirus within minutes from the many surfaces. Hospital or infectious wastes can be managed effectively through proper collection, transport, treatment and final disposal. The health workers must be trained enough and should be aware about the proper disinfection process along with self-protection too. Wasted PPE kits volume can also be decreased by reusing the same after disinfections. As achieved in the past for viral disinfection, the use of UV-C rays with proper precautions can also be explored for COVID-19 disinfection. Waste management especially for biomedical waste management, thermal treatment of waste can be an alternative, as it can generate energy along with reducing waste volume by 80–95%.
Acknowledgements
The authors wish to thank all who assisted in conducting this work.
Declarations
The authors declare that they do not have any personal or financial conflict of interests.
- ACRPlus-Association of Cities and Regions for Sustainable Resource Management (2020) Municipal waste management and COVID-19. https://www.acrplus.org/en/municipal-waste-management-covid-19 . Accessed 4 May 2020
- ADB (2020) Asian Development Bank. Managing infectious medical waste during the COVID-19 pandemic. https://www.adb.org/sites/default/files/publication/578771/managingmedical-waste-covid19.pdf . accessed 4 May 2020
- Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2020 doi: 10.1007/s11469-020-00270-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Amanat F, Krammer F. SARS-CoV-2 vaccines: status report. Immunity. 2020; 52 (4):83–589. doi: 10.1016/j.immuni.2020.03.007. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- American Society of Microbiology (2020). https://asm.org/PressReleases/2020/COVID-19 . Accessed Aug 10 2021
- Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020; 395 (10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ardakani AA, Kanafi AR, Acharya UR, Khadem N, Mohammadi A. Application of deep learning technique to manage COVID-19 in routine clinical practice using CT images: results of 10 convolutional neural networks. Comput Biol Med. 2020; 30 :103795. doi: 10.1016/j.compbiomed.2020.103795. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020; 5 (5):e256. doi: 10.1016/S2468-2667(20)30061-X. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Atalan A. Perspective—Is the lockdown important to prevent the COVID-19 pandemic? Effects on psychology, environment and economy-perspective. Ann Med Surg. 2020; 56 :38–42. doi: 10.1016/j.amsu.2020.06.010. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Balachandar V, Kaavya J, Mahalaxmi I, Arul N, Vivekanandhan G, Bupesh G, Singaravelu G, Anila V, Dhivya V, Harsha G, Kamarajan R. COVID-19: a promising cure for the global panic. Sci Total Environ. 2020; 725 :138277. doi: 10.1016/j.scitotenv.2020.138277. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bhatia A, Bhaskar S (2020) Coronavirus outbreak explained: are air conditioners safe to use during the COVID-19 pandemic. NDTV. https://swachhindia.ndtv.com
- BMWM (2016) Bio-medical waste management rules, 2016. Ministry of Environment, Forest & Climate Change, Delhi – 110032, India. Dated 19 Feb 2020
- Bourouiba L. Turbulent gas clouds and respiratory pathogen emissions. Potential implications for reducing transmission of COVID-19. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.4756. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bremer S, Schneider P, Glavovic B. Climate change and amplified representations of natural hazards in institutional cultures. Oxf Res Encycl Nat Hazard Sci. 2019 doi: 10.1093/acrefore/9780199389407.013.354. [ CrossRef ] [ Google Scholar ]
- Brunner PH, Rechberger H. Waste to energy—key element for sustainable waste management. Waste Manag. 2015; 37 :3–12. doi: 10.1016/j.wasman.2014.02.003. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Callaway E, Cyranoski D, Mallapaty S, Stoye E, Tollefson J. Coronavirus by the numbers. Nature. 2020; 579 :482. doi: 10.1038/d41586-020-00758-2. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Calma J (2020) https://www.theverge.com/2020/3/26/21194647/the-covid-19-pandemic-is-generating-tons-of-medical-waste
- Casanova L, Rutala WA, Weber DJ, Sobsey MD. Survival of surrogate coronaviruses in water. Water Res. 2009; 43 (7):1893–1898. doi: 10.1016/j.watres.2009.02.002. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Napoli RD. Features, evaluation and treatment Corona Virus (COVID-19), NCBI Bookshelf. Treasure Island, FL: StatPearls Publishing; 2020. [ Google Scholar ]
- CDC (2020) https://www.ecdc.europa.eu/sites/default/files/documents/RRA-sixth-updateOutbreak-of-novel-coronavirus-disease-2019-COVID-19.pdf . Accessed 5 July 2020
- Chakraborty I, Maity P. COVID-19 outbreak: migration, effects on society, global environment and prevention. Sci Total Environ. 2020; 728 :138882. doi: 10.1016/j.scitotenv.2020.138882. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chan WC. Nano research for COVID-19. ACS Nano. 2020; 14 (4):3719–3720. doi: 10.1021/acsnano.0c02540. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chartier Y, Emmanuel J, Pieper Ute PA, Philip R, Ruth S, William T, Wilburn S, Zghondi R. Safe management of wastes from health-care activities. Geneva: WHO; 2014. [ Google Scholar ]
- Chen K, Wang M, Huang C, Kinney PL, Anastas PT. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health. 2020; 4 (6):e210–e212. doi: 10.1016/S2542-5196(20)30107-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chin AW, Chu JT, Perera MR, Hui KP, Yen HL, Chan MC, Peiris M, Poon LL. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe. 2020; 1 (1):10. doi: 10.1016/S2666-5247(20)30003-3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Corletta RT, Primack RB, Devictor V, Maasd B, Goswami VR, Bates AE, Koh LP, Regani TJ, Loyolaj R, Pakemanl RJ, Cummingm GS, Pidgeon A, Johns D, Roth R. Impacts of the coronavirus pandemic on biodiversity conservation. Biol Conserv. 2020; 246 :108571. doi: 10.1016/j.biocon.2020.108571. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- CPCB (2020a) Report on assessment of impact of lock down on water quality of river Yamuna- Delhi stretch. Central Pollution Control Board, Ministry of Environment, Forests and Climate Change, Delhi – 110032
- CPCB (2020b) Guidelines for handling, treatment, and disposal of waste generated during treatment/diagnosis/quarantine of COVID-19 patients—Rev. 3, dated 10 June 2020b. Central Pollution Control Board, (Ministry of Environment, Forest & Climate Change), Delhi – 110032, India
- CPCB (2020c) Guidelines for handling, treatment and disposal of waste generated during treatment/diagnosis/quarantine of COVID-19 patients—Rev. 4, dated 17 July 2020c. Central Pollution Control Board, (Ministry of Environment, Forest & Climate Change), Delhi – 110032, India
- Dantas G, Siciliano B, França BB, da Silva CM, Arbilla G. The impact of COVID-19 partial lockdown on the air quality of the city of Rio de Janeiro, Brazil. Sci Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.139085. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dargaville T, Spann K, Celina M. Opinion to address a potential personal protective equipment shortage in the global community during the COVID-19 outbreak. Polymer Degrad Stab. 2020; 176 :109162. doi: 10.1016/j.polymdegradstab.2020.109162. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Darnell ME, Subbarao K, Feinstone SM, Taylor DR. Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV. J Virol Methods. 2004; 121 (1):85–91. doi: 10.1016/j.jviromet.2004.06.006. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Datta P, Mohi GK, Chander J. Biomedical waste management in India: critical appraisal. J Lab Physicians. 2018; 10 (1):6–14. doi: 10.4103/JLP.JLP_89_17. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- DEFRA-Department for Environment Food & Rural Affairs, Government of UK (2020) UK statistics on waste. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/874265/UK_Statistics_on_Waste_statistical_notice_March_2020_accessible_FINAL_rev_v0.5.pdf
- Dhama K, Sharun K, Tiwari R et al (2020) Coronavirus disease 2019—COVID-19. Preprints. 10.20944/preprints202003.0001.v1
- Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, Wit E, Munster VJ. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. N Engl J Med. 2020 doi: 10.1101/2020.03.09.20033217. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychol. 2020; 7 (4):300–302. doi: 10.1016/S2215-0366(20)30073-0. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Elavarasan RM, Pugazhendhi R. Restructured society and environment: a review on potential technological strategies to control the COVID-19 pandemic. Sci Total Environ. 2020; 725 :138858. doi: 10.1016/j.scitotenv.2020.138858. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- EPCA (2020) The Environment Pollution (Prevention and Control) Authority (EPCA). https://www.epca.org.in/EPCA-Reports1999-1917/EPCA-reportno-112.pdf . Accessed on 17 Dec 2020
- Fan VY, Jiang P, Hemzal M, Klemeš JJ. An update of COVID-19 influence on waste management. Sci Total Environ. 2021; 754 :142014. doi: 10.1016/j.scitotenv.2020.142014. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- FAO (2020) Food and Agriculture Organization of the United Nations. Local food systems and COVID-19; a glimpse on India's responses. http://www.fao.org/in-action/foodfor-cities-programme/news/detail/en/c/1272232/
- Ferronato N, Torretta V. Waste mismanagement in developing countries: a review of global issues. Int J Environ Res Public Health. 2019; 16 (6):1060. doi: 10.3390/ijerph16061060. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ford T, Vizard T, Sadler K, et al. Data resource profile: the mental health of children and young people surveys (MHCYP) Int J Epidemiol. 2020 doi: 10.1093/ije/dyz259. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gardiner B (2020) Pollution made COVID-19 worse. Now, lockdowns are clearing the air. National Geographic. https://www.nationalgeographic.com/science/2020/04/pollution-made-the-pandemic-worse-but-lockdowns-clean-the-sky/ . Accessed 15 May 2020
- Gates B. Responding to Covid-19—a once-in-a-century pandemic? N Engl J Med. 2020; 382 (18):1677–1679. doi: 10.1056/NEJMp2003762. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Global Climate report (2019) https://www.ncdc.noaa.gov/sotc/global/201913
- Goel S, Hawi S, Goel G, Thakur VK, Agrawal A, Hoskins C, Pearce O, Hussain T, Upadhyaya HM, Cross G, Barber AH. Resilient and agile engineering solutions to address societal challenges such as coronavirus pandemic. Mater Today Chem. 2020; 17 :100300. doi: 10.1016/j.mtchem.2020.100300. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Silver RC, Everall I, Ford T. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020; 7 :547–560. doi: 10.1016/S2215-0366(20)30168-1. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hopman J, Allegranzi B, Mehtar S. Managing COVID-19 in low-and middle-income countries. JAMA. 2020; 323 (16):1549–1550. doi: 10.1001/jama.2020.4169. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020; 395 (10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Istrate I-R, Iribarren D, Galvez-Martos J-L, Dufour J. Review of life-cycle environmental consequences of waste-to-energy solutions on the municipal solid waste management system. Resour Conser Recov. 2020; 157 :104778. doi: 10.1016/j.resconrec.2020.104778. [ CrossRef ] [ Google Scholar ]
- Kahlert S, Bening CR. Plastic recycling after the global pandemic: resurgence or regression? Resour Conserv Recycl. 2020; 160 :104948. doi: 10.1016/j.resconrec.2020.104948. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020; 104 :246–251. doi: 10.1016/j.jhin.2020.01.022. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Katariya M (2020) 10 Things that have happened for the first time in years during the coronavirus lockdown. Scoopwhoop, https://www.scoopwhoop.com/news/things-that-have-happened-for-the-first-time-inyearsduring-coronavirus-lockdown/
- Kaufman L, Chasan E (2020) Cities wonder whether recycling counts as essential during the virus. Bloomberg Green. https://www.bloomberg.com/news/articles/2020-03-27/cities-wonder-whether-recycling-counts-as-essential-during-the-virus . Accessed 26 April 2020
- Kerimray A, Baimatova N, Ibragimova OP, Bukenov B, Kenessov B, Plotitsyn P, Karaca F. Assessing air quality changes in large cities during COVID-19 lockdowns: the impacts of traffic-free urban conditions in Almaty, Kazakhstan. Sci Total Environ. 2020; 730 :139179. doi: 10.1016/j.scitotenv.2020.139179. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Klemeš JJ, Van Fan Y, Tan RR, Jiang P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew Sustain Energy Rev. 2020; 127 :109883. doi: 10.1016/j.rser.2020.109883. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kulkarni BN, Anantharama V. Repercussions of COVID-19 pandemic on municipal solid waste management: challenges and opportunities. Sci Total Environ. 2020; 743 :140693. doi: 10.1016/j.scitotenv.2020.140693. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kyriakis E, Psomopoulos C, Kalkanis K. Investigating the correlation of purchase power parity with the adopted waste management method in EU28. J Soc Sci. 2019; 8 :162. doi: 10.3390/socsci8050162. [ CrossRef ] [ Google Scholar ]
- Lee PI, Hu YL, Chen PY, Huang YC, Hsueh PR. Are children less susceptible to COVID-19? J Microbiol Immunol Infect. 2020 doi: 10.1016/j.jmii.2020.02.011. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu HC, You JX, Lu C, Chen YZ. Evaluating health-care waste treatment technologies using a hybrid multi-criteria decision making model. Renew Sustain Energy Rev. 2015; 41 :932–942. doi: 10.1016/j.rser.2014.08.061. [ CrossRef ] [ Google Scholar ]
- Lokhandwala S, Gautam P. Indirect impact of COVID-19 on environment: a brief study in Indian context. Environ Res. 2020; 188 :109807. doi: 10.1016/j.envres.2020.109807. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mahajan P, Kaushal J. Epidemic trend of COVID-19 transmission in India during lockdown-1 phase. J Commun Health. 2020 doi: 10.1007/s10900-020-00863-3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mahato S, Pal S, Ghosh KG. Effect of lockdown amid COVID-19 pandemic on air quality of the megacity Delhi, India. Sci Total Environ. 2020; 730 :139086. doi: 10.1016/j.scitotenv.2020.139086. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mallapur C (2020) Sanitation workers at risk from discarded medical waste related to COVID-19. IndiaSpend. https://www.indiaspend.com/sanitation-workersat-risk-from-discarded-medical-waste-related-tocovid-19/
- Mayer F, Bhandari R, Gath S. Critical review on life cycle assessment of conventional and innovative waste-to-energy technologies. Sci Total Environ. 2019; 672 :708–721. doi: 10.1016/j.scitotenv.2019.03.449. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ministry of Health and Family Welfares (MoHFW), Government of India (2020) COVID-19 INDIA. https://www.mohfw.gov.in/
- Mishra RK, Parida M, Rangnekar S. Evaluation and analysis of traffic noise along bus rapid transit system corridor. Int J Environ Sci Technol. 2010; 7 (4):737–750. doi: 10.1007/BF03326183. [ CrossRef ] [ Google Scholar ]
- Mollica GJG, Balestieri JAP. Is it worth generating energy with garbage? Defining a carbon tax to encourage waste-to-energy cycles. Appl Therm Eng. 2020; 173 :115195. doi: 10.1016/j.applthermaleng.2020.115195. [ CrossRef ] [ Google Scholar ]
- Myllavirta L, Dahiya S (2020) Analysis: India's CO2 emissions fall for first time in four decades amid coronavirus. Carbon Brief, https://www.carbonbrief.org/analysis-indias-co2-emissions-fall-for-first-time-in-four-decades-amidcoronavirus#
- National Aeronautics and Space Administration (NASA) (2020) Airborne particle levels plummet in Northern India. Retrieved on 11 May 2020 from https://earthobservatory.nasa.gov/images/146596/airborne-particle-levels-plummet-innorthern-india
- National Environment Agency Singapore (2020)Waste management-public waste collection services during circuit breaker. https://www.nea.gov.sg/our-services/wastemanagement/overview .
- Nghiem LD, Morgan B, Donner E, Short MD. The COVID-19 pandemic: considerations for the waste and wastewater services sector. Case Stud Chem Environ Eng. 2020 doi: 10.1016/j.cscee.2020.100006. [ CrossRef ] [ Google Scholar ]
- Occupational Safety and Health Administration (OSHA) (2020) Guidance on Preparing Workplaces for COVID-19
- Paital B, Das K, Parida SK. Review-Inter nation social lockdown versus medical care against COVID-19, a mild environmental insight with special reference to India. Sci Total Environ. 2020; 728 :138914. doi: 10.1016/j.scitotenv.2020.138914. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peng L, Liu J, Xu W, Luo Q, Chen D, Lei Z, Huang Z, Li X, Deng K, Lin B, Gao Z. SARS-CoV-2 can be detected in urine, blood, anal swabs, and oropharyngeal swabs specimens. J Med Virol. 2020 doi: 10.1002/jmv.25936. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Polk HS. State of global air 2019: a special report on global exposure to air pollution and its disease burden. Boston, MA: Health Effects Institute; 2019. [ Google Scholar ]
- Pujara Y, Pathak P, Sharma A, Govani J. Review on Indian Municipal Solid Waste Management practices for reduction of environmental impacts to achieve sustainable development goals. J Environ Manage. 2019; 248 :109238. doi: 10.1016/j.jenvman.2019.07.009. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Qu G, Li X, Hu L, Jiang G. An imperative need for research on the role of environmental factors in transmission of novel coronavirus (COVID-19) Environ Sci Technol. 2020; 54 :3730–3732. doi: 10.1021/acs.est.0c01102. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rahman MM, Bodrud-Doza M, Griffiths MD, Mamun MA. Biomedical waste amid COVID-19: perspectives from Bangladesh. Lancet Glob Health. 2020; 8 (10):e1262. doi: 10.1016/S2214-109X(20)30349-1. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rajor A, Xaxa M, Mehta R. An overview on characterization, utilization and leachate analysis of biomedical waste incinerator ash. J Environ Manage. 2012; 108 :36–41. doi: 10.1016/j.jenvman.2012.04.031. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ramachandra TV, Bharath HA, Kulkarni G, Han SS. Municipal solid waste: generation, composition and GHG emissions in Bangalore, India. Renew Sustain Energy Rev. 2018; 82 :1122–1136. doi: 10.1016/j.rser.2017.09.085. [ CrossRef ] [ Google Scholar ]
- Randall I (2020) Sound of the sea: underwater noise pollution from ships plummets during the coronavirus lockdown offering respite for 'stressed' whales and other marine life. The Daily Mail. https://mol.im/a/8262147
- Rodriguez-Morales A, Tiwari R, Sah R, Dhama K. COVID-19, an emerging coronavirus infection: current scenario and recent developments—an overview. J Pure Appl Microbiol. 2020; 14 :6150. doi: 10.22207/JPAM.14.1.02. [ CrossRef ] [ Google Scholar ]
- Rosenbloom D, Markard J. A COVID-19 recovery for climate. Science. 2020; 368 (6490):447. doi: 10.1126/science.abc4887. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roujian L, Xian Z, Juan L, et al. Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020; 395 :565–574. doi: 10.1016/S0140-6736(20)30251-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shammi M, Bodrud-Doza M, Islam ARMT, Rahman MM. COVID-19 pandemic, socioeconomic crisis and human stress in resource-limited settings: a case from Bangladesh. Heliyon. 2020; 6 :e04063. doi: 10.1016/j.heliyon.2020.e04063. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sharma HB, Vanapalli KR, Cheela VS, Ranjan VP, Jaglan AK, Dubey B, Goel S, Bhattacharya J. Challenges, opportunities, and innovations for effective solid waste management during and post COVID-19 pandemic. Resour Conser Recycl. 2020; 162 :105052. doi: 10.1016/j.resconrec.2020.105052. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Singh RP, Tyagi VV, Allen T, Ibrahim M, Kothari R. An overview of exploring the possibilities of energy generation from municipal solid waste (MSW) in Indian scenario. Renew Sustain Energy Rev. 2011; 15 :4797–4808. doi: 10.1016/j.rser.2011.07.071. [ CrossRef ] [ Google Scholar ]
- Singh AK, Singh A, Shaikh A, Singh R, Misra A. Chloroquine and hydroxychloroquine in the treatment of COVID-19 with or without diabetes: a systematic search and a narrative review with a special reference to India and other developing countries. Diab Metab Syndr Clin Res Rev. 2020; 14 :241–246. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sinha SN, Paul D, Biswas K. Effects of Moringaoleifera Lam. and Azadirachtaindica A. Juss. leaf extract in treatment of tannery effluent. Our Nat. 2016; 14 :47–53. doi: 10.3126/on.v14i1.16440. [ CrossRef ] [ Google Scholar ]
- Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, Iosifidis C, Agha R. Review- World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020; 76 :71–76. doi: 10.1016/j.ijsu.2020.02.034. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Somani M, Srivastava AN, Gummadivalli SK, Sharma A. Indirect implications of COVID-19 towards sustainable environment: an investigation in Indian context. Bioresour Technol Rep. 2020; 11 :100491. doi: 10.1016/j.biteb.2020.100491. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Soni DK. Regulatory interventions in Covid-19 waste management in India. Natl J Life Sci. 2020; 17 (1):5–7. doi: 10.51365/NJLS.2020.v17i01.002. [ CrossRef ] [ Google Scholar ]
- SWANA - Solid Waste Association of North America article (2020) SWANA reminds all state and local governments that solid waste management is an essential public service. https://swana.org/news/swana-news/article/2020/03/19/swana-reminds-allstate-and-localgovernments-that-solid-waste-management-is-an-essential-publicservice
- Tang W (2020) The medical waste related to COVID-2019 is cleaned up every day—the medical waste treatment market needs to be standardised. 21st Century Business Herald; 2020. www.21jingji.com/2020/3-12/xNMDEzODFfMTU0MjIxNQ.html
- Times of India (TOI) (2020) 350 Tonnes of trash disappear from streets of Ahmedabad. http://timesofindia.indiatimes.com/articleshow/75039037.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst
- UNEP (2020) BASEL: waste management an essential public service in the fight to beat COVID-19. The United Nations Environment Programme (UNEP) and The Basel Convention. http://www.basel.int/Implementation/PublicAwareness/PressReleases/WastemanagementandCOVID19/tabid/8376/Default.aspx
- United Nations Industrial Development Organization (UNIDO) (2020) India's manufacturing reels from the impact of COVID-19. https://www.unido.org/stories/indias-manufacturingreelsimpact-covid-19
- United Nations (2020) The Social Impact of COVID-19. Department of Economics and Social Affairs. https://www.un.org/development/desa/dspd/2020/04/social-impact-ofcovid-19
- United States Environmental Protection Agency (2020) Recycling and sustainable management of food during COVID-19 public health emergency. https://www.epa.gov/coronavirus/recycling-and-sustainable-management-food-duringcoronaviruscovid-19-public-health
- United States Environmental Protection Agency (2017) National overview: facts and figures on materials, wastes and recycling. https://www.epa.gov/facts-and-figuresabout-materials-waste-and-recycling/national-overview-facts-and-figures-materials . Accessed 10 May 2020.
