An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Lumbosacral spondylolisthesis.
Katarzyna Studnicka ; George Ampat .
Affiliations
Last Update: July 22, 2023 .
- Continuing Education Activity
Lumbosacral spondylolisthesis is a forward translation of the fifth lumbar vertebrae over the first sacral vertebrae. Untreated, it may be associated with chronic lower back pain and lead to neurological complications. This activity evaluates the etiology, classification, diagnosis, and treatment options, as well as the role of interprofessional teams in the management of patients with this condition.
- Identify the etiology of lumbar spondylolisthesis.
- Review the evaluation of lumbar spondylolisthesis.
- Outline the management options available for lumbosacral spondylolisthesis.
- Describe some interprofessional team strategies for improving care coordination and communication to advance lumbosacral spondylolisthesis treatment and improve outcomes.
- Introduction
Lumbosacral spondylolisthesis is the forward translation of the fifth lumbar vertebra (L5) over the first sacral vertebra (S1). Bilateral L5 pars defect (spondylolysis) or repetitive stress injury is the primary etiology behind lumbosacral spondylolisthesis. The degree of a slip often correlates with the degree of symptoms.
The prevalence of spondylolysis (pars defect), in the general population, is 6%, and a third of those will subsequently develop a degree of spondylolisthesis. [1] The majority of cases are mild or asymptomatic, and only a relatively small percentage of symptomatic patients require surgical intervention.
The most commonly affected populations are children and adolescents participating in sports that require repetitive lower back hyperextension (divers, pace cricket bowlers, baseball, softball, rugby, weightlifting, sailing, table tennis, wrestlers, gymnasts, dancers, and footballers). They usually present with lower back pain exacerbated by activity. [2] Occasionally pain can radiate to both buttocks and legs, and in advanced cases, the gait pattern and walking distance may be affected. Presentation in adults is more insidious and commonly associated with long-standing degenerative changes secondary to the slip, often leading to spinal canal stenosis and radicular pain.
Management of the majority of the cases is non-operative, but patients who fail non-operative treatment and continue having disabling symptoms may require surgical treatment. [2] [3]
A Wiltse-Newman classification describes different etiology of pars interarticularis failure [4] :
- Type I Dysplastic – congenital defect in pars
- II A pars fatigue fracture
- II B pars elongation due to multiple healed stress fractures
- II C pars acute fracture
- Type III degenerative spondylolisthesis from degenerative facet instability without pars fracture
- Type IV Traumatic – due to acute posterior arch fracture other than pars
- Type V Neoplastic – pathologic destruction of the pars
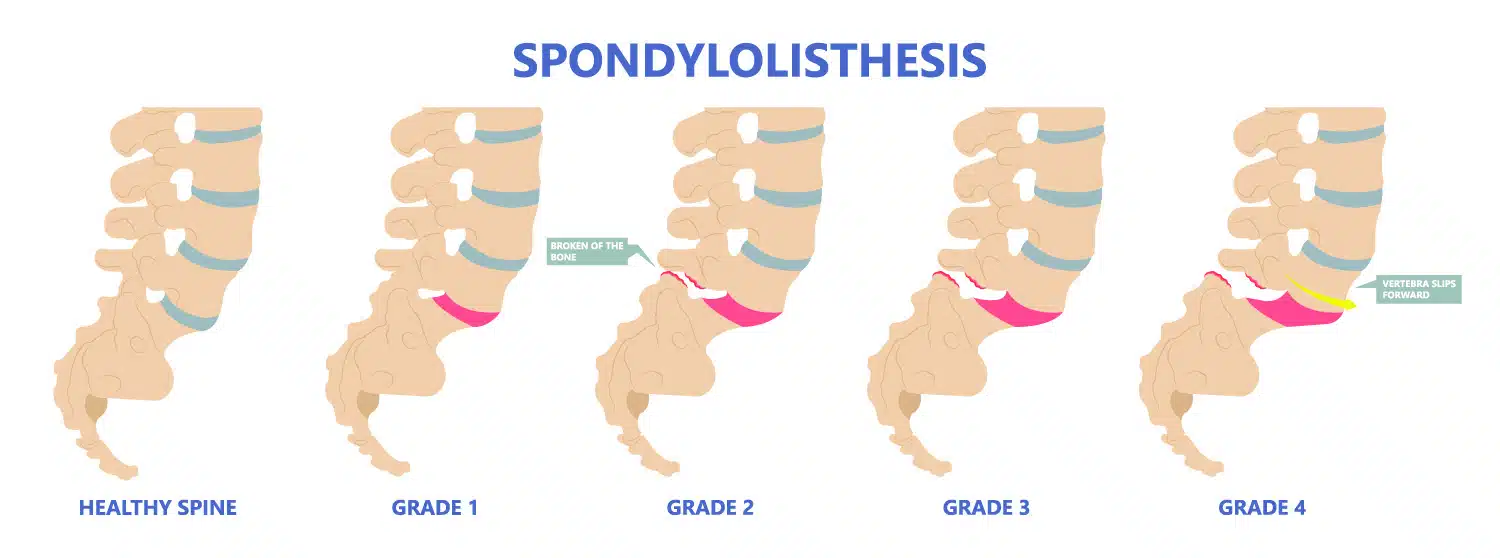
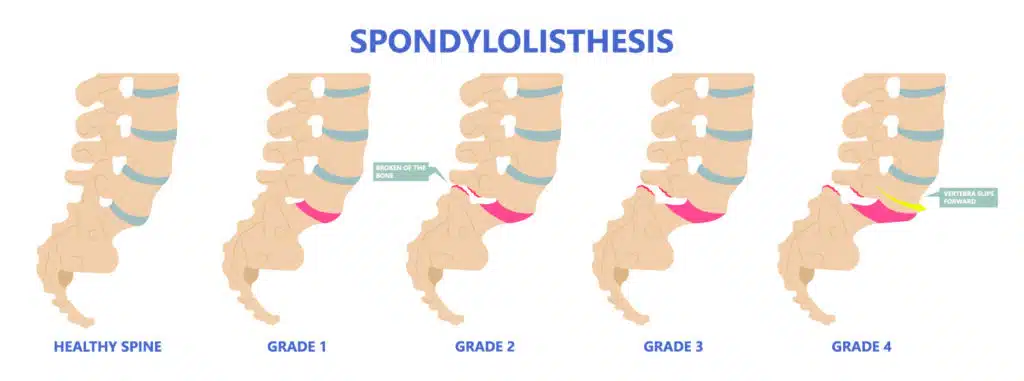
Depending on the degree of the forward slip, the severity of this process is graded as mild, severe, or complete slip (spondyloptosis) - described later in Myerding classification.
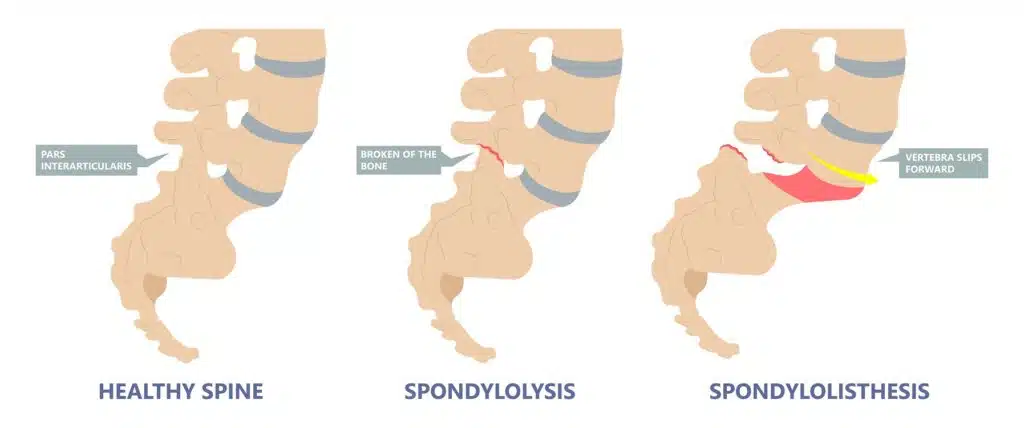
In the most common isthmic spondylolisthesis, which leads to an L5/S1 slip, the following stages have been identified.
- Pars stress reaction (sclerosis with incomplete bone disruption/fracture)
- Spondylolysis (anatomic defect in the pars, radiolucent gap with adjacent bone sclerosis, without any translation of the vertebra)
- Spondylolisthesis (due to bilateral pars defect, forward translation of the superior vertebra over the inferior one)
The second most common types of spondylolisthesis are type I (dysplastic) and III (degenerative). Degenerative spondylolisthesis is most prevalent in the adult population, and levels affected most frequently are L4/L5 followed by L3/L4. Due to the chronicity of the instability, often associated degenerative changes in the intervertebral disc and facet joints occur. They often lead to secondary hypertrophy of the ligamentum flavum and subsequent spinal canal stenosis. This condition usually presents with bilateral buttock pain and neurogenic claudication (back pain eased by sitting down/leaning forward).
- Epidemiology
Estimates are that 4 to 6% of the population has a degree of lumbosacral spondylolisthesis. The majority of cases are asymptomatic. [5]
Most of the symptomatic high-grade slips occur in the pediatric/adolescent population participating in sports involving repetitive hyperextension, while adults tend to present with milder and more chronic onset of symptoms. [6]
The most commonly affected adolescent groups are female dancers or gymnasts with hyperlordosis and hyper flexibility, male football players, or weight lifters with limited motion at lumbar spine undergoing a growth spurt, or novice athletes vigorously training while having poor core strength. [7]
There are reports of familial association and congenital abnormalities, including spina bifida occulta, thoracic hyperkyphosis (Shauerman disease) as predisposing factors as well as general ligamentous laxity.
Several anatomical factors described below predispose to spondylolisthesis.
