How to Write a Case Conceptualization: 10 Examples (+ PDF)

Such understanding can be developed by reading relevant records, meeting with clients face to face, and using assessments such as a mental status examination.
As you proceed, you are forming a guiding concept of who this client is, how they became who they are, and where their personal journey might be heading.
Such a guiding concept, which will shape any needed interventions, is called a case conceptualization, and we will examine various examples in this article.
Before you continue, we thought you might like to download our three Positive CBT Exercises for free . These science-based exercises will provide you with detailed insight into positive Cognitive-Behavioral Therapy (CBT) and give you the tools to apply it in your therapy or coaching.

This Article Contains:
What is a case conceptualization or formulation, 4 things to include in your case formulation, a helpful example & model, 3 samples of case formulations, 6 templates and worksheets for counselors, relevant resources from positivepsychology.com, a take-home message.
In psychology and related fields, a case conceptualization summarizes the key facts and findings from an evaluation to provide guidance for recommendations.
This is typically the evaluation of an individual, although you can extend the concept of case conceptualization to summarizing findings about a group or organization.
Based on the case conceptualization, recommendations can be made to improve a client’s self-care , mental status, job performance, etc (Sperry & Sperry, 2020).

- Summary of the client’s identifying information, referral questions, and timeline of important events or factors in their life . A timeline can be especially helpful in understanding how the client’s strengths and limitations have evolved.
- Statement of the client’s core strengths . Identifying core strengths in the client’s life should help guide any recommendations, including how strengths might be used to offset limitations.
- Statement concerning a client’s limitations or weaknesses . This will also help guide any recommendations. If a weakness is worth mentioning in a case conceptualization, it is worth writing a recommendation about it.
Note: As with mental status examinations , observations in this context concerning weaknesses are not value judgments, about whether the client is a good person, etc. The observations are clinical judgments meant to guide recommendations.
- A summary of how the strengths, limitations, and other key information about a client inform diagnosis and prognosis .
You should briefly clarify how you arrived at a given diagnosis. For example, why do you believe a personality disorder is primary, rather than a major depressive disorder?
Many clinicians provide diagnoses in formal psychiatric terms, per the International Classification of Diseases (ICD-10) or Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Some clinicians will state a diagnosis in less formal terms that do not coincide exactly with ICD-10 or DSM-5 codes. What is arguably more important is that a diagnostic impression, formal or not, gives a clear sense of who the person is and the support they need to reach their goals.
Prognosis is a forecast about whether the client’s condition can be expected to improve, worsen, or remain stable. Prognosis can be difficult, as it often depends on unforeseeable factors. However, this should not keep you from offering a conservative opinion on a client’s expected course, provided treatment recommendations are followed.
Download 3 Free Positive CBT Exercises (PDF)
These detailed, science-based exercises will equip you or your clients with tools to find new pathways to reduce suffering and more effectively cope with life stressors.
Download 3 Free Positive CBT Tools Pack (PDF)
By filling out your name and email address below.
Based on the pointers for writing a case conceptualization above, an example for summarizing an adolescent case (in this instance, a counseling case for relieving depression and improving social skills) might read as follows.
Background and referral information
This is a 15-year-old Haitian–American youth, referred by his mother for concerns about self-isolation, depression, and poor social skills. He reportedly moved with his mother to the United States three years ago.
He reportedly misses his life and friends in Haiti. The mother states he has had difficulty adjusting socially in the United States, especially with peers. He has become increasingly self-isolating, appears sad and irritable, and has started to refuse to go to school.
His mother is very supportive and aware of his emotional–behavioral needs. The youth has been enrolled in a social skills group at school and has attended three sessions, with some reported benefit. He is agreeable to start individual counseling. He reportedly does well in school academically when he applies himself.
Limitations
Behavioral form completed by his mother shows elevated depression scale (T score = 80). There is a milder elevation on the inattention scale (T score = 60), which suggests depression is more acute than inattention and might drive it.
He is also elevated on a scale measuring social skills and involvement (T score = 65). Here too, it is reasonable to assume that depression is driving social isolation and difficulty relating to peers, especially since while living in Haiti, he was reportedly quite social with peers.
Diagnostic impressions, treatment guidance, prognosis
This youth’s history, presentation on interview, and results of emotional–behavioral forms suggest some difficulty with depression, likely contributing to social isolation. As he has no prior reported history of depression, this is most likely a reaction to missing his former home and difficulty adjusting to his new school and peers.
Treatments should include individual counseling with an evidence-based approach such as Cognitive-Behavioral Therapy (CBT). His counselor should consider emotional processing and social skills building as well.
Prognosis is favorable, with anticipated benefit apparent within 12 sessions of CBT.
How to write a case conceptualization: An outline
The following outline is necessarily general. It can be modified as needed, with points excluded or added, depending on the case.
- Client’s gender, age, level of education, vocational status, marital status
- Referred by whom, why, and for what type of service (e.g., testing, counseling, coaching)
- In the spirit of strengths-based assessment, consider listing the client’s strengths first, before any limitations.
- Consider the full range of positive factors supporting the client.
- Physical health
- Family support
- Financial resources
- Capacity to work
- Resilience or other positive personality traits
- Emotional stability
- Cognitive strengths, per history and testing
- The client’s limitations or relative weaknesses should be described in a way that highlights those most needing attention or treatment.
- Medical conditions affecting daily functioning
- Lack of family or other social support
- Limited financial resources
- Inability to find or hold suitable employment
- Substance abuse or dependence
- Proneness to interpersonal conflict
- Emotional–behavioral problems, including anxious or depressive symptoms
- Cognitive deficits, per history and testing
- Diagnoses that are warranted can be given in either DSM-5 or ICD-10 terms.
- There can be more than one diagnosis given. If that’s the case, consider describing these in terms of primary diagnosis, secondary diagnosis, etc.
- The primary diagnosis should best encompass the client’s key symptoms or traits, best explain their behavior, or most need treatment.
- Take care to avoid over-assigning multiple and potentially overlapping diagnoses.
When writing a case conceptualization, always keep in mind the timeline of significant events or factors in the examinee’s life.
- Decide which events or factors are significant enough to include in a case conceptualization.
- When these points are placed in a timeline, they help you understand how the person has evolved to become who they are now.
- A good timeline can also help you understand which factors in a person’s life might be causative for others. For example, if a person has suffered a frontal head injury in the past year, this might help explain their changeable moods, presence of depressive disorder, etc.

Sample #1: Conceptualization for CBT case
This is a 35-year-old Caucasian man referred by his physician for treatment of generalized anxiety.
Strengths/supports in his case include willingness to engage in treatment, high average intelligence per recent cognitive testing, supportive family, and regular physical exercise (running).
Limiting factors include relatively low stress coping skills, frequent migraines (likely stress related), and relative social isolation (partly due to some anxiety about social skills).
The client’s presentation on interview and review of medical/psychiatric records show a history of chronic worry, including frequent worries about his wife’s health and his finances. He meets criteria for DSM-5 generalized anxiety disorder. He has also described occasional panic-type episodes, which do not currently meet full criteria for panic disorder but could develop into such without preventive therapy.
Treatments should include CBT for generalized anxiety, including keeping a worry journal; regular assessment of anxiety levels with Penn State Worry Questionnaire and/or Beck Anxiety Inventory; cognitive restructuring around negative beliefs that reinforce anxiety; and practice of relaxation techniques, such as progressive muscle relaxation and diaphragmatic breathing .
Prognosis is good, given the evidence for efficacy of CBT for anxiety disorders generally (Hofmann, Asnaani, Vonk, Sawyer, & Fang, 2012).
Sample #2: Conceptualization for DBT case
This 51-year-old Haitian–American woman is self-referred for depressive symptoms, including reported moods of “rage,” “sadness,” and “emptiness.” She says that many of her difficulties involve family, friends, and coworkers who regularly “disrespect” her and “plot against her behind her back.”
Her current psychiatrist has diagnosed her with personality disorder with borderline features, but she doubts the accuracy of this diagnosis.
Strengths/supports include a willingness to engage in treatment, highly developed and marketable computer programming skills, and engagement in leisure activities such as playing backgammon with friends.
Limiting factors include low stress coping skills, mild difficulties with attention and recent memory (likely due in part to depressive affect), and a tendency to self-medicate with alcohol when feeling depressed.
The client’s presentation on interview, review of medical/psychiatric records, and results of MMPI-2 personality inventory corroborate her psychiatrist’s diagnosis of borderline personality disorder.
The diagnosis is supported by a longstanding history of unstable identity, volatile personal relationships with fear of being abandoned, feelings of emptiness, reactive depressive disorder with suicidal gestures, and lack of insight into interpersonal difficulties that have resulted in her often stressed and depressive state.
Treatments should emphasize a DBT group that her psychiatrist has encouraged her to attend but to which she has not yet gone. There should also be regular individual counseling emphasizing DBT skills including mindfulness or present moment focus, building interpersonal skills, emotional regulation, and distress tolerance. There should be a counseling element for limiting alcohol use. Cognitive exercises are also recommended.
Of note, DBT is the only evidence-based treatment for borderline personality disorder (May, Richardi, & Barth, 2016). Prognosis is guardedly optimistic, provided she engages in both group and individual DBT treatments on a weekly basis, and these treatments continue without interruption for at least three months, with refresher sessions as needed.
Sample #3: Conceptualization in a family therapy case
This 45-year-old African-American woman was initially referred for individual therapy for “rapid mood swings” and a tendency to become embroiled in family conflicts. Several sessions of family therapy also appear indicated, and her psychiatrist concurs.
The client’s husband (50 years old) and son (25 years old, living with parents) were interviewed separately and together. When interviewed separately, her husband and son each indicated the client’s alcohol intake was “out of control,” and that she was consuming about six alcoholic beverages throughout the day, sometimes more.
Her husband and son each said the client was often too tired for household duties by the evening and often had rapid shifts in mood from happy to angry to “crying in her room.”
On individual interview, the client stated that her husband and son were each drinking about as much as she, that neither ever offered to help her with household duties, and that her son appeared unable to keep a job, which left him home most of the day, making demands on her for meals, etc.
On interview with the three family members, each acknowledged that the instances above were occurring at home, although father and son tended to blame most of the problems, including son’s difficulty maintaining employment, on the client and her drinking.
Strengths/supports in the family include a willingness of each member to engage in family sessions, awareness of supportive resources such as assistance for son’s job search, and a willingness by all to examine and reduce alcohol use by all family members as needed.
Limiting factors in this case include apparent tendency of all household members to drink to some excess, lack of insight by one or more family members as to how alcohol consumption is contributing to communication and other problems in the household, and a tendency by husband and son to make this client the family scapegoat.
The family dynamic can be conceptualized in this case through a DBT lens.
From this perspective, problems develop within the family when the environment is experienced by one or more members as invalidating and unsupportive. DBT skills with a nonjudgmental focus, active listening to others, reflecting each other’s feelings, and tolerance of distress in the moment should help to develop an environment that supports all family members and facilitates effective communication.
It appears that all family members in this case would benefit from engaging in the above DBT skills, to support and communicate with one another.
Prognosis is guardedly optimistic if family will engage in therapy with DBT elements for at least six sessions (with refresher sessions as needed).
Introduction to case conceptualization – Thomas Field
The following worksheets can be used for case conceptualization and planning.
- Case Conceptualization Worksheet: Individual Counseling helps counselors develop a case conceptualization for individual clients.
- Case Conceptualization Worksheet: Couples Counseling helps counselors develop a case conceptualization for couples.
- Case Conceptualization Worksheet: Family Counseling helps counselors develop a case conceptualization for families.
- Case Conceptualization and Action Plan: Individual Counseling helps clients facilitate conceptualization of their own case, at approximately six weeks into counseling and thereafter at appropriate intervals.
- Case Conceptualization and Action Plan: Couples Counseling helps couples facilitate conceptualization of their own case, at approximately six weeks into counseling and thereafter at appropriate intervals.
- Case Conceptualization and Action Plan: Family Counseling helps families facilitate conceptualization of their own case, at approximately six weeks into counseling and thereafter at appropriate intervals.
17 Science-Based Ways To Apply Positive CBT
These 17 Positive CBT & Cognitive Therapy Exercises [PDF] include our top-rated, ready-made templates for helping others develop more helpful thoughts and behaviors in response to challenges, while broadening the scope of traditional CBT.
Created by Experts. 100% Science-based.
The following resources can be found in the Positive Psychology Toolkit© , and their full versions can be accessed by a subscription.
Analyzing Strengths Use in Different Life Domains can help clients understand their notable strengths and which strengths can be used to more advantage in new contexts.
Family Strength Spotting is another relevant resource. Each family member fills out a worksheet detailing notable strengths of other family members. In reviewing all worksheets, each family member can gain a greater appreciation for other members’ strengths, note common or unique strengths, and determine how best to use these combined strengths to achieve family goals.
Four Front Assessment is another resource designed to help counselors conceptualize a case based on a client’s personal and environmental strengths and weaknesses. The idea behind this tool is that environmental factors in the broad sense, such as a supportive/unsupportive family, are too often overlooked in conceptualizing a case.
If you’re looking for more science-based ways to help others through CBT, check out this collection of 17 validated positive CBT tools for practitioners. Use them to help others overcome unhelpful thoughts and feelings and develop more positive behaviors.
In helping professions, success in working with clients depends first and foremost on how well you understand them.
This understanding is crystallized in a case conceptualization.
Case conceptualization helps answer key questions. Who is this client? How did they become who they are? What supports do they need to reach their goals?
The conceptualization itself depends on gathering all pertinent data on a given case, through record review, interview, behavioral observation, questionnaires completed by the client, etc.
Once the data is assembled, the counselor, coach, or other involved professional can focus on enumerating the client’s strengths, weaknesses, and limitations.
It is also often helpful to put the client’s strengths and limitations in a timeline so you can see how they have evolved and which factors might have contributed to the emergence of others.
Based on this in-depth understanding of the client, you can then tailor specific recommendations for enhancing their strengths, overcoming their weaknesses, and reaching their particular goals.
We hope you have enjoyed this discussion of how to conceptualize cases in the helping professions and that you will find some tools for doing so useful.
We hope you enjoyed reading this article. For more information, don’t forget to download our three Positive CBT Exercises for free .
- Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research , 36 (5), 427–440.
- May, J. M., Richardi, T. M., & Barth, K. S. (2016). Dialectical behavior therapy as treatment for borderline personality disorder. The Mental Health Clinician , 6 (2), 62–67.
- Sperry, L., & Sperry, J. (2020). Case conceptualization: Mastering this competency with ease and confidence . Routledge.
Share this article:
Article feedback
What our readers think.
I found this very helpful and MORE understanding. I think I will often visit this page.
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

Youth Counseling: 17 Courses & Activities for Helping Teens
From a maturing body and brain to developing life skills and values, the teen years can be challenging, and mental health concerns may arise. Teens [...]

How To Plan Your Counseling Session: 6 Examples
Planning is crucial in a counseling session to ensure that time inside–and outside–therapy sessions is well spent, with the client achieving a successful outcome within [...]

Applied Positive Psychology in Therapy: Your Ultimate Guide
Without a doubt, this is an exciting time for positive psychology in therapy. Many academics and therapists now recognize the value of this fascinating, evolving [...]
Read other articles by their category
- Body & Brain (49)
- Coaching & Application (57)
- Compassion (26)
- Counseling (51)
- Emotional Intelligence (24)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (45)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (28)
- Positive Communication (20)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (18)
- Positive Parenting (4)
- Positive Psychology (33)
- Positive Workplace (37)
- Productivity (17)
- Relationships (46)
- Resilience & Coping (36)
- Self Awareness (21)
- Self Esteem (38)
- Strengths & Virtues (32)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Is a Case Study?
Weighing the pros and cons of this method of research
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
Verywell / Colleen Tighe
- Pros and Cons
What Types of Case Studies Are Out There?
Where do you find data for a case study, how do i write a psychology case study.
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
The point of a case study is to learn as much as possible about an individual or group so that the information can be generalized to many others. Unfortunately, case studies tend to be highly subjective, and it is sometimes difficult to generalize results to a larger population.
While case studies focus on a single individual or group, they follow a format similar to other types of psychology writing. If you are writing a case study, we got you—here are some rules of APA format to reference.
At a Glance
A case study, or an in-depth study of a person, group, or event, can be a useful research tool when used wisely. In many cases, case studies are best used in situations where it would be difficult or impossible for you to conduct an experiment. They are helpful for looking at unique situations and allow researchers to gather a lot of˜ information about a specific individual or group of people. However, it's important to be cautious of any bias we draw from them as they are highly subjective.
What Are the Benefits and Limitations of Case Studies?
A case study can have its strengths and weaknesses. Researchers must consider these pros and cons before deciding if this type of study is appropriate for their needs.
One of the greatest advantages of a case study is that it allows researchers to investigate things that are often difficult or impossible to replicate in a lab. Some other benefits of a case study:
- Allows researchers to capture information on the 'how,' 'what,' and 'why,' of something that's implemented
- Gives researchers the chance to collect information on why one strategy might be chosen over another
- Permits researchers to develop hypotheses that can be explored in experimental research
On the other hand, a case study can have some drawbacks:
- It cannot necessarily be generalized to the larger population
- Cannot demonstrate cause and effect
- It may not be scientifically rigorous
- It can lead to bias
Researchers may choose to perform a case study if they want to explore a unique or recently discovered phenomenon. Through their insights, researchers develop additional ideas and study questions that might be explored in future studies.
It's important to remember that the insights from case studies cannot be used to determine cause-and-effect relationships between variables. However, case studies may be used to develop hypotheses that can then be addressed in experimental research.
Case Study Examples
There have been a number of notable case studies in the history of psychology. Much of Freud's work and theories were developed through individual case studies. Some great examples of case studies in psychology include:
- Anna O : Anna O. was a pseudonym of a woman named Bertha Pappenheim, a patient of a physician named Josef Breuer. While she was never a patient of Freud's, Freud and Breuer discussed her case extensively. The woman was experiencing symptoms of a condition that was then known as hysteria and found that talking about her problems helped relieve her symptoms. Her case played an important part in the development of talk therapy as an approach to mental health treatment.
- Phineas Gage : Phineas Gage was a railroad employee who experienced a terrible accident in which an explosion sent a metal rod through his skull, damaging important portions of his brain. Gage recovered from his accident but was left with serious changes in both personality and behavior.
- Genie : Genie was a young girl subjected to horrific abuse and isolation. The case study of Genie allowed researchers to study whether language learning was possible, even after missing critical periods for language development. Her case also served as an example of how scientific research may interfere with treatment and lead to further abuse of vulnerable individuals.
Such cases demonstrate how case research can be used to study things that researchers could not replicate in experimental settings. In Genie's case, her horrific abuse denied her the opportunity to learn a language at critical points in her development.
This is clearly not something researchers could ethically replicate, but conducting a case study on Genie allowed researchers to study phenomena that are otherwise impossible to reproduce.
There are a few different types of case studies that psychologists and other researchers might use:
- Collective case studies : These involve studying a group of individuals. Researchers might study a group of people in a certain setting or look at an entire community. For example, psychologists might explore how access to resources in a community has affected the collective mental well-being of those who live there.
- Descriptive case studies : These involve starting with a descriptive theory. The subjects are then observed, and the information gathered is compared to the pre-existing theory.
- Explanatory case studies : These are often used to do causal investigations. In other words, researchers are interested in looking at factors that may have caused certain things to occur.
- Exploratory case studies : These are sometimes used as a prelude to further, more in-depth research. This allows researchers to gather more information before developing their research questions and hypotheses .
- Instrumental case studies : These occur when the individual or group allows researchers to understand more than what is initially obvious to observers.
- Intrinsic case studies : This type of case study is when the researcher has a personal interest in the case. Jean Piaget's observations of his own children are good examples of how an intrinsic case study can contribute to the development of a psychological theory.
The three main case study types often used are intrinsic, instrumental, and collective. Intrinsic case studies are useful for learning about unique cases. Instrumental case studies help look at an individual to learn more about a broader issue. A collective case study can be useful for looking at several cases simultaneously.
The type of case study that psychology researchers use depends on the unique characteristics of the situation and the case itself.
There are a number of different sources and methods that researchers can use to gather information about an individual or group. Six major sources that have been identified by researchers are:
- Archival records : Census records, survey records, and name lists are examples of archival records.
- Direct observation : This strategy involves observing the subject, often in a natural setting . While an individual observer is sometimes used, it is more common to utilize a group of observers.
- Documents : Letters, newspaper articles, administrative records, etc., are the types of documents often used as sources.
- Interviews : Interviews are one of the most important methods for gathering information in case studies. An interview can involve structured survey questions or more open-ended questions.
- Participant observation : When the researcher serves as a participant in events and observes the actions and outcomes, it is called participant observation.
- Physical artifacts : Tools, objects, instruments, and other artifacts are often observed during a direct observation of the subject.
If you have been directed to write a case study for a psychology course, be sure to check with your instructor for any specific guidelines you need to follow. If you are writing your case study for a professional publication, check with the publisher for their specific guidelines for submitting a case study.
Here is a general outline of what should be included in a case study.
Section 1: A Case History
This section will have the following structure and content:
Background information : The first section of your paper will present your client's background. Include factors such as age, gender, work, health status, family mental health history, family and social relationships, drug and alcohol history, life difficulties, goals, and coping skills and weaknesses.
Description of the presenting problem : In the next section of your case study, you will describe the problem or symptoms that the client presented with.
Describe any physical, emotional, or sensory symptoms reported by the client. Thoughts, feelings, and perceptions related to the symptoms should also be noted. Any screening or diagnostic assessments that are used should also be described in detail and all scores reported.
Your diagnosis : Provide your diagnosis and give the appropriate Diagnostic and Statistical Manual code. Explain how you reached your diagnosis, how the client's symptoms fit the diagnostic criteria for the disorder(s), or any possible difficulties in reaching a diagnosis.
Section 2: Treatment Plan
This portion of the paper will address the chosen treatment for the condition. This might also include the theoretical basis for the chosen treatment or any other evidence that might exist to support why this approach was chosen.
- Cognitive behavioral approach : Explain how a cognitive behavioral therapist would approach treatment. Offer background information on cognitive behavioral therapy and describe the treatment sessions, client response, and outcome of this type of treatment. Make note of any difficulties or successes encountered by your client during treatment.
- Humanistic approach : Describe a humanistic approach that could be used to treat your client, such as client-centered therapy . Provide information on the type of treatment you chose, the client's reaction to the treatment, and the end result of this approach. Explain why the treatment was successful or unsuccessful.
- Psychoanalytic approach : Describe how a psychoanalytic therapist would view the client's problem. Provide some background on the psychoanalytic approach and cite relevant references. Explain how psychoanalytic therapy would be used to treat the client, how the client would respond to therapy, and the effectiveness of this treatment approach.
- Pharmacological approach : If treatment primarily involves the use of medications, explain which medications were used and why. Provide background on the effectiveness of these medications and how monotherapy may compare with an approach that combines medications with therapy or other treatments.
This section of a case study should also include information about the treatment goals, process, and outcomes.
When you are writing a case study, you should also include a section where you discuss the case study itself, including the strengths and limitiations of the study. You should note how the findings of your case study might support previous research.
In your discussion section, you should also describe some of the implications of your case study. What ideas or findings might require further exploration? How might researchers go about exploring some of these questions in additional studies?
Need More Tips?
Here are a few additional pointers to keep in mind when formatting your case study:
- Never refer to the subject of your case study as "the client." Instead, use their name or a pseudonym.
- Read examples of case studies to gain an idea about the style and format.
- Remember to use APA format when citing references .
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011;11:100.
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011 Jun 27;11:100. doi:10.1186/1471-2288-11-100
Gagnon, Yves-Chantal. The Case Study as Research Method: A Practical Handbook . Canada, Chicago Review Press Incorporated DBA Independent Pub Group, 2010.
Yin, Robert K. Case Study Research and Applications: Design and Methods . United States, SAGE Publications, 2017.
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
Home > Blog > What is Case Conceptualization & How to Write it (With Examples)
Hate writing progress notes? Get them written automatically.
What is Case Conceptualization & How to Write it (With Examples)
Courtney Gardner, MSW
Hate writing progress notes? Join thousands of happy therapists using Mentalyc AI.
The Ultimate Guide to Case Conceptualization: Our Top Tips, Outlines, and Real-life Examples
As a mental health counselor, case conceptualization is one of the most essential skills you can develop to understand your clients and find the most effective treatment. But for new counselors, the process can be overwhelming. How do you synthesize all the information from your intake and assessment into a cohesive case conceptualization? Which theoretical orientation fits best? What should you include in your conceptualization? Let's dive in and discover the secrets to developing killer case conceptualization skills!
What Is Case Conceptualization?
Case conceptualization is the process of understanding and interpreting a client's presenting problems within the context of their individual history, personality, and current circumstances. It involves gathering and organizing information about the client, identifying patterns and themes, and formulating a comprehensive understanding of the factors contributing to their difficulties. This understanding serves as the foundation for developing a treatment plan and guiding the therapeutic process.
Why Is Case Conceptualization Important to Mental Health Professionals?
Constructing a case conceptualization is crucial for mental health professionals as it helps them better understand their clients' perspectives and needs. Professionals can develop effective therapy outcomes by analyzing clients' experiences, thoughts, behaviors, environment, and biology. This enables them to identify suitable treatment options and establish tailored treatment goals and interventions. A comprehensive approach is vital for providing evidence-based, client-centered therapy, which can lead to profound results, including improved insight, self-esteem, and motivation to make positive changes in their lives.
Let Mentalyc AI Write Your Progress Notes Fast
✅ HIPAA Compliant
✅ Insurance Compliant
✅ SOAP, DAP, EMDR, Intake notes and more
✅ Individual, Couple, Child, Family therapy types
✅ Template Builder
✅ Recording, Dictation, Text & Upload Inputs
How to Write a Case Conceptualization
To provide personalized treatment plans to your clients, it is essential to have a well-developed case conceptualization that helps you understand their mental health needs. You should include the following components early in creating your case conceptualization.
Client Information
Gather essential client information, including age, gender, relationship status, occupation, presenting problem, and relevant family and medical history.
Theoretical Orientation
Determine which theoretical approach fits their needs. This approach will guide the therapist to understand the client's symptoms and experiences through a particular lens. For example, a psychodynamic approach may focus on uncovering unconscious drives or past traumas, while a cognitive-behavioral approach looks at maladaptive thought patterns and behaviors.
If applicable, use the Diagnostic and Statistical Manual of Mental Disorders-V (DSM-5) to identify appropriate diagnoses and diagnostic codes based on your client's symptoms. Explain your conclusions.
The Eight P’s of Case Conceptualization Framework
If you aim to create a comprehensive case conceptualization, you can employ the 8 Ps framework. The Eight Ps framework helps you organize and structure your thoughts and ideas concisely and quickly. Utilizing this framework allows you to analyze and evaluate a case from multiple perspectives and develop a fully formed and well-rounded understanding of the issues at hand.
Take your time back! Get your progress notes done automatically.
Presentation.
What symptoms or life difficulties brought the client in? How do they view these problems?
- Describe the client's symptoms, concerns, and goals. Identify the main issues to address, such as depression, anxiety, trauma, or relationship difficulties. Consider the duration and severity of problems.
Predisposing Factors
What makes the client vulnerable to these problems? Genetics? Trauma?
- Consider the historical or biological factors involved in the current issue. This may include discussing the individual's developmental experiences, family history, or medical conditions. It is also essential to examine the client's natural tendencies, traits, and vulnerabilities that may make specific problems more likely.
Precipitating Factors
What recent events triggered the current problems? Loss of a job? End of a relationship?
- Investigate recent events that may have caused or intensified the client's presenting problem. Identify any losses, changes, or stressors in the client's life. These could include health issues, the end of a relationship, or the loss of a loved one. It is also crucial to examine how the client responded to these events.