- Vellingiri B, Jayaramayya K, Iyer M, Narayanasamy A, Govindasamy V, Giridharan B, Ganesan S, Venugopal A, Venkatesan D, Ganesan H, Rajagopalan K. COVID-19: a promising cure for the global panic. Sci Total Environ. 2020; 725 :138277. doi: 10.1016/j.scitotenv.2020.138277. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weber DJ, Rutala WA, Fischer WA, Kanamori H, Sickbert-Bennett EE. Emerging infectious diseases: focus on infection control issues for novel coronaviruses (Severe Acute Respiratory Syndrome-CoV and Middle East Respiratory Syndrome-CoV), hemorrhagic fever viruses (Lassa and Ebola), and highly pathogenic avian influenza viruses, A(H5N1) and A(H7N9) Am J Infect Control. 2016; 44 (5):E91–E100. doi: 10.1016/j.ajic.2015.11.018. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- WHO (2017) Report on health-care waste management (HCWM) status in Countries of the South-East Asia Region (SEA-EH-593). The World Health Organization. https://apps.who.int/iris/handle/10665/258761 .
- WHO (2018) World Health Organization. Global status report on alcohol and health. https://www.who.int/substance_abuse/publications/global_alcohol_report/en/ .
- WHO, 2020a. Pneumonia of unknown cause- China. World Health Organization.
- WHO (2020b) Coronavirus Disease (COVID-2019) Situation Reports-67. World Health Organization
- WHO (2020c) World Health Organization. WHO-Director-general-s-opening-remarks-at-the-media briefing-on-covid-19. www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19
- WHO (2020d) Water, sanitation, hygiene, and Waste Management For the COVID-19 virus: interim guidance, 23 April 2020d (No. WHO/2019-nCoV/IPC_WASH/2020.3).WorldHealth Organization URL. https://apps.who.int/iris/bitstream/handle/10665/331846/WHO-2019-nCoV-IPC_WASH-2020.3-eng.pdf . Accessed 30 April 2020.
- Windfeld ES, Brooks MS-L. Medical waste management—a review. J Environ Manag. 2015; 163 :98–108. doi: 10.1016/j.jenvman.2015.08.013. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, Niemeyer D, Jones TC, Vollmar P, Rothe C, Hoelscher M. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020; 581 (7809):465–469. doi: 10.1038/s41586-020-2196-x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Bank Urban Development Series (2018) Decision Maker’s Guides for Solid Waste Management Technologies.
- World Bank (2020) Waste workers are protecting our communities during COVID-19. https://blogs.worldbank.org/sustainablecities/waste-workers-are-protecting-ourcommunitiesduring-covid-19 . Accessed 11 May 2020.
- Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020; 92 (6):589–594. doi: 10.1002/jmv.25725. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Resp Med. 2020; 8 (4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yadav P, Samadder SR. A critical review of the life cycle assessment studies on solid waste management in Asian countries. J Clean Prod. 2018; 185 :492–515. doi: 10.1016/j.jclepro.2018.02.298. [ CrossRef ] [ Google Scholar ]
- Yunus AP, Masago Y, Hijioka Y. COVID-19 and surface water quality: improved lake water quality during the lockdown. Sci Total Environ. 2020; 731 :139012. doi: 10.1016/j.scitotenv.2020.139012. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zambrano-Monserrate MA, Ruano MA, Sanchez-Alcalde L. Indirect effects of COVID-19 on the environment. Sci Total Environ. 2020; 728 :138813. doi: 10.1016/j.scitotenv.2020.138813. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zhang W, Du RH, Li B, Zheng XS, Yang XL, Hu B, Wang YY, Xiao GF, Yan B, Shi ZL, Zhou P. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020; 9 (1):386–389. doi: 10.1080/22221751.2020.1729071. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382 :727–733. doi: 10.1056/NEJMoa2001017. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Assessment of knowledge, practice and attitude about biomedical waste management among healthcare professionals during covid-19 crises in al-ahsa.

1. Introduction
2. materials and methods, 2.1. study design, 2.2. study area and setting, 2.3. sample size and sampling method, 2.4. inclusion criteria, 2.5. data collection tool and procedure, 2.5.1. demographic information, 2.5.2. knowledge questionnaire, 2.5.3. practice questionnaire, 2.5.4. attitude scale, 2.6. ethical considerations, 2.7. statistical analysis, 3.1. demographic characteristics of the hcp, 3.2. knowledge level of the hcps on bmw management, 3.3. practice of hcps in bmw management, 3.4. attitude of the hcps towards bmw management, 3.5. association of the knowledge of hcps on bmw management with demographic variables, 4. discussion, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, acknowledgments, conflicts of interest, abbreviations.
| BMW | Biomedical waste |
| COVID-19 | Corona virus disease-19 |
| HCP | Health care professionals |
| IBM | International Business Machines Corporation |
| KPA | Knowledge, practice, and attitude |
| LT | Lab technicians |
| MOH | Ministry of Health |
| NS | Non-significant |
| PPE | Personal protective equipment |
| RT | Respiratory therapists |
| SD | Standard deviation |
| SPSS | Statistical Package for the Social Sciences |
| WHO | World Health Organization |
| WWF | World-wide Fund of Nature |
- Goswami, M.; Goswami, P.J.; Nautiyal, S.; Prakash, S. Challenges and actions to the environmental management of Bio-Medical Waste during COVID-19 pandemic in India. Heliyon 2021 , 7 , e06313. [ Google Scholar ] [ CrossRef ]
- Deress, T.; Hassen, F.; Adane, K.; Tsegaye, A. Assessment of knowledge, attitude, and practice about biomedical waste management and associated factors among the healthcare professionals at Debre Markos town healthcare facilities, northwest Ethiopia. J. Environ. Public Health 2018 , 7672981. [ Google Scholar ] [ CrossRef ]
- Lai, C.C.; Shih, T.P.; Ko, W.C.; Tang, H.J.; Hsueh, P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int. J. Antimicrob. Agents 2020 , 55 , 105924. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rao, D.; Dhakshaini, M.R.; Kurthukoti, A.; Doddawad, V.G. Biomedical Waste Management: A Study on assessment of knowledge, attitude and practices among health care professionals in a tertiary care teaching hospital. Biomed. Pharmacol. J. 2018 , 11 , 1737–1743. [ Google Scholar ] [ CrossRef ]
- Musa, F.; Mohamed, A.; Selim, N. Assessment of nurses’ practice and potential barriers regarding the medical waste management at Hamad medical corporation in Qatar: A cross-sectional Study. Cureus 2020 , 12 , e8281. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Thind, P.S.; Sareen, A.; Singh, D.D.; Singh, S.; John, S. Compromising situation of India’s bio-medical waste incineration units during pandemic outbreak of COVID-19: Associated environmental-health impacts and mitigation measures. Environ. Pollut. 2021 , 276 , 116621. [ Google Scholar ] [ CrossRef ]
- Shammi, M.; Behal, A.; Tareq, S.M. The escalating biomedical waste management to control the environmental transmission of COVID-19 pandemic: A perspective from two south Asian countries. Environ. Sci. Technol. 2021 , 55 , 4087–4093. [ Google Scholar ] [ CrossRef ]
- Yousefi, M.; Oskoei, V.; Jonidi Jafari, A.; Farzadkia, M.; Hasham Firooz, M.; Abdollahinejad, B.; Torkashvand, J. Municipal solid waste management during COVID-19 pandemic: Effects and repercussions. Environ. Sci. Pollut. Res. Int. 2021 , 3 , 1–10. [ Google Scholar ] [ CrossRef ]
- Ammendolia, J.; Saturno, J.; Brooks, A.L.; Jacobs, S.; Jambeck, J.R. An emerging source of plastic pollution: Environmental presence of plastic personal protective equipment (PPE) debris related to COVID-19 in a metropolitan city. Environ. Pollut. 2021 , 269 , 116160. [ Google Scholar ] [ CrossRef ]
- Khoironi, A.; Hadiyanto, H.; Anggoro, S.; Sudarno, S. Evaluation of polypropylene plastic degradation and microplastic identification in sediments at Tambak Lorok coastal area, Semarang, Indonesia. Mar. Pollut. Bull. 2020 , 151 , 110868. [ Google Scholar ] [ CrossRef ]
- Datta, P.; Mohi, G.K.; Chander, J. Biomedical waste management in India: Critical appraisal. J. Lab. Physicians 2018 , 10 , 6–14. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Bhagawati, G.; Nandwani, S.; Singhal, S. Awareness and practices regarding bio-medical waste management among health care workers in a tertiary care hospital in Delhi. Indian J. Med. Microbiol. 2015 , 33 , 580–582. [ Google Scholar ] [ CrossRef ]
- Mihai, F.C. Assessment of COVID-19 waste flows during the emergency state in Romania and related public health and environmental concerns. Int. J. Environ. Res. Public Health 2020 , 17 , 5439. [ Google Scholar ] [ CrossRef ]
- Yadavannavar, M.; Berad, A.S.; Jagirdar, P. Biomedical waste management: A study of knowledge, attitude, and practices in a tertiary health care institution in bijapur. Indian J. Community Med. 2010 , 35 , 170–171. [ Google Scholar ] [ CrossRef ]
- Parida, A.; Capoor, M.R.; Bhowmik, K.T. Knowledge, attitude, and practices of bio-medical waste management rules, 2016; bio-medical waste management (amendment) rules, 2018; and solid waste rules, 2016, among health-care workers in a tertiary care setup. J. Lab. Physicians 2019 , 11 , 292–299. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Shaheen, T.; Ghani, M.; Kausar, S. Gauging the effectiveness of training sessions among nurses regarding biomedical waste management: A quasi-experimental study from a developing country. Cureus 2020 , 12 , e12196. [ Google Scholar ] [ CrossRef ]
- Rashidian, A.; Alinia, C.; Majdzadeh, R. Cost-effectiveness analysis of health care waste treatment facilities in Iran hospitals; a provider perspective. Iran. J. Public Health 2015 , 44 , 352–360. [ Google Scholar ]
- Singh, S.; Dhillon, B.S.; Nityanand; Shrivastava, A.K.; Kumar, B.; Bhattacharya, S. Effectiveness of a training program about Cat a tertiary care teaching institute of North India. J. Educ. Health Promot. 2020 , 9 , 127. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nghiem, L.D.; Morgan, B.; Donner, E.; Short, M.D. The COVID-19 pandemic: Considerations for the waste and wastewater services sector. Case Stud. Chem. Environ. Eng. 2020 , 1 , 100006,. [ Google Scholar ] [ CrossRef ]
- Alshahrani, N.Z.; Alshaiban, H.M.; Alarbash, H.A.; Mahmood, S.E.; Aljunaid, M.A.; Albeshry, A.M.; Sayyad, Y. Knowledge, Attitude and Practices of Healthcare Workers regarding Bio-medical Waste of COVID-19 in Aseer Region, KSA. Int. J. Pharm. Res. 2021 , 13 . [ Google Scholar ] [ CrossRef ]
- Zhang, M.; Zhou, M.; Tang, F.; Wang, Y.; Nie, H.; Zhang, L.; You, G. Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. J. Hosp. Infect. 2020 , 105 , 183–187. [ Google Scholar ] [ CrossRef ]
- Mugabi, B.; Hattingh, S.; Chima, S.C. Assessing knowledge, attitudes, and practices of healthcare workers regarding medical waste management at a tertiary hospital in Botswana: A cross-sectional quantitative study. Niger J. Clin. Pract. 2018 , 21 , 1627–1638. [ Google Scholar ] [ CrossRef ]
- Letho, Z.; Yangdon, T.; Lhamo, C.; Limbu, C.B.; Yoezer, S.; Jamtsho, T.; Chhetri, P.; Tshering, D. Awareness and practice of medical waste management among healthcare providers in National Referral Hospital. PLoS ONE 2021 , 16 , e0243817. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Pandey, A.; Ahuja, S.; Madan, M.; Asthana, A.K. Bio-medical waste management in a tertiary care hospital: An overview. J. Clin. Diagn. Res. 2016 , 10 , DC01–DC03. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ilyas, S.; Srivastava, R.R.; Kim, H. Disinfection technology and strategies for COVID-19 hospital and bio-medical waste management. Sci. Total Environ. 2020 , 20 , 141652. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chethana, T.; Thapsey, H.; Gautham, M.S.; Sreekantaiah, P.; Suryanarayana, S.P. Situation analysis and issues in management of biomedical waste in select small health care facilities in a ward under Bruhat Bengaluru Mahanagara Palike, Bangalore, India. J. Community Health 2014 , 39 , 310–315. [ Google Scholar ] [ CrossRef ]
- Sunmeet, G.A.; Gangawane, A. Knowledge attitude and practices of healthcare personnel towards bio-medical waste disposal management at Arbor Biotech Limited Mumbai. Int. J. Innov. Res. Sci. Eng. 2017 , 3 , 307–316. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Aanandaswamy, T.C.; Rajappa, G.C.; Venkatachala, N.; Kamath, R. Assessment of knowledge, attitude, and practices regarding biomedical waste management among operation room personnel in a tertiary care center. J. Anaesthesiol. Clin. Pharmacol. 2019 , 35 , 106–108. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Akkajit, P.; Romin, H.; Assawadithalerd, M. Assessment of knowledge, attitude, and practice in respect of medical waste management among healthcare workers in clinics. J. Environ. Public Health 2020 , 8745472. [ Google Scholar ] [ CrossRef ]
- Sachan, R.; Patel, M.L.; Nischal, A. Assessment of the knowledge, attitude and practices regarding biomedical waste management amongst the medical and paramedical staff in tertiary health care centre. Int. J. Sci. Res. Public 2012 , 2 , 1–6. [ Google Scholar ]
- Albalushi, A.Y.; Ullah, M.; Makhamri, A.; Alalawi, F.; Khalid, M.; Alghafri, H. Knowledge, attitude and practice of biomedical waste management among health care personnel in a secondary care hospital of Al Buraimi Governorate, Sultanate of Oman. Glob. J. Health Sci. 2018 , 10 , 70. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Singh, T.; Ghimire, T.R.; Agrawal, S.K. Awareness of biomedical waste management in dental students in different dental colleges in Nepal. Biomed. Res. Int. 2018 , 1742326. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Bokhoree, C.; Beeharry, Y.; Makoondlall-Chadee, T.; Doobah, T.; Soomary, N. Assessment of environmental and health risks associated with the management of medical waste in mauritius. APCBEE Procedia 2014 , 9 , 36–41. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Kumar, R.; Samrongthong, R.; Shaikh, B.T. Knowledge, attitude and practices of health staff regarding infectious waste handling of tertiary care health facilities at metropolitan city of Pakistan. J. Ayub. Med. Coll. Abbottabad. 2013 , 25 , 109–112. [ Google Scholar ]
- Dona, D.; Giaquinto, C.; Baraldi, E.; Biffi, A.; Gamba, P.; Saieva, A.M.; Antoniello, L.; Costenaro, P.; Masiero, S.; Sainati, L.; et al. COVID-19 Pandemic: Perspective of an Italian tertiary care pediatric center. Healthcare 2020 , 8 , 311. [ Google Scholar ] [ CrossRef ] [ PubMed ]
Click here to enlarge figure
| Items | N | % | |
|---|---|---|---|
| Age (years) | 20–30 years | 123 | 48.1 |
| 31–40 years | 83 | 32.4 | |
| 41–50 years | 38 | 14.8 | |
| More than 50 years | 12 | 4.7 | |
| Gender | Male | 84 | 32.8 |
| Female | 172 | 67.2 | |
| Educational Qualification (Highest) | Diploma | 28 | 10.9 |
| Bachelor | 152 | 59.4 | |
| Master | 38 | 14.8 | |
| Doctorate | 15 | 5.9 | |
| Others | 23 | 9 | |
| Occupation | Physician | 57 | 22.3 |
| Nurse | 92 | 35.9 | |
| Pharmacist | 18 | 7 | |
| Lab technician (LT) | 22 | 8.6 | |
| Intern (Medical) | 21 | 8.2 | |
| Intern (Nurse) | 26 | 10.2 | |
| Respiratory therapist (RT) | 20 | 7.8 | |
| Professional Experience | 6 months to 1 year | 85 | 33.2 |
| 1–3 years | 53 | 20.7 | |
| 4–6 years | 59 | 23.1 | |
| 6–9 years | 38 | 14.8 | |
| 10 and above years | 21 | 8.2 | |
| Working Area | Government hospital | 132 | 51.6 |
| Private hospital | 78 | 30.5 | |
| Heath centre | 24 | 9.3 | |
| Polyclinic | 22 | 8.6 | |
| HCPs | Physician | Nurse | Pharmacist | Lab Technician | Interns (Medical) | Interns (Nurse) | RT | Total |
|---|---|---|---|---|---|---|---|---|
| Count | 57 | 92 | 18 | 22 | 21 | 26 | 20 | 256 |
| Mean | 14.4 | 13.6 | 13 | 13.1 | 12.8 | 12.5 | 12.3 | 13.1 |
| Median | 16 | 14 | 14 | 14 | 13 | 14 | 13 | 14 |
| Largest | 19 | 19 | 19 | 17 | 19 | 17 | 17 | 19 |
| Smallest | 8 | 7 | 7 | 9 | 7 | 8 | 8 | 7 |
| SD | 3.2 | 3.8 | 3.8 | 2.1 | 3.9 | 3.4 | 3.3 | 3.6 |
| Variance | 10.2 | 14.4 | 14.1 | 4.8 | 15.5 | 11.9 | 9.3 | 12.7 |
| S. No. | Practice on BMW Management | Always | Sometimes | Never |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | ||
| 1 | Does she/he follow the guidelines laid down by Ministry of Heath for BMW management? | 203 (79.3) | 49 (19.1) | 4 (1.6) |
| 2 | Does she/he adhere the infection control policy while handling COVID-19 patients? | 196 (76.6) | 52 (20.3) | 8 (3.1) |
| 3 | Does she/he use all personal protective equipment while handling biomedical wastes? | 72 (28.1) | 163 (63.7) | 21 (8.2) |
| 4 | Does she/he discard all personal protective equipment after handling biomedical wastes? | 72 (28.1) | 163 (63.7) | 21 (8.2) |
| 5 | Does she/he follow proper hand hygiene before and after every procedure and frequently? | 88 (34.4) | 159 (62.1) | 9 (3.5) |
| 6 | Does she/he follow colour coding of containers according to the type of wastes while for disposing BMW? | 177 (69.1) | 51 (19.9) | 28 (10.9) |
| 7 | Does she/he follow policies separating BMW as non-hazardous, hazardous, and sharp waste in segregation? | 102 (39.8) | 82 (32.1) | 31 (12.1) |
| 8 | Does she/he maintain BMW records? | 181 (70.7) | 42 (16.4) | 33 (12.9) |
| 9 | Does she/he take care in preventing sharp related injury like avoid recapping used needle? | 138 (53.9) | 112 (43.8) | 6 (2.3) |
| 10 | Does she/he prevent contamination while handling items of COVID-19 patients and other non-COVID-19 patients? | 192 (75) | 52 (20.3) | 12 (4.7) |
| S. No. | Attitude Questions | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree |
|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | ||
| 1. | Safe disposal of BMW is necessary in health care areas. | 193 (75.4) | 34 (13.2) | 25 (9.8) | 3 (1.2) | 1 (0.4) |
| 2. | BMW management is a team work. | 134 (52.3) | 52 (20.3) | 37 (14.5) | 22 (8.6) | 11 (4.3) |
| 3. | BMW management creates extra burden on my work. * | 31 (12.1) | 42 (16.4) | 78 (30.5) | 42 (16.4) | 63 (24.6) |
| 4. | BMW management is risk to transmit any infectious diseases. * | 15 (5.9) | 27 (10.6) | 44 (17.2) | 46 (18) | 124 (48.3) |
| 5. | Segregate hospital waste into different categories is time consuming. * | 126 (49.2) | 31 (12.1) | 68 (26.6) | 25 (9.8) | 6 (2.3) |
| 6. | PPE is must while handling biomedical waste. | 112 (43.8) | 82 (32) | 41 (16) | 18 (7) | 3 (1.2) |
| 7. | Decontamination and disinfection reduces the infection. | 119 (46.5) | 68 (26.6) | 51 (19.9) | 13 (5) | 5 (2) |
| 8. | Use of colour code for segregation of wastes are must. | 201 (78.5) | 29 (11.4) | 17 (6.6) | 7 (2.7) | 2 (0.8) |
| 9. | Proper BMW management enhance the quality assurance of health care sectors. | 141 (55.1) | 76 (29.7) | 21 (8.2) | 11 (4.3) | 7 (2.7) |
| 10. | Upgrade knowledge on BMW management is mandatory. | 128 (50) | 53 (20.8) | 31 (12) | 29 (11.3) | 15 (5.9) |
| Demographic Variables | Excellent | Good | Poor | X | |
|---|---|---|---|---|---|
| Age (years) | 20–30 years | 45 | 40 | 38 | X = 11.4833 p = 0.074539 NS |
| 31–40 years | 30 | 34 | 19 | ||
| 41–50 years | 22 | 11 | 5 | ||
| More than 50 years | 7 | 4 | 1 | ||
| Gender | Male | 28 | 43 | 13 | X = 14.0327 p = 0.000897 * |
| Female | 75 | 48 | 49 | ||
| Educational Qualification (Highest) | Diploma | 1 | 10 | 17 | X = 70.5972 p—0.00001 * |
| Bachelor | 50 | 66 | 36 | ||
| Master | 30 | 7 | 1 | ||
| Doctorate | 13 | 1 | 1 | ||
| Others | 9 | 11 | 3 | ||
| Occupation | Physician | 31 | 18 | 8 | X = 12.55807 p = 0.4019622 NS |
| Nurse | 31 | 38 | 23 | ||
| Pharmacist | 6 | 7 | 5 | ||
| Lab Technician | 12 | 6 | 4 | ||
| Intern (Medical) | 8 | 11 | 2 | ||
| Intern (Nurse) | 12 | 10 | 6 | ||
| RT | 6 | 9 | 5 | ||
| Professional Experience | I year | 34 | 23 | 28 | X = 19.6762 p = 0.011633 * |
| 1–3 years | 16 | 22 | 15 | ||
| 4–6 years | 20 | 26 | 13 | ||
| 6–9 years | 23 | 10 | 5 | ||
| 10 and above years | 10 | 10 | 1 | ||
| Working Area | Government hospital | 46 | 59 | 27 | X = 12.2509 p = 0.056599 NS |
| Private hospital | 34 | 23 | 21 | ||
| Heath centre | 12 | 6 | 6 | ||
| Polyclinic | 11 | 3 | 8 | ||
| MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
Share and Cite
Jalal, S.M.; Akhter, F.; Abdelhafez, A.I.; Alrajeh, A.M. Assessment of Knowledge, Practice and Attitude about Biomedical Waste Management among Healthcare Professionals during COVID-19 Crises in Al-Ahsa. Healthcare 2021 , 9 , 747. https://doi.org/10.3390/healthcare9060747
Jalal SM, Akhter F, Abdelhafez AI, Alrajeh AM. Assessment of Knowledge, Practice and Attitude about Biomedical Waste Management among Healthcare Professionals during COVID-19 Crises in Al-Ahsa. Healthcare . 2021; 9(6):747. https://doi.org/10.3390/healthcare9060747
Jalal, Sahbanathul Missiriya, Fahima Akhter, Amal Ismael Abdelhafez, and Ahmed Mansour Alrajeh. 2021. "Assessment of Knowledge, Practice and Attitude about Biomedical Waste Management among Healthcare Professionals during COVID-19 Crises in Al-Ahsa" Healthcare 9, no. 6: 747. https://doi.org/10.3390/healthcare9060747
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Biomedical waste management practices and associated factors among health care workers in the era of the covid-19 pandemic at metropolitan city private hospitals, Amhara region, Ethiopia, 2020
Roles Conceptualization, Formal analysis, Investigation, Software, Writing – original draft
Affiliation Debretabor Health Science College, Debre Tabor, South Gondar, Ethiopia
Roles Conceptualization, Formal analysis, Methodology, Software, Validation, Writing – original draft, Writing – review & editing
Affiliation Department of Environmental Health, Bahir Dar University, School of Public Health, Bahir Dar, Ethiopia
Roles Conceptualization, Formal analysis, Methodology, Software, Supervision, Writing – original draft
* E-mail: [email protected]
Roles Formal analysis, Software, Writing – review & editing
Affiliation Public Health Researcher, Addis Ababa, Ethiopia
- Getasew Mitiku,
- Amha Admasie,
- Amsalu Birara,
- Wubante Yalew

- Published: April 6, 2022
- https://doi.org/10.1371/journal.pone.0266037
- Reader Comments
Biomedical waste management is an important precondition to safeguard the healthcare workers and community members, as well as the environment, from being contaminated with infectious substances. However, biomedical waste management practices during the pandemic era of COVID-19 were unknown.