- Pathophysiology
Two mechanisms may cause the lytic defect. The first is the pincer effect due to repeated hyperextension. [8] The inferior facet of L4 and the superior facet of S1 creates a pincer effect on the pars interarticularis, causing a failure of the L5 pars. This condition is more likely to occur in a situation where the sacral slope has a low value with a more horizontally orientated superior sacral endplate. The second mechanism is when there is an increased sacral slope and hence increased traction on the pars interarticularis. [9] The repeated traction on the pars from a downsloping lumbosacral junction results in failure and fracture of the pars interarticularis. In high-grade slips, the anterosuperior part of the sacrum becomes dome-shaped, which may be due to repeated trauma to the anterosuperior apophyseal ring of the S1 vertebrae. [10]
The spinopelvic balance and the global spinal alignment are essential in understanding the etiology, grading, and planning the treatment protocol. [11] These parameters are measured on a standing lateral radiograph. The main parameters and their definitions are as follows.
- Pelvic Tilt (PT) is the angle measured between a line drawn from the center of the superior endplate of S1 to the center of rotation of the femoral head and the vertical reference line. [11]
- Sacral Slope (SS) is the angle between the line drawn along the superior end of the S1 endplate and the horizontal reference line. [11] The pelvic tilt (PT) and the sacral slope are referenced to the vertical and horizontal planes and hence can vary based on the position of the pelvis. Though the standard measurements are on a standing radiograph, the values of PT and SS alter between sitting and standing.
- The Pelvic Incidence (PI) is the angle between a line starting at the midline between centers of rotation of each femoral head drawn towards the midpoint of S1 superior endplate and a line perpendicular to the line drawn along the superior endplate of S1.[10] The normal value is 50 degrees. An increased Pelvic Incidence (PI) is associated with higher severity of slips. [12] In comparison to the PT and SS, the Pelvic Incidence is a fixed value and does not change with the position of the pelvis or in adult life. A value of 70 to 80 degrees presents in patients with significant spondylolisthesis. Pelvic Incidence = Pelvic Tilt + Sacral Slope
- Boxall’s Slip Angle and Dubosset’s lumbosacral angle measures the relationship between L5 and S1. [13] [14] The Boxalls slip angle is measured between the perpendicular to the posterior aspect of the S1 vertebrae and the lower border of L5. If slip angle measures >45 degrees, it is associated with a greater risk of slip progression, instability, and post-op pseudo-arthrosis. It predicts intervention and affects cosmesis as well as prognosis. [11] The Dubosset’s lumbosacral angle is measured between the posterior aspect of the S1 and the upper endplate of the L5. Unlike the slip angle, the lumbosacral angle does not involve surfaces that alter with dysplasia.
Forward translation of the vertebrae may cause a narrowing of the spinal canal at the level of the slip. This situation is rare as most of the slips are only grade I or II, but the secondary canal and foraminal stenosis can occur due to subsequent degenerative changes in facet joints, hypertrophy of ligamentum flavum, hypertrophic fibrous repair tissue of the pars defect, or bulging of L5/S1 disc. In severe L5/S1 slips, the L5 nerve root is most commonly affected by being pulled forward by the superior vertebra.
- History and Physical
Most cases of spondylolisthesis are asymptomatic.
Severe slips are uncommon, and deformity rarely progresses beyond Meyerding grade II (see Evaluation chapter).
Typical history and examination findings in symptomatic cases involve:
- Child participating in back hyperextension activities (gymnastics, football, weight lifting), most common age at presentation is 4 to 6 yrs old.
- In adults insidious onset of axial back pain exacerbated by physical activity, periodic exacerbations that vary in intensity and duration
- L5 radicular symptoms (in severe slips), including weakness of the extensor hallucis longus
- Bladder and bowel dysfunction (including cauda equina syndrome in extreme cases)
- Neurologic claudication secondary to spinal canal stenosis (buttock and leg pain worse with walking but improving with leaning forward or sitting)
Examination Findings
- Pain with back hyperextension. Hyperextending the lower back while standing on one leg is termed the "stork test."
- Limitation of lumbar spine flexion and extension
- Increased popliteal angle
- Gait alteration with abductors weakness (L5) (pelvic waddle)
- Flattened lumbar lordosis or kyphosis of the lumbosacral junction
- Palpable step-off of the spinous process
- Hamstring tightness (in extreme cases walking with hips and knees flexed- due to vertical orientation of the sacrum causing pelvic retroversion and compensatory lumbar hyperlordosis + shortened stride and lurched posture)
- "Heart-shaped" buttocks in severe cases of significant lumbosacral kyphosis and sacral retroversion (sacrum becoming more vertical in orientation and moving away from the head of the femurs).
- Straight leg raise test may be positive.
- Scoliosis may be present - this may be secondary to pain.
Listhetic crisis (rapid progression of symptoms). Common during a growth spurt or increased physical activities with bilateral pars failure.
- Severe back pain aggravated by extension and relieved by rest.
- Neurologic deficit
- Hamstring spasm - walk with a crouched gait
Following the history and examination, the best screening tool is an AP and lateral weight-bearing X-ray of the lumbar spine. [15] Lumbosacral spondylolisthesis can be best assessed mainly on the lateral view, but occasional coronal deformity should not be missed. In cases where clinical examination indicates an abnormal sagittal balance of the spinal column, a whole spine lateral standing X-ray is indicated. In the majority of cases, an isthmic defect will be detected on radiographs but in doubtful cases. An MRI scan is recommended. Oblique X-rays of the lumbosacral junction, Computerised Tomography (CT) scan, SPECT scans may also identify the defect but involve ionic radiation.
MRI scans are more sensitive in identifying pars lesions.MRI can also identify stress reactions that occur even before a fracture line develops. [16] In dysplastic cases, dome-shaped or significantly inclined sacrum can present as well as trapezoid-shaped L5 and dysplastic facets of S1. Neoplasms and infections are an extremely rare primary cause of spondylolisthesis but should merit consideration as a differential diagnosis in patients with constitutional symptoms. To assess dynamic instability, flexion and extension views should be obtained. Either 4 mm of translation or 10 degrees of angulation of motion compared to the adjacent motion segment are diagnostic for spondylolisthesis.
Grading of the forward slip is classified by Meyerding classification:
- Grade I <25% of the width of the vertebra on the lateral view
- Grade II 25 to 50%
- Grade III 50 to 75%
- Grade IV 75 to 100%
- Grade V >100% (spondyloptosis)
Pelvic incidence (PI) has a direct correlation to Meyerding's grade. [12]
The Spinal Deformity Study Group has created a new classification that guides treatment. This scale takes into account the spinopelvic parameters and the overall spinal alignment. [17]
- I < 50% slip, PI <45 degrees, Surgery only if symptoms not controlled by non-operative methods.
- II < 50% slip, PI 45 to 60, Surgery only if symptoms not controlled by non-operative methods.
- III < 50% slip, PI >60 degrees, posterolateral fusion can be considered
- IV >50% slip, balanced pelvis high SS / low PT, decompression + / - Posterolateral fusion may be adequate
- V >50% slip, Unbalanced pelvis (retroverted) Low SS / High PT, reduction of slip, and circumferential fusion may be a consideration.
- VI >50% slip, Unbalanced spine (retroverted pelvis) Low SS / High PT + C7 plumbline anterior to femoral heads reduction of slip and circumferential fusion may be considered.
MRI (T-2 weighted sequence is best to assess spinal canal stenosis, foraminal stenosis, and nerve root impingement, as well as the morphology of lumbar and sacral vertebrae which presence correlated with history and examination findings, will dictate the surgical management). The most commonly affected nerve root is L5.
- Treatment / Management
The majority of the cases can be treated non-operatively by:
- Thoracolumbosacral / lumbosacral brace. [18] In acute cases in the adolescent sportsperson bracing to prevent extension is shown to be superior to just activity modification.
- Activity modification (avoidance of hyperextension) [19]
- Core muscles strengthening focusing on the deep abdominal muscles and the multifidus muscle [20]
- Lumbar flexion-based exercises. [21]
- In cases of adult degenerative spondylolisthesis with canal stenosis, an epidural steroid injection can provide short-term relief. [22]
Non-operative management of acute cases among sportspersons was successful in 95% of patients, and only 5% required surgical intervention. Among that treated non-operatively, 82% returned to their previous level of play. [19] Approximately one-third of patients with spondylolisthesis experience a disease progression over time. Operative treatment is reserved for those with intractable pain or neurological symptoms, including claudication or radiculopathy. [23]
Surgical intervention has shown >80% success in appropriately selected patients, with a low incidence of complications. Surgical techniques include the following:
- In the pediatric population with pars fracture or non-union, surgical repair of the pars may be an option with lag screw or tension band wire technique or pedicle screw hook fixation. [24] [25]
- Uninstrumented fusion in situ, A randomized control trial by Moller [26] showed that there was no advantage in adding instrumentation. Pain, functional disability, and fusion rates were similar in both groups.
- Decompression, Though there was some skepticism in just performing decompression of the nerve roots without fusion, i.e Gills procedure, results show 70 % good results with regards to patient satisfaction. Only grade I and II patients met the inclusion criteria for the study. [27]
- Instrumented posterolateral fusion with decompression is the standard procedure. [26]
- Anterior / posterior / transforaminal and direct lateral lumbosacral interbody fusion, reduction, and fusion. [28] The anterior, posterior, transforaminal, and direct lateral indicate the path through which the interbody device or cage is inserted. Posterior lumbar interbody fusion (PLIF) involves the insertion of the cage between the vertebral bodies medial to facets. Transforaminal lumbar interbody fusion (TLIF) requires facetectomy and a more lateralized and transforaminal approach to the disc space. Anterior Lumbar Interbody Fusion (ALIF) is via a trans or retroperitoneal approach and offers better access to disc space and endplate. They can also be associated with retrograde ejaculation and sexual dysfunction. Direct lateral or the transpsoas approach can only access the disc spaces above the L5 vertebrae. The iliac crest is in the path of reaching the L5/S1 disc on the direct lateral approach. [29]
- Reduction with spondylolectomy (vertebrectomy) of L5 and fusion of L4 on S1. [30] In severe slips removing the L5 vertebrae allows reduction and better spinal alignment
- Sacral dome resection and fusion. [31]
Operative options should be considered only if non-operative options fail or symptoms are significant. The reduction of the slip is controversial as in approximately 20% of cases, it causes L5 nerve root injury. Nevertheless, some evidence suggests better functional and cosmetic outcomes for patients who underwent reduction and instrumented fusion. [32] Foraminal decompression may also be necessary. Interbody fusion with the maintenance of intervertebral space improves the foraminal height, helps restore lumbar lordosis, and avoids fusion to L4 in high-grade slips. Each case requires an individual approach, and factors like the degree of spondylolisthesis, predominant neurological symptoms, and patients comorbidities should be taken into consideration. [33] Minimally invasive surgical techniques are gaining in popularity. [34]
- Differential Diagnosis
- Mechanical or muscular back pain
- Disc degeneration, facet joint osteoarthritis (OA), and/or cyst
- Lumbar canal stenosis secondary to degenerative changes
- Neoplastic process/metastases
- Infection (discitis, TB, paraspinal abscess)
- Vascular claudication (improves at rest in a standing position while neurological claudication improves with lumbar spine flexion - leaning forward or sitting)
Despite the estimate of up to 6% of the population suffering from spondylolisthesis, the majority of them are asymptomatic. Only a small percentage of symptomatic cases will require surgical treatment.