Increase your practice's revenue and reduce therapist burnout
Do they live an active or sedentary lifestyle? Is their personality naturally more dependent or independent?
- Identifying predictable patterns in a person's thinking, feeling, acting, and coping reflects their baseline tendencies in stressful and non-stressful situations.
Perpetuating Factors
What factors in their lives maintain their problems? Avoidance? Unhelpful thoughts?
- Pinpoint and explore the habits, beliefs, or dynamics that maintain the problem. This means looking into their unhealthy coping strategies, cognitive distortions, relationship patterns, lack of social support, unstable living situations, and any other factors that may be contributing to the issue.
Protective Factors and Strengths
What strengths does the client have? A robust support system? Coping skills?
- Note their strengths, resources, and supports that can aid in their healing process. This may include skills, talents, social connections, access to healthcare, spirituality, and other positive factors supporting their treatment and recovery.
How will you address the problems and build on your client's strengths? Treatment modalities? Strategies?
- Establish goals and strategies considering the factors that may have caused or contributed to their condition. Identifying any protective factors the client may already have and developing interventions that build on them is also essential.
- Discuss specific interventions, referrals, and approaches. The plan should be comprehensive, regularly reviewed, and modified to ensure that it effectively reduces the client's distress, helps them change unhealthy patterns, builds new skills, and improves overall functioning. You should also consider your clinical decision-making during the initial planning stages.

Have your progress notes automatically written for you!
What's the likelihood of improvement with treatment?
- Forecast the outcome of treatment for a client based on a combination of risk factors, protective factors, the client's strengths, and their readiness for change. It would help if you discussed your initial impressions regarding the severity of the problem, the client's motivation for change, their responsiveness to intervention, and other relevant factors. You should also estimate the number of sessions required for treatment.
Tips for Mastering Effective Case Conceptualizations
Creating an effective case conceptualization requires a comprehensive, adaptable, and multidimensional approach. It involves analyzing the client's situation, embracing various perspectives, focusing on their strengths, and evolving throughout therapy. Stay curious, keep an open mind, and be willing to learn. Your clients can benefit significantly from these qualities.
Remember the following essential tips to hone your skills and make a lasting impact on your clients:
Focus on the client's strengths.
When assessing problems and symptoms, it is essential to identify your client's strengths, resources, and abilities and build on what's working to motivate change.
Look for themes and patterns.
As you gather information from your client, look for connections between their thoughts, feelings, behaviors, experiences, and relationships. Themes will emerge that shape your conceptualization.
Consider multiple perspectives.
Various theoretical orientations can be applied to comprehend a client's situation better. Exploring different perspectives can offer alternative insights into a case.
Be flexible.
It is essential to regularly revisit and update your case conceptualization as new information arises and as your client progresses.
Paint the whole picture.
An effective case conceptualization should consider cultural context, family and social relationships, medical history, life experiences, environment, and more, not merely focus on the client's symptoms or problems.
Discuss your conceptualization with colleagues.
Bouncing ideas off other therapists or discussing cases during supervision can provide valuable feedback and input, strengthening your case conceptualization from different perspectives.
Continuously evaluate your conceptualization.
During therapy, regularly review how well your understanding of the situation accounts for any new issues or lack of progress and adjust your approach accordingly. A successful interpretation should always remain an evolving theory.
Review research and theory.
It's necessary to base your case conceptualization on established theory and research to give credibility to your formulations and interventions. Keep yourself updated with the latest developments in psychotherapy and counseling.
Case Conceptualization Template
An efficient case conceptualization template helps you structure the essential components of a client's situation and establish the foundation for a focused treatment plan. By following this framework, you can guarantee that you have considered all the relevant factors and gained a comprehensive comprehension of the client and their requirements.
- Presenting problem : Briefly summarize the client's presenting issues and symptoms.
- History : Summarize relevant information about the client's family, developmental, medical, and mental health history.
- Functional analysis : Analyze the environmental, cognitive, and interpersonal factors contributing to or maintaining the client's problems. This includes triggers, consequences, and coping strategies.
- Conceptualization : Explain your theoretical model and how it helps you understand the client's difficulties. Identify key themes, patterns, and underlying processes.
- Goals : Outline the client's objectives for therapy and your treatment goals based on your conceptualization.
- Plan : Propose a treatment plan with specific interventions and strategies that address your conceptualization and the client's goals. Monitor and revise the plan as needed.
Sample Case Conceptualization #1: John
John is a 45-year-old accountant who has struggled with social anxiety and depression for most of his life. He finds it difficult to connect with others and lives a relatively isolated existence. John's anxiety causes distress in work and social situations where interaction with others is required. His anxiety and depressive symptoms have been exacerbated by several major life stressors over the past year, including a breakup with his long-term girlfriend and downsizing at his company, where he was laid off.
John sought counseling to help improve his social skills, increase confidence in social and work settings, and learn strategies to manage anxiety and depression better. Initial treatment focused on cognitive techniques to identify and reframe negative thought patterns related to social situations. Role-playing and exposure techniques were also used to help build comfort in engaging with others. John showed gradual improvement over 12 sessions. He reported feeling less anxious in work meetings and social encounters. John also started dating again and joined a local recreational sports league to increase social interaction.
John felt he had made good progress at termination but would benefit from occasional "booster" sessions to help maintain gains. Recommendations were made for John to continue practicing cognitive and exposure techniques, engage in regular exercise and social activity, and follow up with medication management as needed. John left treatment with improved coping strategies, a more balanced perspective, increased confidence in social abilities, and an overall brighter outlook.
Example of John's Case Conceptualization
I. Presenting Problem
- John sought counseling to address social anxiety, depression, and low self-confidence that had been impacting his work and social life.
- His symptoms had worsened due to recent life stressors, including a breakup and job loss.
II. Background Information
- John has struggled with social anxiety and depression for most of his life.
- He has difficulty connecting with others and lives an isolated existence.
- His anxiety causes distress in social and work situations involving interaction with others.
III. Psychosocial History
- John has a history of social anxiety dating back to childhood.
- He has few close relationships and limited social support.
- Recent life stressors have exacerbated his symptoms.
IV. Diagnostic Considerations
- Social Anxiety Disorder
- Persistent Depressive Disorder
V. Treatment Plan
- Cognitive techniques to identify and challenge negative thoughts
- Exposure exercises to build social skills and confidence
- Medication management as needed
- Recommend regular exercise, social activity, and booster sessions
- Help John develop coping strategies and a more balanced perspective
Sample Case Conceptualization #2: Jane
Jane is a 32-year-old married woman who presented with anxiety, depression, and relationship issues. She reports a lifelong struggle with feelings of inadequacy and low self-esteem. Jane's anxiety and negative self-image have contributed to difficulty asserting herself in her marriage and feeling disconnected from her husband.
Jane's symptoms worsened after the birth of her first child two years ago. She experienced postpartum depression and anxiety, which left her feeling overwhelmed as a new mother. Her husband, John, works long hours and takes on few childcare responsibilities. This has caused conflict and resentment in their relationship.
Jane sought therapy to address her depression, anxiety, and relationship problems. She wants to improve communication with her husband and negotiate a more balanced division of labor. Treatment initially focused on helping Jane identify and challenge negative automatic thoughts. Psychoeducation about assertiveness and conflict resolution strategies was provided. Role plays were used to practice effective communication and negotiation skills with her husband.
With therapy, Jane showed improvement in her mood and confidence. She was able to initiate difficult conversations with her husband about household responsibilities and childcare. Through gradual progress, Jane and her husband have found some compromise. Jane plans to continue working on assertiveness and negotiating skills to improve their relationship further. Medication may be considered in the future if symptoms do not continue to improve with therapy alone.
Example of Jane's Case Conceptualization
I. Presenting Complaints
- Relationship issues with husband
II. History of Presenting Issues
- Lifelong struggle with low self-esteem and negative self-image
- Symptoms worsened after the birth of the first child two years ago
- Experienced postpartum depression and anxiety
- Felt overwhelmed as a new mother
- Husband takes on few childcare responsibilities, causing conflict
- Married for five years, one child, age two
- Husband works long hours
- Limited social support
IV. Conceptualization
- Negative automatic thoughts contribute to anxiety and depression
- Difficulty asserting needs and communicating effectively with her husband stems from low self-esteem
- Unequal division of labor at home breeds resentment and relationship issues
- Cognitive techniques to challenge negative thoughts
- Role plays and assertiveness training to improve communication skills with husband
- Negotiation strategies for dividing household responsibilities more equitably
- Consider medication if symptoms do not improve sufficiently with therapy
Sample Case Conceptualization #3: Sally
Sally is a 45-year-old woman who presented with symptoms of anxiety, depression, and substance abuse issues. She reports a history of trauma from an abusive relationship in her 20s, which left her with trust issues and anxiety in intimate relationships.
Sally currently lives alone and works as an accountant. She struggles with loneliness and social isolation. She copes by drinking alcohol, up to a bottle of wine per night. Sally's alcohol use has negatively impacted her work and personal relationships.
Sally sought therapy to address her depression, anxiety, substance abuse, and difficulty forming close relationships. Treatment focused on building coping skills to reduce alcohol cravings and manage anxiety. Psychoeducation about trauma and its impact on trust was provided. Sally participated in exposure therapy to help her overcome social anxiety and develop healthier social connections. With treatment, Sally was able to reduce her alcohol intake to a safer level. She made progress in confronting trauma-related thoughts and feelings that had previously prevented her from forming close relationships. Sally plans to continue working on coping skills, exposure exercises, and managing trauma symptoms to fully recover from substance abuse and build a more fulfilling social life.
Example of Sally's Case Conceptualization
- Sally presents with symptoms of anxiety, depression, and substance abuse issues stemming from a history of trauma from an abusive relationship.
II. History of the Presenting Problem
- Sally has struggled with loneliness and social isolation for years since the trauma, coping with excessive alcohol use. Her drinking has negatively impacted her work and relationships.
III. Relevant Background Information
- Sally lives alone and works as an accountant
- She has difficulty forming close relationships due to trust issues from her past trauma
- Sally drinks up to a bottle of wine per night to cope with anxiety and depression
- Sally's anxiety, depression, and substance abuse are all interconnected and rooted in her unresolved trauma from the abusive relationship. Her social isolation and lack of coping skills have led to unhealthy drinking patterns.
- Reduce alcohol cravings through coping skill-building
- Provide psychoeducation about trauma and its impact
- Exposure therapy to overcome social anxiety and form healthier relationships
- Continue working on managing trauma symptoms to recover from substance abuse fully
FAQs: Your Top Case Conceptualization Questions Answered
Case conceptualization is a critical first step but can also feel overwhelming. Here are answers to some of the most frequently asked questions to help put your mind at ease.
How do I get started?
Begin by collecting information from intake forms, interviews, observations, and assessments. Look for patterns and connections to the underlying factors influencing your client's symptoms and behaviors. Identify strengths, weaknesses, thought processes, core beliefs, relationships, environment, medical issues, and life events.
What should I include?
A good case conceptualization includes a description of symptoms, diagnosis (if applicable), developmental history, family and relationship dynamics, traumas, coping skills, motivation for change, and goals. It helps determine the factors perpetuating the issues and maintaining the status quo.
How often should I update it?
A case conceptualization is a living document. As you learn more about your client through sessions, revisit and revise your conceptualization. Note any changes in symptoms or life events and adjust treatment plans accordingly. Regular updates, even minor ones, help ensure you accurately understand your client and provide the best care.
Does software help?
Case conceptualization software and apps can help organize and identify patterns in information. They can also assist you in collaborating with colleagues. However, remember that technology should supplement your clinical judgment, not replace it. Software is not capable of determining causation or proposing an effective treatment plan.
You now have what it takes to craft an effective case conceptualization. Armed with the necessary tools and examples, you can begin by considering the eight Ps - problems, precipitating events, predisposing factors, perpetuating factors, protective factors, prognosis, plan, and progress. Infuse each section with rich details about your client, including quotes and observations that bring the case to life. Examine examples from others while ensuring your conceptualization reflects your unique client and therapeutic approach. With regular practice, case conceptualizations will come naturally and aid you in selecting the best interventions and outcomes. Now, get out there and start conceptualizing.
Remember to keep learning and enhancing your practice with Mentalyc. Stay updated on the latest techniques, strategies, and tools by subscribing to our email newsletter. You'll receive emails with actionable therapy advice delivered directly to your inbox. Take advantage of our app's free trial, automatically creating progress notes based on your therapy sessions. With AI-drafted notes , you can quickly review and finalize, saving time and effort. Join our growing community of therapists and mental health professionals dedicated to practical, compassionate client care.
Biopsychosocial Model and Case Formulation . (2022, January 2). PsychDB. https://www.psychdb.com/teaching/biopsychosocial-case-formulation
Jagpat, E. (n.d.). Anatomy of a Clinical Case Conceptualization . Psychology Oral Exam Preparation, Study Materials, Consultation & more. https://psychologyoralexam.com/anatomy-of-a-clinical-case-conceptualization-psychology-oral-exam/
Sperry, L., & Sperry, J. (2016). Case Conceptualization: Mastering this Competency with Ease and Confidence . APA PsycNet. https://psycnet.apa.org/record/2012-34298-000
Zaheer, G. J., & Farmer, R. L. (2020, July 30). Science-Based Case Conceptualization . National Association of School Psychologists (NASP). https://www.nasponline.org/professional-development/a-closer-look-blog/science-based-case-conceptualization
All examples of mental health documentation are fictional and for informational purposes
See More Posts

How to Make Therapy Sessions More Productive and Effective?

Hamilton Anxiety Rating Scale (HAM-A)

A Therapist’s Guide to Build and Manage a Client Waitlist

Mentalyc Inc.

