
- Issue Brief

Health Care Costs: What’s the Problem?
The cost of health care in the United States far exceeds that in other wealthy nations across the globe. In 2020, U.S. health care costs grew 9.7%, to $4.1 trillion, reaching about $12,530 per person. 1 At the same time, the United States lags far behind other high-income countries when it comes to both access to care and some health care outcomes. 2 As a result, policymakers and health care systems are facing increasing demands for more care at lower costs for more people. And, of course, everyone wants to know why their health care costs are so high.
The answer depends, in part, on who’s asking this question: Why does U.S. health care cost so much? Public policy often highlights and targets the total cost of the health care system or spending as a percentage of the gross domestic product (GDP), while most patients (the public) are more concerned with their own out-of-pocket costs and whether they have access to affordable, meaningful insurance. Providers feel public pressure to contain costs while trying to provide the highest-quality care to patients.
This brief is the first in a series of papers intended to better define some of the key questions policymakers should be asking about health care spending: What costs are too high? And can they be controlled through policy while improving access to care and the health of the population?
What (or Who) Is to Blame for the High Costs of Care?
Total U.S. health care spending has increased steadily for decades, as have costs and spending in other segments of the U.S. economy. In 2020, health care spending was $1.5 trillion more than in 2010 and $2.8 trillion more than in 2000. While total spending on clinical care has increased in the past two decades, health care spending as a percentage of GDP has remained steady and has hovered around 20% of GDP in recent years (with the largest single increase being in 2020 during the COVID-19 pandemic). 1 Health care spending in 2020 (particularly public outlays) increased more than in previous years because of increased federal government support of critical COVID-19-related services and expanded access to care during the pandemic. Yet, no single sector’s health care cost — doctors, hospitals, equipment, or any other sector — has increased disproportionately enough over time to be the single cause of high costs.
One of the areas in health care with the highest levels of spending in the United States is hospital care, which has accounted for about 30% of national health care spending 3 for the past 60 years (and has remained very close to 31% for the past 20 years) (Figure 1). Although hospital spending is the focus of many cost-control policies and public attention, the increases are consistent with the increases seen across other areas of health care, such as for physicians and other professional services. Total spending for some smaller parts of nonhospital care has more than doubled over the past few decades and makes up an increasing proportion of total spending. For instance, home health care as a percentage of total spending tripled between 1980 and 2020, from 0.9% to 3.0%, and drug spending nearly doubled as a proportion of health care spending between 1980 and 2006, from 4.8% to 10.5%, and currently represent 8.4% of health care spending. 1
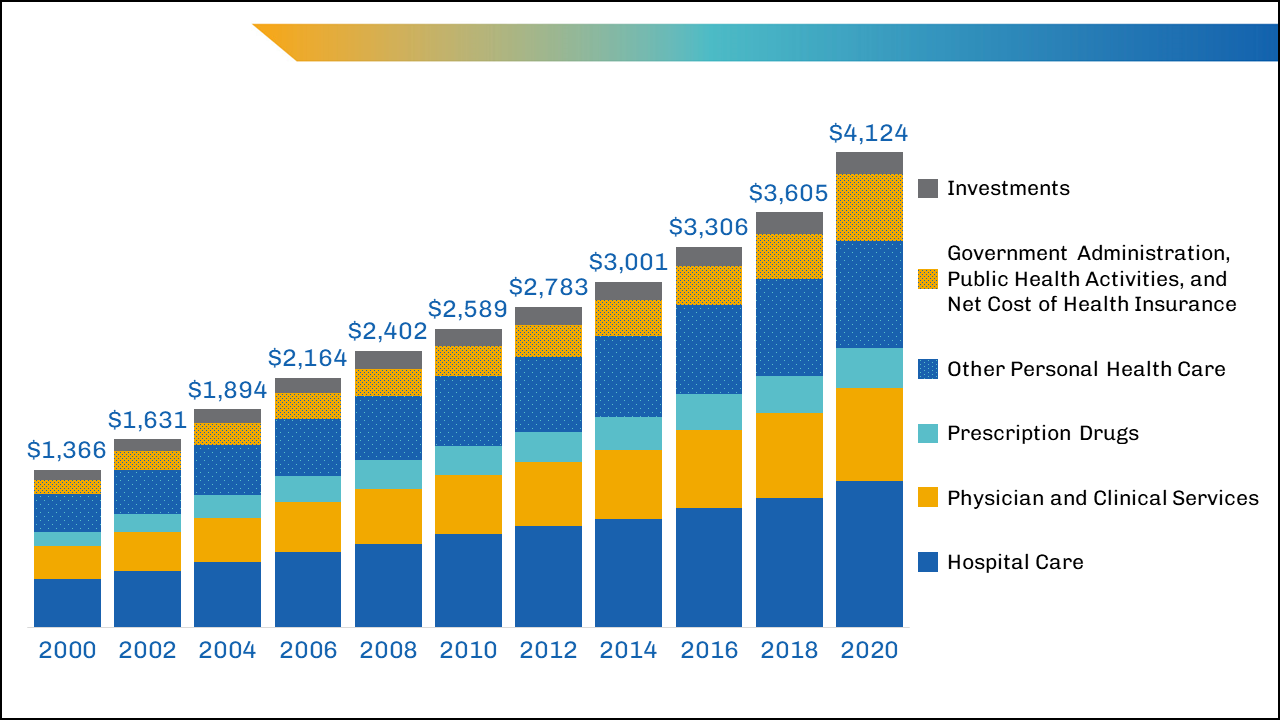
image description
The largest areas of spending that might yield the greatest potential for savings — such as inpatient care and physician-provided care — are unlikely to be reduced by lowering the total number of insured patients or visits per person, given the growing, aging U.S. population and the desire to cover more, not fewer, individuals with adequate health insurance.
In the past decade, policymaker and insurer interventions intended to change the mix of services by keeping patients out of high-cost settings (such as the hospital) have not always succeeded at reducing costs, although they have had other benefits for patients. 4
Breaking Down the Costs of Care
Thinking about total health care spending as an equation, one might define it as the number of services delivered per person multiplied by the number of people to whom services are delivered, multiplied again by the average cost of each service:
Health Care Spending=(number of services delivered per person)×(number of people to whom services are delivered)×(average cost of each service)
Could health care spending be lowered by making major changes to the numbers or types of services delivered or by lowering the average cost per service?
Although recent data on the overall utilization of health care are limited, in 2011, the number of doctor consultations per capita in the United States was below that in many comparable countries, but the number of diagnostic procedures (such as imaging) per capita remained higher. 5 Furthermore, no identifiable groups of individuals (by race/ethnicity, geographic location, etc.) appear to be outliers that consume extraordinary numbers of services. 6 The exception is that the sickest people do cost more to take care of, but even the most cost-conscious policymakers appear to be reluctant to abandon these patients.
In addition to the fact that the average number of health care services delivered per person in the United States was below international benchmarks in 2020,7 the percentage of people in the United States covered by health insurance was also lower than that in many other wealthy nations. Although millions of people gained insurance8 through the Affordable Care Act and provisions enacted during the COVID-19 pandemic, 10% of the nonelderly population remained uninsured in 2020. 9 When policymakers focus on reducing health care spending, considering the equation above, and see that the United States already has a lower proportion of its population insured and fewer services delivered to patients than other wealthy nations, their focus often shifts to the average cost of services.
It's Still the Prices … and the Wages
A report comparing the international prices of health care in 2017 found that the median list prices (charges) for medical procedures in the United States heavily outweighed the list prices in other countries, such as the United Kingdom, New Zealand, Australia, Switzerland, and South Africa. 10
For example, the 2017 U.S. median health care list price for a hospital admission with a hip replacement was $32,500, compared with $20,900 in Australia and $12,200 in the United Kingdom. In comparisons of the list prices of other procedures, such as deliveries by cesarean section, appendectomies, and knee replacements, the U.S. median list prices of elective and needed services were thousands of dollars — if not tens of thousands of dollars — more. 10 Yet, the list price for these services in the United States is often much higher than the actual payments made to providers by public or private insurance companies. 11
Public-payer programs (particularly Medicare and Medicaid) tend to pay hospitals rates that are lower than the cost of delivering care12 (though many economists argue these payments are slightly above actual costs, and providers argue they are at least slightly below actual costs), while private payers historically have paid about twice as much as public payers. 13 (See another brief in this series, “ Surprise! Why Medical Bills Are Still a Problem for U.S. Health Care ,” for more information about public and private payers’ role in health care costs.) However, the average cost per service is still high by international standards, even if it’s not as high as list prices may suggest. The high average costs are partially driven by the highly labor-intensive nature of health care, with labor consuming almost 55% of the share of total U.S. hospital costs in 2018. 14 These costs are growing due to the labor shortages exacerbated by the COVID-19 pandemic.
Reducing U.S. health care spending by reducing labor costs could, theoretically, be achieved by reducing wages or eliminating positions; however, both of those policies would be problematic, with potential unintended consequences, such as driving clinicians away from the workforce at a time of growing need.
Wage reductions, particularly for clinicians, would require a vastly expanded labor pool that would take years to achieve (and even then, lower per person wages for nonphysicians may not decrease total spending related to health care labor). 15 Reducing or replacing clinical workers over time would require major changes to policy (both public and private) and major shifts in how health care is provided — neither of which has occurred rapidly, even since the implementation of the Affordable Care Act.
What’s a Policymaker to Do?
Nearly one in five Americans has medical debt, 16 and affordability is still an issue for a large proportion of the population, whether uninsured or insured, which suggests that policymakers should focus on patients’ costs. This may prove more impactful to the individual than reducing total health care spending.
A majority of the country agrees that the federal government should ensure some basic health insurance for all citizens. 17,18 Although most Americans consider reducing costs to individuals and expanding insurance coverage to be important, no clear consensus about who should bear any associated increased costs exists among patients or policymakers. Half of insured adults currently report difficulty affording medical or dental care, even when they are insured, because of the rising total costs of care and the increasing absolute amount of out-of-pocket spending. 19 Out-of-pocket spending for health care has doubled in the past 20 years, from $193.5 billion in 2000 to $388.6 billion in 2020. 1 These rising health care costs have disproportionately fallen on those with the fewest resources, including people who are uninsured, Black people, Hispanic people, and families with low incomes. 19 Increased cost sharing through copays and coinsurance may force difficult spending choices for even solidly middle-class families.
The severity and burden of out-of-pocket spending are hidden by the use of data averages; on average, U.S. residents have twice the average household net adjusted disposable income 20 of many other comparable nations and spend more than twice 21 as much per capita on health care. Yet, for those who fall outside these averages — average income, average costs, or both — the financial pain felt at the hospital, clinic, and pharmacy is very real.
In any given year, a small number of patients account for a disproportionate amount of health care spending because of the complexity and severity of their illnesses. Even careful international comparisons of end-of-life care for cancer patients demonstrate costs in the United States are similar to those in many comparable nations (although U.S. patients are more likely to receive chemotherapy, they spend fewer days in the hospital during the last 6 months of life than patients in other countries). 22 Similarly, although prevention efforts may delay or avoid the onset of illness in targeted populations, such efforts would not significantly reduce the number of services delivered for many years and may lead to an increase in care delivered over the course of an extended life span.
To the average person in the United States, immediate cost-control efforts might best be focused on reducing the cost burden for families and patients. Policymakers should continue to seek ways to promote better health care quality at lower costs rather than try to achieve unrealistic, drastic reductions in national health care spending. Investing in prevention, seeking to avoid preventable admissions or readmissions, and otherwise improving the quality of care are desirable, but these improvements are not quick solutions to lowering the national health care costs in the near term. Long-term policy actions could incrementally address health care spending but should clearly articulate the problem to be solved, the desired outcomes, and the trade-offs the nation is willing to make (as discussed in two companion pieces).
The U.S. health care system continues to place a disproportionate cost burden on the patients who can least afford it. In the short term, policymakers could focus on targeted subsidies to specific populations — the families and individuals whose household incomes fall outside the average or who have health care expenses that fall outside the average — whose health care costs are unmanageable. Such subsidies could expand existing premium subsidies or triggers that increase support for costs that exceed target amounts. Targeted subsidies are likely to increase total health care spending (especially public spending) but would address the problem of cost from the average consumer, or patient, perspective. Broader policies to ease costs for patients could also be considered by category of service; for instance, consumers have been largely shielded from the increased costs of care related to COVID-19 by the waiving of copays for patients and families. These policies would likely increase national spending as well, but they would make medical care more affordable to some families.
Download Brief
Cite this source: Grover A, Orgera K, Pincus L. Health Care Costs: What's The Problem? Washington, DC: AAMC; 2022. https://doi.org/10.15766/rai_dozyvvh2
- Centers for Medicare & Medicaid Services. National Health Expenditure Data. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet . Published Dec. 1, 2021. Accessed Feb. 24, 2022.
- Schneider EC, Shah A, Doty MM, Tikkanen R, Fields K, Williams RD II. Mirror, Mirror 2021 — Reflecting Poorly: Health Care in the U.S. Compared to Other High-Income Countries. Washington, DC: The Commonwealth Fund. https://doi.org/10.26099/01DV-H208 . Published August 2021. Accessed April 21, 2022.
- Centers for Medicare & Medicaid Services. National Health Expenditure Data: Historical. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical . Published Dec. 15, 2021. Accessed April 22, 2022.
- Berkowitz S, Ricks KB, Wang J, Parker M, Rimal R, DeWalt D. Evaluating a nonemergency medical transportation benefit for accountable care organization members. Health Affairs. 2022;41(3):406-413. doi:10.1377/hlthaff.2021.00449.
- Organisation for Economic Co-operation and Development. Health Care Utilisation. Paris, France: Organisation for Economic Co-operation and Development. https://stats.oecd.org/index.aspx?queryid=30166# . Published Nov. 9, 2021. Accessed Feb. 24, 2022.
- Abelson R. Harris G. Critics question study cited in health debate. New York Times. June 2, 2010. https://www.nytimes.com/2010/06/03/business/03dartmouth.html?ref=business&pagewanted=all . Accessed Feb. 24, 2022.
- The Commonwealth Fund. Selected Health & System Statistics: Average Annual Number of Physician Visits per Capita. https://www.commonwealthfund.org/international-health-policy-center/system-stats/annual-physician-visits-per-capita . Published June 5, 2020. Accessed April 21, 2022.
- Tolbert J, Orgera K. Key Facts About the Uninsured Population. San Francisco, CA: KFF. https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population/ . Published Nov. 6, 2020. Accessed April 21, 2022.
- Tolbert J, Orgera K, Damico A. What Does the CPS Tell Us About Health Insurance Coverage in 2020? San Francisco, CA: KFF. https://www.kff.org/uninsured/issue-brief/what-does-the-cps-tell-us-about-health-insurance-coverage… . Published Sept. 23, 2021. Accessed April 21, 2022.
- Hargraves J, Bloschichak A. International Comparisons of Health Care Prices From the 2017 iFHP Survey. Washington DC: Health Care Cost Institute. https://healthcostinstitute.org/hcci-research/international-comparisons-of-health-care-prices-2017-ifhp-survey . Published Dec. 2019. Accessed April 21, 2022.
- Bai G. Anderson G. Extreme markup: The fifty US hospitals with the highest charge-to-cost ratios. Health Affairs. 2015;34(6):922-928. doi:10.1377/hlthaff.2014.1414.
- Congressional Budget Office. The Prices That Commercial Health Insurers and Medicare Pay for Hospitals’ and Physicians’ Services. Washington, DC: Congressional Budget Office. https://www.cbo.gov/system/files/2022-01/57422-medical-prices.pdf . Published January 2022. Accessed April 21, 2022.
- Lopez E, Neuman T, Jacobson G, Levitt L. How Much More Than Medicare Do Private Insurers Pay? A Review of the Literature. San Francisco, CA: The Henry J. Kaiser Family Foundation. https://www.kff.org/medicare/issue-brief/how-much-more-than-medicare-do-private-insurers-pay-a-review-of-the-literature/ . Published April 15, 2020. Accessed March 22, 2022.
- Daly R. Hospitals Innovate to Control Labor Costs. Westchester, IL: Healthcare Financial Management Association. https://www.hfma.org/topics/hfm/2019/october/hospitals-innovate-to-control-labor-costs.html . Published Oct. 1, 2019. Accessed Feb. 24, 2022.
- Batson BN, Crosby SN, Fitzpatrick, JM. Mississippi frontline: Targeting value-based care with physician-led care teams. J Miss State Med Assoc. 2022;63(1):19-21. https://ejournal.msmaonline.com/publication/?m=63060&i=735364&p=20&ver=html5 .
- Kluender R, Mahoney N, Wong F, et al. Medical debt in the US, 2009-2020. JAMA. 2021;326(3):250-256. doi:10.1001/jama.2021.8694.
- Jones B. Increasing Share of Americans Favor a Single Government Program to Provide Health Care Coverage. Washington, DC: Pew Research Center. https://www.pewresearch.org/fact-tank/2020/09/29/increasing-share-of-americans-favor-a-single-government-program-to-provide-health-care-coverage/ . Published Sept. 29, 2020. Accessed April 21, 2022.
- Bialik K. More Americans Say Government Should Ensure Health Care Coverage. Washington, DC: Pew Research Center. https://www.pewresearch.org/fact-tank/2017/01/13/more-americans-say-government-should-ensure-health-care-coverage/ . Published Jan. 13, 2017. Accessed March 22, 2022.
- Kearney A, Hamel L, Stokes M, Brodie M. Americans’ Challenges With Health Care Costs. San Francisco, CA: The Henry J. Kaiser Family Foundation. https://www.kff.org/health-costs/issue-brief/americans-challenges-with-health-care-costs/ . Published Dec. 14, 2021. Accessed Feb. 24, 2022.
- Organisation for Economic Co-operation and Development. Income. Better Life Index. Paris, France: Organisation for Economic Co-operation and Development. https://www.oecdbetterlifeindex.org/topics/income/ . Accessed April 21, 2022.
- Wager E, Ortaliza J, Cox C; The Henry J. Kaiser Family Foundation. Health System Tracker. How Does Health Spending in the U.S. Compare to Other Countries? San Francisco, CA: The Henry J. Kaiser Family Foundation. https://www.healthsystemtracker.org/chart-collection/health-spending-u-s-compare-countries-2/ . Published Jan. 21, 2022. Accessed April 21, 2022.
- Bekelman JE, Halpern SD, Blankart CR, et al. Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA. 2016;315(3):272-283. doi:10.1001/jama.2015.18603.

