
Vitamin D is both a nutrient we eat and a hormone our bodies make. It is a fat-soluble vitamin that has long been known to help the body absorb and retain calcium and phosphorus ; both are critical for building bone. Also, laboratory studies show that vitamin D can reduce cancer cell growth, help control infections and reduce inflammation. Many of the body’s organs and tissues have receptors for vitamin D, which suggest important roles beyond bone health, and scientists are actively investigating other possible functions.
Few foods naturally contain vitamin D, though some foods are fortified with the vitamin. For most people, the best way to get enough vitamin D is taking a supplement because it is hard to eat enough through food. Vitamin D supplements are available in two forms: vitamin D2 (“ergocalciferol” or pre-vitamin D) and vitamin D3 (“cholecalciferol”). Both are also naturally occurring forms that are produced in the presence of the sun’s ultraviolet-B (UVB) rays, hence its nickname, “the sunshine vitamin,” but D2 is produced in plants and fungi and D3 in animals, including humans. Vitamin D production in the skin is the primary natural source of vitamin D, but many people have insufficient levels because they live in places where sunlight is limited in winter, or because they have limited sun exposure due to being inside much of the time. Also, people with darker skin tend to have lower blood levels of vitamin D because the pigment (melanin) acts like a shade, reducing production of vitamin D (and also reducing damaging effects of sunlight on skin, including skin cancer).

Recommended Amounts
The Recommended Dietary Allowance for vitamin D provides the daily amount needed to maintain healthy bones and normal calcium metabolism in healthy people. It assumes minimal sun exposure.
RDA: The Recommended Dietary Allowance for adults 19 years and older is 600 IU (15 mcg) daily for men and women, and for adults >70 years it is 800 IU (20 mcg) daily.
UL: The Tolerable Upper Intake Level is the maximum daily intake unlikely to cause harmful effects on health. The UL for vitamin D for adults and children ages 9+ is 4,000 IU (100 mcg).
Many people may not be meeting the minimum requirement for the vitamin. NHANES data found that the median intake of vitamin D from food and supplements in women ages 51 to 71 years was 308 IU daily, but only 140 IU from food alone (including fortified products). [1] Worldwide, an estimated 1 billion people have inadequate levels of vitamin D in their blood, and deficiencies can be found in all ethnicities and age groups. [2-4] In the U.S., about 20% of White adults and 75% of Black adults have blood levels of vitamin D below 50 nmol/L. [83] In industrialized countries, doctors are seeing the resurgence of rickets, the bone-weakening disease that had been largely eradicated through vitamin D fortification. [5-7] There is scientific debate about how much vitamin D people need each day and what the optimal serum levels should be to prevent disease. The Institute of Medicine (IOM) released in November 2010 recommendations increasing the daily vitamin D intake for children and adults in the U.S. and Canada, to 600 IU per day. [1] The report also increased the upper limit from 2,000 to 4,000 IU per day. Although some groups such as The Endocrine Society recommend 1,500 to 2,000 IU daily to reach adequate serum levels of vitamin D, the IOM felt there was not enough evidence to establish a cause and effect link with vitamin D and health benefits other than for bone health. Since that time, new evidence has supported other benefits of consuming an adequate amount of vitamin D, although there is still not consensus on the amount considered to be adequate.
Vitamin D and Health
The role of vitamin D in disease prevention is a popular area of research, but clear answers about the benefit of taking amounts beyond the RDA are not conclusive. Although observational studies see a strong connection with lower rates of certain diseases in populations that live in sunnier climates or have higher serum levels of vitamin D, clinical trials that give people vitamin D supplements to affect a particular disease are still inconclusive. This may be due to different study designs, differences in the absorption rates of vitamin D in different populations, and different dosages given to participants. Learn more about the research on vitamin D and specific health conditions and diseases:
Several studies link low vitamin D blood levels with an increased risk of fractures in older adults. Some studies suggest that vitamin D supplementation in certain amounts may prevent such fractures, while others do not. [8-11]
- A meta-analysis of 12 randomized controlled trials that included more than 42,000 people 65+ years of age, most of them women, looked at vitamin D supplementation with or without calcium, and with calcium or a placebo. Researchers found that higher intakes of vitamin D supplements—about 500-800 IU per day—reduced hip and non-spine fractures by about 20%, while lower intakes (400 IU or less) failed to offer any fracture prevention benefit. [12]
- A systematic review looked at the effect of vitamin D supplements taken with or without calcium on the prevention of hip fractures (primary outcome) and fractures of any type (secondary outcome) in older men and postmenopausal women 65+ years of age. It included 53 clinical trials with 91,791 participants who lived independently or in a nursing home or hospital. It did not find a strong association between vitamin D supplements alone and prevention of fractures of any type. However, it did find a small protective effect from all types of fractures when vitamin D was taken with calcium. All of the trials used vitamin D supplements containing 800 IU or less. [13]
- The VITamin D and OmegA-3 TriaL (VITAL) double-blind placebo-controlled randomized trial of 25,871 women and men, 55+ years and 50+ years of age, respectively, did not find a protective effect from vitamin D supplements on bone fractures. [81] The participants were healthy at the start of the study—representative of the general population and not selected based on low bone mass, osteoporosis, or vitamin D deficiency—and were given either 2,000 IU of vitamin D or a placebo taken daily for about five years. Vitamin D did not lower the incidence of total bone fractures or fractures of the hip or spine.
Vitamin D may help increase muscle strength by preserving muscle fibers, which in turn helps to prevent falls, a common problem that leads to substantial disability and death in older people. [14–16] A combined analysis of multiple studies found that taking 700 to 1,000 IU of vitamin D per day lowered the risk of falls by 19%, but taking 200 to 600 IU per day did not offer any such protection. [17] However, the VITAL trial following healthy middle-aged men and women did not find that taking 2,000 IU of vitamin D daily compared with a placebo pill reduced the risk of falls. [82]
Though taking up to 800 IU of vitamin D daily may benefit bone health in some older adults, it is important to be cautious of very high dosage supplements. A clinical trial that gave women 70+ years of age a once-yearly dosage of vitamin D at 500,000 IU for five years caused a 15% increased risk of falls and a 26% higher fracture risk than women who received a placebo. [18] It was speculated that super-saturating the body with a very high dose given infrequently may have actually promoted lower blood levels of the active form of vitamin D that might not have occurred with smaller, more frequent doses. [13]
JoAnn Manson, MD, DrPH , leader of the main VITAL trial and coauthor of the report on fracture, commented:
“We conclude that, in the generally healthy U.S. population of midlife and older adults, vitamin D supplementation doesn’t reduce the risk of fractures or falls. This suggests that only small-to-moderate amounts of vitamin D are needed for bone health and fall prevention, achieved by most community-dwelling adults. Of course, vitamin D deficiency should always be treated and some high-risk patients with malabsorption syndromes, osteoporosis, or taking medications that interfere with vitamin D metabolism will benefit from supplementation.”
Nearly 30 years ago, researchers noticed an intriguing relationship between colon cancer deaths and geographic location: People who lived at higher latitudes, such as in the northern U.S., had higher rates of death from colon cancer than people who lived closer to the equator. [19] Many scientific hypotheses about vitamin D and disease stem from studies that have compared solar radiation and disease rates in different countries. These studies can be a good starting point for other research but don’t provide the most definitive information. The sun’s UVB rays are weaker at higher latitudes, and in turn, people’s vitamin D blood levels in these locales tend to be lower. This led to the hypothesis that low vitamin D levels might somehow increase colon cancer risk. [3]
Animal and laboratory studies have found that vitamin D can inhibit the development of tumors and slow the growth of existing tumors including those from the breast, ovary, colon, prostate, and brain. In humans, epidemiological studies show that higher serum levels of vitamin D are associated with substantially lower rates of colon, pancreatic, prostate, and other cancers , with the evidence strongest for colorectal cancer. [20-32]
However, clinical trials have not found a consistent association:
The Women’s Health Initiative trial, which followed roughly 36,000 women for an average of seven years, failed to find any reduction in colon or breast cancer risk in women who received daily supplements of 400 IU of vitamin D and 1,000 mg of calcium, compared with those who received a placebo. [33,34] Limitations of the study were suggested: 1) the relatively low dose of vitamin D given, 2) some people in the placebo group decided on their own to take extra calcium and vitamin D supplements, minimizing the differences between the placebo group and the supplement group, and 3) about one-third of the women assigned to vitamin D did not take their supplements. 4) seven years may be too short to expect a reduction in cancer risk. [35,36]
A large clinical trial called the VITamin D and OmegA-3 TriaL (VITAL) followed 25,871 men and women 50+ years of age free of any cancers at the start of the study who took either a 2,000 IU vitamin D supplement or placebo daily for a median of five years. [37] The findings did not show significantly different rates of breast, prostate, and colorectal cancer between the vitamin D and placebo groups. The authors noted that a longer follow-up period would be necessary to better assess potential effects of supplementation, as many cancers take at least 5-10 years to develop.
Although vitamin D does not seem to be a major factor in reducing cancer incidence, evidence including that from randomized trials suggests that having higher vitamin D status may improve survival if one develops cancer. In the VITAL trial, a lower death rate from cancer was observed in those assigned to take vitamin D, and this benefit seemed to increase over time since starting on vitamin D. A meta-analysis of randomized trials of vitamin D, which included the VITAL study, found a 13% statistically significant lower risk of cancer mortality in those assigned to vitamin D compared to placebo. [38] These findings are consistent with observational data, which suggest that vitamin D may have a stronger effect on cancer progression than for incidence.
The heart is basically a large muscle, and like skeletal muscle, it has receptors for vitamin D. [39] Immune and inflammatory cells that play a role in cardiovascular disease conditions like atherosclerosis are regulated by vitamin D. [40] The vitamin also helps to keep arteries flexible and relaxed, which in turn helps to control high blood pressure. [41]
In the Health Professionals Follow-up Study nearly 50,000 healthy men were followed for 10 years. [42] Those who had the lowest levels of vitamin D were twice as likely to have a heart attack as men who had the highest levels. Meta-analyses of epidemiological studies have found that people with the lowest serum levels of vitamin D had a significantly increased risk of strokes and any heart disease event compared with those with the highest levels. [40;43-46]
However, taking vitamin D supplements has not been found to reduce cardiovascular risk. A meta-analysis of 51 clinical trials did not demonstrate that vitamin D supplementation lowered the risk of heart attack, stroke, or deaths from cardiovascular disease. [47] The VITamin D and OmegA-3 TriaL (VITAL) came to the same conclusion; it followed 25,871 men and women free of cardiovascular disease who took either a 2,000 IU vitamin D supplement or placebo daily for a median of five years. No association was found between taking the supplements and a lower risk of major cardiovascular events (heart attack, stroke, or death from cardiovascular causes) compared with the placebo. [37]
Vitamin D deficiency may negatively affect the biochemical pathways that lead to the development of Type 2 diabetes (T2DM), including impairment of beta cell function in the pancreas, insulin resistance, and inflammation. Prospective observational studies have shown that higher vitamin D blood levels are associated with lower rates of T2DM. [48]
More than 83,000 women without diabetes at baseline were followed in the Nurses’ Health Study for the development of T2DM. Vitamin D and calcium intakes from diet and supplements were assessed throughout the 20-year study. [49] The authors found that when comparing the women with the highest intakes of vitamin D from supplements with women with the lowest intakes, there was a 13% lower risk of developing T2DM. The effect was even stronger when vitamin D was combined with calcium: there was a 33% lower risk of T2DM in women when comparing the highest intakes of calcium and vitamin D from supplements (>1,200 mg, >800 IU daily) with the lowest intakes (<600 mg, 400 IU).
A randomized clinical trial gave 2,423 adults who had prediabetes either 4000 IU of vitamin D or a placebo daily for two years. The majority of participants did not have vitamin D deficiency at the start of the study. At two years, vitamin D blood levels in the supplement versus placebo group was 54.3 ng/mL versus 28.2 ng/mL, respectively, but no significant differences were observed in rates of T2DM at the 2.5 year follow-up. [50] The authors noted that a lack of effect of vitamin D may have been due to the majority of participants having vitamin D blood levels in a normal range of greater than 20 ng/mL, which is considered an acceptable level to reduce health risks. Notably, among the participants who had the lowest blood levels of vitamin D at the beginning of the study, vitamin D supplementation did reduce risk of diabetes. This is consistent with the important concept that taking additional vitamin D may not benefit those who already have adequate blood levels, but those with initially low blood levels may benefit.
Vitamin D’s role in regulating the immune system has led scientists to explore two parallel research paths: Does vitamin D deficiency contribute to the development of multiple sclerosis, type 1 diabetes, and other so-called “autoimmune” diseases, where the body’s immune system attacks its own organs and tissues? And could vitamin D supplements help boost our body’s defenses to fight infectious disease, such as tuberculosis and seasonal flu?
Multiple Sclerosis The rate of multiple sclerosis (MS) is increasing in both developed and developing countries, with an unclear cause. However, a person’s genetic background plus environmental factors including inadequate vitamin D and UVB exposure have been identified to increase risk. [51] Vitamin D was first proposed over 40 years ago as having a role in MS given observations at the time including that rates of MS were much higher far north (or far south) of the equator than in sunnier climates, and that geographic regions with diets high in fish had lower rates of MS. [52] A prospective study of dietary intake of vitamin D found women with daily intake above 400 IU had a 40% lower risk of MS. [53] In a study among healthy young adults in the US, White men and women with the highest vitamin D serum levels had a 62% lower risk of developing MS than those with the lowest vitamin D levels. [54] The study didn’t find this effect among Black men and women, possibly because there were fewer Black study participants and most of them had low vitamin D levels, making it harder to find any link between vitamin D and MS if one exists. Another prospective study in young adults from Sweden also found a 61% lower risk of MS with higher serum vitamin D levels; [55] and a prospective study among young Finnish women found that low serum vitamin D levels were associated with a 43% increased risk of MS. [56] In prospective studies of persons with MS, higher vitamin D levels have been associated with reduced disease activity and progression. [57,58] While several clinical trials are underway to examine vitamin D as a treatment in persons with MS, there are no clinical trials aimed at prevention of MS, likely because MS is a rare disease and the trial would need to be large and of long duration. Collectively, the current evidence suggests that low vitamin D may have a causal role in MS and if so, approximately 40% of cases may be prevented by correcting vitamin D insufficiency. [59] This conclusion has been strengthened substantially by recent evidence that genetically determined low levels of vitamin D predict higher risk of multiple sclerosis.
Type 1 Diabetes Type 1 diabetes (T1D) is another disease that varies with geography—a child in Finland is about 400 times more likely to develop T1D than a child in Venezuela. [60] While this may largely be due to genetic differences, some studies suggest that T1D rates are lower in sunnier areas. Early evidence suggesting that vitamin D may play a role in T1D comes from a 30-year study that followed more than 10,000 Finnish children from birth: Children who regularly received vitamin D supplements during infancy had a nearly 90% lower risk of developing type 1 diabetes than those who did not receive supplements. [61] However, multiple studies examining the association between dietary vitamin D or trials supplementing children at high risk for T1D with vitamin D have produced mixed and inconclusive results [62] Approximately 40% of T1D cases begin in adulthood. A prospective study among healthy young adults in the US found that White individuals with the highest levels of serum vitamin D had a 44% lower risk of developing T1D in adulthood than those with the lowest levels. [63] No randomized controlled trials on vitamin D and adult onset T1D have been conducted, and it is not clear that they would be possible to conduct. More research is needed in this area.
Flu and the Common Cold The flu virus wreaks the most havoc in the winter, abating in the summer months. This seasonality led a British doctor to hypothesize that a sunlight-related “seasonal stimulus” triggered influenza outbreaks. [64] More than 20 years after this initial hypothesis, several scientists published a paper suggesting that vitamin D may be the seasonal stimulus. [65] Among the evidence they cite:
- Vitamin D levels are lowest in the winter months. [65]
- The active form of vitamin D tempers the damaging inflammatory response of some white blood cells, while it also boosts immune cells’ production of microbe-fighting proteins. [65]
- Children who have vitamin D-deficiency rickets are more likely to get respiratory infections, while children exposed to sunlight seem to have fewer respiratory infections. [65]
- Adults who have low vitamin D levels are more likely to report having had a recent cough, cold, or upper respiratory tract infection. [66]
A randomized controlled trial in Japanese school children tested whether taking daily vitamin D supplements would prevent seasonal flu. [67] The trial followed nearly 340 children for four months during the height of the winter flu season. Half of the study participants received pills that contained 1,200 IU of vitamin D; the other half received placebo pills. Researchers found that type A influenza rates in the vitamin D group were about 40% lower than in the placebo group; there was no significant difference in type B influenza rates.
Although randomized controlled trials exploring the potential of vitamin D to prevent other acute respiratory infections have yielded mixed results, a large meta-analysis of individual participant data indicated that daily or weekly vitamin D supplementation lowers risk of acute respiratory infections. [68] This effect was particularly prominent for very deficient individuals.
The findings from this large meta-analysis have raised the possibility that low vitamin D levels may also increase risk of or severity of novel coronavirus 2019 (COVID-19) infection. Although there is no direct evidence on this issue because this such a new disease, avoiding low levels of vitamin D makes sense for this and other reasons. Thus, if there is reason to believe that levels might be low, such as having darker skin or limited sun exposure, taking a supplement of 1000 or 2000 IU per day is reasonable. This amount is now part of many standard multiple vitamin supplements and inexpensive.
More research is needed before we can definitively say that vitamin D protects against the flu and other acute respiratory infections. Even if vitamin D has some benefit, don’t skip your flu shot. And when it comes to limiting risk of COVID-19, it is important to practice careful social distancing and hand washing.
Tuberculosis Before the advent of antibiotics, sunlight and sun lamps were part of the standard treatment for tuberculosis (TB). [69] More recent research suggests that the “sunshine vitamin” may be linked to TB risk. Several case-control studies, when analyzed together, suggest that people diagnosed with tuberculosis have lower vitamin D levels than healthy people of similar age and other characteristics. [70] Such studies do not follow individuals over time, so they cannot tell us whether vitamin D deficiency led to the increased TB risk or whether taking vitamin D supplements would prevent TB. There are also genetic differences in the receptor that binds vitamin D, and these differences may influence TB risk. [71] Again, more research is needed.
Other A utoimmune Conditions The Vitamin D and Omega 3 trial (VITAL), a randomized double-blind placebo-controlled trial following more than 25,000 men and women ages 50 and older, found that taking vitamin D supplements (2,000 IU/day) for five years, or vitamin D supplements with marine omega-3 fatty acids (1,000 mg/day), reduced the incidence of autoimmune diseases by about 22%, compared with a placebo. Autoimmune conditions observed included rheumatoid arthritis, psoriasis, polymyalgia rheumatica, and autoimmune thyroid diseases (Hashimoto’s thyroiditis, Graves’ disease). [80] The doses in these supplements are widely available and generally well-tolerated. The authors recommended additional trials to test the effectiveness of these supplements in younger populations and those at high risk of developing autoimmune diseases.