Copyright © 2021-2024 Mentalyc Inc. All rights reserved.
Meet the team
About our notes
Feature Request
Privacy Policy
Terms of Use
Business Associate Agreement
Contact Support
Affiliate program
Who we serve
Psychotherapists
Group practice owners
Pre-licensed Clinicians
Become a writer
Help articles
Client consent template
How to upload a session recording to Mentalyc
How to record sessions on Windows? (For online sessions)
How to record sessions on MacBook? (For online sessions)
Popular Blogs
Why a progress note is called a progress note
The best note-taking software for therapists
Writing therapy notes for insurance
How to keep psychotherapy notes compliant in a HIPAA-compliant manner
The best Mental health progress note generator - Mentalyc
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Introduction: Case Studies in the Ethics of Mental Health Research
Joseph millum.
Clinical Center Department of Bioethics/Fogarty International Center, National Institutes of Health, Bethesda, MD
This collection presents six case studies on the ethics of mental health research, written by scientific researchers and ethicists from around the world. We publish them here as a resource for teachers of research ethics and as a contribution to several ongoing ethical debates. Each consists of a description of a research study that was proposed or carried out and an in-depth analysis of the ethics of the study.
Building Global Capacity in Mental Health Research
According to the World Health Organization (WHO), there are more than 450 million people with mental, neurological, or behavioral problems worldwide ( WHO, 2005a ). Mental health problems are estimated to account for 13% of the global burden of disease, principally from unipolar and bipolar depression, alcohol and substance-use disorders, schizophrenia, and dementia. Nevertheless, in many countries, mental health is accorded a low priority; for example, a 2005 WHO analysis found that nearly a third of low-income countries who reported a mental health budget spent less than 1% of their total health budget on mental health ( WHO, 2005b ).
Despite the high burden of disease and some partially effective treatments that can be implemented in countries with weaker healthcare delivery systems ( Hyman et al., 2006 ), there exist substantial gaps in our knowledge of how to treat most mental health conditions. A 2007 Lancet Series entitled Global Mental Health claimed that the “rudimentary level of mental health-service research programmes in many nations also contributes to poor delivery of mental health care” ( Jacob et al., 2007 ). Its recommendations for mental health research priorities included research into the effects of interactions between mental health and other health conditions ( Prince et al., 2007 ), interventions for childhood developmental disabilities ( Patel et al., 2007 ), cost-effectiveness analysis, the scaling up of effective interventions, and the development of interventions that can be delivered by nonspecialist health workers ( Lancet Global Mental Health Group, 2007 ). All of these priorities require research in environments where the prevailing health problems and healthcare services match those of the populations the research will benefit, which suggests that research must take place all around the world. Similarly, many of the priorities identified by the Grand Challenges in Mental Health Initiative require focus on local environments, cultural factors, and the health systems of low- and middle-income countries. All the challenges “emphasize the need for global cooperation in the conduct of research” ( Collins et al., 2011 ).
Notwithstanding the need for research that is sensitive to different social and economic contexts, the trend of outsourcing to medical research to developing countries shows no sign of abating ( Thiers et al., 2008 ). Consequently, a substantial amount of mental health research will, in any case, take place in low- and middle-income countries, as well as rich countries, during the next few years.
The need for local research and the continuing increase in the international outsourcing of research imply that there is a pressing need to build the capacity to conduct good quality mental health research around the world. However, the expansion of worldwide capacity to conduct mental health research requires more than simply addressing low levels of funding for researchers and the imbalance between the resources available in rich and poor countries. People with mental health disorders are often thought to be particularly vulnerable subjects. This may be a product of problems related to their condition, such as where the condition reduces the capacity to make autonomous decisions. It may also result from social conditions because people with mental disorders are disproportionately likely to be poor, are frequently stigmatized as a result of their condition, and may be victims of human rights abuses ( Weiss et al., 2001 ; WHO, 2005a ). As a result, it is vitally important that the institutional resources and expertise are in place for ensuring that this research is carried out ethically.
Discussion at a special session at the 7th Global Forum on Bioethics in Research revealed the perception that many mental health researchers are not very interested in ethics and showed up a lack of ethics resources directly related to their work. This collection of case studies in the ethics of mental health research responds to that gap.
This collection comprises six case studies written by contributors from around the world ( Table 1 ). Each describes a mental health research study that raised difficult ethical issues, provides background and analysis of those issues, and draws conclusions about the ethics of the study, including whether it was ethical as it stood and how it ought to be amended otherwise. Three of the case studies are written by scientists who took part in the research they analyzed. For these cases, we have asked scholars independent of the research to write short commentaries on them. It is valuable to hear how the researchers themselves grapple with the ethical issues they encounter, as well as to hear the views of people with more distance from the research enterprise. Some of the ethical issues raised here have not been discussed before in the bioethics literature; others are more common concerns that have not received much attention in the context of international research. The case studies are intended to both expand academic discussion of some of the key questions related to research into mental health and for use in teaching ethics.
Case studies are an established teaching tool. Ethical analyses of such cases demonstrate the relevance of ethics to the actual practice of medical research and provide paradigmatic illustrations of the application of ethical principles to particular research situations. Concrete cases help generate and guide discussion and assist students who have trouble dealing with ethical concepts in abstraction. Through structured discussion, ethical development and decision-making skills can be enhanced. Moreover, outside of the teaching context, case study analyses provide a means to generate and focus debate on the relevant ethical issues, which can both highlight their importance and help academic discussion to advance.
People working in mental health research can benefit most from case studies that are specific to mental health. Even though, as outlined below, many of the same ethical problems arise in mental health research as elsewhere, the details of how they arise are important. For example, the nature of depression and the variation in effectiveness of antidepressive medication make a difference to how we should assess the ethics of placebo-controlled trials for new antidepressants. Moreover, seeing how familiar ethical principles are applied to one's own research specialty makes it easier to think about the ethics of one's own research. The cases in this collection highlight the commonalities and the variation in the ethical issues facing researchers in mental health around the world.
The current literature contains some other collections of ethics case studies that may be useful to mental health researchers. I note four important collections here, to which interested scholars may want to refer. Lavery et al.'s (2007) Ethical Issues in International Bio-medical Research provides in-depth analyses of ethically problematic research, mostly in low- and middle-income countries, although none of these cases involve mental health. Cash et al.'s (2009) Casebook on Ethical Issues in International Health Research also focuses on research in low- and middle-income countries, and several of the 64 short case descriptions focus on populations with mental health problems. Two further collections focus on mental health research, in particular. Dubois (2007) and colleagues developed short and longer US-based case studies for teaching as part of their “Ethics in Mental Health Research” training course. Finally, Hoagwood et al.'s (1996) book Ethical Issues in Mental Health Research with Children and Adolescents contains a casebook of 61 short case descriptions, including a few from outside the United States and Western Europe. For teachers and academics in search of more case studies, these existing collections should be very useful. Here, we expand on the available resources with six case studies from around the world with extended ethical analyses.
The remainder of this introduction provides an overview of some of the most important ethical issues that arise in mental health research and describes some of the more significant ethics guidance documents that apply.
Ethical Issues in Mental Health Research
The same principles can be applied in assessing the ethics of mental health research as to other research using human participants ( Emanuel et al., 2000 ). Concerns about the social value of research, risks, informed consent, and the fair treatment of participants all still apply. This means that we can learn from the work done in other areas of human subjects research. However, specific research contexts make a difference to how the more general ethical principles should be applied to them. Different medical conditions may require distinctive research designs, different patient populations may need special protections, and different locations may require researchers to respond to study populations who are very poor and lack access to health care or to significant variations in regulatory systems. The ethical analysis of international mental health research therefore needs to be tailored to its particularities.
Each case study in this collection focuses on the particular ethical issues that are relevant to the research it analyzes. Nevertheless, some issues arise in multiple cases. For example, questions about informed consent arise in the context of research with stroke patients, with students, and with other vulnerable groups. To help the reader compare the treatment of an ethical issue across the different case studies, the ethical analyses use the same nine headings to delineate the issues they consider. These are social value, study design, study population, informed consent, risks and benefits, confidentiality, post-trial obligations, legal versus ethical obligations, and oversight.
Here, I focus on five of these ethical issues as they arise in the context of international mental health research: (1) study design, (2) study population, (3) risks and benefits, (4) informed consent, and (5) post-trial obligations. I close by mentioning some of the most important guidelines that pertain to mental health research.
Study Design
The scientific design of a research study determines what sort of data it can generate. For example, the decision about what to give participants in each arm of a controlled trial determines what interventions the trial compares and what questions about relative safety and efficacy it can answer. What data a study generates makes a difference to the ethics of the study because research that puts human beings at risk is ethically justified in terms of the social value of the knowledge it produces. It is widely believed that human subject research without any social value is unethical and that the greater the research risks to participants, the greater the social value of the research must be to compensate ( Council for International Organizations of Medical Sciences [CIOMS], 2002 ; World Medical Association, 2008 ). However, changing the scientific design of a study frequently changes what happens to research participants, too. For example, giving a control group in a treatment trial an existing effective treatment rather than placebo makes it more likely that their condition will improve but may expose them to adverse effects they would not otherwise experience. Therefore, questions of scientific design can be ethically very complex because different possible designs are compared both in terms of the useful knowledge they may generate and their potential impact on participants.
One of the more controversial questions of scientific design concerns the standard of care that is offered to participants in controlled trials. Some commentators argue that research that tests therapeutic interventions is only permissible if there is equipoise concerning the relative merits of the treatments being compared, that is, there are not good reasons to think that participants in any arm of the trial are receiving inferior treatment ( Joffe and Truog, 2008 ). If there is not equipoise, the argument goes, then physician-researchers will be breaching their duty to give their patients the best possible care ( Freedman, 1987 ).
The Bucharest Early Intervention Project (BEIP) described in the case study by Charles Zeanah was a randomized controlled trial comparing foster care with institutional care in Bucharest, Romania. When designing the BEIP, the researchers wrestled with the issue of whether there was genuine equipoise regarding the relative merits of institutional and foster care. One interpretation of equipoise is that it exists when the professional community has not reached consensus about the better treatment ( Freedman, 1987 ). Childcare professionals in the United States were confident that foster care was superior, but there was no such confidence in Romania, where institutional care was the norm. Which, then, was the relevant professional community?
The equipoise requirement is justified by reference to the role morality of physicians: for a physician to give her patient treatment that she knows to be inferior would violate principles of therapeutic beneficence and nonmaleficence. As a result, the equipoise requirement has been criticized for conflating the ethics of the physician-patient relationship with the ethics of the researcher-participant relationship ( Miller and Brody, 2003 ). According to Miller and Brody (2003) , provided that other ethical requirements are met, including an honest null hypothesis, it is not unethical to assign participants to receive treatment regimens known to be inferior to the existing standard of care.
A subset of trial designs that violate equipoise are placebo-controlled trials of experimental treatments for conditions for which proven effective treatments already exist. Here, there is not equipoise because some participants will be assigned to placebo treatment, and ex hypothesi there already exists treatment that is superior to placebo. Even if we accept Miller and Brody's (2003) argument and reject the equipoise requirement, there remain concerns about these placebo-controlled trials. Providing participants with less effective treatment than they could get outside of the trial constitutes a research risk because trial participation makes them worse off. Moreover, on the face of it, a placebo-controlled trial of a novel treatment of a condition will not answer the most important scientific question about the treatment that clinicians are interested in: is this new treatment better than the old one? Consequently, in situations where there already exists a standard treatment of a condition, it has generally been considered unethical to use a placebo control when testing a new treatment, rather than using the standard treatment as an active-control ( World Medical Association, 2008 ).
Some psychiatric research provides scientific reasons to question a blanket prohibition on placebo-controlled trials when an effective intervention exists. For example, it is not unusual for antidepressive drugs to fail to show superiority to placebo in any given trial. This means that active-control trials may seem to show that an experimental drug is equivalent in effectiveness to the current standard treatment, when the explanation for their equivalence may, in fact, be that neither was better than placebo. Increasing the power of an active-control trial sufficiently to rule out this possibility may require an impractically large number of subjects and will, in any case, put a greater number of subjects at risk ( Carpenter et al., 2003 ; Miller, 2000 ). A 2005 trial of risperidone for acute mania conducted in India ( Khanna et al., 2005 ) was criticized for unnecessarily exposing subjects to risk ( Basil et al., 2006 ; Murtagh and Murphy, 2006 ; Srinivasan et al., 2006 ). The investigators' response to criticisms adopted exactly the line of argument just described:
A placebo group was included because patients with mania generally show a high and variable placebo response, making it difficult to identify their responses to an active medication. Placebo-controlled trials are valuable in that they expose the fewest patients to potentially ineffective treatments. In addition, inclusion of a placebo arm allows a valid evaluation of adverse events attributable to treatment v. those independent of treatment. ( Khanna et al., 2006 )
Concerns about the standard of care given to research participants are exacerbated in trials in developing countries, like India, where research participants may not have access to treatment independent of the study. In such cases, potential participants may have no real choice but to join a placebo-controlled trial, for example, because that is the only way they have a chance to receive treatment. In the Indian risperidone trial, the issue of exploitation is particularly stark because it seemed to some that participants were getting less than the international best standard of care, in order that a pharmaceutical company could gather data that was unlikely to benefit many Indian patients.
This is just one way in which trial design may present ethically troubling risks to participants. Other potentially difficult designs include washout studies, in which participants discontinue use of their medication, and challenge studies, in which psychiatric symptoms are experimentally induced ( Miller and Rosenstein, 1997 ). In both cases, the welfare of participants may seem to be endangered ( Zipursky, 1999 ). A variant on the standard placebo-controlled trial design is the withdrawal design, in which everyone starts the trial on medication, the people who respond to the medication are then selected for randomization, and then half of those people are randomized to placebo. This design was used by a Japanese research team to assess the effectiveness of sertraline for depression, as described by Shimon Tashiro and colleagues in this collection. The researchers regarded this design as more likely to benefit the participants because for legal reasons, sertraline was being tested in Japan despite its proven effectiveness in non-Japanese populations. Tashiro and colleagues analyze how the risks and benefits of a withdrawal design compare with those of standard placebo-controlled trials and consider whether the special regulatory context of Japan makes a difference.
Study Population
The choice of study population implicates considerations of justice. The Belmont Report, which lays out the ethical foundations for the United States system for ethical review of human subject research, says:
Individual justice in the selection of subjects would require that researchers … should not offer potentially beneficial research only to some patients who are in their favor or select only “undesirable” persons for risky research. Social justice requires that distinction be drawn between classes of subjects that ought, and ought not, to participate in any particular kind of research, based on the ability of members of that class to bear burdens and on the appropriateness of placing further burdens on already burdened persons. ( National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, 1978 )
Two distinct considerations are highlighted here. The first (“individual justice”) requires that the researchers treat people equally. Morally irrelevant differences between people should not be the basis for deciding whom to enroll in research. For example, it would normally be unjust to exclude women from a phase 3 trial of a novel treatment of early-stage Alzheimer disease, given that they are an affected group. Some differences are not morally irrelevant, however. In particular, there may be scientific reasons for choosing one possible research population over another, and there may be risk-related reasons for excluding certain groups. For example, a functional magnetic resonance imaging study in healthy volunteers to examine the acute effects of an antianxiety medication might reasonably exclude left-handed people because their brain structure is different from that of right-handed people, and a study of mood that required participants to forego medication could justifiably exclude people with severe depression or suicidal ideation.
The second consideration requires that we consider how the research is likely to impact “social justice.” Social justice refers to the way in which social institutions distribute goods, like property, education, and health care. This may apply to justice within a state ( Rawls, 1971 ) or to global justice ( Beitz, 1973 ). In general, research will negatively affect social justice when it increases inequality, for example, by making people who are already badly off even worse off. The quotation from the Belmont Report above suggests one way in which research might violate a requirement of social justice: people who are already badly off might be asked to participate in research and so be made worse off. For example, a study examining changes in the brain caused by alcohol abuse that primarily enrolled homeless alcoholics from a shelter near the study clinic might only put at further risk this group who are already very badly off. An alternative way in which research can promote justice or injustice is through its results. Research that leads to the development of expensive new attention deficit hyperactivity disorder medication is likely to do little, if anything, to make the world more just. Research on how to improve the cognitive development of orphaned children in poor environments (like the BEIP) is much more likely to improve social justice.
This last point suggests a further concern about fairness—exploitation—that frequently arises in the context of international collaborative research in developing countries. Exploitation occurs, roughly, when one party takes “unfair advantage” of the vulnerability of another. This means that the first party benefits from the interaction and does so to an unfair extent ( Wertheimer, 1996 ). These conditions may be met in international collaborative research when the burdens of research fall disproportionately on people and institutions in developing countries, but the benefits of research, such as access to new treatments, accrue to people in richer countries. A number of case studies in this collection raise this concern in one way or another. For example, Virginia Rodriguez analyzes a proposed study of the genetic basis of antisocial personality disorder run by US researchers but carried out at sites in several Latin American countries. One of the central objections raised by one of the local national research ethics committees with regard to this study was that there appeared to be few, if any, benefits for patients and researchers in the host country.
Risks and Benefits
Almost all research poses some risk of harm to participants. Participants in mental health research may be particularly susceptible to risk in several ways. First, and most obviously, they may be physically or psychologically harmed as a result of trial participation. For example, an intervention study of an experimental antipsychotic may result in some serious adverse effects for participants who take the drug. Less obvious but still very important are the potential effects of stopping medication. As mentioned above, some trials of psychoactive medications require that patients stop taking the medications that they were on before the trial ( e.g ., the Japanese withdrawal trial). Stopping their medication can lead to relapse, to dangerous behavior (like attempted suicide), and could mean that their previous treatment regimen is less successful when they attempt to return to it. Participants who were successfully treated during a trial may have similar effects if they do not have access to treatment outside of the trial. This is much more likely to happen in research conducted with poor populations, such as the Indian mania patients.
The harms resulting directly from research-related interventions are not the only risk to participants in mental health research. Participation can also increase the risks of psychosocial harms, such as being identified by one's family or community as having a particular condition. Such breaches of confidentiality need not involve gross negligence on the part of researchers. The mere fact that someone regularly attends a clinic or sees a psychiatrist could be sufficient to suggest that they have a mental illness. In other research, the design makes confidentiality hard to maintain. For example, the genetic research described by Rodriguez involved soliciting the enrollment of the family members of people with antisocial personality disorder.
The harm from a breach of confidentiality is exacerbated when the condition studied or the study population is stigmatized. Both of these were true in the case Sana Loue describes in this collection. She studied the co-occurrence of severe mental illnesses and human immunodeficiency virus risk in African-American men who have sex with men. Not only was there shame attached to the conditions under study, such that they were euphemistically described in the advertisements for the research, but also many of the participants were men who had heterosexual public identities.
Informed Consent
Many people with mental disorders retain the capacity (ability) and competence (legal status) to give informed consent. Conversely, potential participants without mental problems may lack or lose capacity (and competence). Nevertheless, problems with the ability to consent remain particularly pressing with regard to mental health research. This is partly a consequence of psychological conditions that reduce or remove the ability to give informed consent. To study these conditions, it may be necessary to use participants who have them, which means that alternative participants who can consent are, in principle, not available. This occurred in the study of South African stroke patients described by Anne Pope in this collection. The researcher she describes wanted to compare the effectiveness of exercises designed to help patients whose ability to communicate was compromised by their stroke. Given their communication difficulties and the underlying condition, there would inevitably be questions about their capacity. Whether it is permissible to enroll people who cannot give informed consent into a study depends on several factors, including the availability of alternative study populations, the levels of risk involved, and the possible benefits to participants in comparison with alternative health care they could receive.
In research that expects to enroll people with questionable capacity to consent, it is wise to institute procedures for assessing the capacity of prospective participants. There are two general strategies for making these assessments. The first is to conduct tests that measure the general cognitive abilities of the person being assessed, as an IQ test does. If she has the ability to perform these sorts of mental operations sufficiently well, it is assumed that she also has the ability to make autonomous decisions about research participation. A Mini-Mental State Examination might be used to make this sort of assessment ( Kim and Caine, 2002 ). The second capacity assessment strategy focuses on a prospective participant's understanding and reasoning with regard to the specific research project they are deciding about. If she understands that project and what it implies for her and is capable of articulating her reasoning about it, then it is clear that she is capable of consenting to participation, independent of her more general capacities. This sort of assessment requires questions that are tailored to each specific research project and cannot be properly carried out unless the assessor is familiar with that research.
Where someone lacks the capacity to give consent, sometimes a proxy decision maker can agree to trial participation on her behalf. In general, proxy consent is not equivalent to individual consent: unless the proxy was expressly designated to make research decisions by the patient while capacitated, the proxy lacks the power to exercise the patient's rights. As a result, the enrollment of people who lack capacity is only acceptable when the research poses a low net risk to participants or holds out the prospect of benefiting them. When someone has not designated a proxy decision maker for research, it is common to allow the person who has the power to make decisions about her medical care also to make decisions about research participation. However, because medical care is directed at the benefit of the patient, but research generally is not aimed at the benefit of participants, the basis for this assumption is unclear. Its legal basis may be weak, too. For example, in her discussion of research on South African stroke patients, Pope notes the confusion surrounding the legality of surrogate decision makers, given that the South African constitution forbids proxy decision making for adults (unless they have court-appointed curators), but local and international guidance documents seem to assume it.
Although it is natural to think of the capacity to give consent as an all-or-nothing phenomenon, it may be better conceptualized as domain-specific. Someone may be able to make decisions about some areas of her life, but not others. This fits with assumptions that many people make in everyday life. For example, a 10-year-old child may be deemed capable of deciding what clothes she will wear but may not be capable of deciding whether to visit the dentist. The capacity to consent may admit of degrees in another way, too. Someone may have diminished capacity to consent but still be able to make decisions about their lives if given the appropriate assistance. For example, a patient with mild dementia might not be capable of deciding on his own whether he should move in with a caregiver, but his memory lapses during decision making could be compensated for by having his son present to remind him of details relevant to the decision. The concept of supported decision making has been much discussed in the literature on disability; however, its application to consent to research has received little attention ( Herr, 2003 ; United Nations, 2007 ).
The ability to give valid informed consent is the aspect of autonomy that is most frequently discussed in the context of mental health research, but it is not the only important aspect. Several of the case studies in this collection also raise issues of voluntariness and coercion. For example, Douglas Wassenaar and Nicole Mamotte describe a study in which professors enrolled their students, which raises the question of the vulnerability of student subjects to pressure. Here, there is both the possibility of explicit coercion and the possibility that students will feel pressure even from well-meaning researchers. For various reasons, including dependence on caregivers or healthcare professionals and the stigma of their conditions, people with mental illnesses can be particularly vulnerable to coercion.
Post-Trial Obligations
The obligations of health researchers extend past the end of their study. Participants'data remain in the hands of researchers after their active involvement in a study is over, and patients with chronic conditions who enroll in clinical trials may leave them still in need of treatment.
Ongoing confidentiality is particularly important when studying stigmatized populations (such as men who have sex with men as discussed by Sana Loue) or people with stigmatizing conditions (such as bipolar disorder). In research on mental illnesses, as with many medical conditions, it is now commonplace for researchers to collect biological specimens and phenotypic data from participants to use in future research (such as genome-wide association studies). Additional challenges with regard to confidentiality are raised by the collection of data and biological specimens for future research because confidentiality must then be guaranteed in a long period of time and frequently with different research groups making use of the samples.
Biobanking also generates some distinctive ethical problems of its own. One concerns how consent to the future use of biological specimens should be obtained. Can participants simply give away their samples for use in whatever future research may be proposed, or do they need to have some idea of what this research might involve in order to give valid consent? A second problem, which arises particularly in transnational research, concerns who should control the ongoing use of the biobank. Many researchers think that biological samples should not leave the country in which they were collected, and developing country researchers worry that they will not be allowed to do research on the biobanks that end up in developed countries. This was another key concern with the proposed study in Latin America.
In international collaborative research, further questions arise as a result of the disparities between developing country participants and researchers and developed country sponsors and researchers. For example, when clinical trials test novel therapies, should successful therapies be made available after the trial? If they should, who is responsible for ensuring their provision, to whom should they be provided, and in what does providing them consist? In the case of chronic mental illnesses like depression or bipolar disorder, patient-participants may need maintenance treatment for the rest of their lives and may be at risk if treatment is stopped. This suggests that the question of what happens to them after the trial must at least be considered by those who sponsor and conduct the trial and the regulatory bodies that oversee it. Exactly on whom obligations fall remains a matter of debate ( Millum, 2011 ).