In her 2016 essay "Cost of Living" for the Virginia Quarterly Review — later anthologized in The Best American Essays — Emily Maloney unravels the juxtaposition of working to pay down her medical debt at a job where she assigns medical costs to treatments — costs that may, in turn, create the same kind of debt for others.
She writes of being 23 and working as an emergency room technician at a Chicagoland hospital, coding charts into bills, determining what to charge for the level of care each patient received: "Each level had its own exacting specifications, a way of making sense — at least financial sense — of the labyrinthine mess of billing."
But Maloney knew from her own experience that medical billing didn't actually compute in a financial sense. Four years earlier, she had been an ER patient at a hospital in Iowa City after a suicide attempt. That hospital stay resulted in a five-figure bill, one she could scarcely have imagined as a 19-year-old college student. "Sitting on a cot in the emergency room, I filled out paperwork certifying myself the responsible party for my own medical care — signed it without looking, anchoring myself to this debt, a stone dropped in the middle of a stream," Maloney writes.
"Cost of Living" — an indictment of the exorbitant costs of staying alive in America, and the weight of being hounded by a debt that reduces your life to dollars and cents — opens Maloney's debut essay collection of the same name. It's a powerful opening shot, but in the essays that follow, which recount Maloney's experiences as patient, caregiver, observer, and pharmaceutical industry worker, she stumbles before regaining the clarity of purpose and rigor of probing that "Cost of Living" promises.
There are 15 essays in Cost of Living , and the six that follow the titular piece feel as though they are narrated from underwater. Perhaps that is because they trace years in which Maloney herself felt that she had "not gotten the memo regarding how to be a person." She writes of being "too odd for elementary school, then secondary school," of attending seven schools in ten years, of difficulty conversing and maintaining eye contact, of seeing multiple psychologists at once.
Among the murkiest essays is "Clipped," which is at once about working as a dog groomer, deciding whether or not to apply to college, and feeling a need to escape her family. Maloney writes of her home life, "I knew something was wrong, that maybe there was a fire and everyone was inside the house." Something is wrong here, but that something is never clearly identified; I found myself waiting for retrospection that never came. "Clipped" feels, itself, clipped — an issue I had with several other essays, which put too much faith in the power of showing, not telling. "Some Therapy," for instance, is a list of 12 therapists, social workers, psychologists, and psychiatrists that Maloney saw, the reasons she was sent to them, and approximately how much they cost. "A Brief Inventory of My Drugs and Their Retail Price" is, well, what it sounds like. In these instances, I didn't know what to make of the litany: It is clear that both the therapy and the drugs weren't the treatment that Maloney actually needed, but unclear where she places the blame.
That Maloney does not even engage in any kind of questioning in these pieces is what makes them lack tension, fall flat. Later essays, where she takes up the same sort of thinking on the page that gives "Cost of Living" its verve, are far more compelling.
Among the best essays in the collection is "Soft Restraints," where Maloney finds a mirror in a woman she calls Elizabeth, who kept thrashing in her ER bed — and digs into the problem of female patients not being taken seriously. Elizabeth's chart labeled her as having borderline personality disorder and fibromyalgia, "a made-up diagnosis for us then, a kind of early aughts placeholder for female hysteria." In contrast is another woman who presents with "the worst headache of her life" and cannot stop crying. "Usually things like this were some kind of conversion disorder, or maybe psychosis," Maloney writes, but instead of resting in that assumption, this patient is sent for a CT scan that reveals a brain tumor the size of a small orange. Maloney herself ended up more like the "orange woman": she was eventually diagnosed correctly with a developmental disorder, hypothyroidism, and a vitamin deficiency, but realizes how she could have become Elizabeth: "It doesn't take much to get addicted to someone taking an interest in who you are, that sometimes all you are looking for is an answer, an explanation for why you feel this way, maybe a box to check or a space to occupy." This kind of zoom out and sustained inquiry is what I longed for in earlier pieces.
The essay that I cannot stop thinking about, though, is "Failures in Communication," where Maloney digs into the ethics of how physicians talk to patients about what is happening inside their bodies. Here, Maloney is no longer an ER tech but a pure observer in a teaching hospital in Pittsburgh, shadowing in an ICU step-down unit for a bioethics course she took while completing her MFA. This unit is where people go after they have survived intensive care, where "patients are responsive, awake, alert...but nevertheless very sick. This is the hardest part of patients and families to understand: that their loved one may still die, even though he seems fine."
In this liminal space between the worst of sickness and the beginning of what may be recovery or relapse, patients listen as medical students present their cases—explain what is keeping them in a hospital bed—to a group of residents, interns, attending physicians, and nurses during rounds. Medical students must "learn two languages, one for the patients and one for medicine." The language for patients isn't just medical jargon translated into what a layperson may understand, but a language with carefully regulated "nuance, tone, meter, facial expression," one that may include more or less information in order to manage the anxiety of patients and their family members. Writing of the case of woman whose husband always "assumes the worst," Maloney locates the conundrum that comes when translating from one language to another: "The information is incomplete, or they wait to tell the husband until they are sure they are going to do this procedure or that...Is making [patients] the last to know helping or hurting them? Where is the line?"
We will all someday land on the wrong side of the hospital bed, be at the mercy of caregivers who must determine how to treat us, how to talk to us, how to charge us. In the era of COVID — which Maloney touches on only briefly in the last essay — the precarity of health is all the more real. At its best, Cost of Living offers insight into the subculture of medicine and incites the reader to think more deeply about what our health care system is costing us all.
Kristen Martin's writing has also appeared in The New York Times Magazine, The Believer, The Baffler, and elsewhere. She tweets at @kwistent .
- Search Search Please fill out this field.
- US & World Economies
- GDP Growth & Recessions
The Rising Cost of Health Care by Year and Its Causes
See for yourself whether Obamacare increased health care costs
:max_bytes(150000):strip_icc():format(webp)/image0-MichaelBoyle-30f78c37d3174fe298f9407f0b5413e2.jpeg)
What Caused This Increase?
Government policy, preventable chronic diseases.
- Health Care Costs and the ACA
Inflation Reduction Act
Healthcare costs by year, frequently asked questions (faqs).
Sam Edwards / Getty Images
In 2020, U.S. health care costs totaled $4.1 trillion. That makes health care one of the country's largest expenses. Health spending accounted for 19.7% of the nation's gross domestic product (GDP).
In comparison, national health expenditures totaled $27.2 billion in 1960, just 5% of GDP. That translates to an annual health care cost of $12,530 per person in 2020 versus roughly $150 per person in 1960.
Keep reading to learn more about health expenditures and how the Affordable Care Act (ACA) aimed to control costs.
Key Takeaways
- Health care costs began rapidly rising in the 1960s as more Americans became insured and the demand for health care services surged.
- Health care costs have also increased due to preventable diseases, including complications related to nutrition or weight issues.
- Recent government attempts to stem the growth in health care costs include the Affordable Care Act and Inflation Reduction Act.
There were two causes of this massive increase: government policy and lifestyle changes.
Demand for Health Care Services
The government created programs like Medicare and Medicaid to help those without the private insurance most Americans rely upon. These programs spurred demand for health care services. That gave providers the ability to raise prices.
A study in Health Affairs co-authored by Princeton University health economist Uwe Reinhardt found that Americans use the same amount of healthcare as residents of other nations. They just pay more for them.
For example, U.S. hospital prices are 60% higher than those in other countries. Government efforts to reform healthcare and cut costs raised them instead.
Chronic Illnesses
Chronic illnesses, such as diabetes and heart disease, have increased. In 2020, the health care costs of people with at least one chronic condition were responsible for 86% of health care spending. More than half of all Americana adults have at least one of them.
These illnesses are expensive and difficult to treat. As a result, the sickest 5% of the population consumed 50% of total health care costs in 2019. The healthiest 50% only consumed 3% of the nation's health care costs.
The U.S. medical profession does a heroic job of saving lives, but it comes at a cost. Medicare spending for patients in the last year of life accounts for about 25% of the Medicare budget.
Between 1961 and 1965, health care spending increased by an average of 8.9% a year. That's because health insurance expanded. As it covered more people, the demand for health care services rose. By 1965, households paid out-of-pocket for 44% of all medical expenses. Health insurance paid for 24%.
From 1966 to 1973, health care spending rose by an average of 11.9% a year. Medicare and Medicaid covered more people and allowed them to use more health care services. Medicaid allowed senior citizens to move into expensive nursing home facilities.
As demand increased, so did prices. Health care providers put more money into research. It created more innovative, but expensive, technologies.
Medicare helped create an overreliance on hospital care. By 2012, there were 131 million emergency room visits. An astonishing one out of five adults used the emergency room that year.
In 1971, President Nixon implemented wage-price controls to stop mild inflation. Controls on health care prices created higher demand. In 1973, Nixon authorized Health Maintenance Organizations (HMO) to cut costs.
These prepaid plans restricted users to a particular medical group. The HMO ACT of 1973 provided millions of dollars in start-up funding for HMOs. It also required employers to offer them when available.
From 1974 to 1982, health care prices rose by an average of 14.1% a year for three reasons. First, prices rebounded after the wage-price controls expired in 1974. Second, Congress exempted some corporations from regulation with the Employee Retirement Income Security Act of 1974, and companies offered lower-cost, flexible plans. Third, home health care took off, growing by 32.5% a year.
Between 1983 and 1992, health care costs rose by an average of 9.9% each year. Home health care prices increased by 18.3% per year.
In 1986, Congress passed the Emergency Medical Treatment and Labor Act. It forced hospitals to accept anyone who showed up at the emergency room. Prescription drug costs rose by 12.1% a year. One reason is that the FDA allowed prescription drug companies to advertise on television.
Between 1993 and 2013, healthcare spending grew by an average of 6% a year.
In the early 1990s, health insurance companies tried to control costs by spreading the use of HMOs once again. Congress then tried to control costs with the Balanced Budget Act in 1997. Instead, it forced many healthcare providers out of business.
Because of this, Congress relented on payment restrictions in the Balanced Budget Refinement Act in 1999 and the Benefits Improvement and Protection Act of 2000. The act also extended coverage to more children through the Children's Health Insurance Program.
After 1998, people rebelled and demanded more choice in providers. As demand increased again, so did prices. Between 1997 and 2007, drug prices tripled, according to a study in Health Affairs.
One reason is that pharmaceutical companies invented new types of prescription drugs. They advertised straight to consumers and created additional demand. The number of drugs with sales that topped $1 billion increased to 52 in 2006 from six in 1997.
The U.S. government approved expensive drugs even if they were not much better than existing remedies. Other developed countries were more cost-conscious.
In 2003, the Medicare Modernization Act added Medicare Part D to cover prescription drug coverage. It also changed the name of Medicare Part C to the Medicare Advantage program, and the number of people using those plans increased to 28 million by 2022. Those costs rose faster than the cost of Medicare itself.
The nation’s reliance on the health insurance model increased administration costs. Various studies have found that administration makes up about 15% to 25% of U.S. healthcare costs. That's twice the administrative costs in Canada.
About half of those administrative costs in the U.S. are due to the complexity of billing. About half of those administrative costs in the U.S. are due to the complexity of billing. For example, in a 2018 JAMA study, U.S. physicians used 14.5% of their primary care revenue on administrative billing costs.
A big reason is that there are so many types of payers. In addition to Medicare and Medicaid, there are thousands of different private insurers. Each has its own requirements, forms, and procedures.
Hospitals and doctors must also chase down people who don't pay their portion of the bill. That doesn't happen in countries with universal healthcare .
The reliance on corporate private insurance created healthcare inequality . Those without insurance often couldn't afford visits to a primary care physician. By 2009, half of the people (46.3%) who visited an emergency room said they went because they had no other place to go for healthcare.
The Emergency Medical Treatment and Labor Act required hospitals to treat anyone who showed up in the emergency room. Uncompensated care costs hospitals more than $38 billion per year, some of which are passed on to the government.
The second cause of rising healthcare costs is an epidemic of preventable diseases. The four leading causes of non-accidental death are heart disease, cancer, COVID-19, and chronic obstructive pulmonary disorder, as of October 2022. Chronic health conditions cause most of them.
These issues can either be prevented or would cost less to treat if caught in time. Risk factors for heart disease and strokes are poor nutrition and obesity. Smoking is a risk factor for lung cancer (the most common type) and COPD. Obesity is also a risk factor for other common forms of cancer.
These diseases can cost more than $5,000 per person. The average cost of treating diabetes, for example, is $16,750 per person annually as of 2021.
These diseases are difficult to manage because patients get tired of taking the medications. Those who cut back find themselves in the emergency room with heart attacks, strokes, and other complications.
How the ACA Slowed the Rise of Healthcare Costs
By 2009, rising healthcare costs were consuming the federal budget. Medicare and Medicaid cost $671 billion in 2008. Payroll taxes cover less than half of Medicare and none of Medicaid.
This is part of so-called mandatory spending also generally includes federal and veterans' pensions , welfare, and interest on the debt . It consumed 60% of the federal budget. Congress knew something had to be done to rein in these costs.
Federal healthcare costs are part of the mandatory budget . That means they must be paid. As a result, they are eating up funding that could have gone to discretionary budget items, such as defense, education, or rebuilding infrastructure.
Obamacare's goal is to reduce these costs. First, it required insurance companies to provide preventive care for free so patients could treat chronic conditions before requiring expensive hospital emergency room treatments. It also reduced payments to Medicare Advantage insurers.
From 2010, when the Affordable Care Act was signed, through 2019, healthcare costs rose by 4.2% a year. It achieved its goal of lowering the growth rate of healthcare spending.
In 2010, the government predicted that Medicare costs would rise by 20% in just five years. That’s from $12,376 per beneficiary in 2014 to $14,913 by 2019. Instead, analysts were shocked to find out spending had dropped by over $1,200 per person, to $11,167 by 2014.
This price decrease happened due to four specific reasons:
- The ACA reduced payments to Medicare Advantage providers. The providers' costs for administering Parts A and B were rising much faster than the government’s costs. The providers couldn't justify the higher prices and appeared as though they were overcharging the government.
- Medicare began rolling out accountable care organizations, bundled payments, and value-based payments. Hospital readmissions dropped by 150,000 in both 2012 and 2013; hospitals increased efficiency and quality of care to avoid penalties for those who underperform.
- High-income earners paid more in Medicare payroll taxes and Part B and D premiums.
- In 2013, sequestration lowered Medicare payments by 2% to providers and plans.
Based on these new trends, Medicare spending was projected to grow by 7.9% a year between 2018 and 2028.
In 2022, the Inflation Reduction Act took effect. The wide-ranging bill included several components designed to soften the rise of health care costs for average consumers. While the details vary by state, the nationwide effects include capping prescription drug costs at $2,000, allowing Medicare to negotiate costs with drug companies, and limiting drug price hikes to the broader inflation rate.
Sources: Centers for Medicare and Medicaid Services, Federal Reserve Bank of Minneapolis.
Which tax supports healthcare costs for retirees?
The Medicare tax withheld from employee paychecks supports the cost of Medicare coverage for retirees. Employees and employers split the tax, and they each pay 1.45%. Self-employed individuals pay the full 2.9% Medicare tax themselves.
How do fraud and abuse impact the cost of healthcare?
Federal authorities have estimated that fraud accounts for between 3% and 10% of total healthcare spending. In 2017, for example, an audit found roughly $95 billion in improper Medicare and Medicaid spending. That's about 8% of the $1.1 trillion the government spent on health coverage programs.
FRED, Federal Reserve Bank of St. Louis. " Gross Domestic Product ."
Centers for Medicare & Medicaid Services. " Historical ," Download "National Health Expenditures by Type of Service and Source of Funds, CY 1960-2020."
United States Census Bureau. " Historical Population Change Data (1910-2020) ."
Health Affairs. " It’s the Prices, Stupid: Why the United States Is So Different From Other Countries ."
OCED iLibrary. " Comparing Price Levels of Hospital Services Across Countries ."
Halsted R. Holman. " The Relation of the Chronic Disease Epidemic to the Health Care Crisis ." ACR Open Rheumatology .
Centers for Disease Control and Prevention. " Chronic Diseases in America ."
Peterson-KFF Health System Tracker. " How Do Health Expenditures Vary Across the Population? "
Ian Duncan et al. " Medicare Cost at End of Life ." The American Journal of Hospice & Palliative Care .
Centers for Medicare and Medicaid Services. " History of Health Spending in the United States, 1960-2013 ," Pages 7-9.
Centers for Disease Control and Prevention. " Emergency Department Use in the Country’s Five Most Populous States and the Total United States, 2012 ."
Centers for Medicare and Medicaid Services. " History of Health Spending in the United States, 1960-2013 ," Pages 10, 15.
GovInfo. " Health Maintenance Organization Act of 1973 ."
U.S. Department of Labor. " ERISA ."
Centers for Medicare and Medicaid Services. " History of Health Spending in the United States, 1960-2013 ," Page 12.
Centers for Medicare and Medicaid Services. " History of Health Spending in the United States, 1960-2013 ," Pages 14, 17.
Centers for Medicare and Medicaid Services. " Emergency Medical Treatment & Labor Act (EMTALA) ."
Centers for Medicare and Medicaid Services. " History of Health Spending in the United States, 1960-2013 ," Pages 17, 33.
Julie Donohue. " A History of Drug Advertising: The Evolving Roles of Consumers and Consumer Protection ." The Milbank Quarterly .
Centers for Medicare and Medicaid Services. " History of Health Spending in the United States, 1960-2013 ," Page 7.
Centers for Medicare and Medicaid Services. " History of Health Spending in the United States, 1960-2013 ," Pages 18-22.
Health Affairs. " Prescription Drug Spending Trends in the United States: Looking Beyond the Turning Point ."
Kaiser Family Foundation. " Medicare Advantage in 2022: Enrollment Update and Key Trends ."
National Center for Biotechnology Information. " Medicare Modernization: The New Prescription Drug Benefit and Redesigned Part B and Part C ."
JAMA Network. " Administrative Expenses in the US Health Care System: Why So High? "
Annals of Internal Medicine. " Health Care Administrative Costs in the United States and Canada, 2017 ."
The New England Journal of Medicine. " Costs of Health Care Administration in the United States and Canada ."
JAMA Network. " Administrative Costs Associated With Physician Billing and Insurance-Related Activities at an Academic Health Care System ."
Centers for Disease Control and Prevention. " Emergency Room Use Among Adults Aged 18–64: Early Release of Estimates From the National Health Interview Survey, January–June 2011 ."
Centers for Medicare & Medicaid Services. " Certification and Compliance for the Emergency Medical Treatment and Labor Act (EMTALA) ," Page 1.
American Hospital Association. " Uncompensated Care Cost Fact Sheet ," Page 3.
Centers for Disease Control and Prevention. " Leading Causes of Death ."
Centers for Disease Control and Prevention. " Heart Disease and Stroke ."
Centers for Disease Control and Prevention. " What Are the Risk Factors for Lung Cancer? "
American Lung Association. " COPD Causes and Risk Factors ."
Centers for Disease Control and Prevention. " Obesity and Cancer ."
Centers for Disease Control and Prevention. " How Type 2 Diabetes Affects Your Workforce ."
National Academies Press. " 5 Options for Medicare and Medicaid ."
Congressional Research Service. " Mandatory Spending Since 1962 ," Page 7.
Peterson-KFF Health System Tracker. " How Has U.S. Spending on Healthcare Changed Over Time? "
Kaiser Family Foundation. " The Mystery of the Missing $1,200 Per Person: Can Medicare’s Spending Slowdown Continue? "
Health Affairs. " Recent Growth in Medicare Advantage Enrollment Associated With Decreased Fee-for-Service Spending in Certain US Counties ."
National Center for Biotechnology Information. " Hospital Readmissions Reduction Program ."
Kaiser Family Foundation. " What Are the Implications of Repealing the Affordable Care Act for Medicare Spending and Beneficiaries? "
Centers for Medicare & Medicaid Services. " Additional Information Regarding the Mandatory Payment Reductions in the Medicare Advantage, Part D, and Other Programs ," Page 1.
Kaiser Family Foundation. " The Facts on Medicare Spending and Financing ."
Congress.gov. " H.R.5376 - Inflation Reduction Act of 2022 ."
Centers for Medicare and Medicaid Services. " Historical ," Download "NHE Summary, Including Share of GDP, CY 1960-2018."
Federal Reserve Bank of Minneapolis. " Consumer Price Index, 1913- ."
Internal Revenue Service. " Topic No. 751 Social Security and Medicare Withholding Rates ."
Health Affairs. " Combating Fraud in Health Care: An Essential Component of Any Cost Containment Strategy ."
Government Accountability Office. " Medicare and Medicaid: CMS Needs To Fully Align Its Antifraud Efforts With the Fraud Risk Framework. "

- University News
- Faculty & Research
- Health & Medicine
- Science & Technology
- Social Sciences
- Humanities & Arts
- Students & Alumni
- Arts & Culture
- Sports & Athletics
- The Professions
- International
- New England Guide
The Magazine
- Current Issue
- Past Issues
Class Notes & Obituaries
- Browse Class Notes
- Browse Obituaries
Collections
- Commencement
- The Context
- Harvard Squared
- Harvard in the Headlines
Support Harvard Magazine
- Why We Need Your Support
- How We Are Funded
- Ways to Support the Magazine
- Special Gifts
- Behind the Scenes
Classifieds
- Vacation Rentals & Travel
- Real Estate
- Products & Services
- Harvard Authors’ Bookshelf
- Education & Enrichment Resource
- Ad Prices & Information
- Place An Ad
Follow Harvard Magazine:
Features | Forum
The World’s Costliest Health Care
…and what America might do about it
May-June 2020

Americans use a lot of technologically sophisticated, expensive medical services—slighting more effective, routine care. Photograph by Rui Vieira/PA Wire/AP Images
L ONG BEFORE the presidential primaries, or a paralyzing pandemic, Harvard Magazine asked several faculty experts to write about issues that would be shaped by the national elections, that mattered to the future of the country—and that would probably be addressed inadequately during the extended campaign.
One issue was the federal budget and its chronic, enormous deficits. When we approached Karen Dynan and Douglas Elmendorf to explain all that red ink (and what, if anything, to do about it) , the state of play was an unlikely mix: a record U.S. economic expansion and very low unemployment, paradoxically accompanied by trillion-dollar annual deficits and historically low interest rates. Those figures now seem quaint. The coronavirus has caused a precipitous recession, or worse, and attempts to offset potentially cataclysmic job losses are yielding a multi-trillion-dollar budget gap that will need to be paid for some day; at the same time, government interest rates have fallen even further. In this context, Dynan and Elmendorf’s analysis is especially timely and relevant.
Spending on health care is central to the long-term budgetary challenges. So it is especially useful to pair their essay with David Cutler’s nuanced explanations of why American health care costs so much: about $3.5 trillion per year (that’s the norm , before an emergency like COVID-19)—of which one-third is wasted. The sources of that waste, in terms of health value received for dollars spent, may surprise you. It has certainly proven resistant to political repair. Given the relatively poor results Americans receive for all they spend, fixing health care matters: for citizens’ well-being, the country’s fiscal soundness, and extending essential medical services to those who lack access now.
Harvard Magazine presents these thoughtful commentaries as a service to readers—and as a contribution to better public debate. You can learn more from all three authors on their segments of the Ask a Harvard Professor podcast .
~ The Editors
* * *
A lec Smith died of diabetic ketoacidosis, though it is probably fairer to say that he died from high healthcare costs. The 26-year-old from Rochester, Minnesota, had just moved out of his parents’ home and didn’t have enough money to afford his insulin. He decided to ration his remaining supply until his next paycheck, a week later. Alas, he was not able to make it. Alec died alone in his apartment, vomiting and having difficulty breathing, from a condition that never should have occurred.
Alec’s story is extreme in its outcome, but not in its outlines. Nearly half of Americans say they have delayed or skipped medical care because of the cost. People who face higher costs for medical care are diagnosed with cancer at later stages of the disease and take fewer medications . Even the very sick use less care when their out-of-pocket costs rise. Health suffers .

A Medicare enrollee awaits a prescription in Chicago. The U.S. health system entails extraordinary administrative expenses. Photograph by Tim Boyle/Getty Images
The United States has many problems in medical care, from the large share of the population still uninsured (about 10 percent of us) to one of the lowest life expectancies in the developed world. Underlying all these problems is the high cost of medical care. We do not guarantee adequate access to medical care because we cannot figure out how to pay for it.
The harm from high medical spending goes well beyond the medical sector. Many firms have outsourced low-wage workers because providing them health benefits is too expensive. Government spending for schools and environmental programs are starved because resources go to health care instead. Warren Buffett called medical costs the “tapeworm of American economic competitiveness.” Oncologists have invented a term, “financial toxicity,” to consider along with biochemical toxicity in deciding on the appropriate treatment.
Americans agree with Buffett. Two-thirds of Americans want the federal government to regulate the price of medical care. Indeed, the public has a clear theory for explaining high medical spending: unconstrained greed. Pharmaceutical companies put profits above patients, and insurance executives are paid millions to deny coverage. The government should stop both.
And people are right, to a point. Allowing the makers of life-saving medications to price their products without constraint is a recipe for premature death. But the issue is more complex than just greed. Even if the United States cut every pharmaceutical price in half and eliminated all profits on health insurance, the gap between U.S. medical spending and that of other rich countries would fall by less than a quarter. Health care is more than just rapacious profits in drugs and insurance.
The reality is that the healthcare problem is multifaceted. But that is not the same as saying nothing can be done. On the contrary, it means there is even more to do. Three areas are essential to tackle if we want to reduce health spending to near the level in other countries.
Administration Adds Up
The largest component of higher U.S. medical spending is the cost of healthcare administration . About one-third of healthcare dollars spent in the United States pays for administration; Canada spends a fraction as much. Whole occupations exist in U.S. medical care that are found nowhere else in the world, from medical-record coding to claim-submission specialists.
Healthcare administration needn’t be so costly. Even in other countries with multiple payers and private providers—including Germany and Switzerland—healthcare administration is less than half the cost of the U.S. equivalent. The key requirement for reducing administrative costs is standardization. Grocery-store checkout is simple because all products have bar codes and credit-card machines are uniform. Mobile banking is easy because the Federal Reserve has put standards in place for how banks interface with each other. But every health insurer requires a different bar-code-equivalent and payment-systems submission. And even in 2020, it is virtually impossible to send medical records electronically from one hospital to another. Almost all hospitals have electronic medical records, but there is no federal requirement that they interface. Indeed, many providers take active steps to avoid electronic interchange, because keeping records local ensures that fewer patients will switch doctors.
Standardization occurs when big participants decide they want it. In healthcare, the big participant is the government. Only the federal government has the buying power and administrative reach to force payers and providers to adopt billing and interface rules. The federal government could commit to a date by which all interactions are standardized and set up the infrastructure to make that happen. To date, however, the public sector has shirked its responsibility. The federal government sees its role as providing insurance to people—Medicare and Medicaid in particular—but not looking out for the system as a whole. That thinking will need to change if progress is to be made.
Greed and Gouging
Greed is the second part of excessive health spending. The U.S. list price for insulin is 10 times higher than that in Canada. Relief for Alec could have come after a short bus ride north. But pharmaceuticals are not the whole story. Prestigious hospitals charge multiple times what less prestigious hospitals do for the same service. While that may be justified in the case of complex surgery, it surely is not for an x-ray.
It is no mystery why pharmaceutical prices are higher in the United States than in Canada and at star hospitals as compared to community institutions. Prices rise when there is nowhere else to go. Traveling to Canada for insulin is not something most Americans can do—though Alec Smith’s mother now leads such trips, or did when she was able to do so. And few people are willing to switch from a star hospital to a community institution, even if the price is much lower.
Economists’ favorite solution to such “sticky” demand is to help people become more mobile. Play different insulin suppliers off against each other to bargain for a lower price. Have interactive websites to help people shop for lower-priced imaging. Alas, all attempts to make these policies work have so far been unsuccessful. Many employers have created websites where their employees can search for more and less expensive services. Uniformly, they find that raising costs to patients via co-pays and deductibles, for example,reduces utilization but engenders relatively little price shopping. It is not that people think the star hospital is necessarily better. Rather, their physician directs them there, and they are afraid to ask about cheaper alternatives. Pharmaceuticals are a partial exception. People will often choose generic drugs, if available, over a brand name—but they do not do so in sufficient amounts to materially lower the cost of drugs. And federal laws make it illegal for bulk reimportation of drugs from Canada. The result is that star hospitals are overflowing with patients, and insulin prices keep rising.
If prices cannot be tamed by demand, a growing number of economists call for price regulation. Fiat can accomplish what reasoning cannot.
Price regulation is not hard to implement: “Thou shalt not price higher than X” is not a particularly difficult rule to enforce. The state of Maryland does this for hospitals, and most European countries do this for pharmaceuticals.
The major challenge to implementing such a policy is the possible unintended consequences. If pharmaceutical manufacturers or academic hospitals got less money, what would they cut out? Would executive compensation fall (likely a good thing)—or would money for research and development dry up? We are not certain of the answer to this, and so regulation comes with a side dose of concern. That said, every example of a family afraid to visit the emergency department because of the cost, and thus waiting to see if a sick child gets worse , pushes the case for price regulation forward.
In Love with Medical Services
The final part of higher medical spending in the United States is higher utilization . The United States has the most technologically sophisticated medical system of any country, and it shows up in spending: the U.S. has four times the number of MRIs per capita as Canada, and three times the number of cardiac surgeons. Americans don’t see the doctor any more often than Canadians do, and are not hospitalized any more frequently, but when they do interact with the medical system, it is much more intensively.
Outcomes for this greater intensity are not easy to find. Despite the more intensive U.S. cardiovascular care, heart-attack survival is no better. Indeed, U.S. death rates for heart disease have been rising relative to other rich countries. The greater degree of imaging in this country detects more cancers, but many of these would never have become clinically apparent. Many cancers grow slowly, and often the patient dies of something else long before the cancer would have become noticeable.
And even as the United States overdoes high-tech care, it underprovides routine care. Effective medications to treat high blood pressure and high cholesterol have been around for decades, yet only half of people with these risk factors are successfully treated. Mental illness is underdiagnosed and undertreated despite its enormous social cost.
The reason for the disparity between high-tech and routine care is not hard to ferret out. Cardiac surgery and MRIs—famously lucrative—are overprovided, but no one is paid to make sure hypertensive patients take their medications.