This study was aimed to assess biomedical waste management practices and associated factors among health care workers during the COVID-19 pandemic era at metropolitan city private hospitals, Amhara Region, Ethiopia.
An institutional-based cross-sectional study was conducted at metropolitan city private hospitals in Amhara Region. Simple random sampling was used to select 431 study participants. Data were collected through a self-administered questionnaire and observational checklists. The data were cleaned, coded, and entered into the Epi-data version 4.6, and then exported to SPSS version 20. for analysis. Variables with a p-value less than 0.05 were considered as significant factors in multivariable logistic regression analysis and AOR with a 95% confidence level was used to measure the strength of association.
The proportion of health care workers who had good practices in biomedical waste management was 49.4%. Participants who had MSc education level, [AOR = 4.20, 95% CI (1.01, 17.40)], Bachelor degree [AOR = 3.52, 95% CI (2.13, 5.82)], got training on biomedical waste management [AOR = 4.33, 95% CI (2.71, 6.93)], access to color-coded three bins in their working department [AOR = 6.24.95% CI (3.84, 10.13)] and those who had good attitude (AOR = 2.64, 95% CI (1.65, 4.22), were significantly associated with biomedical waste management practices in private hospitals.
The practice of biomedical waste management in the study area was low. Level of education, taking training on biomedical waste management, availability of color-coded three bins, and attitude of health care workers were significantly associated with biomedical waste management practices. Hence, in-service training is recommended to improve biomedical waste management practices.
Citation: Mitiku G, Admasie A, Birara A, Yalew W (2022) Biomedical waste management practices and associated factors among health care workers in the era of the covid-19 pandemic at metropolitan city private hospitals, Amhara region, Ethiopia, 2020. PLoS ONE 17(4): e0266037. https://doi.org/10.1371/journal.pone.0266037
Editor: Jianguo Wang, China University of Mining and Technology, CHINA
Received: August 27, 2021; Accepted: March 13, 2022; Published: April 6, 2022
Copyright: © 2022 Mitiku et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: Bahir Dar University, College of Medicine and Health Sciences funded this research, and Getasew Mitiku received the award. The funder has no role in study design, data collection, analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Abbreviations: AIDS, Acquired Immunodeficiency Syndrome; BMW, Biomedical waste; BMWM, Biomedical waste management; HBV, Hepatitis B Virus; HCB, Hepatitis C Virus; HCWs, Health Care Workers; HIV, Human Immunodeficiency Virus; IPC, Infection Prevention and Control; NGOs, Non-Governmental Organization; PPE, Personal Protective Equipment; SOP, Standard Operating Procedure; WHO, World Health Organization
Introduction
Biomedical waste (BMW) is any waste that is generated during the diagnosis, treatment, or immunization of human beings or animals or from research activities, and contains potentially harmful microorganisms which will infect hospital communities and the general public [ 1 , 2 ].
BMW includes sharps, non-sharps, blood, body parts, chemicals, pharmaceuticals, medical devices, and radioactive materials [ 3 ]. Common sources of biomedical waste include hospitals, nursing homes, clinics, laboratories, offices of physicians, dental, and veterinarians, home health care, and funeral homes [ 4 , 5 ]. BMWs are considered because they represent the second hazardous waste globally after radiation waste [ 6 ].
Biomedical waste is a relevant problem for several countries and poses serious public health threats worldwide [ 7 ]. Nearly 3.2 million tons of biomedical waste is generated by hospitals alone annually and the Environmental Protection Agency (EPA.2019) estimates that 10% to 15% of all biomedical waste is potentially hazardous [ 8 ].
According to the World Health Organization (WHO), nearly 85% of waste generated by the hospitals is general waste and about 15% of waste is biomedical waste, composed of 10% of infectious wastes and 5% of non-infectious wastes like radioactive and chemical wastes [ 9 ]. In developing countries, especially in Africa, BMW has not received the attention it deserves [ 10 ].
Biomedical waste management (BMWM) is the process of segregation, collection, storage, treatment, transport and disposal, and other safety measures of waste in health institutions [ 11 ]. Proper BMWM includes vital steps, such as segregation, collection, storage, transportation, treatment, and final disposal, of waste generated in health care settings [ 12 ]. Improper BMWM, which includes hazardous wastes (10–25%) mixed with the non-hazardous waste (75–90%) can result in the whole bulk waste becoming potentially hazardous [ 13 ]. There are international agreements and Conventions which are particularly pertinent in BMWM, environment protection, and its sustainable development and thus they should be kept in mind by preparing waste management policies [ 14 ]. Adequate knowledge, attitude, and practice (KAP) of health care workers (HCWs) are key factors for having a successful BMWM system, as they are important preconditions to safeguard the community [ 15 ], and the environment from being contaminated with infectious substances [ 16 ].
In Ethiopia, public hospitals provide training associated with infection prevention and healthcare waste management to waste handlers, environmental professionals, and heads of departments, but there was no published evidence indicating that private hospitals provide any training associated with healthcare waste management and infection prevention for health care workers [ 17 ].
In the Ethiopian context, there was no separate regulation specific for the HCFs to enforce them for the proper management of hazardous waste. However there are three BWM guidelines prepared by the Federal Ministry of Health (FMoH), Food, Medicine and Healthcare Administration and Control Authority (FMHACA), and Federal Environmental Protection Authority (FEPA) independently which are not, updated and lacked proper compliance on their implementation[ 18 – 21 ].
COVID-19 has been reported to first begin in December 2019 [ 22 ] while the WHO announced a Global Pandemic in March 2020. COVID-19 has been rapidly spreading all over the world, forcing countries and governments to adopt strict and specific measures to contain the pandemic. According to the Federal Ministry of Health of Ethiopia, the first COVID-19 case was reported in March 2020, and measures for tackling the pandemic have been taken ever since. In this regard, proper disposal of the waste is strongly relevant, as it may lead to the spread of communicable diseases [ 23 ]. Abundant use of medical technologies in hospitals and safety measures to stop the dissemination of the COVID-19 have led to a tremendous increase in BMW generation [ 24 ]. The generation rate was reported about 9200 tons/day of PW, with a total generation of more than 3.3 million tons per year in India [ 25 ], and The total mean weight of waste generation rate in the hospital was 492.5 kg/day in Ethiopia [ 26 ]. Moreover, the waste generated in health care facilities during the treatment and laboratory tests is highly contagious and hazardous [ 23 ].
According to the WHO 2018 report, the biomedical waste generation rate in low-income countries was 0.2kg of hazardous waste per hospital bed per day [ 27 ]. However, the Biomedical waste generation rates vary across different hospitals in Ethiopia where the generation rate ranges from (0.164–1.94) kg/bed/ day, and (0.396–0.866) kg/bed day (0.92kg/bed/day and/or 0.75kg/) patient/day hazardous waste [ 28 – 31 ]. Health facilities in Ethiopia have chosen incineration to treat BMW [ 32 , 33 ], but 80% of hospital incinerators used low-temperature technology that generates air pollutants [ 34 ].
The BMW is often the source of over 30 dangerous blood-borne pathogens [ 35 ]. Worldwide, about 5.2 million people (including 4 million children) die each year due to exposure to BMW [ 36 ], The hazards of exposure to hospital waste can range from developing gastroenteritis, respiratory and skin infections, as well as more deadly diseases like Human Immunodeficiency Virus Acquired Immunodeficiency Syndrome (HIV/AIDS), and Hepatitis B (HBV); moreover, injections with contaminated syringes caused 21 million hepatitis B infections (32% of all new infections), 2 million hepatitis C (HCV) infections (40% of all new infections) and 260,000 HIV infections (5% of all new infections) [ 37 , 38 ].
In developing countries, the management of BMW is becoming a growing concern in urban areas [ 39 ]. However, Pathogens and toxic chemicals in BMW can pose serious health risks for waste collectors, patients, and health care workers. Among these risks, HIV/AIDS, HBV, and HCV can be mentioned. HIV, HCV, and HBV have the risk of transmission 0.3%, 1.8%, and 30%, respectively from one sharp injury [ 40 ].
Few studies conducted in Ethiopia indicated that lack of training, awareness, staff resistance, managerial poor commitment, lack of adequate resources, negligence, and unfavorable attitude of the healthcare staff were the main identified challenges of BMWM [ 21 , 28 , 41 , 42 ]. Therefore, assessing the practice of BWM and its associated factors among health care workers is a pivotal element to halting this burden. Accordingly, this study is planned to assess the practice of biomedical waste management and associated factors among health care workers in private hospitals of the metropolitan city of the Amhara region.
Amhara Region is found in Northwestern Ethiopia and has an estimated acreage of about 170000 square kilometers. The region borders Tigray within the North, Afar within the East, Oromiya within the South, Benishangul-Gumz within the Southwest, and also the country of Sudan to the West. The region has three metropolitan cities (Bahir Dar, Gondar, and Dessie). In line with the population size estimation of 2016, the total population was 1,937,081. (797,794 in Bahir Dar 740,859, in Gondar, and 398,428 in Dessie). In these metropolitan cities, there are eight private hospitals namely Gamby, Adinas, Afelas, Dreamcare, Ethiogeneral, Batty, Selam, and Ibex with six hundred ninety healthcare workers.
Study design and period
An institutional-based cross-sectional study was carried out from November 25 to December 25/2020.
The source and study population of the study were all health care workers who were working in private hospitals in metropolitan cities of the Amhara region (Bahir Dar, Dessie, and Gondar). The study unit was, randomly selected health care workers.
Inclusion and exclusion criteria
Health care workers in private hospitals who were employed 6 months or longer were included in the study, However, health care workers who were unable to communicate due to illness were not eligible for the study.
Sample size determination and sampling procedure
The sample size was determined using Epi-info version 7 considering (78.9%) biomedical waste management practice in Debre Markos Town Healthcare Facilities, Amhara region [ 43 ]; at 4% of the marginal error, 95% of confidence level (CL), and a 10% response rate. Therefore, the sample size was 440. Amhara Region has three metropolitan cities. All private hospitals in the metropolitan cities in the region were identified by name and included in the study. The sample size was allocated proportionally to each private hospital. Then simple random sampling was employed to select healthcare workers from each private.
Study variables
Biomedical waste management practice was our dependent variable. On the other side, socio-demographic characteristics of respondents, Healthcare facility-related factors, Knowledge of HCWs, and Attitude of HCWs were the independent variables of the study.
Data collection method and instruments
The data were collected using a self-administered questionnaire and observational checklist. The questionnaire was comprised of socio-demographic characteristics, knowledge, attitude, and healthcare facility-related factors. The questionnaire and observational checklist were first developed in English and then translated into Amharic, by English and Amharic language professionals to check its consistency. Data were collected by 5 trained clinical nurses and supervised by 3 trained BSC Environmental Health Professionals.
Quality control
The training was given to data collectors, and supervisors regarding the objective of the study, a basic skill of communication, how to conduct the self-administered questionnaire for one day. Before the actual data collection, pre-testing was conducted on 5% of the sample size at Debre Tabor Referral Hospital and the necessary correction was made based on the pre-testing findings. The completeness of the questionnaire was checked every day by the supervisors and principal investigator. These supervisors were available throughout the data collection period.
Data processing and analysis
Data were entered into Epi-data software version 4.6 and then exported to the SPSS software version 20 for analysis. Descriptive statistics were carried out to illustrate the means, standard deviations, and frequencies of the demographic profile, knowledge, attitude, and BMWM practice. Binary logistic regression analysis was made to identify variables having an association with the dependent variable. Then all independent variables with a p-value < 0.25 in the bivariable analysis were entered into multivariable logistic regressions to control the effect of confounding. Model fitness was checked using the Hosmer Lemeshow test. Finally, variables with a p-value less than 0.05 were considered as significant factors, and AOR with a 95% confidence level was used to measure the strength of association.
Ethical statement
Ethical clearance was obtained from the ethical review board of the college of medicine and health science, Bahir Dar University. Communication with different official administrators was done through a formal letter obtained from Bahir Dar University and the metropolitan cities health bureau. Before starting data collection, the participants had read the objective, benefits, and risks of the study to get informed verbal consent of participants. The right of the respondent to withdraw from the interview or not to participate was respected. To keep the confidentiality of any information provided by study participants, the data collection procedure was anonymous.
Operational definition of terms
Biomedical waste, medical waste, healthcare waste, and hospital waste are terms that have been used interchangeably [ 41 ]. However, healthcare waste has been more frequently used by published articles so far [ 44 ].
Biomedical waste management practice
The response to questions related to biomedical waste management practice was summed up and calculated the mean. The mean and above indicated good practice and the below mean indicated poor practice towards biomedical waste management practice [ 39 ].
The response of knowledge questions was summed up and a total score was computed with value and taken mean score. The mean and above indicated good knowledge and the below mean indicated poor knowledge towards biomedical waste management practice [ 43 ].
Attitude is a judgment of individual behavior as good or poor and was measured based on the 5 points Likert scale by summing the Likert questions. The mean and above indicated a good attitude and the bellow mean indicated a poor attitude towards biomedical waste management practice [ 43 ].
Health care workers
HCWs are people who are involved in the promotion, protection, and enhancement of population health. In this study, the term health care worker was standing for clinical staff and cleaners [ 43 ].
Socio-demographic and healthcare-related characteristics
A total of 431 HCWs have participated in the study and the response rate was 98%. About, 245 (56.8%) were females. The mean age of the respondents was 29 years (with SD±4.68). Regarding educational status, 256 (59.4%) were first degree, and 12 (2.8%) were certificate and bellow. More than half, (52%) of the HCWs had more than 5 years of work experience. ( Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0266037.t001
Health care facility-related factors
Regarding training access, 201 (46.6%) of health care workers had taken BMWM training. About 388 (90%) workers were working 8 hours a day in different work environments such as 155 (36%) in OPD, 132 (30.6%) in Ward, and the rest in the laboratory, emergency, pharmacy, and others. In the working environment, only 223 (51.7%) of them had three bins for waste segregation. ( Table 2 )
https://doi.org/10.1371/journal.pone.0266037.t002
As stated in Fig 1 below, among the studied participants, 178 (41.3%), 63 (14.6%)), and 58 (13.2%) were nurses, doctors, and cleaners respectively ( Fig 1 ).
https://doi.org/10.1371/journal.pone.0266037.g001
Knowledge of health care workers
From the total health care workers, 290 (67.3%) HCWs knew the benefit of BMWM. About 269(62.4%), and 283(65.7%) were aware that infectious and general wastes, should be placed in yellow, and black, respectively. Besides, 233(54.1%) were aware of a safety box should be filled a maximum of 3/4 th . 168 (39%) health care workers knew the maximum storage time (48 hours) limit of infectious wastes before treatment or disposal. Based on the summary of knowledge questions the mean score of HCW’s knowledge in biomedical waste management was 7.96 with SD±1.50 on a range of 1 to 13 questions. More than half, (62.4%) of Health care workers had good knowledge about biomedical waste management ( Table 3 ).
https://doi.org/10.1371/journal.pone.0266037.t003
The attitude of health care workers
Among all Health care workers, 174 (40.4%) strongly agreed with the statement proper biomedical waste disposal is important and 167 (34.7%) health care workers strongly agreed with the statement BMWs should be segregated into different categories. Based on the summary of Attitude questions, the mean score of HCWs’ Attitude in biomedical waste management was 53.68 with SD±8.753 on a range of 1to 14 questions. More than half (53.4%) of Health care workers had a good attitude about biomedical waste management ( Table 4 ).
https://doi.org/10.1371/journal.pone.0266037.t004
The practice of Health care workers
This study revealed that 98 (22.7%) health care workers encountered sharp injury at their health care service delivery. Regarding PPE, 337 (78.2%) and 332 (77.0%) of HCWs always used gloves and gowns while handling or working with BMWs respectively. Based on the summary of practice questions, the mean score of HCWs practice in this study was 6.77with SD ±1.42 on a range of 1 to 12 questions. Less than half (49.4%) of health care workers had a good practice of biomedical waste management with (95% CI: 44.6%, 54.2%) ( Table 5 ).
https://doi.org/10.1371/journal.pone.0266037.t005
Among the studied participants, HCWs who had high scores of biomedical waste management practice 66% and 60.7% were medical doctors and nurses respectively. whereas HCWs who had list scores of BMWM practice 17.5% and 5.9% were cleaners and radiographers respectively ( Fig 2 ).
https://doi.org/10.1371/journal.pone.0266037.g002
Observation result
In the selected private hospital of each metropolitan city, observation was done at seven working departments such as OPDs, wards, laboratory, emergency, maternity, minor OR, pharmacy, and X-ray rooms of health care workers. Regarding the working department, more than half (62.5%) of departments had visual aid of biomedical waste containers. Gloves were available for each patient care cleaning device in all departments, except outpatient pharmacy departments. Three color-coding bins and leveled bins were available in Laboratory, Emergency, Maternity, and Minor OR departments, but not in other departments. The autoclave was available in some departments (maternity, Laboratory, and minor OR) but not in other departments rather it was available as a health care facility level in one fixed area. Personal protective equipment like heavy-duty gloves, aprons, and boots was available in maternity, emergency, laboratory, and minor OR rooms but not in others.