Worst prognosis in cases of:
- Very young age at presentation
- Female
- Slip angle >45 degrees
- High-grade slip
- Degenerative slip (most commonly in adults)
- Complications
- The most common reported neurological complication after lumbosacral spondylolisthesis surgery is L5 nerve root dysfunction. It is most frequently associated with high-grade slips and attempts of slip reduction as well as foraminal stenosis decompression. L5 nerve root dysfunction is usually transient and resolves within a few months in the postoperative period. In their cadaveric study, Petraco et al. found out that 71% of total nerve strain occurs during the second half of the reduction. [35]
- Pseudoarthrosis
- Adjacent segment disease (2 to 3%)
- Surgical site infection (0.1 to 2%)
- Positioning neuropathy: Lateral femoral cutaneous nerve - from a prone position with iliac bolster, ulnar nerve, or brachial plexopathy with inappropriate arm position) [36]
Complication rate increases with age, increased intraoperative blood loss, longer operative time, the number of levels fused.
- Deterrence and Patient Education
Sports coaches and personal trainers working with children and adolescents especially those practicing gymnastics, football, or weight lifting, should be aware of the symptoms of spondylosis and spondylolisthesis. They should be able to identify cases when pain does not improve after rest and basic stretching and strengthening exercises. These sportspersons need to be referred for specialist evaluation to diagnose and treat. This is particularly important as braces that prevent extension and activity reduction have shown excellent results.
Affected patients should be educated about the importance of activity modifications and physiotherapy and engage with core muscle strengthening and flexion exercises for symptomatic treatment.
They should receive reassurance that most of the symptoms are transient. But at the same time, especially those with a high risk of slip progression should be followed up by a specialist Orthopedic surgeon and educated about symptoms and signs of slip progression and potentially serious complications like cauda equina syndrome.
- Pearls and Other Issues
Pars interarticularis defects were common in sportsperson involved in increased activity. Hyperextension of the spine during the sport was a risk factor. In cricket fast bowlers extended and laterally flexed their spine, before throwing the ball to increase the speed of delivery. This repetitive movement increased the likelihood of developing a pars defect. In a recent review pars interarticularis defects were more common in the following sports, diving (35.38%), cricket (31.97%), baseball/softball (26.91%), rugby (22.22%), weightlifting (19.49%), sailing (17.18%), table tennis (15.63%), and wrestling (14.74%). [19] The suspicion that young adolescent sportspersons could develop spondylolysis is crucial in early diagnosis and prevention of progression. Bracing and activity restriction has shown excellent results with a good return to the same level of play.
- Enhancing Healthcare Team Outcomes
A high level of suspicion within sports coaches, general practitioners, and parents is needed to recognize patients with symptoms of spondylolisthesis.
Groups at risk like adolescent gymnasts, football players, and weight lifters should undergo health screening checks at regular intervals, and those with a history of lower back pain associated with activities undergo further evaluation and examination with those with suggestive signs and symptoms undergoing radiological investigations.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
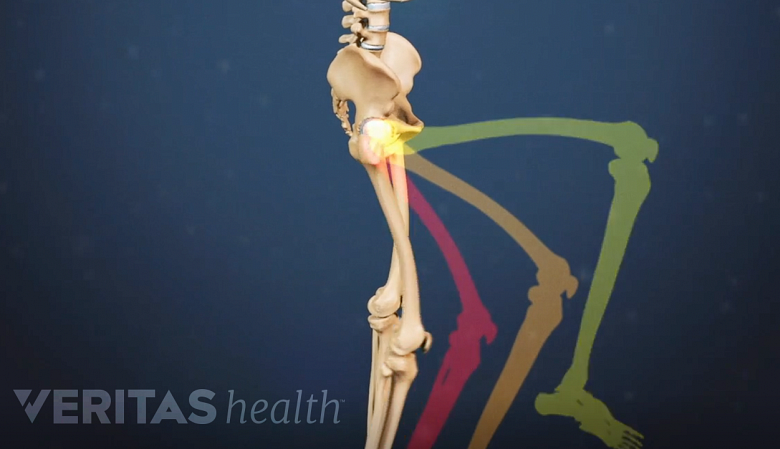
Spino pelvic parameters showing Pelvic tilt (PT), Sacral slope (SS) and Pelvic incidence (PI). Pelvic incidence (PI) = Pelvic tilt (PT) + Sacral slope (SS) Contributed by George Ampat FRCS
Spondylolysis with Spondylolisthesis, showing spino pelvic parameters, slip, dysplasia of upper endplate of S1, Slip angle (SA = angle between inferior endplate of L5 and line perpendicular to the S1 posterior wall) and lumbo sacral angle (LSA = angle (more...)
Lateral X-ray of the pelvis and lower lumbar spine showing spondylolysis and spondylolisthesis. Contributed by George Ampat FRCS
A - Degree of slip - Meyerding's grading. B - Spinopelvic parameters Slip angle (SA) and Lumbosacral angle (LSA). C Spinopelvic parameters showing Sacral slope (SS), Pelvic tilt (PT) and Pelvic incidence (PI). Contributed by George Ampat FRCS
Whole spine X-ray showing C7 plumbline. A vertical line dropped from the C7 vertebra. Should fall just behind the heads of the femurs. This allows economic weight bearing. Contributed by George Ampat FRCS
Disclosure: Katarzyna Studnicka declares no relevant financial relationships with ineligible companies.
Disclosure: George Ampat declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2023 Jul 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Spondylolysis and spondylolisthesis in children. [Instr Course Lect. 1983] Spondylolysis and spondylolisthesis in children. Hensinger RN. Instr Course Lect. 1983; 32:132-51.
- [Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis: a retrospective radiological and clinical analysis]. [Acta Chir Orthop Traumatol Cec...] [Adjacent segment degeneration after lumbosacral fusion in spondylolisthesis: a retrospective radiological and clinical analysis]. Zencica P, Chaloupka R, Hladíková J, Krbec M. Acta Chir Orthop Traumatol Cech. 2010 Apr; 77(2):124-30.
- Review Spondylolysis and spondylolisthesis in children and adolescents: II. Surgical management. [J Am Acad Orthop Surg. 2006] Review Spondylolysis and spondylolisthesis in children and adolescents: II. Surgical management. Cheung EV, Herman MJ, Cavalier R, Pizzutillo PD. J Am Acad Orthop Surg. 2006 Aug; 14(8):488-98.
- Epidemiology, Treatment, and Performance-Based Outcomes in American Professional Baseball Players With Symptomatic Spondylolysis and Isthmic Spondylolisthesis. [Am J Sports Med. 2020] Epidemiology, Treatment, and Performance-Based Outcomes in American Professional Baseball Players With Symptomatic Spondylolysis and Isthmic Spondylolisthesis. Gould HP, Winkelman RD, Tanenbaum JE, Hu E, Haines CM, Hsu WK, Kalfas IH, Savage JW, Schickendantz MS, Mroz TE. Am J Sports Med. 2020 Sep; 48(11):2765-2773. Epub 2020 Aug 14.
- Review Acute progression of spondylolysis to isthmic spondylolisthesis in an adult. [Spine (Phila Pa 1976). 2002] Review Acute progression of spondylolysis to isthmic spondylolisthesis in an adult. Stone AT, Tribus CB. Spine (Phila Pa 1976). 2002 Aug 15; 27(16):E370-2.
Recent Activity
- Lumbosacral Spondylolisthesis - StatPearls Lumbosacral Spondylolisthesis - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Spondylolisthesis
Spondylolisthesis is slippage of a lumbar vertebra in relation to the vertebra below it. Anterior slippage (anterolisthesis) is more common than posterior slippage (retrolisthesis). Spondylolisthesis has multiple causes. It can occur anywhere in the spine and is most common in the lumbar and cervical regions. Lumbar spondylolisthesis may be asymptomatic or cause pain when walking or standing for a long time. Treatment is symptomatic and includes physical therapy with lumbar stabilization.
There are five types of spondylolisthesis, categorized based on the etiology:
Type I, congenital: caused by agenesis of superior articular facet
Type II, isthmic: caused by a defect in the pars interarticularis (spondylolysis)
Type III, degenerative: caused by articular degeneration as occurs in conjunction with osteoarthritis
Type IV, traumatic: caused by fracture, dislocation, or other injury
Type V, pathologic: caused by infection, cancer, or other bony abnormalities
Spondylolisthesis usually involves the L3-L4, L4-L5, or most commonly the L5-S1 vertebrae.
Types II (isthmic) and III (degenerative) are the most common.
Type II often occurs in adolescents or young adults who are athletes and who have had only minimal trauma; the cause is a weakening of lumbar posterior elements by a defect in the pars interarticularis (spondylolysis). In most younger patients, the defect results from an overuse injury or stress fracture with the L5 pars being the most common level.
Type III (degenerative) can occur in patients who are > 60 and have osteoarthritis ; this form is six times more common in women than men.
Anterolisthesis requires bilateral defects for type II spondylolisthesis. For type III (degenerative) there is no defect in the bone.

ZEPHYR/SCIENCE PHOTO LIBRARY
Spondylolisthesis is graded according to the percentage of vertebral body length that one vertebra subluxes over the adjacent vertebra:
Grade I: 0 to 25%
Grade II: 25 to 50%
Grade III: 50 to 75%
Grade IV: 75 to 100%
Spondylolisthesis is evident on plain lumbar x-rays. The lateral view is usually used for grading. Flexion and extension views may be done to check for increased angulation or forward movement.