- A promising report in the Archives of Internal Medicine suggests that taking vitamin D supplements may reduce overall mortality rates: A combined analysis of multiple studies found that taking modest levels of vitamin D supplements was associated with a statistically significant 7% reduction in mortality from any cause. [72] The analysis looked at the findings from 18 randomized controlled trials that enrolled a total of nearly 60,000 study participants; most of the study participants took between 400 and 800 IU of vitamin D per day for an average of five years. Keep in mind that this analysis has several limitations, chief among them the fact that the studies it included were not designed to explore mortality in general, or explore specific causes of death. A recent meta-analysis suggests that this reduction in mortality is driven mostly by a reduction in cancer mortality. [38] More research is needed before any broad claims can be made about vitamin D and mortality. [73]
- A large cohort study of more than 307,000 White European participants found a 25% increased risk of premature deaths from any cause in those who had vitamin D blood levels of 25 nmol/L (10 ng/ml), compared with those who had 50 nmol/L (20 ng/ml) (the National Academy of Medicine cites a vitamin D blood level of 50 nmol/L as adequate for most people). [74] Similar increases in risks were seen for deaths due to cardiovascular disease, cancer, and respiratory disease, and risks increased sharply among those with even lower levels of vitamin D. Although the numbers of non-White participants were small, the findings were similar in this group. The study used Mendelian randomization, which measured genetic variations to confirm these findings. This confirmation is important because it documents that the adverse health outcomes among people with low levels of vitamin D represent a causal relationship between vitamin D deficiency and premature death. Specifically, this method removed potential confounding by factors such as obesity, smoking, and alcohol intake.
In an analysis of more than 427,000 White European participants using Mendelian randomization, a 54% higher risk of dementia was seen among participants with low vitamin D blood levels of <25 nmol/L compared with those having adequate levels of 50 nmol/L. [75]
Food Sources
Few foods are naturally rich in vitamin D3. The best sources are the flesh of fatty fish and fish liver oils. Smaller amounts are found in egg yolks, cheese, and beef liver. Certain mushrooms contain some vitamin D2; in addition some commercially sold mushrooms contain higher amounts of D2 due to intentionally being exposed to high amounts of ultraviolet light. Many foods and supplements are fortified with vitamin D like dairy products and cereals.
- Cod liver oil
- Orange juice fortified with vitamin D
- Dairy and plant milks fortified with vitamin D
- Fortified cereals

Is There a Difference Between Vitamin D3 and Vitamin D2 Supplements?
Ultraviolet light.
Vitamin D3 can be formed when a chemical reaction occurs in human skin, when a steroid called 7-dehydrocholesterol is broken down by the sun’s UVB light or so-called “tanning” rays. The amount of the vitamin absorbed can vary widely. The following are conditions that decrease exposure to UVB light and therefore lessen vitamin D absorption:
- Use of sunscreen; correctly applied sunscreen can reduce vitamin D absorption by more than 90%. [78]
- Wearing full clothing that covers the skin.
- Spending limited time outdoors.
- Darker skin tones due to having higher amounts of the pigment melanin, which acts as a type of natural sunscreen. [79]
- Older ages when there is a decrease in 7-dehydrocholesterol levels and changes in skin, and a population that is likely to spend more time indoors.
- Certain seasons and living in northern latitudes above the equator where UVB light is weaker. [78] In the northern hemisphere, people who live in Boston (U.S.), Edmonton (Canada), and Bergen (Norway) can’t make enough vitamin D from the sun for 4, 5, and 6 months out of the year, respectively. [78] In the southern hemisphere, residents of Buenos Aires (Argentina) and Cape Town (South Africa) make far less vitamin D from the sun during their winter months (June through August) than they can during their spring and summer months. [78] The body stores vitamin D from summer sun exposure, but it must last for many months. By late winter, many people in these higher-latitude locales are deficient. [79]
Note that because ultraviolet rays can cause skin cancer, it is important to avoid excessive sun exposure and in general, tanning beds should not be used.
Signs of Deficiency and Toxicity
Vitamin D deficiency may occur from a lack in the diet, poor absorption, or having a metabolic need for higher amounts. If one is not eating enough vitamin D and does not receive enough ultraviolet sun exposure over an extended period (see section above), a deficiency may arise. People who cannot tolerate or do not eat milk, eggs, and fish, such as those with a lactose intolerance or who follow a vegan diet, are at higher risk for a deficiency. Other people at high risk of vitamin D deficiency include:
- People with inflammatory bowel disease (ulcerative colitis, Crohn’s disease) or other conditions that disrupt the normal digestion of fat. Vitamin D is a fat-soluble vitamin that depends on the gut’s ability to absorb dietary fat.
- People who are obese tend to have lower blood vitamin D levels. Vitamin D accumulates in excess fat tissues but is not easily available for use by the body when needed. Higher doses of vitamin D supplementation may be needed to achieve a desirable blood level. Conversely, blood levels of vitamin D rise when obese people lose weight.
- People who have undergone gastric bypass surgery, which typically removes the upper part of the small intestine where vitamin D is absorbed.
Conditions resulting from prolonged vitamin D deficiency:
- Rickets: A condition in infants and children of soft bones and skeletal deformities caused by failure of bone tissue to harden.
- Osteomalacia: A condition in adults of weak and softened bones that can be reversed with supplementation. This is different than osteoporosis, in which the bones are porous and brittle and the condition is irreversible.
Vitamin D toxicity most often occurs from taking supplements. The low amounts of the vitamin found in food are unlikely to reach a toxic level, and a high amount of sun exposure does not lead to toxicity because excess heat on the skin prevents D3 from forming. It is advised to not take daily vitamin D supplements containing more than 4,000 IU unless monitored under the supervision of your doctor.
Symptoms of toxicity:
- Weight loss
- Irregular heart beat
- Hardening of blood vessels and tissues due to increased blood levels of calcium, potentially leading to damage of the heart and kidneys
Did You Know?
Catching the sun’s rays in a sunny office or driving in a car unfortunately won’t help to obtain vitamin D as window glass completely blocks UVB ultraviolet light.
Vitamins and Minerals
- Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, D.C.: National Academies Press, 2010. https://www.ncbi.nlm.nih.gov/books/NBK56070/
- Holick MF. Vitamin D deficiency. New England Journal of Medicine . 2007 Jul 19;357(3):266-81.
- Gordon CM, DePeter KC, Feldman HA, Grace E, Emans SJ. Prevalence of vitamin D deficiency among healthy adolescents. Archives of pediatrics & adolescent medicine . 2004 Jun 1;158(6):531-7.
- Lips PT. Worldwide status of vitamin D nutrition. The Journal of steroid biochemistry and molecular biology . 2010 Jul 1;121(1-2):297-300.
- Robinson PD, Högler W, Craig ME, Verge CF, Walker JL, Piper AC, Woodhead HJ, Cowell CT, Ambler GR. The re-emerging burden of rickets: a decade of experience from Sydney. Archives of Disease in Childhood . 2006 Jul 1;91(7):564-8.
- Kreiter SR, Schwartz RP, Kirkman Jr HN, Charlton PA, Calikoglu AS, Davenport ML. Nutritional rickets in African American breast-fed infants. The Journal of pediatrics . 2000 Aug 1;137(2):153-7.
- Misra M, Pacaud D, Petryk A, Collett-Solberg PF, Kappy M. Vitamin D deficiency in children and its management: review of current knowledge and recommendations. Pediatrics . 2008 Aug 1;122(2):398-417.
- Boonen S, Lips P, Bouillon R, Bischoff-Ferrari HA, Vanderschueren D, Haentjens P. Need for additional calcium to reduce the risk of hip fracture with vitamin D supplementation: evidence from a comparative metaanalysis of randomized controlled trials. The Journal of Clinical Endocrinology & Metabolism . 2007 Apr 1;92(4):1415-23.
- Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B. Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. Jama . 2005 May 11;293(18):2257-64.
- Cauley JA, LaCroix AZ, Wu L, Horwitz M, Danielson ME, Bauer DC, Lee JS, Jackson RD, Robbins JA, Wu C, Stanczyk FZ. Serum 25-hydroxyvitamin D concentrations and risk for hip fractures. Annals of internal medicine . 2008 Aug 19;149(4):242-50.
- Cauley JA, Parimi N, Ensrud KE, Bauer DC, Cawthon PM, Cummings SR, Hoffman AR, Shikany JM, Barrett-Connor E, Orwoll E. Serum 25-hydroxyvitamin D and the risk of hip and nonspine fractures in older men. Journal of Bone and Mineral Research . 2010 Mar;25(3):545-53.
- Bischoff-Ferrari HA, Willett WC, Wong JB, Stuck AE, Staehelin HB, Orav EJ, Thoma A, Kiel DP, Henschkowski J. Prevention of nonvertebral fractures with oral vitamin D and dose dependency: a meta-analysis of randomized controlled trials. Archives of internal medicine . 2009 Mar 23;169(6):551-61.
- Avenell A, Mak JC, O’Connell D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database of Systematic Reviews . 2014(4).
- Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, Wong JB. Effect of vitamin D on falls: a meta-analysis. Jama . 2004 Apr 28;291(16):1999-2006.
- Broe KE, Chen TC, Weinberg J, Bischoff-Ferrari HA, Holick MF, Kiel DP. A higher dose of vitamin D reduces the risk of falls in nursing home residents: a randomized, multiple-dose study. Journal of the American Geriatrics Society . 2007 Feb;55(2):234-9.
- Bischoff-Ferrari HA, Orav EJ, Dawson-Hughes B. Effect of cholecalciferol plus calcium on falling in ambulatory older men and women: a 3-year randomized controlled trial. Archives of internal medicine . 2006 Feb 27;166(4):424-30.
- Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, Orav JE, Stuck AE, Theiler R, Wong JB, Egli A, Kiel DP, Henschkowski J. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ . 2009 Oct 1;339:b3692.
- Sanders KM, Stuart AL, Williamson EJ, Simpson JA, Kotowicz MA, Young D, Nicholson GC. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. Jama . 2010 May 12;303(18):1815-22.
- Garland CF, Garland FC. Do sunlight and vitamin D reduce the likelihood of colon cancer?. International journal of epidemiology . 1980 Sep 1;9(3):227-31.
- Garland CF, Gorham ED, Mohr SB, Garland FC. Vitamin D for cancer prevention: global perspective. Annals of epidemiology . 2009 Jul 1;19(7):468-83.
- McCullough ML, Zoltick ES, Weinstein SJ, Fedirko V, Wang M, Cook NR, Eliassen AH, Zeleniuch-Jacquotte A, Agnoli C, Albanes D, Barnett MJ. Circulating vitamin D and colorectal cancer risk: an international pooling project of 17 cohorts. JNCI: Journal of the National Cancer Institute . 2019 Feb 1;111(2):158-69.
- Yin L, Grandi N, Raum E, Haug U, Arndt V, Brenner H. Meta-analysis: longitudinal studies of serum vitamin D and colorectal cancer risk. Alimentary pharmacology & therapeutics . 2009 Jul;30(2):113-25.
- Wu K, Feskanich D, Fuchs CS, Willett WC, Hollis BW, Giovannucci EL. A nested case–control study of plasma 25-hydroxyvitamin D concentrations and risk of colorectal cancer. Journal of the National Cancer Institute . 2007 Jul 18;99(14):1120-9.
- Gorham ED, Garland CF, Garland FC, Grant WB, Mohr SB, Lipkin M, Newmark HL, Giovannucci E, Wei M, Holick MF. Optimal vitamin D status for colorectal cancer prevention: a quantitative meta analysis. American journal of preventive medicine . 2007 Mar 1;32(3):210-6.
- Giovannucci E. Epidemiological evidence for vitamin D and colorectal cancer. Journal of Bone and Mineral Research . 2007 Dec;22(S2):V81-5.
- Lin J, Zhang SM, Cook NR, Manson JE, Lee IM, Buring JE. Intakes of calcium and vitamin D and risk of colorectal cancer in women. American journal of epidemiology . 2005 Apr 15;161(8):755-64.
- Huncharek M, Muscat J, Kupelnick B. Colorectal cancer risk and dietary intake of calcium, vitamin D, and dairy products: a meta-analysis of 26,335 cases from 60 observational studies. Nutrition and cancer . 2008 Dec 31;61(1):47-69.
- Bertone-Johnson ER, Chen WY, Holick MF, Hollis BW, Colditz GA, Willett WC, Hankinson SE. Plasma 25-hydroxyvitamin D and 1, 25-dihydroxyvitamin D and risk of breast cancer. Cancer Epidemiology and Prevention Biomarkers . 2005 Aug 1;14(8):1991-7.
- Garland CF, Gorham ED, Mohr SB, Grant WB, Giovannucci EL, Lipkin M, Newmark H, Holick MF, Garland FC. Vitamin D and prevention of breast cancer: pooled analysis. The Journal of steroid biochemistry and molecular biology . 2007 Mar 1;103(3-5):708-11.
- Lin J, Manson JE, Lee IM, Cook NR, Buring JE, Zhang SM. Intakes of calcium and vitamin D and breast cancer risk in women. Archives of Internal Medicine . 2007 May 28;167(10):1050-9.
- Robien K, Cutler GJ, Lazovich D. Vitamin D intake and breast cancer risk in postmenopausal women: the Iowa Women’s Health Study. Cancer causes & control . 2007 Sep 1;18(7):775-82.
- Freedman DM, Chang SC, Falk RT, Purdue MP, Huang WY, McCarty CA, Hollis BW, Graubard BI, Berg CD, Ziegler RG. Serum levels of vitamin D metabolites and breast cancer risk in the prostate, lung, colorectal, and ovarian cancer screening trial. Cancer Epidemiology and Prevention Biomarkers . 2008 Apr 1;17(4):889-94.
- Wactawski-Wende J, Kotchen JM, Anderson GL, Assaf AR, Brunner RL, O’sullivan MJ, Margolis KL, Ockene JK, Phillips L, Pottern L, Prentice RL. Calcium plus vitamin D supplementation and the risk of colorectal cancer. New England Journal of Medicine . 2006 Feb 16;354(7):684-96.
- Chlebowski RT, Johnson KC, Kooperberg C, Pettinger M, Wactawski-Wende J, Rohan T, Rossouw J, Lane D, O’Sullivan MJ, Yasmeen S, Hiatt RA. Calcium plus vitamin D supplementation and the risk of breast cancer. JNCI: Journal of the National Cancer Institute . 2008 Nov 19;100(22):1581-91.
- Holick MF. Calcium plus vitamin D and the risk of colorectal cancer. N Engl J Med . 2006; 354:2287-8; author reply 2287-8.
- Giovannucci E. Calcium plus vitamin D and the risk of colorectal cancer. N Engl J Med . 2006; 354:2287-8; author reply 2287-8.
- Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, Mora S, Gibson H, Gordon D, Copeland T, D’Agostino D, Friedenberg G. Vitamin D supplements and prevention of cancer and cardiovascular disease. New England Journal of Medicine . 2019 Jan 3;380(1):33-44.
- Keum N, Lee DH, Greenwood DC, Manson JE, Giovannucci E. Vitamin D supplementation and total cancer incidence and mortality: a meta-analysis of randomized controlled trials. Annals of Oncology . 2019 May 1;30(5):733-43.
- Giovannucci E. Expanding roles of vitamin D. J Clin Endocrinol Metab . 2009; 94:418-20.
- Norman PE, Powell JT. Vitamin D and cardiovascular disease. Circulation research . 2014 Jan 17;114(2):379-93.
- Holick MF. The vitamin D deficiency pandemic and consequences for nonskeletal health: mechanisms of action. Molecular aspects of medicine . 2008 Dec 1;29(6):361-8.
- Giovannucci E, Liu Y, Hollis BW, Rimm EB. 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Archives of internal medicine . 2008 Jun 9;168(11):1174-80.
- Pilz S, März W, Wellnitz B, Seelhorst U, Fahrleitner-Pammer A, Dimai HP, Boehm BO, Dobnig H. Association of vitamin D deficiency with heart failure and sudden cardiac death in a large cross-sectional study of patients referred for coronary angiography. The Journal of Clinical Endocrinology & Metabolism . 2008 Oct 1;93(10):3927-35.
- Pilz S, Dobnig H, Fischer JE, Wellnitz B, Seelhorst U, Boehm BO, März W. Low vitamin D levels predict stroke in patients referred to coronary angiography. Stroke . 2008 Sep 1;39(9):2611-3.
- Booth TW, Lanier PJ. Vitamin D deficiency and risk of cardiovascular disease. Circulation Res117. 2008;503:511.
- Dobnig H, Pilz S, Scharnagl H, Renner W, Seelhorst U, Wellnitz B, Kinkeldei J, Boehm BO, Weihrauch G, Maerz W. Independent association of low serum 25-hydroxyvitamin D and 1, 25-dihydroxyvitamin D levels with all-cause and cardiovascular mortality. Archives of internal medicine . 2008 Jun 23;168(12):1340-9.
- Elamin MB, Abu Elnour NO, Elamin KB, Fatourechi MM, Alkatib AA, Almandoz JP, Liu H, Lane MA, Mullan RJ, Hazem A, Erwin PJ. Vitamin D and cardiovascular outcomes: a systematic review and meta-analysis. The Journal of Clinical Endocrinology & Metabolism . 2011 Jul 1;96(7):1931-42.
- Mitri J, Pittas AG. Vitamin D and diabetes. Endocrinol Metab Clin North Am . 2014 Mar;43(1):205-32.
- Pittas AG, Dawson-Hughes B, Li T, Van Dam RM, Willett WC, Manson JE, Hu FB. Vitamin D and calcium intake in relation to type 2 diabetes in women. Diabetes care . 2006 Mar 1;29(3):650-6.
- Pittas AG, Dawson-Hughes B, Sheehan P, Ware JH, Knowler WC, Aroda VR, Brodsky I, Ceglia L, Chadha C, Chatterjee R, Desouza C, Dolor R, Foreyt J, Fuss P, Ghazi A, Hsia DS, Johnson KC, Kashyap SR, Kim S, LeBlanc ES, Lewis MR, Liao E, Neff LM, Nelson J, O’Neil P, Park J, Peters A, Phillips LS, Pratley R, Raskin P, Rasouli N, Robbins D, Rosen C, Vickery EM, Staten M; D2d Research Group. Vitamin D Supplementation and Prevention of Type 2 Diabetes. N Engl J Med . 2019 Aug 8;381(6):520-530
- Dobson R, Giovannoni G. Multiple sclerosis–a review. European journal of neurology . 2019 Jan;26(1):27-40.
- Goldberg P. Multiple sclerosis: vitamin D and calcium as environmental determinants of prevalence: (A viewpoint) part 1: sunlight, dietary factors and epidemiology. International Journal of Environmental Studies . 1974 Jan 1;6(1):19-27.
- Munger KL, Zhang SM, O’reilly E, Hernan MA, Olek MJ, Willett WC, Ascherio A. Vitamin D intake and incidence of multiple sclerosis. Neurology . 2004 Jan 13;62(1):60-5.
- Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. Jama . 2006 Dec 20;296(23):2832-8.
- Salzer J, Hallmans G, Nyström M, Stenlund H, Wadell G, Sundström P. Vitamin D as a protective factor in multiple sclerosis. Neurology . 2012 Nov 20;79(21):2140-5.
- Munger KL, Hongell K, Åivo J, Soilu-Hänninen M, Surcel HM, Ascherio A. 25-Hydroxyvitamin D deficiency and risk of MS among women in the Finnish Maternity Cohort. Neurology . 2017 Oct 10;89(15):1578-83.
- Ascherio A, Munger KL, White R, Köchert K, Simon KC, Polman CH, Freedman MS, Hartung HP, Miller DH, Montalbán X, Edan G. Vitamin D as an early predictor of multiple sclerosis activity and progression. JAMA neurology . 2014 Mar 1;71(3):306-14.
