An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List


A Comprehensive Review on the Impacts of Smoking on the Health of an Individual
Jerin varghese, pramita muntode gharde.
- Author information
- Article notes
- Copyright and License information
Jerin Varghese [email protected]
Corresponding author.
Received 2023 Aug 19; Accepted 2023 Oct 5; Collection date 2023 Oct.
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Long-term smoking for several years has been known to cause severe ailments in humans from the beginning. Even after knowing that this dangerous addiction is a life-threatening deal, still, ironically, the prevalence of smoking is more or less not getting reduced to a desirable extent. Those who smoke are becoming miserable because of their habit of smoking. Still, on the other hand, due to passive smoking, many more innocent lives are also adversely affected for no fault. This aspect of smoking, i.e., passive or second-hand smoking, is a fearful complication of smoking which is seldom seen with other modes of addiction. Time and again, numerous researches have highlighted the adverse effects of smoking on the human body and the interference it does bring in one's life. Smoking contributes to the deterioration of many preexisting ailments and depletes many valuable aspects of the human body. Smoking thus has a devastating effect on almost all of the tissues of our body and thus exerts its effect on nearly all the major organs. This review article is made by analysing various findings from many researches conducted across the globe by having a thorough search of Pubmed database, which in turn is the main methodology of the article. This review article aims to provide a simple and subtle understanding of the ill effects of smoking on the human body by serving the readers with a readymade platter of comprehensive knowledge about smoking coupled with efforts to eliminate the associated myths.
Keywords: risk-factors, negative impact, various systems of human body, harmful effects, cigarette smoking
Introduction and background
Since the beginning of the human race, men have abused various smokes to get euphorbia. Depending on the availability of the smokable stuff, the content being rolled and its effects vary. Numerous types of smoke-producing products are available in the market [ 1 ]. Almost all of them, irrespective of the design of the smoke-propelling device, are harmful to the human body. Even after knowing that smoking is a significant cause of several ailments in the community, the prevalence of smoking is ironically increasing daily [ 2 ]. The health impacts of smoking have been put forward in the community with the help of various campaigns and other means in simple language [ 3 ]. Still, the effect of these campaigns on the education of smoke-related health issues is only short term and in the long run, is not very helpful in making the users of smoke-related products abstain from them in large numbers [ 4 ].
Unlike other addictions, one of the most dangerous and feared adverse effects of smoking is that those who smoke are ruining their own life and becoming a risky threat to many more innocent lives around them by paving the way for them to their graves. Passive smoking is a dreaded complication of smoking, and people who have nothing to do with it suffer because of those around them who smoke [ 5 ]. Even though smoking is prohibited in public places, the extent to which a smoker pays attention to it is seldom impressive and respectful [ 6 - 11 ]. In families where some member of the family does smoke, other members seldom are spared from the ill effects of passive smoking [ 12 , 13 ]. Strict rules and regulations need to be put forward, and in a way, making sure it is imposed correctly and promptly would solve the issue of passive smoking considerably. Smoking areas exist in many airports, offices, etc., where a person can smoke without letting that smoke reach a non-smoker, and this is a reality already; better strategies like these are needed to prevent passive smoking in our community.
Those who smoke and drink are considered to have more severe health ailments. Drinking and smoking increases the intensity of harm a body needs to bear and is a matter of great concern. The easy availability of smoke-related products near areas where drinks are available is a primary culprit behind this dangerous deed. Enforcements must be planned and carried out successfully to help smokers abstain from this fatal mixture of addictions. Those who smoke need proper care and counselling, and time and over, it has been evident that many smokers benefited and gave up their habit of smoking after such eventful counselling sessions and guidance [ 14 ]. The prevalence of such activities needs to be increased and made available to the general public to ensure it is not limited only to the wealthy and affluent class. Media does play a crucial role in the promotion of smoking. Seeing a favorite actor smoking does impact their fans from adopting similar actions [ 15 , 16 ]. Over the past couple of years, the narration of women being smokers has been portrayed in various movies and series, making many female viewers deviate towards smoking. Advertisements of smoke-related products are another way people get influenced to smoke. Although regulations are imposed in this respect on commercial ads, there are many surrogate advertisements in our community where the product is indirectly promoted and advertised by renowned celebrities, sports personalities, social influencers, stars, etc. [ 17 , 18 ].