An uninsured father and son at a health clinic in Denver. Lack of coverage persists for a significant share of the population. Photograph by John Moore/Getty Images
Addressing the misallocation of medical resources is the most difficult technical challenge in lowering medical spending. How does one get a health system to perform fewer MRIs but do them on the right patients, and use the money saved to extend more primary care? The Canadian policy for overprovision is simple: limit the total amount of high-tech care available. Canadian governments ration the number of scanners that can be bought and how many hospitals can have open-heart surgery facilities. Within the available supply, physicians decide how the services are allocated. In a highly professional system like Canada’s, doctors perform the allocation rules very well. Thus, outcomes are better in Canada than in the United States, at a fraction of the cost.
The U.S. government once tried this type of technology rationing—it went by the name of Certificate of Need regulation. In the 1970s and 1980s, state governments had systems to approve each new scanner or addition to a hospital’s footprint and were supposed to say no when it was not necessary. But the policy was not very effective . Without a firm limit on what was allowed to be spent on medical care, it was too difficult for technology boards to deny hospitals. That set of policies has been left in the dustbin of failed cost-containment efforts.
Over time, insurers evolved other ways to try to restrict care. Some insurers have gone with a high cost-sharing strategy: make people pay more when they use care. Those willing to pay a higher cost can have the service. This is the strategy that leads to high out-of-pocket costs for insulin and emergency-department use. The second strategy is to keep an eagle eye on what physicians want to do, to make sure that all care is medically necessary. While good in theory, the administrative costs of this policy have proven to be a disaster.
The most recent economic idea is shared savings: don’t pay physicians a fee for each service, with higher rates for surgery and imaging than for medical management. Instead, set a target amount of spending for the average patient. If spending comes in below the target and quality is sufficiently high, the provider group gets to share in the savings. Thus, physicians have incentives to limit their own use of imaging to necessary cases and to figure out ways to extend primary-care practice. This policy was first tested in Massachusetts and has since gone national .
To date, there is no evidence that shared-savings programs will lead this country to the much lower Canadian or European levels of medical spending and better health outcomes.
The evidence so far is that shared savings programs have been modestly successful . Cost growth falls in shared-savings programs and quality seems to improve. But the savings are not as big as hoped for. To date, there is no evidence that shared-savings programs will lead this country to the much lower Canadian or European levels of medical spending and better health outcomes.
This discouraging record leads to deep questioning about how to make progress in medical care. Can the current system be a basis for good medical and economic outcomes, or must one make more radical change? Proponents of the latter view fall into two camps. On the left are those who reason that the only successful healthcare models internationally are single-payer systems, so the United States must move in that direction to do materially better. On the right are those who argue that only markets can provide the combination of price and quality that people want, so the country needs to remove government from the equation as much as possible. Not surprisingly, many Democrats espouse the former, and Republicans sign on to the latter.
In Rochester, Minnesota, and elsewhere in the country, people want none of this bigger debate. Phrases like “choice” and “single payer” are not helpful, let alone “incentives for interoperability of healthcare records.” Recall that Americans have a firm view of the problem: greed. Every conversation about something other than greed seems entirely beside the point.
This creates a special problem for the healthcare policymaker. In addition to figuring out what is technically correct, we need to learn how to explain those reforms to worried people. Can we promise that any policy will prevent deaths like Alec Smith’s and not harm people in other ways? Speaking morally, as well as economically, is the biggest challenge in health policy.
David Cutler is Eckstein professor of applied economics in the Faculty of Arts and Sciences, professor in the department of global health and population at the School of Public Health, and a faculty member at the Harvard Kennedy School.
You might also like

“It’s Tournament Time”
Harvard women’s basketball prepares for Ivy Madness.

A Harvard Agenda Shaped by Speech
The work underway in the Faculty of Arts and Sciences

Dialogue, not Debate
American University’s Lara Schwartz, J.D. ’98, teaches productive disagreement.
Most popular
AWOL from Academics
Behind students' increasing pull toward extracurriculars

Why Americans Love to Hate Harvard
The president emeritus on elite universities’ academic accomplishments—and a rising tide of antagonism
More to explore

Winthrop Bell
Brief life of a philosopher and spy: 1884-1965

John Harvard's Journal
Talking about Talking
Fostering healthy disagreement

A Dogged Observer
Novelist and psychiatrist Daniel Mason takes the long view.
The Issue of Rising Medical Costs Essay
Healthcare policy initiative.
The healthcare industry is experiencing various issues and challenges that might affect the professionals’ performance, on stakeholders’ perception, and the quality of patient care. One of the problems that have a substantial impact on different aspects of healthcare is the issue of increased medical costs. The purpose of this paper is to investigate this challenge and its implications and propose a policy that will work towards overcoming the problem and improving the situation.
Rapid growth in medical costs can have various insinuations for the US population. Among them, it is possible to mention the fact that it will become more difficult for individuals to afford proper medical treatment and required drug purchases. The Centers for Medicare and Medical Services estimated that throughout the next ten years, healthcare costs would rise by more than 5% annually (“Healthcare costs for Americans,” 2019).
In such a way, the individuals might experience significant difficulties in affording such healthcare industry components, as hospital care or spending for prescribed drugs. Two factors are the most dominant in causing such a rapid increase. The prices for healthcare prices within the industry are rising, and the population of the nation is growing older, having a higher percentage of people aged over 65 (“Healthcare costs for Americans,” 2019). Consequently, those factors drive medical costs upward, which affects the way American families receive healthcare services.
Besides influencing the lives of patients, increased medical expenditures also have an impact on the work of healthcare professionals. The professionals can have challenges in offering the best solution in a situation when the patients who require extended treatment or expensive drug prescription. In attempts to provide the best healthcare service, the professionals might create further financial issues for the individuals.
Moreover, nurses and doctors can have moral worries when they can see that patients cannot afford the best cure for them. Therefore, employees within the healthcare industry can have psychological issues that might interfere with their performance in specific cases and cause higher turnover rates in the long-term.
One of the policies to advocate that will have a favorable impact on the overall situation in the future is the work on disease prevention. According to Cutler (2017), this policy “is both healthier for the individual and less expensive for the system” (p. 508). Thus, with a higher chance of avoiding specific diseases, the individuals would not need such extensive medical care, and the system will have lower expenditures for the treatment.
For example, new drugs for hypertension and high cholesterol have substantially reduced the likelihood of cardiovascular diseases, which implicates lower spending on treatment and medication (Cutler, 2017). Consequently, finding medicines to reduce the number of other chronic illnesses can decrease specific medical costs.
Still, disease prevention is a long-term policy, the effects of which might not be evident right away. While actively integrating disease prevention strategies, the industry can use such approaches as cutting prices for the drugs and offering bundling payment options for the individuals (Cutler, 2017). Those techniques can lower the financial burden for the patients and make them more willing to come and seek medical treatment without fear of not being able to pay for it.
It is crucial to employ an effective campaign to address the current issue and propose the policy and approaches aiming to improve the situation. Advocating the problem and suggested solutions through social media and reaching pharmaceutical companies, as well as integrating bundled payment options within specific healthcare facilities, can be the first step.
The Twitter post to highlight the problem can be: With CMS estimating a rapid growth in medical costs, it is critical to cut the pharmaceutical prices and integrate bundled payments. In conclusion, the issue of growing expenditures in the healthcare industry presents severe challenges for all the parties involved, and there is a need for action to change the situation.
Cutler, D. M. (2017). Rising medical costs mean more rough times ahead. Jama , 318 (6), 508-509.
Healthcare costs for Americans projected to grow at an alarmingly high rate . (2019). Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, May 20). The Issue of Rising Medical Costs. https://ivypanda.com/essays/the-issue-of-rising-medical-costs/
"The Issue of Rising Medical Costs." IvyPanda , 20 May 2022, ivypanda.com/essays/the-issue-of-rising-medical-costs/.
IvyPanda . (2022) 'The Issue of Rising Medical Costs'. 20 May.
IvyPanda . 2022. "The Issue of Rising Medical Costs." May 20, 2022. https://ivypanda.com/essays/the-issue-of-rising-medical-costs/.
1. IvyPanda . "The Issue of Rising Medical Costs." May 20, 2022. https://ivypanda.com/essays/the-issue-of-rising-medical-costs/.
Bibliography
IvyPanda . "The Issue of Rising Medical Costs." May 20, 2022. https://ivypanda.com/essays/the-issue-of-rising-medical-costs/.
- U.S. Healthcare System and Organizational Structures
- American Healthcare Services Payment Differences
- Evidence-Based Practice in Nursing Intervention
- Hotel Services and Pricing Strategies
- Promoting Equity With Healthcare Reforms
- Physician-Hospital Arrangements and Development in the Healthcare Industry
- Relationship Between Doctors and Pharmaceutical Industries
- Facilitation of Sun Pharmaceutical Industries Ltd
- Pharmaceutical Industry and Drugs
- Practices in the Pharmaceutical Industry
- Need Assessment and GAP Analysis Mayo Clinic
- Process of Funding Acute Inpatient Services
- Zero Based Budgeting (ZBB) Overview
- Financing Health Care in US Cost vs. Quality
- IRS Regulations and Healthcare
- Search Search Please fill out this field.
- Overall Healthcare Costs
Why Are Healthcare Costs Rising?
The aging population, increase in chronic illnesses, increased ambulatory costs, rising insurance premiums.
- RRising Government Costs
Higher Out-of-Pocket Costs
The fear factor, cost of covid-19, patching u.s. healthcare, the bottom line.
- Health Insurance
Why Do Healthcare Costs Keep Rising?
:max_bytes(150000):strip_icc():format(webp)/jp_profileinv__jim_probasco-5bfc262746e0fb005118b333.jpg)
Ariel Courage is an experienced editor, researcher, and former fact-checker. She has performed editing and fact-checking work for several leading finance publications, including The Motley Fool and Passport to Wall Street.
:max_bytes(150000):strip_icc():format(webp)/ArielCourage-50e270c152b046738d83fb7355117d67.jpg)
Americans now spend close to $13,000 on average on healthcare each year. High insurance premiums, high deductibles, and other out-of-pocket expenses are just some of the costs associated with health and wellness in the country, and those costs are only going higher.
One reason for rising healthcare costs is government policy. Since the inception of Medicare for retired Americans and Medicaid for low-income people, providers have been able to increase prices with the knowledge that the government, not the individual, will be paying the bills.
Still, there’s much more to rising healthcare costs lately, including the impact of the COVID-19 pandemic on the cost structure.
Key Takeaways
- Healthcare costs in the United States have been rising for decades and are expected to keep increasing.
- Nearly 18% of U.S. GDP went to healthcare in 2021, almost twice other developed nations despite comparatively poor results for patients.
- In the long term, the financial impact of COVID-19-related healthcare spending is not expected to significantly affect healthcare spending in general.
- The No Surprises Act and other recent legislation offer some help when it comes to unexpected healthcare billing.
Overall Costs of Healthcare
Healthcare costs have risen dramatically in the United States over the past several decades. According to the Commonwealth Fund, healthcare spending as a percentage of GDP rose from 8.2% in 1980 to 17.8% in 2021.
Americans are not getting better outcomes for their money compared to their peers. Americans had the highest death rate due to COVID-19 among its peer nations. They have a lower life expectancy, a higher rate of avoidable deaths, and the highest rates of infant and maternal deaths.
But the costs in dollars are only going up. In 2023, healthcare spending is expected to rise by 5.1%, from $4.2 trillion in 2022, according to the Centers for Medicare and Medicaid Services.
Where does that money go? According to the U.S. Centers for Medicare and Medicaid Services (CMS), healthcare spending can be broken down into 10 categories:
- Hospital care (31%)
- Physician services (20%)
- Prescription drugs (10%)
- Other personal healthcare costs (5%)
- Nursing care facilities (5%)
- Dental services (4%)
- Home healthcare (3%)
- Other professional services (3%)
- Other non-durable medical products (2%)
- Durable medical equipment (2%)
A 2023 study by the Peter G. Peterson Foundation blamed rising prices on three big factors: population growth, population aging, and rising prices for healthcare products and services.
An earlier study by the Journal of the American Medical Association (JAMA) adds additional factors, citing an increase in chronic illnesses and the rising costs of health insurance, among others.
Protection Against Rising Costs
The No Surprises Act and other legislation contained in the Consolidated Appropriations Act (CAA), 2021, are designed to protect consumers from a lack of transparency in healthcare billing. This legislation took effect on Jan. 1, 2022.
Healthcare gets more expensive as the population expands, particularly when the growth is attributable to longer lifespans.
Older people spend more on healthcare than younger people, and they tend to require more expensive procedures, such as knee replacements and heart bypass surgery.
Americans aged 65 and over represented 16% of the population in 2021, and that number is expected to reach 20% by 2030.
Therefore, it’s not surprising that 50% of the increase in healthcare spending comes from increased costs for services, especially inpatient hospital care.
The authors of the JAMA study point to diabetes as the medical condition responsible for the greatest increase in spending over the study period, which was 1996 through 2013.
The increased cost of diabetes medications alone was responsible for $44.4 billion of the $64.4 billion increase in costs to treat that disease.
After diabetes, conditions with the greatest increase in costs were:
- Lower back and neck pain: $57.2 billion
- High blood pressure: $46.6 billion
- High cholesterol: $41.9 billion
- Depression: $30.8 billion
- Urinary disease: $30.2 billion
- Osteoarthritis: $29.9 billion
- Bloodstream infection: $26 billion
- Falls: $26 billion
- Oral disease: $25.3 billion
Ambulatory care, including outpatient hospital services and emergency room care, increased the most of all treatment categories studied.
To some extent, that is a transferral of services from inpatient hospital care to outpatient care.
The trend speeded up during the COVID-19 pandemic when healthcare providers moved to virtual services to avoid crowded waiting rooms.
The average annual premium for health insurance in 2022 was $7,911 for single people. For family coverage, it averaged $22,463 for family coverage, a 43 percent increase since 2012.
The high cost of American health insurance has a number of causes. The website eHealth cites administrative costs, increasing prices for prescription drugs, and "lifestyle choices."
Rising Government Costs
Nearly 92% of Americans now have health insurance.
That's the good news.
Government programs like Medicare, Medicaid, and the Affordable Care Act have increased overall demand for medical services, resulting in higher prices as well.
What’s more, increases in the incidence of chronic conditions such as diabetes and heart disease, especially among seniors, have had a direct impact on increases in the cost of medical care. Chronic diseases constitute 85% of healthcare costs, and more than half of all Americans have a chronic illness.
Higher insurance premiums are only part of the picture. Americans are paying more out of pocket than ever before.
A shift to high-deductible health plans (HDHPs) that require out-of-pocket payments of up to $14,000 per family has added greatly to the cost of healthcare.
Employer contributions to HDHPs help to mitigate the higher deductible. According to one study, HDHP enrollees paid 20% of their total premium while preferred provider organization (PPO) enrollees paid up to 27% of theirs.
Avoidance of medical care due to concerns about unpredictable costs has been a problem for some years. A 2019 survey by the Physicians Advocacy Institute (PAI) found patients avoiding care due to anxieties about the potential costs of deductibles under their HDHPs.
The COVID-19 pandemic made it worse. A Kaiser Family Foundation poll suggests that up to 50% of the public has either avoided or postponed medical care due to concerns about exposure to COVID-19, further exacerbating the problem.
Avoiding care results in higher overall healthcare costs, as the delay makes treatable conditions more costly to treat.
COVID-19, with the increased need for testing, treatment, and care, was expected to change the cost of healthcare, although experts didn't agree on whether it would cause costs to rise or fall.
In fact, early on, healthcare spending fell, mostly due to patients postponing treatment for other illnesses. More recently, utilization and spending have rebounded.
In the grand scheme of things, COVID may not alter the trajectory of healthcare spending a great deal. Though short-term spending fell, it is expected to grow at an average annual rate of 5.4% and reach $6.2 trillion by 2028.
There have been recent attempts to patch the U.S. healthcare system. In particular, they address the lack of transparency that drives some people to avoid going to the doctor and others saddled with unexpected debt.
Lack of Transparency
From the view of the consumer, it’s difficult to predict the actual cost of healthcare. Most people know the cost of care is going up, but with few details and complicated medical bills, it’s not easy to know what you’re getting for your money.
That lack of transparency in healthcare was addressed in the Consolidated Appropriations Act (CAA) of 2021. One section of this act removes gag clauses related to price and quality information. Another, targeting health insurance, requires disclosure of direct and indirect compensation for brokers and consultants to the insurance companies.
The law became effective on Jan. 1, 2022.
The No Surprises Act
Additional CAA legislation, known as the No Surprises Act , addresses surprise billing. Another leading cause of rising healthcare costs, surprise billing can happen when a patient's treatment involves unanticipated out-of-network services, such as an anesthesiologist.
In addition to outlawing surprise medical and hospital bills, the act ends surprise air ambulance bills, requires transparency regarding in-network and out-of-network deductibles and out-of-pocket limitations, implements protections against provider discrimination, and requires an external review in the case of certain surprise bills.
Dispute resolution, patient protection, and transparency are mandated. Providers are required to issue fair and honest advance cost estimates.
This act also went into effect at the start of 2022.
How Much Does the Cost of Healthcare Rise Each Year?
According to the American Medical Association (AMA), healthcare costs are rising by about 4.5% a year. Spending on healthcare in the United States increased by 4.6% in 2019—to $3.8 trillion across the country, or $11,582 per person. This growth rate is in line with 2018 (4.7%) and slightly faster than what was observed in 2017 (4.3%).
What Is the Cost of the Average Health Insurance Premium?
The average annual premium for health insurance in 2022 was $7,911 for single people, and $22,463 for family coverage.
These numbers vary widely depending on where you live, your age, and the type of coverage you choose. But no matter which type of health insurance you buy, you're likely to see your costs rise year by year.
Why Did Health Insurance Premiums Go Up in 2021?
In addition to the long-term trend of increasing healthcare costs, short-term factors can make a big difference. Many people saw the cost of their health insurance increase faster than the average in 2021. This was primarily due to the cost of COVID-19 testing and treatment.
Americans spend a huge amount on healthcare every year, and the costs keep rising. In part, this increase is due to the inception of national programs like Medicare, Medicaid, and the Affordable Care Act, which extended free or subsidized healthcare to many more Americans. There are also short-term factors, such as the 2020 financial crisis and the COVID-19 pandemic, that push up the cost of health insurance.
The fact remains that the U.S., with its dependence on private insurers, has a unique healthcare system and it has evolved into the world's most expensive.
Health System Tracker. " The state of the U.S. healthcare system in 2022 and the outlook for 2023 ."
The Commonwealth Fund. " U.S. Health Care From a Global Perspective, 2022 ."
Centers for Medicaid and Medicare Services. " National Health Expenditure Projections 2022-2031 ."
U.S. Centers for Medicare and Medicaid Services. “ National Health Expenditures 2019 Highlights .”
JAMA: Journal of the American Medical Association. “ Factors Associated with Increases in US Health Care Spending, 1996–2013 .”
Peter G. Peterson Foundation. “ Why Are Americans Paying More for Healthcare? ”
U.S. Congress. “ Consolidated Appropriations Act (CAA), 2021 ,” Page 1,576.
American Hospital Association. " The Changing Ambulatory Care Landscape ."
eHealth. " Why is Health Insurance so Expensive? "
The Kaiser Family Foundation. " 2022 Employer Health Benefits Survey ."
U.S. Census Bureau. " Health Insurance Coverage in the United States: 2021 ."
National Center for Biotechnology Information. “ The Relation of the Chronic Disease Epidemic to the Health Care Crisis .”
Society for Human Resource Management. “ High-Deductible Plans More Common, but So Are Choices .”
Physicians Advocacy Institute. “ PAI-NORC Survey Shows High Deductible Health Plans Are a Barrier to Needed Care .”
Kaiser Family Foundation, Kaiser Health News. “ Nearly Half of Americans Delayed Medical Care Due to Pandemic .”
Peterson-KFF Health System Tracker. “ How Have Health Spending and Utilization Changed During the Coronavirus Pandemic? ”
U.S. Centers for Medicare and Medicaid Services. “ National Health Expenditure Data: NHE Fact Sheet .”
Journal of Accountancy. “ How COVID-19 Could Affect Health Spending .”
U.S. Congress. “ Consolidated Appropriations Act (CAA), 2021 ,” Page 1,709.
American Medical Association. “ Trends in Health Care Spending .”
Insurance Journal. “ Healthcare Costs, Premiums Likely to Rise for Years Due to COVID-19 .”
:max_bytes(150000):strip_icc():format(webp)/senior-couple-making-a-doctor-s-appointment--1141415536-5474527726e54332814e0112f345d7c9.jpg)
- Terms of Service
- Editorial Policy
- Privacy Policy
- Your Privacy Choices
Home — Essay Samples — Nursing & Health — Nursing — Argumentative Essay On Health Care Cost
Argumentative Essay on Health Care Cost
- Categories: Nursing
About this sample

Words: 949 |
Published: Mar 13, 2024
Words: 949 | Pages: 2 | 5 min read
Table of contents
Escalating costs, implications for individuals and society, potential solutions, rising drug prices, price variation for medical services, administrative costs.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Heisenberg
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
3 pages / 1405 words
3 pages / 1217 words
3 pages / 1407 words
3 pages / 1241 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Nursing
Ball J. & Pike G. (2009). Shift length: A literature review. Nursing Management (Harrow), 16(4), 22-25.Bogossian, F., Winters-Chang, P., & Tuckett, A. (2014). Extended work shifts and the impact on patient safety, productivity, [...]
To further my education and interest in nursing, I decided to become a HOSA member through my school. This year, I am participating in the Clinical Nursing event and have started studying for the competitive event for the [...]
Chatfield, S., Nolan, R., Crawford, J., & Hallam, J. (2016). Factors affecting adherence to hand hygiene in nursing: A systematic review. Journal of Hospital Infection, 92(4), 305-314.Gould, D. J., Moralejo, D., Drey, N., & [...]
Bock, R. (2019). Hand Hygiene Compliance and Glove Use. Retrieved October 26, 2019, from https://www.sciencedirect.com/science/article/abs/pii/S0196655318312069.
The role of a nurse is often seen as one of care and compassion, providing support and medical treatment to those in need. However, there is another aspect to nursing that is equally important but often overlooked - that of the [...]
Bureau of Labor Statistics. ( 2019, September 4). Registered nurses. Retrieved from
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
- Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
Article Critique
- Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
- Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
- Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
Research Paper
- Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring
Health Care in the United States, Essay Example
Pages: 4
Words: 1013
Hire a Writer for Custom Essay
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
In the United States, there has long been discussion about the quality and nature of the delivery of healthcare. The debates have included who may receive such services, whether or not healthcare is a privilege or an entitlement, whether and how to make patient care affordable to all segments of the population, and the ways in which the government should, or should not, be involved in the provision of such services. Indeed, many people feel that the healthcare in this country is the best in the world; others believe tha (The Free Dictionary)t our health delivery system is broken. This paper shall examine different aspects of the healthcare system in our country, discussing whether it has been successful in providing essential services to American citizens.
The delivery of healthcare services is considered to be a system; according to the Free Diction- ary (Farlex, 2010), a system is defined as “a group of interacting, interrelated, or interdependent elements forming a complex whole.” This is an apt description of our healthcare structure, as it is compiled of patients, medical and mental health providers, hospitals, clinics, laboratories, insurance companies, and many other parties that are reliant on each other and that, when combined, make up the entity known as our healthcare system.
Those who believe that our healthcare system is the best in the world often point to the fact that leaders as well as private citizens from countries throughout the world frequently come to the United States to have surgeries and other treatments that they require for survival. A more cynical view of this phenomenon is that if people have the money, they are able to purchase quality care in the U.S., a “survival of the fittest” situation. Those who lack the resources to travel to the U.S. for medical treatment are simply out of luck, and often will die without the needed care.
In fact, reports by the World Health Organization and other groups consistently indicate that while the United States spends more than any other country on healthcare costs, Americans receive lower quality, less efficient and less fairness from the system. These conclusions come as a result of studying quality of care, access to care, equity and the ability to lead long, productive lives. (World Health Organization,2001.) What cannot be disputed is that the cost of healthcare is constantly rising, a fact which was the precipitant to the large movement to reform healthcare in our country in 2010. More than 10 years ago, the goal of managed care was to drive down the costs of healthcare, but those promises did not materialize (Garsten, 2010.) A large segment of the population is either uninsured or underinsured, and it is speculated that over the next decade, these problems will only increase while other difficulties will arise (Garson, 2010.)
When examining the healthcare system, there are three aspects of care that call for evaluation: the impact of delivering care on the patient, the benefits and harms of that treatment, and the functioning of the healthcare system, as described in an article by Adrian Levy. Levy argues that each of these outcomes should be assessed and should include both the successes and the limitations of each aspect. The idea is that there should be operational measurements of patients’ interactions with the healthcare system that would include patients’ experiences in hospitals, using measurements of their functional abilities and their qualities of life following discharge. The results of patients’ interactions with the healthcare system should be utilized to develop and improve the delivery of healthcare treatment, as well as to develop policy changes that would affect the entire field of healthcare in the United States.
One view of the state of American healthcare is that the system is fragmented; there have been many failed attempts by several presidents to introduce the idea of universal healthcare. Instead, American citizens are saddled with a system in which government pays either directly or indirectly for over 50% of the healthcare in our country, but the actual delivery of insurance and of care is undertaken by an assortment of private insurers, for-profit hospitals, and other parties who raise costs without increasing quality of service (Wells, Krugman, 2006.) If the United States were to switch to a single-payer system such as that provided in Canada, the government would directly provide insurance which would most likely be less expensive and provide better results than our current system.
It is clear that throwing money at a problem does not necessarily resolve it; the fact that the United States spends more than twice as much on healthcare provision as any other country in the world only makes it more ironic that when it comes to evaluating the service, Americans fall appallingly flat. In my opinion, if the new healthcare reform bill had included a public option which would have taken the profit margin out of the equation, the nation and its citizens would have been in a much better position to receive quality healthcare. The fact that people die every day from preventable illnesses and conditions simply because they do not have affordable insurance is a national disgrace. In addition, many of the people who have been the most adamantly against government “intrusion” into their healthcare are actually on Medicaid or Medicare, federally-funded programs. Their lack of understanding of what the debate actually involves is striking, and they are rallying against what is in their own best interests. These are people that equate Federal involvement in healthcare as socialism. Unless and until our healthcare system is able to provide what is needed to all of its citizens, all claims that we have the best healthcare system in the world are, sadly, utterly hollow.
Adrian R Levy (2005, December). Categorizing outcomes of Health Care delivery. Clinical and investigative medicine, pp. 347-351.
Arthur Garson (2000). The U.S. Healthcare System 2010: Problems Principles and Potential Solutions. Retrieved July 3, 2010, from Circulation: The Journal of the American Heart Association: http://circ.ahajournals.org/cgi/reprint/101/16/2015
The Free Dictionary. (n.d.). Farlex. Retrieved July 3, 2010. http://www.thefreedictionary.com/system
World Health Organization. (2003, July). WHO World Health Report 2000. Retrieved July 3, 2010, from State of World Health: http://faculty.washington.edu/ely/Report2000.htm
Stuck with your Essay?
Get in touch with one of our experts for instant help!
Using Learning Journals in Continuing and Higher Education, Article Critique Example
Prolonged Exposure Therapy, Research Paper Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Essay Samples & Examples
Voting as a civic responsibility, essay example.
Pages: 1
Words: 287