- Fitzgerald KC, Munger KL, Köchert K, Arnason BG, Comi G, Cook S, Goodin DS, Filippi M, Hartung HP, Jeffery DR, O’Connor P. Association of vitamin D levels with multiple sclerosis activity and progression in patients receiving interferon beta-1b. JAMA neurology . 2015 Dec 1;72(12):1458-65.
- Ascherio A, Munger KL. Epidemiology of multiple sclerosis: from risk factors to prevention—an update. InSeminars in neurology 2016 Apr (Vol. 36, No. 02, pp. 103-114). Thieme Medical Publishers.
- Gillespie KM. Type 1 diabetes: pathogenesis and prevention. Cmaj . 2006 Jul 18;175(2):165-70.
- Hyppönen E, Läärä E, Reunanen A, Järvelin MR, Virtanen SM. Intake of vitamin D and risk of type 1 diabetes: a birth-cohort study. The Lancet . 2001 Nov 3;358(9292):1500-3.
- Rewers M, Ludvigsson J. Environmental risk factors for type 1 diabetes. The Lancet . 2016 Jun 4;387(10035):2340-8.
- Munger KL, Levin LI, Massa J, Horst R, Orban T, Ascherio A. Preclinical serum 25-hydroxyvitamin D levels and risk of type 1 diabetes in a cohort of US military personnel. American journal of epidemiology . 2013 Mar 1;177(5):411-9.
- Hope-Simpson RE. The role of season in the epidemiology of influenza. Epidemiology & Infection . 1981 Feb;86(1):35-47.
- Cannell JJ, Vieth R, Umhau JC, Holick MF, Grant WB, Madronich S, Garland CF, Giovannucci E. Epidemic influenza and vitamin D. Epidemiology & Infection . 2006 Dec;134(6):1129-40.
- Ginde AA, Mansbach JM, Camargo CA. Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Archives of internal medicine . 2009 Feb 23;169(4):384-90.
- Urashima M, Segawa T, Okazaki M, Kurihara M, Wada Y, Ida H. Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren. The American journal of clinical nutrition . 2010 May 1;91(5):1255-60.
- Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa D, Ginde AA, Goodall EC. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ . 2017 Feb 15;356:i6583.
- Zasloff M. Fighting infections with vitamin D. Nature medicine . 2006 Apr;12(4):388-90.
- Nnoaham KE, Clarke A. Low serum vitamin D levels and tuberculosis: a systematic review and meta-analysis. International journal of epidemiology . 2008 Feb 1;37(1):113-9.
- Chocano-Bedoya P, Ronnenberg AG. Vitamin D and tuberculosis. Nutrition reviews . 2009 May 1;67(5):289-93.
- Autier P, Gandini S. Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Archives of internal medicine . 2007 Sep 10;167(16):1730-7.
- Giovannucci E. Can vitamin D reduce total mortality?. Archives of Internal Medicine . 2007 Sep 10;167(16):1709-10.
- Sutherland JP, Zhou A, Hyppönen E. Vitamin D Deficiency Increases Mortality Risk in the UK Biobank: A Nonlinear Mendelian Randomization Study. Annals of Internal Medicine . 2022 Oct 25.
- Navale SS, Mulugeta A, Zhou A, Llewellyn DJ, Hyppönen E. Vitamin D and brain health: an observational and Mendelian randomization study. The American Journal of Clinical Nutrition . 2022 Apr 22.
- Tripkovic L, Lambert H, Hart K, Smith CP, Bucca G, Penson S, Chope G, Hyppönen E, Berry J, Vieth R, Lanham-New S. Comparison of vitamin D2 and vitamin D3 supplementation in raising serum 25-hydroxyvitamin D status: a systematic review and meta-analysis. The American journal of clinical nutrition . 2012 Jun 1;95(6):1357-64.
- Wilson LR, Tripkovic L, Hart KH, Lanham-New SA. Vitamin D deficiency as a public health issue: using vitamin D 2 or vitamin D 3 in future fortification strategies. Proceedings of the Nutrition Society . 2017 Aug;76(3):392-9.
- Holick MF. Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr . 2004; 79:362-71
- Holick MF. Vitamin D deficiency. N Engl J Med . 2007; 357:266-81.
- Hahn J, Cook NR, Alexander EK, Friedman S, Walter J, Bubes V, Kotler G, Lee IM, Manson JE, Costenbader KH. Vitamin D and marine omega 3 fatty acid supplementation and incident autoimmune disease: VITAL randomized controlled trial. BMJ . 2022 Jan 26;376:e066452.
- LeBoff MS, Chou SH, Ratliff KA, et al. Supplemental Vitamin D and Incident Fractures in Midlife and Older Adults. N Engl J Med . 2022 Jul 28;387:299-309.
- LeBoff MS, Murata EM, Cook NR, Cawthon P, Chou SH, Kotler G, Bubes V, Buring JE, Manson JE. VITamin D and OmegA-3 TriaL (VITAL): effects of vitamin D supplements on risk of falls in the US population. The Journal of Clinical Endocrinology & Metabolism . 2020 Sep;105(9):2929-38.
- Ames BN, Grant WB, Willett WC. Does the high prevalence of vitamin D deficiency in African Americans contribute to health disparities?. Nutrients . 2021 Feb 3;13(2):499. *W.B.G. receives funding from Bio-Tech Pharmacal, Inc. (Fayetteville, AR). The other authors have no conflicts of interest to declare.
Last reviewed March 2023
Terms of Use
The contents of this website are for educational purposes and are not intended to offer personal medical advice. You should seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The Nutrition Source does not recommend or endorse any products.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 20 January 2020
Vitamin D deficiency 2.0: an update on the current status worldwide
- Karin Amrein ORCID: orcid.org/0000-0003-0915-085X 1 , 2 ,
- Mario Scherkl 1 ,
- Magdalena Hoffmann ORCID: orcid.org/0000-0003-1668-4294 1 , 3 , 4 ,
- Stefan Neuwersch-Sommeregger 5 , 6 ,
- Markus Köstenberger 5 , 6 ,
- Adelina Tmava Berisha 7 ,
- Gennaro Martucci ORCID: orcid.org/0000-0001-8443-2414 8 ,
- Stefan Pilz 1 &
- Oliver Malle 1
European Journal of Clinical Nutrition volume 74 , pages 1498–1513 ( 2020 ) Cite this article
213k Accesses
674 Citations
510 Altmetric
Metrics details
- Endocrine system and metabolic diseases
- Risk factors
Vitamin D testing and the use of vitamin D supplements have increased substantially in recent years. Currently, the role of vitamin D supplementation, and the optimal vitamin D dose and status, is a subject of debate, because large interventional studies have been unable to show a clear benefit (in mostly vitamin D replete populations). This may be attributed to limitations in trial design, as most studies did not meet the basic requirements of a nutrient intervention study, including vitamin D-replete populations, too small sample sizes, and inconsistent intervention methods regarding dose and metabolites. Vitamin D deficiency (serum 25-hydroxyvitamin D [25(OH)D] < 50 nmol/L or 20 ng/ml) is associated with unfavorable skeletal outcomes, including fractures and bone loss. A 25(OH)D level of >50 nmol/L or 20 ng/ml is, therefore, the primary treatment goal, although some data suggest a benefit for a higher threshold. Severe vitamin D deficiency with a 25(OH)D concentration below <30 nmol/L (or 12 ng/ml) dramatically increases the risk of excess mortality, infections, and many other diseases, and should be avoided whenever possible. The data on a benefit for mortality and prevention of infections, at least in severely deficient individuals, appear convincing. Vitamin D is clearly not a panacea, and is most likely efficient only in deficiency. Given its rare side effects and its relatively wide safety margin, it may be an important, inexpensive, and safe adjuvant therapy for many diseases, but future large and well-designed studies should evaluate this further. A worldwide public health intervention that includes vitamin D supplementation in certain risk groups, and systematic vitamin D food fortification to avoid severe vitamin D deficiency, would appear to be important. In this narrative review, the current international literature on vitamin D deficiency, its relevance, and therapeutic options is discussed.
Similar content being viewed by others

Targeted 25-hydroxyvitamin D concentration measurements and vitamin D3 supplementation can have important patient and public health benefits
Official recommendations for vitamin d through the life stages in developed countries.

The health effects of vitamin D supplementation: evidence from human studies
Introduction.
Vitamin D testing has exponentially increased in recent years [ 1 ]. The definition and relevance of vitamin D deficiency are still under debate. Recent large observational data have suggested that ~40% of Europeans are vitamin D deficient, and 13% are severely deficient [ 2 ]. The relevance of this widespread deficiency and necessity for supplementation has been questioned [ 3 ]. Certainly, vitamin D is not a panacea. Because more often than not, trials have included non-deficient individuals, it is not surprising that interventional trials have usually not been able to find a benefit of vitamin D supplementation on clinical outcomes. This was also reflected in meta-analyses on the topic that were carried out with poor methodological standards [ 4 ]. Consequently, many authors have dismissed a role of vitamin D on important clinical outcomes, and suggested that vitamin D may be more an associative than a causal factor in acute and chronic disease.
On the other hand, a low vitamin D status is emerging as a very common condition worldwide, and several studies from basic science to clinical applications have highlighted a strong association with chronic diseases, as well as acute conditions. Moreover, the large amount of observational data currently available are also accompanied by pathophysiological associations of vitamin D with energy homeostasis, and regulation of the immune and endocrine systems [ 5 ].
Recent negative interventional trials may be biased by substantial methodological and study design errors, making it impossible to show the potential contributing role of vitamin D supplementation in a deficient population. Typically, most studies have missed important prerequisites for a nutrient intervention trial: the absence of the problem to be solved—vitamin D deficiency, often ridiculously small sample sizes, and varying interventional regimes regarding dose and metabolite. Even the recent very large trials did not exclusively include deficient populations [ 6 , 7 , 8 ]. Moreover, interventional regimes have used a one-size-fits-all approach without taking into account individual differences in BMI and vitamin D metabolism.
Articles were individually retrieved up to October 2019 by search in PubMed (MEDLINE). Studies were excluded if they were not in English. Across the last few decades, vitamin D-related research/publications have dramatically increased. Therefore, we decided to focus on the largest, most relevant, and most recent studies that are now in this version of the review.
All authors supplied a first draft paper on a specific topic. All papers were then exchanged and discussed among authors by e-mail.
Definition of vitamin D deficiency
Serum 25(OH)D is considered to be the best marker for assessing vitamin D status, and reliably reflects the free fractions of the vitamin D metabolites, despite the fact that, in theory, the bioavailable fractions may be more clinically informative [ 9 , 10 ]. A range of below 75 nmol/L (or 30 ng/ml) of serum/plasma 25(OH)D concentration is considered vitamin D deficiency by most authors [ 11 , 12 ]. A cutoff of <25 or <30 nmol/L (or 10/12 ng/ml) increases the risk of osteomalacia and nutritional rickets dramatically, and therefore is considered to determine severe vitamin D deficiency [ 13 , 14 , 15 , 16 ]. The clinical practice guidelines of the Endocrine Society Task Force on Vitamin D [ 12 ] have defined a cutoff level of 50 nmol/L as vitamin D deficient. Furthermore, different societies and expert bodies have defined 50 nmol/L as “vitamin D requirement of nearly all normal healthy persons,” by using bone health as the main basis. For example, a cutoff level of 50 nmol/L is recommended by the Institute of Medicine (IOM, USA) in their “Dietary Reference Intakes”. Vitamin D levels of <30 nmol/L (or 12 ng/ml) should likely be prevented with a public health approach [ 17 ]. There are many large and relevant risk groups for vitamin D deficiency (Table 1 ).
Prevalence of vitamin D deficiency worldwide
Prevalence rates of severe vitamin D deficiency, defined as 25(OH)D <30 nmol/L (or 12 ng/ml), of 5.9% (US) [ 18 ], 7.4% (Canada) [ 19 ], and 13% (Europe) [ 2 ] have been reported. Estimates of the prevalence of 25(OH)D levels <50 nmol/L (or 20 ng/ml) have been reported as 24% (US), 37% (Canada), and 40% (Europe) [ 2 , 17 , 18 , 19 ]. This may vary by age, with lower levels in childhood and the elderly [ 17 ], and also ethnicity in different regions, for example, European Caucasians show lower rates of vitamin D deficiency compared with nonwhite individuals [ 2 , 17 ]. Worldwide, many countries report very high prevalences of low vitamin D status. 25(OH)D levels <30 nmol/L (or 12 ng/ml) in >20% of the population are common in India, Tunisia, Pakistan, and Afghanistan. For example, it has been estimated that 490 million individuals are vitamin D deficient in India [ 2 , 17 ].
Specific categories of patients have a very high prevalence of vitamin D deficiency. Often, they are characterized by an insufficiency or failure of organs involved in vitamin D metabolism. Patients with chronic renal failure and on hemodialysis, renal transplant recipients affected with liver disease or after liver transplantation may have a prevalence of vitamin D deficiency ranging from 85 to 99% [ 20 , 21 , 22 ].
Vitamin D deficiency in critical illness
Similarly, critically ill patients have a very high prevalence of vitamin D deficiency, and low vitamin D levels are clearly associated with greater illness severity, morbidity, and mortality in both adult and pediatric intensive care unit (ICU) patients, as well as medical and surgical ICUs [ 23 ]. However, as in most other populations, the most important question remains unanswered: whether low vitamin D is an innocent bystander, simply reflecting greater disease severity, or represents an independent and modifiable risk factor amenable to rapid normalization through loading dose supplementation [ 24 , 25 ].
The question is meaningful, since in this subgroup of patients, many factors contribute to low levels: hemodilution, reduced production and conversion by the liver, reduced synthesis of vitamin D-binding protein, higher consumption during the acute phase of disease and systemic inflammation, and increased tissue demand and enhanced catabolism of metabolites. More data are emerging from basic science about the immediate and late effects of vitamin D supplementation on endocrine, autocrine, and paracrine and genomic targets.
Vitamin D replacement
Metabolites.
It cannot be emphasized enough that various vitamin D metabolites with a very different efficacy, half-life, and risk of toxicity exist. This is discussed in detail in “Vitamin D supplementation: cholecalciferol, calcifediol and calcitriol” by Reinold Vieth et al. in this special issue.
Interval, target level, and dose
For some time, bolus dosing was en vogue because it was thought to be interesting for practical reasons. With the exception of critical care, bolus doses with long dosing intervals are not used. They are no longer recommended because of the higher risk of adverse effects (falls and fractures) associated with them [ 26 ]. Moreover, the 2017 individual patient data meta-analysis by Martineau et al. showed a clear benefit for vitamin D on acute respiratory infection when daily or weekly dosing was used, but not with longer dosing intervals [ 16 ]. In the intensive care, however, a typical daily dose is inefficient, and an upfront loading dose (followed by a daily dose) is necessary to improve vitamin D levels rapidly [ 27 ].
It is also important to note that different dosing regimes may have different effects on clinical outcomes. Because a daily dose leads to stable availability of various vitamin D metabolites, this could be an important explanation for many of the negative vitamin D intervention trials [ 28 ].
To maintain optimal vitamin D status, use of vitamin D supplementation is often required, as sunlight exposure and dietary intake alone is usually insufficient in most individuals [ 29 , 30 , 31 ]. Currently, there is no international consensus on the optimal level for vitamin D supplementation. Recommendations differ in many countries, and range from 400 to 2000 IU daily [ 11 ]. A safe and commonly available dose of 25 μg of vitamin D3 (1000 IU) raises 25-hydroxyvitamin D [25(OH)D] serum level by 15–25 nmol/L on average (over weeks/months) [ 32 , 33 ]; it should be noted that there is a nonlinear response of serum 25(OH)D, with a steeper rise with <1 IU/day of vitamin D, and a more flattened response with >1 IU/day. This is evidenced by several studies in all age groups [ 11 , 34 ].
By using the above-mentioned recommended vitamin D supplementation levels, there is no need to monitor serum or urinary calcium or renal function [ 35 , 36 ]. There is no international consensus on the safe upper level for vitamin D supplementation. While the upper daily limit given by the Endocrine Society is 10,000 IU [ 12 ], the IOM and The European Food and Safety Authority recommend staying below 4000 IU/day (100 µg) [ 37 , 38 ]. Most countries have prudently set the safe upper level at 50 μg daily (2000 IU) for adults [ 35 ]. However, this level was set despite the availability of adequate studies of dose–response relationships or toxicity. There is no convincing evidence that daily intakes of up to 125 μg (5000 IU) elicit severe adverse effects [ 39 ]. It has been reported that an intake of 1250 µg (50,000 IU) once every 2 weeks for several years, equivalent to 89.3 µg (3571 IU) daily, did not cause hypercalcemia or other evidence of hypervitaminosis D [ 40 ]. Small studies showed that even a daily consumption of up to 250 μg (10,000 IU) of vitamin D over long periods did not cause adverse effects in healthy adults [ 32 , 33 ], though some studies revealed a negative impact on bone mineral density by using high-dose vitamin D supplementation of 10,000 IU/day [ 11 ]. Nevertheless, supplementation of >10,000 IU of vitamin D is rarely necessary in clinical practice.
As there is no evidence that increasing the recommended daily dose of vitamin D supplementation up to 50 μg (2000 IU) would cause severe side effects in the general population, and considering that 20 μg (800 IU) is the lowest dose consistently associated with a bone benefit, it seems reasonable to recommend a daily dose of 20–50 μg (800–2000 IU) (levels 2–4 evidence, grades B–D recommendation) [ 39 ]. In general, a daily vitamin D of 800 IU appears to be sufficient to achieve a target 25(OH)D level of at least 50 nmol/L (or 20 ng/mL) in most healthy individuals, whereas 2000 IU is sufficient to achieve a level of at least 75 nmol/L (or 30 ng/mL).
Some data suggest that a higher 25(OH)D level than 50 nmol/L (or 20 ng/mL) may be required for optimal risk reduction for various endpoints [ 41 , 42 , 43 , 44 ].
The use of vitamin D supplementation has increased substantially. Growing awareness of vitamin D in the general population, and over-the-counter vitamin D with partially very high doses, include the risk for uncontrolled use and exogenous hypervitaminosis D, resulting in high concentrations of serum 25(OH)D or free 1,25-dihydroxyvitamin D [1,25(OH) 2 D], leading to hypercalciuria and finally hypercalcemia [ 45 ]. Reports of vitamin D overdose are rare in the literature. Serum 25(OH)D usually exceeds 375 nmol/l (or 150 ng/ml), and factors such as high-calcium intake contribute to the risk of hypercalcemia [ 46 ]. However, there are also endogenous causes of hypervitaminosis D, such as increased production of 1,25(OH) 2 D as part of granulomatous disorders or lymphomas [ 47 ]. Having a long half-life in the tissues, vitamin D accumulation due to excessive intake lasts up to 18 months [ 48 ], and may cause chronic toxic effects such as nephrocalcinosis following hypercalcemia and hypercalciuria [ 47 ].