Regarding health care facilities, 37.5% of them had onsite storage rooms of biomedical wastes. The infection prevention and control committee was available only in two of them. All private hospitals had an incinerator, but it was not fenced (except one general hospital). Infection prevention and control guidelines were available in some hospitals’ infection prevention offices rather than in each working department. A placenta pit was available in all private hospitals.
Factors associated with biomedical waste management practice
In the bi-variable binary logistic regression analysis; age, attitude, knowledge of HCWs, level of education, training, availability of three bins, information about biomedical waste, information about biomedical waste management, and work experience were factors associated with biomedical waste management practice.
To start with the findings of socio-demographic factor, the odds of good biomedical waste management practice was found to increase by more than 4 times among health care workers who hold MSc and above the level of education when compared with a diploma and below [AOR = 4.20, 95% CI: (1.01, 17.40)].
Health care workers who took training on biomedical waste management had an association with biomedical waste management practice. Health care workers who took training [AOR = 4.33, 95% CI: (2.71, 6.93)] were 4.3 times more likely to practice good biomedical waste management than their counterparts.
The availability of three bins (black bin, yellow bin, and safety box) in the working department was associated with good biomedical waste management practice. Availability of three bins in the working department [AOR = 6.24. 95% CI (3.84, 10.13)] was 6.2 times more likely to practice good biomedical waste management than not the availability of three bins.
Health care workers who had a good attitude [(AOR = 2.64, 95% CI: (1.65, 4.22] were 2.6 times more likely to practice good biomedical waste management than those who had a poor attitude ( Table 6 ).
https://doi.org/10.1371/journal.pone.0266037.t006
In this study, 213 (49.4%) health care workers had a good practice of BMWM with (95% CI: 44.6%, 54.2%). This finding is in line with the finding of two previous studies done in South Africa and Biyem- Assi District Hospital in Yaoundé, which reported 53.9% and 50% respectively [ 45 , 46 ]. However, the finding of this study is found to be higher than the findings of three studies done in Rwanda, Jigjiga, and Gondar town, which reported 33.5%, 42.3%, and 31.5 of good practices respectively. [ 39 , 47 , 48 ]. This disagreement might be partly explained by a difference in health facility setup., since the above-mentioned studies (Jigjiga and Gondar) had a mixing of hospitals and health centers and the other study (in Rwanda) had only one district hospital. But the current study included only general hospitals. So, hospitals might have good practice of BMWM due to the presence of health care workers who had a high level of education than the health centers. But, the finding of this study is found to be lower than the finding of other previous studies done at Debre Markos Town in Ethiopia, in a tertiary hospital in Puducherry (Southern India) and Mahatma Gandhi Government Hospital of India, which reported 78.9%, 69.3%, and 54.7% were found respectively [ 43 , 49 , 50 ]. The low level of practice shown in this study might be due to the more availability of 3 bins in 81.4% of health care workers in their working department at Debre Markos Town than the current studied health care workers (51.7%) and cultural differences of Indian health care setup and this local area.
In the present study, there was a significant association between the level of education and biomedical waste management practices. Health care workers who held MSc and above education level were 4.20 times more likely to practice good biomedical waste management than those who were diploma and below and health care workers who were degree level of education also were 3.52 times more likely to practice good biomedical waste management than those who were diploma and below. This finding was similar to the finding of a study done in the Capital city of Uganda [ 51 ]. This indicates that educational status development helps to improve the practice of health care workers on biomedical waste management [ 52 ].
The other finding worth highlighting is related to training, a significant association between taking training and biomedical waste management practice was found. Health care workers who took training on BMWM had 4.33 times more likely to practice good biomedical waste management than those who didn’t take the training. This finding was in agreement with the previous studies conducted in Gondar town, Ethiopia, and the capital city of Uganda [ 48 , 51 ]. It is due to getting waste management training of all those who are responsible for handling wastes is important to improve BMWM [ 53 , 54 ].
Availability of color-coded three bins was significantly associated with biomedical waste management practice. Health care workers who had three bins in their working department were 6.24 times more likely to practice biomedical waste management than those who had no three bins. The finding was supported by the previous study done in Debre Markos town, Ethiopia [ 43 ]. This is due to the availability of three bins that make waste segregation being simple and safe to separate hazardous wastes from non-hazardous general wastes [ 55 ].
The attitude of health care workers was significantly associated with biomedical waste management practice. Health care workers who had a good attitude toward BMWM had 2.64 times more likely to practice good biomedical waste management than those who had a poor attitude toward BMWM. This finding was supported by the studies done in Biyem- Assi District Hospital in Yaoundé (Cameroon) and Agartala, Tripura (North-eastern India) [ 45 , 56 ]. The possible explanation might be due to a good attitude of health care workers helps to practice good biomedical waste management; because the level of attitude was one of the factors, which affect practice as seen in other studies. The study was conducted in all metropolitan cities’ private hospitals of the Amhara region, which covered all private hospitals in three cities. But there may be socially desirable bias for the practice of BMWM during data collection time. In this study, the quantification of the generation rate of biomedical wastes should have been measured.
Biomedical waste management practice was low among health care workers which is a risk of COVID 19 pandemic transmission. The level of education, taking training on BMWM, availability of three bins, and attitude of health care workers was found to have a significant association with biomedical waste management practice. Therefore, it was determined that it is better to provide in-service training programs on biomedical waste management and upgrade their educational level for health care professionals by regional health bureau and city administration health departments, as well as it is recommended to implement a three-bin system in the hospitals. Finally, all private hospitals should acknowledge the health care workers who practiced good biomedical waste management.
Although the study was conducted in private hospitals, the health tier system in Ethiopia both for private and public Hospitals is similar except for the ownership. Therefore, the finding can apply to other similar public hospitals within and across regions as well as in the least and middle-income countries.

Supporting information
S1 file. data collection tool english version..
https://doi.org/10.1371/journal.pone.0266037.s001
S2 File. Data collection tool Amharic version.
https://doi.org/10.1371/journal.pone.0266037.s002
S3 File. Data.
https://doi.org/10.1371/journal.pone.0266037.s003
Acknowledgments
We acknowledge data collectors and supervisors for their contribution to the overall success of this study and all respondents for their cooperation, time, and genuine response. Our great thanks go to Dr.Mesafint Molla and Francesco Giulietti for their support in editing the language of the manuscript.
- View Article
- Google Scholar
- PubMed/NCBI
- 19. Food MaHAaCAF (2005) Healthcare waste management directive. Addis Ababa: Food, Medicine and Healthcare Administration and Control Authority (FMHACA).
- 25. Ministry of Environment FaCC, Govt. of India (2019) Annual report 2018–19, Plastic Waste Management Rules (As per Rule ‘17(4)’ of PWM Rules, 2018)
- 27. WHO (2018) Fact sheet on Health care waste managment. Available from: https://www.who.int/news-room/fact-sheets/detail/health-care-waste .
- 33. Kasahun AaFA (2014) A Public–Private Partnership Framework for a Common Health Care Waste Treatment Facility for Addis Ababa City. Arlington, VA: AIDSTAR-One. https://doi.org/10.1016/j.ympev.2014.07.023 pmid:25109650
- 37. Ethiopia FDRo, Health Mo (2019) Infection Control and Waste Management Plan (ICWMP) For Biosafety Level Three (BSL3) National Reference.
- 52. Ali (2000) Manual of waste management at medical centres.
- 54. Ethiopian Food MaHAa, Authority C (2005,Addis Abeba) Healthcare Waste Management Directive.
- Increase Font Size
21 Biomedical wastes: Definition, sources, classification, collection, segregation, Treatment and disposal
Dr. J. Rajesh Banu
1.Objectives:
- To know what is biomedical waste and its source of generation To gain knowledge about the different types of biomedical waste. To explain the steps of biomedical waste management
- To describe the proper mode of collecting and segregating the biomedical waste To understand the risks of biomedical waste, its method of treatment and disposal
2. Biomedical Waste: Definition:
Bio-medical waste means “any solid and/or liquid waste produced during diagnosis, treatment or vaccination of human beings or animals. Biomedical waste creates hazard due to two principal reasons: infectivity and toxicity. Figure 1 shows some of the biomedical waste
Figure 1.Biomedical waste
3. Sources:
The source of biomedical waste is the place or the location at which biomedical waste has been generated. The source of biomedical waste is classified into two types based on the quantity of waste generated. They include major and minor source. Major source generates more amount of biomedical waste compared to minor source and also there is regular generation of biomedical waste in the major source which includes government hospitals, private hospitals, nursing home and dispensaries. Minor source includes physicians and dental clinics. Figure 2 shows the details of the various source of biomedical waste generation
Figure 2 Sources of biomedical waste
4. Classification:
The classification of the biomedical waste is carried out based on its characteristics, source of generation and the level of hazard to the environment. The biomedical waste is classified into two types:
1. Non hazardous waste
2. Hazardous waste
4.1 Non-hazardous waste:
About 75% to 90 % of biomedical waste characteristics were similar to that of domestic waste and are non-risky in nature. This waste is generated mainly from the organization and maintenance of hospital and health care centers.
4.2 Hazardous waste:
The remaining 10 – 25% of biomedical waste falls under the hazardous waste categories. The hazardous waste contains infectious characteristics of about 15% – 18 % and toxicity characteristics of about 5% – 7%. The various hazardous wastes includes,
Infectious waste: Waste containing pathogens; e.g. excreta; laboratory cultures; isolation wards waste; swabs, materials, or equipments that have been in contact with infected patients.
Pathological waste: Human tissues or fluids e.g. body parts; blood and other body fluids; fetuses.
Pharmaceutical waste: Waste containing pharmaceuticals; e.g. pharmaceuticals that are expired or no longer needed; contaminated pharmaceuticals (bottles, boxes).
Genotoxic waste: Waste containing cytostatic drugs (often used in cancer therapy)/ genotoxic chemicals.
Chemical waste: Waste containing chemical substances e.g. laboratory reagents; film developer; disinfectants and solvents that are expired or no longer needed.
Wastes with high content of heavy metals: Batteries, Broken thermometers, blood pressure gauges, Pressurized containers, gas cylinders, gas cartridges, aerosol cans.
Radioactive waste from radiotherapy: Waste containing radioactive substances e.g. unused liquids from laboratory research; contaminated glassware, packages or absorbent paper; urine and excreta from patients treated or tested with uncapped radionuclide
5. Biomedical Waste management:
Proper management of biomedical waste is highly essential since it induces various risk to the human health and to the surrounding ecosystem that leads to the ecological hazard, professional hazard and public hazard. Steps involved in biomedical waste management was shown in Figure 3
Figure 3. Steps involved in biomedical waste management
5.1 Segregation
To avoid mixing of the biomedical waste with other, a container should be set to the side with colour coding bags at the point of generation. The sorting or separation of waste into different categories is referred as segregation. Segregation will decrease or minimize the risks in addition to rate of managing and disposal. Segregation is the most important and critical step in bio-medical waste management. Only, effective segregation can confirm the effective bio-medical waste management.
5.1.1 How does segregation help?
Segregation plays an effective role in handling and treatment of waste. It reduces the quantity of waste and if done effectively, it can avoid the mixing of biomedical waste with any other type of waste especially municipal waste. Segregation will avoid the reuse of certain biomedical waste like used syringes, needles and other plastics. Some materials like plastics can be recycled after proper disinfection and these can be reused for non-food grade products.
During segregation process, the biomedical waste must be separated under the following categories shown in Table 1. Category no.1 includes the Human anatomical waste in which the human tissues, organs, body parts are considered. Animal waste falls under the Category No. 2. It includes Animal tissues, organs, body parts, carcasses, bleeding parts, fluid, blood and experimental animals used in research, waste generated by veterinary hospitals and colleges, discharges from hospitals, animal houses. Category No. 3 is the Microbiology & Biotechnology waste which contain Wastes from laboratory cultures, stocks or specimen of live microorganisms or attenuated vaccines; human and animal cell cultures used in research; infectious agents from research and industrial laboratories; wastes from production of biologicals, toxins and devices used for transfer of cultures. The Category No. 4 includes waste Sharps in which Needles, syringes, scalpels, blades, glass, etc. that may cause puncture and cuts. This includes both used and unused sharps. Discarded Medicine and Cytotoxic drugs falls under the Category No 5 which consists of wastes comprising of outdated, contaminated and discarded medicines. The soiled waste is included in the Category No. 6 containing items contaminated with body fluids including cotton, dressings, soiled plaster casts, lines, bedding and other materials contaminated with blood.
Table 1. Categories of Waste (Source: Biomedical Waste (Handling and management Rules 1998)
Category No 7 is the solid waste which includes waste generated from disposable items other than the waste sharps such as tubing, catheters, intravenous sets, etc. Liquid waste falls under the category no. 8, it consists of waste generated from the laboratory and washing, cleaning, housekeeping and disinfecting activities. Category No 9 includes incineration ash i.e., ash from incineration of any biomedical waste. Chemical Waste falls under Category No 10 and consists of Chemicals used in production of biologicals, chemicals used in disinfection and as insecticides etc.
5.2 Collection and storage
The collection of biomedical waste involves the installation of different colour coded containers for biomedical wastes obtained from varying sources. The containers/ bins should be placed in a location so that 100 % collection is achieved. The bins and bags that hold the biohazard symbol as shown in Figure 4 represents the nature of waste. The symbols in biomedical waste management is generally used as a warning to take precautions while exposing to those substances. The biohazard symbol was developed by the Dow Chemical Company in 1966 for their containment products.
Subsequent to collection, the biomedical waste is stored in specific containers and stored in a proper place. The extent of storage should not exceed beyond 8-10 h in big hospitals containing more than 250 bedded and 24 h in nursing homes. Each container must be clearly labelled with the location being mentioned in them. The purpose of labelling is to trace the waste at the source. Storage spot must be clear with a warning sign.
Figure 4 Symbols
Collection of the biomedical waste was carried out in its specific coloured bags. In the yellow colour bags, the categories 1,2,3 and 6 waste will be collected and this bags are made up of plastic materials. The Red bags are made up of disinfected container or plastic in which Category 3, 6 & 7 waste will be collected. The Blue/ White Translucent bags collect Category 4 & 7 waste which is made up of Plastic/ puncture proof container. The black coloured plastic bags are used for the collection of waste under category 5, 9 & 10. Figure 5 shows the collection of biomedical waste in the colour coded boxes
5.3 Transportation
The collected wastes are transported in trolleys or in enclosed wheelbarrow for treatment. The operator should ensure to avoid manual loading. The bags / Container containing biomedical wastes must be tied/ lidded before hauling for treatment. Vehicles used for transporting should be special to avoid contact to, and direct contact with the operator, scavengers and the public. While transporting the containers, it must be properly enclosed. The effects of traffic accidents should be incorporated in the design, and the driver must be trained in the actions which must be followed in case of an accidental spillage. The interior of the containers should also be rinsed thoroughly.
Figure 5. Collection of biomedical waste in a colour coded boxes (Source: Biomedical Waste Handling and management Rules 1998)
5.3.1 Trolleys
The use of trolleys will make the elimination of infectious waste possible at the source itself, instead of accumulation a new category of waste.
5.3.2 Wheelbarrows
Wheelbarrows are used to transfer the waste from the point source to the collection centres. There are two types of wheelbarrow – covered and open. Wheelbarrows are made of steel and provided with two wheels and a handle. Open dumping should not be done. Only packed waste (in plastic bags) should be carried. To prevent corrosion, care should be taken to prevent the liquid waste from spilling into the wheelbarrow. Wheelbarrows also come in various sizes depending on the utility.
5.3.3 Chutes
Chutes are vertical conduits provided for easy transportation of biomedical waste vertically in case of establishment with more than two floors. Chutes should be produced from stainless steel. It should have a self-closing lid. These chutes have to be sterilized on a daily basis with formaldehyde vapours. The linen that are contaminated with blood or other body fluids from each floor must be bundled in soiled linen or in plastic bags before expelling into the chute.
Alternately, elevators with mechanical winches or electrical winches can be used to bring down waste containers from each floor. Chutes are essential to keep away from horizontal transport of waste thereby diminishing the routing of the waste within the premises and hence reducing the risk of secondary contamination.
5.3.4 Dustbins
It is very important to calculate the amount of waste generated at each point. Dustbins should be of such capacity so that it can be placed at this specific site and that they do not overflow between each cycle of waste collection. Dustbins have to be cleaned subsequently at each cycle of clearance of waste with disinfectants. Dustbins can be wrinkled with plastic bags, which are chlorine-free, and colour coded as per the law.
5.4 Treatment and disposal
Before its final disposal of biomedical waste, it must be disinfected. Anatomical waste can be disposed by deep burial. Syringes to be cut (with hub cutters) and chemically disinfected with1% bleaching powder solution at source of generation before final disposal into sharps pit. Infected plastics to be chemically disinfected or autoclaved, shredded and recycled and sent for final disposal into municipal dumps.
5.4.1Incineration
Most of the hazardous biomedical wastes was treated by the method of incineration to reduce organic and combustible waste to inorganic incombustible matter. Incineration is a high temperature, dry oxidation process that results in significant reduction of waste volume and weight. Wastes that cannot be reused, recycled or pose problem in disposing in landfills are treated by incineration. Examples of wastes that cannot be incinerated are chemical wastes, wastes containing high mercury or cadmium ( broken thermometers, second-hand batteries, and lead lined wooden panels, sealed ampules or ampules containing heavy metals), silver salts, pressurized gas containers, photographic or radiographic wastes, halogenated plastics such as PVC.
The advantages of incinerator include high reduction of waste volume in addition to good disinfection competence. It helps to save the space in the landfill. The ash generated can be disposed of safely in the landfills. The major disadvantage of incineration includes high operating cost as they are energy intensive process. Also it releases a huge amount of atmospheric pollutants. The need for cyclic removal of slag and dirt, inadequacy in demolishing anti-thermal chemicals and drugs such as cyto toxic are its other disadvantages.
5.4.2 Autoclaving of Biomedical Waste
Autoclave treats the bio-medical waste through the mechanism of disinfection. The biomedical waste was subjected to following temperature and pressure based on its residence time:
i. If the autoclave residence time is not less than 60 minutes, the temperature should not be less than 121oC with the pressure of 15 pounds per square inch (psi); or
ii. If the autoclave residence time is not less than 45 minutes, the temperature should not be less than 135oC with the pressure of 31 pounds per square inch (psi); or
iii. If the autoclave residence time is not less than 30 minutes, the temperature should not be less than 149oC with the pressure of 52 pounds per square inch (psi);
While operating a gravity flow autoclave, biomedical waste is subjected to all three condition, whereas in vacuum autoclave, the biomedical waste is first subjected to one pre-vacuum autoclave (minimum) to purge the autoclave of all air. Succeeding this first and second conditions are applied. Bacillus stearothermophilus spore dials or spore strips with at least 1 × 104 spores per ml.is used as biological indicator of autoclave. The operating conditions of autoclave include a residence time less than of 30 minutes, temperature less than 121oC or a pressure must be less than 15 psi. On reaching certain temperature, the chemical indicator strip/tape changes colour that indicates the attainment of specific temperature. It may be essential to use more than one strip at various locations on the waste package to ensure the effectively autoclaving of inner content of the waste in the package.
5.4.3 Biomedical Liquid Waste
Before disposing the liquid form of biomedical waste into the sewer, it must be treated. Pathological waste after being treated with chemical disinfectants are flushed into the sewage system. Likewise, the chemical waste is neutralized with suitable reagents and then either flushed or treated in the sewage treatment plant. Mostly they are neutralized and dumped in sewer network. Highly skilled operators are required for this technique as it involves handling of hazardous substances. The biomedical waste effluent generated from the various source should conform to the following limits shown in Table 2. Environment (Protection) Act, 1986 prescribes the discharge limits of these waste into public sewers.
Table 2 . Disposal standard for biomedical waste Parameters Permissible limits
5.4.4 Microwave Treatment
Microwave treatment uses a frequency and wavelength of 2450 MHz and 12.24 cm, respectively for the destruction of microorganisms. The infectious contaminants in water with biomedical waste are destroyed by heat conduction when it is rapidly heated by the microwaves. By bacteriological and biological tests, the efficiency of the microwave disinfection was ensured regularly. The biomedical waste is evenly heated to a temperature of 97-100°C by means of microwaves in treatment chamber. Treatment of biomedical waste by microwaving can be carried out in the source itself. No shredding is required for microwave treatment of waste.
Most infectious wastes except body parts, human organs, infected animals carcasses and metal objects are suitable for treatment by microwave technique. This method shows good disinfection competence with good waste shrinking capacity. Similar to incineration this method also involves high operating costs. It is an eco-friendly process with potential operation and maintenance problems.
5.4.5 Deep Burial
Deep burial process is done in pits or trench of about 2 meters deep. The pits are half filled with waste, 50 cm soil and then with waste. The pits are covered with galvanized iron / wire meshes. When wastes are added to the pit, a layer of 10 cm of soil shall be added to enclose the waste. The deep burial site should be impermeable with no shallow well in the nearby area. The pits should be away from the habitation to avoid infection to surface or ground water. The site selected should not be a flooding or eroding zone and should be approved by the authority.
5.4.6 Inertization
Assimilation of waste with cement and other substances before disposal is called inertization process. This decreases the risk of entry of toxic substances into the surface or groundwater. A typical percentage of the mixture is 65% pharmaceutical waste, 15 % cement and 5 %water. A homogenous mass is created and cubes or pellets are produced and then stored. This process is economical and not suitable for infectious waste.