Mild to moderate spondylolisthesis (anterolisthesis of ≤ 50%), particularly in the young, may cause little or no pain. Spondylolisthesis can predispose to later development of foraminal stenosis . Spondylolisthesis is generally stable over time (ie, permanent and limited in degree).
Treatment of spondylolisthesis is usually symptomatic. Physical therapy with lumbar stabilization exercises may be helpful.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Spondylolisthesis: Definition, Causes, Symptoms, and Treatment
by Dave Harrison, MD • Last updated November 26, 2022
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Reddit (Opens in new window)
What is Spondylolisthesis?
The spine is comprised of 33 bones, called vertebra , stacked on top of each other interspaced by discs . Spondylolisthesis is a condition where one vertebra slips forward or backwards relative to the vertebra below. More specifically, retrolisthesis is when the vertebra slips posteriorly or backwards, and anterolisthesis is when the vertebra slips anteriorly or forward.
Spondylosis vs Spondylolisthesis
Spondylosis and Spondylolisthesis are different conditions. They can be related but are not the same. Spondylosis refers to a fracture of a small bone, called the pars interarticularis, which connects the facet joint of the vertebra to the one below. This may lead to instability and ultimately slippage of the vertebra. Spondylolisthesis, on the other hand, refers to slippage of the vertebra in relation to the one below.
Types and Causes of Spondylolisthesis
There are several types of spondylolisthesis, often classified by their underlying cause:
Degenerative Spondylolisthesis
Degenerative spondylolisthesis is the most common cause, and is due to general wear and tear on the spine. Overtime, the bones and ligaments which hold the spine together may become weak and unstable.
Isthmic Spondylolisthesis
Isthmic spondylolisthesis is the result of another condition, called “ spondylosis “. Spondylosis refers to a fracture of a small bone, called the pars interarticularis, which connects the facet joint of the vertebra to the one below. If this interconnecting bone is broken, it can lead to slippage of the vertebra. This can sometimes occur during childhood or adolsence but go unnoticed until adulthood when degenerative changes cause worsening slippage.
Congenital Spondylolisthesis
Congenital spondylolisthesis occurs when the bones do not form correctly during fetal development
Traumatic Spondylolisthesis
Traumatic spondylolisthesis is the result of an injury such as a motor vehicle crash
Pathologic Spondyloslisthesis
Pathologic spondylolisthesis is when other disorders weaken the points of attachment in the spine. This includes osteoporosis, tumors, or infection that affect the bones and ligaments causing them to slip.
Iatrogenic Spondylolisthesis
Iatrogenic spondylolisthesis is the result of a prior surgery. Some operations of the spine, such as a laminectomy, may lead to instability. This can cause the vertebra to slip post operatively.
Spondylolisthesis Grades
Spondylolisthesis is classified based on the degree of slippage relative to the vertebra below
- Grade 1 : 1 – 25 % forward slip. This degree of slippage is usually asymptomatic.
- Grade 2: 26 – 50 % forward slip. May cause mild symptoms such as stiffness and pain in your lower back after physical activity, but it’s not severe enough to affect your everyday activities.
- Grade 3 : 51 – 75 % forward slip. May cause moderate symptoms such as pain after physical activity or sitting for long periods.
- Grade 4: 76 – 99% forward slip. May cause moderate to severe symptoms.
- Grade 5: Is when the vertebra has slipped completely of the spinal column. This is a severe condition known as “spondyloptysis”.
Symptoms of Spondylolisthesis
Spondylolisthesis can cause compression of spinal nerves and in severe cases, the spinal cord. The symptoms will depend on which vertebra is affected.
Cervical Spondylolisthesis (neck)
- Arm numbness or tingling
- Arm weakness
Lumbar Spondylolisthesis (low back)
- Buttock pain
- Leg numbness or tingling
- Leg weakness
Diagnosing Spondylolisthesis
Your doctor may order imaging tests to confirm the diagnosis and determine the severity of your spondylolisthesis. The most common imaging tests used include:
- X-rays : X-rays can show the alignment of the vertebrae and any signs of slippage.
- CT scan: A CT scan can provide detailed images of the bones and soft tissues in your back, allowing your doctor to see any damage or abnormalities.
- MRI: An MRI can show the spinal cord and nerves, as well as any herniated discs or other soft tissue abnormalities.
Treatments for Spondylolisthesis
Medications.
For those experiencing pain, oral medications are first line treatments. This includes non-steroidal anti-inflammatory medications (NSAIDs) such as ibuprofen, acetaminophen, or in severe cases opioids or muscle relaxants (with extreme caution). Topical medications such as lidocaine patches are also sometimes used.
Physical Therapy
Physical therapy can help improve mobility and strengthen muscles around your spine to stabilize your neck and lower back. You may also receive stretching exercises to improve flexibility and balance exercises to improve coordination.
Surgery is reserved for severe cases of spondylolisthesis in which there is a high degree of instability and symptoms of nerve compression.
In these cases a spinal fusion may be necessary. This surgery joins two or more vertebra together using rods and screws, in order to improve stability.
Reference s
- Alfieri A, Gazzeri R, Prell J, Röllinghoff M. The current management of lumbar spondylolisthesis. J Neurosurg Sci. 2013 Jun;57(2):103-13. PMID: 23676859.
- Stillerman CB, Schneider JH, Gruen JP. Evaluation and management of spondylolysis and spondylolisthesis. Clin Neurosurg. 1993;40:384-415. PMID: 8111991.
About the Author
Dave Harrison, MD
Dr. Harrison is a board certified Emergency Physician with a part time appointment at San Francisco General Medical Center and is an Assistant Clinical Professor-Volunteer at the UCSF School of Medicine. Dr. Harrison attended medical school at Tufts University and completed his Emergency Medicine residency at the University of Southern California. Dr. Harrison manages the editorial process for SpineInfo.com.
Select a Location

SEARCH THIS SITE
- All Conditions & Treatments
- Brain Tumor Center
- Cerebrovascular Diseases
- Face Pain & Headaches
- Memory Disorders
- Movement Disorders
- Multiple Sclerosis (MS)
- Neuro-Oncology
- Neurocritical Care
- Neuromuscular Disorders
- Radiation Oncology
- Sleep Disorders
- Spine Disorders and Back Pain
- Neurologists & Neurosurgeons
- Our Locations
Lumbar Spondylolisthesis
What is lumbar spondylolisthesis.
Lumbar spondylolisthesis occurs when a vertebra in the lower spine shifts out of place and onto the bone below it, often because of weakness or a stress fracture. It is more common in young athletes and older adults who suffer from arthritis. It can cause pain, stiffness, and muscle spasms.
Non-surgical options are often successful in relieving the symptoms, but sometimes surgery is needed. Spinal fusion is one of the more common options to relieve lumbar spondylolisthesis.
What You Can Expect at UTHealth Neurosciences
The UTHealth Neurosciences Spine Center brings together a multidisciplinary team of board-certified, fellowship-trained neurosurgeons, neurologists, researchers, and pain management specialists who work together to help provide relief for even the most complex problems. Your team will share insights, leading to better treatment decisions and outcomes.
We first investigate nonsurgical treatment options, including medical management, pain management, physical therapy, rehabilitation, and watchful waiting. When surgery is needed, our neurosurgeons routinely employ innovative minimally invasive techniques. Throughout the treatment process, we will work closely with the doctor who referred you to ensure a smooth transition back to your regular care. While you are with us, you will receive expert care, excellent communication, and genuine compassion.
Causes of Lumbar Spondylolisthesis
Usually lumbar spondylolisthesis results from spondylolysis, a crack or stress fracture in the pars interarticularis, the thin portion of the vertebra that connects the upper and lower facet joints.
In children, spondylolisthesis usually occurs between the fifth bone in the lower back (lumbar vertebra) and the first bone in the sacrum (pelvis) area. The injury is most commonly seen in children and adolescents who participate in sports that involve repeated stress on the lower back, including football, weightlifting, and gymnastics. Repetitive stress can cause a fracture on one or both sides of the vertebra. It also may be caused by a birth defect in the lumbar spine or an acute injury.
In adults, the most common cause is abnormal wear on the cartilage and bones, such as through arthritis. The condition affects people over the age of 50 and is more common in women than in men. Bone disease and fractures also can cause lumbar spondylolisthesis. Genetics may play a role, as some people are born with thinner-than-normal vertebral bone.
Early Signs of Lumbar Spondylolisthesis and Diagnosis
Symptoms of spondylolisthesis may vary from none to mild to severe. The most common symptom is low back pain.
The condition can cause lordosis (swayback). In later stages it may result in kyphosis (roundback) as the upper spine falls off the lower spine. General symptoms are lower back pain; muscle tightness in the hamstrings; pain, numbness, or tingling in the thighs and buttocks; tenderness in the area of the vertebra that is out of place; weakness in the legs; and difficulty standing and walking.
Our spine specialists diagnose spondylolisthesis by taking a thorough medical history, conducting a physical exam, and asking you to undergo imaging studies that may include X-ray, CT scan, or MRI scan.
Treatments for Lumbar Spondylolisthesis
Your doctor may use X-rays, CT scans, or an MRI, as well as a physical exam, to determine the severity of your condition. Initial treatment may include rest, physical therapy, nonsteroidal anti-inflammatory drugs, oral corticosteroids, and/or bracing that limits movement of the spine and allows the fracture to heal.
Surgery may be recommended for patients who have severe or high-grade slippage of the vertebra, such as when more than 50% of the fractured vertebra slips forward on the vertebra below it. The procedures most often recommended for people with lumbar spondylolisthesis are spinal fusion or a laminectomy to decompress the nerves.
Anatomy of the neck and spine
The spine is divided into the following regions:
- The cervical region (vertebrae C1-C7) encompasses the first seven vertebrae under the skull. Their main function is to support the weight of the head, which averages 10 pounds. The cervical vertebrae are more mobile than other areas, with the atlas and axis vertebra facilitating a wide range of motion in the neck. Openings in these vertebrae allow arteries to carry blood to the brain and permit the spinal cord to pass through. They are the thinnest and most delicate vertebrae.