Ethics Guidelines
A number of important policy documents are relevant to the ethics of research into mental disorders. The WMA's Declaration of Helsinki and the CIOMS' Ethical Guidelines for Biomedical Research both consider research on individuals whose capacity and/or competence to consent is impaired. They agree on three conditions: a) research on these people is justified only if it cannot be carried out on individuals who can give adequate informed consent, b) consent to such research should be obtained from a proxy representative, and c) the goal of such research should be the promotion of the health of the population that the research participants represent ( Council for International Organizations of Medical Sciences, 2002 ; World Medical Association, 2008 ). In addition, with regard to individuals who are incapable of giving consent, Guideline 9 of CIOMS states that interventions that do not “hold out the prospect of direct benefit for the individual subject” should generally involve no more risk than their “routine medical or psychological examination.”
In 1998, the US National Bioethics Advisory Commission (NBAC) published a report entitled Research Involving Persons with Mental Disorders That May Affect Decision-making Capacity ( National Bioethics Advisory Commission, 1998 ). As the title suggests, this report concentrates on issues related to the capacity or competence of research participants to give informed consent. Its recommendations are largely consistent with those made in the Declaration of Helsinki and CIOMS, although it is able to devote much more space to detailed policy questions (at least in the United States context). Two domains of more specific guidance are of particular interest. First, the NBAC report considers the conditions under which individuals who lack the capacity to consent may be enrolled in research posing different levels of risk and supplying different levels of expected benefits to participants. Second, it provides some analysis of who should be recognized as an appropriate proxy decision maker (or “legally authorized representative”) for participation in clinical trials.
Finally, the World Psychiatric Association's Madrid Declaration gives guidelines on the ethics of psychiatric practice. This declaration may have implications for what is permissible in psychiatric research, insofar as the duties of psychiatrists as personal physicians are also duties of psychiatrists as medical researchers. It also briefly considers the ethics of psychiatric research, although it notes only the special vulnerability of psychiatric patients as a concern distinctive of mental health research ( World Psychiatric Association, 2002 ).
The opinions expressed are the author's own. They do not reflect any position or policy of the National Institutes of Health, U.S. Public Health Service, or Department of Health and Human Services.
Disclosure : The author declares no conflict of interest.
- Basil B, Adetunji B, Mathews M, Budur K. Trial of risperidone in India—concerns. Br J Psychiatry. 2006; 188 :489–490. [ PubMed ] [ Google Scholar ]
- Beitz C. Political theory and international relations. Princeton, NJ: Princeton University Press; 1973. [ Google Scholar ]
- Carpenter WT, Appelbaum PS, Levine RJ. The Declaration of Helsinki and clinical trials: A focus on placebo-controlled trials in schizophrenia. Am J Psychiatry. 2003; 160 :356–362. [ PubMed ] [ Google Scholar ]
- Cash R, Wikler D, Saxena A, Capron A, editors. Casebook on ethical issues in international health research. Geneva, Switzerland: World Health Organization; 2009. Available at: http://whqlibdoc.who.int/publications/2009/9789241547727_eng.pdf . [ Google Scholar ]
- Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS on behalf of the Scientific Advisory Board and the Executive Committee of the Grand Challenges on Global Mental Health. Grand challenges in global mental health. Nature. 2011; 475 :27–30. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Council for International Organizations of Medical Sciences. The international ethical guidelines for biomedical research involving human subjects. [Accessed on January 31, 2012]; 2002 Available at: http://www.cioms.ch/publications/layout_guide2002.pdf . [ PubMed ]
- DuBois JM. Ethical research in mental health. New York, NY: Oxford University Press; 2007. [ Google Scholar ]
- Emanuel EJ, Wendler D, Grady C. What makes clinical research ethical? JAMA. 2000; 283 :2701–2711. [ PubMed ] [ Google Scholar ]
- Freedman B. Equipoise and the ethics of clinical research. N Engl J Med. 1987; 317 :141–145. [ PubMed ] [ Google Scholar ]
- Herr SS. Self-determination, autonomy, and alternatives for guardianship. In: Herr SS, Gostin LO, Koh HH, editors. The human rights of persons with intellectual disabilities: Different but equal. Oxford, UK: Oxford University Press; 2003. pp. 429–450. [ Google Scholar ]
- Hoagwood K, Jensen PS, Fisher CB. Ethical issues in mental health research with children and adolescents. Mahwah, NJ: Lawrence Erlbaum Associates; 1996. [ Google Scholar ]
- Hyman S, Chisholm D, Kessler R, Patel V, Whiteford H. Chapter 31: Mental disorders. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, Mills A, Musgrove P, editors. Disease control priorities in developing countries. 2nd. Washington, DC; New York, NY: Oxford University Press and the World Bank; 2006. [ Google Scholar ]
- Jacob KS, Sharan P, Mirza I, Garrido-Cumbrera M, Seedat S, Mari JJ, Sreenivas V, Saxena S. Global Mental Health 4: Mental health systems in countries: where are we now? Lancet. 2007; 370 :1061–1077. [ PubMed ] [ Google Scholar ]
- Joffe S, Truog RD. Equipoise and randomization. In: Emanuel EJ, Grady C, Crouch RA, Lie RK, Miller FG, Wendler D, editors. The oxford textbook of clinical research ethics. Oxford, UK: Oxford University Press; 2008. pp. 245–260. [ Google Scholar ]
- Khanna S, Vieta E, Lyons B, Grossman F, Eerdekens M, Kramer M. Risperidone in the treatment of acute mania: Double-blind, placebo-controlled study. Br J Psychiatry. 2005; 187 :229–234. [ PubMed ] [ Google Scholar ]
- Khanna S, Vieta E, Lyons B, Grossman F, Kramer M, Eerdekens M. Trial of risperidone in India—concerns. Authors' reply. Br J Psychiatry. 2006; 188 :491. [ Google Scholar ]
- Kim SYH, Caine ED. Utility and limits of the Mini Mental State Examination in evaluating consent capacity in Alzheimer's disease. Psychiatr Serv. 2002; 53 :1322–1324. [ PubMed ] [ Google Scholar ]
- Lancet Global Mental Health Group. Global Mental Health 6: Scale up services for mental disorders: a call for action. Lancet. 2007; 370 :1241–1252. [ PubMed ] [ Google Scholar ]
- Lavery J, Grady C, Wahl ER, Emanuel EJ, editors. Ethical issues in international biomedical research: A casebook. New York, NY: Oxford University Press; 2007. [ Google Scholar ]
- Miller FG, Rosenstein DL. Psychiatric symptom-provoking studies: An ethical appraisal. Biol Psychiatry. 1997; 42 :403–409. [ PubMed ] [ Google Scholar ]
- Miller FG. Placebo-controlled trials in psychiatric research: An ethical perspective. Biol Psychiatry. 2000; 47 :707–716. [ PubMed ] [ Google Scholar ]
- Miller FG, Brody H. A critique of clinical equipoise: Therapeutic misconception in the ethics of clinical trials. Hastings Cent Rep. 2003; 33 :19–28. [ PubMed ] [ Google Scholar ]
- Millum J. Post-trial access to antiretrovirals: Who owes what to whom? Bioethics. 2011; 25 :145–154. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Murtagh A, Murphy KC. Trial of risperidone in India—concerns. Br J Psychiatry. 2006; 188 :489. [ PubMed ] [ Google Scholar ]
- National Bioethics Advisory Commission. Research involving persons with mental disorders that may affect decision-making capacity. [Accessed January 31, 2012]; 1998 Available at: http://bioethics.georgetown.edu/nbac/capacity/toc.htm .
- National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont Report: Ethical principles and guidelines for the protection of human subjects of research. Washington, DC: DHEW Publication; 1978. pp. 78–0012. No. (OS) [ PubMed ] [ Google Scholar ]
- Patel V, Araya R, Chatterjee S, Chisholm D, Cohen A, De Silva M, Hosman C, McGuire H, Rojas G, van Ommeren M. Global Mental Health 3: Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet. 2007; 370 :991–1005. [ PubMed ] [ Google Scholar ]
- Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A. Global Mental Health 1: No health without mental health. Lancet. 2007; 370 :859–877. [ PubMed ] [ Google Scholar ]
- Rawls J. A theory of justice. Cambridge, MA: Harvard University Press; 1971. [ Google Scholar ]
- Thiers FA, Sinskey AJ, Berndt ER. Trends in the globalization of clinical trials. Nature Rev Drug Discov. 2008; 7 :13–14. [ Google Scholar ]
- Srinivasan S, Pai SA, Bhan A, Jesani A, Thomas G. Trial of risperidone in India—concerns. Br J Psychiatry. 2006; 188 :489. [ PubMed ] [ Google Scholar ]
- United Nations. Legal capacity and supported decision-making in from exclusion to equality: Realizing the rights of persons with disabilities. Geneva, Switzerland: United Nations; 2007. Available at: http://www.un.org/disabilities/default.asp?id=242 . [ Google Scholar ]
- Weiss MG, Jadhav S, Raguram R, Vounatsou P, Littlewood R. Psychiatric stigma across cultures: Local validation in Bangalore and London. Anthropol Med. 2001; 8 :71–87. [ Google Scholar ]
- Wertheimer A. Exploitation. Princeton, UK: Princeton University Press; 1996. [ Google Scholar ]
- World Health Organization. Glaring inequalities for people with mental disorders addressed in new WHO effort. [Accessed January 31, 2012]; 2005a Available at: http://www.who.int/mediacentre/news/notes/2005/np14/en/index.html .
- World Health Organization. Mental Health Atlas: 2005. [Accessed January 31, 2012]; 2005b Available at: http://www.who.int/mental_health/evidence/mhatlas05/en/index.html .
- World Medical Association. The Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. [Accessed January 31, 2012]; 2008 Available at: http://www.wma.net/en/30publications/10policies/b3/index.html .
- World Psychiatric Association. Madrid Declaration on Ethical Standards for Psychiatric Practice. [Accessed January 31, 2012]; 2002 Available at: http://www.wpanet.org/detail.php?section_id=5&content_id=48 .
- Zipursky RB. Ethical issues in schizophrenia research. Curr Psychiatry Rep. 1999; 1 :13–19. [ PubMed ] [ Google Scholar ]
International Journal of Mental Health Systems welcomes well-described Case studies. These will usually present a major programme intervention or policy option relevant to the journal field. Manuscripts that include a rigorous assessment of the processes and the impact of the study, as well as recommendations for the future, will generally be considered favourably.
International Journal of Mental Health Systems strongly encourages that all datasets on which the conclusions of the paper rely should be available to readers. We encourage authors to ensure that their datasets are either deposited in publicly available repositories (where available and appropriate) or presented in the main manuscript or additional supporting files whenever possible. Please see Springer Nature’s information on recommended repositories . Where a widely established research community expectation for data archiving in public repositories exists, submission to a community-endorsed, public repository is mandatory. A list of data where deposition is required, with the appropriate repositories, can be found on the Editorial Policies Page .
Authors who need help depositing and curating data may wish to consider uploading their data to Springer Nature’s Research Data Support or contacting our Research Data Support Helpdesk . Springer Nature’s Research Data Support provides data deposition and curation to help authors follow good practice in sharing and archiving of research data, and can be accessed via an online form . The services provide secure and private submission of data files, which are curated and managed by the Springer Nature Research Data team for public release, in agreement with the submitting author. These services are provided in partnership with figshare. Checks are carried out as part of a submission screening process to ensure that researchers who should use a specific community-endorsed repository are advised of the best option for sharing and archiving their data. Use of Research Data Support is optional and does not imply or guarantee that a manuscript will be accepted.
Preparing your manuscript
The information below details the section headings that you should include in your manuscript and what information should be within each section.
Please note that your manuscript must include a 'Declarations' section including all of the subheadings (please see below for more information).
Title page
The title page should:
- "A versus B in the treatment of C: a randomized controlled trial", "X is a risk factor for Y: a case control study", "What is the impact of factor X on subject Y: A systematic review, A case report etc."
- or, for non-clinical or non-research studies: a description of what the article reports
- if a collaboration group should be listed as an author, please list the Group name as an author. If you would like the names of the individual members of the Group to be searchable through their individual PubMed records, please include this information in the “Acknowledgements” section in accordance with the instructions below
- Large Language Models (LLMs), such as ChatGPT , do not currently satisfy our authorship criteria . Notably an attribution of authorship carries with it accountability for the work, which cannot be effectively applied to LLMs. Use of an LLM should be properly documented in the Methods section (and if a Methods section is not available, in a suitable alternative part) of the manuscript
- indicate the corresponding author
The Abstract should not exceed 350 words. Please minimize the use of abbreviations and do not cite references in the abstract. The abstract must include the following separate sections:
- Background: why the case should be reported and its novelty
- Case presentation: a brief description of the patient’s clinical and demographic details, the diagnosis, any interventions and the outcomes
- Conclusions: a brief summary of the clinical impact or potential implications of the case report
Keywords
Three to ten keywords representing the main content of the article.
The Background section should explain the background to the case report or study, its aims, a summary of the existing literature.
Case presentation
This section should include a description of the patient’s relevant demographic details, medical history, symptoms and signs, treatment or intervention, outcomes and any other significant details.
Discussion and Conclusions
This should discuss the relevant existing literature and should state clearly the main conclusions, including an explanation of their relevance or importance to the field.
List of abbreviations
If abbreviations are used in the text they should be defined in the text at first use, and a list of abbreviations should be provided.
Declarations
All manuscripts must contain the following sections under the heading 'Declarations':
Ethics approval and consent to participate
Consent for publication, availability of data and materials, competing interests, authors' contributions, acknowledgements.
- Authors' information (optional)
Please see below for details on the information to be included in these sections.
If any of the sections are not relevant to your manuscript, please include the heading and write 'Not applicable' for that section.
Manuscripts reporting studies involving human participants, human data or human tissue must:
- include a statement on ethics approval and consent (even where the need for approval was waived)
- include the name of the ethics committee that approved the study and the committee’s reference number if appropriate
Studies involving animals must include a statement on ethics approval and for experimental studies involving client-owned animals, authors must also include a statement on informed consent from the client or owner.
See our editorial policies for more information.
If your manuscript does not report on or involve the use of any animal or human data or tissue, please state “Not applicable” in this section.
If your manuscript contains any individual person’s data in any form (including any individual details, images or videos), consent for publication must be obtained from that person, or in the case of children, their parent or legal guardian. All presentations of case reports must have consent for publication.
You can use your institutional consent form or our consent form if you prefer. You should not send the form to us on submission, but we may request to see a copy at any stage (including after publication).
See our editorial policies for more information on consent for publication.
If your manuscript does not contain data from any individual person, please state “Not applicable” in this section.
All manuscripts must include an ‘Availability of data and materials’ statement. Data availability statements should include information on where data supporting the results reported in the article can be found including, where applicable, hyperlinks to publicly archived datasets analysed or generated during the study. By data we mean the minimal dataset that would be necessary to interpret, replicate and build upon the findings reported in the article. We recognise it is not always possible to share research data publicly, for instance when individual privacy could be compromised, and in such instances data availability should still be stated in the manuscript along with any conditions for access.
Authors are also encouraged to preserve search strings on searchRxiv https://searchrxiv.org/ , an archive to support researchers to report, store and share their searches consistently and to enable them to review and re-use existing searches. searchRxiv enables researchers to obtain a digital object identifier (DOI) for their search, allowing it to be cited.
Data availability statements can take one of the following forms (or a combination of more than one if required for multiple datasets):
- The datasets generated and/or analysed during the current study are available in the [NAME] repository, [PERSISTENT WEB LINK TO DATASETS]
- The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
- All data generated or analysed during this study are included in this published article [and its supplementary information files].
- The datasets generated and/or analysed during the current study are not publicly available due [REASON WHY DATA ARE NOT PUBLIC] but are available from the corresponding author on reasonable request.
- Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
- The data that support the findings of this study are available from [third party name] but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of [third party name].
- Not applicable. If your manuscript does not contain any data, please state 'Not applicable' in this section.
More examples of template data availability statements, which include examples of openly available and restricted access datasets, are available here .
BioMed Central strongly encourages the citation of any publicly available data on which the conclusions of the paper rely in the manuscript. Data citations should include a persistent identifier (such as a DOI) and should ideally be included in the reference list. Citations of datasets, when they appear in the reference list, should include the minimum information recommended by DataCite and follow journal style. Dataset identifiers including DOIs should be expressed as full URLs. For example:
Hao Z, AghaKouchak A, Nakhjiri N, Farahmand A. Global integrated drought monitoring and prediction system (GIDMaPS) data sets. figshare. 2014. http://dx.doi.org/10.6084/m9.figshare.853801
With the corresponding text in the Availability of data and materials statement:
The datasets generated during and/or analysed during the current study are available in the [NAME] repository, [PERSISTENT WEB LINK TO DATASETS]. [Reference number]
If you wish to co-submit a data note describing your data to be published in BMC Research Notes , you can do so by visiting our submission portal . Data notes support open data and help authors to comply with funder policies on data sharing. Co-published data notes will be linked to the research article the data support ( example ).
All financial and non-financial competing interests must be declared in this section.
See our editorial policies for a full explanation of competing interests. If you are unsure whether you or any of your co-authors have a competing interest please contact the editorial office.
Please use the authors initials to refer to each authors' competing interests in this section.
If you do not have any competing interests, please state "The authors declare that they have no competing interests" in this section.
All sources of funding for the research reported should be declared. If the funder has a specific role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript, this should be declared.
The individual contributions of authors to the manuscript should be specified in this section. Guidance and criteria for authorship can be found in our editorial policies .
Please use initials to refer to each author's contribution in this section, for example: "FC analyzed and interpreted the patient data regarding the hematological disease and the transplant. RH performed the histological examination of the kidney, and was a major contributor in writing the manuscript. All authors read and approved the final manuscript."
Please acknowledge anyone who contributed towards the article who does not meet the criteria for authorship including anyone who provided professional writing services or materials.
Authors should obtain permission to acknowledge from all those mentioned in the Acknowledgements section.
See our editorial policies for a full explanation of acknowledgements and authorship criteria.
If you do not have anyone to acknowledge, please write "Not applicable" in this section.
Group authorship (for manuscripts involving a collaboration group): if you would like the names of the individual members of a collaboration Group to be searchable through their individual PubMed records, please ensure that the title of the collaboration Group is included on the title page and in the submission system and also include collaborating author names as the last paragraph of the “Acknowledgements” section. Please add authors in the format First Name, Middle initial(s) (optional), Last Name. You can add institution or country information for each author if you wish, but this should be consistent across all authors.
Please note that individual names may not be present in the PubMed record at the time a published article is initially included in PubMed as it takes PubMed additional time to code this information.
Authors' information
This section is optional.
You may choose to use this section to include any relevant information about the author(s) that may aid the reader's interpretation of the article, and understand the standpoint of the author(s). This may include details about the authors' qualifications, current positions they hold at institutions or societies, or any other relevant background information. Please refer to authors using their initials. Note this section should not be used to describe any competing interests.
Footnotes can be used to give additional information, which may include the citation of a reference included in the reference list. They should not consist solely of a reference citation, and they should never include the bibliographic details of a reference. They should also not contain any figures or tables.
Footnotes to the text are numbered consecutively; those to tables should be indicated by superscript lower-case letters (or asterisks for significance values and other statistical data). Footnotes to the title or the authors of the article are not given reference symbols.
Always use footnotes instead of endnotes.
Examples of the Vancouver reference style are shown below.
See our editorial policies for author guidance on good citation practice
Web links and URLs: All web links and URLs, including links to the authors' own websites, should be given a reference number and included in the reference list rather than within the text of the manuscript. They should be provided in full, including both the title of the site and the URL, as well as the date the site was accessed, in the following format: The Mouse Tumor Biology Database. http://tumor.informatics.jax.org/mtbwi/index.do . Accessed 20 May 2013. If an author or group of authors can clearly be associated with a web link, such as for weblogs, then they should be included in the reference.
Example reference style:
Article within a journal
Smith JJ. The world of science. Am J Sci. 1999;36:234-5.
Article within a journal (no page numbers)
Rohrmann S, Overvad K, Bueno-de-Mesquita HB, Jakobsen MU, Egeberg R, Tjønneland A, et al. Meat consumption and mortality - results from the European Prospective Investigation into Cancer and Nutrition. BMC Medicine. 2013;11:63.
Article within a journal by DOI
Slifka MK, Whitton JL. Clinical implications of dysregulated cytokine production. Dig J Mol Med. 2000; doi:10.1007/s801090000086.
Article within a journal supplement
Frumin AM, Nussbaum J, Esposito M. Functional asplenia: demonstration of splenic activity by bone marrow scan. Blood 1979;59 Suppl 1:26-32.
Book chapter, or an article within a book
Wyllie AH, Kerr JFR, Currie AR. Cell death: the significance of apoptosis. In: Bourne GH, Danielli JF, Jeon KW, editors. International review of cytology. London: Academic; 1980. p. 251-306.
OnlineFirst chapter in a series (without a volume designation but with a DOI)
Saito Y, Hyuga H. Rate equation approaches to amplification of enantiomeric excess and chiral symmetry breaking. Top Curr Chem. 2007. doi:10.1007/128_2006_108.
Complete book, authored
Blenkinsopp A, Paxton P. Symptoms in the pharmacy: a guide to the management of common illness. 3rd ed. Oxford: Blackwell Science; 1998.
Online document
Doe J. Title of subordinate document. In: The dictionary of substances and their effects. Royal Society of Chemistry. 1999. http://www.rsc.org/dose/title of subordinate document. Accessed 15 Jan 1999.
Online database
Healthwise Knowledgebase. US Pharmacopeia, Rockville. 1998. http://www.healthwise.org. Accessed 21 Sept 1998.
Supplementary material/private homepage
Doe J. Title of supplementary material. 2000. http://www.privatehomepage.com. Accessed 22 Feb 2000.
University site
Doe, J: Title of preprint. http://www.uni-heidelberg.de/mydata.html (1999). Accessed 25 Dec 1999.
Doe, J: Trivial HTTP, RFC2169. ftp://ftp.isi.edu/in-notes/rfc2169.txt (1999). Accessed 12 Nov 1999.
Organization site
ISSN International Centre: The ISSN register. http://www.issn.org (2006). Accessed 20 Feb 2007.
Dataset with persistent identifier
Zheng L-Y, Guo X-S, He B, Sun L-J, Peng Y, Dong S-S, et al. Genome data from sweet and grain sorghum (Sorghum bicolor). GigaScience Database. 2011. http://dx.doi.org/10.5524/100012 .
Figures, tables and additional files
See General formatting guidelines for information on how to format figures, tables and additional files.
Submit manuscript
- Editorial Board
- Manuscript editing services
- Instructions for Editors
- Sign up for article alerts and news from this journal
Annual Journal Metrics
2022 Citation Impact 3.6 - 2-year Impact Factor 3.9 - 5-year Impact Factor 1.582 - SNIP (Source Normalized Impact per Paper) 1.138 - SJR (SCImago Journal Rank)
2023 Speed 44 days submission to first editorial decision for all manuscripts (Median) 290 days submission to accept (Median)
2023 Usage 1,612,135 downloads 428 Altmetric mentions
- More about our metrics
International Journal of Mental Health Systems
ISSN: 1752-4458
- Submission enquiries: [email protected]
- Last edited on January 27, 2024
Biopsychosocial Model and Case Formulation
Table of contents, diagnosis versus formulation, the formulation table, "jane doe", biological and social factors, psychological factors, completed table, method 1 (sequential), method 2 (narrative), method 3 (advanced), method 4 (chronological), common phrases to use, do's and dont's, another example, "templates".
The Biopsychosocial Model and Case Formulation (also known as the Biopsychosocial Formulation ) in psychiatry is a way of understanding a patient as more than a diagnostic label. Hypotheses are generated about the origins and causes of a patient's symptoms. The most common and clinically practical way to formulate is through the biopsychosocial approach, first described in 1980 by George Engel. [1] [2] Biopsychosocial formulation combines biological, psychological, and social factors to understand a patient, and uses this to guide both treatment and prognosis. Your formulation of a patient evolves and changes as you collect more information. Formulation is like cooking, and there is no 'right' or 'wrong' way to do it, but most get better over time with increasing clinical experience.
Buy on Amazon
<small> PsychDB is an Amazon Associate and earns from qualifying purchases. Thank you for supporting our site!</small> </HTML>
Diagnosis is not the same as formulation! In mental health, when there is a group of consistent symptoms seen in a population, these symptoms can be categorized into a distinct entity, called a diagnosis (this is what the DSM-5 does). For example, we diagnose someone with a major depressive episode if they meet 5 of the 9 symptomatic criteria. However, formulation tells us how the person became depressed as a result of their genetics , personality , psychological factors , biological factors, social circumstances ( childhood adverse events and social determinants of health ), and their environment.
You are probably already formulating, but just don't know it. Like most things in medicine, there are multifactorial causes of diseases, illnesses, and disorders. For example, type II diabetes does not develop because of a single pathophysiological cause. The patient may have a strong family history of the disease, a sedentary job, environmental exposures, and/or a nutritionally-poor diet. These factors all combine to cause the person to develop diabetes. Understanding how each factor contributes to a disease can better guide treatment decisions. In psychiatry, formulation appears more complicated because human behaviour and the brain itself is extraordinarily complex. However, like with anything, the more you practice, the better you will become at formulating.
What Are You Formulating?
Why is a biopsychosocial approach important, formulation in a nutshell.
The biopsychosocial model considers the “4 Ps” for each of the biological, psychological, and social factors:
- Predisposing factors are areas of vulnerability that increase the risk for the presenting problem. Examples include genetic (i.e. -family history) predisposition for mental illness or prenatal exposure to alcohol.
- Precipitating factors are typically thought of as stressors or other events (they could be positive or negative) that may be precipitants of the symptoms. Examples include conflicts about identity, relationship conflicts, or transitions.
- Perpetuating factors are any conditions in the patient, family, community, or larger systems that exacerbate rather than solve the problem. Examples include unaddressed relationship conflicts, lack of education, financial stresses, and occupation stress (or lack of employment)
- Protective factors include the patient’s own areas of competency, skill, talents, interest and supportive elements. Protective factors counteract the predisposing, precipitating, and perpetuating factors.
The “4 Ps” can be laid out in a 3 x 4 table to systematically do formulation and identity factors. Note that this table is extremely comprehensive and long, and not everything will (or should!) apply to your case. It is important to remember that not everything will fit neatly into each box. For example, many precipitating and perpetuating factors may overlap and fit in other boxes. Use this table as a general guide, but don't memorize it for the sake of memorizing it!
Biopsychosocial Model
Filling out the table.
- As you can see in the table above, it's a lot of questions to ask and a lot of things to think about!
- Let's do a simplified formulation for the patient (Jane Doe) below. The image ( figure 1 ) provides a guide on how to put information into the formulation table.
- These psychological symptoms/factors are then observed by the clinician to give a psychiatric diagnosis.
- This is why the psychological section of the table is filled last, so we can understand what biological and social factors led to the development of these symptoms.
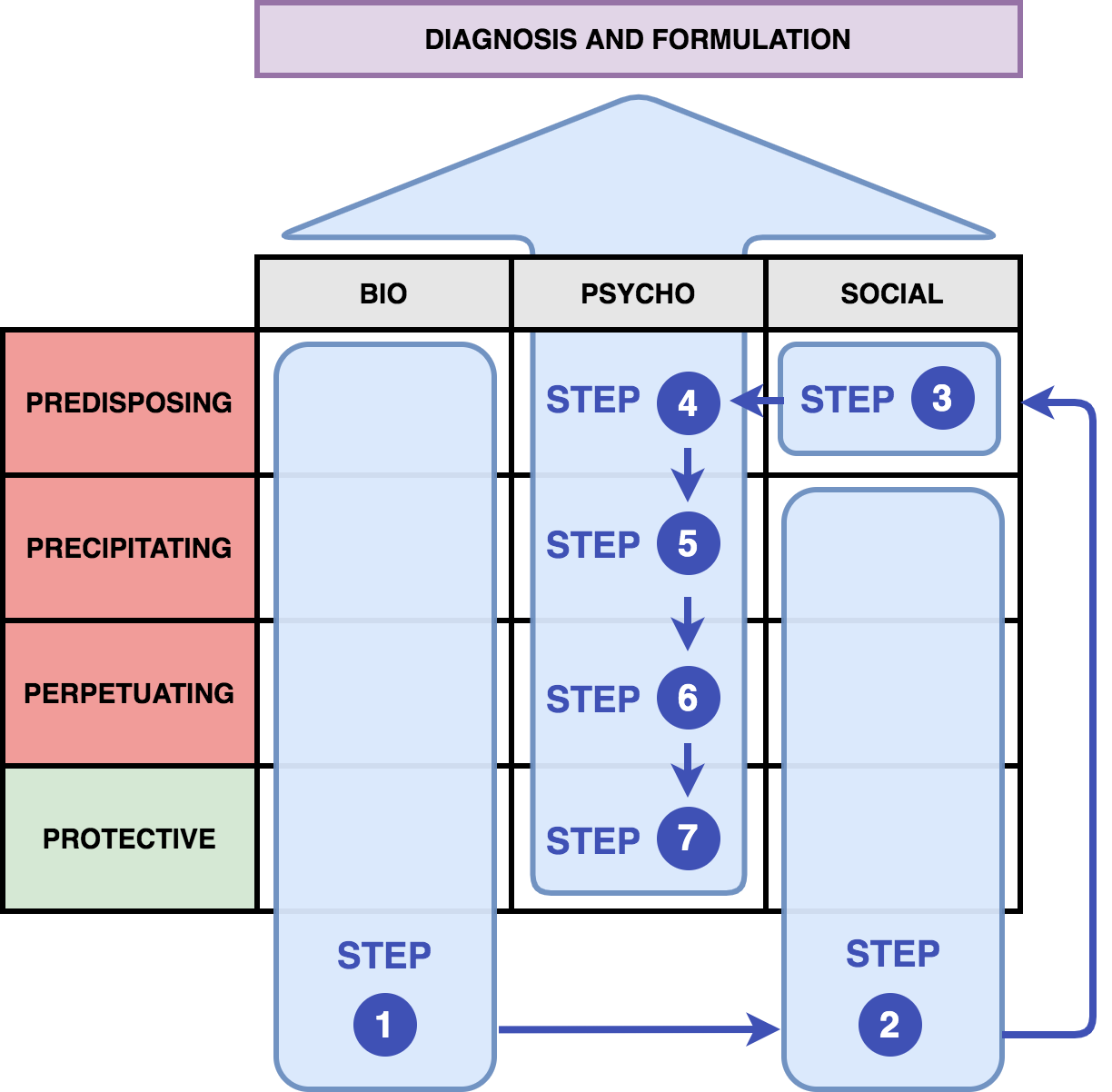
- Jane Doe is a 30-year-old female who presents to the emergency room with acute suicidal ideation and self-harm
- Jane has been working at a start up company for the past 2 years. She was suddenly fired from her job today due to conflicts at work with co-workers and being late at work several times from sleeping in. After being told she was fired from her job, she went home and self-harmed to cope with the distress of this loss. She also drank 10 beers prior to arriving in the hospital. She subsequently planned to overdose on her medications. A concerned best friend called and talked to her this evening, and brought her to the hospital. Her mood was stable prior to this job loss, and she had no self-harm or suicidal thoughts in the past 1 year.
- Increasing alcohol use for the past 3 months, drinking up to 5 beers per day.
- Sertraline (Zoloft) 75mg PO daily
- She has a past history of borderline personality disorder , depression , and alcohol use disorder (moderate). She used to be a soccer player and has a history of multiple concussions. She does have a psychiatrist that she sees every month. She previously completed a course of dialectical behavioural therapy , which was helpful.
- Depression and bipolar disorder on maternal side of her family. There is a history of alcohol use disorder on paternal side.
- Born in Canada. University-educated. There was a parental divorce at age 5. She describes an invalidating childhood, where parents did not acknowledge or praise her. She experienced sexual abuse and trauma at age 12. She is in a 2-year relationship with a male partner, and there have been recent arguments about the direction of their relationship. She describes a long-standing fear of being abandoned in relationships, and reports having very intense relationships with friends/family. Financially, she is struggling to pay rent and living from paycheque-to-paycheque. Developmentally, there may have been some speech delay . Collateral information from the patient's older brother describe her childhood temperament as being avoidant and fearful of her parents.
Steps 1 and 2
Sample formulation for jane doe.
Now that you've filled in the easy parts from the history, the hardest part is conceptualizing the predisposing social factors (Step 3), and all of the psychological factors (Steps 4, 5, 6, 7). This is where you'll need to be creative and also think more in-depth about your patient. Ideally, each step should flow logically and intuitively into the next based on your framework, as you'll see in our case of Jane Doe. Having a framework for understanding of different psychological treatments and psychological theories can be helpful in making your psychological formulation flow intuitively (e.g. - attachment theory , cognitive behavioural therapy , dialectical behavioural therapy , interpersonal therapy , psychodynamic therapy ). However, this can be done intuitively even without an in-depth understanding of these frameworks (we don't need to be Freud to do this). The more cases you go through (and more of the sample formulations below) the more comfortable you will be with formulating!