Since the 1930s, public health officials in the United States and the United Kingdom have recommended routine fortification of foods like milk to prevent vitamin D deficiency and low vitamin D status, which was expected to be an effective public health strategy [ 46 ]. However, there was an increased incidence of hypercalcemia due to massive intakes of vitamin D from various food fortifications. In some cases, hypercalcemia was associated with drinking vitamin D-fortified milk, revealing a fortification of up to 232,565 IU instead of standard 400 IU/quart, and consequently, prohibition of milk fortification [ 49 ]. However, current evidence suggests that vitamin D fortification prevents deficiency safely and effectively [ 50 , 51 ]. Feeding animals might represent an additional source of vitamin D without compromising product quality. For example, consumption of vitamin D-enriched eggs from hens fed with additional vitamin D3 resulted in a zero prevalence <25 nmol/L, while the control group showed an usual seasonal decline in winter with 22% being <25 nmol/L [ 52 ]. The rationale and guidance for systematic vitamin D food fortification, including a call for action, has recently been published by an expert group of vitamin D scientists.
Selected RCTs in recent years
Several very large randomized controlled trials have been or are being performed in recent years. They are summarized in Table 2 [ 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 ].
Effect size and basic statistical principles
Though it appears attractive to dismiss any relevant effect of vitamin D on all the conditions that have been studied in those partly very large trials in recent years, it must be considered that often the basic principles for optimal design of a nutrient intervention study were not fulfilled [ 64 ], e.g., measurement of vitamin D at baseline and choosing vitamin D deficiency as an inclusion criterion, using a meaningful intervention able to change vitamin D status, and verification of vitamin D status improvement by repeat measurement.
Moreover, even in the largest trials including thousands of individuals, the sample size was still too small when mostly individuals without vitamin D deficiency and a low baseline risk were included. By modeling future intervention trials, Brenner et al. reported that several hundreds of thousands of participants would be necessary to be able to show an effect on mortality [ 65 ].
On the other hand, even a very small effect may be useful for a substance with such an excellent safety profile and low cost, especially when considering a public health approach. However, to show a small, but meaningful benefit on important outcomes like mortality or infections, very large population samples are needed, but such trials are very costly and will likely be scant.
Important systematic reviews and meta-analyses
The association of vitamin D supplementation on a number of endpoints including mortality has been explored in more detail in the last few years. Selected relevant systematic reviews and meta-analyses are summarized in Table 3 [ 16 , 66 , 67 ].
Selected target organs, conditions, and endpoints
Vitamin D deficiency has been strongly associated with various health outcomes, including all-cause mortality [ 68 ]. A 2014 Cochrane meta-analysis showed a relevant and significant lower all-cause mortality of ~7% and cancer mortality of ~13% in patients who received vitamin D3 [ 69 ]. The results of a meta-analysis by using individual participant data conducted by Gaksch et al., analyzing almost 17,000 individuals, showed a strong association between low 25(OH)D and increased risk of all-cause mortality [ 70 ]. Using a Mendelian randomization with genetic variants in the vitamin D synthesis pathway, the analysis of Aspelund et al. supports a causal relationship between vitamin D deficiency and increased all-cause mortality. However, despite a cohort of >10,000 participants, it was still too underpowered to confirm a causal relationship [ 71 ].
The effect of vitamin D on the lungs has a strong rationale, demonstrated by basic science, due to its immunomodulant, anti-inflammatory, and anti-infective role that has been highlighted in patients with community-acquired infections, acute respiratory failure, as well as in lung transplantation recipients (this is a very specific model for severe infective and inflammatory lung disease) [ 21 ].
Vitamin D supplementation reveals direct anti-inflammatory properties in the lungs. This is due to local inhibition of nuclear factor-κB and mitogen-activated protein kinase activity, reducing the secretion of inflammatory cytokines and chemokines involved in the lung inflammatory process and extravascular leaking, such as interleukin (IL)-1β, IL-6, and IL-8. This, in turn, also influences the number of inflammatory cells infiltrating the interstitial space [ 72 ]. Moreover, 1,25(OH) 2 D is also implicated in the reduction of oxidative stress by inhibiting anti-protease activity, and acting on the nuclear factor erythroid-related factor 2, a transcriptional regulator of most antioxidant genes. Moreover, vitamin D acts with well-known anti-infectious properties by increasing proliferation of monocytes to macrophages (acting as a fine-tuner of the innate and adaptive immunity), and determining a transcriptional upregulation of cathelicidin also in the airway epithelial cells. Finally, 1,25(OH) 2 D inhibits the expression of several metalloproteinases in airway smooth-muscle cells and alveolar macrophages, thus being involved in the tissue remodeling pathway by regulating the process of bronchial airway muscle activation and extracellular matrix deposition by fibroblasts. All these complex pathways, partially modified by vitamin D, warrant supplementation in patients with respiratory disease. Significant benefits have already been shown in adults and children with asthma, and for the prevention of respiratory tract infections, particularly in severe vitamin D deficiency.
Sepsis, a complication of severe infection, is characterized by signs of systemic inflammation expressed with failure of organs often remote from the site of the initial infection. Septic patients have high mortality and lower circulating levels of vitamin D. The interest in vitamin D for infection has risen after the recognition of the expression of the vitamin D receptor, ubiquitous in cells of the innate and adaptive immune system. Vitamin D is an important link between Toll-like receptor activation and antibacterial responses. The in vivo supplementation of a high dose of cholecalciferol (400.000 IU as a single bolus) in the early stage of sepsis and septic shock has been shown able to safely and rapidly increase the level of vitamin D, as well as the circulating level of cathelicidin, a vitamin D-dependent endogenous anti-microbial and endotoxin-binding peptide largely found in human neutrophils [ 73 ]. These findings were corroborated by the significant reduction of IL-1β and IL-6, which play important roles in the early inflammatory response.
Organ transplantation recipients
Several studies have highlighted that lower 25(OH)D levels are associated with prolonged hospitalization and mortality, also in the postsurgical setting. Given its wide immunobiological effects, vitamin D has been frequently considered a potential modulating factor after solid organ (and stem cell) transplantation (mainly liver, kidney, and lung). The transplantation recipient population is particularly prone to infections, mainly in the early stage after transplantation, due to immunomodulation/chronic immunosuppressive therapy and to long-term bone dysfunction. The recipients of solid organ transplantation are, by definition, vitamin D insufficient for manifold reasons, including limited sunlight exposure, limited physical activity, reduced dietary intake of vitamin D in food, as well as liver and kidney dysfunction according to their main disease. As an example, in liver transplantation recipients (a group of patients with very low vitamin D levels), osteoporosis has a high prevalence, with a large decline in bone mineral density in the first year after transplantation. Moreover, a negative association between low vitamin D levels and graft function, as well as a role of vitamin D in reducing the recurrence of hepatitis C virus infection, has been demonstrated. Several interventional trials on vitamin D supplementation in lung and kidney recipients are ongoing under the hypothesis that vitamin D supplementation may contribute to reducing the occurrence of rejection by it immunomodulating action.
In 2019, two Cochrane analyses on vitamin D and pregnancy were published. They suggested that vitamin D supplementation may reduce gestational diabetes, low birthweight, and preeclampsia, but a higher than currently recommended dose appeared to have no additional benefit except for possible further reduction of gestational diabetes [ 74 , 75 ]. However, several studies in recent years have highlighted that women are at high risk for vitamin D deficiency, and this is associated with adverse pregnancy outcomes, including preeclampsia and gestational diabetes [ 76 , 77 , 78 , 79 , 80 ]. It has been demonstrated that vitamin D supplementation is able to reduce adverse pregnancy outcomes when a higher level is achieved, with an increasing efficacy when the target level is raised from 20 to 40 ng/mL or 50 ng/mL. Interestingly, the maximum change is achieved 6–8 weeks after initiating the treatment, likely exerting the genomic actions of vitamin D [ 81 , 82 , 83 ]. Three major adverse pregnancy outcomes appear to improve with vitamin D supplementation: a 60% reduction in preeclampsia, a 50% reduction in gestational diabetes, and a 40% reduction in preterm delivery [ 84 ]. These data are consistent with previous work on the topic [ 82 ]. Moreover, following the genomic and epigenetic effects of vitamin D supplementation, vitamin D deficiency during pregnancy also seems able to induce specific genomic pathways relevant to autoimmune disease in childhood and later in life [ 85 , 86 ]. The placenta can convert 25(OH)D to the active form 1,25(OH) 2 D, similarly to the kidneys; therefore, more basic research should shed light in the future on the specific vitamin D metabolism during pregnancy [ 85 ]. The FDA has recently approved the statement “Pregnant women who have higher serum vitamin D levels have a decreased risk of preterm birth.”
Taking into account the recent literature, vitamin D deficiency is associated with worse outcomes during pregnancy, and at least 400–600 IU of daily vitamin D supplementation is reasonable for women with a vitamin D level <40 ng/mL, with higher required doses in more severe deficiency.
Vitamin D supplementation as a strategy for preventing cancer was considered, as results from several observational studies suggested an association between vitamin D deficiency and risk for several types of cancer [ 87 ]. It was already assumed in 1980 that calcitriol could inhibit the growth of malignant melanoma cells [ 88 ]. Ecologic studies revealed a decreased cancer mortality in areas with greater sun exposure [ 11 ]. Over the decades, vitamin D and its anticancer action was investigated for various malignancies resulting in mixed findings [ 89 ]. Hence, the cancer-protective effect of vitamin D remained unclear. In 2014, two meta-analyses revealed no significant decrease in the incidence of cancer in association with vitamin D supplementation, but a significant reduction in the rate of death from cancer [ 90 , 91 ]. However, as most of the data derive from observational studies, correlation does not imply causation. Investigating cancer incidence following vitamin D plus calcium supplementation, Lappe et al. revealed a non-, but nearly significant (hazard ratio 0.70; 95% CI 0.47–1.02) 30% risk reduction compared with placebo [ 92 ]. A recent large RCT using a daily dose of 2000 IU vitamin D3 conducted by Manson et al. [ 7 ], analyzing the incidence of cancer following vitamin D supplementation in over 25,000 participants, did not reveal a significant reduction neither of invasive cancer of any type nor in the rate of death from any cause. However, subgroup analyses revealed a significant lower cancer incidence in normal-weight individuals. Considering that the study was not adjusted for this comparison, this finding should be considered hypothesis-generating. An ongoing long-term RCT [ 93 ], investigating vitamin D supplementation and the incidence of cancer and precancerous lesions in a high-risk population (overweight adults with prediabetes), will provide further and important data on the causality.
Several studies demonstrated a link between 25(OH)D levels and diabetes, and revealed a higher frequency of vitamin D deficiency in patients with type 1 diabetes mellitus (T1DM) compared with healthy individuals [ 94 , 95 , 96 , 97 ]. Investigating prenatal vitamin D exposure of the fetus, a lower gestational 25(OH)D level [ 98 ] or avoiding vitamin D-fortified food [ 99 ] was significantly associated with higher risk of developing T1DM. In infancy, vitamin D supplementation [ 100 ] or vitamin D-fortified margarine [ 99 ] was shown to reduce the risk of developing type 1 diabetes mellitus. The effect of vitamin D supplementation on T1DM onset seems to be dependent on life stage. Supplementation between 7 and 12 months of age resulted in an almost twofold lower risk of developing T1DM compared with earlier supplementation [ 101 ]. In adolescents, many studies revealed no association between 25(OH)D level and onset of T1DM [ 102 , 103 , 104 ]. However, there is a clear effect of vitamin D in young adults, as low 25(OH)D levels were significantly associated with developing T1DM [ 105 ]. However, according to the available literature, the cause-and-effect relationship is inconclusive. On the other hand, diabetes per se results in physiological changes too, such as increased renal elimination of vitamin D-binding protein compared with healthy individuals [ 106 ]. Therefore, the value of hypovitaminosis D as a trigger for developing T1DM remains unclear. Vitamin D deficiency was also shown to have a negative impact on insulin resistance [ 107 ]. Hence, a higher risk of developing type 2 diabetes mellitus (T2DM) in individuals with low 25(OH)D levels was assumed. However, vitamin D supplementation did overall not result in a lower risk of developing T2DM [ 6 , 108 ]. In the recent D2D study by Pittas et al., vitamin D did not significantly reduce new onset of diabetes, but vitamin D deficiency was no inclusion criterion, and only a minority of included patients had a 25(OH)D level <50 nmol//L (or 20 ng/mL). Moreover, the hypothesized treatment effect used for the sample size calculation was relatively large (hazard ratio 0.75 for the vitamin D group). The actual hazard ratio for vitamin D as compared with placebo was 0.88 (95% confidence interval, 0.75–1.04; P = 0.12). Interestingly, the effect appeared to be stronger in patients with a BMI <30. However, a post hoc subgroup analysis of individuals with a 25(OH)D level below 12 ng/ml (30 nmol/l) revealed a significantly reduced risk of developing T2DM (hazard ratio 0.38; 95% CI, 0.18–0.80).
Musculoskeletal effects of vitamin D
The detrimental effects of vitamin D deficiency on the musculoskeletal system were the first visible mode of action that was attributed to vitamin D (i.e., rickets in children).
The necessity of an adequate vitamin D status for muscle and bone health is undebated, and therefore not discussed in detail in this review.
Vitamin D intoxication and hypersensitivity
Vitamin D intoxication is rare and usually only occurs at very high supplementation doses [ 109 ]. However, various mutations in vitamin D metabolizing enzymes that may lead to increased sensitivity to standard vitamin D supplementation or even endogenous vitamin D intoxication with hypercalcemia, hypercalciuria, and nephrocalcinosis/chronic renal insufficiency have been described [ 110 ]. Typically, these mutations affect CYP24A1, the enzyme that catabolizes 1,25OHD2 to the inactive metabolite 24,25OHD2. Therefore, a diagnosis can be made by using the ratio of 24,25:25 D and does not necessarily require genetic testing.
This condition has been termed idiopathic infantile hypercalcemia, but due to the greatly varying clinical phenotypes, patients may well become symptomatic only in adulthood. Currently, no causal treatment is available, but avoidance of a high-calcium diet, UV-B exposure, and vitamin D or calcium supplements is advised.
Vitamin D deficiency is highly prevalent, but the literature to support vitamin D supplementation is unsatisfactory to date. Unless major funding sources are used for vitamin D research, it appears sensible to focus on vitamin D-deficient populations with a high event rate. Vitamin D is clearly not a panacea, but may be an important, inexpensive, and safe adjuvant therapy for many diseases and stages of life, including pregnancy, childhood, and old age. Public health efforts to prevent severe vitamin D deficiency should therefore be further promoted.
In the critically ill setting, one large vitamin D supplementation trial has recently been published (VIOLET [ 111 ]) and one is still ongoing (NCT03096314 and NCT03188796). VIOLET randomized patients with 25(OH)D levels below 50 nmol/L (or 20 ng/ml) “at risk for ARDS” to one single high dose of vitamin D3 (540,000 IU), and evaluated its effect on the primary outcome: 90-day mortality. It was prematurely stopped in mid-2018 after inclusion of ca. One-third of the patients originally planned, and no differences in mortality and secondary endpoints have been reported, with no differences in subgroup analyses and safety endpoints [ 111 ].
VITDALIZE is a European multicenter RCT, including severely vitamin D-deficient ICU patients with a 25 OH D level <30 nmol/L (or 12 ng/ml), and randomizes patients to a loading dose of oral/enteral vitamin D3 (540,000 IU) followed by 4000 IU daily for 90 days, with the primary outcome being 28-day mortality. Recruitment is ongoing in Austria and Belgium, should be expanded to other European countries in 2020, and will likely continue for a few more years.
Crowe FL, Jolly K, MacArthur C, Manaseki-Holland S, Gittoes N, Hewison M, et al. Trends in the incidence of testing for vitamin D deficiency in primary care in the UK: a retrospective analysis of The Health Improvement Network (THIN), 2005–2015. BMJ Open. 2019;9:e028355. https://doi.org/10.1136/bmjopen-2018-028355
Article Google Scholar
Cashman KD, Dowling KG, Škrabáková Z, Gonzalez-Gross M, Valtueña J, De Henauw S, et al. Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr. 2016;103:1033–44. https://doi.org/10.3945/ajcn.115.120873
Article CAS Google Scholar
Zhang Y, Fang F, Tang J, Jia L, Feng Y, Xu P, et al. Association between vitamin D supplementation and mortality: systematic review and meta-analysis. BMJ. 2019;366:l4673. https://doi.org/10.1136/bmj.l4673
Amrein K, Martucci G, McNally JD. When not to use meta-analysis: analysing the meta-analyses on vitamin D in critical care. Clin Nutr. 2017;36:1729–30. https://doi.org/10.1016/j.clnu.2017.08.009 .
Bouillon R, Carmeliet G, Lieben L, Watanabe M, Perino A, Auwerx J. et al. Vitamin D and energy homeostasis: of mice and men. Nat Rev Endocrinol. 2014;10:79–87. https://doi.org/10.1038/nrendo.2013.226 .
Pittas AG, Dawson-Hughes B, Sheehan P, Ware JH, Knowler WC, Aroda VR, et al. Vitamin D supplementation and prevention of type 2 diabetes. N. Engl J Med. 2019;381:520–30. https://doi.org/10.1056/NEJMoa1900906
Manson JE, Cook NR, Lee I-M, Christen W, Bassuk SS, Mora S, et al. Vitamin D supplements and prevention of cancer and cardiovascular disease. N Engl J Med. 2018;380:33–44. https://doi.org/10.1056/NEJMoa1809944
Grant WB, Boucher BJ. Why secondary analyses in vitamin d clinical trials are important and how to improve vitamin d clinical trial outcome analyses—a comment on “Extra-Skeletal Effects of Vitamin D, Nutrients 2019, 11, 1460”. Nutrients. 2019;11:2182.
Martucci G, Tuzzolino F, Arcadipane A, Pieber TR, Schnedl C, Urbanic Purkart T. et al. The effect of high-dose cholecalciferol on bioavailable vitamin D levels in critically ill patients: a post hoc analysis of the VITdAL-ICU trial. Intensiv Care Med. 2017;43:1732–4. https://doi.org/10.1007/s00134-017-4846-5 .
De Pascale G, Quraishi SA. Vitamin D status in critically ill patients: the evidence is now bioavailable!. Crit Care. 2014;18:449. https://doi.org/10.1186/cc13975 .
Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington, DC: The National Academies Press; 2011.
Google Scholar
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2011;96:1911–30. https://doi.org/10.1210/jc.2011-0385
EFSA Panel on Dietetic Products N, Allergies. Dietary reference values for vitamin D. EFSA J. 2016;14:e04547. https://doi.org/10.2903/j.efsa.2016.4547
Braegger C, Campoy C, Colomb V, Decsi T, Domellof M, Fewtrell M, et al. Vitamin D in the healthy european paediatric population. J Pediatr Gastroenterol Nutr. 2013;56:692–701. https://doi.org/10.1097/MPG.0b013e31828f3c05
Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, et al. Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab. 2016;101:394–415. https://doi.org/10.1210/jc.2015-2175
Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583. https://doi.org/10.1136/bmj.i6583
Cashman KD. Vitamin D deficiency: defining, prevalence, causes, and strategies of addressing. Calcif Tissue Int. 2019. https://doi.org/10.1007/s00223-019-00559-4
Schleicher RL, Sternberg MR, Looker AC, Yetley EA, Lacher DA, Sempos CT, et al. National estimates of serum total 25-Hydroxyvitamin D and metabolite concentrations measured by liquid chromatography–Tandem mass spectrometry in the US population during 2007–2010. J Nutr. 2016;146:1051–61. https://doi.org/10.3945/jn.115.227728
Sarafin K, Durazo-Arvizu R, Tian L, Phinney KW, Tai S, Camara JE, et al. Standardizing 25-hydroxyvitamin D values from the Canadian Health Measures Survey. Am J Clin Nutr. 2015;102:1044–50. https://doi.org/10.3945/ajcn.114.103689
Courbebaisse M, Alberti C, Colas S, Prie D, Souberbielle JC, Treluyer JM. et al. Vitamin D supplementation in renAL transplant recipients (VITALE): a prospective, multicentre, double-blind, randomized trial of vitamin D estimating the benefit and safety of vitamin D3 treatment at a dose of 100,000 UI compared with a dose of 12,000 UI in renal transplant recipients: study protocol for a double-blind, randomized, controlled trial. Trials. 2014;15:430. https://doi.org/10.1186/1745-6215-15-430 .