Undoubtedly, smoking is a major risk factor for many respiratory ailments but the adverse effects of smoking aren't limited to just the respiratory system. The false notion among the community that smoking causes only respiratory-related ailments had prevailed in our community a couple of decades prior. However, as newer research surfaced, this belief got a shattering setback. Today, smoking is considered hazardous to almost all the varied systems of our body, and no doubt further research would add more ill effects of tobacco to the already proven list. Smoking acts as a precipitating factor in the causation of various diseases. Making more and more people aware of the impact of smoking would probably decrease the number of smokers. Mass campaigns that are effective, acceptable and understandable to the general public are needed to save the lives of those addicted to this fatal smoking habit [ 3 , 19 ]. A comprehensive strategy to make the person know the effects of smoking in their personalized life would be a better idea. Many myths revolve around smoking, which needs to be corrected [ 20 ]. Considering one form of smoking over another by believing that the latter is better and harmless is common among smokers. There is a constant struggle between the cigarette companies to bring safer cigarettes as it is a worse fact that this fatal habit has destroyed many lives, and the saga is still continuing. Many such products, which look like cigarettes (for example, herbal cigarettes, ayurvedic cigarettes, etc.) are also available in the market, urging smokers to use them safely without any significant health concerns [ 21 , 22 ]. More or less, these products have been a failure at even the ground level as these products were not able to rise to the standard demands of a smoker and thus turned out to be an unacceptable idea for those who smoke. Moreover, a massive lot of anti-nicotine products like anti-nicotine gums, medications, etc., are available for smokers to aid them in getting rid of nicotinic cigarettes, but this is made handy by only a few smokers who are determined to give up smoking; the majority do use such products for a while and then gradually get back to their initial states. Similar misconceptions are frequent in our community, which must be addressed appropriately. Unless and until the layperson is not made aware of the facts, the intensity of damage caused by misinformation will keep increasing.
Search methodology
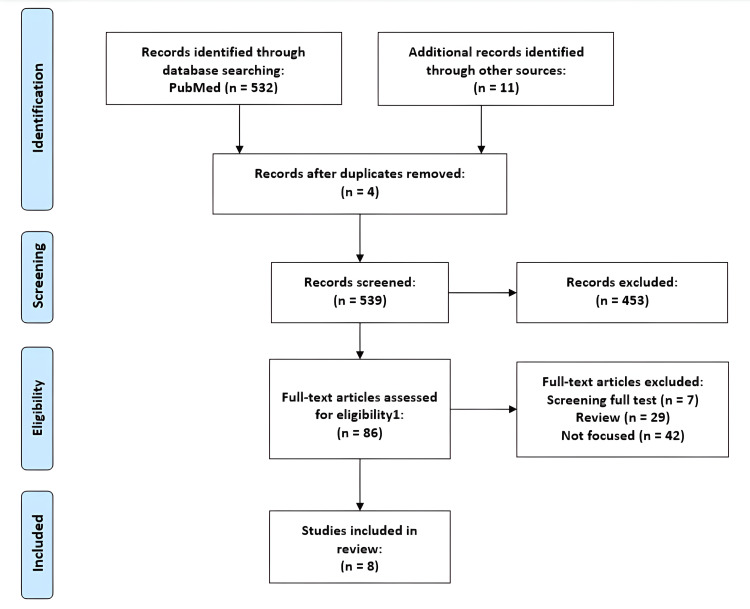
This review article was made after careful assessment and evaluation of the various researches conducted across the globe on the impacts of smoking on the health of an individual. The primary database used for the search is PubMed along with certain researches obtained from other databases and sources. The duration of the publication of articles considered for the purpose of review is within the past 25 years. Those articles which couldn't put forth a definite and precise conclusion and those whose results were found to be doubtful are excluded. A PRISMA flow diagram of the review indicating the screening process is summarized in Figure 1 below.
Figure 1. PRISMA flow diagram of the review process.
Effect of smoking on the respiratory system
The various aspects of smoking-related issues concerning the respiratory system are well known to humankind. When we say ill effects of smoking, the first image that runs to our mind is damaged lungs. Undoubtedly, smoking does have a profound impact on our respiratory system. The major respiratory illness associated with smoking includes bronchial asthma, Chronic Obstructive Pulmonary Disease (COPD), emphysema, interstitial lung diseases, lung fibrosis, lung cancer, etc. [ 23 ], which is schematically represented in Figure 2 below. Smoking is a crucial factor in the causation and worsening of many respiratory illnesses. It is a common scenario where smoking is portrayed to be directly linked with the respiratory system in many anti-smoke campaigns to educate the general public regarding the impacts of smoking. A large number of acute eosinophilic pneumonia cases do have smoking as a precipitating factor [ 24 ]. Almost all of the varied types of pneumonia get worsened and are affected by the habit of smoking. Smoke is a precipitating factor and thus could easily be linked to various pulmonary ailments. Smoking leads to the proliferation of a wide variety of cells. Different hypothesis has popped up over time regarding the proliferation of cells in individuals who smoke, and many of these hypotheses have been scientifically proven to be correct through research. The proliferation of Langerhans' cells is an essential entity in this respect. To a great extent, the proliferation of Langerhans' cells is related to cigarette smoking, thereby leading to Pulmonary Langerhans' cell histiocytosis [ 25 ]. More or less, every smoker harms one or the other part of their bronchial architecture due to smoking. Bronchiolitis, an inflammatory bronchial reaction, is often found in those who smoke. It won't be wrong to say that almost all smokers have respiratory bronchiolitis [ 26 ]. There has been a firm relationship between smoking and respiratory bronchiolitis-associated interstitial lung disease (RB-ILD) and desquamative interstitial pneumonia (DIP) [ 27 ]. The relationship of smoking with respiratory bronchiolitis-associated interstitial lung disease (RB-ILD) and desquamative interstitial pneumonia (DIP) is being further explored to aid in framing effective management strategies to compact these ailments. Idiopathic Pulmonary Fibrosis (IPF) exact cause is not yet known and is suggestive by its name, but cigarette smoking is a significant risk factor for Idiopathic Pulmonary Fibrosis [ 28 ]. The correlation between smoking and Idiopathic Pulmonary Fibrosis (IPF) is profound. Emphysema and pulmonary fibrosis are