- The thoracic region (vertebrae T1-T12) is composed of 12 small bones in the upper chest. Thoracic vertebrae are the only ones that support the ribs. Muscle tension from poor posture, arthritis, and osteoporosis are common sources of pain in this region.
- The lumbar region (vertebrae L1-L5) features vertebrae that are much larger to absorb the stress of lifting and carrying heavy objects. Injuries to the lumbar region can result in some loss of function in the hips, legs, and bladder control.
- The sacral region (vertebrae S1-S5) includes a large bone at the bottom of the spine. The sacrum is triangular-shaped and consists of five fused bones that protect the pelvic organs.
Spine Disease and Back Pain
Arthrodesis Artificial Disc Replacement Cauda Equina Syndrome Cervical corpectomy Cervical disc disease Cervical discectomy and fusion Cervical herniated disc Cervical laminectomy Cervical laminoforaminotomy Cervical radiculopathy Cervical spondylosis (degeneration) Cervical stenosis Cervical spinal cord injury Degenerative Disc Disease Foraminectomy Foraminotomy Herniated discs Injections for Pain Kyphoplasty Laminoplasty Lumbar herniated disc Lumbar laminectomy Lumbar laminotomy Lumbar radiculopathy Lumbar spondylolisthesis Lumbar spondylosis (degeneration) Lumbar stenosis
Neck Pain Peripheral Nerve Disorders Radiofrequency Ablation Scoliosis Spinal cord syrinxes Spinal deformities Spinal injuries Spinal fractures and instability Spinal Cord Stimulator Trial and Implantation Spinal Fusion Spinal Radiosurgery Spine and spinal cord tumors Spondylolisthesis Stenosis Tethered spinal cord Thoracic herniated disc Thoracic spinal cord injury Transforaminal Lumbar Interbody Fusion Vertebroplasty
At UTHealth Neurosciences, we offer patients access to specialized neurological care at clinics across the greater Houston area. To ask us a question, schedule an appointment, or learn more about us, please call (713) 486-8100, or click below to send us a message. In the event of an emergency, call 911 or go to the nearest Emergency Room.
- McGovern Medical School Facebook Page
- McGovern Medical School X Page
- McGovern Medical School Instagram Page
- McGovern Medical School YouTube Page
- McGovern Medical School LinkedIn Page
- Medical School IT (MSIT)
- Campus Carry
- Emergency Info
- How to report sexual misconduct
- University Website Policies

- See All Locations
- Primary Care
- Urgent Care Facilities
- Emergency Rooms
- Surgery Centers
- Medical Offices
- Imaging Facilities
- Browse All Specialties
- Diabetes & Endocrinology
- Digestive & Liver Diseases
- Ear, Nose & Throat
- General Surgery
- Neurology & Neurosurgery
- Obstetrics & Gynecology
- Orthopaedics
- Pain Medicine
- Pediatrics at Guerin Children’s
- Urgent Care
- Medical Records Request
- Insurance & Billing
- Pay Your Bill
- Advanced Healthcare Directive
- Initiate a Request
- Help Paying Your Bill
Spondylolisthesis
Spondylolisthesis is a displacement of a vertebra in which the bone slides out of its proper position onto the bone below it. Most often, this displacement occurs following a break or fracture.
Surgery may be necessary to correct the condition if too much movement occurs and the bones begin to press on nerves.
Other complications may include:
- Chronic back pain
- Sensation changes
- Weakness of the legs
- Temporary or permanent damage of spinal nerve roots
- Loss of bladder control
When a vertebra slips out of proper alignment, discs can be damaged. To surgically correct this condition, a spinal surgeon removes the damaged disc. The slipped vertebra is then brought back into line, relieving pressure on the spinal nerve.
Types of spondylolisthesis include:
- Dysplastic spondylolisthesis , caused by a defect in part of the vertebra
- Isthmic spondylolisthesis , may be caused by repetitive trauma and is more common in athletes exposed to hyperextension motions
- Degenerative spondylolisthesis , occurs with cartilage degeneration because of arthritic changes in the joints
- Traumatic spondylolisthesis , caused by a fracture of the pedicle, lamina or facet joints as a result of direct trauma or injury to the vertebrae
- Pathologic spondylolisthesis , caused by a bone defect or abnormality, such as a tumor
Symptoms may vary from mild to severe. In some cases, there may be no symptoms at all.
Spondylolisthesis can lead to increased lordosis (also called swayback), and in later stages may result in kyphosis, or round back, as the upper spine falls off the lower.
Symptoms may include:
- Lower back pain
- Muscle tightness (tight hamstring muscle)
- Pain, numbness or tingling in the thighs and buttocks
- Tenderness in the area of the vertebra that is out of place
- Weakness in the legs
- Stiffness, causing changes in posture and gait
- A semi-kyphotic posture (leaning forward)
- A waddling gate in advanced cases
- Lower-back pain along the sciatic nerve
- Changes in bladder function
Spondylolisthesis may also produce a slipping sensation when moving into an upright position and pain when sitting and trying to stand.
Spondylolisthesis may appear in children as the result of a birth defect or sudden injury, typically occurring between the fifth bone in the lower back (lumbar vertebra) and the first bone in the sacrum (pelvis).
In adults, spondylolisthesis is the result of abnormal wear on the cartilage and bones from conditions such as arthritis , trauma from an accident or injury, or the result of a fracture, tumor or bone abnormality.
Sports that place a great deal of stress on bones may cause additional deterioration, fractures and bone disease, which may cause the bones of the spine to become weak and shift out of place.
A simple X-ray of the back will show any cracks, fractures or vertebrae slippage that are the signs of spondylolisthesis.
A CT scan or an MRI may be used to further diagnose the extent of the damage and possible treatments.
Treatment for spondylolisthesis will depend on the severity of the vertebra shift. Stretching and exercise may improve some cases as back muscles strengthen.
Non-invasive treatments include:
- Heat/Ice application
- Pain medicine (Tylenol and/or NSAIDS)
- Physical therapy
- Epidural injections
Surgery may be needed to fuse the shifted vertebrae if the patient has:
- Severe pain that does not get better with treatment
- A severe shift of a spine bone
- Weakness of muscles in a leg or both legs
Surgical process realigns the vertebrae, fixing them in place with a small rod that is attached with a pedicle screw, adding stability to the spine with or without the addition to an interbody (bone graft or cage) placed between the vertebra from the side or front.
Choose a doctor and schedule an appointment.
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.
(1-800-233-2771)
Available 7 days a week, 6 am - 9 pm PT
Expert Care for Life™ Starts Here
Looking for a physician.
Spondylolisthesis
Spondylolisthesis is where one of the bones in your spine, called a vertebra, slips forward. It can be painful, but there are treatments that can help.
It may happen anywhere along the spine, but is most common in the lower back.
Check if you have spondylolisthesis
The main symptoms of spondylolisthesis include:
- pain in your lower back, often worse when standing or walking and relieved when sitting or bending forward
- pain spreading to your bottom or thighs
- tight hamstrings (the muscles in the back of your thighs)
- pain, numbness or tingling spreading from your lower back down 1 leg ( sciatica )
Spondylolisthesis does not always cause symptoms.
Spondylolisthesis is not the same as a slipped disc . This is when the tissue between the bones in your spine pushes out.

Non-urgent advice: See a GP if:
- you have lower back pain that does not go away after 3 to 4 weeks
- you have pain in your thighs or bottom that does not go away after 3 to 4 weeks
- you're finding it difficult to walk or stand up straight
- you're worried about the pain or you're struggling to cope
- you have pain, numbness and tingling down 1 leg for more than 3 or 4 weeks
What happens at your GP appointment
If you have symptoms of spondylolisthesis, the GP may examine your back.
They may also ask you to lie down and raise 1 leg straight up in the air. This is painful if you have tight hamstrings or sciatica caused by spondylolisthesis.
The GP may arrange an X-ray to see if a bone in your spine has slipped forward.
You may have other scans, such as an MRI scan , if you have pain, numbness or weakness in your legs.
Treatments for spondylolisthesis
Treatments for spondylolisthesis depend on the symptoms you have and how severe they are.
Common treatments include:
- avoiding activities that make symptoms worse, such as bending, lifting, athletics and gymnastics
- taking anti-inflammatory painkillers such as ibuprofen or stronger painkillers on prescription
- steroid injections in your back to relieve pain, numbness and tingling in your leg
- physiotherapy to strengthen and stretch the muscles in your lower back, tummy and legs
The GP may refer you to a physiotherapist, or you can refer yourself in some areas.
Waiting times for physiotherapy on the NHS can be long. You can also get it privately.
Surgery for spondylolisthesis
The GP may refer you to a specialist for back surgery if other treatments do not work.
Types of surgery include:
- spinal fusion – the slipped bone (vertebra) is joined to the bone below with metal rods, screws and a bone graft
- lumbar decompression – a procedure to relieve pressure on the compressed spinal nerves
The operation is done under general anaesthetic , which means you will not be awake.
Recovery from surgery can take several weeks, but if often improves many of the symptoms of spondylolisthesis.
Talk to your surgeon about the risks and benefits of spinal surgery.
Causes of spondylolisthesis
Spondylolisthesis can:
- happen as you get older – the bones of the spine can weaken with age
- run in families
- be caused by a tiny crack in a bone (stress fracture) – this is more common in athletes and gymnasts
Page last reviewed: 01 June 2022 Next review due: 01 June 2025
- Degenerative Spondylolisthesis Symptoms
By: Marco Funiciello, DO, Physiatrist
Peer-Reviewed
Degenerative spondylolisthesis typically causes low back pain along with a cluster of symptoms and signs in one or both legs.