Vos R, Ruttens D, Verleden SE, Vandermeulen E, Bellon H, Van Herck A, et al. High-dose vitamin D after lung transplantation: a randomized trial. J Heart Lung Transplant. 2017;36:897–905. https://doi.org/10.1016/j.healun.2017.03.008 .
Zhou Q, Li L, Chen Y, Zhang J, Zhong L, Peng Z, et al. Vitamin D supplementation could reduce the risk of acute cellular rejection and infection in vitamin D deficient liver allograft recipients. Int Immunopharmacol. 2019;75:105811 https://doi.org/10.1016/j.intimp.2019.105811 .
Cariolou M, Cupp MA. Importance of vitamin D in acute and critically ill children with subgroup analyses of sepsis and respiratory tract infections: a systematic review and meta-analysis. Crit care (Lond, Engl). 2019;9:e027666. 10.1136/bmjopen-2018-027666.
Lee P, Nair P, Eisman JA, Center JR. Vitamin D deficiency in the intensive care unit: an invisible accomplice to morbidity and mortality? Intensive care Med. 2009;35:2028–32. https://doi.org/10.1007/s00134-009-1642-x .
Martucci G, McNally D, Parekh D, Zajic P, Tuzzolino F, Arcadipane A. et al. Trying identify who may benefit most future Vitam D intervention trials: a post hoc Anal VITDAL-ICU study excluding early deaths. Crit Care. 2019;23:200. https://doi.org/10.1186/s13054-019-2472-z .
Sanders KM, Stuart AL, Williamson EJ, Simpson JA, Kotowicz MA, Young D, et al. Annual High-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA. 2010;303:1815–22. https://doi.org/10.1001/jama.2010.594
Amrein K, Papinutti A, Mathew E, Vila G, Parekh D. Vitamin D and critical illness: what endocrinology can learn from intensive care and vice versa. Endocr Connect. 2018;7:R304–R315. https://doi.org/10.1530/EC-18-0184
Hollis BW, Wagner CL. The role of the parent compound vitamin D with respect to metabolism and function: why clinical dose intervals can affect clinical outcomes. J Clin Endocrinol Metab. 2013;98:4619–28. https://doi.org/10.1210/jc.2013-2653
Roth DE, Martz P, Yeo R, Prosser C, Bell M, Jones AB. Are national vitamin D guidelines sufficient to maintain adequate blood levels in children? Can J Public Health. 2005;96:443–9. e-pub ahead of print 2005/12/15.
Rucker D, Allan JA, Fick GH, Hanley DA. Vitamin D insufficiency in a population of healthy western Canadians. CMAJ. 2002;166:1517–24.
Vieth R, Cole DE, Hawker GA, Trang HM, Rubin LA. Winter time vitamin D insufficiency is common in young Canadian women, and their vitamin D intake does not prevent it. Eur J Clin Nutr. 2001;55:1091–7. https://doi.org/10.1038/sj.ejcn.1601275.
Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr. 2003;77:204–10. https://doi.org/10.1093/ajcn/77.1.204.
Hathcock JN, Shao A, Vieth R, Heaney R. Risk assessment for vitamin D. Am J Clin Nutr. 2007;85:6–18. https://doi.org/10.1093/ajcn/85.1.6
Pfeifer M, Begerow B, Minne HW, Abrams C, Nachtigall D, Hansen C. Effects of a short-term vitamin D and calcium supplementation on body sway and secondary hyperparathyroidism in elderly women. J Bone Miner Res. 2000;15:1113–8. https://doi.org/10.1359/jbmr.2000.15.6.1113
Medicine Io. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. The Washington, DC: National Academies Press; 1997.
Aloia JF, Patel M, DiMaano R, Li-Ng M, Talwar SA, Mikhail M, et al. Vitamin D intake to attain a desired serum 25-hydroxyvitamin D concentration. Am J Clin Nutr. 2008;87:1952–8. https://doi.org/10.1093/ajcn/87.6.1952
Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the institute of medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96:53–58. https://doi.org/10.1210/jc.2010-2704
EFSA Panel on Dietetic Products N, Allergies. Scientific opinion on the tolerable upper intake level of vitamin D. EFSA J. 2012;10:2813. https://doi.org/10.2903/j.efsa.2012.2813
Hanley DA, Cranney A, Jones G, Whiting SJ, Leslie WD, Cole DEC, et al. Vitamin D in adult health and disease: a review and guideline statement from Osteoporosis Canada. CMAJ. 2010;182:E610–E618. https://doi.org/10.1503/cmaj.080663 . e-pub ahead of print 2010/07/12
Pietras SM, Obayan BK, Cai MH, Holick MF. Vitamin D2 treatment for vitamin D deficiency and insufficiency for up to 6 Years. JAMA Intern Med. 2009;169:1806–18. https://doi.org/10.1001/archinternmed.2009.361
McDonnell SL, Baggerly CA, French CB, Baggerly LL, Garland CF, Gorham ED, et al. Breast cancer risk markedly lower with serum 25-hydroxyvitamin D concentrations ≥60 vs <20 ng/ml (150 vs 50 nmol/L): Pooled analysis of two randomized trials and a prospective cohort. PLOS ONE. 2018;13:e0199265. https://doi.org/10.1371/journal.pone.0199265
Madden JM, Murphy L, Zgaga L, Bennett K. De novo vitamin D supplement use post-diagnosis is associated with breast cancer survival. Breast Cancer Res Treat. 2018;172:179–90. https://doi.org/10.1007/s10549-018-4896-6
Mirhosseini N, Vatanparast H, Kimball SM. The association between Serum 25(OH)D status and blood pressure in participants of a community-based program taking vitamin D supplements. Nutrients. 2017;9:1244.
Rusińska A, Płudowski P, Walczak M, Borszewska-Kornacka MK, Bossowski A, Chlebna-Sokół D, et al. Vitamin D supplementation guidelines for general population and groups at risk of vitamin D deficiency in poland—recommendations of the polish society of pediatric endocrinology and diabetes and the expert panel with participation of national specialist consultants and representatives of scientific societies. Front Endocrinol. 2018;9. https://doi.org/10.3389/fendo.2018.00246
Dudenkov DV, Yawn BP, Oberhelman SS, Fischer PR, Singh RJ, Cha SS, et al. Changing incidence of serum 25-Hydroxyvitamin D values above 50 ng/mL: a 10-year population-based study. Mayo Clin Proc. 2015;90:577–86. https://doi.org/10.1016/j.mayocp.2015.02.012
Holick MF. Vitamin D is not as toxic as was once thought: a historical and an up-to-date perspective. Mayo Clin Proc. 2015;90:561–4. https://doi.org/10.1016/j.mayocp.2015.03.015
Tebben PJ, Singh RJ, Kumar R. Vitamin D-mediated hypercalcemia: mechanisms, diagnosis, and treatment. Endocr Rev. 2016;37:521–47. https://doi.org/10.1210/er.2016-1070
Jones G. Pharmacokinetics of vitamin D toxicity. Am J Clin Nutr. 2008;88:582S–586S. https://doi.org/10.1093/ajcn/88.2.582S
Jacobus CH, Holick MF, Shao Q, Chen TC, Holm IA, Kolodny JM, et al. Hypervitaminosis D associated with drinking milk. N. Engl J Med. 1992;326:1173–7. https://doi.org/10.1056/nejm199204303261801
Jääskeläinen T, Itkonen ST, Lundqvist A, Erkkola M, Koskela T, Lakkala K, et al. The positive impact of general vitamin D food fortification policy on vitamin D status in a representative adult Finnish population: evidence from an 11-y follow-up based on standardized 25-hydroxyvitamin D data. Am J Clin Nutr. 2017;105:1512–20. https://doi.org/10.3945/ajcn.116.151415
Madsen KH, Rasmussen LB, Andersen R, Mølgaard C, Jakobsen J, Bjerrum PJ, et al. Randomized controlled trial of the effects of vitamin D–fortified milk and bread on serum 25-hydroxyvitamin D concentrations in families in Denmark during winter: the VitmaD study. Am J Clin Nutr. 2013;98:374–82. https://doi.org/10.3945/ajcn.113.059469
Hayes A, Duffy S, O’Grady M, Jakobsen J, Galvin K, Teahan-Dillon J, et al. Vitamin D–enhanced eggs are protective of wintertime serum 25-hydroxyvitamin D in a randomized controlled trial of adults. Am J Clin Nutr. 2016;104:629–37. https://doi.org/10.3945/ajcn.116.132530
Manson JE, Cook NR, Lee I-M, Christen W, Bassuk SS, Mora S, et al. Marine n−3 fatty acids and prevention of cardiovascular disease and cancer. N. Engl J Med. 2018;380:23–32. https://doi.org/10.1056/NEJMoa1811403
Scragg RKR. Overview of results from the Vitamin D assessment (ViDA) study. J Endocrinol Invest. 2019. https://doi.org/10.1007/s40618-019-01056-z
Scragg R, Stewart AW, Waayer D, Lawes CMM, Toop L, Sluyter J, et al. Effect of monthly high-dose vitamin D supplementation on cardiovascular disease in the vitamin D assessment study: a randomized clinical trial. JAMA Cardiol. 2017;2:608–16. https://doi.org/10.1001/jamacardio.2017.0175
Bischoff-Ferrari H, Vitamin D3—Omega3—home exercise—healthy ageing and longevity trial (DO-HEALTH). ClinicalTrials.gov; 2012. https://clinicaltrials.gov/ct2/show/NCT01745263 .
Tuomainen T-P, Finnish vitamin D trial (FIND). ClinicalTrials.gov; 2011. https://clinicaltrials.gov/ct2/show/NCT01463813 .
London School of Hygiene & Tropical Medicine. Vitamin D and longevity (VIDAL) trial: randomised feasibility study. ISRCTN Registry; 2011. https://doi.org/10.1186/ISRCTN46328341 .
Schoenmakers I, Francis RM, McColl E, Chadwick T, Goldberg GR, Harle C, et al. Vitamin D supplementation in older people (VDOP): Study protocol for a randomised controlled intervention trial with monthly oral dosing with 12,000 IU, 24,000 IU or 48,000 IU of vitamin D3. Trials. 2013;14:299. https://doi.org/10.1186/1745-6215-14-299
Ng K, Nimeiri HS, McCleary NJ, Abrams TA, Yurgelun MB, Cleary JM, et al. Effect of high-dose vs standard-dose vitamin D3 supplementation on progression-free survival among patients with advanced or metastatic colorectal cancer: the SUNSHINE randomized clinical trial. JAMA. 2019;321:1370–9. https://doi.org/10.1001/jama.2019.2402
Rosendahl J, Valkama S, Holmlund-Suila E, Enlund-Cerullo M, Hauta-alus H, Helve O, et al. Effect of higher vs standard dosage of vitamin D3 supplementation on bone strength and infection in healthy infants: a randomized clinical trial. JAMA Pediatrics. 2018;172:646–54. https://doi.org/10.1001/jamapediatrics.2018.0602
Sluyter JD, Camargo CA Jr., Stewart AW, Waayer D, Lawes CMM, Toop L, et al. Effect of monthly, high-dose, long-term vitamin D supplementation on central blood pressure parameters: a randomized controlled trial substudy. J Am Heart Assoc. 2017;6:e006802. https://doi.org/10.1161/JAHA.117.006802
Thompson BT. Vitamin D to improve outcomes by leveraging early treatment (VIOLET). ClinicalTrials.gov; 2017. https://clinicaltrials.gov/ct2/show/NCT03096314
Heaney RP. Guidelines for optimizing design and analysis of clinical studies of nutrient effects. Nutr Rev. 2014;72:48–54. https://doi.org/10.1111/nure.12090
Brenner H, Jansen L, Saum K-U, Holleczek B, Schöttker B. Vitamin D supplementation trials aimed at reducing mortality have much higher power when focusing on people with low serum 25-hydroxyvitamin D concentrations. J Nutr. 2017;147:1325–33. https://doi.org/10.3945/jn.117.250191
Avenell A, Mak JCS, O'Connell D. Vitamin D and vitamin D analogues for preventing fractures in post‐menopausal women and older men. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.CD000227.pub4
Bjelakovic G, Nikolova D, Bjelakovic M, Gluud C. Vitamin D supplementation for chronic liver diseases in adults. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD011564
Pludowski P, Holick MF, Pilz S, Wagner CL, Hollis BW, Grant WB, et al. Vitamin D effects on musculoskeletal health, immunity, autoimmunity, cardiovascular disease, cancer, fertility, pregnancy, dementia and mortality—A review of recent evidence. Autoimmun Rev. 2013;12:976–89. https://doi.org/10.1016/j.autrev.2013.02.004
Bjelakovic G, Gluud LL, Nikolova D, Whitfield K, Wetterslev J, Simonetti RG, et al. Vitamin D supplementation for prevention of mortality in adults. Cochrane Datab Syst Rev. 2014. https://doi.org/10.1002/14651858.CD007470.pub3
Gaksch M, Jorde R, Grimnes G, Joakimsen R, Schirmer H, Wilsgaard T, et al. Vitamin D and mortality: Individual participant data meta-analysis of standardized 25-hydroxyvitamin D in 26916 individuals from a European consortium. PLOS ONE. 2017;12:e0170791. https://doi.org/10.1371/journal.pone.0170791
Aspelund T, Grübler MR, Smith AV, Gudmundsson EF, Keppel M, Cotch MF, et al. Effect of genetically low 25-hydroxyvitamin D on mortality risk: mendelian randomization analysis in 3 large european cohorts. Nutrients. 2019;11:74. https://doi.org/10.3390/nu11010074
Berlanga-Taylor AJ, Leclair TR, Zakai N, Bunn JY, Gianni M, Heyland DK, et al. Vitamin D supplementation in mechanically ventilated patients in the medical intensive care unit. BMJ Open. 2019. https://doi.org/10.1136/bmjopen-2018-02766610.1002/jpen .
Quraishi SA, De Pascale G, Needleman JS, Nakazawa H, Kaneki M, Bajwa EK. et al. Effect of cholecalciferol supplementation on vitamin D status and cathelicidin levels in sepsis: a randomized, placebo-controlled trial. Crit Care Med. 2015;43:1928–37. https://doi.org/10.1111/ene.1278810.1097/ccm.0000000000001148 .
Palacios C, Trak-Fellermeier MA, Martinez RX, Lopez-Perez L, Lips P, Salisi JA. et al. Regimens of vitamin D supplementation for women during pregnancy. Cochrane Database Syst Rev. 2019;10:Cd013446 https://doi.org/10.1002/14651858.cd013446 . e-pub ahead of print 2019/10/04.
Palacios C, Kostiuk LK, Pena-Rosas JP. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst Rev. 2019;7:Cd008873 https://doi.org/10.1002/14651858.CD008873.pub4 . e-pub ahead of print 2019/07/28.
Holick MF. A call to action: pregnant women in-deed require vitamin D supplementation for better health outcomes. J Clin Endocrinol Metab. 2018;104:13–15. https://doi.org/10.1210/jc.2018-01108
Mithal A, Wahl DA, Bonjour J-P, Burckhardt P, Dawson-Hughes B, Eisman JA, et al. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int. 2009;20:1807–20. https://doi.org/10.1007/s00198-009-0954-6
Fogacci S, Fogacci F, Banach M, Michos ED, Hernandez AV, Lip GYH, et al. Vitamin D supplementation and incident preeclampsia: a systematic review and meta-analysis of randomized clinical trials. Clin Nutr. 2019. https://doi.org/10.1016/j.clnu.2019.08.015
Rodrigues MRK, Lima SAM, Mazeto GMFDSS, Calderon IMP, Magalhães CG, Ferraz GAR. et al. Mazeto GMFdS, Calderon IMP, Magalhães CG, Ferraz GAR et al. Efficacy of vitamin D supplementation in gestational diabetes mellitus: systematic review and meta-analysis of randomized trials. PLOS ONE. 2019;14:e0213006. https://doi.org/10.1371/journal.pone.0213006 .
Akbari S, Khodadadi B, Ahmadi SAY, Abbaszadeh S, Shahsavar F. Association of vitamin D level and vitamin D deficiency with risk of preeclampsia: a systematic review and updated meta-analysis. Taiwan J Obstet Gynecol. 2018;57:241–7. https://doi.org/10.1016/j.tjog.2018.02.013
McDonnell SL, Baggerly KA, Baggerly CA, Aliano JL, French CB, Baggerly LL, et al. Maternal 25(OH)D concentrations ≥40 ng/mL associated with 60% lower preterm birth risk among general obstetrical patients at an urban medical center. PloS ONE. 2017;12:e0180483–e0180483. https://doi.org/10.1371/journal.pone.0180483
Wagner CL, Baggerly C, McDonnell S, Baggerly KA, French CB, Baggerly L. et al. Post-hoc analysis of vitamin D status and reduced risk of preterm birth in two vitamin D pregnancy cohorts compared with South Carolina March of Dimes 2009–211 rates. J Steroid Biochem Mol Biol. 2016;155:245–51. https://doi.org/10.1016/j.jsbmb.2015.10.022 .