Table 3 shows the treatment and disposal method of the different categories of biomedical waste. The process such as incineration, deep burial, disinfecting process and municipal landfill disposal will be carried out. Category 1, 2, 3, 5 & 6 can be incinerated. Disinfecting process includes chemical treatment, autoclaving, microwaving and mutilation shredding was carried for waste under category 3, 4, 6, 7, 8 and 10. Category 1 and 2 can be disposed off by deep burial. Category 9 waste was disposed by municipal landfill.
Table 3. Treatment and disposal of biomedical waste (Source: Biomedical Waste (Handling and management Rules 1998)
6 Summary
In this lecture, we have learn about:
- The biomedical medical waste and its impact on environment
- The classification of biomedical waste and its level of toxicity.
- Method of segregation, collection, storage and transportation.
- Various disposal method and treatment techniques.
- Environmental protection training & research institute, “Bio – medical waste management self-learning document for nurses & paramedical”, (2015).
- Kamleshtewary, Vijay kumar, Pamittiwary, “Biomedical waste management a step towards a healthy future”, Chapter 162, (2007), reffered page 927 – 932
- Patil AD, Shekdar AV. “Health-care waste management in India” Journal of Environmental Management 63 (2001): 211–220
- http://en.wikipedia.org/wiki/Biomedical_waste
- DOI: 10.31031/SBB.2018.01.000522
- Corpus ID: 134379402
A Review on Biomedical Waste and its Management
- P. Sharma , A. Sharma , +1 author Somani Ps
- Published in Significances of… 6 June 2018
- Environmental Science, Medicine
15 References
A study : biomedical waste management in india, current perspectives on biomedical waste management: rules, conventions and treatment technologies, advantages and disadvantages of healthcare waste treatment and disposal alternatives: malaysian scenario, biomedical waste management: a study of knowledge, attitude, and practices in a tertiary health care institution in bijapur, a case study to review compliance to biomedical waste management rules in a tertiary care hospital, awareness and practices regarding bio-medical waste management among health care workers in a tertiary care hospital in delhi, assessment of medical waste management within selected hospitals in gaza strip palestine: a pilot study, biomedical waste management: a study of knowledge, attitude and practice among health care personnel at tertiary care hospital in rajkot, incineration or autoclave a comparative study in isfahan hospitals waste management system (2010), awareness and practices regarding biomedical waste management among health-care workers in a tertiary care hospital in delhi: comment, related papers.
Showing 1 through 3 of 0 Related Papers
- Content Guidelines
- Privacy Policy
Upload Your Knowledge on Environmental Pollution:
Essay on biomedical waste management.
Here is an essay on ‘Biomedical Waste Management’ for class 11 and 12. Find paragraphs, long and short essays on ‘Biomedical Waste Management’ especially written for school and college students.
ADVERTISEMENTS:
Essay Contents:
- Essay on the Waste Minimization Methods
Essay # 1. Introduction to Biomedical Waste Management :
Hospitals and other health-care establishments have a ‘duty of care’ for the environment and for public health, and have particular responsibilities in relation to the waste they produce. Unfortunately, medical wastes are not given proper attention and these wastes are disposed of together with municipal and industrial solid wastes.
Every hospital must possess a tailor-made waste disposal policy for itself, constituted by the intelligentsia-nominees of the administration. The ‘3 R’ principle of reduce; reuse and recycle should be the basis for good management practices.
Biomedical waste (BMW) means any waste, which is generated during the diagnosis, treatment or immunization of human beings or animals or in research activities pertaining thereto or in the production or testing of biologicals, and including categories of BMW (Management and Handling) (Second Amendment) Rules, 2000 by Ministry of Environment and Forests Notification; Biologicals means any preparation made from organisms or micro-organisms or product of metabolism and biochemical reactions intended for use in the diagnosis, immunization or the treatment of human beings or animals or in research activities pertaining thereto.
Infectious wastes include all those medical wastes, which have the potential to transmit viral, bacterial or parasitic diseases. It includes both human and animal infectious waste and waste generated in laboratories, and veterinary practice. Infectious waste is hazardous in nature. Any waste with a potential to pose a threat to human health and life is called hazardous waste. However, if the infectious component gets mixed with the general non-infectious waste, the entire bulk of waste becomes potentially infectious.
This becomes all the more important in a situation peculiar to a developing country like India where poverty and ignorance induce many persons to sift and sort through dumped waste to make a living out of recyclables thus being exposed to danger of contracting diseases from hazardous components of waste. By hospital wastes, it means especially the bio-medical wastes generated in different departments of the hospitals.
Biomedical waste—a term that is more appropriate than infectious waste, because there is no safe and simple method to test waste for infectiousness. The term waste management is used rather than waste disposal because our discussion is much broader than just the disposal process.
For waste management to be efficient, the waste should be managed at every step – from acquisition of materials that eventually become waste, to waste generation, discard, collection, containment, handling, accumulation, storage, transport, treatment, and finally disposal. ‘Disposal’ refers to the final disposition of waste or waste treatment products, such as placement in a landfill. Thus, management must extend from ‘cradle to the groove’—that is, from the point of generation to ultimate disposal.
Essay # 2. Nature and Quantum of Hospital Wastes :
Three major categories of health care facilities existing in India are:
(i) Outpatient Clinics or Dispensaries :
This category constitutes the largest number of clinics or dispensaries in the private sector; subcentres manned by the Female Health workers and primary health care centres (PHCs) in the rural areas and dispensaries, mobile dispensaries, health and family welfare posts providing outpatient care in government sector.
(ii) Outpatient and Inpatient Care Hospitals :
The network of Community Health Centres with 30 or more beds is the most important peripheral health facility that provides inpatients care in rural areas in public sector. Small nursing homes in private sector also provide inpatient as well as outpatient care in peripheral rural areas.
(iii) The Next Tier :
The next tier of hospitals ranges from sub-divisional and district hospitals, medical college hospitals to specialty hospitals in public sector. Similar hospitals in private sector provide both inpatient and outpatient care.
It is estimated that in most of the health care settings, about 85% of the waste generated is non- hazardous, about 10% is infectious wastes and 5% non-infectious but hazardous waste. It is estimated that the quantity of waste generated from hospitals in India ranges from 1-2 kg/bed/day.
Waste generated in developing countries contains much less disposable articles and plastics than waste generated in developed countries, the differences are partly due to differences in use of disposables in health care and partly due to life styles of the population.
Essay # 3. Knowledge of the Risk :
The potential for infections from contact with non-sharp medical waste is virtually nonexistent. The only medical waste that has been associated with infectious diseases transmission is contaminated sharps. Obviously, this potential for transmission exists when infectious sharps are mishandled and are not properly discarded or contained. The rising trends of HBV and HIV infection in the community and among health care providers has led to an increasing awareness about the risk associated with this lackadaisical practice.
WHO has estimated that, in 2000, injections with contaminated syringes caused:
i. 21 million hepatitis B virus (HBV) infections (32% of all new infections);
ii. Two million hepatitis C virus (HCV) infections (40% of all new infections); and
iii. 2,60,000 HIV infections (5% of all new infections).
Best evidence from prospective studies with aggressive monitoring suggests that the incidence of needle stick injuries is significantly higher than reported through passive surveillance, ranging from 14 to 839 needle stick injuries per 1,000 health care workers per year. The economic cost of managing these injuries is substantial, ranging from 51$ to 3,766$ (2002 US$).
This amount excludes the cost of treating the long-term complications of needle stick injuries, such as HIV and hepatitis B and C infections, each of which can cost several hundreds of thousands of dollars to manage. Another potential health risk for medical waste handlers is physical injury due to handling heavy and cumbersome waste containers. Physical and health hazards are also associated with the high operating temperatures of incinerators and steam sterilizers and with toxic gases vented into the atmosphere after waste treatment.
Multi-Hazardous Waste :
Multi-hazardous waste includes waste that is infectious and that contains radionuclides and/or hazardous chemicals. An example is waste contaminated with blood or body fluids and with a chemotherapy drug. Multi-hazardous waste is best managed and treated separately from other infectious waste. It should be noted that mercury thermometers are not infectious waste, and they should not be classified and managed as such. All unwanted or broken mercury thermometers should be managed and disposed of as hazardous chemical waste.
They should never be placed in sharps containers. Because mercury is a component of dental amalgam, comprising about 50 per cent of amalgam among other metals, in recent years the concern has affected dental practices and even educational curricula in the dental schools. Both the California Dental Association and the American Dental Association have developed recommendations for best practice that dental offices should follow when handling dental amalgam waste.
Elements and consecutive steps of the biomedical waste management plan are:
Essay # 4. Source Separation and Waste Segregation :
Source separation of waste means separating, at the point of generation and discard, wastes with distinct characteristics into separate waste streams (such as infectious waste, radioactive waste, etc.). Separation is usually accomplished by using different and distinct waste collection containers for each type of waste. Such separation is best done when materials are discarded as waste (at the point of waste generation), because the person who discards the waste is generally most knowledgeable about its nature.
Brief instructions at the point of discard (e.g., posted about the waste container) facilitate compliance with source separation, as does placing containers for the different waste types as close as possible to the point of waste generation. Waste segregation means keeping waste streams separate from the point of generation through collection and handling, accumulation, storage, transport, and treatment. For source separation and waste segregation to be successful there must be an explicit label on each bag and shall be non-washable and prominently visible.
Choice of Bins or Receptacles:
Hospital managers may prefer to use plastic or metal bins for waste storage in order to save on the cost and paperwork of buying large number of on-strip sacs. However, since the cost of hospital waste management is found to be significantly less than 1% of the hospital budget in many cases, the small saving by not providing facilities for waste storage may be regarded insignificant. The extra expenditure involved in buying plastic bags is justified by improved hygiene, hospital infection control and convenience in disposal.
Essay # 5. Waste Minimization Methods :
Waste minimization is an important aspect of medical waste management. This importance derives from a variety of considerations including regulatory requirements to reduce and to minimize the quantities of wastes generated, cost savings that can be realized when smaller quantities of waste must be managed and disposed of as medical waste, cost savings that can be realized when some wastes are reused or recycled, increased environmental awareness by the institution and its employees and institutional concerns about community relations.
Source reduction means reducing the quantities of waste generated. One approach is through strict definition of waste type accompanied by source separation for the different waste streams. Source reduction is also achieved by product substitution, that is, the substitution of products that generate less waste. One example in the hospital setting is the use of devices such as needle less intravenous systems that reduce sharps generation and protect healthcare workers from exposure to blood-borne pathogens.
This is to be noted that the reverse happened with auto-disable syringes that resulted in greatly increased volumes of used injection materials—200 times as much as those of sterilizable syringes. Though India is planning to use the auto-disable syringes, it is important to examine the flaws in their design too. Another example is the substitution of reusable items for the single-use items that gained wide acceptance, because they eliminated the need for on-site reprocessing.
Product substitution is also important in minimizing the quantities of chemical and radioactive wastes generated in various laboratory analyses like a fluorescent based method (Mycobacterial Growth Indicator Tube, MGIT) replacing the radioactive method (BACTEC) for the rapid diagnosis of Mycobacterium tuberculosis. Recycling reduces the quantities of wastes generated by reusing certain materials, with or without prior reprocessing, rather than discarding them.
Other wastes that lend themselves to recycling are solvents, packaging materials, paper and aluminium cans. Many solvents can be redistilled for reuse. An alternative approach for some solvents is incineration with heat recovery. Proper management is essential for implementation of a waste minimization program. The good management program includes an employee awareness program, employee training, purchasing strategies, and inventory control.
Related Articles:
- Essay on Biomedical Waste | Waste Management
- How to Dispose Biomedical Waste? | Waste Management
Upload and Share Your Article:
- Description *
- Author Name *
- Author Email Id. (required) *
- File Drop files here or Select files Max. file size: 128 MB, Max. files: 5.
- Email This field is for validation purposes and should be left unchanged.
Essay , Waste Management , Hospitals , Biomedical Waste Management
Privacy Overview
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |
Poor Economic Outlook and Lack of Security Undermine Kabardino-Balkaria’s Governor

Advertisement
An overview for biomedical waste management during pandemic like COVID-19
- Published: 06 June 2022
- Volume 20 , pages 8025–8040, ( 2023 )
Cite this article

- V. S. Kanwar 1 ,
- A. Sharma 1 ,
- M. Kanwar ,
- A. L. Srivastav ORCID: orcid.org/0000-0003-0238-7395 1 &
- D. K. Soni 3
5217 Accesses
8 Citations
Explore all metrics
Amid COVID-19, world has gone under environmental reformation in terms of clean rivers and blue skies, whereas, generation of biomedical waste management has emerged as a big threat for the whole world, especially in the developing nations. Appropriate biomedical waste management has become a prime concern worldwide in the pandemic era of COVID-19 as it may affect environment and living organisms up to a great extent. The problem has been increased many folds because of unexpected generations of hazardous biomedical waste which needs extraordinary attentions. In this paper, the impacts and future challenges of solid waste management especially the biomedical waste management on environment and human beings have been discussed amid COVID-19 pandemic. The paper also recommends some guidelines to manage the bulk of medical wastes for the protection of human health and environment. The paper summarizes better management practices for the wastes including optimizing the decision process, infrastructure, upgrading treatment methods and other activities related with the biological disasters like COVID-19. As achieved in the past for viral disinfection, use of UV- rays with proper precautions can also be explored for COVID-19 disinfection. For biomedical waste management, thermal treatment of waste can be an alternative, as it can generate energy along with reducing waste volume by 80–95%. The Asian Development Bank observed that additional biomedical waste was generated ranged from 154 to 280 tons/day during the peak of COVID-19 pandemic in Asian megacities such as Manila, Jakarta, Wuhan, Bangkok, Hanoi, Kuala Lumpur.
Similar content being viewed by others

Challenges and measures during management of mounting biomedical waste in COVID-19 pandemic: an Indian approach
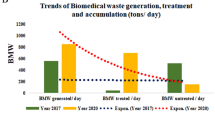
The influence of COVID-19 pandemic on biomedical waste management, the impact beyond infection

Current Scenario of Biomedical Waste Management in India: A Case Study
Explore related subjects.
- Environmental Chemistry
Avoid common mistakes on your manuscript.
Introduction
COVID-19 (or Coronavirus disease 2019) originated from the animals (meat/fisheries market of the Wuhan city, China) can cause severe infections to the human respiration system (Cascella et al. 2020 ; Roujian et al. 2020 ; Zhu et al. 2020 ; Xu et al. 2020 ). Firstly, it was diagnosed in the end of December, 2019 in Wuhan city of China when like pneumonia symptoms were observed in the local residents of Wuhan (WHO 2020a ; Lokhandwala and Gautam 2020 ; Sohrabi et al. 2020 ). Other health problems were also got detected because of CIVID-19 infections including breath shortness, fever, pain in muscles and head (Huang et al. 2020 ). WHO declared worldwide human health emergency (pandemic) due to fast rate of COVID-19 infections as it took around 3 months durations only to reach in 100 nations. Moreover, 10 million people of the world got infected with COVID-19 till the last of May, 2020, whereas up to last week of June, 2020, COVID-19 infections reached in 216 countries (WHO 2020b ). Even top economic nations of the world (USA, Germany, France, Spain, Japan, Singapore, Italy etc.) were stuck in the raising COVID-19 infections among the community people (Amanat and Krammer 2020 ). However, USA was and still on the top in terms of highest numbers of both infections and deaths due this pandemic (CDC 2020 ). In Asia, India is on the top position reading deaths as well infections due to corona virus (MoHFW 2020 ). In the absence of vaccine, testing of COVID-19 has become very important to prevent its further infections and reverse-transcription polymerase chain reaction, medical imaging and computed tomography are the recommended methods of detection (Ardakani et al. 2020 ). Despite of infecting huge population, the fatality rate of COVID-19in India is less than Middle East respiratory syndrome (MERS, year 2012) and severe acute respiratory syndrome (SARS CoV-1 year 2003) and more than the Spanish flu (year 1918) as shown in Fig. 1 .
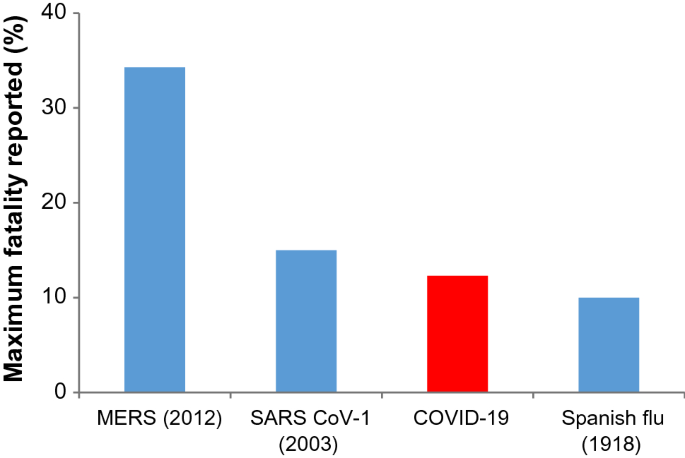
Source : Modified from Goel et al. 2020 )
Human fatality rates of different viral infections (
From Fig. 1 , it was observed that in year 2012, MERS had affected people of 27 countries of the world with maximum fatality rate of 34.3% followed by SARS CoV-1 in year 2003 with 15%. In 1918, the fatality rate of Spanish flu was rescored as 10% which is less than COVID-19 (12.3%) (Callaway et al. 2020 ; Goel et al. 2020 ). However, according to Gates ( 2020 ), it can kill only 1% of total infected persons including old aged people as well as adults, if they were already suffering with some serious health disorders. However, it can spread easily among the humans as compared to other illness (Goel et al. 2020 ). Because of this reason, initially, rate of infection was slow and later through community transmission; it has reached in every part of the world (Anderson et al. 2020 ; Shammi et al. 2020 ).
Factors responsible for the transmission of COVID-19
As per the studies, it has been found that several days are required for complete inactivation of COVID-19 virus (Casanova et al. 2009 ; Qu et al. 2020 ). It is quite evident corona virus is mostly spreading through physical contacts between the individuals knowingly or unknowingly. However, it can also infect the healthy people through the skin, mouth, nose and eyes of any COVID-19 patient after direct or indirect interactions. The virus can survive on the various types of surfaces (medical wastes, plastic etc.) or environment for a specific time (Weber et al. 2016 ; Qu et al. 2020 ). Further, the chances of viral infection may be governed by several factors including stability of virus containing aerosols in the air (usually 3 h is reported), active periods of the virus on the surfaces like steel (7 days), glasses and currency papers (4 days). Even after applying soap on the hands, additional five minutes are required to inactivate the virus. Hence, it is advisable that one should avoid touching any part of the face within 5 min of hand wash (Goel et al. 2020 ).Other factors of COVID-19 transmission may also be considered as sneezing, coughing, and talking with any infected person. In many studies, presence of COVID-19 virus has been diagnosed in the excreta, tear, urine and other body secretions of the infected people (Zhang et al. 2020 ; Xia et al. 2020 ; Peng et al. 2020 ). In Japan, a study has shown that COVID-19 transmission is also possible through the lighter water droplets containing virus. As lighter water droplets (or aerosols) when come in the contact of any COVID-19 infected person and thereafter it can transmit into healthy people. However, this type of airborne infection depends upon the local weather conditions (wet or dry) (Chin and Poon 2020 ; Wölfel et al. 2020 ). Moreover, a theory of asymptomatic or oligosymptomatic infections are also reported in the literatures (Wölfel et al. 2020 ). There are different types of which can trigger in the transmission of the COVID-19 (Fig. 2 ).
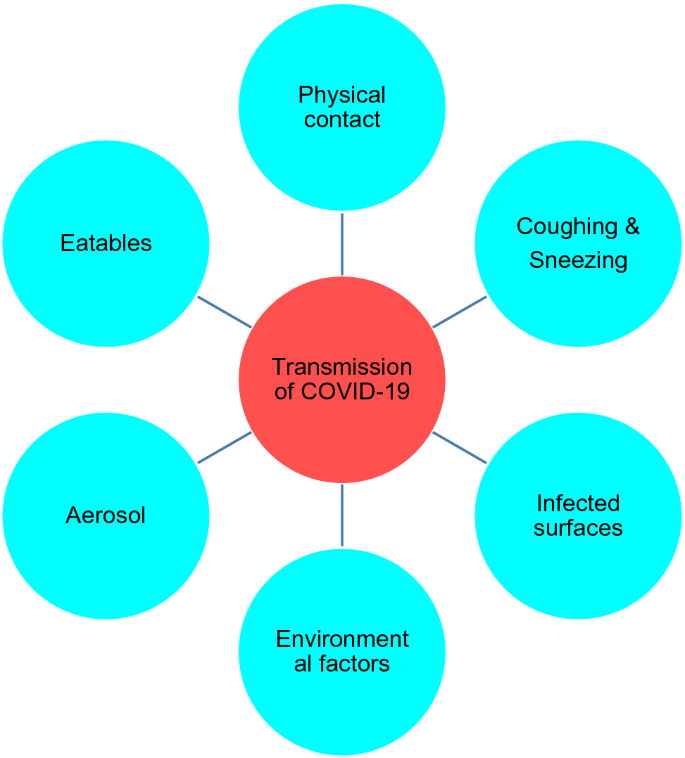
Responsible factors for the human transmission of COVID-19
Most importantly, poor people (may be due to insanitary practices), elderly persons, workers of waste management authorities are in high risk zone of COVID-19 infection. However, their restricted movement can reduce the chance of pandemic outbreak (United Nations 2020 ). Because of this reason, in USA and Singapore, recycling of waste materials has been discontinued or carried out with less frequency to reduce the risk of further transmission of COVID-19 among the sanitary workers (Zambrano-Monserrate et al. 2020 ; National Environmental Agency, Singapore 2020 ). In developing world, situation has become very critical during this pandemic because of unemployment during lockdown and panic of infection among waste management people, and ultimately, it may affect the economy of the nations too (World Bank 2020 ). According to Nghiem et al. ( 2020 ) and Kulkarni and Anantharama ( 2020 ) it can be managed by adopting best practices of waste management to safeguard the health of these workers during handling of contagious wastes. Major objective of the present research paper is to explore the practices which can be helpful in the management of biomedical wastes during pandemic like COVID-19. Moreover, alternatives options and challenges of future have also been discussed.