seen in patients with Interstitial Lung Diseases (ILD) who continue to smoke [ 29 ]. In fact, smoking is attributed to be a key player in working the cases of Interstitial Lung Diseases (ILD) to such an extent that irreversible changes are brought about in the lungs of the patients suffering from the ailment. Smoking interferes with the homeostasis of many elements in our body, be it macroelements or microelements. The impact of smoking is more dreaded in the homeostasis of microelements in particular, one of the most significant examples being the influence of smoking on iron homeostasis. Iron homeostasis of the cells gets disrupted when exposed to cigarette smoke particles, which ultimately is assumed to lead to the development of non-neoplastic injury of the lungs [ 30 ]. Even e-cigarettes interfere with the respiratory health of adolescents with asthma [ 31 ], and thus are no better alternative. Lung perfusion in Magnetic Resonance Imaging (MRI) studies was found to be increased after using electronic nicotine delivery systems, while it decreased exposure to tobacco smoke [ 32 ]. The prognosis of respiratory illness is worsened by the habit of smoking to a great extent. Whatever the source of smoke, almost all the varied smoke is harmful to the proper functioning of our alveolar complex. The deposition of toxins and tar in the lungs is a dreaded complication of smoking, leading to irreversible damage to the typical architecture over prolonged years. The incomplete combustion of smoke-producing substances adds to the terror, and many researchers have highlighted that these substances that are not entirely burnt cause more adverse pulmonary ailments when compared with those that burn out completely.

Figure 2. A schematic representation of the impacts of smoking on the respiratory system of an individual.
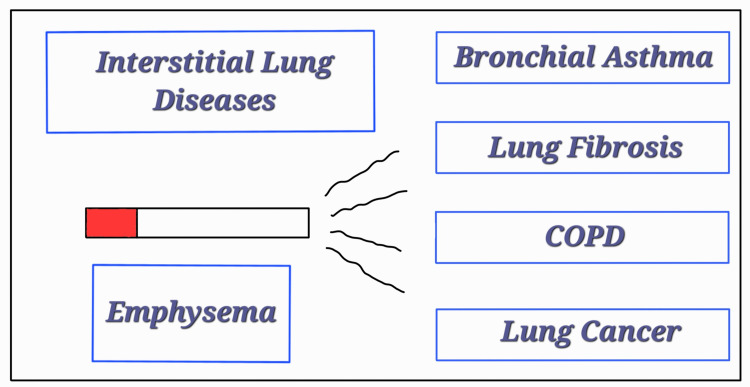
COPD = Chronic Obstructive Pulmonary Disease
Effect of smoking on the cardiovascular system (CVS)
Smoking causes various cardiovascular ailments in humans and is a leading risk factor in the causation of cardiovascular diseases worldwide; it is also a preventable cause of mortality in individuals with cardiovascular diseases [ 33 ]. Abstinence from smoking is often advised after almost all of the cardiovascular events, whether it be a major or minor one, which showcases the influence of smoking on a person's cardiovascular health. Various studies have shown that those who had abstained from smoking benefited from the same, as there was a notably better prognosis of cardiovascular ailments in these individuals compared to those who continued smoking. It is a clearly evident and scientifically proven fact that the prognosis of cardiovascular events is adversely affected when a patient with cardiovascular ailments smokes. Almost all of the cigarettes in the market contain nicotine in some or other amount. Nicotine is a primary cigarette component, accelerating atherogenesis, thereby leading to coronary artery heart disease [ 34 ]. Abolishing the false belief that hookah smoking is far less harmful than conventional cigarettes is necessary. Because of hookah's overlapping toxicants and chemical profile, its harmful effects on the cardiovascular system are comparable to regular cigarettes [ 35 ]. The constituents of hookah smoke, like carbon monoxide, oxidants, phenols, nicotine, heavy metals, etc., are proven to cause serious cardiovascular issues in those who smoke them [ 36 ]. Hence, considering hookah as an alternative to cigarette smoking is no good. Waterpipe smoking, too, has adverse cardiovascular effects, which at times are comparable to the smoking of regular cigarettes [ 37 ] and thus has to be avoided. Cigarette smoking causes dysfunctioning of the cardiovascular system by many mechanisms, one of the most common and notable being the mechanism involving an increment of oxidative stress [ 38 ]. An increase in oxidative stress is bound to damage the structures of the cardiovascular system. Passive smokers also suffer from cardiovascular ailments because of the smoking habits of the people near them. In second-hand smoking, vascular inflammation is promoted by increased oxidative stress [ 39 ]. The effects of second-hand smoke on the cardiovascular system are fast and substantially comparable to those caused by primary smoking [ 40 ]. The levels of cardiovascular disease risk biomarkers like homocysteine and fibrinogen are disproportionately increased in passive smokers, which points to the fact that passive smokers suffer from cardiovascular disease risk [ 41 ]. The elevated levels of C-reactive proteins in second-hand smokers indicate the long-term cardiovascular risk in these individuals [ 42 ]. Thus, from the frame of cardiovascular health, both smokers, i.e., the primary and the second-hand smokers, are affected similarly in many respects. Serum levels of cotinine were on the higher side in second-hand smokers compared to those without exposure to smoke, which alarms that second-hand smokers are at a greater risk [ 43 ] when compared to the real culprits. The myocardium and the artery vessels are adversely affected by the smoke, and thus, this leads to worsening cardiovascular health [ 44 ]. Many radiological findings reinforced and validated that smoking causes remarkable changes in an individual's cardiovascular system. B-mode ultrasound measurement of carotid artery intimal-medial thickness showed increased smoking led to increased initial-medial thickness [ 45 ]. Specific, irreversible changes are brought about by long-term smoking in the progression of atherosclerosis [ 46 ]. The prognosis of hypertension is badly worsened as a result of smoking. Because of an accelerated rate of atherosclerosis in hypertensive smokers, hypertension usually progresses to renovascular and malignant hypertension, which are severe forms of hypertension [ 47 ].