Steps 3, 4, 5, 6, and 7
Jane doe's formulation, completed biopsychosocial formulation table, completed formulation of jane doe, presenting your formulation.
You've got your table all filled out now. Now what? How do you present all this information and data? Remember there is no “right” or “wrong” way to present your formulation. But the most important thing about formulation is that it should be intuitive and flow logically. Some different presentation styles are suggested here.
The “4 Ps” formulation table can be a very rigid and systematized way of presenting a formulation. At its most basic, you could present each box sequentially and describe each factor. Most learners will use this method as it is the most “simple.” It is usually presented as Predisposing → Precipitating → Perpetuating → Protective factors. As you get better and more expert at formulating, you may not need to use this rigid structured format, and instead, will be able to present a more intuitive and organic formulation of the patient instead (see other methods below).
- Brief summarizing statement that includes demographic information, chief complaint, and presenting problems from patient's perspective and signs and symptoms (onset, severity, pattern)
- Predisposing factors
- Precipitating factors
- Perpetuating factors
- Strengths and protective factors
- Integrative statement: how these factors interact to lead to the current situation and level of functioning, prognosis, and potential openings for intervention
Example: 4 Ps Table Formulation of Jane Doe
- Jane Doe presents with a diagnosis of borderline personality disorder and history of depression. She presents to hospital today with acute suicidal ideation and self-harm after being fired from her job.
- Predisposing factors : Her predisposing biological factors include a family history of mental disorders and substance use, concussion history, and a fearful/anxious temperament at birth. Her predisposing social factors include a history of sexual trauma at a young age, and early parental divorce. These led to her predisposing psychological factors, including a history of invalidation by her parents, and fears of abandonment during childhood.
- Precipitating factors : Her precipitating biological factors include a 3-month history of increasing alcohol use. Her precipitating social factors is her being fired from her current job. These led to her precipitating psychological factors, which resulted in her underlying feelings of abandonment and invalidation re-activated after being fired from work.
- Perpetuating factors : Her perpetuating biological factors include being on a subtherapeutic dose of her medication, and her ongoing alcohol use. Her perpetuating social factors includes her ongoing relationship conflicts and financial stressors. Her perpetuating psychological factors include her lack of adaptive coping strategies and ongoing self-harm.
- Strengths and protective factors : She is medically healthy, and has previously responded well to therapy. She also is supported by a good friend, and sees a psychiatrist regularly.
- Integrative Statement : The acute stressor of losing her job has re-activated the psychological processes described above. The patient is psychologically minded and thus would benefit from treatment with dialectical behavioural therapy. Her medications could also be further optimized as well. Overall, her prognosis is good due to her protective factors as mentioned above.
The narrative formulation of the patient is a less rigid presentation structure where you may not choose to present everything in the 4 Ps table, and instead focus on the key factors that you think are relevant:
- [Patient] presents with a [diagnosis]. They are biologically predisposed because of [reasons]. They struggle with the following [psychological difficulties]. Their underlying temperament is [temperament], which further exacerbates the symptoms.
- Childhood/adult trauma (if any)
- Attachment style
- About themselves
- About others
- About the world
- (i) death of their spouse
- (ii) stopping medications
- (iii) loss of job
- (iv) re-experiencing of trauma
- They have the following: [protective factors]
Example: Narrative Formulation of Jane Doe
- Jane Doe presents with a diagnosis of borderline personality disorder and history of depression. She is biologically predisposed, with a family history of depression and alcohol use disorder in her immediate family members. She struggles with the following psychological difficulties, including fears of abandonment. Her underlying temperament is anxious, which further exacerbates her symptoms.
- Her underlying history of experiencing trauma and sexual abuse at a young age
- A history of invalidating experiences in childhood
- That she is not deserving of love or close relationships, a core belief of her being “unlovable”, and that self-harm is the main way of coping with stressors
- That others may leave or abandon her any time, increased rejection sensitivity, and a future fear of being rejected
- That the world can be a fearful and scary place
- After being fired from her job, she experienced strong feelings of rejection, and was unable to cope with this major stressor. This may have reactivated/exacerbated her emotional dysregulation, and resulted in negative coping styles such as her self-harming and suicidal ideation. She also appears to use alcohol as a way of managing distressing emotions, but does not have any psychological coping strategies. This has further exacerbated her alcohol use disorder.
- She has the following protective factors, including a supportive psychiatrist and friend. She has also previously responded well to psychotherapy and appears to be psychologically-minded.
A much more advanced and nuanced presentation might be using a more comprehensive formulation that integrates the 4Ps formulation through multiple lenses (e.g. - Eriksonian developmental stages , psychodynamic defenses , and dialectical behavioural ):
- Current stressors, plus salient developmental history
- “The patient presents at this time with [problem and symptoms], in the context of [situation and stressors]”
- Genetics, temperament, medical history, substances, medications
- “The patient has the following [genetic vulnerabilities, medical history]”
- “The patient grew up in a family characterized by [factors], with a caregiver who was [distant/available/invalidating]”
- “ Attachment was likely [secure/insecure/disorganized] given [developmental history]”
- “The patient may have had difficulty in [stage of development], and this is reflected in [examples from adult relationships]
- “It appears that the patient may have struggled with conflicts in early life. It also appears they may have had difficulty with [drives], stemming from [psychoanalytic concept]
- Control/regulation of drives
- “These experiences impacted the patient's view of themselves as being [view of self], and this has continued into adulthood based on [experiences].”
- “The patient appears to have adopted [defense mechanisms] as coping strategies by early adulthood, and these have continued on…”
- “The patient's interpersonal relationships appear to be [give examples of patterns of relationships]”
- These underlying factors may have precipitated the patient's [current presentation]. These symptoms have been maintained by [psychological factors/personality factors], and [social/environmental factors]
- “We would anticipate when engaging in treatment, the patient may have [resistance/transference/countertransference]. However, patient has the following [protective factors], which may be a good prognostic factor. Based on these factors, the following [treatment and management] would be the most helpful for this patient.
Example: Advanced Formulation of Jane Doe
- Jane Doe is a 30-year-old female who presents with acute suicidal ideation in the context of a job loss. She notably has a past history of childhood trauma and abuse.
- The patient has genetic vulnerabilities for mental illness in her family history, a history of anxious temperament, ongoing substance use, and subtherapeutic medication levels.
- She has several early developmental and pathogenic psychological factors, including growing up in a family characterized by invalidation, with parents who were distant and unavailable. This likely led to an attachment style that was likely insecure and disorganized. Due to her history of abuse at age 12, she may have struggled with identity versus role confusion during that Eriksonian stage of psychosocial development. As she was unable to develop a sense of self and personal identity, these psychological factors are reflected in her adulthood with unstable relationships, and fears of abandonment. This has led to her adulthood self-perception of being unworthy of being loved, a constant fear of rejection, and increased rejection sensitivity. The patient appears to have adopted self-harming as a primitive coping strategy by early adulthood, and these have continued on in adulthood.
- Precipitating and perpetuating factors: the stressor of losing her job has reactivated these more primitive defense mechanisms and coping strategies. These symptoms have been further perpetuated by the personality factors and traits described above, and her ongoing financial stressors. Her ongoing alcohol use is another example of a maladaptive coping strategy.
- We would anticipate when engaging in treatment, the patient may have difficulties with using primitive defense mechanisms. However, the patient has protective factors including psychological mindedness and previous response to therapy, which is a good prognostic factor. Based on these factors, dialectical behavioural therapy would be the most helpful for this patient.
Yet another way to present a formulation is in chronological order, starting from birth until present time:
- Genetics (family history)
- Birth (issues at birth, developmental history, developmental stages)
- Childhood (attachment style, neurodevelopment, milestones, trauma)
- Adolescence (relationships, trauma, school performance, substances)
- Adulthood (occupation, relationships, children, environment, stressors)
- Integrative statement (of how genetics, birth, childhood, adolescence, and adulthood factors contribute to current presentation, and how this directs your treatment/management)
Having certain common phrases to use can be helpful to structure your presentation. Here are some examples:
- “From a biological perspective, the patient is vulnerable because…”
- “The patient's early childhood and developmental history suggest…”
- “Used substances as a coping style in [the past], and now this is occurring again (or there is a relapse) due to [social factor].”
- “Used substances as a coping style in [the past], and now this is occurring again (or there is a relapse) due to [psychological vulnerability].”
- “I wonder if… [psychological factor] is contributing to [current symptoms/struggles]”
- Use your own words and personal style
- Tell a story and narrative that is unique to your patient
- Be specific and demonstrate your understanding of the patient as a person and not a diagnosis
- Use words like precipitating, protective, and perpetuating factors to anchor your listener
- Focus on the most salient features and be concise
- Try and use a psychological theory (but only if you understand it)
- Be confident in your presentation!
- Include too much extra detail
- Try to be perfect only to overwhelm yourself
- Be generic (your formulation needs to be unique to your patient)
- Tell the patient's whole story all over again
- Mention life events or trauma without an understanding of its meaning or impact
- Try to formulate a “grand unified theory” of the patient and over-reach with your theory (if it doesn’t fit, it doesn’t fit! And that's okay!)
- Cover every box in the 4 Ps just for the sake of doing it (not all boxes will always apply!)
Beyond Basic Formulation
A good formulation should be integrative, and let you understand how all of the patient's factors interact to lead to the current situation. This gives you a sense of their current level of functioning, prognosis, and guides your direction for treatment and management decisions.
A good biopsychosocial formulation allows you to come up with a comprehensive and holistic treatment plan for your patient. Here is an example of a set of treatment recommendations for Jane Doe:
- What level of care is required (outpatient or inpatient)?
- Jane is able to articulate a safe plan to stay with a friend, and is suitable for outpatient care
- Jane might benefit from an increase of her sertraline from 75mg to 100mg and beyond (maximum dose of 200mg), for her mood dysregulation and depressive symptoms
- Jane might benefit from the use of anti-craving medications such as gabapentin or acamprosate to reduce her cravings for alcohol use
- Dialectical behavioural therapy (DBT) would be the most appropriate for Jane
- Jane would also benefit from motivational interviewing for her alcohol use
- Long-term, Jane might also benefit from a more in-depth understanding of how her past trauma affects her present self and symptoms. This could be achieved with more specific and in depth trauma therapy, but given the acuity of her symptoms, this is something that would follow after DBT.
- Jane could benefit from accessing support from her company's HR department to understand what options she has after her job termination
- Substance use groups such as Alcoholic's Anonymous
- Increasing connections to her friends and social supports
For good measure, here is another sample formulation for someone with a diagnosis of schizophrenia . Note that in this example, since the precipitating cause for acute psychosis (also applies to manic episodes ) is more “biological,” it may be harder to identify underlying psychological factors (but that's OK too – even the most “biological” psychiatric disorders can often be precipitated by psychosocial stressors). Again let's fill out the easiest parts of the table first:
Sample Formulation for Schizophrenia (Initial)
Now here is one potential example of a predisposing social and psychological formulation of psychosis (again, there are no right or wrong ways to formulate, it depends on the patient you have in front of you!)
Example of A Possible Psychological Formulation of Psychosis/Schizophrenia
Here's what the completed table would look like with the psychological factors incorporated.
Completed Formulation for Schizophrenia (Initial)
As you do more formulation, you will notice that patients tend to present in “templates,” that is, certain diagnoses tend to follow a certain common theme of predisposing, precipitating, and perpetuating factors. The more you formulate, it can be helpful to have a rough template of different formulations for different diagnoses (e.g. - depression, self-harm, mania/psychosis, anxiety, etc.) It will make your job of formulating much easier.
The following readings below are excellent resources to further develop your formulation skills:
- Selzer, R., & Ellen, S. (2014). Formulation for beginners. Australasian Psychiatry, 22(4), 397-401.
- Winters, N. C., Hanson, G., & Stoyanova, V. (2007). The case formulation in child and adolescent psychiatry. Child and Adolescent Psychiatric Clinics, 16(1), 111-132.
- Weerasekera, P. (1993). Formulation: A multiperspective model. The Canadian Journal of Psychiatry, 38(5), 351-358.
Beyond the Biopsychosocial Model
- Kendler, K. S. (2012). The dappled nature of causes of psychiatric illness: Replacing the organic–functional/hardware–software dichotomy with empirically based pluralism. Molecular psychiatry, 17(4), 377-388.
How to Write a Case Study
This guide explains how to write a descriptive case study. A descriptive case study describes how an organization handled a specific issue. Case studies can vary in length and the amount of details provided. They can be fictional or based on true events.
Why should you write one? Case studies can help others (e.g., students, other organizations, employees) learn about
- new concepts,
- best practices, and
- situations they might face.
Writing a case study also allows you to critically examine your organizational practices.
The following pages provide examples of different types of case study formats. As you read them, think about what stands out to you. Which format best matches your needs? You can make similar stylistic choices when you write your own case study.
ACF Case Studies of Community Economic Development This page contains links to nine case studies that describe how different organizations performed economic development activities in their communities.
National Asthma Control Program Wee Wheezers This case study describes a public health program.
CDC Epidemiologic Case Studies This page contains links to five classroom-style case studies on foodborne diseases.
ATSDR Environmental Health and Medicine This page contains links to approximately 20 classroom-style case studies focused on exposures to environmental hazards.
What are your goals ? What should your intended readers understand or learn after reading your case? Pick 1–5 realistic goals. The more goals you include, the more complex your case study might need to be.
Who is your audience? You need to write with them in mind.
What kind of background knowledge do they have? Very little, moderate, or a lot of knowledge. Be sure to explain special terms and jargon so that readers with little to moderate knowledge can understand and enjoy your case study.
What format do you need to use? Will your case study be published in a journal, online, or printed as part of a handout? Think about how word minimums or maximums will shape what you can talk about and how you talk about it. For example, you may be allowed fewer words for a case study written for a print textbook than for a webpage.
What narrative perspective will you use? A first-person perspective uses words such as “I” and” “we” to tell a story. A third-person perspective uses pronouns and names such as “they” or “CDC”. Be consistent throughout your case study.
Depending on your writing style, you might prefer to write everything that comes to your mind first, then organize and edit it later. Some of you might prefer to use headings or be more structured and methodical in your approach. Any writing style is fine, just be sure to write! Later, after you have included all the necessary information, you can go back and find more appropriate words, ensure your writing is clear, and edit your punctuation and grammar.
- Use clear writing principles, sometimes called plain language. More information can be found in the CDC’s Guide to Clear Writing [PDF – 5 MB] or on the Federal Plain Language website .
- Use active voice instead of passive voice. If you are unfamiliar with active voice, review resources such as NCEH/ATSDR’s Training on Active Voice , The National Archive’s Active Voice Tips , and USCIS’ Video on Active Voice .
- Word choice is important. If you use jargon or special terminology, define it for readers.
- CDC has developed many resources to help writers choose better words. These include the NCEH/ATSDR Environmental Health Thesaurus , CDC’s National Center for Health Marketing Plain Language Thesaurus for Health Communicators [PDF – 565 KB] , CDC’s Everyday Words for Public Health Communication [PDF – 282 KB] , and the NCEH/ATSDR’s Clear Writing Hub .
After writing a draft, the case study writer or team should have 2–3 people, unfamiliar with the draft, read it over. These people should highlight any words or sentences they find confusing. They can also write down one or two questions that they still have after reading the draft. The case study writer or team can use those notes make edits.
- Review your goals for the case study. Have you met each goal? Make any necessary edits.
- Check your sentence length. If your sentence has more than 20 words, it might be too long. Limit each sentence to one main idea.
- Use common words and phrases. Review a list of commonly misused words and phrases.
- Be sure you have been consistent with your verb tenses throughout.
Finally, the writer/team should have someone with a good eye for detail review the case study for grammar and formatting issues. You can review the CDC Style Guide [PDF – 1.36 MB] for clarification on the use of punctuation, spelling, tables, etc.
Green BN, Johnson CD. How to write a case report for publication. Journal of Chiropractic Medicine. 2006;5(2):72-82. https://doi.org/10.1016/S0899-3467(07)60137-2
Scholz RW, Tietje O. Types of case studies. In: Embedded Case Study Methods . Thousand Oaks (CA): SAGE Publications, Inc.; 2002. P. 9-14. doi:10.4135/9781412984027
Warner C. How to Write a Case Study [online]. 2009. Available from URL: https://www.asec.purdue.edu/lct/HBCU/documents/HOWTOWRITEACASESTUDY.pdf [PDF – 14.5 KB]
Title: Organization: Author(s):
Goals: After reading this case study, readers should
Introduction Who is your organization? What is your expertise? Provide your audience with some background information, such as your expertise. This provides context to help them understand your decisions. (How much should you write? A few sentences to 1 paragraph)
What problem did you address? Who identified the problem? Provide some background on who noticed the problem and how it was reported. Were multiple organizations or people involved in identifying and addressing the problem? This will help the reader understand how and why decisions were made. (1 paragraph)
Case Details Provide more information about the community. What factors affected your decisions? Describe the community. The context, or setting, is very important to readers. What are some of the unique characteristics that affected your decisions? (1 paragraph)
How did you address the problem? Start at the beginning. Summarize what happened, in chronological order. If you know which section of the publication your case study is likely to be put in, you can specify how your actions addressed one or more of the main points of the publication/lesson.
What challenge(s) did you encounter? Address them now if you have not already.
What was the outcome? What were your notable achievements? Explain how your actions or the outcomes satisfy your learning goals for the reader. Be clear about the main point. For example, if you wanted readers to understand how your organization dealt with a major organizational change, include a few sentences that reiterate how you encountered and dealt with the organizational change. (A few sentences to 1 paragraph)
Conclusion Summarize lessons learned. Reiterate your main point(s) for the reader by explaining how your actions, or the outcomes, meet your goals for the reader.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Children's mental health case studies
- Food, health and nutrition
- Mental wellbeing
- Mental health
Explore the experiences of children and families with these interdisciplinary case studies. Designed to help professionals and students explore the strengths and needs of children and their families, each case presents a detailed situation, related research, problem-solving questions and feedback for the user. Use these cases on your own or in classes and training events
Each case study:
- Explores the experiences of a child and family over time.
- Introduces theories, research and practice ideas about children's mental health.
- Shows the needs of a child at specific stages of development.
- Invites users to “try on the hat” of different specific professionals.
By completing a case study participants will:
- Examine the needs of children from an interdisciplinary perspective.
- Recognize the importance of prevention/early intervention in children’s mental health.
- Apply ecological and developmental perspectives to children’s mental health.
- Predict probable outcomes for children based on services they receive.
Case studies prompt users to practice making decisions that are:
- Research-based.
- Practice-based.
- Best to meet a child and family's needs in that moment.
Children’s mental health service delivery systems often face significant challenges.
- Services can be disconnected and hard to access.
- Stigma can prevent people from seeking help.
- Parents, teachers and other direct providers can become overwhelmed with piecing together a system of care that meets the needs of an individual child.
- Professionals can be unaware of the theories and perspectives under which others serving the same family work
- Professionals may face challenges doing interdisciplinary work.
- Limited funding promotes competition between organizations trying to serve families.
These case studies help explore life-like mental health situations and decision-making. Case studies introduce characters with history, relationships and real-life problems. They offer users the opportunity to:
- Examine all these details, as well as pertinent research.
- Make informed decisions about intervention based on the available information.
The case study also allows users to see how preventive decisions can change outcomes later on. At every step, the case content and learning format encourages users to review the research to inform their decisions.
Each case study emphasizes the need to consider a growing child within ecological, developmental, and interdisciplinary frameworks.
- Ecological approaches consider all the levels of influence on a child.
- Developmental approaches recognize that children are constantly growing and developing. They may learn some things before other things.
- Interdisciplinary perspectives recognize that the needs of children will not be met within the perspectives and theories of a single discipline.
There are currently two different case students available. Each case study reflects a set of themes that the child and family experience.
The About Steven case study addresses:
- Adolescent depression.
- School mental health.
- Rural mental health services.
- Social/emotional development.
The Brianna and Tanya case study reflects themes of:
- Infant and early childhood mental health.
- Educational disparities.
- Trauma and toxic stress.
- Financial insecurity.
- Intergenerational issues.
The case studies are designed with many audiences in mind:
Practitioners from a variety of fields. This includes social work, education, nursing, public health, mental health, and others.
Professionals in training, including those attending graduate or undergraduate classes.
The broader community.
Each case is based on the research, theories, practices and perspectives of people in all these areas. The case studies emphasize the importance of considering an interdisciplinary framework. Children’s needs cannot be met within the perspective of a single discipline.
The complex problems children face need solutions that integrate many and diverse ways of knowing. The case studies also help everyone better understand the mental health needs of children. We all have a role to play.
These case has been piloted within:
Graduate and undergraduate courses.
Discipline-specific and interdisciplinary settings.
Professional organizations.
Currently, the case studies are being offered to instructors and their staff and students in graduate and undergraduate level courses. They are designed to supplement existing course curricula.
Instructors have used the case study effectively by:
- Assigning the entire case at one time as homework. This is followed by in-class discussion or a reflective writing assignment relevant to a course.
- Assigning sections of the case throughout the course. Instructors then require students to prepare for in-class discussion pertinent to that section.
- Creating writing, research or presentation assignments based on specific sections of course content.
- Focusing on a specific theme present in the case that is pertinent to the course. Instructors use this as a launching point for deeper study.
- Constructing other in-class creative experiences with the case.
- Collaborating with other instructors to hold interdisciplinary discussions about the case.
To get started with a particular case, visit the related web page and follow the instructions to register. Once you register as an instructor, you will receive information for your co-instructors, teaching assistants and students. Get more information on the following web pages.
- Brianna and Tanya: A case study about infant and early childhood mental health
- About Steven: A children’s mental health case study about depression
Cari Michaels, Extension educator
Reviewed in 2023
© 2024 Regents of the University of Minnesota. All rights reserved. The University of Minnesota is an equal opportunity educator and employer.
- Report Web Disability-Related Issue |
- Privacy Statement |
- Staff intranet
147 Case Studies: Real Stories Of People Overcoming Struggles of Mental Health
At Tracking Happiness, we’re dedicated to helping others around the world overcome struggles of mental health.
In 2022, we published a survey of 5,521 respondents and found:
- 88% of our respondents experienced mental health issues in the past year.
- 25% of people don’t feel comfortable sharing their struggles with anyone, not even their closest friends.
In order to break the stigma that surrounds mental health struggles, we’re looking to share your stories.
Overcoming struggles
They say that everyone you meet is engaged in a great struggle. No matter how well someone manages to hide it, there’s always something to overcome, a struggle to deal with, an obstacle to climb.
And when someone is engaged in a struggle, that person is looking for others to join him. Because we, as human beings, don’t thrive when we feel alone in facing a struggle.
Let’s throw rocks together
Overcoming your struggles is like defeating an angry giant. You try to throw rocks at it, but how much damage is one little rock gonna do?
Tracking Happiness can become your partner in facing this giant. We are on a mission to share all your stories of overcoming mental health struggles. By doing so, we want to help inspire you to overcome the things that you’re struggling with, while also breaking the stigma of mental health.
Which explains the phrase: “Let’s throw rocks together”.
Let’s throw rocks together, and become better at overcoming our struggles collectively. If you’re interested in becoming a part of this and sharing your story, click this link!
Case studies
April 25, 2024
How I’m Seeking Moments of Happiness Despite Struggling With Depression
“The diagnosis I longed for finally arrived, but it didn’t bring the expected empowerment. While it sheds light on my struggles, it also serves as a reminder that this is a part of me that won’t simply vanish. Though mental health can be managed, I know it will always leave its mark. The most challenging part is not always pinpointing why I feel the way I do.”
Struggled with: Depression Negative body image
Helped by: Medication Therapy
April 24, 2024
How Boxing and Therapy Help Me Recover My Identity After Extreme Weight Loss
“When my body changed so drastically and rapidly, it broke my sense of self-identity. About a year into my weight loss, I began to experience early dissociation, depersonalization, and dissociative amnesia. I broke into two people. Me of now and her of before.”
Struggled with: Depression Dissociative amnesia
Helped by: Exercise Self-improvement Therapy
April 18, 2024
How Therapy, Medication and Baking Help Me Navigate Depression and OCD
“I was hospitalized for my eating disorder and my depression several times throughout my college career struggling with the will to live… I was desperate to be “normal” but my brain really got in the way of that.”
Struggled with: Anxiety Depression Eating disorder OCD Suicidal
Helped by: Medication Self-improvement Therapy Treatment
April 16, 2024
How I Found My Self-Worth After Battling Chronic Pain, Anxiety and Panic Attacks
“I remember being floored with a horrible throat infection, and I was just crying. I was done suffering, I couldn’t do it anymore, I was really broken down. That was about 2 years ago now, and it shifted something in my brain. Instead of going down the drain – and keeping that negativity going – it suddenly hit me that I’m the only one responsible for how I feel.”
Struggled with: Anxiety Chronic pain Panic attacks Stress
Helped by: Medication Self-Care Self-improvement Therapy
April 11, 2024
How a Mindset Change Helped Me Break Free From Childhood Trauma and Toxicity
“My mother said she wanted to end it in bloodshed and she waited for him to come home from his late-night meeting. She thought better of it when he was late arriving home. She was overwhelmed with thoughts of her in prison and me in foster care. To say that she made the right decision in achieving the goal of a good life is an answer I struggled to answer for many years.”
Struggled with: Abuse Anxiety Childhood CPTSD Depression
Helped by: Mindfulness Reinventing yourself Self-improvement Therapy
April 9, 2024
Healing From Postpartum Depression With Therapy, Friends & Exercise
“I wasn’t sure how to feel better for a while. People talk about ‘getting help’ but that’s a blanket term and unfortunately it’s not a band-aid you can just put on and suddenly be yourself again. It takes time to find the right therapist, medication if that’s what you decide to do, to find a new rhythm with family, and in my case, I really needed friends locally.”
Struggled with: Postpartum depression
Helped by: Exercise Social support Therapy
April 4, 2024
My Journey from Loneliness and Isolation to Creating an Online Haven for Seniors
“When one is home alone, all day, with nothing to do, nobody to speak with, stuck with their thoughts both good and bad, it’s easy to slip back into a depressive state. Feeling unneeded, unwanted, no happiness, no joy, no reason to get out of bed – just suffering with “the blahs”.”
Struggled with: Depression Loneliness
Helped by: Self-improvement Social support
April 2, 2024
Surviving a Workplace Shooting and Navigating PTSD, Insomnia With Marathons and Prayers
“My symptoms began immediately following a workplace shooting on Saturday, November 28, 2015, and were exasperated due to the activity of the company, the criminals, and the cops. The company treated me as if I were a criminal, the criminals attempted to kill me three additional times, and the cops (Houston Police Department Organized Crime Unit) treated me as if I was a thorn in their flesh.”
Struggled with: Depression Insomnia PTSD Stress
Helped by: Exercise Religion Treatment Volunteering
March 28, 2024
How The Support of Others Helped Me Heal After a Mental Breakdown
“I do not recommend having a breakdown when trying to raise boys. I would cry, eat all the time, and feel like my brain was full of fuzz. I could barely function. There was that day when I got home from taking the kids to school, and thought to myself that if there was a gun in the house, someone else would have had to pick them up from school that day.”
Struggled with: Depression Divorce Stress
Helped by: Journaling Social support Therapy
March 26, 2024
Journaling and Therapy Helped Me After Surviving a Car Accident and a Late Pregnancy Loss
“I vividly remember one day a few months after getting hit by the car when I wondered if my life would ever feel peaceful, pain-free, or joyful again. I was simply getting in and out of the passenger seat of a vehicle, my whole body gripped with pain and stiffness when I experienced a flash of fear that my health would never improve.”
Struggled with: Chronic pain Depression Grief PTSD
Helped by: Journaling Therapy

Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
- Theresa Cerulli, MD
- Tina Matthews-Hayes, DNP, FNP, PMHNP
Custom Around the Practice Video Series
Experts in psychiatry review the case of a 27-year-old woman who presents for evaluation of a complex depressive disorder.

EP: 1 . Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
Ep: 2 . clinical significance of bipolar disorder, ep: 3 . clinical impressions from patient case #1, ep: 4 . diagnosis of bipolar disorder, ep: 5 . treatment options for bipolar disorder, ep: 6 . patient case #2: 47-year-old man with treatment resistant depression (trd), ep: 7 . patient case #2 continued: novel second-generation antipsychotics, ep: 8 . role of telemedicine in bipolar disorder.
Michael E. Thase, MD : Hello and welcome to this Psychiatric Times™ Around the Practice , “Identification and Management of Bipolar Disorder. ”I’m Michael Thase, professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Joining me today are: Dr Gustavo Alva, the medical director of ATP Clinical Research in Costa Mesa, California; Dr Theresa Cerulli, the medical director of Cerulli and Associates in North Andover, Massachusetts; and Dr Tina Matthew-Hayes, a dual-certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.
Today we are going to highlight challenges with identifying bipolar disorder, discuss strategies for optimizing treatment, comment on telehealth utilization, and walk through 2 interesting patient cases. We’ll also involve our audience by using several polling questions, and these results will be shared after the program.
Without further ado, welcome and let’s begin. Here’s our first polling question. What percentage of your patients with bipolar disorder have 1 or more co-occurring psychiatric condition? a. 10%, b. 10%-30%, c. 30%-50%, d. 50%-70%, or e. more than 70%.
Now, here’s our second polling question. What percentage of your referred patients with bipolar disorder were initially misdiagnosed? Would you say a. less than 10%, b. 10%-30%, c. 30%-50%, d. more than 50%, up to 70%, or e. greater than 70%.
We’re going to go ahead to patient case No. 1. This is a 27-year-old woman who’s presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode. It began back in the fall, and she described the episode as occurring right “out of the blue.” Further discussion revealed, however, that she had talked with several confidantes about her problems and that she realized she had been disappointed and frustrated for being passed over unfairly for a promotion at work. She had also been saddened by the unusually early death of her favorite aunt.
Now, our patient has a past history of ADHD [attention-deficit/hyperactivity disorder], which was recognized when she was in middle school and for which she took methylphenidate for adolescence and much of her young adult life. As she was wrapping up with college, she decided that this medication sometimes disrupted her sleep and gave her an irritable edge, and decided that she might be better off not taking it. Her medical history was unremarkable. She is taking escitalopram at the time of our initial evaluation, and the dose was just reduced by her PCP [primary care physician]from 20 mg to 10 mg because she subjectively thought the medicine might actually be making her worse.
On the day of her first visit, we get a PHQ-9 [9-item Patient Health Questionnaire]. The score is 16, which is in the moderate depression range. She filled out the MDQ [Mood Disorder Questionnaire] and scored a whopping 10, which is not the highest possible score but it is higher than 95% of people who take this inventory.
At the time of our interview, our patient tells us that her No. 1 symptom is her low mood and her ease to tears. In fact, she was tearful during the interview. She also reports that her normal trouble concentrating, attributable to the ADHD, is actually substantially worse. Additionally, in contrast to her usual diet, she has a tendency to overeat and may have gained as much as 5 kg over the last 4 months. She reports an irregular sleep cycle and tends to have periods of hypersomnolence, especially on the weekends, and then days on end where she might sleep only 4 hours a night despite feeling tired.
Upon examination, her mood is positively reactive, and by that I mean she can lift her spirits in conversation, show some preserved sense of humor, and does not appear as severely depressed as she subjectively describes. Furthermore, she would say that in contrast to other times in her life when she’s been depressed, that she’s actually had no loss of libido, and in fact her libido might even be somewhat increased. Over the last month or so, she’s had several uncharacteristic casual hook-ups.
So the differential diagnosis for this patient included major depressive disorder, recurrent unipolar with mixed features, versus bipolar II disorder, with an antecedent history of ADHD. I think the high MDQ score and recurrent threshold level of mixed symptoms within a diagnosable depressive episode certainly increase the chances that this patient’s illness should be thought of on the bipolar spectrum. Of course, this formulation is strengthened by the fact that she has an early age of onset of recurrent depression, that her current episode, despite having mixed features, has reverse vegetative features as well. We also have the observation that antidepressant therapy has seemed to make her condition worse, not better.
Transcript Edited for Clarity
Dr. Thase is a professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Dr. Alva is the medical director of ATP Clinical Research in Costa Mesa, California.
Dr. Cerulli is the medical director of Cerulli and Associates in Andover, Massachusetts.
Dr. Tina Matthew-Hayes is a dual certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.