Impacts of COVID-19 pandemic
(i) impact on the human health.
Human respiration system is the main target of this COVID-19 virus. Moreover, this has become more dangerous for the elderly people or the people who are suffering with sever diseases related with cardiac system, diabetes, cancer, or else (Dhama et al. 2020 ; Rodriguez-Morales et al. 2020 ; Mahajan and Kaushal 2020 ). However, it has also found that children are not a common victim of the COVID-19 virus (Huang et al. 2020 ) because usually they do not go outside the home as well as less travelling exercise (Lee et al. 2020 ). Chen et al. ( 2020 ) reported that only in China health recovery of the citizens was so better due to an improvement in air quality amid COVID-19 lockdown periods. Therefore, due to lockdown, the pollution load of environmental systems (atmosphere, hydrosphere and lithosphere) has decreased worldwide and this may be helpful for the protection of public health. Figure 3 shows the confirmed infections of COVID-19 in top ten countries as on Sept. 30, 2020.
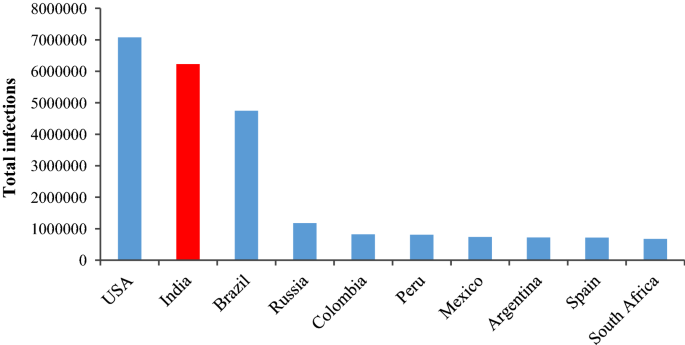
Total COVID-19 infections in top 10 mostly affected countries (WHO 2020b ) (assessed on the 30.09.2020)
From Fig. 3 , it appears that till Sept. 30, most affected countries with COVID-19 infections are USA, Indian, Brazil, Russia and Columbia. Similar problems have been observed in the Bangladesh during lockdown periods amid COVID-19 pandemic (Hopman et al. 2020 ). Transmission of corona virus through air is also reported (Bourouiba 2020 ) and can be prevented by using face mask at crowded places (Klemeš et al. 2020 ). Moreover, during the crisis maintaining employment opportunities along with public health protection has become top priorities of the government authorities. For public health protection, there are many issues should be handles with due care like advancement of medical standards, easy availability of testing facility, revisions of policies for local public etc. (WHO 2020b ; Sharma et al. 2020 ). In addition to these, many psychological disorders have been observed especially among patients due to this pandemic as studied in United Kingdom (Ford et al. 2020 ; Holmes et al. 2020 ). Figure 4 summarises the diverse types of impacts observed during the COVID-19 outbreak.
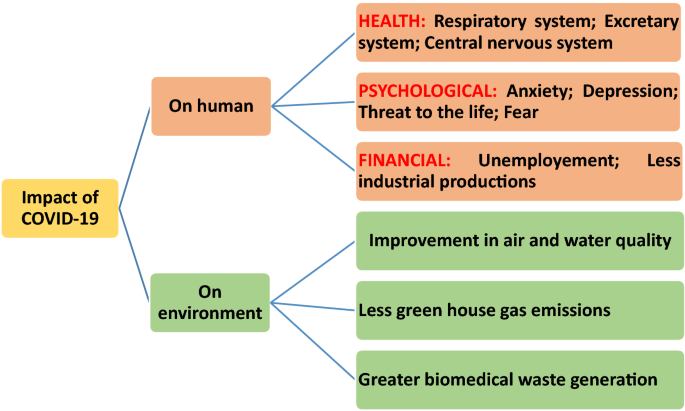
Impact of COVID-19 on the environment and human beings
Elderly people are found at the larger risks of COVID-19 and during quarantine period, there is a great chance of developing mental disorders (for example, anxiety, guiltiness, dementia, depression etc.) because of loneliness (Armitage and Nellums 2020 ; Holmes et al. 2020 ; Ahorsu et al. 2020 ; Shammi et al. 2020 ).These mental problems may be responsible for the increase in number of suicide cases in the society (Duan and Zhu 2020 ). However, few medicines are recommended in case of emergency situation for COVID-19 patients (Singh et al. 2020 ). Recently, Goel et al. ( 2020 ) reported that silver coated grapheme oxide sheets and chiral gold nanohybrids for the inhibition as well as detection of the different types of viruses including corona virus. According to Chan ( 2020 ) application of different types of nano-materials should also be explored against the coronavirus. Because of unavailability of proper medication, “social lockdown” or “social distancing” has been imposed to stop the transmission of COVID-19 virus across the world (Paital et al. 2020 ; Zambrano-Monserrate et al. 2020 ; Lokhandwala and Gautam 2020 ; Somani et al. 2020 ). During lockdown, restrictions were imposed on every type of public meetings, industries and automobiles to maintain social distancing. Due to shutdown of factories and vehicles many positive changes have been observed in the cosmopolitan environment.
(ii) Impact on the environmental systems
In twenty-first century, there are many challenges for whole world including severe environmental quality diminution (Chakraborty and Maity 2020 ) due to over industrialization as well as unorganized fast urbanization as it requires huge demand of natural resources. Because of overexploitation of resources, ecological systems have been deteriorated which includes air pollution, water quality degradation, soil contamination, global warming, threat to the biodiversity, human health problems etc. (Bremer et al. 2019 ). Amid COVID-19 pandemic, world has gone into complete lockdown except essential commodities which imposed ban on the opening of industries as well as movement of the vehicles. Hence, during lockdown periods emission of harmful gases and wastewater discharges were decreased significantly and considerable environmental healing was observed across the world (Australia, China, France, Germany, India, Italy, Iran, Spain, South Korea, Taiwan, Turkey, United Kingdom and USA) since March 2020 (Chakraborty and Maity 2020 ; Elavarasan and Pugazhendhi 2020 ; Atalan 2020 ). As it has been observed that air pollution is responsible for > 7 million human deaths in whole world and out of it, 1.2 million deaths were reported in only in India (WHO 2018 ; Polk 2019 ). Significant reduction in the concentration of air pollutants (particulate matters and greenhouse gases) was reported from the various parts of the world like Kazakhstan (Kerimray et al. 2020 ), India (Mahato et al. 2020 ) and Brazil (Dantas et al. 2020 ). Besides, industries and automobiles, operations of aeroplanes were also affected during lockdown and it was also helped in the reduction of greenhouse gases in the atmosphere (Corletta et al. 2020 ). However, level of indoor air pollutants (including black carbon of smoke) was increased amid lockdown as most of the people were got stuck inside their homes (NASA 2020 ). Availability of adequate natural ventilation (not any artificial systems like air conditioner etc.) inside the homes could dilute the concentrations of indoor air pollutants (Bhatia and Bhaskar 2020 ; Somani et al. 2020 ). Moreover, concentrations of greenhouse gases were also remarkably decreased during lockdown periods, for example 2600 metric tons of carbon dioxide was decreased across the global amid COVID-19 pandemic (Global Climate Report 2019 ) due to less energy demand as around 64% of total electrical energy is getting produced from the natural gas and coals (Somani et al. 2020 ). In India, the carbon dioxide emission was decreased in between 15 and 30% during March to April, 2020 (Myllavirta and Dahiya 2020 ). Similarly, due to closure of machines and restricted vehicle movements, level of noise also got decreased as reported in many countries such as China (19%), USA (36%) and United Kingdom (54%) (Somani et al. 2020 ). Moreover, decrease in oceanic noise levels were also observed during lockdown due to limited waterways traffic and it could have provided a better environment for aquatic lives (Ian Randall 2020 ). In India, around 40–75% noise level reductions were reported from the various states or cities (for example, Karnataka, Delhi, Bengaluru, Kolkata ) due to non-movements of the trains (Somani et al. 2020 ) as trains and other vehicles are the principal causes of noise pollution in megacities of India (Mishra et al. 2010 ). Furthermore, biodiversity conservation via revival of natural shelters for marine organisms (turtles), other aquatic lives, birds, wild life animals were found to be very rapid due to less movement of human beings (Corletta et al. 2020 ; Zambrano-Monserrate et al. 2020 ) as the reports were published in the countries like Mexico, Spain, India as well as Ecuador (Zambrano-Monserrate et al. 2020 ; Somani et al. 2020 ). Self-purification capacities of many rivers/lakes increased amid lockdown because of less wastewater discharge as most of the pollution in surface water reservoirs is due to the raw sewage mixing into them (Sinha et al. 2016 ; CPCB 2020a ; Corletta et al. 2020 ; Zambrano-Monserrate et al. 2020 ). In India, amid lockdown, water quality of rivers Ganga and Yamuna were improved for bathing and aquaculture purpose as observed by the Central Pollution Control Board (CPCB) than previous years (CPCB 2020a ). Most importantly, Uttarakhand Pollution Control Board of India stated that Ganga river water at Haridwar (location: Har-ki-Pauri) was improved for drinking purpose after more than 30 years (Katariya 2020 ). Similarly, (Yunus et al. 2020 ) reported ~ 15.6% water pollution reduction in the Venbanad Lake of Kerala province of India. These improvements were observed in many Indian states ( Uttrakhand, UttarPradesh, West Bengal, Karnataka, Tamilnadu ) because of very less number of visitors, drastic decrease in the volume of the untreated effluents (~ 500%) during lockdown periods (Somani et al. 2020 ).
Challenges of biomedical waste generation and its proper management amid COVID-19 pandemic
Apart from some environmental benefits, great negative impacts will be observed across the globe due to COVID-19 pandemic including public health crisis (WHO 2020a ) including hurdles in the recycling of the wastes (Calma 2020 ), economical emergency and unemployment (Atalan 2020 ), proper management and disposal of hospital wastes and need of extra disinfectants (Zambrano-Monserrate et al. 2020 ). Certainly, COVID-19 pandemic is one of the greatest challenges for everyone such as the scientists, industrialists, doctors, paramedical staffs, police, municipal authorities, government authorities as well as local public of the world. Since its beginning in 2019 from China, researchers of the world are working 24 h a day to develop effective medication/or vaccine against it. However, no any solution is reported till now against this virus (Vellingiri et al. 2020 ). Because of high mutagenic characters and continuous morphological changes in the COVID-19, development of its vaccine is facing difficulties (American Society of Microbiology 2020 ). Therefore, governments of most of the nations have imposed compulsory national lockdowns to keep safe their citizens except essential supplies of the goods and medicines. Apart from it, individual physical distancing and self-quarantine were also recommended for each person to ensure wellbeing (Balachandar et al. 2020 ). On the other hand, because of the lockdown, worldwide huge economical loss is expected in near future (Somani et al. 2020 ) due to closure of industries and manufacturing units (United Nations Industrial Development Organization 2020 ). Because of shutting industries, product supply chain of goods has been ruined (Kahlert and Bening 2020 ; Kulkarni and Anantharama 2020 ). In addition to huge economical loss, health workers and hospitals of the world (both developed and developing countries) are under tremendous pressure due to exponential rate of COVID-19 infections. Moreover, critical patients are not getting proper care due to unavailability of intensive care units in most of the hospitals. Health workers are using personal protective equipments (for example, face mask, transparent face shield, gloves etc.) to protect themselves from this virus and providing these safety devices are also a challenge for the authorities (Dargaville et al. 2020 ). Some misconceptions have been spread into the society that intake of lemon beverages, wine etc. can be used as medications against Coronavirus (Shammi et al. 2020 ). Moreover, in most of the countries, numbers of unemployed personas have been increased due to the pandemic (Kulkarni and Anantharama 2020 ). In order to handle these challenges, many governments are planning effective strategies for the sustainable development of the world after COVID-19 era (Rosenbloom and Markard 2020 ).
Owing to lockdown amid COVID-19 pandemic, world has gone under environmental reformation in terms of clean rivers and blue skies, whereas, this pandemic has created lots of problems in the management of solid waste (Gardiner 2020 ). Appropriate solid waste management has been a big challenge for the world especially to the developing nations. COVID-19 pandemic has boosted this problem many folds because of unexpected generations of waste materials (especially biomedical waste: a type of hazardous waste). It needs to be given extraordinary attentions by the waste management authorities and governments (Ferronato and Torretta 2019 ; Kaufman and Chasan 2020 ) as the compositions and volumes of the waste materials has been changed (Mallapur 2020 ). Moreover, Fan et al. ( 2021 ) reported that during COVID-19 pandemic many challenges have been emerged while managing waste materials because of changes observed in the volume, types, composition, disposal rate, frequency of collection, availability of treatment options, funds availability etc. as shown in Fig. 5 .

modified from Fan et al. 2021 )
Common challenges of infected waste management during pandemic (
In order to prevent transmission of COVID-19, lockdown was imposed in many countries which increased online shopping for the household products especially in developed countries. This panic situation has created a big concern of proper waste management in terms of collection, recycle, treatment as well as disposal (Zambrano-Monserrate et al. 2020 ; Nghiem et al. 2020 ). Moreover, Rahman et al. ( 2020 ) observed that hospital waste can cause severe environmental as well as public health problems as 5.2 million people of the world are dying annually due to mismanagement of hospital waste materials. During the pandemic, the composition of medical waste has changed drastically as it contains huge quantities of discarded masks, gloves, PPE kits etc. (UNEP 2020 ; Somani et al. 2020 ) and it could be dangerous for the society (especially workers of waste management authorities) in terms of increasing transmission due to mishandling of such types of infected wastes (Sharma et al. 2020 ). Similar, concern was also expressed by Occupational Safety and Health Administration (OSHA) regarding further infections among the workers of waste management authorities (OSHA 2020 ). Further, wastage of plastic waste also got increased across the world which is being used by pharmaceutical industries for packaging purpose (WHO 2020d ). Therefore, World Health Organization, Central Pollution Control Board (India), OSHA and other prestigious international organizations have developed new guidelines to manage the waste materials (especially hospital wastes) during COVID-19 (Somani et al. 2020 ; Kulkarni and Anantharama 2020 ). According to WHO, > 80% wastes of the hospitals were found in the category of noncontiguous wastes which can be treated and managed similar as municipal waste materials (WHO 2020d ). Normally, biomedical wastes are waste generated from the hospitals and veterinary medical premises including syringe, pathological materials, pharmaceutics etc. (Sharma et al. 2020 ; Somani et al. 2020 ). Due to COVID-19 pandemic, huge mass of plastic wastes has been increased across the world as it is being used in personal protection kits (for example, gloves, masks, face shield, ventilator etc.) (Klemeš et al. 2020 ). In India, waste management authorities are in more trouble due to fear of infection as safety measures are not good in the comparison of developed countries. During, lockdown in India, the bulk of biomedical waste was found to be greater than the municipal solid wastes (Somani et al. 2020 ). Significant reduction in municipal solid waste quantity was attributed to the shutdown of markets, shops, hotels, commercial premises, offices, transport etc. (Somani et al. 2020 ), whereas, huge amount of biomedical waste was generated probably because of high numbers of the COVID-19 infected persons admitted in the hospitals. In USA, huge quantities of food waste were generated during lockdown as most of the commercial institutes (like hotels, restaurants, mess etc.) had already purchased the raw materials (Kulkarni and Anantharama 2020 ). During lockdown, similar observations of change in the quantity and composition of waste materials have been reported from North America (SWANA 2020 ) and China (Klemeš et al. 2020 ). According to Klemeš et al. ( 2020 ), only in Hubei (China), around 370% increase in biomedical waste after COVID-19 infections. However, the quantity of municipal solid waste was generated less than 30% during pandemic. Nghiem et al. ( 2020 ) and Zambrano-Monserrate et al. ( 2020 ) have also studied the change in the waste composition (and quantity) along with their negative impacts of change in waste generation on the environment and health workers. They found that transmission of virus in community has significantly affected waste recycling facilities around the world. For instance, in United Kingdom, 46% material recovery process was stopped due to lockdown amid COVID-19 pandemic and similarly 31% recycling units of USA were also closed in the similar situations (Somani et al. 2020 ).
Contagious biomedical wastes can spread disease in living organisms and their mishandling may also be responsible for soil contamination, water pollution (both groundwater and surface water), injuries and death of ecofriendly microbes (Datta et al. 2018 ). Incineration is one of the preferred options for the waste management especially biomedical (or infectious) wastes in developed countries as shown in Fig. 6 .
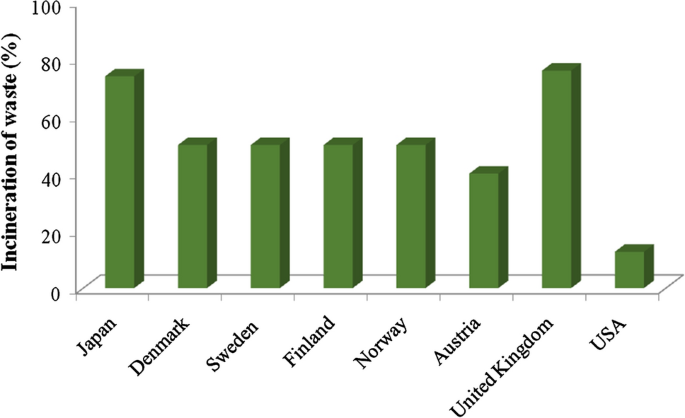
Proportion of incineration for energy recovery in developed countries before COVID-19 pandemic
From the above figure, it is visible that Japan used to treat municipal solid waste through 74% incineration, 17% recycling and only 3% as landfill disposal before the pandemic (Mollica and Balestieri 2020 ). In Wuhan (China), normally 40 tons of biomedical waste was generated every day and after COVID-19 infections, it was reached up to 240 tons/day. Therefore, the increase in infectious wastes was around 6 times more as compared to normal days. This huge bulk of medical waste created big challenge to the management authorities as Wuhan administration could incinerate only 49 tons (maximum) of waste every day. Moreover, this will not be economical for any country as the costs of incineration for hazardous and municipal solid wastes in China were calculated as 281.7–422.6 USD/tons and 14.1 USD/tons, respectively (Tang 2020 ; Klemeš et al. 2020 ). According to WHO ( 2017 ), usually, 85% biomedical wastes are not hazardous in nature, rest 10% may be infectious along with 5% radioactive wastes. Before pandemic, except USA (12.7% only) (United States Environmental Protection Agency 2017 ), many developed countries incinerate their waste materials to recover energy such as 50% municipal waste incinerated in Denmark, Finland, Norway and Sweden (Istrate et al. 2020 ); 40% in Austria (Kyriakis et al. 2019 ); 76% in United Kingdom (DEFRA Government of UK 2020 ). However, recycling of the waste reported 32% in Austria (including composting) (Kyriakis et al. 2019 ); 45% in United Kingdom (DEFRA Government of UK 2020 ), and 35.2% in USA (both recycling and composting) (United States Environmental Protection Agency 2017 ). Therefore, it can be seen from the above results that collection and recycling of waste materials has been disturbed due COVID-19 pandemic. Moreover, pandemic has caused huge economical losses by many ways to the affected countries along with an unseen fear of its infections. Datta et al. ( 2018 ) studied that in India by the year 2017, 500 MT/day biomedical wastes were generated and infrastructure of managing biomedical waste is not good. Hence, based on the data of biomedical waste generated in Wuhan (> 6 times) during pandemic, India this situation is expected. However, till now biomedical waste generation data is not available for whole India (Somani et al. 2020 ). Further, according to one Indian leading newspaper in Gurugram (India), only in 2 months of pandemic, the quantity of biomedical wastes has increased around 40 times as compared to normal months. Similarly, before pandemic 550–600 kg biomedical waste was generated every day in Ahmadabad. Now, it has already increased up to 1000 kg/day during pandemic with an expectation of reaching up to 3000 kg/day especially in the red zones (COVID-19 containment zones (TOI 2020 ; Somani et al. 2020 ). Tables 1 and 2 shows the biomedical waste generation in some Asian cities and Indian cities/states.
From Table 1 , it can be seen that around every Asian city, the quantity of biomedical wastes has been increased many folds during the outbreak of COVID-19 in the community. In terms of maximum additional biomedical waste was generated in the capital of Philippines, i.e., Manila followed by Jakarta (Indonesia). In, Wuhan (China) and Bangkok (Thailand), 210 tons of additional biomedical waste was generated amid COVID-19 pandemic (ADB 2020 ). Improper medical waste handling may increase the number of COVID-19 infections in the community (Peng et al. 2020 ) due to presence of pathogenic microbes (Windfeld and Brooks 2015 ). Due to airborne infections of the COVID-19 virus in healthy people, use of masks, gloves, face cover etc. has been also increased up to dangerous levels in the world (Bourouiba 2020 ). At global level, 89 million masks and 76 million gloves are required against the protection from COVID-19 infection (WHO 2020c ). According to UNEP ( 2020 ), appropriate management of extra waste materials generated during COVID-19 pandemic has become a major concern for the countries. Therefore, medical wastes from the COVID-19 affected zones/hospitals need to be disinfected with careful handling. Treatment of medical waste can be carried out by using thermal techniques such as autoclaving, incineration, microwave and plasma method. However, selection above processes of waste treatment will be governed by many factors like economic feasibility, easy and safe handling, eco-friendly nature as well as harmless to the society (Liu et al. 2015 ). In order to reduce the chance of infection in the community, effective medical waste (or infectious waste) management should be adapted. Apart from collection and transport, trained manpower should be involved in this activity and disinfection of infectious waste should be compulsory (Klemeš et al. 2020 ).