Effect of smoking on the reproductive system
Smoking adversely affects men's and women's reproductive systems. The fetus, too, suffers because of the smoking habits of a pregnant woman. The influence of smoke on the intrauterine life of a fetus is well known, and smoking is contraindicated during pregnancy. Women who smoke should stop smoking at any cost to have a healthy baby. It is a heartbreaking reality that a fetus seldom gets spared from being a victim of various ailments because of the act of smoking by their pregnant mother. Considering the multiple aspects of smoking-related issues linked with the reproductive capability of an individual, one could say that smoking is a great curse for a healthy reproductive life. Smoking causes testosterone imbalance in men along with the causation of erectile dysfunction, muscle weakness, etc. In women, undesirable hormonal changes occur due to long-term cigarette smoking, thereby interfering with proper reproductive functionality. Especially during gestation, the continuation of smoking is undoubtedly a contrary factor to the birth of a healthy baby. Smoking is linked with erectile dysfunction, thereby contributing to infertility in males. The normal physiology of the nitric oxide signal transduction pathway is altered because of cigarette smoking, which is thought to be the main contributing factor in the causation of erectile dysfunction in individuals who smoke [ 48 ]. Erectile dysfunction is often related to endothelial diseases, and smoking is a significant risk factor in developing endothelial diseases; thus, smoking does affect erectile function by its effect on the causation of endothelial diseases [ 49 ]. Documentation supports the fact that there is a dose-response relationship between the risk of erectile dysfunction and cigarette smoking [ 50 ]. Smoking, to any degree, is harmful to a man's reproductive health, and thus, one must abstain from it. Smoking has a severe negative impact on the hormonal balance of an individual, which, when coupled with the effects of smoking on other organs linked with reproduction, leads to complex fertility issues [ 51 ]. Although cigarette smoking doesn't have a massive impact on the testosterone fraction that is available biologically, it brings about changes in the sex hormone binding globulin (SHBG), thereby having its say in the free and total levels of testosterone in a man who smokes [ 52 ]. SHBG is an essential factor that determines the reproductive fitness of an individual, and thus, smoking, with its harmful effect on the SHBG, definitely worsens the reproductive health of the concerned. Reduced femur length and head size after the first trimester are frequently found in women who smoke during pregnancy [ 53 ]. Reduced fetal measurements are seldom seen in the first trimester, but it is common in the second and third trimesters in cases of maternal smoking [ 54 ]. This doesn't mean it is safe to smoke in the first trimester. Children born to women who used to smoke during their pregnancy have been found to have lower birth weights [ 55 ]. Intrauterine growth retardation is considered to be the attributable factor causing the low birth weight of newborns in maternal smokers [ 56 ]. Significant intrauterine retardation of growth has been found in the babies born to mothers who smoke. Maternal smoking has been reported to cause developmental delay issues in children, some of which are almost irreversible and fatal. Infants exposed to smoke are more prone to long-term adverse health impacts than those not exposed. Also, a pregnant woman should take special care to keep herself and her growing fetus safe from second-hand smoke, which has similar adverse effects.