The Week in Review: April 1-5

Blue Light, Depression, and Bipolar Disorder

An Update on Bipolar I Disorder

Four Myths About Lamotrigine

Recap: Mood Disorders 2024
Evidence-Based Novel Therapies for Bipolar Depression: Top 5 Takeaways
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

A sample case study: Mrs Brown
On this page, social work report, social work report: background, social work report: social history, social work report: current function, social work report: the current risks, social work report: attempts to trial least restrictive options, social work report: recommendation, medical report, medical report: background information, medical report: financial and legal affairs, medical report: general living circumstances.
This is a fictitious case that has been designed for educative purposes.
Mrs Beryl Brown URN102030 20 Hume Road, Melbourne, 3000 DOB: 01/11/33
Date of application: 20 August 2019
Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke, which has left her with moderate weakness in her left arm and leg. A diagnosis of vascular dementia was also made, which is overlaid on a pre-existing diagnosis of Alzheimer’s disease (2016). Please refer to the attached medical report for further details.
I understand that Mrs Brown has been residing in her own home, a two-story terrace house in Melbourne, for almost 60 years. She has lived alone since her husband died two years ago following a cardiac arrest. She has two daughters. The youngest daughter Jean has lived with her for the past year, after she lost her job. The eldest daughter Catherine lives on the Gold Coast with her family. Mrs Brown is a retired school teacher and she and both daughters describe her as a very private woman who has never enjoyed having visitors in her home. Mrs Brown took much encouragement to accept cleaning and shopping assistance once a week after her most recent admission; however, she does not agree to increase service provision. Jean has Enduring Power of Attorney (EPOA) paperwork that indicates that Mrs Brown appointed her under an EPOA two years ago. She does not appear to have appointed a medical treatment decision maker or any other decision-supporter.
I also understand from conversations with her daughters that Jean and Mrs Brown have always been very close and that there is a history of long-standing conflict between Catherine and Jean. This was exacerbated by the death of their father. Both daughters state they understand the impact of the stroke on their mother’s physical and cognitive functioning, but they do not agree on a discharge destination. Mrs Brown lacks insight into her care needs and says she will be fine once she gets back into her own home. Repeated attempts to discuss options with all parties in the same room have not resulted in a decision that is agreeable to all parties.
Mrs Brown has a history of Alzheimer’s disease; type II diabetes – insulin dependent; hypertension; high cholesterol and osteoarthritis. She has had two recent admissions to hospital for a urinary tract infection and a fall in the context of low blood sugars. She is currently requiring one to two people to assist her into and out of bed and one person with managing tasks associated with post-toilet hygiene. She can walk slowly for short distances with a four-wheel frame with one person to supervise. She benefits from prompting to use her frame; she needs someone to cut her food and to set her up to eat and drink regularly and to manage her medication routine. She requires one person to assist her to manage her insulin twice daily.
The team believe that Mrs Brown’s capacity for functional improvement has plateaued in the last ten days. They recommend that it is in her best interests to be discharged to a residential care setting due to her need for one to two people to provide assistance with the core tasks associated with daily living. Mrs Brown is adamant that she wants to return home to live with Jean who she states can look after her. Jean, who has a history of chronic back pain, has required several admissions to hospital over the past five years, and states she wants to be able to care for her mother at home. Jean states she is reluctant to agree to extra services as her mother would not want this. Her sister Catherine is concerned that Jean has not been coping and states that given this is the third admission to hospital in a period of few months, believes it is now time for her mother to enter residential care. Catherine states that she is very opposed to her mother being discharged home.
Mrs Brown is at high risk of experiencing falls. She has reduced awareness of the left side of her body and her ability to plan and process information has been affected by her stroke. She is now requiring one to two people to assist with all her tasks of daily living and she lacks insight into these deficits. Mrs Brown is also at risk of further significant functional decline which may exacerbate Jean’s back pain. Jean has stated she is very worried about where she will live if her mother is to enter residential care.
We have convened two family meetings with Mrs Brown, both her daughters and several members of the multi-disciplinary team. The outcome of the first meeting saw all parties agree for the ward to provide personalised carer training to Jean with the aim of trialling a discharge home. During this training Jean reported significant pain when transferring her mother from the bed and stated she would prefer to leave her mother in bed until she was well enough to get out with less support.
The team provided education to both Jean and Catherine about the progressive impact of their mother’s multiple conditions on her functioning. The occupational therapist completed a home visit and recommended that the downstairs shower be modified so that a commode can be placed in it safely and the existing dining room be converted into a bedroom for Mrs Brown. Mrs Brown stated she would not pay for these modifications and Jean stated she did not wish to go against her mother’s wishes. The team encouraged Mrs Brown to consider developing a back-up plan and explore residential care options close to her home so that Jean could visit often if the discharge home failed. Mrs Brown and Jean refused to consent to proceed with an Aged Care Assessment that would enable Catherine to waitlist her mother’s name at suitable aged care facilities. We proceeded with organising a trial overnight visit. Unfortunately, this visit was not successful as Jean and Catherine, who remained in Melbourne to provide assistance, found it very difficult to provide care without the use of an accessible bathroom. Mrs Brown remains adamant that she will remain at home. The team is continuing to work with the family to maximise Mrs Brown’s independence, but they believe that it is unlikely this will improve. I have spent time with Jean to explore her adjustment to the situation, and provided her with information on community support services and residential care services. I have provided her with information on the Transition Care Program which can assist families to work through all the logistics. I have provided her with more information on where she could access further counselling to explore her concerns. I have sought advice on the process and legislative requirements from the Office of the Public Advocate’s Advice Service. I discussed this process with the treating team and we decided that it was time to lodge an application for guardianship to VCAT.
The treating team believe they have exhausted all least restrictive alternatives and that a guardianship order is required to make a decision on Mrs Brown’s discharge destination and access to services. The team recommend that the Public Advocate be appointed as Mrs Brown’s guardian of last resort. We believe that this is the most suitable arrangement as her daughters are not in agreement about what is in their mother’s best interests. We also believe that there is a potential conflict of interest as Jean has expressed significant concern that her mother’s relocation to residential care will have an impact on her own living arrangements.
Mrs Brown’s medical history includes Alzheimer’s disease; type II diabetes; hypertension; high cholesterol and osteoarthritis. She was admitted to Hume Hospital on 3 March 2019 following a stroke that resulted in moderate left arm and leg weakness. This admission was the third hospital admission in the past year. Other admissions have been for a urinary tract infection, and a fall in the context hypoglycaemia (low blood sugars), both of which were complicated by episodes of delirium.
She was transferred to the subacute site under my care, a week post her admission, for slow-stream rehabilitation, cognitive assessment and discharge planning.
Mrs Brown was diagnosed with Alzheimer’s disease by Dr Joanne Winters, Geriatrician, in April 2016. At that time, Mrs Brown scored 21/30 on the Standardised Mini-Mental State Examination (SMMSE). During this admission, Mrs Brown scored 15/30. I have undertaken cognitive assessment and agree with the diagnosis; further cognitive decline has occurred in the context of the recent stroke. There are global cognitive deficits, but primarily affecting memory, attention and executive function (planning, problem solving, mental flexibility and abstract reasoning). The most recent CT-Brain scan shows generalised atrophy along with evidence of the new stroke affecting the right frontal lobe. My assessments suggest moderate to severe mixed Alzheimer’s and vascular dementia.
While able to recall some key aspects of her financial affairs, including the general monetary value of her pension and regular expenses, Mrs Brown was unable to account for recent expenditure (for repairs to her home) or provide an estimate of its value, and had difficulty describing her investments. In addition, I consider that she would be unable to make complex financial decisions due to her level of cognitive impairment. Accordingly, I am of the view that Mrs Brown now lacks capacity to make financial decisions.
Mrs Brown states that she previously made an Enduring Power of Attorney (EPOA) but could no longer recall aspects of the EPOA, such as when it would commence and the nature of the attorney’s powers. Moreover, she confused the EPOA with her will. Her understanding of these matters did not improve with education, and therefore I consider that she no longer has capacity to execute or revoke an EPOA.
Mrs Brown acknowledges that she needs some assistance but lacks insight into the type of assistance that she requires, apart from home help for cleaning and shopping. She does not appreciate her risk of falling. She is unable to get in and out of bed without at least one person assisting her. She frequently forgets to use her gait aid when mobilising and is not able to describe how she would seek help in the event of falling. She is not able to identify or describe how she would manage her blood sugar levels, and this has not improved with education. Accordingly, I consider that she lacks capacity to make decisions about accommodation arrangements and services.
Mrs Brown does not agree with the treating team’s recommendation to move into residential care and maintains her preference to return home. This is in spite of a failed overnight trial at home with both her daughters assisting her. Unfortunately, she was unable to get out of bed to get to the toilet and required two people to assist her to do so in the morning. In light of these matters, and in the context of family disagreement regarding the matter, the team recommends that the Office of the Public Advocate be appointed as a guardian of last resort.
Reviewed 22 July 2022
- Hospitals & health services
- Public hospitals in Victoria
- Patient care
- Ambulance and patient transport
- Non-emergency patient transport
- Non-emergency patient transport review
- NEPT legislation and clinical practice protocols
- Non-emergency patient transport licensing
- NEPT licensing fees
- NEPT services information and guidance
- First Aid Services
- First aid licences
- First aid services information and guidance
- First aid service fees
- Victorian State Trauma System
- Acute medicine
- Emergency care
- Surgical services
- Better at Home
- Critical care
- Hospital in the Home
- Virtual care (Telehealth)
- Perinatal and reproductive services
- Rehabilitation and complex care
- Renal health
- Renal services in Victoria
- Funding for renal services
- Different approaches to haemodialysis
- Specialist clinics
- Access to non-admitted services
- Minimum referral information
- Communication toolkit
- Integrated care
- HealthLinks: Chronic Care
- Community Health Integrated Program (CHIP) guidelines
- Service coordination in Victoria
- Victorian integrated care online resources
- Specialist clinics programs
- Specialist clinics reform
- Specialty diagnostics, therapeutics and programs
- Older people in hospital
- End of life and palliative care in Victoria
- Legislation and reform initiatives
- Quality, safety and service improvement
- Planned surgery recovery and reform program
- Digital Health
- Roadmap and Maturity Model
- Standards and guidelines
- Policies and frameworks
- Health Information Sharing Legislation Reform
- My Health Record
- Public hospital accreditation in Victoria
- Credentialing for senior medical staff in Victoria
- Clinical risk management
- Preventing infections in health services
- Healthy choices
- Victorian Perinatal Data Collection
- Rural health
- Improving Access to Primary Care in Rural and Remote Areas Initiative
- Rural x-ray services
- Rural health regions and locations
- Rural and regional medical director role
- Victorian Patient Transport Assistance Scheme
- Rural and isolated practice registered nurses
- Urgent care in regional and rural Victoria
- Private health service establishments
- Private hospitals
- Day procedure centres
- Mobile health services
- Fees for private health service establishments in Victoria
- Design resources for private health service establishments
- Professional standards in private health service establishments
- Legislation updates for private health service establishments
- Complaints about private health service establishments
- Cosmetic procedures
- Guideline for providers of liposuction
- Private hospital funding agreement
- Boards and governance
- About health service boards in Victoria
- Information and education
- Education resources for boards
- Sector leadership
- Data, reporting and analytics
- Health data standards and systems
- Funding, performance and accountability
- Statements of Priorities
- Performance monitoring framework
- Integrity governance framework and assessment tool
- Pricing and funding framework
- Patient fees and charges
- Fees and charges for admitted patients
- Non-admitted patients - fees and charges
- Other services
- Planning and infrastructure
- Sustainability in Healthcare
- Medical equipment asset management framework
- Health system design, service and infrastructure planning
- Complementary service and locality planning
- Primary & community health
- Primary care
- Community pharmacist pilot
- EOI - Victorian Community Pharmacist Statewide Pilot
- Victorian Community Pharmacist Statewide Pilot – Resources for pharmacists
- Emergency Response Planning Tool
- Working with general practice
- Victorian Supercare Pharmacies
- NURSE-ON-CALL
- Priority Primary Care Centres
- Local Public Health Units
- Community health
- Community health services
- Community health pride
- Registration and governance of community health centres
- Community Health Directory
- Community Health Program in Victoria
- Community health population groups
- Dental health
- Access to public dental care services
- Victoria's public dental care fees
- Victoria's public dental care waiting list
- Dental health for SRS residents
- Dental health program reporting
- Smile Squad school dental program
- Maternal and Child Health Service
- Nursery Equipment Program
- Maternal and Child Health Service Framework
- Maternal and Child Health Service resources
- Child Development Information System
- Early parenting centres
- Maternal Child and Health Reporting, Funding and Data
- Baby bundle
- Sleep and settling
- Maternal and Child Health Workforce professional development
- Aboriginal Maternal and Child Health
- Public Dental and Community Health Program funding model review
- Public health
- Women's Health and Wellbeing Program
- Inquiry into Women's Pain
- Inquiry into Women's Pain submissions
- Support groups and programs
- About the program
- Victorian Women's Health Advisory Council
- Cemeteries and crematoria
- Cemetery trust member appointments
- Cemetery search
- Cemeteries and crematoria complaints
- Exhumations
- Governance and finance
- Cemetery grants
- Interments and memorials
- Land and development
- Legislation governing Victorian cemeteries and crematoria
- Cemeteries and crematoria publications
- Repatriations
- Rights of interment
- Medicines and Poisons Regulation
- Patient Schedule 8 treatment permits
- Schedule 8 MDMA and Schedule 8 psilocybine
- Schedule 9 permits for clinical trials
- Documents and forms to print or download
- Legislation and Approvals
- Frequently Asked Questions - Medicines and Poisons Regulation
- Health practitioners
- Licences and permits to possess (& possibly supply) scheduled substances
- Medicinal cannabis
- Pharmacotherapy (opioid replacement therapy)
- Recent updates
- Environmental health
- Improving childhood asthma management in Melbourne's inner west
- Climate and weather, and public health
- Environmental health in the community
- Environmental health in the home
- Environmental health professionals
- Face masks for environmental hazards
- Human health risk assessments
- Lead and human health
- Per- and poly-fluoroalkyl substances (PFAS)
- Pesticide use and pest control
- Food safety
- Information for community groups selling food to raise funds
- Food businesses
- Food safety information for consumers
- Food regulation in Victoria
- Food safety library
- Food allergens
- Introducing Standard 3.2.2A: Food safety management tools
- Immunisation
- Respiratory syncytial virus (RSV) immunisation
- Seasonal influenza vaccine
- Immunisation schedule and vaccine eligibility criteria
- Ordering vaccine
- Immunisers in Victoria
- Immunisation provider information
- Cold chain management
- Adverse events following immunisation reporting
- Vaccine error management
- Vaccination for infants and children
- Vaccination for adolescents
- Vaccination program for adults
- Vaccination for special-risk groups
- Immunisation resources order form
- Victorian coverage rates for Victoria
- Infectious diseases guidelines & advice
- Infection control guidelines
- Disease information and advice
- Advice to the cruise industry: reporting infections
- Notifiable infectious diseases, conditions and micro-organisms
- Notification procedures for infectious diseases
- Infectious diseases surveillance in Victoria
- Germicidal ultraviolet light
- Protecting patient privacy in Victoria
- Population health systems
- Evidence and evaluation
- Health promotion
- Health status of Victorians
- Municipal public health and wellbeing planning
- Population screening
- Cancer screening
- Conditions not screened
- Improving outcomes in under-screened groups
- Infant hearing screening
- Newborn bloodspot screening
- Prenatal screening
- Screening registers
- Preventive health
- Type 2 diabetes and cardiovascular disease prevention
- Eye health promotion
- Injury prevention
- Healthy eating
- Oral health promotion
- Physical activity
- Sexual health
- Sex worker health
- Decriminalisation of sex work
- Automatic mutual recognition
- Domestic smoke detectors
- Lasers, IPL and LED devices for cosmetic treatments and beauty therapy
- Victoria's regulatory framework for radiation
- Radiation newsletter
- Tobacco reforms
- Tobacco reform legislation and regulations
- E-cigarettes and vaping
- Quitting smoking and vaping
- Smoke-free and vape-free areas
- Building entrances
- Children's indoor play centres
- Public hospitals and health centres
- Children's recreational areas
- Playground equipment
- Skate parks
- Swimming pools
- Under-age sporting events
- Enclosed workplaces
- Government buildings
- Learning environments
- Outdoor dining
- Outdoor drinking areas
- Patrolled beaches
- Train platforms and bus and tram shelters
- Under-age music or dance events
- Tobacco and e-cigarette retailers
- Making a report or complaint
- Resources and factsheets
- Alternative water supplies
- Aquatic facilities
- Blue-green algae (cyanobacteria)
- Drinking water in Victoria
- Legionella risk management
- Private drinking water
- Recreational water use and possible health risks
- Water fluoridation
- Chief Health Officer
- About the Chief Health Officer
- Chief Health Officer publications
- Health alerts and advisories
- Mental health
- Mental Health and Wellbeing Act 2022
- Mental Health and Wellbeing Act 2022 Handbook
- Community information
- Mental Health and Wellbeing Act 2022 in your language
- About Victoria's mental health services
- Area-based services
- Statewide and specialist mental health services
- Mental Health Community Support Services
- Support and intervention services
- Language services - when to use them
- Access to mental health services across areas
- Transport for people in mental health services
- Practice and service quality
- Medical Treatment Planning and Decisions Act
- Service quality
- Specialist responses
- Mental health and wellbeing reform
- Reform activity updates
- Priority areas
- Latest news
- Working with consumers and carers
- Consumer and carer engagement
- Consumer and Carer Experience Surveys
- Family support and crisis plans
- Consumer and carer financial support
- Supporting children whose parents have a mental illness
- Supporting parents with a mental illness
- Prevention and promotion
- Early intervention in mental illness
- Mental health promotion in Victoria
- Suicide prevention in Victoria
- Priorities and transformation
- Supporting the social and emotional wellbeing of Aboriginal and Torres Strait Islander Victorians
- National mental health strategy
- Rights and advocacy
- Making a complaint about a mental health service
- Chief Psychiatrist
- About the Chief Psychiatrist
- Principles in the Mental Health and Wellbeing Act and the Chief Psychiatrist's guidelines
- Obligations under the Mental Health and Wellbeing Act 2022
- Reporting a failure to comply with the Mental Health and Wellbeing Act 2022
- Governance and committees
- Reporting obligations for clinical mental health and wellbeing services
- Mental health and wellbeing support
- Making a complaint and seeking advocacy
- Second psychiatric opinion and process of review by Chief Psychiatrist
- Office of the Chief Psychiatrist's reform activities and news
- Oversight of forensic mental health and wellbeing services
- Resources and reports
- Chief psychiatrist guidelines
- Chief Mental Health Nurse
- About Victoria's Chief Mental Health Nurse
- Best practice
- Reducing restrictive interventions
- Research and reporting
- Mental health performance reports
- Reporting requirements and business rules for clinical mental health services
- Alcohol & drugs
- Alcohol and other drug treatment services
- Overview of Victoria's alcohol and drug treatment system
- Pathways into alcohol and other drugs treatment
- Prevention and harm reduction
- Medically supervised injecting room
- Victoria's Take-Home Naloxone Program
- Community-based AOD treatment services in Victoria
- Residential treatment services
- Mildura statewide alcohol and drug residential treatment service
- Drug rehabilitation plan
- Hospital-based services
- Forensic services
- Pharmacotherapy treatment
- Services for Aboriginal people
- Services for young people
- Statewide and specialist services
- Compulsory treatment
- Family and peer support
- Public intoxication reform
- New public intoxication response services
- Policy, research and legislation
- Alcohol and drug research and data
- Legislation governing alcohol and other drug treatment
- Alcohol and other drug service standards and guidelines
- Alcohol and other drug client charter and resources
- Alcohol and other drug treatment principles
- Service quality and accreditation
- Alcohol and other drug program guidelines
- Maintenance pharmacotherapy
- Drink and Drug Driving Behaviour Change Program
- Alcohol and Other Drug Residential Rehabilitation Facility Design Guidelines
- Specialist Family Violence Advisor capacity building program in mental health and alcohol and other drug services - Victoria
- Alcohol and other drug workforce
- Learning and development
- Alcohol and other drug workforce Minimum Qualification Strategy
- Workforce data and planning
- Funding and reporting for alcohol and other drug services
- Funding of alcohol and other drugs services in Victoria
- Reporting requirements and business rules for alcohol and other drug services
- Drug alerts
- 25C-NBOMe and 4-FA sold as '2C-B'
- Novel stimulants sold as MDMA, cocaine or speed
- Protonitazene sold as ketamine
- High potency benzodiazepine tablets
- MDMA adulterated with PMMA
- 25B-NBOH sold as powdered 'LSD'
- Green 'UPS' pills containing N-ethylpentylone (no MDMA)
- N-ethylpentylone in cocaine
- Ageing & aged care
- Supporting independent living
- Low cost accommodation support programs
- Personal Alert Victoria
- Dementia services
- Victorian Aids and Equipment Program
- Residential aged care services
- Public sector residential aged care services
- Safety and quality in public sector residential aged care
- Physical and social environments
- Emergency preparedness in residential aged care services
- My Aged Care assessment services
- Home and Community Care Program for Younger People
- HACC data reporting
- HACC PYP fees policy and schedule of fees
- Wellbeing and participation
- Age-friendly Victoria
- Healthy ageing
- Seniors participation
- Dementia-friendly environments
- Designing for people with dementia
- Maintaining personal identity
- Personal enjoyment
- Interior design
- Dining areas, kitchens and eating
- Bedrooms and privacy
- Gardens and outdoor spaces
- Assistive technology
- Staff education and support
- Strategies, checklists and tools
- Our Strategic Plan 2023-27
- Our organisation
- Our secretary
- Leadership charter
- Our services
- Our vision and values
- Specialist offices
- Senior officers in health
- Human Research Ethics Committee (HREC)
- Gifts, benefits and hospitality policy
- Information Asset Register
- Health legislation
- Health legislation overview
- Health Complaints legislation
- Health Records Act
- Human Tissue Act 1982
- Public Health and Wellbeing Act 2008
- Voluntary Assisted Dying Act
- Victoria's pandemic management framework
- Independent Pandemic Management Advisory Committee
- Pandemic Order Register
- Our ministers
- Our role in emergencies
- State Health Emergency Response Arrangements
- Emergency type
- Department's responsibilities in emergencies
- Health services’ responsibilities in emergencies
- Aboriginal employment
- Current vacancies
- Employment programs for students and graduates
- Rise program
- Inclusion and diversity at the Department of Health
- Health workforce
- Working in health
- Information sharing and MARAM
- Child Safe Standards
- Regulatory functions
- Reviews of decisions
- Victorian Public Healthcare Awards
- Aboriginal healthcare workers
- Mental health workforce
- Lived and living experience workforces
- Engaging with lived and living experience workforces
- Our workforce, our future
- Nursing and midwifery
- Free nursing and midwifery study
- Additional funding for nursing and midwifery positions
- Becoming a nurse or midwife
- Undergraduate nursing and midwifery scholarships
- Undergraduate student employment programs
- Nursing and midwifery graduates
- Nursing and midwifery graduate sign-on bonus
- Working as a nurse or midwife
- Enrolled nurse to registered nurse transition scholarships
- Support for new nurse practitioners
- Postgraduate scholarships for nurses and midwives
- Nurse practitioners
- Returning to nursing or midwifery
- Refresher pathway for nurses and midwives
- Re-entry pathway scholarships for nurses and midwives
- Nursing and midwifery - legislation and regulation
- Nursing and midwifery program - health sector
- Allied health workforce
- Education and training
- Enterprise agreements
- Worker health and wellbeing
- Working with us
- Grants and programs
- Freedom of Information
- Part II - Information Statements
- Procurement policies
- Protective markings
- Health and medical research
- Sponsorship application information
- Publications
- Annual reports
- Fact sheets
- Strategies, plans and charters
- Policies, standards and guidelines
- Research and reports
- Forms and templates
- Communities
- Designing for Diversity
- Vulnerable children
- Vulnerable children - responsibilities of health professionals
- Identifying and responding to children at risk
- Older people
- Aboriginal health
- Improving health for Victorians from culturally and linguistically diverse backgrounds
- Asylum seeker and refugee health in Victoria
- News and media hub
- Media releases
- Health alerts
- Feedback and complaints
- Make a payment
- Fees, charges and penalties subject to automatic indexation
- Our campaigns
Share this page
- Facebook , opens a new window
- X (formerly Twitter) , opens a new window
- LinkedIn , opens a new window
- Warning Signs and Symptoms
- Mental Health Conditions
- Common with Mental Illness
- Mental Health By the Numbers
- Individuals with Mental Illness
- Family Members and Caregivers
- Kids, Teens and Young Adults
- Veterans & Active Duty
- Identity and Cultural Dimensions
- Frontline Professionals
- Mental Health Education
- Support Groups
- NAMI HelpLine
- Publications & Reports
- Podcasts and Webinars
- Video Resource Library
- Justice Library
- Find Your Local NAMI
- Find a NAMIWalks
- Attend the NAMI National Convention
- Fundraise Your Way
- Create a Memorial Fundraiser
- Pledge to Be StigmaFree
- Awareness Events
- Share Your Story
- Partner with Us
- Advocate for Change
- Policy Priorities
- NAMI Advocacy Actions
- Policy Platform
- Crisis Intervention
- State Fact Sheets
- Public Policy Reports
- About Mental Illness
Types of Mental Health Professionals
Many types of mental health care professionals can help you achieve your recovery goals. These professionals work in inpatient facilities, such as general hospitals and psychiatric facilities, and outpatient facilities, such as community mental health clinics, schools and private practices.
Health care professional job titles and specialties can vary by state. The descriptions below give an overview of what to look for and what credentials to expect from a mental health professional. Finding the right professional is easier when you understand the different areas of expertise and training.
The NAMI HelpLine can provide information on how to find various mental health professionals and resources in your area. Please note that we are unable to provide specific recommendations to individual providers as we are unable to speak to the quality of their care.
Assessment And Therapy
Therapists can help someone better understand and cope with thoughts, feelings and behaviors. They can also offer guidance and help improve a person’s ability to achieve life goals. These mental health professionals may also help assess and diagnosis mental health conditions.
Psychologists
Psychologists hold a doctoral degree in clinical psychology or another specialty such as counseling or education. They are trained to evaluate a person’s mental health using clinical interviews, psychological evaluations and testing. They can make diagnoses and provide individual and group therapy. Some may have training in specific forms of therapy like cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT) and other behavioral therapy interventions.
Degree requirements: Doctor of Philosophy (Ph.D.) in a field of psychology or Doctor of Psychology (Psy.D.). Licensure & credentials: Psychologists are licensed by licensure boards in each state.
Counselors, Clinicians, Therapists
These masters-level health care professionals are trained to evaluate a person’s mental health and use therapeutic techniques based on specific training programs. They operate under a variety of job titles—including counselor, clinician, therapist or something else—based on the treatment setting. Working with one of these mental health professionals can lead not only to symptom reduction but to better ways of thinking, feeling and living.
Degree requirements: master’s degree (M.S. or M.A.) in a mental health-related field such as psychology, counseling psychology, marriage or family therapy, among others. Licensure & Certification: Varies by specialty and state. Examples of licensure include:
- LPC, Licensed Professional Counselor
- LMFT, Licensed Marriage and Family Therapist
- LCADAC, Licensed Clinical Alcohol & Drug Abuse Counselor
Clinical Social Workers
Clinical social workers are trained to evaluate a person’s mental health and use therapeutic techniques based on specific training programs. They are also trained in case management and advocacy services.
Degree requirements: master’s degree in social work (MSW). Licensure & credentials: Examples of licensure include:
- LICSW, Licensed Independent Social Workers
- LCSW, Licensed Clinical Social Workers
- ACSW, Academy of Certified Social Workers
Prescribe And Monitor Medication
The following health care professionals can prescribe medication . They may also offer assessments, diagnoses and therapy.
Psychiatrists
Psychiatrists are licensed medical doctors who have completed psychiatric training. They can diagnose mental health conditions, prescribe and monitor medications and provide therapy. Some have completed additional training in child and adolescent mental health, substance use disorders or geriatric psychiatry.
Degree requirements: Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO), plus completion of residency training in psychiatry. Licensure & credentials: Licensed physician in the state where they are practicing; may also be designated as a Board Certified Psychiatrist by the Board of Neurology and Psychiatry.
Psychiatric Or Mental Health Nurse Practitioners
Psychiatric or mental health nurse practitioners can provide assessment, diagnosis and therapy for mental health conditions or substance use disorders. In some states, they are also qualified to prescribe and monitor medications. Requirements also vary by state as to the degree of supervision necessary by a licensed psychiatrist.
Degree requirements: Master of Science (MS) or Doctor of Philosophy (Ph.D.) in nursing with specialized focus on psychiatry. Licensure & credentials: Licensed nurse in the state where they are practicing. Examples of credentials include, but are not limited to:
- NCLEX, National Council Licensure Examination
- PMHNP-BC, Board Certification in psychiatric nursing through the American Academy of Nurses Credentialing Center
Primary Care Physicians
Primary care physicians and pediatricians can prescribe medication, but you might consider visiting someone who specializes in mental health care. Primary care and mental health professionals should work together to determine an individual’s best treatment plan.
Degree requirements: Doctor of Medicine (M.D.) or Doctor of Osteopathic Medicine (DO). Licensure & credentials: Licensed physician in the state where they are practicing.
Family Nurse Practitioners
Family nurse practitioners (FNP) can provide general medical services like those of a primary care physician, based on each state’s laws. Like primary care physicians, they can prescribe medication, but you might consider visiting someone who specializes in mental health care. Family nurse practitioners and mental health professionals should work together to determine an individual’s best treatment plan.
Degree requirements: Master of Science (M.S.) or Doctor of Philosophy (Ph.D.) in nursing. Licensure & credentials: Licensed nurse in the state where they are practicing. Examples of credentials include:
- FNP-BC, Family Nurse Practitioner Board Certified
Psychiatric Pharmacists
Psychiatrist pharmacists are advanced-practice pharmacists who specialize in mental health care. They can prescribe or recommend appropriate medications if allowed in their state and practice setting. They are skilled at medication management—meaning they evaluate responses and modify treatment, manage medication reactions and drug interactions, and provide education about medications. Many have completed additional training in child/adolescent psychiatry, substance use disorders or geriatric psychiatry.
Degree requirements: Doctor of Pharmacy (PharmD). Completion of residency training in psychiatric pharmacy is not required, but is common. Licensure & credentials: Licensed pharmacist in the state where they practice; may also be designated a Board Certified Psychiatric Pharmacist by the Board of Pharmacy Specialties.
Other Professionals You May Encounter
Certified peer specialists.
These specialists have lived experience with a mental health condition or substance use disorder. They are often trained, certified and prepared to assist with recovery by helping a person set goals and develop strengths. They provide support, mentoring and guidance.
Social Workers
Social workers (B.A. or B.S.) provide case management, inpatient discharge planning services, placement services and other services to support healthy living.
Pastoral Counselors
Pastoral counselors are clergy members with training in clinical pastoral education. They are trained to diagnose and provide counseling. Pastoral counselors can have equivalents to a doctorate in counseling.
Updated April 2020