Hollis BW, Johnson D, Hulsey TC, Ebeling M, Wagner CL. Vitamin D supplementation during pregnancy: double-blind, randomized clinical trial of safety and effectiveness. J Bone Min Res. 2011;26:2341–57. https://doi.org/10.1002/jbmr.463
Rostami M, Tehrani FR, Simbar M, Bidhendi Yarandi R, Minooee S, Hollis BW, et al. Effectiveness of prenatal vitamin D deficiency screening and treatment program: a stratified randomized field trial. J Clin Endocrinol Metab. 2018;103:2936–48. https://doi.org/10.1210/jc.2018-00109
Hossein-nezhad A, Holick MF. Optimize dietary intake of vitamin D: an epigenetic perspective. Curr Opin Clin Nutr Metab Care. 2012;15:567–79. https://doi.org/10.1097/MCO.0b013e3283594978
Novakovic B, Sibson M, Ng HK, Manuelpillai U, Rakyan V, Down T, et al. Placenta-specific methylation of the vitamin D 24-hydroxylase gene: implications for feedback autoregulation of active vitamin D levels at the fetomaterial interface. J Biol Chem. 2009;284:14838–48. https://doi.org/10.1074/jbc.M809542200
McDonnell SL, Baggerly C, French CB, Baggerly LL, Garland CF, Gorham ED, et al. Serum 25-hydroxyvitamin D concentrations ≥40 g/ml are associated with >65% lower cancer risk: pooled analysis of randomized trial and prospective cohort study. PLOS ONE. 2016;11:e0152441 https://doi.org/10.1371/journal.pone.0152441
Colston K, Colston MJ, Feldman D. 1,25-Dihydroxyvitamin D3 and malignant melanoma: the presence of receptors and inhibition of cell growth in culture. Endocrinology. 1981;108:1083–6. https://doi.org/10.1210/endo-108-3-1083
Garland CF, Garland FC. Do sunlight and vitamin D reduce the likelihood of colon cancer? Int J Epidemiol. 1980;9:227–31. https://doi.org/10.1093/ije/9.3.227
Keum N, Giovannucci E. Vitamin D supplements and cancer incidence and mortality: a meta-analysis. Br J Cancer. 2014;111:976. https://doi.org/10.1038/bjc.2014.294
Bjelakovic G, Gluud LL, Nikolova D, Whitfield K, Krstic G, Wetterslev J, et al. Vitamin D supplementation for prevention of cancer in adults. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.CD007469.pub2
Lappe J, Watson P, Travers-Gustafson D, Recker R, Garland C, Gorham E, et al. Effect of vitamin D and calcium supplementation on cancer incidence in older women: a randomized clinical trial. JAMA. 2017;317:1234–43. https://doi.org/10.1001/jama.2017.2115
Chatterjee R, Erban JK, Fuss P, Dolor R, LeBlanc E, Staten M, et al. Vitamin D supplementation for prevention of cancer: the D2d cancer outcomes (D2dCA) study. Contemp Clin Trials. 2019;81:62–70. https://doi.org/10.1016/j.cct.2019.04.015
Greer RM, Portelli SL, Hung BS-M, Cleghorn GJ, McMahon SK, Batch JA, et al. Serum vitamin D levels are lower in Australian children and adolescents with type 1 diabetes than in children without diabetes. Pediatr Diabetes. 2013;14:31–41. https://doi.org/10.1111/j.1399-5448.2012.00890.x
Daga RA, Laway BA, Shah ZA, Mir SA, Kotwal SK, Zargar AH. High prevalence of vitamin D deficiency among newly diagnosed youth-onset diabetes mellitus in north India. Arquivos Brasileiros de Endocrinologia Metabologia. 2012;56:423–8.
Federico G, Genoni A, Puggioni A, Saba A, Gallo D, Randazzo E, et al. Vitamin D status, enterovirus infection, and type 1 diabetes in Italian children/adolescents. Pediatr Diabetes. 2018;19:923–9. https://doi.org/10.1111/pedi.12673
Rasoul MA, Al-Mahdi M, Al-Kandari H, Dhaunsi GS, Haider MZ. Low serum vitamin D status is associated with high prevalence and early onset of type-1 diabetes mellitus in Kuwaiti children. BMC Pediatr. 2016;16:95–95. https://doi.org/10.1186/s12887-016-0629-3
Sørensen IM, Joner G, Jenum PA, Eskild A, Torjesen PA, Stene LC. Maternal serum levels of 25-hydroxy-vitamin D during pregnancy and risk of type 1 diabetes in the offspring. Diabetes. 2012;61:175. https://doi.org/10.2337/db11-0875
Jacobsen R, Moldovan M, Vaag AA, Hypponen E, Heitmann BL. Vitamin D fortification and seasonality of birth in type 1 diabetic cases: D-tect study. J Devel Orig Health Dis. 2016;7:114–9. https://doi.org/10.1017/S2040174415007849 . e-pub ahead of print 2015/10/27.
Dong J-Y, Zhang W, Chen JJ, Zhang Z-L, Han S-F, Qin L-Q. Vitamin D intake and risk of type 1 diabetes: a meta-analysis of observational studies. Nutrients. 2013;5:3551–62.
Stene LC, Joner G, Group NCDS. Use of cod liver oil during the first year of life is associated with lower risk of childhood-onset type 1 diabetes: a large, population-based, case-control study. Am J Clin Nutr. 2003;78:1128–34. https://doi.org/10.1093/ajcn/78.6.1128
Raab J, Giannopoulou EZ, Schneider S, Warncke K, Krasmann M, Winkler C, et al. Prevalence of vitamin D deficiency in pre-type 1 diabetes and its association with disease progression. Diabetologia. 2014;57:902–8. https://doi.org/10.1007/s00125-014-3181-4
Mäkinen M, Mykkänen J, Koskinen M, Simell V, Veijola R, Hyöty H, et al. Serum 25-hydroxyvitamin D concentrations in children progressing to autoimmunity and clinical type 1 diabetes. J Clin Endocrinol Metab. 2016;101:723–9. https://doi.org/10.1210/jc.2015-3504
Simpson M, Brady H, Yin X, Seifert J, Barriga K, Hoffman M, et al. No association of vitamin D intake or 25-hydroxyvitamin D levels in childhood with risk of islet autoimmunity and type 1 diabetes: the Diabetes Autoimmunity Study in the Young (DAISY). Diabetologia. 2011;54:2779. https://doi.org/10.1007/s00125-011-2278-2
Rak K, Bronkowska M. Immunomodulatory effect of vitamin D and its potential role in the prevention and treatment of type 1 diabetes mellitus—a narrative review. Molecules. 2018;24:53.
Thrailkill KM, Jo C-H, Cockrell GE, Moreau CS, Fowlkes JL. Enhanced excretion of vitamin D binding protein in type 1 diabetes: a role in vitamin D deficiency? J Clin Endocrinol Metab. 2011;96:142–9. https://doi.org/10.1210/jc.2010-0980
Kayaniyil S, Vieth R, Retnakaran R, Knight JA, Qi Y, Gerstein HC, et al. Association of vitamin d with insulin resistance and β-Cell dysfunction in subjects at risk for type 2 diabetes. Diabetes Care. 2010;33:1379–81. https://doi.org/10.2337/dc09-2321
Kawahara T, Suzuki G, Inazu T, Mizuno S, Kasagi F, Okada Y, et al. Rationale and design of Diabetes Prevention with active Vitamin D (DPVD): a randomised, double-blind, placebo-controlled study. BMJ Open. 2016;6:e011183. https://doi.org/10.1136/bmjopen-2016-011183
Galior K, Grebe S, Singh R. Development of vitamin D toxicity from overcorrection of vitamin D deficiency: a review of case reports. Nutrients. 2018;10:953.
Schlingmann KP, Kaufmann M, Weber S, Irwin A, Goos C, John U, et al. Mutations in CYP24A1 and Idiopathic Infantile Hypercalcemia. N Engl J Med. 2011;365:410–21. https://doi.org/10.1056/NEJMoa1103864
National Heart, Lung, and Blood Institute, PETAL Clinical Trials Network, Ginde A, Brower R, et al. Early high-dose vitamin D3 for critically Ill, vitamin D–deficient patients. N Engl J Med. 2019. https://doi.org/10.1056/NEJMoa1911124
Amrein K, Schnedl C, Holl A, Riedl R, Christopher KB, Pachler C, et al. Effect of high-dose vitamin D3 on hospital length of stay in critically Ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial. JAMA. 2014;312:1520–30. https://doi.org/10.1001/jama.2014.13204
BMJ Open. 2019;9:e031083. https://doi.org/10.1136/bmjopen-2019-031083
Download references
Author information
Authors and affiliations.
Department of Internal Medicine, Division of Endocrinology and Diabetology, Medical University of Graz, Graz, Austria
Karin Amrein, Mario Scherkl, Magdalena Hoffmann, Stefan Pilz & Oliver Malle
Thyroid Endocrinology Osteoporosis Institute Dobnig, Graz, Austria
Karin Amrein
Executive Department for Quality and Risk Management, University Hospital Graz, Graz, Austria
Magdalena Hoffmann
Research Unit for Safety in Health, Division of Plastic, Aesthetic and Reconstructive Surgery, Department of Surgery, Medical University of Graz, Graz, Austria
Department of Anaesthesiology and Intensive Care Medicine, Klinikum Klagenfurt am Wörthersee, Klagenfurt am Wörthersee, Austria
Stefan Neuwersch-Sommeregger & Markus Köstenberger
Immunology and Pathophysiology, Otto Loewi Research Center, Medical University of Graz, Heinrichstrasse 31a, A-8010, Graz, Austria
Department of Psychiatry and Psychotherapeutic Medicine, Medical University of Graz, Graz, Austria
Adelina Tmava Berisha
Department of Anesthesia and Intensive Care, IRCCS-ISMETT (Istituto Mediterraneo per i Trapianti e Terapie ad Alta Specializzazione), Palermo, Italy
Gennaro Martucci
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Karin Amrein .
Ethics declarations
Conflict of interest.
KA has received speaker honoraria and an unrestricted grant from Fresenius Kabi. The other authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Amrein, K., Scherkl, M., Hoffmann, M. et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr 74 , 1498–1513 (2020). https://doi.org/10.1038/s41430-020-0558-y
Download citation
Received : 06 October 2019
Revised : 17 December 2019
Accepted : 06 January 2020
Published : 20 January 2020
Issue Date : November 2020
DOI : https://doi.org/10.1038/s41430-020-0558-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
High-dose vitamin d3 supplementation shows no beneficial effects on white blood cell counts, acute phase reactants, or frequency of respiratory infections.
- Gustav Wall-Gremstrup
- Martin Blomberg Jensen
Respiratory Research (2024)
Vitamin D metabolism in critically ill patients with acute kidney injury: a prospective observational study
- Lynda K. Cameron
- Lesedi Ledwaba-Chapman
- Marlies Ostermann
Critical Care (2024)
Impact of vitamin D supplementation on the clinical outcomes of COVID-19 pneumonia patients: a single-center randomized controlled trial
- Pitchaya Dilokpattanamongkol
- Chadakan Yan
- Porpon Rotjanapan
BMC Complementary Medicine and Therapies (2024)
Prevalence of vitamin D deficiency and its association with cardiometabolic risk factors among healthcare workers in the Eastern Cape province, South Africa; cross-sectional study
- Oladele Vincent Adeniyi
- Charity Masilela
- Jaya A. George
Scientific Reports (2024)
An ultra-sensitive and high-throughput trapping-micro-LC-MS method for quantification of circulating vitamin D metabolites and application in multiple sclerosis patients
- Murali Ramanathan
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
The Health Benefits of Vitamin D3
A type of vitamin D sourced from animal-based foods and sunlight
- Why You Need It
- Are You Deficient?
- Other Benefits
Possible Risks
Frequently asked questions.
Vitamin D3 ( cholecalciferol) has a few health benefits, including helping the body absorb calcium. Foods such as fish, beef liver, eggs, and cheese naturally contain vitamin D3. It can also be produced in the skin following exposure to ultraviolet (UV) radiation from the sun.
Supplement forms of vitamin D3 are also available and may be used for general health, as well as the treatment or prevention of vitamin D deficiency .
Vitamin D3 is one of two types of vitamin D . It differs from vitamin D2 (ergocalciferol) in both its structure and sources.
The article explains what vitamin D supplements do and the benefits/drawbacks of vitamin D3 specifically. It also lists other important sources of vitamin D3.
Why You Need Vitamin D
Vitamin D, also referred to as calciferol , is a fat-soluble vitamin (meaning one that is broken down by fat and oils in the gut). It is commonly referred to as the "sunshine vitamin" because the D3 type can be naturally produced in the body following exposure to the sun.
Vitamin D has many functions in the body, chief of which include:
- Bone growth
- Bone remodeling
- Regulation of muscle contractions
- Conversion of blood glucose (sugar) into energy
Not getting enough vitamin D can lead to an array of health concerns, including:
- Delayed growth in kids
- Rickets in kikds
- Osteomalacia (loss of bone minerals) in adults and adolescents
- Osteoporosis (porous, thinning bones) in adults
How Much Vitamin D Do I Need?
Current guidelines from the National Institutes of Health recommend that people ages 1 to 70 years should get 600 international units (IUs) of vitamin D per day from all sources. Adults over 70 need 800 IUsdaily.
How Do I Know If I Need More Vitamin D?
If you do not obtain enough vitamin D to meet the body's needs you are considered to have a vitamin D deficiency . This can be diagnosed through blood testing.
However, the U.S. Preventive Services Task Force does not recommend routine vitamin D screening in adults without symptoms of deficiency.
Not everyone who is low in vitamin D experiences symptoms. Those who do may notice:
- Muscle and/or bone pain
- Muscle weakness
- History of fractures
- Muscle twitching
If you suspect you could be vitamin D deficient, ask your healthcare provider to test your blood levels or take an at-home test .
Causes for vitamin D deficiency are many, including diseases or conditions that limit fat absorption and the breakdown of vitamin D in the gut. As such, you are at greater risk for vitamin D deficiency if you have:
- Celiac disease
- Crohn’s disease
- Cystic fibrosis
- Gastric bypass surgery
- Liver disease
- Malnutrition
- Ulcerative colitis
People who are older, are housebound, or have dark skin are also more vulnerable to vitamin D deficiency.
Vitamin D deficiency affects almost 50% of the population worldwide. Both vitamin D2 and D3 can be used to treat this, with vitamin D3 generally being the preferred choice.
Vitamin D3 vs. Vitamin D2
Vitamin D2 and vitamin D3 are chemically similar and are both well-absorbed in the gut. Where they differ significantly is in their sources:
- Vitamin D2 is naturally found in mushrooms, including shiitake, Portobello, and crimini mushrooms. The vitamin D content increases when these mushrooms are exposed to UV radiation.
- Vitamin D3 is naturally found in animals and animal-derived products like milk. It is also directly synthesized in the skin when it is exposed to ultraviolet B (UVB) radiation.
Aside from the fact that vitamin D3 is likely easier to consume in your day-to-day diet, unless you are a vegetarian or vegan, vitamin D3 has proven superior to vitamin D2 in two other important ways:
- Vitamin D3 has better bioavailability , meaning more of the vitamin enters the bloodstream and can be used by the body
- Vitamin D3 has a better half-life , meaning it stays in circulation for longer
Some studies suggest that vitamin D3 raises the vitamin D level in the bloodstream 87% more than vitamin D2.
On the downside, vitamin D3 in supplements has historically been synthesized using lanolin derived from sheep's wool. This makes it unsuitable for those who choose to avoid animal-based products.
With that said, some manufacturers have been able to synthesize vitamin D3 from algae and lichen.
Vitamin D3 For Those Without Deficiency
Beyond its use in treating vitamin D deficiency, vitamin D3 may offer health benefits to certain people without such deficiency—in particular, those with high blood pressure or osteoporosis.
Hypertension
Hypertension , more commonly known as high blood pressure, is cardiovascular disease commonly seen in people with vitamin D deficiency.
Recent studies suggest that vitamin D3 may help lower blood pressure in people with hypertension and vitamin D deficiency as well as certain groups of people with hypertension only.
According to a 2019 review of studies in the journal Medicine involving 1,687 people, vitamin D3 was able to significantly reduce systolic ("top number") blood pressure in people over the age of 50 and those with obesity .
This is important because isolated systolic hypertension can increase the risk of stroke, heart disease, and chronic kidney disease over time.
Osteoporosis
Osteoporosis is a frequent consequence of long-term vitamin D deficiency, so common wisdom would suggest that vitamin D supplements may help prevent or slow the progression of this common, aging-related bone disease. There is some evidence to support this claim.
A 2013 study from the University of Western Australia found that the use of vitamin D3 in nursing home residents aged 70 and over significantly reduced the incidence of hip fractures. In addition, low-dose vitamin D3 (400 IU) also increased bone mass density in the femoral (thigh) bone .
Unproven Benefits
Despite claims to the contrary, there is no evidence that vitamin D3 supplements can reduce the risk of cancer, coronary heart disease, or stroke. With that said, the supplements pose little, if any, harm if taken at the prescribed dose.
Sources of Vitamin D3
Whether you are nutritionally deficient or simply want to meet your recommended daily allowance (RDA) of vitamin D, you can obtain ample supplies of vitamin D3 from animal-based foods, dietary supplements, and sun exposure.
Dietary Sources
Food should always be the first source of vitamin D. Here are some of the best dietary sources of vitamin D3 to bolster your intake:
Some manufacturers of fruit juices, dairy products, margarine, and plant-based milk add vitamin D3 to boost their product's nutritional value, as well.
Supplements
As convenient as they are, supplements should never be your primary source of vitamin D (or any nutrient, for that matter). They are really only intended for when you are not getting enough from your diet.
Vitamin D3 is readily available in supplement form and sold as capsules, softgels, gummies, and liquid drops. Most are formulated in doses higher than you need per day—between 2,000 and 10,000 IUs—but this is not a concern as only a portion will be absorbed. The rest will be passed in urine.
Talk to your healthcare provider about the best dose for you based on your age and medical history.
Sun Exposure
Vitamin D3 is unique in that (unlike vitamin D2) you can get it from the sun.
When exposed to UVB light, an organic compound in the skin called 7-dehydrocholesterol will activate and start churning out vitamin D3. The rate of production can vary by your age and skin tone, with older people and those with darker skin getting the least benefit.
Sunscreen can also decrease production by blocking both UV rays.
Getting a little sunlight every day can help you maintain your vitamin D levels, but it’s not the safest or most reliable way to get it given the risk of skin cancer.
Vitamin D3 is generally regarded as safe, but it can on rare occasions cause toxic effects if you take too much. This is referred to as hypervitaminosis D .
With vitamin D toxicity, the balance of minerals like calcium and potassium is upset. This can lead to a condition known as hypercalcemia , in which too much calcium builds up in the body. This can lead to symptoms like:
- Stomach upset
- Constipation
- An increased risk of bone fractures
Vitamin D toxicity was common in the 1940s when daily doses of 200,000 to 300,000 IUs per day were commonly recommended to treat chronic illnesses like tuberculosis and rheumatoid arthritis .
Today, vitamin D toxicity is considered a rare occurrence.
Recent studies have shown that vitamin D3 doses of 20,000 IUs per day are tolerable in adults with no signs of toxicity.
Vitamin D helps you absorb calcium and phosphate from food. It is important for bone and muscle strength and immune function, and it may have other benefits such as helping prevent inflammatory disease.
There are two types; vitamin D3 is more efficient in terms of how it can be used in the body than vitamin D2. You can get vitamin D from food or supplements, and your body can make D3 when exposed to sunshine.
Vitamin D3 is a fat-soluble vitamin. This means that taking it with fat helps it absorb better. It doesn’t matter what time of day you take it, but you should eat fat-containing food when you do.
There are some at-home tests that can measure the amount of vitamin D in your blood. All you need to do is place a drop of blood on a test strip and mail it to the test's manufacturer or designated lab for processing.
A lack of vitamin D can cause you to feel lethargic. Supplementing with D3 could, over time, help you feel more energetic, but only if you have a deficiency.
People with hyperparathyroidism, kidney disease, or hypercalcemia (high blood calcium) should typically avoid vitamin D3 supplements. Certain medications can also interact with vitamin D. Speak with your healthcare provider or pharmacist before starting any supplement.
National Institutes of Health Office of Dietary Supplements. Vitamin D: fact sheet for health professionals .
US Preventive Services Task Force, et al. Screening for vitamin D deficiency in adults: US Preventive Services Task Force recommendation statement . JAMA . 2021;325(14):1436-1442 . doi:10.1001/jama.2021.3069
Yale Medicine. Vitamin D Deficiency .
Nair R, Maseeh A. Vitamin D: the “sunshine” vitamin . J Pharmacol Pharmacother. 2012 Apr-Jun;3(2):118–26. doi:10.4103/0976-500X.95506
Tripkovic L, Lambert H, Hart K, et al. Comparison of vitamin D2 and vitamin D3 supplementation in raising serum 25-hydroxyvitamin D status: a systematic review and meta-analysis . Am J Clin Nutr. 2012 Jun;95(6):1357–64. doi:10.3945/ajcn.111.031070
MedlinePlus. Cholecalciferol (vitamin D3) .