Other effects of smoking
Smoking does cause relevant ill effects on many of the organs of our body, which is seldom understood and given very little importance by the general public due to the lack of knowledge and mere ignorance. These changes that smoking brings to our body may sound less harmful at first, but they may even be permanently irreversible when they progress to an advanced level. Smoking reduces the generalized immune status of an individual, and smokers are more prone to ailments than those who don't smoke. Smokers get infected by pathogens more readily than non-smokers. Smoking harms the oral immunity of an individual. Smoking reduces the host's oral immunity against Candida albicans and thus makes the individual susceptible to oral infections involving Candida [ 57 ]. The natural oral and nasopharyngeal bacterial flora gets disturbed due to smoking, thereby leading to the colonization of these sites by potentially pathogenic organisms [ 58 ]. Smokers have lesser aerobic and anaerobic microorganisms with interfering capacity than non-smokers, threatening the normal oral flora [ 59 ]. The disturbed composition of the flora gets reversed on cessation of smoking, highlighting that smoking is the primary factor responsible for disturbed oral flora [ 60 ]. In cases of chain smokers, it becomes more or less impossible for the normal oral flora to get reestablished. The reduction in smoking is estimated to reduce the probability of the development of Alzheimer's disease [ 61 ], thereby having its say in a condition that has a profound impact on an individual's life. Otoacoustic Emissions (OAE) are generally reduced in smokers compared to non-smokers [ 62 ]. Smoking cessation leads to a reduction in the incidence of periodontitis and is also helpful in the better prognosis of those undergoing treatment [ 63 ]. Smoking is a massive hurdle in achieving and maintaining desirable oral health. Smoking interferes with the skeletal system of our body and is proven to be a crucial factor in the prognosis of many orthopaedic conditions. Smoking causes delayed union of fractures, thereby leading to a more extended recovery period and poorer prognosis [ 64 ]. Disorders of the lumbar disc and the metabolism of bones are affected adversely by smoking [ 65 ]. Post-operative infection rates steadily increase when the patient who underwent surgery is a smoker [ 66 ]. Smoking plays a crucial role in cancers of other organs, too, other than the lungs. Smoking is considered a significant risk factor in the causation of neoplastic changes in most of the malignancies found in human beings in one way or another. In patients with glaucoma, optic nerve vessel density is found to be reduced in association with the intensity of smoking [ 67 ]. Smoking leads to dryness of the eyes as it interferes with the normal lubrication of the eyes by causing damage to the meibomian glands of our eyes [ 68 ]. The various researches reviewed in order to formulate this review have been summarized in Table 1 .
Table 1. Summary of the revised articles.
Conclusions.
Smoking is undisputedly a significant risk factor in the development of many chronic illnesses in humans and thus is a hurdle in living a healthy and happy life. The adverse effects smoking has on the proper functioning of the human body should seldom be neglected. The impact of smoking on the various systems of the human body has been tried to be incorporated in this review article. To completely sum up the effects of smoking in a single article is nearly impossible, as hardly one could find an organ system that is unaffected by smoking. The health benefits that could be achieved due to smoking cessation and the overall well-being it could bring to the community is a highly desirable phenomenon. As smoking is a risk factor in the causation of various diseases, abstinence from smoking provides huge protection from several ailments. The issue of passive smoking also needs to be acknowledged and addressed appropriately to ensure the safety of those who don't smoke. Advanced research, which is currently ongoing, promises to achieve a greater understanding of the various unknown aspects of smoking and hopefully let these studies enlighten more and more smokers and prevent them from dooming their lives with smoke.
The authors have declared that no competing interests exist.
- 1. Acute effects of heat-not-burn, electronic vaping, and traditional tobacco combustion cigarettes: the Sapienza University of Rome-vascular assessment of proatherosclerotic effects of smoking (SUR-VAPES) 2 randomized trial. Biondi-Zoccai G, Sciarretta S, Bullen C, et al. J Am Heart Assoc. 2019;8:0. doi: 10.1161/JAHA.118.010455. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Prevalence and determinants of tobacco smoking among low-income urban adolescents. Mallol J, Urrutia-Pereira M, Mallol-Simmonds MJ, Calderón-Rodríguez L, Osses-Vergara F, Matamala-Bezmalinovic A. Pediatr Allergy Immunol Pulmonol. 2021;34:60–67. doi: 10.1089/ped.2021.0018. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Anti-smoking campaigns. Evans WG. https://pubmed.ncbi.nlm.nih.gov/23951764/ SADJ. 2013;68:58–59. [ PubMed ] [ Google Scholar ]