Utilitarianism and Its Applications, Essay Example
Words: 356
The Age-Related Changes of the Older Person, Essay Example
Pages: 2
Words: 448
The Problems ESOL Teachers Face, Essay Example
Pages: 8
Words: 2293
Should English Be the Primary Language? Essay Example
Words: 999
The Term “Social Construction of Reality”, Essay Example
Words: 371
📕 Studying HQ
120+ healthcare argumentative essay topics [+outline], dr. wilson mn.
- August 3, 2022
- Essay Topics and Ideas , Samples
If you’re a nursing student, then you know how important it is to choose Great Healthcare argumentative essay topics.
After all, your essay will be graded on both the content of your argument and how well you defend it. That’s why it’s so important to choose topics that you’re passionate about and that you can research thoroughly.
What You'll Learn
Strong Healthcare argumentative essay topics
To help you get started, here are some strong Healthcare argumentative essay topics to consider:
- Is there a nurse shortage in the United States? If so, what are the causes, and what can be done to mitigate it?
- What are the benefits and drawbacks of various types of Nurse staffing models?
- What are the implications of the current opioid epidemic on nurses and patients?
- Are there any ethical considerations that should be taken into account when providing care to terminally ill patients?
- What are the most effective ways to prevent or treat healthcare-acquired infections?
- Should nurses be allowed to prescribe medication? If so, under what circumstances?
- How can nurses best advocate for their patients’ rights?
- What is the role of nurses in disaster relief efforts?
- The high cost of healthcare in the United States.
- The debate over whether or not healthcare is a human right.
- The role of the government in providing healthcare.
- The pros and cons of the Affordable Care Act.
- The impact of healthcare on the economy.
- The problem of access to healthcare in rural areas.
- The debate over single-payer healthcare in the United States.
- The pros and cons of private health insurance.
- The rising cost of prescription drugs in the United States.
- The use of medical marijuana in the United States.
- The debates over end-of-life care and assisted suicide in the United States.
As you continue, thestudycorp.com has the top and most qualified writers to help with any of your assignments. All you need to do is place an order with us.
Controversial Healthcare topics
There is no shortage of controversial healthcare topics to write about. From the high cost of insurance to the debate over medical marijuana, there are plenty of issues to spark an interesting and thought-provoking argumentative essay.
Here are some Controversial healthcare argumentative essay topics to get you started:
1. Is healthcare a right or a privilege?
2. Should the government do more to regulate the healthcare industry?
3. What is the best way to provide quality healthcare for all?
4. Should medical marijuana be legalized?
5. How can we control the rising cost of healthcare?
6. Should cloning be used for medical research?
7. Is it ethical to use stem cells from embryos?
8. How can we improve access to quality healthcare?
9. What are the implications of the Affordable Care Act?
10. What role should pharmaceutical companies play in healthcare?
11. The problems with the current healthcare system in the United States.
12. The need for reform of the healthcare system in the United States.
Great healthcare argumentative essay topics
Healthcare is a controversial and complex issue, and there are many different angles that you can take when writing an argumentative essay on the topic. Here are some great healthcare argumentative essay topics to get you started:
1. Should the government provide free or low-cost healthcare to all citizens?
2. Is private healthcare better than public healthcare?
3. Should there be more regulation of the healthcare industry?
4. Are medical costs too high in the United States?
5. Should all Americans be required to have health insurance?
6. How can the rising cost of healthcare be controlled?
7. What is the best way to provide healthcare to aging Americans?
8. What role should the government play in controlling the cost of prescription drugs?
9. What impact will the Affordable Care Act have on the healthcare system in the United States?
Hot healthcare argumentative essay topics
Healthcare is always a hot-button issue. Whether it’s the Affordable Care Act, single-payer healthcare, or something else entirely, there’s always plenty to debate when it comes to healthcare. Here are some great healthcare argumentative essay topics to help get you started.
1. Is the Affordable Care Act working?
2. Should the government do more to provide healthcare for its citizens?
3. Should there be a single-payer healthcare system in the United States?
4. What are the pros and cons of the Affordable Care Act?
5. What impact has the Affordable Care Act had on healthcare costs in the United States?
6. Is the Affordable Care Act sustainable in the long run?
7. What challenges does the Affordable Care Act face?
8. What are the potential solutions to the problems with the Affordable Care Act?
9. Is single-payer healthcare a good idea?
10. What are the pros and cons of single-payer healthcare?
Argumentative topics related to healthcare
Healthcare is always an ever-evolving issue. It’s one of those topics that everyone has an opinion on and is always eager to discuss . That’s why it makes for such a great topic for an argumentative essay . If you’re looking for some fresh ideas, here are some great healthcare argumentative essay topics to get you started.
1. Is our healthcare system in need of a complete overhaul?
3. Are rising healthcare costs making it difficult for people to access care?
4. Is our current healthcare system sustainable in the long term?
5. Should we be doing more to prevent disease and promote wellness?
6. What role should the private sector play in providing healthcare?
7. What can be done to reduce the number of errors in our healthcare system?
8. How can we make sure that everyone has access to quality healthcare?
9. What can be done to improve communication and collaboration between different parts of the healthcare system?
10. How can we make sure that everyone has access to the care they need when they need it?
Argumentative essay topics about health
There are many different stakeholders in the healthcare debate, and each one has their own interests and perspectives. Here are some great healthcare argumentative essay topics to get you started:
1. Who should pay for healthcare?
2. Is healthcare a right or a privilege?
3. What is the role of the government in healthcare?
4. Should there be limits on what treatments insurance companies must cover?
5. How can we improve access to healthcare?
6. What are the most effective methods of preventing disease?
7. How can we improve the quality of care in our hospitals?
8. What are the best ways to control costs in the healthcare system?
9. How can we ensure that everyone has access to basic care?
10. What are the ethical implications of rationing healthcare?
Medical argumentative essay topics
- Is healthcare a fundamental human right?
2. Should there be limits on medical research using human subjects?
3. Should marijuana be legalized for medicinal purposes?
4. Should the government do more to regulate the use of prescription drugs?
5. Is alternative medicine effective?
6. Are there benefits to using placebos in medical treatment?
7. Should cosmetic surgery be covered by health insurance?
8. Is it ethical to buy organs on the black market?
9. Are there risks associated with taking herbal supplements?
10. Is it morally wrong to end a pregnancy?
11. Should physician-assisted suicide be legal?
12. Is it ethical to test new medical treatments on animals?
13. Should people with terminal illnesses have the right to end their lives?
14. Is it morally wrong to sell organs for transplantation?
15. Are there benefits to using stem cells from embryos in medical research?
16. Is it ethical to use human beings in medical experiments?
17. Should the government do more to fund medical research into cancer treatments?
18. Are there risks associated with genetic engineering of humans?
19. Is it ethical to clones humans for the purpose
Argumentative essays on mental illness
- Should there be more focus on mental health in schools?
- Are our current treatments for mental illness effective?
- Are mental health disorders more common now than they were in the past?
- How does social media impact mental health?
- How does trauma impact mental health?
- What are the most effective treatments for PTSD?
- Is therapy an effective treatment for mental illness?
- What causes mental illness?
- How can we destigmatize mental illness?
- How can we better support those with mental illness?
- Should insurance companies cover mental health treatments?
- What are the most effective treatments for depression?
- Should medication be used to treat mental illness?
- What are the most effective treatments for anxiety disorders?
- What are the most effective treatments for OCD?
- What are the most effective treatments for eating disorders?
- What are the most effective treatments for bipolar disorder?
- How can we better support caregivers of those with mental illness?
- What role does stigma play in mental illness?
![120+ healthcare argumentative essay topics [+outline] 1 120+ healthcare argumentative essay topics [+outline] 1](https://i0.wp.com/studyinghq.com/wp-content/uploads/2022/08/image-17-796x1030.png?resize=796%2C1030&ssl=1)
Start by filling this short order form order.studyinghq.com
And then follow the progressive flow.
Having an issue, chat with us here
Cathy, CS.
New Concept ? Let a subject expert write your paper for You
Related Posts
- Term-Long Project Nursing Paper Example
- Case Study on Moral Status
- Applying the Concepts of Epidemiology and Nursing Research on Measles Nursing Paper Essay
- A Comprehensive Guide to Writing a Nursing Research Paper
- 50 Potential Research Summary Topics
- Free Essays
- Citation Generator
- Topic Generator
- Paraphrasing Tool
- Conclusion Maker
- Research Title Generator
- Thesis Statement Generator
- Summarizing Tool
- How to Guides
- Essay Topics and Ideas
- Manage Orders
- Business StudyingHq
- Writing Service
- Discounts / Offers
Study Hub:
- Studying Blog
- Topic Ideas
- Business Studying
- Nursing Studying
- Literature and English Studying
Writing Tools
- Terms and Conditions
- Privacy Policy
- Confidentiality Policy
- Cookies Policy
- Refund and Revision Policy
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Contact Us:
📞 +15512677917
2012-2024 © studyinghq.com. All rights reserved
- Open access
- Published: 15 March 2024
Cost and economic evidence for asset-based approaches to health improvement and their evaluation methods: a systematic review
- Alice Wreford 1 , 2 ,
- Linda Birt 1 , 3 ,
- Jennifer A. Whitty 1 , 4 ,
- Sarah Hanson 1 ,
- Susan Conquer 5 &
- Adam P. Wagner 1 , 2
BMC Public Health volume 24 , Article number: 814 ( 2024 ) Cite this article
121 Accesses
2 Altmetric
Metrics details
Asset-based approaches (ABAs) tackle health inequalities by empowering people in more disadvantaged communities, or targeted populations, to better utilise pre-existing local community-based resources. Using existing resources supports individuals to better manage their own health and its determinants, potentially at low cost. Targeting individuals disengaged with traditional service delivery methods offers further potential for meaningful cost-savings, since these people often require costly care. Thus, improving prevention, and management, of ill-health in these groups may have considerable cost implications.
To systematically review the extent of current cost and economic evidence on ABAs, and methods used to develop it.
Search strategy terms encompassed: i) costing; ii) intervention detail; and iii) locality. Databases searched: Medline, CENTRAL and Wed of Science. Researchers screened 9,116 articles. Risk of bias was assessed using the Critical Appraisal Skills Programme (CASP) tool. Narrative synthesis summarised findings.
Twelve papers met inclusion criteria, representing eleven different ABAs. Within studies, methods varied widely, not only in design and comparators, but also in terms of included costs and outcome measures. Studies suggested economic efficiency, but lack of suitable comparators made more definitive conclusions difficult.
Economic evidence around ABAs is limited. ABAs may be a promising way to engage underserved or minority groups, that may have lower net costs compared to alternative health and wellbeing improvement approaches. ABAs, an example of embedded services, suffer in the context of economic evaluation, which typically consider services as mutually exclusive alternatives. Economics of the surrounding services, mechanisms of information sharing, and collaboration underpin the success of assets and ABAs. The economic evidence, and evaluations in general, would benefit from increased context and detail to help ensure more nuanced and sophisticated understanding of the economics of ABAs. Further evidence is needed to reach conclusions about cost-effectiveness of ABAs.
Peer Review reports
Asset based approaches to health
In the United Kingdom (UK) a growing and ageing population, and increasing burden on health services, is leading to an emphasis on prevention, integration of services and supporting people to manage their own health [ 1 ]. Historically, approaches to improve population health have utilised a ‘deficit model’ : focusing on identifying the problems and needs of the population that require costly curative services [ 2 , 3 , 4 ]. This undermines the role that individuals and communities can play as active participants to create, acquire and maintain their own health [ 2 ]. The NHS Long Term Plan (2019) calls for a shift towards a pro-active model for health and well-being, whereby society values and tries to enable a state of complete physical, mental and social well-being, as opposed to waiting for individuals to reach ill-health before receiving support and treatment [ 5 , 6 ]. This recognising that positive health and social outcomes can be achieved more successfully and efficiently if there is a shift away from a ‘doing to’ culture (whereby individuals are treated once they become unwell) to one that respects meaningful and ‘preventative’ social change (where individuals are supported and empowered to make healthier choices, promoting continued good health) [ 7 ].
‘Assets’ and ‘asset-based approaches’ (ABAs) aim to identify and utilise health promoting or protective factors that are most likely to lead to higher degrees of overall health and wellbeing, achievement, and sustainability [ 2 ]. ‘Assets’ are community resources, and can refer to financial resources, physical infrastructure, facets of social capital or individual capabilities [ 8 ]. Assets operate across multiple levels, for example enabling self-esteem and resilience at the individual-level, supportive friendship and peer networks at community-level, and provision of positive environmental and organisational resources to promote health and well-being at structural-levels [ 9 ]. ABAs build on the skills of local people, the power of local associations and the supportive functions of institutions and services, to build stronger, more sustainable communities [ 10 ]. ABAs are considered a subset of community-based interventions, distinctly implementing interventions which aim to build capacity, engagement, knowledge and/or resources within a defined community asset e.g., local churches, existing community groups, local parks or hyperlocal geographical areas. They make visible and value the skills, knowledge, connections and potential in a community [ 11 ].
Generally speaking, health and wellbeing services suffer from disparity in uptake and provision, such that uptake is socially patterned, and services are more likely to be successfully accessed by affluent groups—termed the ‘ inverse prevention law’ [ 12 , 13 ]. Therefore, preventative health interventions may not reach the most disadvantaged and those furthest from reaching their full health potential [ 12 ]. Consequentially, preventative services may benefit from ABAs. One of the main advantage of ABAs, beyond standard community interventions, is that they can engage: i) members of society who are more likely to be disengaged with traditional methods of service delivery; and ii) specific populations (e.g. cancer survivors). They do this by tapping into existing community networks, making use of existing rapport and trusted connections, to facilitate health-related conversations and information sharing which otherwise may not occur. Therefore, equitable community-based development may be best supported through ABAs [ 14 , 15 ]. Further, building on existing assets potentially reduces high-level start-up costs, such as reducing the need for highly trained staff to address participant care needs, alongside delivering engagement and implementing strategies. In ABAs, individuals working in established groups are typically already well-versed at meeting their participants’ needs [ 16 ]. Since there are reduced start-up costs, and engagement is expected to be high, from an economic perspective, ABAs offer a potentially efficient approach to delivering benefits for participants.
Economic evaluation of ABAs
Decision-makers must routinely make choices about how to prioritise public health problems and related interventions within limited budgets and resources. In making such choices, decision-makers can benefit by knowing the financial resources required to implement each intervention and how money invested compares to outcomes achieved [ 17 ]. Economic comparisons are challenging in the context of: i) comparing one ABA to another ABA; and ii) comparing ABAs to other types of health and social care interventions. To date, it is unclear what economic evidence has been collected in the context of ABAs and what methods have been used to generate this evidence.
Well-established frameworks, known as economic evaluations (EEs), inform decision-makers about the comparative costs and outcomes (or ‘benefits’) of a range of mutually exclusive courses of action for health and social care. From this definition, it is worth emphasising that EEs do not exclusively focus on costs—outcomes/benefits are crucially important too. Typically, EEs involve exploring which option will maximise health and social care outcomes, most commonly in the form of quality-adjusted life years (QALYs) that seek to capture impacts on life extension and its quality, subject to the constraints of the health sector budget. Public health and social care interventions, including ABAs, may be considered complex interventions, in that they offer flexibility in intervention delivery and individual-level variability in outcomes (e.g. improving choice, access and participation in healthcare, education, housing, employment, social activity and personal care) [ 18 ]. Complex intervention research “goes beyond asking whether an intervention works in the sense of achieving its intended outcome – to asking a broader range of questions (e.g., identifying what other impact it has… taking account of how it interacts with the context in which it is implemented, how it contributes to system change…)” (P.1, [ 19 ]). Therefore, while EEs may be appropriate to assess the value of ABAs, the use of health-focused outcomes, such as QALYs, are unlikely to capture their full impacts. Wider wellbeing outcomes, often measured as wellbeing adjusted life years (WALYs or WELBYs), have received growing interest in the evaluation of public health interventions [ 20 , 21 ]. While these measures purport to measure and value a broader range of dimensions of health and wellbeing, they are generally viewed as sub-optimal for evaluating complex interventions where the full spectrum of benefits extends well beyond health [ 22 ].
Beyond outcome measurement, the EE techniques that typically utilise QALYs (e.g. cost-utility analyses) generally focus on the health care sector (health perspective), often again ‘missing’ some of the important wider societal impacts. A wider societal perspective may be adopted, capturing costs across sectors (e.g. beyond health) with the aim of maximising welfare gain to society [ 23 ]. However, this approach is still limited, with impact primarily affecting the ‘cost side’ of the equation. EEs which seek to capture the full range of health and non-health costs and benefits across different sectors (e.g. cost consequence analysis, cost benefit analysis or multicriteria decision analysis) may be more relevant in this context. However, these approaches require multidimensional datasets, potentially complex modelling approaches, and offer an opportunity for inappropriate interpretation of results if the evaluation is not appropriately designed for the decision context [ 24 ].
Importantly, health equity, a key objective in public health policy, is rarely captured in economic evaluations [ 25 ]. With the increasing awareness of inequity in health improvement, it is essential that health economic methodologies develop to capture this under-reported outcome. Health economics is regularly centred in the quasi-egalitarian value judgement that ‘a QALY is a QALY’ ; where “QALYs are equally weighted and the health outcome is worth the same no matter how it is achieved, or by whom it accrues” (P.231, [ 25 ]). This assumption conflicts with an increasing focus on improving health equity and reaching under-served populations. As ABAs seek to reach those furthest from their health potential, there is opportunity for intervention impact to be greater than it would be for the general population. Specifically in the context of prevention, health improving behavioural shifts (e.g. increased use of health services) may be more impactful when initial behaviours were more harmful (i.e. those who rarely access services may see greater health and wellbeing improvements than those who already regularly engage with services). More broadly, the formerly prevalent view of health gain maximisation – where the objective is primarily to maximise total health benefit [ 26 , 27 ] – may be undervaluing some interventions as it does not capture the entire impact and value of engaging disengaged individuals to effectively manage their own health. Thus, one might question the applicability of non-targeted health maximising of QALYs in the community care setting – perhaps it does matter by whom it is accrued, providing an argument for weighting cost per QALY by who is benefitting. Additionally, others have noted that allocation of health care resources solely based on health maximation can lead to discrimination against certain groups [ 28 ].
A challenge in evaluating ABAs is establishing a suitable alternative to compare the ABA to. In the case of novel asset-based interventions, which are unique in their localised social structures, appropriate comparators are not always clear. The intervention may be compared to the ‘absence of the intervention’ and/ or ‘standard care’. However collecting data for these alternatives is challenging with ABA interventions, since they often involve whole communities in a specific locale (e.g. potential lack of unaffected ‘control’ individuals) and often utilise information sharing and capacity building (consequently statistical ‘contamination’ is likely between intervention and control groups—discussed further later). Absence of a suitable alternative precludes a full EE, and more generally can make it difficult to robustly determine the impact of an intervention.
To better support development and evaluation in complex intervention settings, the National Institute of Health Research and the UK Medical Research Council Guidance commissioned a framework [originally developed 2006; last updated 2021] [ 19 ]. This guidance is well positioned for ABA development as it recognises the context specific complexity, framing interventions as events in a wider system. The framework appreciates the pragmatic embedding of services, and its conflict with the assumptions of mutual exclusivity of interventions required for current EE methods – suggesting supporting qualitative studies may be useful to support interpretation of EEs [ 19 ]. The framework highlights crucial aspects of evaluation design, including appropriate: comparator; choice of outcome measure or evidence of change; study design; and, costs (including implementation and set-up costs) [ 19 ].
Recent developments in the guidance have focused on giving attention to properties of the intervention itself, such as: range of behaviours targeted; expertise and skills required by those delivering and receiving the intervention; number of groups; community setting; and, level of flexibility of the intervention or its components. Appropriate design of complex interventions allows for flexibility in implementation, whilst maintaining the integrity of the core intervention components. This recognises that the ‘same’ ABA applied in two different settings may look different as they appropriately and intentionally adapt to the community setting and target demographic needs. These flexible properties of the intervention have implications for many aspects of its evaluation, and subsequent interpretation. Thus, intervention detail will be considered within this review.
To make best use of scarce public budgets, it is important to understand the current cost and economic evidence base for ABAs. Further, to inform future research, we want to investigate the methods used to create the current evidence. Thus, this systematic review seeks to address:
What designs, methods, and outcomes measures have been used to produce cost and economic evidence?
What is the accrued evidence for the cost and economic impact of ABAs?
The protocol for this systematic review has been registered in PROSPERO (CRD42021236548). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed [ 29 ].
Patient and public involvement (PPI) and stakeholder contribution
Given the broad array of potential community assets, and the flexibility of ABAs, it is challenging to outline a formal or universal definition. Hence, PPI partners and stakeholders were closely involved in defining and categorising ABAs, development, and finalisation of the search terms and strategy, and evaluating the quality of evidence found (e.g., reflecting on the range of outcome measures used and their suitability). They brought specific experience to the review through their roles as a local authority commissioning manager and local Healthwatch co-production facilitator [‘Healthwatch’ is a health and social care champion in England, which ensures service providers and decisions makers listen to public feedback, with the aim to improve care ( https://www.healthwatch.co.uk/ ) ]. Each was familiar with ABAs prior to involvement in this study. This level of partner involvement was essential in the exploratory work to help ensure the questions asked of the literature and focus of analysis resonated with public health practice.
Search strategy
The search strategy consisted of three broad components capturing terms associated with: i) costing; ii) intervention detail; and iii) locality. The search strategy was developed with PPI contribution (outlined in Sect. " Inclusion and exclusion criteria "). The second component (intervention detail) received careful attention, helping to ensure eligible papers where the intervention was not explicitly termed or identified as an ABA were captured. Terms included: ‘asset’; 'coproduction’; ‘community development’; ‘capabilities’; ‘resilience’; ‘salutogenesis’; ‘self-care’; ‘participatory approach’; ‘peer support’; ‘intervention’; ‘social prescription’; ‘health promotion’; ‘lay worker’; ‘wellbeing officer’; ‘community health worker’; ‘capacity’; and ‘upskill’. Complete search terms are given in Supplementary Material 1 .
Electronic bibliographic databases [MEDLINE (via PubMED); Cochrane Centre Register of Controlled Trials (CENTRAL); and Web of Science] were searched on 07.03.23, with no publication date restrictions.
Inclusion and exclusion criteria
The following inclusion and exclusion criteria were employed.
Inclusion – all required:
Interventions categorised as ABA (following our above definition), even when not explicitly named or labelled as such.
Studies which evaluated the ‘cost’, or ‘ costs and benefits’ relating to at least one ABA.
Interventions delivered by non-clinical professionals – e.g. community members, community service staff. Interventions may involve a training component, supportive role or be co-produced with health practitioners.
Peer reviewed papers only.
English language only.
Exclusion, where any of the following apply:
Interventions delivered in clinical settings (i.e. interventions centred in hospital or General Practices).
Community setting not detailed.
Interventions administered via telephone or cyber communication, unbound by geographical constraint.
Interventions delivered exclusively by a clinical professional.
Studies which do not report cost(s) associated with the intervention.
Study selection
Database search results were extracted to a citation manager (Endnote X9) where duplicates were identified and removed. Study details (including title and abstracts) were uploaded to web-based software Rayyan ( https://www.rayyan.ai/ ) for screening. Article abstracts were shared between two researchers (AW & LB). Within Rayyan, each reviewer recorded for each article whether it was rejected or put forward for stage two review.
Articles selected for full-text review were independently compared to the inclusion/ exclusion criteria by two reviewers (AW & LB) to finally determine their inclusion. Where these reviewers disagreed, a third reviewer (JAW) arbitrated.
Data extraction
A data extraction table was developed in MS Excel (Supplementary Material 2 ), capturing 20 study characteristics, and populated by AW.
Included studies were categorised into three groups:
Reporting only implementation and running costs (IRC);
Reporting implementation and running costs AND health and/or social care related costs (IRHSC);
Including an economic evaluation (EE) (thus a joint comparison of costs and benefits comparing the ABA to suitable comparator).
Studies categorised to i) IRC and ii) IRHSC did not require a study comparator.
Quality of reporting assessment
The Critical Appraisal Skills Programme (CASP) quality appraisal tool (reported in full in Supplementary Material 3 ) was used to assess the risk of bias. CASP was selected as it can be used to assess a wide range of both qualitative and quantitative studies, including, randomised controlled trials, cohort studies and economic evaluations [ 30 ]. For each study, a CASP checklist relevant to its study type was selected.
Literature search and evaluation for study inclusion
A summary of the process of review and selection is given in the PRISMA flow diagram (Fig. 1 ).
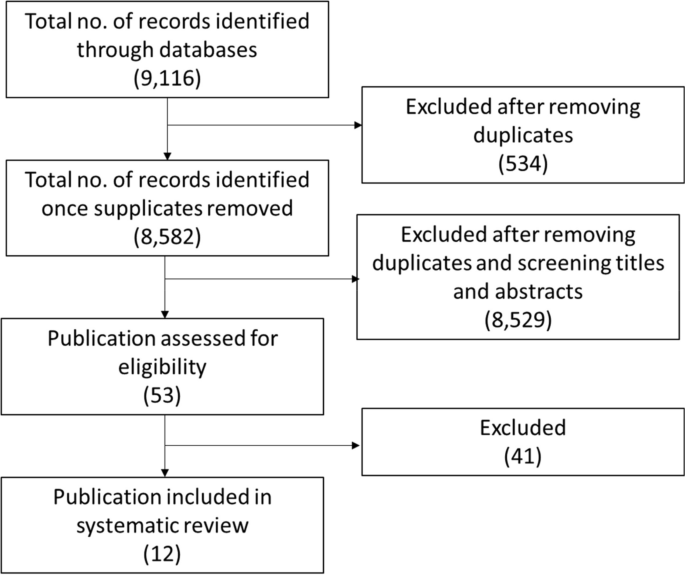
PRISMA diagram for search process
Searches yielded a total of 9,116 results, of which 534 were identified as duplicates. Subsequently, 8,582 abstracts were screened. Of the screened abstracts, 8,529 studies were excluded, with unanimous (100%) agreement between primary reviewers (AW & LB). The 53 remaining papers underwent full text review: 48 had their inclusion/exclusion status agreed between by the first two reviewers (AW & LB), with disagreement on the remaining five studies resolved by the third reviewer (JAW). Twelve publications were agreed for inclusion.
Studies were appraised using the CASP tools relevant to study type (Tables 1 , 2 and 3 ).
Overview of studies
Twelve papers, representing eleven different ABAs, met the inclusion criteria: Pizzi 2014 [ 37 ] assesses the cost-effectiveness of the ABA reported in Gitlin 2012 [ 36 ]. Characteristics of included studies relate to the 11 ABAs, treating Pizzi 2014 and Gitlin 2012 as one study.
Most papers [ n = 10] were published between 2010–2020, with two published in 2001–2002 [ 31 , 40 ]. Papers were categorised to: reporting only implementation and running costs (IRC) [ n = 1: [ 36 ]]; reporting implementation and running costs AND health and/or social care related costs (IRHSC) [ n = 2: [ 32 , 34 ]]; and including an economic evaluation (EE) [ n = 9: [ 31 , 33 , 35 , 37 , 38 , 39 , 40 , 41 , 42 ]]. Here forward, where counted, paper categories are indicated with subscripts.
The reported ABAs were delivered in the: USA [ n = 7: n IRC = 1 [ 36 ], n IRHSC = 1 [ 32 ], n EE = 5 [ 31 , 35 , 37 , 38 , 39 ]]; Australia [n EE = 1 [ 33 ]]; and the UK [ n = 4: n IRHSC = 1 [ 34 ], n EE = 3 [ 40 , 41 , 42 ]]. Among selected studies, only one labelled its intervention as an ABA [ 42 ], with others using phrases such as “delivered through community-based organisations” (P.2, [ 36 ]) and “engage with social networks and build social capital to enable community ownership” (P.104, [ 33 ]). Table 4 details phrases used to describe the ABAs among included papers.
The ABAs included: peer support services [ n = 2: n IRHSC = 1 [ 34 ], n EE = 1 [ 41 ]]; signposting services [n EE = 1 [ 42 ]]; educational programmes without a screening component [ n = 6: n IRHSC = 1 [ 32 ], n EE = 5 [ 31 , 33 , 35 , 39 , 40 ]]; and educational programmes with a screening component [ n= 2: n IRC = 1 [ 36 ], n EE = 1 [ 37 ]]. ABAs were delivered by: upskilled staff from within an existing asset [ n = 4: n IRC = 1 [ 36 ], n IRHSC = 1 [ 32 ], n EE = 2 [ 35 , 37 ]]; training public members associated with the asset [n EE = 5 [ 31 , 39 , 40 , 41 , 42 ]]; introducing skilled workers to the asset [ n = 2: n IRHSC = 1 [ 34 ], n EE = 1 [ 33 ]]; and by connecting members from across the community network [n EE = 1 [ 38 ]].
Each ABA was run across multiple community sites. Approaches included non-religious community venues [ n = 9: i.e. senior centres [ n = 4: n IRC = 1 [ 36 ], n EE = 3 [ 32 , 35 , 37 ]], bars [n EE = 1 [ 31 ]], community centres [ n = 4: n IRHSC = 2 [ 32 , 34 ], n EE = 2 [ 41 , 42 ]], and a primary school [n EE = 1 [ 33 ]] or cultural or religious spaces [n EE = 2 [ 39 , 40 ]]. One study (engaging African American and Latino adults with depressive symptoms) operated across both religious (faith centres) and non-religious spaces (senior centres and barber shops) venues [n EE = 1 [ 38 ]]. See Table 2 for further intervention delivery detail.
Targeted populations included: ‘gay and bisexual men’ [n EE = 1 [ 31 ]]; individuals ≥ 55 [ n = 3: n IRC = 1 [ 36 ], n IRHSC = 1 [ 32 ], n EE = 1 [ 37 ]]; school students [n EE = 1 [ 33 ]]; ‘Black and minority ethnic groups’ [ n = 5: n IRC = 1 [ 36 ], n EE = 4 [ 37 , 38 , 39 , 40 ]]; and, adults i) with type 2 Diabetes [n EE = 1 [ 41 ]], ii) with depressive symptoms (African Americans and Latinos) [n EE = 1 [ 38 ]], iii) up to two years post stroke [n IRHSC = 1 [ 34 ]] iv) who are obese [n EE = 1 [ 35 ]] and v) residing in North England (County Durham) [n EE = 1 [ 42 ]]. County Durham, a mixed rural and urban area, was of interest as resident health is typically poorer than the national average; the service aimed to predominately work with the county’s 30% most deprived communities (no further detail provided on how these communities were defined or identified) [ 42 ].
What designs, methods and outcomes measures have been used to produce cost and economic evidence?
Table 5 summaries the designs, methods and outcome measures used to produce the economic evidence on ABAs.
The study designs used to evaluate the ABAs included: cohort studies [ n = 3: n IRHSC = 1 [ 32 ], n EE = 2 [ 31 , 33 ])]; individual-level randomised controlled trials (RCTs) [ n = 3: n IRC = 1 [ 36 ], n IRHSC = 1 [ 34 ] (feasibility trail for larger scale study), n EE = 1 [ 37 ]]; cluster RCTs (with ‘clusters’ typically corresponding to the community asset) [n EE = 4 [ 35 , 38 , 39 , 41 ]]; a before and after study [n EE = 1 [ 42 ]]; and, a panel study [n EE = 1 [ 40 ]].
All studies compared, at the minimum, health/wellbeing outcomes against/between:
post intervention outcomes between participation/ non-participation [n IRHSC = 1 [ 32 ]];
pre- and post- intervention outcomes [n EE = 1 [ 33 ]];
four-month wait-list control group (the control group received the intervention four-months after the intervention arm) [ n = 2: n IRC = 1 [ 36 ], n EE = 1 [ 37 ]];
non-ABA intervention (technical assistance offered through webinar and primary care site visits, ‘traditional’ style intervention delivered for the evaluation) [n EE = 1 [ 38 ]];
healthcare professional delivered service versus ABA lay worker delivered service [n EE = 1: [ 35 ]]
standard/typical care, and [n EE = 4 [ 34 , 39 , 40 , 41 ]];
forecasted intervention outcomes through behaviour change models [n EE = 2 [ 31 , 42 ]].
Primary outcome and secondary outcomes (either health/ wellbeing and/or economic outcomes) were explicitly specified in four papers: in one instance both were cost outcomes [n IRHSC = 1 [ 32 ]]; in two instances both were health outcomes [ n = 2: n IRC = 1 [ 36 ], n IRHSC = 1 [ 34 ]]; and in a single instance both were measures of cost-effectiveness [‘Incremental cost effectiveness ratio’ (ICER): a summary measure, dividing the difference in total cost by the difference in the chosen measure of health outcome or effect; n EE = 1 [ 37 ]]. In all other cases health outcome was reported alongside aggregated cost or within cost-effectiveness measures (not identified as primary or secondary outcomes).
Health outcome measures utilised included: i) PHQ-9 and change in categorical diagnosis [n IRC = 1, [ 36 ]]; ii) infections averted and QALY gained [n EE = 1, [ 31 ]]; iii) ICECAP-A, Footnote 1 WEMWBS, Footnote 2 HADS Footnote 3 ; RSES, Footnote 4 SF-36 V.1 Footnote 5 and HSDS-111 Footnote 6 [n IRHSC = 1, [ 34 ]]; iv) achieved behaviour change [n EE = 1 [ 42 ]]; v) weight loss [n EE = 1 [ 39 ]]; and, vi) EQ-5D and HUI-3- derived QALY [n EE = 1, [ 37 ]].
Seven studies report aggregate cost [ n = 7: n IRC = 1 [ 36 ], n IRHSC = 2 [ 32 , 34 ], n EE = 4 [ 31 , 33 , 38 , 41 ]], with five reporting cost within cost-effectiveness measures: ICER [n EE = 2 [ 37 , 40 ]], ‘value for money’ assessment [n EE = 1 [ 42 ]] and ‘cost per kg loss’ [n EE = 2 [ 35 , 39 ]].
Table 6 summaries the accrued evidence for the cost impact of the ABAs. Gitlin 2012 [ 36 ] [clustered randomised trial], assigned to IRC, reported cost without comparison. Thus, a conclusion based on this paper, as to whether the ABA is cost-effective cannot be reached. The later published economic evaluation by Pizzi et al. [ 37 ] explores the cost-effectiveness of the ABA costed in the Gitlin 2012 [ 36 ] (details given below).
Category IRHSC consists of two studies. Similarly to Gitlin 2012 [ 36 ], Ellis-Hill 2019 [ 34 ] [feasibility study] reported cost without a comparison, thus cost-effectiveness cannot be determined [ 34 ]. The study notes the lack of suitable comparators within existing literature, precluding easily overcoming the lack of study comparator. Further, the authors make recommendations for more appropriate use of wellbeing measures to support evaluation of intervention impact. Within a retrospective cohort design, Mayer et al. [ 32 ] compared participating older adults within senior centres, against non-participating community members. Compared to the non-participants, during the year following the ABA, participants had lower, but non-significant ( P = 0.58), total health care costs and no difference in hospitalisation. The authors note that ABA participants had significantly higher levels of comorbidity ( P < 0.001) than the non-participant control. Thus, the comparison may be confounded by the typical increase in hospitalisation seen when comorbidity severity is higher: the ABA impact may be undervalued due to disparity in the study arms. Further, to assess bias, they assessed inclination to use preventative health services – the intervention arm had significantly higher scores, suggesting a stronger tendency to access/use services. Given this, Mayer 2010 [ 32 ] is suggestive of a dominant intervention [“A dominant treatment option is one that is both less costly and results in better health outcome than the comparator treatment” [ 43 ]].
Nine studies were categorised as EEs, with varying degrees of detail. Using a population-level model Kahn 2001 [ 31 ] estimated 5.0 to 6.2 HIV infections averted over five years, at a societal cost of $18,000 or less per infection averted ( excluding savings from HIV medical costs averted). These authors emphasise different time frames, epidemic scenarios, cost perspectives and modelling inputs lead to a range in cost per infection averted ($4,500 to $46,400) [ 31 ]. They believe this compares favourably with other programmes (e.g. Biloxi: $12,000 to $65,000 per HIV case averted) [ 31 ]. When savings from HIV medical costs averted are included, the program “eliminates more in HIV medical costs than it costs to implement” (P. 487, [ 31 ]).
Stevens [ 40 ] used Monte Carlo simulation, estimating intervention costs of £56,986, and reduction in in smoking of 3–7%, resulting in a mean cost of just over £105 per life year gained [ 40 ]. Intervention success was noted, in particular, among those not in full time employment. No explicit statement about cost effectiveness was made by the authors. Krukowski [ 35 ] compared intervention implementation costs (training; recruitment; materials; ongoing implementation support) of $165 per participant to mean weight loss of 3.7 kg per participant, considered cost-effective compared to a professionally delivered service [ 35 ].
Pizzi [ 37 ] reported mean incremental costs of $146 per participant per month, with an incremental utility of 0.046 (EQ-5D derived). Base case ICERs, compared to 4-month control, were $64,896 per QALY (EQ-5D) and $36,875 per QALY (HUI-3). Sensitivity analysis yielded cost/QALY range of $20,500-$76,500. The study concludes cost effectiveness compared to threshold values [such thresholds are “the maximum amount a decision-maker is willing to pay for a unit of health outcome” [ 44 ]]. Pizzi et al. consider thresholds identified in the literature (US $50,000-$100,000/QALY), and previously reported range of ICERs for pharmacological and neurological depression interventions [ 37 ]. Eckermann [ 33 ] used an investment multiplier to assess cost effectiveness of an initial government grant, estimating the multiplier impact on total community activity (up to two years) was 5.07 ($226,737 against $44,758 invested). They label this as a successful return on investment (without comparison to any particular threshold), alongside success in health promotion and community network is concluded [ 33 ].
Wingate [ 41 ] conducted a cost comparison, arguing against a cost effectiveness analysis given no statistically significant difference in condition-specific outcome measure or quality of life assessment between alternatives. Per participant per annum, implementation costs were £13.84, out-of-pocket costs £11.41, but the NHS incurred a cost-saving £138.38 – overall, a saving of £113.13 [ 41 ]. Consequently, the authors conclude the intervention is cost effective, highlighting reductions in self-reported healthcare utilisation. Chung et al. [ 38 ] use a cost consequence framework, reporting disaggregated direct and indirect costs across various service sectors. The study comparator had lower overall costs, due to higher start-up costs (to engage and train staff and organisations within the ABA) and no significant differences in 12-month service use cost. However, the authors note capacity was successfully built within community staff, with information shared within the organisation, with potential longer-term benefits not captured in the 12-month evaluation. This omission was common across all studies – none valued the benefit of building capacity/upskilling staff.
Visram [ 42 ] conducted a value for money assessment. They estimated total public sector cost savings of £2,406,920 (health gain and cost saving to NHS: £1,477,911; costs offset to NHS from asset mapping and signposting: £798,800; social care: £126,326; criminal justice: £3,883) [ 42 ] against service delivery costs of £3,528,894, giving an overall cost of £1,121,974. With an unweighted total health gain of 287.7 QALYs, this results in a cost per QALY of £3,900. Thus, the intervention was deemed cost effective against National Institute for Health and Care Excellence recommended threshold value £20,000-£30,000 per QALY gained [ 42 ].
Yeary [ 39 ] report per participant mean intervention costs of $348.95 and mean weight loss of 2.53 kg, resulting in a cost of $138 per kg lost. They argue their results indicate cost effectiveness but refrain from giving a concluding statement, due to concerns around the appropriateness of the comparator [there was no ‘true’ control group as both arms received the same core weight loss programme, with the intervention arm receiving a further 12 maintenance sessions]. Mean weight loss was higher in the ABA intervention than a real world setting comparison, based on literature values (an intervention causing an additional 2.1 kg weight loss compared to control) [ 39 ]. The authors report challenges to overcoming the lack of intervention comparator through utilising literature values, emphasising that in previous literature costs and outcomes were not reported separately by race: “Given blacks typically loose less weight than white in behavioural weight loss interventions, cost per pound lost may be considerably higher among blacks” (P.2, [ 39 ]).
Overall, three papers, representing two ABAs explicitly, report that interventions were well received/ enjoyed/ appreciated by participants, noting them as highly valued or increasing confidence both during intervention participation and beyond ( n = 3: n IRC = 1 [ 36 ], n IRHSC = 1 [ 34 ], n EE = 1 [ 37 ]). No paper reported this using formal research methods – either qualitatively or through metrics – rather relying on informal research observations. The same studies explicitly mention good engagement and ‘buy-in’ from ABA facilitators.
ABAs in principle seem desirable given pressure to reduce demand on public services and find ways to mitigate inequalities. However, the economic literature about them is extremely limited. A high proportion of included studies suggest that ABAs are cost-effective, a result potentially subject to publication bias, whereby only evidence from ABAs with positive economic findings are published, skewing the published evidence base. If present, as time progresses, publication bias becomes increasingly concerning as “in the presence of publication bias, belief in the relationship increases iteratively with each positive publication” (P.150, [ 45 ]). However, with this important caution in mind, we observed: all included ABAs claimed to successfully target and engage underserved, minority or vulnerable populations; such claims would be better substantiated with more formalised capture of participant socioeconomic status. Among the included papers, methods varied, not only in design and comparators, but also in terms of included costs, and outcome measures, likely reflecting the broad scope of ABAs. The prescriptive nature of economic evaluation frameworks may constrain ABA evaluation. Short comings were noted, in both undervaluing of health and wellbeing outcomes, the impact on those beyond the main intervention recipients and short term (time horizon) follow-up of the evaluation.
While studies claimed engagement of underserved populations, none formally reported measured socioeconomic status of participants. Whilst target populations may be assumed, or considered, marginalised, underserved, or residents of more deprived localities, inequality could be better assessed through measurement of socioeconomic status (e.g. income level) or deprivation [e.g. in the UK postcodes (a series alphanumeric characters denoting geographical area used within postal addresses) can be used as a proxy measure for socioeconomic status using established datasets e.g. Index of Multiple Deprivation]. For example, it cannot be known if the more affluent community members (or people who travelling from other more affluent communities) were attending these groups, potentially subverting the ABA aim of engaging the most deprived or marginalised. The importance of this concern will vary by community: if every community member is considered ‘deprived’, engaging any member may be of value. Given the equity improvement focus, more information about the communities in which the ABAs are delivered may help further inform implementation. Reporting of these factors is needed to meaningfully value and prioritise ABAs as a whole and assess their position in inequality improvement – particularly in the context of scare public sector resources. In isolation, ABAs may not fully solve problems of engagement of the underserved but may go some way to resolving them.
Careful consideration should be given to the contextual appropriateness of ABAs. ABAs are useful as they utilise existing resources and can effectively engage people not normally reached. However, it presumes that localities have resources upon which to build. Thus, inequalities may be perpetuated were ABAs to be utilised exclusively: communities short of assets may continue to receive no additional interventions. Thus, exclusively relying on ABAs may perpetuate some inequalities. Perhaps, optimally, one might consider ABAs as one ‘tool’ within a wider ‘toolkit’ of approaches for engaging underserved individuals.
Health outcomes were measured within all publications. Ellis-Hill 2019 [ 34 ] explored outcome measures for a larger trial and was the only study to include holistic capability measures (e.g. WEMWBS or ICECAP-A). The authors concluded that measures of emotional well-being would be the most relevant study outcome. This adds evidence to the argument that health specific measures (e.g. QALYs) may not fully capture benefits in this setting – ABAs may be better evaluated using more generic measures of wellbeing. Three studies also explicitly reported improvements in participant ‘ enjoyment’ , yet this was not measured, in any capacity, within the utilised costing frameworks. Consequences of social gain (e.g. increasing social confidence to support future engagement or gaining knowledge of services through naturalistic conversations) and emotional well-being improvements should also be considered – holistic capability measures may capture some of these effects.
In ABA evaluation, costs and time horizon need to be carefully considered. Where set-up and training costs are included in intervention delivery costings, ABAs may be disadvantaged if they are compared over short time horizons (1–2 years) – it may be better to consider them one-off set-up costs. However, costing should consider costs of training new staff, maintaining staff, and other ongoing costs – sensitivity analyses may be useful for exploring such points. Further, short time horizons made evidencing long-term impact, and subsequent costs, challenging.
A general challenge of evaluations of preventative or complex interventions, also evidenced here, is capturing the wider life course benefit accrued from engagement with behaviour change interventions. Without a complete retrospective dataset, with a large sample size and an appropriate comparator, it is challenging to definitively assess the impact of such interventions. It is also unknown what would have happened in the absence of the intervention. In some instances (e.g. [ 31 ] and [ 42 ]), authors made attempts to overcome this by utilising established behaviour change models in their evaluations, including sensitivity analysis to understand the impact of adopted assumptions. However, these models may undervalue ABA contributions if benefits are valued on their contribution/ outcome in the general population (c.f. the earlier consideration of differing weight loss value in white versus black populations).
A key ABA feature, building community capacity, was not captured in costing evaluation frameworks. Given employment is recognised as a ‘social determinant of health’ and a key influencer on overall personal wellbeing, upskilling staff and the wider community, it may well have consequences beyond the intervention focus [ 46 , 47 ]. Building capacity among staff may offer improved employment opportunities—increasing income—positively contributing to staff’s social determinates of health, potentially reducing their use of health and wellbeing services. However, unmentioned in any included study, is how this may contribute to staff-turnover, perhaps increasing recruitment and training costs.
Relatedly, ABAs are also undervalued where ‘spill over’ effects are not considered, which is of concern since ABAs often impact beyond intervention recipients (e.g. information is shared beyond the sample population to others in the target population or capacity is built among asset staff). Economic evaluation frameworks typically capture the intervention impact on the group of participating individuals. Social return on investment [a “…performance measure similar to ‘return on investment’ but takes a broader societal perspective to valuing cost and benefits. Social and environmental factors are considered, in addition to economic variables to estimate benefit and cost” [ 48 ]] may be better suited to captured the wider social and environmental benefits of the intervention, including benefits of building capacity among staff.
Another overlooked cost includes failed engagement of assets – approaching a community asset for an ABA, possibly even developing a unique approach to match their space, population needs, staffing etc., and the proposed intervention not commencing. Publication bias likely plays a role here – if the intervention does not commence, then there is little to evaluate and report/publish. Such costs should be considered to ensure realistic and appropriate costing of ABA implementation.
Among the identified studies assessing cost-effectiveness, in all but one [ 38 ] ABAs were found to be cost-effective, either delivering benefits at a lower cost than an alternative or accruing additional benefits at an acceptable additional cost. However, authors acknowledge the robustness of these conclusions was diminished by the appropriateness of utilised comparators. Inherent to ABA interventions are engaging specific populations, linked to an existing asset in a specific localised area. Consequently, randomisation options are significantly impacted: individual level randomisation will often be infeasible. Therefore, outcome comparisons may be confounded by factors such as population differences. This may be alleviated in part by using analysis that adjusts for such differences: for example, when comparing outcomes between those engaging and not engaging in the intervention, it may be wise to adjust for inclination to engage with services, as discussed in Mayer 2010 [ 32 ]. However, this can only address known and measured confounders. Some studies utilised a comparison between participant and non-participants (e.g. [ 32 ]): however, the validity of this design may be decreased with some ABA interventions, where ‘participation’ may not always be clear-cut (for example in information sharing interventions) – statistical contamination may occur between comparison groups.
Some evaluations had no comparator. Among these, some sought to compare outcomes to values from literature to demonstrate beneficial impacts. However, two studies noted they were inhibited from doing so because of a lack of relevant literature. This reinforces the more general consideration of the need for improved representation of underserved populations in literature. This general goal may be supported through disaggregating study data by population group (e.g. sub-group analysis).
Some ABAs promote access to other health and wellbeing improvement services, employment, and job services. From the current evidence base it is unclear whether ABA participation does indeed support access to secondary services. A key motivation for utilising ABAs is to help people from disengaged populations to take preventative action, potentially reducing their future use of other health and social care resources. By failing to measure the impact on wider health and wellbeing services, the value of ABAs may be either i) grossly undervalued or ii) missing costly impacts on wider services. Such considerations are also impacted by the adopted time horizon: health and social service costs may rise in the short term (e.g. increased use of screening services).
As the emphasis on community intervention grows, ABAs, and their economic evidence, should be contextualised to the current economic and political climate. For example, the publication gap 2020–23 may be a consequence of the COVID-19 pandemic. Community assets suffered because of government-imposed restrictions preventing in-person gatherings, diminishing community participation. As we move toward to a post lockdown era, entering a cost-of-living crisis, there is significantly higher demand on community assets (such as libraries or foodbanks). Consequently, adopting an ABA and ‘asking’ more of community assets should be considered with caution. For example, in a number of the ABAs evaluated, there was no mention of venue or room hire costs; with current rising costs, the ability of assets to ‘absorb’ increased costs (e.g. hiring a room for longer to deliver a ABA) is likely significantly reduced. Consequently, policy makers should consider if it is sustainable, or indeed ethical, to ‘push’ the responsibility of ABAs on to already stretched assets.
In conducting this review, we found many of the excluded screened papers made mention of ABAs being ‘economically efficient’ without formally evaluating this domain. It is important such claims are validated with evidence, so that the reality of implementation is known. Further, publications generally lacked details on implementation strategies, resulting in the possible exclusion of some papers which may have been an ABA. As the weight of evidence of community intervention increases, implementation strategies should be routinely reported, and consistent terminology employed. This allows for an inference of community impact, in the instances where economic impact fails to fully capture the contextualised social value .
Conclusions
Economic literature on ABAs is extremely limited. ABAs seem to be a promising way to successfully target and engage underserved, minority or vulnerable populations, and may not result in a higher net cost when compared to other approaches to health and wellbeing improvement. The included ABAs represent a broad range of approaches, with methods of evaluation varying widely, not only in design and comparators, but also in terms of included costs, and outcome measures. The current use of economic evaluation methodologies do not capture well the full impacts of ABAs, likely both undervaluing health and wellbeing outcomes (i.e. capacity building, holistic health improvements, increased secondary health and wellbeing service use, and long-term impact on health) and staff capacity building, as well as underestimating delivery costs (i.e. venue higher and failed asset engagement). Current economic evidence struggles due to lack of appropriate intervention comparator, made challenging by the hyper-local nature of ABAs.
In health economics generally, interventions are typically considered as mutually exclusive occurrences, however in the context of community health, and specifically ABAs, this approach typically misses the economic reality of embedding services. The economics of the surrounding services, mechanisms of information sharing, and collaboration underpin the success of assets and ABAs. The economic evidence, and evaluations in general, would benefit from further detail to help ensure more nuanced and sophisticated application of ABAs. Further evidence is needed to determine the cost-effectiveness of ABAs.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
ICEpop CAPability measure for adults.
Warwick-Edinburgh Mental Well-being Scale.
Hospital Anxiety and Depression Scale.
Rosenberg Self-Esteem Scale.
Medical Outcomes Short Form Health Survey.
Head Injury Semantic Differential Scale.
Abbreviations
Asset-based approaches
Critical Appraisal Skills Programme
Cochrane Centre Register of Controlled Trials
Community Health Workers
- Economic evaluation
East of England
EuroQol five dimension questionnaire
Hospital Anxiety and Depression Scale
Head Injury Semantic Differential Scale
ICEpop CAPability measure for adults
National Health Service
Patient Health Questionnaire – 9
Patient and public involvement
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Quality adjusted life-years
Rosenberg Self-Esteem Scale
Medical Outcomes Short Form Health Survey
Wellbeing adjusted life years
Warwick-Edinburgh Mental Well-being Scale
Alderwick H, Dunn P, Mckenna H, Walsh N, Ham C. Sustainability and transformational plan in the NHS: How are they being developed in practice? [report]. The King's Fund; 2016. Available from: https://www.kingsfund.org.uk/insight-and-analysis/reports/stps-in-the-nhs .
Van Tine B, Nuwan Darshana W, Antony M, Steven M. Health assets in a global context: a systematic review of the literature. BMJ Open. 2019;9(2):e023810.
Article Google Scholar
Brooks F, Kendall S. Making sense of assets: what can an assets based approach offer public health? Crit Public Health. 2013;23(2):127–30.
Morgan A, Ziglio E. Revitalising the evidence base for public health: an assets model. Promot Educ. 2007;Suppl 2:17–22.
Article PubMed Google Scholar
Baker D. Developing and implementing a robust asset-based approach to public health. Perspect Public Health. 2014;134(3):129–30.
NHS. About the NHS Long Term Plan. 2019. Available from: https://www.longtermplan.nhs.uk/about/ .
Google Scholar
Scottish community development centre. Asset Based Approaches. 2019. Available from: https://www.scdc.org.uk/what/assets-scotland .
Scottish Public Health Observatory. Assets Public Health Infromation for Scotland. 2019. Available from: https://www.scotpho.org.uk/life-circumstances/assets . Updated 24 October 29.
Morgan A, Ziglio E. Revitalising the evidence base for public health: an assets model. Promot Educ. 2007;14(2_suppl):17–22.
Community Development Practice Hub. ABCD Institue Chicago USA. 2021. Available from: https://www.bvsc.org/abcd-institute-chicago-usa .
Glasgow Centre for Population Health. Putting asset based approaches into practice: identification, mobilisation and measurement of assests [report]. Glasgow; 2012. Available from: https://www.gcph.co.uk/publications/362_concepts_series_10-putting_asset_based_approaches_into_practice .
Hanson S, Jones A. A spatial equity analysis of a publuc health intervention: a case study of an outdoor walking group provider within local authorities in England. Int J Equity Health. 2015;14:106.
Article PubMed PubMed Central Google Scholar
Acheson D. Independent Inquiry into Inequalities in Health Report. 1998.
Rippon S, Hopkin T. Head, hands and heart: asset-based approaches in health care [report]. London: The Health Foundation; 2015. Available from: https://www.health.org.uk/publications/head-hands-and-heart-assetbased-approaches-in-health-care .
Rippon S, South J. Promoting Asset Based Approaches for Health and Wellbeing: Exploring a Theory of Change and Challenges in Evaluation [report]. Leeds: Leeds Beckett; 2017. Available from: https://eprints.leedsbeckett.ac.uk/id/eprint/4497/ .
Herlitz L, Macintyre H, Osborn T, Bonell C. The sustainability of public health interventions in schools: a systematic review. Implement Sci. 2020;15(1):4.
Zaza S, Briss P, Harris K. Understanding and using economic evidence. Task Force on Community Service: the Guide to Community Prevention Services, What Works to Promote Health? New York: Oxford University Press; 2005. p. 449–63.
Payne K, McAllister M, Davies LM. Valuing the economic benefits of complex interventions: when Maximising health is not sufficient. Health Econ. 2013;22(3):258–71.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;74:n2061.
Johnson R, Jenkinson D, Stinton C, Taylor-Phillips S, Madan J, Stewart-Brown S, et al. Where’s WALY? : A proof of concept study of the ‘wellbeing adjusted life year’ using secondary analysis of cross-sectional survey data. Health Qual Life Outcomes. 2016;14(1):126.
Brazier J, Ratcliffe J, Saloman J, Tsuchiya A. Measuring and Valuing Health Benefits for Economic Evaluation. 2nd ed. Oxford University Pres; 2016.
Book Google Scholar
Wildman J, McMeekin P, Grieve E, Briggs A. Economic evaluation of integrated new technologies for health and social care: Suggestions for policy makers, users and evaluators. Soc Sci Med. 2016;169:141–8.
Byford S, Raftery J. Perspectives in economic evaluation. BMJ. 1998;316(7143):1529–30.
Article CAS PubMed PubMed Central Google Scholar
Baltussen R, Marsh K, Thokala P, Diaby V, Castro H, Cleemput I, et al. Multicriteria Decision Analysis to Support Health Technology Assessment Agencies: Benefits, Limitations, and the Way Forward. Value in Health. 2019;22(11):1283–8.
Cookson R, Drummond M, Weatherly H. Explicit incorporation of equity considerations into economic evaluation of public health interventions. Health Econ Policy Law. 2009;4(2):231–45.
Edwards RT, Charles JM, Lloyd-Williams H. Public health economics: a systematic review of guidance for the economic evaluation of public health interventions and discussion of key methodological issues. BMC Public Health. 2013;13(1):1001.
Lindholm LA, Emmelin MA, Rosén ME. Health maximization rejected: the view of Swedish politicians. Eur J Public Health. 1997;7(4):405–10.
Kocot E, Kotarba P, Dubas-Jakóbczyk K. The application of the QALY measure in the assessment of the effects of health interventions on an older population: a systematic scoping review. Arch Public Health. 2021;79(1):201.
Moher D LA, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009;6:e1000097.
Critical Appraisal Skills Programme. CASP Checklist; 2019. Available from: https://casp-uk.net/referencing/ .
Kahn JG, Kegeles SM, Hays R, Beltzer N. Cost-effectiveness of the Mpowerment Project, a community-level intervention for young gay men. J Acquir Immune Defic Syndr. 2001;27(5):482–91.
Article CAS PubMed Google Scholar
Mayer C, Williams B, Wagner EH, LoGerfo JP, Cheadle A, Phelan EA. Health care costs and participation in a community-based health promotion program for older adults. Prev Chronic Dis. 2010;7(2):A38.
PubMed PubMed Central Google Scholar
Eckermann S, Dawber J, Yeatman H, Quinsey K, Morris D. Evaluating return on investment in a school based health promotion and prevention program: the investment multiplier for the Stephanie Alexander Kitchen Garden National Program. Soc Sci Med. 2014;114:103–12.
Ellis-Hill C, Thomas S, Gracey F, Lamont-Robinson C, Cant R, Marques EMR, et al. HeART of Stroke: randomised controlled, parallel-arm, feasibility study of a community-based arts and health intervention plus usual care compared with usual care to increase psychological well-being in people following a stroke. BMJ Open. 2019;9(3):e021098.
Krukowski RA, Pope RA, Love S, Lensing S, Felix HC, Prewitt TE, et al. Examination of costs for a lay health educator-delivered translation of the Diabetes Prevention Program in senior centers. Prev Med. 2013;57(4):400–2.
Gitlin LN, Harris LF, McCoy M, Chernett NL, Jutkowitz E, Pizzi LT. A community-integrated home based depression intervention for older African Americans: [corrected] description of the Beat the Blues randomized trial and intervention costs. BMC Geriatr. 2012;12:4.
Pizzi LT, Jutkowitz E, Frick KD, Suh DC, Prioli KM, Gitlin LN. Cost-effectiveness of a community-integrated home-based depression intervention in older African Americans. J Am Geriatr Soc. 2014;62(12):2288–95.
Chung B, Ong M, Ettner SL, Jones F, Gilmore J, McCreary M, et al. 12-Month cost outcomes of community engagement versus technical assistance for depression quality improvement: a partnered, cluster randomized, comparative-effectiveness trial. Ethn Dis. 2018;28(Suppl 2):349–56.
Yeary KHK, Kaplan CM, Hutchins E. Implementation costs of a community health worker delivered weight loss intervention in black churches serving underserved communities. Prev Med Rep. 2020;18:101084-.
Stevens W, Thorogood M, Kayikki S. Cost-effectiveness of a community anti-smoking campaign targeted at a high risk group in London. Health Promot Int. 2002;17(1):43–50.
Wingate L, Graffy J, Holman D, Simmons D. Can peer support be cost saving? An economic evaluation of RAPSID: a randomized controlled trial of peer support in diabetes compared to usual care alone in East of England communities. BMJ Open Diabetes Res Care. 2017;5(1):e000328.
Visram S, Walton N, Akhter N, Lewis S, Lister G. Assessing the value for money of an integrated health and wellbeing service in the UK. Soc Sci Med. 2020;245:112661.
York Health Economics Consortium. Dominance; 2016. Available from: https://yhec.co.uk/glossary/dominance/ .
York Health Economics Consortium. Cost-Effectiveness Threshold York. 2016. Available from: https://yhec.co.uk/glossary/cost-effectiveness-threshold/ .
Joober R, Schmitz N, Annable L, Boksa P. Publication bias: what are the challenges and can they be overcome? J Psychiatry Neurosci. 2012;37(3):149–52.
Armenti K, Sweeney MH, Lingwall C, Yang L. Work: a social determinant of health worth capturing. Int J Environ Res Public Health. 2023;20(2):1199.
Office for National Statistics. What matters most to personal well-being? 2013. Available from: https://webarchive.nationalarchives.gov.uk/ukgwa/20160107113217/http:/www.ons.gov.uk/ons/rel/wellbeing/measuring-national-well-being/what-matters-most-to-personal-well-being-in-the-uk-/sty-personal-well-being.html .
York Health Economics Consortium. Social Return on Investment. 2016. Available from: https://yhec.co.uk/glossary/social-return-on-investment/ .
Download references
Acknowledgements
Dr. Rory Cameron. University of East Anglia
Dr. Jurgen Grotz, University of East Anglia
Dr. Guy Peryer. University of East Anglia
Helen Risebro, University of East Anglia
Nadia Jones, Local Authority Stakeholder
This study is funded by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration East of England (NIHR ARC EoE) at Cambridgeshire and Peterborough NHS Foundation Trust. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
LB's time was supported by the NIHR Applied Research Collaboration East of England Inclusive Involvement in Practice-led Research theme.
Author information
Authors and affiliations.
University of East Anglia, Norwich, UK
Alice Wreford, Linda Birt, Jennifer A. Whitty, Sarah Hanson & Adam P. Wagner
NIHR Applied Research Collaboration (ARC) East of England (EoE) Health Economics and Prioritisation in Health and Social Care Theme, Cambridge, UK
Alice Wreford & Adam P. Wagner
School of Healthcare, University of Leicester, Leicester, UK
Evidera, The Ark, 2nd floor, 201 Talgarth Road, London, W6 8BJ, UK
Jennifer A. Whitty
Healthwatch Suffolk, Ipswich, UK
Susan Conquer
You can also search for this author in PubMed Google Scholar
Contributions
AW acted as the main contributor on this review, contributing to and leading on each stage. LB contributed to the conception and design of the review, as well as the identification of papers, analysis, and revisions to the manuscript. JW and SH contributed to the design, methods and revisions on the manuscript. JW also supported paper identification by resolving conflicts. SC, acted as PPI, contributing to the conception, design, data extraction and interpretation of data. APW closely supervised AW on each stage of this project, acting as a major contributor to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Alice Wreford .
Ethics declarations
Consent for publication.
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wreford, A., Birt, L., Whitty, J.A. et al. Cost and economic evidence for asset-based approaches to health improvement and their evaluation methods: a systematic review. BMC Public Health 24 , 814 (2024). https://doi.org/10.1186/s12889-024-18231-4
Download citation
Received : 30 October 2023
Accepted : 28 February 2024
Published : 15 March 2024
DOI : https://doi.org/10.1186/s12889-024-18231-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Community development
- Social connection
- Marginalised
- Inequalities
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
End the Phone-Based Childhood Now
The environment in which kids grow up today is hostile to human development.