Degenerative Spondylolisthesis: Common Symptoms and Signs
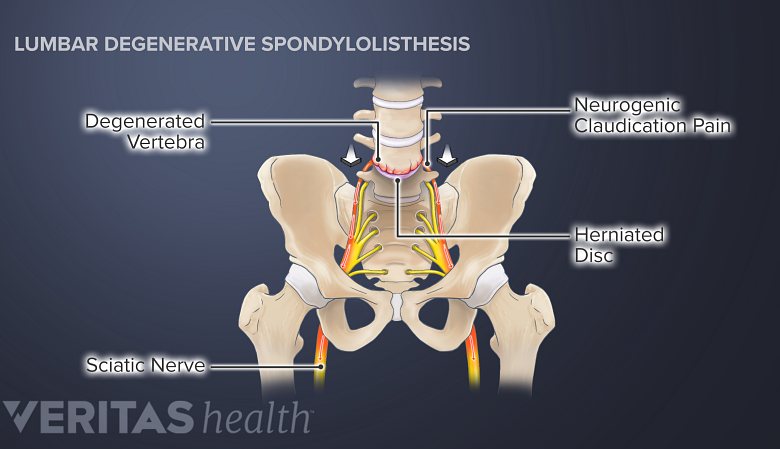
Degenerative spondylolisthesis symptoms include neurogenic claudication, sciatica, and radiculopathy.
In degenerative spondylolisthesis, the degenerated facet joints and other parts of the vertebral bone tend to increase in size. The enlarged, abnormal bone then encroaches upon the central canal and/or nerve hole (foramen) causing spinal stenosis or foraminal stenosis.
In This Article:
- Degenerative Spondylolisthesis
- Degenerative Spondylolisthesis Treatment
- Surgery for Degenerative Spondylolisthesis
Degenerative Spondylolisthesis Video
These changes typically result in some combination of the following symptoms and signs.
Persistent low back pain
Low back pain caused by degenerative spondylolisthesis is usually persistent and described as a consistent dull ache, 1 Cushnie D, Johnstone R, Urquhart JC, Gurr KR, Bailey SI, Bailey CS. Quality of Life and Slip Progression in Degenerative Spondylolisthesis Treated Nonoperatively. Spine (Phila Pa 1976). 2018;43(10):E574-E579. doi:10.1097/BRS.0000000000002429 but it may also feel like a sharp, stabbing sensation for some individuals.
The pain is typically localized in the low back region and may worsen with physical activity, standing, or walking.
Neurogenic claudication
Intermittent neurogenic claudication affects around 75% of people with degenerative spondylolisthesis. It is characterized by episodes of low back pain that radiate to both legs, along with accompanying sensations of tingling, a sensation of weakness, and hamstring spasm. 2 Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(4):36917. doi: 10.52965/001c.36917. PMID: 35910544; PMCID: PMC9329062. , 3 García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Espondilolistesis degenerativa lumbar I: principios generales. Acta Ortop Mex. 2020;34(5):324-328.. , 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
It is possible to have any combination of symptoms and they typically occur during walking variable distances or prolonged standing. 2 Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(4):36917. doi: 10.52965/001c.36917. PMID: 35910544; PMCID: PMC9329062.
Sciatica: Radiating leg pain
Back pain may radiate into the buttock, thighs, and into the leg and foot. 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
Radiating leg pain is commonly known as sciatica . This pain occurs due to the irritation, compression, or inflammation of spinal nerve roots in the lower back. 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
Radiculopathy: Abnormal sensations, weakness, and loss of muscle reflexes
When the spinal nerve roots are compressed or sufficiently inflamed and neurologic deficits are present, the condition is called radiculopathy . Radiculopathy may cause leg weakness and affect muscle reflexes. Additionally, numbness may be felt in the thigh, leg, and/or foot. 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
It may be challenging to perform activities that require strength, such as walking, climbing stairs, or lifting objects.
Little Known Symptoms of Degenerative Spondylolisthesis
As degenerative spondylolisthesis progresses, the symptoms may lessen due to compensatory mechanisms of the spine that increase spinal stability and prevent further progression.
However, in some individuals, the progression may continue and cause the following symptoms and signs.
Sleep disturbances
Back pain and leg pain may cause disturbed sleep or trouble falling asleep. 5 Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(3):327-335. doi:10.1007/s00586-007-0543-3
For this reason, some individuals may choose to sleep in the fetal position (sleeping on the side with knees bent close to the chest) to relieve leg symptoms. 5 Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(3):327-335. doi:10.1007/s00586-007-0543-3
Restless leg syndrome
Leg pain and claudication may sometimes cause restless legs syndrome. In this condition, aching or burning pain in the calves causes an irresistible urge to move the legs continuously, causing disturbed sleep. 5 Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(3):327-335. doi:10.1007/s00586-007-0543-3
Difficulty walking and imbalance
Degenerative spondylolisthesis may cause difficulty walking and maintaining balance.
As degenerative spondylolisthesis progresses, difficulties with walking and maintaining balance may be experienced. These signs arise from nerve compression caused by the slipped vertebra and associated degenerative changes, Altered posture, muscle weakness and reduced coordination may result. 6 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/
There are many nerves in our legs that are responsible for relaying information to the brain about position and balance. If these nerves are irritated or compressed in the spine then the brain may not get the necessary information needed for good balance and posture control.
These changes can impact mobility and function, making it harder to engage in normal daily activities.
Limited range of motion
Degenerative spondylolisthesis can affect lumbar range of motion due to the degenerative bone changes that prevent full segmental motion. Muscle spasm and stiffness may result.
Individuals may find it challenging to twist or engage in activities that involve spinal movement. This restricted range of motion can contribute to discomfort and stiffness in the affected area.
Menopause-Related Spondylolisthesis Symptoms
The onset of menopause may accelerate normal degenerative changes of the lumbar vertebrae, discs, facet joints, and ligaments. 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
Typically, the symptoms associated with this progression include low back pain, stiffness, and/or pain radiating down the leg (sciatica). 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
Read more about Sciatica Symptoms
Diagnosis of Degenerative Spondylolisthesis
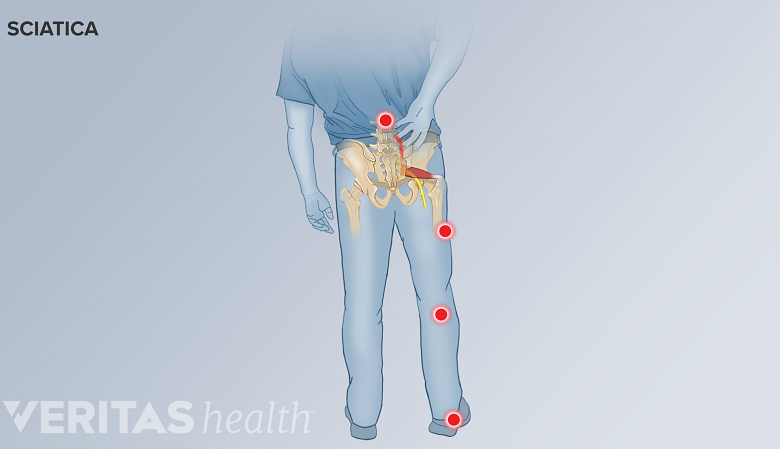
Radiating sciatica pain may occur in degenerative spondylolisthesis.
A physician trained in musculoskeletal conditions can help diagnose degenerative spondylolisthesis.
A comprehensive assessment of the patient’s history, past medical history, thorough physical examination, and review of any prior tests and imaging studies are performed.
During the review of patient history and the physical examination, physicians typically check for 7 Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022;92(6):e2021313. Published 2022 Jan 19. doi:10.23750/abm.v92i6.10526 :
- Pain pattern. Physicians ask about localized or radiating pain and the pattern of pain distribution to check if sciatica is present.
- Postural effects. In degenerative spondylolisthesis, pain is exacerbated while bending backward and relieved when bending forward.
- History of symptoms. Neurogenic claudication and hamstring spasm while walking or standing for variable periods of time may indicate spinal stenosis caused by degenerative spondylolisthesis.
If these symptoms and signs are noticed, the physician may order imaging tests to further investigate the condition.
Imaging Tests for Degenerative Spondylolisthesis
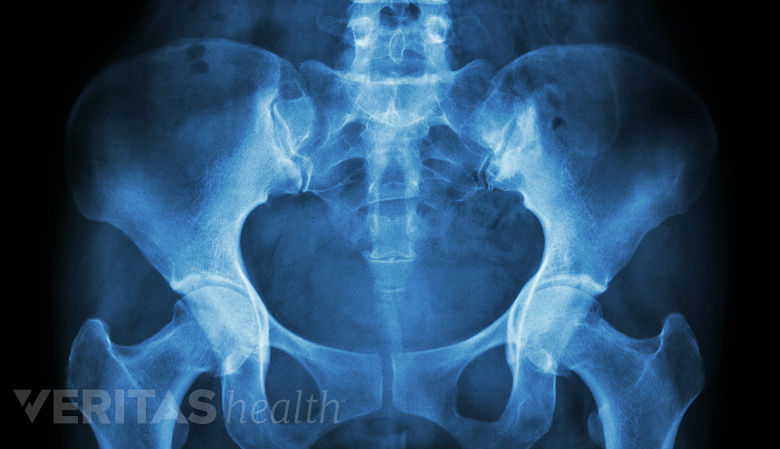
X-rays are helpful in diagnosing and assessing the extent of degenerative spondylolisthesis.
Imaging tests may help confirm the diagnosis of degenerative spondylolisthesis and provide evidence of the extent of progression of the condition.
- Standing lateral radiographs are considered the most reliable and standard test for diagnosing degenerative spondylolisthesis. 7 Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022;92(6):e2021313. Published 2022 Jan 19. doi:10.23750/abm.v92i6.10526
- Flexion-extension radiographs are used to determine if there is any motion of one vertebra upon the other (translation) and/or instability during spinal movements. 7 Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022;92(6):e2021313. Published 2022 Jan 19. doi:10.23750/abm.v92i6.10526
- Magnetic resonance imaging (MRI) scans may be used to check for spinal stenosis, nerve root compression, spinal cord involvement, and disc degeneration. 3 García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Espondilolistesis degenerativa lumbar I: principios generales. Acta Ortop Mex. 2020;34(5):324-328.. , 7 Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022;92(6):e2021313. Published 2022 Jan 19. doi:10.23750/abm.v92i6.10526 Some researchers consider MRI scans as the most reliable test to diagnose spinal stenosis in degenerative lumbar spondylolisthesis. 8 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed.; 2016.
- CT scans are used if bone involvement such as spondylolysis or isthmic spondylolisthesis is suspected, as these scans provide detailed evaluation of bone integrity.