- 4. The impact of media campaigns on smoking cessation activity: a structural vector autoregression analysis. Langley TE, McNeill A, Lewis S, Szatkowski L, Quinn C. Addiction. 2012;107:2043–2050. doi: 10.1111/j.1360-0443.2012.03958.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Passive smoking. Chesebro MJ. https://pubmed.ncbi.nlm.nih.gov/3284305/ Am Fam Physician. 1988;37:212–218. [ PubMed ] [ Google Scholar ]
- 6. Effect of anti-smoking legislation in public places. Bhat N, Oza S, Reddy JJ, Mitra R, Rahul P, Singh S. https://pubmed.ncbi.nlm.nih.gov/26322216/ Addict Health. 2015;7:87–91. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Impact of a smoking ban in public places: a rapid assessment in the Seychelles. Viswanathan B, Plumettaz C, Gedeon J, Bovet P. Tob Control. 2011;20:427–430. doi: 10.1136/tc.2010.041590. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Smoking at the workplaces in Italy after the smoking ban in the Lazio Region. Ruscitti LE, Castellani F, La Torre G, De Giusti M, Dominici F, Valente P. Med Lav. 2021;112:44–57. doi: 10.23749/mdl.v112i1.8779. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Facilitators and barriers of smokers' compliance with smoking bans in public places: a systematic review of quantitative and qualitative literature. Zhou L, Niu L, Jiang H, Jiang C, Xiao S. Int J Environ Res Public Health. 2016;13:1228. doi: 10.3390/ijerph13121228. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Compliance with the smoking ban in enclosed, semiopen and open areas of workplaces and public places in Chile. Peruga A, Molina X, Delgado I, et al. Tob Control. 2021;30:570–573. doi: 10.1136/tobaccocontrol-2020-055632. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Evaluation of the smoking ban in public places in France one year and five years after its implementation: findings from the ITC France survey. Fong GT, Craig LV, Guignard R, et al. https://pubmed.ncbi.nlm.nih.gov/24803715/ Bull Epidemiol Hebd (Paris) 2013;20:217–223. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Smoking habit in parents and exposure to environmental tobacco smoke in elementary school children of Milan. Campo L, Boniardi L, Polledri E, Longhi F, Scuffi C, Fustinoni S. Sci Total Environ. 2021;796:148891. doi: 10.1016/j.scitotenv.2021.148891. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. The negative impact of parental smoking on adolescents' health-promoting behaviors: a cross-sectional study. Chen MY. Int J Environ Res Public Health. 2021;18:2514. doi: 10.3390/ijerph18052514. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Individual behavioural counselling for smoking cessation. Lancaster T, Stead LF. Cochrane Database Syst Rev. 2017;3:0. doi: 10.1002/14651858.CD001292. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Smoking in movies and adolescent smoking initiation: longitudinal study in six European countries. Morgenstern M, Sargent JD, Engels RC, et al. Am J Prev Med. 2013;44:339–344. doi: 10.1016/j.amepre.2012.11.037. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Smoking in movies and increased smoking among young adults. Song AV, Ling PM, Neilands TB, Glantz SA. Am J Prev Med. 2007;33:396–403. doi: 10.1016/j.amepre.2007.07.026. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Impact of cigarette advertising on smoking behaviour in Spanish adolescents as measured using recognition of billboard advertising. López ML, Herrero P, Comas A, et al. Eur J Public Health. 2004;14:428–432. doi: 10.1093/eurpub/14.4.428. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. The relationship between tobacco advertisements and smoking status of youth in India. Shah PB, Pednekar MS, Gupta PC, Sinha DN. https://pubmed.ncbi.nlm.nih.gov/19256752/ Asian Pac J Cancer Prev. 2008;9:637–642. [ PubMed ] [ Google Scholar ]
- 19. Mass media campaigns to promote smoking cessation among adults: an integrative review. Durkin S, Brennan E, Wakefield M. Tob Control. 2012;21:127–138. doi: 10.1136/tobaccocontrol-2011-050345. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Slaying myths about passive smoking. Jamrozik K. Tob Control. 2005;14:294–295. doi: 10.1136/tc.2005.014092. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 21. How do herbal cigarettes compare to tobacco? A comprehensive review of their sensory characters, phytochemicals, and functional properties. Abdel Rahman RT, Kamal N, Mediani A, Farag MA. ACS Omega. 2022;7:45797–45809. doi: 10.1021/acsomega.2c04708. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Asian herbal-tobacco cigarettes: "not medicine but less harmful"? Chen A, Glantz S, Tong E. Tob Control. 2007;16:0. doi: 10.1136/tc.2006.016568. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Smoking and respiratory diseases [Article in Japanese] Ishii Y. https://pubmed.ncbi.nlm.nih.gov/23631228/ Nihon Rinsho. 2013;71:416–420. [ PubMed ] [ Google Scholar ]