Listen to this article
Produced by ElevenLabs and News Over Audio (NOA) using AI narration.
This article was featured in the One Story to Read Today newsletter. Sign up for it here .
S omething went suddenly and horribly wrong for adolescents in the early 2010s. By now you’ve likely seen the statistics : Rates of depression and anxiety in the United States—fairly stable in the 2000s—rose by more than 50 percent in many studies from 2010 to 2019. The suicide rate rose 48 percent for adolescents ages 10 to 19. For girls ages 10 to 14, it rose 131 percent.
The problem was not limited to the U.S.: Similar patterns emerged around the same time in Canada, the U.K., Australia, New Zealand , the Nordic countries , and beyond . By a variety of measures and in a variety of countries, the members of Generation Z (born in and after 1996) are suffering from anxiety, depression, self-harm, and related disorders at levels higher than any other generation for which we have data.
The decline in mental health is just one of many signs that something went awry. Loneliness and friendlessness among American teens began to surge around 2012. Academic achievement went down, too. According to “The Nation’s Report Card,” scores in reading and math began to decline for U.S. students after 2012, reversing decades of slow but generally steady increase. PISA, the major international measure of educational trends, shows that declines in math, reading, and science happened globally, also beginning in the early 2010s.
Read: It sure looks like phones are making students dumber
As the oldest members of Gen Z reach their late 20s, their troubles are carrying over into adulthood. Young adults are dating less , having less sex, and showing less interest in ever having children than prior generations. They are more likely to live with their parents. They were less likely to get jobs as teens , and managers say they are harder to work with. Many of these trends began with earlier generations, but most of them accelerated with Gen Z.
Surveys show that members of Gen Z are shyer and more risk averse than previous generations, too, and risk aversion may make them less ambitious. In an interview last May , OpenAI co-founder Sam Altman and Stripe co-founder Patrick Collison noted that, for the first time since the 1970s, none of Silicon Valley’s preeminent entrepreneurs are under 30. “Something has really gone wrong,” Altman said. In a famously young industry, he was baffled by the sudden absence of great founders in their 20s.
Generations are not monolithic, of course. Many young people are flourishing. Taken as a whole, however, Gen Z is in poor mental health and is lagging behind previous generations on many important metrics. And if a generation is doing poorly––if it is more anxious and depressed and is starting families, careers, and important companies at a substantially lower rate than previous generations––then the sociological and economic consequences will be profound for the entire society.
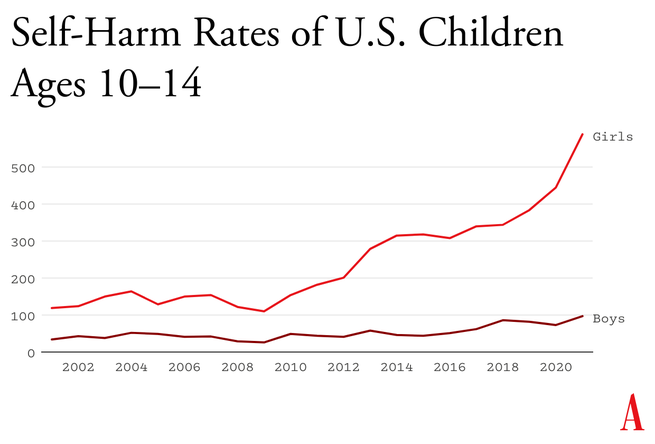
What happened in the early 2010s that altered adolescent development and worsened mental health? Theories abound , but the fact that similar trends are found in many countries worldwide means that events and trends that are specific to the United States cannot be the main story.
I think the answer can be stated simply, although the underlying psychology is complex: Those were the years when adolescents in rich countries traded in their flip phones for smartphones and moved much more of their social lives online—particularly onto social-media platforms designed for virality and addiction . Once young people began carrying the entire internet in their pockets, available to them day and night, it altered their daily experiences and developmental pathways across the board. Friendship, dating, sexuality, exercise, sleep, academics, politics, family dynamics, identity—all were affected. Life changed rapidly for younger children, too, as they began to get access to their parents’ smartphones and, later, got their own iPads, laptops, and even smartphones during elementary school.
Jonathan Haidt: Get phones out of schools now
As a social psychologist who has long studied social and moral development, I have been involved in debates about the effects of digital technology for years. Typically, the scientific questions have been framed somewhat narrowly, to make them easier to address with data. For example, do adolescents who consume more social media have higher levels of depression? Does using a smartphone just before bedtime interfere with sleep? The answer to these questions is usually found to be yes, although the size of the relationship is often statistically small, which has led some researchers to conclude that these new technologies are not responsible for the gigantic increases in mental illness that began in the early 2010s.
But before we can evaluate the evidence on any one potential avenue of harm, we need to step back and ask a broader question: What is childhood––including adolescence––and how did it change when smartphones moved to the center of it? If we take a more holistic view of what childhood is and what young children, tweens, and teens need to do to mature into competent adults, the picture becomes much clearer. Smartphone-based life, it turns out, alters or interferes with a great number of developmental processes.
The intrusion of smartphones and social media are not the only changes that have deformed childhood. There’s an important backstory, beginning as long ago as the 1980s, when we started systematically depriving children and adolescents of freedom, unsupervised play, responsibility, and opportunities for risk taking, all of which promote competence, maturity, and mental health. But the change in childhood accelerated in the early 2010s, when an already independence-deprived generation was lured into a new virtual universe that seemed safe to parents but in fact is more dangerous, in many respects, than the physical world.
My claim is that the new phone-based childhood that took shape roughly 12 years ago is making young people sick and blocking their progress to flourishing in adulthood. We need a dramatic cultural correction, and we need it now.
Brain development is sometimes said to be “experience-expectant,” because specific parts of the brain show increased plasticity during periods of life when an animal’s brain can “expect” to have certain kinds of experiences. You can see this with baby geese, who will imprint on whatever mother-sized object moves in their vicinity just after they hatch. You can see it with human children, who are able to learn languages quickly and take on the local accent, but only through early puberty; after that, it’s hard to learn a language and sound like a native speaker. There is also some evidence of a sensitive period for cultural learning more generally. Japanese children who spent a few years in California in the 1970s came to feel “American” in their identity and ways of interacting only if they attended American schools for a few years between ages 9 and 15. If they left before age 9, there was no lasting impact. If they didn’t arrive until they were 15, it was too late; they didn’t come to feel American.
Human childhood is an extended cultural apprenticeship with different tasks at different ages all the way through puberty. Once we see it this way, we can identify factors that promote or impede the right kinds of learning at each age. For children of all ages, one of the most powerful drivers of learning is the strong motivation to play. Play is the work of childhood, and all young mammals have the same job: to wire up their brains by playing vigorously and often, practicing the moves and skills they’ll need as adults. Kittens will play-pounce on anything that looks like a mouse tail. Human children will play games such as tag and sharks and minnows, which let them practice both their predator skills and their escaping-from-predator skills. Adolescents will play sports with greater intensity, and will incorporate playfulness into their social interactions—flirting, teasing, and developing inside jokes that bond friends together. Hundreds of studies on young rats, monkeys, and humans show that young mammals want to play, need to play, and end up socially, cognitively, and emotionally impaired when they are deprived of play .
One crucial aspect of play is physical risk taking. Children and adolescents must take risks and fail—often—in environments in which failure is not very costly. This is how they extend their abilities, overcome their fears, learn to estimate risk, and learn to cooperate in order to take on larger challenges later. The ever-present possibility of getting hurt while running around, exploring, play-fighting, or getting into a real conflict with another group adds an element of thrill, and thrilling play appears to be the most effective kind for overcoming childhood anxieties and building social, emotional, and physical competence. The desire for risk and thrill increases in the teen years, when failure might carry more serious consequences. Children of all ages need to choose the risk they are ready for at a given moment. Young people who are deprived of opportunities for risk taking and independent exploration will, on average, develop into more anxious and risk-averse adults .
From the April 2014 issue: The overprotected kid
Human childhood and adolescence evolved outdoors, in a physical world full of dangers and opportunities. Its central activities––play, exploration, and intense socializing––were largely unsupervised by adults, allowing children to make their own choices, resolve their own conflicts, and take care of one another. Shared adventures and shared adversity bound young people together into strong friendship clusters within which they mastered the social dynamics of small groups, which prepared them to master bigger challenges and larger groups later on.
And then we changed childhood.
The changes started slowly in the late 1970s and ’80s, before the arrival of the internet, as many parents in the U.S. grew fearful that their children would be harmed or abducted if left unsupervised. Such crimes have always been extremely rare, but they loomed larger in parents’ minds thanks in part to rising levels of street crime combined with the arrival of cable TV, which enabled round-the-clock coverage of missing-children cases. A general decline in social capital ––the degree to which people knew and trusted their neighbors and institutions–– exacerbated parental fears . Meanwhile, rising competition for college admissions encouraged more intensive forms of parenting . In the 1990s, American parents began pulling their children indoors or insisting that afternoons be spent in adult-run enrichment activities. Free play, independent exploration, and teen-hangout time declined.
In recent decades, seeing unchaperoned children outdoors has become so novel that when one is spotted in the wild, some adults feel it is their duty to call the police. In 2015, the Pew Research Center found that parents, on average, believed that children should be at least 10 years old to play unsupervised in front of their house, and that kids should be 14 before being allowed to go unsupervised to a public park. Most of these same parents had enjoyed joyous and unsupervised outdoor play by the age of 7 or 8.
But overprotection is only part of the story. The transition away from a more independent childhood was facilitated by steady improvements in digital technology, which made it easier and more inviting for young people to spend a lot more time at home, indoors, and alone in their rooms. Eventually, tech companies got access to children 24/7. They developed exciting virtual activities, engineered for “engagement,” that are nothing like the real-world experiences young brains evolved to expect.