The waste management as well as waste recycling process of the developed nations has been disturbed due to this COVID-19 outbreak. Figure 7 shows the waste management practices adapted by developed countries.
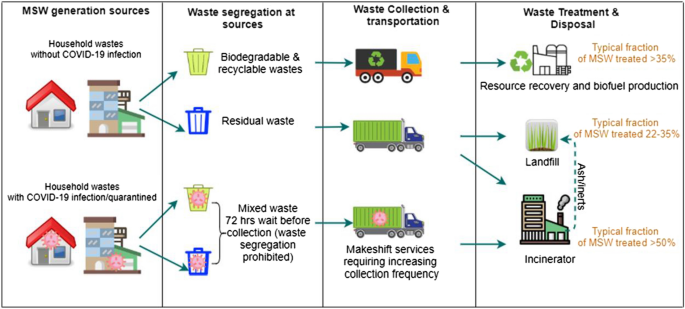
Management practices for solid wastes in some developed countries (ACRPlus 2020 ; Nghiem et al. 2020 ; Kulkarni and Anantharama 2020 ). (Reprinted from Kulkarni and Anantharama 2020 with permission from Elsevier)
From Fig. 7 , it can be seen that in developed countries waste management practice involves segregation of the waste at the source of generation followed by their effective collection, transpiration, treatment and disposal. However, during COVID-19 outbreak, the waste collection guidelines were changed as segregation and collection of the wastes from the infected area is carried out after a waiting period of 72 h (ACRPlus 2020 ; Nghiem et al. 2020 ). In most of the Asian countries like Bangladesh, India, Indonesia, Malaysia, Myanmar and Thailand, municipal solid wastes are getting managed by land-filling (Yadav and Samadder 2018 ). Integrated solid waste management system can be a good alternative for the recycling of wastes and also producing energy from the waste materials (Ramachandra et al. 2018 ). Lack of scientific designing of land-fill sites for waste disposal may lead several environmental problems such as air pollution, water pollution, soil pollution, marine pollution and vector borne-diseases among humans (Pujara et al. 2019 ). Therefore, mishandling of the biomedical wastes will be more dangerous as it may cause infections in the living organisms.
Biomedical waste management is a big challenge for every country especially during this pandemic time. According to the WHO, most of the developing countries do not have advanced systems for the management of biomedical wastes (Chartier et al. 2014 ). Chartier et al. ( 2014 ) proposed a close pit (as shown in Fig. 8 a) which should have a dimension of 2 m and 3 m and can be made by clay or geo-synthetic materials used at the base. This arrangement can be used for the safe management of biomedical wastes in emergency situations such as COVId-19 pandemic.
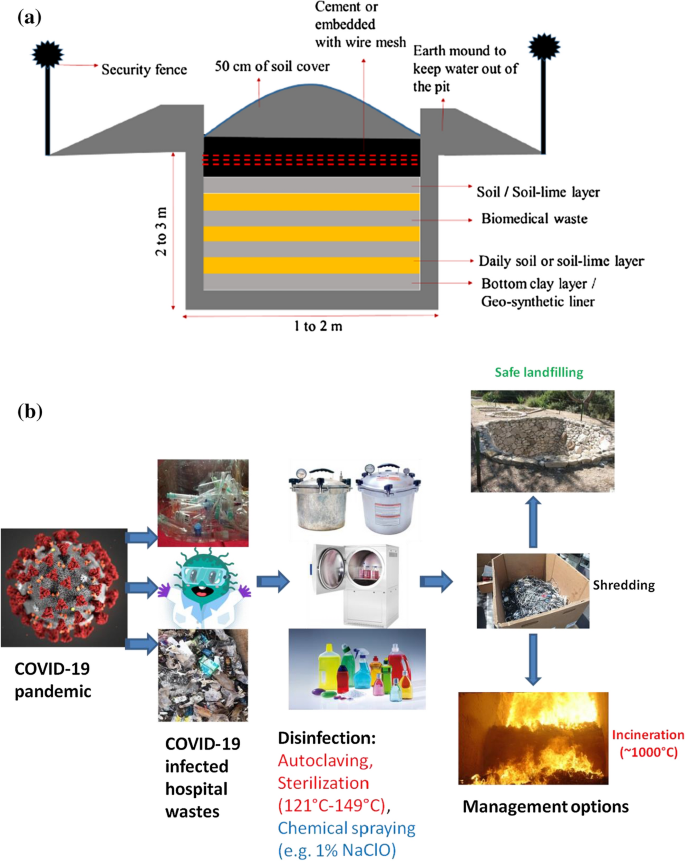
a Layout of a pit for onsite disposal of biomedical wastes in low-income countries during COVID-19 like emergency situation (Chartier et al. 2014 ; Sharma et al. 2020 ). (Reprinted from Sharma et al. 2020 with permission from Elsevier). b COVID-19 infected waste handling procedure for low income countries
Figure 8 a gives a temporary arrangement for the effective and safe disposal of biomedical wastes in low-income countries (Chartier et al. 2014 ; Sharma et al. 2020 ). Further, Fig. 8 b can be adopted during the handling infected hospital wastes.
Figure 8 b gives a detail outline for the management of infected wastes generated during the pandemic like COVID-19. In this diagram, it can be seen that disinfection of hospital waste has become very important as recommended by many government authorities of the world. For disinfection, autoclaving and sterilization of the tools can be carried out at the temperature ranged between 121 and 149 °C or with the spraying of 0.1% of NaClO. After, disinfection processes, the medical wastes can be shredded and incinerated (~ 1000 °C temperature) followed by ultimate disposal in landfills. Further, incineration has been considered as the best method for the treatment of hazardous wastes (e.g. medical wastes) as it will condense the weight along with volume of the wastes (Rajor et al. 2012 ). Even, US Environmental Protection Agency (USEPA 2020 ) issued special guidelines for managing food wastes of residential colonies and other commercial buildings during pandemic. Similarly, Government of India issued guidelines for the management of waste products generated during sudden lockdown. These wastes included perishable agricultural products as well (FAO 2020 ). According to Klemeš et al. ( 2020 ), environment and human health can be protected well after appropriate waste management. Hospital or infectious wastes can be managed effectively through proper collection, transport, treatment and final disposal. It also requires trained health workers who should be aware about the proper disinfection process along with self-protection too. Wasted PPE kits volume can also be decreased, if these materials (like antiviral masks, face shields etc.) can be reused after disinfections (Goel et al. 2020 ).Previously, viral disinfection was achieved by using UV-C rays (at 254 nm) in 40 min (Darnell et al. 2004 ), but in case of COVID-19, it is a matter of exploration. Moreover, it was also reported that UV-C rays can lead skin and eye disorders. Therefore, it must be examined before suggesting the application of UV-C rays as a disinfectant (Goel et al. 2020 ).Thermal treatment of waste can be an alternative for their management as it will generate energy along with reducing waste volume by 80–95%, and mineralization etc. (Singh et al. 2011 ; Brunner and Rechberger 2015 ; World Bank 2018 ). Implementation of these technologies were successful in some developed and developing countries and land-filling has become a rare practice in the developed nations because of land scarcity or/and environmental pollutions. Further, due to high investments, in developing countries it is still inaccessible (Mayer et al. 2019 ). Apart from the above advantages, incineration generates the ash residues which may contain toxic metals etc. Similarly, groundwater contamination may happen due to the disposal of such residues in the landfills (Rajor et al. 2012 ). Dargaville et al. ( 2020 ) recommended some steps to reduce the wastage of PPE kits which includes:
To explore the possibility of recycling of PPE kits (gloves, mask, face shield etc.);
Disinfection should be ensured before recycling
One of the best disinfection methods should be shared with everyone (especially medical workers)
Material’s properties should be examined before recycling
Fix the guidelines for their number of recycling
Exchange of recycled materials should not be allowed
Time to time expert’s (material science, clinical doctors, virologist etc.) guidelines should be shared.
These are the general guidelines to be followed everywhere to reduce the quantity of medical wastes along with the human health and environmental protections (Dargaville et al. 2020 ).According to WHO, thermal treatment and/or application of conventional biocidal materials can be integrated with waste treatment systems for inactivating Coronavirus before the disposal of biomedical wastes (Kampf et al. 2020 ). Apart from these options of biomedical waste management; some extra efforts are needed to upgrade the existing waste management systems so that it can deal with emergency situations like this pandemic (COVID-19).
Some challenges observed as wastes are also generated from the mildly infected or asymptomatic people that may have viral infections. COVID-19 virus can be present in active form for different time periods (few hours to days) on the cardboards, plastic materials and metallic objects (Kampf et al. 2020 ; Doremalen et al. 2020 ; Nghiem et al. 2020 ). Somani et al. ( 2020 ) observed other waste materials which may be considered as infectious in nature, if not treated properly. These wastes are syringe, needles, masks, gloves, medicines, discarded materials from the home quarantine patients etc. Mishandling of these wastes may trigger the chance of more infections in public as well as health workers (Sharma et al. 2020 ; Kulkarni and Anantharama 2020 ).Further studies have shown that in between 21 and 23 °C temperature in presence of 40% relative humidity, the survival time of Coronavirus was 7 days. However, in atmosphere, with 65% relative humidity the activation time was drastically reduced up to 3 h with same temperature range (Doremalen et al. 2020 ). Kampf et al. ( 2020 ) reported 9 days active period of Coronavirus on the metal, glass or plastic. Further, Chin et al. ( 2020 ) found that at 70 °C, COVID-19 virus did not survive more than 5 min. National Biodefense Analysis and Countermeasures Centre, USA found in the initial studies that direct sunlight can be very effective to inactivate the Coronavirus within minutes from the many surfaces (Goel et al. 2020 ). Better management of the wastes can be carried out by optimizing the decision process, infrastructure, upgrading treatment methods and other activities related with the biological disasters like COVID-19 (Klemeš et al. 2020 ).
Provisions for biomedical waste management in India amid COVID-19
According to Bio-Medical Waste Management Rules, 2016 passed by Indian parliament data of biomedical waste generation should be updated on daily basis by the health care service providers and also, they must expose monthly information on their website (BMWM 2016 ). These rules were amended at time to time as per the need of the hour to make the effective biomedical waste management in the country. Amid COVID-19 pandemic, like other countries, Indian government has also taken many initiations for the purpose of quarantine, isolation, sampling, laboratory works etc. These initiatives were in agreement with the guidelines of various international (WHO, CDC etc.) and national agencies (MoH&FW, ICMR, CPCB etc.) such as application of separate colour storage basket or double layered bags with proper labelling, separate collection for biomedical wastes etc. During COVID-19 pandemic, some activities were recommended for the rapid and effective waste management by the Indian government to reduce the chance of further infections such as use PPE kits especially by the health workers/waste management people, providing training for their safety, record maintenance, extra working times for treatment facilities etc. (Soni 2020 ). CPCB has developed a mobile app, i.e., ‘COVID19BWM’ for the daily updation of the generation of biomedical wastes from COVID-19 related places. Moreover, 0.5% chlorine solution was recommended for the disinfection purpose where the patients wards. However, COVID-19 waste and their storage places should be disinfected with 1% sodium hypochlorite solution on daily basis (CPCB 2020b ). These guidelines were revised again (on July 17, 2020) and some significant amendments were carried out to fight with the COVID-19 virus such as rail coaches can also be used as isolation wards the materials used by COVID-19 patients included in the category of biomedical waste and their treatment should be mandatory as per the guidelines provided by CPCB and yellow bags can be used for their collection. It was mandatory that do not mix the municipal solid wastes with the waste generated from the COVID-19 infected places/homes (CPCB 2020c ). There, it can be said that despite of being a developing nation, Indian authorities are also doing lots of efforts to reduce the numbers of COVID-19 infections in the community.
Amid COVID-19, world has gone under environmental reformation in terms of clean rivers and blue skies, whereas, this pandemic has hurdled the appropriate solid waste management process and the same has emerged as a big threat for the world especially to the developing nations. Researchers have suggested some steps to reduce the wastage of biomedical waste and explored the mechanisms of safe and hygienic recycling. As advised by the WHO, developing countries, who are deficient of advanced systems for the management of biomedical wastes should follow the temporary solution of a close pit with a dimension of 2 m and 3 m and can be made by clay or geo-synthetic materials used at the base and the same arrangement can be used for the safe management of biomedical wastes in emergency situations such as COVId-19 pandemic wastes in emergency situations. The paper summarizes that better management of the wastes can be carried out by optimizing the decision process, infrastructure, upgrading treatment methods and other activities related with the biological disasters like COVID-19. National Biodefense Analysis and Countermeasures Centre, USA found in the initial studies that direct sunlight can be very effective to inactivate the Coronavirus within minutes from the many surfaces. Hospital or infectious wastes can be managed effectively through proper collection, transport, treatment and final disposal. The health workers must be trained enough and should be aware about the proper disinfection process along with self-protection too. Wasted PPE kits volume can also be decreased by reusing the same after disinfections. As achieved in the past for viral disinfection, the use of UV-C rays with proper precautions can also be explored for COVID-19 disinfection. Waste management especially for biomedical waste management, thermal treatment of waste can be an alternative, as it can generate energy along with reducing waste volume by 80–95%.
ACRPlus-Association of Cities and Regions for Sustainable Resource Management (2020) Municipal waste management and COVID-19. https://www.acrplus.org/en/municipal-waste-management-covid-19 . Accessed 4 May 2020
ADB (2020) Asian Development Bank. Managing infectious medical waste during the COVID-19 pandemic. https://www.adb.org/sites/default/files/publication/578771/managingmedical-waste-covid19.pdf . accessed 4 May 2020
Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH (2020) The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. https://doi.org/10.1007/s11469-020-00270-8
Article Google Scholar
Amanat F, Krammer F (2020) SARS-CoV-2 vaccines: status report. Immunity 52(4):83–589. https://doi.org/10.1016/j.immuni.2020.03.007
Article CAS Google Scholar
American Society of Microbiology (2020). https://asm.org/PressReleases/2020/COVID-19 . Accessed Aug 10 2021
Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD (2020) How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 395(10228):931–934
Ardakani AA, Kanafi AR, Acharya UR, Khadem N, Mohammadi A (2020) Application of deep learning technique to manage COVID-19 in routine clinical practice using CT images: results of 10 convolutional neural networks. Comput Biol Med 30:103795
Armitage R, Nellums LB (2020) COVID-19 and the consequences of isolating the elderly. Lancet Public Health 5(5):e256. https://doi.org/10.1016/S2468-2667(20)30061-X
Atalan A (2020) Perspective—Is the lockdown important to prevent the COVID-19 pandemic? Effects on psychology, environment and economy-perspective. Ann Med Surg 56:38–42
Balachandar V, Kaavya J, Mahalaxmi I, Arul N, Vivekanandhan G, Bupesh G, Singaravelu G, Anila V, Dhivya V, Harsha G, Kamarajan R (2020) COVID-19: a promising cure for the global panic. Sci Total Environ 725:138277
Bhatia A, Bhaskar S (2020) Coronavirus outbreak explained: are air conditioners safe to use during the COVID-19 pandemic. NDTV. https://swachhindia.ndtv.com
BMWM (2016) Bio-medical waste management rules, 2016. Ministry of Environment, Forest & Climate Change, Delhi – 110032, India. Dated 19 Feb 2020
Bourouiba L (2020) Turbulent gas clouds and respiratory pathogen emissions. Potential implications for reducing transmission of COVID-19. J Am Med Assoc. https://doi.org/10.1001/jama.2020.4756
Bremer S, Schneider P, Glavovic B (2019) Climate change and amplified representations of natural hazards in institutional cultures. Oxf Res Encycl Nat Hazard Sci. https://doi.org/10.1093/acrefore/9780199389407.013.354
Brunner PH, Rechberger H (2015) Waste to energy—key element for sustainable waste management. Waste Manag 37:3–12. https://doi.org/10.1016/j.wasman.2014.02.003
Callaway E, Cyranoski D, Mallapaty S, Stoye E, Tollefson J (2020) Coronavirus by the numbers. Nature 579:482
Calma J (2020) https://www.theverge.com/2020/3/26/21194647/the-covid-19-pandemic-is-generating-tons-of-medical-waste
Casanova L, Rutala WA, Weber DJ, Sobsey MD (2009) Survival of surrogate coronaviruses in water. Water Res 43(7):1893–1898
Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Napoli RD (2020) Features, evaluation and treatment Corona Virus (COVID-19), NCBI Bookshelf. StatPearls Publishing, Treasure Island, FL
Google Scholar
CDC (2020) https://www.ecdc.europa.eu/sites/default/files/documents/RRA-sixth-updateOutbreak-of-novel-coronavirus-disease-2019-COVID-19.pdf . Accessed 5 July 2020
Chakraborty I, Maity P (2020) COVID-19 outbreak: migration, effects on society, global environment and prevention. Sci Total Environ 728:138882
Chan WC (2020) Nano research for COVID-19. ACS Nano 14(4):3719–3720. https://doi.org/10.1021/acsnano.0c02540
Chartier Y, Emmanuel J, Pieper Ute PA, Philip R, Ruth S, William T, Wilburn S, Zghondi R (2014) Safe management of wastes from health-care activities. WHO, Geneva
Chen K, Wang M, Huang C, Kinney PL, Anastas PT (2020) Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health 4(6):e210–e212
Chin AW, Chu JT, Perera MR, Hui KP, Yen HL, Chan MC, Peiris M, Poon LL (2020) Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe 1(1):10
Corletta RT, Primack RB, Devictor V, Maasd B, Goswami VR, Bates AE, Koh LP, Regani TJ, Loyolaj R, Pakemanl RJ, Cummingm GS, Pidgeon A, Johns D, Roth R (2020) Impacts of the coronavirus pandemic on biodiversity conservation. Biol Conserv 246:108571
CPCB (2020a) Report on assessment of impact of lock down on water quality of river Yamuna- Delhi stretch. Central Pollution Control Board, Ministry of Environment, Forests and Climate Change, Delhi – 110032
CPCB (2020b) Guidelines for handling, treatment, and disposal of waste generated during treatment/diagnosis/quarantine of COVID-19 patients—Rev. 3, dated 10 June 2020b. Central Pollution Control Board, (Ministry of Environment, Forest & Climate Change), Delhi – 110032, India
CPCB (2020c) Guidelines for handling, treatment and disposal of waste generated during treatment/diagnosis/quarantine of COVID-19 patients—Rev. 4, dated 17 July 2020c. Central Pollution Control Board, (Ministry of Environment, Forest & Climate Change), Delhi – 110032, India
Dantas G, Siciliano B, França BB, da Silva CM, Arbilla G (2020) The impact of COVID-19 partial lockdown on the air quality of the city of Rio de Janeiro, Brazil. Sci Total Environ. https://doi.org/10.1016/j.scitotenv.2020.139085
Dargaville T, Spann K, Celina M (2020) Opinion to address a potential personal protective equipment shortage in the global community during the COVID-19 outbreak. Polymer Degrad Stab 176:109162
Darnell ME, Subbarao K, Feinstone SM, Taylor DR (2004) Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV. J Virol Methods 121(1):85–91
Datta P, Mohi GK, Chander J (2018) Biomedical waste management in India: critical appraisal. J Lab Physicians 10(1):6–14
DEFRA-Department for Environment Food & Rural Affairs, Government of UK (2020) UK statistics on waste. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/874265/UK_Statistics_on_Waste_statistical_notice_March_2020_accessible_FINAL_rev_v0.5.pdf
Dhama K, Sharun K, Tiwari R et al (2020) Coronavirus disease 2019—COVID-19. Preprints. https://doi.org/10.20944/preprints202003.0001.v1
Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, Wit E, Munster VJ (2020) Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. N Engl J Med. https://doi.org/10.1101/2020.03.09.20033217
Duan L, Zhu G (2020) Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychol 7(4):300–302
Elavarasan RM, Pugazhendhi R (2020) Restructured society and environment: a review on potential technological strategies to control the COVID-19 pandemic. Sci Total Environ 725:138858
EPCA (2020) The Environment Pollution (Prevention and Control) Authority (EPCA). https://www.epca.org.in/EPCA-Reports1999-1917/EPCA-reportno-112.pdf . Accessed on 17 Dec 2020
Fan VY, Jiang P, Hemzal M, Klemeš JJ (2021) An update of COVID-19 influence on waste management. Sci Total Environ 754:142014
FAO (2020) Food and Agriculture Organization of the United Nations. Local food systems and COVID-19; a glimpse on India's responses. http://www.fao.org/in-action/foodfor-cities-programme/news/detail/en/c/1272232/
Ferronato N, Torretta V (2019) Waste mismanagement in developing countries: a review of global issues. Int J Environ Res Public Health 16(6):1060
Ford T, Vizard T, Sadler K et al (2020) Data resource profile: the mental health of children and young people surveys (MHCYP). Int J Epidemiol. https://doi.org/10.1093/ije/dyz259
Gardiner B (2020) Pollution made COVID-19 worse. Now, lockdowns are clearing the air. National Geographic. https://www.nationalgeographic.com/science/2020/04/pollution-made-the-pandemic-worse-but-lockdowns-clean-the-sky/ . Accessed 15 May 2020
Gates B (2020) Responding to Covid-19—a once-in-a-century pandemic? N Engl J Med 382(18):1677–1679
Global Climate report (2019) https://www.ncdc.noaa.gov/sotc/global/201913
Goel S, Hawi S, Goel G, Thakur VK, Agrawal A, Hoskins C, Pearce O, Hussain T, Upadhyaya HM, Cross G, Barber AH (2020) Resilient and agile engineering solutions to address societal challenges such as coronavirus pandemic. Mater Today Chem 17:100300
Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Silver RC, Everall I, Ford T (2020) Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 7:547–560. https://doi.org/10.1016/S2215-0366(20)30168-1
Hopman J, Allegranzi B, Mehtar S (2020) Managing COVID-19 in low-and middle-income countries. JAMA 323(16):1549–1550
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet 395(10223):497–506
Istrate I-R, Iribarren D, Galvez-Martos J-L, Dufour J (2020) Review of life-cycle environmental consequences of waste-to-energy solutions on the municipal solid waste management system. Resour Conser Recov 157:104778. https://doi.org/10.1016/j.resconrec.2020.104778
Kahlert S, Bening CR (2020) Plastic recycling after the global pandemic: resurgence or regression? Resour Conserv Recycl 160:104948. https://doi.org/10.1016/j.resconrec.2020.104948
Kampf G, Todt D, Pfaender S, Steinmann E (2020) Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 104:246–251. https://doi.org/10.1016/j.jhin.2020.01.022
Katariya M (2020) 10 Things that have happened for the first time in years during the coronavirus lockdown. Scoopwhoop, https://www.scoopwhoop.com/news/things-that-have-happened-for-the-first-time-inyearsduring-coronavirus-lockdown/
Kaufman L, Chasan E (2020) Cities wonder whether recycling counts as essential during the virus. Bloomberg Green. https://www.bloomberg.com/news/articles/2020-03-27/cities-wonder-whether-recycling-counts-as-essential-during-the-virus . Accessed 26 April 2020
Kerimray A, Baimatova N, Ibragimova OP, Bukenov B, Kenessov B, Plotitsyn P, Karaca F (2020) Assessing air quality changes in large cities during COVID-19 lockdowns: the impacts of traffic-free urban conditions in Almaty, Kazakhstan. Sci Total Environ 730:139179. https://doi.org/10.1016/j.scitotenv.2020.139179
Klemeš JJ, Van Fan Y, Tan RR, Jiang P (2020) Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew Sustain Energy Rev 127:109883
Kulkarni BN, Anantharama V (2020) Repercussions of COVID-19 pandemic on municipal solid waste management: challenges and opportunities. Sci Total Environ 743:140693
Kyriakis E, Psomopoulos C, Kalkanis K (2019) Investigating the correlation of purchase power parity with the adopted waste management method in EU28. J Soc Sci 8:162. https://doi.org/10.3390/socsci8050162
Lee PI, Hu YL, Chen PY, Huang YC, Hsueh PR (2020) Are children less susceptible to COVID-19? J Microbiol Immunol Infect. https://doi.org/10.1016/j.jmii.2020.02.011
Liu HC, You JX, Lu C, Chen YZ (2015) Evaluating health-care waste treatment technologies using a hybrid multi-criteria decision making model. Renew Sustain Energy Rev 41:932–942
Lokhandwala S, Gautam P (2020) Indirect impact of COVID-19 on environment: a brief study in Indian context. Environ Res 188:109807
Mahajan P, Kaushal J (2020) Epidemic trend of COVID-19 transmission in India during lockdown-1 phase. J Commun Health. https://doi.org/10.1007/s10900-020-00863-3
Mahato S, Pal S, Ghosh KG (2020) Effect of lockdown amid COVID-19 pandemic on air quality of the megacity Delhi, India. Sci Total Environ 730:139086. https://doi.org/10.1016/j.scitotenv.2020.139086
Mallapur C (2020) Sanitation workers at risk from discarded medical waste related to COVID-19. IndiaSpend. https://www.indiaspend.com/sanitation-workersat-risk-from-discarded-medical-waste-related-tocovid-19/
Mayer F, Bhandari R, Gath S (2019) Critical review on life cycle assessment of conventional and innovative waste-to-energy technologies. Sci Total Environ 672:708–721. https://doi.org/10.1016/j.scitotenv.2019.03.449
Ministry of Health and Family Welfares (MoHFW), Government of India (2020) COVID-19 INDIA. https://www.mohfw.gov.in/
Mishra RK, Parida M, Rangnekar S (2010) Evaluation and analysis of traffic noise along bus rapid transit system corridor. Int J Environ Sci Technol 7(4):737–750. https://doi.org/10.1007/BF03326183
Mollica GJG, Balestieri JAP (2020) Is it worth generating energy with garbage? Defining a carbon tax to encourage waste-to-energy cycles. Appl Therm Eng 173:115195. https://doi.org/10.1016/j.applthermaleng.2020.115195
Myllavirta L, Dahiya S (2020) Analysis: India's CO2 emissions fall for first time in four decades amid coronavirus. Carbon Brief, https://www.carbonbrief.org/analysis-indias-co2-emissions-fall-for-first-time-in-four-decades-amidcoronavirus#
National Aeronautics and Space Administration (NASA) (2020) Airborne particle levels plummet in Northern India. Retrieved on 11 May 2020 from https://earthobservatory.nasa.gov/images/146596/airborne-particle-levels-plummet-innorthern-india
National Environment Agency Singapore (2020)Waste management-public waste collection services during circuit breaker. https://www.nea.gov.sg/our-services/wastemanagement/overview .