He S, Hao X. The effect of vitamin D3 on blood pressure in people with vitamin D deficiency: a system review and meta-analysis . Medicine (Baltimore). 2019 May;98(19):e15284. doi:10.1097/MD.0000000000015284
Geddes JAA, Inderjeeth CA. Evidence for the treatment of osteoporosis with vitamin D in residential care and in the community dwelling elderly . Biomed Res Int. 2013;2013:463589. doi:10.1155/2013/463589
Danik JS, Manson JE. Vitamin D and cardiovascular disease . Curr Treat Options Cardiovasc Med . 2012 Aug;14(4):414–24. doi:10.1007/s11936-012-0183-8
Marcinowska-Suchowierska E, Kupisz-Urbańska M, Łukaszkiewicz J, Płudowsk P, Jones G. Vitamin D toxicity–a clinical perspective . Front Endocrinol (Lausanne). 2018;9:550. doi:10.3389/fendo.2018.00550
Nowak A, Boesch L, Andres E, et al. Effect of vitamin D3 on self-perceived fatigue: A double-blind randomized placebo-controlled trial . Medicine (Baltimore) . 2016;95(52):e5353. doi:10.1097/MD.0000000000005353
National Institutes of Health, Office of Dietary Supplements. Vitamin D fact sheet for consumers .
By Yvelette Stines Stines is a Michigan-based health writer, book author, and communications specialist.
Should you take vitamin D? Here’s the science
Some people take too much, and too many get too little. Experts explain who needs D supplements, and why.
By Katarina Zimmer / Knowable Magazine | Published Apr 21, 2024 12:00 PM EDT

This article was originally featured on Knowable Magazine .
Nutritional science is supposed to chart a course to our healthier selves. But contradictory scientific results and interpretations can muddy the waters—and few nutrients have recently demonstrated that more clearly than vitamin D.
At one point, it seemed that everyone should be taking vitamin D supplements, and that doing so would protect against a whole host of maladies, from bone problems to heart disease and cancer. More recently, new studies appear to have debunked many of those claims.
But a closer look at the research reveals a more nuanced message around vitamin D supplements: They can be key to correcting deficiencies, though people who already have enough—which is most of the American public—are generally unlikely to see benefits from taking large doses. Experts have come to worry about supplement enthusiasts overdosing in the belief that more is better or, at the other extreme, some nutrient-deprived people shunning them altogether.
Ultimately, says Roger Bouillon , an endocrinologist at KU Leuven in Belgium, “it’s like for most things. You need an optimal amount: not too little, not too much.”
Yet working out who needs vitamin D supplements, how much, and what the specific health benefits are, remains tricky, with questions remaining. Here’s some of what we know.
What does vitamin D do, and where does it come from?
The importance of vitamin D came to light at the start of the Industrial Revolution in the late 1700s, when people in northern climes crowded in dark, polluted cities and spent more time working indoors. The majority of children in cities like Boston developed rickets, wherein bones soften, weaken and often deform.
Scientists eventually discovered that exposure to sunlight would cure and prevent the disease. Later, researchers learned that UV light from the Sun kick-starts a reaction that generates vitamin D. The vitamin gets converted into its active form in the kidneys and then is shuttled to the intestine, where it stimulates cells to move calcium, a key building block of bones , into the bloodstream. “The most important thing vitamin D does is intestinal calcium absorption,” says Sylvia Christakos , a biochemist at Rutgers New Jersey Medical School.
Though the effects are most severe in children, vitamin D deficiencies can also cause a softening of adult bones called osteomalacia , and increase the risk of osteoporosis, where bones become weak, brittle and more prone to fractures . Though experts debate what exactly constitutes a vitamin D deficiency—and know that healthy levels may vary from person to person—everyone agrees that blood levels should not go below 12 nanograms per milliliter to avoid severe deficiency.
Such severe deficiencies—and the bone ailments they cause—are still rampant across the world. Surprisingly, more than 30 percent of people in some sunny Middle Eastern countries are severely deficient, which may be partly attributed to skin-covering traditional clothing. By contrast, in Finland , a sun-deprived country with dark winters, severe deficiencies are relatively rare, thanks to government policies to fortify dairy products with extra vitamin D.
In contrast, around 20 percent of the United Kingdom’s population is severely deficient by some estimates, due to its northern, cloudy weather and a lack of fortified foods. The United States, where many dairy products, and some juices and breakfast cereals, are fortified, falls somewhere in the middle: Around 6 percent of people are severely deficient . “For the most part in the US, we don’t see frank nutrient deficiencies,” says Regan Bailey , a nutrition expert at Texas A&M University who recently coauthored a review on supplement use among the public in the Annual Review of Nutrition. (Some research groups have produced much larger deficiency estimates by using blood level thresholds that many experts say are too high to qualify as nutrient deficiencies.)
Since 2010, the National Academy of Medicine has recommended relatively modest daily doses : 400 international units (IUs) for babies, 600 IUs for everyone up to age 70 and 800 IUs for older people. These doses are designed to achieve levels of 20 nanograms per milliliter—more than enough to avoid severe deficiencies—for otherwise healthy people in the United States.
Most people should be able to get these doses through brief sun exposure, says John Christopher Gallagher, an endocrinologist at Creighton University in Omaha, Nebraska. Measuring vitamin D production in the skin is not an exact science, but five to 10 minutes’ daily exposure without sunblock of just the face, neck, hands and arms should do the trick in the sunnier months, even in temperate places like Boston. While it’s entirely possible to get enough vitamin D this way, the official stance of the American Academy of Dermatology is to not get vitamin D from sun exposure.
Fortified dairy products and other foods will also provide enough. Foods that naturally contain vitamin D, such as fatty fish, egg yolks, red meat, liver and irradiated or sun-dried mushrooms, which are especially rich in vitamin D due to their increased exposure to UV light, can also help. “If you’re out and about and you have sun exposure during some months of the year,” Gallagher says, “you probably get plenty of vitamin D.” That’s especially true if you have enough dairy in your diet.
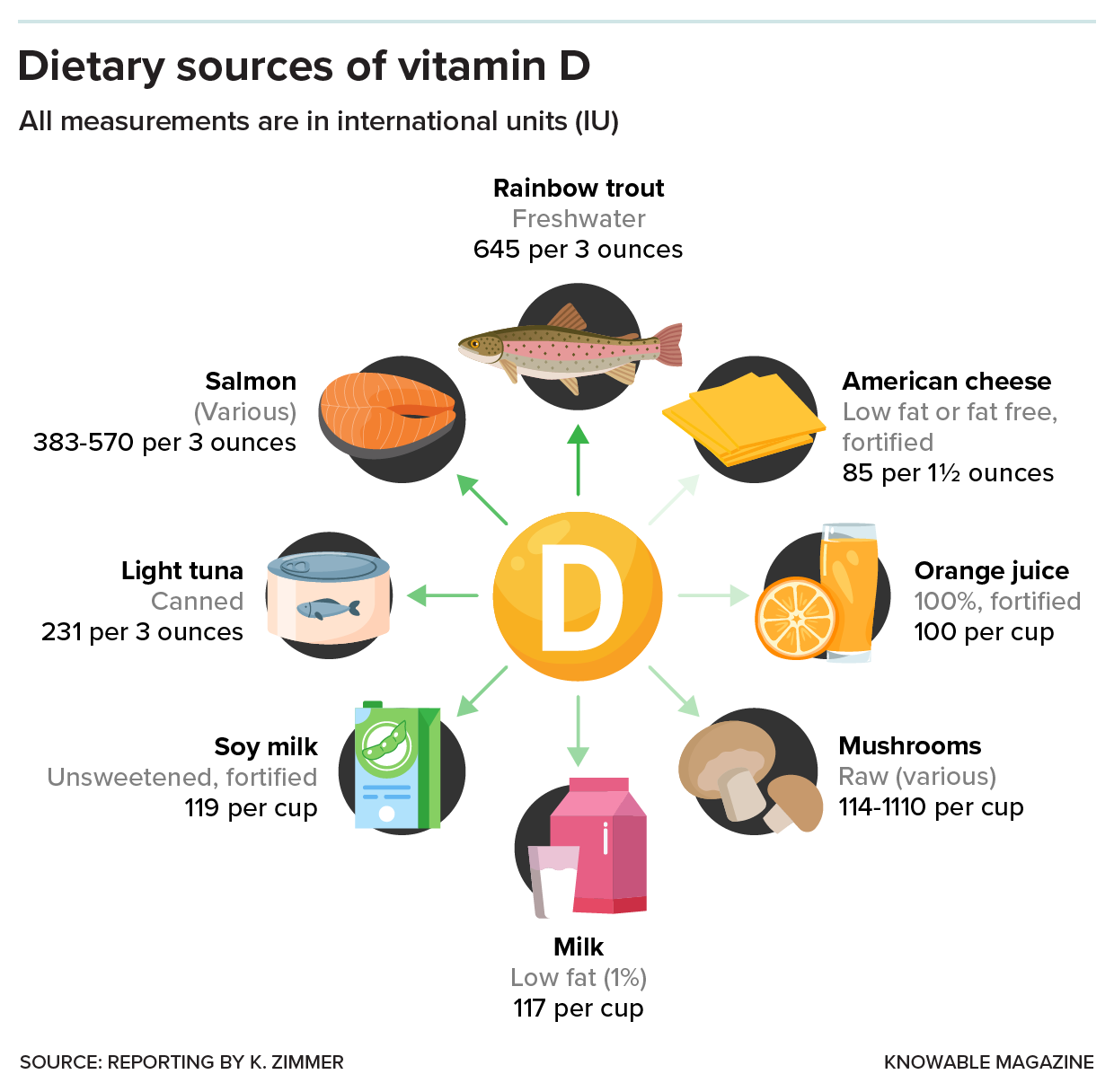
Does anyone need supplements?
Generally, people need supplements only when they’re not likely to get enough from natural or dietary sources, health experts say. Deficiency-prone populations include breastfed infants who don’t get fortified formula, elderly people (whose skin makes vitamin D less efficiently) and pregnant women. People with dark skin tones should also take care to get sufficient vitamin D, because melanin pigmentation in the skin blocks UV light. People in northern latitudes like England “should all take a supplement during the winter,” adds nutritional scientist Susan Lanham-New of the University of Surrey in the UK, although that’s less important in places like the United States that have food fortification.
Experts worry that it’s often the people already getting enough vitamin D through diet and lifestyle who are the most likely to take supplements, Christakos notes. Meanwhile, communities who need vitamin D supplements the most might not realize their need and may have read news reports suggesting that the supplements aren’t necessary.
That’s an especially dangerous message in countries where deficiencies are common—for instance in the UK, where physicians still see children with deficiency-related ailments, says Martin Hewison , a molecular endocrinologist at the University of Birmingham in that country. One of his UK colleagues is struggling to persuade some of her vitamin D-deficient patients to take supplements because they believe it is a waste of time.
For anyone concerned that they’re not getting enough vitamin D, experts say that up to 1,000 IUs a day would more than suffice. If possible, Lanham-New adds, make sure it’s vitamin D3, a version typically extracted from sheep wool that appears to be better at raising vitamin D blood levels than D2 , which is often vegan and mushroom-based.
But avoid the high doses—of 5,000, 10,000 or 20,000 IUs, or even higher—that can be found in drugstores or online, stresses JoAnn Manson , an endocrinologist and epidemiologist at Brigham and Women’s Hospital and Harvard Medical School. Too much vitamin D, even when taken occasionally, can sometimes cause bone health to deteriorate and lead to an overdose of calcium in the blood and urine, resulting in nausea and even kidney failure. There are reports of people in the UK and US ending up in the hospital after taking excessive doses .
Some experts have advised that Black Americans, in particular, take higher doses of supplements—for instance, 2,500 IUs—as they’re especially prone to low levels. But here’s a mystery: Even though 17.5 percent of African Americans have deficient levels of vitamin D, those vitamin-deficient Blacks tend to have better bone health than comparably deficient white Americans, notes biomedical scientist LaVerne Brown of the National Institutes of Health. It’s possible, she says, that African Americans need less vitamin D than other populations, perhaps because they’re better at metabolizing vitamin D to its final active form. If that’s true, then high doses may have a greater risk of causing harm in African Americans.
“We just don’t have the studies that are focusing on these populations in order to come up with definitive answers,” Brown says. In the meantime, an expert panel meeting in 2017 concluded that the current recommended intake should be enough for African Americans, the same as everyone else. “Anything above 800 IU, it’s not clear that there’s a real need for that,” Brown says.
Could higher doses have benefits?
More than two decades ago, scientists began to make observations suggesting that vitamin D at higher doses could have benefits beyond bone health. Dozens of studies described strong correlations between people’s vitamin D levels and a range of diseases like cardiovascular disease, type 2 diabetes and certain cancers. The lower someone’s vitamin D levels were, the likelier they were to have these diseases, while higher levels were associated with being healthier.
Other research showed that many cell types—in the lungs, heart and immune system—have receptors for the vitamin to dock onto , hinting at far-reaching effects across the body. Giving vitamin D to lab mice with conditions mimicking human diseases could often improve their ailments. Vitamin D, it seemed, might help to tackle the major diseases of our time.
From New Zealand to Europe to North America, scientists launched large clinical trials, enrolling thousands of people over multiple years, to test whether vitamin D supplements would decrease their risk of disease. Importantly, the studies focused on members of the general public, who were largely healthy and had adequate levels of vitamin D. These people then received relatively large doses, of 2,000 or 4,000 IUs or even higher. The studies asked whether there were benefits from getting more than the recommended dietary allowance and ending up with blood levels even higher than 20 or 30 nanograms per milliliter, Manson explains.
To the disappointment of many scientists, giving these generous doses to healthy people didn’t change their risk of developing cancer, heart disease or asthma, nor did it significantly prevent the progression to type 2 diabetes . Extra vitamin D beyond the recommended levels didn’t even do anything to improve bone health or reduce the risk of fractures .

There may be a simple biological reason why more vitamin D isn’t necessarily better: The version of vitamin D found in supplements needs to be converted in the liver and kidneys to reach its final, active form—and that process is probably tightly controlled, says Bouillon. “The body regulates that so you have the exact amount, and not more than what you need.”
The takeaway, many experts agree, is that most healthy people aren’t going to benefit from high doses of vitamin D if they already have enough. The tantalizing associations that led researchers to suspect additional powers of vitamin D could have been an illusion: People with illnesses may end up with lower vitamin D levels because of the diseases themselves, or the unhealthy lifestyles that caused them, says Bouillon.
Are larger doses ever helpful?
A few of the recent trials hinted that some groups of people may benefit from higher doses, but these possible benefits need to be confirmed in further studies, says Manson, who ran one of the trials, called VITAL, which studied nearly 26,000 US adults over five years and looked at supplements of 2,000 IUs of vitamin D as well as omega-3 fatty acids. In that study, participants didn’t have a lower risk of developing cancer but they did have a 25 percent lower chance of it metastasizing or becoming fatal. Perhaps, says Manson, vitamin D makes tumors less likely to metastasize and kill. VITAL also reported that high doses of vitamin D made people less likely to develop certain autoimmune conditions like rheumatoid arthritis, psoriasis and lupus.
Manson notes that these benefits appeared to be most visible among people with a healthy weight, compared to overweight or obese participants. But she cautions that more research is needed to understand these observations and confirm the observed benefits of larger doses.
Physicians in clinical practice, of course, have leeway in prescribing higher doses to certain people as they see fit, such as for osteoporosis patients, or people with conditions that hamper the absorption of vitamin D through the diet, like Crohn’s disease and ulcerative colitis.
What don’t we know yet?
As they probe potential effects of higher doses in non-deficient people, researchers still don’t know how many roles vitamin D might have. The trouble is that recent trials don’t tell us whether having enough vitamin D is important for maintaining healthy heart function or avoiding cancer, for instance—only that having more than that won’t help in most cases.
To prove that adequate vitamin D has health benefits beyond keeping bones strong, scientists need more research in which some deficient people receive supplements and the rest receive a placebo. But such studies are hard to conduct in places like the US, where severe deficiencies are relatively rare. It’s also not ethically justifiable to seek out people who are deficient and then deprive half of them of much-needed supplements, because of the risk of poor bone health in vitamin D-deficient people.
Some scientists believe that having enough vitamin D could be key to maintaining heart and immune system health and preventing diabetes and cancer—and perhaps even be important for brain function, athletic performance and other claims. The evidence is particularly strong in the immune system, says Hewison, whose research points to key roles of vitamin D in immune cells; and indeed, human trials that by chance included some deficient people show benefits of supplementation in warding off infections.
But there just aren’t enough data yet, Hewison says. “I think this is the issue facing the field as a whole.”
This article originally appeared in Knowable Magazine , an independent journalistic endeavor from Annual Reviews. Sign up for the newsletter .
Editor’s note: This story was updated on April 23, 2024, to correct editorial style for identifying racial groups.
Like science, tech, and DIY projects?
Sign up to receive Popular Science's emails and get the highlights.
Vitamin D and Human Health
Affiliation.
- 1 Department of Histology, Medical University of Gdańsk, 80-211 Gdańsk, Poland. [email protected].
- PMID: 30609781
- PMCID: PMC6337085
- DOI: 10.3390/ijms20010145
Vitamin D is currently one of the hottest topics in research and clinics, as well as in everyday life. Over the past decades, scientists gathered overwhelming evidence indicating that the observed global vitamin D deficiency not only has a negative impact on human skeletal system, but also facilitates development and progression of multiple disease of civilization, including cardiovascular diseases, diabetes, autoimmune disease, and cancer. This Special Issue, entitled "Vitamin D and Human Health", summarizes recent advances in our understanding of pleiotropic activity of vitamin D in the form of eight comprehensive reviews. Furthermore, eight research papers provide new insight into vitamin D research and highlight new directions.
Keywords: analogs of vitamin D; extra-skeletal effects of vitamin D; supplementation; therapy and prevention; vitamin D; vitamin D activity and metabolism; vitamin D deficiency.
Publication types
- Introductory Journal Article
- Adaptive Immunity
- Cardiovascular Diseases / metabolism
- Cardiovascular Diseases / pathology
- Dietary Supplements
- Neoplasms / metabolism
- Neoplasms / pathology
- Receptors, Calcitriol / genetics
- Receptors, Calcitriol / metabolism
- Vitamin D / analogs & derivatives
- Vitamin D / blood
- Vitamin D / metabolism*
- Vitamin D Deficiency / metabolism
- Vitamin D Deficiency / pathology
- Receptors, Calcitriol
Home — Essay Samples — Nursing & Health — Human Physiology — Vitamin D for human body
Vitamin D for Human Body
- Categories: Human Physiology Prostate Cancer Vitamins
About this sample

Words: 327 |
Published: Mar 1, 2019
Words: 327 | Page: 1 | 2 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr Jacklynne
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 416 words
2 pages / 698 words
5 pages / 2476 words
3 pages / 1416 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Minerals and water are foundational components of the human body, each playing a unique and essential role in maintaining physiological functions and overall health. In this essay, we will explore the importance of minerals, [...]
Enzymes are essential biological molecules that catalyze biochemical reactions in living organisms. One such enzyme, amylase, plays a crucial role in the digestion of carbohydrates in the human . This essay will explore the [...]