The first wave came ashore in the 1990s with the arrival of dial-up internet access, which made personal computers good for something beyond word processing and basic games. By 2003, 55 percent of American households had a computer with (slow) internet access. Rates of adolescent depression, loneliness, and other measures of poor mental health did not rise in this first wave. If anything, they went down a bit. Millennial teens (born 1981 through 1995), who were the first to go through puberty with access to the internet, were psychologically healthier and happier, on average, than their older siblings or parents in Generation X (born 1965 through 1980).
The second wave began to rise in the 2000s, though its full force didn’t hit until the early 2010s. It began rather innocently with the introduction of social-media platforms that helped people connect with their friends. Posting and sharing content became much easier with sites such as Friendster (launched in 2003), Myspace (2003), and Facebook (2004).
Teens embraced social media soon after it came out, but the time they could spend on these sites was limited in those early years because the sites could only be accessed from a computer, often the family computer in the living room. Young people couldn’t access social media (and the rest of the internet) from the school bus, during class time, or while hanging out with friends outdoors. Many teens in the early-to-mid-2000s had cellphones, but these were basic phones (many of them flip phones) that had no internet access. Typing on them was difficult––they had only number keys. Basic phones were tools that helped Millennials meet up with one another in person or talk with each other one-on-one. I have seen no evidence to suggest that basic cellphones harmed the mental health of Millennials.
It was not until the introduction of the iPhone (2007), the App Store (2008), and high-speed internet (which reached 50 percent of American homes in 2007 )—and the corresponding pivot to mobile made by many providers of social media, video games, and porn—that it became possible for adolescents to spend nearly every waking moment online. The extraordinary synergy among these innovations was what powered the second technological wave. In 2011, only 23 percent of teens had a smartphone. By 2015, that number had risen to 73 percent , and a quarter of teens said they were online “almost constantly.” Their younger siblings in elementary school didn’t usually have their own smartphones, but after its release in 2010, the iPad quickly became a staple of young children’s daily lives. It was in this brief period, from 2010 to 2015, that childhood in America (and many other countries) was rewired into a form that was more sedentary, solitary, virtual, and incompatible with healthy human development.
In the 2000s, Silicon Valley and its world-changing inventions were a source of pride and excitement in America. Smart and ambitious young people around the world wanted to move to the West Coast to be part of the digital revolution. Tech-company founders such as Steve Jobs and Sergey Brin were lauded as gods, or at least as modern Prometheans, bringing humans godlike powers. The Arab Spring bloomed in 2011 with the help of decentralized social platforms, including Twitter and Facebook. When pundits and entrepreneurs talked about the power of social media to transform society, it didn’t sound like a dark prophecy.
You have to put yourself back in this heady time to understand why adults acquiesced so readily to the rapid transformation of childhood. Many parents had concerns , even then, about what their children were doing online, especially because of the internet’s ability to put children in contact with strangers. But there was also a lot of excitement about the upsides of this new digital world. If computers and the internet were the vanguards of progress, and if young people––widely referred to as “digital natives”––were going to live their lives entwined with these technologies, then why not give them a head start? I remember how exciting it was to see my 2-year-old son master the touch-and-swipe interface of my first iPhone in 2008. I thought I could see his neurons being woven together faster as a result of the stimulation it brought to his brain, compared to the passivity of watching television or the slowness of building a block tower. I thought I could see his future job prospects improving.
Touchscreen devices were also a godsend for harried parents. Many of us discovered that we could have peace at a restaurant, on a long car trip, or at home while making dinner or replying to emails if we just gave our children what they most wanted: our smartphones and tablets. We saw that everyone else was doing it and figured it must be okay.
It was the same for older children, desperate to join their friends on social-media platforms, where the minimum age to open an account was set by law to 13, even though no research had been done to establish the safety of these products for minors. Because the platforms did nothing (and still do nothing) to verify the stated age of new-account applicants, any 10-year-old could open multiple accounts without parental permission or knowledge, and many did. Facebook and later Instagram became places where many sixth and seventh graders were hanging out and socializing. If parents did find out about these accounts, it was too late. Nobody wanted their child to be isolated and alone, so parents rarely forced their children to shut down their accounts.
We had no idea what we were doing.
The numbers are hard to believe. The most recent Gallup data show that American teens spend about five hours a day just on social-media platforms (including watching videos on TikTok and YouTube). Add in all the other phone- and screen-based activities, and the number rises to somewhere between seven and nine hours a day, on average . The numbers are even higher in single-parent and low-income families, and among Black, Hispanic, and Native American families.
These very high numbers do not include time spent in front of screens for school or homework, nor do they include all the time adolescents spend paying only partial attention to events in the real world while thinking about what they’re missing on social media or waiting for their phones to ping. Pew reports that in 2022, one-third of teens said they were on one of the major social-media sites “almost constantly,” and nearly half said the same of the internet in general. For these heavy users, nearly every waking hour is an hour absorbed, in full or in part, by their devices.