Know the warning signs of mental illness

Learn more about common mental health conditions
NAMI HelpLine is available M-F, 10 a.m. – 10 p.m. ET. Call 800-950-6264 , text “helpline” to 62640 , or chat online. In a crisis, call or text 988 (24/7).
Evidence-based Approaches to Support Student Mental Health
- Andrea Feldman
- 24 April 2024
The college years throw a lot of new challenges at us. Maybe you’re the first in your family to go to college. You’re developing a new sense of independence. Figuring out how to live with roommates. Dealing with new financial responsibilities and academic pressures.
That’s a lot all by itself — but as Associate Professor Sam Rosenthal noted during her recent Health Equity lecture outlining the behavioral health of college-age students, a staggering 75% of mental health disorders are established by the mid-twenties. That means that the 18-25 cohort exhibits the highest rates of anxiety and depressive symptoms, and they’re also extremely vulnerable to developing parallel addictive behaviors.
“Those with social support reduce their risk of insomnia by 33%, their risk of anxiety by 47% and their risk of depression by 50%. That’s dramatic.”
But the data is only one side of the story, and Rosenthal prefaced her talk by noting, “I do want you to know we’re going to get to a positive note of the solutions by the end.” And it may not surprise you to learn that community-building — strengthening our real-world bonds to others — plays a crucial role in improving our individual mental health. (Put down that phone, while you’re at it.)
A Career Built on Studying Behavioral Health
Rosenthal has built an impressive career on her research into the multi-factor forces driving mental-health trends in young adults.
In addition to teaching and serving as the director of JWU’s Center for Student Research and Interdisciplinary Collaboration, she serves as an evaluator for the Rhode Island Department of Health and as the lead epidemiologist for the State Epidemiological Outcomes Workgroup (SEOW). Under the aegis of SEOW, she administers the RI Young Adult Survey (RIYAS), which focuses on the behavioral health of 18-25-year-olds.
Assessing the Pandemic Spike
Depression rates among young adults have doubled in the past 10 years. But the pandemic sent these rates soaring — Rosenthal calls the spike “extreme” — due to a polycrisis of factors, including social isolation, disrupted academic studies, and unprecedented loss. During the 2020-21 academic year, noted Rosenthal, 60% of college-age students reported at least one mental health disorder, and 75% experienced psychological distress. 1 in 5 young adults in Rhode Island reported losing a loved one to Covid-19.
Once you start taking into account the social upheaval of recent years — from gun violence to racial discrimination, climate change anxiety and political turmoil — and you have a massive amount of collective trauma having a ripple effect on already fragile mental health states.
Rosenthal provided a top-level overview of two recent studies. The Healthy Mind study surveyed more than 76,000 students from 400 institutions during the 2022-23 academic year. In October 2022, Rosenthal and her co-researchers used an NIH grant to survey 586 JWU students assessing their levels of depression, anxiety, insomnia and social support.
While the Healthy Mind study clocked depression rates at 41%, the JWU case study reported 53% — that’s “higher than what we saw in the national study, but actually comparable to what we saw in the Rhode Island state study,” explained Rosenthal. “And also we have a huge representation of sexual gender minority students, which is likely to be driving some of these higher rates for us as well.” (The JWU study demographics broke down as 15.1% cisgender male, 47.4% cisgender female and 37.5% sexual or gender minority.)
So, what are the solutions for combatting these numbers? For Rosenthal, who has done multiple studies correlating social media use and depression, building up social support networks is “critically important”: “Those with social support reduce their risk of insomnia by 33%, their risk of anxiety by 47% and their risk of depression by 50%. That’s dramatic.”
“Gratitude is really powerful. I often tell my students to break up anxiety with gratitude.”
Mindfulness, Quiet Hours & Other Mental Health Boosts
Rosenthal opened the conversation to students and faculty in the audience to share their ideas for boosting our community connections and strengthening overall well-being.
Sarah and Jasmine, two undergraduate students in the Public Health program , shared how much JWU’s 3-credit Mindfulness for Health & Wellbeing class helped them. (This course is currently an elective, but there is talk of making it requirement.)
The course provides students with the opportunity to learn the principles of mindfulness, develop their own mindfulness mediation practice, and apply principles of mindfulness to daily life.
Prior to taking the class, Jasmine had been struggling with time management. Having never meditated before, it took her some time to acclimate to the practice. But now, she says, “I feel like this class has definitely not only forced me to try new things, but I’ve made it a part of my daily routine. It’s definitely helped me!”
Initially, Sarah noted that she “had a really hard time sitting down with myself and going through [the process].” Gradually, with the guidance of Professor Jennifer Swanberg, “I've been able to develop my own practice that I find beneficial. There are those times where I still feel frustration, but now I feel more prepared to deal with it.”
In the Occupational Therapy department, faculty celebrate Grati-Tuesdays, where they keep a running list of what they are thankful for. “Gratitude is really powerful,” noted Assistant Professor Kathryn Burke. “I often tell my students to break up anxiety with gratitude. Thinking about something that you’re grateful for can sometimes help get your brain out of that downward spiral that everything is terrible.”
Other suggestions included:
- A peer mentorship program to help increase social support
- Moving 11:59pm assignment deadlines to 8pm
- Minimizing the number of early morning classes
- Enforcing quiet hours in residence halls
- Expanding the number of safe community spaces (like the Bridge for Diversity, Equity and Social Justice ) where students can share with their peers
“Creating a sense of belonging is crucially important,” concluded Rosenthal. “We need to have safe spaces to hold people when the rest of the world feels unsafe.”
JWU has a wealth of confidential mental health resources, including counseling services in Providence and Charlotte . Individual counseling sessions and consultations are available by appointment, as well as resources for mental health screenings, education and crisis intervention.
Related Reading:
6 Ways College Students Can Improve Their Mental Health
Self-Care Tips to Use During Exams
JWU Alumni Share Insight on DEI and Belonging
Apply Visit Transfer Explore from Home

Related Posts

OTD Student Experiences 'Humanity' Through Butler Hospital Fieldwork

Ten Years On, JWU's PA Program Is Going Strong
How Community Action Can Improve Black Maternal Health Outcomes
- Arts & Sciences 77
- Business 50
- Engineering & Design 53
- Culinary 148
- Health & Wellness 42
- Hospitality Management 92
- Covid-19 12
- Experiential Education 45
- Students 121
- Request information
- Start your application

An official website of the United States government, Department of Justice.
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Cross-Site Analysis and Case Study of STOP Program Grantee Perspectives on Violence Prevention and Mental Health Training Program Implementation
This paper explores STOP Program grantee perspectives on violence prevention and mental health training program implementation.
In this study, researchers examined factors that influence the implementation of violence prevention and mental health training programs in schools, with a particular focus on implementation readiness and school mental health capacity. Several promising results were found that may contribute to ongoing efforts to improve school safety. In response to the Students, Teachers, and Officers Preventing (STOP) School Violence Act of 2018 (H.R. 4909), 128 grantees across the U.S. were awarded funding through the Bureau of Justice Assistance (BJA) in 2018 and 2019 to improve school safety by implementing programs in the Violence Prevention and Mental Health Training category. The major goals of this study were to 1) understand the challenges and facilitators of implementing violence prevention and mental health training programs through a broad cross-site analysis, 2) assess contextual factors influencing implementation, as well as regional and population variances through targeted, comprehensive case studies, and 3) provide evidence to inform program implementation in violence prevention and mental health programs in schools to improve program outcomes and sustainability. Understanding the environment of implementation, grantees’ capacity to carry out planned activities, and the perspectives of implementation team members are critical components to learning what factors support and inhibit implementation and ultimately, the extent to which programming will be replicable and scalable as federal funding continues to support mental health and violence prevention initiatives. The study was conducted at two levels: 1) a cross-site analysis of grantees who have been awarded funding in the Violence Prevention and Mental Health Training category over the two award years (2018 and 2019), and 2) a case study analysis of six grantee sites.
Additional Details
Related topics, similar publications.
- Understanding the Trafficking of Children for the Purposes of Labor in the United States
- Mechanisms Underlying Desistance from Crime: Individual and Social Pathways
- The ethics and urgency of identifying domestic minor sex trafficking victims in clinical settings

IMAGES
VIDEO
COMMENTS
Sample #3: Conceptualization in a family therapy case. This 45-year-old African-American woman was initially referred for individual therapy for "rapid mood swings" and a tendency to become embroiled in family conflicts. Several sessions of family therapy also appear indicated, and her psychiatrist concurs.
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
Include a completed CCD with the case write -up. PART FOUR: THE CASE CONCEPTUALIZATION SUMMARY HISTORY OF CURRENT ILLNESS, PRECIPITANTS AND LIFE STRESSORS: The first occurrence of Abe's psychiatric symptoms began 2 ½ years ago when Abe began to display mild depressive and anxious symptoms. The precipitant was difficulty at work; his new boss
Sara, a 35-year-old married female. Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks. Bleiberg, K.L., & Markowitz, J.C. (2008).
Here are four tips to consider while writing a psychology case study: Remember to use the rules of APA formatting. Use fictitious names instead of referring to the patient as a client. Refer to previous case studies to understand how to format and stylize your study. Proofread and revise your report before submitting it.
Creating an effective case conceptualization requires a comprehensive, adaptable, and multidimensional approach. It involves analyzing the client's situation, embracing various perspectives, focusing on their strengths, and evolving throughout therapy. Stay curious, keep an open mind, and be willing to learn.
INTRODUCTION. Case presentation in an academic psychiatry traditionally follows one of the following three formats: 4DP format (ideal and lengthy format; described in the following section), "Case Summary" (CS) (medium format), or "Case Formulation" (CF) (short format), in order of the decreasing length, duration, and the gradual transition from the use of layman terms (in the history ...
General Instructions: This model case history is quite comprehensive. Most case histories are under 10 pages (size 10 font). Number of pages do not necessarily translate to a better mark. Reading this model case history, one will have an excellent understanding of the patient's history, development, current situation and presentation.
Monson, C. M. & Shnaider, P. (2014). Treating PTSD with cognitive-behavioral therapies: Interventions that work. Washington, DC: American Psychological Association. Updated July 31, 2017. Date created: 2017. This case example explains how Jill's therapist used a cognitive intervention with a written worksheet as a starting point for engaging in ...
This chapter focuses on Stage 2, the empirical - or 'primary research' - aspect of the study, which we conducted using the case study method. We start with an outline of the specific research methods used, after which we provide a descriptive overview of the individual case study sites; we then present our findings, organised according to a number of analytical themes.
Philip, a 60-year-old who was in a traffic accident (PDF, 294KB) This case example from the European Journal of Psychotraumatology details an assisted self-study application of cognitive therapy for PTSD. Philip developed PTSD and comorbid major depression following a traffic accident. He was treated in six sessions of cognitive therapy with ...
Abstract. This collection presents six case studies on the ethics of mental health research, written by scientific researchers and ethicists from around the world. We publish them here as a resource for teachers of research ethics and as a contribution to several ongoing ethical debates. Each consists of a description of a research study that ...
International Journal of Mental Health Systems welcomes well-described Case studies. These will usually present a major programme intervention or policy option relevant to the journal field. Manuscripts that include a rigorous assessment of the processes and the impact of the study, as well as recommendations for the future, will generally be ...
The Biopsychosocial Model and Case Formulation (also known as the Biopsychosocial Formulation) in psychiatry is a way of understanding a patient as more than a diagnostic label.Hypotheses are generated about the origins and causes of a patient's symptoms. The most common and clinically practical way to formulate is through the biopsychosocial approach, first described in 1980 by George Engel.
Proofreading and editing your draft. After writing a draft, the case study writer or team should have 2-3 people, unfamiliar with the draft, read it over. These people should highlight any words or sentences they find confusing. They can also write down one or two questions that they still have after reading the draft.
Mental health. Children's mental health case studies. Explore the experiences of children and families with these interdisciplinary case studies. Designed to help professionals and students explore the strengths and needs of children and their families, each case presents a detailed situation, related research, problem-solving questions and ...
At Tracking Happiness, we're dedicated to helping others around the world overcome struggles of mental health. In 2022, we published a survey of 5,521 respondents and found: 88% of our respondents experienced mental health issues in the past year. 25% of people don't feel comfortable sharing their struggles with anyone, not even their ...
Identify a case(s) for student to read and review. Provide specific prompts that you would like the student to address as a part of the assignment. Include prompts that have the student address the case from a clinical and macro viewpoint as well as consider some ethical considerations.
We're going to go ahead to patient case No. 1. This is a 27-year-old woman who's presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode.
Clinical case scenarios: Common mental health disorders in primary care (May 2012) Page 6 of 85 The longstanding relationship that GPs often have with patients can help to optimise the quality of an assessment and in establishing the characterisation of their problems. Validated tools such as PHQ-9 and GAD-7 can help support the
Conceptualizing a case systemically can be challenging, because of the many family members and influences that are relevant to our work with clients. In the practicum courses I teach, students are required to write a case summary and present the case to the class. In this post, I outline and explain the sections of the case summary assignment.
I understand that Mrs Brown has been residing in her own home, a two-story terrace house in Melbourne, for almost 60 years. She has lived alone since her husband died two years ago following a cardiac arrest. She has two daughters. The youngest daughter Jean has lived with her for the past year, after she lost her job.
nothing major. His health was relatively good, except for moderately high blood pressure, which he developed in his late forties. He didn't have any physical limitations. CURRENT NON-PSYCHIATRIC MEDICATIONS, TREATMENT, ADHERENCE AND SIDE EFFECTS: Abe was taking Vasotec, 10 mg, 2x per day with full adherence to treat high blood pressure. He had no
middle socio-economic status. The case study used patient (client), his family members and the case record file as sources to collect information which were reliable and adequate. The case was referred to the dept. of psychiatric social work for psychosocial management and intervention from the OPD of LGBRIMH, Tezpur. Brief clinical history
Many types of mental health care professionals can help you achieve your recovery goals. These professionals work in inpatient facilities, such as general hospitals and psychiatric facilities, and outpatient facilities, such as community mental health clinics, schools and private practices. Health care professional job titles and specialties can vary by state. The descriptions below give […]
Associate Professor Sam Rosenthal shared case studies outlining the student mental health landscape — and evidence-backed pathways for improving social support and outcomes. ... JWU has a wealth of confidential mental health resources, including counseling services in Providence and Charlotte. Individual counseling sessions and consultations ...
The major goals of this study were to 1) understand the challenges and facilitators of implementing violence prevention and mental health training programs through a broad cross-site analysis, 2) assess contextual factors influencing implementation, as well as regional and population variances through targeted, comprehensive case studies, and 3 ...
This can ultimately have a negative impact on mental health. "As a person builds a high tolerance for the use of social media it causes internal and external conflict," he said. "You know it ...
Mental health visits for assisted living residents living with dementia dropped as the pandemic set in, a new study finds. The report, which was published Wednesday in the Journal of the American Geriatrics Society, used data from 102,758 fee-for-service Medicare beneficiaries with Alzheimer's disease or a related dementia. People came from ...
This case study delves into Hertfordshire's strategic integration of health visiting and family support services to optimise the Healthy Child Programme. It outlines initiatives aimed at strengthening mental health support from the antenatal period to school age, enhancing workforce development, and providing targeted care for children with SEND.