Water is a fundamental substance for all living organisms on Earth. It plays a crucial role in various biological processes, including metabolism, digestion, and temperature regulation. One of the unique properties of water is [...]
The ancient philosophy asserting that "a healthy mind resides in a healthy body" has stood the test of time, reverberating through centuries as a guiding principle for holistic wellness. This statement advocates for the [...]
In the history of psychology, there have been many different fields of interest. Human development, especially, has been one of the interesting fields of study for many psychologists. Freud, Erikson, and Piaget are all great [...]
Optimism is a point of view that includes being positive and having hope for the best outcome. It is believing in the best even when the situation might seem the worst. It is very important to have optimism in today’s world. [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Vitamin D and Calcium Supplementation Essay
Vitamin d and calcium, literature review, methodology.
The associated with vitamin D and calcium publications are primarily based on their respective supplements’ health effects. They have clarified an interesting scenario regarding the consumption of these elements. The landscape of vitamin D and Ca can be observed across different populations. To test the prevalence of vitamin D and Ca deficiency, similarities, and differences, alongside their health benefits, a cross-sectional study was deliberated in Sharjah, United Arab Emirates. The research established that these elements are synergistic and integral for immunological functions, including the formation of healthy teeth. However, they displayed characteristic physiological differences. Sources and resources used in the study were obtained from internet sources. Sites like Google Books, Google Scholar, and EBSCOhost were used to acquire possible research information. Intending to seek facts and evidence surrounding the health benefits of Ca and vitamin D, the research established research gaps like the high prevalence of vitamin D and Ca deficiencies among the study group regardless of the increasing literacy and education levels.

Introduction
There have been numerous publications associated with the various aspects of vitamin D and calcium. The studies primarily focus on the physiological and therapeutic aspects of the micronutrient. The florid scientific literature does not eliminate the uncertainty on numerous issues. For example, there is no consensus on the importance of vitamin D and calcium in people’s health and well-being. Endless debates have been highlighted, including the standard means of measuring the 25-hydroxyvitamin D (25(OH) D), precursors, and metabolites. Excessive calcium absorption could lead to nephrolithiasis and nephrocalcinosis 1 . The other debate is associated with hypovitaminosis in the general population concerning a specific clinical condition such as pregnancy and health condition. The research will focus on vitamin D and calcium issues concerning the modalities used to ensure sufficiency and health benefits. The target group will be the United Arab Emirates population that has faced significant health issues associated with the nutrients.
Roles of Vitamin D in the Body
Vitamin D is essential for physiology and anatomy. First, vitamin D is preventing rickets’ development. The formation of healthy bones is dependent on this element’s presence, but it is also influenced by calcium. Vitamin D enhances dietary calcium intake, a mineral integral to the formation of such bust bones. Secondly, it promotes the physiology of parathyroid glands. Because they balance calcium levels via the kidney, vitamin D is directly involved in homeostasis maintenance 2 . Calcium and/or vitamin D insufficiency condition parathyroid glands to break down bones to obtain calcium or vitamin D.
Functions of Ca
While 99% of it is located in teeth, bones, calcium is also found in body fluids, blood, tissues, and nerve cells. The intake of calcium helps with the coagulation, healthy forming of bones, sending and reception of nerve signals, squeezing and relaxing muscle cells, releasing hormones and other chemicals essential for body functioning, and maintaining a regular heartbeat. After a human being stops growing, calcium is vital to maintaining the bone structure. The mineral is also crucial in ensuring that the bone density growth is minimal. Noteworthy, diminishing bone density is a natural part experienced in the aging process. The mineral is also essential in the cardiovascular system because it is one of the agents supporting blood clotting. Some studies have correlated much calcium intake with a low prevalence of high blood pressure 3 . The rationale behind the indication is that calcium is responsible for relaxing the muscles surrounding blood vessels.
Effects of Vitamin D and Ca Deficiency in the Body
Poor immunity, allergic responses, and enhanced weight loss.
Their physiological functions inform the effects of Vitamin D-Calcium deficiencies. First, Vitamin D promotes immunity and is expressed on immunologic cells such as B and T cells and antigen. Secondly, Vitamin D can help prevent various infectious diseases; therefore, it can improve current global public health associated with the COVID-19 pandemic 4 . Calcium is required for activating the immune system when it enters immune cells, especially those involved in allergic responses. In lymphocytes, calcium ions act as intermediaries that trigger lymphocytes’ actions. Vitamin D and calcium combination enhances calcium absorption, hence a necessity among obese individuals because of enhanced weight loss. Current evidence on vitamin D and calcium combination also cite helping with the weight loss. The latter indirectly reduces comorbidities like hypertension or diabetes. Therefore, vitamin D and calcium deficiency leads to low immune and allergic responses. The rationale of this argument regards the pivotal roles they play in enhancing immunity and allergic reactions.
Diseases like Osteoporosis and Poor Related Physiological Functions
Vitamin D and calcium are equally integral to the formation of healthy bones and teeth, and this vitamin insufficiency leads to poor Ca absorption. Because both of these elements are similarly essential, in case of deficiency, bones will be degraded, as well as physiological functions like the formation of bone marrow and immune cells.
Gaps in Existing Literature
The following are some of the gaps in the literature;
- High rates of supplement ignorance across the sample population
- Even though the global community is becoming more literate, vitamin D and calcium deficiencies are equally increasing. The scene is quite surprising because increasing literacy across the global population should inform the appreciation of vitamin D and calcium supplements.
- Medical professionals’ response and roles in addressing or stressing the importance and benefits of supplements across the study group of the global population.
- Vitamin D and calcium interplay and their concomitant/synergistic roles in facilitating human health and well-being.
- The increasing vitamin D and calcium deficiency despite increasing literacy across the global population.
Aims of the Paper
The primary aim of this paper is to clear the debate surrounding vitamin D and calcium supplements. The discussion covers the prevalence of vitamin D and calcium deficiency in the UAE. The discussion is based on a practical approach via a cross-sectional study in Sharjah to display vitamin D and calcium prevalence, alongside the specimen’s health effects.
Research Design
A cross-sectional research design was used to study the specimen, n=480, in Sharjah. They were randomly selected from Sharjah’s population. The study grouped aged between 5 to 79 years. The actual research was conducted at the American University of Sharjah, UAE 5 . Ethical values and competence are crucial elements in such studies. A mixed methodology was used in the survey to acquire qualitative and quantitative data about the topic. Qualitative and quantitative data is necessary to account for a given phenomenon according to the figures captured among the participants 6 . An open-ended questionnaire was administered to the patients to obtain data on their condition. They elaborated on their health based on vitamin D deficiency. A survey was also conducted across Sharjah’s medical facilities to establish the trends and patterns of consumption of drugs concerning vitamin D deficiency and calcium-related complications. The survey stretched to the business sector to obtain statistical data and qualitative comments from supplement dealers. The study majorly discovered demographic information on the prevalence of vitamin D deficiency, their dietary practices, exposure to the sun, immunity, and comorbidities related to low immunity. The data captured the specific figure of Sharjah’s vitamin D deficient individuals. The latter was also tied to calcium-related health issues like osteoporosis, low immunity, and weak teeth.
A demonstration of the research and search phrases are highlighted in Fig. 1. The process involved searching through databases to identify critical literature. Some of these databases and research browse include ‘EBSCOhost,’ ‘Google Books,’ ‘Science Direct,’ and ‘Google Scholar.’ However, the search was run using essential words and phrases relevant to the research topic. These are ‘vitamin D,’ ‘calcium mineral,’ ‘Hypovitaminosis D,’ ‘Osteomalacia,’ ‘Osteoporosis,’ ‘Calcium,’ and ‘Vitamin.’ Age and relevance filters were further used to qualify or discredit material found using this technique. For instance, papers were only considered if published after 2015 to increase data relevance and accuracy. Twelve articles were eventually considered after critical evaluation for relevance to the study.
Research Agents Used and the Wording Employed to Acquire the Sources
The following flow chart shows research agents and wording used to acquire data in the research;
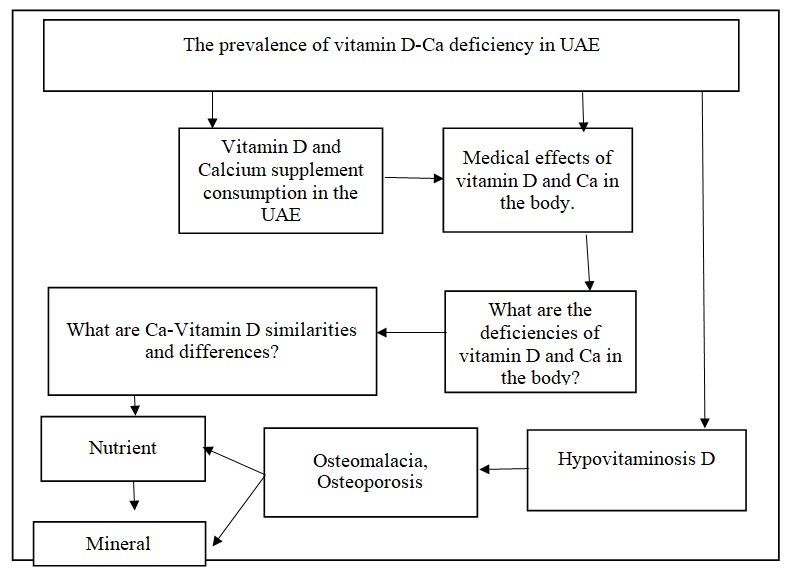
The Prevalence of Vitamin D and Calcium Deficiency in UAE
UAE’s vitamin D deficiency victims rangers between 50% to 90% of the total population who suffer from osteoporosis 7 8 .The study found that at least 90% of the participants were suffering from vitamin D deficiency. The conclusion that 90% of the population experienced vitamin D deficiency was drawn from the results’ multidimensional elements. The most prevalent aspect of vitamin D deficiency across the specimen were fatigue, painful bones, and muscle weaknesses. Both young and elderly participants complained about the complications mentioned above. They were registered to have consumed painkillers and medicines addressing bone-related disorders. The medical practitioners and clinicians in the medical facilities commented on the same by asserting the vitamin D deficiency resulted in those conditions due to low calcium absorption. Data collected from medical facilities and supplement dealers indicated low supplement consumption. While 92% of supplement dealers cited caution among Sharjah’s residents on safety issues surrounding the supplements, medical facilities stressed that UAE residents would never consume supplements whatsoever. The study group indicated an attitude and negative perception of the supplements based on perceived adverse effects and health implications conferred by supplements. Participants also stated that they were not exposed to the sun.
Nutritional entries often fail to emphasize the importance of calcium as a singular mineral in the human body. Most studies are quick to divert from this topic after highlighting the essential role of vitamin D and calcium deficiency instances. Nimri notes that “Vitamin D deficiency is most often associated with inadequate calcium intakes and causes bone degeneration or osteoporosis” 9 .Therefore, Ca deficiency cases are overshadowed by vitamin D deficiency issues, making it difficult to locate information for this statistic alone. However, Nimri explains the decrease in Ca intake among youth by the popularity of carbonated drinks over healthier choices like milk. Therefore, cases of vitamin D are a manifestation of Ca deficiencies that contributes to weak bones.
The Prevalence of the Usage of Vitamin D and Calcium Supplements
While 70% of the study group were unaware of the importance of sun exposure in acquiring vitamin D, 30% were unconcerned with exposure to the sun. 60% of the study group indicated that they never consume foods rich in vitamin D like fish liver oils and fatty fish like tuna, salmon, mackerel, and trout. Laboratory tests on calcium deficiency were tied to vitamin D deficiency. Individuals composing 90% of participants found with vitamin D deficiency were found with calcium deficiency. The figure indicated a direct relationship between vitamin D deficiency and calcium deficiency. 20% of the affected population was subjected to treatment to test the parathyroid organs’ effectiveness and roles.
The Medical Effects of the Supplements
Medical effects of ca supplements.
- Constipation
- Prevention against osteoporosis by inhibiting osteopenia
- Formation of strong teeth and bones
- Weight loss
- Regulation of phosphorus, magnesium, and potassium in the blood
Medical Effects of Vitamin D Supplements
- High calcium absorption
- Regulates phosphorus and calcium absorption
- Boosting immunity and preventing depression
- Promoting weight loss
Similarities Between Vitamin D and Calcium
- Maintaining homeostasis of the skeletal system.
- Formation of strong bones and teeth
- A healthy skeletal system produces vibrant blood cells.
- White blood cells are integral to fighting diseases.
- Hypertension
- Musculoskeletal diseases 10
- The two elements need and/or rely on each other to deliberate their functions
- They can be supplied by diet and supplements.
Differences Between Vitamin D and Calcium
Vitamin D and calcium differences regard physiological elements and sources. While vitamin D is freely and naturally available from the sun and enhances Ca absorption, the final is integral for forming healthy teeth and bones. Unlike vitamin D, Ca not be obtained freely from the sun. It can be obtained from diet and supplements.
Al Kattub (2017) argues that vitamin D deficiency predisposes individuals to heart disease, kidney disease, hypertension, liver disease, and disease 11 . The argument encapsulates a multidimensional element on the subject because of Vitamin D and Calcium interaction and immunity development roles. Further, organ failure is another contributing factor to the conditions mentioned above. Vitamin D is needed to facilitate calcium absorption from dietary foodstuffs, and calcium is required in order to form a robust immune system. Therefore, individuals suffering from vitamin D deficiency will undoubtedly suffer from calcium deficiency and equally low immunity. Sharjah’s studied population is a classic reflection and illustration of the perspective issued above. The community stressed that they hardly consume vitamin D rich foods mentioned earlier and are do not bask in the sun. The sun is a free source of vitamin D. Therefore, they are not immune to the health complications and developmental problems associated with vitamin D and calcium deficiency.
Vitamin D and calcium is found to be an element among the study population. With the laboratory tests revealing abnormally minimal metabolites and precursors of 25-hydroxyvitamin D and the participants’ confession of minimal and/or no consumption of vitamin D rich foods, the conclusion that the debate surrounds negligence and negative perception of supplements is inevitable. 90% of the specimen would have been saved via supplement consumption. However, the negative perception of supplements prevented their consumption and informed unsatisfactory purchases from dealers. Medical and health issues found among the participants are an image of caution and safety issues posited regardless of whether they are relevant. Arguably, the safety issues and concerns are somewhat blown out of proportion because the supplements pass quality tests and safety measures and guidelines established to guide their manufacturing and production.
- Abrahamsen, B. (2017). The calcium and vitamin D controversy. Therapeutic Advances in Musculoskeletal Disease, 9 (5), 107-114. Web.
- Baran, M., & Jones, J. (2016). Mixed methods research for improved scientific study .
Ferretti, M., Cavani, F., Roli, L., Checchi, M., Magarò, M. S., Bertacchini, J., & Palumbo, C. (2019). Interaction among Calcium Diet Content, PTH (1-34) Treatment and Balance of Bone Homeostasis in Rat Model: The Trabecular Bone as Keystone. International Journal of Molecular Sciences, 20 (3). Web.
- Khazai, N., Judd, S. E., &Tangpricha, V. (2008). Calcium and vitamin D: skeletal and extraskeletal health. Current rheumatology reports , 10 (2), 110-117.
- Kuttab, J. (2017). Vitamin D deficiency could cause deadly diseases, warn UAE doctors. Web.
Liu, M., Yao, X., & Zhu, Z. (2019). Associations between serum calcium, 25(OH)D level and bone mineral density in older adults. Journal of Orthopaedic Surgery and Research, 14 , 1-7. Web.
- Nimri, L. F. (2018). Vitamin D status of female UAE college students and associated risk factors. Journal of Public Health , 40 (3), e284-e290.
Palacios, C., & Gonzalez, L. (2014). Is vitamin D deficiency a major global public health problem?. The Journal of steroid biochemistry and molecular biology , 144 , 138-145.
Reid, I. R., &Bolland, M. J. (2019). Controversies in medicine: the role of calcium and vitamin D supplements in adults. Medical Journal of Australia , 211 (10), 468-473.
Sahay, M., & Sahay, R. (2012). Rickets–vitamin D deficiency and dependency. Indian journal of endocrinology and metabolism , 16 (2), 164.
Shakoor, H., Feehan, J., Al Dhaheri, A. S., Ali, H. I., Platat, C., Ismail, L. C.,… & Stojanovska, L. (2020). Immune-boosting role of vitamins D, C, E, zinc, selenium and omega-3 fatty acids: could they help against COVID-19?. Maturitas .
- Liu, M., Yao, X., & Zhu, Z. (2019). Associations between serum calcium, 25(OH)D level, and bone mineral density in older adults. Journal of Orthopaedic Surgery and Research, 14 , 1-7. Web.
- Ferretti, M., Cavani, F., Roli, L., Checchi, M., Magarò, M. S., Bertacchini, J., & Palumbo, C. (2019). Interaction among Calcium Diet Content, PTH (1-34) Treatment and Balance of Bone Homeostasis in Rat Model: The Trabecular Bone as Keystone. International Journal of Molecular Sciences, 20 (3) Web.
- Shakoor, H., Feehan, J., Al Dhaheri, A. S., Ali, H. I., Platat, C., Ismail, L. C.,… & Stojanovska, L. (2020). Immune-boosting role of vitamins D, C, E, zinc, selenium, and omega-3 fatty acids: could they help against COVID-19. Maturitas .
- Palacios, C., & Gonzalez, L. (2014). Is vitamin D deficiency a significant global public health problem? The Journal of steroid biochemistry and molecular biology , 144 , 138-145.
- Nimri, L. F. (2018). Vitamin D status of female UAE college students and associated risk factors, e284.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 27). Vitamin D and Calcium Supplementation. https://ivypanda.com/essays/vitamin-d-and-calcium-supplementation/
"Vitamin D and Calcium Supplementation." IvyPanda , 27 Mar. 2024, ivypanda.com/essays/vitamin-d-and-calcium-supplementation/.
IvyPanda . (2024) 'Vitamin D and Calcium Supplementation'. 27 March.
IvyPanda . 2024. "Vitamin D and Calcium Supplementation." March 27, 2024. https://ivypanda.com/essays/vitamin-d-and-calcium-supplementation/.
1. IvyPanda . "Vitamin D and Calcium Supplementation." March 27, 2024. https://ivypanda.com/essays/vitamin-d-and-calcium-supplementation/.
Bibliography
IvyPanda . "Vitamin D and Calcium Supplementation." March 27, 2024. https://ivypanda.com/essays/vitamin-d-and-calcium-supplementation/.
- Osteoporosis, Risk Factors, Treatment, & T Score
- Vitamin A Supplementation for Infants
- Thiamine Supplementation in the Critically Ill
- Calcium Is An Essential Mineral For Our Bodies
- Folate: The Introduction Into ESCs Pregnancy Supplement
- Vitamin D and Dyslipidemia in Metabolic Syndrome
- Osteoporosis: Definition, Epidemiology, and Pathophysiology
- Osteoporosis: Pathophysiology and Management
- The effect of glucosamine supplementation on people
- Vitamin and Supplement Treatments: Good or Bad?
- Food Safety Policy and Inspection Services
- A Nutrition and Coaching Plan for an Obese Woman
- Nutrition Coach Certification and Planning
- Regulation of Metabolism and Eating Disorders
- Understanding the Lived Experience of Chronic Illness

- Our Services
- --> Resumes & CV -->