If an MRI is not possible, computed tomography (CT) scans with myelography may be used as an alternative test. 7 Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022;92(6):e2021313. Published 2022 Jan 19. doi:10.23750/abm.v92i6.10526 , 8 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed.; 2016.
MRI scans or CT scans may also be used if severe neurogenic claudication is present, bowel and/or bladder incontinence is reported, and/or tumors are suspected.
- 1 Cushnie D, Johnstone R, Urquhart JC, Gurr KR, Bailey SI, Bailey CS. Quality of Life and Slip Progression in Degenerative Spondylolisthesis Treated Nonoperatively. Spine (Phila Pa 1976). 2018;43(10):E574-E579. doi: 10.1097/BRS.0000000000002429
- 2 Li N, Scofield J, Mangham P, Cooper J, Sherman W, Kaye A. Spondylolisthesis. Orthop Rev (Pavia). 2022 Jul 27;14(4):36917. doi: 10.52965/001c.36917 . PMID: 35910544; PMCID: PMC9329062.
- 3 García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Espondilolistesis degenerativa lumbar I: principios generales. Acta Ortop Mex. 2020;34(5):324-328..
- 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi: 10.1016/j.jot.2016.11.001
- 5 Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(3):327-335. doi: 10.1007/s00586-007-0543-3
- 6 Studnicka K, Ampat G. Lumbosacral Spondylolisthesis. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560679/
- 7 Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022;92(6):e2021313. Published 2022 Jan 19. doi: 10.23750/abm.v92i6.10526
- 8 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed.; 2016.
Dr. Marco Funiciello is a physiatrist with Princeton Spine and Joint Center. He has a decade of clinical experience caring for spine and muscle conditions with non-surgical treatments.
- Degenerative Spondylolisthesis Symptoms "> Share on Facebook
- Degenerative Spondylolisthesis Symptoms "> Share on Pinterest
- Degenerative Spondylolisthesis Symptoms "> Share on X
- Subscribe to our newsletter
- Print this article
- Degenerative Spondylolisthesis Symptoms &body=https://www.spine-health.com/conditions/spondylolisthesis/degenerative-spondylolisthesis-symptoms&subject= Degenerative Spondylolisthesis Symptoms "> Email this article
Editor’s Top Picks
Spondylolysis and spondylolisthesis, leg pain and numbness: what might these symptoms mean, sciatica symptoms, lumbar radiculopathy, isthmic spondylolisthesis symptoms.
Popular Videos

Lower Back Pain Treatment Video

Cervical Disc Replacement Surgery Video

Lumbar Herniated Disc Video

4 Steps to Relieve Sciatica Pain Video
Undergoing a Spinal Fusion?
Learn how bone growth stimulation therapy can help your healing process
Sponsored by Orthofix
Health Information (Sponsored)
- Take the Chronic Pain Quiz
- Suffering from Lumbar Spinal Stenosis? Obtain Long Term Pain Relief
- Learn How Bone Growth Therapy Can Help You
- Learn How Cedars-Sinai's Experts Can Relieve Your Pain
- Find a Doctor
- Transfer a Patient
- Patient Portal
Lumbar Spondylolisthesis
What is lumbar spondylolisthesis.
Lumbar spondylolisthesis is a condition in which a bone (vertebra) in the lumbar spine (lower back) slips forward out of position onto the bone below it. It may occur as a result of a defect, an injury, degeneration due to aging, or a disease.
Looking for a Second Opinion?
Lumbar Spondylolisthesis Symptoms
Depending on the degree of the slip, symptoms of lumbar spondylolisthesis can vary from mild to severe or not be present at all.
Symptoms may include:
- Lower back pain
- Muscle tightness
- Pain, numbness, or tingling in your thighs and buttocks
- Tenderness in the area where the vertebra is out of place
- Weakness in your legs
- Muscle spasms in your hamstring muscles
- Pain, numbness, or tingling down your leg or foot if slipped vertebra is pressing on a nerve
An imaging test is needed to determine whether or not you have lumbar spondylolisthesis. Contact a medical professional if you are having symptoms.
Lumbar Spondylolisthesis Treatments
Treatment for lumbar spondylolisthesis depends on the severity of the slip and your symptoms, along with your overall health. Minor slips may improve with conservative treatment, such as rest, pain medication, physical therapy, and a back brace.
For more severe cases, surgery may be recommended. Procedures for lumbar spondylolisthesis include:
- Decompressive laminectomy – part of the vertebra that is pressing on the nerves is removed to relieve symptoms
- Spinal fusion – two or more bones of the spine are fused together with real bone or synthetic materials
Additional Information
How common is lumbar spondylolisthesis.
Spondylolisthesis is the most common cause of back pain in teens.
Who gets lumbar spondylolisthesis?
In younger people, symptoms of spondylolisthesis often begin during their teenage growth spurt. Spondylolisthesis due to degeneration usually occurs after age 40.
Spondylolisthesis can be caused by spondylolysis, a defect in the connection between vertebrae that can lead to stress fractures. These stress fractures can weaken the bones so much that one slips out of place.
Fractures in the vertebrae can also be caused by certain sports that put a lot of stress on the lower back, such as gymnastics and weightlifting.
How is lumbar spondylolisthesis diagnosed?
Your doctor will likely perform a physical exam and an imaging test, such as an MRI scan or a CT scan, to diagnose lumbar spondylolisthesis.
Additional Resources
MedlinePlus | Spondylolisthesis
Find a Lumbar Spondylolisthesis Specialist
Get a Second Opinion for Lumbar Spondylolisthesis
Fast. Easy. Secure.
To give you the best possible experience, this site uses cookies. By continuing to use the site, you agree that we can save them on your device.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
All About the Lumbosacral Joint (L5-S1)
Where it is and and what it does
Spondylolisthesis
The lumbosacral joint, also called L5-S1, is a term used to describe a part of the spine. L5-S1 is the exact spot where the lumbar spine ends and the sacral spine begins. The lumbosacral joint is the joint that connects these bones.
L5-S1 is composed of the last bone in the low back, called L5, and the triangle-shaped bone beneath, known as the sacrum. The sacrum is made of five fused bones, of which the S1 is the topmost.
This article goes over the anatomy and function of the L5-S1. It also covers some of the medical problems that can affect this part of the spine.
The spinal column is the structure that allows you to stand upright. It also helps you twist, bend, and otherwise alter your trunk and neck position.
There are typically 24 movable bones in the spine that connect to the sacrum, a bony structure located below the lumbar vertebrae, and the coccyx, also called the tailbone. The sacrum and the coccyx each consist of multiple bones that fuse over time.
The vertebrae, which is another name for the spinal bones, are broken down into sections from top to tail, as follows.
- Cervical spine : Located in the neck, it has seven bones, labeled as C1 to C7
- Thoracic spine : Located in the mid-back, it has 12 bones. The thoracic spine vertebrae are labeled T1 to T12.
- Lumbar spine : Corresponding to your low back, it has five bones. These bones are labeled L1 to L5.
- Sacrum : This triangularly shaped bone is formed of five bones. These bones start to fuse soon after birth and continue to do so until they are completely fused by around the age of 30. The individual fused bones are labeled S1 to S5.
- Coccyx : The tailbone is likewise made of individual bones that are movable at birth but fuse over time. The coccyx is semi-fused, and in many cases fully fused, by adulthood. The component bones are labeled as Co1 to Co4. Most people have four segments, but some have three or five.
Each area of the spine has a curve, and these curves go in opposing directions. In the neck and lower back, the spinal curve points forward, as viewed in profile. The thoracic and sacral curves go back.
The areas where the spinal curve directions change are called junctional levels. Injury risk may be higher at junctional levels because your body weight shifts direction as the curves shift directions.
The L5-S1 junction is located between the lumbar curve and the sacral curve. The lumbar curve sweeps forward. The sacral curve opposes the direction of the lumbar curve and goes backward.
The L5-S1 junction is particularly vulnerable to misalignment, wear and tear, and injury. This is because the top of the sacrum is positioned at an angle in most people. Aging and injury may increase the vulnerability of the L5-S1 junction even more.
L5-S1 is one of the two most common sites for back surgery. The other is the area just above, called L4-L5.
In the low back, the L5-S1 junction is often the site of a problem known as spondylolisthesis . Spondylolisthesis occurs when a vertebra slips forward relative to the bone immediately beneath it.
The most common variety of this condition is called degenerative spondylolisthesis. It generally occurs when the spine starts to wear down with age.
Isthmic spondylolisthesis is another common variant. Isthmic spondylolisthesis starts as a tiny fracture in the pars interarticularis . This is an area of bone in the back that connects the adjoining parts of the facet joint .
While these types of fractures tend to occur before the age of 15, symptoms often do not develop until adulthood. Degeneration of the spine in later adulthood can further worsen the condition.
The angle of the sacrum may contribute to spondylolisthesis. This is because the S1 tips down in the front and up in the back rather than being horizontal to the ground. Individuals with a greater tilt will usually have a higher risk of spondylolisthesis.
Spondylolisthesis is typically treated with non-surgical interventions. These could include:
- Pain medications
- Heat and/or ice application
- Physical therapy
- Epidural steroid injections
Spinal fusion surgery can be effective for treating symptoms related to spondylolisthesis. However, it requires a lot of recovery time and can have additional risks. Usually, non-surgical care is tried for at least six months. If you haven't gotten relief by then, surgery may be an option.
The L5-S1 is also called the lumbosacral joint. It is the part of the spine where the lumbar spine ends and the sacral spine begins. It helps you twist, bend, and stand upright.
Because of its location, the L5-S1 is vulnerable to wear and tear and injury. One of the more common problems with the L5-S1 is spondylolisthesis, which occurs when a vertebra slips forward. This condition is usually treated non-surgically.
Frequently Asked Questions
A disc herniation at L5-S1 is a common cause of sciatica. Symptoms of sciatica include burning, numbness, pain, or tingling that radiates from the buttock down the leg to the knee or foot. The pain is often sharp and may feel like an electric shock.
Disc problems at L5-S1 herniation can also cause lower back pain and stiffness. It can also trigger painful muscle spasms that cause your back to go out.