In Thoreau’s terms, how much of life is exchanged for all this screen time? Arguably, most of it. Everything else in an adolescent’s day must get squeezed down or eliminated entirely to make room for the vast amount of content that is consumed, and for the hundreds of “friends,” “followers,” and other network connections that must be serviced with texts, posts, comments, likes, snaps, and direct messages. I recently surveyed my students at NYU, and most of them reported that the very first thing they do when they open their eyes in the morning is check their texts, direct messages, and social-media feeds. It’s also the last thing they do before they close their eyes at night. And it’s a lot of what they do in between.
The amount of time that adolescents spend sleeping declined in the early 2010s , and many studies tie sleep loss directly to the use of devices around bedtime, particularly when they’re used to scroll through social media . Exercise declined , too, which is unfortunate because exercise, like sleep, improves both mental and physical health. Book reading has been declining for decades, pushed aside by digital alternatives, but the decline, like so much else, sped up in the early 2010 s. With passive entertainment always available, adolescent minds likely wander less than they used to; contemplation and imagination might be placed on the list of things winnowed down or crowded out.
But perhaps the most devastating cost of the new phone-based childhood was the collapse of time spent interacting with other people face-to-face. A study of how Americans spend their time found that, before 2010, young people (ages 15 to 24) reported spending far more time with their friends (about two hours a day, on average, not counting time together at school) than did older people (who spent just 30 to 60 minutes with friends). Time with friends began decreasing for young people in the 2000s, but the drop accelerated in the 2010s, while it barely changed for older people. By 2019, young people’s time with friends had dropped to just 67 minutes a day. It turns out that Gen Z had been socially distancing for many years and had mostly completed the project by the time COVID-19 struck.
Read: What happens when kids don’t see their peers for months
You might question the importance of this decline. After all, isn’t much of this online time spent interacting with friends through texting, social media, and multiplayer video games? Isn’t that just as good?
Some of it surely is, and virtual interactions offer unique benefits too, especially for young people who are geographically or socially isolated. But in general, the virtual world lacks many of the features that make human interactions in the real world nutritious, as we might say, for physical, social, and emotional development. In particular, real-world relationships and social interactions are characterized by four features—typical for hundreds of thousands of years—that online interactions either distort or erase.
First, real-world interactions are embodied , meaning that we use our hands and facial expressions to communicate, and we learn to respond to the body language of others. Virtual interactions, in contrast, mostly rely on language alone. No matter how many emojis are offered as compensation, the elimination of communication channels for which we have eons of evolutionary programming is likely to produce adults who are less comfortable and less skilled at interacting in person.
Second, real-world interactions are synchronous ; they happen at the same time. As a result, we learn subtle cues about timing and conversational turn taking. Synchronous interactions make us feel closer to the other person because that’s what getting “in sync” does. Texts, posts, and many other virtual interactions lack synchrony. There is less real laughter, more room for misinterpretation, and more stress after a comment that gets no immediate response.
Third, real-world interactions primarily involve one‐to‐one communication , or sometimes one-to-several. But many virtual communications are broadcast to a potentially huge audience. Online, each person can engage in dozens of asynchronous interactions in parallel, which interferes with the depth achieved in all of them. The sender’s motivations are different, too: With a large audience, one’s reputation is always on the line; an error or poor performance can damage social standing with large numbers of peers. These communications thus tend to be more performative and anxiety-inducing than one-to-one conversations.
Finally, real-world interactions usually take place within communities that have a high bar for entry and exit , so people are strongly motivated to invest in relationships and repair rifts when they happen. But in many virtual networks, people can easily block others or quit when they are displeased. Relationships within such networks are usually more disposable.
From the September 2015 issue: The coddling of the American mind
These unsatisfying and anxiety-producing features of life online should be recognizable to most adults. Online interactions can bring out antisocial behavior that people would never display in their offline communities. But if life online takes a toll on adults, just imagine what it does to adolescents in the early years of puberty, when their “experience expectant” brains are rewiring based on feedback from their social interactions.
Kids going through puberty online are likely to experience far more social comparison, self-consciousness, public shaming, and chronic anxiety than adolescents in previous generations, which could potentially set developing brains into a habitual state of defensiveness. The brain contains systems that are specialized for approach (when opportunities beckon) and withdrawal (when threats appear or seem likely). People can be in what we might call “discover mode” or “defend mode” at any moment, but generally not both. The two systems together form a mechanism for quickly adapting to changing conditions, like a thermostat that can activate either a heating system or a cooling system as the temperature fluctuates. Some people’s internal thermostats are generally set to discover mode, and they flip into defend mode only when clear threats arise. These people tend to see the world as full of opportunities. They are happier and less anxious. Other people’s internal thermostats are generally set to defend mode, and they flip into discover mode only when they feel unusually safe. They tend to see the world as full of threats and are more prone to anxiety and depressive disorders.
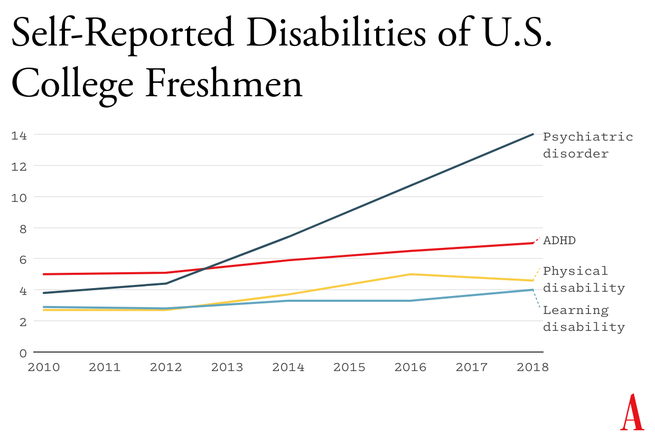
A simple way to understand the differences between Gen Z and previous generations is that people born in and after 1996 have internal thermostats that were shifted toward defend mode. This is why life on college campuses changed so suddenly when Gen Z arrived, beginning around 2014. Students began requesting “safe spaces” and trigger warnings. They were highly sensitive to “microaggressions” and sometimes claimed that words were “violence.” These trends mystified those of us in older generations at the time, but in hindsight, it all makes sense. Gen Z students found words, ideas, and ambiguous social encounters more threatening than had previous generations of students because we had fundamentally altered their psychological development.
Staying on task while sitting at a computer is hard enough for an adult with a fully developed prefrontal cortex. It is far more difficult for adolescents in front of their laptop trying to do homework. They are probably less intrinsically motivated to stay on task. They’re certainly less able, given their undeveloped prefrontal cortex, and hence it’s easy for any company with an app to lure them away with an offer of social validation or entertainment. Their phones are pinging constantly— one study found that the typical adolescent now gets 237 notifications a day, roughly 15 every waking hour. Sustained attention is essential for doing almost anything big, creative, or valuable, yet young people find their attention chopped up into little bits by notifications offering the possibility of high-pleasure, low-effort digital experiences.
It even happens in the classroom. Studies confirm that when students have access to their phones during class time, they use them, especially for texting and checking social media, and their grades and learning suffer . This might explain why benchmark test scores began to decline in the U.S. and around the world in the early 2010s—well before the pandemic hit.
The neural basis of behavioral addiction to social media or video games is not exactly the same as chemical addiction to cocaine or opioids. Nonetheless, they all involve abnormally heavy and sustained activation of dopamine neurons and reward pathways. Over time, the brain adapts to these high levels of dopamine; when the child is not engaged in digital activity, their brain doesn’t have enough dopamine, and the child experiences withdrawal symptoms. These generally include anxiety, insomnia, and intense irritability. Kids with these kinds of behavioral addictions often become surly and aggressive, and withdraw from their families into their bedrooms and devices.
Social-media and gaming platforms were designed to hook users. How successful are they? How many kids suffer from digital addictions?
The main addiction risks for boys seem to be video games and porn. “ Internet gaming disorder ,” which was added to the main diagnosis manual of psychiatry in 2013 as a condition for further study, describes “significant impairment or distress” in several aspects of life, along with many hallmarks of addiction, including an inability to reduce usage despite attempts to do so. Estimates for the prevalence of IGD range from 7 to 15 percent among adolescent boys and young men. As for porn, a nationally representative survey of American adults published in 2019 found that 7 percent of American men agreed or strongly agreed with the statement “I am addicted to pornography”—and the rates were higher for the youngest men.
Girls have much lower rates of addiction to video games and porn, but they use social media more intensely than boys do. A study of teens in 29 nations found that between 5 and 15 percent of adolescents engage in what is called “problematic social media use,” which includes symptoms such as preoccupation, withdrawal symptoms, neglect of other areas of life, and lying to parents and friends about time spent on social media. That study did not break down results by gender, but many others have found that rates of “problematic use” are higher for girls.
Jonathan Haidt: The dangerous experiment on teen girls
I don’t want to overstate the risks: Most teens do not become addicted to their phones and video games. But across multiple studies and across genders, rates of problematic use come out in the ballpark of 5 to 15 percent. Is there any other consumer product that parents would let their children use relatively freely if they knew that something like one in 10 kids would end up with a pattern of habitual and compulsive use that disrupted various domains of life and looked a lot like an addiction?
During that crucial sensitive period for cultural learning, from roughly ages 9 through 15, we should be especially thoughtful about who is socializing our children for adulthood. Instead, that’s when most kids get their first smartphone and sign themselves up (with or without parental permission) to consume rivers of content from random strangers. Much of that content is produced by other adolescents, in blocks of a few minutes or a few seconds.
This rerouting of enculturating content has created a generation that is largely cut off from older generations and, to some extent, from the accumulated wisdom of humankind, including knowledge about how to live a flourishing life. Adolescents spend less time steeped in their local or national culture. They are coming of age in a confusing, placeless, ahistorical maelstrom of 30-second stories curated by algorithms designed to mesmerize them. Without solid knowledge of the past and the filtering of good ideas from bad––a process that plays out over many generations––young people will be more prone to believe whatever terrible ideas become popular around them, which might explain why v ideos showing young people reacting positively to Osama bin Laden’s thoughts about America were trending on TikTok last fall.
All this is made worse by the fact that so much of digital public life is an unending supply of micro dramas about somebody somewhere in our country of 340 million people who did something that can fuel an outrage cycle, only to be pushed aside by the next. It doesn’t add up to anything and leaves behind only a distorted sense of human nature and affairs.
When our public life becomes fragmented, ephemeral, and incomprehensible, it is a recipe for anomie, or normlessness. The great French sociologist Émile Durkheim showed long ago that a society that fails to bind its people together with some shared sense of sacredness and common respect for rules and norms is not a society of great individual freedom; it is, rather, a place where disoriented individuals have difficulty setting goals and exerting themselves to achieve them. Durkheim argued that anomie was a major driver of suicide rates in European countries. Modern scholars continue to draw on his work to understand suicide rates today.
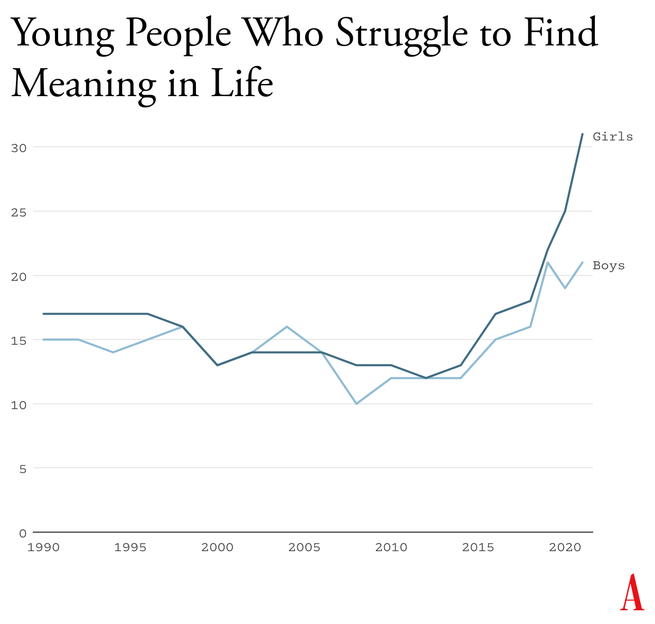
Durkheim’s observations are crucial for understanding what happened in the early 2010s. A long-running survey of American teens found that , from 1990 to 2010, high-school seniors became slightly less likely to agree with statements such as “Life often feels meaningless.” But as soon as they adopted a phone-based life and many began to live in the whirlpool of social media, where no stability can be found, every measure of despair increased. From 2010 to 2019, the number who agreed that their lives felt “meaningless” increased by about 70 percent, to more than one in five.
An additional source of evidence comes from Gen Z itself. With all the talk of regulating social media, raising age limits, and getting phones out of schools, you might expect to find many members of Gen Z writing and speaking out in opposition. I’ve looked for such arguments and found hardly any. In contrast, many young adults tell stories of devastation.
Freya India, a 24-year-old British essayist who writes about girls, explains how social-media sites carry girls off to unhealthy places: “It seems like your child is simply watching some makeup tutorials, following some mental health influencers, or experimenting with their identity. But let me tell you: they are on a conveyor belt to someplace bad. Whatever insecurity or vulnerability they are struggling with, they will be pushed further and further into it.” She continues:
Gen Z were the guinea pigs in this uncontrolled global social experiment. We were the first to have our vulnerabilities and insecurities fed into a machine that magnified and refracted them back at us, all the time, before we had any sense of who we were. We didn’t just grow up with algorithms. They raised us. They rearranged our faces. Shaped our identities. Convinced us we were sick.
Rikki Schlott, a 23-year-old American journalist and co-author of The Canceling of the American Mind , writes ,
The day-to-day life of a typical teen or tween today would be unrecognizable to someone who came of age before the smartphone arrived. Zoomers are spending an average of 9 hours daily in this screen-time doom loop—desperate to forget the gaping holes they’re bleeding out of, even if just for … 9 hours a day. Uncomfortable silence could be time to ponder why they’re so miserable in the first place. Drowning it out with algorithmic white noise is far easier.
A 27-year-old man who spent his adolescent years addicted (his word) to video games and pornography sent me this reflection on what that did to him:
I missed out on a lot of stuff in life—a lot of socialization. I feel the effects now: meeting new people, talking to people. I feel that my interactions are not as smooth and fluid as I want. My knowledge of the world (geography, politics, etc.) is lacking. I didn’t spend time having conversations or learning about sports. I often feel like a hollow operating system.
Or consider what Facebook found in a research project involving focus groups of young people, revealed in 2021 by the whistleblower Frances Haugen: “Teens blame Instagram for increases in the rates of anxiety and depression among teens,” an internal document said. “This reaction was unprompted and consistent across all groups.”
How can it be that an entire generation is hooked on consumer products that so few praise and so many ultimately regret using? Because smartphones and especially social media have put members of Gen Z and their parents into a series of collective-action traps. Once you understand the dynamics of these traps, the escape routes become clear.

Social media, in contrast, applies a lot more pressure on nonusers, at a much younger age and in a more insidious way. Once a few students in any middle school lie about their age and open accounts at age 11 or 12, they start posting photos and comments about themselves and other students. Drama ensues. The pressure on everyone else to join becomes intense. Even a girl who knows, consciously, that Instagram can foster beauty obsession, anxiety, and eating disorders might sooner take those risks than accept the seeming certainty of being out of the loop, clueless, and excluded. And indeed, if she resists while most of her classmates do not, she might, in fact, be marginalized, which puts her at risk for anxiety and depression, though via a different pathway than the one taken by those who use social media heavily. In this way, social media accomplishes a remarkable feat: It even harms adolescents who do not use it.
From the May 2022 issue: Jonathan Haidt on why the past 10 years of American life have been uniquely stupid
A recent study led by the University of Chicago economist Leonardo Bursztyn captured the dynamics of the social-media trap precisely. The researchers recruited more than 1,000 college students and asked them how much they’d need to be paid to deactivate their accounts on either Instagram or TikTok for four weeks. That’s a standard economist’s question to try to compute the net value of a product to society. On average, students said they’d need to be paid roughly $50 ($59 for TikTok, $47 for Instagram) to deactivate whichever platform they were asked about. Then the experimenters told the students that they were going to try to get most of the others in their school to deactivate that same platform, offering to pay them to do so as well, and asked, Now how much would you have to be paid to deactivate, if most others did so? The answer, on average, was less than zero. In each case, most students were willing to pay to have that happen.
Social media is all about network effects. Most students are only on it because everyone else is too. Most of them would prefer that nobody be on these platforms. Later in the study, students were asked directly, “Would you prefer to live in a world without Instagram [or TikTok]?” A majority of students said yes––58 percent for each app.
This is the textbook definition of what social scientists call a collective-action problem . It’s what happens when a group would be better off if everyone in the group took a particular action, but each actor is deterred from acting, because unless the others do the same, the personal cost outweighs the benefit. Fishermen considering limiting their catch to avoid wiping out the local fish population are caught in this same kind of trap. If no one else does it too, they just lose profit.
Cigarettes trapped individual smokers with a biological addiction. Social media has trapped an entire generation in a collective-action problem. Early app developers deliberately and knowingly exploited the psychological weaknesses and insecurities of young people to pressure them to consume a product that, upon reflection, many wish they could use less, or not at all.
The trap here is that each child thinks they need a smartphone because “everyone else” has one, and many parents give in because they don’t want their child to feel excluded. But if no one else had a smartphone—or even if, say, only half of the child’s sixth-grade class had one—parents would feel more comfortable providing a basic flip phone (or no phone at all). Delaying round-the-clock internet access until ninth grade (around age 14) as a national or community norm would help to protect adolescents during the very vulnerable first few years of puberty. According to a 2022 British study , these are the years when social-media use is most correlated with poor mental health. Family policies about tablets, laptops, and video-game consoles should be aligned with smartphone restrictions to prevent overuse of other screen activities.
The trap here, as with smartphones, is that each adolescent feels a strong need to open accounts on TikTok, Instagram, Snapchat, and other platforms primarily because that’s where most of their peers are posting and gossiping. But if the majority of adolescents were not on these accounts until they were 16, families and adolescents could more easily resist the pressure to sign up. The delay would not mean that kids younger than 16 could never watch videos on TikTok or YouTube—only that they could not open accounts, give away their data, post their own content, and let algorithms get to know them and their preferences.
Most schools claim that they ban phones, but this usually just means that students aren’t supposed to take their phone out of their pocket during class. Research shows that most students do use their phones during class time. They also use them during lunchtime, free periods, and breaks between classes––times when students could and should be interacting with their classmates face-to-face. The only way to get students’ minds off their phones during the school day is to require all students to put their phones (and other devices that can send or receive texts) into a phone locker or locked pouch at the start of the day. Schools that have gone phone-free always seem to report that it has improved the culture, making students more attentive in class and more interactive with one another. Published studies back them up .
Many parents are afraid to give their children the level of independence and responsibility they themselves enjoyed when they were young, even though rates of homicide, drunk driving, and other physical threats to children are way down in recent decades. Part of the fear comes from the fact that parents look at each other to determine what is normal and therefore safe, and they see few examples of families acting as if a 9-year-old can be trusted to walk to a store without a chaperone. But if many parents started sending their children out to play or run errands, then the norms of what is safe and accepted would change quickly. So would ideas about what constitutes “good parenting.” And if more parents trusted their children with more responsibility––for example, by asking their kids to do more to help out, or to care for others––then the pervasive sense of uselessness now found in surveys of high-school students might begin to dissipate.
It would be a mistake to overlook this fourth norm. If parents don’t replace screen time with real-world experiences involving friends and independent activity, then banning devices will feel like deprivation, not the opening up of a world of opportunities.
The main reason why the phone-based childhood is so harmful is because it pushes aside everything else. Smartphones are experience blockers. Our ultimate goal should not be to remove screens entirely, nor should it be to return childhood to exactly the way it was in 1960. Rather, it should be to create a version of childhood and adolescence that keeps young people anchored in the real world while flourishing in the digital age.
In recent decades, however, Congress has not been good at addressing public concerns when the solutions would displease a powerful and deep-pocketed industry. Governors and state legislators have been much more effective, and their successes might let us evaluate how well various reforms work. But the bottom line is that to change norms, we’re going to need to do most of the work ourselves, in neighborhood groups, schools, and other communities.
Read: Why Congress keeps failing to protect kids online
There are now hundreds of organizations––most of them started by mothers who saw what smartphones had done to their children––that are working to roll back the phone-based childhood or promote a more independent, real-world childhood. (I have assembled a list of many of them.) One that I co-founded, at LetGrow.org , suggests a variety of simple programs for parents or schools, such as play club (schools keep the playground open at least one day a week before or after school, and kids sign up for phone-free, mixed-age, unstructured play as a regular weekly activity) and the Let Grow Experience (a series of homework assignments in which students––with their parents’ consent––choose something to do on their own that they’ve never done before, such as walk the dog, climb a tree, walk to a store, or cook dinner).
Even without the help of organizations, parents could break their families out of collective-action traps if they coordinated with the parents of their children’s friends. Together they could create common smartphone rules and organize unsupervised play sessions or encourage hangouts at a home, park, or shopping mall.