Nghiem LD, Morgan B, Donner E, Short MD (2020) The COVID-19 pandemic: considerations for the waste and wastewater services sector. Case Stud Chem Environ Eng. https://doi.org/10.1016/j.cscee.2020.100006
Occupational Safety and Health Administration (OSHA) (2020) Guidance on Preparing Workplaces for COVID-19
Paital B, Das K, Parida SK (2020) Review-Inter nation social lockdown versus medical care against COVID-19, a mild environmental insight with special reference to India. Sci Total Environ 728:138914
Peng L, Liu J, Xu W, Luo Q, Chen D, Lei Z, Huang Z, Li X, Deng K, Lin B, Gao Z (2020) SARS-CoV-2 can be detected in urine, blood, anal swabs, and oropharyngeal swabs specimens. J Med Virol. https://doi.org/10.1002/jmv.25936
Polk HS (2019) State of global air 2019: a special report on global exposure to air pollution and its disease burden. Health Effects Institute, Boston, MA
Pujara Y, Pathak P, Sharma A, Govani J (2019) Review on Indian Municipal Solid Waste Management practices for reduction of environmental impacts to achieve sustainable development goals. J Environ Manage 248:109238
Qu G, Li X, Hu L, Jiang G (2020) An imperative need for research on the role of environmental factors in transmission of novel coronavirus (COVID-19). Environ Sci Technol 54:3730–3732
Rahman MM, Bodrud-Doza M, Griffiths MD, Mamun MA (2020) Biomedical waste amid COVID-19: perspectives from Bangladesh. Lancet Glob Health 8(10):e1262
Rajor A, Xaxa M, Mehta R (2012) An overview on characterization, utilization and leachate analysis of biomedical waste incinerator ash. J Environ Manage 108:36–41
Ramachandra TV, Bharath HA, Kulkarni G, Han SS (2018) Municipal solid waste: generation, composition and GHG emissions in Bangalore, India. Renew Sustain Energy Rev 82:1122–1136. https://doi.org/10.1016/j.rser.2017.09.085
Randall I (2020) Sound of the sea: underwater noise pollution from ships plummets during the coronavirus lockdown offering respite for 'stressed' whales and other marine life. The Daily Mail. https://mol.im/a/8262147
Rodriguez-Morales A, Tiwari R, Sah R, Dhama K (2020) COVID-19, an emerging coronavirus infection: current scenario and recent developments—an overview. J Pure Appl Microbiol 14:6150
Rosenbloom D, Markard J (2020) A COVID-19 recovery for climate. Science 368(6490):447. https://doi.org/10.1126/science.abc4887
Roujian L, Xian Z, Juan L et al (2020) Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 395:565–574
Shammi M, Bodrud-Doza M, Islam ARMT, Rahman MM (2020) COVID-19 pandemic, socioeconomic crisis and human stress in resource-limited settings: a case from Bangladesh. Heliyon 6:e04063
Sharma HB, Vanapalli KR, Cheela VS, Ranjan VP, Jaglan AK, Dubey B, Goel S, Bhattacharya J (2020) Challenges, opportunities, and innovations for effective solid waste management during and post COVID-19 pandemic. Resour Conser Recycl 162:105052
Singh RP, Tyagi VV, Allen T, Ibrahim M, Kothari R (2011) An overview of exploring the possibilities of energy generation from municipal solid waste (MSW) in Indian scenario. Renew Sustain Energy Rev 15:4797–4808. https://doi.org/10.1016/j.rser.2011.07.071
Singh AK, Singh A, Shaikh A, Singh R, Misra A (2020) Chloroquine and hydroxychloroquine in the treatment of COVID-19 with or without diabetes: a systematic search and a narrative review with a special reference to India and other developing countries. Diab Metab Syndr Clin Res Rev 14:241–246
Sinha SN, Paul D, Biswas K (2016) Effects of Moringaoleifera Lam. and Azadirachtaindica A. Juss. leaf extract in treatment of tannery effluent. Our Nat 14:47–53
Sohrabi C, Alsafi Z, O’Neill N, Khan M, Kerwan A, Al-Jabir A, Iosifidis C, Agha R (2020) Review- World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg 76:71–76
Somani M, Srivastava AN, Gummadivalli SK, Sharma A (2020) Indirect implications of COVID-19 towards sustainable environment: an investigation in Indian context. Bioresour Technol Rep 11:100491
Soni DK (2020) Regulatory interventions in Covid-19 waste management in India. Natl J Life Sci 17(1):5–7
SWANA - Solid Waste Association of North America article (2020) SWANA reminds all state and local governments that solid waste management is an essential public service. https://swana.org/news/swana-news/article/2020/03/19/swana-reminds-allstate-and-localgovernments-that-solid-waste-management-is-an-essential-publicservice
Tang W (2020) The medical waste related to COVID-2019 is cleaned up every day—the medical waste treatment market needs to be standardised. 21st Century Business Herald; 2020. www.21jingji.com/2020/3-12/xNMDEzODFfMTU0MjIxNQ.html
Times of India (TOI) (2020) 350 Tonnes of trash disappear from streets of Ahmedabad. http://timesofindia.indiatimes.com/articleshow/75039037.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst
UNEP (2020) BASEL: waste management an essential public service in the fight to beat COVID-19. The United Nations Environment Programme (UNEP) and The Basel Convention. http://www.basel.int/Implementation/PublicAwareness/PressReleases/WastemanagementandCOVID19/tabid/8376/Default.aspx
United Nations Industrial Development Organization (UNIDO) (2020) India's manufacturing reels from the impact of COVID-19. https://www.unido.org/stories/indias-manufacturingreelsimpact-covid-19
United Nations (2020) The Social Impact of COVID-19. Department of Economics and Social Affairs. https://www.un.org/development/desa/dspd/2020/04/social-impact-ofcovid-19
United States Environmental Protection Agency (2020) Recycling and sustainable management of food during COVID-19 public health emergency. https://www.epa.gov/coronavirus/recycling-and-sustainable-management-food-duringcoronaviruscovid-19-public-health
United States Environmental Protection Agency (2017) National overview: facts and figures on materials, wastes and recycling. https://www.epa.gov/facts-and-figuresabout-materials-waste-and-recycling/national-overview-facts-and-figures-materials . Accessed 10 May 2020.
Vellingiri B, Jayaramayya K, Iyer M, Narayanasamy A, Govindasamy V, Giridharan B, Ganesan S, Venugopal A, Venkatesan D, Ganesan H, Rajagopalan K (2020) COVID-19: a promising cure for the global panic. Sci Total Environ 725:138277
Weber DJ, Rutala WA, Fischer WA, Kanamori H, Sickbert-Bennett EE (2016) Emerging infectious diseases: focus on infection control issues for novel coronaviruses (Severe Acute Respiratory Syndrome-CoV and Middle East Respiratory Syndrome-CoV), hemorrhagic fever viruses (Lassa and Ebola), and highly pathogenic avian influenza viruses, A(H5N1) and A(H7N9). Am J Infect Control 44(5):E91–E100
WHO (2017) Report on health-care waste management (HCWM) status in Countries of the South-East Asia Region (SEA-EH-593). The World Health Organization. https://apps.who.int/iris/handle/10665/258761 .
WHO (2018) World Health Organization. Global status report on alcohol and health. https://www.who.int/substance_abuse/publications/global_alcohol_report/en/ .
WHO, 2020a. Pneumonia of unknown cause- China. World Health Organization.
WHO (2020b) Coronavirus Disease (COVID-2019) Situation Reports-67. World Health Organization
WHO (2020c) World Health Organization. WHO-Director-general-s-opening-remarks-at-the-media briefing-on-covid-19. www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19
WHO (2020d) Water, sanitation, hygiene, and Waste Management For the COVID-19 virus: interim guidance, 23 April 2020d (No. WHO/2019-nCoV/IPC_WASH/2020.3).WorldHealth Organization URL. https://apps.who.int/iris/bitstream/handle/10665/331846/WHO-2019-nCoV-IPC_WASH-2020.3-eng.pdf . Accessed 30 April 2020.
Windfeld ES, Brooks MS-L (2015) Medical waste management—a review. J Environ Manag 163:98–108
Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, Niemeyer D, Jones TC, Vollmar P, Rothe C, Hoelscher M (2020) Virological assessment of hospitalized patients with COVID-2019. Nature 581(7809):465–469
World Bank Urban Development Series (2018) Decision Maker’s Guides for Solid Waste Management Technologies.
World Bank (2020) Waste workers are protecting our communities during COVID-19. https://blogs.worldbank.org/sustainablecities/waste-workers-are-protecting-ourcommunitiesduring-covid-19 . Accessed 11 May 2020.
Xia J, Tong J, Liu M, Shen Y, Guo D (2020) Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol 92(6):589–594
Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L (2020) Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Resp Med 8(4):420–422
Yadav P, Samadder SR (2018) A critical review of the life cycle assessment studies on solid waste management in Asian countries. J Clean Prod 185:492–515. https://doi.org/10.1016/j.jclepro.2018.02.298
Yunus AP, Masago Y, Hijioka Y (2020) COVID-19 and surface water quality: improved lake water quality during the lockdown. Sci Total Environ 731:139012. https://doi.org/10.1016/j.scitotenv.2020.139012
Zambrano-Monserrate MA, Ruano MA, Sanchez-Alcalde L (2020) Indirect effects of COVID-19 on the environment. Sci Total Environ 728:138813. https://doi.org/10.1016/j.scitotenv.2020.138813
Zhang W, Du RH, Li B, Zheng XS, Yang XL, Hu B, Wang YY, Xiao GF, Yan B, Shi ZL, Zhou P (2020) Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect 9(1):386–389
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382:727–733
Download references
Acknowledgements
The authors wish to thank all who assisted in conducting this work.
Author information
Authors and affiliations.
Chitkara University School of Engineering and Technology, Chitkara University, Solan, Himachal Pradesh, India
V. S. Kanwar, A. Sharma & A. L. Srivastav
Chitkara University School of Computer Applications, Chitkara University, Solan, Himachal Pradesh, India
Central Pollution Control Board, Lucknow, India
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to A. L. Srivastav .
Ethics declarations
Conflict of interest.
The authors declare that they do not have any personal or financial conflict of interests.
Additional information
Editorial responsibility: Samareh Mirkia.
Rights and permissions
Reprints and permissions
About this article
Kanwar, V.S., Sharma, A., Rinku et al. An overview for biomedical waste management during pandemic like COVID-19. Int. J. Environ. Sci. Technol. 20 , 8025–8040 (2023). https://doi.org/10.1007/s13762-022-04287-5
Download citation
Received : 20 September 2021
Revised : 01 February 2022
Accepted : 10 May 2022
Published : 06 June 2022
Issue Date : July 2023
DOI : https://doi.org/10.1007/s13762-022-04287-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Biomedical waste management
- Environmental impact
- Fatality rate
- Thermal treatment
- Find a journal
- Publish with us
- Track your research

COMMENTS
Biomedical Waste Management Rules, 2016 (BMWM Rules, 2016) specify that every healthcare facility shall take all necessary steps to ensure that BMW is handled without any adverse effect on human and environmental health. This document contains six schedules, including the category of BMW, the color coding and type of containers, and labels for ...
Comprehensive management of biomedical waste relies on a. blend of ed ucation and awareness efforts. Education and. dissemination of knowledge ensure that healthcare personnel, waste handlers and ...
For proper disposal management of biomedical waste the Ministry of Environment and Forests has published the Bio-Medical Waste Rules, 1998. This review explains the hospital waste management and ...
The aim of this review article is to provide systematic evidence-based information along with a comprehensive study of BMW in an organized manner. The waste generated in various hospitals and healthcare facilities, including the waste of industries, can be grouped under biomedical waste (BMW). The constituents of this type of waste are various infectious and hazardous materials. This waste is ...
Introduction. Biomedical waste (BMW) is any waste that is generated during the diagnosis, treatment, or immunization of human beings or animals or from research activities, and contains potentially harmful microorganisms which will infect hospital communities and the general public [1,2].BMW includes sharps, non-sharps, blood, body parts, chemicals, pharmaceuticals, medical devices, and ...
Biomedical Waste Management and Its Importance: A Systematic Review Himani S. Bansod , Prasad Deshmukh 1. C om u nity M ed c ,J aw hrlN gD I sfH E R Wardha, IND 2. Head and Neck Surgery, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education ... We focused on papers written in the English language, published within the last ...
For biomedical waste management, thermal treatment of waste can be an alternative, as it can generate energy along with reducing waste volume by 80-95%. ... glasses and currency papers (4 days). Even after applying soap on the hands, additional five minutes are required to inactivate the virus. Hence, it is advisable that one should avoid ...
Bio-Medical waste management (BMWM) is necessary to protect local community health and environment, to reduce its financial loss and to preserve its social and aesthetic values. BMWM encompasses the waste generation, segregation, collection, transportation, processing and disposal. The BMWM system is complex and challenging.
Biomedical waste (BMW) management is an essential practice of healthcare professionals (HCPs) for preventing health and also environmental hazards. Coronavirus disease (COVID-19) has become a global pandemic, posing significant challenges for healthcare sectors. A cross-sectional study was performed to assess the knowledge, practice, and attitude on BMW management among HCPs when taking care ...
Essay # 2. Classification and Categories of Biomedical Waste: Approximately 85% of the biomedical waste is innocuous and as harmless as any other municipal waste. The remaining 15%, however, differs from other waste in that it can be injurious to human or animal health and deleterious to the environment.
Background Biomedical waste management is an important precondition to safeguard the healthcare workers and community members, as well as the environment, from being contaminated with infectious substances. However, biomedical waste management practices during the pandemic era of COVID-19 were unknown. Objective This study was aimed to assess biomedical waste management practices and ...
T oday, biomedical. waste management has become one of major issue of concern in India taking into account the rate of growth of population and rapid urbanization. This. paper includes biomedical ...
This article reviews the impact of biomedical waste on water, soil, air quality, the environment, and human health. Hospitals and nursing homes generate increasing amount of biomedical waste in an unscientific manner. As such, poor waste management practices by these institutions cause exposure to health hazards and actual environmental problems.
Steps involved in biomedical waste management . 5.1 Segregation . To avoid mixing of the biomedical waste with other, a container should be set to the side with colour coding bags at the point of generation. The sorting or separation of waste into different categories is referred as segregation. Segregation will decrease or minimize the risks ...
apart from other domestic waste streams and collected by specialized municipal or waste management entities [2]. II. OBJECTIVES a) The decision to utilize an appropriate technique for biomedical waste management is made. b) We are analyzing the impact of coronavirus on the production of biomedical waste while upholding the integrity of the
The purpose is to spread knowledge among the personnel involved in health care services to prevent transmission of the diseases in the society and to protect public health and environment. Biomedical waste is highly hazardous which can give rise to serious diseases that may be fatal; therefore it is a matter of global concern. Biomedical waste management is of great importance to reduce the ...
Essay # 1. Introduction to Biomedical Waste Management: Hospitals and other health-care establishments have a 'duty of care' for the environment and for public health, and have particular responsibilities in relation to the waste they produce. Unfortunately, medical wastes are not given proper attention and these wastes are disposed of ...
Brutal police operations in Kabardino-Balkaria in recent months have prompted some experts to conclude that the republic's governor is building a "police republic."
Amid COVID-19, world has gone under environmental reformation in terms of clean rivers and blue skies, whereas, generation of biomedical waste management has emerged as a big threat for the whole world, especially in the developing nations. Appropriate biomedical waste management has become a prime concern worldwide in the pandemic era of COVID-19 as it may affect environment and living ...
About Nalchik. Nalchik is the capital of Kabardino-Balkaria. Being a fairly large city, Nalchik is also a resort-like resort city of the Caucasus Mineral Waters, as well as an important intermediate point on its way to mountain attractions such as Elbrus. The city is located on the banks of the river of the same name, at the foot of the Greater ...
Refworld is the leading source of information necessary for taking quality decisions on refugee status. Refworld contains a vast collection of reports relating to situations in countries of origin, policy documents and positions, and documents relating to international and national legal frameworks. The information has been carefully selected and compiled from UNHCR's global network of field ...
AgroSMART 2019 in the first decade of May. Grain was sowed in the phase of full ripeness. Technological methods for keeping crops were based on the generally accepted system of cultivation