Yes. Disc problems at L5-S1 can cause bowel problems. Some research links irritable bowel syndrome to herniated disks in the lower back. Additional studies found disc problems at L5-S1 can lead to difficulty controlling your anal sphincter.
Pain from L5-S1 is typically treated with heat or ice, over-the-counter anti-inflammatory medications, prescription pain medicine or muscle relaxers, physical therapy, chiropractic adjustments, and epidural steroid injections. If these measures do not help, surgery may be required.
American Academy of Orthopaedic Surgeons. Spondylolysis and spondylolisthesis .
Gong S, Hou Q, Chu Y, Huang X, Yang W, Wang Z. Anatomical factors and pathological parts of isthmic fissure and degenerative lumbar spondylolisthesis . Chronic Dis Prev Rev . 2019;9:1-6
American Association of Neurological Surgeons. Herniate disc .
Bertilson BC, Heidermakr A, Stockhaus M. Irritable bowel syndrome–a neurological spine problem . JAMMR . 2015;4(24):4154–68. doi:10.9734/BJMMR/2014/9746
Akca N, Ozdemir B, Kanat A, Batcik OE, Yazar U, Zorba OU. Describing a new syndrome in L5-S1 disc herniation: Sexual and sphincter dysfunction without pain and muscle weakness . J Craniovertebr Junction Spine . 2014;5(4):146–50. doi:10.4103/0974-8237.147076
By Anne Asher, CPT Anne Asher, ACE-certified personal trainer, health coach, and orthopedic exercise specialist, is a back and neck pain expert.
Does intraoperative reduction result in better outcomes in low-grade lumbar spondylolisthesis after transforaminal lumbar interbody fusion? A systematic review and meta-analysis
Affiliations.
- 1 Department of Spinal Surgery, Gaoyou People's Hospital, Yangzhou, Jiangsu, China.
- 2 Department of Orthopedics, The Third Clinical Medical College of Yangzhou University, Yangzhou, Jiangsu, China.
- 3 Department of Medical Image, Gaoyou People's Hospital, Yangzhou, Jiangsu, China.
- 4 Department of Orthopedics, Gaoyou Hospital of Integrated Traditional Chinese and Western Medicine, Yangzhou, Jiangsu, China.
- PMID: 38681050
- PMCID: PMC11045973
- DOI: 10.3389/fmed.2024.1350064
Objective: This study aimed to compare the clinical efficacy and safety of reduction vs. arthrodesis in situ with transforaminal lumbar interbody fusion (TLIF) for low-grade lumbar spondylolisthesis.
Study design: Systematic review and meta-analysis.
Methods: A comprehensive literature search was implemented in PubMed, Embase, and Cochrane Library databases. Randomized or non-randomized controlled trials that were published until July 2023 that compared reduction vs. arthrodesis in situ techniques with minimally invasive or open-TLIF for low-grade spondylolisthesis were selected. The quality of the included studies was evaluated by the Newcastle-Ottawa Scale (NOS). Data were extracted according to the predefined outcome measures, including operation time and intraoperative blood loss; short- and long-time follow-up of visual analog scale (VAS) back pain (VAS-BP) and Oswestry Disability Index (ODI); slippage and segmental lordosis; and the complication and fusion rate.
Results: Five studies ( n = 495 patients) were finally included. All of them were retrospective cohort studies with Evidence Level II. The pooled data revealed that both techniques had similar patient-reported outcomes (VAS, ODI, and good and excellent rate) during short- and long-term follow-up. In addition, no significant differences were observed in the fusion and complication rates. However, although the reduction group did achieve better slippage correction, it was associated with increased operation time and intraoperative blood loss compared with the in situ arthrodesis group.
Conclusions: Based on the available evidence, intraoperative reduction does not result in better clinical outcomes in low-grade spondylolisthesis after minimally invasive or open-TLIF, and the in situ arthrodesis technique could be an alternative.
Keywords: arthrodesis in situ; meta-analysis; reduction; spondylolisthesis; transforaminal lumbar interbody fusion.
Copyright © 2024 Qin, Zhu, Zhou and Guan.
Publication types
- Systematic Review
Grants and funding

IMAGES
VIDEO
COMMENTS
Spondylolisthesis is a spinal condition that causes lower back pain. It occurs when one of your vertebrae, the bones of your spine, slips out of place onto the vertebra below it. Most of the time, nonsurgical treatment can relieve your symptoms. If you have severe spondylolisthesis, surgery is successful in most cases.
Spondylolisthesis is a slipping of vertebra that occurs, in most cases, at the base of the spine. ... (lumbar spondylolisthesis). ... The symptoms may come on slowly and vary in how serious they are.
In spondylolisthesis, one of the bones in your spine — called a vertebra — slips forward and out of place. This may occur anywhere along the spine, but is most common in the lower back (lumbar spine). In some people, this causes no symptoms at all. Others may have back and leg pain that ranges from mild to severe.
Lumbosacral spondylolisthesis is the forward translation of the fifth lumbar vertebra (L5) over the first sacral vertebra (S1). Bilateral L5 pars defect (spondylolysis) or repetitive stress injury is the primary etiology behind lumbosacral spondylolisthesis. The degree of a slip often correlates with the degree of symptoms.
Symptoms of spondylolisthesis can include localized lower back pain and/or - if there is associated nerve compression - pain ... Samuel AM, Moore HG, Cunningham ME. Treatment for Degenerative Lumbar Spondylolisthesis: Current Concepts and New Evidence. Curr Rev Musculoskelet Med. 2017 Dec;10(4):521-529. doi: 10.1007/s12178-017-9442-3. ...
Spondylolisthesis. Spondylolisthesis is partial displacement of a bone in the lower back. Injuries or a degenerative condition can cause this disorder. Pain is felt in the low back and may travel down one or both legs. The diagnosis is based on the results of imaging tests. Treatment includes measures to relieve pain.
Spondylolysis and spondylolisthesis occur in the lumbar spine. The five vertebrae in the lower back comprise the lumbar spine. Other parts of your spine include: Spinal cord and nerves. These "electrical cables" travel through the spinal canal carrying messages between your brain and muscles. Nerve roots branch out from the spinal cord through ...
Spondylolisthesis has multiple causes. It can occur anywhere in the spine and is most common in the lumbar and cervical regions. Lumbar spondylolisthesis may be asymptomatic or cause pain when walking or standing for a long time. Treatment is symptomatic and includes physical therapy with lumbar stabilization.
Symptoms . Many people with spondylolisthesis have no obvious symptoms. Sometimes the condition is not discovered until an X-ray is taken for an unrelated injury or condition. ... Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52 ...
Symptoms of Spondylolisthesis. Spondylolisthesis can cause compression of spinal nerves and in severe cases, the spinal cord. The symptoms will depend on which vertebra is affected. Cervical Spondylolisthesis (neck) Neck pain. Arm pain. Arm numbness or tingling. Arm weakness.
Both spondylolysis and spondylolisthesis are often asymptomatic, and the degree of spondylolisthesis does not necessarily correlate with the incidence or severity of symptoms, even when a patient is experiencing back pain. However, these 2 entities have been reported to be the most common underlying causes of persistent low back pain among ...
Bone disease and fractures also can cause lumbar spondylolisthesis. Genetics may play a role, as some people are born with thinner-than-normal vertebral bone. Early Signs of Lumbar Spondylolisthesis and Diagnosis. Symptoms of spondylolisthesis may vary from none to mild to severe. The most common symptom is low back pain.
Lumbar spondylolisthesis in the lumbar (lower) spine is the most common form, so pain symptoms usually start in that area of the back. ... Some people do not experience spondylolisthesis symptoms, while other people feel near-constant pain. Symptoms depend on the grade of slippage. Visible symptoms can include swayback, which is when the lower ...
Spondylolisthesis is a displacement of a vertebra in which the bone slides out of its proper position onto the bone below it. Most often, this displacement occurs following a break or fracture. ... Symptoms may vary from mild to severe. In some cases, there may be no symptoms at all. ... (lumbar vertebra) and the first bone in the sacrum ...
The lumbosacral joint may develop wear-and-tear arthritis (osteoarthritis) over time due to its high load-bearing function. ... Most commonly, spondylolisthesis of L5 is caused by repetitive stress to the pars interarticularis and is most has commonly seen in children and adolescents. ... Common Symptoms and Signs Stemming from L5-S1. Save
Spondylolisthesis. Spondylolisthesis occurs when one vertebra in the spinal column becomes fractured and the spine slips out of place, usually in the lumbar area. Back pain, numbness in the extremities, or sensory loss can be caused by nerve root compression as a result of the slippage. Related conditions include spondylosis which is arthritis ...
These symptoms may indicate severe progression of spondylolisthesis leading to a serious condition known as cauda equina syndrome, which requires urgent surgical intervention. 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific ...
lumbar decompression - a procedure to relieve pressure on the compressed spinal nerves; ... Recovery from surgery can take several weeks, but if often improves many of the symptoms of spondylolisthesis. Talk to your surgeon about the risks and benefits of spinal surgery. Causes of spondylolisthesis. Spondylolisthesis can:
Degenerative spondylolisthesis symptoms include neurogenic claudication, sciatica, and radiculopathy. In degenerative spondylolisthesis, the degenerated facet joints and other parts of the vertebral bone tend to increase in size. The enlarged, abnormal bone then encroaches upon the central canal and/or nerve hole (foramen) causing spinal ...
Lumbar Spondylolisthesis Symptoms. Depending on the degree of the slip, symptoms of lumbar spondylolisthesis can vary from mild to severe or not be present at all. Symptoms may include: Lower back pain; Muscle tightness; Pain, numbness, or tingling in your thighs and buttocks; Stiffness; Tenderness in the area where the vertebra is out of place
Spondylolisthesis. FAQ. The lumbosacral joint, also called L5-S1, is a term used to describe a part of the spine. L5-S1 is the exact spot where the lumbar spine ends and the sacral spine begins. The lumbosacral joint is the joint that connects these bones. L5-S1 is composed of the last bone in the low back, called L5, and the triangle-shaped ...
with lumbar spinal stenosis symptoms because it allows for cross-sectional measurement of the spinal canal2,5,20,21 ... patients without spondylolisthesis or lumbar scoliosis,
PubMed