P arents are fed up with what childhood has become. Many are tired of having daily arguments about technologies that were designed to grab hold of their children’s attention and not let go. But the phone-based childhood is not inevitable.
We didn’t know what we were doing in the early 2010s. Now we do. It’s time to end the phone-based childhood.
This article is adapted from Jonathan Haidt’s forthcoming book, The Anxious Generation: How the Great Rewiring of Childhood Is Causing an Epidemic of Mental Illness .

When you buy a book using a link on this page, we receive a commission. Thank you for supporting The Atlantic.
The Philippines economy in 2024: Stronger for longer?
The Philippines ended 2023 on a high note, being the fastest growing economy across Southeast Asia with a growth rate of 5.6 percent—just shy of the government's target of 6.0 to 7.0 percent. 1 “National accounts,” Philippine Statistics Authority, January 31, 2024; "Philippine economic updates,” Bangko Sentral ng Pilipinas, November 16, 2023. Should projections hold, the Philippines is expected to, once again, show significant growth in 2024, demonstrating its resilience despite various global economic pressures (Exhibit 1). 2 “Economic forecast 2024,” International Monetary Fund, November 1, 2023; McKinsey analysis.
The growth in the Philippine economy in 2023 was driven by a resumption in commercial activities, public infrastructure spending, and growth in digital financial services. Most sectors grew, with transportation and storage (13 percent), construction (9 percent), and financial services (9 percent), performing the best (Exhibit 2). 3 “National accounts,” Philippine Statistics Authority, January 31, 2024. While the country's trade deficit narrowed in 2023, it remains elevated at $52 billion due to slowing global demand and geopolitical uncertainties. 4 “Highlights of the Philippine export and import statistics,” Philippine Statistics Authority, January 28, 2024. Looking ahead to 2024, the current economic forecast for the Philippines projects a GDP growth of between 5 and 6 percent.
Inflation rates are expected to temper between 3.2 and 3.6 percent in 2024 after ending 2023 at 6.0 percent, above the 2.0 to 4.0 percent target range set by the government. 5 “Nomura downgrades Philippine 2024 growth forecast,” Nomura, September 11, 2023; “IMF raises Philippine growth rate forecast,” International Monetary Fund, July 16, 2023.
For the purposes of this article, most of the statistics used for our analysis have come from a common thread of sources. These include the Central Bank of the Philippines (Bangko Sentral ng Pilipinas); the Department of Energy Philippines; the IT and Business Process Association of the Philippines (IBPAP); and the Philippines Statistics Authority.
The state of the Philippine economy across seven major sectors and themes
In the article, we explore the 2024 outlook for seven key sectors and themes, what may affect each of them in the coming year, and what could potentially unlock continued growth.
Financial services
The recovery of the financial services sector appears on track as year-on-year growth rates stabilize. 6 Philippines Statistics Authority, November 2023; McKinsey in partnership with Oxford Economics, November 2023. In 2024, this sector will likely continue to grow, though at a slower pace of about 5 percent.
Financial inclusion and digitalization are contributing to growth in this sector in 2024, even if new challenges emerge. Various factors are expected to impact this sector:
- Inclusive finance: Bangko Sentral ng Pilipinas continues to invest in financial inclusion initiatives. For example, basic deposit accounts (BDAs) reached $22 million in 2023 and banking penetration improved, with the proportion of adults with formal bank accounts increasing from 29 percent in 2019 to 56 percent in 2021. 7 “Financial inclusion dashboard: First quarter 2023,” Bangko Sentral ng Pilipinas, February 6, 2024.
- Digital adoption: Digital channels are expected to continue to grow, with data showing that 60 percent of adults who have a mobile phone and internet access have done a digital financial transaction. 8 “Financial inclusion dashboard: First quarter 2023,” Bangko Sentral ng Pilipinas, February 6, 2024. Businesses in this sector, however, will need to remain vigilant in navigating cybersecurity and fraud risks.
- Unsecured lending growth: Growth in unsecured lending is expected to continue, but at a slower pace than the past two to three years. For example, unsecured retail lending for the banking system alone grew by 27 percent annually from 2020 to 2022. 9 “Loan accounts: As of first quarter 2023,” Bangko Sentral ng Pilipinas, February 6, 2024; "Global banking pools,” McKinsey, November 2023. Businesses in this field are, however, expected to recalibrate their risk profiling models as segments with high nonperforming loans emerge.
- High interest rates: Key interest rates are expected to decline in the second half of 2024, creating more accommodating borrowing conditions that could boost wholesale and corporate loans.
Supportive frameworks have a pivotal role to play in unlocking growth in this sector to meet the ever-increasing demand from the financially underserved. For example, financial literacy programs and easier-to-access accounts—such as BDAs—are some measures that can help widen market access to financial services. Continued efforts are being made to build an open finance framework that could serve the needs of the unbanked population, as well as a unified credit scoring mechanism to increase the ability of historically under-financed segments, such as small and medium-sized enterprises (SMEs), to access formal credit. 10 “BSP launches credit scoring model,” Bangko Sentral ng Pilipinas, April 26, 2023.
Energy and Power
The outlook for the energy sector seems positive, with the potential to grow by 7 percent in 2024 as the country focuses on renewable energy generation. 11 McKinsey analysis based on input from industry experts. Currently, stakeholders are focused on increasing energy security, particularly on importing liquefied natural gas (LNG) to meet power plants’ requirements as production in one of the country’s main sources of natural gas, the Malampaya gas field, declines. 12 Myrna M. Velasco, “Malampaya gas field prod’n declines steeply in 2021,” Manila Bulletin , July 9, 2022. High global inflation and the fact that the Philippines is a net fuel importer are impacting electricity prices and the build-out of planned renewable energy projects. Recent regulatory moves to remove foreign ownership limits on exploration, development, and utilization of renewable energy resources could possibly accelerate growth in the country’s energy and power sector. 13 “RA 11659,” Department of Energy Philippines, June 8, 2023.
Gas, renewables, and transmission are potential growth drivers for the sector. Upgrading power grids so that they become more flexible and better able to cope with the intermittent electricity supply that comes with renewables will be critical as the sector pivots toward renewable energy. A recent coal moratorium may position natural gas as a transition fuel—this could stimulate exploration and production investments for new, indigenous natural gas fields, gas pipeline infrastructure, and LNG import terminal projects. 14 Philippine energy plan 2020–2040, Department of Energy Philippines, June 10, 2022; Power development plan 2020–2040 , Department of Energy Philippines, 2021. The increasing momentum of green energy auctions could facilitate the development of renewables at scale, as the country targets 35 percent share of renewables by 2030. 15 Power development plan 2020–2040 , 2022.
Growth in the healthcare industry may slow to 2.8 percent in 2024, while pharmaceuticals manufacturing is expected to rebound with 5.2 percent growth in 2024. 16 McKinsey analysis in partnership with Oxford Economics.
Healthcare demand could grow, although the quality of care may be strained as the health worker shortage is projected to increase over the next five years. 17 McKinsey analysis. The supply-and-demand gap in nursing alone is forecast to reach a shortage of approximately 90,000 nurses by 2028. 18 McKinsey analysis. Another compounding factor straining healthcare is the higher than anticipated benefit utilization and rising healthcare costs, which, while helping to meet people's healthcare budgets, may continue to drive down profitability for health insurers.
Meanwhile, pharmaceutical companies are feeling varying effects of people becoming increasingly health conscious. Consumers are using more over the counter (OTC) medication and placing more beneficial value on organic health products, such as vitamins and supplements made from natural ingredients, which could impact demand for prescription drugs. 19 “Consumer health in the Philippines 2023,” Euromonitor, October 2023.
Businesses operating in this field may end up benefiting from universal healthcare policies. If initiatives are implemented that integrate healthcare systems, rationalize copayments, attract and retain talent, and incentivize investments, they could potentially help to strengthen healthcare provision and quality.
Businesses may also need to navigate an increasingly complex landscape of diverse health needs, digitization, and price controls. Digital and data transformations are being seen to facilitate improvements in healthcare delivery and access, with leading digital health apps getting more than one million downloads. 20 Google Play Store, September 27, 2023. Digitization may create an opportunity to develop healthcare ecosystems that unify touchpoints along the patient journey and provide offline-to-online care, as well as potentially realizing cost efficiencies.
Consumer and retail
Growth in the retail and wholesale trade and consumer goods sectors is projected to remain stable in 2024, at 4 percent and 5 percent, respectively.
Inflation, however, continues to put consumers under pressure. While inflation rates may fall—predicted to reach 4 percent in 2024—commodity prices may still remain elevated in the near term, a top concern for Filipinos. 21 “IMF raises Philippine growth forecast,” July 26, 2023; “Nomura downgrades Philippines 2024 growth forecast,” September 11, 2023. In response to challenging economic conditions, 92 percent of consumers have changed their shopping behaviors, and approximately 50 percent indicate that they are switching brands or retail providers in seek of promotions and better prices. 22 “Philippines consumer pulse survey, 2023,” McKinsey, November 2023.
Online shopping has become entrenched in Filipino consumers, as they find that they get access to a wider range of products, can compare prices more easily, and can shop with more convenience. For example, a McKinsey Philippines consumer sentiment survey in 2023 found that 80 percent of respondents, on average, use online and omnichannel to purchase footwear, toys, baby supplies, apparel, and accessories. To capture the opportunity that this shift in Filipino consumer preferences brings and to unlock growth in this sector, retail organizations could turn to omnichannel strategies to seamlessly integrate online and offline channels. Businesses may need to explore investments that increase resilience across the supply chain, alongside researching and developing new products that serve emerging consumer preferences, such as that for natural ingredients and sustainable sources.
Manufacturing
Manufacturing is a key contributor to the Philippine economy, contributing approximately 19 percent of GDP in 2022, employing about 7 percent of the country’s labor force, and growing in line with GDP at approximately 6 percent between 2023 and 2024. 23 McKinsey analysis based on input from industry experts.
Some changes could be seen in 2024 that might affect the sector moving forward. The focus toward building resilient supply chains and increasing self-sufficiency is growing. The Philippines also is likely to benefit from increasing regional trade, as well as the emerging trend of nearshoring or onshoring as countries seek to make their supply chains more resilient. With semiconductors driving approximately 45 percent of Philippine exports, the transfer of knowledge and technology, as well as the development of STEM capabilities, could help attract investments into the sector and increase the relevance of the country as a manufacturing hub. 24 McKinsey analysis based on input from industry experts.
To secure growth, public and private sector support could bolster investments in R&D and upskill the labor force. In addition, strategies to attract investment may be integral to the further development of supply chain infrastructure and manufacturing bases. Government programs to enable digital transformation and R&D, along with a strategic approach to upskilling the labor force, could help boost industry innovation in line with Industry 4.0 demand. 25 Industry 4.0 is also referred to as the Fourth Industrial Revolution. Priority products to which manufacturing industries could pivot include more complex, higher value chain electronic components in the semiconductor segment; generic OTC drugs and nature-based pharmaceuticals in the pharmaceutical sector; and, for green industries, products such as EVs, batteries, solar panels, and biomass production.
Information technology business process outsourcing
The information technology business process outsourcing (IT-BPO) sector is on track to reach its long-term targets, with $38 billion in forecast revenues in 2024. 26 Khriscielle Yalao, “WHF flexibility key to achieving growth targets—IBPAP,” Manila Bulletin , January 23, 2024. Emerging innovations in service delivery and work models are being observed, which could drive further growth in the sector.
The industry continues to outperform headcount and revenue targets, shaping its position as a country leader for employment and services. 27 McKinsey analysis based in input from industry experts. Demand from global companies for offshoring is expected to increase, due to cost containment strategies and preference for Philippine IT-BPO providers. New work setups continue to emerge, ranging from remote-first to office-first, which could translate to potential net benefits. These include a 10 to 30 percent increase in employee retention; a three- to four-hour reduction in commute times; an increase in enabled talent of 350,000; and a potential reduction in greenhouse gas emissions of 1.4 to 1.5 million tons of CO 2 per year. 28 McKinsey analysis based in input from industry experts. It is becoming increasingly more important that the IT-BPO sector adapts to new technologies as businesses begin to harness automation and generative AI (gen AI) to unlock productivity.
Talent and technology are clear areas where growth in this sector can be unlocked. The growing complexity of offshoring requirements necessitates building a proper talent hub to help bridge employee gaps and better match local talent to employers’ needs. Businesses in the industry could explore developing facilities and digital infrastructure to enable industry expansion outside the metros, especially in future “digital cities” nationwide. Introducing new service areas could capture latent demand from existing clients with evolving needs as well as unserved clients. BPO centers could explore the potential of offering higher-value services by cultivating technology-focused capabilities, such as using gen AI to unlock revenue, deliver sales excellence, and reduce general administrative costs.
Sustainability
The Philippines is considered to be the fourth most vulnerable country to climate change in the world as, due to its geographic location, the country has a higher risk of exposure to natural disasters, such as rising sea levels. 29 “The Philippines has been ranked the fourth most vulnerable country to climate change,” Global Climate Risk Index, January 2021. Approximately $3.2 billion, on average, in economic loss could occur annually because of natural disasters over the next five decades, translating to up to 7 to 8 percent of the country’s nominal GDP. 30 “The Philippines has been ranked the fourth most vulnerable country to climate change,” Global Climate Risk Index, January 2021.
The Philippines could capitalize on five green growth opportunities to operate in global value chains and catalyze growth for the nation:
- Renewable energy: The country could aim to generate 50 percent of its energy from renewables by 2040, building on its high renewable energy potential and the declining cost of producing renewable energy.
- Solar photovoltaic (PV) manufacturing: More than a twofold increase in annual output from 2023 to 2030 could be achieved, enabled by lower production costs.
- Battery production: The Philippines could aim for a $1.5 billion domestic market by 2030, capitalizing on its vast nickel reserves (the second largest globally). 31 “MineSpans,” McKinsey, November 2023.
- Electric mobility: Electric vehicles could account for 15 percent of the country’s vehicle sales by 2030 (from less than 1 percent currently), driven by incentives, local distribution, and charging infrastructure. 32 McKinsey analysis based on input from industry experts.
- Nature-based solutions: The country’s largely untapped total abatement potential could reach up to 200 to 300 metric tons of CO 2 , enabled by its biodiversity and strong demand.
The Philippine economy: Three scenarios for growth
Having grown faster than other economies in Southeast Asia in 2023 to end the year with 5.6 percent growth, the Philippines can expect a similarly healthy growth outlook for 2024. Based on our analysis, there are three potential scenarios for the country’s growth. 33 McKinsey analysis in partnership with Oxford Economics.
Slower growth: The first scenario projects GDP growth of 4.8 percent if there are challenging conditions—such as declining trade and accelerated inflation—which could keep key policy rates high at about 6.5 percent and dampen private consumption, leading to slower long-term growth.
Soft landing: The second scenario projects GDP growth of 5.2 percent if inflation moderates and global conditions turn out to be largely favorable due to a stable investment environment and regional trade demand.
Accelerated growth: In the third scenario, GDP growth is projected to reach 6.1 percent if inflation slows and public policies accommodate aspects such as loosening key policy rates and offering incentive programs to boost productivity.
Focusing on factors that could unlock growth in its seven critical sectors and themes, while adapting to the macro-economic scenario that plays out, would allow the Philippines to materialize its growth potential in 2024 and take steps towards achieving longer-term, sustainable economic growth.
Jon Canto is a partner in McKinsey’s Manila office, where Frauke Renz is an associate partner, and Vicah Villanueva is a consultant.
The authors wish to thank Charlene Chua, Charlie del Rosario, Ryan delos Reyes, Debadrita Dhara, Evelyn C. Fong, Krzysztof Kwiatkowski, Frances Lee, Aaron Ong, and Liane Tan for their contributions to this article.
Explore a career with us
Related articles.

The Philippines Growth Dialogues

What does 2023 hold for the Philippines’ economy?

On the verge of a digital banking revolution in the Philippines

IMAGES
COMMENTS
The cost of health care in the United States far exceeds that in other wealthy nations across the globe. In 2020, U.S. health care costs grew 9.7%, to $4.1 trillion, reaching about $12,530 per person. 1 At the same time, the United States lags far behind other high-income countries when it comes to both access to care and some health care ...
Health Care Spending in America Essay. Healthcare spending growth rate trends show astounding estimates. Since 1960, spending has risen from $27 billion ($143 per capita, 5.1% pf GDP) to amazing $1,678.9 billion ($5,670 per capita, 15.3% of GDP, 2003 data) (HHS, 2005).
Denisha Cook HLT- 06/01/ Professor Maria Nunes Health Care Cost, Access and Affordability Healthcare cost has been an ongoing issue in the United States for generations but aside from the cost of healthcare being a problem there are other problems that the healthcare sector face such as access to healthcare as well as the quality of healthcare being provided.
In her 2016 essay "Cost of Living" for the Virginia Quarterly Review — later anthologized in The Best American Essays — Emily Maloney unravels the juxtaposition of working to pay down her ...
Photo: Sam Edwards / Getty Images. In 2020, U.S. health care costs totaled $4.1 trillion. That makes health care one of the country's largest expenses. Health spending accounted for 19.7% of the nation's gross domestic product (GDP). In comparison, national health expenditures totaled $27.2 billion in 1960, just 5% of GDP.
Reducing Health Care Costs Full-Scale. Executives of major companies, like Coca-Cola Enterprises in Atlanta, believed that -200 was especially helpful in rehabilitation and prevention of re-injury, as employees usually resumed work when their backs stopped hurting, thinking the injury was already treated.
Life-saving items such as cardiac defibrillators typically cost more than $20,000, while higher complexity models can cost roughly $40,000. Common items like artificial knees and hips often cost in excess of $5,000. Hospitals are also investing in new technologies and improving how care is delivered. In 2017 alone, hospitals invested more than ...
The impact of prescription drug access on healthcare costs. Every year since 2006, the cost of prescription drug prices has increased at a rate that far exceeds the general inflation rate, according to a report by AARP.Between 2019 and 2020, that increase was more than three times higher than general inflation at 4.8% versus 1.3%.
Spending on health care is central to the long-term budgetary challenges. So it is especially useful to pair their essay with David Cutler's nuanced explanations of why American health care costs so much: about $3.5 trillion per year (that's the norm, before an emergency like COVID-19)—of which one-third is wasted.
Jama, 318 (6), 508-509. Healthcare costs for Americans projected to grow at an alarmingly high rate. (2019). Web. This essay, "The Issue of Rising Medical Costs" is published exclusively on IvyPanda's free essay examples database. You can use it for research and reference purposes to write your own paper.
Adults in households with annual incomes under $40,000 are more than three times as likely as adults in households with incomes over $90,000 to say it is difficult to afford their health care ...
Healthcare Cost Essay. Health Care Systems and Transcultural Health Care 100% (6) 4. HLT-205 assignment 1 (Timeline) Health Care Systems and Transcultural Health Care 100% (5) More from: Health Care Systems and Transcultural Health Care HLT-205. Grand Canyon University. 130 Documents. Go to course. 6.
In February 2013, Time magazine published an exposé on health care costs, "Bitter Pill: Why Medical Bills are Killing Us," by journalist Stephen Brill [9]. Shortly after, the then-Secretary of the Department of Health and Human Services, Kathleen Sebelius, took the unprecedented step of making available online the 2011 chargemaster prices ...
Health Care: Cost, Access, Quality, and the Role Technology Plays. Samantha Watson Grand Canyon University HLT- Jessie Kernagis April 24, 2022. Introduction "A new study finds that the cost of health care in the United States increased nearly $ trillion from 1996 to 2013" (2020). The cost of healthcare in the United States has been slowly rising for decades.
The United States spends an extraordinary amount of money on health care. n 2009, health spending was $2.47 trillion dollars and accounted for 17.3% of the U.S. economy in 2009 (Pickert, 2010). This was a significant increase over the 2008 figure of $2.34 trillion and "was the largest one-year jump since 1960" (Pickert, 2010).
In the United States in 2012, the cost of healthcare per person averaged about $9000 per year. In 2012, data from CMS stated that the total spending on healthcare in 2012 was $2.8 trillion (1). Despite competition in the health care field, two of the very prominent reasons for high costs are high administrative costs, the use of costly new ...
The average American now spends close to $13,000 a year on healthcare, and the costs are still rising. But why? ... These include white papers, government data, original reporting, and interviews ...
Escalating Costs. The cost of health care in the United States has been steadily increasing over the past few decades. According to the Centers for Medicare and Medicaid Services, national health care spending reached $3.8 trillion in 2019, accounting for 17.7% of the country's Gross Domestic Product (GDP).
Essays.io ️ Health Care in the United States, Essay Example from students accepted to Harvard, Stanford, and other elite schools ... What cannot be disputed is that the cost of healthcare is constantly rising, a fact which was the precipitant to the large movement to reform healthcare in our country in 2010. More than 10 years ago, the goal ...
on health care costs. Speci fi cally, the study found billing costs represented 14.5% of professional revenue for primary care visits, 25.2% for emergency room visits, 8% for general medi-
Amy Olsen HLT 205 June 8, 2019 Maria Nunes Health Care Essay: Cost, Access, and Quality In today's world all Americans want the very best quality healthcare at their disposal and at the very least amount of money. However, nobody thinks about what the bottom line is, or who is the one pay for it. People want it and they want it now.
Download. Essay, Pages 5 (1003 words) Views. 1507. The United States of America has been struggling to resolve the issues of its health care system for decades now. Looking at the history of previous policies, all issues have stemmed from one major common factor, the cost of health care. With cost at an all-time high, the quality of and access ...
Here are some great healthcare argumentative essay topics to get you started: 1. Should the government provide free or low-cost healthcare to all citizens? 2. Is private healthcare better than public healthcare? 3. Should there be more regulation of the healthcare industry? 4. Are medical costs too high in the United States? 5.
Asset-based approaches (ABAs) tackle health inequalities by empowering people in more disadvantaged communities, or targeted populations, to better utilise pre-existing local community-based resources. Using existing resources supports individuals to better manage their own health and its determinants, potentially at low cost. Targeting individuals disengaged with traditional service delivery ...
Investing in comprehensive water supply, sanitation, and hygiene and health care waste management can yield substantial benefits, with a benefit-cost ratio of 5.8 for all economic costs. Beyond preventing health care-associated infections, improved cleanliness and infrastructure are crucial for patient satisfaction, impacting future health ...
The ability to access health care influences the cost, as well as does the quality of that health care treatment and the technology used, all these factors have a significant impact on one another when it comes to overall health care treatment. The Cost of Health Care The cost to receive health care treatment in the United States began rising ...
The decline in mental health is just one of many signs that something went awry. Loneliness and friendlessness among American teens began to surge around 2012. Academic achievement went down, too.
The Philippines ended 2023 on a high note, being the fastest growing economy across Southeast Asia with a growth rate of 5.6 percent—just shy of the government's target of 6.0 to 7.0 percent. 1 "National accounts," Philippine Statistics Authority, January 31, 2024; "Philippine economic updates," Bangko Sentral ng Pilipinas, November 16, 2023. ...