- 24. Diffuse lung diseases in cigarette smokers. Vassallo R. Semin Respir Crit Care Med. 2012;33:533–542. doi: 10.1055/s-0032-1325162. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Smoking-related interstitial pneumonias and pulmonary Langerhans cell histiocytosis. Caminati A, Harari S. Proc Am Thorac Soc. 2006;3:299–306. doi: 10.1513/pats.200512-135TK. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Respiratory bronchiolitis-associated interstitial lung disease (RB-ILD) Goeckenjan G. Pneumologie. 2003;57:278–287. doi: 10.1055/s-2003-39368. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Desquamative interstitial pneumonia and respiratory bronchiolitis-associated interstitial lung disease. Ryu JH, Myers JL, Capizzi SA, Douglas WW, Vassallo R, Decker PA. Chest. 2005;127:178–184. doi: 10.1378/chest.127.1.178. [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. The relationship between cigarette smoking and some types of idiopathic interstitial pneumonias [Article in Polish] Gasior G, Pierzchała W, Ograbek-Król M. https://pubmed.ncbi.nlm.nih.gov/18717043/ Wiad Lek. 2008;61:48–52. [ PubMed ] [ Google Scholar ]
- 29. Tobacco smoking is associated with combined pulmonary fibrosis and emphysema and worse outcomes in interstitial lung disease. Douglas D, Keating L, Strykowski R, et al. Am J Physiol Lung Cell Mol Physiol. 2023;325:233–243. doi: 10.1152/ajplung.00083.2023. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. Cigarette smoke particle-induced lung injury and iron homeostasis. Ghio AJ, Pavlisko EN, Roggli VL, Todd NW, Sangani RG. Int J Chron Obstruct Pulmon Dis. 2022;17:117–140. doi: 10.2147/COPD.S337354. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Potential effects of E-cigarettes and vaping on pediatric asthma. Di Cicco M, Sepich M, Ragazzo V, Peroni DG, Comberiati P. Minerva Pediatr. 2020;72:372–382. doi: 10.23736/S0026-4946.20.05973-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. MRI shows lung perfusion changes after vaping and smoking. Nyilas S, Bauman G, Korten I, et al. Radiology. 2022;304:195–204. doi: 10.1148/radiol.211327. [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Effects of tobacco smoking on cardiovascular disease. Kondo T, Nakano Y, Adachi S, Murohara T. Circ J. 2019;83:1980–1985. doi: 10.1253/circj.CJ-19-0323. [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Cardiovascular toxicity of nicotine: implications for electronic cigarette use. Benowitz NL, Burbank AD. Trends Cardiovasc Med. 2016;26:515–523. doi: 10.1016/j.tcm.2016.03.001. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 35. The effects of hookah/waterpipe smoking on general health and the cardiovascular system. Qasim H, Alarabi AB, Alzoubi KH, Karim ZA, Alshbool FZ, Khasawneh FT. Environ Health Prev Med. 2019;24:58. doi: 10.1186/s12199-019-0811-y. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 36. Cardiovascular effects of Hookah smoking: potential implications for cardiovascular risk. Rezk-Hanna M, Benowitz NL. Nicotine Tob Res. 2019;21:1151–1161. doi: 10.1093/ntr/nty065. [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Waterpipe use and its cardiovascular effects: a systematic review and meta-analysis of case-control, cross-sectional, and non-randomized studies. Mahfooz K, Vasavada AM, Joshi A, et al. Cureus. 2023;15:0. doi: 10.7759/cureus.34802. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 38. The pathophysiology of cigarette smoking and cardiovascular disease: an update. Ambrose JA, Barua RS. J Am Coll Cardiol. 2004;43:1731–1737. doi: 10.1016/j.jacc.2003.12.047. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Secondhand smoke as an acute threat for the cardiovascular system: a change in paradigm. Raupach T, Schäfer K, Konstantinides S, Andreas S. Eur Heart J. 2006;27:386–392. doi: 10.1093/eurheartj/ehi601. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Cardiovascular effects of secondhand smoke: nearly as large as smoking. Barnoya J, Glantz SA. Circulation. 2005;111:2684–2698. doi: 10.1161/CIRCULATIONAHA.104.492215. [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Exposure to secondhand smoke and biomarkers of cardiovascular disease risk in never-smoking adults. Venn A, Britton J. Circulation. 2007;115:990–995. doi: 10.1161/CIRCULATIONAHA.106.648469. [ DOI ] [ PubMed ] [ Google Scholar ]
- 42. Secondhand smoke exposure and C-reactive protein levels in youth. Wilkinson JD, Lee DJ, Arheart KL. Nicotine Tob Res. 2007;9:305–307. doi: 10.1080/14622200601080299. [ DOI ] [ PubMed ] [ Google Scholar ]
- 43. Secondhand tobacco smoke exposure among children and adolescents: United States, 2003-2006. Marano C, Schober SE, Brody DJ, Zhang C. Pediatrics. 2009;124:1299–1305. doi: 10.1542/peds.2009-0880. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Interactive effect of combined exposure to active and passive smoking on cardiovascular system. Leone A. Recent Pat Cardiovasc Drug Discov. 2011;6:61–69. doi: 10.2174/157489011794578437. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Active and passive smoking are associated with increased carotid wall thickness. The Atherosclerosis Risk in Communities Study. Howard G, Burke GL, Szklo M, Tell GS, Eckfeldt J, Evans G, Heiss G. https://pubmed.ncbi.nlm.nih.gov/8203995/ Arch Intern Med. 1994;154:1277–1282. [ PubMed ] [ Google Scholar ]
- 46. Cigarette smoking and progression of atherosclerosis: the atherosclerosis risk in communities (ARIC) study. Howard G, Wagenknecht LE, Burke GL, et al. JAMA. 1998;279:119–124. doi: 10.1001/jama.279.2.119. [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Cigarette smoking and hypertension. Virdis A, Giannarelli C, Neves MF, Taddei S, Ghiadoni L. Curr Pharm Des. 2010;16:2518–2525. doi: 10.2174/138161210792062920. [ DOI ] [ PubMed ] [ Google Scholar ]
- 48. Effects of cigarette smoking on erectile dysfunction. Kovac JR, Labbate C, Ramasamy R, Tang D, Lipshultz LI. Andrologia. 2015;47:1087–1092. doi: 10.1111/and.12393. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 49. Smoking and erectile dysfunction: evidence based analysis. McVary KT, Carrier S, Wessells H. https://pubmed.ncbi.nlm.nih.gov/11586190/ J Urol. 2001;166:1624–1632. [ PubMed ] [ Google Scholar ]
- 50. Cigarette smoking and erectile dysfunction among Chinese men without clinical vascular disease. He J, Reynolds K, Chen J, et al. Am J Epidemiol. 2007;166:803–809. doi: 10.1093/aje/kwm154. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Cigarette smoking and hormones. Marom-Haham L, Shulman A. Curr Opin Obstet Gynecol. 2016;28:230–235. doi: 10.1097/GCO.0000000000000283. [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Effect of cigarette smoking on levels of bioavailable testosterone in healthy men. English KM, Pugh PJ, Parry H, Scutt NE, Channer KS, Jones TH. https://pubmed.ncbi.nlm.nih.gov/11352783/ Clin Sci (Lond) 2001;100:661–665. [ PubMed ] [ Google Scholar ]
- 53. A systematic review of maternal smoking during pregnancy and fetal measurements with meta-analysis. Abraham M, Alramadhan S, Iniguez C, et al. PLoS One. 2017;12:0. doi: 10.1371/journal.pone.0170946. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 54. First trimester maternal tobacco smoking habits and fetal growth. Prabhu N, Smith N, Campbell D, et al. Thorax. 2010;65:235–240. doi: 10.1136/thx.2009.123232. [ DOI ] [ PubMed ] [ Google Scholar ]
- 55. Maternal smoking as a model for environmental epigenetic changes affecting birthweight and fetal programming. Suter MA, Anders AM, Aagaard KM. Mol Hum Reprod. 2013;19:1–6. doi: 10.1093/molehr/gas050. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 56. Low birthweight, preterm births and intrauterine growth retardation in relation to maternal smoking. Horta BL, Victora CG, Menezes AM, Halpern R, Barros FC. Paediatr Perinat Epidemiol. 1997;11:140–151. doi: 10.1046/j.1365-3016.1997.d01-17.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 57. Smoking increases oral mucosa susceptibility to Candida albicans infection via the Nrf2 pathway: In vitro and animal studies. Ye P, Chen W, Huang F, et al. J Cell Mol Med. 2021;25:7948–7960. doi: 10.1111/jcmm.16724. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 58. The impact of smoking on oral and nasopharyngeal bacterial flora. Brook I. J Dent Res. 2011;90:704–710. doi: 10.1177/0022034510391794. [ DOI ] [ PubMed ] [ Google Scholar ]
- 59. Effects of exposure to smoking on the microbial flora of children and their parents. Brook I. Int J Pediatr Otorhinolaryngol. 2010;74:447–450. doi: 10.1016/j.ijporl.2010.01.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Effect of smoking cessation on the microbial flora. Brook I, Gober AE. Arch Otolaryngol Head Neck Surg. 2007;133:135–138. doi: 10.1001/archotol.133.2.135. [ DOI ] [ PubMed ] [ Google Scholar ]
- 61. Smoking and increased Alzheimer's disease risk: a review of potential mechanisms. Durazzo TC, Mattsson N, Weiner MW. Alzheimers Dement. 2014;10:122–145. doi: 10.1016/j.jalz.2014.04.009. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 62. Otoacoustic emissions in smoking and nonsmoking young adults. Jedrzejczak WW, Koziel M, Kochanek K, Skarzynski H. Clin Exp Otorhinolaryngol. 2015;8:303–311. doi: 10.3342/ceo.2015.8.4.303. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 63. Smoking cessation and response to periodontal treatment. Alexandridi F, Tsantila S, Pepelassi E. Aust Dent J. 2018;63:140–149. doi: 10.1111/adj.12568. [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. The effects of smoking on fracture healing. Sloan A, Hussain I, Maqsood M, Eremin O, El-Sheemy M. Surgeon. 2010;8:111–116. doi: 10.1016/j.surge.2009.10.014. [ DOI ] [ PubMed ] [ Google Scholar ]
- 65. Effects of smoking on orthopaedic disorders and surgery [Article in Hebrew] Steinberg EL, Luger E, Mamam E, Steinberg S. https://pubmed.ncbi.nlm.nih.gov/12858830/ Harefuah. 2003;142:442-445, 485. [ PubMed ] [ Google Scholar ]
- 66. Cigarette smoking and its orthopedic consequences. Kwiatkowski TC, Hanley EN Jr, Ramp WK. https://pubmed.ncbi.nlm.nih.gov/8886197/ Am J Orthop (Belle Mead NJ) 1996;25:590–597. [ PubMed ] [ Google Scholar ]
- 67. Effects of smoking on optic nerve head microvasculature density in glaucoma. Eslani M, Nishida T, Weinreb RN, et al. J Glaucoma. 2022;31:710–716. doi: 10.1097/IJG.0000000000002081. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 68. Effects of chronic smoking on the meibomian glands. Muhafiz E, Aslan Bayhan S, Bayhan HA, Gürdal C. Int Ophthalmol. 2019;39:2905–2911. doi: 10.1007/s10792-019-01139-z. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (358.4 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES